Reproductive System Male Reproductive System The Scrotum Sac












- Slides: 63
Reproductive System
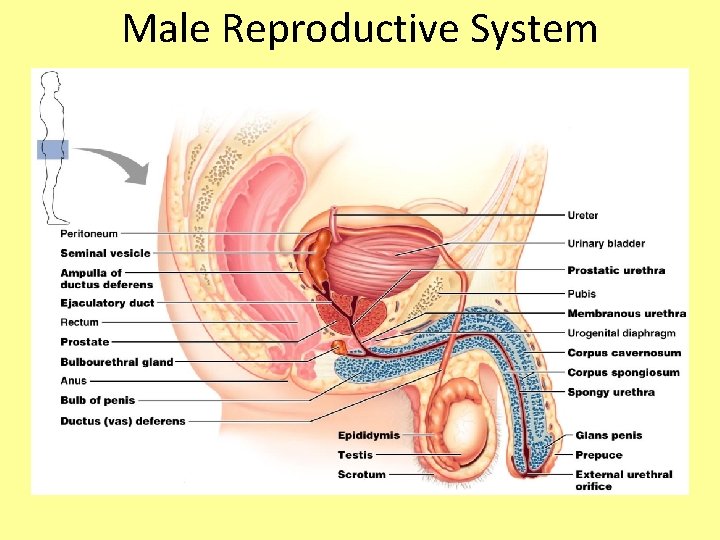
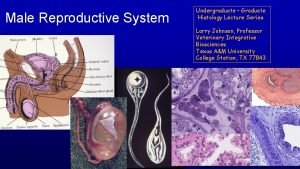
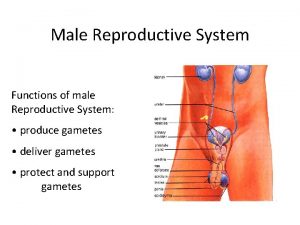
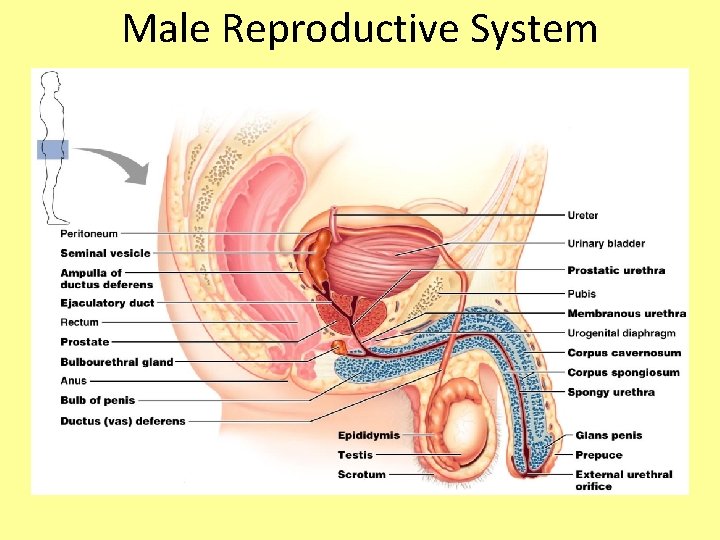
Male Reproductive System
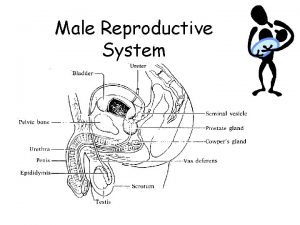
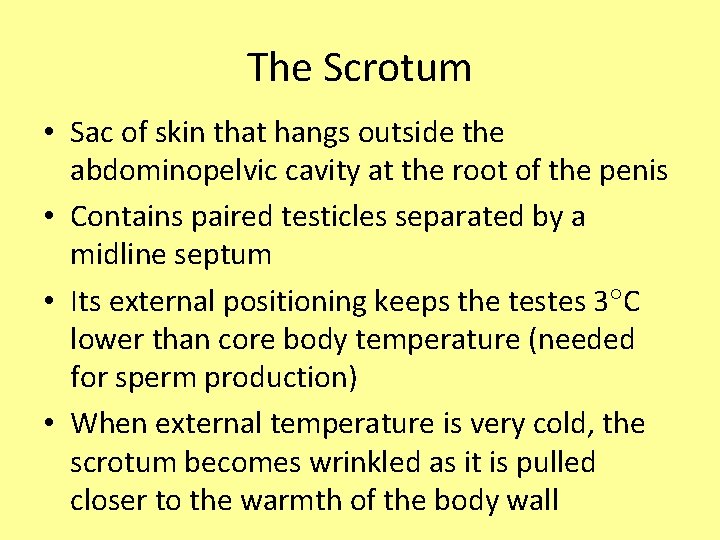
The Scrotum • Sac of skin that hangs outside the abdominopelvic cavity at the root of the penis • Contains paired testicles separated by a midline septum • Its external positioning keeps the testes 3 C lower than core body temperature (needed for sperm production) • When external temperature is very cold, the scrotum becomes wrinkled as it is pulled closer to the warmth of the body wall
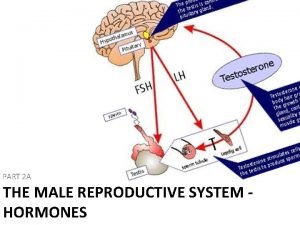
The Testes • Each testis is divided into 250 -300 lobules, each containing 1 -4 seminiferous tubules • Seminiferous tubules produce the sperm stimulated by FSH released by pituitary • Interstitial cells around the tubules produce androgens (testosterone) – stimulated by LH released by pituitary • Once the sperm are made, they continue to the epididymis

The Testes
The Epididymis • First part of male duct system • Provides a temporary storage site for the immature sperm cells – Trip through takes about 20 days – Sperm learn how to swim here! • When a male is sexually stimulated, the walls of the epididymis contract to propel sperm into the ductus deferens
