The Reproductive System Chapter 16 1 Outline Functions
- Slides: 59
The Reproductive System Chapter 16 1
Outline • • Functions of the Reproductive Systems Male Reproductive System – • Penis Anatomy; Testes and Sperm; Hormonal Regulation Female Reproductive System – – Genital Tract Hormonal Levels and Ovulation v v – Fertilization and Pregnancy v v v – Steps of Fertilization Cleavage of Cells Implantation Development before Birth v v – Ovarian Cycle Uterine Cycle Extra-embryonic Membranes Fetal Circulation Birth v Female Breast and Lactation 2
Functions of the Reproductive System • • To produce offspring; maintain the species. Estrogen stimulates fat deposition. Estrogen stimulates liver to produce important transport proteins. Estrogen stimulates synthesis of bone matrix proteins, prevents bone loss. Testosterone stimulates synthesis of proteins for skeletal muscle and bone growth. Testosterone influences liver and kidney enzymes and stimulates release of erythropoietin. Both hormones influence cardiovascular health. 3
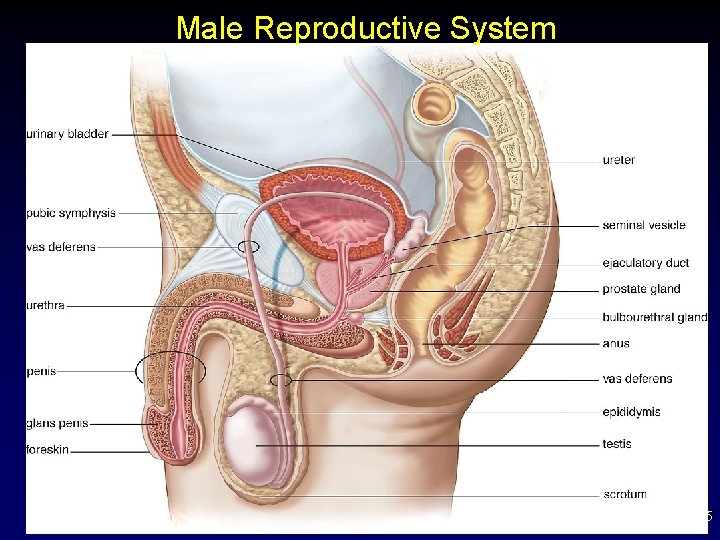
Male Reproductive System • • Male gonads, testes, are paired organs suspended in scrotum – Sperm, the male reproductive cells, are produced in testes and mature in epididymis (some storage in epididymis) v Travel to vas deferens for storage v Each vas deferens empties into a ejaculatory duct v Sperm are ejaculated from urethra Ejaculate consists of a fluid called semen composed of sperm and secretions from the seminal vesicles, prostate gland, and bulbourethral glands – Seminal vesicles- 60% of total volume; alkaline, viscous, clotting proteins, fructose – Prostate gland- 25% of total volume; slightly acidic, milky, citric acid, proteolytic enzymes-breakdown clot caused by seminal vesicle secretions, lysozyme & seminalplasmin- both antibiotic – Bulbourethral gland- alkaline, mucus 4
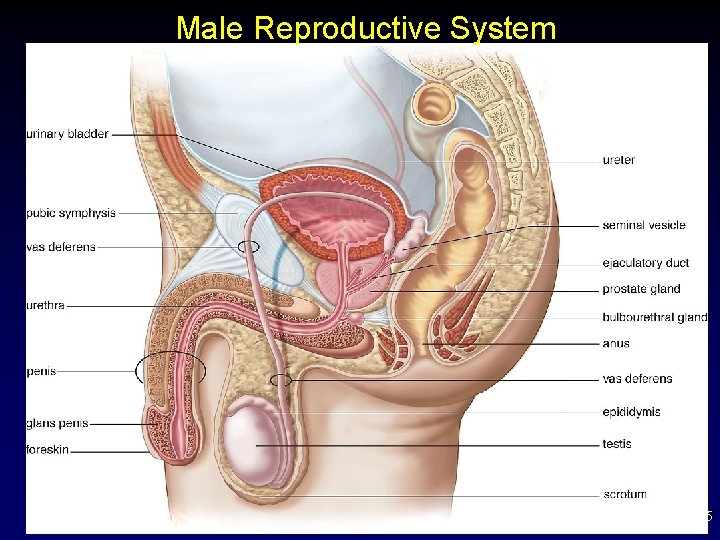
Male Reproductive System 5
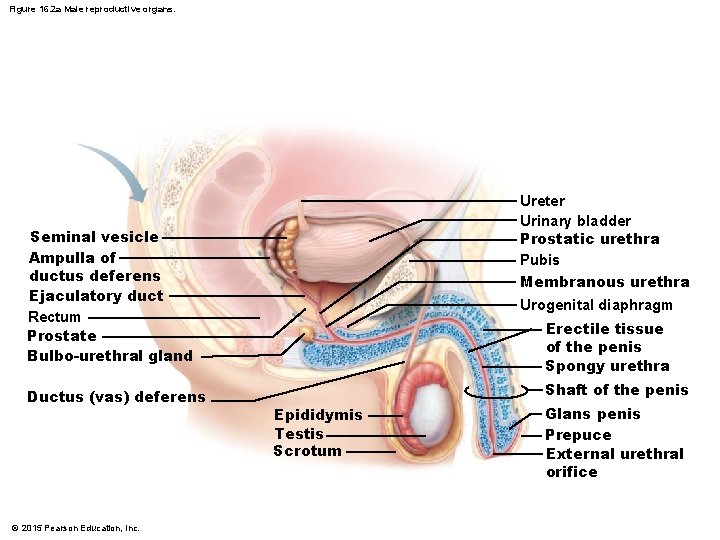
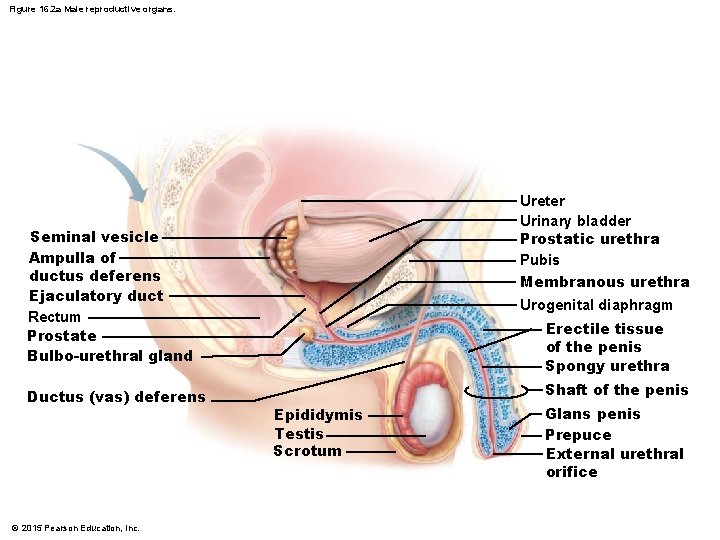
Figure 16. 2 a Male reproductive organs. Ureter Urinary bladder Prostatic urethra Pubis Membranous urethra Seminal vesicle Ampulla of ductus deferens Ejaculatory duct Rectum Prostate Bulbo-urethral gland Ductus (vas) deferens © 2015 Pearson Education, Inc. Urogenital diaphragm Erectile tissue of the penis Spongy urethra Shaft of the penis Epididymis Testis Scrotum Glans penis Prepuce External urethral orifice
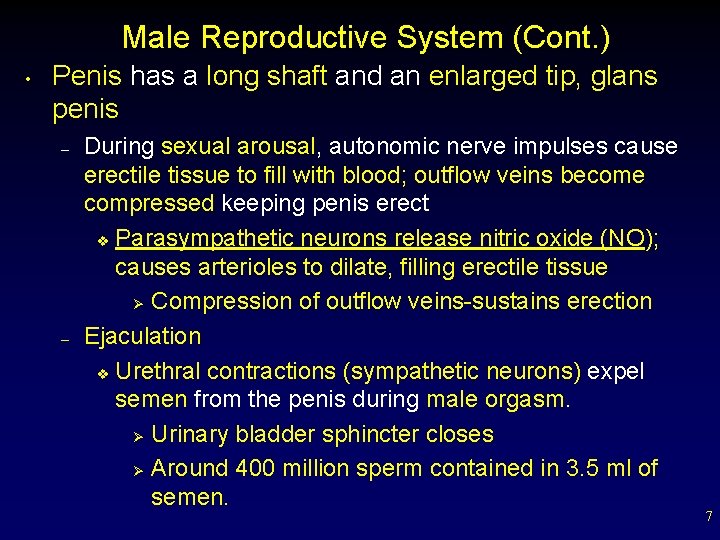
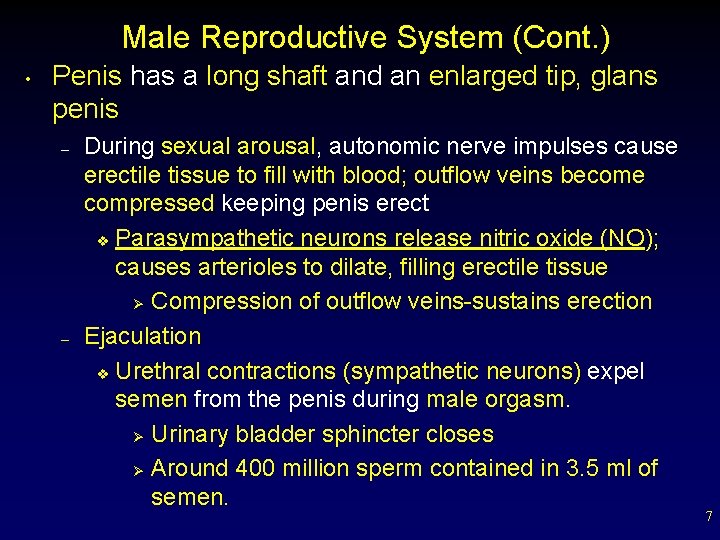
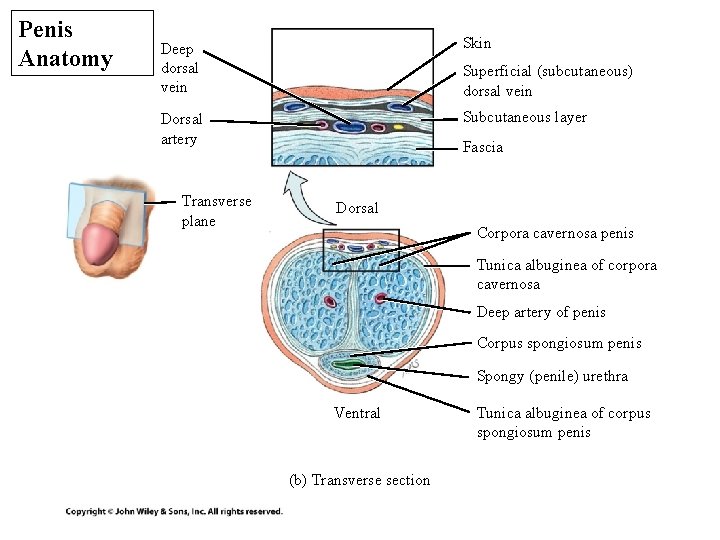
Male Reproductive System (Cont. ) • Penis has a long shaft and an enlarged tip, glans penis – – During sexual arousal, autonomic nerve impulses cause erectile tissue to fill with blood; outflow veins become compressed keeping penis erect v Parasympathetic neurons release nitric oxide (NO); causes arterioles to dilate, filling erectile tissue Ø Compression of outflow veins-sustains erection Ejaculation v Urethral contractions (sympathetic neurons) expel semen from the penis during male orgasm. Ø Urinary bladder sphincter closes Ø Around 400 million sperm contained in 3. 5 ml of semen. 7
