Reproductive System Male Reproductive System Spermatogenesis The Male
- Slides: 33
Reproductive System Male Reproductive System Spermatogenesis
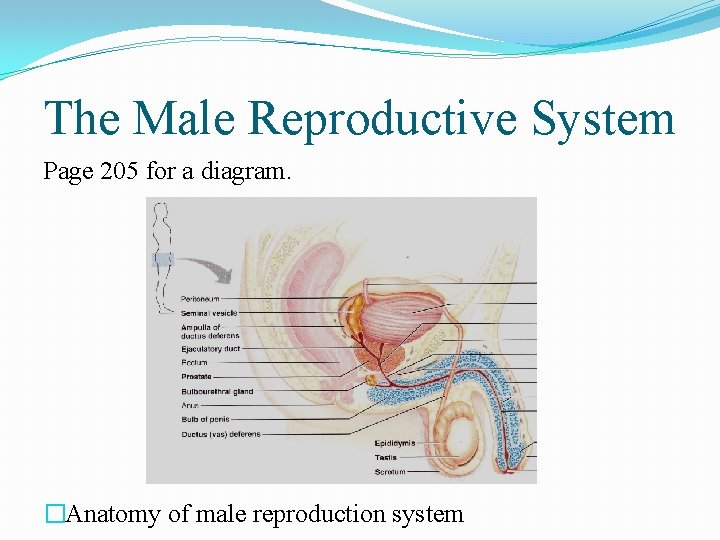
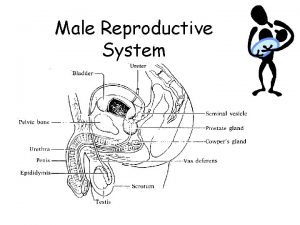
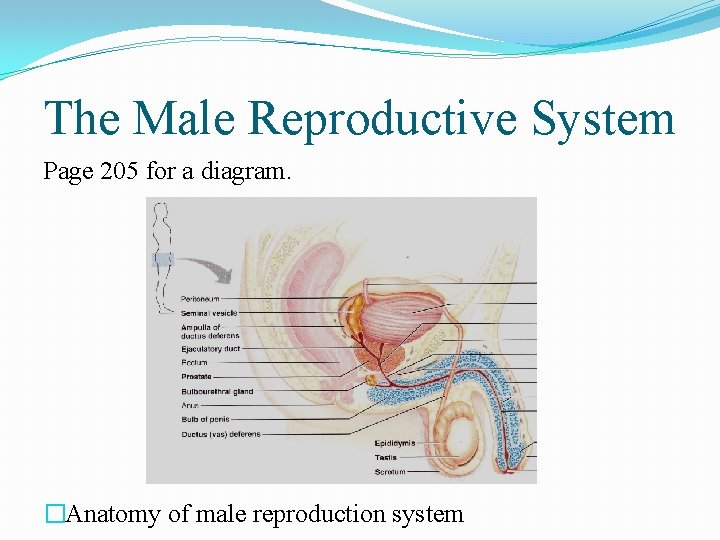
The Male Reproductive System Page 205 for a diagram. �Anatomy of male reproduction system
Scrotum � Sac of skin containing muscle that hangs outside the body at the base of the penis � Contains paired oval testes � Importance: � Sperm cannot be produced in abundance at core body temperature (37 o. C) therefore it is external from the body which results in a 3 o. C drop in temperature. � Temperature Control � When cold, the testes are pulled closer to the body for warmth through wrinkling of the scrotum to increase thickness and reduce heat loss � When hot, skin is loose to increase the surface area for cooling and hang lower, away from the body. Movement controlled by muscles.
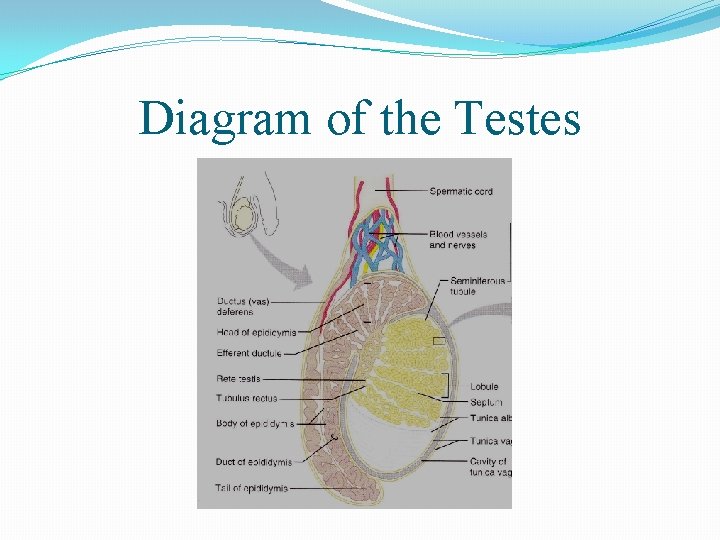
Testes �“Male gonads” �The testes contain lobules with each lobule containing four tightly coiled seminiferous tubules (sperm factories). �Surrounding these seminiferous tubules are interstitial cells which