The Reproductive System Male and Female General Reproduction

- Slides: 28
The Reproductive System Male and Female
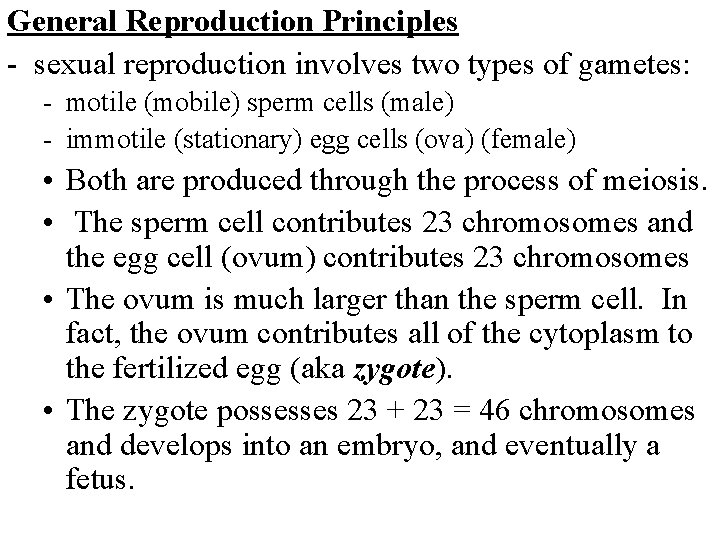
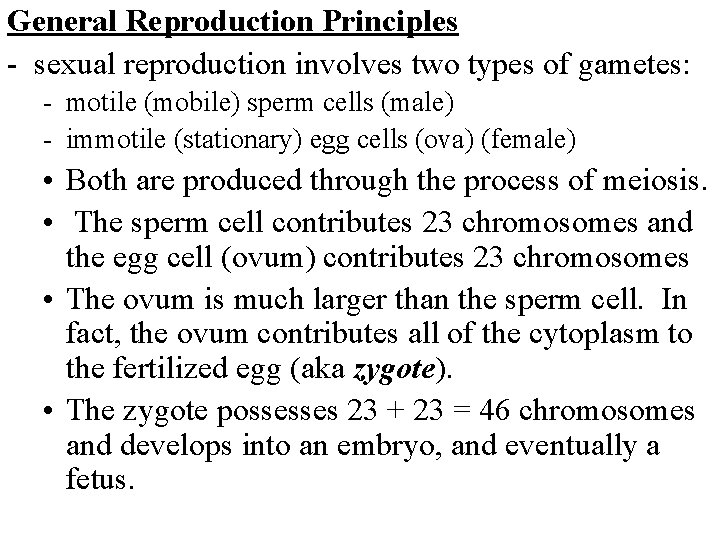
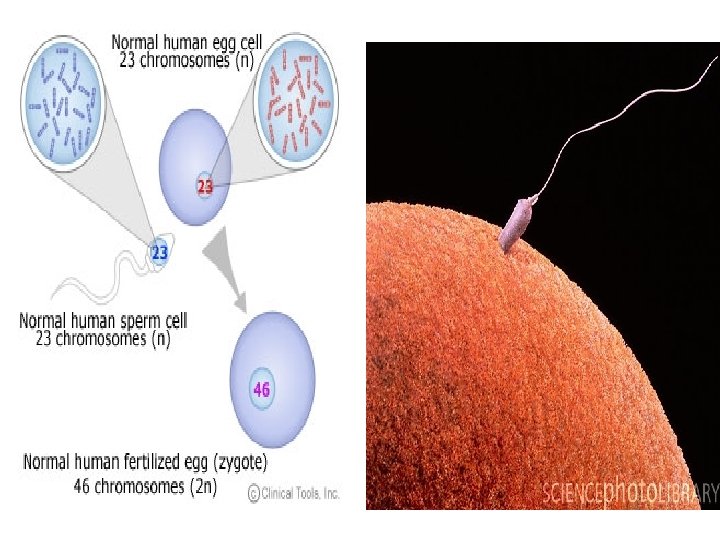
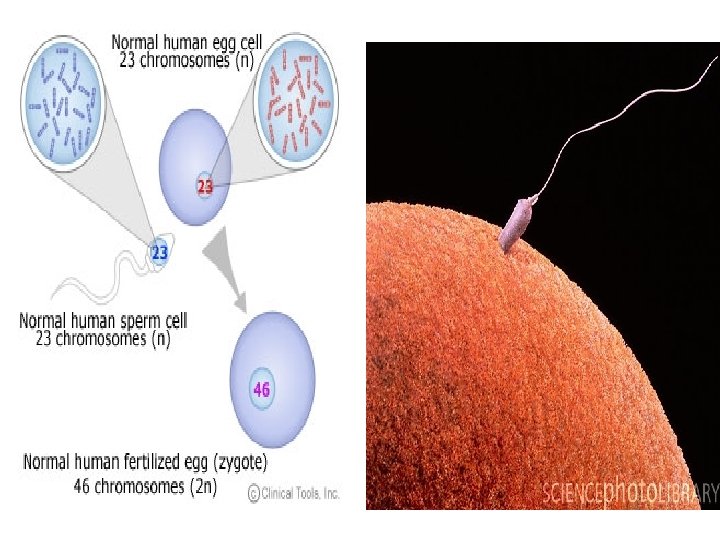
General Reproduction Principles - sexual reproduction involves two types of gametes: - motile (mobile) sperm cells (male) - immotile (stationary) egg cells (ova) (female) • Both are produced through the process of meiosis. • The sperm cell contributes 23 chromosomes and the egg cell (ovum) contributes 23 chromosomes • The ovum is much larger than the sperm cell. In fact, the ovum contributes all of the cytoplasm to the fertilized egg (aka zygote). • The zygote possesses 23 + 23 = 46 chromosomes and develops into an embryo, and eventually a fetus.
