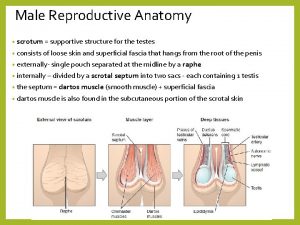
Male genital system MALE GENITAL SYSTEM PENIS SCROTUM








- Slides: 38
Male genital system
MALE GENITAL SYSTEM • PENIS • SCROTUM, TESTIS, & EPIDIDYMIS • PROSTATE
PENIS • MALFORMATIONS • INFLAMMATORY LESIONS • NEOPLASMS
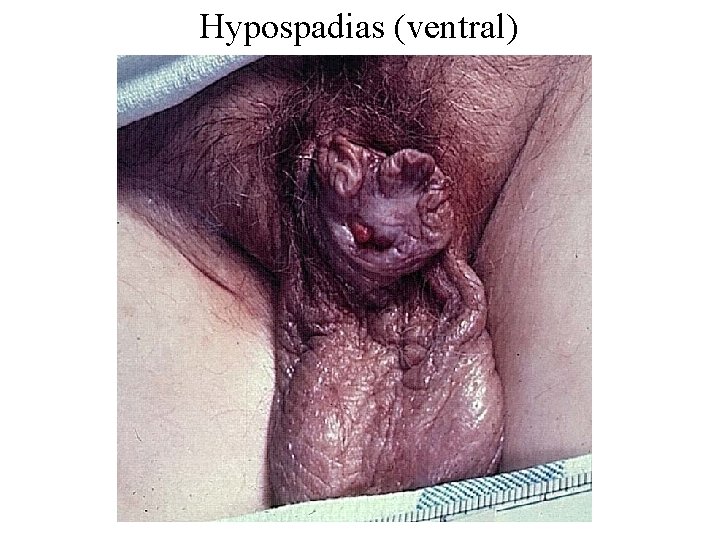
MALFORMATIONS OF THE PENIS Abnormal location of urethral orifice along penile shaft – Hypospadias (ventral aspect) • Most common (1/250 live male births) – Epispadias (dorsal aspect)
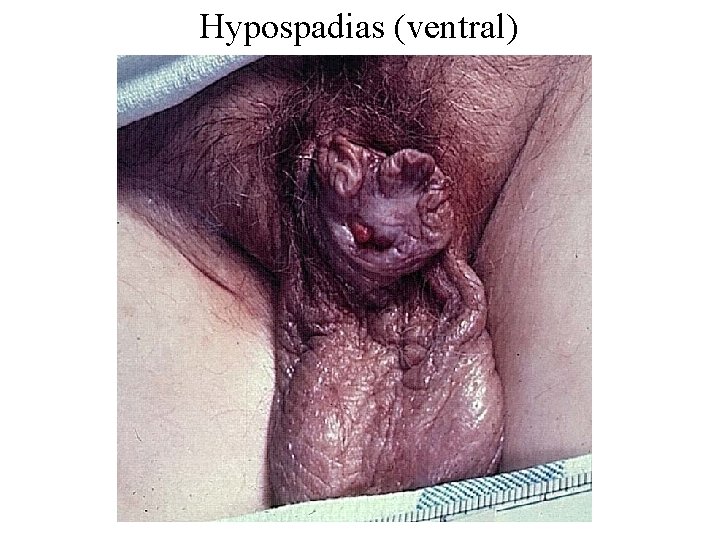
Hypospadias (ventral)

Epispadias (dorsal)
HYPOSPADIAS AND EPISPADIAS – May be associated with other genital abnormalities • Inguinal hernias • Undescended testes – Clinical consequences • Constriction of orifice • Urinary tract obstruction • Urinary tract infection • Impaired reproductive function
INFLAMMATORY LESIONS OF THE PENIS • Sexually transmitted diseases • Balanitis (balanoposthitis) – Inflammation of the glans (plus prepuce) – Associated with poor local hygiene in uncircumcised men • Smegma – Distal penis is red, swollen, tender • +/- Purulent discharge
