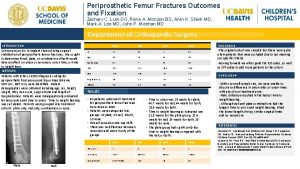
Fractures of The Hip and The Femur Femoral






























- Slides: 116
Fractures of The Hip and The Femur
Femoral neck fracture Intracapsular fractures It is the commonest fracture in the elderly More in women Risk factors: Osteoporosis Osteomalacia Diabetes Alcoholism Chronic debilitating disease
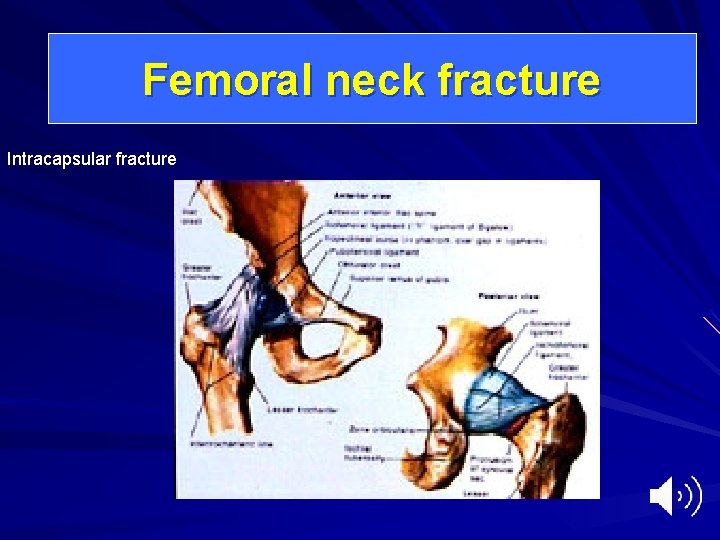
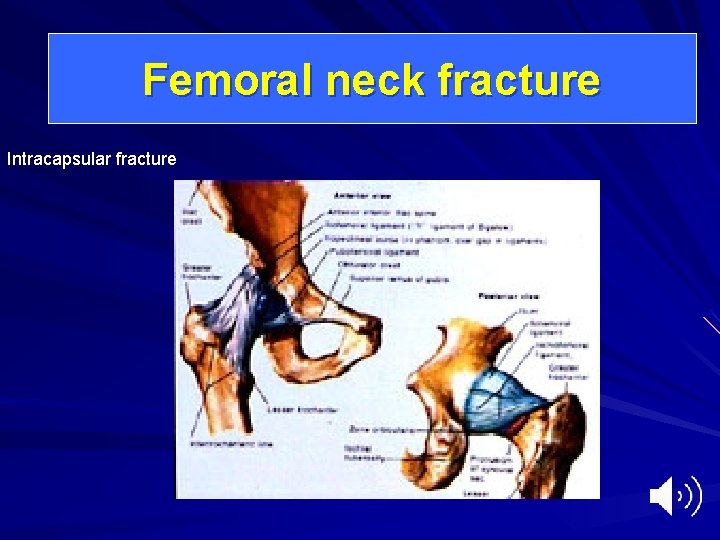
Femoral neck fracture Intracapsular fracture
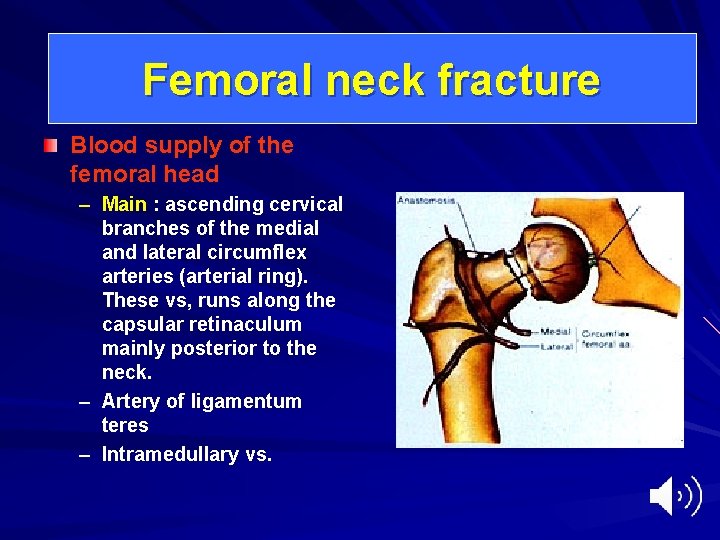
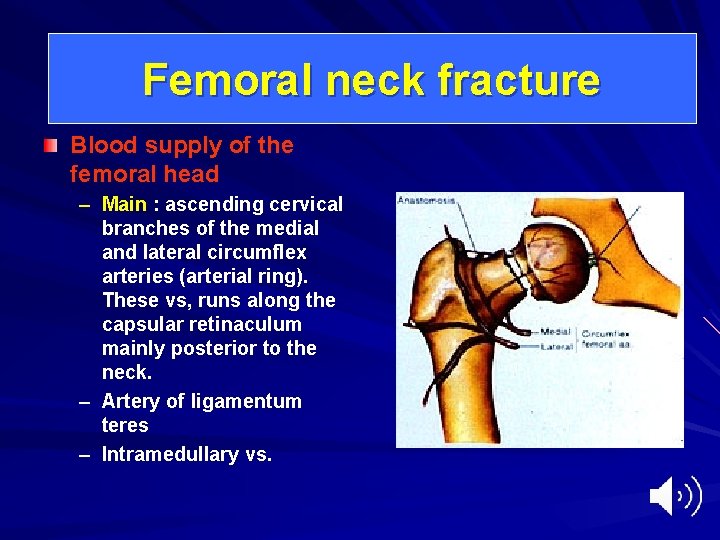
Femoral neck fracture Blood supply of the femoral head – Main : ascending cervical branches of the medial and lateral circumflex arteries (arterial ring). These vs, runs along the capsular retinaculum mainly posterior to the neck. – Artery of ligamentum teres – Intramedullary vs.
Femoral neck fracture Mechanism of injury: – External rotation of the leg (twisting) – Simple fall on the greater trochanter – In young individual, severe trauma Fall from height RTA
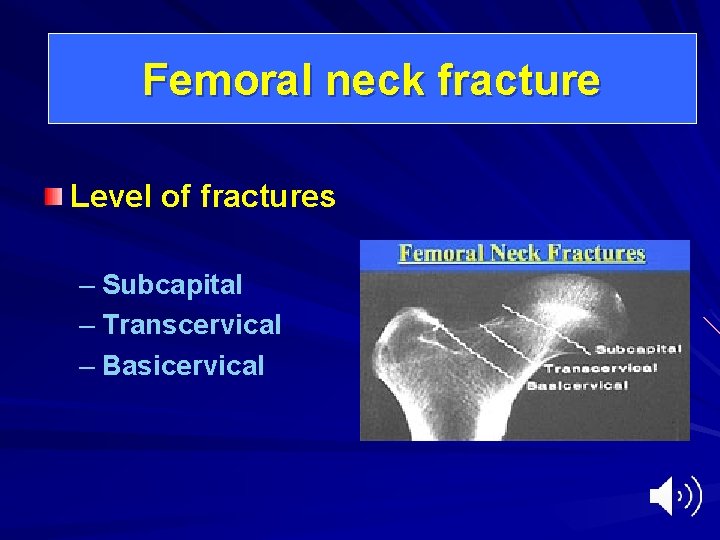
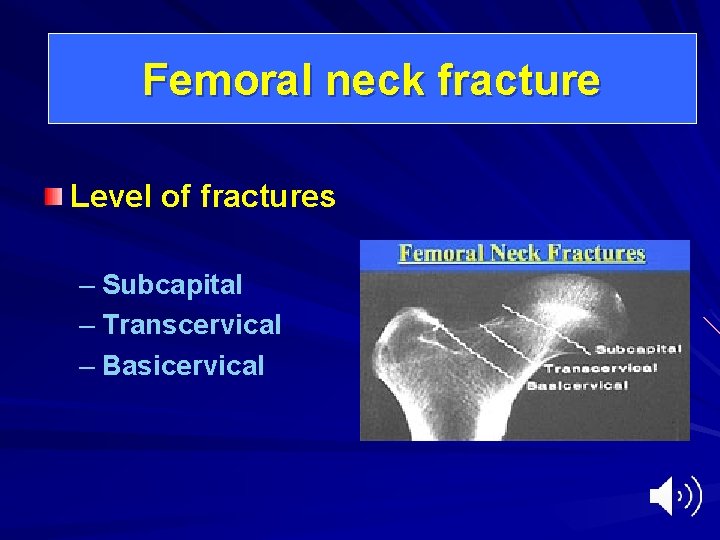
Femoral neck fracture Level of fractures – Subcapital – Transcervical – Basicervical

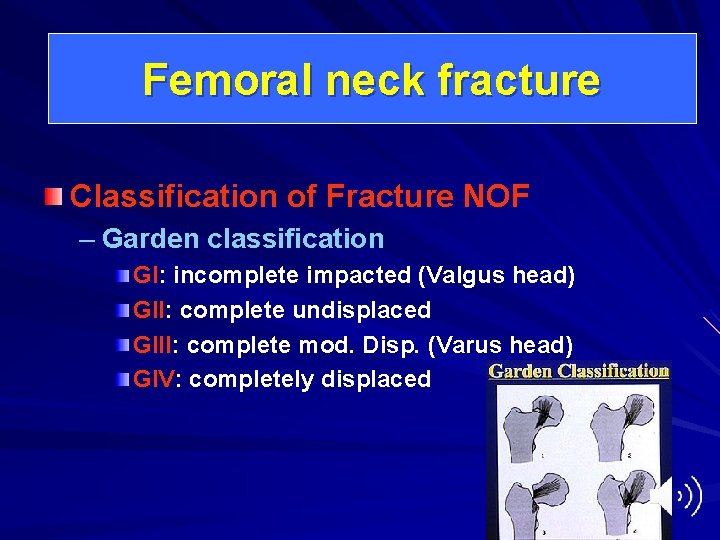
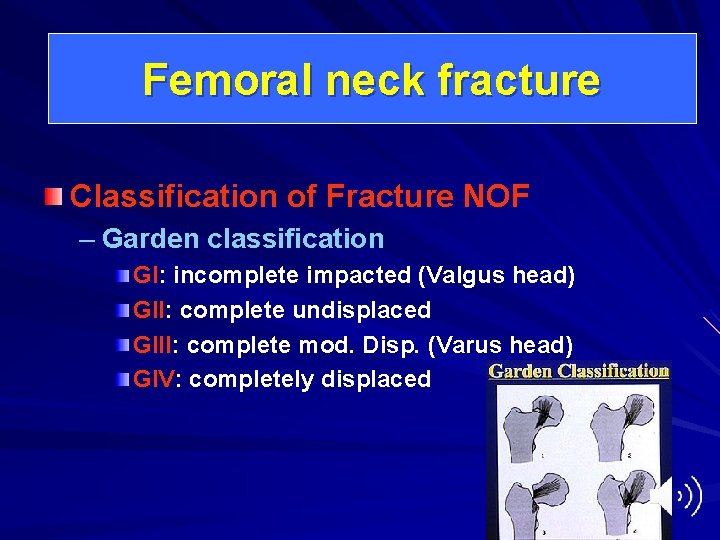
Femoral neck fracture Classification of Fracture NOF – Garden classification GI: incomplete impacted (Valgus head) GII: complete undisplaced GIII: complete mod. Disp. (Varus head) GIV: completely displaced