Penis Anatomy Deep dorsal vein Skin Dorsal artery Subcutaneous layer Transverse plane Superficial (subcutaneous) dorsal vein Fascia Dorsal Corpora cavernosa penis Tunica albuginea of corpora cavernosa Deep artery of penis Corpus spongiosum penis Spongy (penile) urethra Ventral (b) Transverse section Tunica albuginea of corpus spongiosum penis
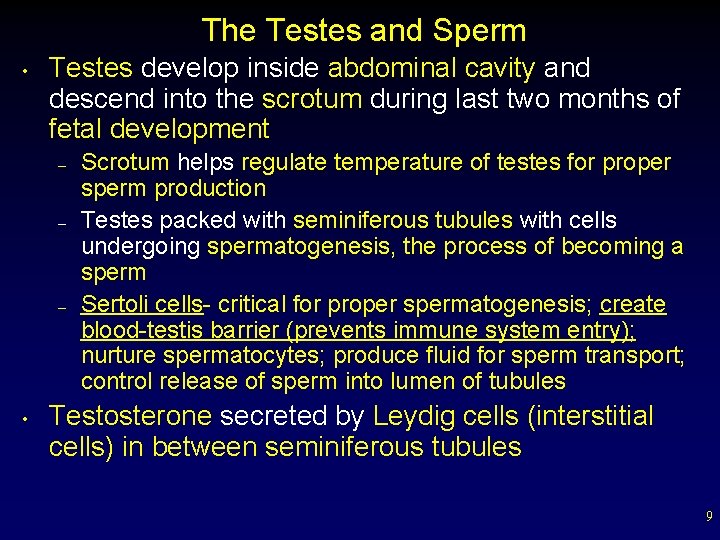
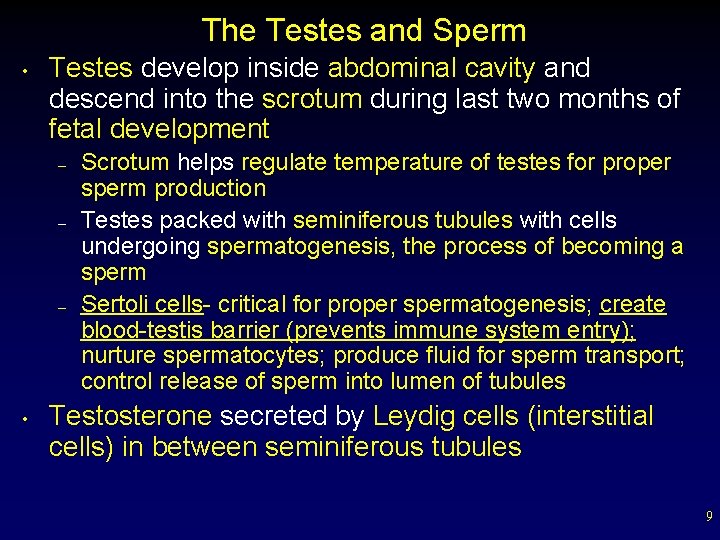
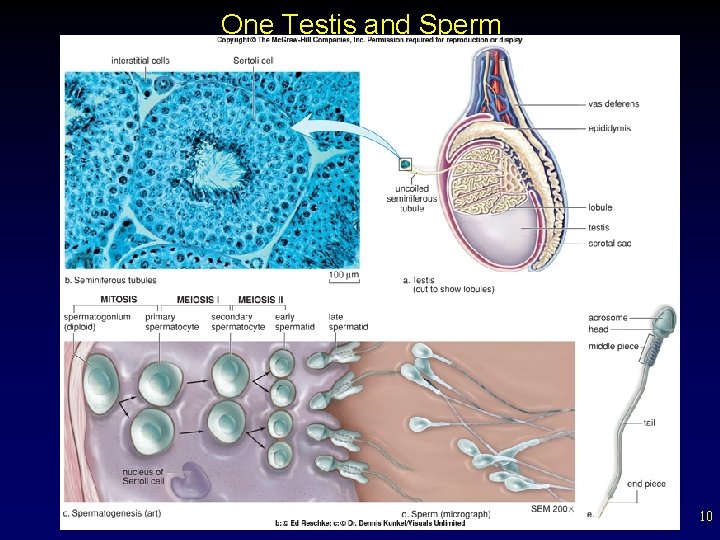
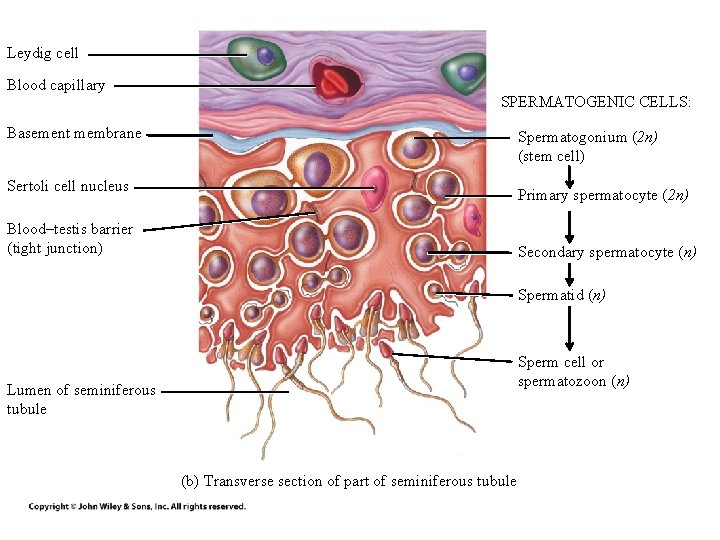
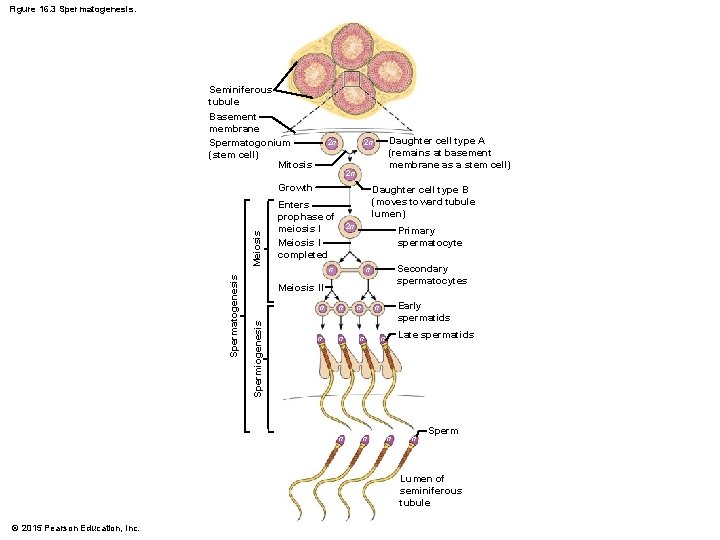
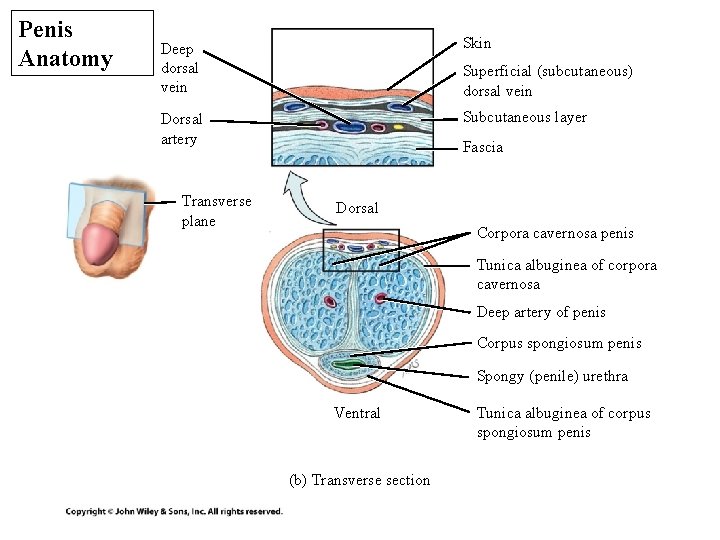
The Testes and Sperm • Testes develop inside abdominal cavity and descend into the scrotum during last two months of fetal development – – – • Scrotum helps regulate temperature of testes for proper sperm production Testes packed with seminiferous tubules with cells undergoing spermatogenesis, the process of becoming a sperm Sertoli cells- critical for proper spermatogenesis; create blood-testis barrier (prevents immune system entry); nurture spermatocytes; produce fluid for sperm transport; control release of sperm into lumen of tubules Testosterone secreted by Leydig cells (interstitial cells) in between seminiferous tubules 9
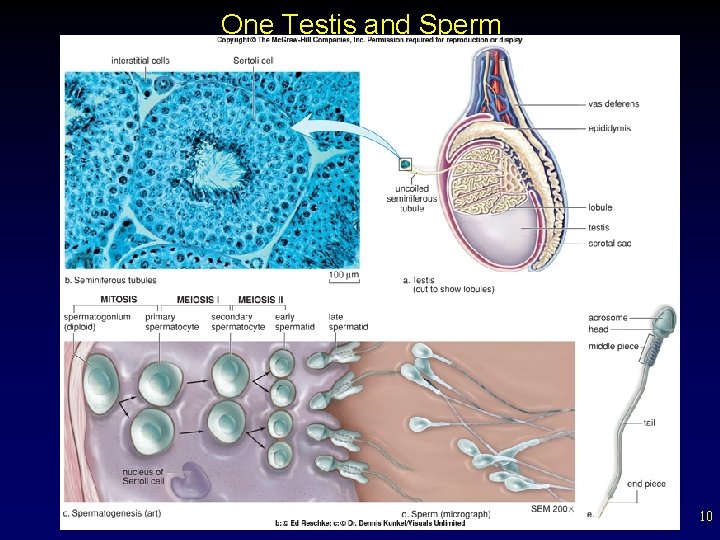
One Testis and Sperm 10
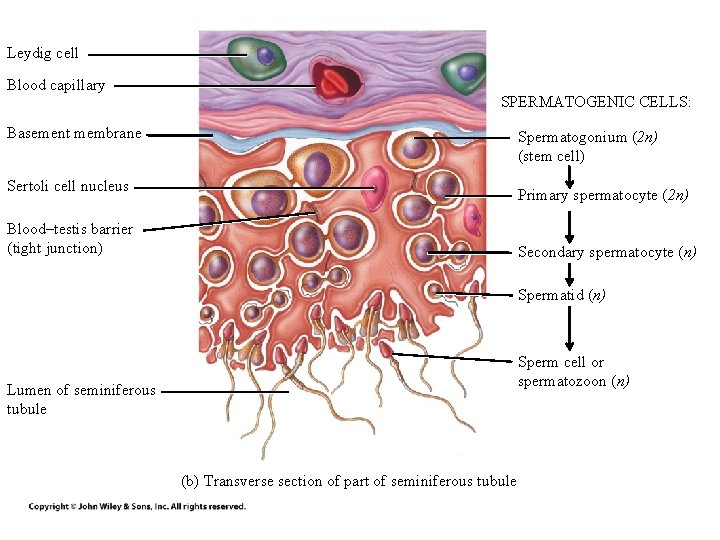
Leydig cell Blood capillary SPERMATOGENIC CELLS: Basement membrane Spermatogonium (2 n) (stem cell) Sertoli cell nucleus Primary spermatocyte (2 n) Blood–testis barrier (tight junction) Secondary spermatocyte (n) Spermatid (n) Sperm cell or spermatozoon (n) Lumen of seminiferous tubule (b) Transverse section of part of seminiferous tubule
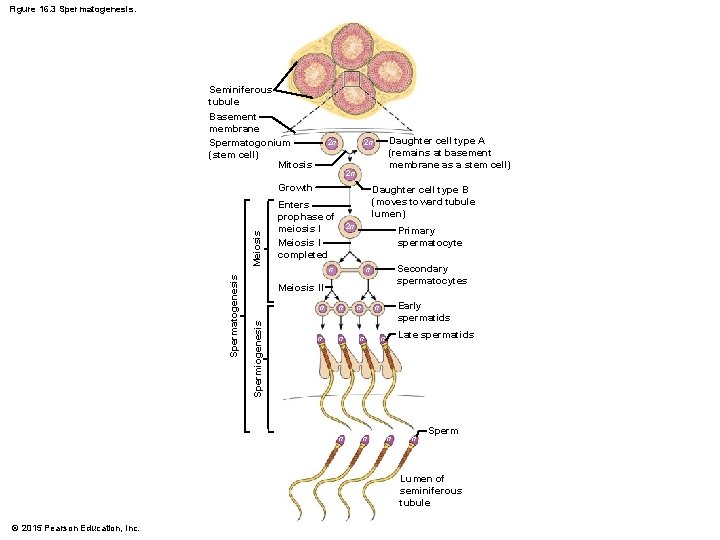
Figure 16. 3 Spermatogenesis. Seminiferous tubule Basement membrane Spermatogonium (stem cell) Mitosis 2 n 2 n Meiosis Growth Daughter cell type B (moves toward tubule lumen) Enters prophase of meiosis I Meiosis I completed 2 n Primary spermatocyte n Secondary spermatocytes n Meiosis II Spermiogenesis Spermatogenesis Daughter cell type A (remains at basement membrane as a stem cell) 2 n n n n Early spermatids n n n Late spermatids n n n Sperm Lumen of seminiferous tubule © 2015 Pearson Education, Inc.
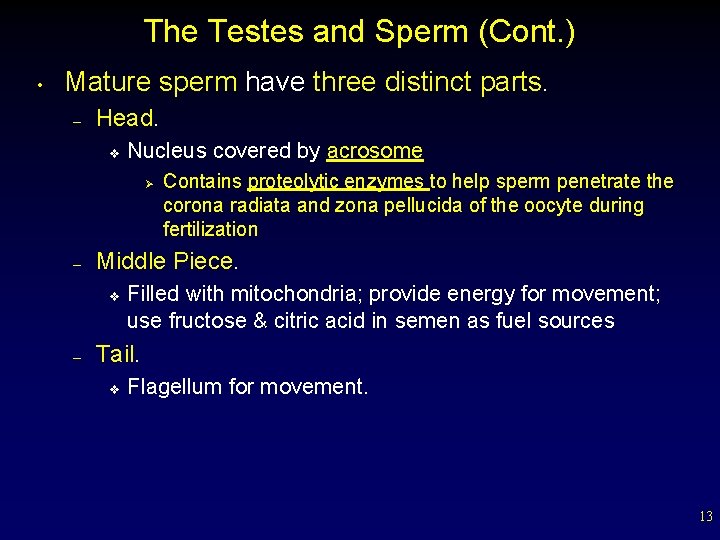
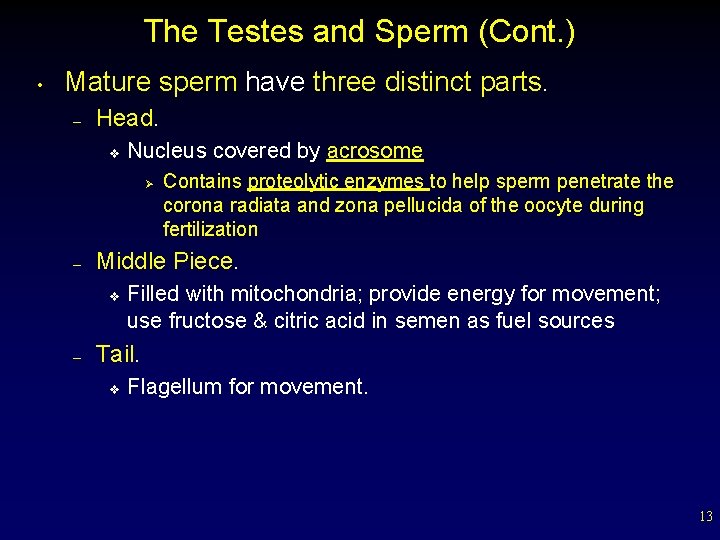
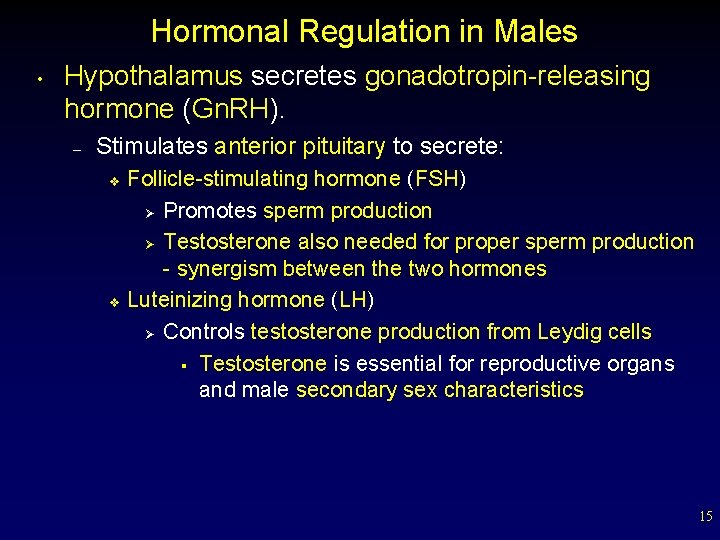
The Testes and Sperm (Cont. ) • Mature sperm have three distinct parts. – Head. v Nucleus covered by acrosome Ø – Middle Piece. v – Contains proteolytic enzymes to help sperm penetrate the corona radiata and zona pellucida of the oocyte during fertilization Filled with mitochondria; provide energy for movement; use fructose & citric acid in semen as fuel sources Tail. v Flagellum for movement. 13
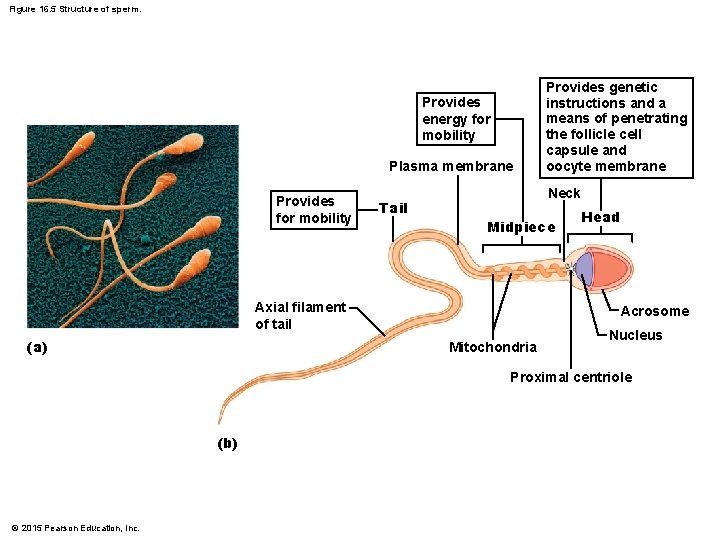
Figure 16. 5 Structure of sperm. Provides energy for mobility Plasma membrane Provides for mobility Tail Neck Midpiece Axial filament of tail (a) Provides genetic instructions and a means of penetrating the follicle cell capsule and oocyte membrane Head Acrosome Mitochondria Nucleus Proximal centriole (b) © 2015 Pearson Education, Inc.