INFLAMMATORY LESIONS OF THE PENIS • PHIMOSIS – PREPUCE CANNOT BE EASILY RETRACTED OVER GLANS – MAY BE CONGENITAL – USUALLY ASSOCIATED WITH BALANOPOSTHITIS AND SCARRING – PARAPHIMOSIS (TRAPPED GLANS) • URETHRAL CONSTRICTION
INFLAMMATORY LESIONS OF THE PENIS • FUNGAL INFECTIONS – CANDIDIASIS • ESPECIALLY IN DIABETICS • EROSIVE, PAINFUL, PRURITIC • CAN INVOLVE ENTIRE MALE EXTERNAL GENITALIA
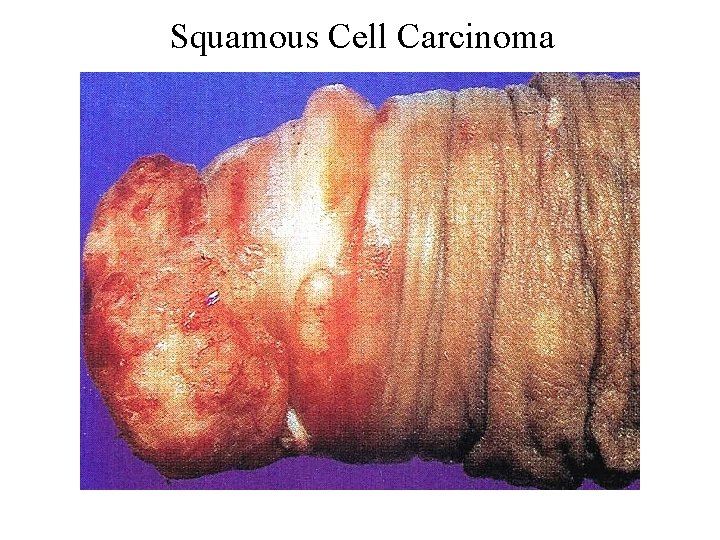
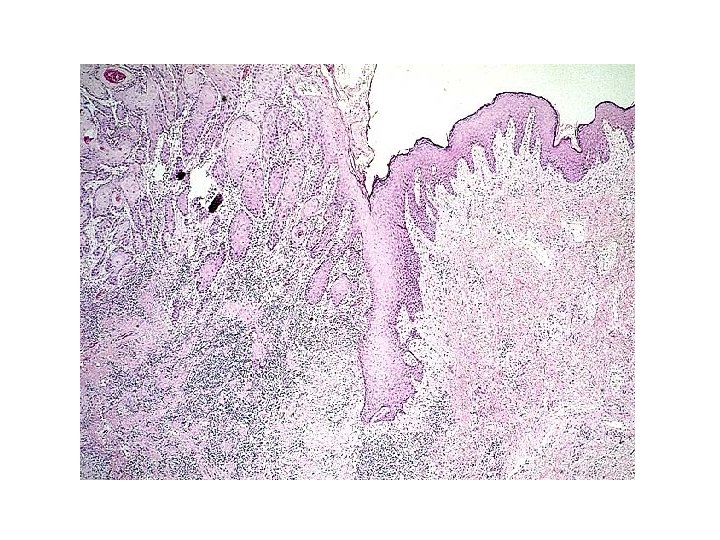
NEOPLASMS OF THE PENIS • SQUAMOUS CELL CARCINOMA (SCC) – EPIDEMIOLOGY • UNCOMMON – LESS THAN 1 % OF CA IN US MEN • UNCIRCUMCISED MEN BETWEEN 40 AND 70 – PATHOGENESIS • POOR HYGIENE, SMEGMA, SMOKING • HUMAN PAPILLOMA VIRUS (16 AND 18) • CIS FIRST, THEN PROGRESSION TO INVASIVE SQUAMOUS CELL CARCINOMA
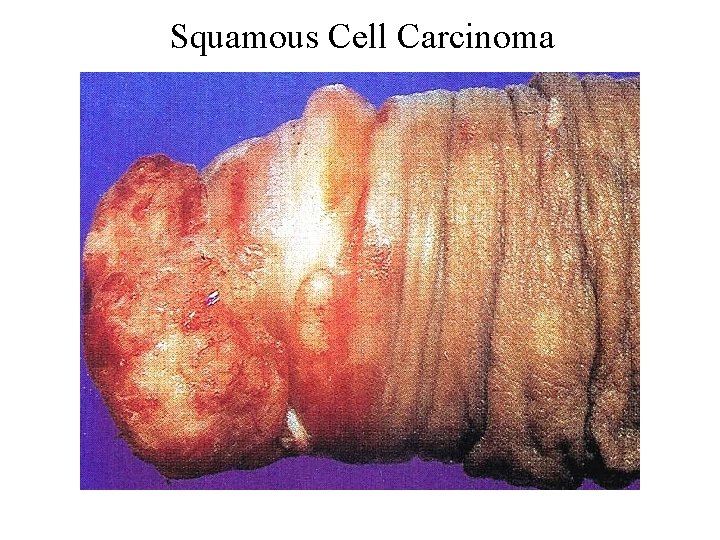
Squamous Cell Carcinoma
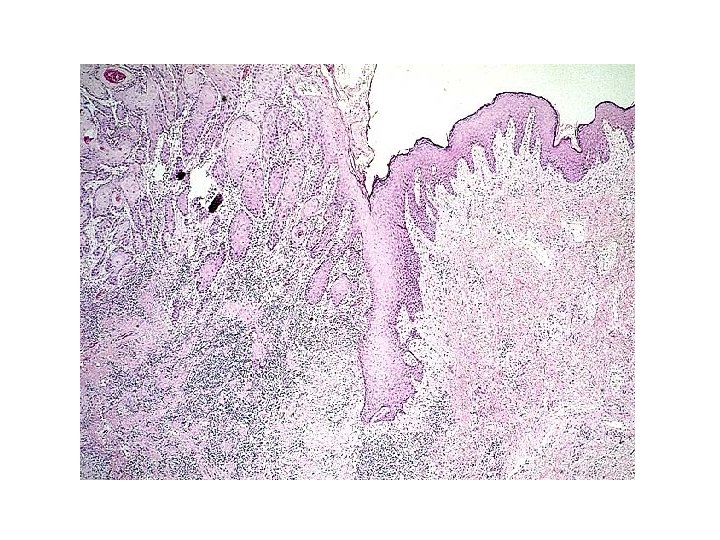

