Male Reproductive System Functions of male Reproductive System












- Slides: 37

Male Reproductive System Functions of male Reproductive System: • produce gametes • deliver gametes • protect and support gametes

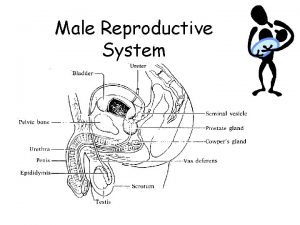
Functions of the parts of the Male Reproductive System • Scrotum: Sac that holds the testicles. Testicles are held outside the body to maintain proper temperature for sperm production • Testis: Two oval shaped structures that create sperm. Each sperm cell contains haploid (n) the chromosome number • Epididymis: Oval shaped structure that lies on top of the testis. It stores sperm. Sperm become motile here.
Male Reproductive System • Vas deferens: Hollow tube leading from the testis to the urethra. It carries sperm from the testis to the penis. • Cowper`s Gland: A small gland that adds an alkaline ( Basic ) fluid to help neutralize the acidity of the female reproductive tract. • Prostate Gland: Adds fluid to sperm. This fluid helps to neutralize the acidity of the female reproductive tract.
Male Reproductive System • Seminal Vesicles: Glands that secrete a mucus like fluid with sperm. This fluid contains fructose that provides energy for sperm. • Urethra: Opening through which sperm and urine exit the male body. • Penis: The reproductive organ of the male. • Semen: Male reproductive fluid containing sperm and other fluids.
Structure of a Male Testicle • A male testicle is comprised of the following structures. • Seminiferous Tubules: These are long coiled tubes within a testicle where sperm are produced. • Sertoli Cells: These are cells that surround the seminiferous tubules and help to nourish the sperm as they are developing. • Epididymis: oval shaped structure in the testicle that stores sperm after creation. Sperm mature here and become motile

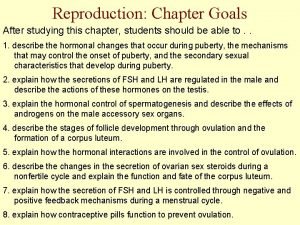
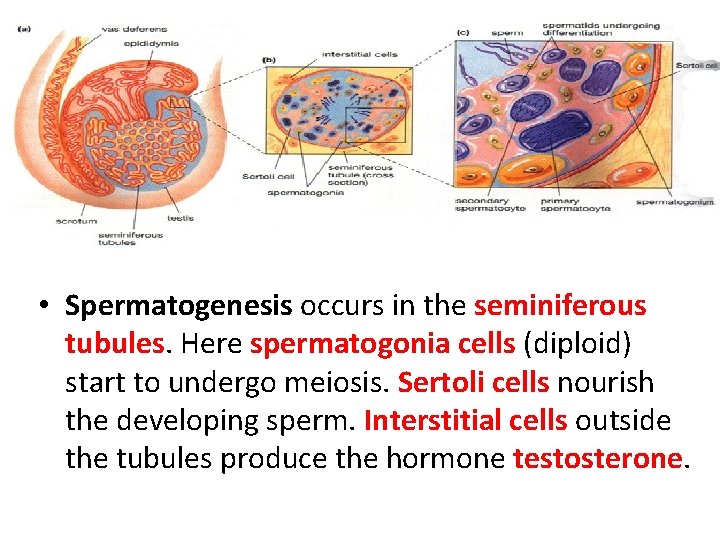
Function #1: Production of Spermatogenesis occurs in the testes after puberty. From the testes they are deposited into the epididymas where they are stored. and then vas deferens to begin swimming and prepare to be deposited into the female. Sperm cells are haploid and are produced in the tubules within the testes.
