Human Reproduction Male Reproductive Anatomy Spermatogenesis and Male







- Slides: 33
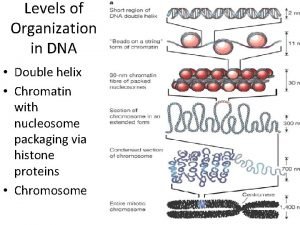
Human Reproduction Male Reproductive Anatomy Spermatogenesis and Male Hormones Male Reproductive Technologies and Birth Control Female Reproductive Anatomy Oogenesis and Female Hormones Uterine and Ovarian Cycles Development of the Fetus Parturition and Lactation Reproductive Technologies Teratogens and Birth Defects

Reproduction Ø Ø Reproduction ensures the survival of a species. Sexual reproduction produces offspring with new and unique characteristics that may increase their chance of survival. In advanced forms of reproduction, there are 2 types of gametes (sex cells). These are sperm, produced by the male, and eggs (ovum), produced by the female. Each of these gametes contains one half of the full complement of DNA required in a complete individual. Human females produce about 400 mature eggs from around ages 12 to 50. This is a relatively small number since females have about 400, 000 egg cells at birth! Males produce up to 1 billion sperm each day from the ages of about 13 to 80 or 90! The average gestational period for a human is 266 days.
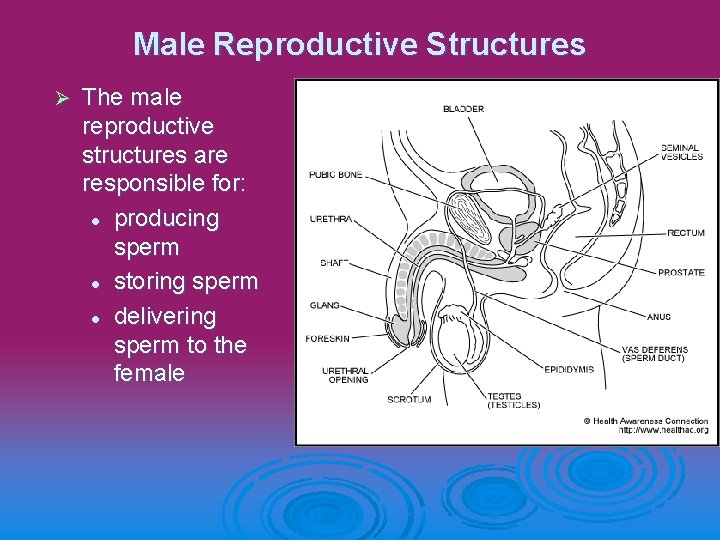
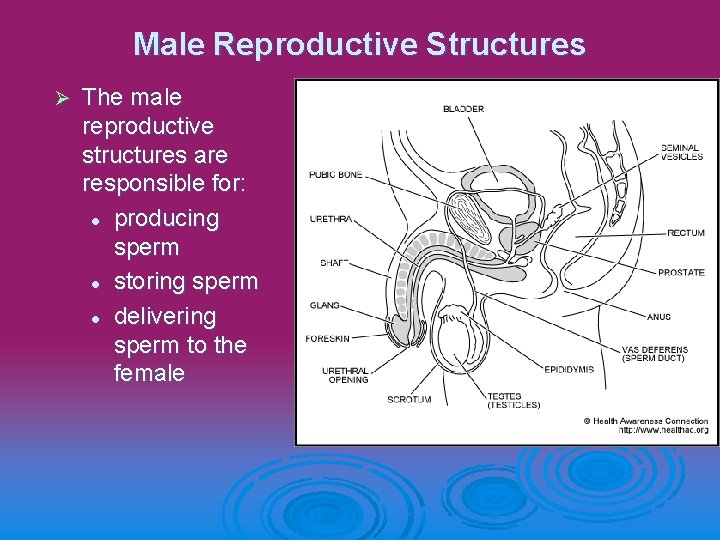
Male Reproductive Structures Ø The male reproductive structures are responsible for: l producing sperm l storing sperm l delivering sperm to the female
Sperm Producing Structures Scrotum –holds the testes away from the body to keep them cool. Sperm production only occurs at temperatures about 3 degrees below body temperature. Ø Testis – are the organs responsible for spermatogenesis. They develop inside the abdominal cavity of a male fetus and descend only about 