Femoral neck fracture Garden I and II Stable Garden III and IV Unstable
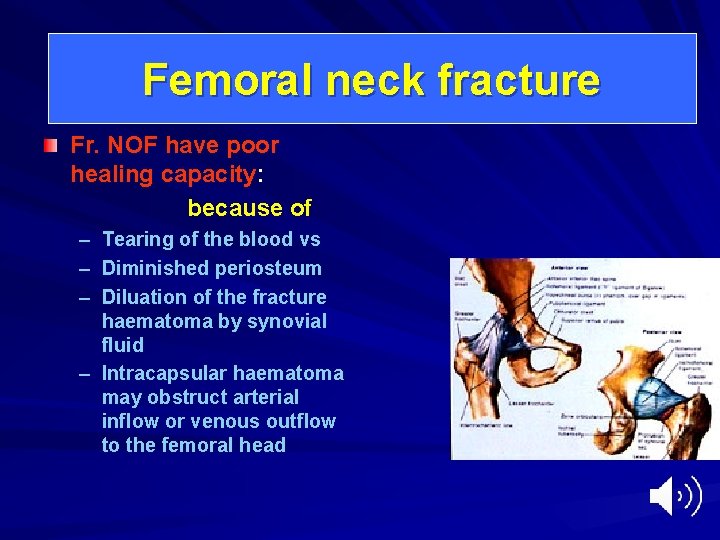
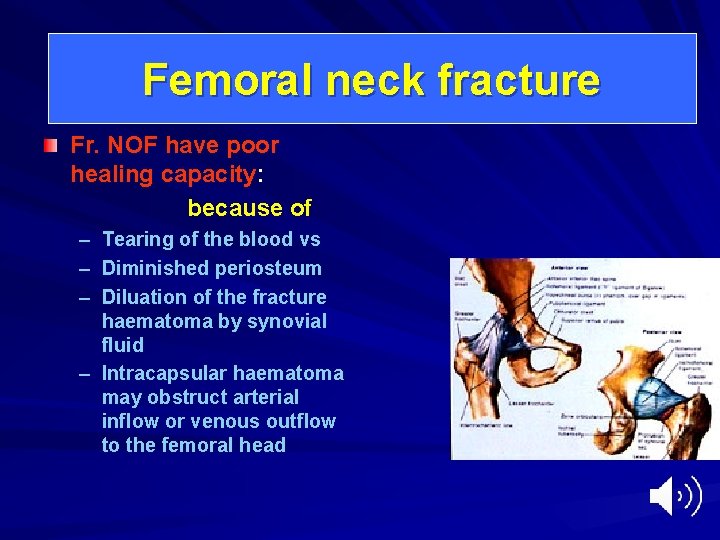
Femoral neck fracture Fr. NOF have poor healing capacity: because of – – – Tearing of the blood vs Diminished periosteum Diluation of the fracture haematoma by synovial fluid – Intracapsular haematoma may obstruct arterial inflow or venous outflow to the femoral head
Femoral neck fracture Clinical features: – – – History of trauma Severe pain Unable to bear weight Deformity : external rotation, and shortening Impacted fracture no deformity, can bear weight
Femoral neck fracture X-rays : – Identify the fracture – Level of the fracture – Degree of displacement
Femoral neck fracture Treatment of fracture NOF: Urgent Generally is internal fixation Depends on the : Age of the patients Degree of displacement
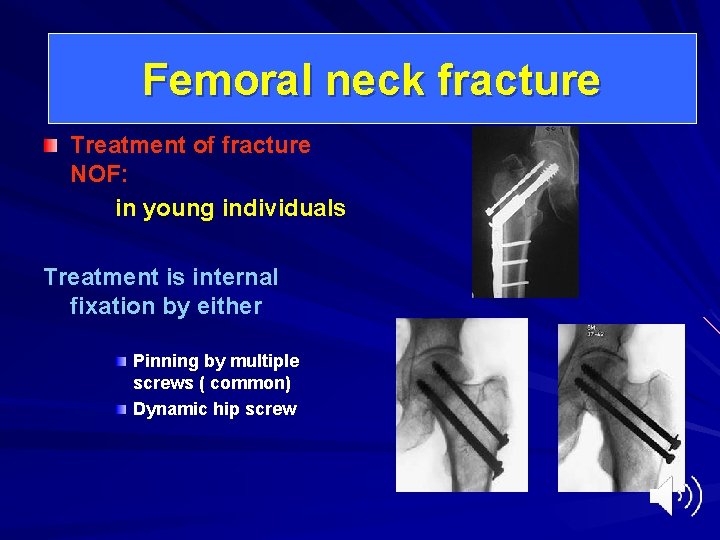
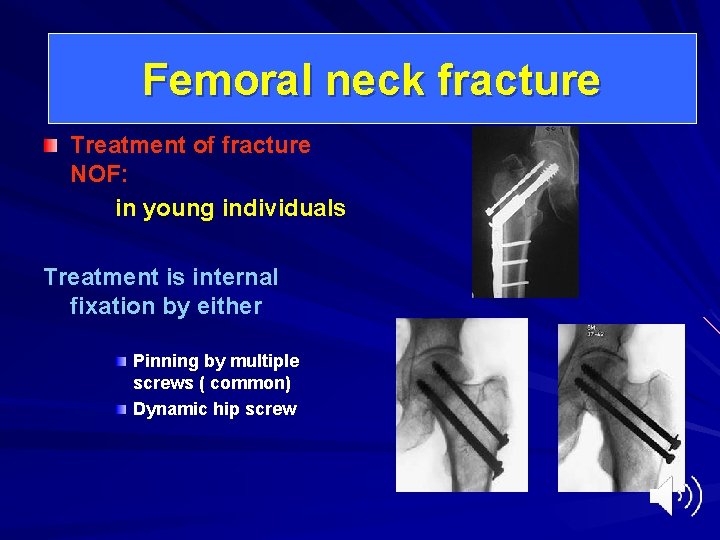
Femoral neck fracture Treatment of fracture NOF: in young individuals Treatment is internal fixation by either Pinning by multiple screws ( common) Dynamic hip screw
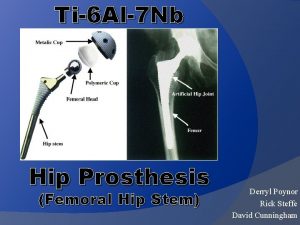
Femoral neck fracture Treatment of fracture NOF: Goal: In elderly – Aim: Early mobilization Garden I and II by internal fixation Garden III and IV by prosthetic replacement: Austin Moore hemiarthroplasty Thomson prosthesis Bipolar prosthesis Total hip arthroplasty
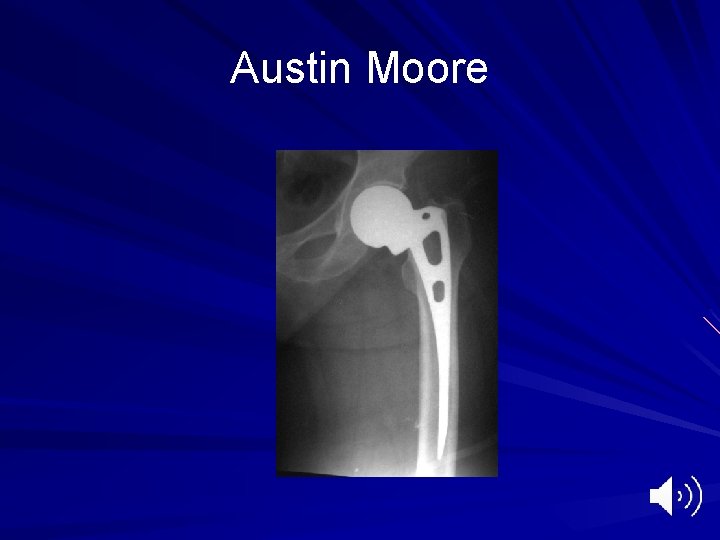
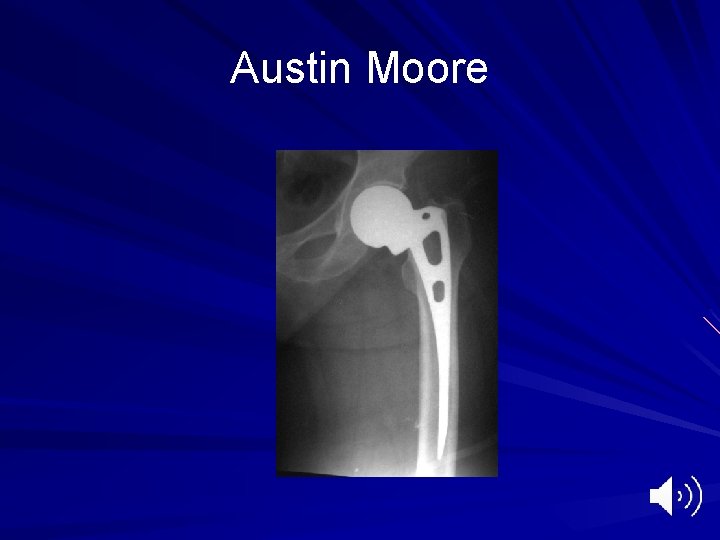
Austin Moore
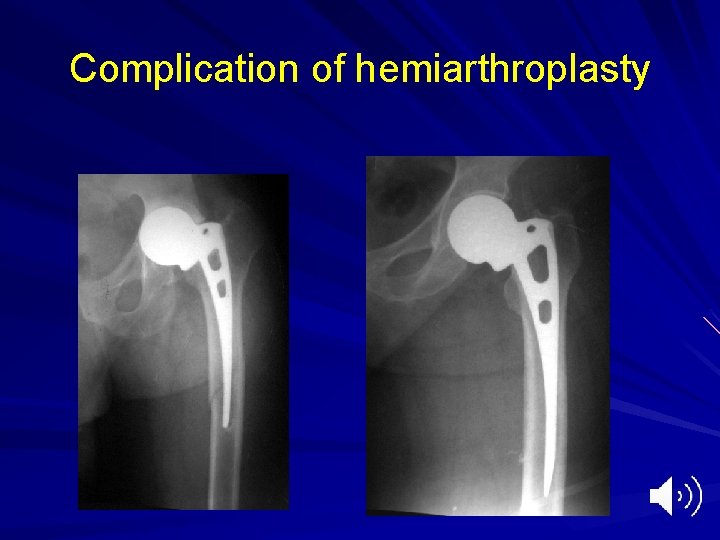
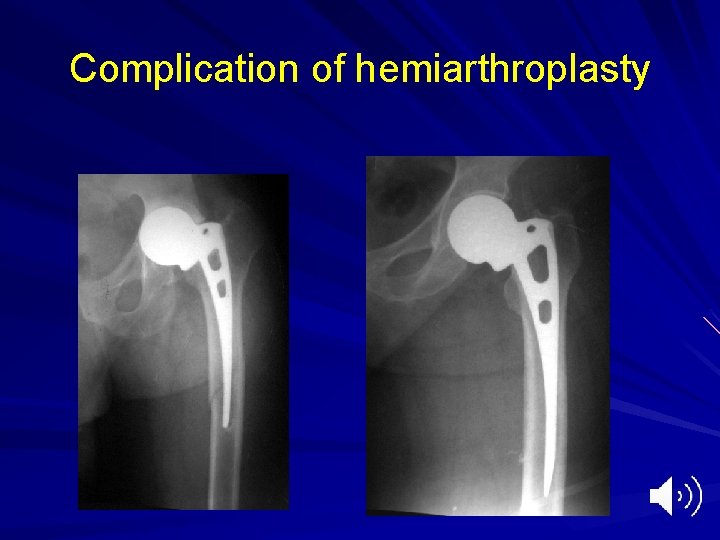
Complication of hemiarthroplasty