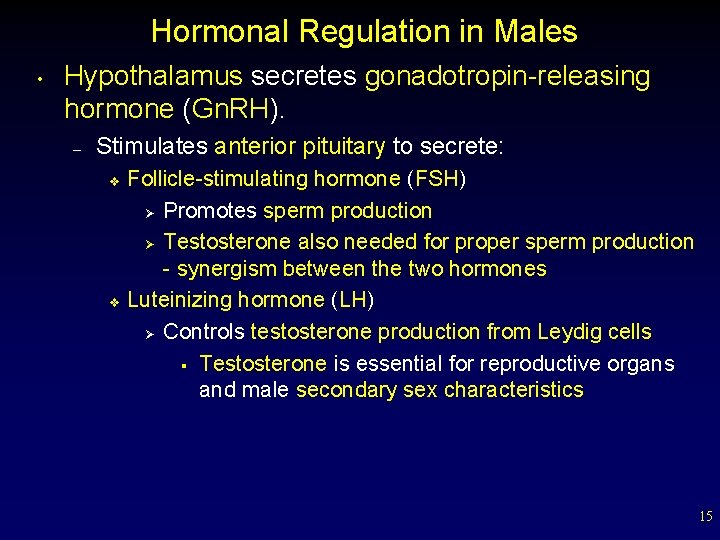
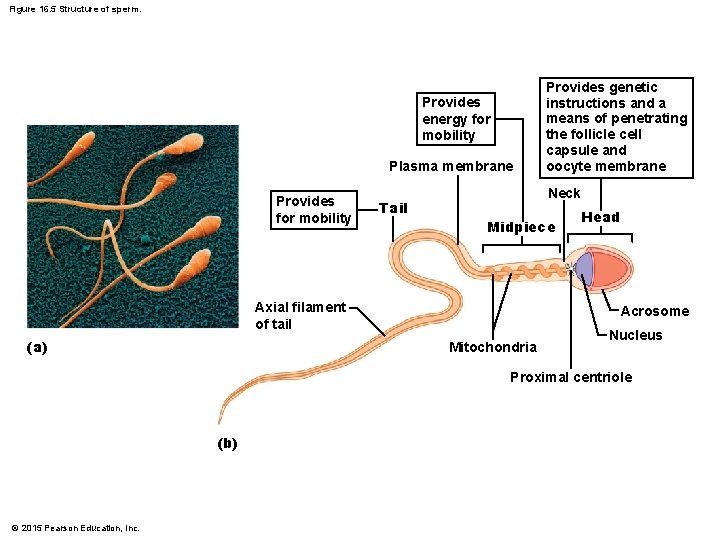
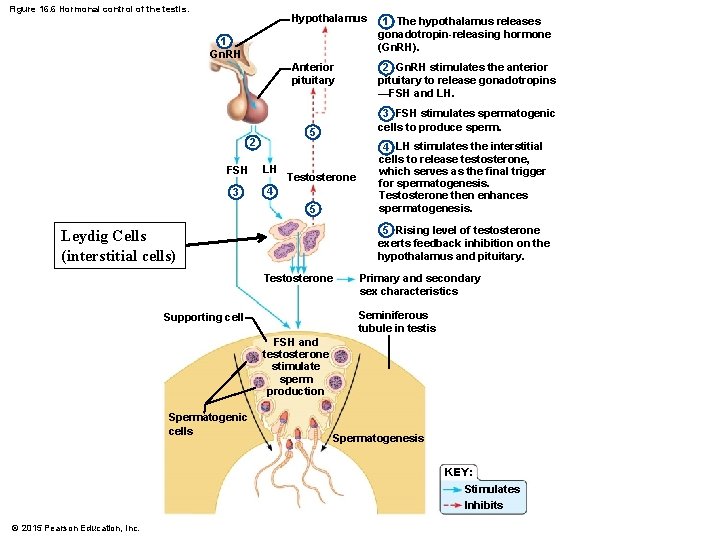
Hormonal Regulation in Males • Hypothalamus secretes gonadotropin-releasing hormone (Gn. RH). – Stimulates anterior pituitary to secrete: v v Follicle-stimulating hormone (FSH) Ø Promotes sperm production Ø Testosterone also needed for proper sperm production - synergism between the two hormones Luteinizing hormone (LH) Ø Controls testosterone production from Leydig cells § Testosterone is essential for reproductive organs and male secondary sex characteristics 15
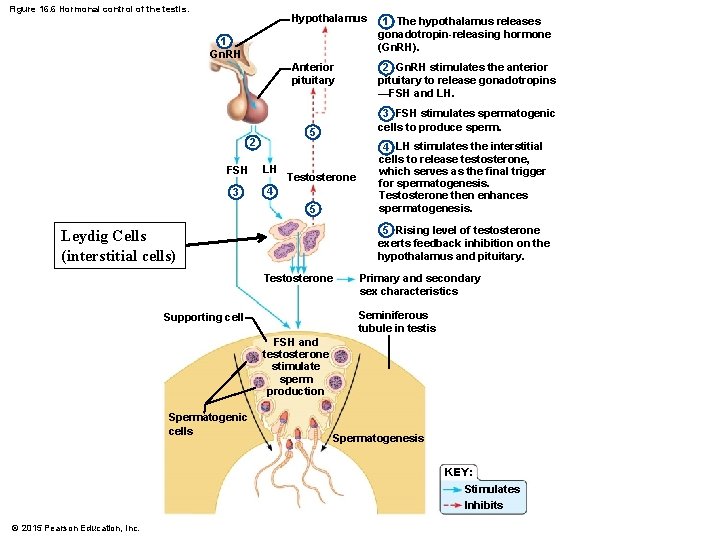
Figure 16. 6 Hormonal control of the testis. Hypothalamus 1 The hypothalamus releases gonadotropin-releasing hormone (Gn. RH). Anterior pituitary 2 Gn. RH stimulates the anterior pituitary to release gonadotropins —FSH and LH. 1 Gn. RH 3 FSH stimulates spermatogenic cells to produce sperm. 5 2 FSH LH 3 4 Testosterone 5 4 LH stimulates the interstitial cells to release testosterone, which serves as the final trigger for spermatogenesis. Testosterone then enhances spermatogenesis. 5 Rising level of testosterone exerts feedback inhibition on the hypothalamus and pituitary. Leydig Cells (interstitial cells) Testosterone Primary and secondary sex characteristics Seminiferous tubule in testis Supporting cell FSH and testosterone stimulate sperm production Spermatogenic cells Spermatogenesis KEY: Stimulates Inhibits © 2015 Pearson Education, Inc.
Female Reproductive System 17
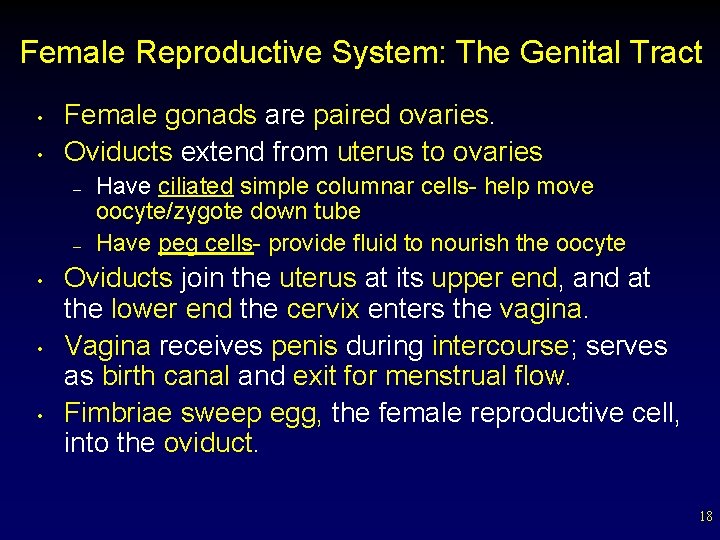
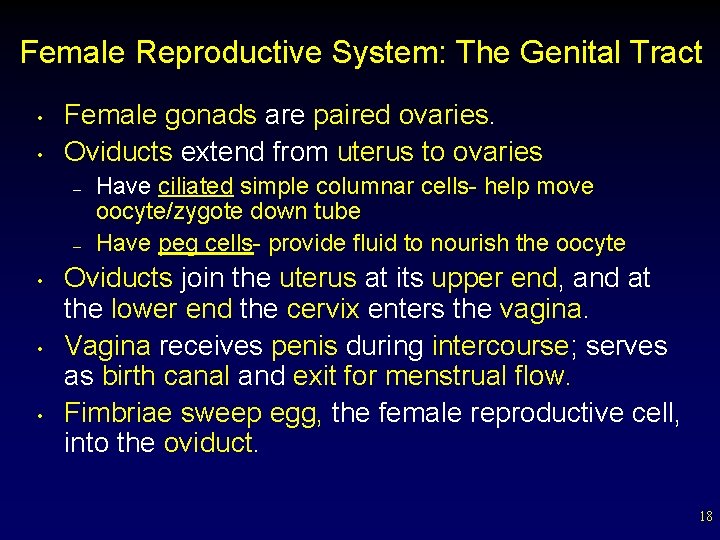
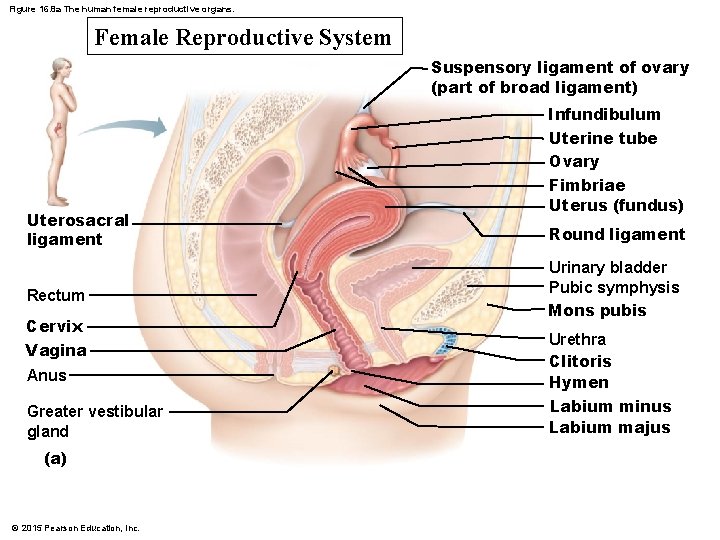
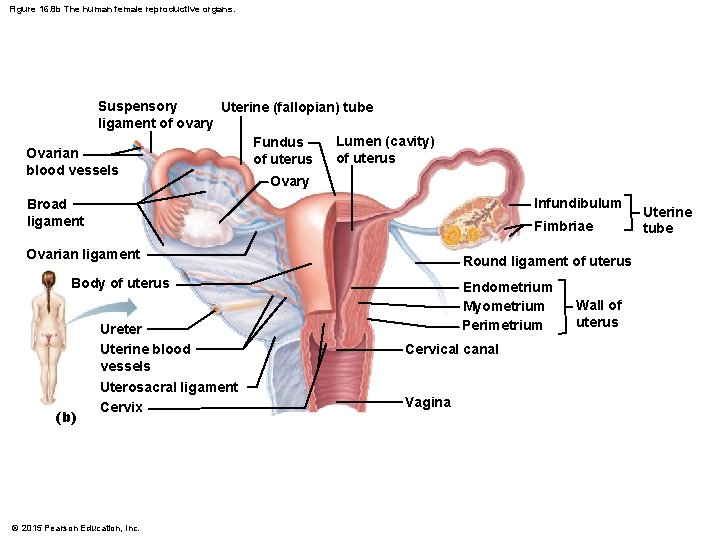
Female Reproductive System: The Genital Tract • • Female gonads are paired ovaries. Oviducts extend from uterus to ovaries – – • • • Have ciliated simple columnar cells- help move oocyte/zygote down tube Have peg cells- provide fluid to nourish the oocyte Oviducts join the uterus at its upper end, and at the lower end the cervix enters the vagina. Vagina receives penis during intercourse; serves as birth canal and exit for menstrual flow. Fimbriae sweep egg, the female reproductive cell, into the oviduct. 18
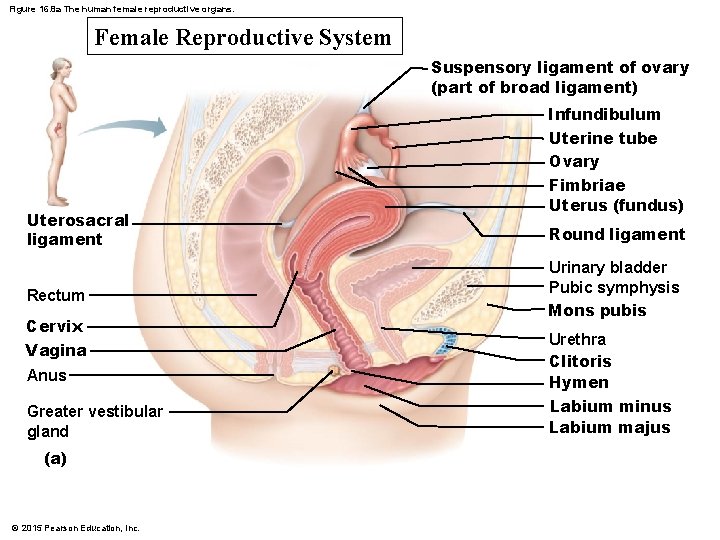
Figure 16. 8 a The human female reproductive organs. Female Reproductive System Suspensory ligament of ovary (part of broad ligament) Infundibulum Uterosacral ligament Rectum Cervix Vagina Anus Greater vestibular gland (a) © 2015 Pearson Education, Inc. Uterine tube Ovary Fimbriae Uterus (fundus) Round ligament Urinary bladder Pubic symphysis Mons pubis Urethra Clitoris Hymen Labium minus Labium majus
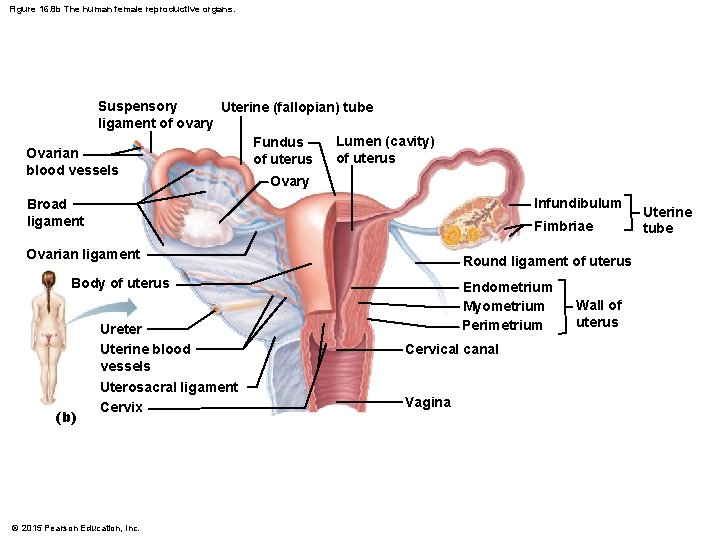
Figure 16. 8 b The human female reproductive organs. Suspensory Uterine (fallopian) tube ligament of ovary Lumen (cavity) Fundus Ovarian of uterus blood vessels Ovary Infundibulum Broad ligament Fimbriae Ovarian ligament Round ligament of uterus Body of uterus (b) Endometrium Myometrium Perimetrium Ureter Uterine blood vessels Cervical canal Uterosacral ligament Cervix Vagina © 2015 Pearson Education, Inc. Wall of uterus Uterine tube
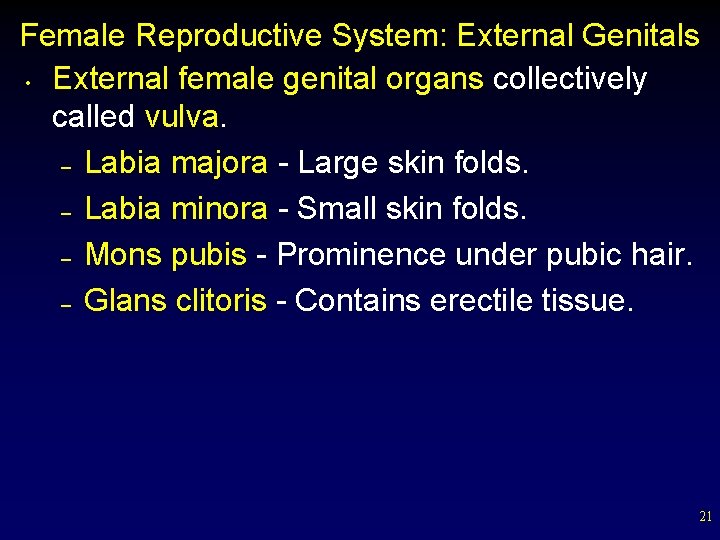
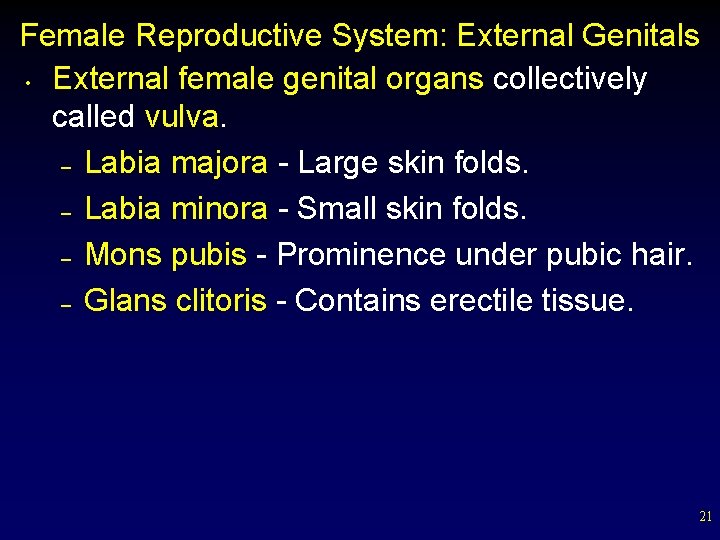
Female Reproductive System: External Genitals • External female genital organs collectively called vulva. – Labia majora - Large skin folds. – Labia minora - Small skin folds. – Mons pubis - Prominence under pubic hair. – Glans clitoris - Contains erectile tissue. 21
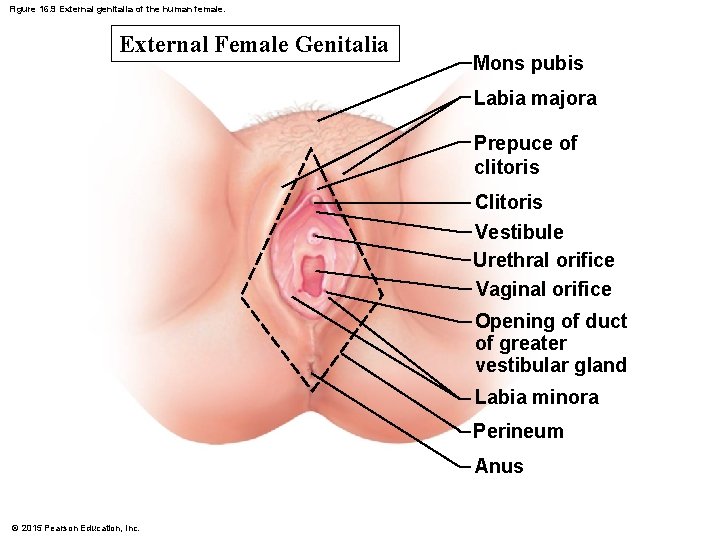
Figure 16. 9 External genitalia of the human female. External Female Genitalia Mons pubis Labia majora Prepuce of clitoris Clitoris Vestibule Urethral orifice Vaginal orifice Opening of duct of greater vestibular gland Labia minora Perineum Anus © 2015 Pearson Education, Inc.