2 months before birth. The testes hold seminiferous tubule that produce sperm. Ø Epididymis – holds spermatozoa for about 2 -4 days while they mature Ø Vas Deferens – stores sperm, and conducts sperm during ejaculation. When a male has a vasectomy, the vas deferens if cut and tied off, to prevent conduction of sperm. Ø
Semen Producing Structures Seminal Vesicle – produces a rich nutrient fluid that is an important component of semen. Ø Prostate Gland – produces a white, milky, alkaline fluid component of semen. This fluid neutralizes the acidity of urethra and the vagina, allowing sperm to survive. Ø Cowper’s Gland – produces a rich alkaline mucous that becomes part of the seminal fluid. This also neutralizes any acid sperm might be exposed to. Ø
Structures for Sperm Delivery Ø Ø Ejaculatory Duct – is responsible for the movement of fluid from the seminal vesicle to the vas deferens. Urethra – is responsible for conduction of urine and semen out of the penis. During ejaculation, a sphincter muscle closes off the bladder, preventing urine from exiting the urethra. Penis – is the male organ for copulation. Beneath the skin, lies the urethra surrounded by spongy protective tissue that expands to form the glans penis. Prepuce (foreskin) – is a loose sheath of skin covering the glans penis of uncircumcised males. The foreskin produces oily secretions
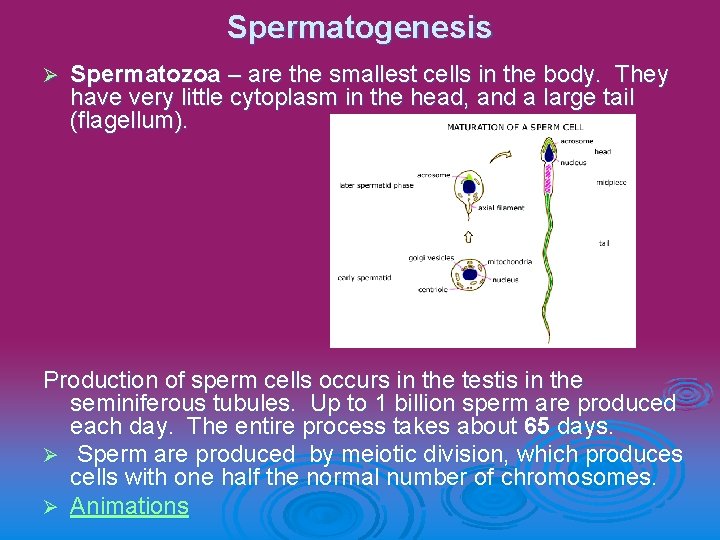
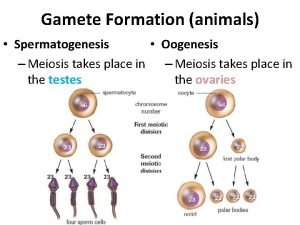
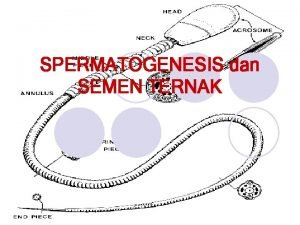
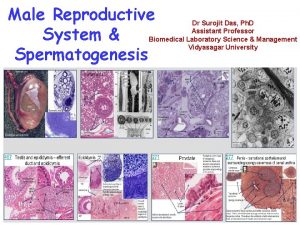
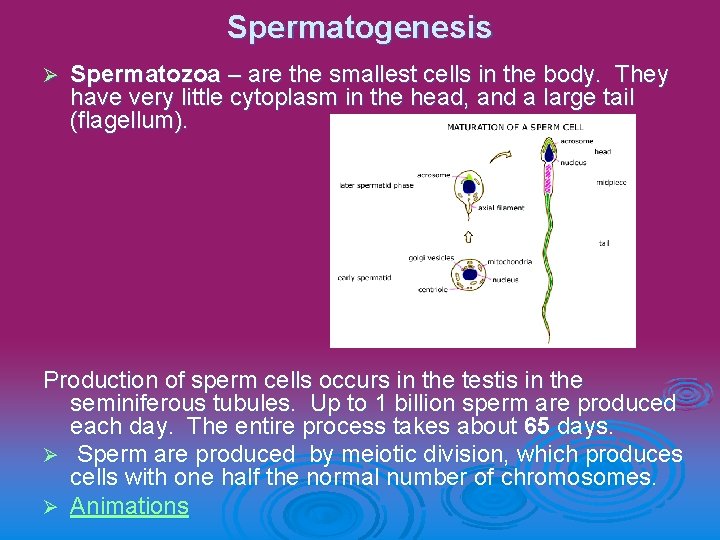
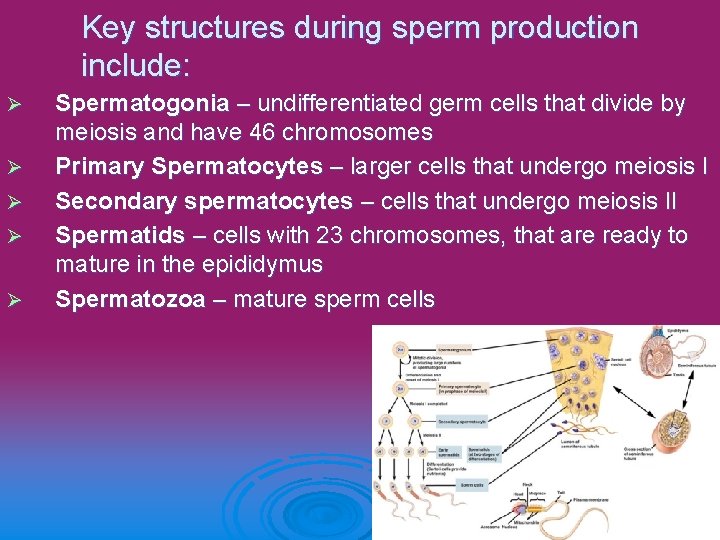