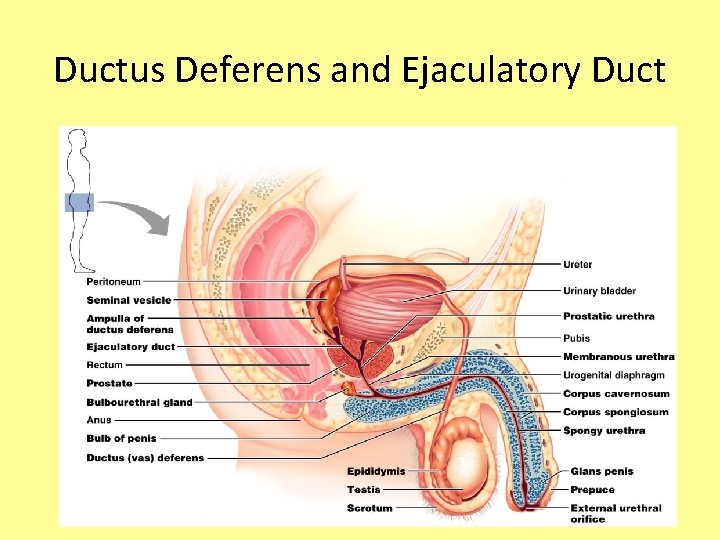
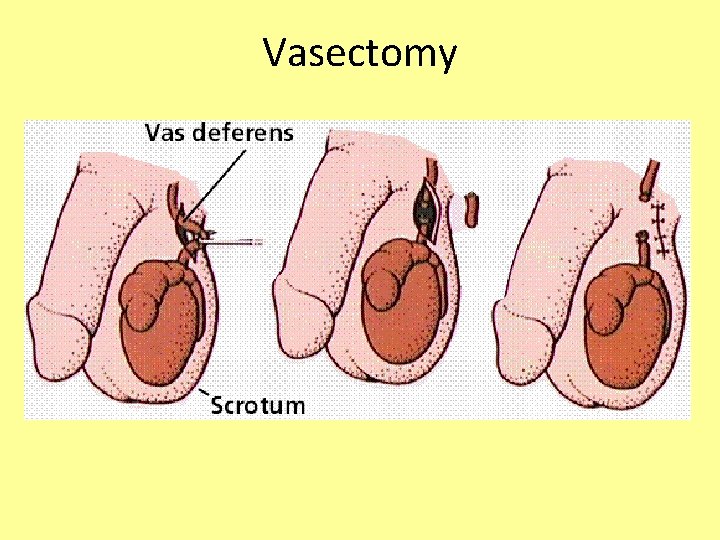
Ductus Deferens and Ejaculatory Duct • Propels sperm from the epididymis up into the pelvis, and back down to join up with the urethra • Also called the vas deferens • During an ejaculation, smooth muscles around the duct contract to create peristaltic waves that squeeze the sperm forward • Vasectomy – cutting and ligating the ductus deferens, which is a nearly 100% effective form of birth control
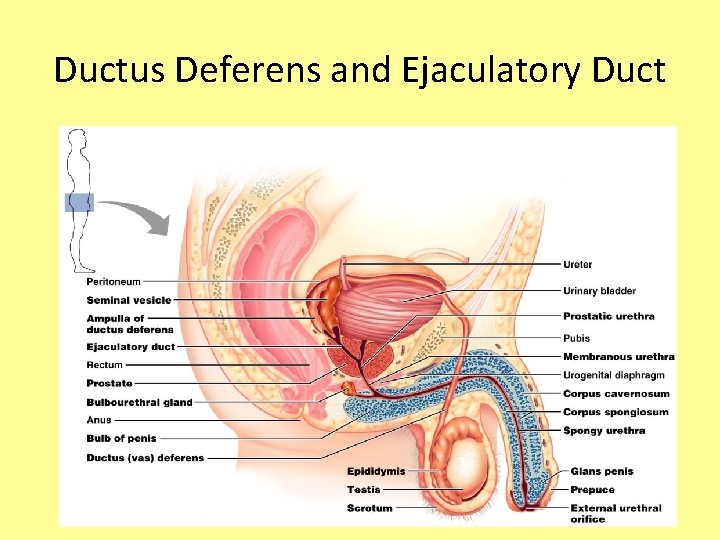
Ductus Deferens and Ejaculatory Duct
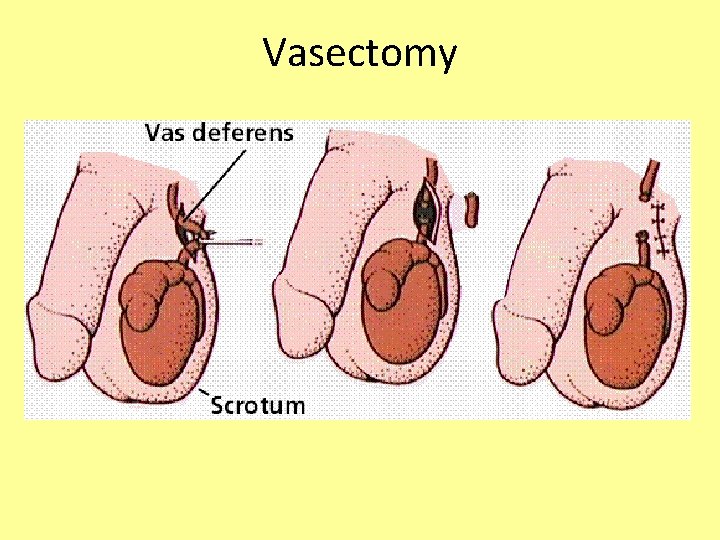
Vasectomy
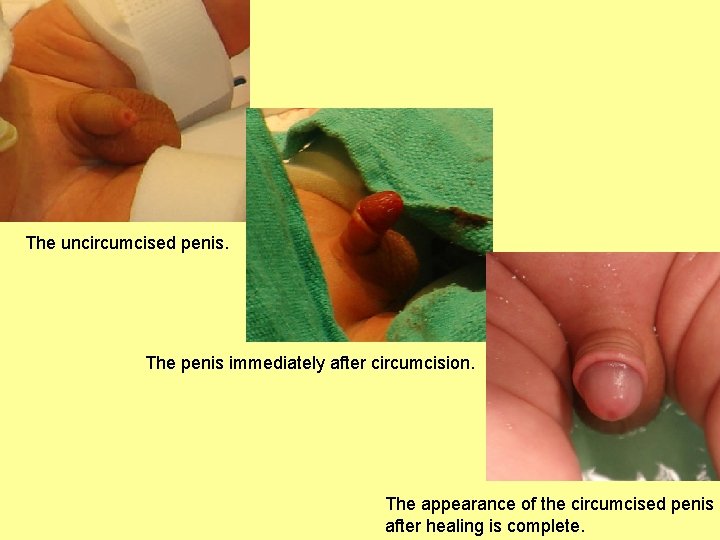
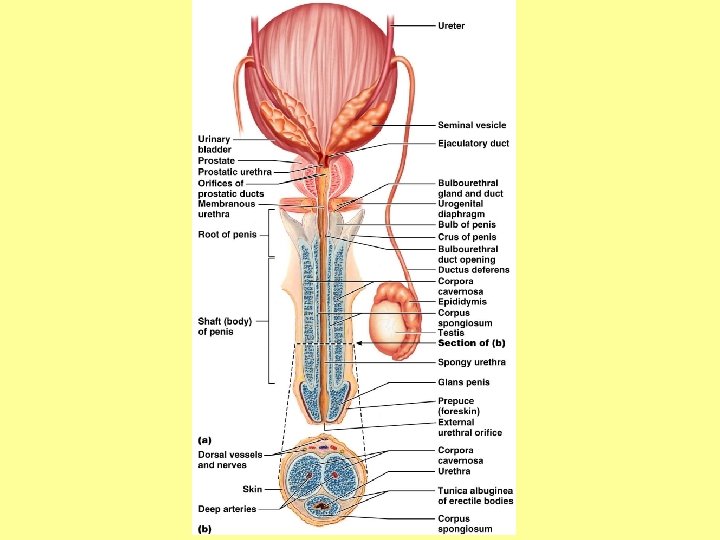
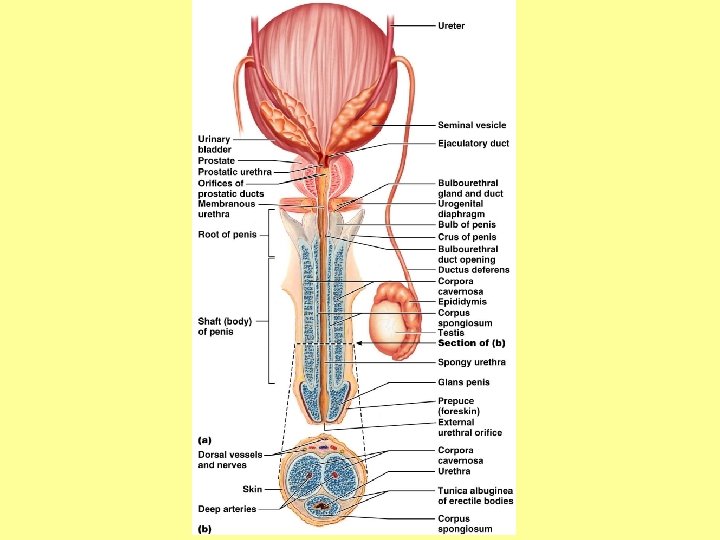
The Penis • A copulatory organ designed to deliver sperm into the female reproductive tract • Consists of an attached root and a free shaft that ends in the glans penis • Prepuce, or foreskin – cuff of skin covering the distal end of the penis – Circumcision – surgical removal of the foreskin after birth
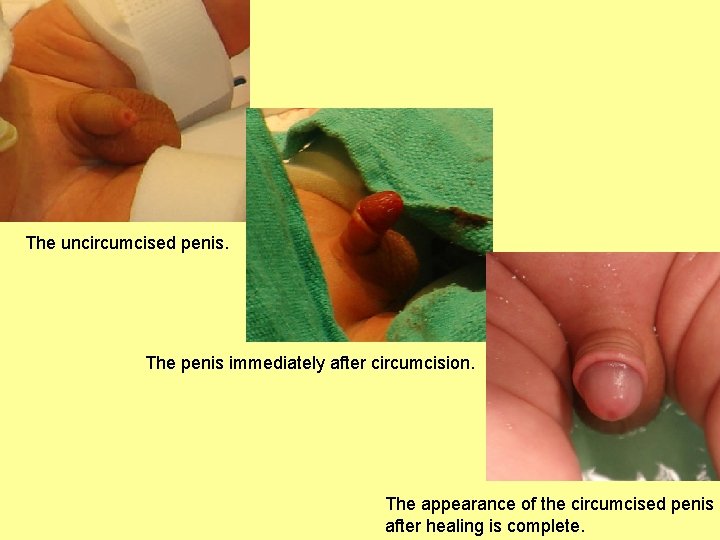
The uncircumcised penis. The penis immediately after circumcision. The appearance of the circumcised penis after healing is complete.
