Male Reproductive System 11 Jan22 Male Reproductive System





- Slides: 47
Male Reproductive System 11 -Jan-22 Male Reproductive System 1

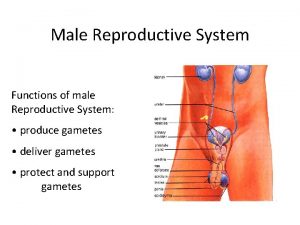
Overview n n n Physiologic anatomy Spermatogenesis Endocrine function of testes Regulation of sex hormones Control of testicular function 11 -Jan-22 Male Reproductive System 2
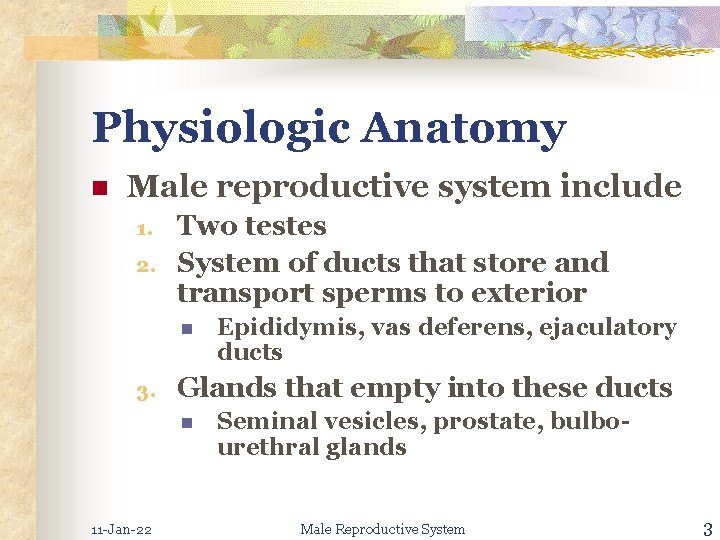
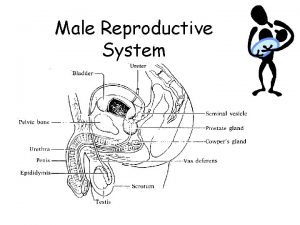
Physiologic Anatomy n Male reproductive system include 1. 2. Two testes System of ducts that store and transport sperms to exterior n 3. Glands that empty into these ducts n 11 -Jan-22 Epididymis, vas deferens, ejaculatory ducts Seminal vesicles, prostate, bulbourethral glands Male Reproductive System 3
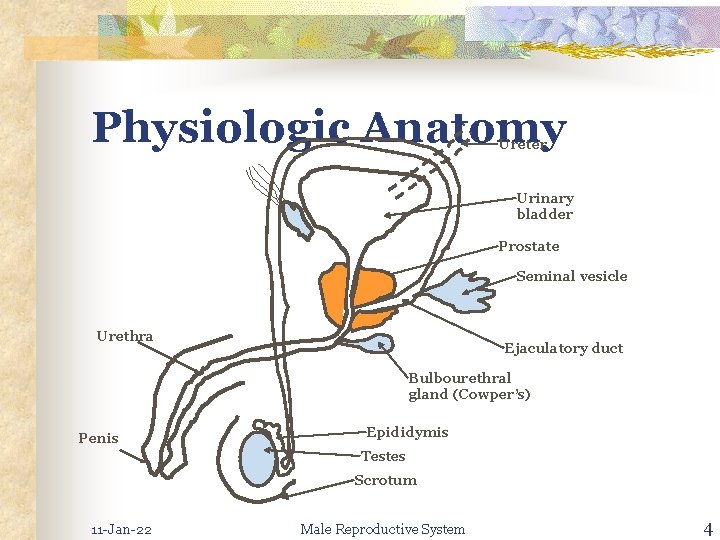
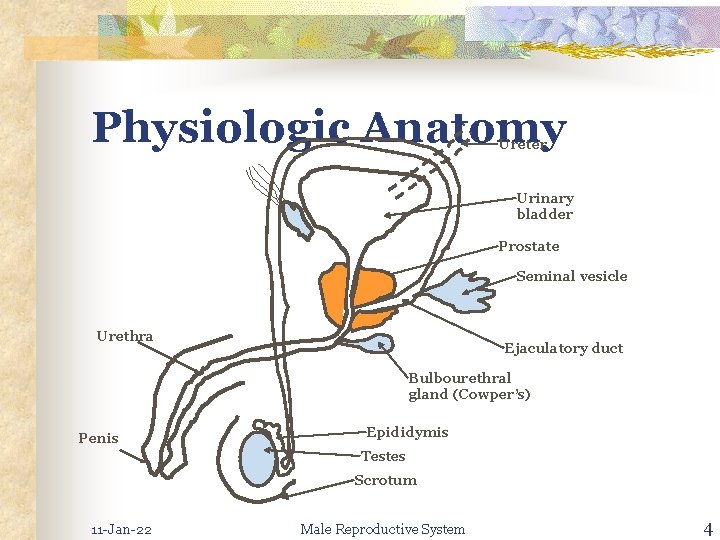
Physiologic Anatomy Ureter Urinary bladder Prostate Seminal vesicle Urethra Ejaculatory duct Bulbourethral gland (Cowper’s) Penis Epididymis Testes Scrotum 11 -Jan-22 Male Reproductive System 4
Physiologic Anatomy n The duct system, glands and penis n n Male accessory reproductive system Testes n Located in abdomen n During n embryonic development At 7 th month of development n Descend 11 -Jan-22 into scrotum Male Reproductive System 5
Physiologic Anatomy n Suspended outside the body in the scrotum n Temperature n 11 -Jan-22 regulation Special requirement for spermatogenesis Male Reproductive System 6
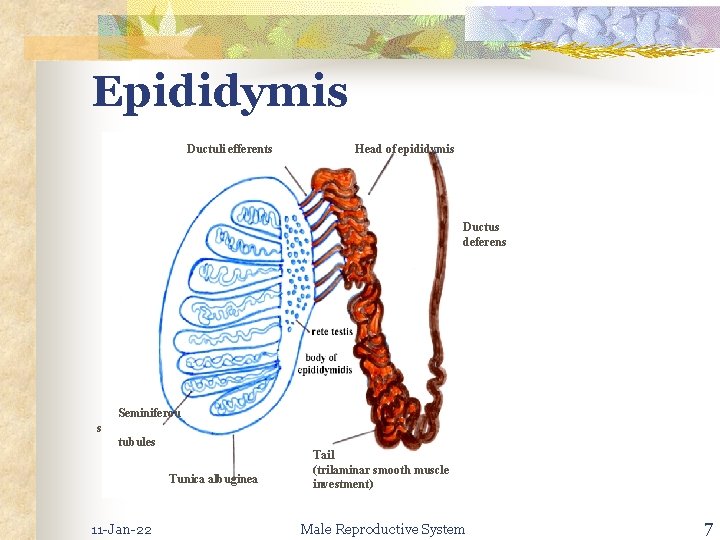
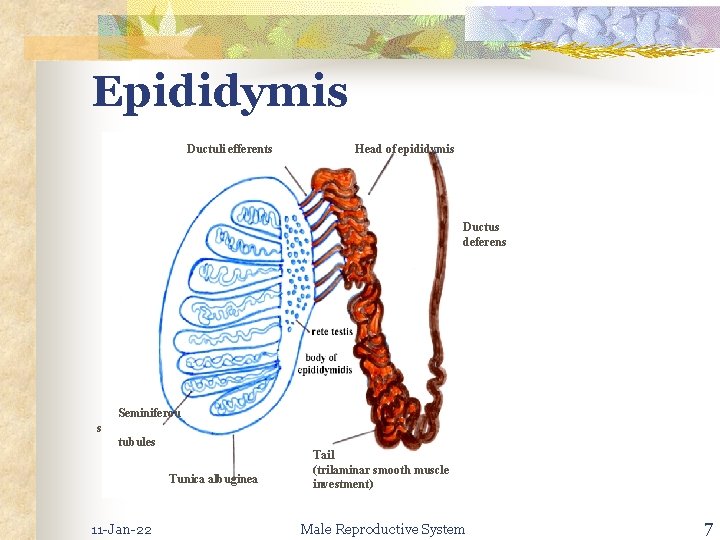
Epididymis Ductuli efferents Head of epididymis Ductus deferens Seminiferou s tubules Tunica albuginea 11 -Jan-22 Tail (trilaminar smooth muscle investment) Male Reproductive System 7
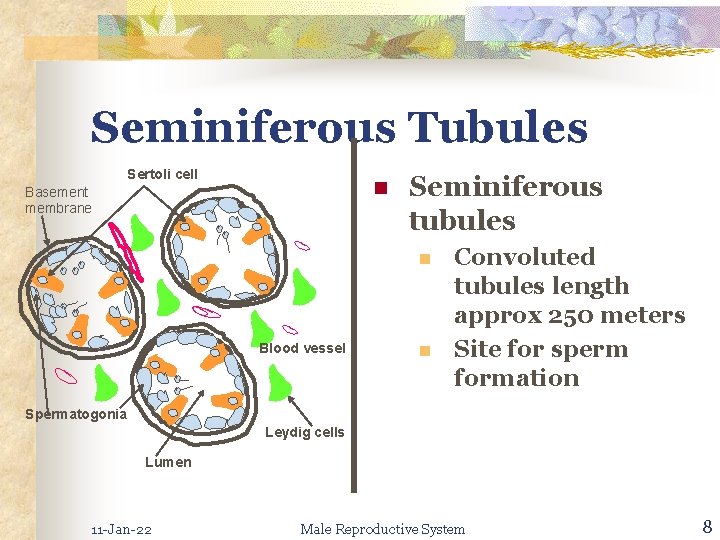
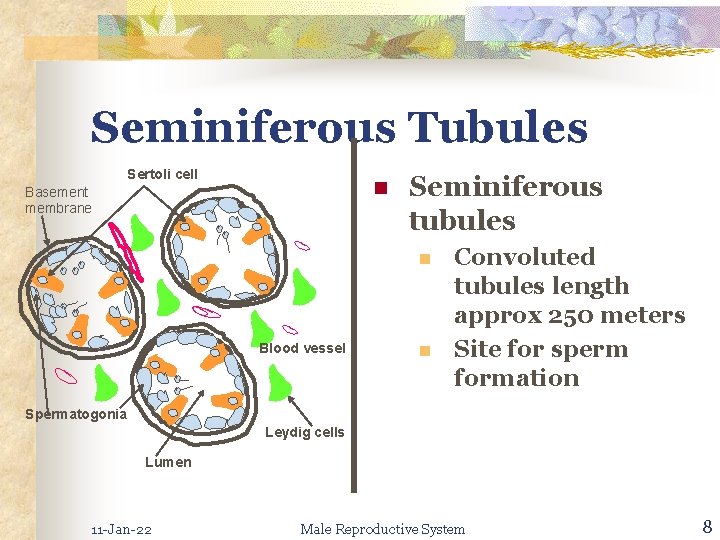
Seminiferous Tubules Sertoli cell n Basement membrane Seminiferous tubules n Blood vessel n Convoluted tubules length approx 250 meters Site for sperm formation Spermatogonia Leydig cells Lumen 11 -Jan-22 Male Reproductive System 8