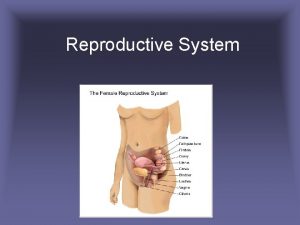
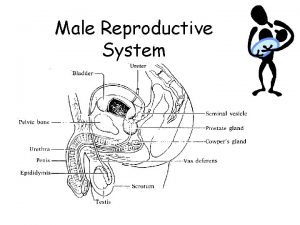
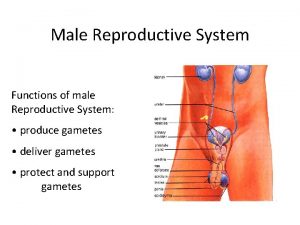
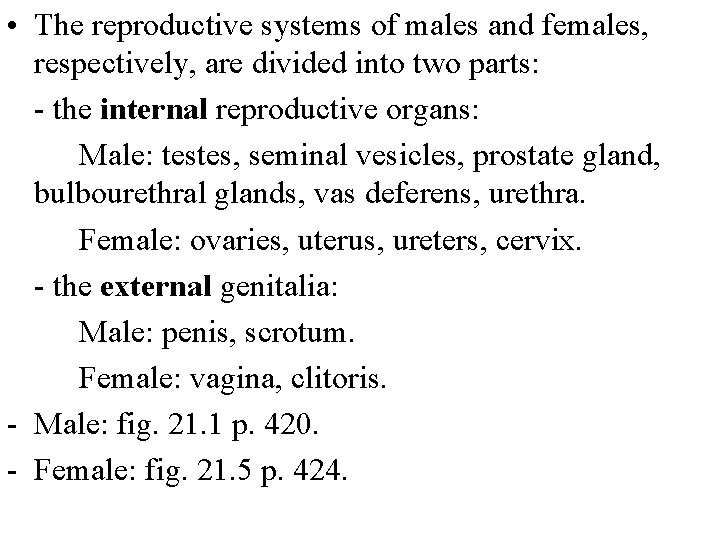
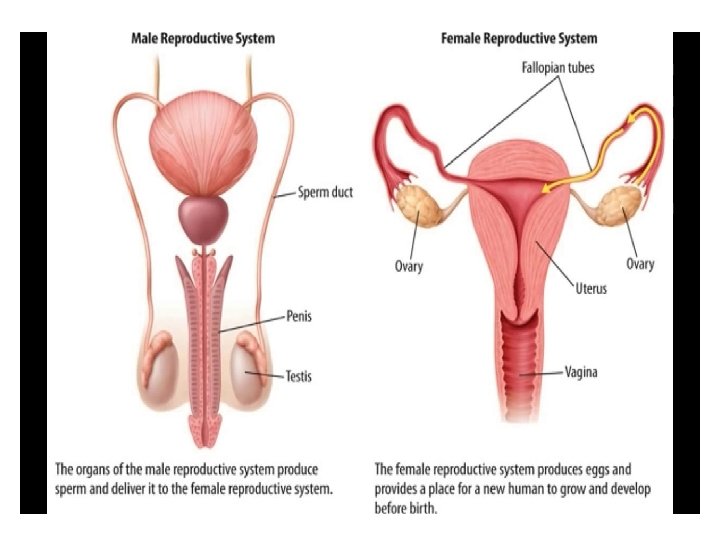
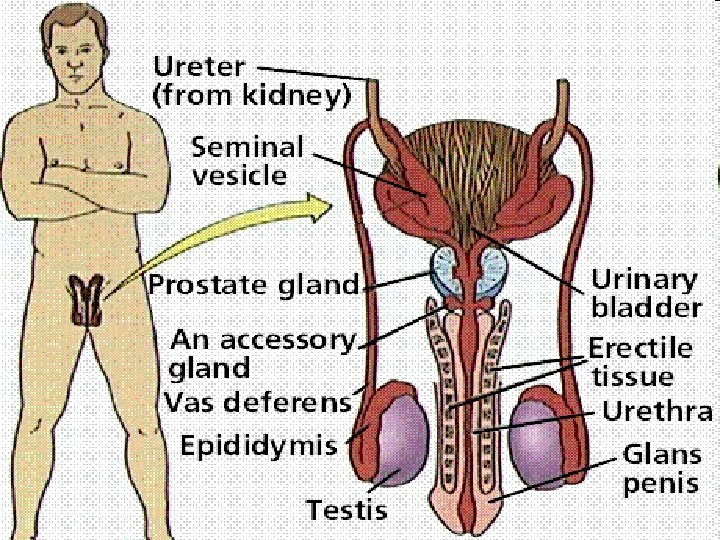
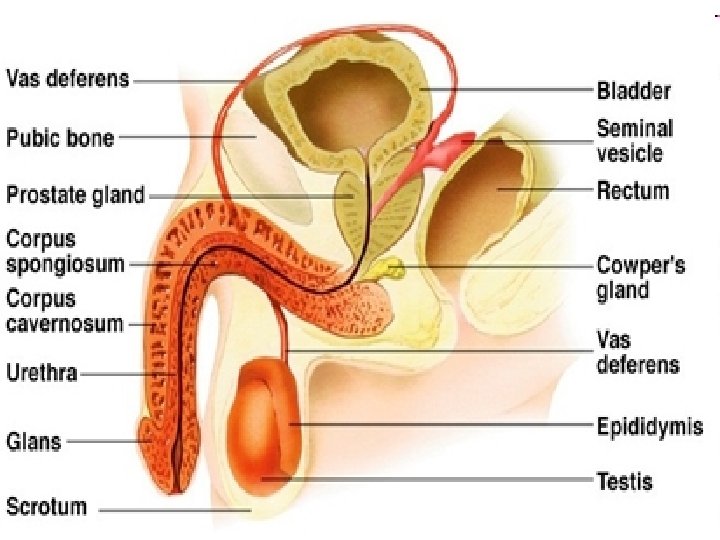
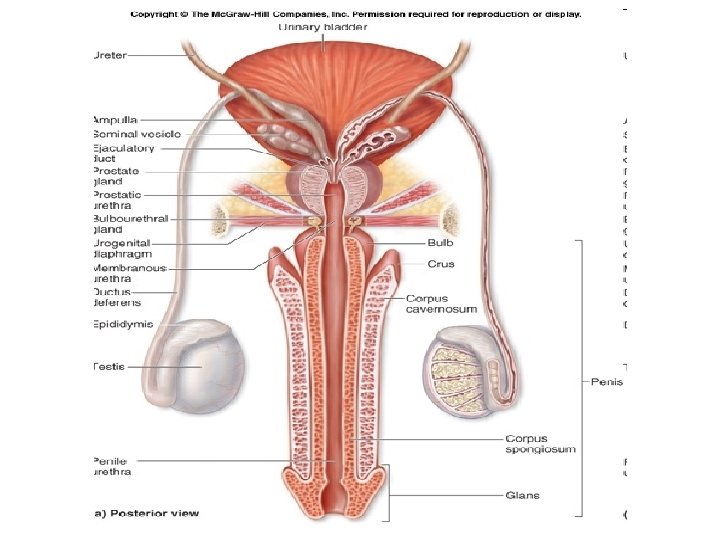
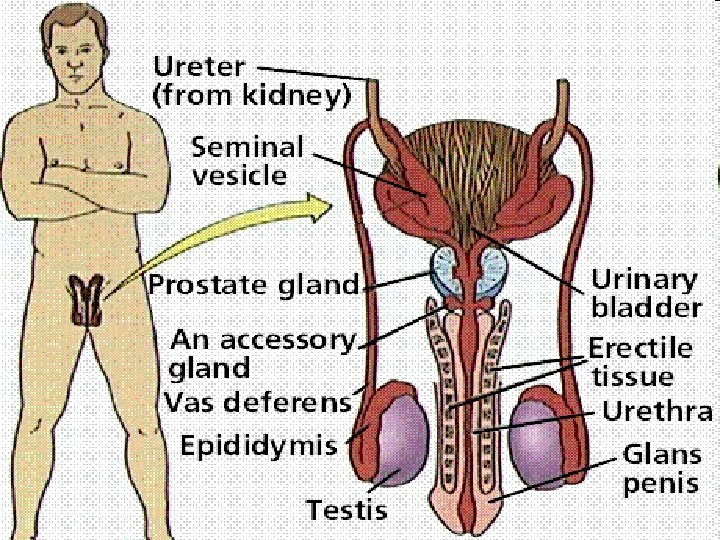
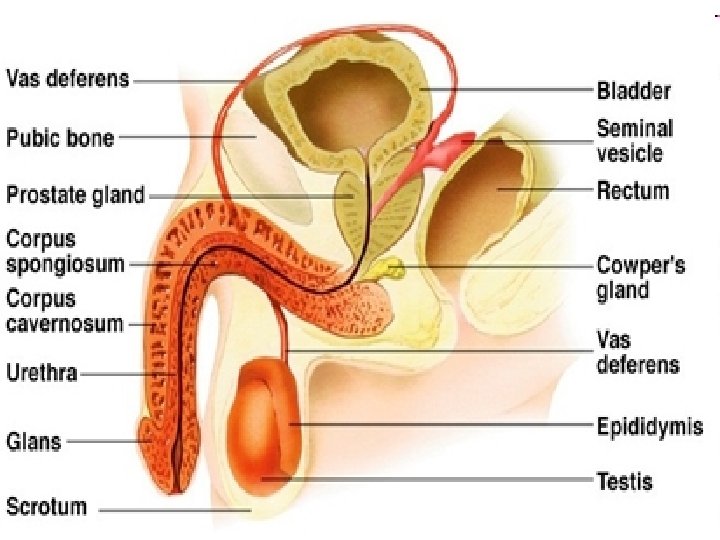