produce androgens (natural or synthetic compound that stimulates or controls the development and maintenance of masculine characteristics) such as testosterone. �Site of spermatogenesis
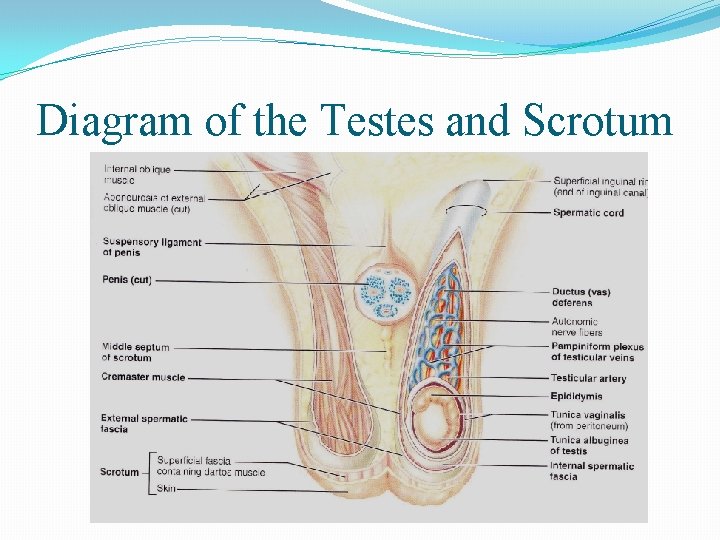
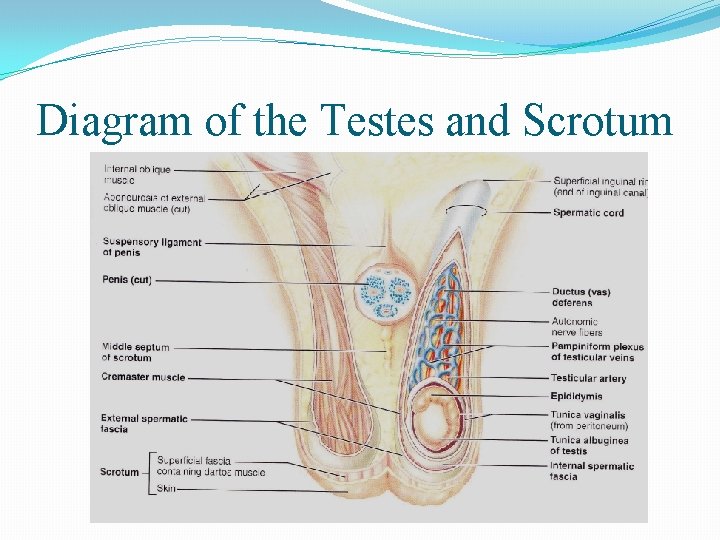
Diagram of the Testes and Scrotum
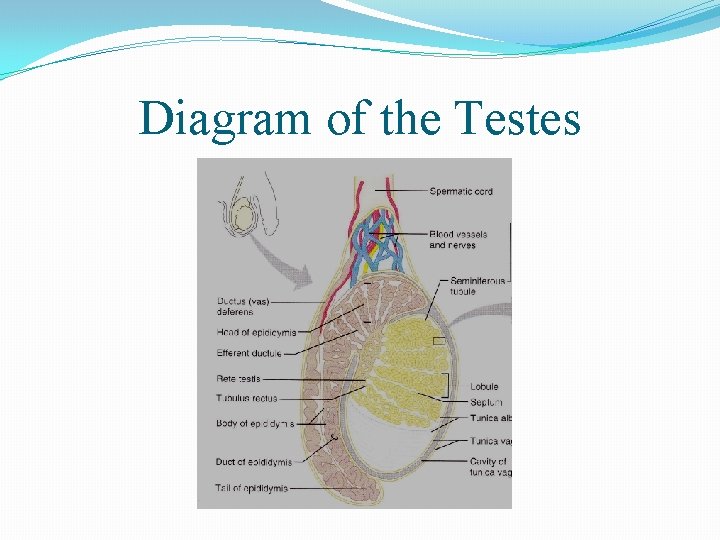
Diagram of the Testes
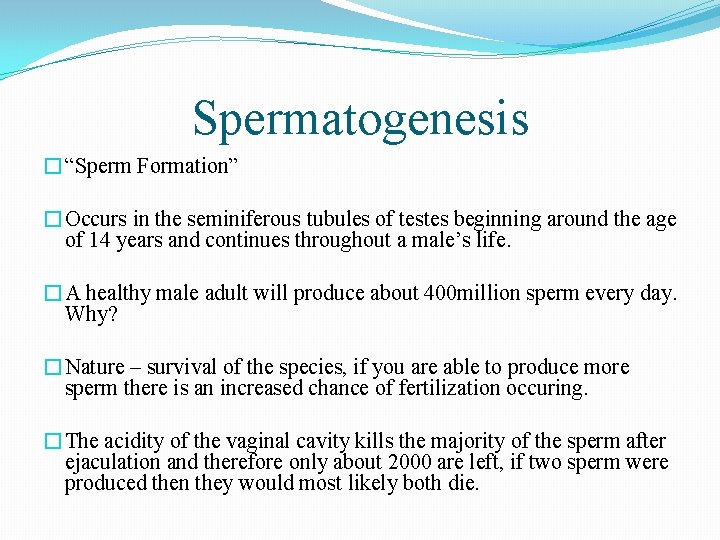
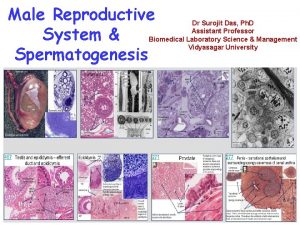
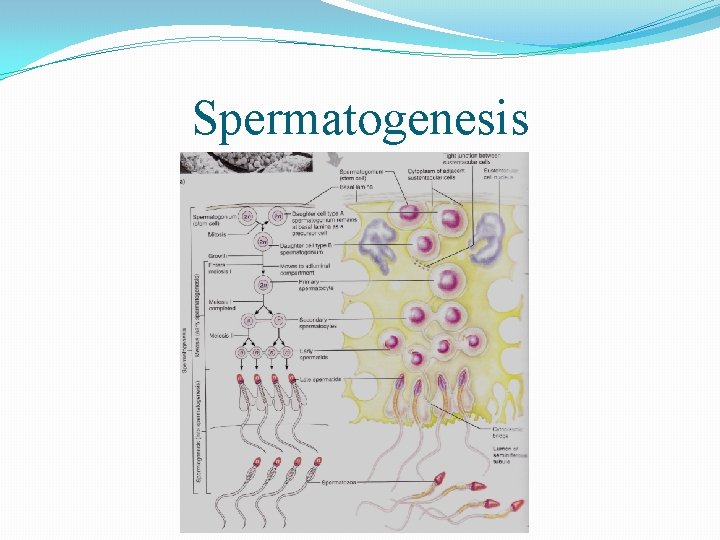
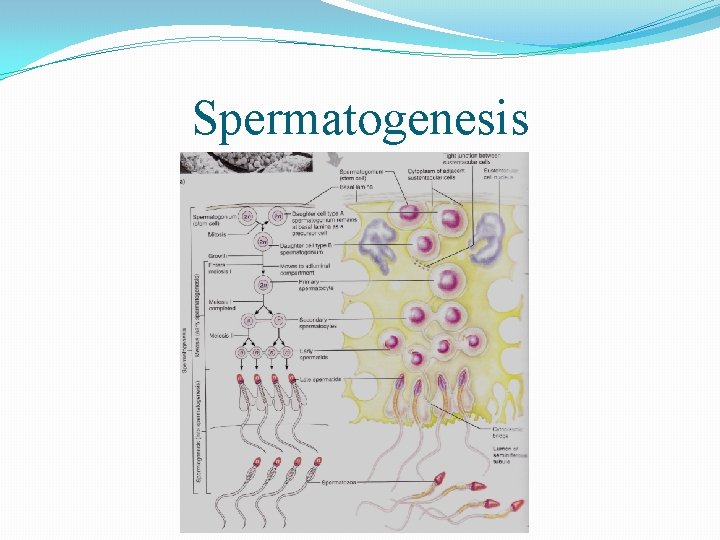
Spermatogenesis �“Sperm Formation” �Occurs in the seminiferous tubules of testes beginning around the age of 14 years and continues throughout a male’s life. �A healthy male adult will produce about 400 million sperm every day. Why? �Nature – survival of the species, if you are able to produce more sperm there is an increased chance of fertilization occuring. �The acidity of the vaginal cavity kills the majority of the sperm after ejaculation and therefore only about 2000 are left, if two sperm were produced then they would most likely both die.
Spermatogenesis �Three main stages: �Spermatogonia: Formation of spermatocytes �Meiosis: Spermatocytes to Spermatids �Spermiogenesis: Spermatids to Sperm