Spermatogenesis Ø Spermatozoa – are the smallest cells in the body. They have very little cytoplasm in the head, and a large tail (flagellum). Production of sperm cells occurs in the testis in the seminiferous tubules. Up to 1 billion sperm are produced each day. The entire process takes about 65 days. Ø Sperm are produced by meiotic division, which produces cells with one half the normal number of chromosomes. Ø Animations
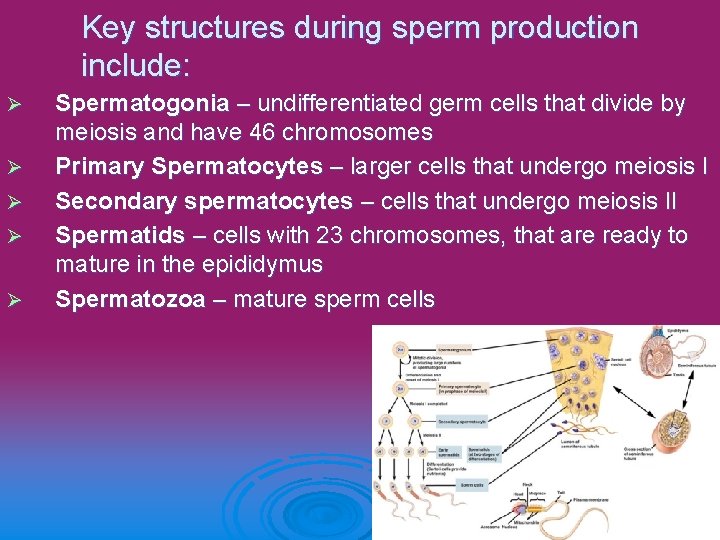
Key structures during sperm production include: Ø Ø Ø Spermatogonia – undifferentiated germ cells that divide by meiosis and have 46 chromosomes Primary Spermatocytes – larger cells that undergo meiosis I Secondary spermatocytes – cells that undergo meiosis II Spermatids – cells with 23 chromosomes, that are ready to mature in the epididymus Spermatozoa – mature sperm cells
Seminal Fluid Is produced by three different glands: Ø Seminal Vesicles – secrete a fluid high in fructose that provides energy sperm need to swim Ø Prostate Gland – produces a milky white alkaline fluid that neutralizes the acidity of the vagina Ø Cowper’s Gland – secretes a buffered fluid that cleanses and neutralizes the acidity in the urethra
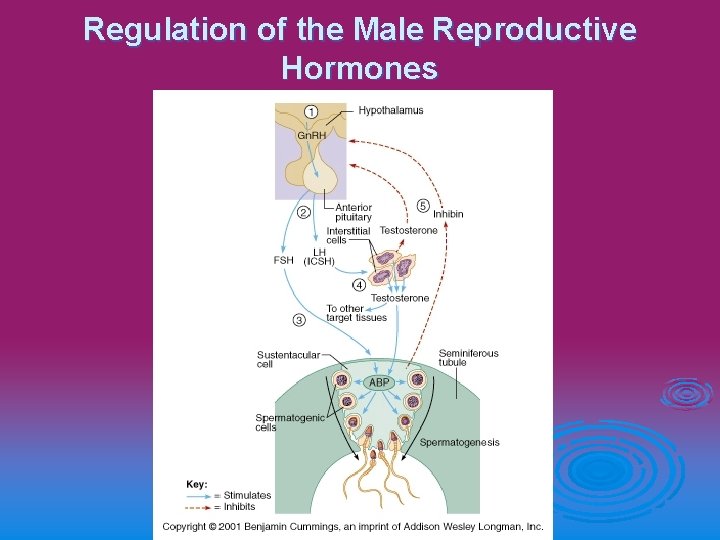
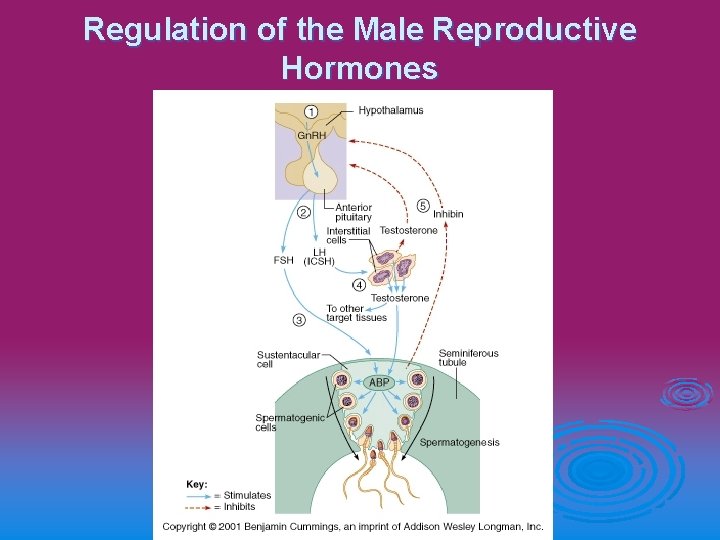
Regulation of the Male Reproductive Hormones
Male Reproductive Hormones Ø Ø Ø Gn. RH – gonadotropic releasing hormone, stimulates the anterior pituitary to release LH and FSH LH / ICSH – luteinizing hormone, stimulates the interstitial cells of the testes to produce testosterone FSH – follicle stimulating hormone, stimulates production of sperm in the seminiferous tubules, acts on the sertoli cells Testosterone – responsible for male secondary sex characteristics, required for sperm production Interstitial Cells – surround the seminiferous tubules, produce testosterone when stimulated by LH Sertoli Cells – provide nutrients and support for developing sperm, affected by inhibin and FSH