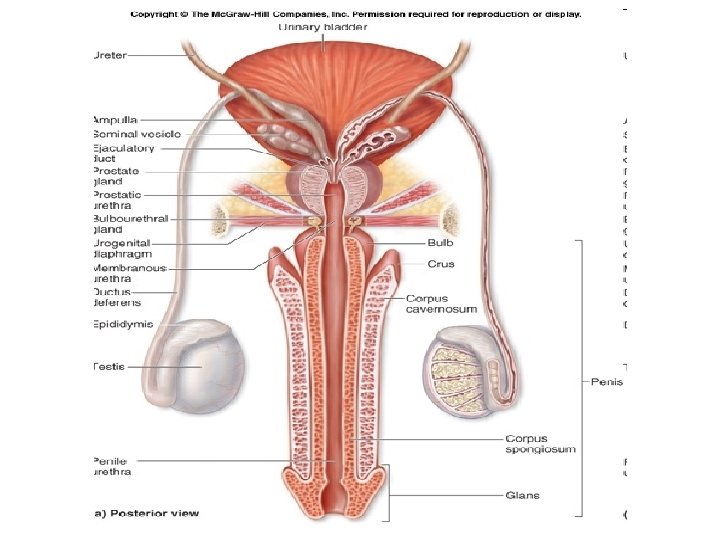
• The reproductive systems of males and females, respectively, are divided into two parts: - the internal reproductive organs: Male: testes, seminal vesicles, prostate gland, bulbourethral glands, vas deferens, urethra. Female: ovaries, uterus, ureters, cervix. - the external genitalia: Male: penis, scrotum. Female: vagina, clitoris. - Male: fig. 21. 1 p. 420. - Female: fig. 21. 5 p. 424.