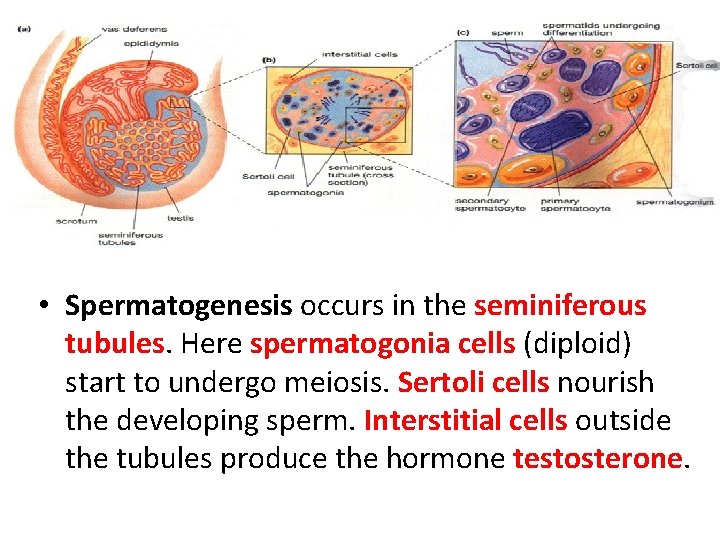
• Spermatogenesis occurs in the seminiferous tubules. Here spermatogonia cells (diploid) start to undergo meiosis. Sertoli cells nourish the developing sperm. Interstitial cells outside the tubules produce the hormone testosterone.
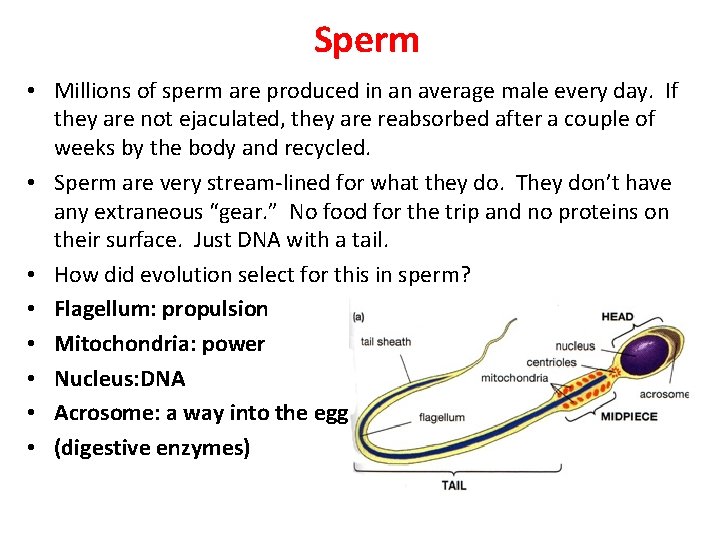
Structure of a Human Sperm • The human sperm consists of 3 main parts. • The head: contains a nucleus and an acrosome which is a small section at the top of the head that contains enzymes to digest the membrane of the egg. • Mid section: contains the mitochondria that gives the sperm energy • Tail: consists of a long flagellum that propels the sperm forward.
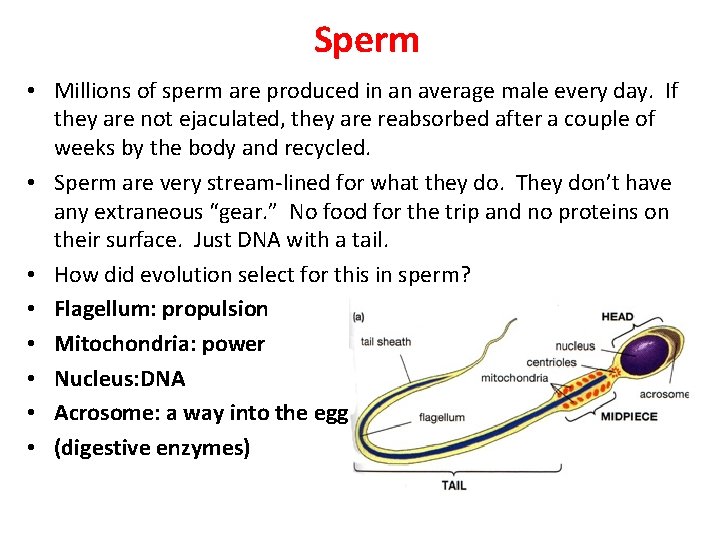
Sperm • Millions of sperm are produced in an average male every day. If they are not ejaculated, they are reabsorbed after a couple of weeks by the body and recycled. • Sperm are very stream-lined for what they do. They don’t have any extraneous “gear. ” No food for the trip and no proteins on their surface. Just DNA with a tail. • How did evolution select for this in sperm? • Flagellum: propulsion • Mitochondria: power • Nucleus: DNA • Acrosome: a way into the egg… • (digestive enzymes)
Formation of Sperm within a Male. • Sperm are created within the testicles of males through a process known as spermatogenesis. • Spermatogenesis is controlled by a series of hormones within the male. • 1. FSH( Follicle Stimulating Hormone) Hormone released by the anterior pituitary that causes spermatogenesis to occur. 2. Inhibin Hormone released by the seminiferous tubules. Works on the hypothalamus to slow the production of releasing factors that control release of FSH and Inhibin work in a negative feedback loop to control sperm production in males.