Spermatogonia �“Sperm Seed” �Occurring within the seminiferous tubules, before puberty the mitotic division of spermatogonia takes place and both daughter cells become spermatogonia. �During puberty, the spermatogonia division through mitosis results in a seperation of the daughter cells, one remains in the same spot to produce more spermatogonia by mitosis and the other moves towards the lumen where it becomes a primary spermatocyte.
Recap of Meiosis �Meiosis: The production of four haploid (n) gametes from one mother cell. �Interphase �Meiosis 1 �prophase 1, metaphase 1, anaphase 1, telophase 1(cytokinesis) �Meiosis 2 �prophase 2, metaphase 2, anaphase 2, telophase 2 (cytokinesis). �Benefits: Genetic transfer resulting in variance in genetic information which can lead to adaptations for survival.
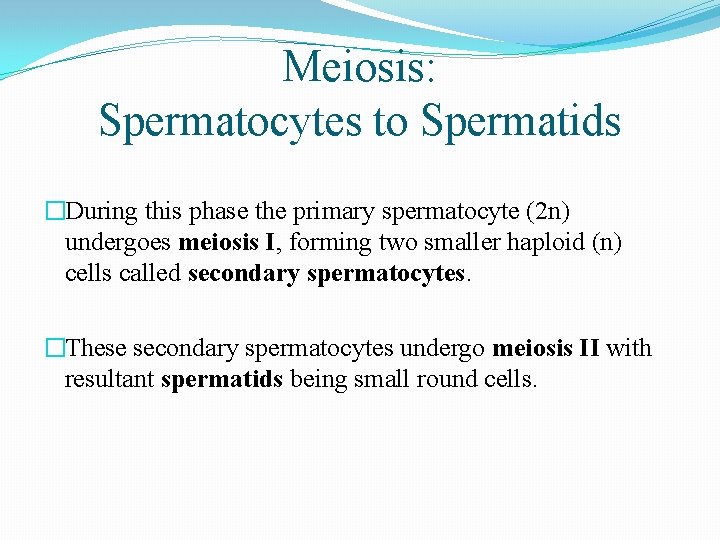
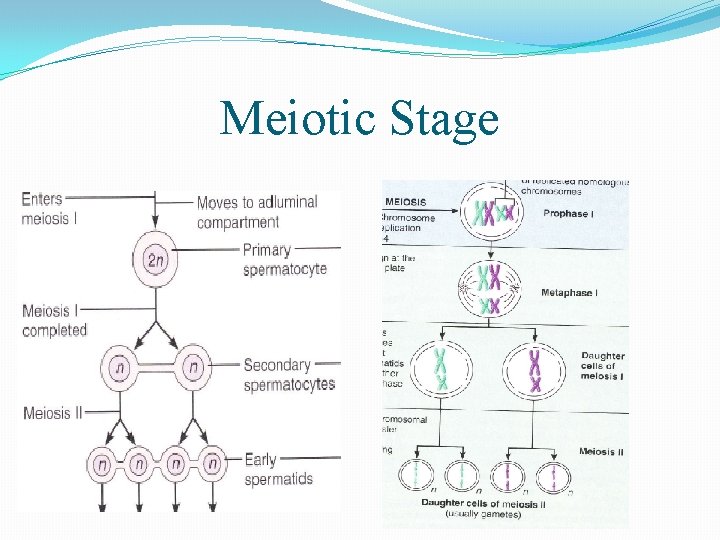
Meiosis: Spermatocytes to Spermatids �During this phase the primary spermatocyte (2 n) undergoes meiosis I, forming two smaller haploid (n) cells called secondary spermatocytes. �These secondary spermatocytes undergo meiosis II with resultant spermatids being small round cells.