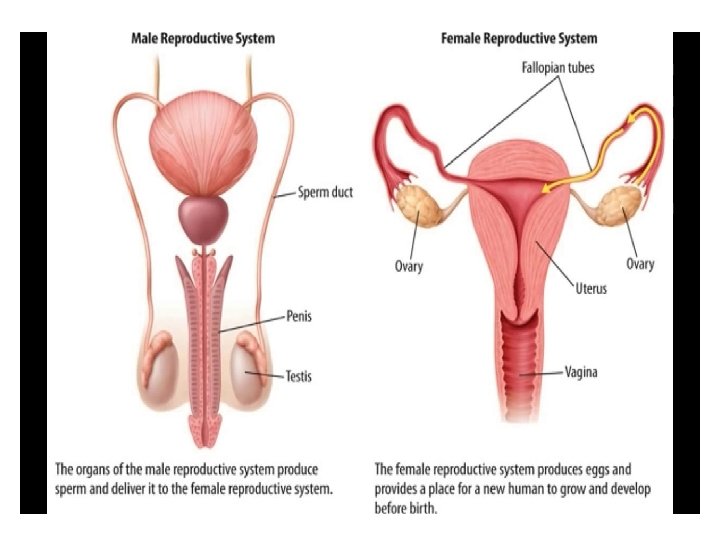
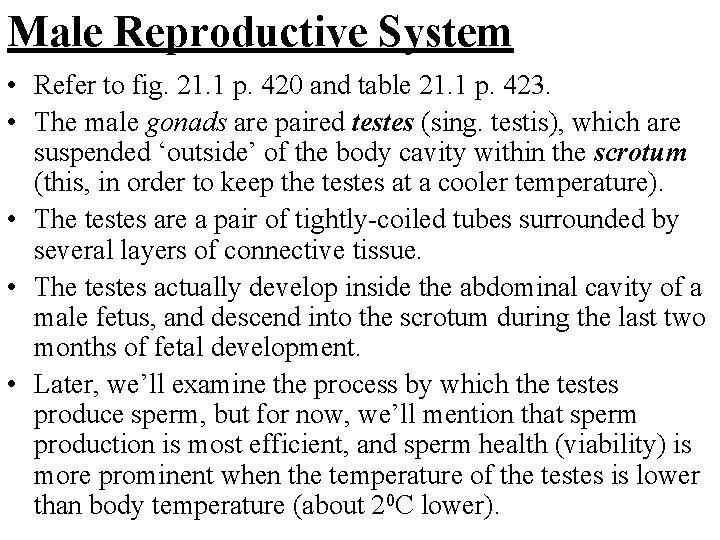
Male Reproductive System • Refer to fig. 21. 1 p. 420 and table 21. 1 p. 423. • The male gonads are paired testes (sing. testis), which are suspended ‘outside’ of the body cavity within the scrotum (this, in order to keep the testes at a cooler temperature). • The testes are a pair of tightly-coiled tubes surrounded by several layers of connective tissue. • The testes actually develop inside the abdominal cavity of a male fetus, and descend into the scrotum during the last two months of fetal development. • Later, we’ll examine the process by which the testes produce sperm, but for now, we’ll mention that sperm production is most efficient, and sperm health (viability) is more prominent when the temperature of the testes is lower than body temperature (about 20 C lower).
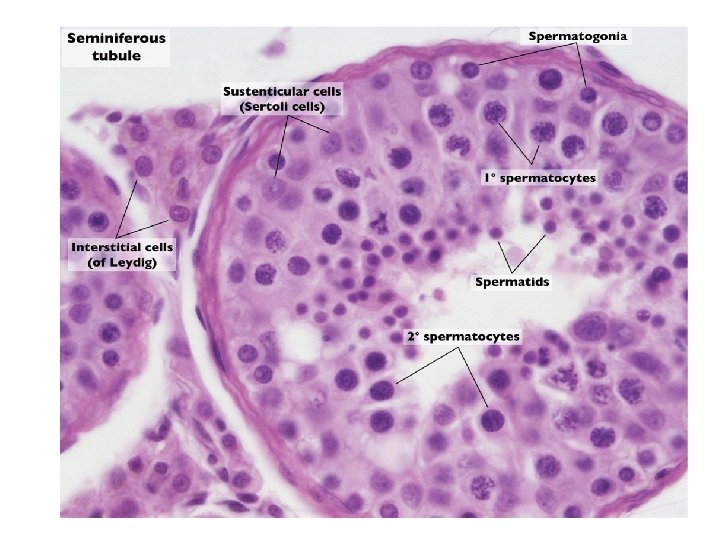
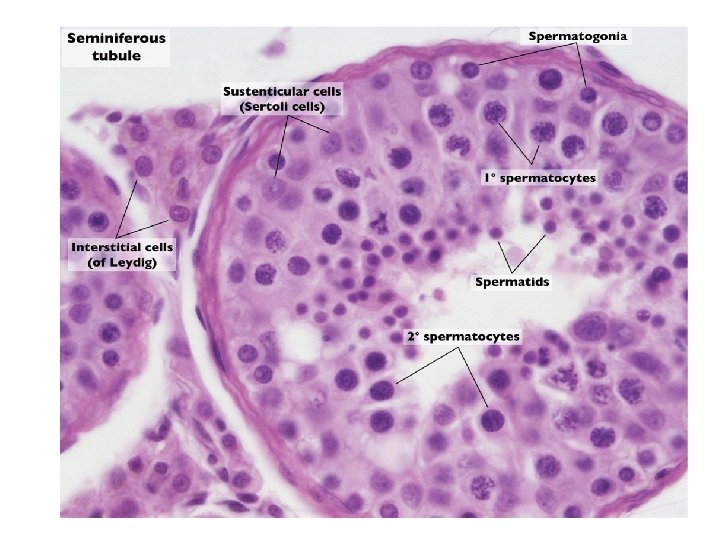
Anatomy/Physiology of the Testes (fig. 21. 3 p. 422): i. Seminiferous Tubules – make up the ‘tubular’ portion of the testes (uncoiled = length of about 250 m); they are primarily responsible for producing sperm cells (a process known as spermatogenesis); they are packed with immature sperm cells called spermatogonia at their outer tubule walls; these spermatogonia eventually mature to become sperm cells. ii. Sertoli Cells – support, nourish, and regulate cells that are destined to become sperm cells; they also secrete the hormone inhibin as sperm cells are produced in order to regulate their numbers (a form of negative feedback). iii. Interstitial (Leydig) Cells – scattered between the seminiferous tubules they produce testosterone (the primary male sex hormone).
