Meiosis Where does meiosis occur Where does mitosis
- Slides: 87
Meiosis Where does meiosis occur? Where does mitosis occur? What is the difference between them?
Meiosis Where does meiosis occur? Gonads Where does mitosis occur? Somatic Cells What is the difference between them? Mitosis is diploid and meiosis is haploid
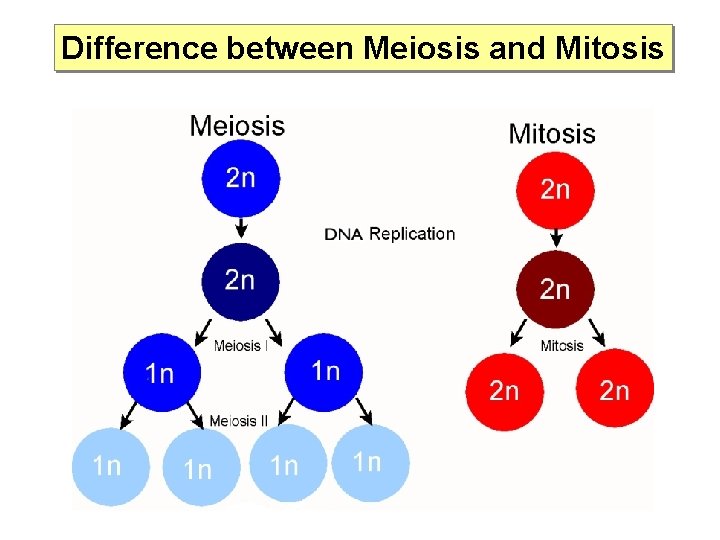
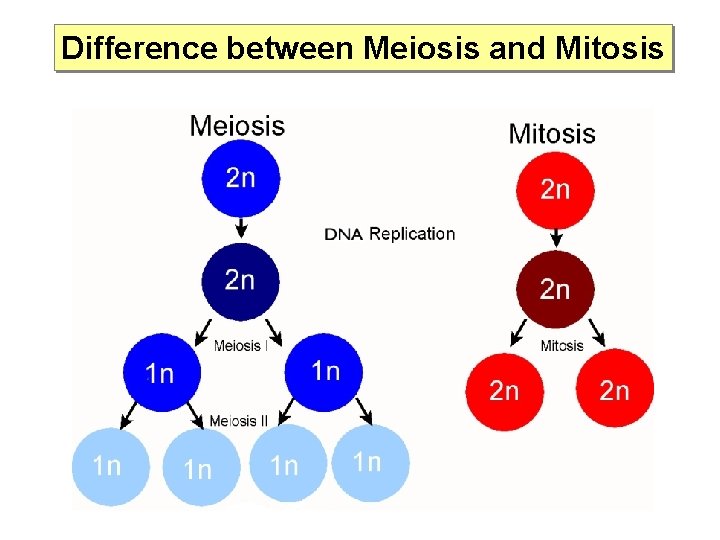
Difference between Meiosis and Mitosis
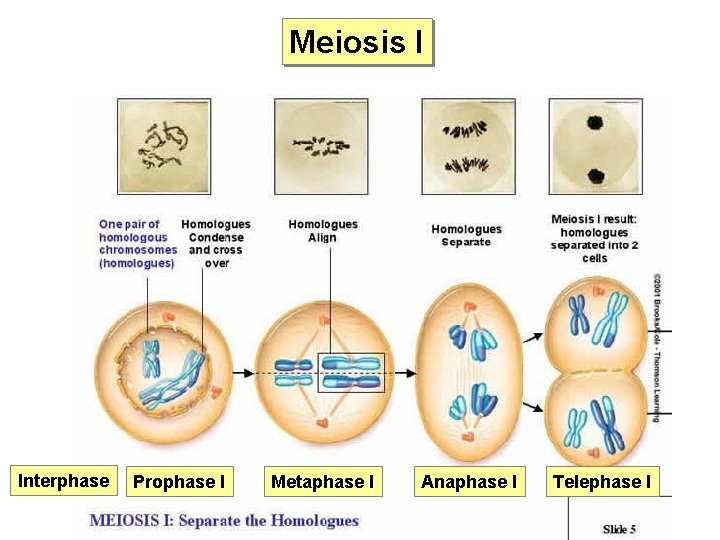
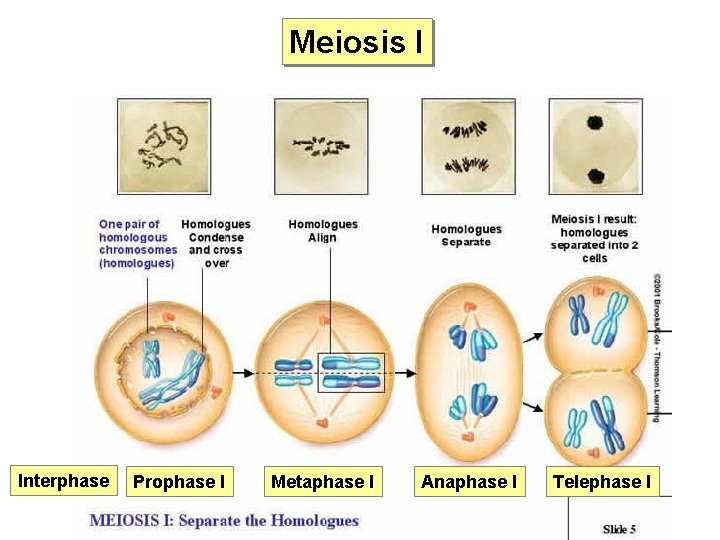
Meiosis I Interphase Prophase I Metaphase I Anaphase I Telephase I
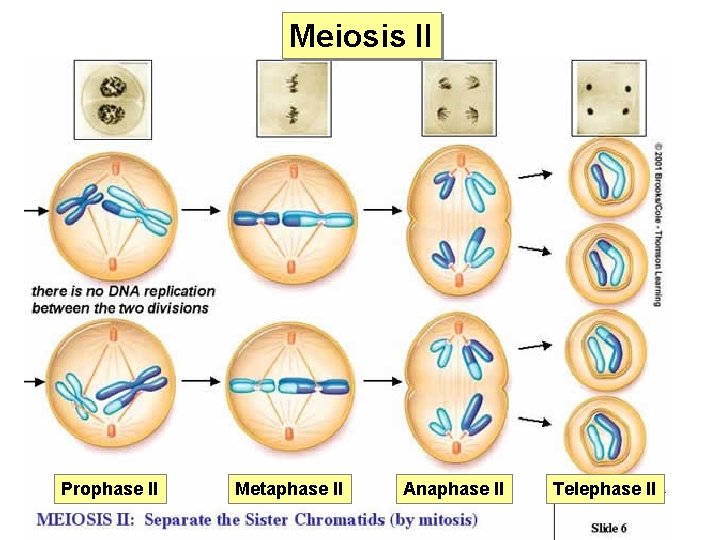
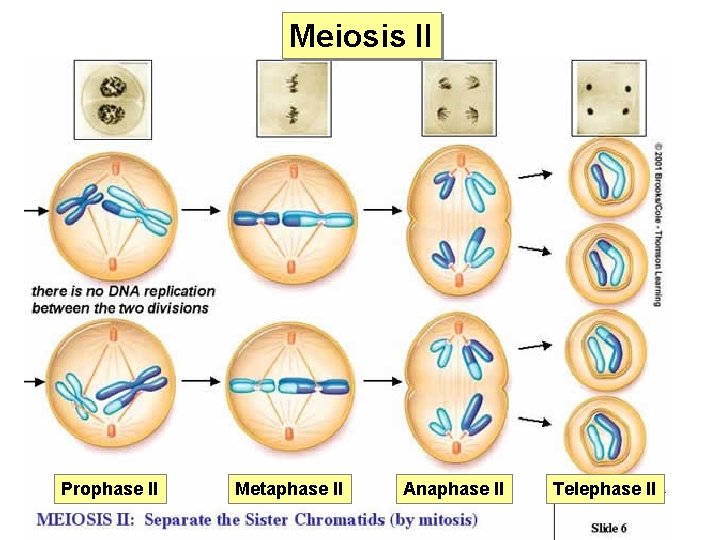
Meiosis II Prophase II Metaphase II Anaphase II Telephase II
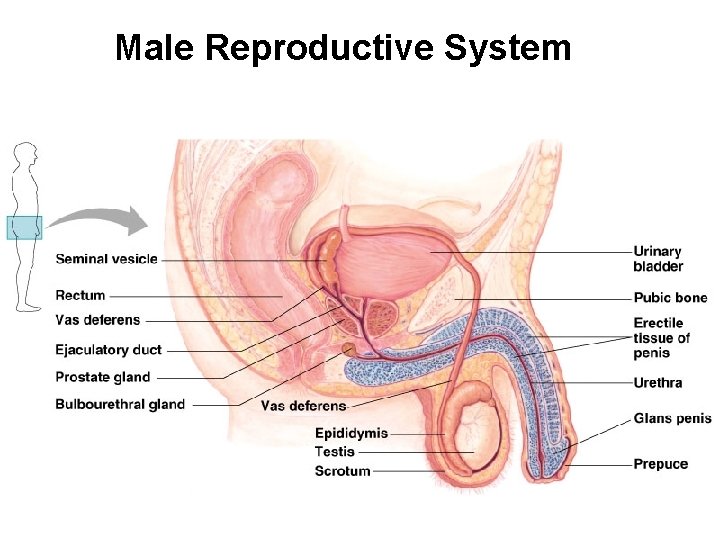
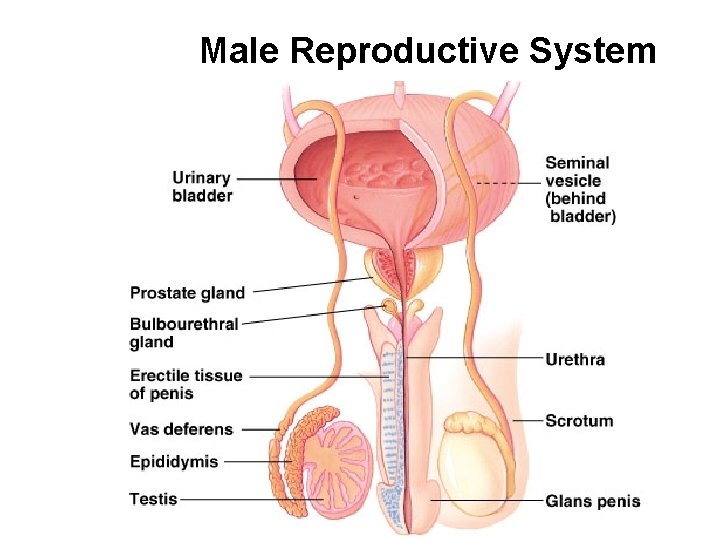
Male Reproductive System
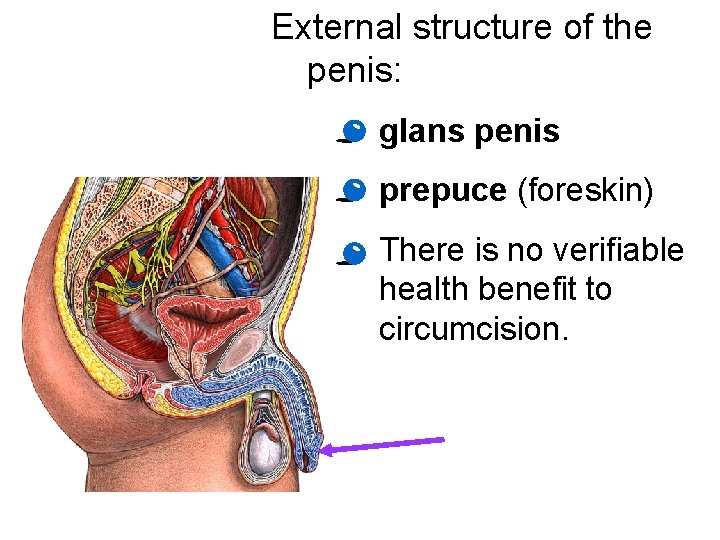
Human reproduction involves intricate anatomy and complex behavior Reproductive Anatomy of the Human Male. · External: - penis - scrotum · Internal: - gonads - accessory sex glands and ducts.
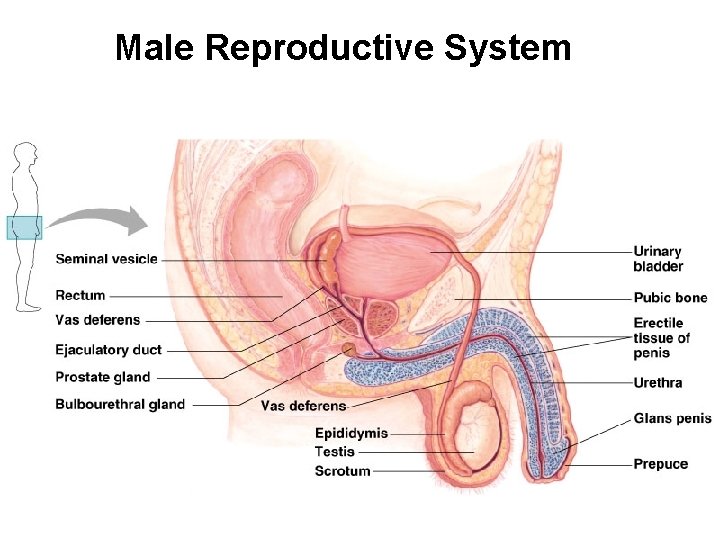
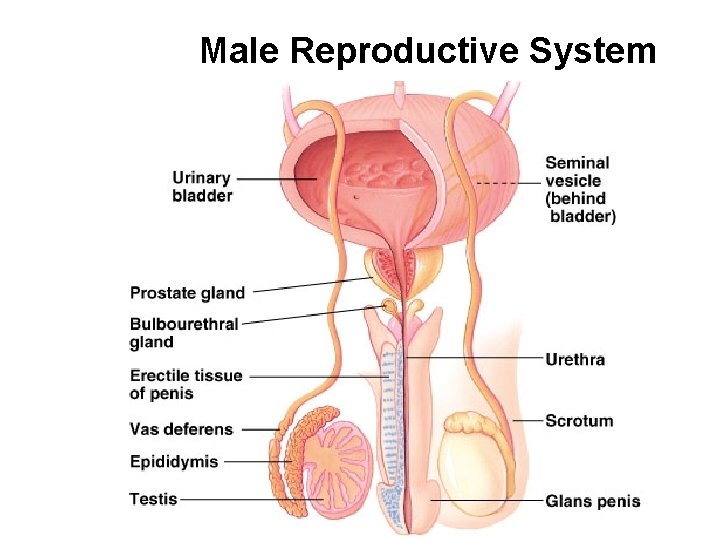
Male Reproductive System
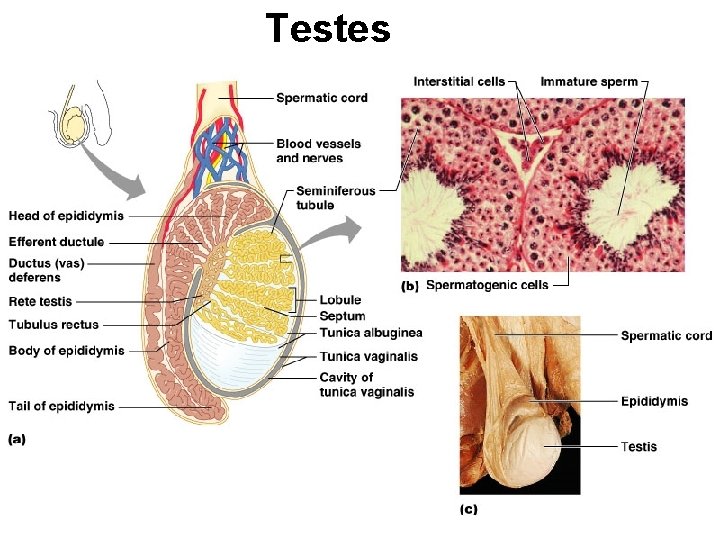
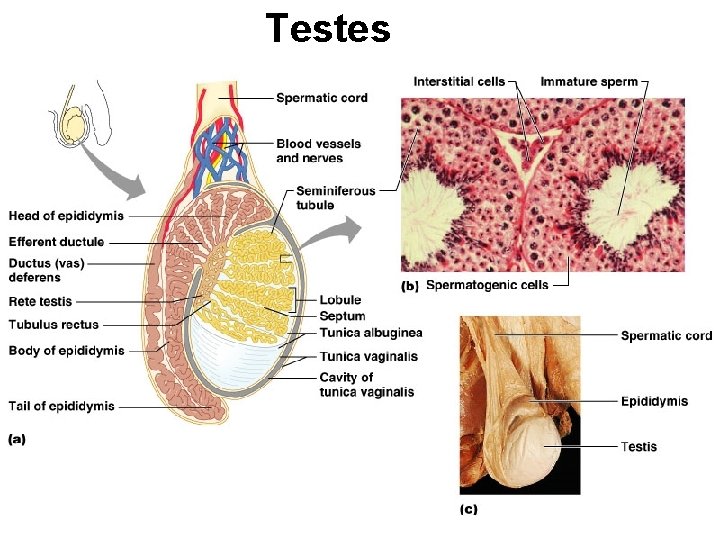
Testes
Male Reproductive System
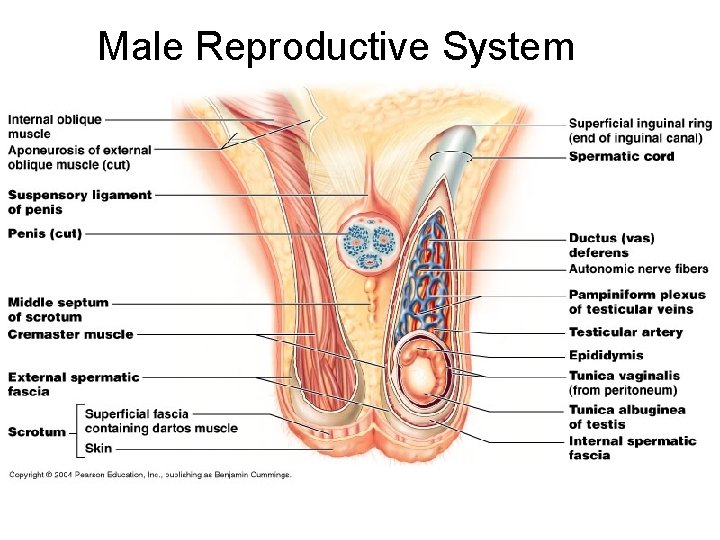
Male Reproductive System
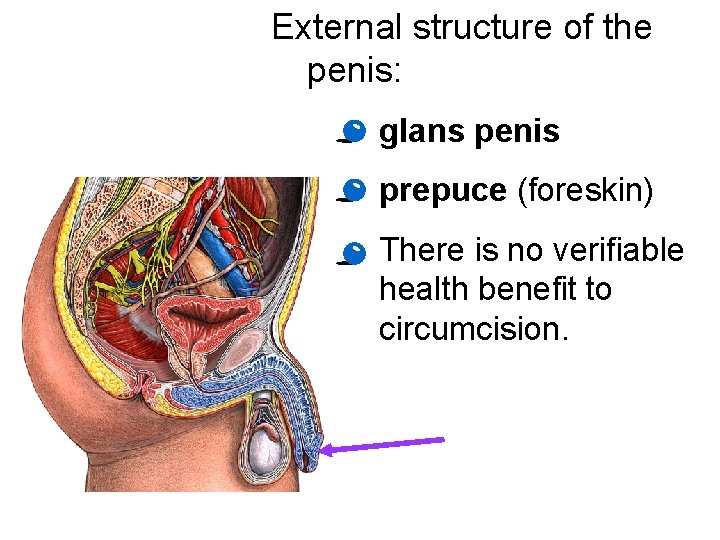
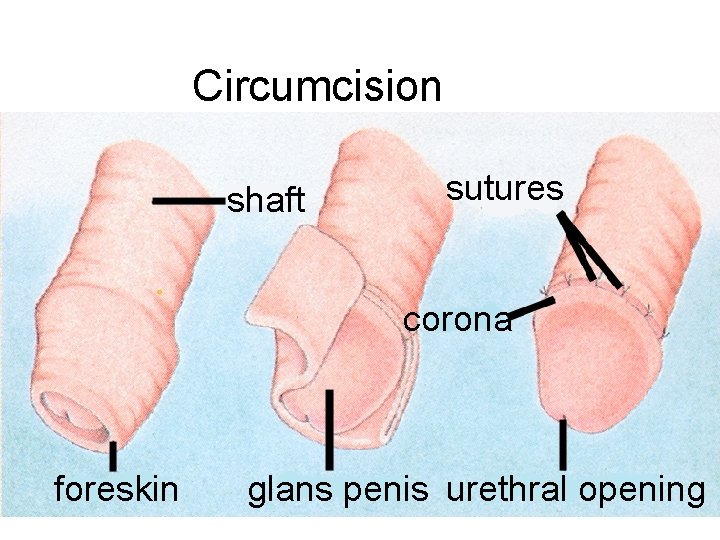
External structure of the penis: · glans penis · prepuce (foreskin) · There is no verifiable health benefit to circumcision.