Inhibin FSH Negative Feedback Loop • If sperm count is high, Inhibin is released by seminiferous tubules. This causes the hypothalamus to NOT produce releasing factors. If there are no releasing factors, then the pituitary does not release FSH. If FSH is not released from the pituitary, spermatogenesis does not begin and sperm production is slowed. • Sperm count fall • The opposite happens if sperm count is low.

At puberty the hypothalamus releases gonadotropin-releasing hormone (Gn. RH). Gn. RH stimulates the pituitary to produce luteinizing hormone (LH) and follicle stimulating hormone (FSH) LH causes the interstitial cells in the testes to produce testosterone. LH and FSH stimulate spermatogonia in the testes. Too much testosterone triggers a negative feedback loop which stops production of Gn. RH If FSH was suppressed, but LH continued a man would be infertile but not impotent.
Other Male Reproductive Hormones • 1. LH(Lutenizing Hormone) – Hormone released by the pituitary that causes the interstitial cells of the testicles to produce the hormone Testosterone. 2. Testosterone q major male hormone. Responsible for the development of secondary sex characteristics in a male. – Secondary Sex characteristics in males enlargement of penis and testicles facial hair lower voice increased muscle mass

Function #2: Delivery of the Sperm • In order to deliver the gametes into the females’ reproductive tract and to the females’ gametes, the penis must become erect. • Blood flows into the erectile tissue and the build up of blood pressure causes the penis to become rigid. Further stimulation of the nerves on the penis triggers a series of smooth muscle contractions that propel the sperm out of the penis. • The sensation of orgasm occurs when the control of the body rapidly switches from one nervous center (the parasympathetic) to another (the sympathetic).
• So once sperm are formed and then sped on their way out of the vas deferens by muscular contractions, they are mixed with three solutions on their way, and then ejaculated into the female reproductive tract. • Seminal Vesicles: • fructose-rich fluid: energy for mitochondria • protaglandins: initiate female muscle contractions • Prostrate Gland: • alkaline (basic) fluid: neutralize the acids in the vagina • Bulbourethral Gland: • lubrication for penis to enter vagina and for sperm to move more easily through the urethra • The resulting mixture is called Semen. • an ejaculation releases about 3 m. L of semen
Function #3: Protection of the Sperm • Of the millions of sperm cells ejaculated into a female, only a few will survive to meet the egg a couple of days later. • This is because the environment into which the sperm will enter is very harsh and the vast majority die: • no energy source • very acidic • The male body provides these things to the sperm cell to aid it on its journey to find the female gamete (the egg): • sugar • a basic solution to neutralize the acid • Why is the environment so harsh? What does evolution say?