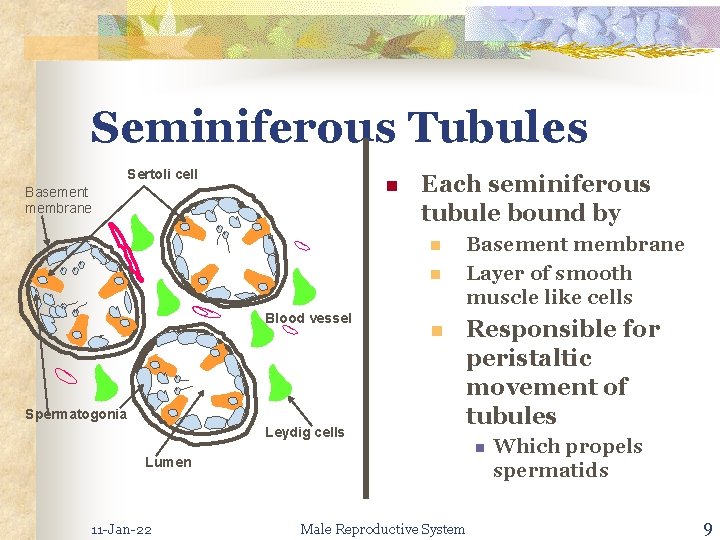
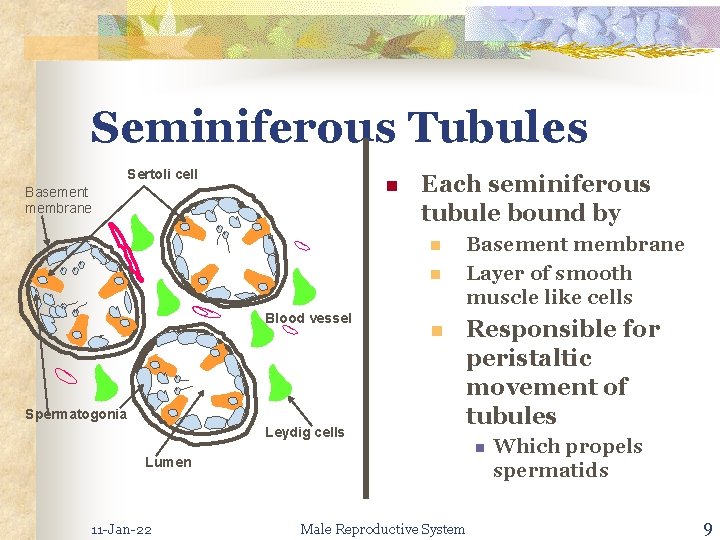
Seminiferous Tubules Sertoli cell n Basement membrane Each seminiferous tubule bound by n n Blood vessel Spermatogonia Leydig cells n Basement membrane Layer of smooth muscle like cells Responsible for peristaltic movement of tubules n Lumen 11 -Jan-22 Male Reproductive System Which propels spermatids 9

Seminiferous Tubules Sertoli cell n Basement membrane Each seminiferous tubule bound by n n Blood vessel n The centre of the tubules (lumen) n Spermatogonia Leydig cells Germ cells (spermatogonia) Sertoli cells Filled with fluid rich in n Androgens, estrogens, K+, Inositol, glutamic acid Lumen 11 -Jan-22 Male Reproductive System 10
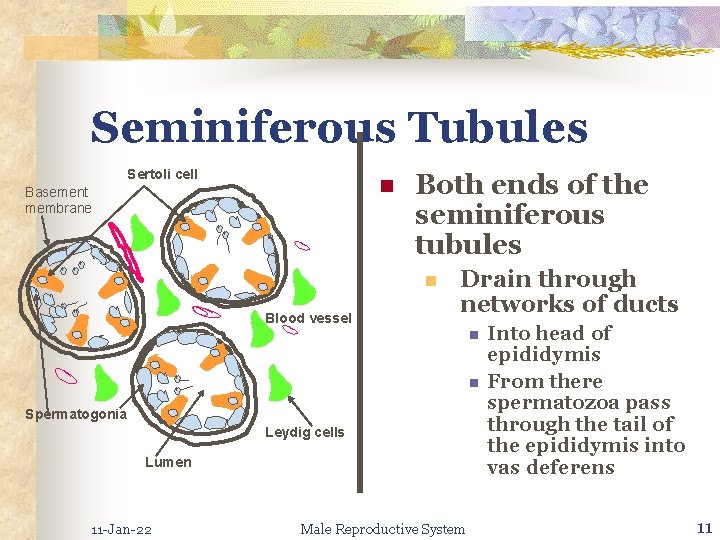
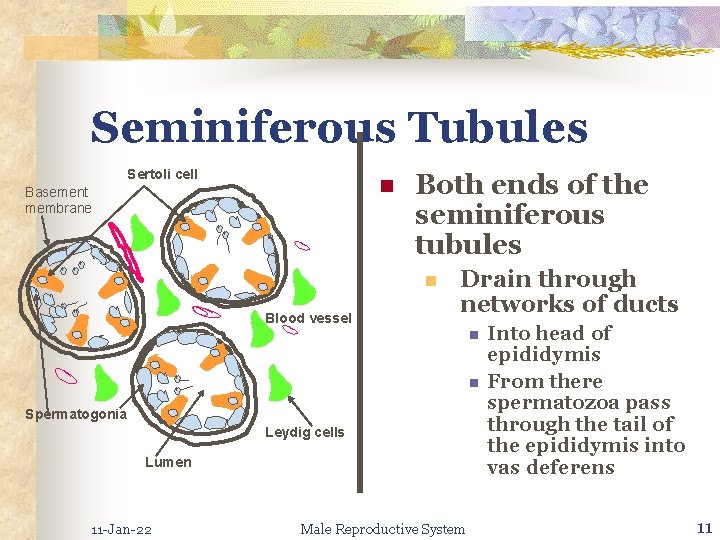
Seminiferous Tubules Sertoli cell n Basement membrane Both ends of the seminiferous tubules n Blood vessel Drain through networks of ducts n n Spermatogonia Leydig cells Lumen 11 -Jan-22 Male Reproductive System Into head of epididymis From there spermatozoa pass through the tail of the epididymis into vas deferens 11
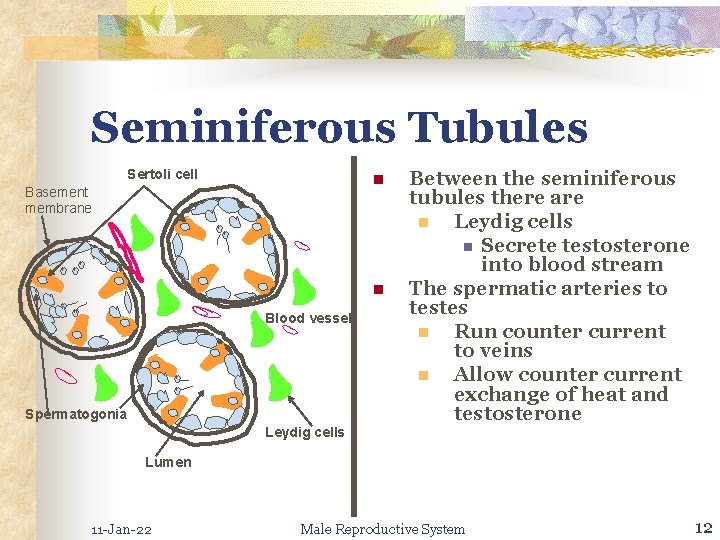
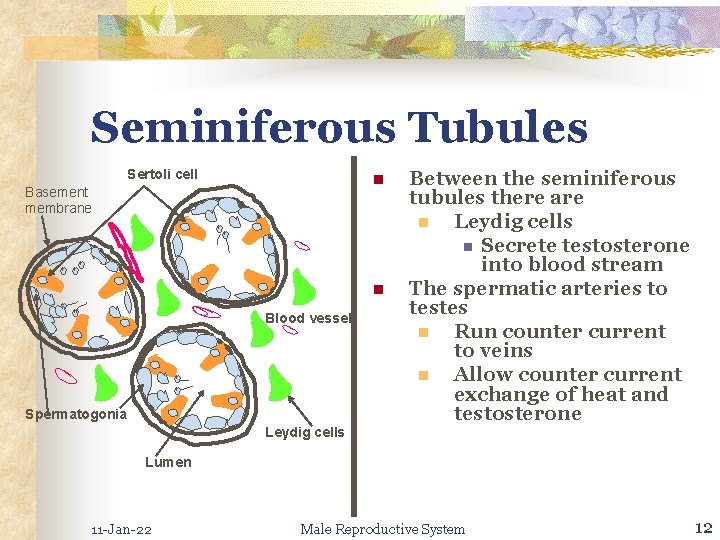
Seminiferous Tubules Sertoli cell n Basement membrane n Blood vessel Spermatogonia Leydig cells Between the seminiferous tubules there are n Leydig cells n Secrete testosterone into blood stream The spermatic arteries to testes n Run counter current to veins n Allow counter current exchange of heat and testosterone Lumen 11 -Jan-22 Male Reproductive System 12
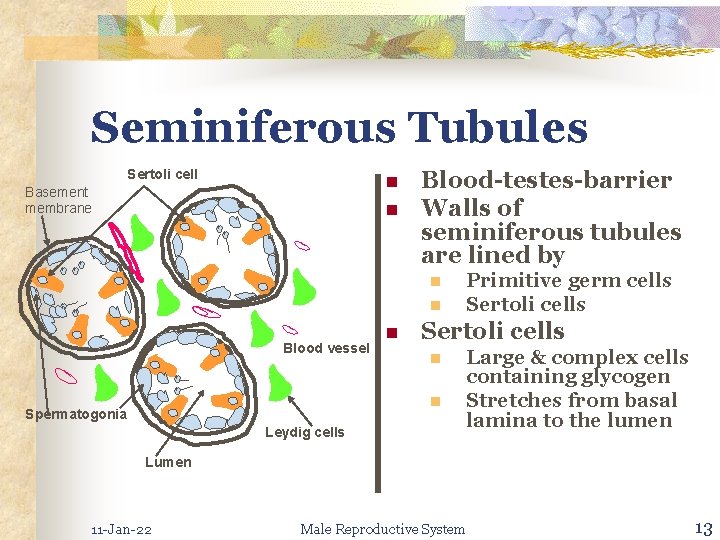
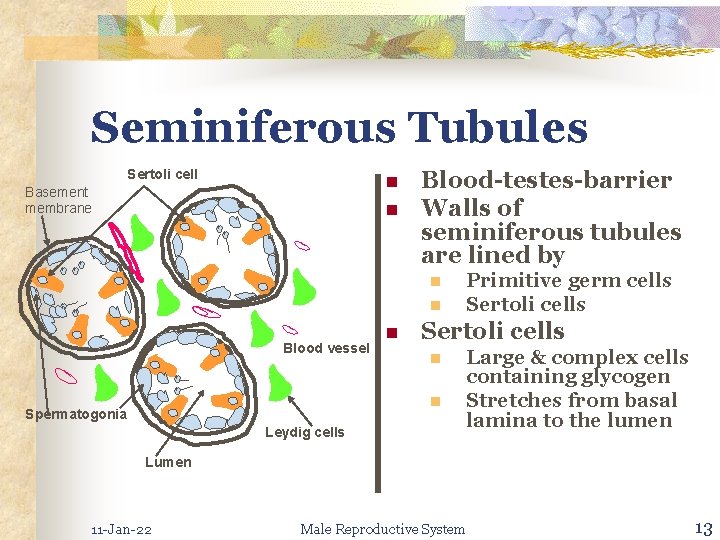
Seminiferous Tubules Sertoli cell n Basement membrane n Blood-testes-barrier Walls of seminiferous tubules are lined by n n Blood vessel n Sertoli cells n n Spermatogonia Leydig cells Primitive germ cells Sertoli cells Large & complex cells containing glycogen Stretches from basal lamina to the lumen Lumen 11 -Jan-22 Male Reproductive System 13