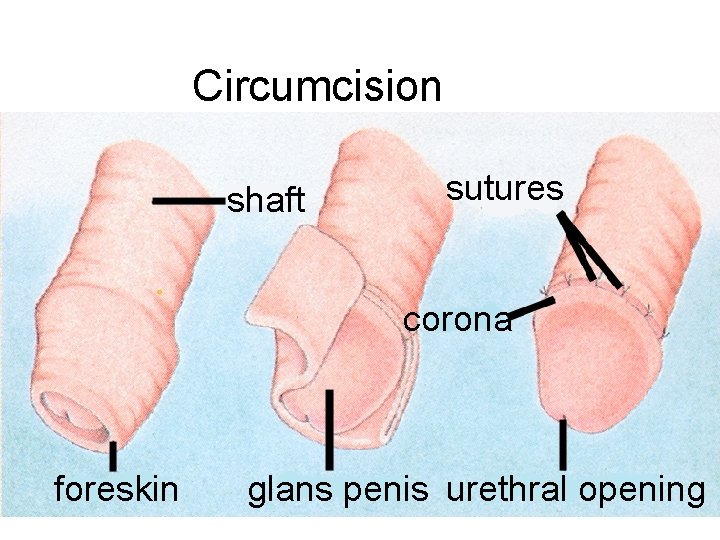
Circumcision shaft sutures corona foreskin glans penis urethral opening
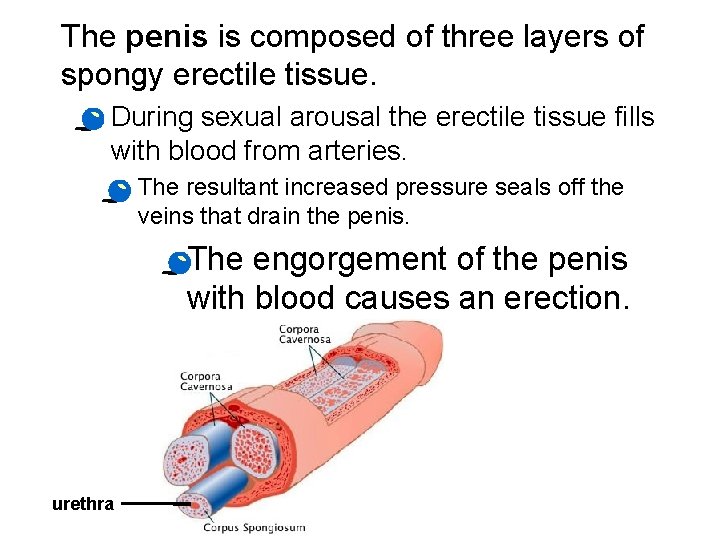
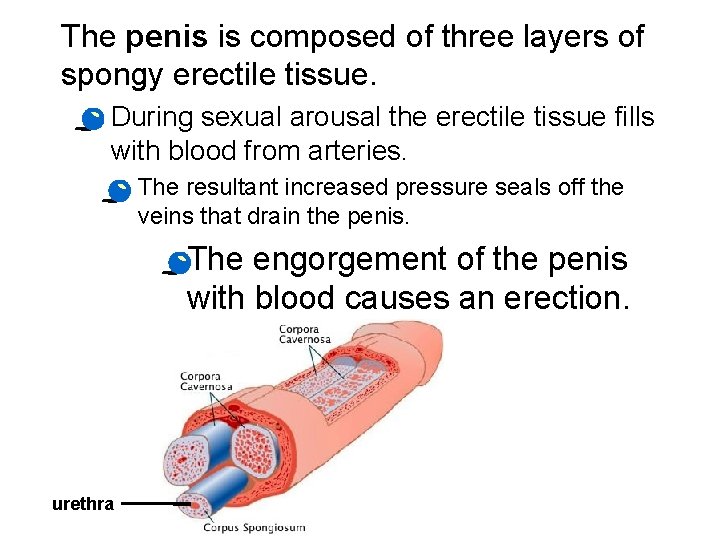
The penis is composed of three layers of spongy erectile tissue. · During sexual arousal the erectile tissue fills with blood from arteries. · The resultant increased pressure seals off the veins that drain the penis. · The engorgement of the penis with blood causes an erection. urethra
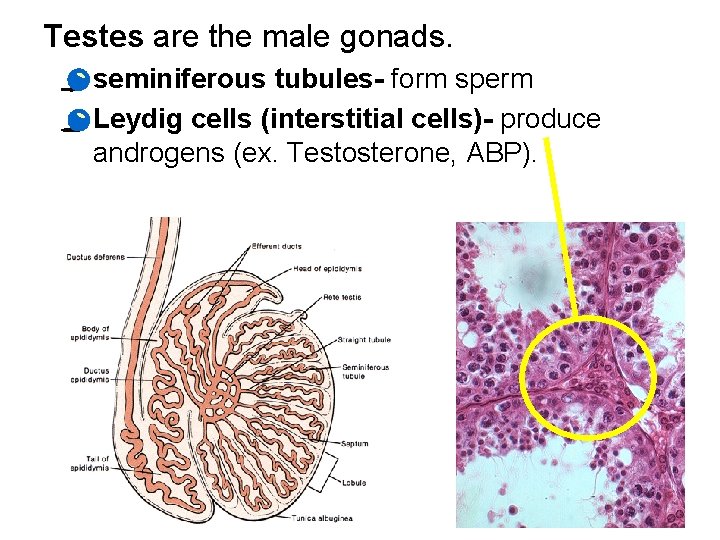
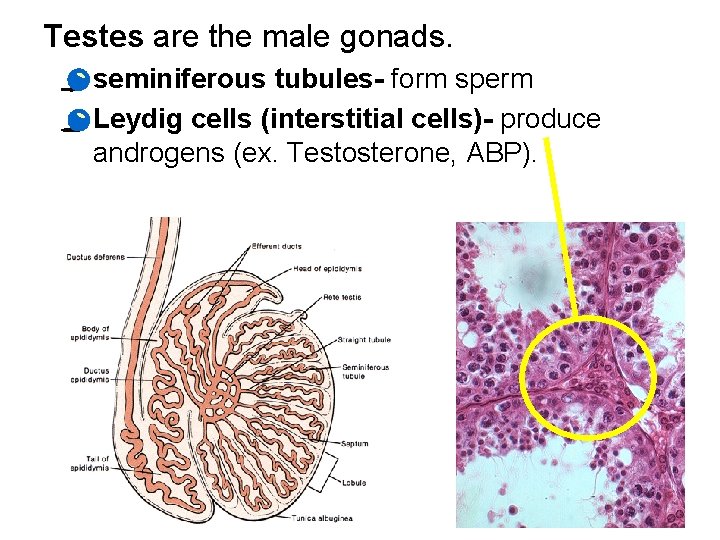
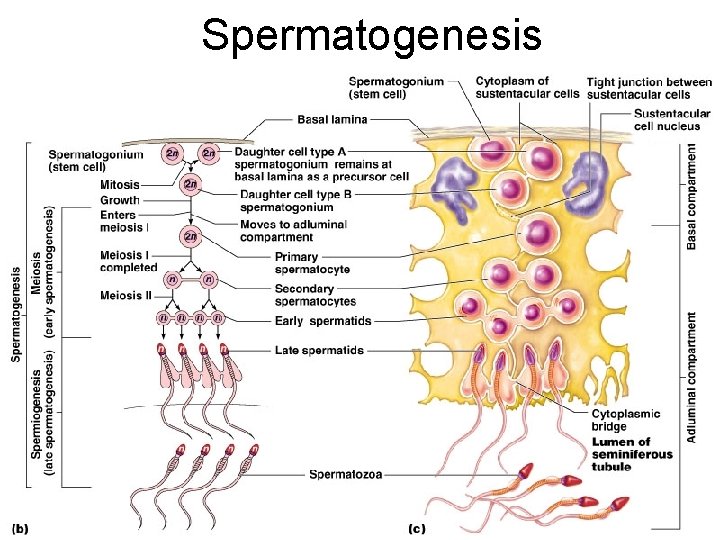
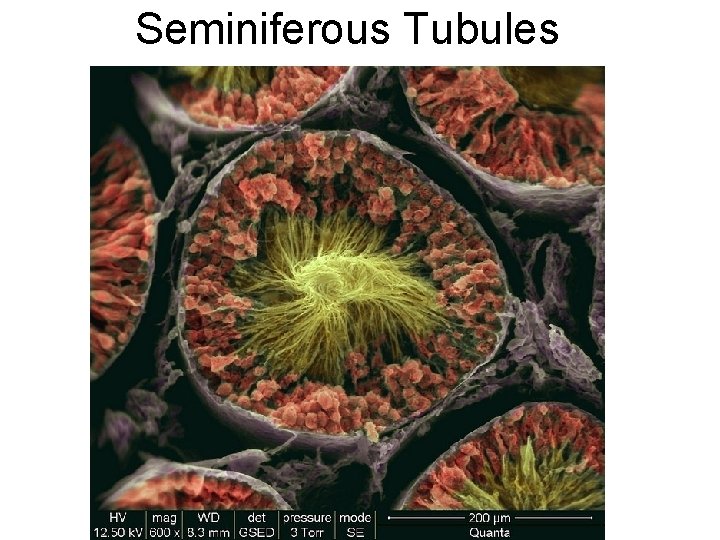
Testes are the male gonads. · seminiferous tubules- form sperm · Leydig cells (interstitial cells)- produce androgens (ex. Testosterone, ABP).
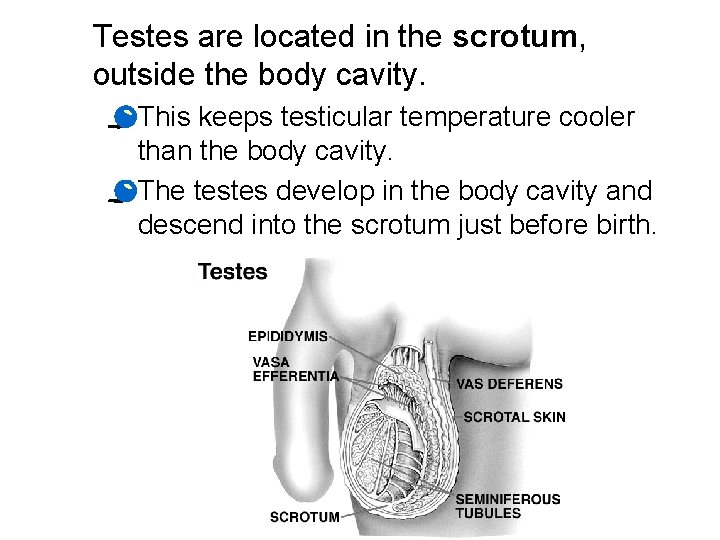
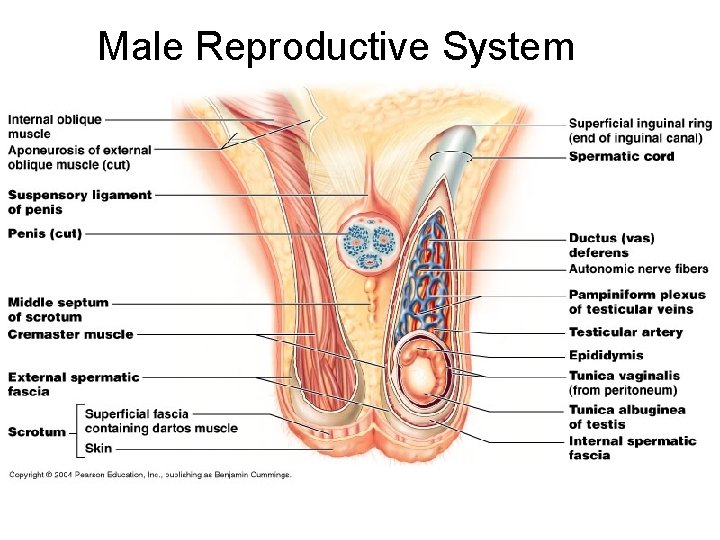
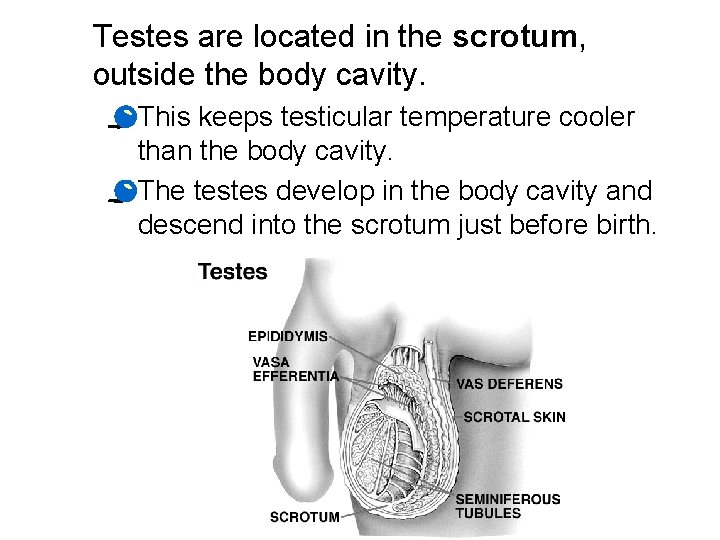
Testes are located in the scrotum, outside the body cavity. · This keeps testicular temperature cooler than the body cavity. · The testes develop in the body cavity and descend into the scrotum just before birth.