The Penis • Internal penis includes the urethra (which carries both semen and urine) and three cylindrical bodies of erectile tissue • Erectile tissue – spongy network of connective tissue and smooth muscle riddled with vascular spaces; assists with erection and ejaculation • Erection – during sexual excitement, the erectile tissue fills with blood causing the penis to enlarge and become rigid (which makes penetration easier)
The Penis
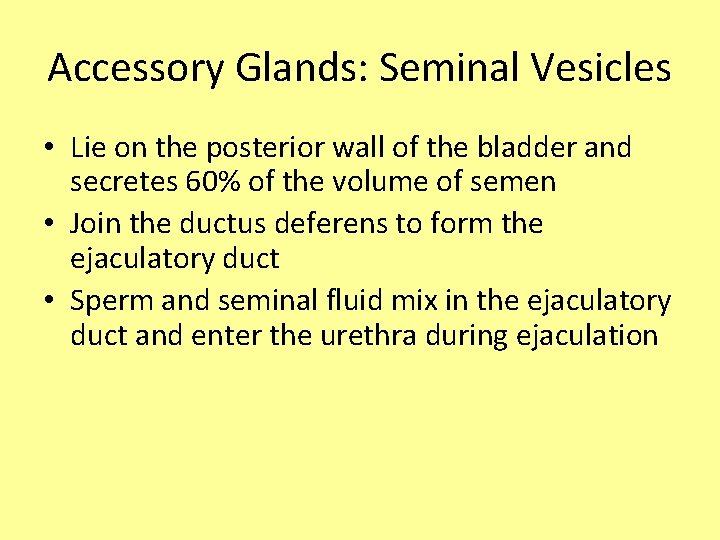
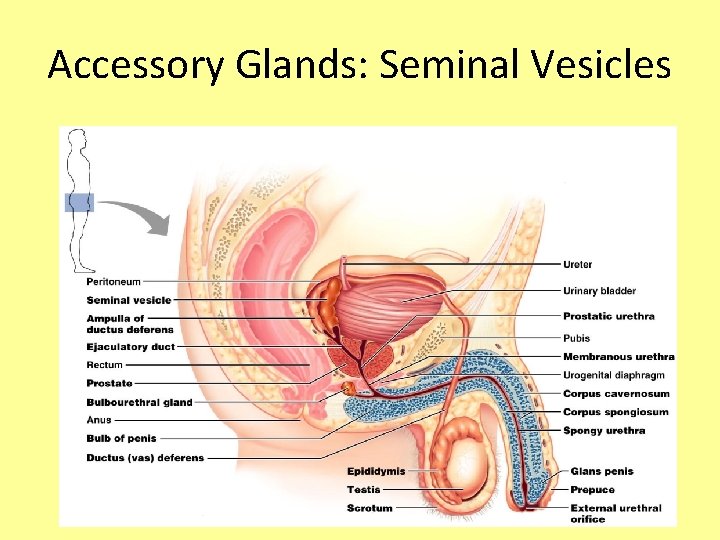
Accessory Glands: Seminal Vesicles • Lie on the posterior wall of the bladder and secretes 60% of the volume of semen • Join the ductus deferens to form the ejaculatory duct • Sperm and seminal fluid mix in the ejaculatory duct and enter the urethra during ejaculation
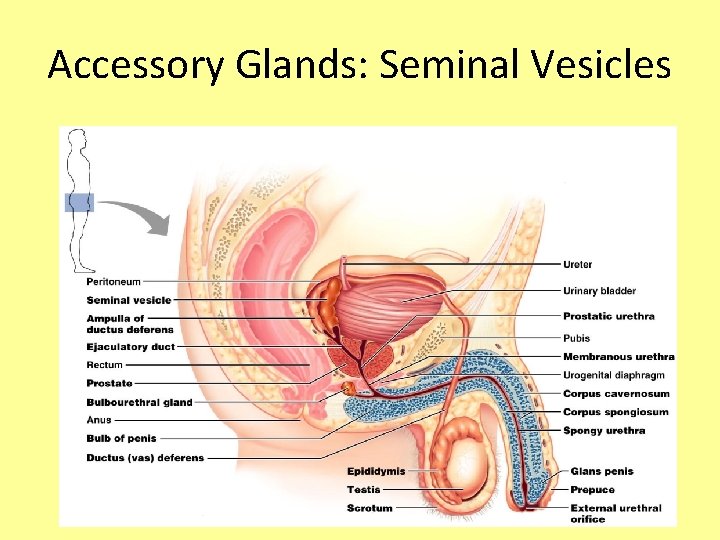
Accessory Glands: Seminal Vesicles

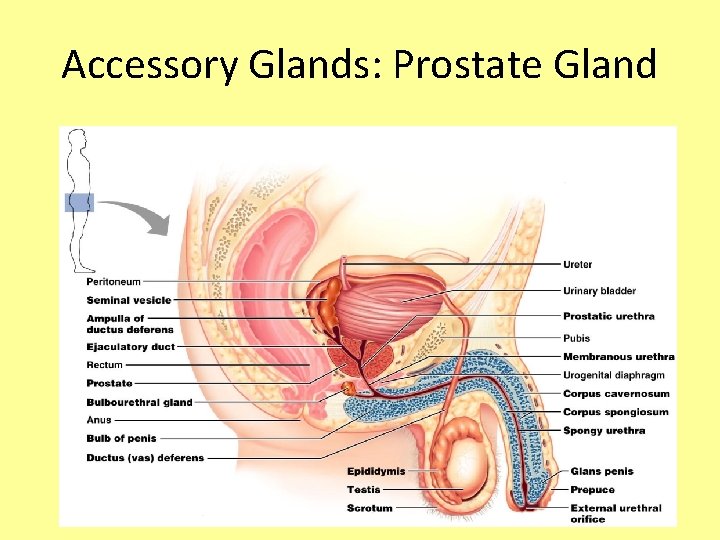
Accessory Glands: Prostate Gland • Doughnut-shaped gland that encircles part of the urethra inferior to the bladder • Its milky fluid, which contains citrate (Vitamin C), enzymes, and prostate-specific antigen (PSA), accounts for one-third of the semen volume • Fluid helps to activate sperm • Fluid made enters the urethra during ejaculation
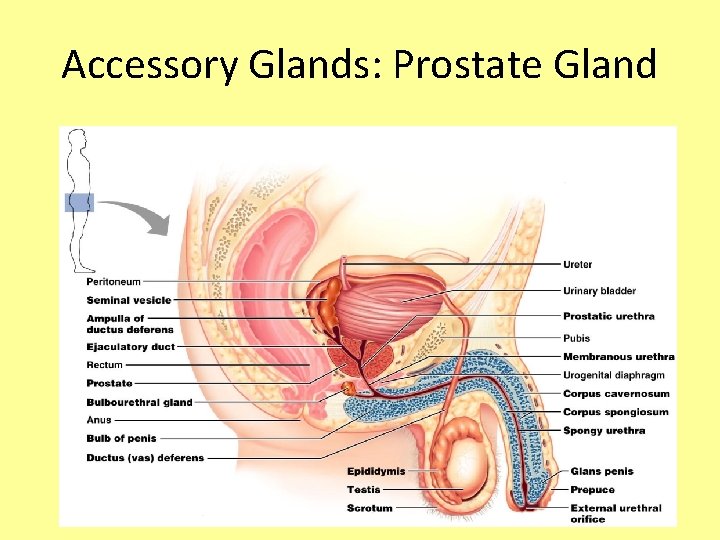
Accessory Glands: Prostate Gland
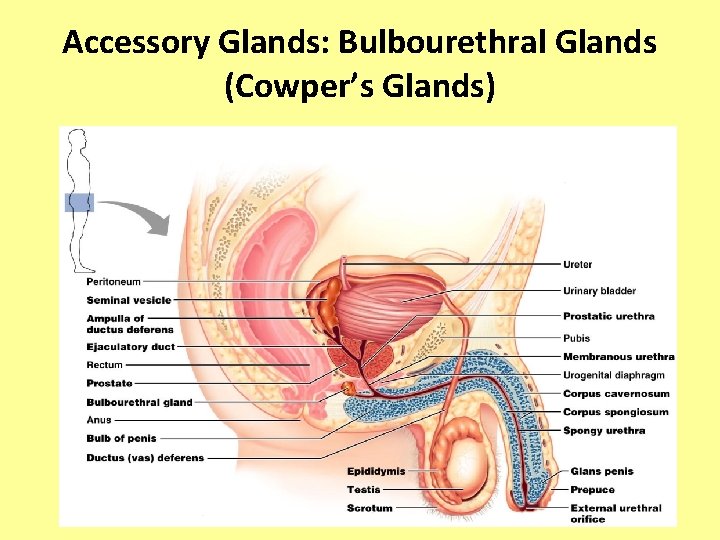