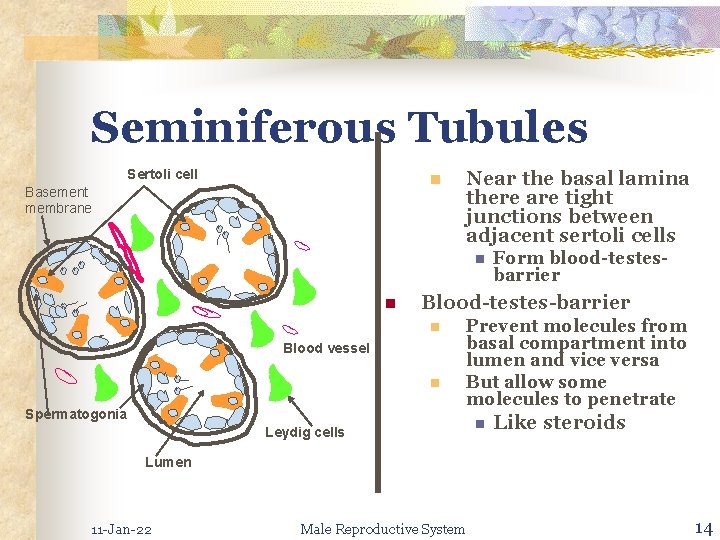
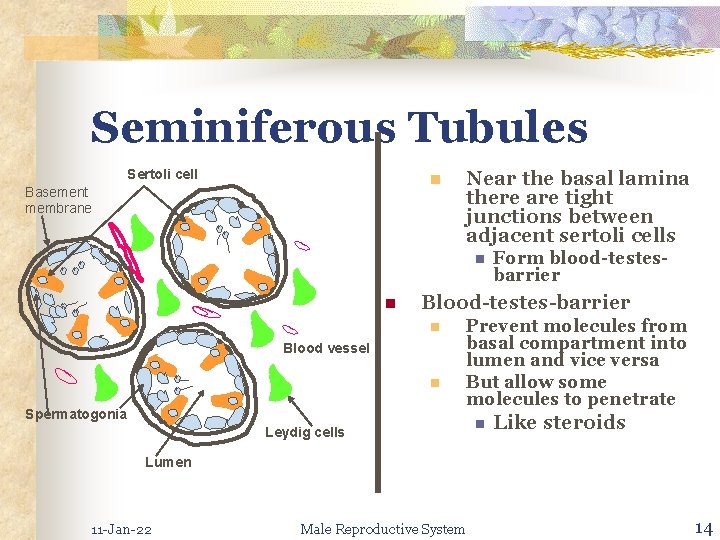
Seminiferous Tubules Sertoli cell n Basement membrane Near the basal lamina there are tight junctions between adjacent sertoli cells n n Blood-testes-barrier n Blood vessel n Spermatogonia Form blood-testesbarrier Prevent molecules from basal compartment into lumen and vice versa But allow some molecules to penetrate Leydig cells n Like steroids Lumen 11 -Jan-22 Male Reproductive System 14
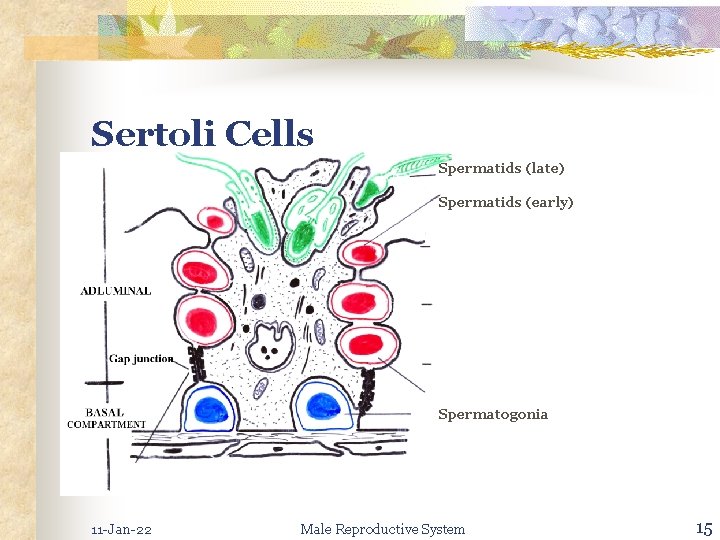
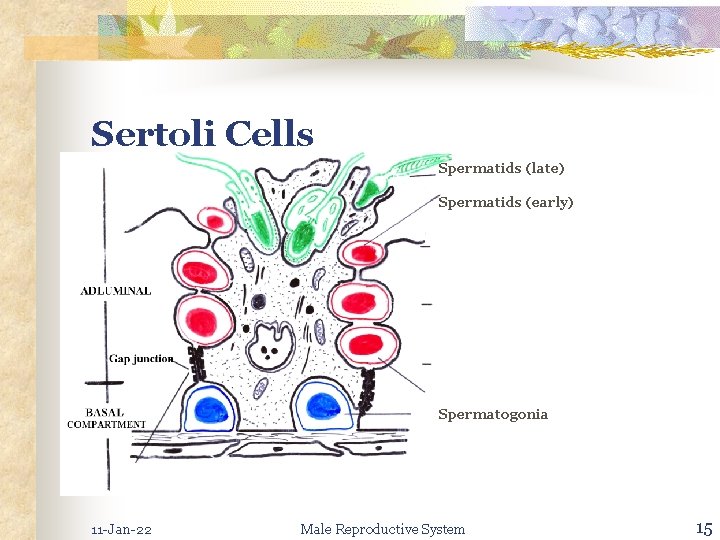
Sertoli Cells Spermatids (late) Spermatids (early) Spermatogonia 11 -Jan-22 Male Reproductive System 15
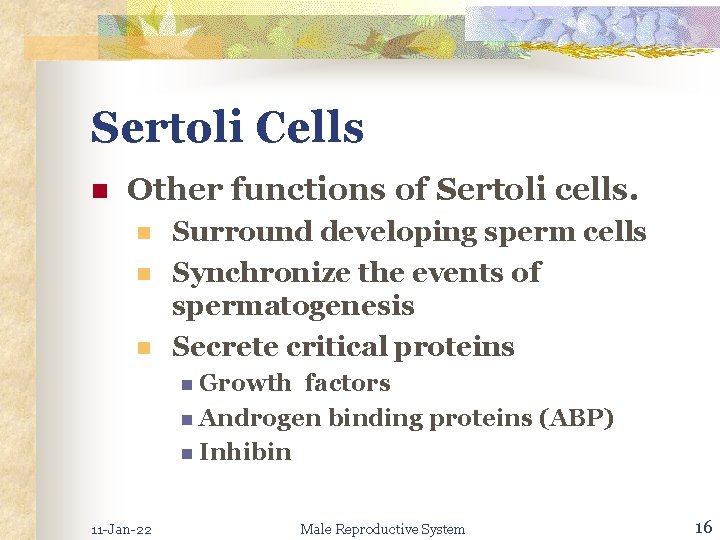
Sertoli Cells n Other functions of Sertoli cells. n n n Surround developing sperm cells Synchronize the events of spermatogenesis Secrete critical proteins n Growth factors n Androgen binding proteins (ABP) n Inhibin 11 -Jan-22 Male Reproductive System 16
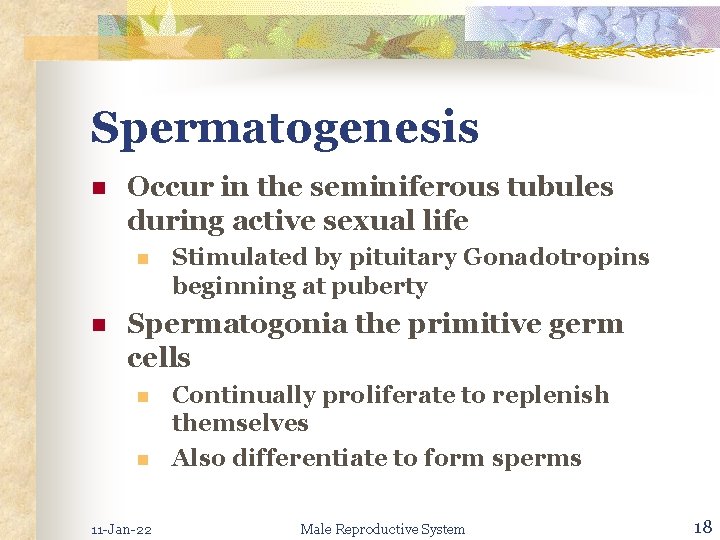
Spermatogenesis n Occur in the seminiferous tubules during active sexual life n n Stimulated by pituitary Gonadotropins beginning at puberty Spermatogonia the primitive germ cells n n 11 -Jan-22 Continually proliferate to replenish themselves Also differentiate to form sperms Male Reproductive System 18

Spermatogenesis n Spermatogonia n Mature into primary spermatocyte n Mitosis n (46 chromosome) Primary spermatocyte undergo meiosis n Reducing the number of chromosomes n Two stage process 11 -Jan-22 Male Reproductive System 19
Spermatogenesis n Secondary spermatocyte (23 chromosomes) n n 11 -Jan-22 Spermatid (23 chromosomes) Spermatozoa Male Reproductive System 20
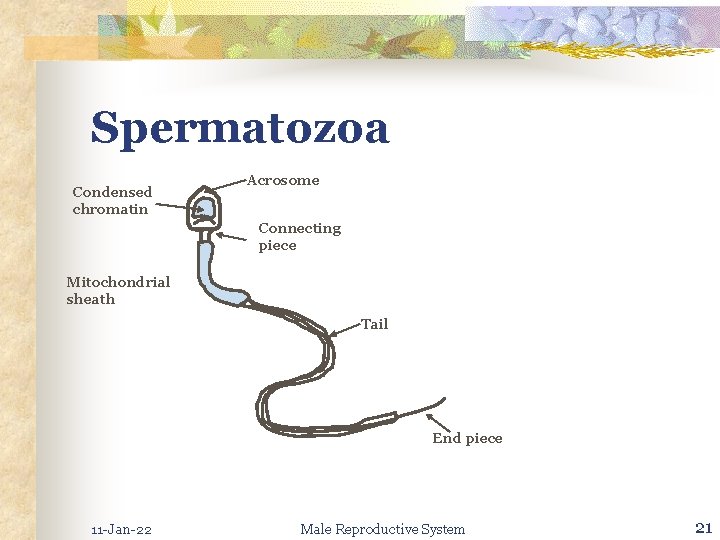
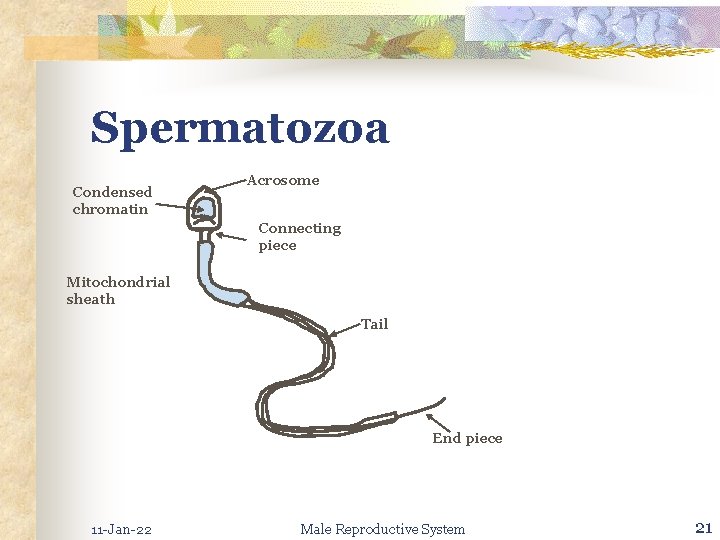
Spermatozoa Condensed chromatin Acrosome Connecting piece Mitochondrial sheath Tail End piece 11 -Jan-22 Male Reproductive System 21
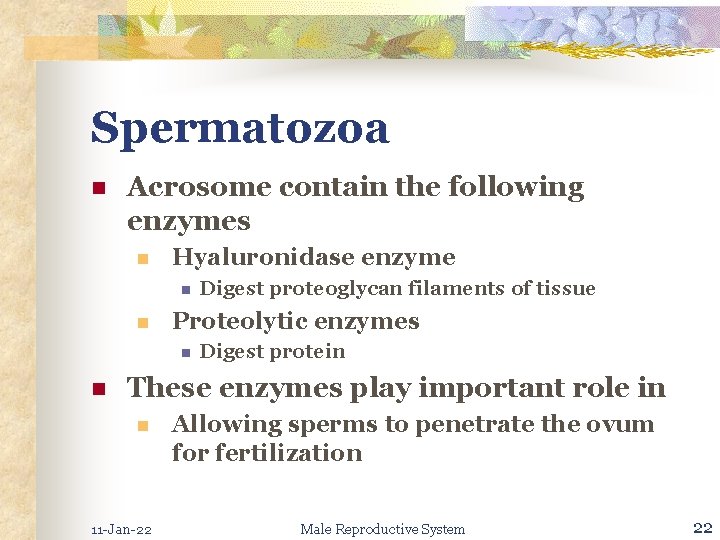