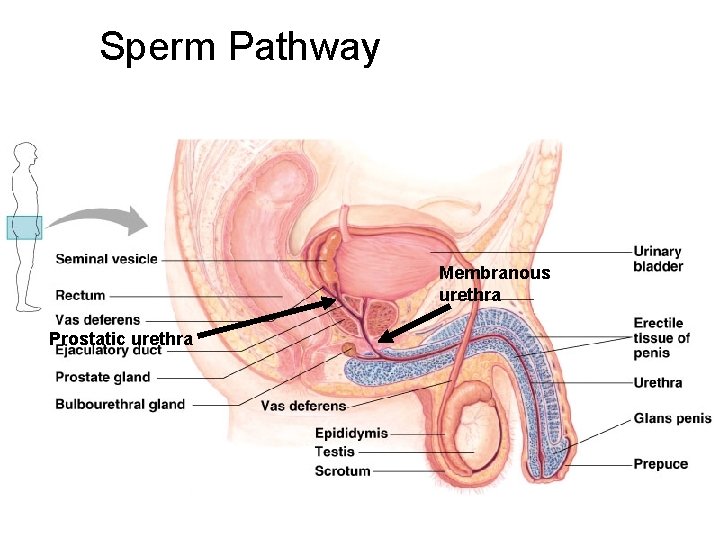
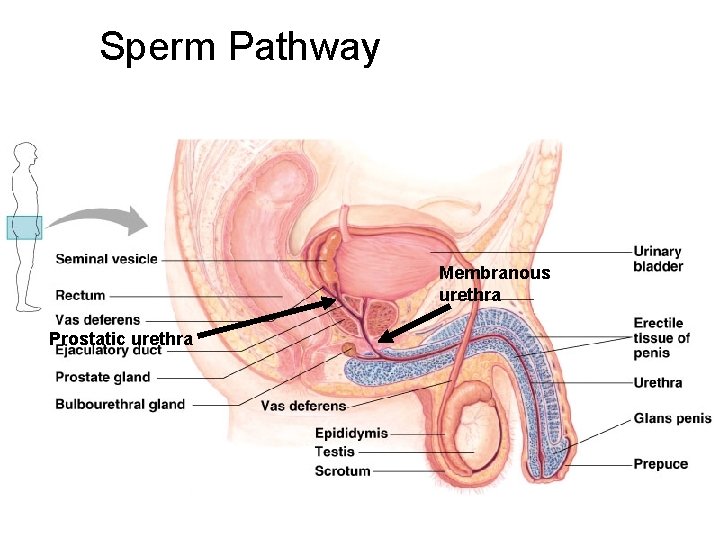
Sperm Pathway Membranous urethra Prostatic urethra
Semen · Seminal fluid is thick, yellowish, and alkaline. · It contains mucus, fructose, a coagulating enzyme, ascorbic acid, and prostaglandins. · Accessory glands: 1. seminal vesicle 2. prostate gland 3. bulbourethral gland
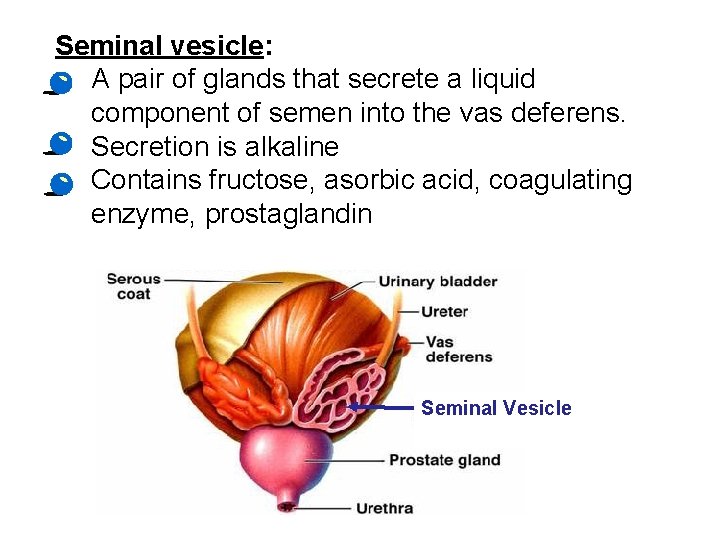
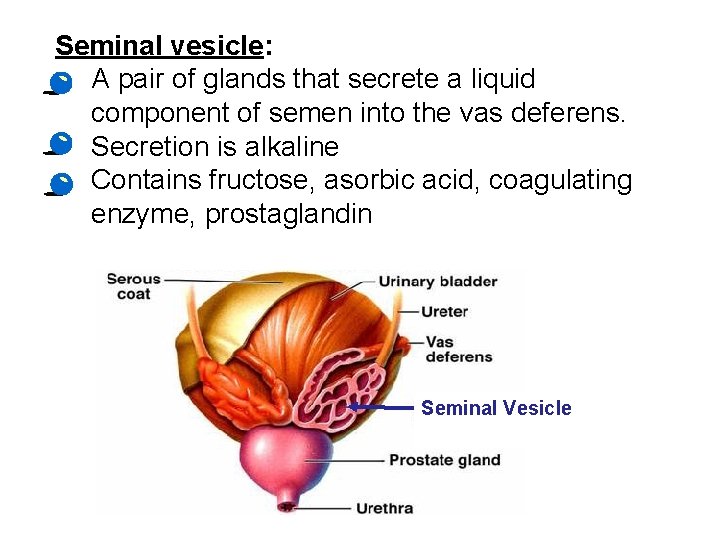
Seminal vesicle: • A pair of glands that secrete a liquid component of semen into the vas deferens. • Secretion is alkaline • Contains fructose, asorbic acid, coagulating enzyme, prostaglandin Seminal Vesicle
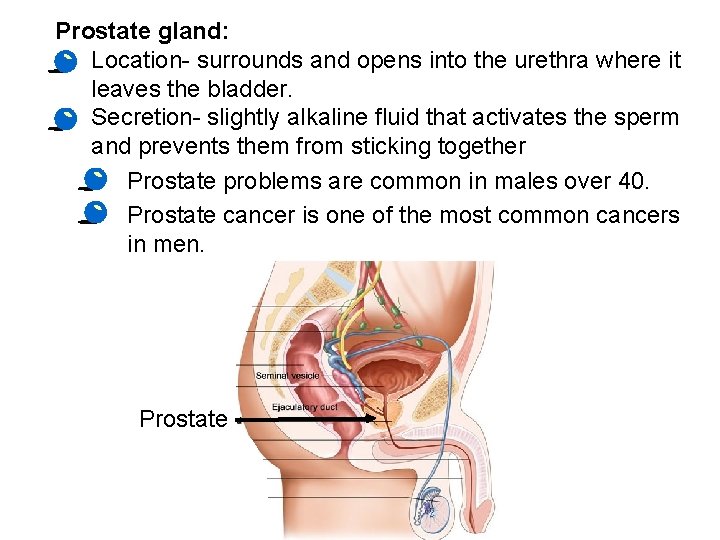
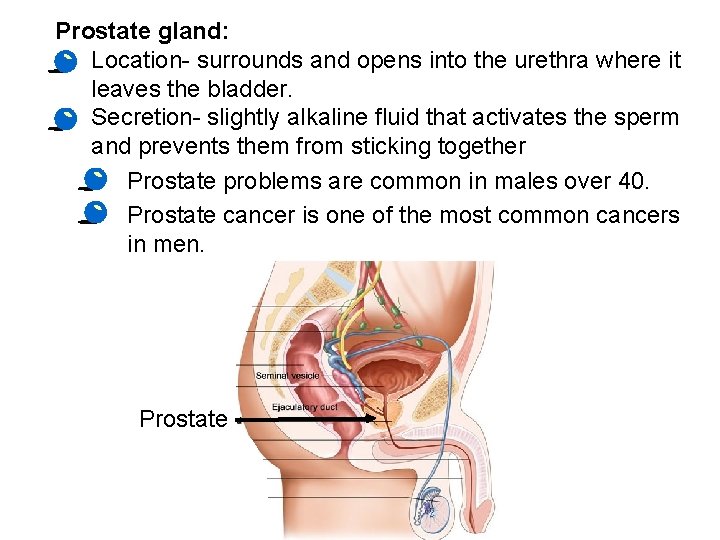
Prostate gland: • Location- surrounds and opens into the urethra where it leaves the bladder. • Secretion- slightly alkaline fluid that activates the sperm and prevents them from sticking together · Prostate problems are common in males over 40. · Prostate cancer is one of the most common cancers in men. Prostate
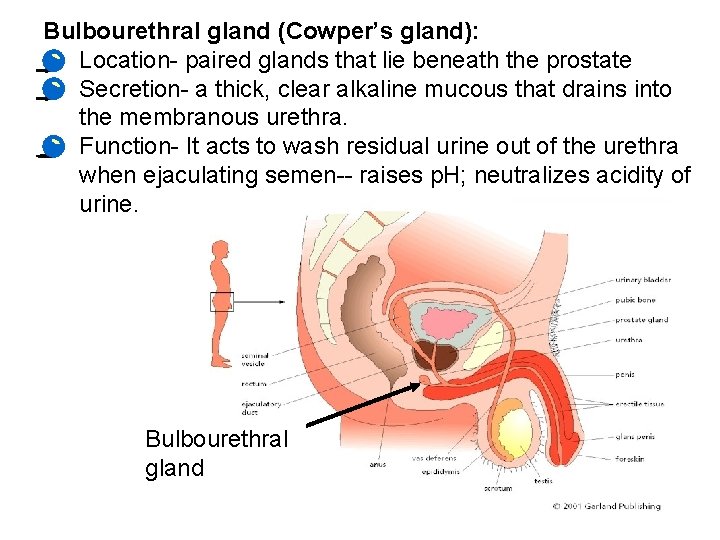
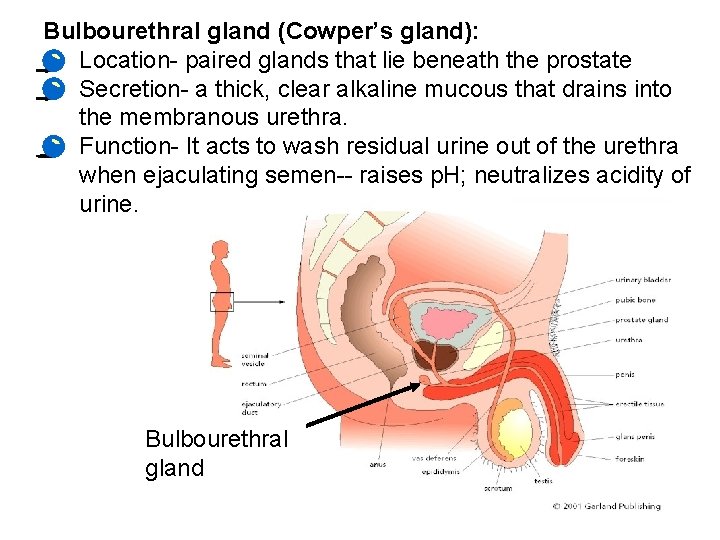
Bulbourethral gland (Cowper’s gland): • Location- paired glands that lie beneath the prostate • Secretion- a thick, clear alkaline mucous that drains into the membranous urethra. • Function- It acts to wash residual urine out of the urethra when ejaculating semen-- raises p. H; neutralizes acidity of urine. Bulbourethral gland
Ejaculation · Ejaculation propels sperm from the epididymis to the vas deferens. · The vas deferens run from the scrotum and behind the urinary bladder. · Here each vas deferens joins with a duct from the seminal vesicle to form an ejaculatory duct. · The ejaculatory ducts open into the urethra. · The urethra drains both the excretory and reproductive systems.
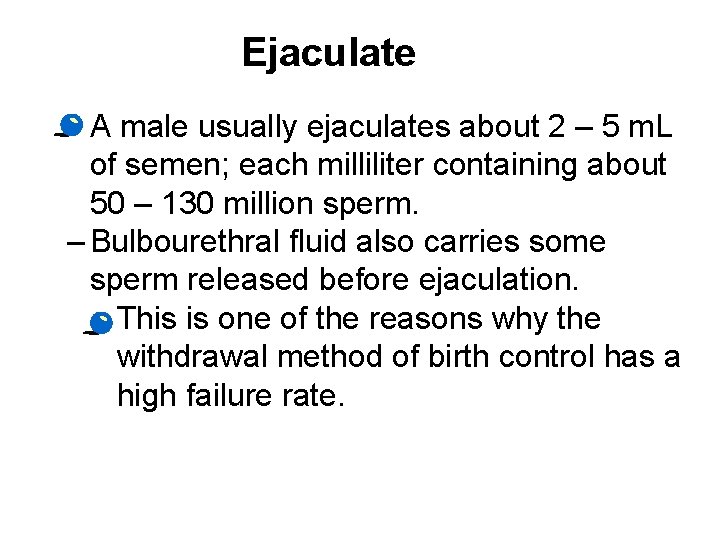
Ejaculate · A male usually ejaculates about 2 – 5 m. L of semen; each milliliter containing about 50 – 130 million sperm. – Bulbourethral fluid also carries some sperm released before ejaculation. • This is one of the reasons why the withdrawal method of birth control has a high failure rate.