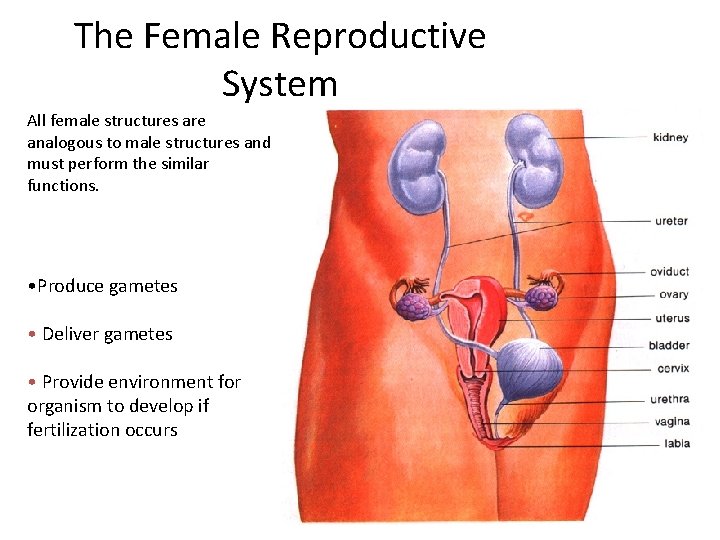
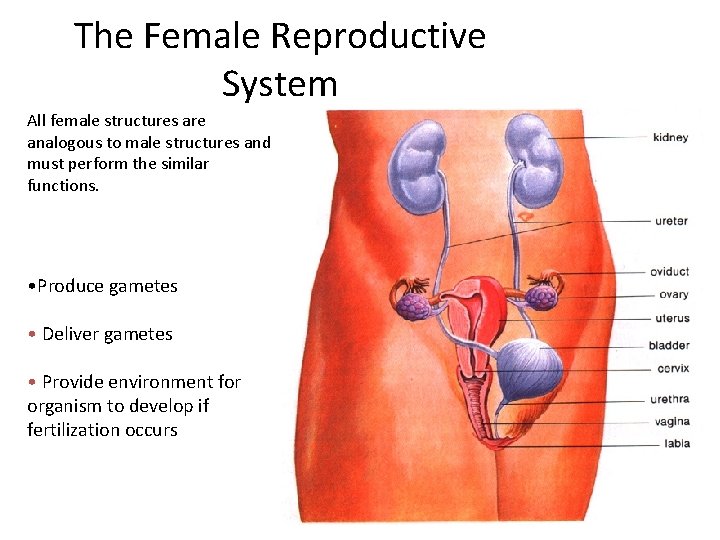
The Female Reproductive System All female structures are analogous to male structures and must perform the similar functions. • Produce gametes • Deliver gametes • Provide environment for organism to develop if fertilization occurs
Functions of the Parts of the Female Reproductive System • Vagina: • Cervix; from • Uterus: opening through which sperm enters on its way to fertilize an egg. Small opening at the top of the vagina and the base of the uterus. It supports the fetus and prevents foreign material entering the uterus. Large muscular chamber where the embryo attaches and the fetus develops. • Ovary: creates ova(egg) for fertilization. Each egg contains haploid (n) chromosome number.

Female Reproductive System • Fallopian Tubes(oviduct): Tubes that lead from the ovaries (not attached) to the uterus. Where fertilization occurs. It conducts the egg to the uterus. • Fimbriae: Finger like projections on the opening of the oviduct that helps sweep eggs from the ovary into the oviduct. • Endometrium: The lining of the uterus. It contains a rich blood supply to provide nutrients for a developing embryo.
Functions #1/#2: Produce and Deliver Eggs • A female is born with all the egg cells that she will ever have. They are immature primary oocytes and only develop into mature egg cells when the woman enters sexual maturity • From puberty (around age 12) until menopause (around age 50) a female will release 1 egg per 28 days (on average) unless fertilization occurs. • Eggs are stored and mature in the ovary. They travel down the fallopian tube(oviduct) to the uterus.
• Many primary oocytes die each day so that by puberty only about 400, 000 remain. • This is more than enough to produce 1 egg every month from puberty till menopause • How many is that if a woman comes into puberty at 13 and menopause at 50?