Spermatozoa n Acrosome contain the following enzymes n Hyaluronidase enzyme n n Proteolytic enzymes n n Digest proteoglycan filaments of tissue Digest protein These enzymes play important role in n 11 -Jan-22 Allowing sperms to penetrate the ovum for fertilization Male Reproductive System 22
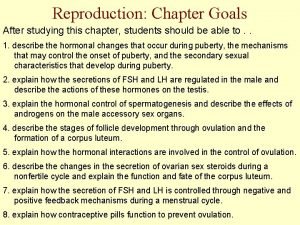
Hormonal Factors for Spermatogenesis n Testosterone n n n Secreted by leydig cells Essential for growth & division of testicular germinal cells Lutenizing hormone (LH) n n 11 -Jan-22 Secreted by ant. Pituitary Stimulate leydig cells to produce testosterone Male Reproductive System 23
Hormonal Factors for Spermatogenesis n Follicle – stimulating hormone (FSH) n n n 11 -Jan-22 Secreted by anterior pituitary Stimulate Sertoli cells Enable the process of spermiogenesis to occur Male Reproductive System 24
Hormonal Factors for Spermatogenesis n Estrogens n Formed from testosterone by n The sertoli cells when stimulated by FSH n n Essential for spermiogenesis Growth hormone n n 11 -Jan-22 Control background metabolic process of the testes Promote division of spermatogonia Male Reproductive System 25
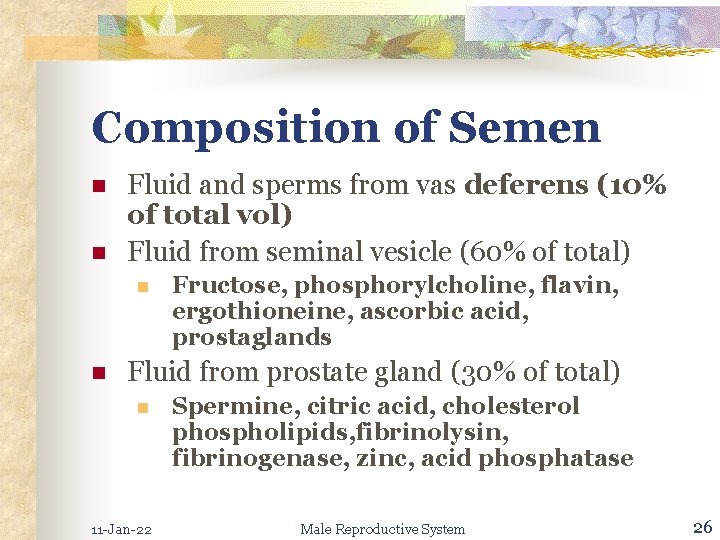
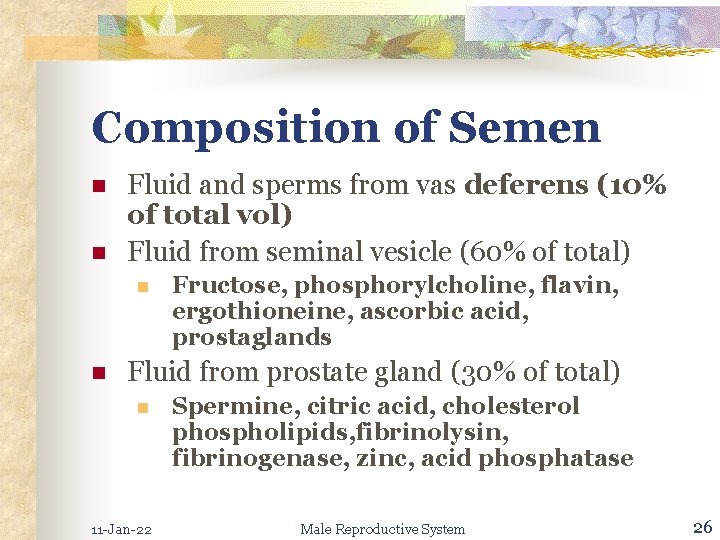
Composition of Semen n n Fluid and sperms from vas deferens (10% of total vol) Fluid from seminal vesicle (60% of total) n n Fructose, phosphorylcholine, flavin, ergothioneine, ascorbic acid, prostaglands Fluid from prostate gland (30% of total) n 11 -Jan-22 Spermine, citric acid, cholesterol phospholipids, fibrinolysin, fibrinogenase, zinc, acid phosphatase Male Reproductive System 26
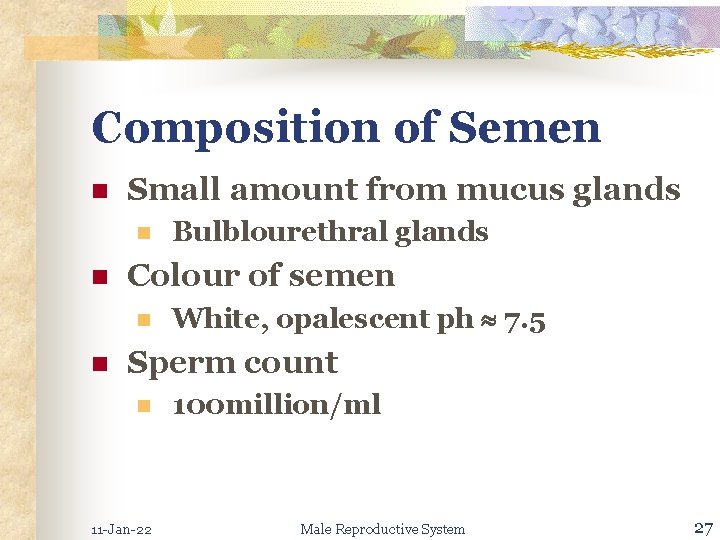
Composition of Semen n Small amount from mucus glands n n Colour of semen n n Bulblourethral glands White, opalescent ph 7. 5 Sperm count n 11 -Jan-22 100 million/ml Male Reproductive System 27
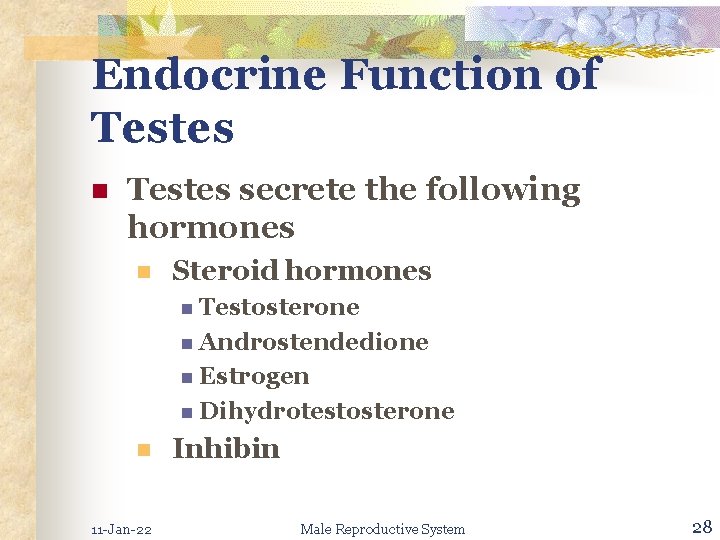
Endocrine Function of Testes n Testes secrete the following hormones n Steroid hormones n Testosterone n Androstendedione n Estrogen n Dihydrotestosterone n 11 -Jan-22 Inhibin Male Reproductive System 28