Female Reproductive Structures Ø The female reproductive structures are responsible for - reception of sperm - producing an egg - nourishing and protecting the fetus - delivering the baby
Internal Structures Ø Ø Ø Vagina – facilitates intercourse by accepting the penis, acts as the birth canal during labor, p. H is generally acidic Cervix – Thick muscular tissue that plugs closed with mucous during pregnancy and prevents material from getting into the uterus, and holds the baby in Uterus (womb) – pear shaped muscular organ (5 cm wide) that houses the developing fetus during pregnancy (30 cm wide), strong contractions help push the baby out during birth Oviducts / fallopian tubes – responsible for the conduction of the ovum (egg) from the ovaries to the uterus, this is where fertilization usually takes place Fimbrae – small fingerlike projections at the ends of the oviducts that sweep to draw the egg into the fallopian tube Ovaries – produce the ovum from follicles found in the outer cortex (most females are born with about 2 million follicles, and only 300 -400, 000 will remain at puberty)
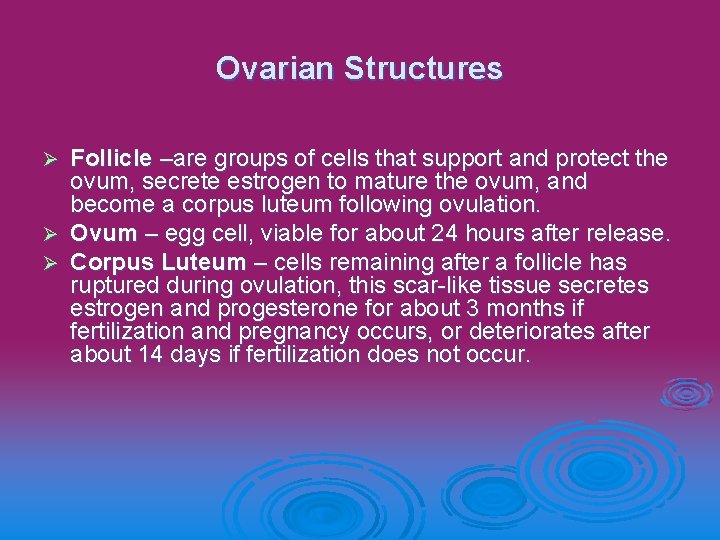
Ovarian Structures Follicle –are groups of cells that support and protect the ovum, secrete estrogen to mature the ovum, and become a corpus luteum following ovulation. Ø Ovum – egg cell, viable for about 24 hours after release. Ø Corpus Luteum – cells remaining after a follicle has ruptured during ovulation, this scar-like tissue secretes estrogen and progesterone for about 3 months if fertilization and pregnancy occurs, or deteriorates after about 14 days if fertilization does not occur. Ø