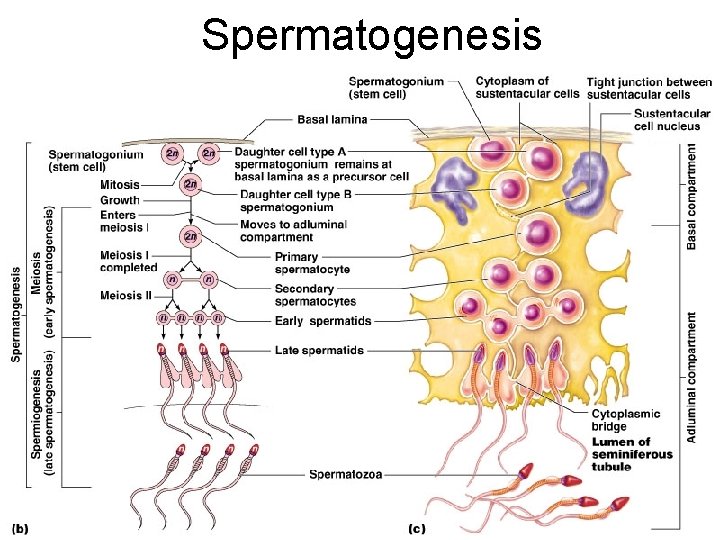
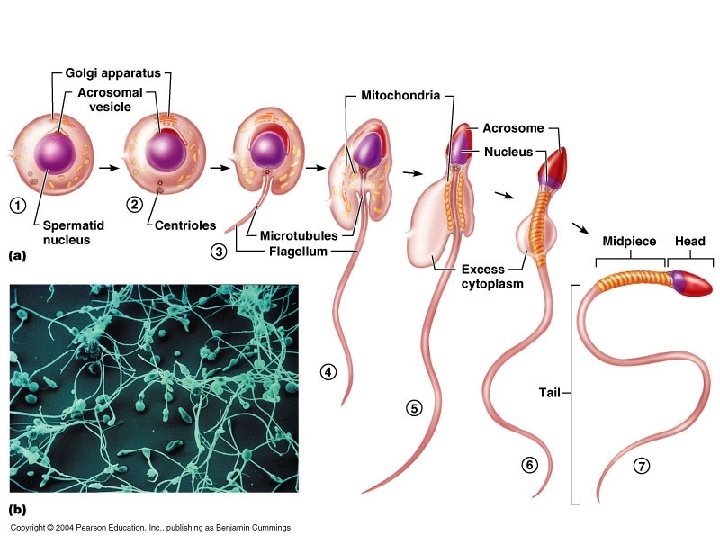
Spermatogenesis
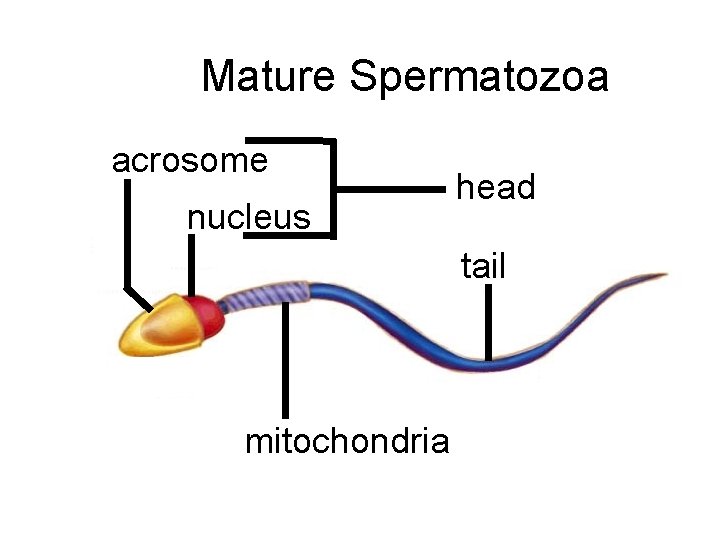
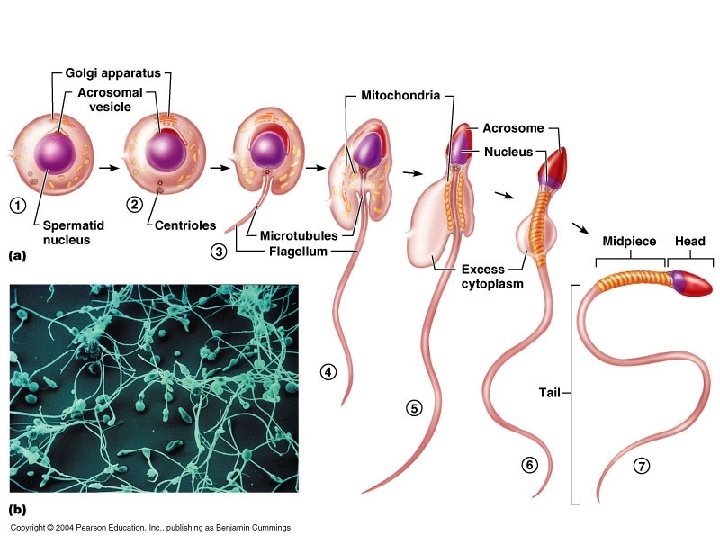
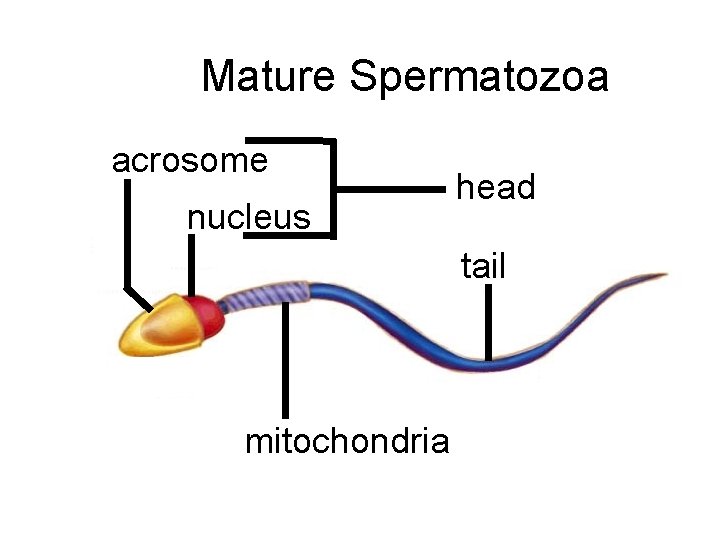
Mature Spermatozoa acrosome nucleus head tail mitochondria
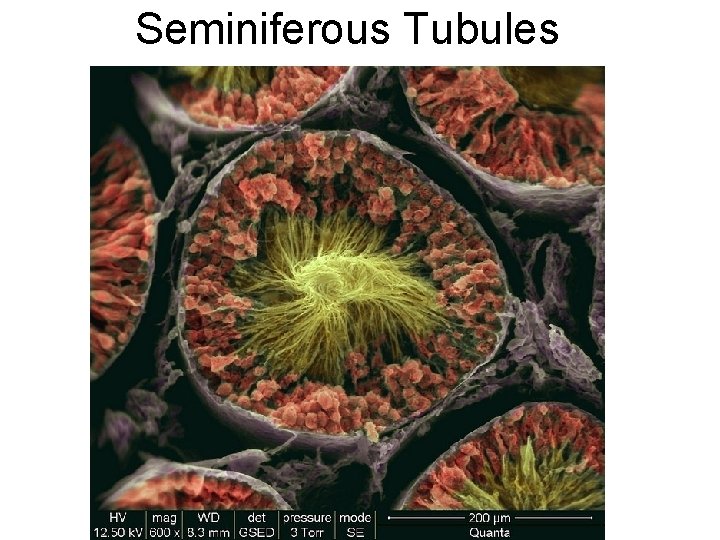
Seminiferous Tubules
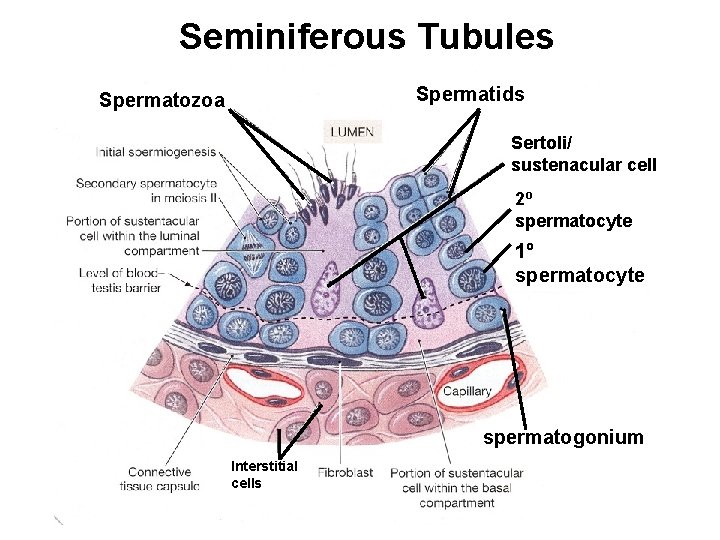
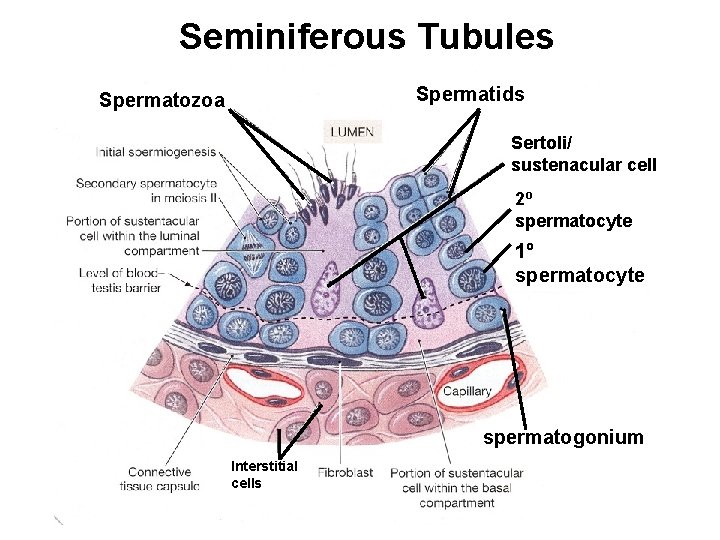
Seminiferous Tubules Spermatids Spermatozoa Sertoli/ sustenacular cell 2º spermatocyte 1º spermatocyte spermatogonium Interstitial cells
Cell Types • Interstitial Cells (Leydig Cells) produce testosterone • Sertoli (Sustenacular) nurse cells help to promote spermatogenesis
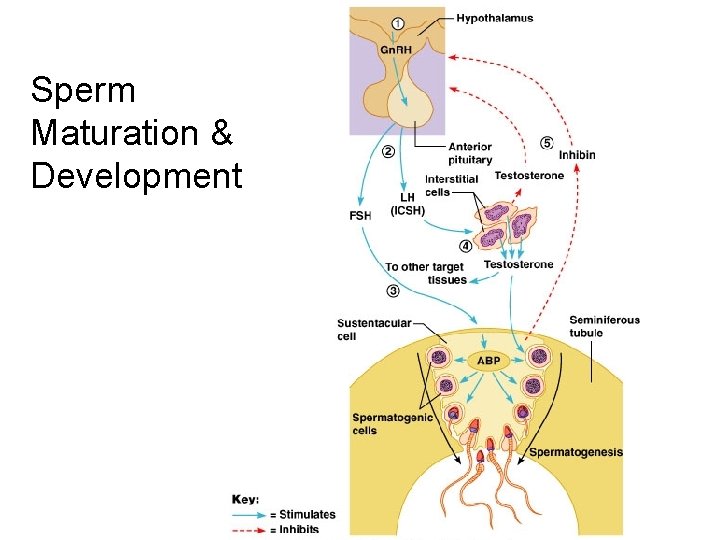
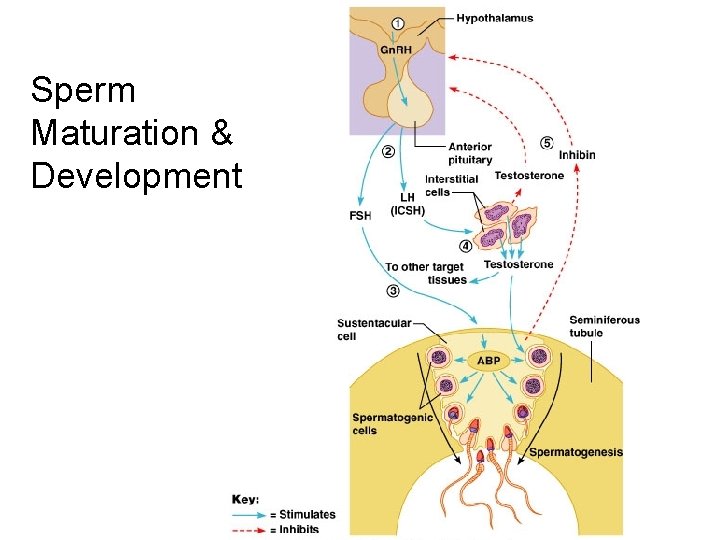
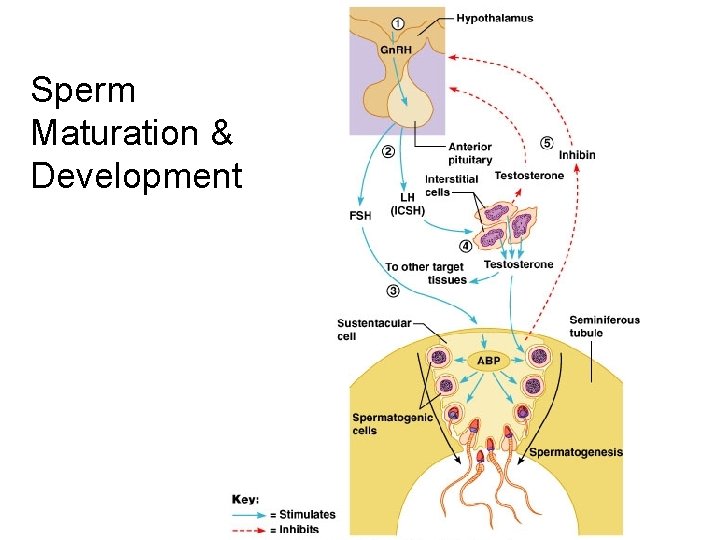
Sperm Maturation & Development
Hormones Involved in Spermatogenesis • • • Gonadotropin Releasing Hormone (Gn. RH) Follicle Stimulating Hormone (FSH) Interstitial Cell Stimulating Hormone (ICSH=LH) Testosterone Inhibin ABP
Hormones involved with spermatogenesis Gn. RH Gonadotropin Releasing Hormone • Secreted from the hypothalamus • Stimulates the secretion of FSH & LH
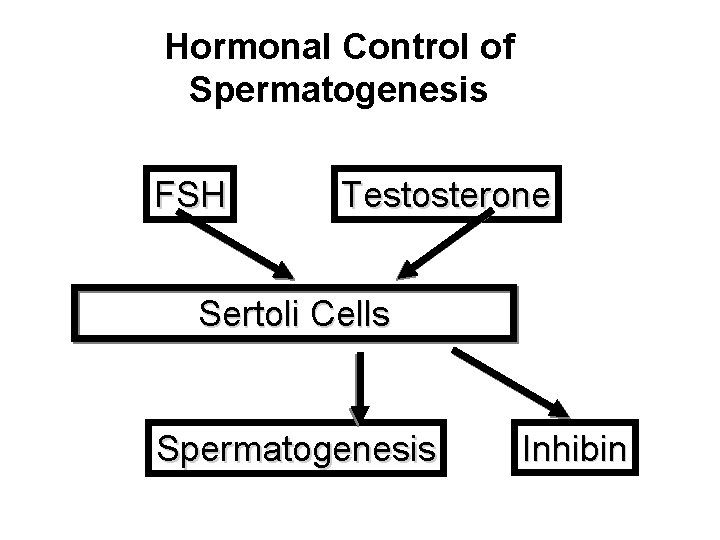
Hormones involved with spermatogenesis FSH Follicle Stimulating Hormone • Stimulates the secretion of ABP by the Sertoli cells(androgen binding protein) ABP keeps testosterone levels high in the area of spermatogenesis
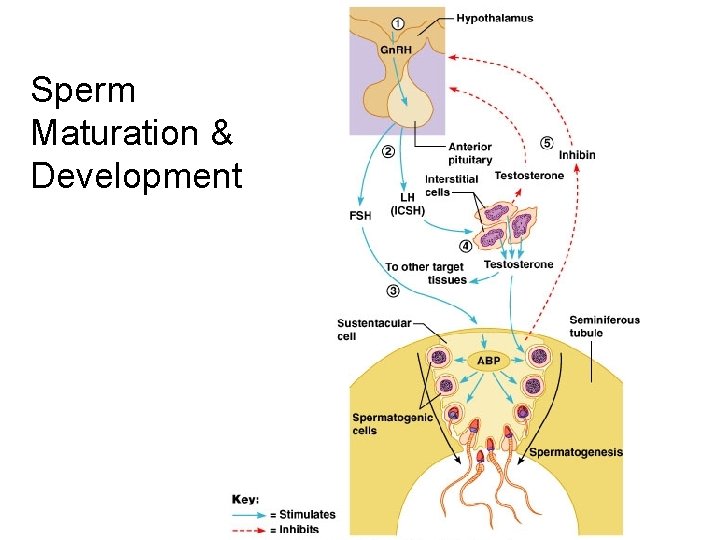
Sperm Maturation & Development
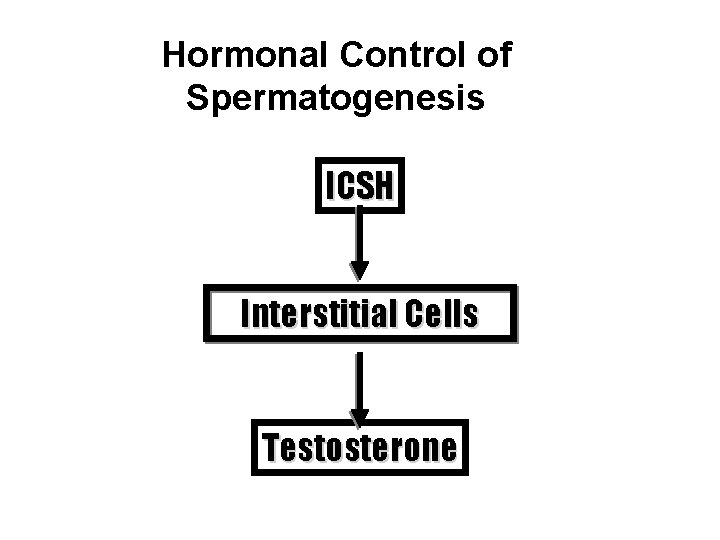
Hormones involved with spermatogenesis LH ( Luteinizing Hormone) • Binds to the interstitial cells of the testes stimulating testosterone release.