SCC OF THE PENIS • Clinical course – Usually indolent – Locally invasive – Has spread to inguinal lymph nodes in 25% of cases at presentation – Distant mets rare – 5 yr survival • 70% without ln mets • 27% with ln mets
LESIONS INVOLVING THE SCROTUM • Inflammation – Tinea cruris (jock itch) • Superficial dermatophyte infection • Scaly, red, annular plaques, pruritic • Inguinal crease to upper thigh • Squamous cell carcinoma – Historical significance – Chimney sweeps used to have this
LESIONS INVOLVING THE SCROTUM • Scrotal enlargement – Hydrocele - most common cause • Accumulation of serous fluid within tunica vaginalis • Infections, tumor, idiopathic – Hematocele – Chylocele • Filiariasis - elephantiasis – Testicular disease

Hydrocele

LESIONS OF THE TESTES • CONGENITAL • INFLAMMATORY • NEOPLASTIC

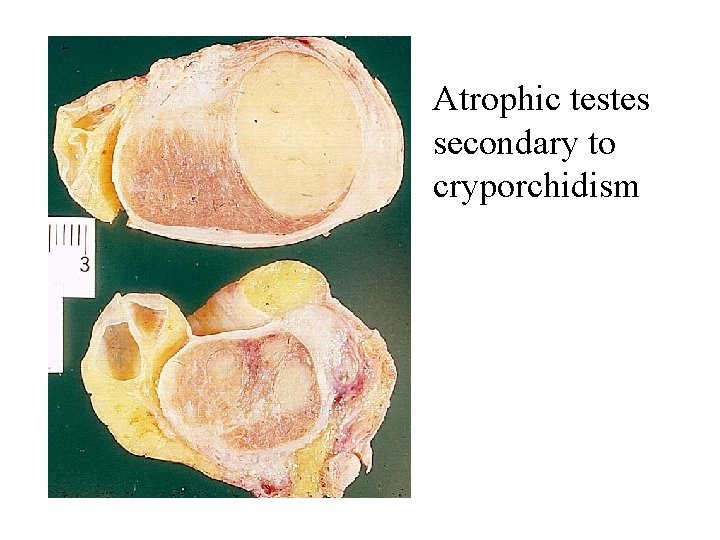
Cryptorchidism and testicular atrophy • Failure of testicular descent • Epidemiology – About 1% of males (at 1 yr) – Right > left, 10% bilateral • Pathogenesis – Hormonal abnormalities – Testicular abnormalities – Mechanical problems