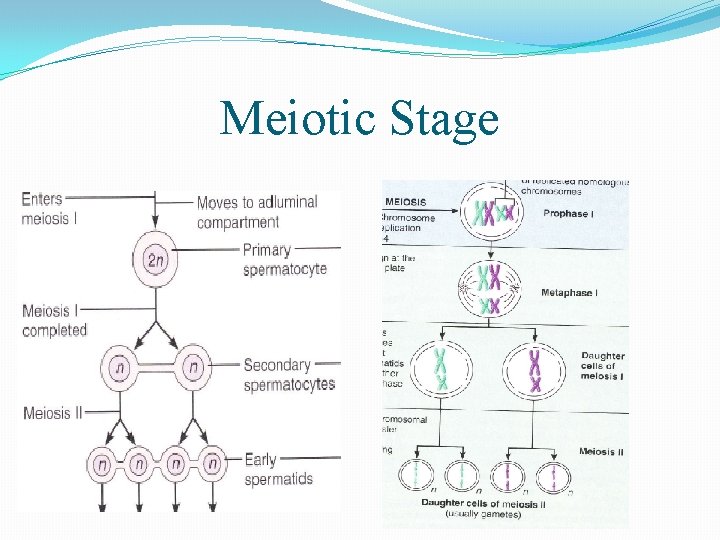
Meiotic Stage
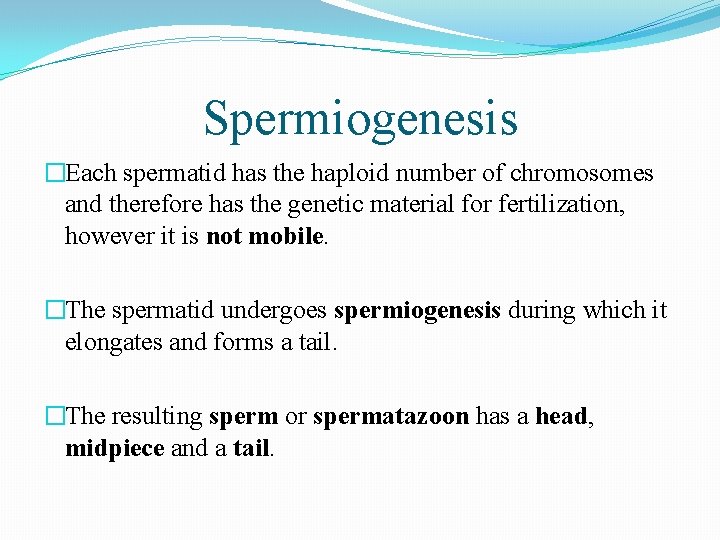
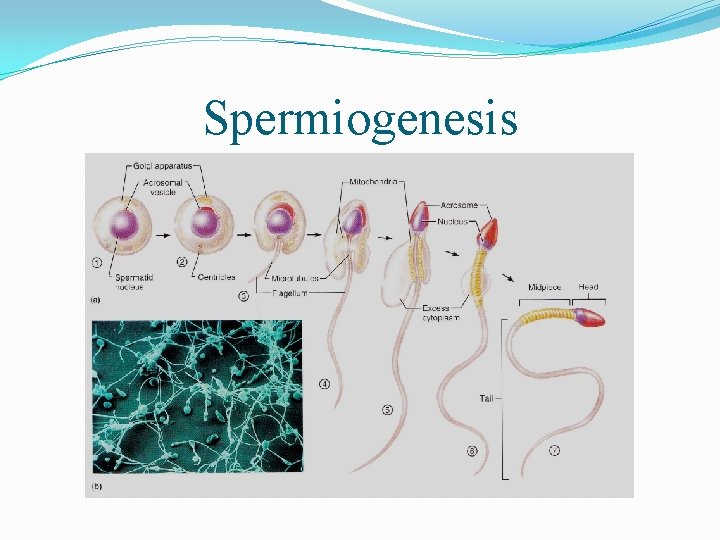
Spermiogenesis �Each spermatid has the haploid number of chromosomes and therefore has the genetic material for fertilization, however it is not mobile. �The spermatid undergoes spermiogenesis during which it elongates and forms a tail. �The resulting sperm or spermatazoon has a head, midpiece and a tail.