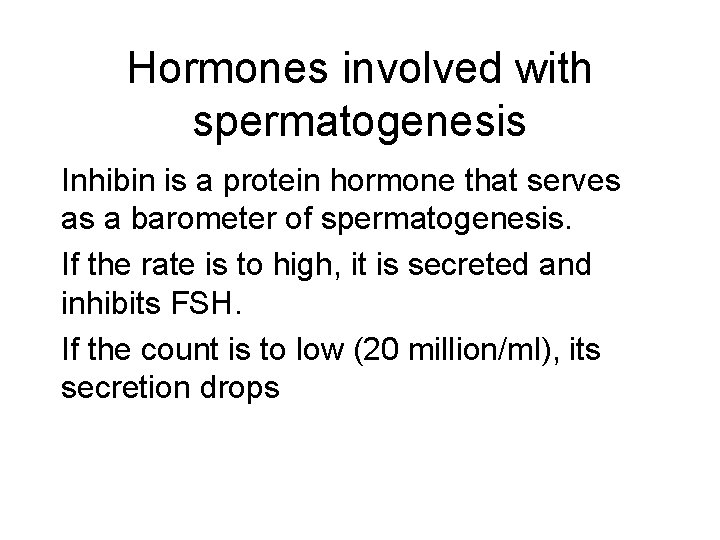
Hormones involved with spermatogenesis Inhibin is a protein hormone that serves as a barometer of spermatogenesis. If the rate is to high, it is secreted and inhibits FSH. If the count is to low (20 million/ml), its secretion drops
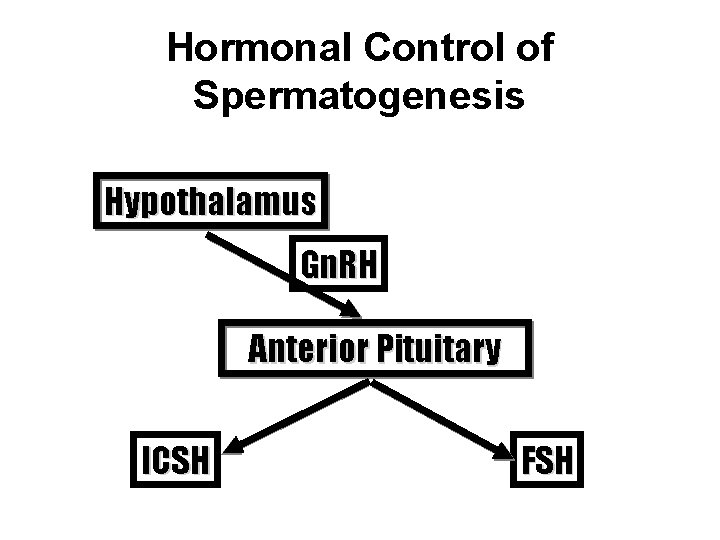
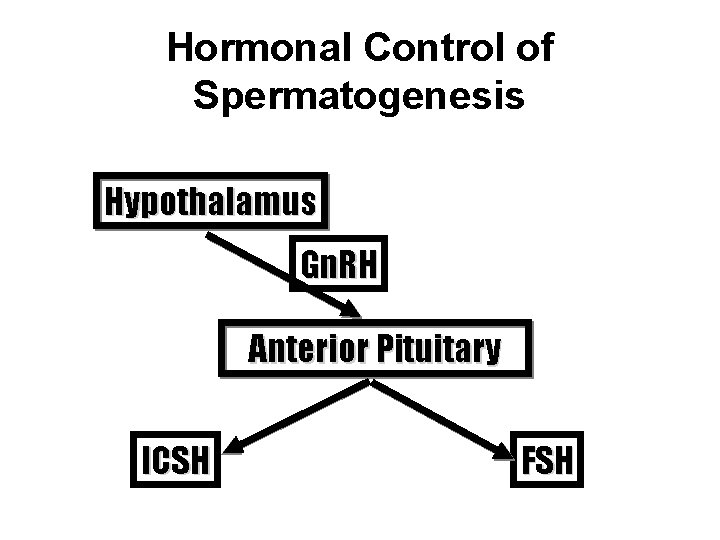
Hormonal Control of Spermatogenesis Hypothalamus Gn. RH Anterior Pituitary ICSH FSH
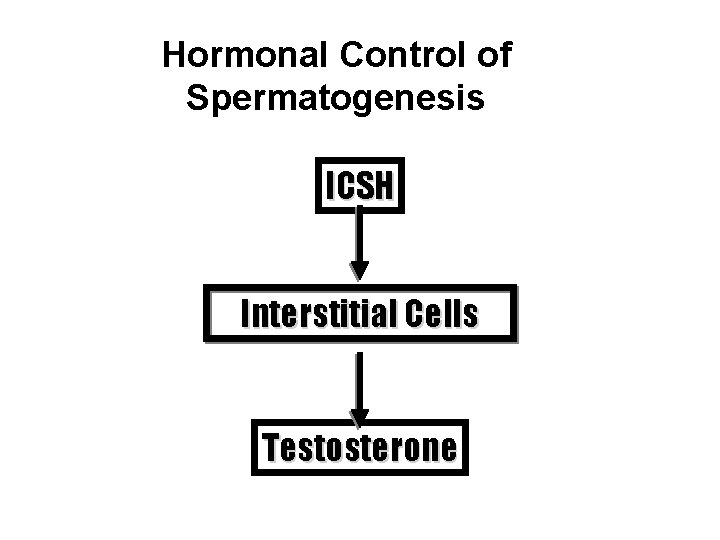
Hormonal Control of Spermatogenesis ICSH Interstitial Cells Testosterone
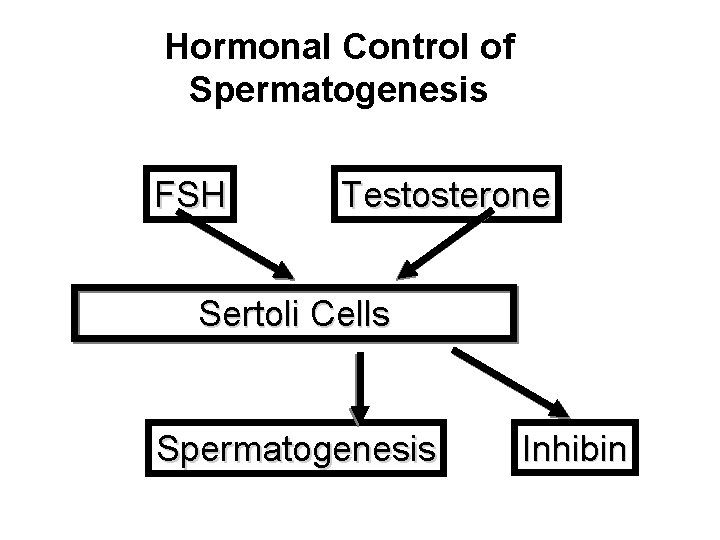
Hormonal Control of Spermatogenesis FSH Testosterone Sertoli Cells Spermatogenesis Inhibin
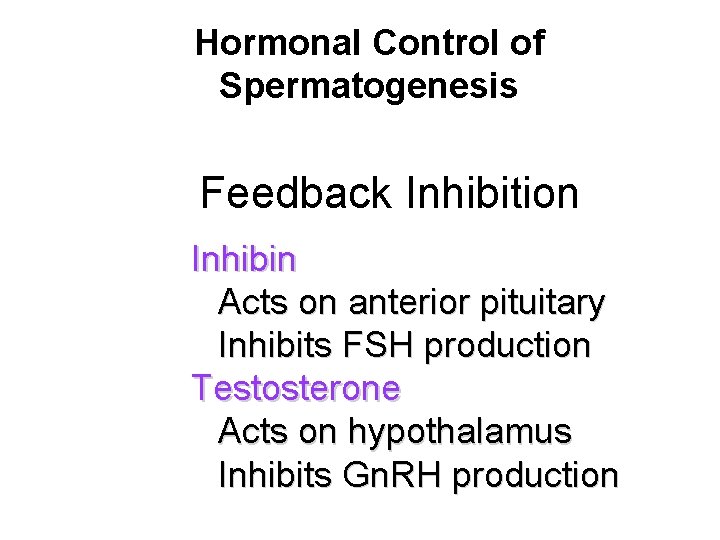
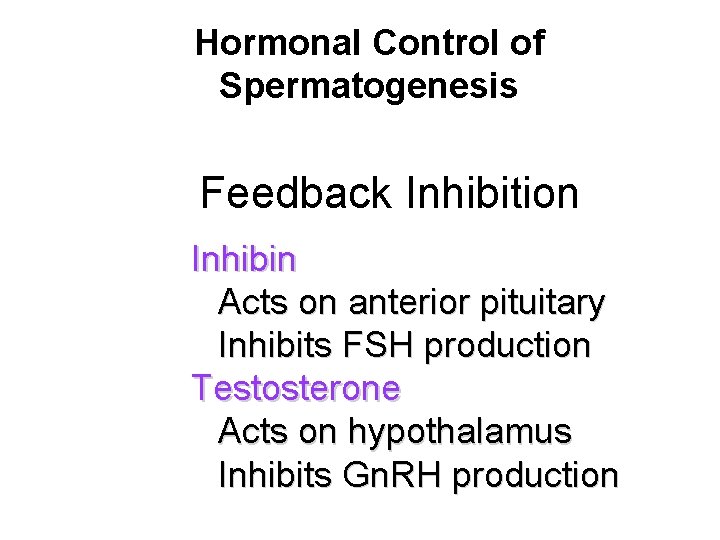
Hormonal Control of Spermatogenesis Feedback Inhibition Inhibin Acts on anterior pituitary Inhibits FSH production Testosterone Acts on hypothalamus Inhibits Gn. RH production
• • Some Other Effects of Testosterone muscle and bone growth facial and pubic hair growth thickening of vocal cords growth of pharyngeal cartilage hair follicle effects stimulates sebaceous glands Increased BMR
Female Reproductive System
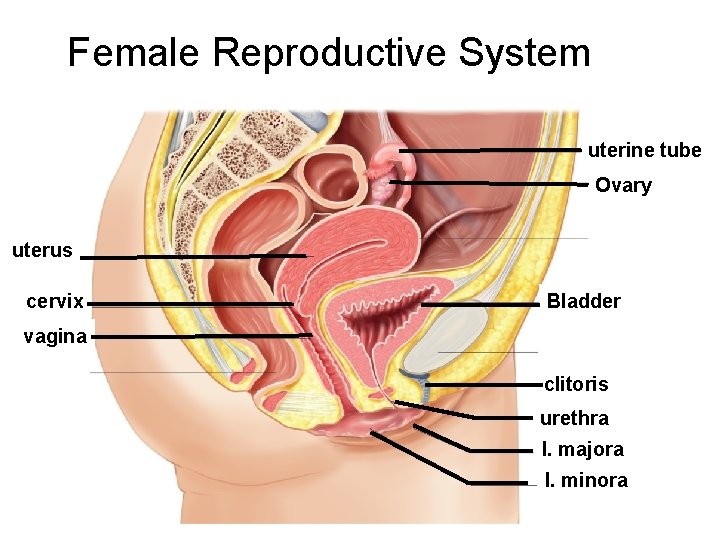
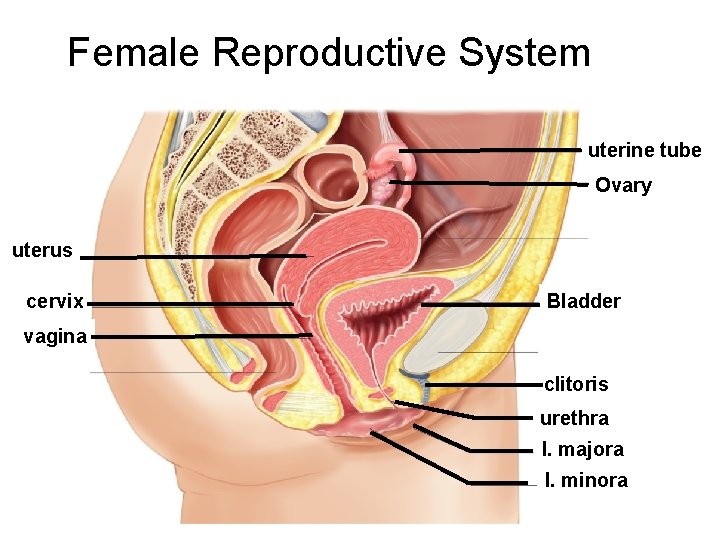
Female Reproductive System uterine tube Ovary uterus cervix Bladder vagina clitoris urethra l. majora l. minora
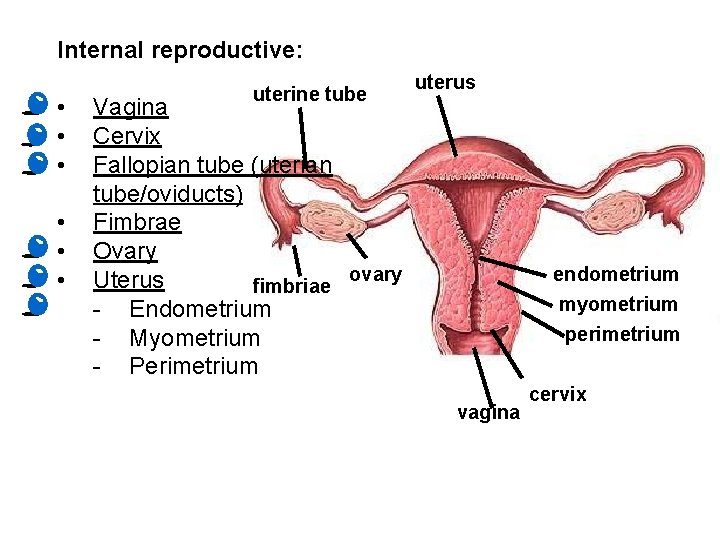
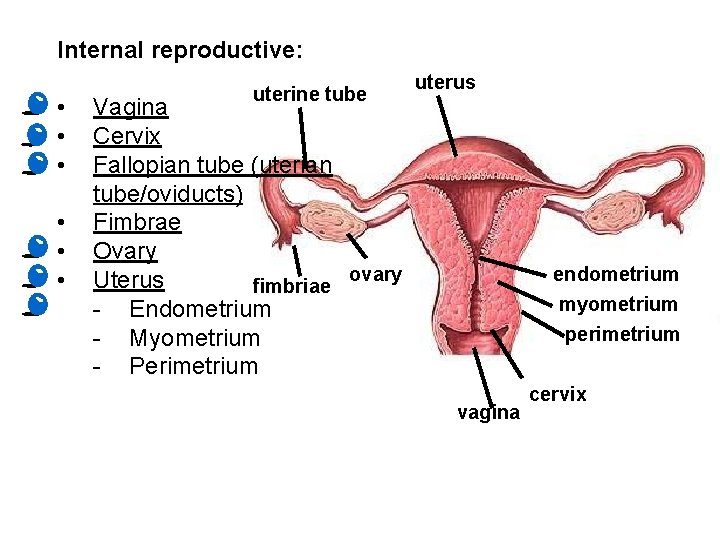
Internal reproductive: • • • uterine tube uterus Vagina Cervix Fallopian tube (uterian tube/oviducts) Fimbrae Ovary ovary Uterus fimbriae - Endometrium - Myometrium - Perimetrium endometrium myometrium perimetrium vagina cervix
Vagina • Is about 8 to 10 cm long • It extends from the exterior to the cervix • It is the female copulatory organ
Cervix • This is a narrow neck and is the outlet of the uterus into the vagina • This is call the external os • The glands of the cervix lubricate the vagina and can block the entry of sperm unless it is at mid cycle
Uterus Its function is to receive, retain and nourish ta fertilized ovum. The non pregnant human female uterus is the size of an inverted pear.
Uterus The rounded region superior to the entrance of the fallopian tubes is the fundus. The portion between the fundus and the cervix is the body.