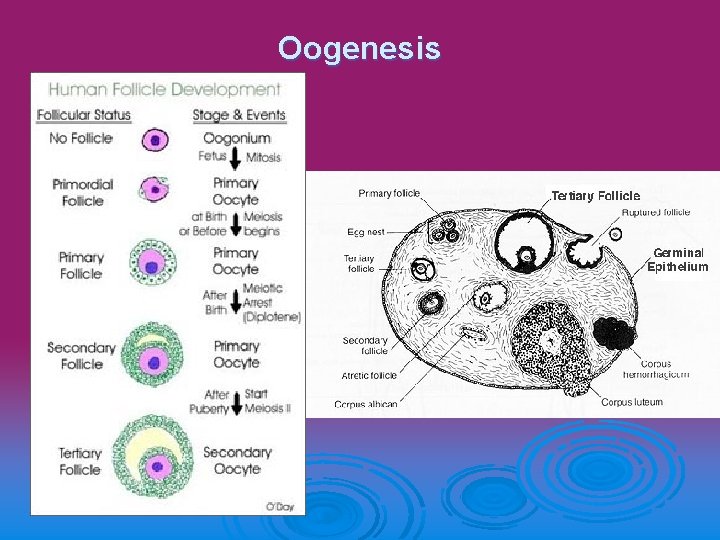
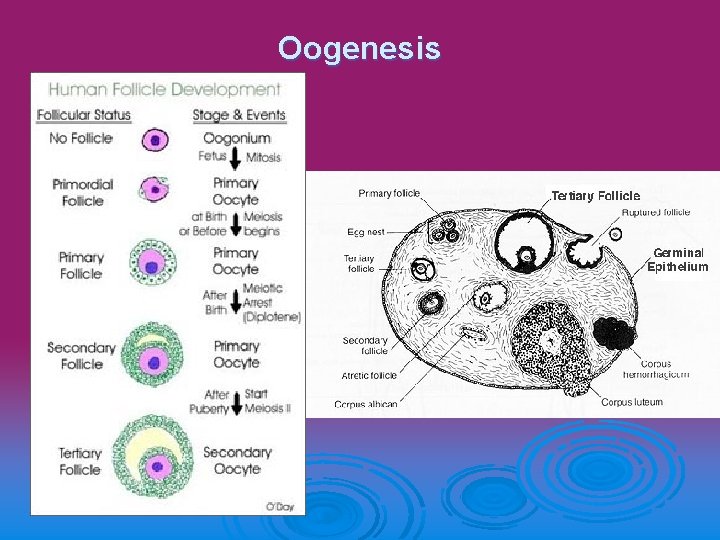
Oogenesis
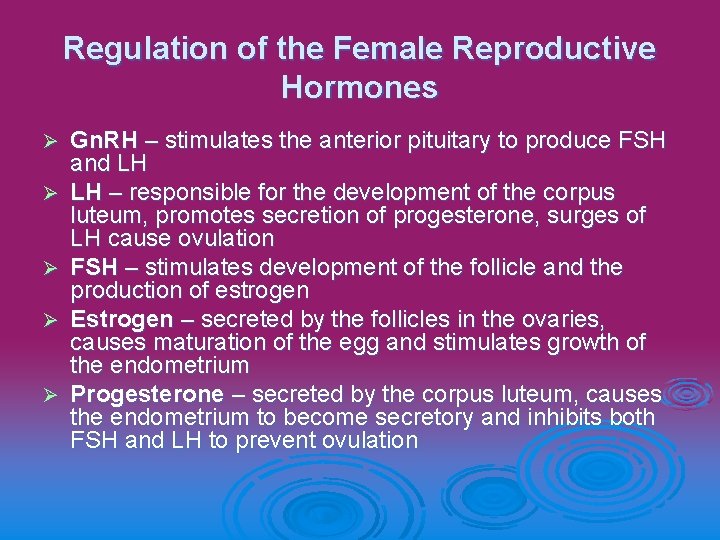
Regulation of the Female Reproductive Hormones Ø Ø Ø Gn. RH – stimulates the anterior pituitary to produce FSH and LH LH – responsible for the development of the corpus luteum, promotes secretion of progesterone, surges of LH cause ovulation FSH – stimulates development of the follicle and the production of estrogen Estrogen – secreted by the follicles in the ovaries, causes maturation of the egg and stimulates growth of the endometrium Progesterone – secreted by the corpus luteum, causes the endometrium to become secretory and inhibits both FSH and LH to prevent ovulation
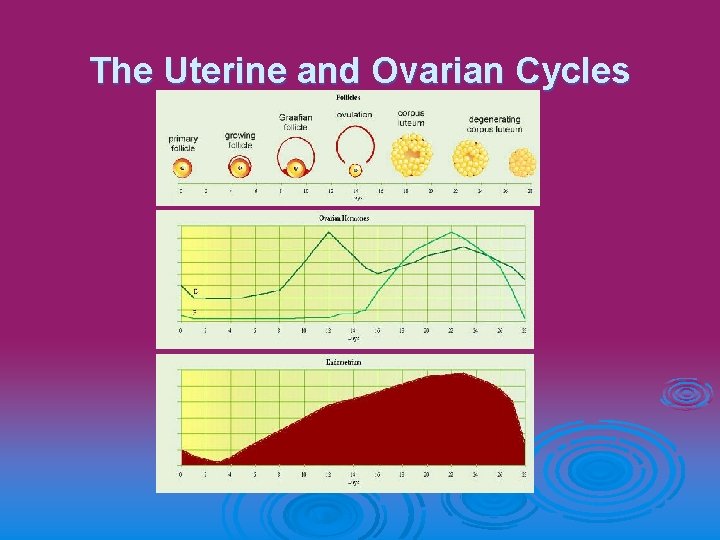
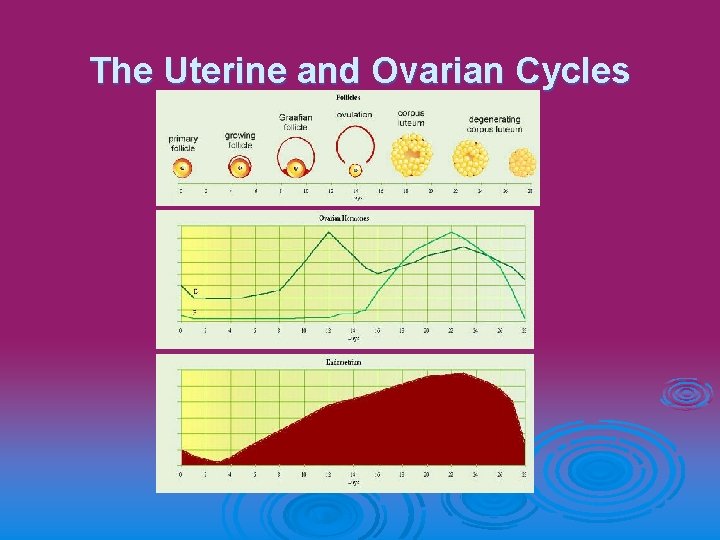
The Uterine and Ovarian Cycles

The Ovarian Cycle Ø Ø Ø Ø Day 1 -13: Follicular Phase FSH is secreted by the anterior pituitary and promotes formation of he follicle. The follicle releases estrogen, which promotes growth of the endometrium. Day 14: Ovulation - The ovum is released causing the follicle to rupture. This lowers the levels of FSH produced. Day 15 – 28: Luteal Phase LH is secreted by the anterior pituitary and promotes formation of the corpus luteum, which produces progesterone, inhibits Gn. RH, LH and FSH, preventing subsequent ovulation. No Fertilization corpus luteum degenerates, estrogen and progesterone levels drop, and menstruation occurs. Fertilization corpus luteum is maintained by HCG (human chorionic gonadotropic hormone) secreted by the developing embryo. Gn. RH, LH and FSH are inhibited by progesterone, and ovulation cannot occur during pregnancy. Estrogen levels also remain high to maintain the endometrium.