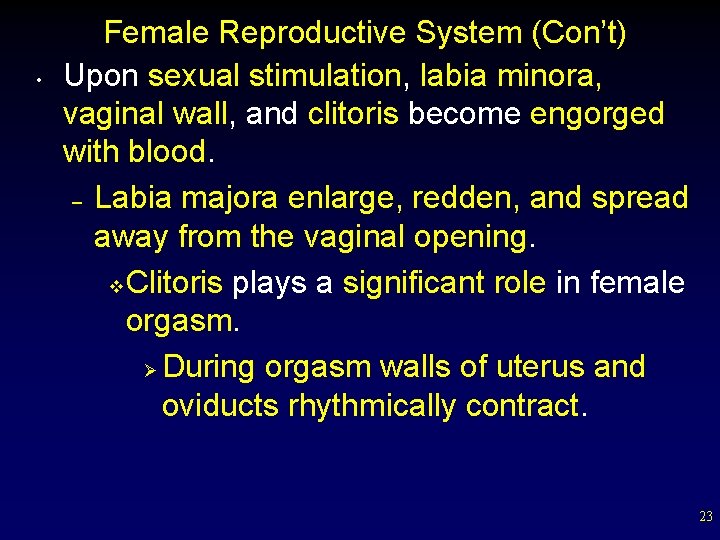
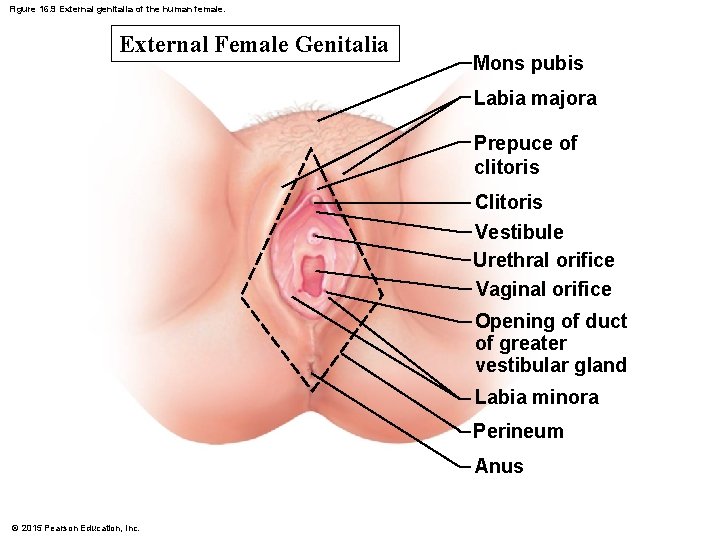
• Female Reproductive System (Con’t) Upon sexual stimulation, labia minora, vaginal wall, and clitoris become engorged with blood. – Labia majora enlarge, redden, and spread away from the vaginal opening. v Clitoris plays a significant role in female orgasm. Ø During orgasm walls of uterus and oviducts rhythmically contract. 23
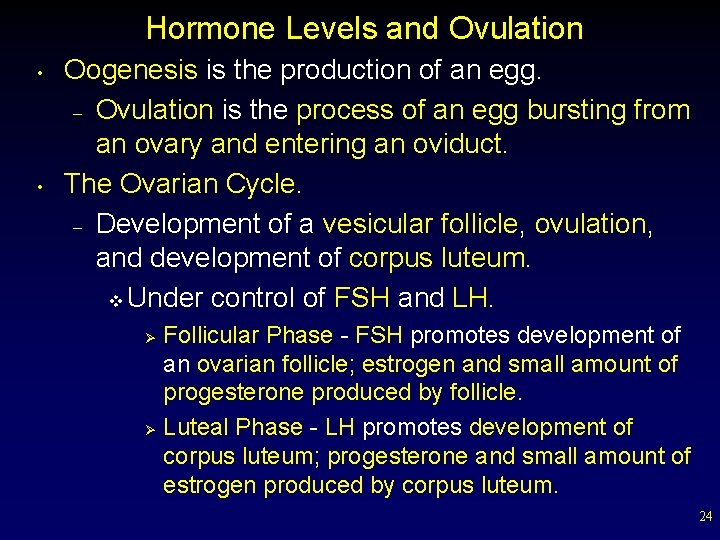
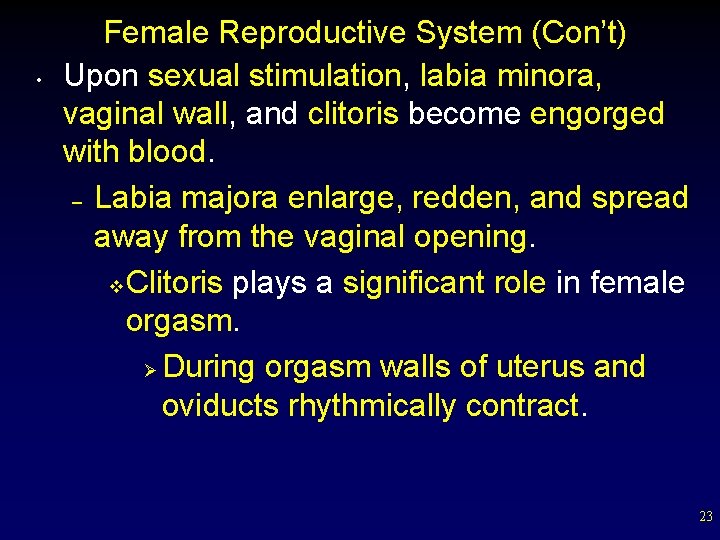
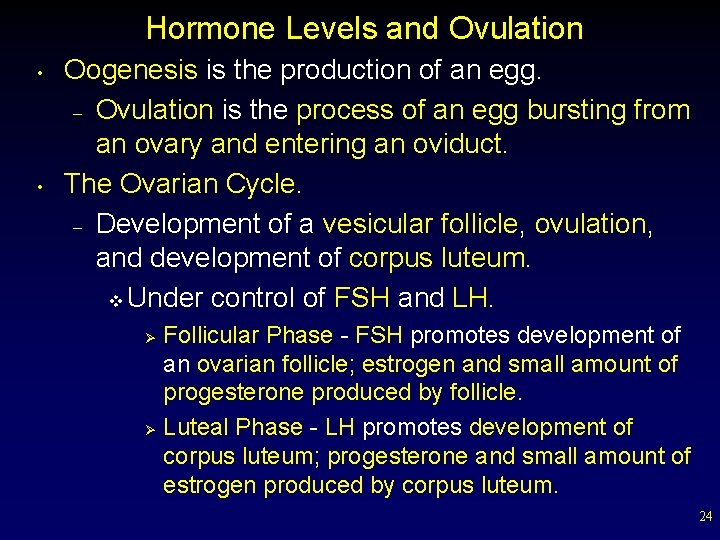
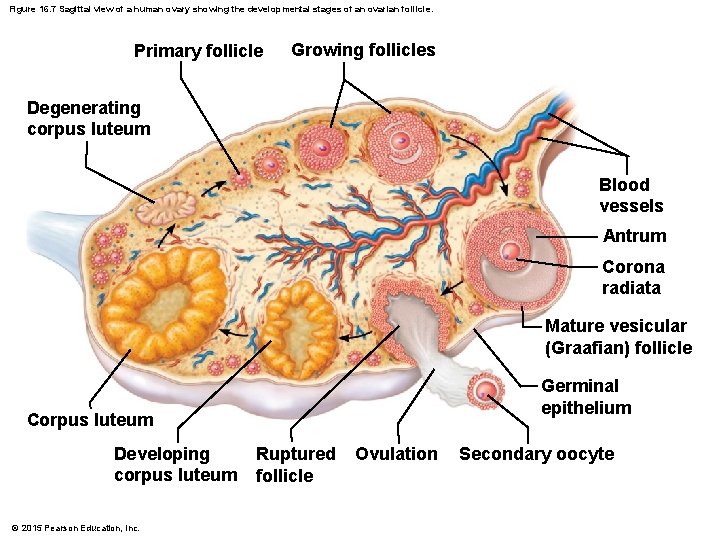
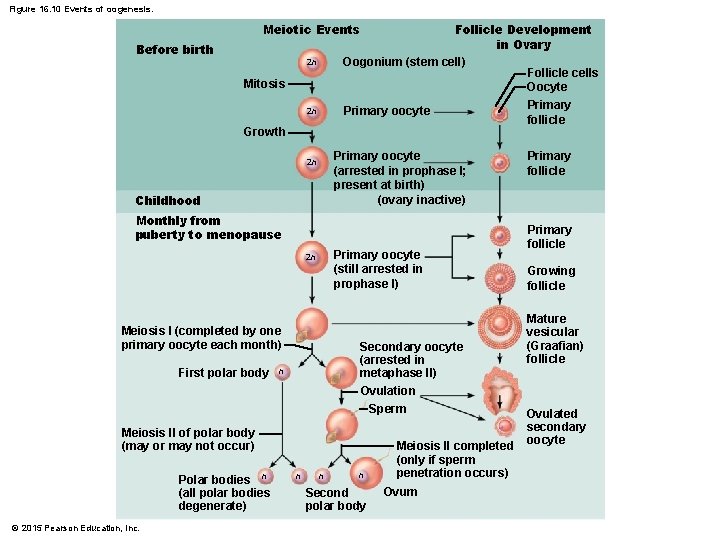
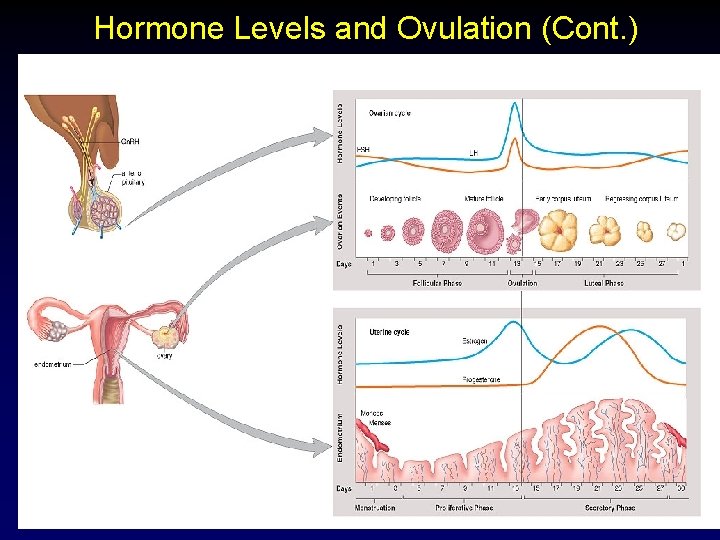
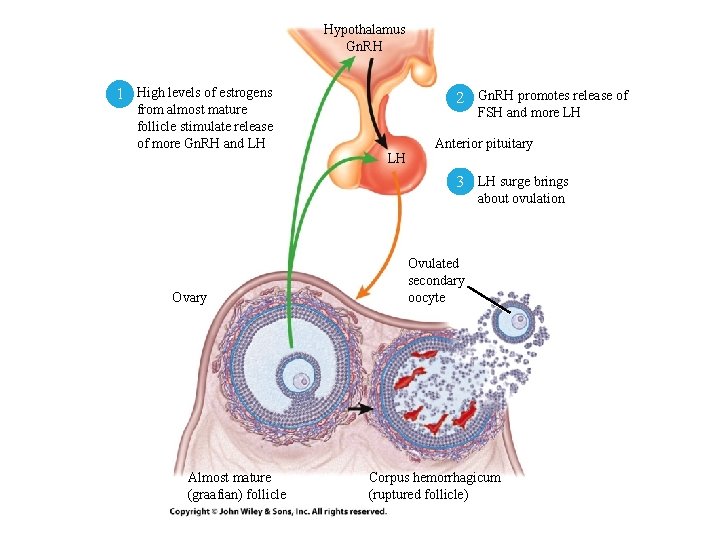
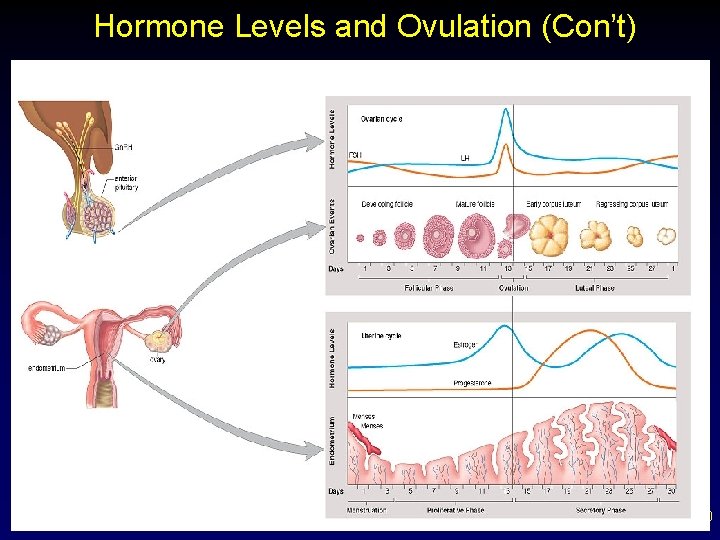
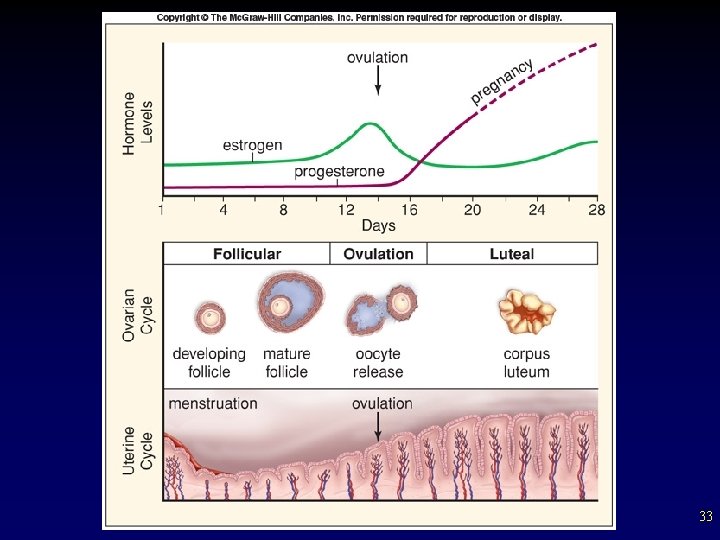
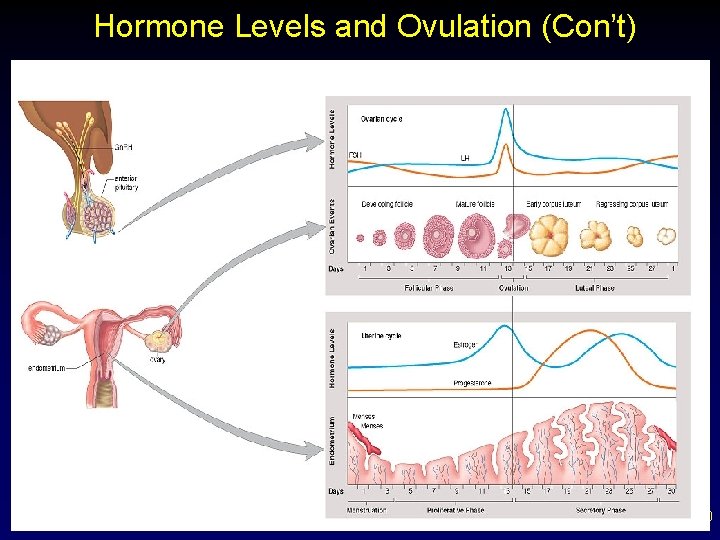
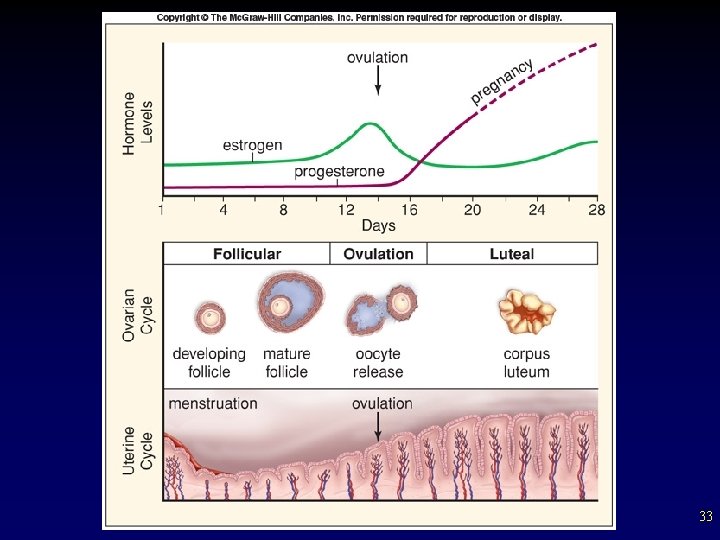
Hormone Levels and Ovulation • • Oogenesis is the production of an egg. – Ovulation is the process of an egg bursting from an ovary and entering an oviduct. The Ovarian Cycle. – Development of a vesicular follicle, ovulation, and development of corpus luteum. v Under control of FSH and LH. Follicular Phase - FSH promotes development of an ovarian follicle; estrogen and small amount of progesterone produced by follicle. Ø Luteal Phase - LH promotes development of corpus luteum; progesterone and small amount of estrogen produced by corpus luteum. Ø 24
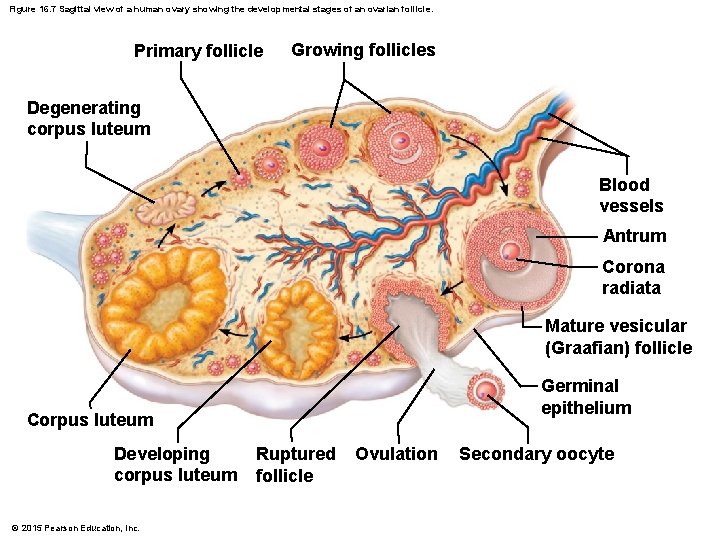
Figure 16. 7 Sagittal view of a human ovary showing the developmental stages of an ovarian follicle. Primary follicle Growing follicles Degenerating corpus luteum Blood vessels Antrum Corona radiata Mature vesicular (Graafian) follicle Germinal epithelium Corpus luteum Developing corpus luteum © 2015 Pearson Education, Inc. Ruptured follicle Ovulation Secondary oocyte
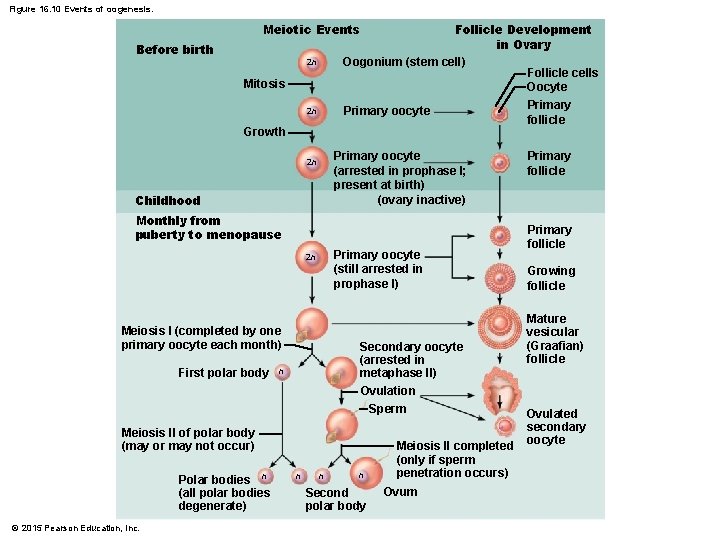
Figure 16. 10 Events of oogenesis. Follicle Development in Ovary Oogonium (stem cell) Follicle cells Oocyte Primary oocyte follicle Meiotic Events Before birth 2 n Mitosis 2 n Growth Primary oocyte (arrested in prophase I; present at birth) (ovary inactive) 2 n Childhood Monthly from puberty to menopause Primary oocyte (still arrested in prophase I) 2 n Meiosis I (completed by one primary oocyte each month) First polar body Secondary oocyte (arrested in metaphase II) Ovulation n Sperm Meiosis II of polar body (may or may not occur) Polar bodies n (all polar bodies degenerate) © 2015 Pearson Education, Inc. n n n Second polar body Meiosis II completed (only if sperm penetration occurs) Ovum Primary follicle Growing follicle Mature vesicular (Graafian) follicle Ovulated secondary oocyte
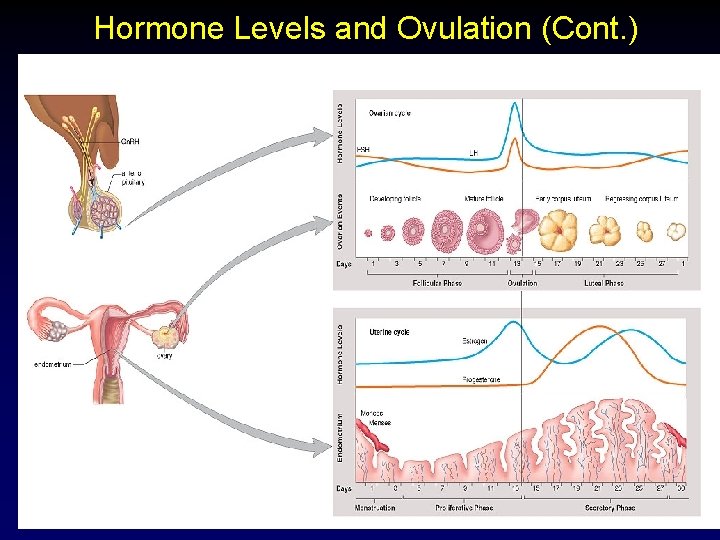
Hormone Levels and Ovulation (Cont. ) 27
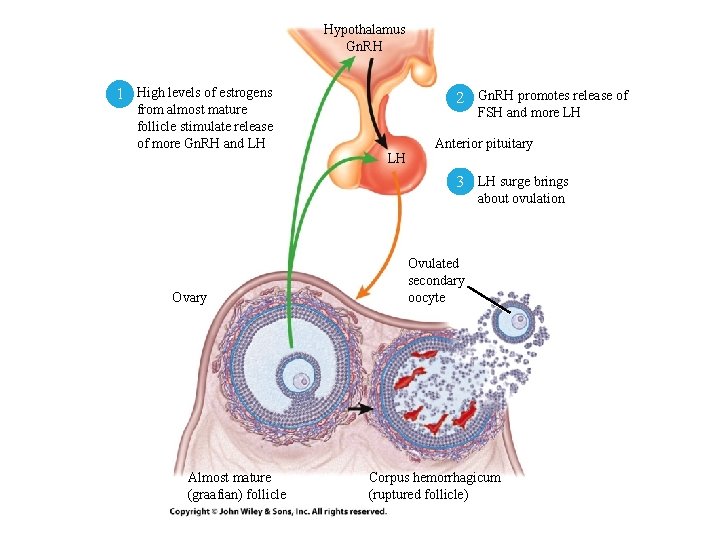