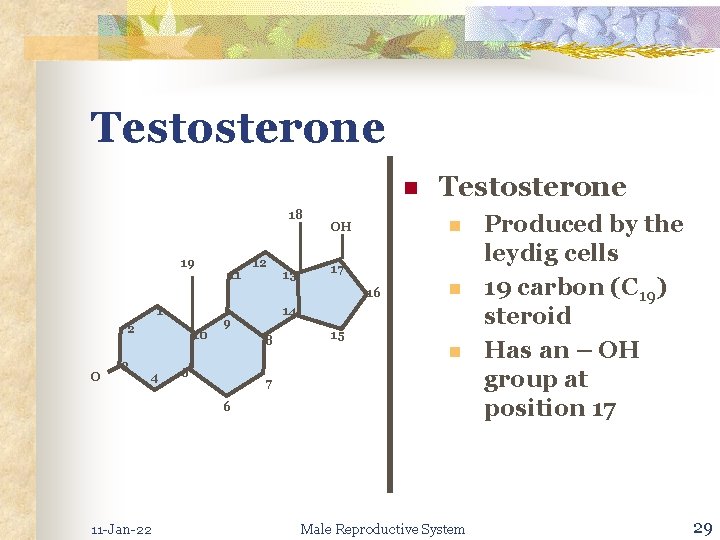
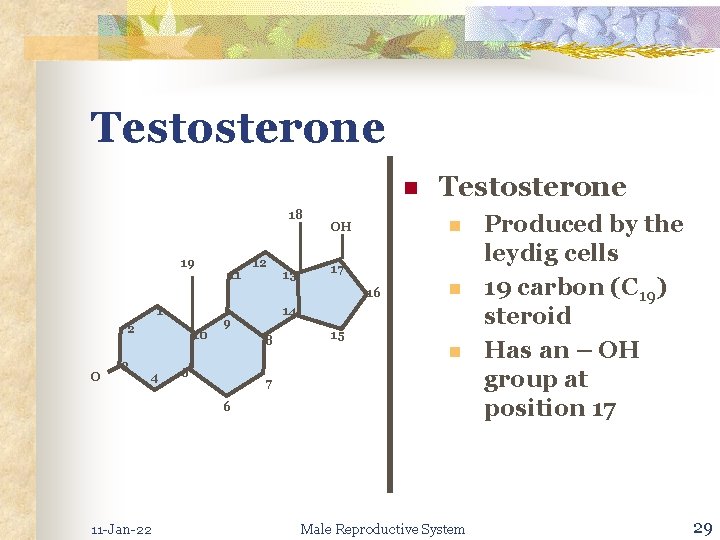
Testosterone n 18 19 11 12 13 n OH 17 16 1 2 O 3 10 4 n 14 9 8 5 Testosterone 15 n 7 6 11 -Jan-22 Male Reproductive System Produced by the leydig cells 19 carbon (C 19) steroid Has an – OH group at position 17 29
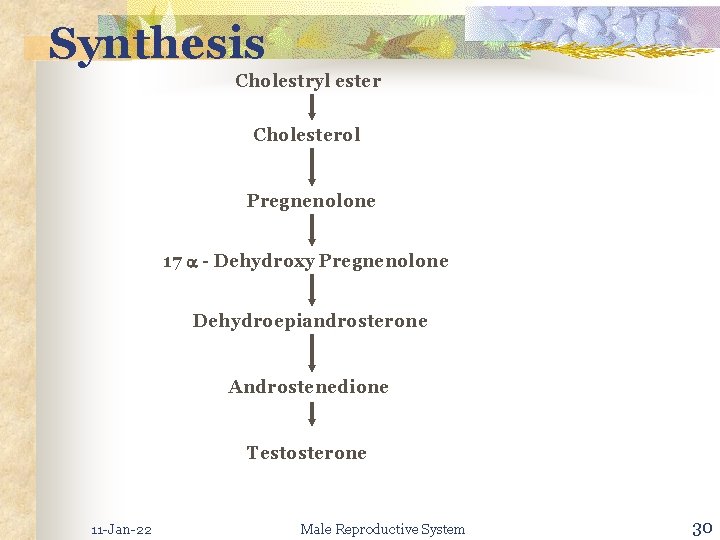
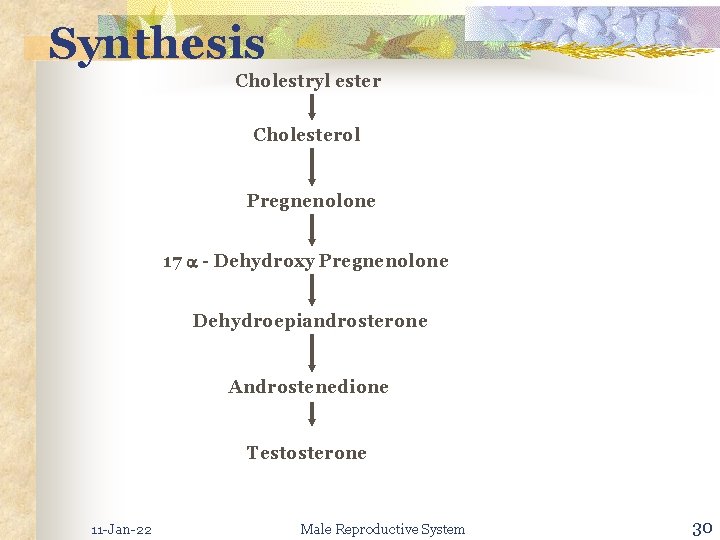
Synthesis Cholestryl ester Cholesterol Pregnenolone 17 - Dehydroxy Pregnenolone Dehydroepiandrosterone Androstenedione Testosterone 11 -Jan-22 Male Reproductive System 30
Secretion n n Normal man secretes 4 – 9 mg/d (13. 9 – 31. 3 mol/d) Small amounts are also secreted n 11 -Jan-22 Adrenals Male Reproductive System 31
Secretion n 98% of secreted testosterone is bound to plasma proteins n n n 11 -Jan-22 65 bound to - globulin(Gonadal steroid binding globulin) 33% bound to albumin A very small % of testosterone is not bound Male Reproductive System 32
Androstenedione n Also secrete by the testis n n About 2. 5 mg/d Important precursor of estrogen in man n Non endocrine tissue convert n Androgen → estrogen n Brain, skin, liver have the enzyme Aromatase 11 -Jan-22 Male Reproductive System 33

Dihydrotestosterone (DHT) n Synthesized by testis Sertoli cells n Testosterone → Dihydrotestosterone n By n 5 reductase Only 20% of plasma Dihydrotestosterone is from testis origin 11 -Jan-22 Male Reproductive System 34
Dihydrotestosterone (DHT) n Remainder comes from peripheral tissues n n Conversion of testosterone → DHT has twice the biological activity of testosterone 11 -Jan-22 Male Reproductive System 35
Estrogens n Major portion of plasma estradiol, estrogen are n n Derived from testosterone androstenedione Sertoli & leydig cells secretes small amounts of estrogens 11 -Jan-22 Male Reproductive System 36
Estrogens n Brain, skin, liver, mammary glands adipose tissue n n Have aromatase enzyme Can convert n Testosterone & androstenedione to n Estradiol n Estrogen 11 -Jan-22 Male Reproductive System 37