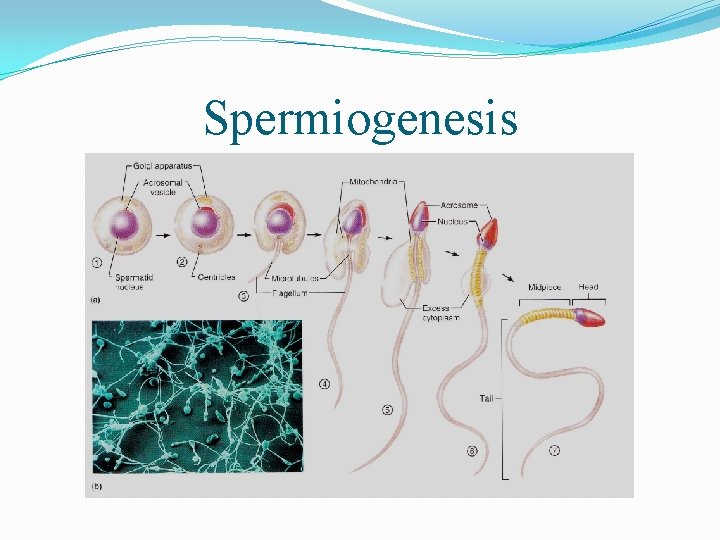
Spermiogenesis
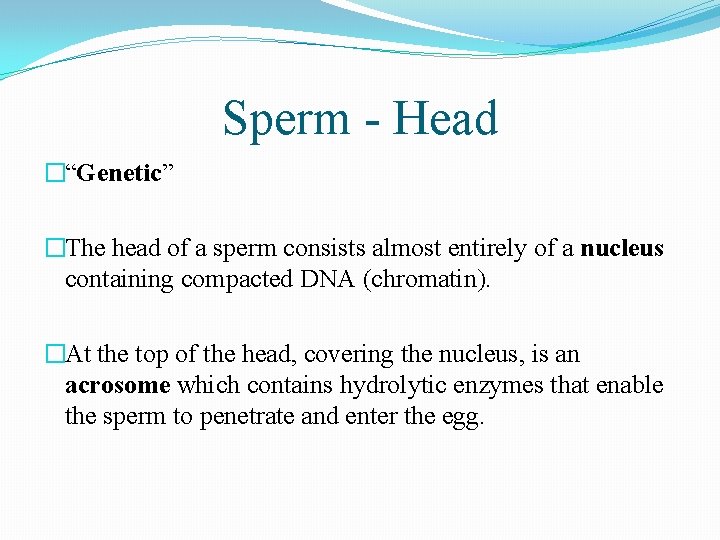
Sperm - Head �“Genetic” �The head of a sperm consists almost entirely of a nucleus containing compacted DNA (chromatin). �At the top of the head, covering the nucleus, is an acrosome which contains hydrolytic enzymes that enable the sperm to penetrate and enter the egg.
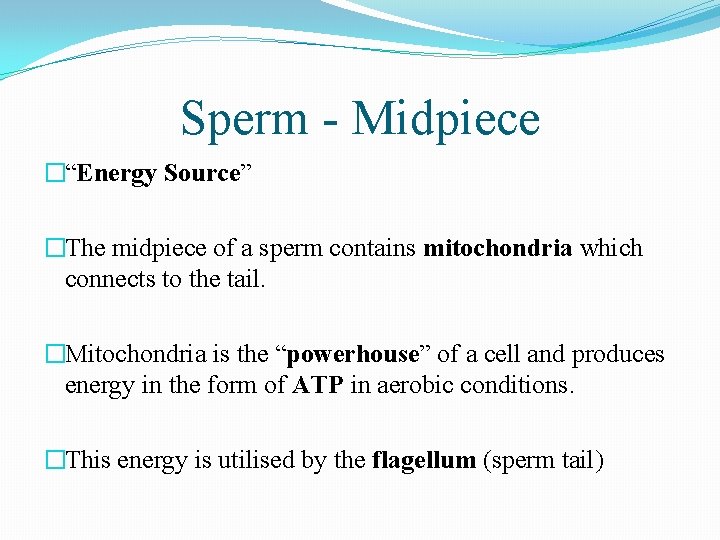
Sperm - Midpiece �“Energy Source” �The midpiece of a sperm contains mitochondria which connects to the tail. �Mitochondria is the “powerhouse” of a cell and produces energy in the form of ATP in aerobic conditions. �This energy is utilised by the flagellum (sperm tail)
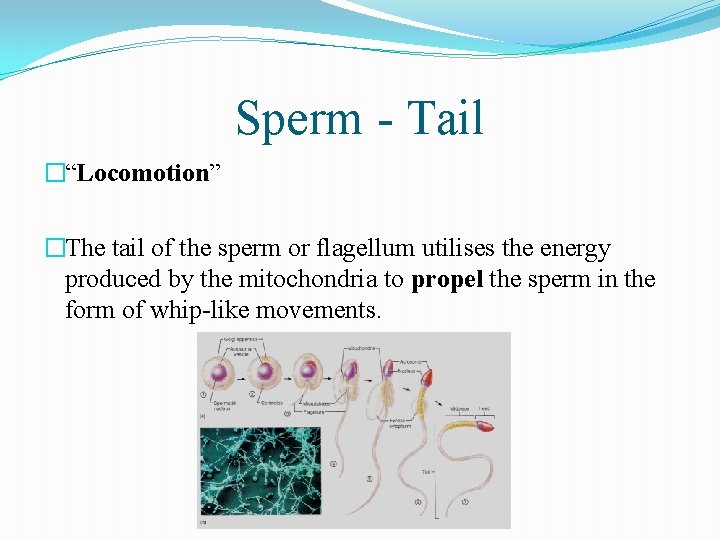
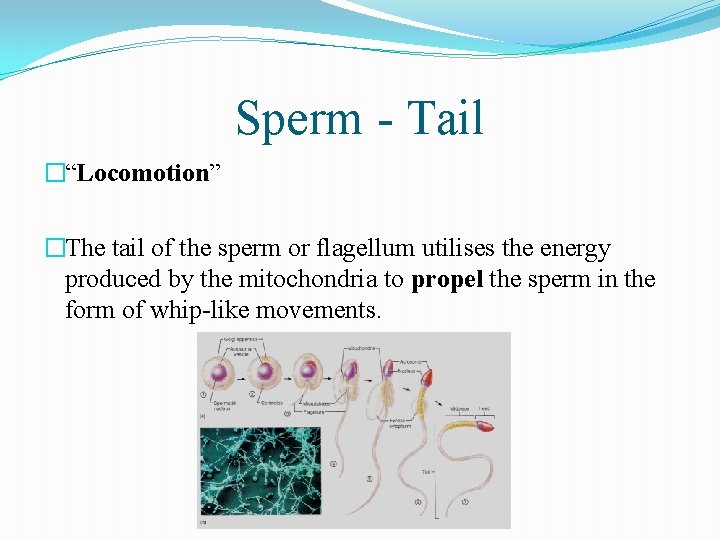
Sperm - Tail �“Locomotion” �The tail of the sperm or flagellum utilises the energy produced by the mitochondria to propel the sperm in the form of whip-like movements.
Spermatogenesis
Purpose of Sperm �The purpose of sperm is to provide protection and transport of the genetic material from the male to the ova (egg) in the female so fertilization can occur.