Accessory Glands: Bulbourethral Glands (Cowper’s Glands) • Pea-sized glands inferior to the prostate • Produce thick, clear mucus prior to ejaculation that neutralizes traces of acidic urine in the urethra
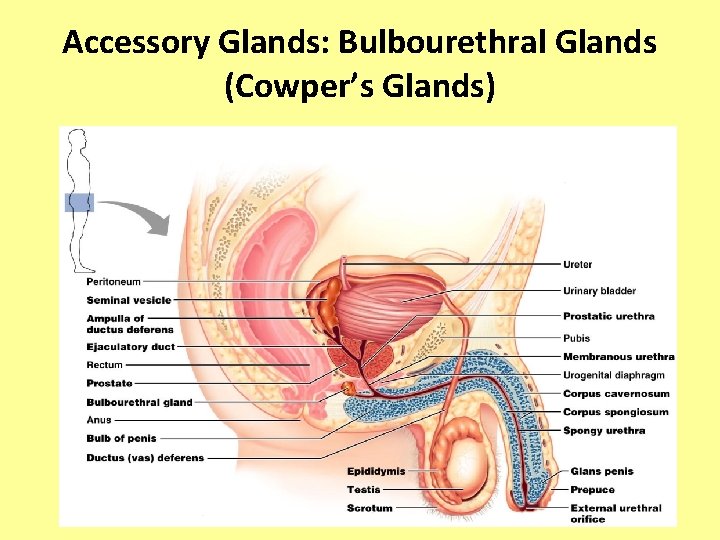
Accessory Glands: Bulbourethral Glands (Cowper’s Glands)
Semen • Milky white, sticky mixture of sperm and accessory gland secretions • Provides a transport medium and nutrients (fructose), protects and activates sperm, and facilitates their movement • Prostaglandins in semen: – Decrease the viscosity of mucus in the cervix – Stimulate reverse peristalsis in the uterus – Facilitate the movement of sperm through the female reproductive tract
Semen • Sperm are most active at neutral p. H, and can even die off at p. H of 4 and below! • However, vaginal p. H is normally 3. 5 -3. 9! • Seminal fluid and prostate gland fluid has a p. H of 7. 27. 6, which will help to neutralize out the vagina… but this doesn’t last forever! • p. H in vagina will drop back down to 4. 0 within 8 hours – so the lifetime of sperm in the vaginal canal is 8 hours max; lifetime in the uterus and fallopian tubes is about 48 hours • Only 2 -5 m. L of semen are ejaculated, but it contains 50 -130 million sperm per m. L
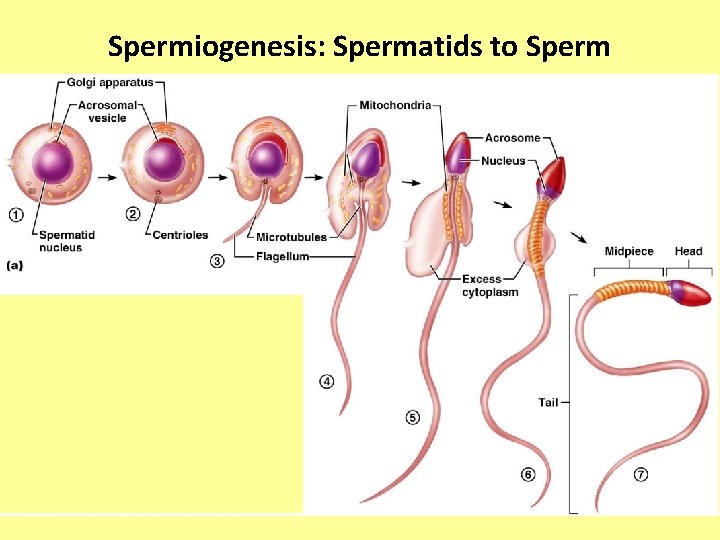
Sperm • Sperm have three major regions – Head – contains DNA and has a helmetlike acrosome containing hydrolytic enzymes that allow the sperm to penetrate and enter the egg – Midpiece – contains mitochondria spiraled around the tail filaments – Tail – a typical flagellum produced by a centriole