Hypothalamus Gn. RH 1 High levels of estrogens 2 Gn. RH promotes release of from almost mature follicle stimulate release of more Gn. RH and LH FSH and more LH LH Anterior pituitary 3 LH surge brings about ovulation Ovary Almost mature (graafian) follicle Ovulated secondary oocyte Corpus hemorrhagicum (ruptured follicle)
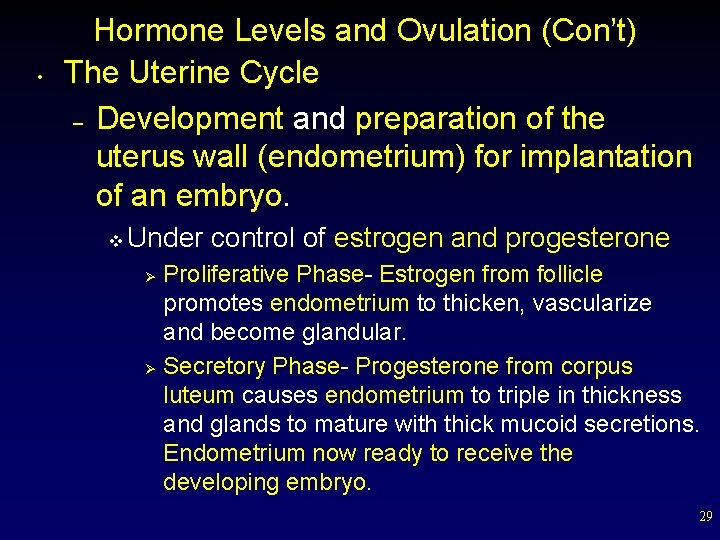
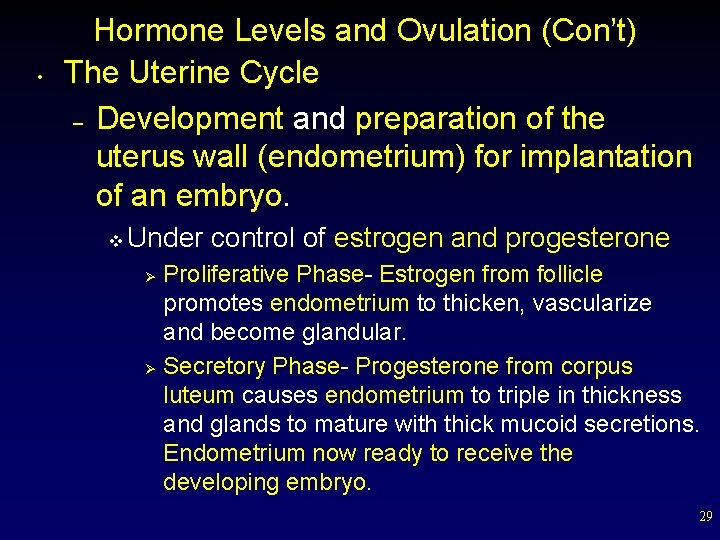
• Hormone Levels and Ovulation (Con’t) The Uterine Cycle – Development and preparation of the uterus wall (endometrium) for implantation of an embryo. v Under control of estrogen and progesterone Proliferative Phase- Estrogen from follicle promotes endometrium to thicken, vascularize and become glandular. Ø Secretory Phase- Progesterone from corpus luteum causes endometrium to triple in thickness and glands to mature with thick mucoid secretions. Endometrium now ready to receive the developing embryo. Ø 29
Hormone Levels and Ovulation (Con’t) 30
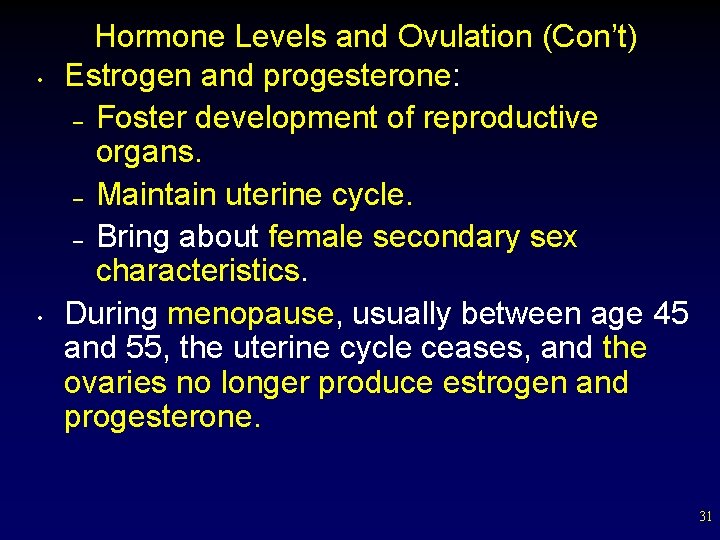
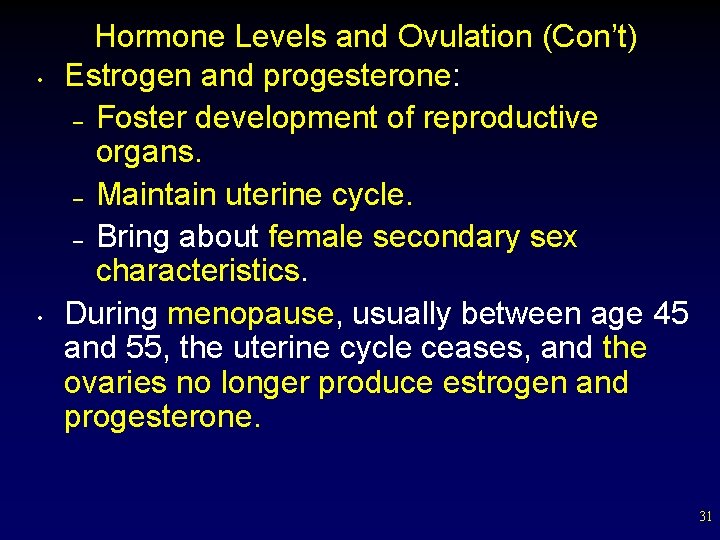
• • Hormone Levels and Ovulation (Con’t) Estrogen and progesterone: – Foster development of reproductive organs. – Maintain uterine cycle. – Bring about female secondary sex characteristics. During menopause, usually between age 45 and 55, the uterine cycle ceases, and the ovaries no longer produce estrogen and progesterone. 31
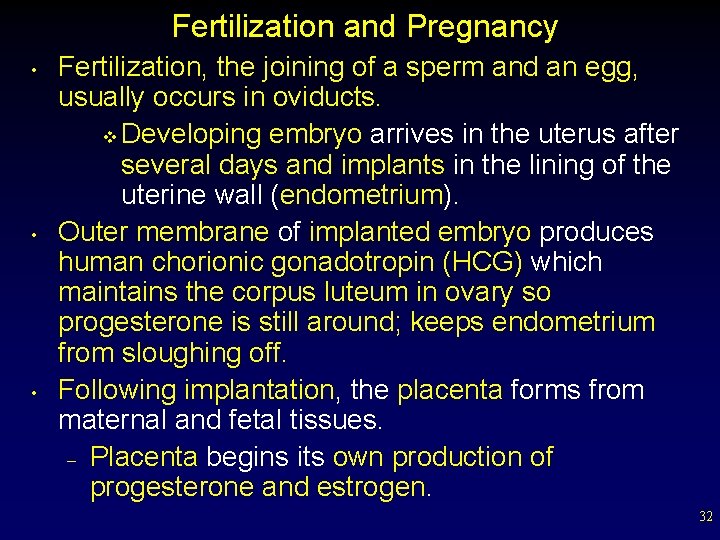
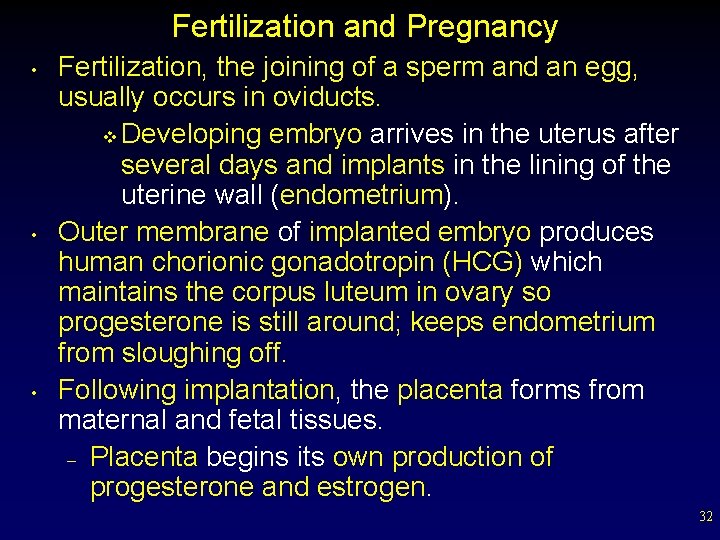
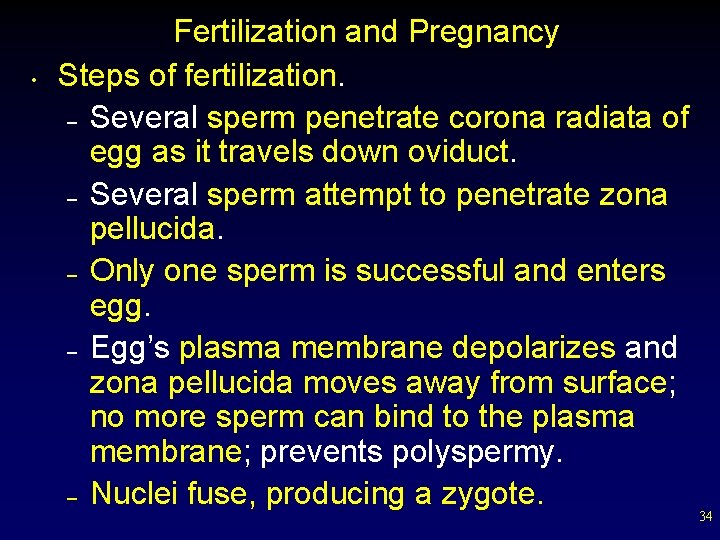
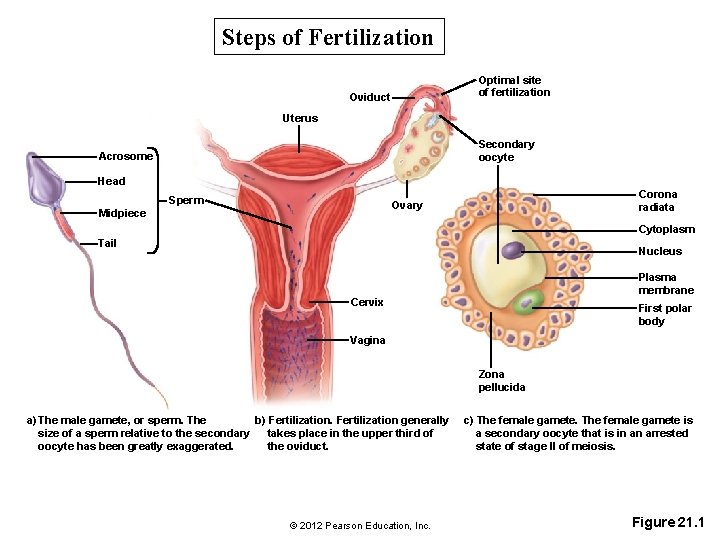
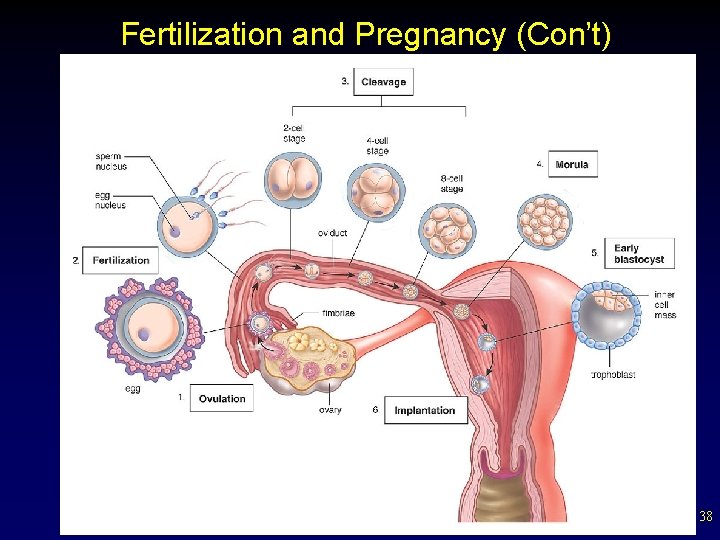
Fertilization and Pregnancy • • • Fertilization, the joining of a sperm and an egg, usually occurs in oviducts. v Developing embryo arrives in the uterus after several days and implants in the lining of the uterine wall (endometrium). Outer membrane of implanted embryo produces human chorionic gonadotropin (HCG) which maintains the corpus luteum in ovary so progesterone is still around; keeps endometrium from sloughing off. Following implantation, the placenta forms from maternal and fetal tissues. – Placenta begins its own production of progesterone and estrogen. 32
33
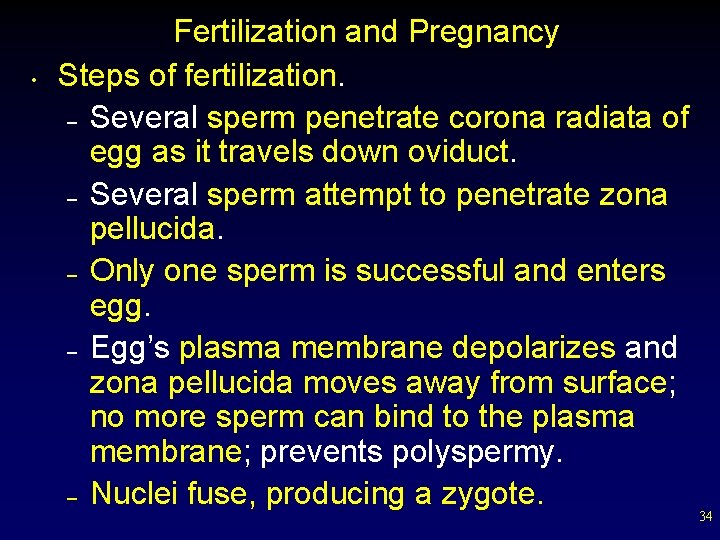
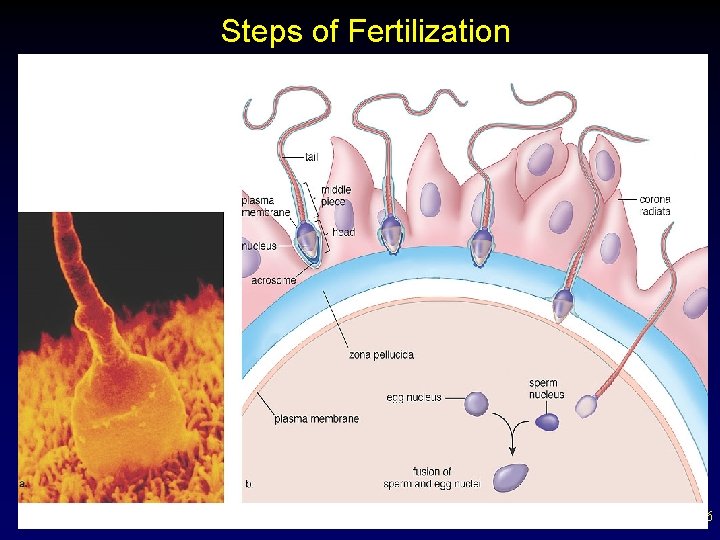
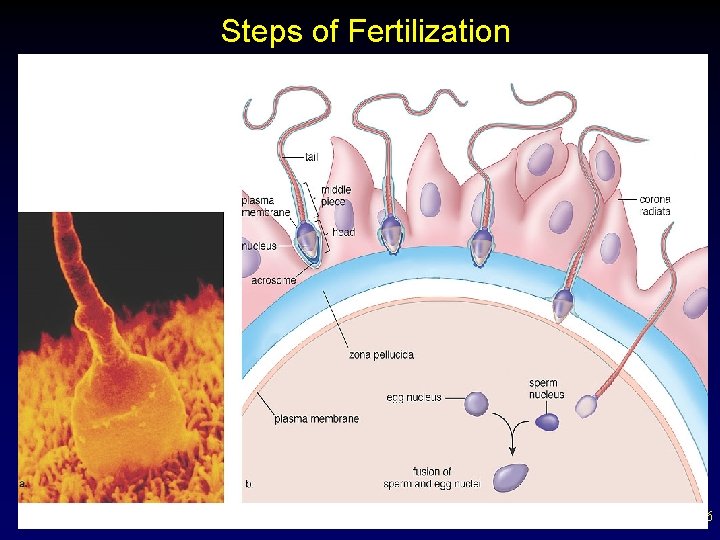
• Fertilization and Pregnancy Steps of fertilization. – Several sperm penetrate corona radiata of egg as it travels down oviduct. – Several sperm attempt to penetrate zona pellucida. – Only one sperm is successful and enters egg. – Egg’s plasma membrane depolarizes and zona pellucida moves away from surface; no more sperm can bind to the plasma membrane; prevents polyspermy. – Nuclei fuse, producing a zygote. 34
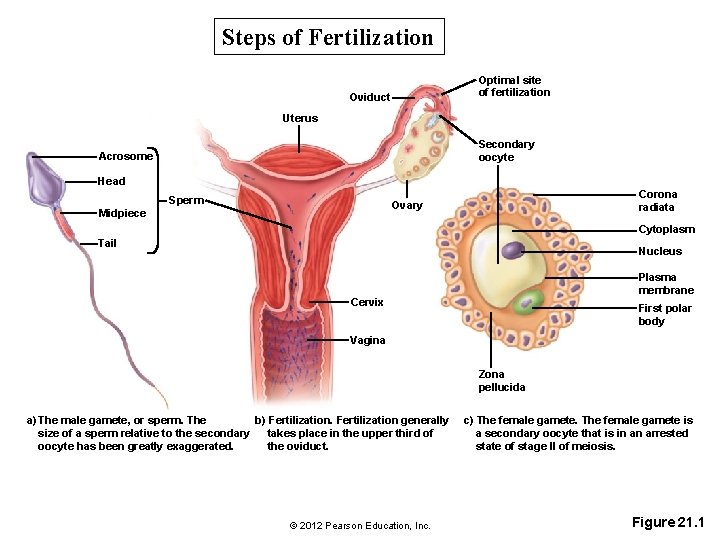