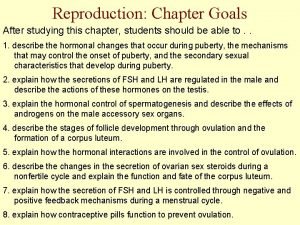
Hormonal Regulation of Spermatogenesis � FSH (Follicle Stimulating Hormone) � Informs spermatogenic cells (cells that form sperm) to produce testosterone which stimulates spermatogenesis. � LH (Luteinizing Hormone) � Introduction of LH results in the testosterone being released, triggering spermatogenesis. � Testosterone (extra information) � Hormone which controls the regulation of FSH and LH, � when sperm count is high - restricts FSH release � when sperm count is low - allows FSH release to continue � FSH and LH are found in both males and females however they play a larger role within the production of the ova.
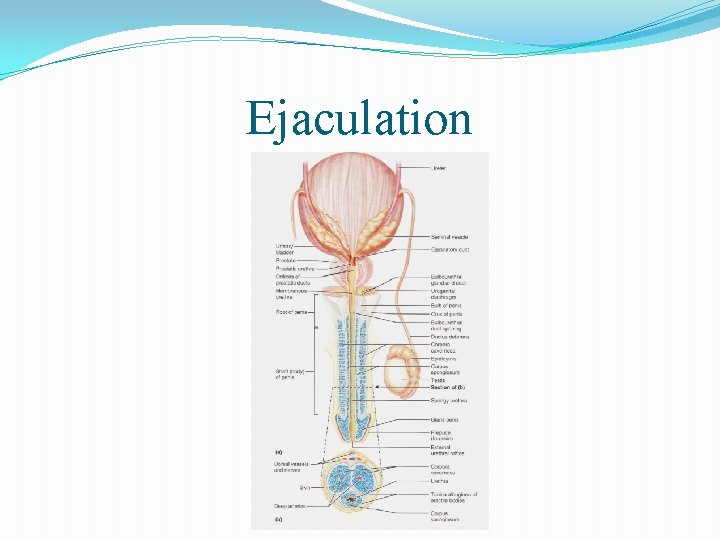
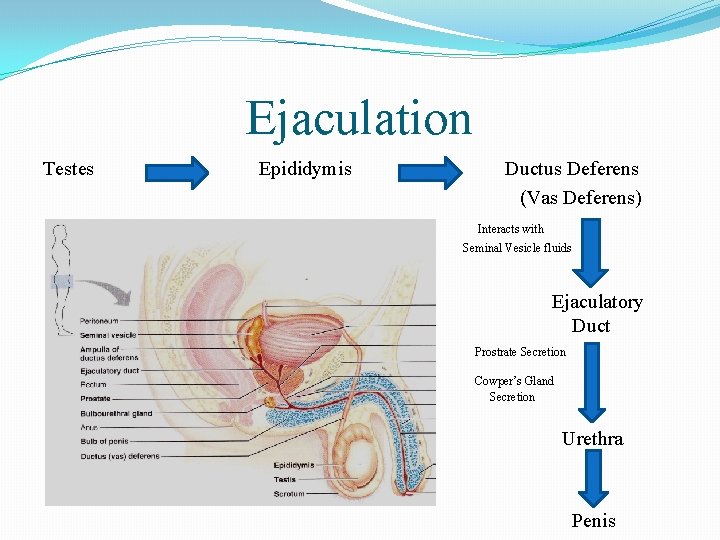
Ejaculation - Epididymis �The epidydimis consists of a coiled duct of approximately 6 metres which allows for nutrients transport to the sperm in the lumen. �The sperm swim through the epidydimis until reaching the ductus deferens or vas deferens, a process which takes about 20 days.