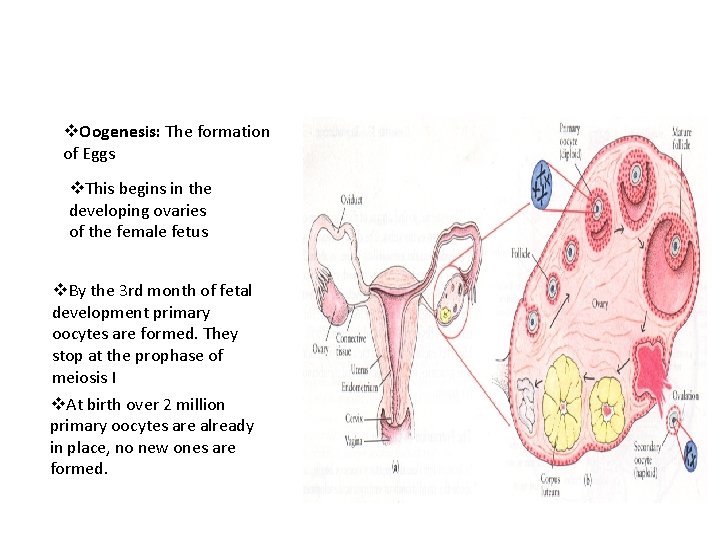
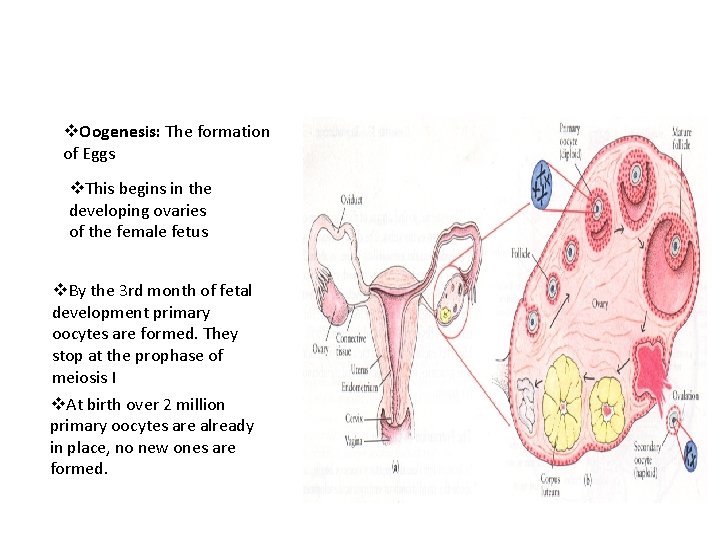
v. Oogenesis: The formation of Eggs v. This begins in the developing ovaries of the female fetus v. By the 3 rd month of fetal development primary oocytes are formed. They stop at the prophase of meiosis I v. At birth over 2 million primary oocytes are already in place, no new ones are formed.