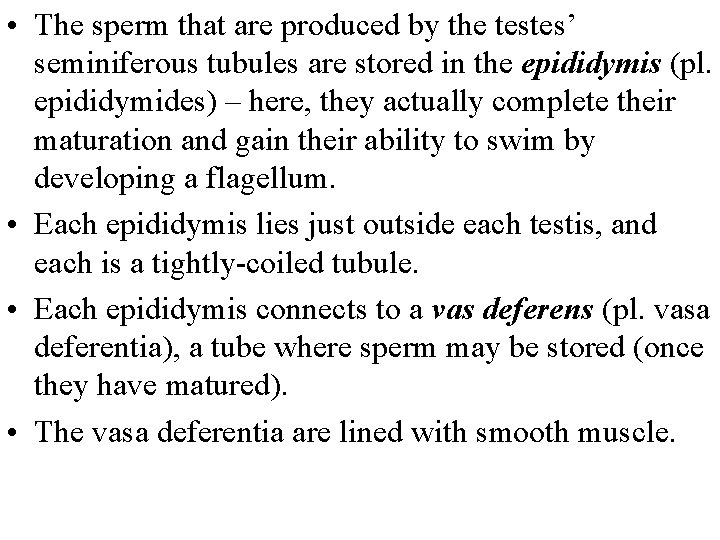
• The sperm that are produced by the testes’ seminiferous tubules are stored in the epididymis (pl. epididymides) – here, they actually complete their maturation and gain their ability to swim by developing a flagellum. • Each epididymis lies just outside each testis, and each is a tightly-coiled tubule. • Each epididymis connects to a vas deferens (pl. vasa deferentia), a tube where sperm may be stored (once they have matured). • The vasa deferentia are lined with smooth muscle.
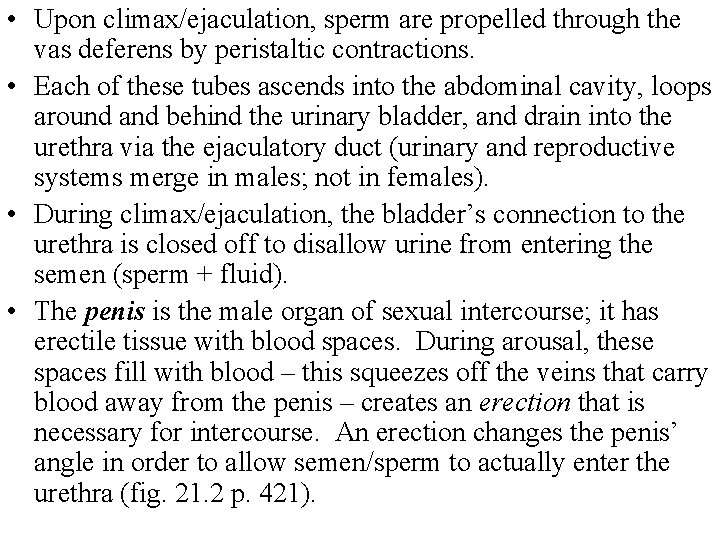
• Upon climax/ejaculation, sperm are propelled through the vas deferens by peristaltic contractions. • Each of these tubes ascends into the abdominal cavity, loops around and behind the urinary bladder, and drain into the urethra via the ejaculatory duct (urinary and reproductive systems merge in males; not in females). • During climax/ejaculation, the bladder’s connection to the urethra is closed off to disallow urine from entering the semen (sperm + fluid). • The penis is the male organ of sexual intercourse; it has erectile tissue with blood spaces. During arousal, these spaces fill with blood – this squeezes off the veins that carry blood away from the penis – creates an erection that is necessary for intercourse. An erection changes the penis’ angle in order to allow semen/sperm to actually enter the urethra (fig. 21. 2 p. 421).
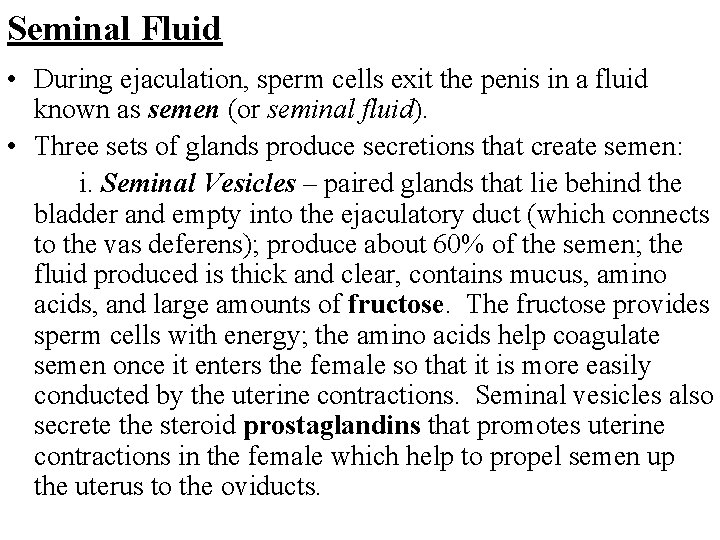
Seminal Fluid • During ejaculation, sperm cells exit the penis in a fluid known as semen (or seminal fluid). • Three sets of glands produce secretions that create semen: i. Seminal Vesicles – paired glands that lie behind the bladder and empty into the ejaculatory duct (which connects to the vas deferens); produce about 60% of the semen; the fluid produced is thick and clear, contains mucus, amino acids, and large amounts of fructose. The fructose provides sperm cells with energy; the amino acids help coagulate semen once it enters the female so that it is more easily conducted by the uterine contractions. Seminal vesicles also secrete the steroid prostaglandins that promotes uterine contractions in the female which help to propel semen up the uterus to the oviducts.