Ejaculation - Ductus Deferens �“Vas Deferens” �Continuing from the epididymis duct, the vas deferens consists of a spermatic cord which eventually forms the ampulla, joining with the seminal vesicles to form the ejaculatory duct. �The vas deferens is the site of a vasectomy where the cord is cut and tied at the ends so the sperm cannot escape.
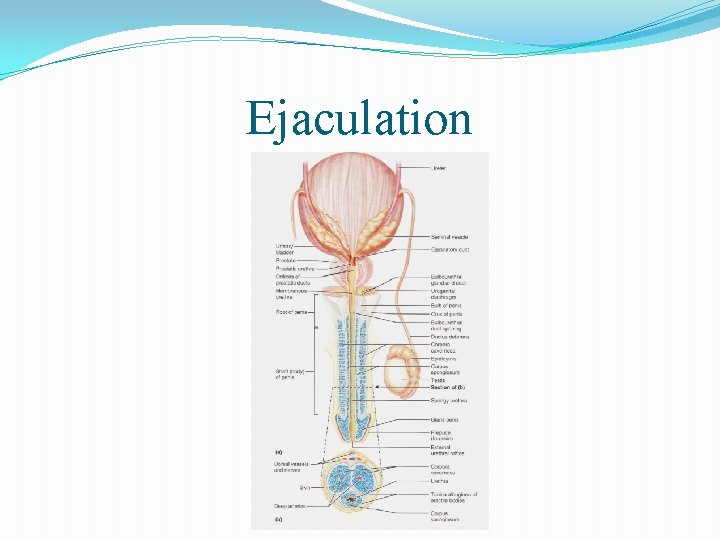
Ejaculation
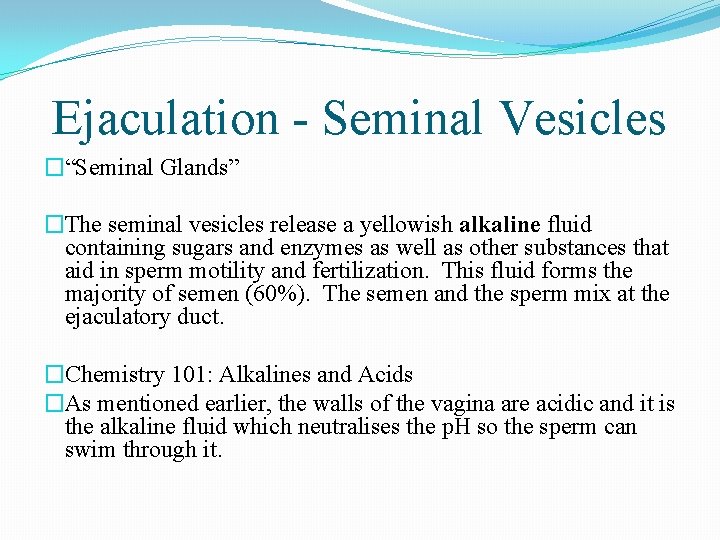
Ejaculation - Seminal Vesicles �“Seminal Glands” �The seminal vesicles release a yellowish alkaline fluid containing sugars and enzymes as well as other substances that aid in sperm motility and fertilization. This fluid forms the majority of semen (60%). The semen and the sperm mix at the ejaculatory duct. �Chemistry 101: Alkalines and Acids �As mentioned earlier, the walls of the vagina are acidic and it is the alkaline fluid which neutralises the p. H so the sperm can swim through it.
Ejaculation - Urethra �The urethra is a tube which is utilised in both reproductive and urinary systems, �linking from the ejaculatory duct for the reproductive system �linking from the urinary bladder for the urinary system �The Prostate Gland the Balbourethral Glands (Cowper’s Glands) enter the urethra during the reproductive system.
Ejaculation - Prostate Gland �The prostate gland encircles the beginning of the urethra and secretes a milky fluid containing nutrients and enzymes for the sperm. �This secretion makes up approximately 33% (one-third) of semen, with the resulting 6% made up of sperm and Cowper’s glands secretions.
Ejaculation - Cowper’s Glands �“Bulbourethral Glands” �Produce a thick, clear mucus which drains into the urethra when a man becomes sexually excited and neutralises acidic urine in the urethra.
Semen �The secretions of the accessory glands (seminal vesicles, prostate gland, Cowper’s glands) along with sperm, is collectively known as semen. �As mentioned earlier, the secretions of the accessory glands provide the sperm with a nutrient source and are utilised by the sperm for protection (alkaline) however they are also used as a mode of transport (liquid used to swim in).
Ejaculation - Penis �Along with the scrotum forms the external male genitalia. �Copulatory organ, designed to deliver sperm into the female reproductive tract. �When excited, blood begins to enter the penis rapidly with muscles preventing its release, resulting in an erection.
Ejaculation - Orgasm �Ejaculation is the propulsion of semen from the male reproductive system. �In order for this propulsion to occur, impulses reach a critical level, resulting in: �The reproductive ducts and accessory glands contracting, emptying and further contents into the urethra �Muscles contracting at the bladder preventing urine release �Contractions of the penis, propelling semen at a speed of 5 m/s. �This event of ejaculation is referred to as an orgasm or climax.