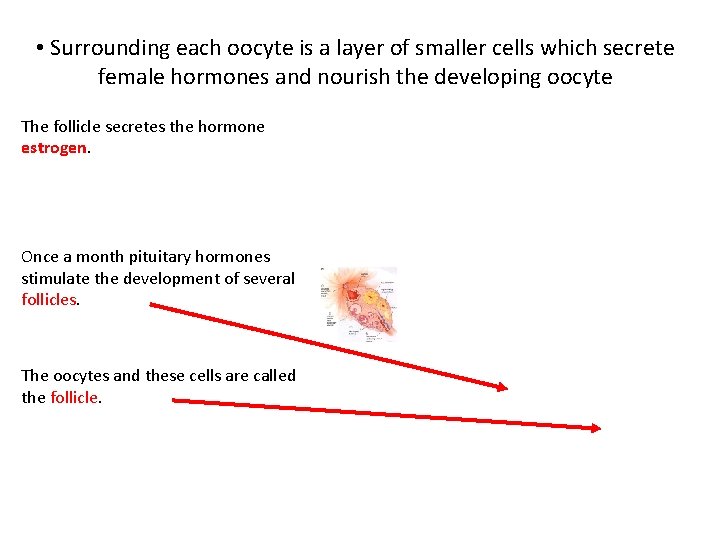
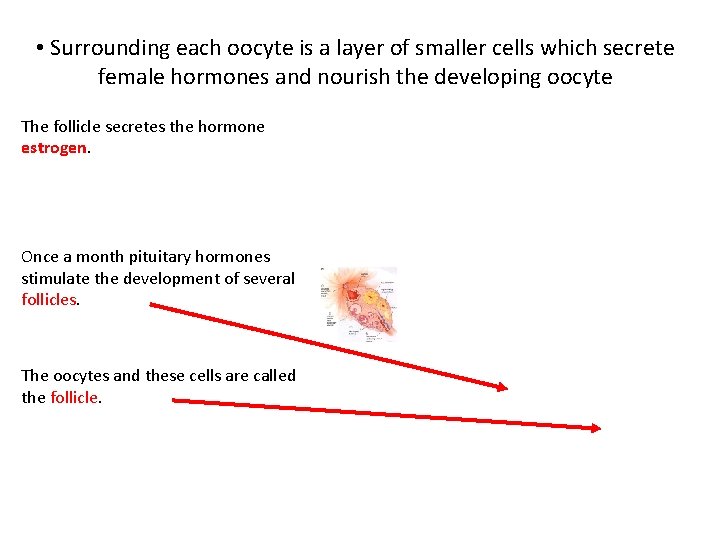
• Surrounding each oocyte is a layer of smaller cells which secrete female hormones and nourish the developing oocyte The follicle secretes the hormone estrogen. Once a month pituitary hormones stimulate the development of several follicles. The oocytes and these cells are called the follicle.

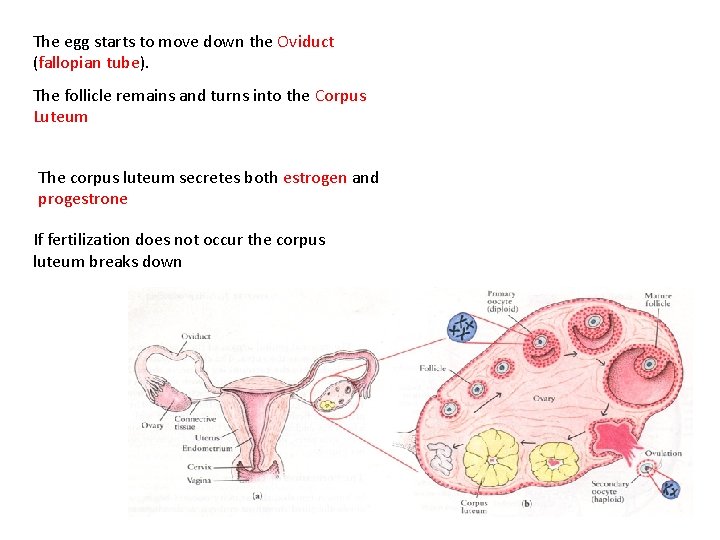
The follicle ruptures and releases the secondaary oocyte and the fimbriae move it into the oviduct
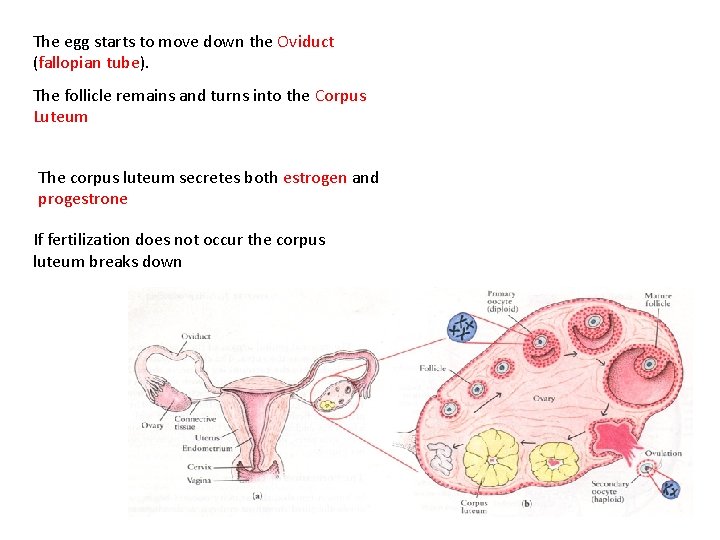
The egg starts to move down the Oviduct (fallopian tube). The follicle remains and turns into the Corpus Luteum The corpus luteum secretes both estrogen and progestrone If fertilization does not occur the corpus luteum breaks down