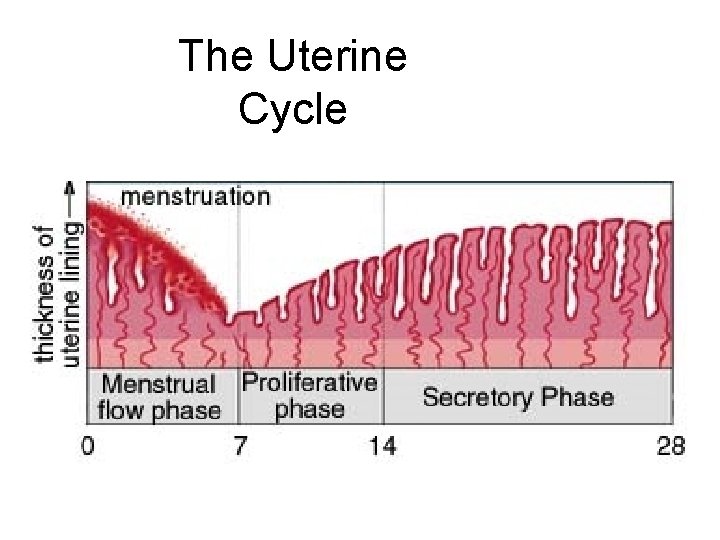
Uterus The uterus has three layers: • Endometrium: mucosal lining of columnar epithelium
Uterus The uterus has three layers: • Endometrium: mucosal lining of columnar epithelium • Myometrium: layers of smooth muscle
Uterus The uterus has three layers: • Endometrium: mucosal lining of columnar epithelium • Myometrium: layers of smooth muscle • Perimetrium: incomplete serous layer
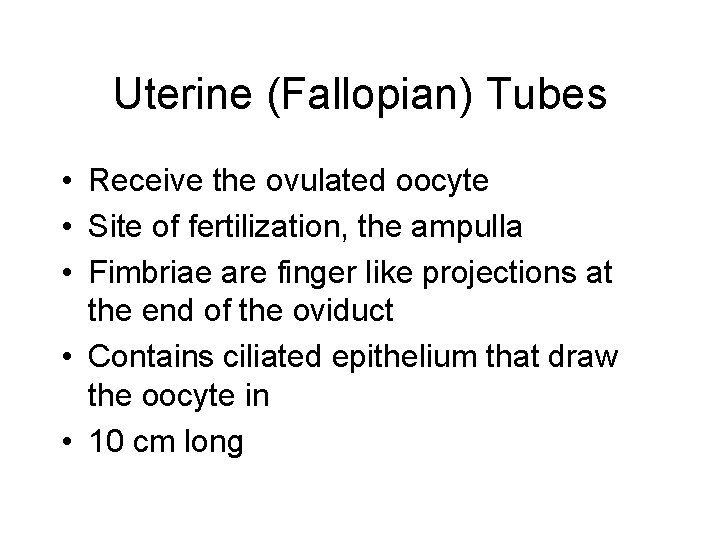
Uterine (Fallopian) Tubes • Receive the ovulated oocyte
Uterine (Fallopian) Tubes • Receive the ovulated oocyte • Site of fertilization, the ampulla
Uterine (Fallopian) Tubes • Receive the ovulated oocyte • Site of fertilization, the ampulla • Fimbriae are finger like projections at the end of the oviduct
Uterine (Fallopian) Tubes • Receive the ovulated oocyte • Site of fertilization, the ampulla • Fimbriae are finger like projections at the end of the oviduct • Contains ciliated epithelium that draw the oocyte in
Uterine (Fallopian) Tubes • Receive the ovulated oocyte • Site of fertilization, the ampulla • Fimbriae are finger like projections at the end of the oviduct • Contains ciliated epithelium that draw the oocyte in • 10 cm long
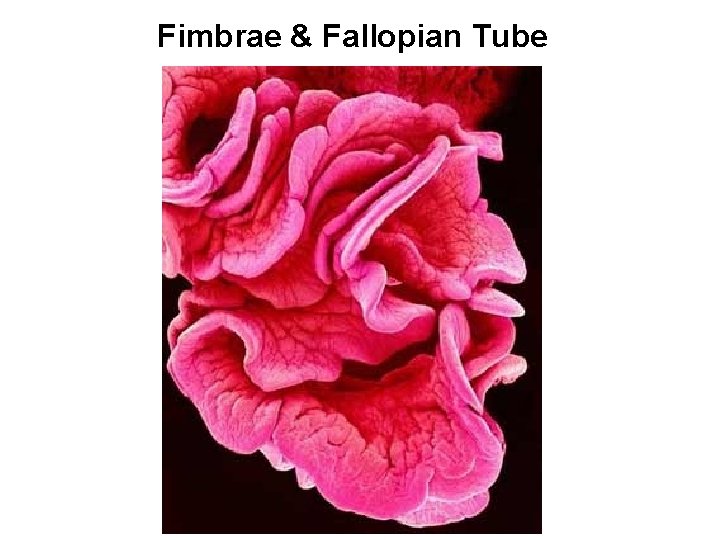
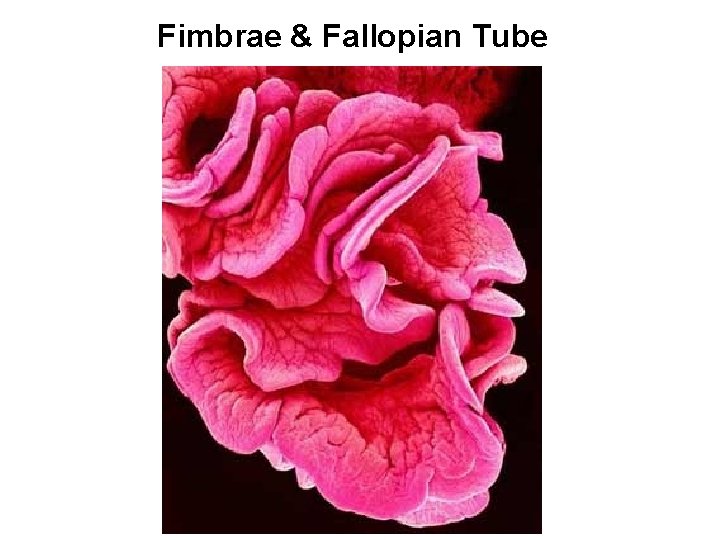
Fimbrae & Fallopian Tube
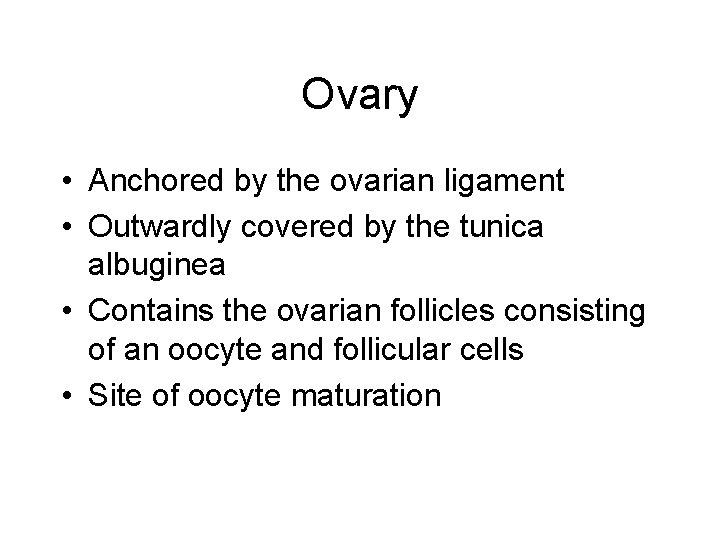
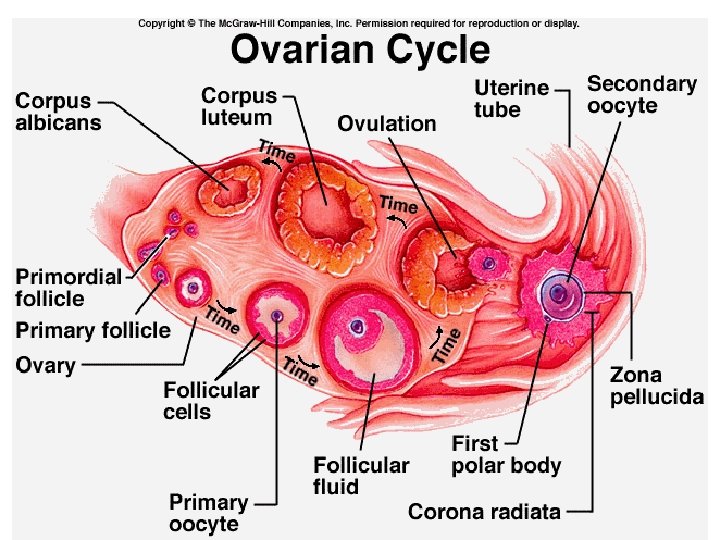
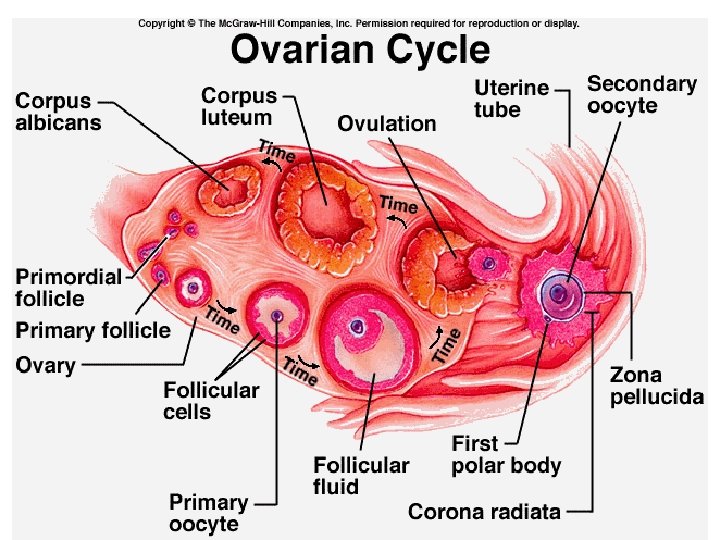
Ovary • Anchored by the ovarian ligament • Outwardly covered by the tunica albuginea • Contains the ovarian follicles consisting of an oocyte and follicular cells • Site of oocyte maturation
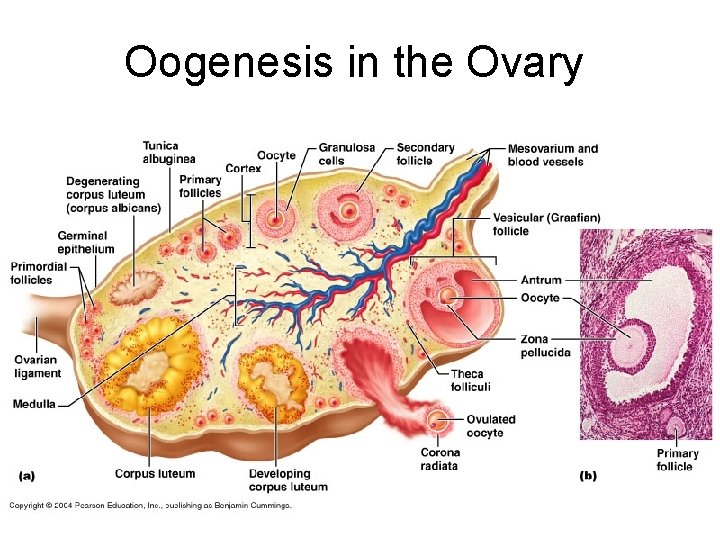
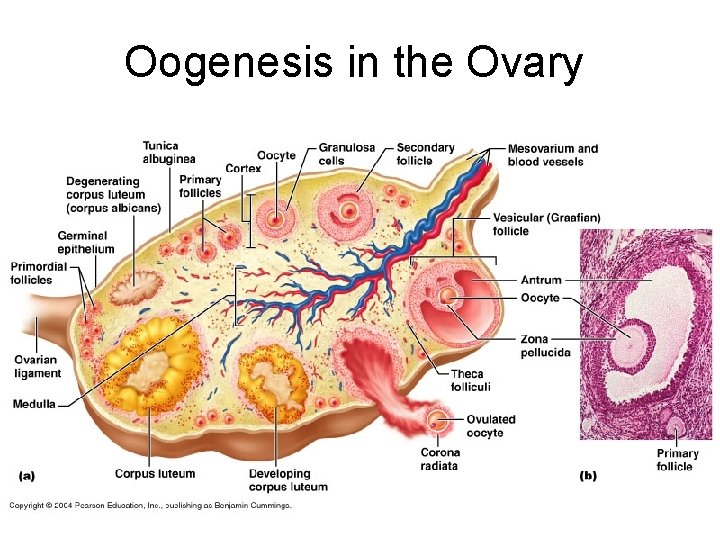
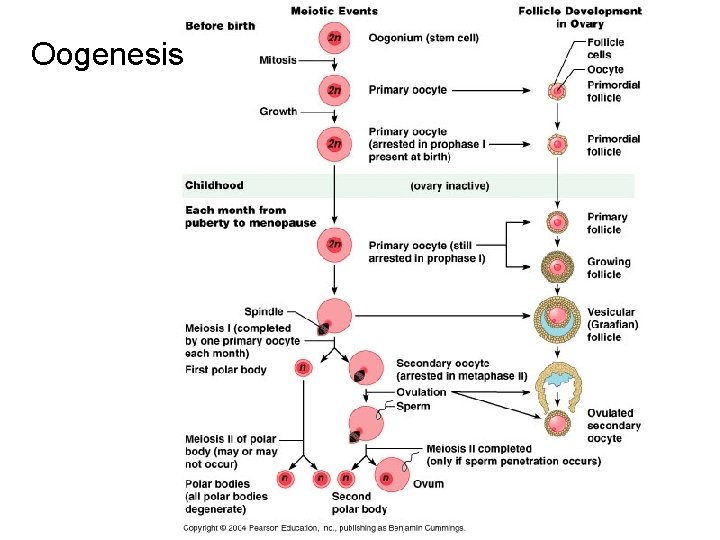
Oogenesis in the Ovary
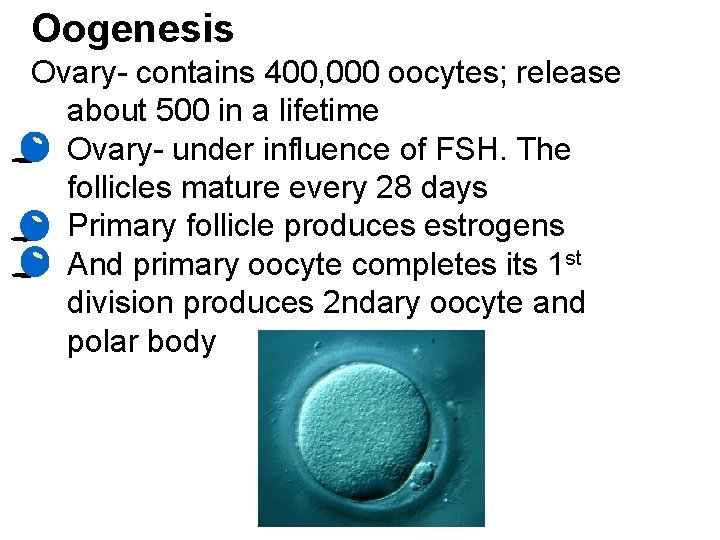
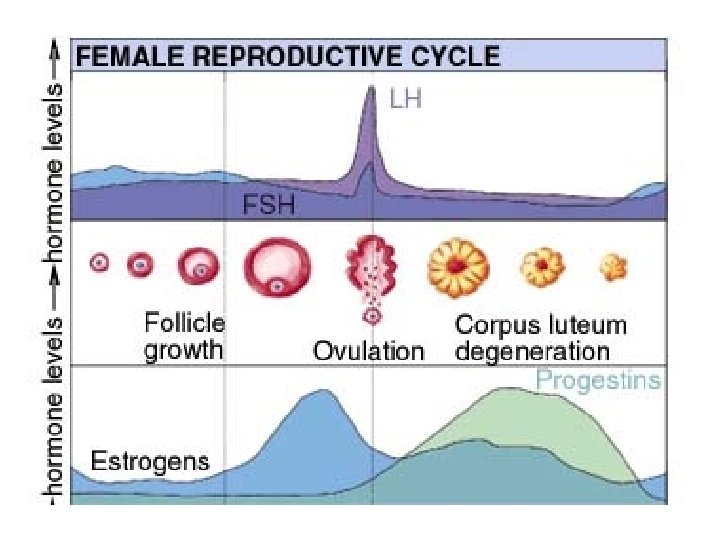
Oogenesis Ovary- contains 400, 000 oocytes; release about 500 in a lifetime • Ovary- under influence of FSH. The follicles mature every 28 days • Primary follicle produces estrogens • And primary oocyte completes its 1 st division produces 2 ndary oocyte and polar body
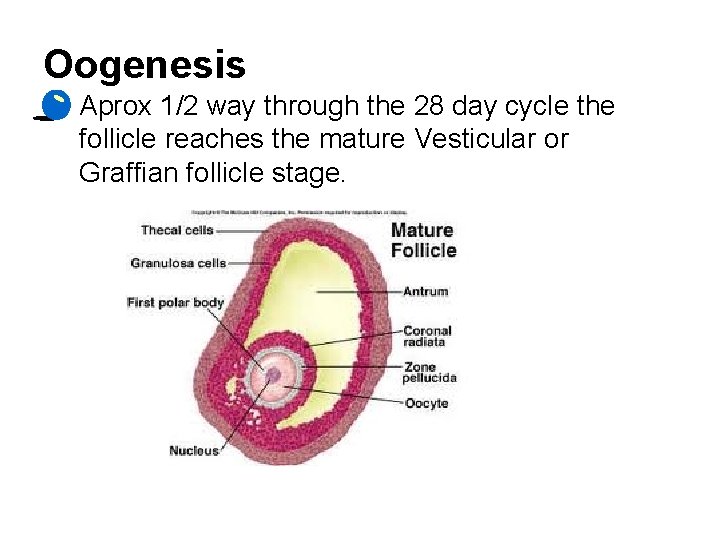
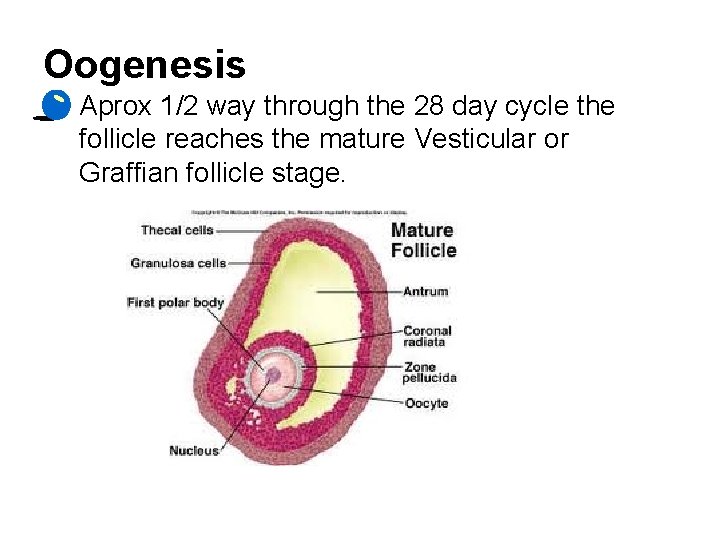
Oogenesis • Aprox 1/2 way through the 28 day cycle the follicle reaches the mature Vesticular or Graffian follicle stage.
Oogenesis • Estrogen levels rise and release LH and FSH and triggers ovulation.