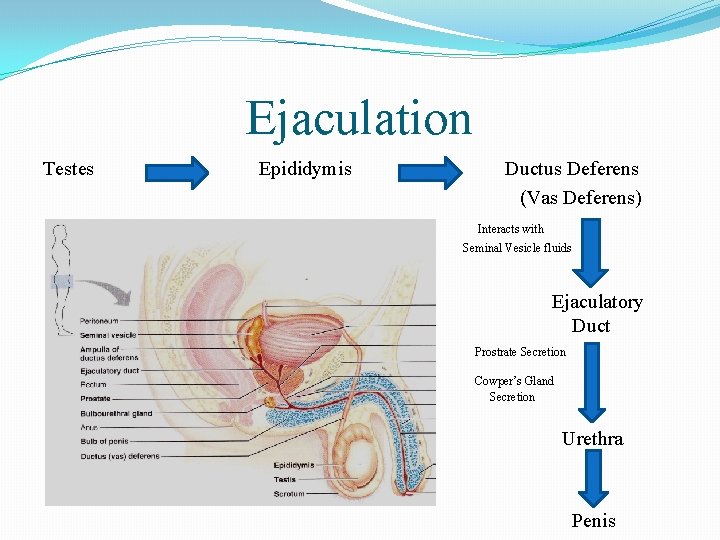
Ejaculation Testes Epididymis Ductus Deferens (Vas Deferens) Interacts with Seminal Vesicle fluids Ejaculatory Duct Prostrate Secretion Cowper’s Gland Secretion Urethra Penis
Summary �Importance of Scrotal Sac �Spermatogenesis-Where it occurs, How it occurs, Why is it important? �Importance of Sperm �Ejaculation process- Starts at testes, then to epididymis, then to vas deferens. . . What occurs at each section? �Importance of Semen
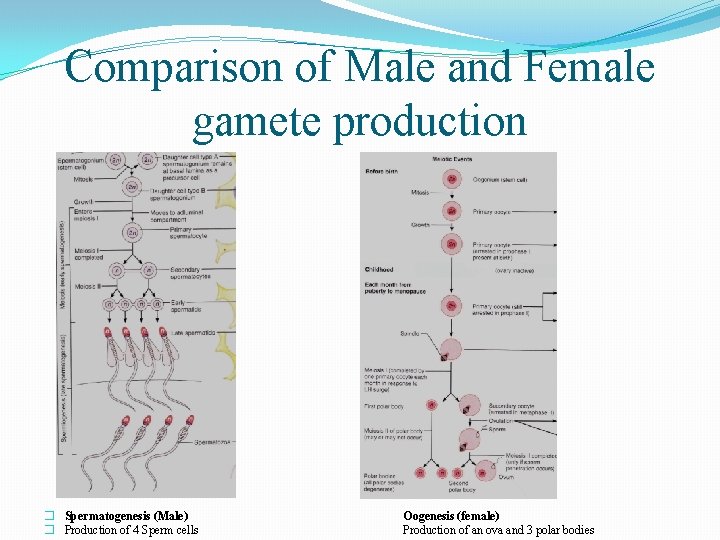
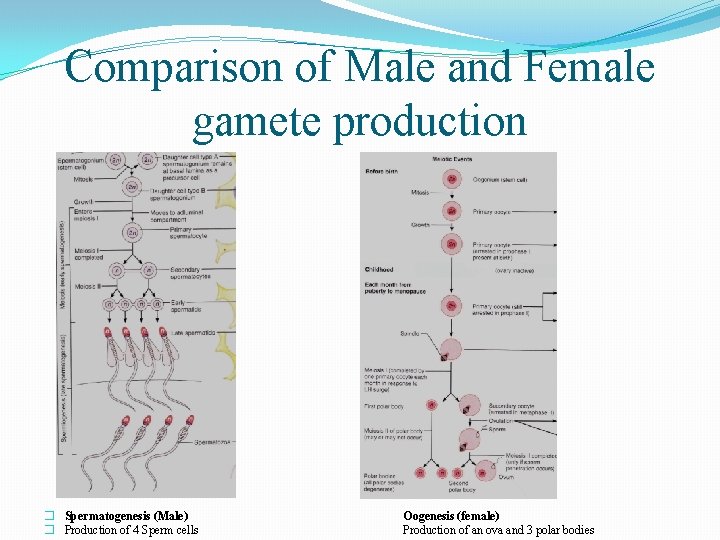
Comparison of Male and Female gamete production � Spermatogenesis (Male) � Production of 4 Sperm cells Oogenesis (female) Production of an ova and 3 polar bodies
 Male reproductive system from front
Male reproductive system from front Reproductive system function
Reproductive system function Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Exercise 42 anatomy of the reproductive system
Exercise 42 anatomy of the reproductive system Oogenesis
Oogenesis Spermiogenesis
Spermiogenesis Female and male reproductive system
Female and male reproductive system Produces a lubricating mucus that cleanses the urethra
Produces a lubricating mucus that cleanses the urethra Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male plant reproductive system
Male plant reproductive system Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Male reproductive system produces sperm cells
Male reproductive system produces sperm cells Male reproductive system
Male reproductive system Prostate anatomy
Prostate anatomy Examples of asexual reproduction
Examples of asexual reproduction Disease traductor
Disease traductor Diagram of male and female reproductive system of fish
Diagram of male and female reproductive system of fish Reproductive system of pila
Reproductive system of pila Uterus pig
Uterus pig Female part of a flower
Female part of a flower Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Boar reproductive system
Boar reproductive system Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Male reproductive system labeled
Male reproductive system labeled Pathway of semen
Pathway of semen Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male plant reproductive system
Male plant reproductive system Summary of male reproductive system
Summary of male reproductive system