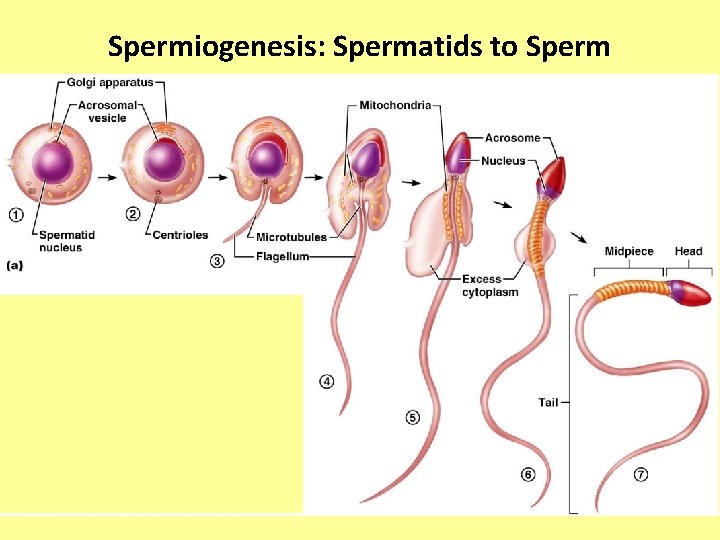
Spermiogenesis: Spermatids to Sperm

Secondary Male Characteristics • Deeper voice due to enlarged larynx • Increased hair growth over body, especially in axillary and pubic regions, as well as on face • Enlargement of skeletal muscles • Increased heaviness of bones • Long, narrow pelvis • All are due to testosterone levels
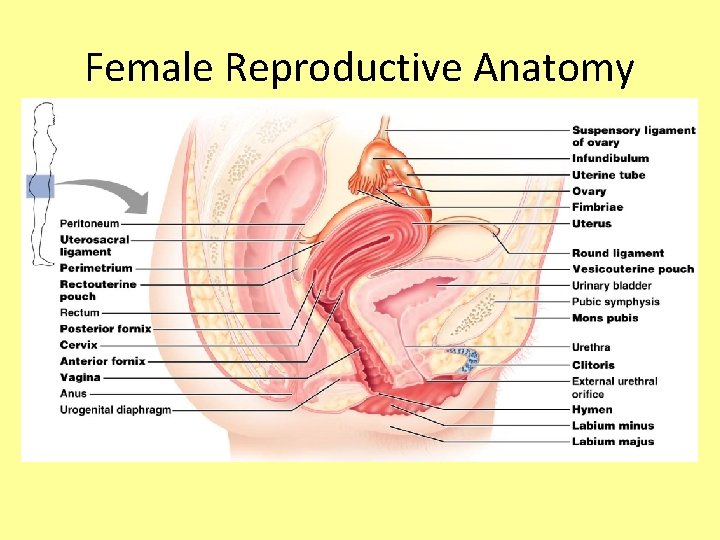
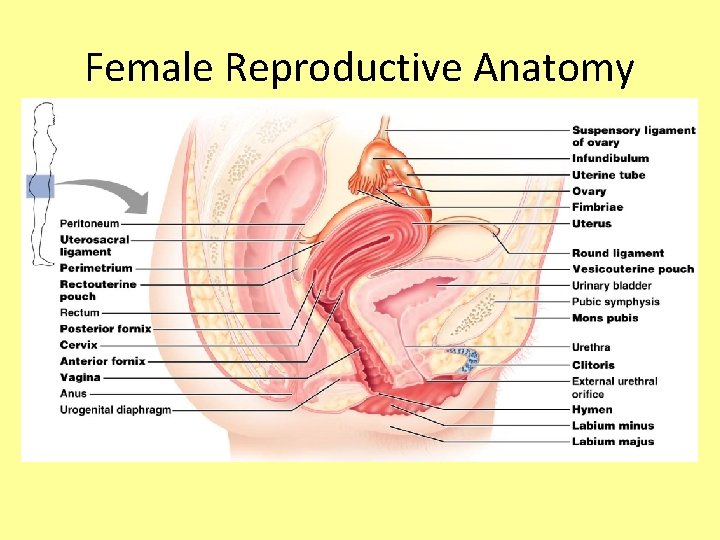
Female Reproductive Anatomy
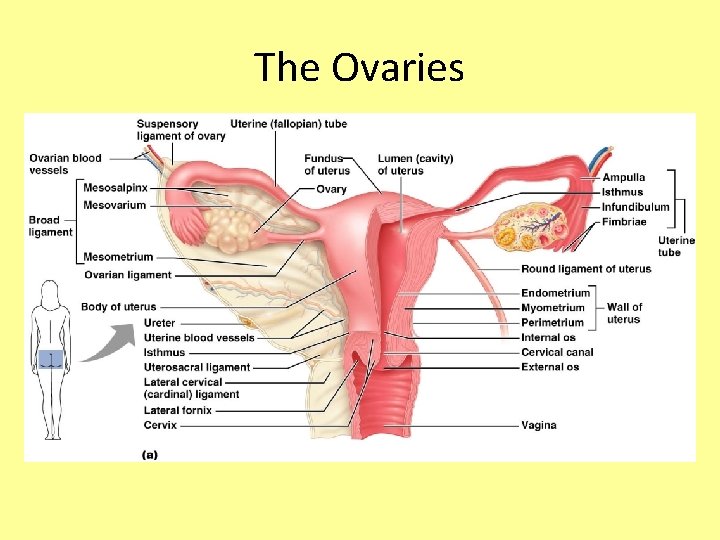
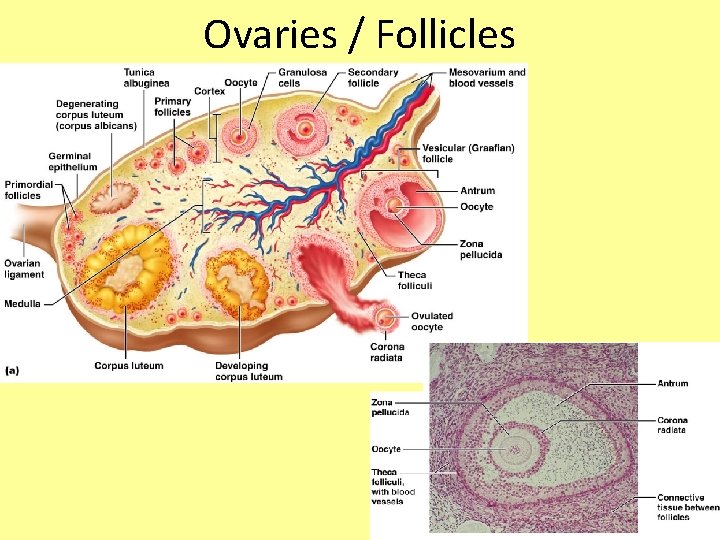
The Ovaries • Paired organs on each side of the uterus held in place by several ligaments • About the size & shape of almonds • Embedded in the ovary are follicles
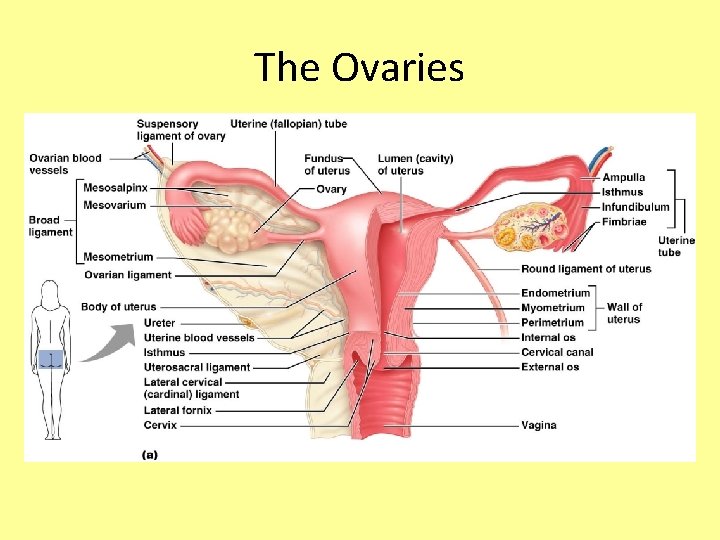
The Ovaries
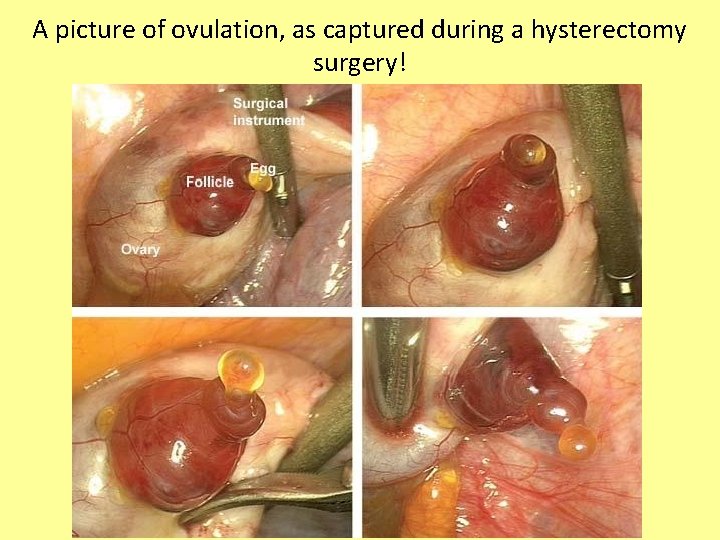
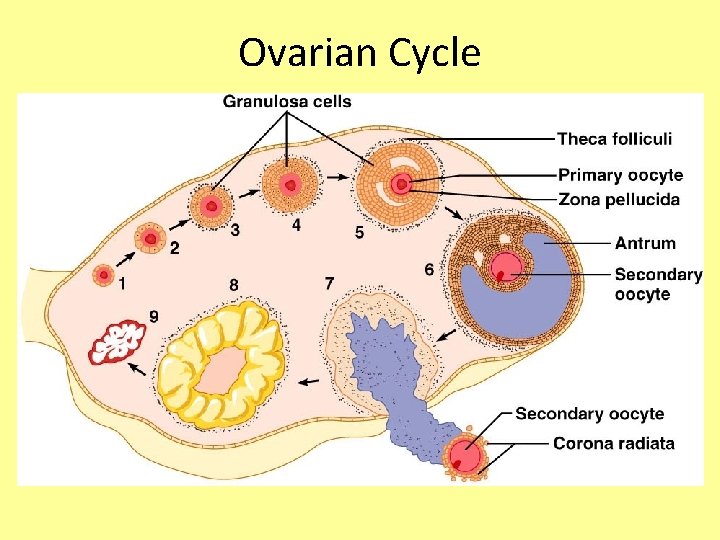
Follicles • Each follicle consists of an immature egg called an oocyte • Oocytes are surrounded by layers of follicle cells, which will mature – because of FSH released from pituitary • When follicle is mature, the developing egg (ova) will be released (ovulation) – stimulated by LH released from pituitary • After ovulation, the ruptured follicle is called a corpus luteum, which eventually degenerates
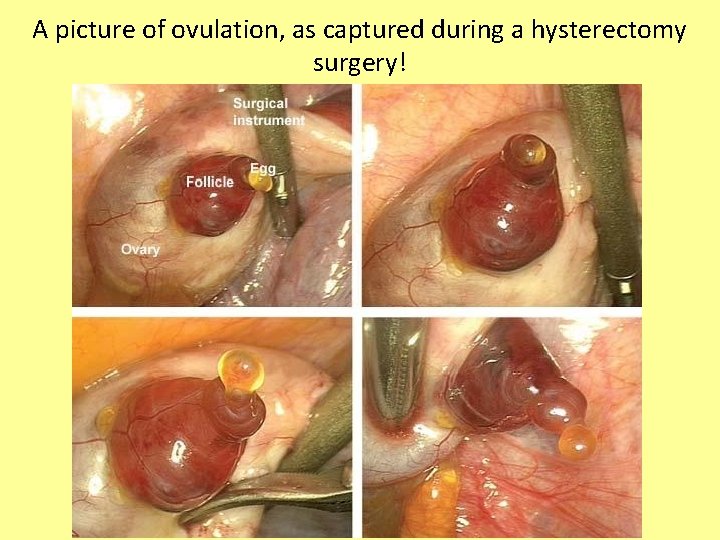
A picture of ovulation, as captured during a hysterectomy surgery!