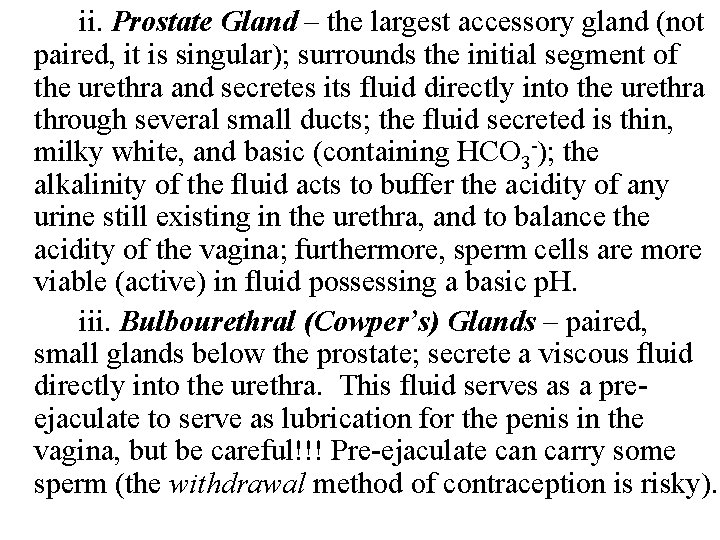
ii. Prostate Gland – the largest accessory gland (not paired, it is singular); surrounds the initial segment of the urethra and secretes its fluid directly into the urethra through several small ducts; the fluid secreted is thin, milky white, and basic (containing HCO 3 -); the alkalinity of the fluid acts to buffer the acidity of any urine still existing in the urethra, and to balance the acidity of the vagina; furthermore, sperm cells are more viable (active) in fluid possessing a basic p. H. iii. Bulbourethral (Cowper’s) Glands – paired, small glands below the prostate; secrete a viscous fluid directly into the urethra. This fluid serves as a preejaculate to serve as lubrication for the penis in the vagina, but be careful!!! Pre-ejaculate can carry some sperm (the withdrawal method of contraception is risky).
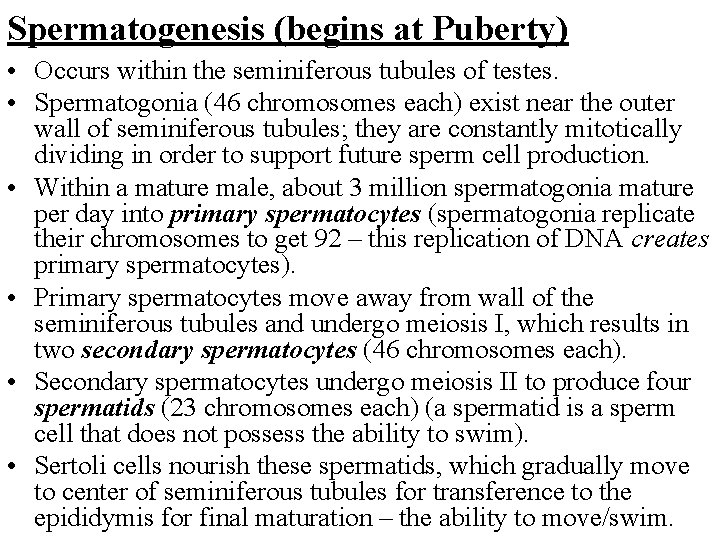
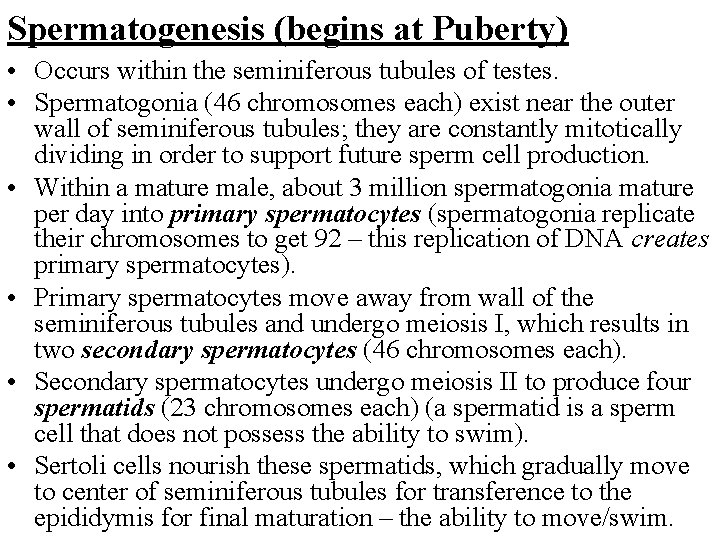
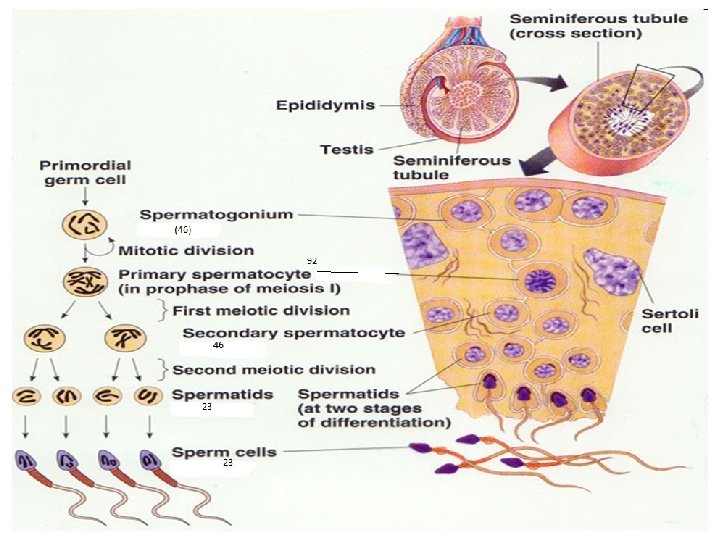
Spermatogenesis (begins at Puberty) • Occurs within the seminiferous tubules of testes. • Spermatogonia (46 chromosomes each) exist near the outer wall of seminiferous tubules; they are constantly mitotically dividing in order to support future sperm cell production. • Within a mature male, about 3 million spermatogonia mature per day into primary spermatocytes (spermatogonia replicate their chromosomes to get 92 – this replication of DNA creates primary spermatocytes). • Primary spermatocytes move away from wall of the seminiferous tubules and undergo meiosis I, which results in two secondary spermatocytes (46 chromosomes each). • Secondary spermatocytes undergo meiosis II to produce four spermatids (23 chromosomes each) (a spermatid is a sperm cell that does not possess the ability to swim). • Sertoli cells nourish these spermatids, which gradually move to center of seminiferous tubules for transference to the epididymis for final maturation – the ability to move/swim.