Femoral neck fracture Complication of Fracture NOF – Avascular Necrosis of the femoral head. Due to disruption of the blood supply Lead to collapse of the femoral head Pain and osteoarthritis

Femoral neck fracture Complication of Fracture NOF – Avascular Necrosis of the femoral head. – Treatment: THR
Femoral neck fracture Complication of Fracture NOF – Nonunion: common in displaced fractures Due to Instability of the fracture ( high oblique fracture) Poor blood supply Imperfect reduction Inadequate fixation Diminished periosteum Dilution of fr hematoma

Femoral neck fracture Complication of Fracture NOF – Nonunion: Treatment: depends on the cause and age of patient: – Young patients Subtrochanteric osteotomy Transfer forces from vertical shear into compression forces
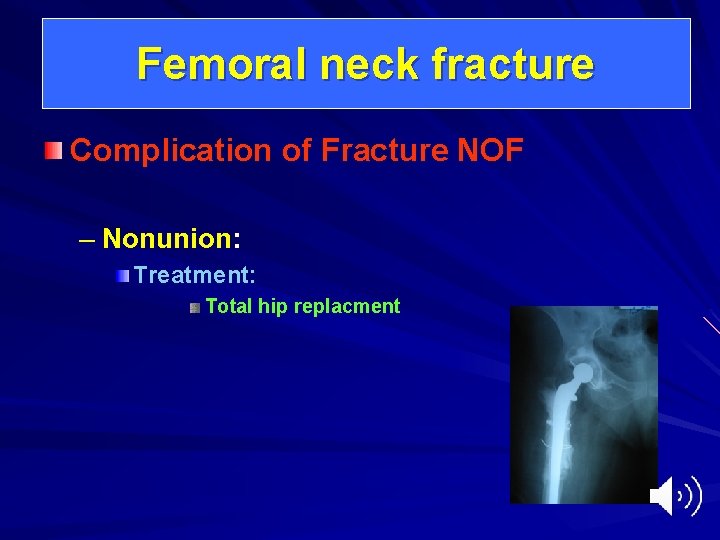
Femoral neck fracture Complication of Fracture NOF – Nonunion: Treatment: Total hip replacment
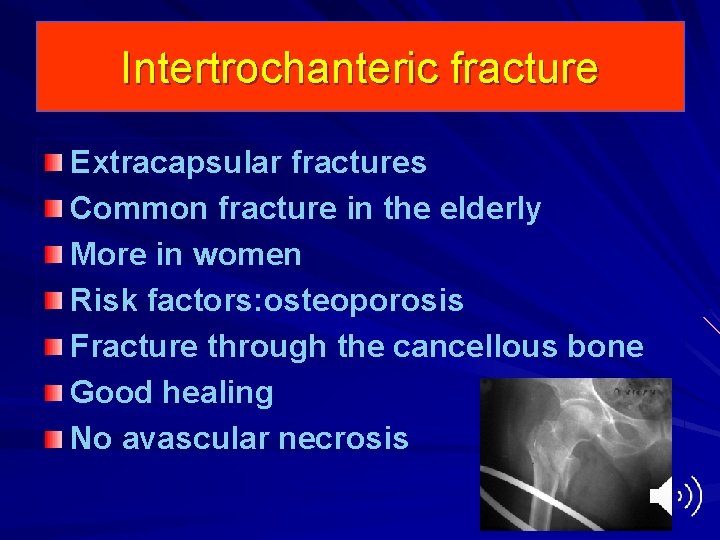
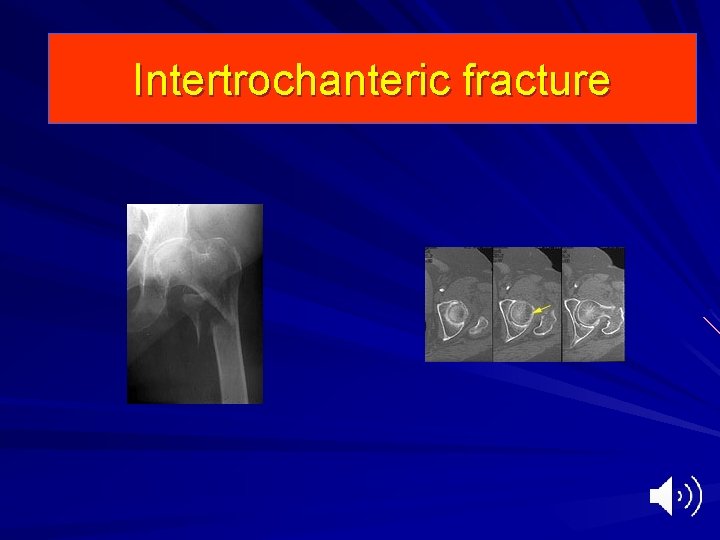
Intertrochanteric fracture Extracapsular fractures Common fracture in the elderly More in women Risk factors: osteoporosis Fracture through the cancellous bone Good healing No avascular necrosis
Intertrochanteric fracture Mechanism of injury – Twisting injury ( external rotation) – Direct fall on the greater trochanter

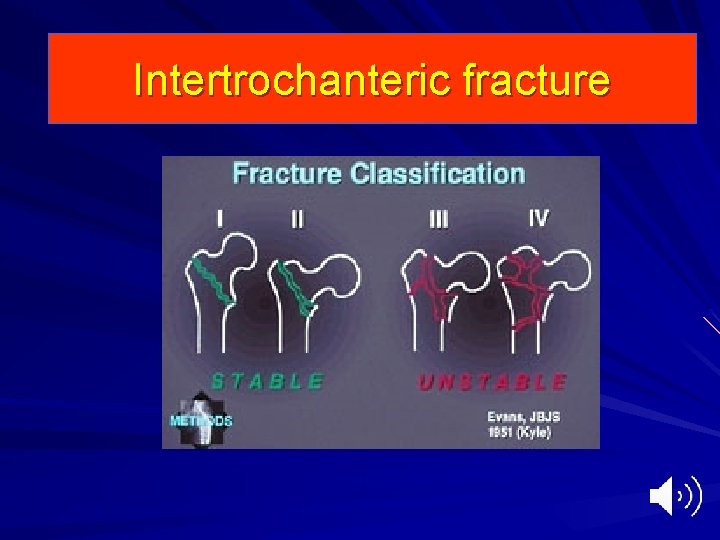
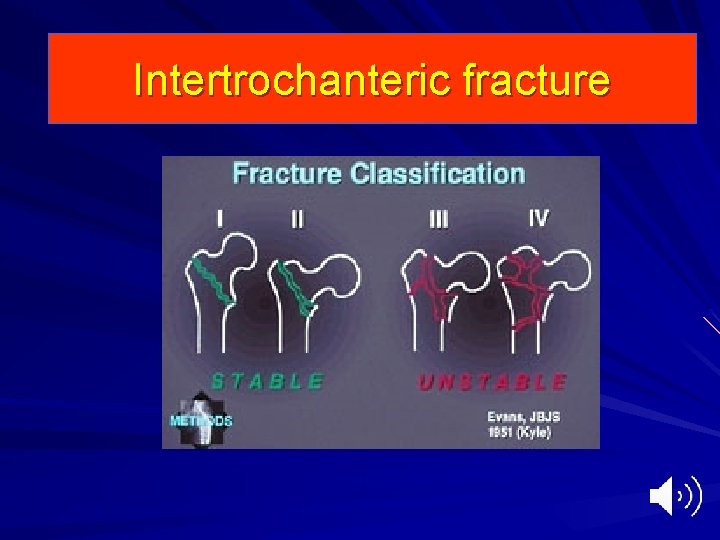
Intertrochanteric fracture Pathological anatomy: divided into – Stable fracture: good contact between bony surfaces – Unstable fracture: – Four part fracture – Posteromedial comminuation – High oblique fracture – Reversed obliquity
Intertrochanteric fracture