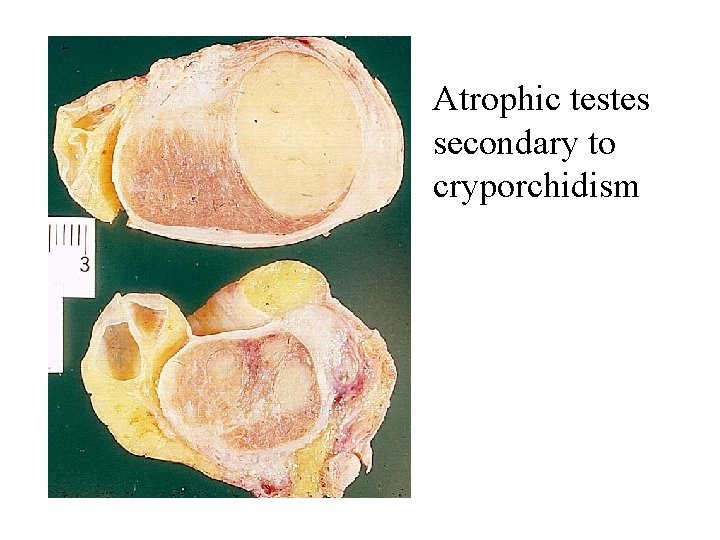
Atrophic testes secondary to cryporchidism
Cryptorchidism and testicular atrophy • Clinical course – When unilateral, may see atrophy in contralateral testis – Sterility – Increased risk of malignancy (3 -5 x) – Orchiopexy • May help prevent atrophy • May not eliminate risk of malignancy
Other causes of testicular atrophy • • Chronic ischemia Inflammation or trauma Hypopituitarism Excess female sex hormones – Therapeutic administration – Cirrhosis • Malnutrition • Irradiation • Chemotherapy
Inflammatory lesions of the testis • Usually involve the epididymis first • Sexually transmitted diseases • Nonspecific epididymitis and orchitis – Secondary to uti • Bacterial and non-bacterial – Swelling, tenderness – Acute inflammatory infiltrate
Inflammatory lesions of the testis • Mumps – 20% of adult males with mumps – Edema and congestion – Chronic inflammatory infiltrate – May cause atrophy and sterility • Tuberculosis – Granulomatous inflammation – Caseous necrosis
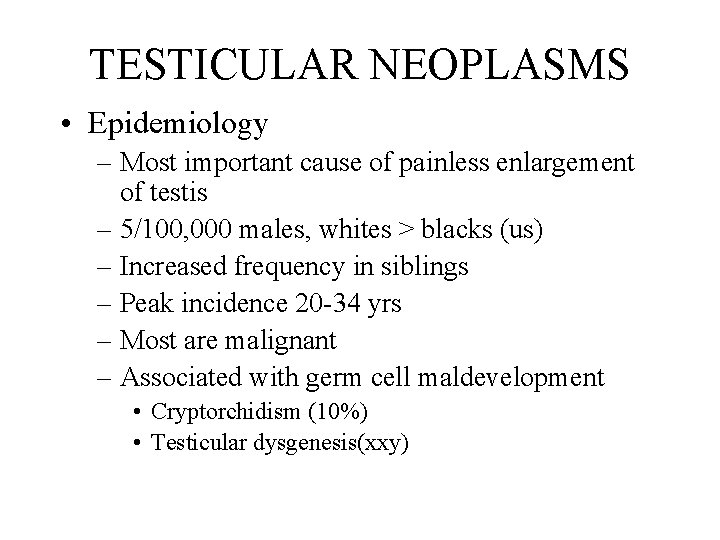