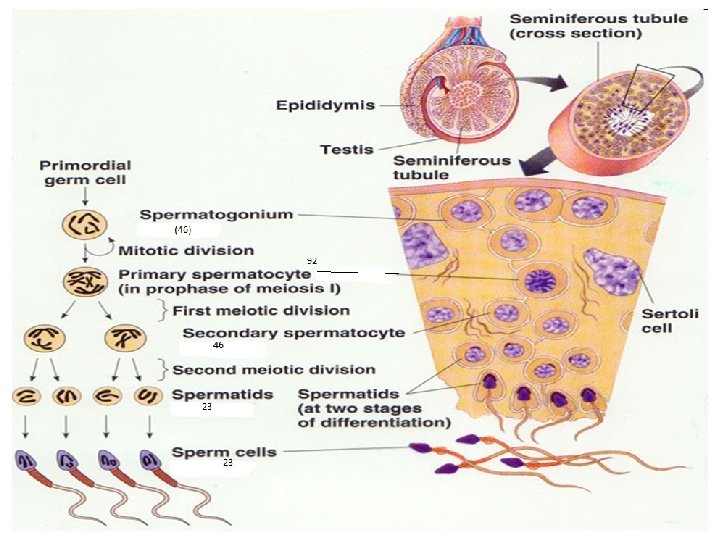
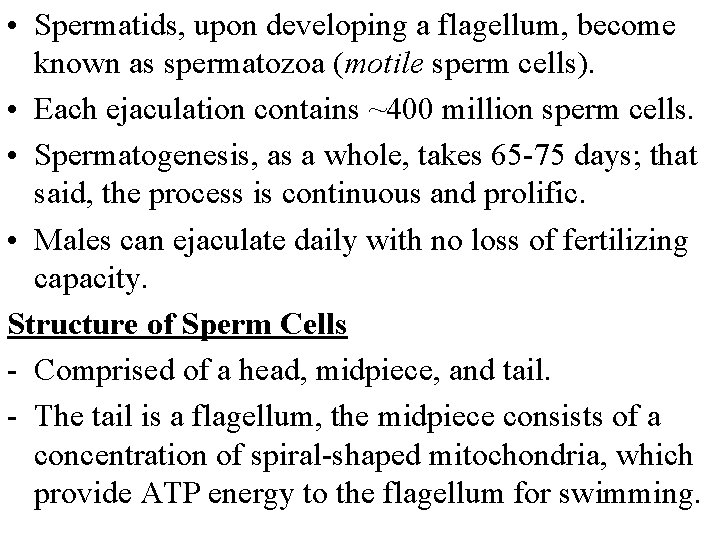
• Spermatids, upon developing a flagellum, become known as spermatozoa (motile sperm cells). • Each ejaculation contains ~400 million sperm cells. • Spermatogenesis, as a whole, takes 65 -75 days; that said, the process is continuous and prolific. • Males can ejaculate daily with no loss of fertilizing capacity. Structure of Sperm Cells - Comprised of a head, midpiece, and tail. - The tail is a flagellum, the midpiece consists of a concentration of spiral-shaped mitochondria, which provide ATP energy to the flagellum for swimming.
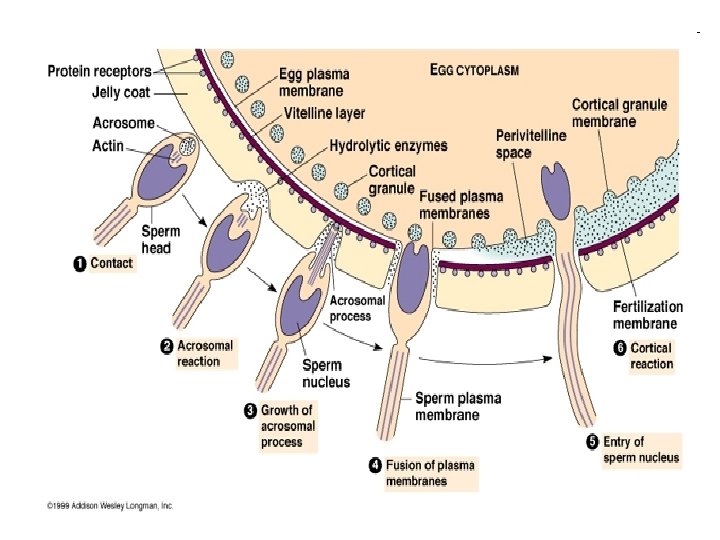
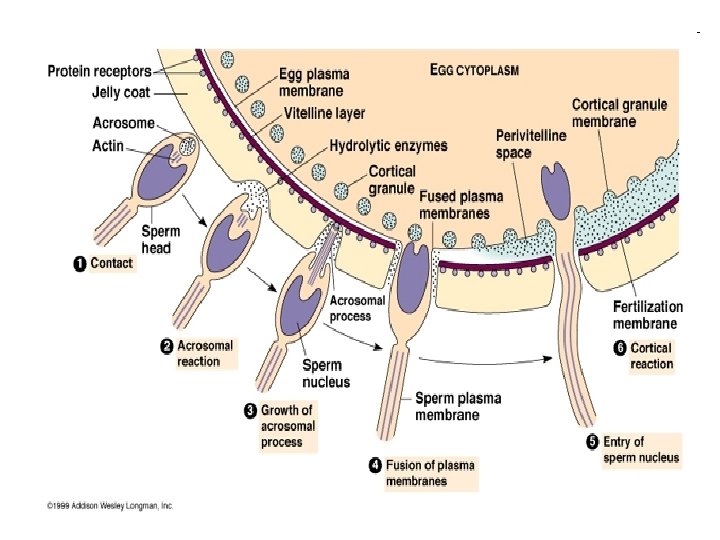
• The head contains the nucleus (23 chromosomes), which is behind, and therefore protected by, the acrosome – a specialized lysosome containing enzymes required to penetrate the ovum (egg cell) so that DNA may be injected into the egg in order to fertilize it. • Only one sperm penetrates and injects its DNA into an egg. This is because after fertilization, an egg’s membrane alters its chemical composition so that the acrosomal enzymes are no longer able to penetrate it.