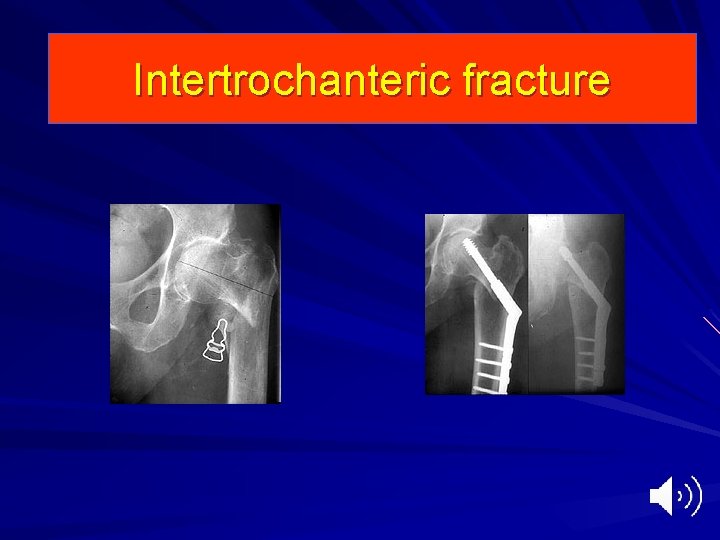
Intertrochanteric fracture
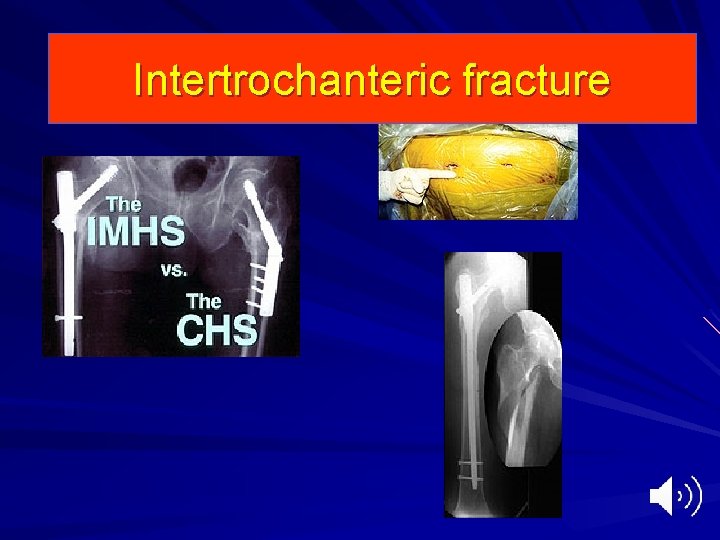
Intertrochanteric fracture
Intertrochanteric fracture Clinical features – History of trauma – Unable to stand – Deformity, external rotation and shortening – Severe pain – splinting
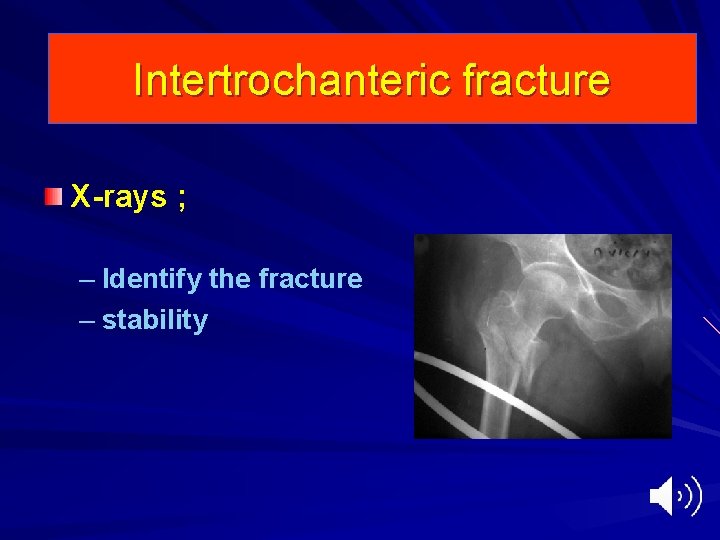
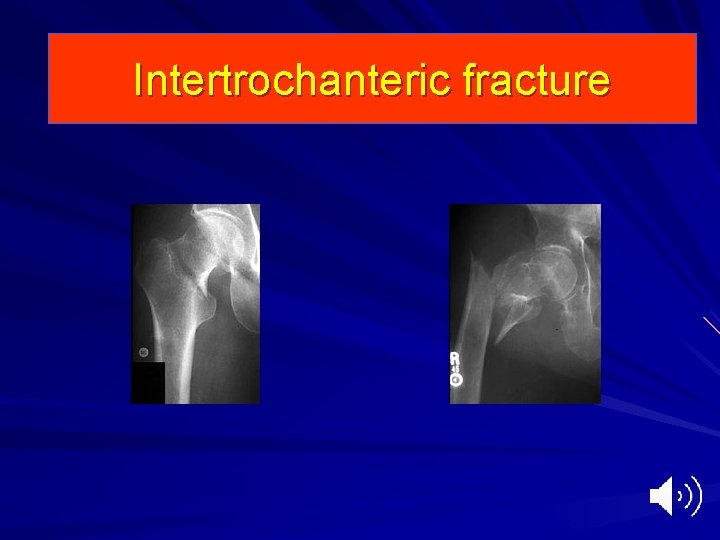
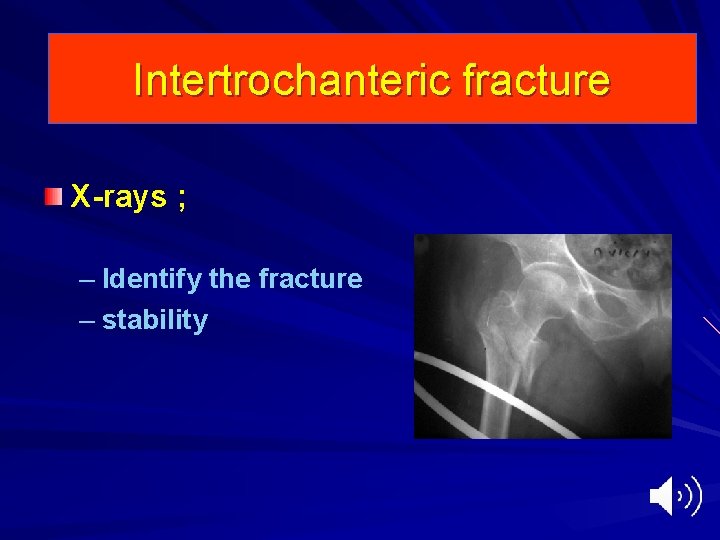
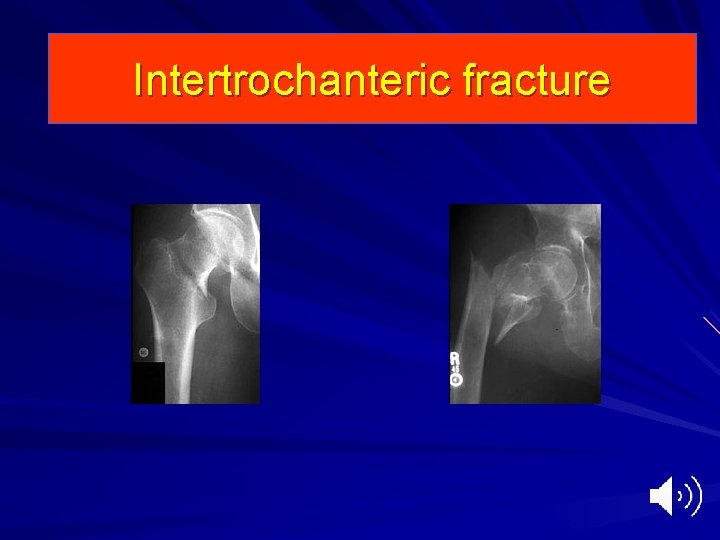
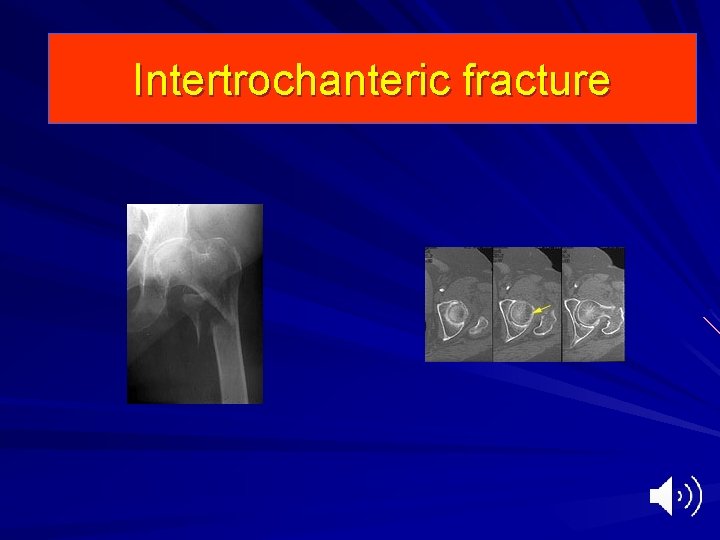
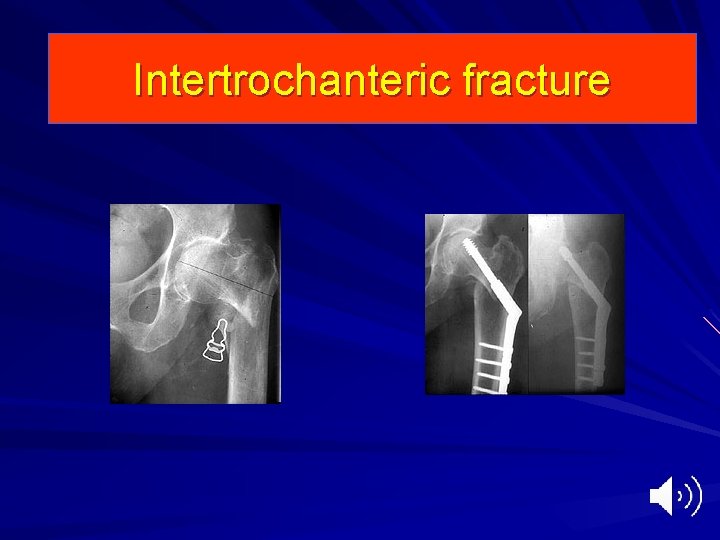
Intertrochanteric fracture X-rays ; – Identify the fracture – stability
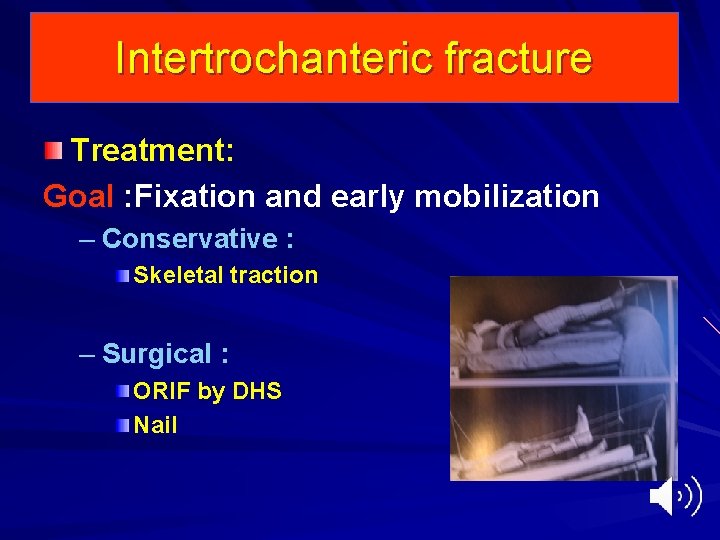
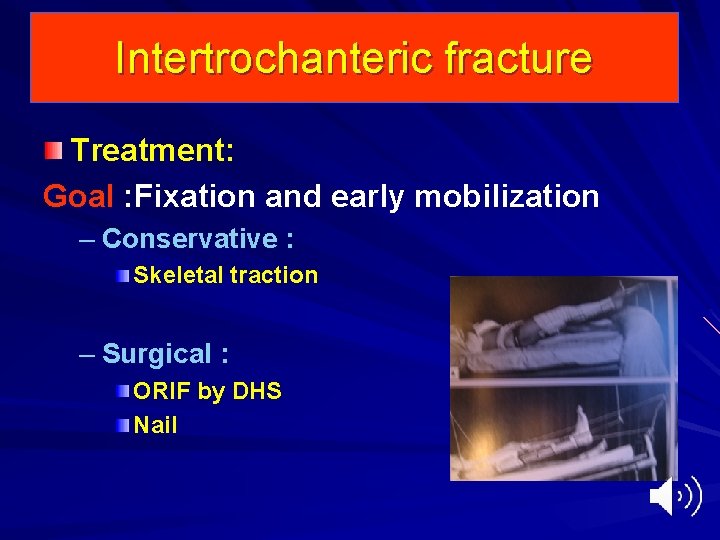
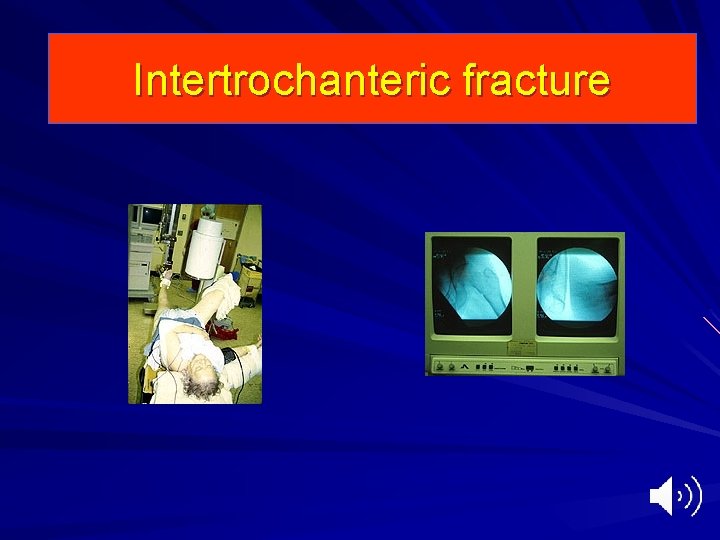
Intertrochanteric fracture Treatment: Goal : Fixation and early mobilization – Conservative : Skeletal traction – Surgical : ORIF by DHS Nail
Intertrochanteric fracture
Intertrochanteric fracture