Estrogens n Thus estrogen in males are derived from n n 11 -Jan-22 Testes From peripheral conversion of testosterone & androstenedione Male Reproductive System 38
Effects of Testosterone in the Male n Testosterone n Is essential for spermatogenesis n n Leydig cells secrete testosterone Enters the sertoli cells Facilitate spermatogenesis It induces differentiation of n n 11 -Jan-22 Male accessory reproductive organs and maintain their functions Morphology & function of entire male duct systems, glands and penis Male Reproductive System 39
Effects of Testosterone in the Male n Induces male secondary sex characteristics n n Growth and distributions of hair External genitalia n Penis, n scrotum Internal genitalia n Seminal vesicle, prostate, bulbourethral glands 11 -Jan-22 Male Reproductive System 40

Effects of Testosterone in the Male n Testosterone n n 11 -Jan-22 Stimulate protein anabolism, bone growth and cessation of bone growth Maintain sex drive, libido and enhances aggressiveness Male Reproductive System 41
Effects of Testosterone in the Male n Testosterone n Production of Gn. RH by hypothalamus n n LH, FSH secretion by pit Directly inhibits LH secretion via action on the ant. Pit 11 -Jan-22 Male Reproductive System 42
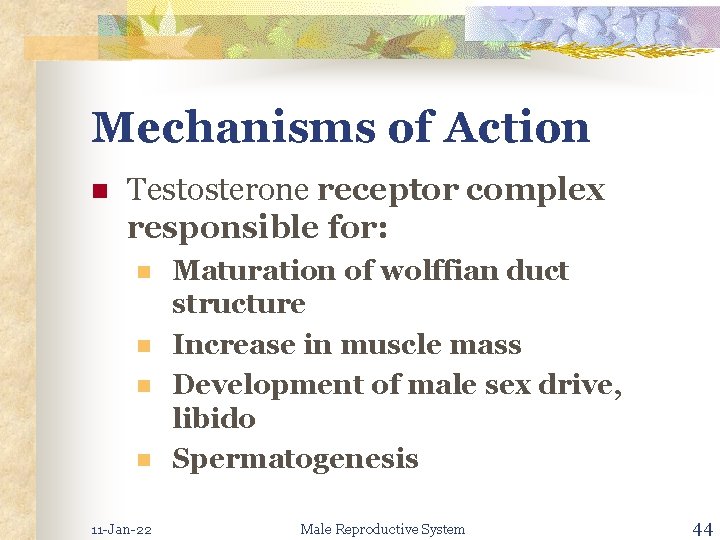
Mechanisms of Action n n Testosterone cross plasma membrane readily Combine with specific receptors n n 11 -Jan-22 Influence transcriptions of genes → RNA Result in synthesis of new proteins which underlie the overall responses to the hormone Male Reproductive System 43
Mechanisms of Action n Testosterone receptor complex responsible for: n n 11 -Jan-22 Maturation of wolffian duct structure Increase in muscle mass Development of male sex drive, libido Spermatogenesis Male Reproductive System 44
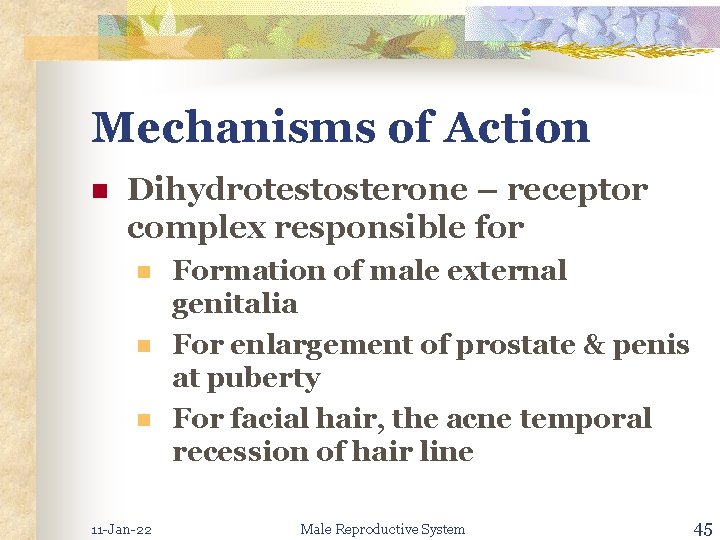
Mechanisms of Action n Dihydrotestosterone – receptor complex responsible for n n n 11 -Jan-22 Formation of male external genitalia For enlargement of prostate & penis at puberty For facial hair, the acne temporal recession of hair line Male Reproductive System 45