TESTICULAR NEOPLASMS • Epidemiology – Most important cause of painless enlargement of testis – 5/100, 000 males, whites > blacks (us) – Increased frequency in siblings – Peak incidence 20 -34 yrs – Most are malignant – Associated with germ cell maldevelopment • Cryptorchidism (10%) • Testicular dysgenesis(xxy)
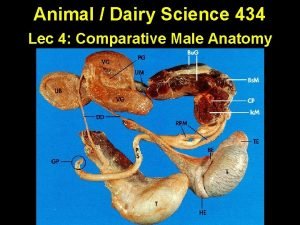
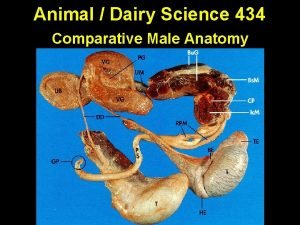
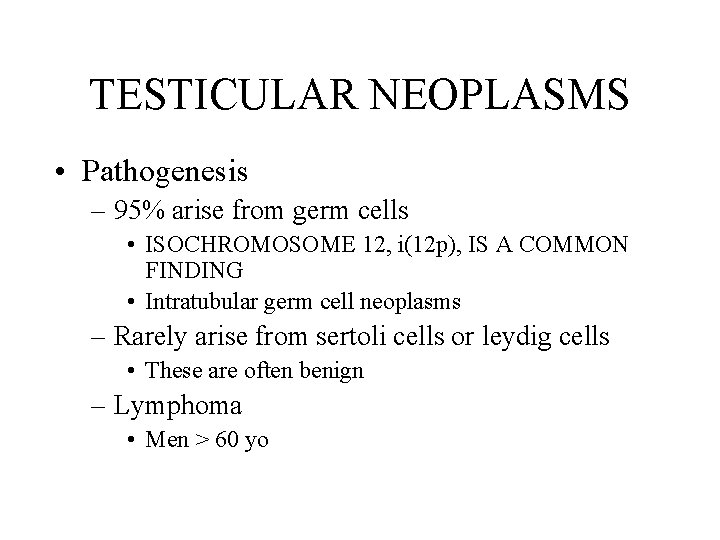
TESTICULAR NEOPLASMS • Pathogenesis – 95% arise from germ cells • ISOCHROMOSOME 12, i(12 p), IS A COMMON FINDING • Intratubular germ cell neoplasms – Rarely arise from sertoli cells or leydig cells • These are often benign – Lymphoma • Men > 60 yo
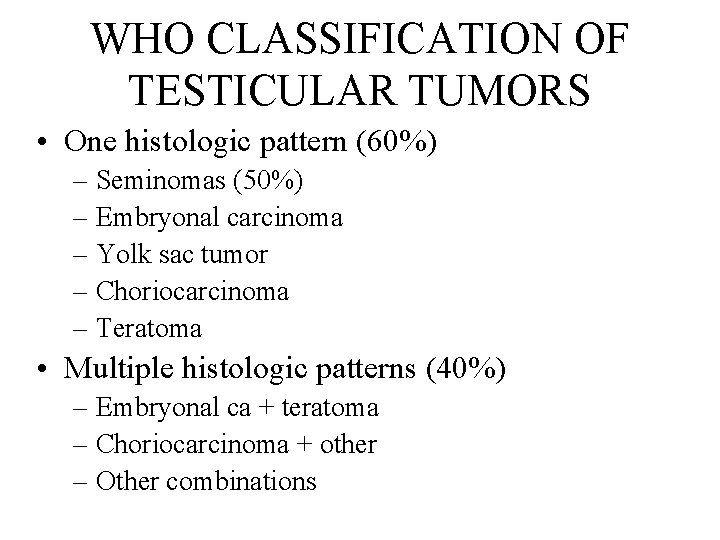
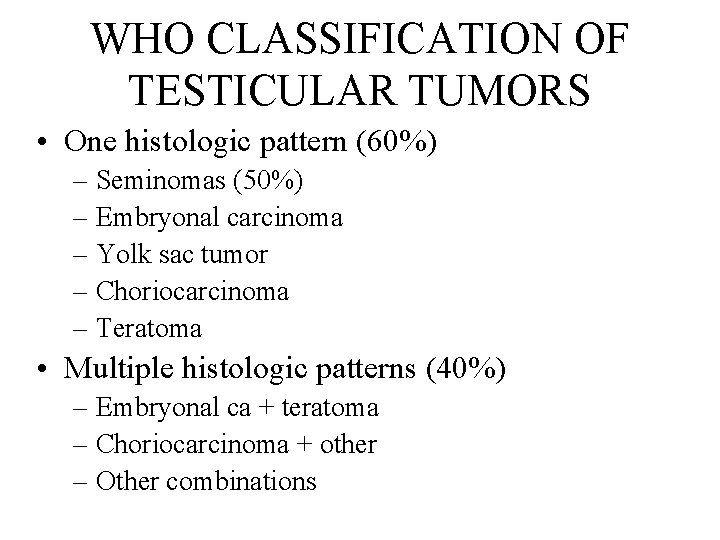
WHO CLASSIFICATION OF TESTICULAR TUMORS • One histologic pattern (60%) – Seminomas (50%) – Embryonal carcinoma – Yolk sac tumor – Choriocarcinoma – Teratoma • Multiple histologic patterns (40%) – Embryonal ca + teratoma – Choriocarcinoma + other – Other combinations