A note about oocytes… • Females are born with approximately 700, 000 oocytes at birth combined in the two ovaries… this is the lifetime supply, and no more will develop • The number already decreases down to 400, 000 by puberty, and only about 500 eggs will be released during a woman’s lifetime • This is different than in the males, where sperm continue to be produced throughout the reproductive lifetime
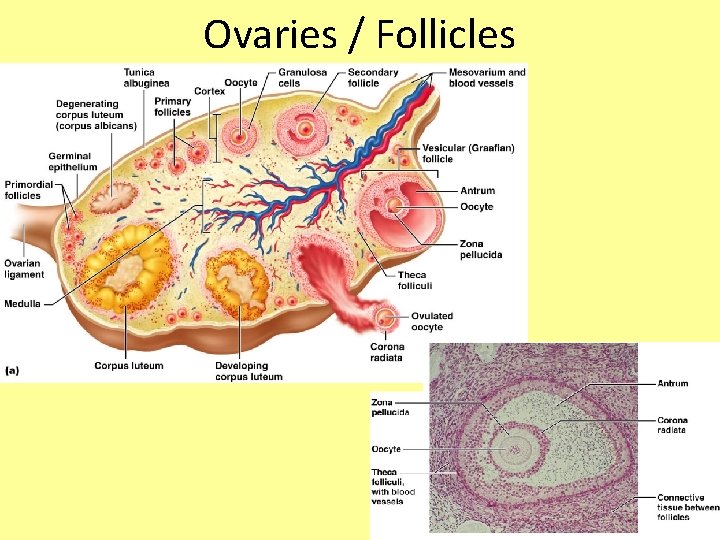
Ovaries / Follicles
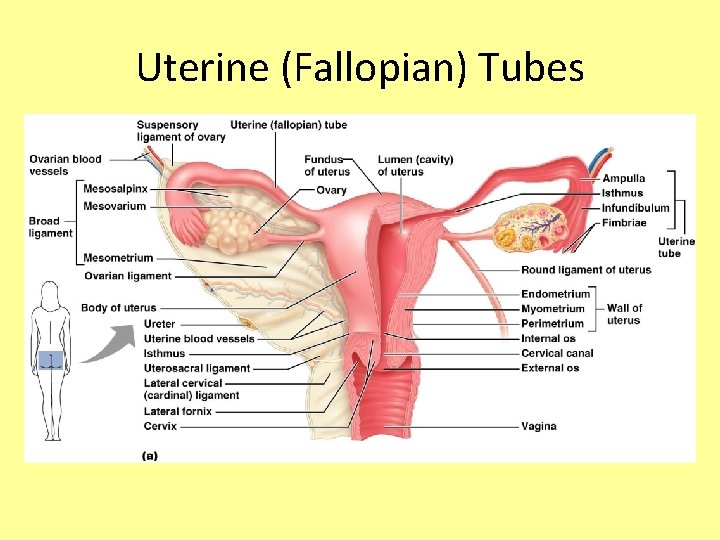
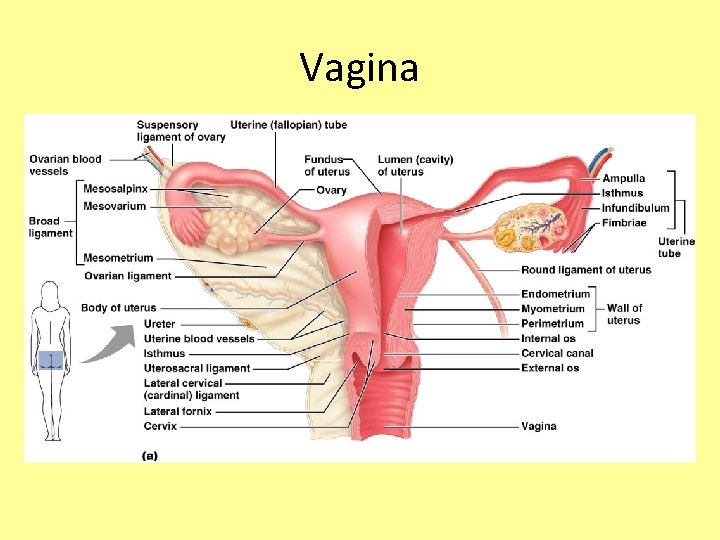
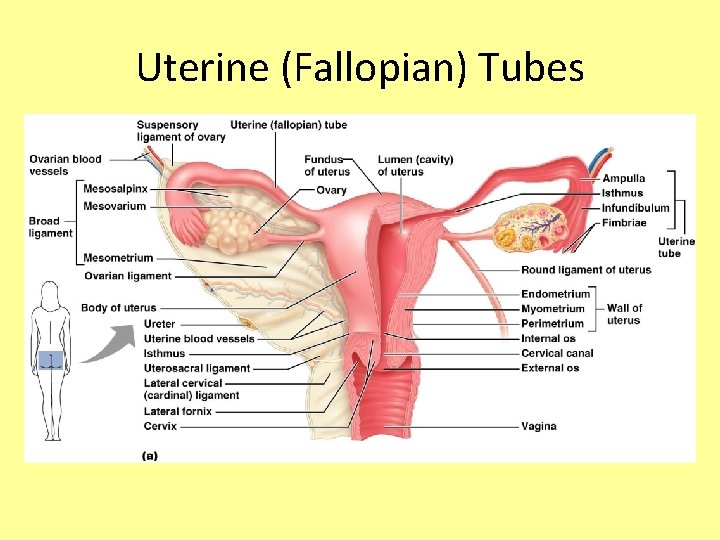
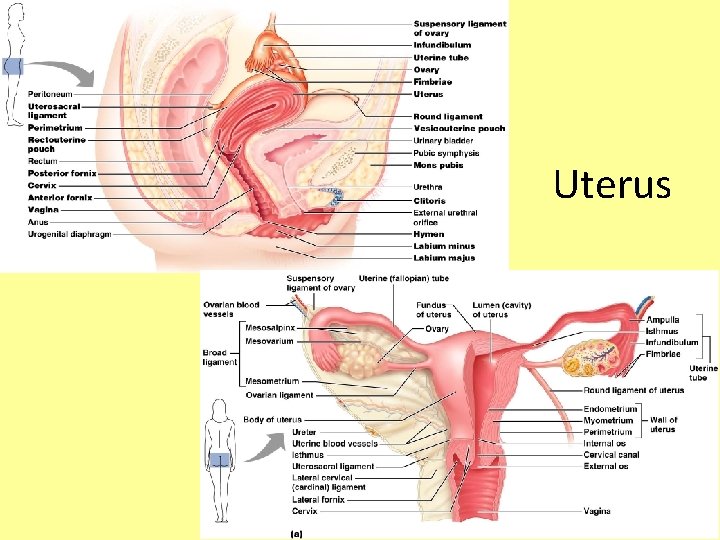
Uterine (Fallopian) Tubes • Each tube is about 10 cm long and 1 cm in diameter • Allows egg (ova) to travel from ovary to uterus • Usually the site of fertilization • End of tube near the ovary expands to form a funnel-shaped infundibulum, which has fingerlike extensions (fimbriae)
Uterine (Fallopian) Tubes • The uterine tubes have no contact with the ovaries and the ovulated ovais cast into the peritoneal cavity • Beating cilia on the fimbriae create currents to carry the ova into the uterine tube • The ova is carried toward the uterus by peristalsis and ciliary action
Uterine (Fallopian) Tubes

Ectopic Pregnancy • While ova get fertilized in the uterine tubes, the egg should not implant here! • If the egg is implanted anywhere other than the uterus, this is called an ectopic pregnancy • 98% of ectopic pregnancies occur in the uterine tubes • Most will resolve themselves naturally through a miscarriage, but sometimes surgery is required to remove the fetus or internal bleeding can occur

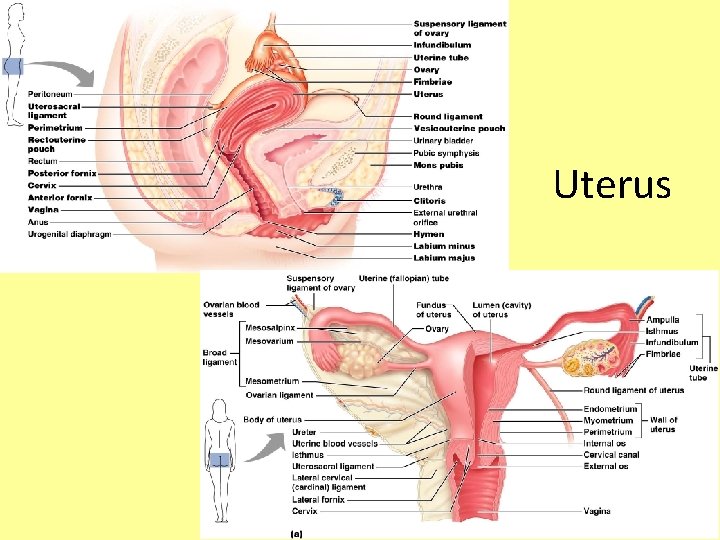
Uterus • Hollow, thick-walled organ located in the pelvis anterior to the rectum and posterosuperior to the bladder • Where implantation of fertilized ova occurs • About the size and shape of a pear • Body – major portion of the uterus • Fundus – rounded region superior to the entrance of the uterine tubes • Cervix – narrow neck which projects into the vagina inferiorly
Uterus
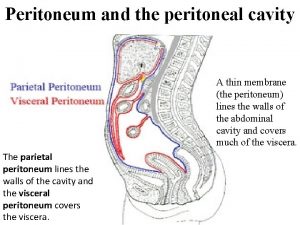
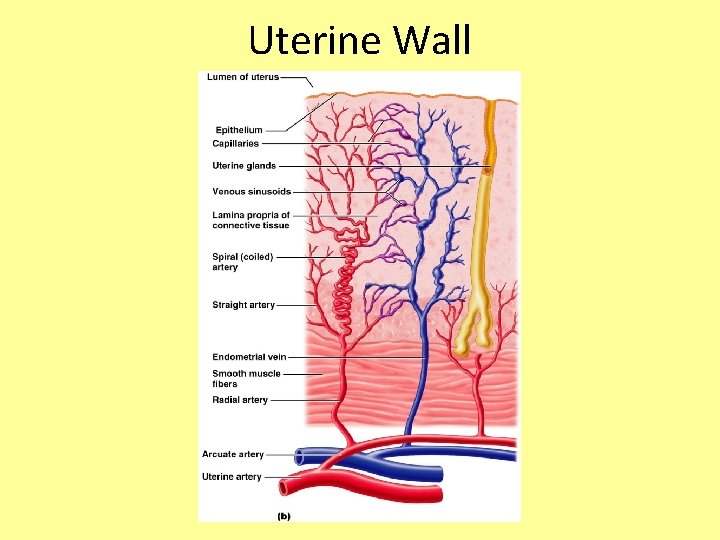
Uterine Wall • Wall composed of three layers – Perimetrium – outermost serous layer; the visceral peritoneum – Myometrium – middle layer; interlacing layers of smooth muscle; contracts during childbirth – Endometrium – mucosal lining of the uterine cavity
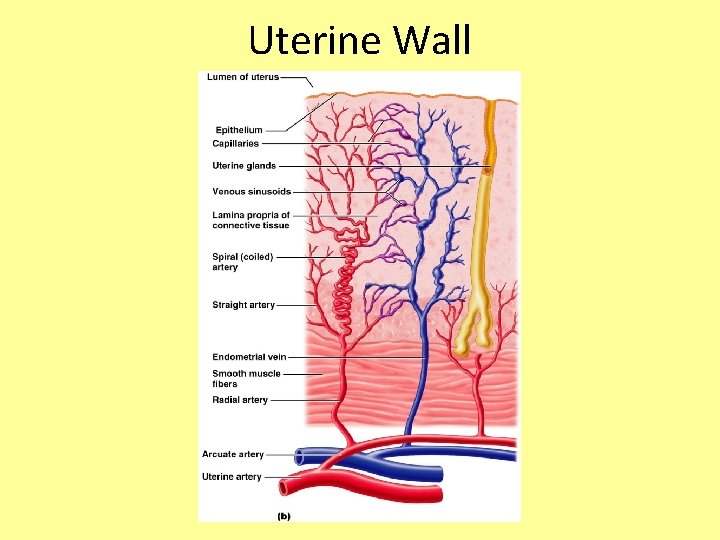
Uterine Wall
Endometrium • If fertilization occurs, the fertilized egg burrows into the endometrium and resides there for the rest of development • When a woman is not pregnant, the endometrial lining sloughs off periodically (approximately every 28 days) in response to hormone levels
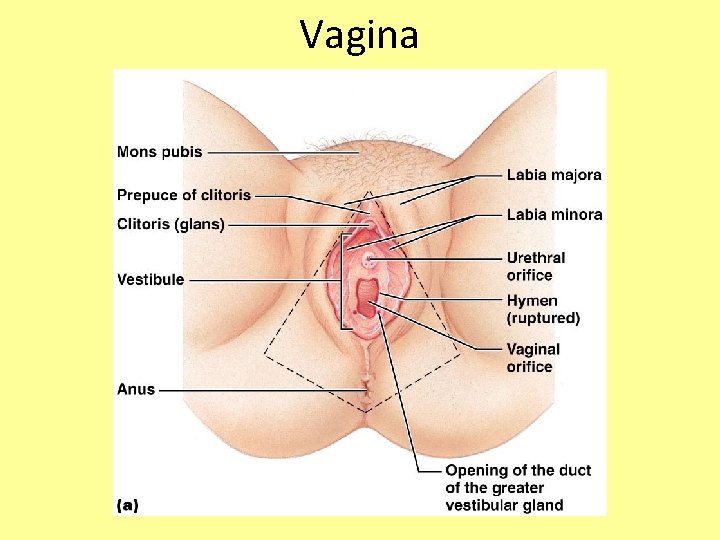
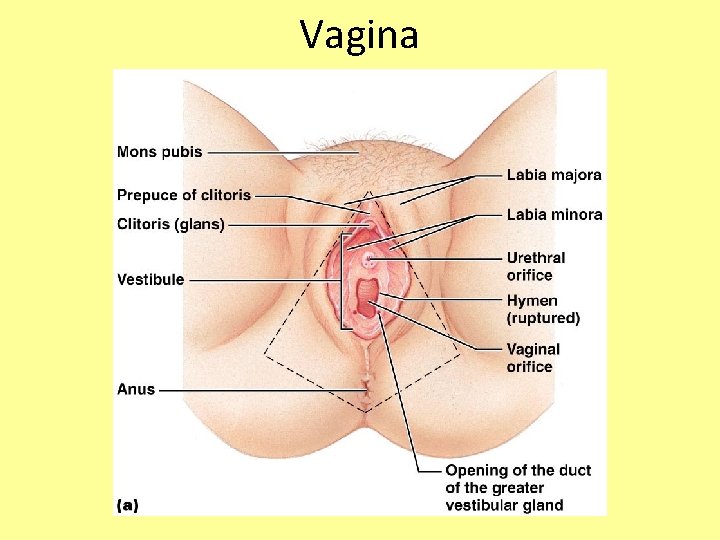
Vagina • Thin-walled tube about 3 to 4 inches long extending from the cervix to the exterior of the body • The urethra is embedded in the anterior wall • Provides a passageway for male penetration, birth, and menstrual flow • The labial folds protect the vaginal opening and the urethral opening