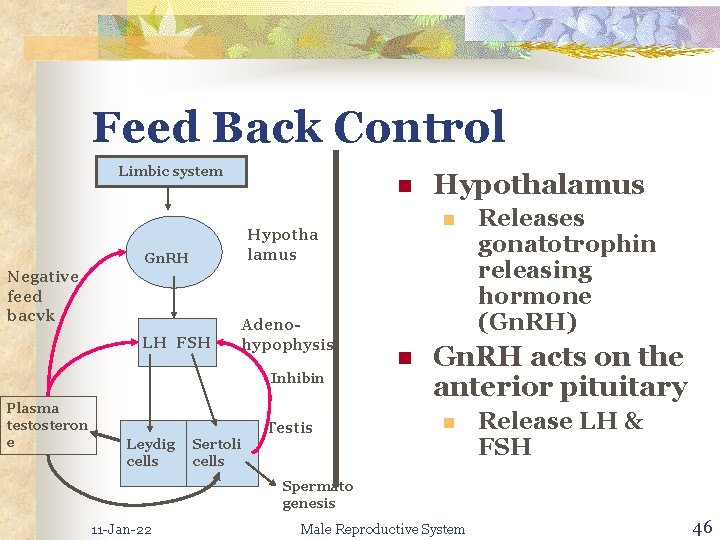
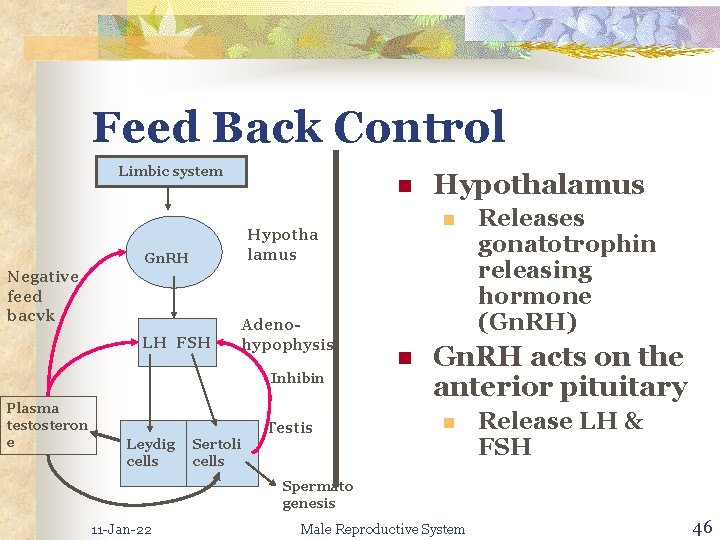
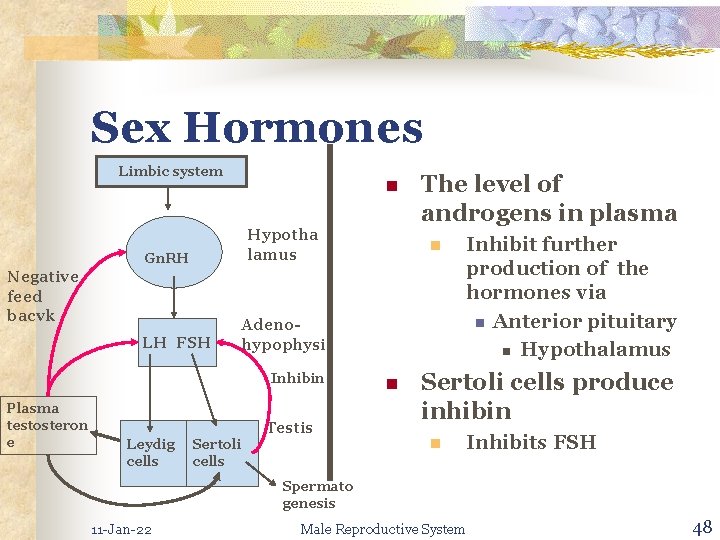
Feed Back Control Limbic system n Negative feed bacvk LH FSH Adenohypophysis Inhibin Plasma testosteron e Leydig cells n Hypotha lamus Gn. RH Sertoli cells Testis Hypothalamus n Releases gonatotrophin releasing hormone (Gn. RH) Gn. RH acts on the anterior pituitary n Release LH & FSH Spermato genesis 11 -Jan-22 Male Reproductive System 46
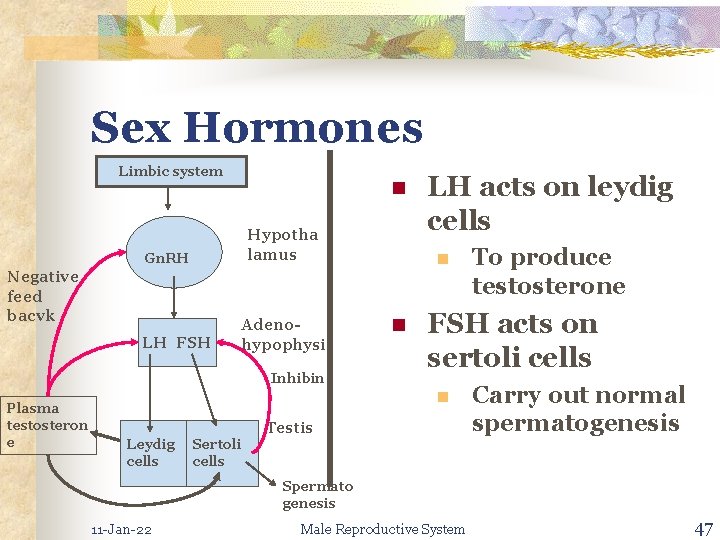
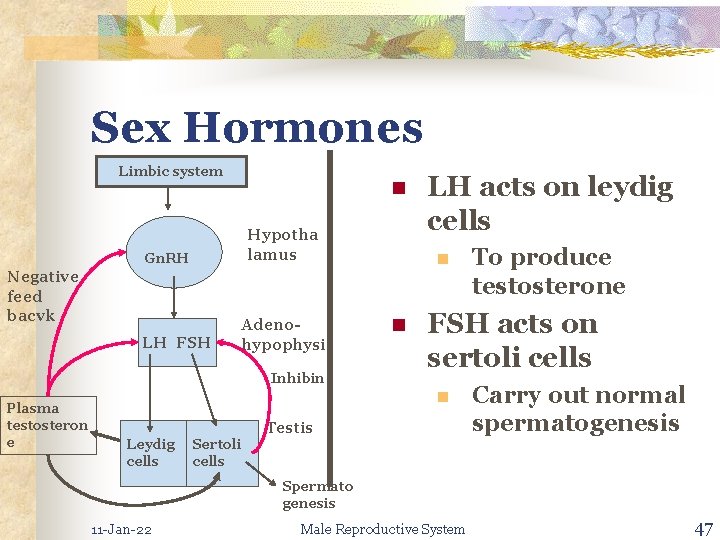
Sex Hormones Limbic system n Hypotha lamus Gn. RH Negative feed bacvk LH FSH Adenohypophysis Inhibin Plasma testosteron e LH acts on leydig cells n n FSH acts on sertoli cells n Leydig cells Sertoli cells To produce testosterone Testis Carry out normal spermatogenesis Spermato genesis 11 -Jan-22 Male Reproductive System 47
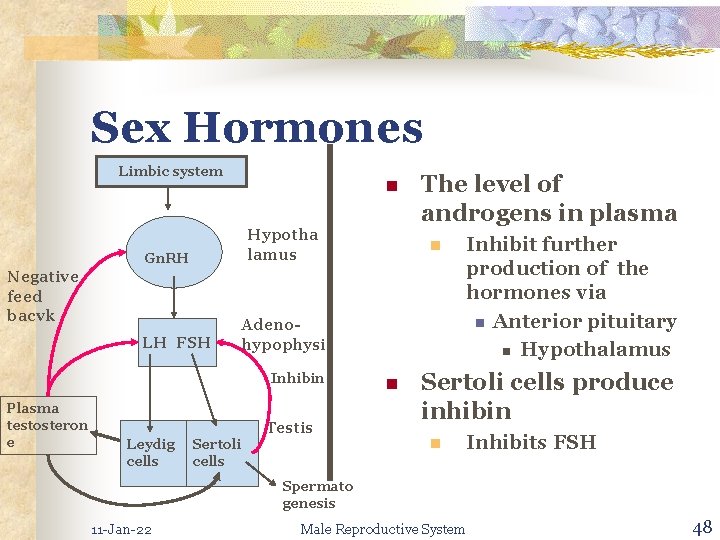
Sex Hormones Limbic system n Hypotha lamus Gn. RH Negative feed bacvk LH FSH Leydig cells n Adenohypophysis Inhibin Plasma testosteron e The level of androgens in plasma Sertoli cells Testis n Inhibit further production of the hormones via n Anterior pituitary n Hypothalamus Sertoli cells produce inhibin n Inhibits FSH Spermato genesis 11 -Jan-22 Male Reproductive System 48
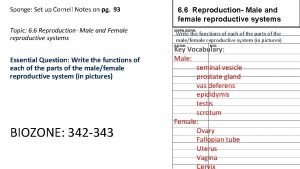
 Function of the vagina
Function of the vagina Reproductive system function
Reproductive system function Development of female reproductive system
Development of female reproductive system Exercise 42 review male reproductive system
Exercise 42 review male reproductive system Male reproductive system lateral view
Male reproductive system lateral view Function of fsh
Function of fsh Parts of male and female reproductive system
Parts of male and female reproductive system Parts of and functions of female reproductive system