Intertrochanteric fracture
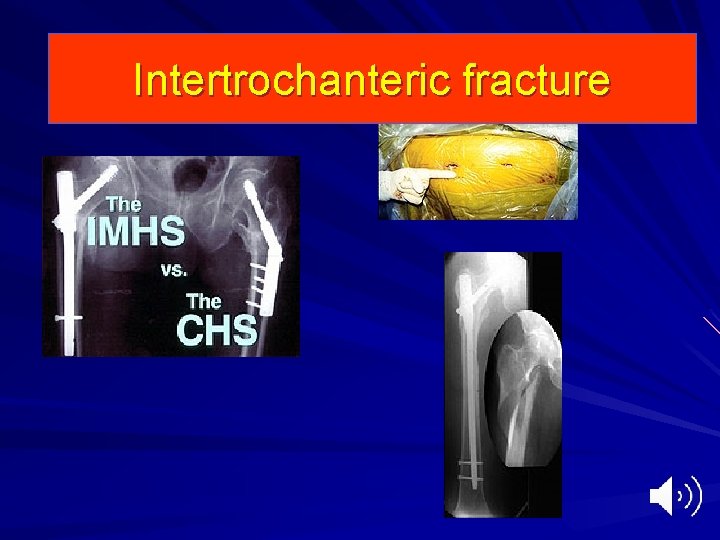
Intertrochanteric fracture
Intertrochanteric fracture Complications: – Conservative : Varus deformity Shortening Prolonged bed recumbency : – Bed sores – UTI – GIT – DVT
Intertrochanteric fracture Complications – Surgical : Failure of fixation Malunion ( varus deformity) Non-union Infection


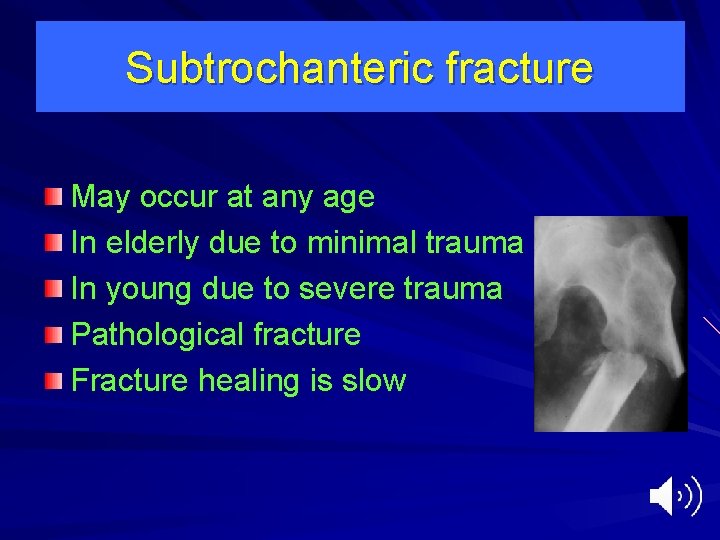
Subtrochanteric fracture May occur at any age In elderly due to minimal trauma In young due to severe trauma Pathological fracture Fracture healing is slow
Subtrochanteric fracture Clinical features: – Severe pain – Deformity, external rotation, shortening – Crepitus – Unable to walk
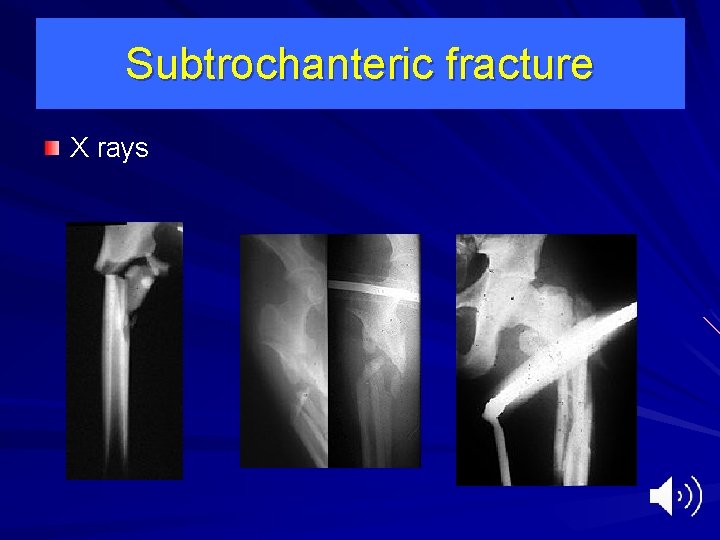
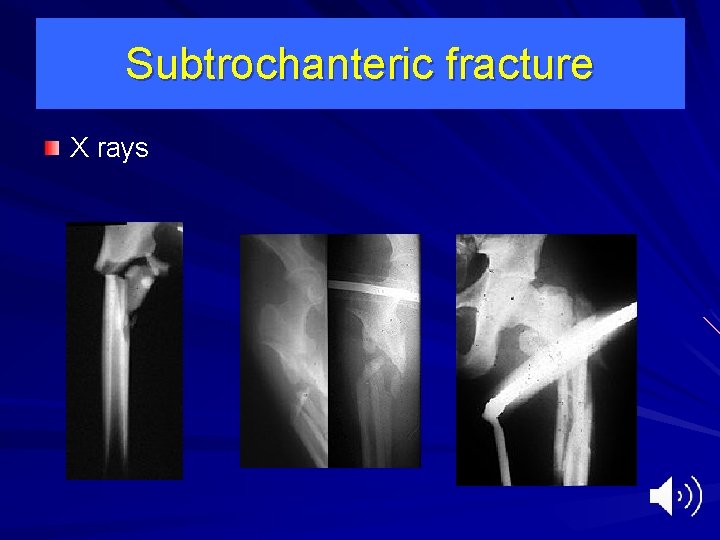
Subtrochanteric fracture X rays
Subtrochanteric fracture Treatment – Conservative: – Traction and cast brace
Subtrochanteric fracture Treatment – Surgical : Reduction and internal fixation by – DCS – Interlocking nail

Subtrochanteric fracture

Dislocation of the hip Hossam Elshafie, MD Prof. Orthopaedic surgery Alexandria University hospitals
Dislocation of the hip Definition: Complete loss of contact between opposing articular surfaces Subluxation Incomplete loss of contact between the articular surfaces
Dislocation of the hip Types: – Posterior – Anterior – central
Dislocation of the hip Posterior dislocation of the hip: – Mechanism of injury: – RTA, knee strike against dashboard – Fall from height – Pathologic anatomy – Anterior thrust on the knee with hip in adduction and flexion will through the head out of the acetabulum posteriorly , may be associated with posterior wall fracture of the acetabulum
Dislocation of the hip Posterior dislocation of the hip: – Clinical features; Deformity: The hip in position of flexion adduction and internal rotation. shortening Severe pain Restriction of mobility of the hip Examine for sciatic nerve palsy
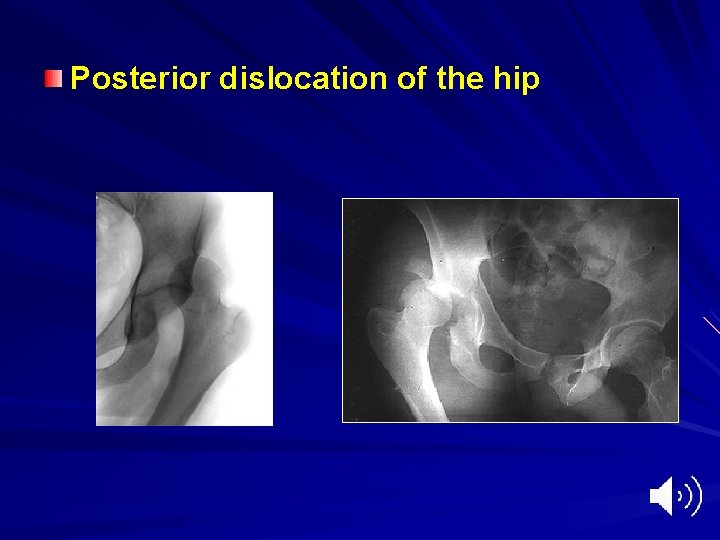
Dislocation of the hip Posterior dislocation of the hip: – X-rays: – Femoral head out of the acetabulum superiorly – Interruption of Shenton’s line – Lesser trochanter is not seen due to rotation – May be associated with post. Lip fracture of the acetabulum
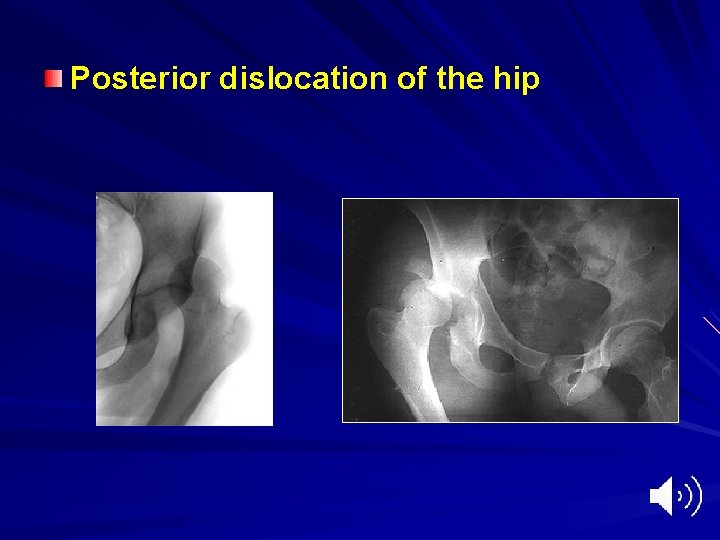
Posterior dislocation of the hip


Dislocation of the hip Posterior dislocation of the hip: – Treatment Should be reduced as soon as possible (why) Under GA Closed manipulation Reduction by gradual traction in the line of the femur (add, Int. Rot), gradual flexion hip and knee to 90 deg. , with minimal rotation, avoid abduction it may cause fracture of the NOF.
Dislocation of the hip Posterior dislocation of the hip: – Treatment Following reduction , traction is applied for 3 weeks Surgical treatment: – Unreduced dislocation – Associated fracture of the head of the femur or acetabulum
Dislocation of the hip Posterior dislocation of the hip: – Complications : Sciatic nerve injury Vascular injury (superior gluteal artery) Associated fracture (femoral head, acetabulum, femoral shaft) Avascular necrosis ( delayed reduction) Myositis ossificans Unreduced dislocation Osteoarthritis
Dislocation of the hip Anterior dislocation of the hip – Less common than posterior – Due to a posteriorly directed force on the femur with the hip in abduction and external rotation. – This will lever the head out anteriorly
Dislocation of the hip Anterior dislocation of the hip Types: Pubic Obturator perineal
Dislocation of the hip Anterior dislocation of the hip – Clinical features: The leg lies in external rotation, abduction and slight flexion Apparent lengthening The femoral head is palpable in the groin Loss of all movement Severe pain
Dislocation of the hip Anterior dislocation of the hip X-rays: Will show position of the head

Dislocation of the hip Anterior dislocation of the hip – Treatment Gentle traction with the knee and hip kept in flexion Then gentle internal rotation Assistance support the pelvis Followed by traction for 3 weeks
Dislocation of the hip Anterior dislocation of the hip – Complications ; – Avascular necrosis – Traumatic ossification
Dislocation of the hip Central dislocation of the hip – Mechanism of injury RTA Fall from a height A blow over the greater trochanter
Dislocation of the hip Central dislocation of the hip Pathological anatomy: There is disruption of the floor of the acetabulum The head is pushed inward through the acetabulum in to the pelvis