The Uterine Cycle Ø Ø Ø Ø Day 1 -5: Menstruation All hormone levels are low. The endometrium is sloughed off and the lining is shed. This is known as menstrual bleeding. Day 5 – 14: Proliferative Phase FSH promotes formation of the follicle, which produces estrogen. The estrogen causes vascularization / thickening of the endometrium in preparation to receive a fertilized egg. Day 14: Ovulation - A surge of LH causes the corpus luteum to form. Day 15 -28: Secretory Phase The corpus luteum secretes progesterone. If fertilization does not occur, the corpus luteum will degenerate after about 10 days. When the corpus luteum degenerates, the levels of estrogen and progesterone drop sharply, and menstruation begin. If fertilization does occur, the corpus luteum continues producing estrogen and progesterone, maintaining the uterine lining. http: //www. msnbc. com/news/wld/graphics/menstrual_cycle_dw 2. swf
Fertilization and Pregnancy Fertilization – sperm are deposited into the vagina, where they travel through the cervix, through the uterus and up into the fallopian tube. Sperm usually meet the ovum in the fallopian tube. Only one spermatozoa will fertilize an egg. Once a sperm has penetrated the egg, enzymatic changes on the head of the sperm, and the outer coating of the egg, prevent penetration from other sperm. Ø http: //www. uchsc. edu/ltc/fert. swf Ø

Implantation- the fertilized egg (embryo) embeds itself in the endometrium. The embryo produces HCG (human chorionic gonadotropic hormone) which maintains the corpus luteum for about 2 -3 months. This hormone is detected in blood or urine with a pregnancy test, as early as the first day of a missed period. Ø Placenta – forms around the fetus. The placenta is responsible for the exchange of gases, delivery of nutrients and removal of wastes for the fetus. There is no blood shared between the mother and the fetus. A fetus may have a different blood type than the mother. Ø
How old are you? Ø Gestational age – the length of pregnancy is 38 to 40 weeks, or 266 days. The gestational age is calculated from the first day of the mother’s last menstrual period. Ø Fertilization age – is the actual age of the fetus. It is usually estimated to be about two weeks shorter than the date of the last menstrual period. To calculate due date: LMP – 3 months + 7 days Ø h. CG Pregnancy Test (ELISA) Ø
Early Stages of Embryonic Development: Ø Ø Ø Zygote –fertilized egg, divides by cleavage, mitosis with no increase in size Morula – solid ball of cells the same size as the fertilized egg Blastula – hollow ball of cells filled with fluid, outer layer forms the chorion, inner layer forms the fetus Gastrula – the blastula pushes in (invaginates) and forms the 3 primary germ layers, the hollow space forms a primitive gut BERP: Overview
Germ Layers Endoderm – forms the lining of the GI tract, trachea, bronchi, lungs, gallbladder, urethra, liver, pancreas, thyroid and urinary bladder Ø Mesoderm – forms the muscles, dermis, connective tissue, bone, cartilage, blood vessels, kidneys and reproductive organs Ø Ectoderm – forms the epidermis of the skin, hair, nails, nervous system, spinal cord, retina, lens, inner ear, lining of the nose, mouth, anus and tooth enamel Ø