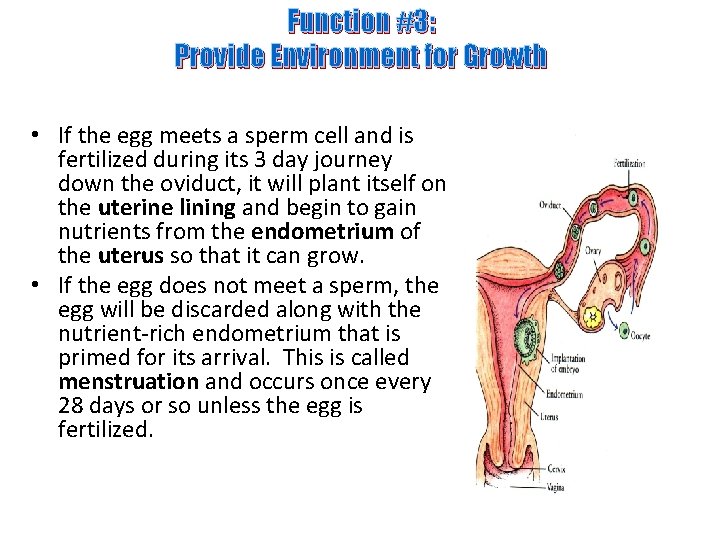
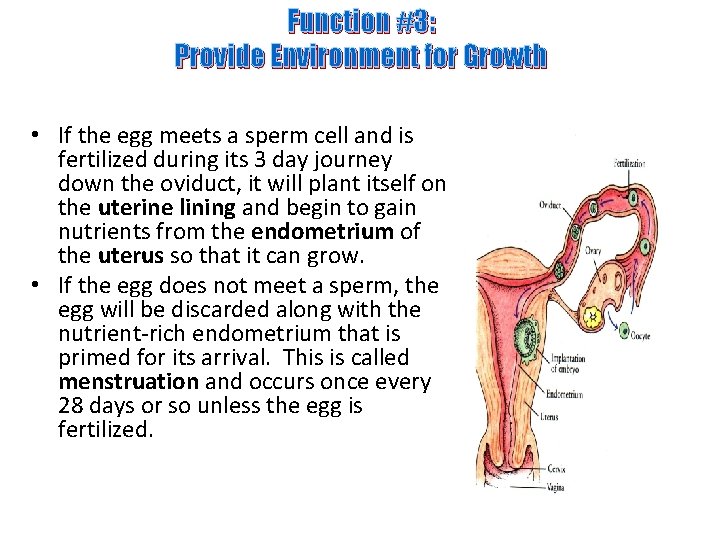
Function #3: Provide Environment for Growth • If the egg meets a sperm cell and is fertilized during its 3 day journey down the oviduct, it will plant itself on the uterine lining and begin to gain nutrients from the endometrium of the uterus so that it can grow. • If the egg does not meet a sperm, the egg will be discarded along with the nutrient-rich endometrium that is primed for its arrival. This is called menstruation and occurs once every 28 days or so unless the egg is fertilized.
The Female Menstrual Cycle • The female menstrual cycle normally follows a 28 day pattern that functions in the release of a mature egg for the purpose of fertiziation. The cycle can be from 20 -45 dyas long.