Steps of Fertilization Optimal site of fertilization Oviduct Uterus Secondary oocyte Acrosome Head Sperm Corona radiata Ovary Midpiece Cytoplasm Tail Nucleus Plasma membrane Cervix First polar body Vagina Zona pellucida a) The male gamete, or sperm. The b) Fertilization generally size of a sperm relative to the secondary takes place in the upper third of oocyte has been greatly exaggerated. the oviduct. © 2012 Pearson Education, Inc. c) The female gamete is a secondary oocyte that is in an arrested state of stage II of meiosis. Figure 21. 1
Steps of Fertilization 36
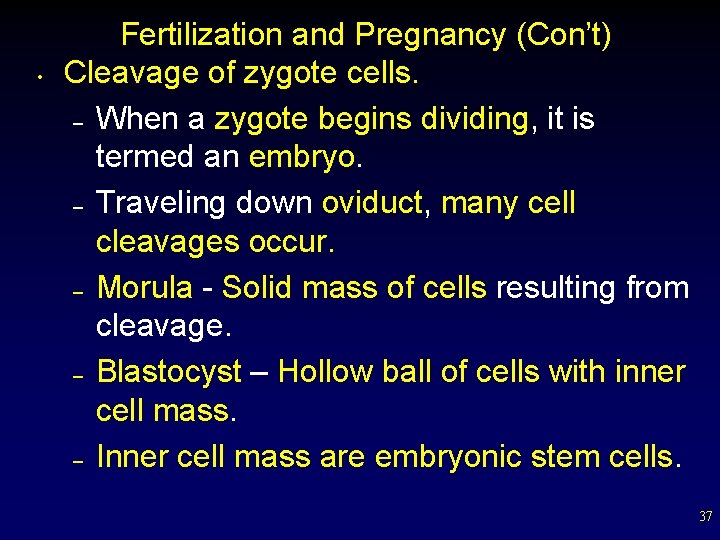
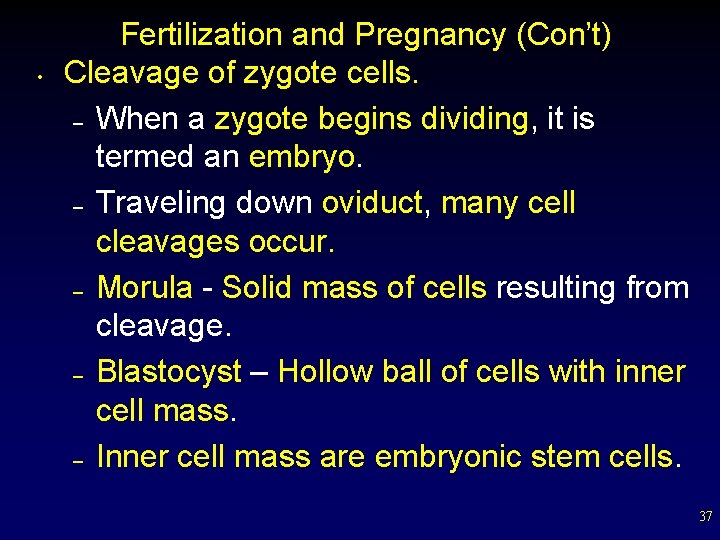
• Fertilization and Pregnancy (Con’t) Cleavage of zygote cells. – When a zygote begins dividing, it is termed an embryo. – Traveling down oviduct, many cell cleavages occur. – Morula - Solid mass of cells resulting from cleavage. – Blastocyst – Hollow ball of cells with inner cell mass. – Inner cell mass are embryonic stem cells. 37
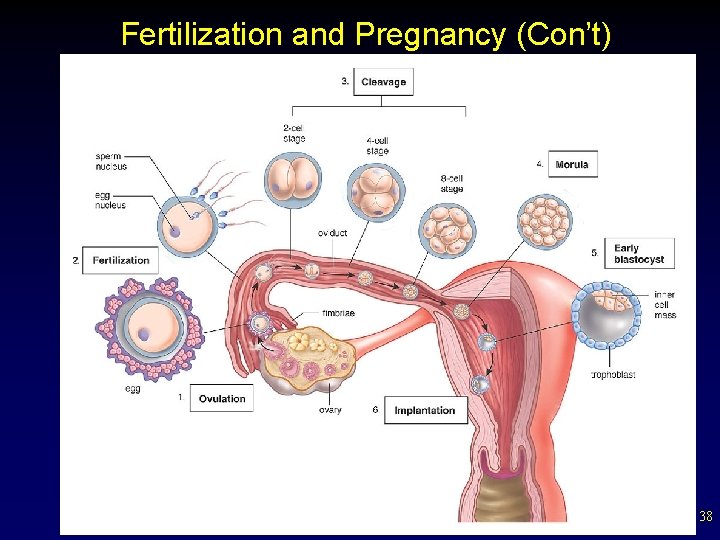
Fertilization and Pregnancy (Con’t) 38
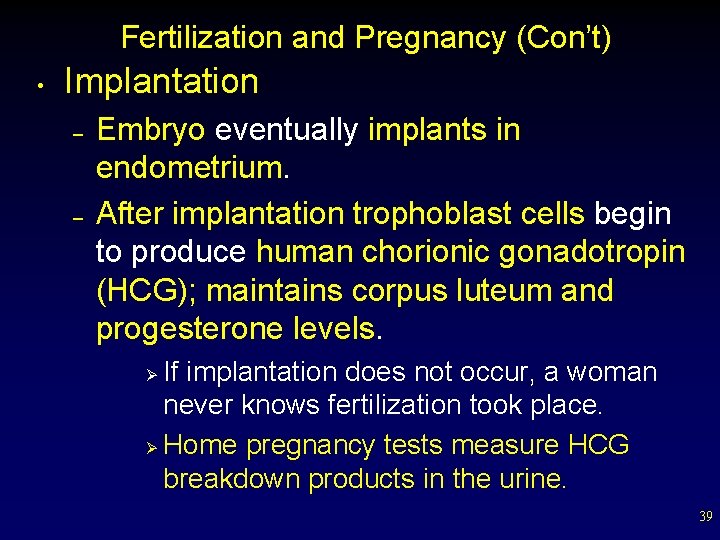
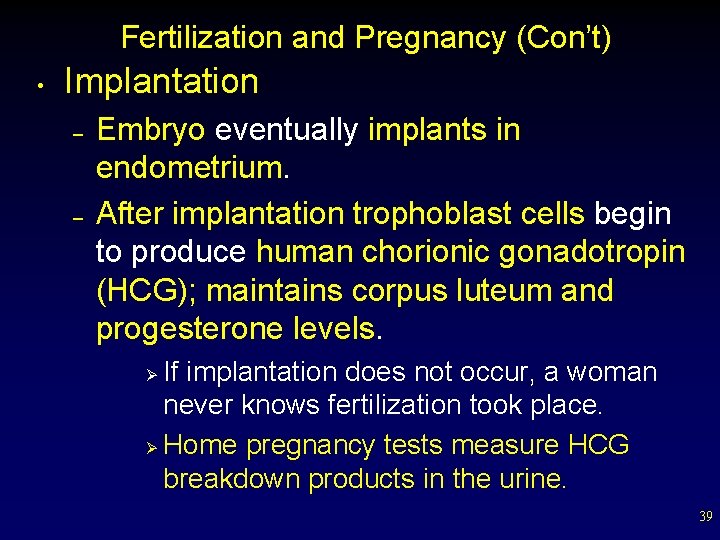
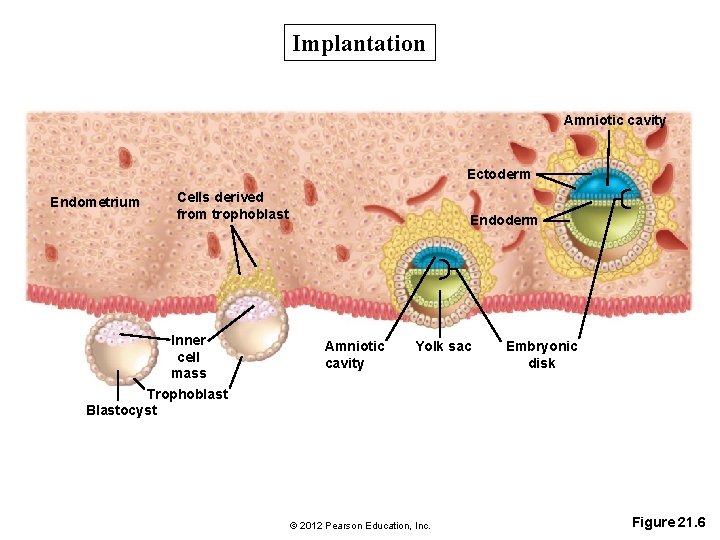
Fertilization and Pregnancy (Con’t) • Implantation – – Embryo eventually implants in endometrium. After implantation trophoblast cells begin to produce human chorionic gonadotropin (HCG); maintains corpus luteum and progesterone levels. If implantation does not occur, a woman never knows fertilization took place. Ø Home pregnancy tests measure HCG breakdown products in the urine. Ø 39
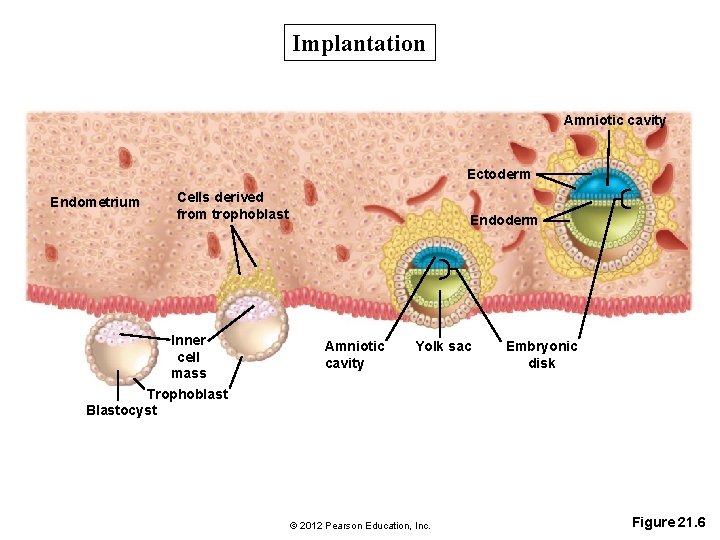
Implantation Amniotic cavity Ectoderm Endometrium Cells derived from trophoblast Inner cell mass Trophoblast Blastocyst Endoderm Amniotic cavity Yolk sac © 2012 Pearson Education, Inc. Embryonic disk Figure 21. 6
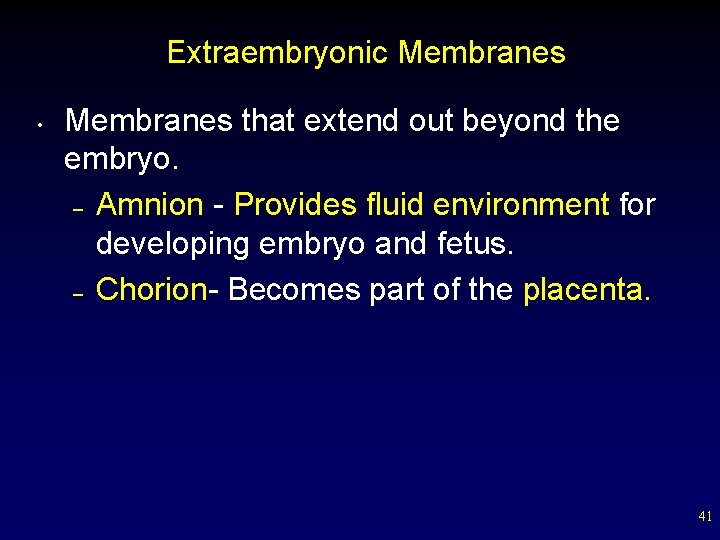
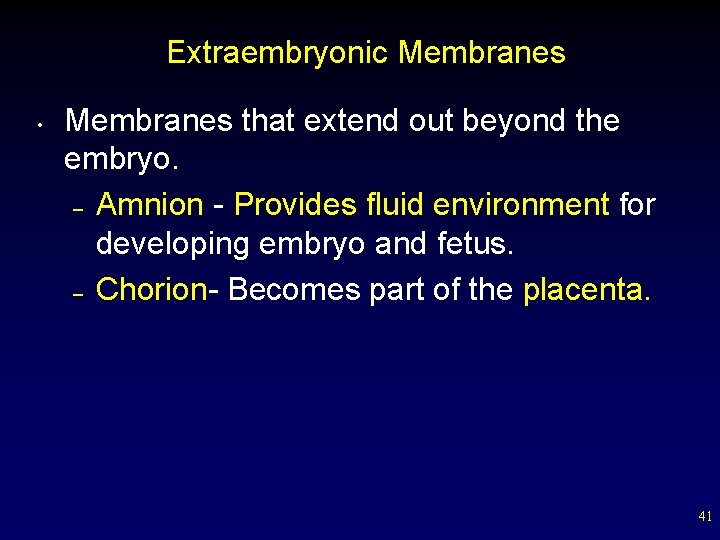
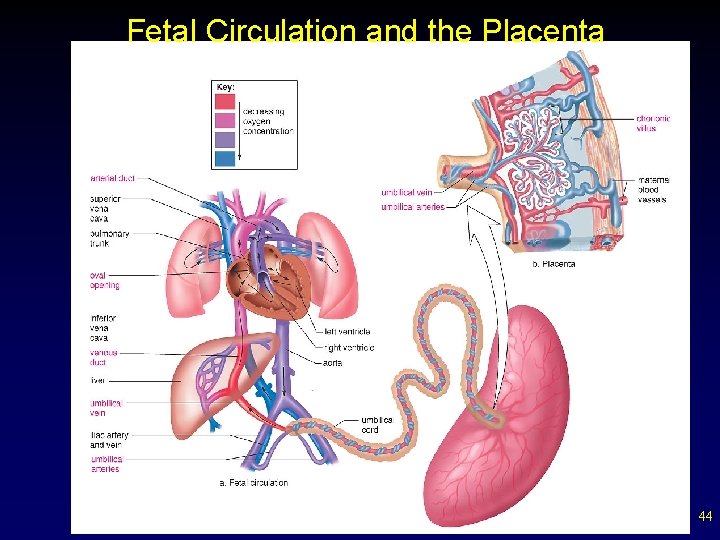
Extraembryonic Membranes • Membranes that extend out beyond the embryo. – Amnion - Provides fluid environment for developing embryo and fetus. – Chorion- Becomes part of the placenta. 41
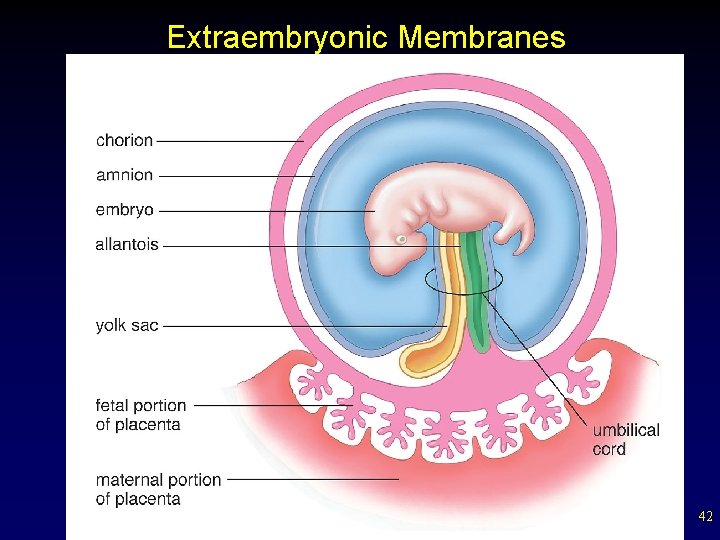
Extraembryonic Membranes 42
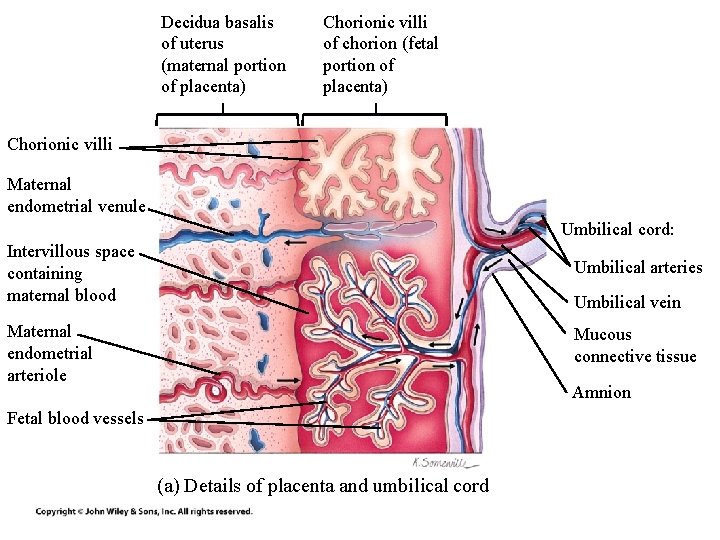
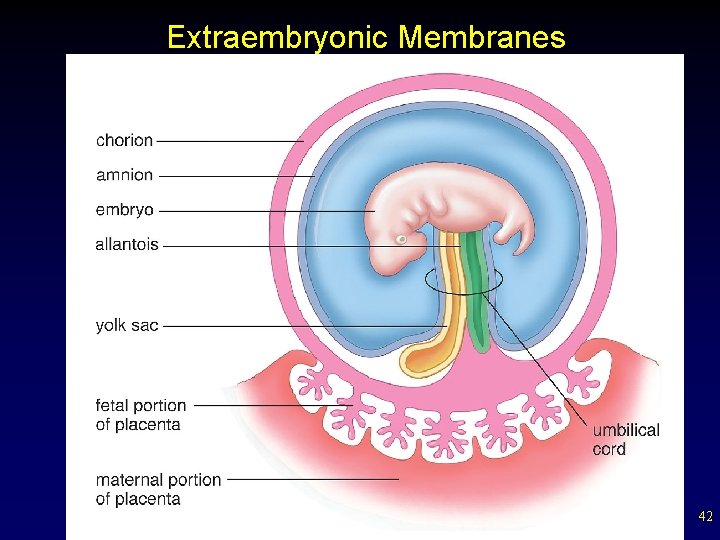
Decidua basalis of uterus (maternal portion of placenta) Chorionic villi of chorion (fetal portion of placenta) Chorionic villi Maternal endometrial venule Umbilical cord: Intervillous space containing maternal blood Umbilical arteries Maternal endometrial arteriole Mucous connective tissue Umbilical vein Amnion Fetal blood vessels (a) Details of placenta and umbilical cord
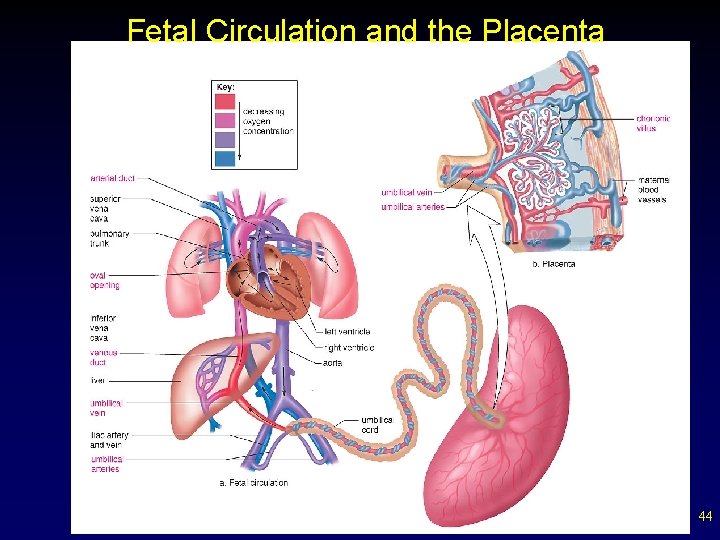
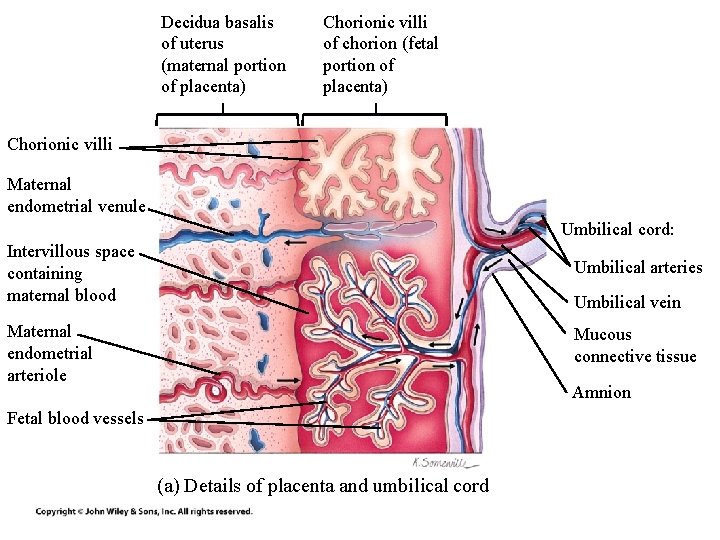
Fetal Circulation and the Placenta 44
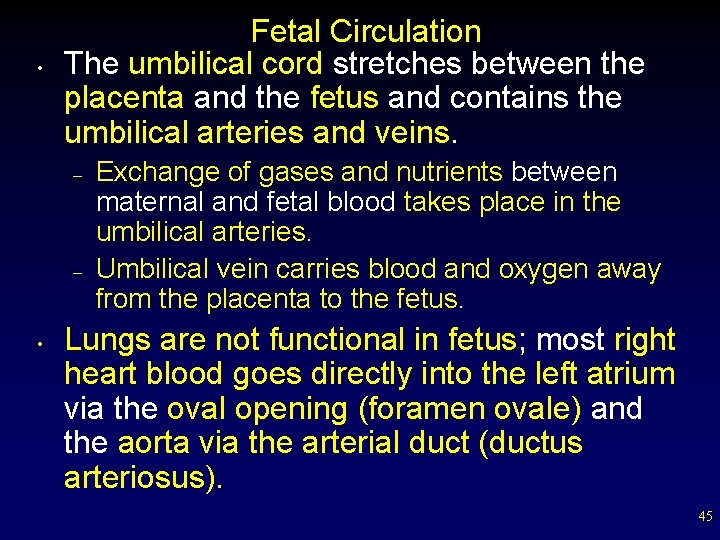
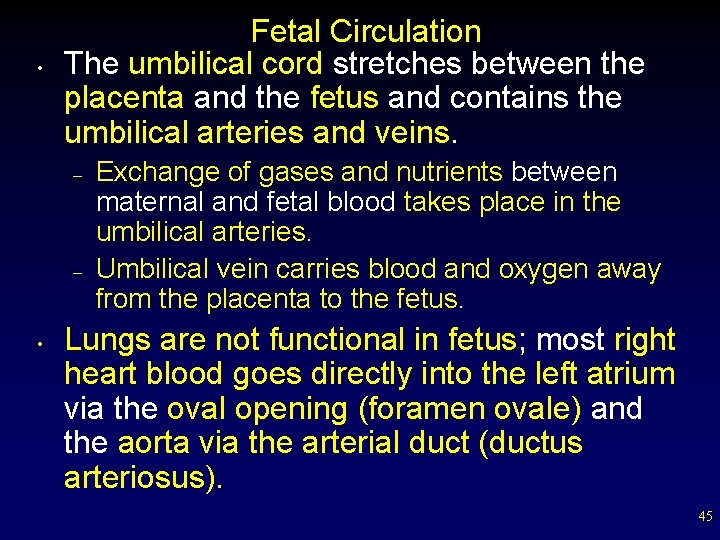
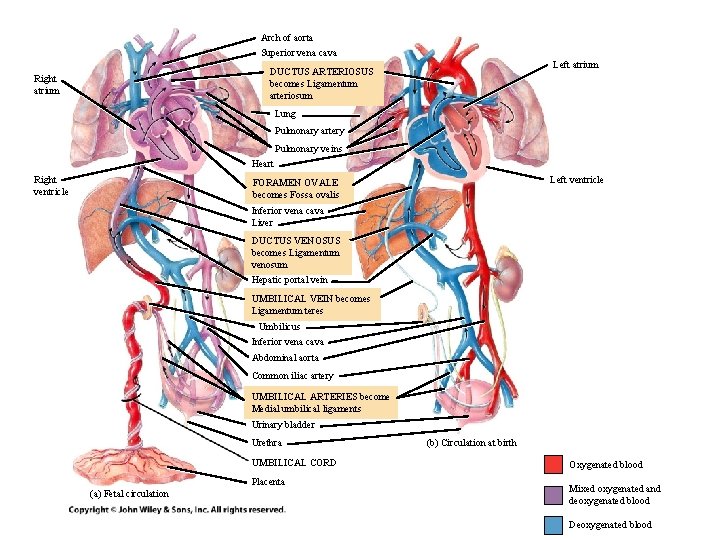