The first month… Ø Ø Ø Neurula – appearance of the nervous system in a neural tube (21 days) Somites – blocklike portions of the neurula that give rise to the segmented muscles and vertebral bones Coelom – forms the gut cavity Pharyngeal pouches – primitive gill slits Stage 1
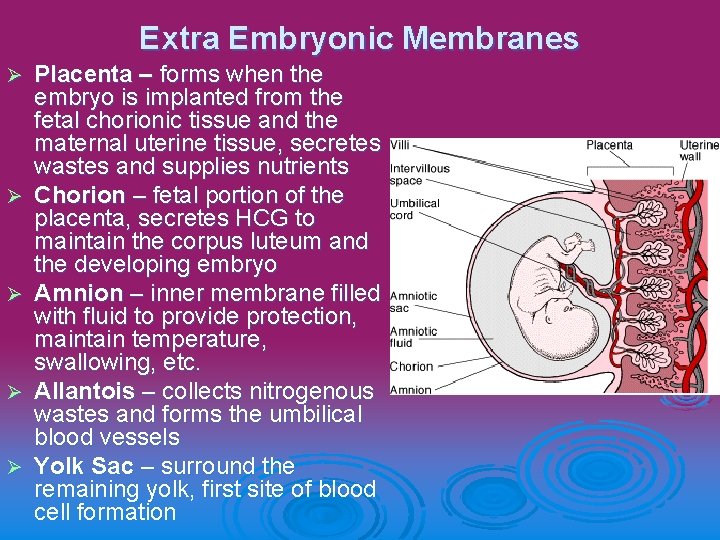
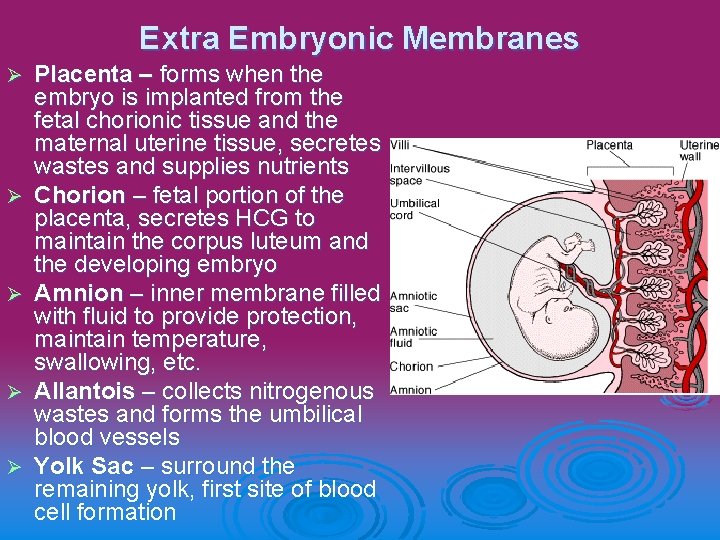
Extra Embryonic Membranes Ø Ø Ø Placenta – forms when the embryo is implanted from the fetal chorionic tissue and the maternal uterine tissue, secretes wastes and supplies nutrients Chorion – fetal portion of the placenta, secretes HCG to maintain the corpus luteum and the developing embryo Amnion – inner membrane filled with fluid to provide protection, maintain temperature, swallowing, etc. Allantois – collects nitrogenous wastes and forms the umbilical blood vessels Yolk Sac – surround the remaining yolk, first site of blood cell formation

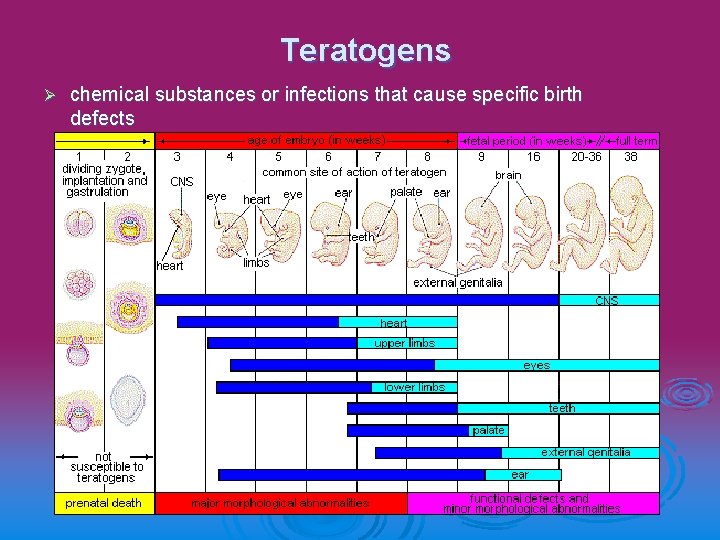
Milestones of Development Ø Ø Ø Ø 1 week – fertilization, cleavage, morula, blastocyst 2 weeks – implantation, chorion secretes HCG, 3 germ layers form 3 weeks – nervous system is evident, heart begins to form (2 tubes) 4 -5 weeks – limb buds appear, eyes, ears and nose develop, umbilical cord is attached to placenta 6 -8 weeks – fetus is recognizable as a human, all organ system are developed, reflexes begin (size = 1. 5”, 0. 5 g) 9 -16 weeks – heartbeat is audible with a stethoscope, bone replaces cartilage, eyelashes, etc formed (size = 6”, 0. 5 lb) 17 -28 weeks – movement if felt by mother, lanugo and vernix caseosa covers the skin, eyelids open (size = 12”, 3 lb) 20 -40 weeks – fetus moves to head down position, significant weight gain, lungs mature after about 32 weeks (size = 21”, 7. 5 lbs)
Virtual Develoment Ø Conception to Birth, Anatomical Travelogue
Parturition and Lactation Ø Ø Ø Parturition – birth caused by the release of prostoglandins that cause the release of oxytocin from the posterior pituitary of the mother. Parturition takes place in 3 stages: Stage 1 – dilation and effacement of the cervix, mucous plug dislodges, uterine contractions open the cervix Stage 2 – delivery of the baby, cervix is dilated to about 10 cm, intense contractions every 1 -2 min push the baby down the birth canal Stage 3 – delivery of the placenta UAB Health System | Childbirth

The average labor lasts about 12 hours, but can range from 1 hour to 36 hours. Sometimes if the delivery does not go well, or if the baby or mother is at risk, a ceasarean section may be required. This involves removing the baby from an incision in the front of the abdomen. Ø Immediately after the baby is born, the mother is encouraged to nurse the infant. At the end of pregnancy, prolactin stimulates the glandular tissue in the breasts to produce fluids, colostrum and milk. Colostrum is a rich fluid containing mostly sugar and proteins. This first milk is believed to play a role in early immunity. Regular suckling stimulates the pituitary gland to release oxytocin, which causes uterine contractions and the “let down” of milk. At the peak of production, a woman can make as much as 1. 5 L of milk each day. Ø