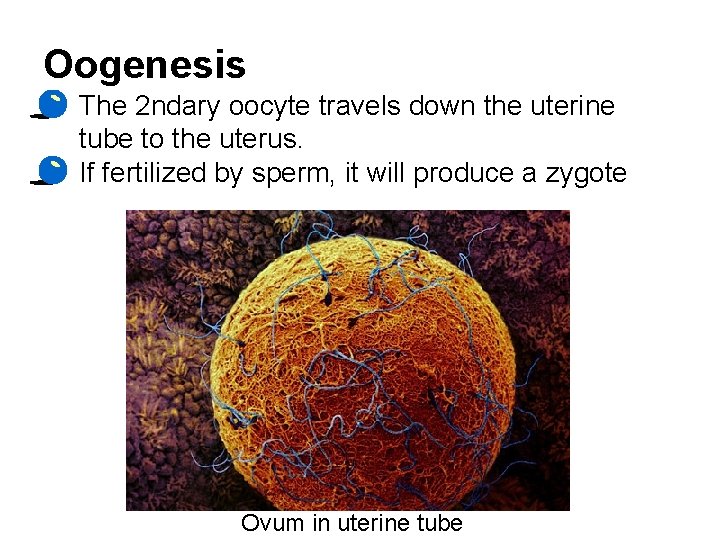
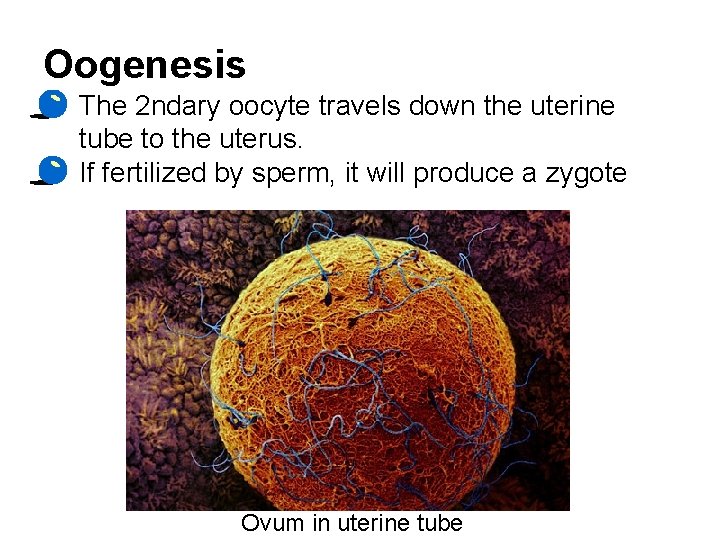
Oogenesis • The 2 ndary oocyte travels down the uterine tube to the uterus. • If fertilized by sperm, it will produce a zygote Ovum in uterine tube
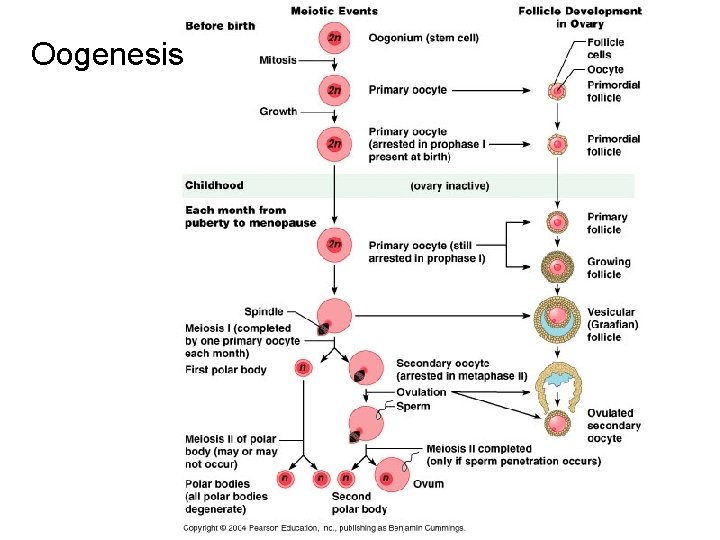
Oogenesis
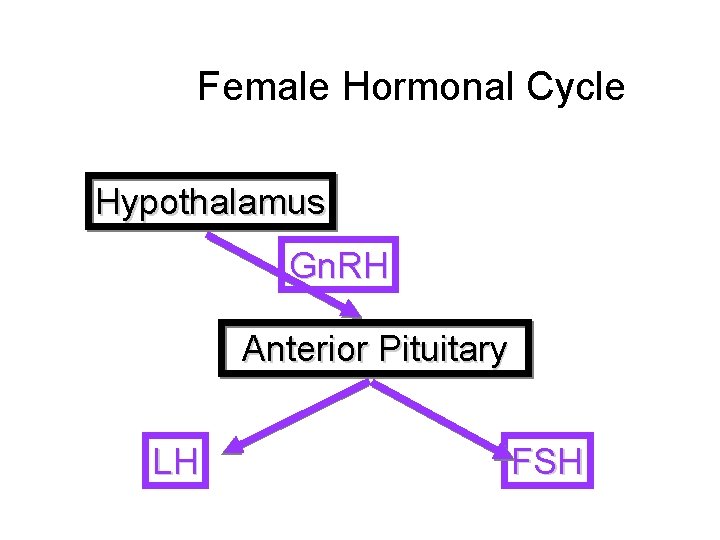
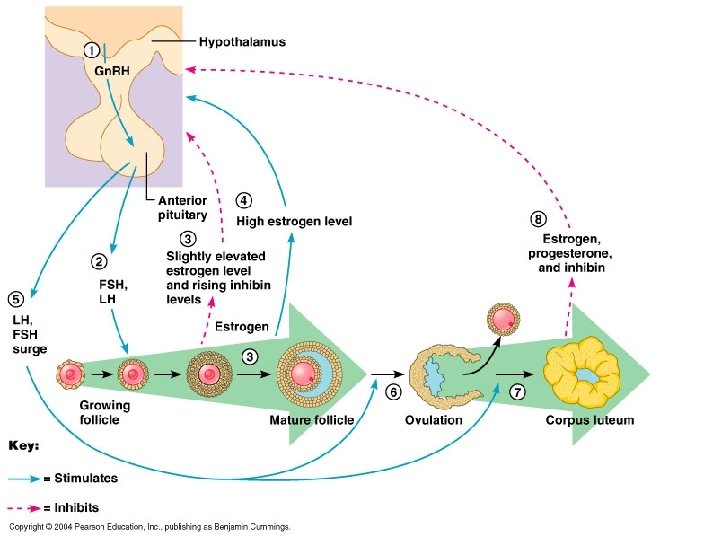
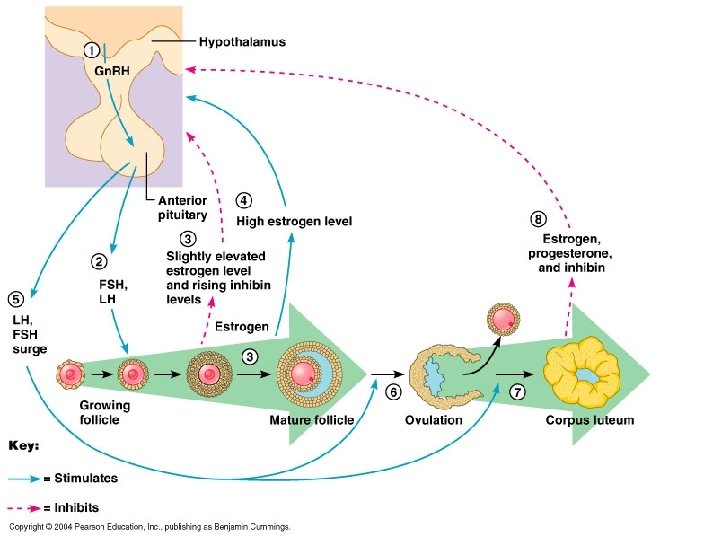
Hormones Involved in the Female Reproductive Cycle • • Gonadotropin Releasing Hormone (Gn. RH) Follicle Stimulating Hormone (FSH) Luteinizing Hormone (LH) Estrogen Progesterone Inhibin Relaxin
Gn. RH • Gonadotropin Releasing Hormone is secreted from the pituitary and through the portal system stimulates FSH release
FSH • FSH exerts its primary effects on the follicles in the ovary. • The follicular cells are stimulated to secrete estrogen
Estrogen Primary female secondary sex hormone Stimulates proliferation of the endometrial lining, (proliferative phase). Stimulates the production of watery cervical mucus.
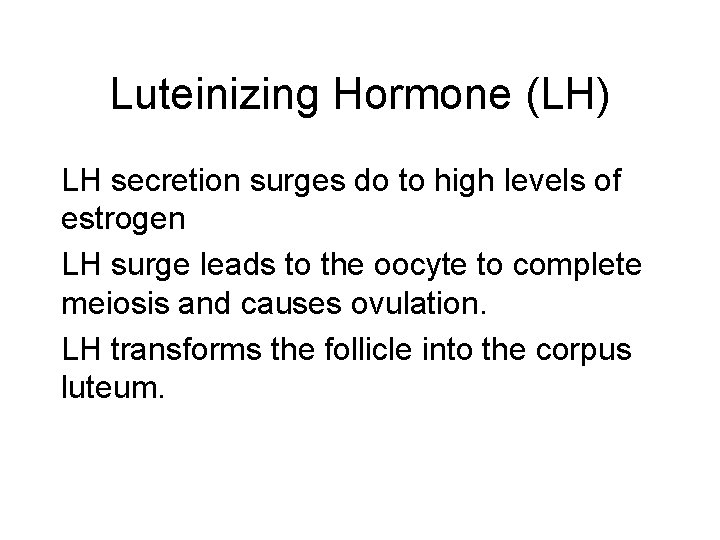
Luteinizing Hormone (LH) LH secretion surges do to high levels of estrogen LH surge leads to the oocyte to complete meiosis and causes ovulation. LH transforms the follicle into the corpus luteum.
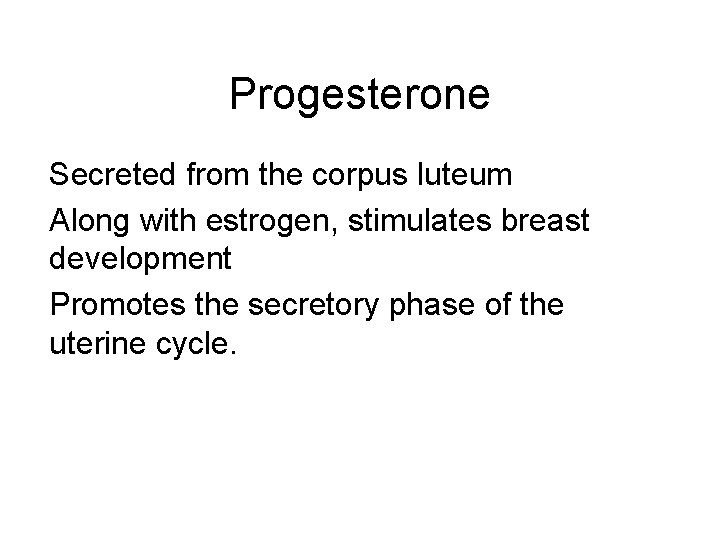
Progesterone Secreted from the corpus luteum Along with estrogen, stimulates breast development Promotes the secretory phase of the uterine cycle.
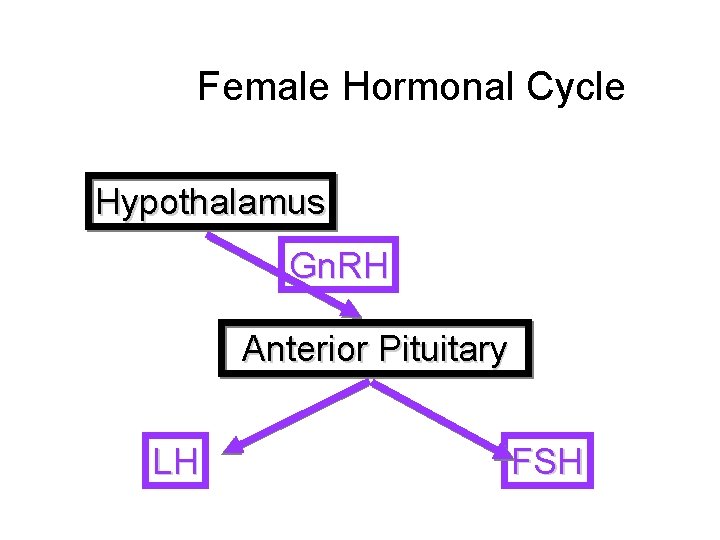
Female Hormonal Cycle Hypothalamus Gn. RH Anterior Pituitary LH FSH
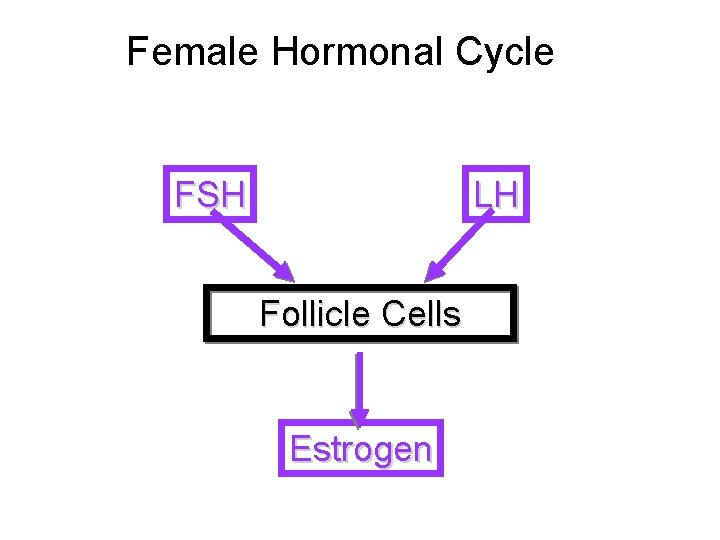
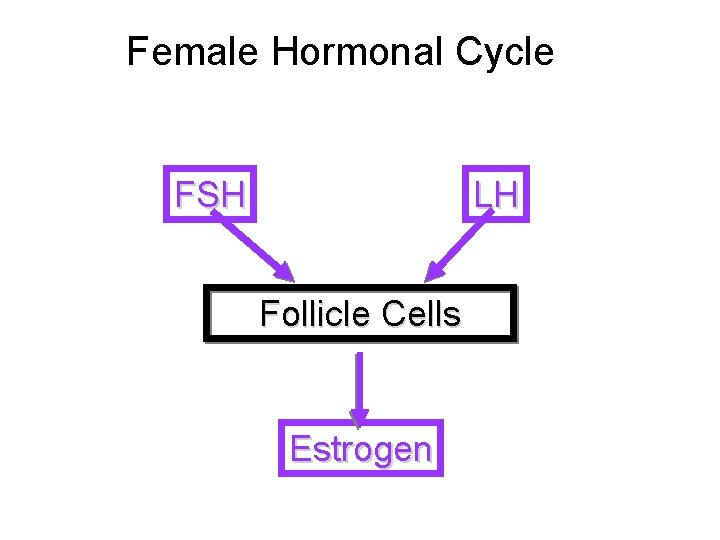
Female Hormonal Cycle FSH LH Follicle Cells Estrogen
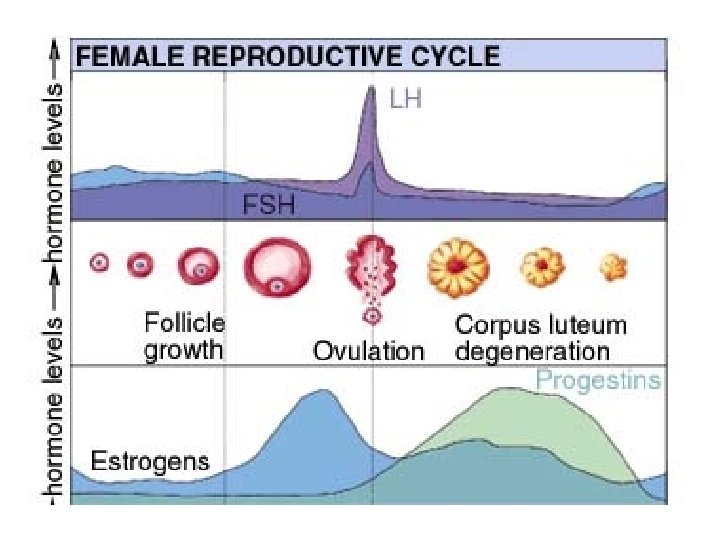
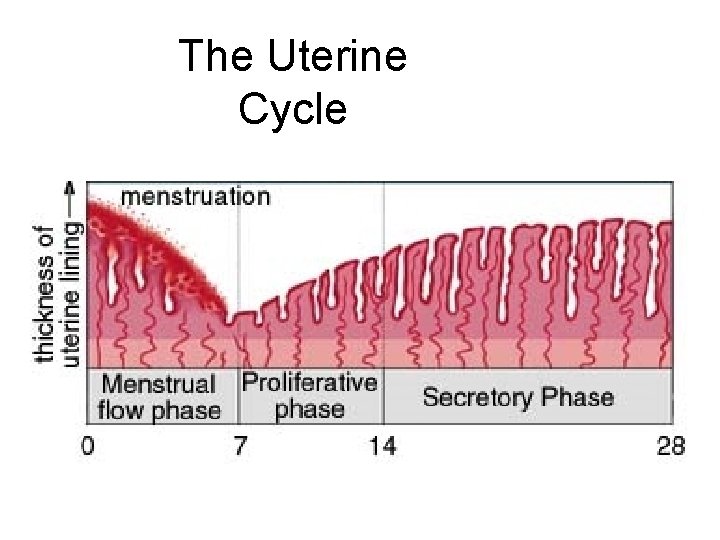
The Uterine Cycle
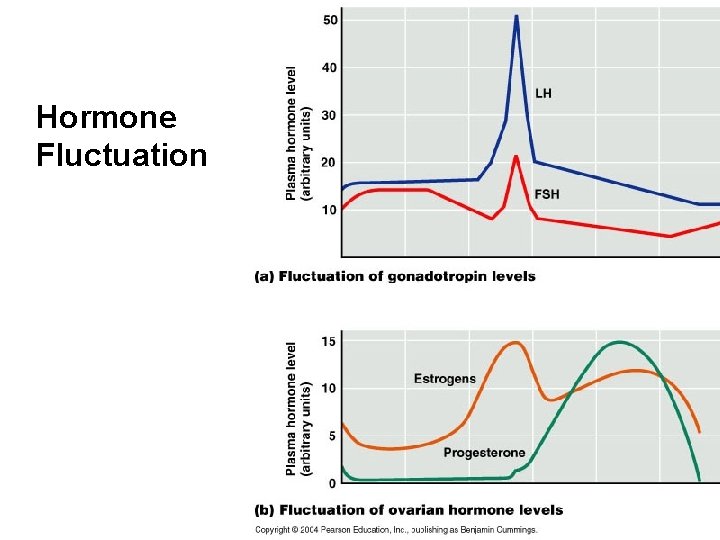