Parts of and functions of female reproductive system Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male reproductive system of a plant
Male reproductive system of a plant Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is the sperm located
Where is the sperm located Male cow reproductive system diagram
Male cow reproductive system diagram What does the prostate do
What does the prostate do Male reproductive system plants
Male reproductive system plants Function of male reproductive system
Function of male reproductive system Male fish reproductive system
Male fish reproductive system Female reproductive system of pila
Female reproductive system of pila Pig male reproductive system
Pig male reproductive system Male plant reproductive system
Male plant reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Cow reproduction system
Cow reproduction system Pearson
Pearson Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ Female reproductive system label
Female reproductive system label Pathway of semen
Pathway of semen Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male plant reproductive system
Male plant reproductive system Summary of the reproductive system
Summary of the reproductive system Fornix of vagina
Fornix of vagina Cat male reproductive system
Cat male reproductive system Note on male reproductive system
Note on male reproductive system Where does meiosis occur in plants
Where does meiosis occur in plants Functions of bulbourethral gland
Functions of bulbourethral gland Similarities between male and female reproductive system
Similarities between male and female reproductive system Male reproductive system of mammals
Male reproductive system of mammals Chapter 16 lesson 3 the female reproductive system
Chapter 16 lesson 3 the female reproductive system Figure 16-5 is a sagittal view of the female
Figure 16-5 is a sagittal view of the female Male reproductive system labelled
Male reproductive system labelled Reproductive system
Reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Folliculogenesis
Folliculogenesis