Reproductive Technologies and Health Ø Ø Ø Pap Smear – a sample of cervical cells are taken and examined for abnormal growth (cancer) Ultrasound – uses sound waves to view the baby in the womb Ultrasound Scan Fetal Video Clips Amniocentesis – sampling of the cells from the amniotic fluid at about 16 weeks to check for genetic abnormalities Chorionic Villus Sampling – sampling of cells from the chorion at about 5 weeks to check for genetic abnormalities http: //www. pbs. org/wgbh/nova/miracle/windows. html
Fertility Technologies Ø Ø Ø Ø Ø IVF – in vitro fertilization – fertilizing the egg in a petri dish, and implanting the embryo 2 -4 days later Life Changine Science - Program 3: IVF AID – artificial insemination by donor Egg Screening – testing and selecting eggs to be fertilized TSE – testicular sperm extraction ICSI – intracytoplasmic sperm injection GIFT – gamete intra-fallopian transfer AH – assisted hatching Embryo Transfer – implantation of an embryo into the womb or fallopian tube Fertility Drugs – induce ovulation, usually many ova are produced at one time, often results in multiples
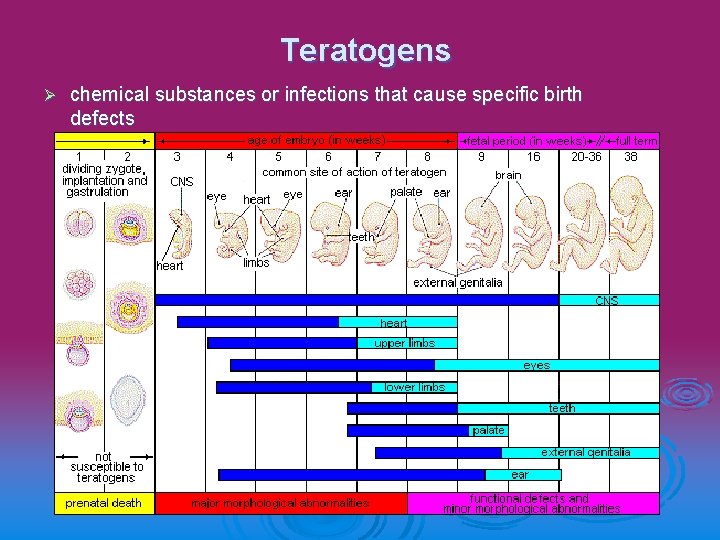
Teratogens Ø chemical substances or infections that cause specific birth defects
 Seminal vesicle function
Seminal vesicle function Chapter 2 human reproductive anatomy and physiology
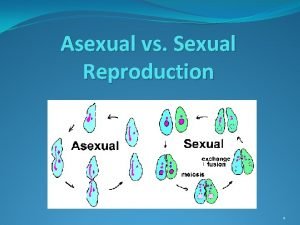
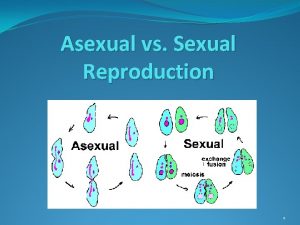
Chapter 2 human reproductive anatomy and physiology Sexual reproduction and asexual reproduction
Sexual reproduction and asexual reproduction The disadvantages of sexual reproduction
The disadvantages of sexual reproduction Venn diagram of asexual and sexual
Venn diagram of asexual and sexual Function of reproductive system
Function of reproductive system Male and female reproductive system
Male and female reproductive system Female and male reproductive system
Female and male reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ 90/2
90/2 Penis circumcised
Penis circumcised Male fish reproductive system
Male fish reproductive system Difference between oogenesis and spermatogenesis
Difference between oogenesis and spermatogenesis Gamete production
Gamete production Meiosis 1 spermatogenesis
Meiosis 1 spermatogenesis Chiasma
Chiasma Oogenesis defination
Oogenesis defination Testis and spermatogenesis
Testis and spermatogenesis Function of vagina
Function of vagina Anatomy of the reproductive system exercise 42
Anatomy of the reproductive system exercise 42 Corpus albicans vs corpus luteum
Corpus albicans vs corpus luteum Round ligament of uterus
Round ligament of uterus Figure of male reproductive system
Figure of male reproductive system Reproductive physiology
Reproductive physiology Reproduction system of plants
Reproduction system of plants Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is sperm stored in the male body
Where is sperm stored in the male body Male reproductive system
Male reproductive system Asexual reproduction
Asexual reproduction Disease traductor
Disease traductor Reproductive system of pila
Reproductive system of pila Fetal pig urinary system labeled
Fetal pig urinary system labeled Male plant reproductive system
Male plant reproductive system