• Fetal Circulation The umbilical cord stretches between the placenta and the fetus and contains the umbilical arteries and veins. – – • Exchange of gases and nutrients between maternal and fetal blood takes place in the umbilical arteries. Umbilical vein carries blood and oxygen away from the placenta to the fetus. Lungs are not functional in fetus; most right heart blood goes directly into the left atrium via the oval opening (foramen ovale) and the aorta via the arterial duct (ductus arteriosus). 45
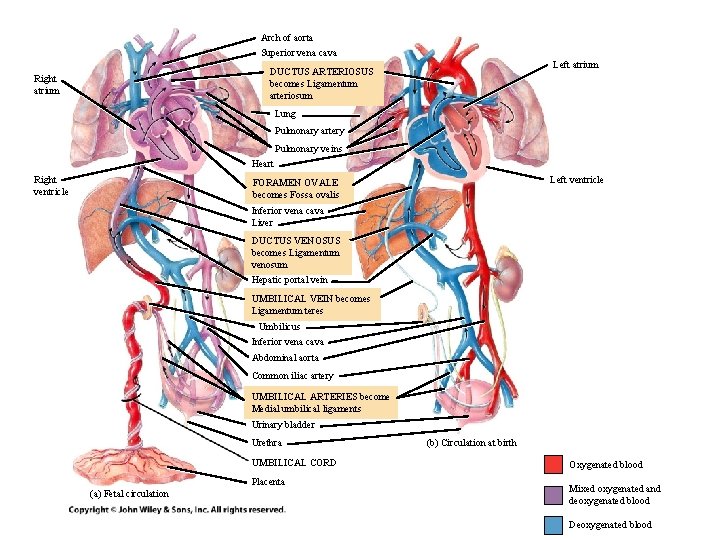
Arch of aorta Superior vena cava Left atrium DUCTUS ARTERIOSUS becomes Ligamentum arteriosum Right atrium Lung Pulmonary artery Pulmonary veins Heart Right ventricle Left ventricle FORAMEN OVALE becomes Fossa ovalis Inferior vena cava Liver DUCTUS VENOSUS becomes Ligamentum venosum Hepatic portal vein UMBILICAL VEIN becomes Ligamentum teres Umbilicus Inferior vena cava Abdominal aorta Common iliac artery UMBILICAL ARTERIES become Medial umbilical ligaments Urinary bladder Urethra UMBILICAL CORD Placenta (a) Fetal circulation (b) Circulation at birth Oxygenated blood Mixed oxygenated and deoxygenated blood Deoxygenated blood
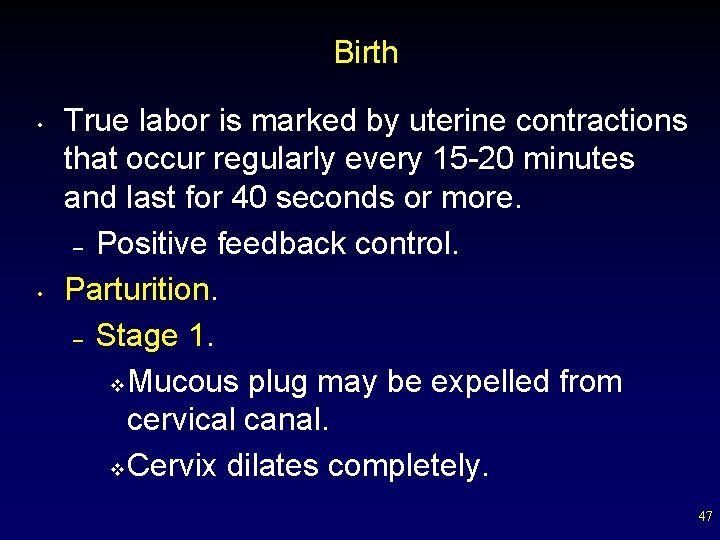
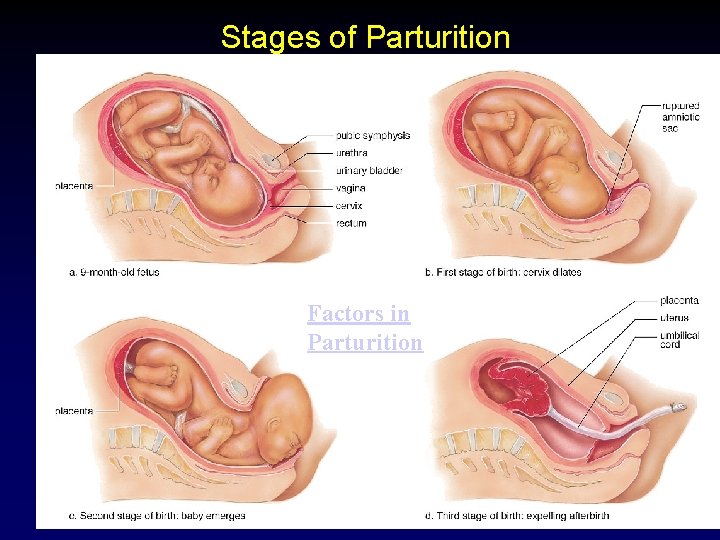
Birth • • True labor is marked by uterine contractions that occur regularly every 15 -20 minutes and last for 40 seconds or more. – Positive feedback control. Parturition. – Stage 1. v Mucous plug may be expelled from cervical canal. v Cervix dilates completely. 47
Birth – – Stage 2. v Baby’s head descends into the vagina. v Baby is delivered. Stage 3. v Placenta delivered. 48
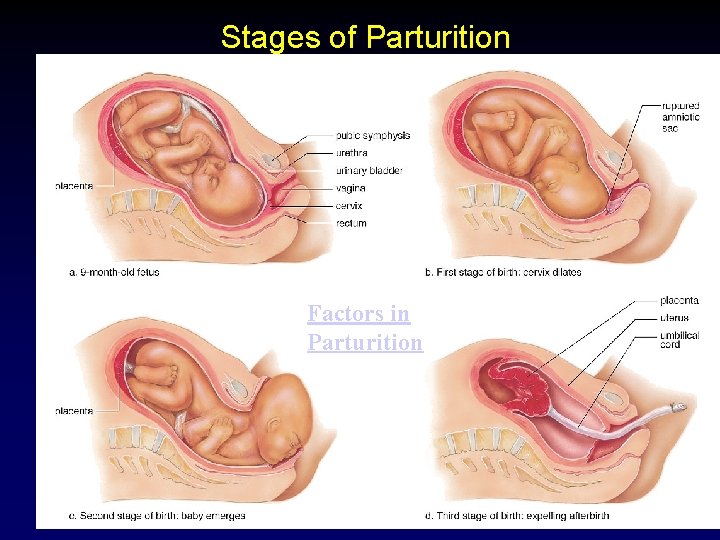
Stages of Parturition Factors in Parturition 49
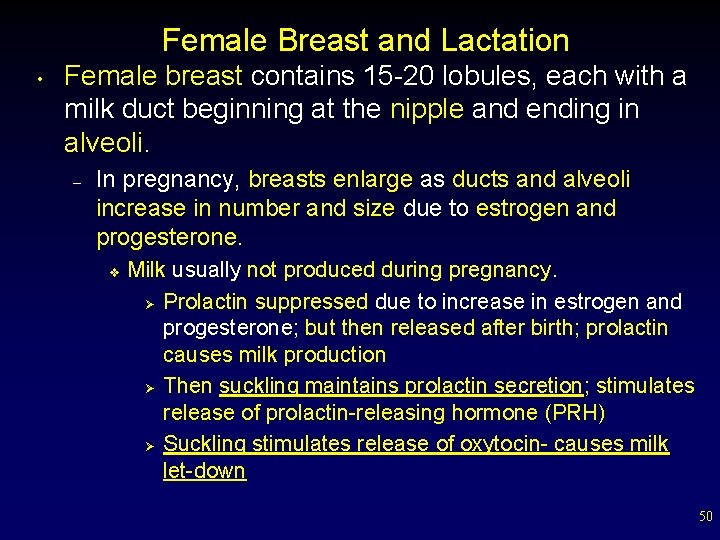
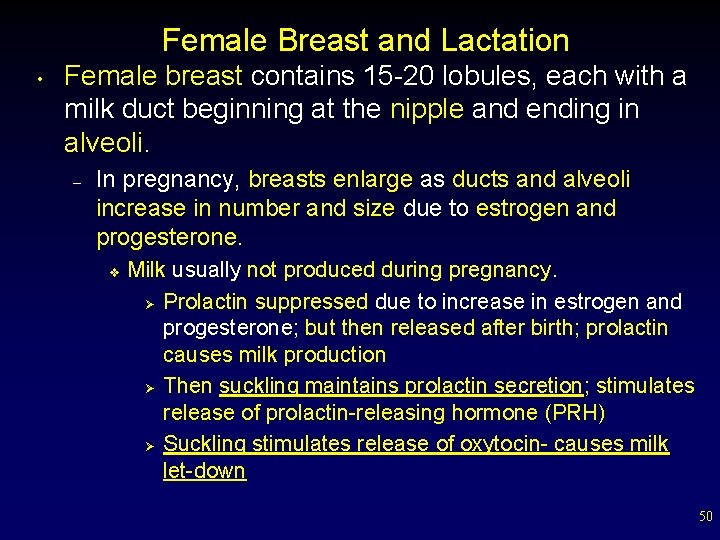
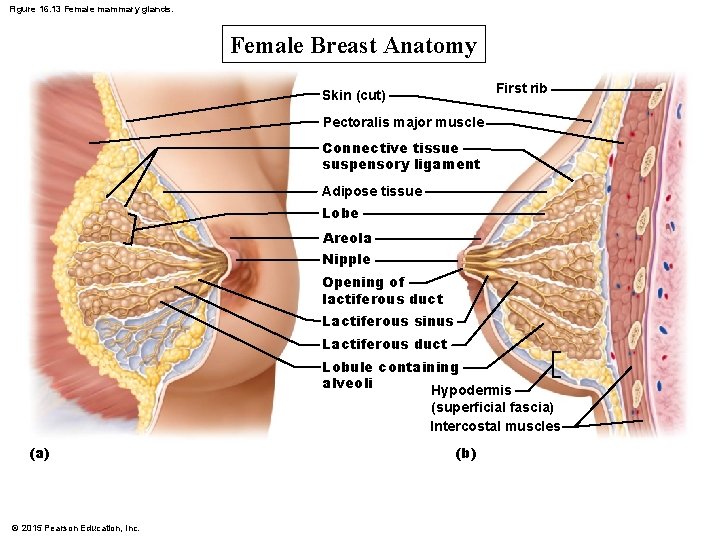
Female Breast and Lactation • Female breast contains 15 -20 lobules, each with a milk duct beginning at the nipple and ending in alveoli. – In pregnancy, breasts enlarge as ducts and alveoli increase in number and size due to estrogen and progesterone. v Milk usually not produced during pregnancy. Ø Prolactin suppressed due to increase in estrogen and progesterone; but then released after birth; prolactin causes milk production Ø Then suckling maintains prolactin secretion; stimulates release of prolactin-releasing hormone (PRH) Ø Suckling stimulates release of oxytocin- causes milk let-down 50
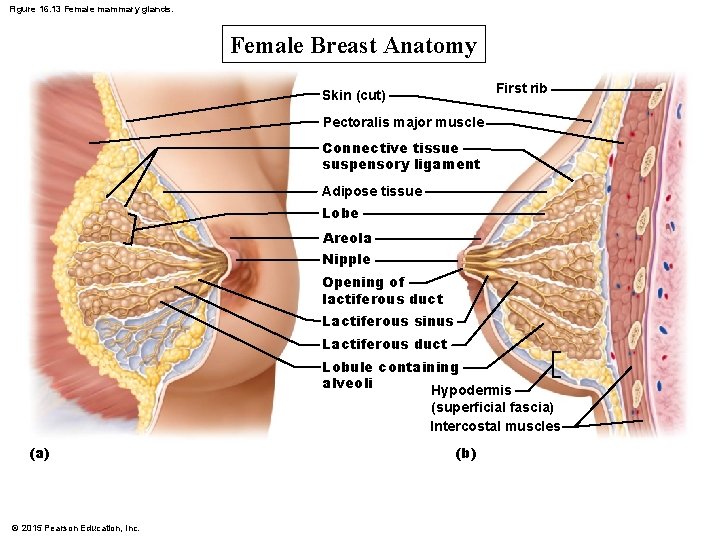
Figure 16. 13 Female mammary glands. Female Breast Anatomy First rib Skin (cut) Pectoralis major muscle Connective tissue suspensory ligament Adipose tissue Lobe Areola Nipple Opening of lactiferous duct Lactiferous sinus Lactiferous duct Lobule containing alveoli Hypodermis (superficial fascia) Intercostal muscles (a) © 2015 Pearson Education, Inc. (b)
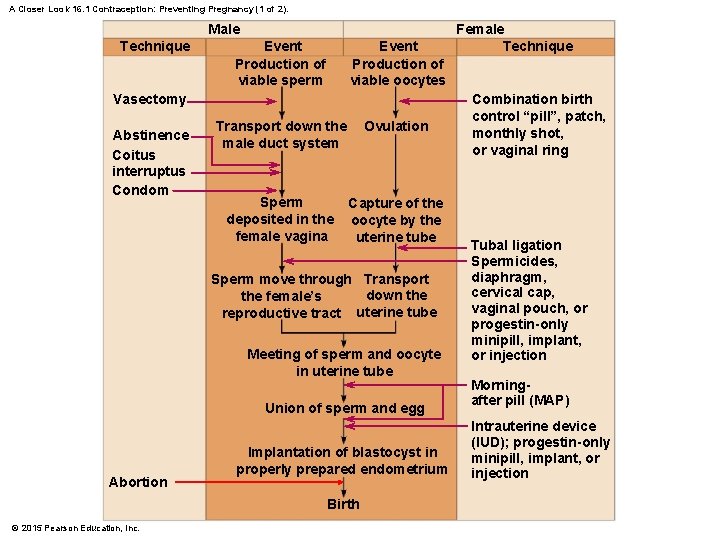
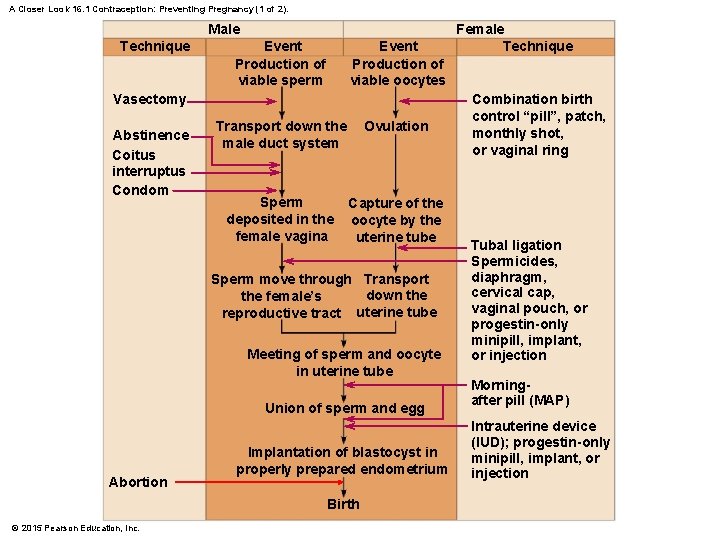