Dislocation of the hip Central dislocation of the hip – Treatment: – Skeletal traction through the tibia – May be combined with side traction through the trochanter – Maintained for 6 weeks – ORIF of fracture acetabulum
Dislocation of the hip Central dislocation of the hip – Complications – Severe bleeding – Shock – Soft tissue injury – Avascular necrosis – Osteoarthritis of the hip
Femoral shaft fracture Hossam Elshafie, MD Prof. Orthopaedics and traumatology Alexandria university hospitals
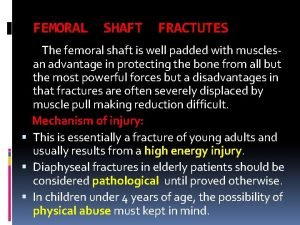
Femur Fractures Common injury due to major violent trauma 1 femur fracture/ 10, 000 people More common in people < 25 yr or >65 yr Femur fracture leads to reduced activity for 107 days, the average length of hospital stay is 25 days Motor vehicle, motorcycle, auto-pedestrian, aircraft, and gunshot wound accidents are most frequent causes Markedly displaced due to strong muscle pull May be open Elderly people pathological fracture
Anatomy Long tubular bone, anterior bow, flair at femoral condyles Blood supply – Metaphyseal vessels – Single nutrient artery in diaphysis enters through the linea aspera – Nutrient artery communicates with medullary arteries in intramedullary canal – Medullary arteries supply 2/3 of endosteal blood supply

Femoral shaft fracture Mechanism of injury: – Direct trauma as hit by a car Comminuted Segmental fr – Indirect ; fall from height Twisting (spiral) Angulation (oblique)
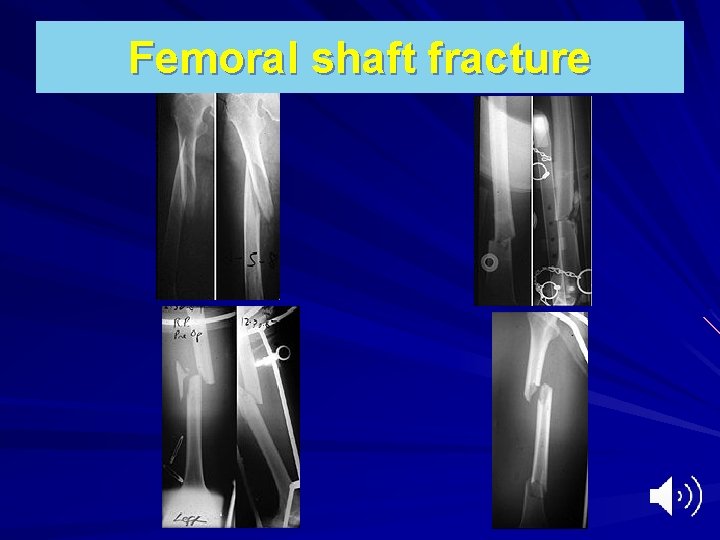
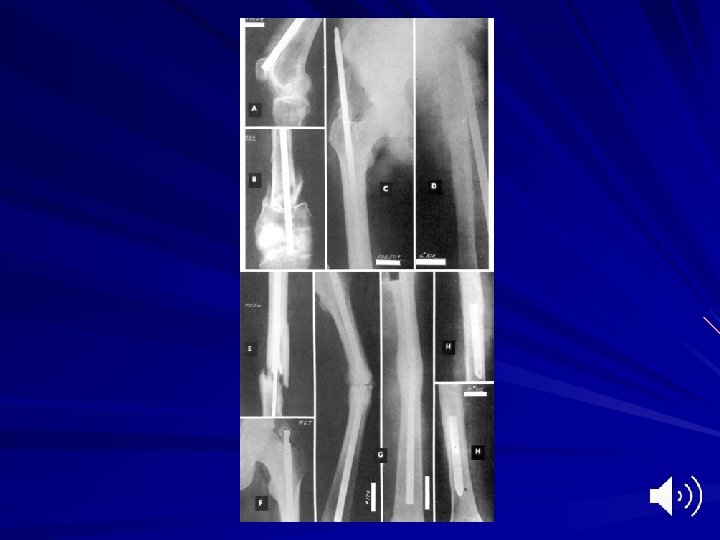
Femoral shaft fracture Pathological anatomy: – Fracture may be transverse, oblique, spiral, or comminuted or segmental – Fracture may be proximal, middle or in the distal third
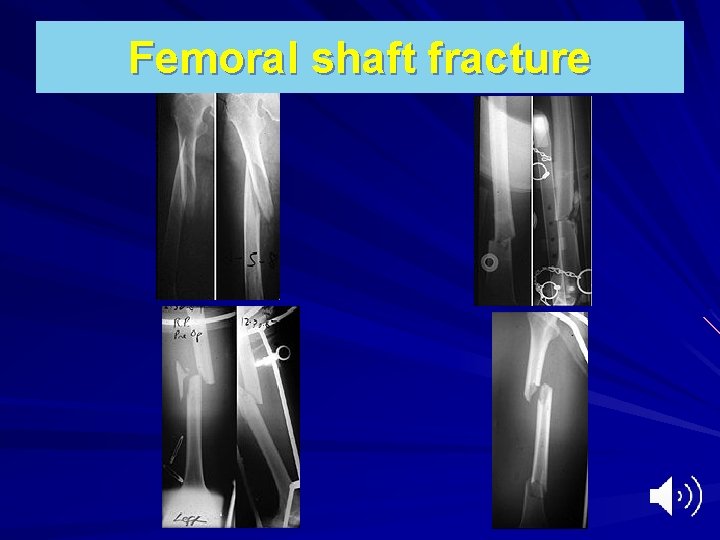
Femoral shaft fracture
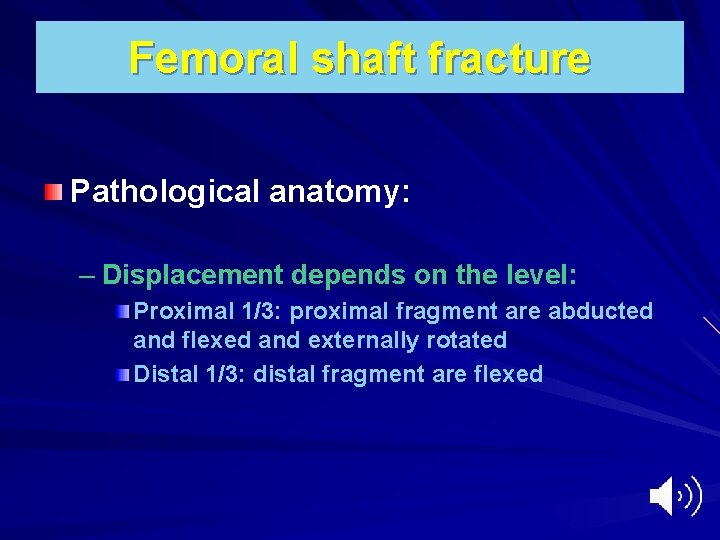
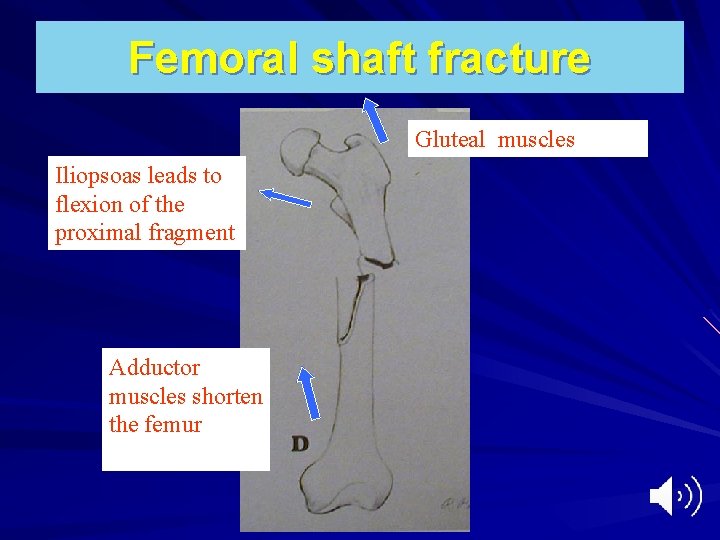
Femoral shaft fracture Pathological anatomy: – Displacement depends on the level: Proximal 1/3: proximal fragment are abducted and flexed and externally rotated Distal 1/3: distal fragment are flexed
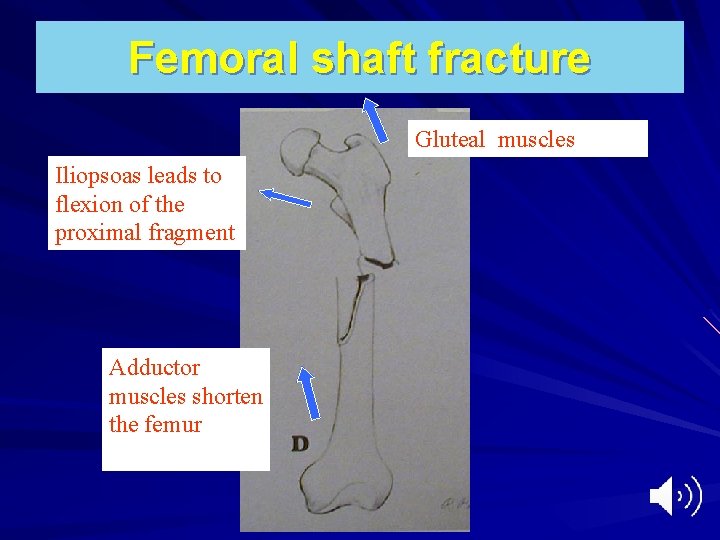
Femoral shaft fracture Gluteal muscles Iliopsoas leads to flexion of the proximal fragment Adductor muscles shorten the femur
Femoral shaft fracture Pathological anatomy: – Extensive soft tissue damage – Bleeding
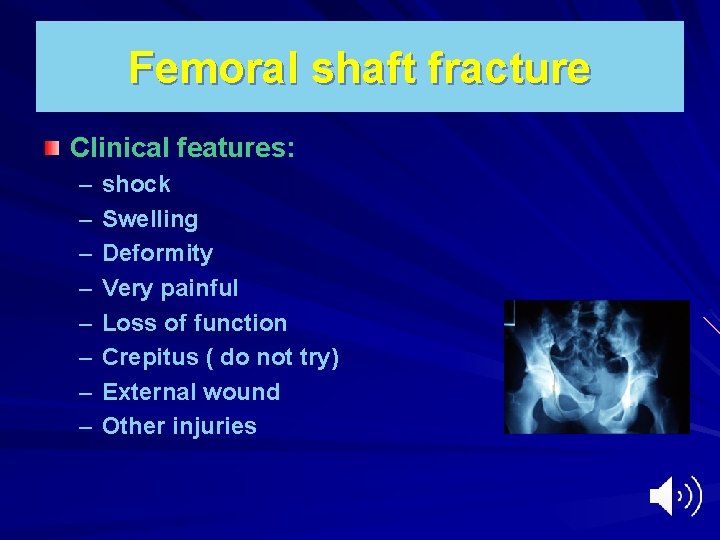
Femoral shaft fracture Clinical features: – – – – shock Swelling Deformity Very painful Loss of function Crepitus ( do not try) External wound Other injuries
Femoral shaft fracture Diagnosis ; – Immobilization of the limb in splint – X-Ray include both hip and knee joints – Two views (AP, Lateral)
Femoral shaft fracture Emergency treatment : – Treatment of shock A : airway and control of Cx spine B: breathing and oxygenation C; circulation and control of bleeding D: disability E: exposure and avoidance of hypothermia – Immobilization in a splint (Thomas splint) – Advantage of splintage: Relief pain Reduces bleeding Easy transfer – Treatment of other life threatening injuries