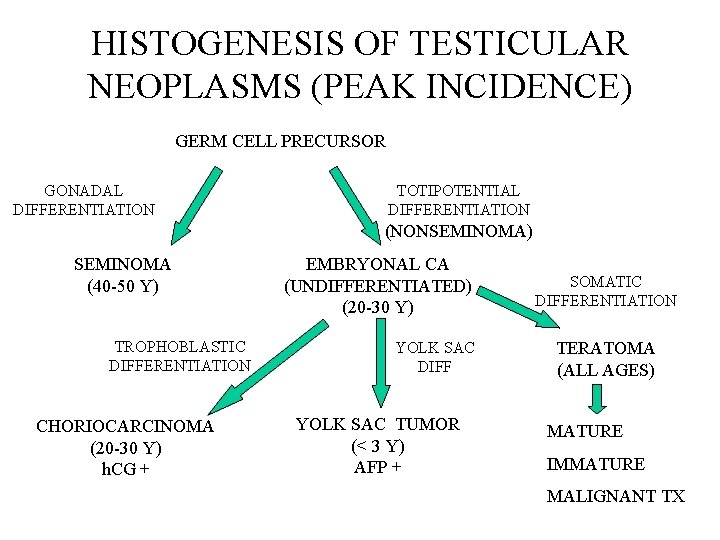
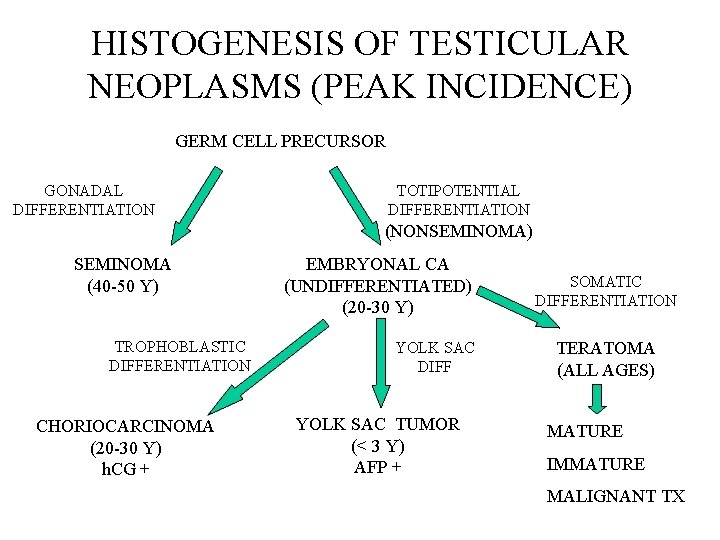
HISTOGENESIS OF TESTICULAR NEOPLASMS (PEAK INCIDENCE) GERM CELL PRECURSOR GONADAL DIFFERENTIATION TOTIPOTENTIAL DIFFERENTIATION (NONSEMINOMA) SEMINOMA (40 -50 Y) TROPHOBLASTIC DIFFERENTIATION CHORIOCARCINOMA (20 -30 Y) h. CG + EMBRYONAL CA (UNDIFFERENTIATED) (20 -30 Y) YOLK SAC DIFF YOLK SAC TUMOR (< 3 Y) AFP + SOMATIC DIFFERENTIATION TERATOMA (ALL AGES) MATURE IMMATURE MALIGNANT TX

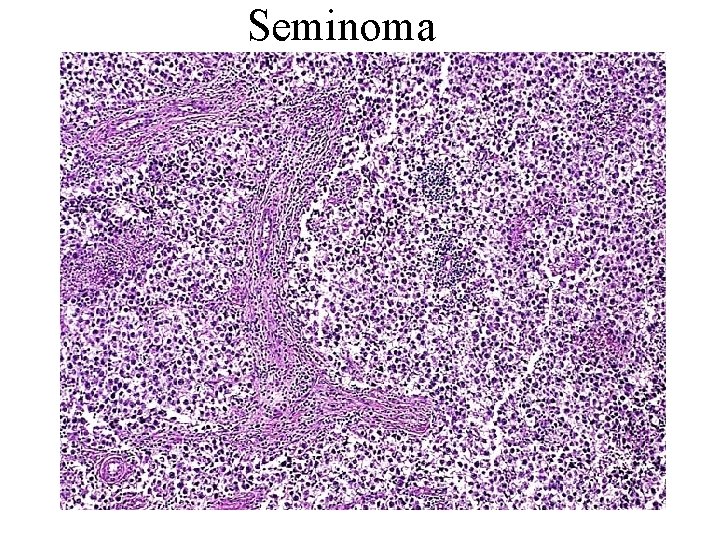
Seminoma, with focal hemorrhage and necrosis
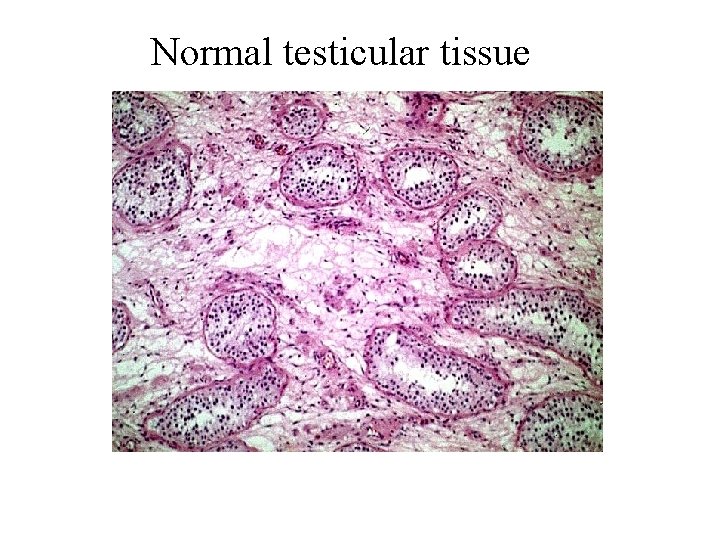
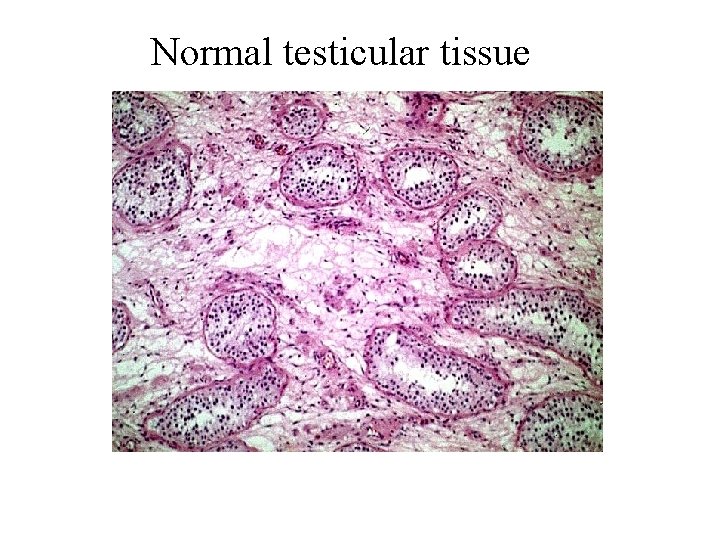
Normal testicular tissue
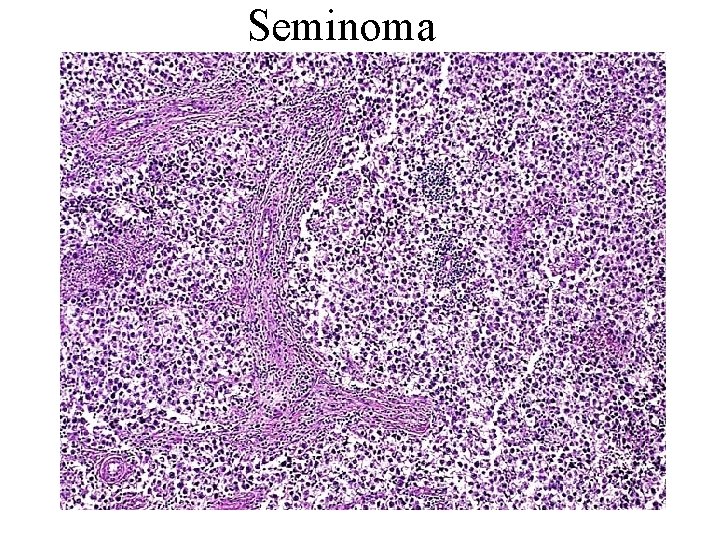
Seminoma


Seminoma Syncytiotrophoblast
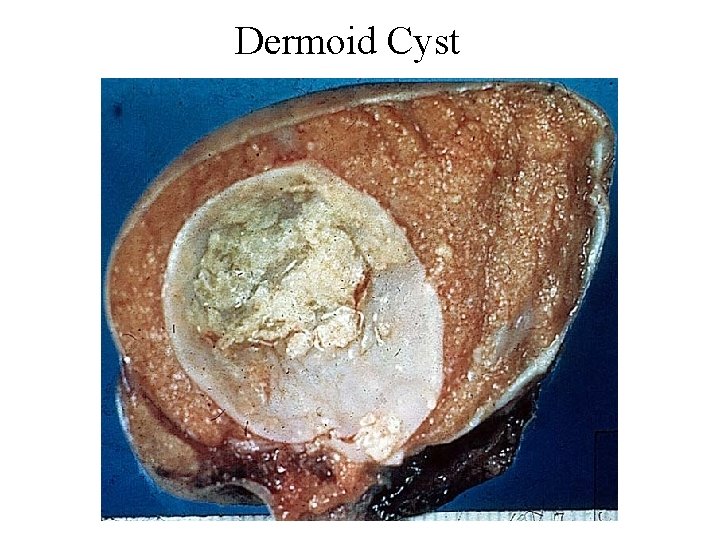
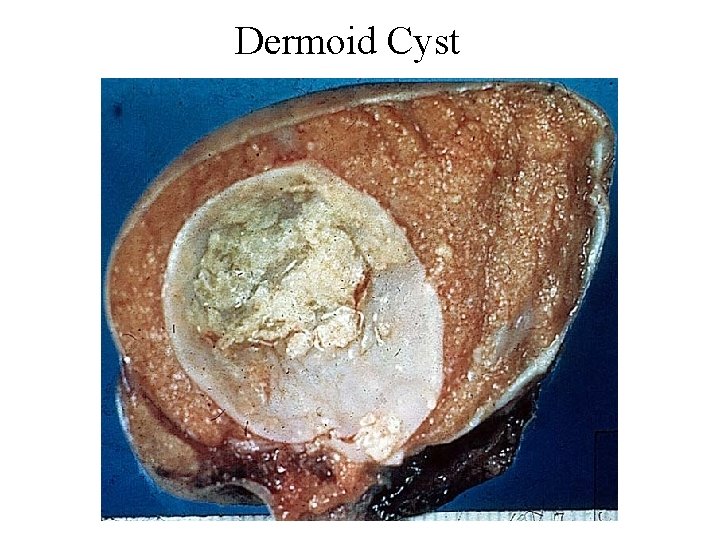
Dermoid Cyst
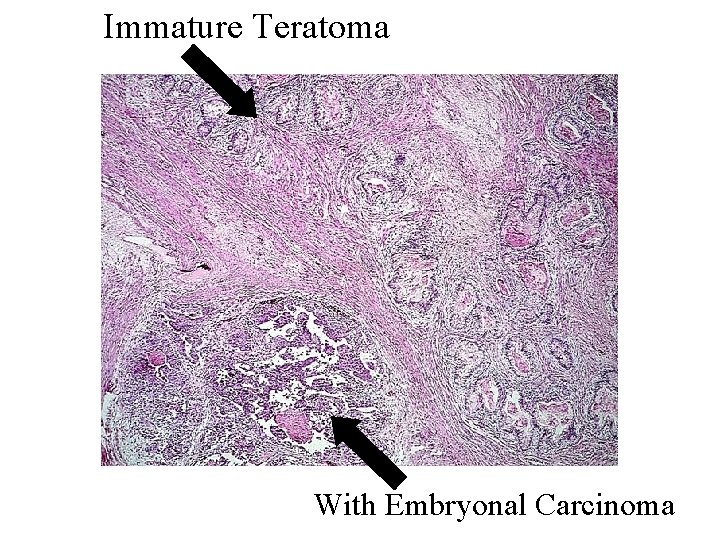
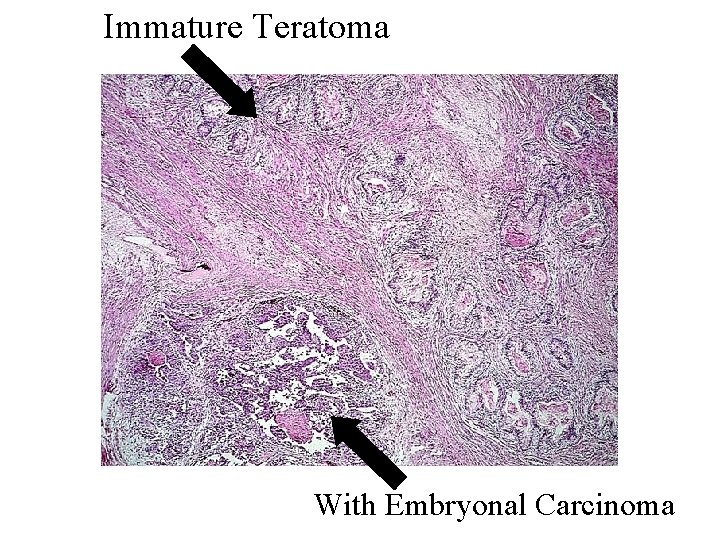
Immature Teratoma With Embryonal Carcinoma
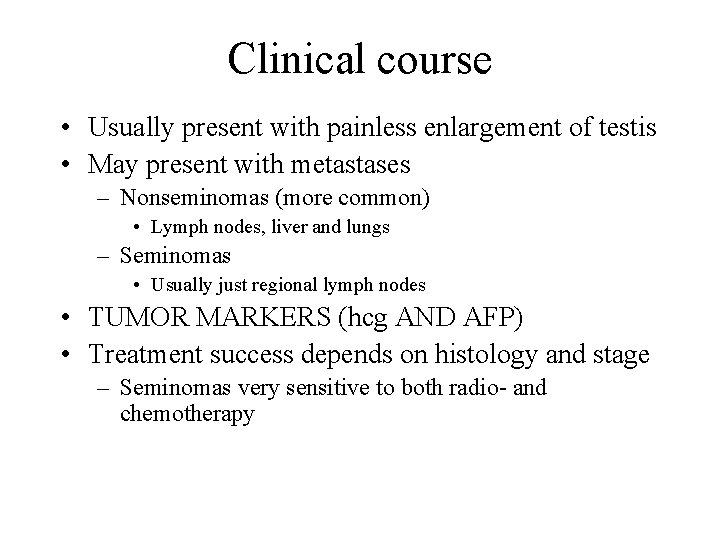