Stages of the Female Menstrual Cycle • The Follicle Stage: days 1 -14 (approximately) During this stage a hormone called FSH (follicle Stimulating Hormone) from the pituitary gland causes a follicle in the ovary to release the hormone estrogen • Estrogen: pregnancy causes the lining of the uterus to build up in blood supply and tom thicken in preparation for a • Ovulation-Day 14 During this stage a hormone called LH (luteinizing hormone)is released from the pituitary gland that causes the follicle to break open and release an egg
• Luteal Stage- Day 15 -Day 28 During this stage the left over follicle (now called the Corpus Luteum) releases Progesterone which keeps the uterine lining prepared for pregnancy. • Menstruation – Day 28 - Day 1 If no egg is fertilized, then estrogen and progesterone levels begin to drop. This causes the uterine lining to shed and it passes out through the vagina along with blood. As this is happening, FSH is being released and this causes another follicle to mature. The cycle begins to repeat itself

Female Hormones • 1. FSH ( Follicle Stimulating Hormone) Hormone released from the pituitary (under hypothalamus control) that causes follicles within the ovary to release estrogen • 2. Estrogen: Hormone released from a follicle that causes the endometrium to thicken and increase blood supply in preparation for pregnancy 3. Luteinizing hormone (LH) Hormone released by the pitutarty (under control of the hypothalamus) that causes ovulation ( release of egg from the follicle) 4. Progesterone Hormone created and released from the Corpus Luteum that maintains the uterus during Pregnancy
Female Hormone Treatments • As females get older there is a reduction in the amount of estrogen and progesterone they produce. This causes menopause • Menopause is the stopping of the menstrual cycle in woman • It is characterized by the stopping of the cycle, hot flashes, and loss of bone density
Hormone Replacement Therapy and Contraception • Hormone replacement therapy is a treatment for women who have entered menopause. It is done to counteract the declining amounts of progesterone and estrogen in females • The hormones estrogen and progesterone are given to woman in low doses(usually by pill or injection) to alleviate some of the symptoms of menopause
Benefits of Hormone Replacement Therapy • • Reduces bone loss(osteoporosis) Decreased rate of macular degeneration Improved memory Decreased chances of urinary infections

Risks of Hormone Replacenemt Therapy • • Increased risk of cancer Headaches Blood clots Stomach upset
Sexually Transmitted Infections(STI’s) • These are diseases transmitted mainly through sexual contact • Causes: most are caused by either a bacteria or a virus • Note: bacterial STI’s are curable whereas viral STI’s are NOT curable but symptoms are treatable.

Assignment • • • Research each of the following STI’s HIV and Aids Chlamydia Hepatitis Genital Herpes Syphilis Gonorrhea HPV Human papillomavirus Pubic Lice Trichomoniasis
 Function of the vagina
Function of the vagina Male function
Male function Frog testis labeled
Frog testis labeled Exercise 42 anatomy of the reproductive system
Exercise 42 anatomy of the reproductive system Oogenesis
Oogenesis Copyright
Copyright Female and male reproductive system
Female and male reproductive system Male reproductive system
Male reproductive system Reproductive physiology
Reproductive physiology Male reproductive system in plants
Male reproductive system in plants Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where semen stored
Where semen stored Male cow reproductive system diagram
Male cow reproductive system diagram Male prostate anatomy
Male prostate anatomy Male reproductive system plants
Male reproductive system plants Function of male reproductive system
Function of male reproductive system Diagram of male and female reproductive system of fish
Diagram of male and female reproductive system of fish Female reproductive system of pila
Female reproductive system of pila Mammary papilla pig
Mammary papilla pig Female part of a flower
Female part of a flower Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Cow reproductive anatomy
Cow reproductive anatomy Pearson
Pearson Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Female reproductive system label
Female reproductive system label Pathway of sperm in male reproductive system
Pathway of sperm in male reproductive system 90/2
90/2 Plants reproductive system
Plants reproductive system Summary of male reproductive system
Summary of male reproductive system Female anatomy
Female anatomy Cat male reproductive system
Cat male reproductive system Note on male reproductive system
Note on male reproductive system Prostatic urethra
Prostatic urethra