Femoral shaft fracture Definitive treatment: Early management is vital, specially multiple fractures Be aware of Fat embolism ARDS Multiple organ failure
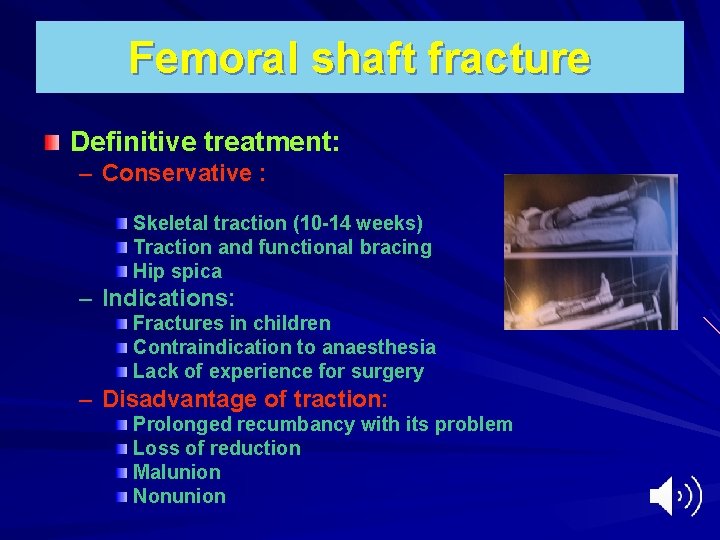
Femoral shaft fracture Definitive treatment: – Conservative : Skeletal traction (10 -14 weeks) Traction and functional bracing Hip spica – Indications: Fractures in children Contraindication to anaesthesia Lack of experience for surgery – Disadvantage of traction: Prolonged recumbancy with its problem Loss of reduction Malunion Nonunion
Traction Allows constant controlled force for initial stabilization of long bone fractures and aids in reduction during operative procedure Option for skeletal vs skin traction is case dependent
Skin Traction Limited force can be applied - generally not to exceed 10 lbs Can cause soft tissue problems especially in elderly or rheumatoid type skin Not as powerful when used during operative procedure for both length or rotational control
Skin Traction An option to provide temporary comfort in intertrochanteric hip fractures Max of 10 lbs of traction Watch closely for skin problems, especially in elderly or rheumatoid patients
Skeletal Traction More powerful with greater control than skin traction Permits pull up to 20% of body weight for the lower extremity Requires local anesthesia for pin insertion if patient is awake Preferred method of temporizing long bone, pelvic, and acetabular fractures until operative treatment can be performed
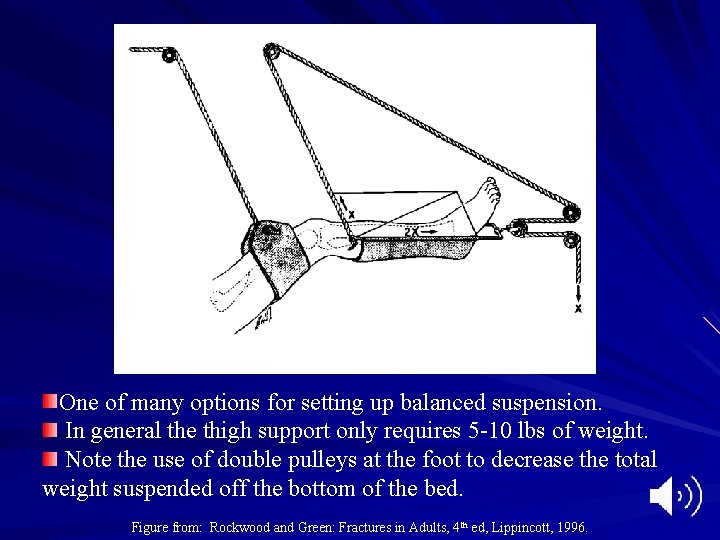
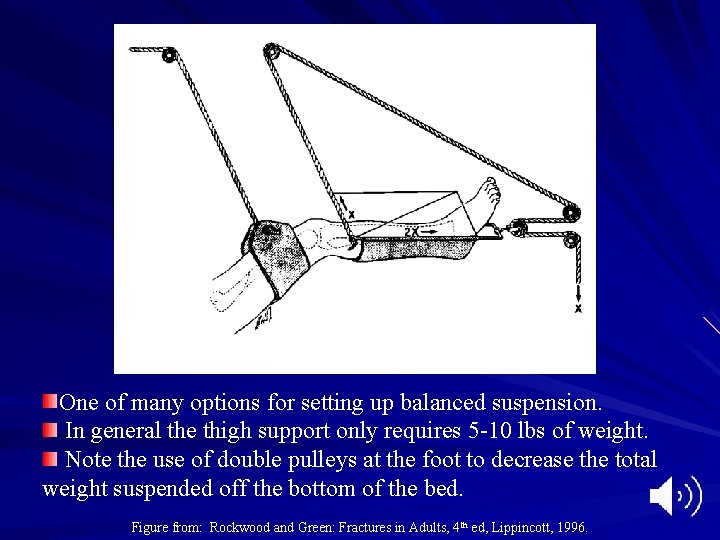
One of many options for setting up balanced suspension. In general the thigh support only requires 5 -10 lbs of weight. Note the use of double pulleys at the foot to decrease the total weight suspended off the bottom of the bed. Figure from: Rockwood and Green: Fractures in Adults, 4 th ed, Lippincott, 1996.
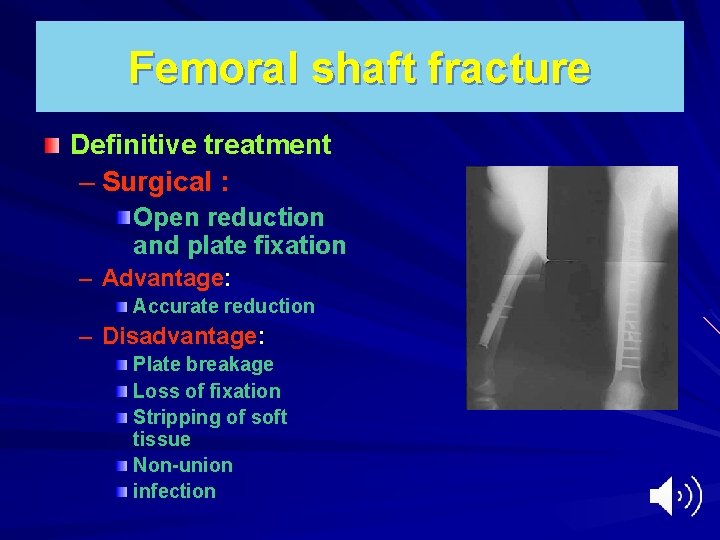
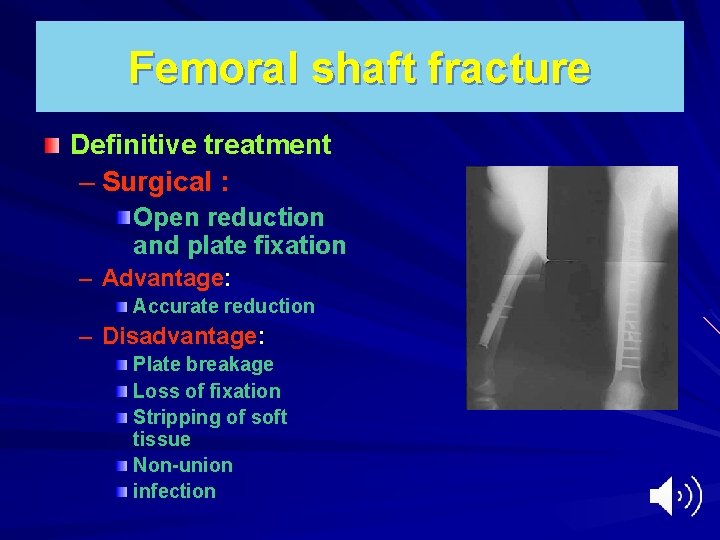
Femoral shaft fracture Definitive treatment – Surgical : Open reduction and plate fixation – Advantage: Accurate reduction – Disadvantage: Plate breakage Loss of fixation Stripping of soft tissue Non-union infection



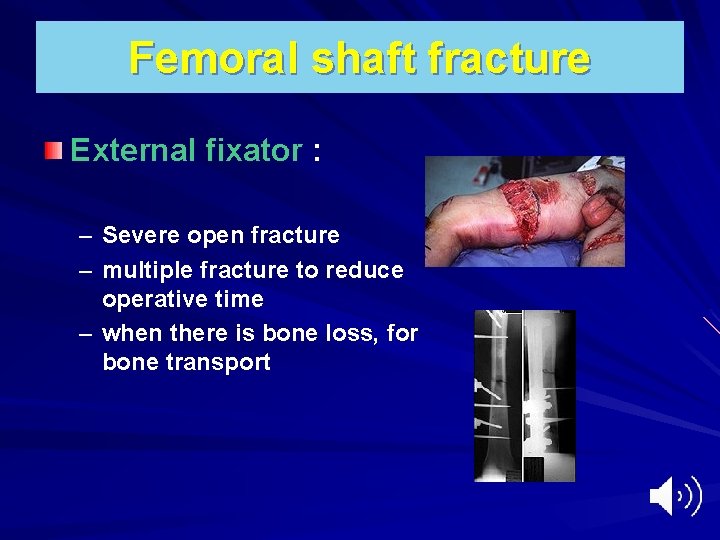
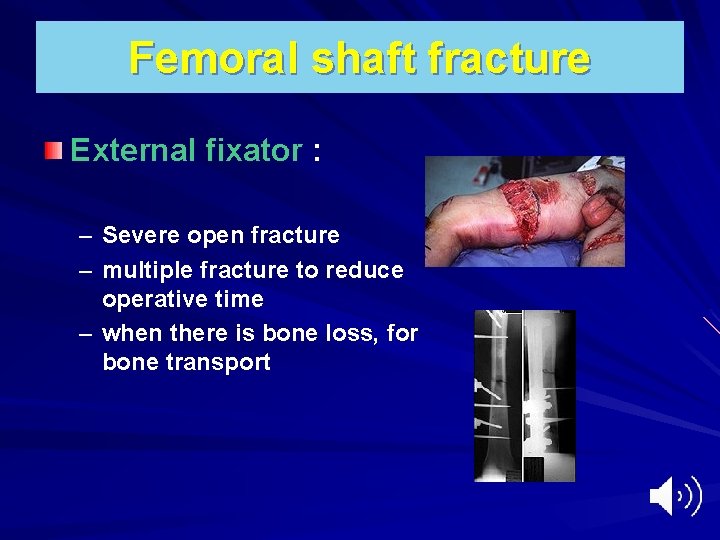
Femoral shaft fracture External fixator : – Severe open fracture – multiple fracture to reduce operative time – when there is bone loss, for bone transport