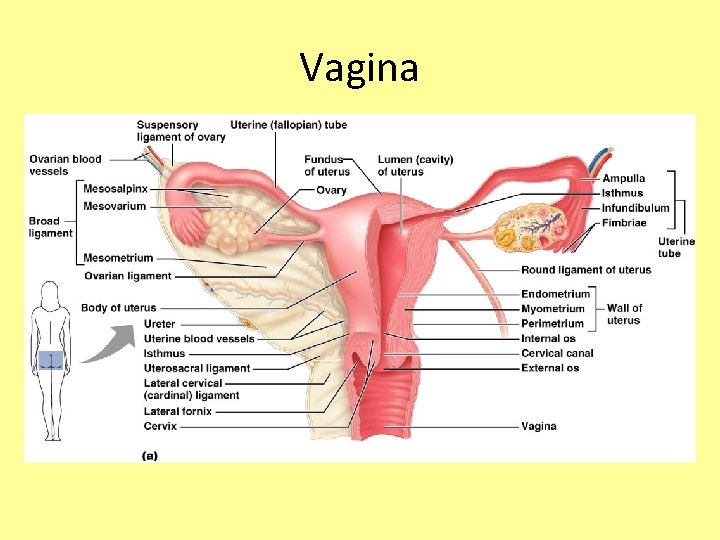
Vagina
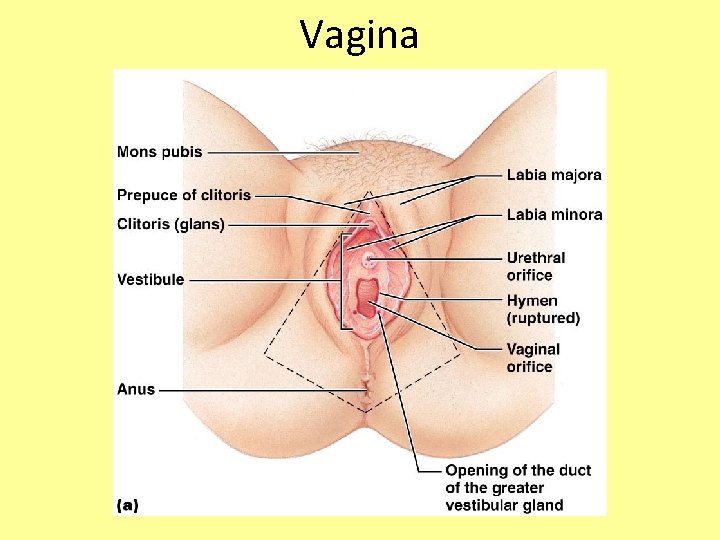
Vagina
External Genitalia • Clitoris (homologous to the penis) – Erectile tissue that become swollen with blood during sexual excitement • Greater vestibular glands – Secretions lubricate the distal end of the vagina during intercourse
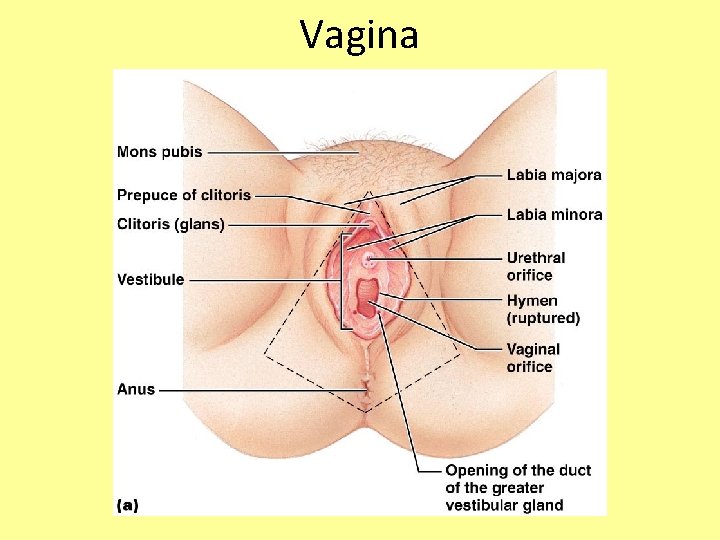
Vagina
Monthly Female Cycles • Include the Ovarian Cycle and the Menstrual Cycle
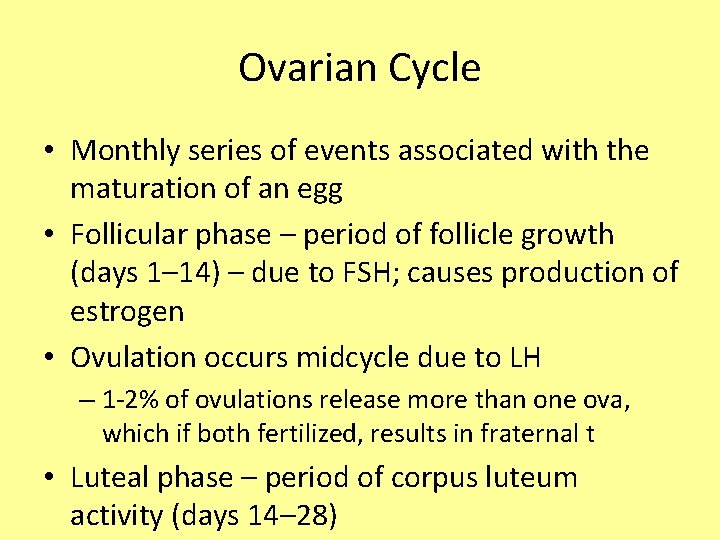
Ovarian Cycle • Monthly series of events associated with the maturation of an egg • Follicular phase – period of follicle growth (days 1– 14) – due to FSH; causes production of estrogen • Ovulation occurs midcycle due to LH – 1 -2% of ovulations release more than one ova, which if both fertilized, results in fraternal t • Luteal phase – period of corpus luteum activity (days 14– 28)
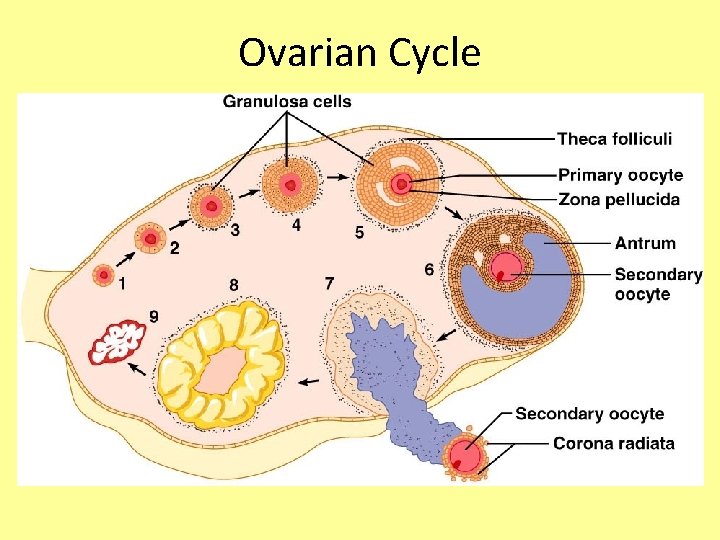
Ovarian Cycle
Luteal Phase • The corpus luteum secretes progesterone and estrogen • If pregnancy does not occur, the corpus luteum degenerates in 10 days and levels of progesterone and estrogen will decrease • If pregnancy does occur, the corpus luteum continues to produces hormones until the placenta takes over that role (at about 3 months)

Uterine (Menstrual) Cycle • Series of cyclic changes that the uterine endometrium goes through each month in response to ovarian hormones in the blood
Uterine (Menstrual) Cycle • Days 1 -5: Menstrual (Menses) Phase – uterus sheds all but the deepest part of the endometrium • Days 4 -14: Proliferative (Follicular) Phase – endometrium rebuilds itself due to rising estrogen levels (released from growing follicles) • Days 15 -28: Secretory (Luteal) phase – endometrium prepares for implantation of the embryo by increasing blood flow and nutrients due to rising progesterone levels (released from corpus luteum)
Menses • If fertilization does not occur, progesterone levels fall, depriving the endometrium of hormonal support • Arteries in uterine wall kink and go into spasms and endometrial cells begin to die • This causes the layer to disintegrate and slough off, opening up blood vessels to allow blood flow • Average blood loss during this period is 50 to 150 m. L (about ¼ to ½ cup, but can vary from woman to woman)

Secondary Female Characteristics • Development of breast tissue • Increased deposition of fat in hip and breast areas • Widening and lightening of the pelvis • Growth of armpit and pubic hair • All are due to estrogen and progesterone levels




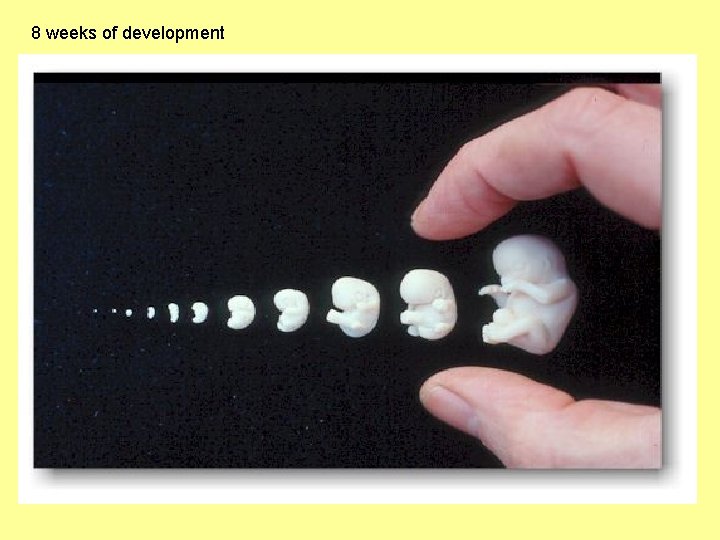
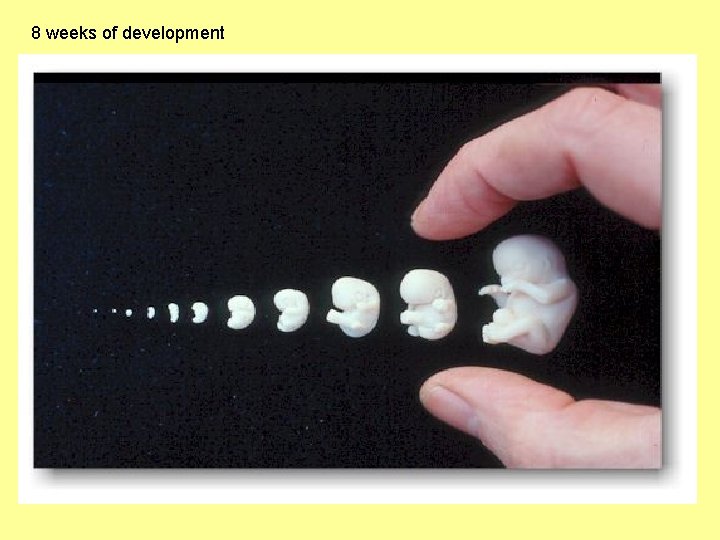
8 weeks of development

 Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Peritoneal cavity where is it
Peritoneal cavity where is it Gastrocolic ligament
Gastrocolic ligament Peritoneal sac
Peritoneal sac Lesser sac vs greater sac
Lesser sac vs greater sac Male reproductive system from front