A Closer Look 16. 1 Contraception: Preventing Pregnancy (1 of 2). Male Technique Event Production of viable sperm Event Production of viable oocytes Vasectomy Abstinence Coitus interruptus Condom Transport down the male duct system Ovulation Sperm deposited in the female vagina Capture of the oocyte by the uterine tube Sperm move through Transport down the female’s reproductive tract uterine tube Meeting of sperm and oocyte in uterine tube Union of sperm and egg Abortion Implantation of blastocyst in properly prepared endometrium Birth © 2015 Pearson Education, Inc. Female Technique Combination birth control “pill”, patch, monthly shot, or vaginal ring Tubal ligation Spermicides, diaphragm, cervical cap, vaginal pouch, or progestin-only minipill, implant, or injection Morningafter pill (MAP) Intrauterine device (IUD); progestin-only minipill, implant, or injection
Homeostasis • • • Estrogen stimulates fat deposition. Estrogen stimulates liver to produce important transport proteins. Estrogen stimulates synthesis of bone matrix proteins, prevents bone loss. Testosterone stimulates synthesis of proteins for skeletal muscle and bone growth. Testosterone influences liver and kidney enzymes and stimulates release of erythropoietin. Both hormones influence cardiovascular health. 53
1. Need to Know Functions of the reproductive system A. To produce offspring B. Positive effects of estrogens on liver transport proteins, bone matrix, fat deposition, cardiovascular health C. Positive effects of testosterone on skeletal muscle and bone growth, erythropoietin, cardiovascular health 54
Need to Know (Cont. ) 2. Female reproductive system A. General Anatomy B. Process of ovulation and it’s controls C. Ovarian cycle, follicular phase, luteal phase, hormones produced by what D. Uterine cycle, endometrial changes, proliferative phase, secretory phase, hormones involved E. Fertilization and pregnancy, human chorionic gonadotropin where made and why, placenta progesterone 55
Need to Know (Cont. ) 3. Male reproductive system A. General Anatomy B. Sperm production where and how, which hormones control what C. Hormonal negative feedback regulation for sperm production D. Testosterone is produced where 56
Need to Know (Cont. ) 4. Fertilization and Pregnancy A. Steps of fertilization 1. Only one sperm enters egg 2. Changes in cell membrane and zona pellucida prevent more sperm from getting in 3. Nuclei fuse, zygote is formed B. Cleavage of zygote cells 1. Occurs in the oviducts 2. Blastocyst is what implants 3. Inner cell mass of the blastocyst are embryonic stem cells 57
5. Need to Know (Cont. ) Fertilization and Pregnancy (Cont. ) C. Implantation 1. After implantation trophoblast cells produce human chorionic gonadotropin (HCG) 2. Understand how this maintains pregnancy by maintaining progesterone levels 58
6. Need to Know (Cont. ) Female breast and lactation A. Understand the interaction of prolactin and oxytocin on milk production and letdown 59