Femoral shaft fracture
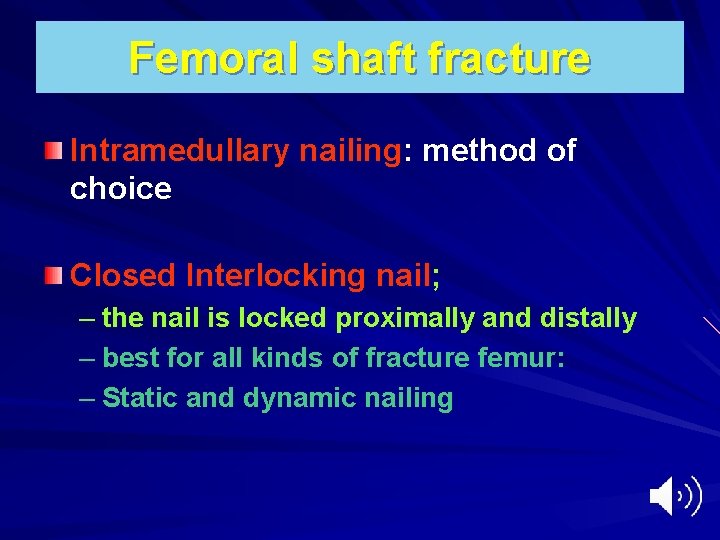
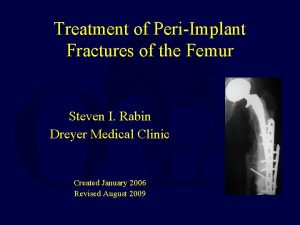
Femoral shaft fracture Intramedullary nailing: method of choice Closed Interlocking nail; – the nail is locked proximally and distally – best for all kinds of fracture femur: – Static and dynamic nailing
Femoral shaft fracture Interlocking nail – Advantages: – Suitable for comminuted fracture – It control rotation – Prevent collapse of the fracture – Allow early weight bearing in stable fr – Biological fixation ( closed fixation)
Interlocking nail Disadvantages: – demanding technique – exposure to irradiation. – Reaming may increase risk of fat embolism – Special equipment







Femoral shaft fracture Intramedullary nailing: Open unlocked nail: – Ordinary nail, Kuntscher nail. Indicated in proximal and middle 1/3 fracture It gives good fixation, cheap fixation, No need for special equipment

Disavantage: – Not suitable for distal 1/3 fracture and comminuted fractures – bleeding – Loss of fracture haematoma – Infection – Delayed union – Non-union
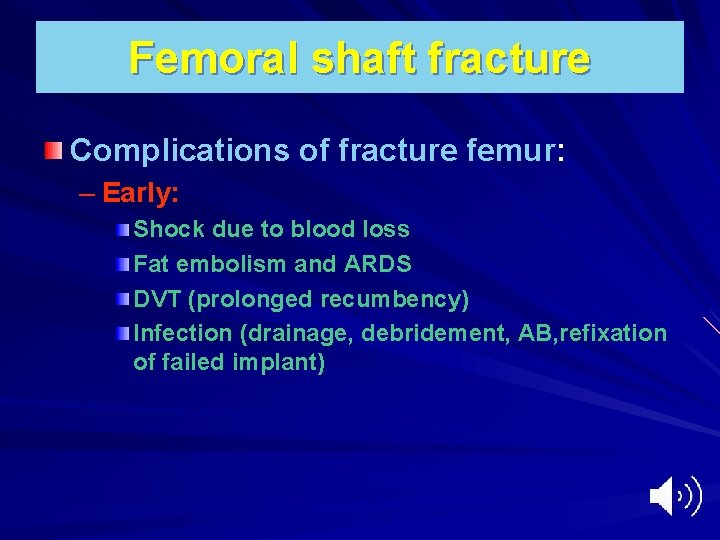
Femoral shaft fracture Complications of fracture femur: – Early: Shock due to blood loss Fat embolism and ARDS DVT (prolonged recumbency) Infection (drainage, debridement, AB, refixation of failed implant)
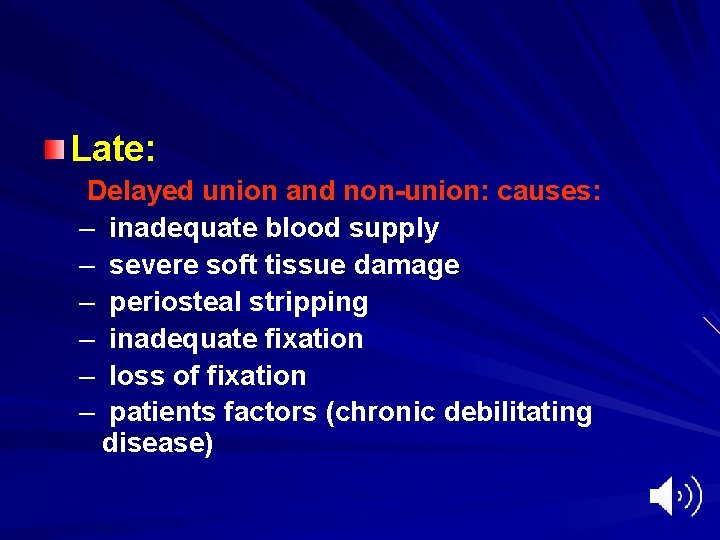
Late: Delayed union and non-union: causes: – inadequate blood supply – severe soft tissue damage – periosteal stripping – inadequate fixation – loss of fixation – patients factors (chronic debilitating disease)
 Femur femur
Femur femur Femoral canal structures
Femoral canal structures Femoral canal and femoral sheath
Femoral canal and femoral sheath Poem about hip hop
Poem about hip hop Hip to the hop to the hippity hop
Hip to the hop to the hippity hop Concentric fractures
Concentric fractures Concentric fracture glass definition
Concentric fracture glass definition Sternum and humerus
Sternum and humerus Virtual bone lab
Virtual bone lab Borders of femur
Borders of femur Olecranon fractures irving
Olecranon fractures irving Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Classification des fractures supracondyliennes
Classification des fractures supracondyliennes Disjonction symphyse pubienne classification
Disjonction symphyse pubienne classification Dry vs wet suction chest tube
Dry vs wet suction chest tube Bone cancer fractures
Bone cancer fractures Panfacial fractures sequencing
Panfacial fractures sequencing Classification of open fractures
Classification of open fractures Classification of open fractures
Classification of open fractures Open fracture treatment
Open fracture treatment Lisa kasman
Lisa kasman Types of fractures with pictures
Types of fractures with pictures Types of fractures with pictures
Types of fractures with pictures Ilioposas
Ilioposas Acetabulum ossification
Acetabulum ossification Types of glass fractures
Types of glass fractures Slidetodoc.com
Slidetodoc.com Fracture bois vert
Fracture bois vert Weber classification of ankle fractures
Weber classification of ankle fractures Pelvic extension
Pelvic extension Tubérosité naviculaire
Tubérosité naviculaire Ap pelvis grafisi
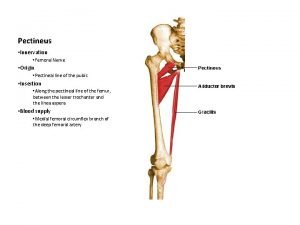
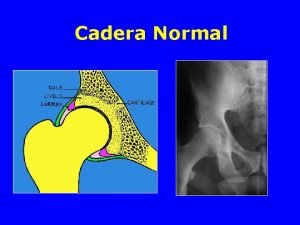
Ap pelvis grafisi Pectineus origin
Pectineus origin Rciu dysharmonieux fémur
Rciu dysharmonieux fémur Femur length
Femur length Equipo de traccion cutanea
Equipo de traccion cutanea Arco di shenton
Arco di shenton Spring ligament
Spring ligament Spinotuberositaire
Spinotuberositaire Sidération quadriceps
Sidération quadriceps Fracture de trélat et hoffa fémur
Fracture de trélat et hoffa fémur Orif with p&s
Orif with p&s Piriform fossa femur
Piriform fossa femur Borders of femur
Borders of femur Condyles of femur
Condyles of femur Osteosarcoma femur icd 10
Osteosarcoma femur icd 10 Jugular notch
Jugular notch Femur proximal übersetzung
Femur proximal übersetzung Icd 10 fraktur femur
Icd 10 fraktur femur Fractura trohanteriana
Fractura trohanteriana Bone tuberosity
Bone tuberosity Fémur
Fémur Fracture trochantéro-diaphysaire
Fracture trochantéro-diaphysaire Greater trochanter
Greater trochanter Patellar tendinitis moi
Patellar tendinitis moi Neck of femur
Neck of femur Ossa membri superioris kemikleri
Ossa membri superioris kemikleri Bryant's traction
Bryant's traction Femur hueso
Femur hueso Femur cast
Femur cast Subtrochanteric
Subtrochanteric Clou gamma long
Clou gamma long Femur projections
Femur projections Tibial torsion and femoral anteversion
Tibial torsion and femoral anteversion Bassini vs shouldice
Bassini vs shouldice Sublingual hernia
Sublingual hernia Difference between femoral and inguinal hernia
Difference between femoral and inguinal hernia Quad muscles action
Quad muscles action Types of drowning
Types of drowning Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Rom of hip abduction
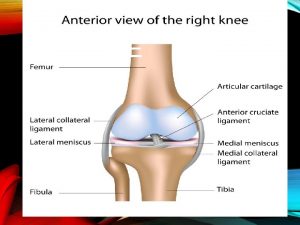
Rom of hip abduction Joint
Joint Hip joint type and subtype
Hip joint type and subtype Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Anatomy of the thigh hip groin and pelvis
Anatomy of the thigh hip groin and pelvis Hip and elbow dysplasia
Hip and elbow dysplasia Types of roof plan
Types of roof plan Hip and waist
Hip and waist Juxta femoral flush ligation
Juxta femoral flush ligation Volume de líquidos deficiente nanda
Volume de líquidos deficiente nanda Femoral triange
Femoral triange Screw home mechanism
Screw home mechanism Bony
Bony Arteria poplitea
Arteria poplitea Region femoral
Region femoral Pulso axilar
Pulso axilar Santral damar yolu
Santral damar yolu Eksternal oblik kenar
Eksternal oblik kenar Biceps femoral perro
Biceps femoral perro Biceps femoral origem e inserção
Biceps femoral origem e inserção Peroneo anterior
Peroneo anterior Atl fémorale
Atl fémorale Hesselbach's triangle
Hesselbach's triangle Pulsation of popliteal artery
Pulsation of popliteal artery Femoral pulse in child
Femoral pulse in child Pulso femoral
Pulso femoral Pulsos perifericos
Pulsos perifericos Deep venous system
Deep venous system Femoral endarterectomy
Femoral endarterectomy Left upper sternal border
Left upper sternal border Femoral approach
Femoral approach érythrose de déclivité
érythrose de déclivité Popliteal pulse
Popliteal pulse Dorsalis pedis artery supplies blood to
Dorsalis pedis artery supplies blood to Dorsal arch veins
Dorsal arch veins Nucleus medical term
Nucleus medical term Intermascular septa
Intermascular septa Femoral triangle contents
Femoral triangle contents Quad origin
Quad origin Anastomose cruciforme
Anastomose cruciforme Femoral navel
Femoral navel Dorsalis pedis pulse
Dorsalis pedis pulse Tricep braquial funcion
Tricep braquial funcion Groshong kateter
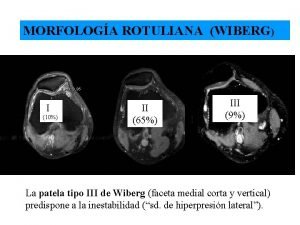
Groshong kateter Patela alta tipo 2 de wiberg
Patela alta tipo 2 de wiberg Muscle obturateur interne
Muscle obturateur interne Conducto de hunter
Conducto de hunter