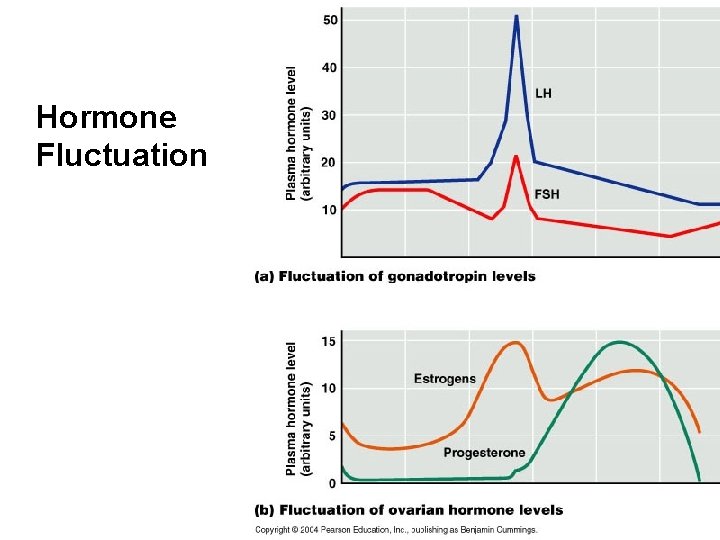
Hormone Fluctuation
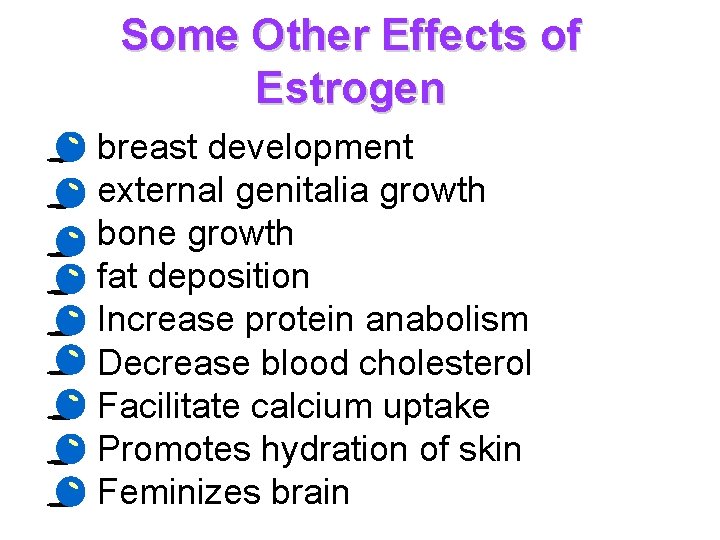
Some Other Effects of Estrogen • • • breast development external genitalia growth bone growth fat deposition Increase protein anabolism Decrease blood cholesterol Facilitate calcium uptake Promotes hydration of skin Feminizes brain
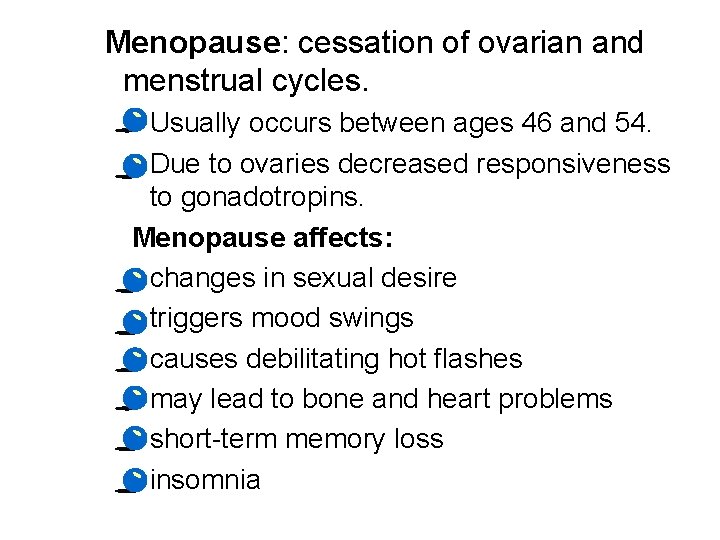
Menopause: cessation of ovarian and menstrual cycles. · Usually occurs between ages 46 and 54. · Due to ovaries decreased responsiveness to gonadotropins. Menopause affects: · changes in sexual desire · triggers mood swings · causes debilitating hot flashes · may lead to bone and heart problems · short-term memory loss · insomnia
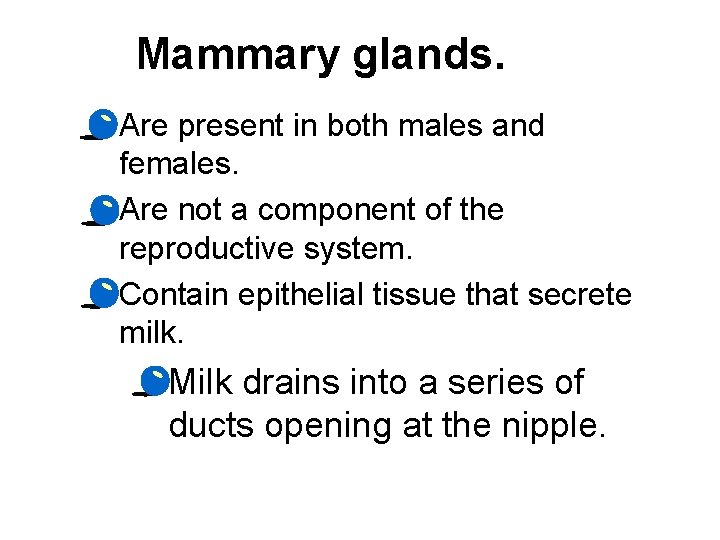
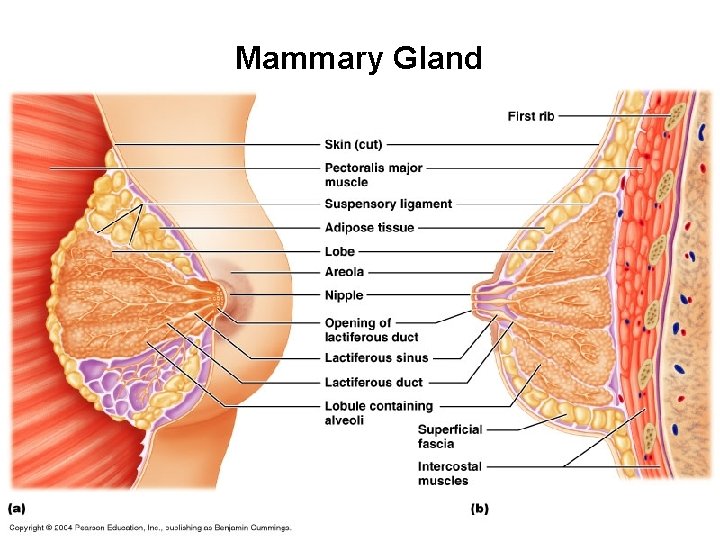
Mammary glands. · Are present in both males and females. · Are not a component of the reproductive system. · Contain epithelial tissue that secrete milk. · Milk drains into a series of ducts opening at the nipple.
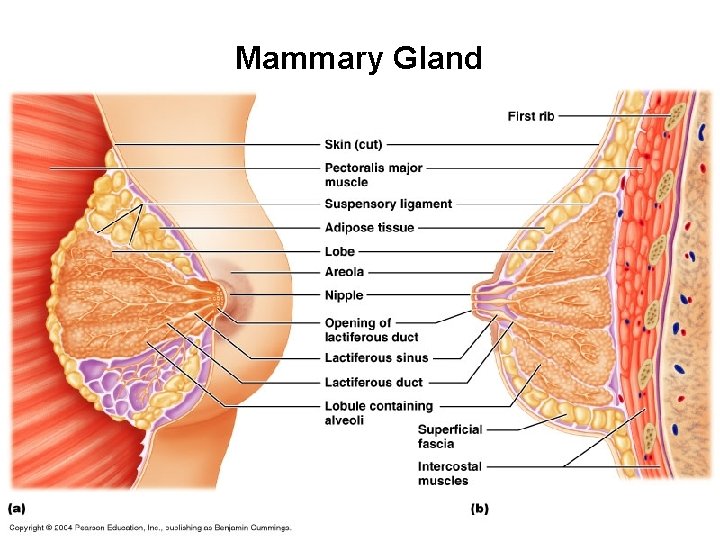
Mammary Gland
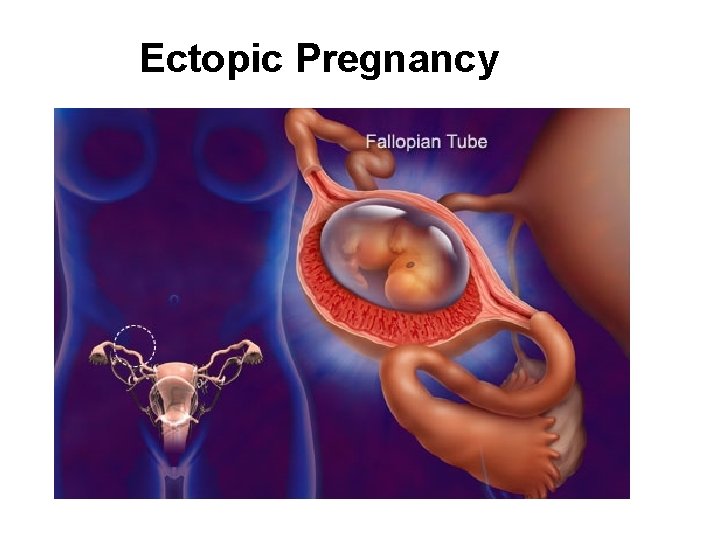
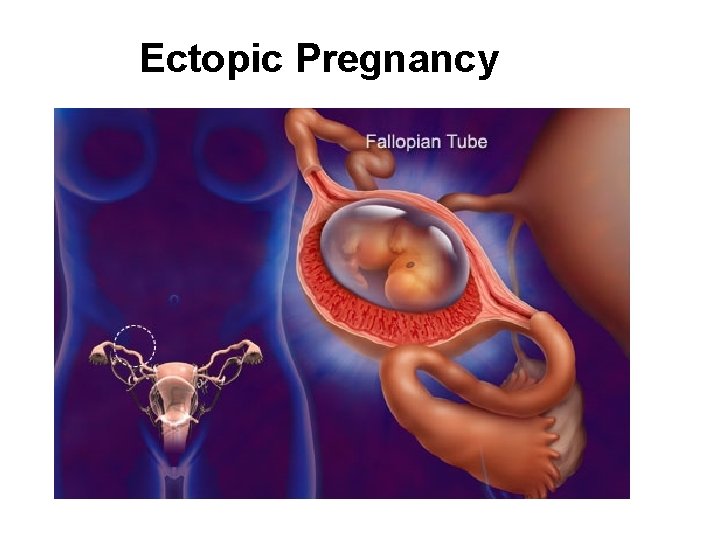
Ectopic Pregnancy
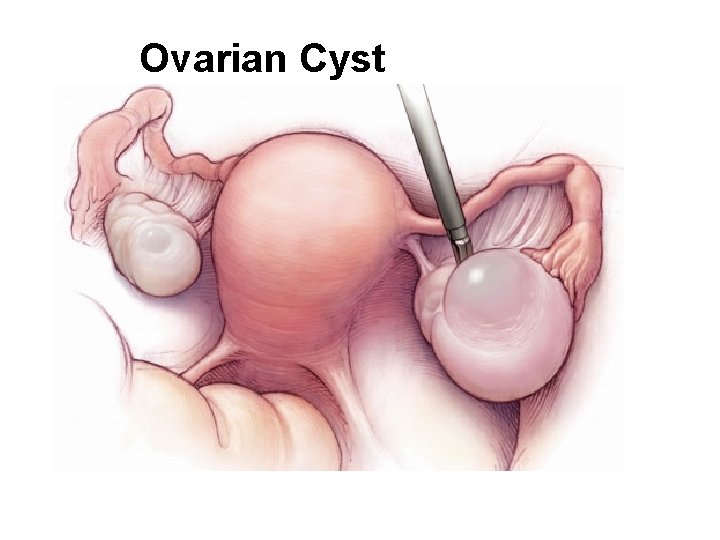
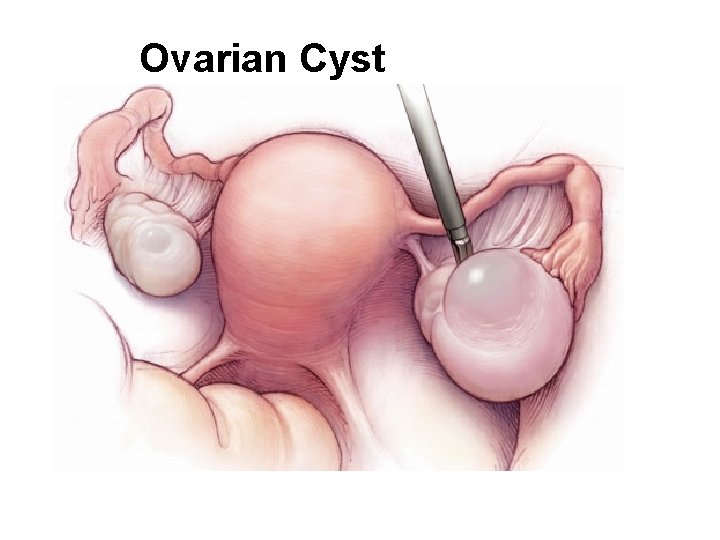
Ovarian Cyst
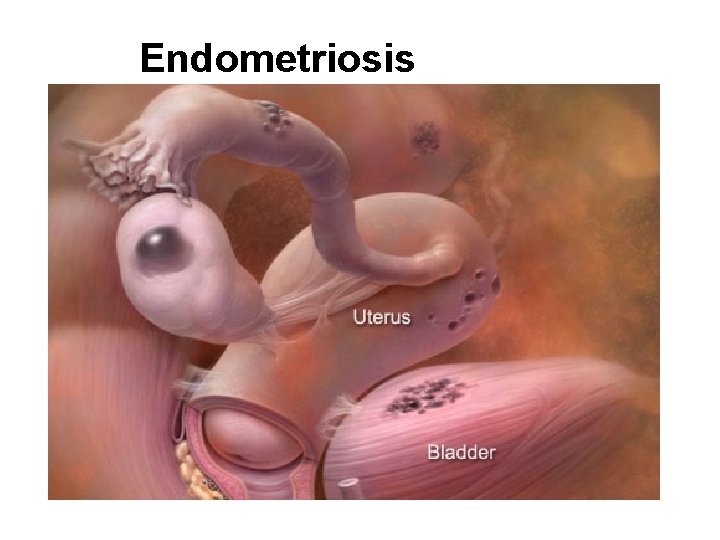
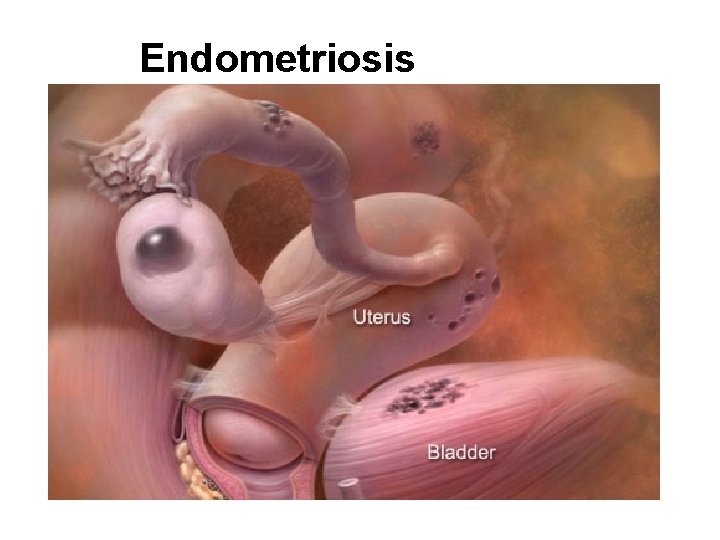
Endometriosis
Life’s Greatest Miracle • http: //www. pbs. org/wgbh/nova/ miracle/program. html
INQUIRY 1. Where are sperm cells formed within the testes? 2. What portion of the sperm contains 23 chromosomes? 3. What 3 accessory glands produce seminal fluid? 4. What is the term for the primary human sex organs? 5. What structure is formed following ovulation? 6. What hormones are produced from the corpus luteum? 7. List several effective means for preventing conception.