Clinical course • Usually present with painless enlargement of testis • May present with metastases – Nonseminomas (more common) • Lymph nodes, liver and lungs – Seminomas • Usually just regional lymph nodes • TUMOR MARKERS (hcg AND AFP) • Treatment success depends on histology and stage – Seminomas very sensitive to both radio- and chemotherapy
Thank You
 Male genital variation
Male genital variation Reproductive system function
Reproductive system function Does urine and sperm come from the same tube
Does urine and sperm come from the same tube Function of prostate gland
Function of prostate gland I ii iii
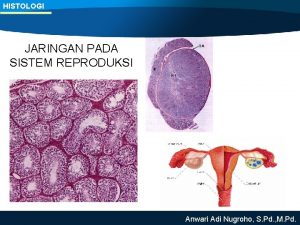
I ii iii Testis katmanları
Testis katmanları Cylindrical pendant organ located anterior to the scrotum
Cylindrical pendant organ located anterior to the scrotum Male reproductive system
Male reproductive system Hernia protrusion
Hernia protrusion Caverna corporum cavernosum
Caverna corporum cavernosum V
V Kryptorchismus
Kryptorchismus Bell clapper deformity pictures
Bell clapper deformity pictures Epididymiis
Epididymiis Orchidodesis adalah
Orchidodesis adalah Terminologi medis sistem reproduksi pria
Terminologi medis sistem reproduksi pria Epididymitis treatment
Epididymitis treatment Ductus ejaculatoris
Ductus ejaculatoris Scrotum anatomie
Scrotum anatomie Female reproductive system external
Female reproductive system external Gemiddelde penislengte
Gemiddelde penislengte Um jeito diferente de ver o salmo 23
Um jeito diferente de ver o salmo 23 Penis envy freud
Penis envy freud Nunc habemus endiviam
Nunc habemus endiviam Penis é um musculo
Penis é um musculo Anapsidní lebka
Anapsidní lebka Temeno hlavy
Temeno hlavy Women body parts name
Women body parts name Platypus adalah
Platypus adalah Glandula vesicalis
Glandula vesicalis Site:slidetodoc.com
Site:slidetodoc.com Uterine axis
Uterine axis Penis anatom
Penis anatom Child penis
Child penis Kids penis
Kids penis Ovarian ligament
Ovarian ligament Le serpent penis
Le serpent penis Glans penis
Glans penis Glans penis
Glans penis