Male reproductive system from front Functions of reproductive system
Functions of reproductive system Development of female reproductive system
Development of female reproductive system Exercise 42 review male reproductive system
Exercise 42 review male reproductive system Oogenesis
Oogenesis Dot quizlet
Dot quizlet What is reproductive system
What is reproductive system Parts of and functions of female reproductive system
Parts of and functions of female reproductive system Reproductive physiology
Reproductive physiology Male reproductive system in plants
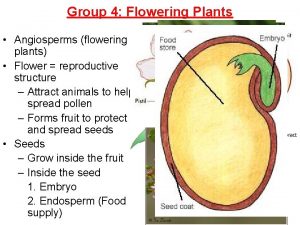
Male reproductive system in plants Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is the sperm stored
Where is the sperm stored Functions of testes
Functions of testes Male prostate
Male prostate Male reproductive system plants
Male reproductive system plants Disease traductor
Disease traductor Fish reproductive system
Fish reproductive system Reproductive system of pila
Reproductive system of pila Fetal pig diagram labeled answers
Fetal pig diagram labeled answers Female part of a flower
Female part of a flower Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Base of prostate gland
Base of prostate gland Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Anatomy of a pig
Anatomy of a pig Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ Female reproductive system label
Female reproductive system label Pathway of sperm in male reproductive system
Pathway of sperm in male reproductive system Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male plant reproductive system
Male plant reproductive system Summary of male reproductive system
Summary of male reproductive system Female reproductive system external
Female reproductive system external Layers of scrotum anatomy
Layers of scrotum anatomy What is seminal vesicle in male reproductive system
What is seminal vesicle in male reproductive system Where in the female reproductive system does meiosis occur
Where in the female reproductive system does meiosis occur Male genital
Male genital Uncircumcised penis
Uncircumcised penis Male reproductive system of mammals
Male reproductive system of mammals Chapter 16 lesson 2 the male reproductive system
Chapter 16 lesson 2 the male reproductive system Parturition
Parturition Male reproductive system labelled
Male reproductive system labelled Male reproductive system
Male reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Folliculogenesis
Folliculogenesis Male reproductive system table
Male reproductive system table Primary spermatocyte
Primary spermatocyte Lesson 2 the male reproductive system
Lesson 2 the male reproductive system Epididymiis
Epididymiis Male reproductive system of birds
Male reproductive system of birds Dorsal vein of the penis
Dorsal vein of the penis Opuberty
Opuberty Male reproductive system
Male reproductive system Gandotropin
Gandotropin Glans penis
Glans penis Where is pollen produced
Where is pollen produced