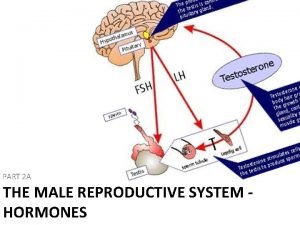
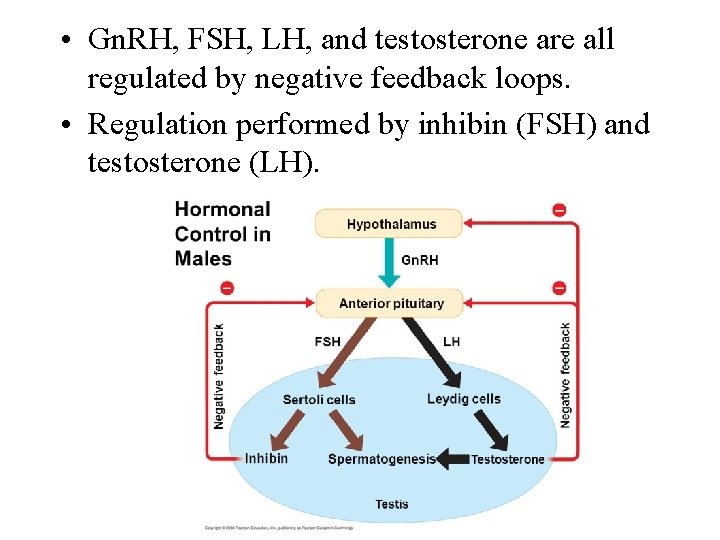
Hormonal Control (Male Sex Hormones) • • See fig. 21. 4 p. 423. The hypothalamus possesses the ultimate control over the testes with respect to spermatogenesis and testosterone production. The hypothalamus governs by secreting gonadotropin-releasing hormone (Gn. RH), which travels a short distance to stimulate the anterior pituitary gland to release the gonadotropic hormones follicle-stimulating hormone (FSH) and luteinizing hormone (LH). • FSH has two effects: 1. Promotes spermatogenesis in the seminiferous tubules of the testes; 2. Promotes production of hormone inhibin in the Sertoli cells of the testes.
• More specifically, FSH stimulates spermatogonia (on the edges of the seminiferous tubules) to become primary spermatocytes. • Inhibin feeds back negatively on the anterior pituitary to slow/stop FSH release so that epididymis is not overloaded with sperm. • LH targets the interstitial cells of the testes and stimulates them to produce testosterone, the primary sex hormone in males. • Testosterone is directly responsible for the development of the primary and secondary sexual characteristics of males. • The primary characteristics include those associated with the actual reproductive system – development of the vasa deferentia, the penis, scrotum, and testes (these characteristics are associated with pre-puberty testosterone).
• Testosterone is also responsible for a male’s sex drive and erections, which are lower during prepuberty years. • At puberty, Gn. RH secretions increase, which leads to increased FSH, LH, spermatogenesis, and testosterone. • In an interesting hormonal cross-over, testosterone also plays an important role in spermatogenesis FSH stimulates developing sperm cells to absorb testosterone, which promotes the maturation of sperm cells (ie. Without testosterone, sperm would not be mature or viable).
• Puberty-associated testosterone promotes a male’s secondary sexual characteristics, including: - increased facial/body hair; - growth of larynx (deeper voice, larger Adam’s Apple); - greater skeletal muscle development; - increased oil/sweat gland secretions (pimples); - possible receding hairline; - increased height, broader shoulders, longer legs relative to trunk length (relative to females). *Increased testosterone at puberty also contributes to further maturation of the primary characteristics (ie. leads to final maturation of penis and testes, increased sex drive etc. ). *Testosterone levels in blood feed back negatively upon the hypothalamus and the anterior pituitary to slow/stop Gn. RH/LH release so as to regulate testosterone (ie. testosterone regulates itself!)
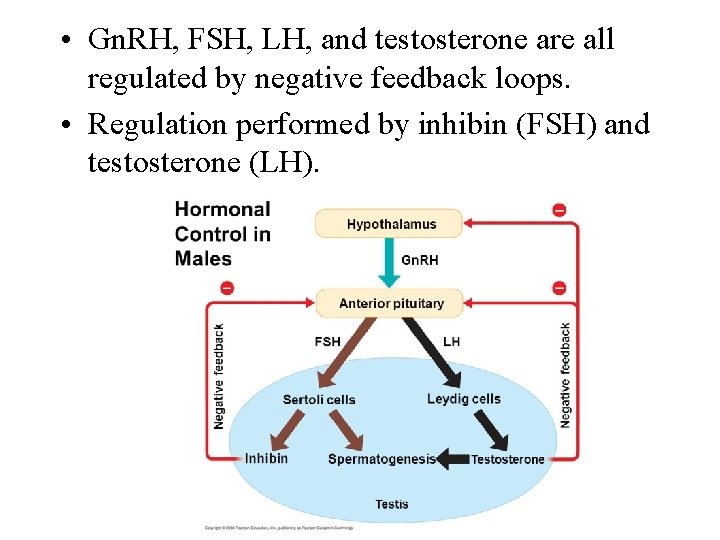
• Gn. RH, FSH, LH, and testosterone are all regulated by negative feedback loops. • Regulation performed by inhibin (FSH) and testosterone (LH).
 Female testes
Female testes Male fallopian tube
Male fallopian tube Similarities between male and female reproductive system
Similarities between male and female reproductive system 90/2
90/2 Similarities between female and male reproductive system
Similarities between female and male reproductive system Cartilaginous fish reproduction
Cartilaginous fish reproduction Ovarian ligament
Ovarian ligament Reproductive system function
Reproductive system function Function of reproductive organs
Function of reproductive organs Pearson education
Pearson education What are primary sexual characteristics
What are primary sexual characteristics Function of cervix
Function of cervix Exercise 42 review male reproductive system
Exercise 42 review male reproductive system Oogenesis diagram
Oogenesis diagram Dot quizlet
Dot quizlet Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Reproduction in human
Reproduction in human Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where semen is stored
Where semen is stored Cow male reproductive system
Cow male reproductive system Seminal duct
Seminal duct Male reproductive system plants
Male reproductive system plants Disease traductor
Disease traductor Uterus is the part of which system in pila...?
Uterus is the part of which system in pila...? Male fetal pig reproductive system labeled
Male fetal pig reproductive system labeled Male plant reproductive system
Male plant reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland