Common femoral artery stenosis is surgery still the
- Slides: 28
Common femoral artery stenosis; is surgery still the best revascularization Richard F. Neville, MD Associate Director, INOVA Heart and Vascular Institute Vice Chairman, Department of Surgery Director, Vascular Services
Richard F. Neville, MD Disclosures Scientific Advisory Board: WL Gore Graftworx Cormatrix Tissue Analytics
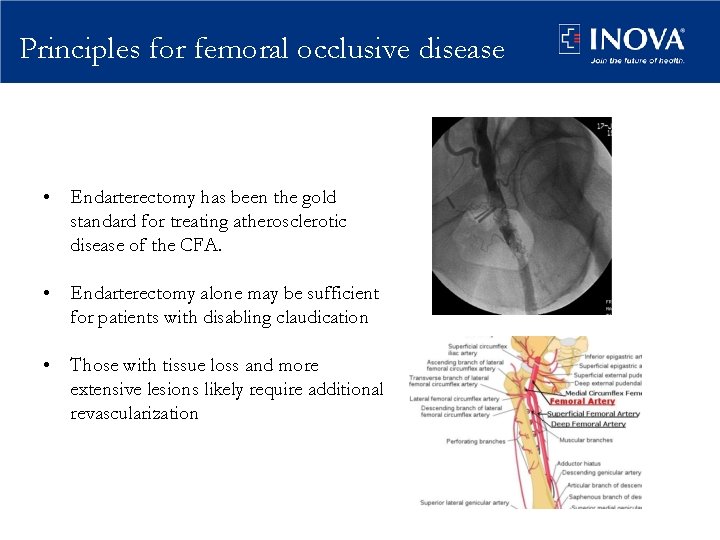
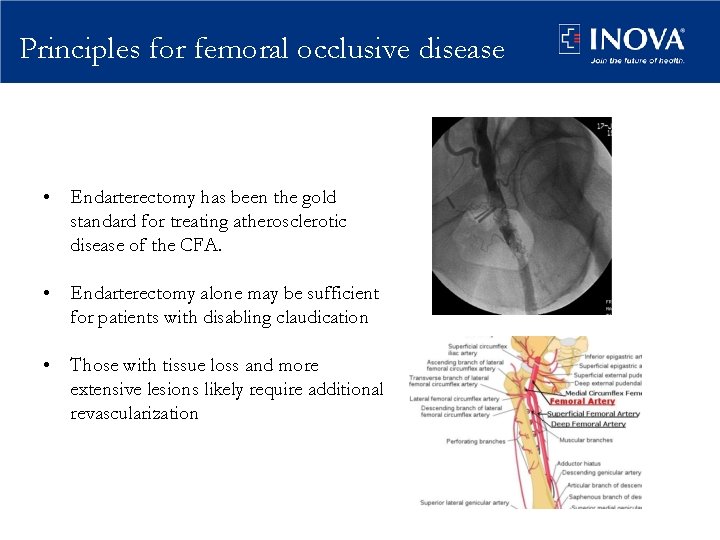
Principles for femoral occlusive disease • Endarterectomy has been the gold standard for treating atherosclerotic disease of the CFA. • Endarterectomy alone may be sufficient for patients with disabling claudication • Those with tissue loss and more extensive lesions likely require additional revascularization
CFA occlusive disease: contemporary results • 65 Common femoral thromboendarerectomy cases – Claudication 68%, – CLI 32% • 100% Technical success • 95% Hemodynamic success – ABI increase 0. 24 • 5% Complications • Patency – 1 year 93% – 5 year 91% – Assisted primary 100% • CHF – predictor of re-intervention Patel V, et al. J Vasc Surg 2008; 48(4): 872 -7
CFA endarterectomy • Primary patency 90 -96% to 8 years follow up – Assisted primary patency 100% • Amputation Free survival – 94% 10 years • Complications – Hematoma / seroma – Nerve injury – Pseudoaneurysm – Infection: Prior surgery, drain in place Ballotta E, et al. Surgery 2010; 147(2): 268 -274 Kechagias A, et al. World J Surg 2008; 32(1): 51 -54
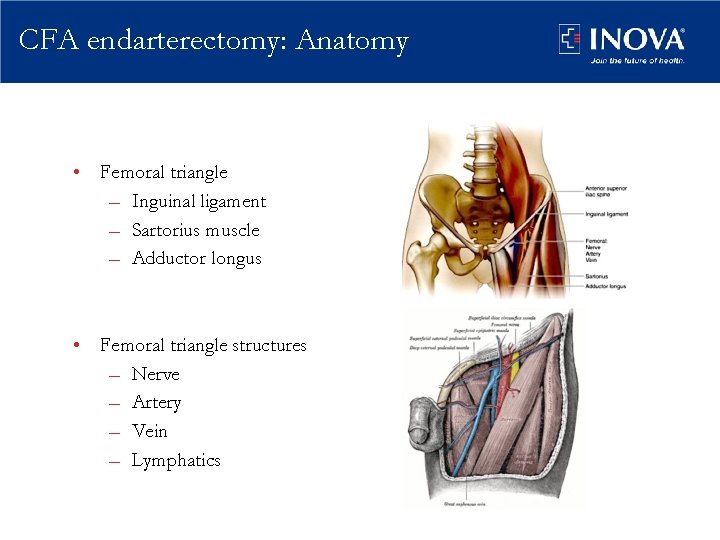
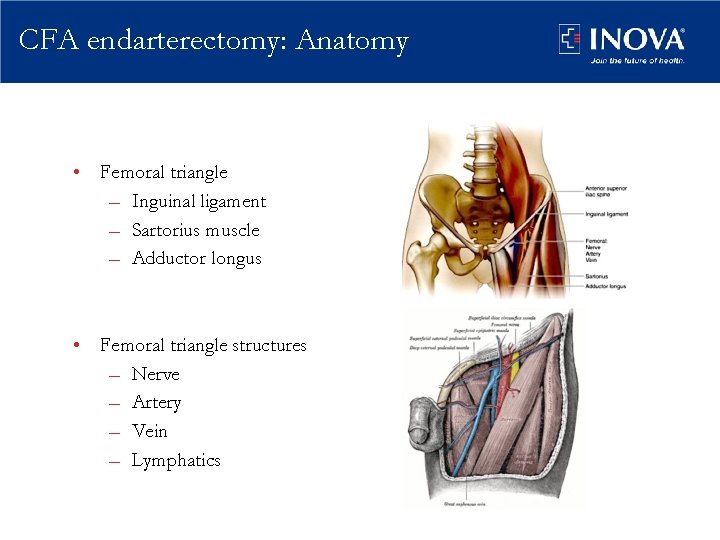
CFA endarterectomy: Anatomy • Femoral triangle – Inguinal ligament – Sartorius muscle – Adductor longus • Femoral triangle structures – Nerve – Artery – Vein – Lymphatics
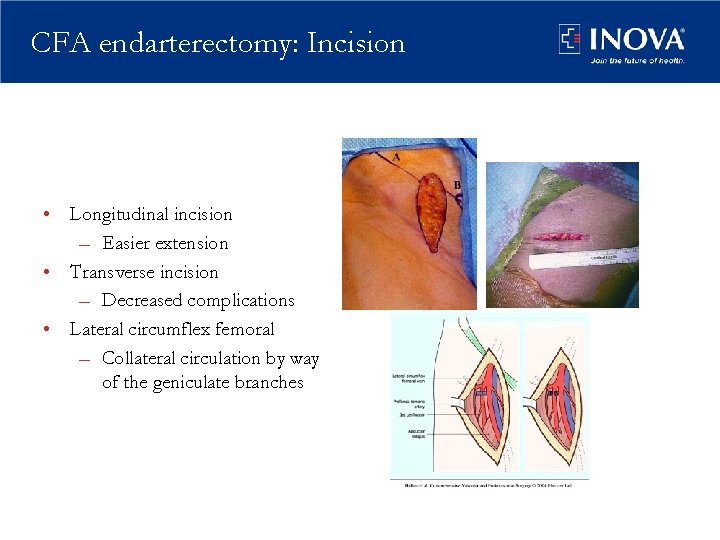
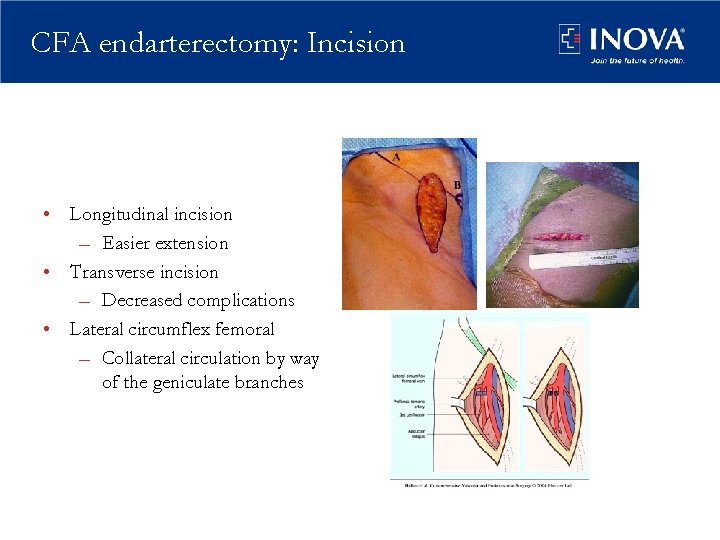
CFA endarterectomy: Incision • Longitudinal incision – Easier extension • Transverse incision – Decreased complications • Lateral circumflex femoral – Collateral circulation by way of the geniculate branches
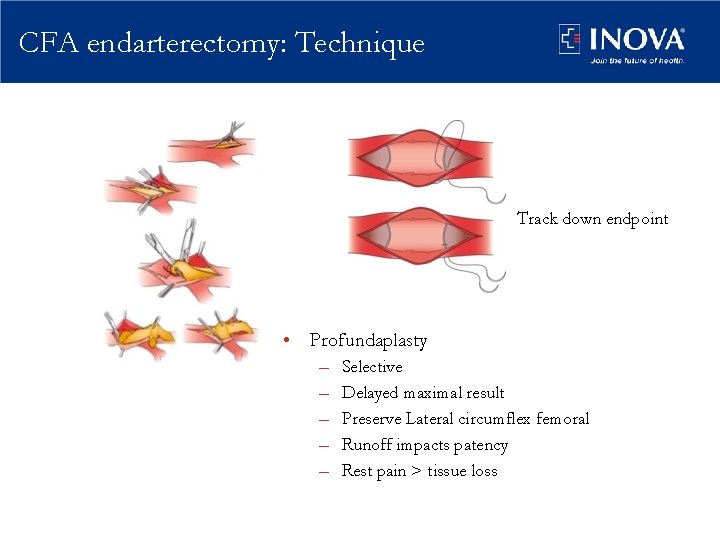
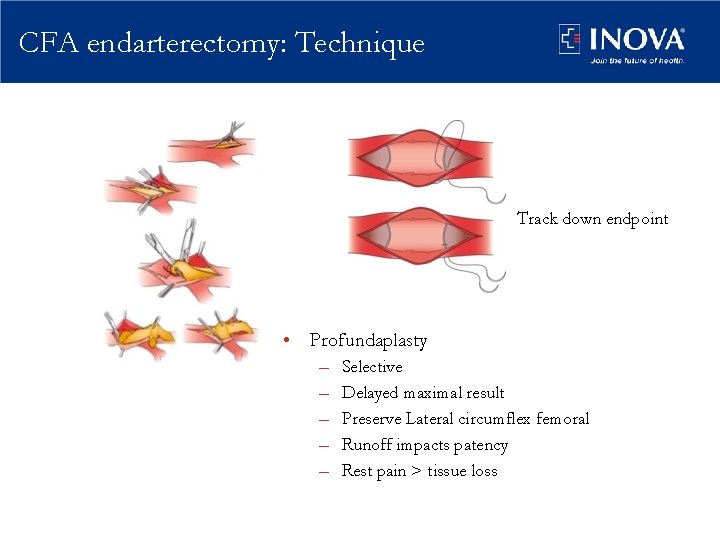
CFA endarterectomy: Technique Track down endpoint • Profundaplasty – – – Selective Delayed maximal result Preserve Lateral circumflex femoral Runoff impacts patency Rest pain > tissue loss
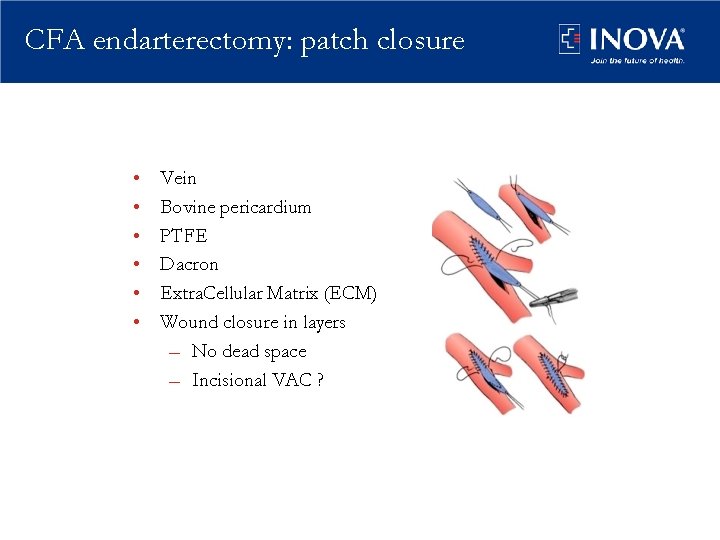
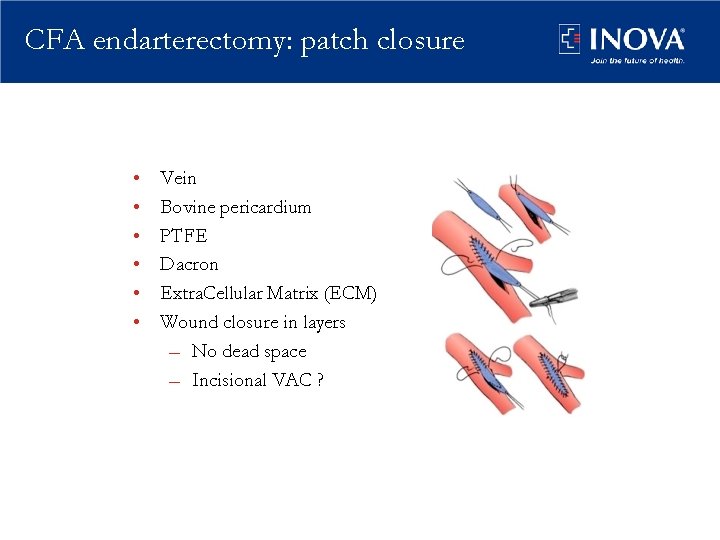
CFA endarterectomy: patch closure • • • Vein Bovine pericardium PTFE Dacron Extra. Cellular Matrix (ECM) Wound closure in layers – No dead space – Incisional VAC ?
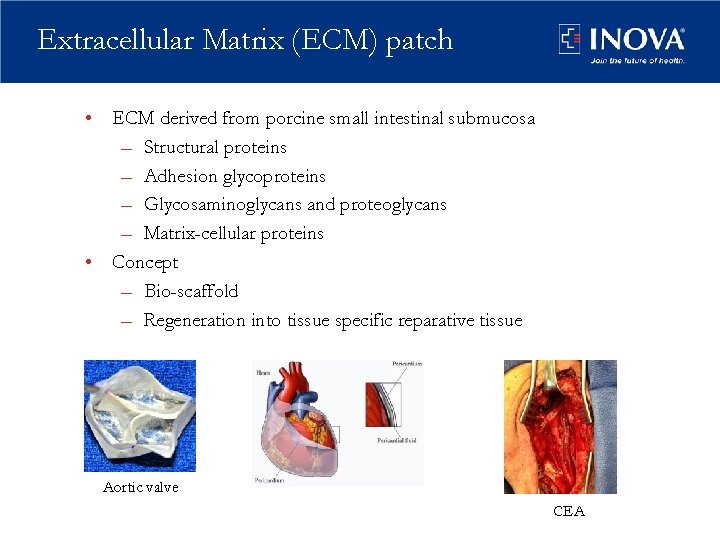
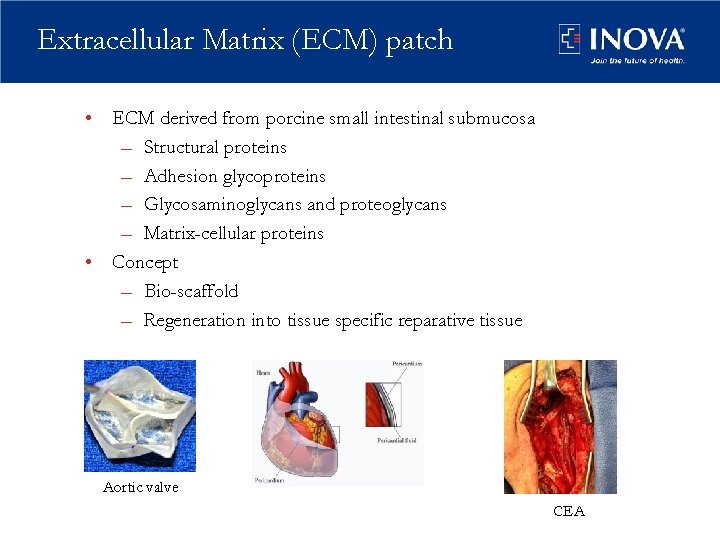
Extracellular Matrix (ECM) patch • ECM derived from porcine small intestinal submucosa – Structural proteins – Adhesion glycoproteins – Glycosaminoglycans and proteoglycans – Matrix-cellular proteins • Concept – Bio-scaffold – Regeneration into tissue specific reparative tissue Aortic valve CEA
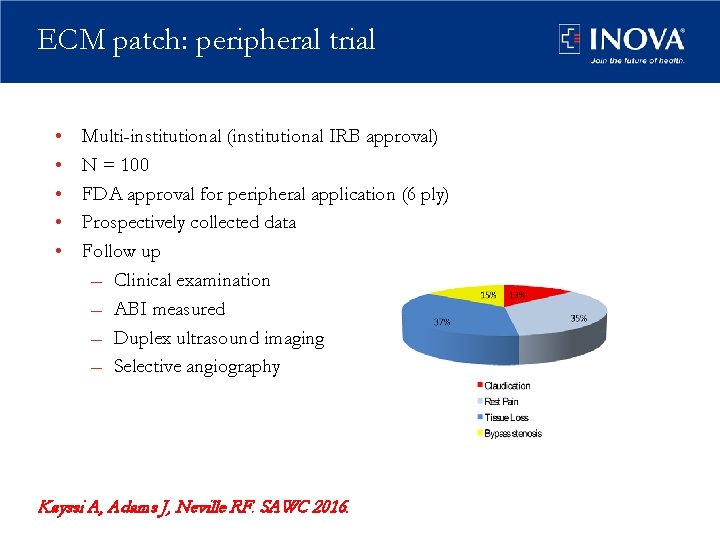
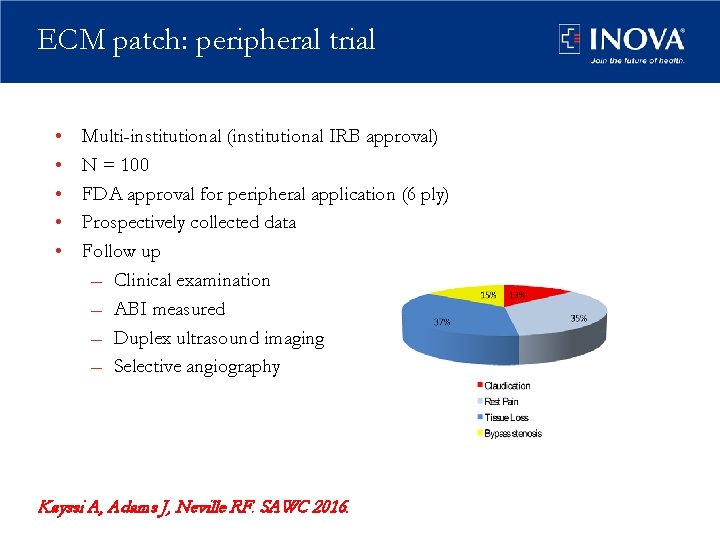
ECM patch: peripheral trial • • • Multi-institutional (institutional IRB approval) N = 100 FDA approval for peripheral application (6 ply) Prospectively collected data Follow up – Clinical examination – ABI measured – Duplex ultrasound imaging – Selective angiography Kayssi A, Adams J, Neville RF. SAWC 2016.
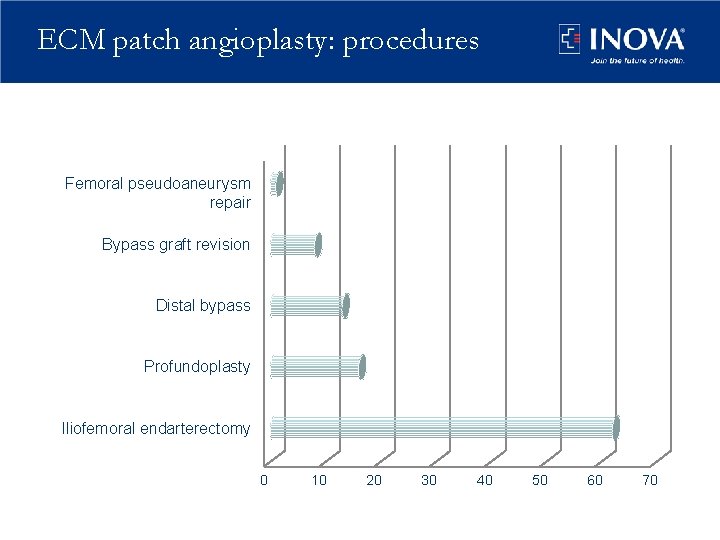
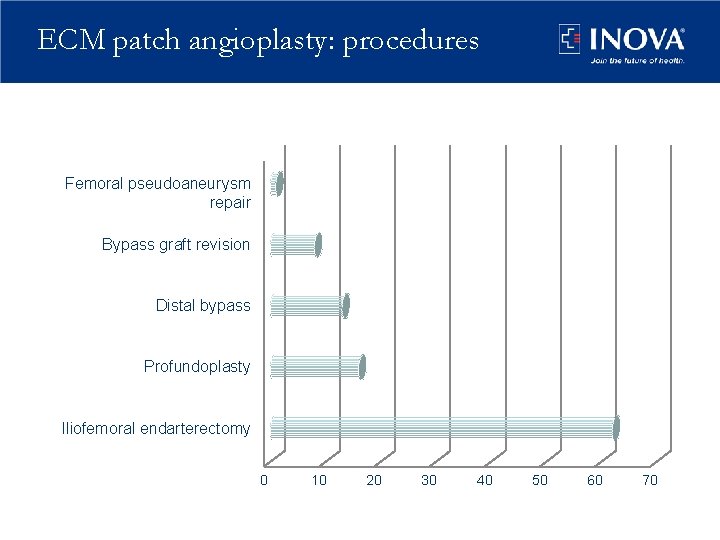
ECM patch angioplasty: procedures Femoral pseudoaneurysm repair Bypass graft revision Distal bypass Profundoplasty Iliofemoral endarterectomy 0 10 20 30 40 50 60 70
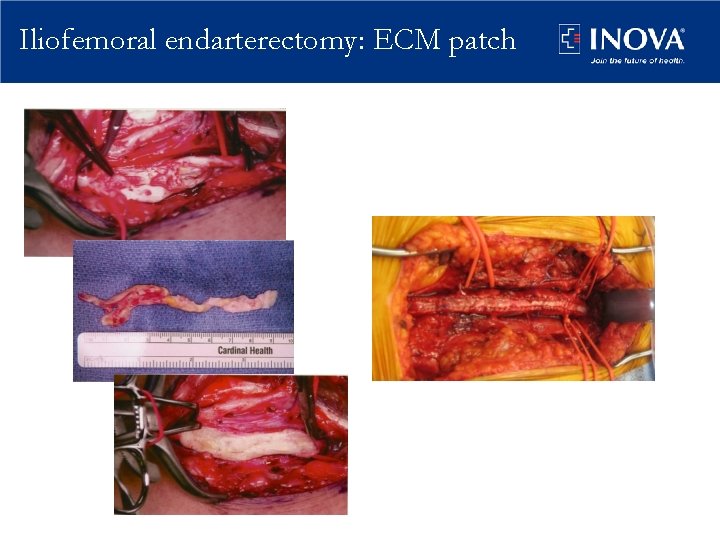
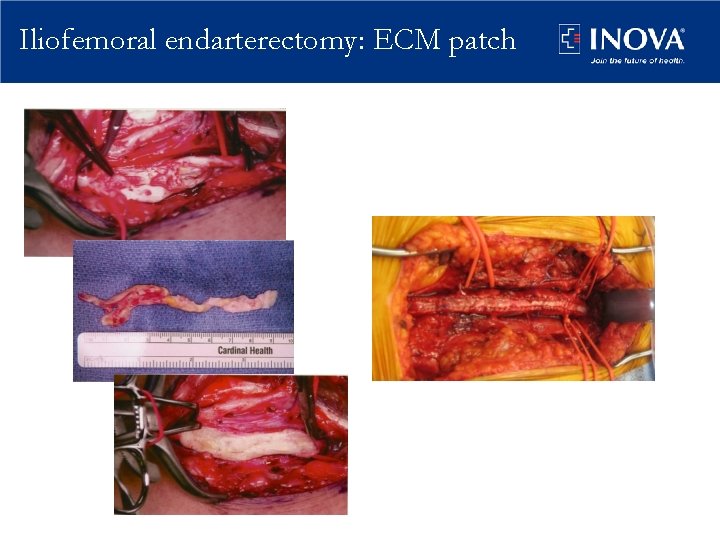
Iliofemoral endarterectomy: ECM patch
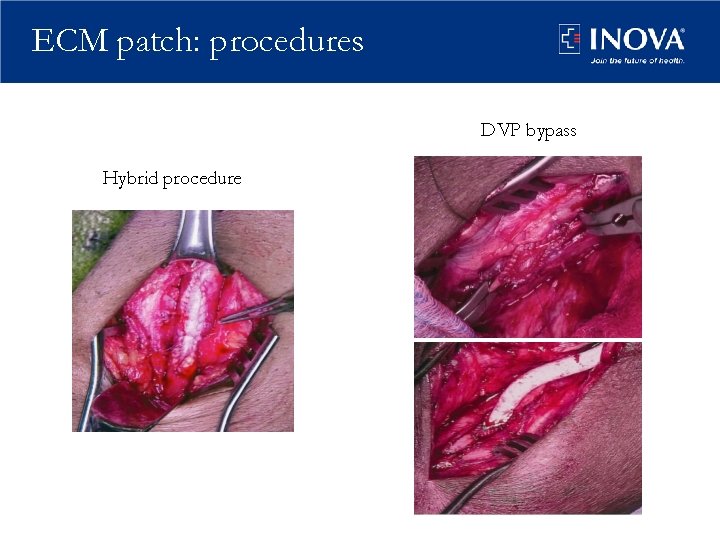
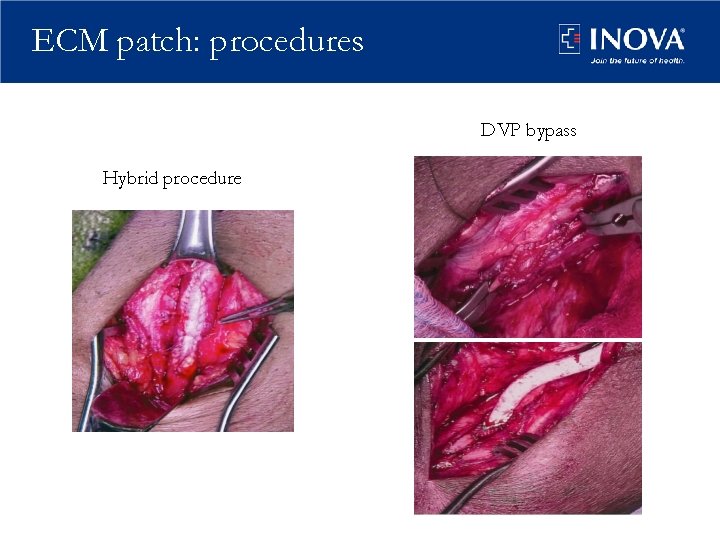
ECM patch: procedures DVP bypass Hybrid procedure
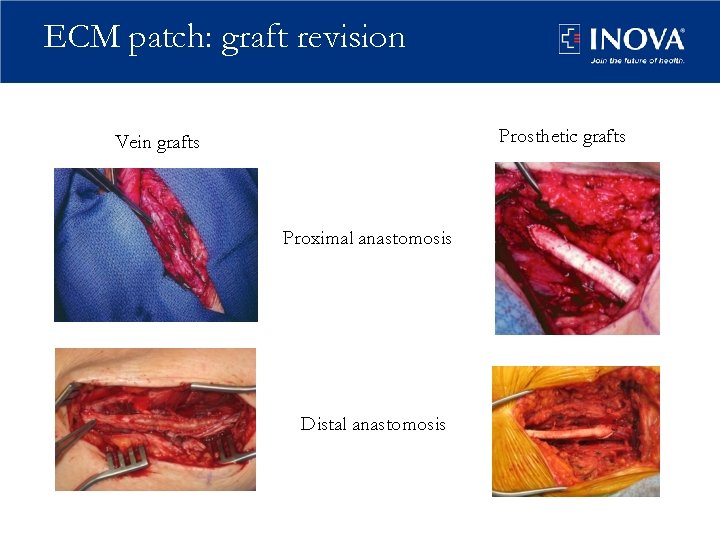
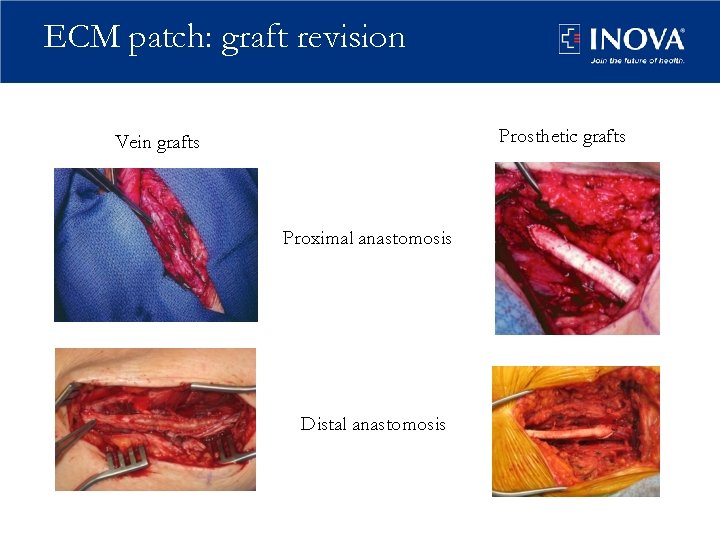
ECM patch: graft revision Prosthetic grafts Vein grafts Proximal anastomosis Distal anastomosis
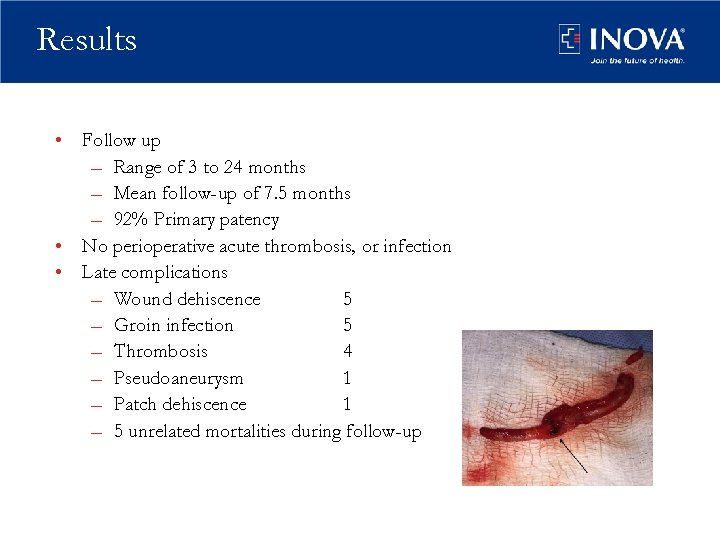
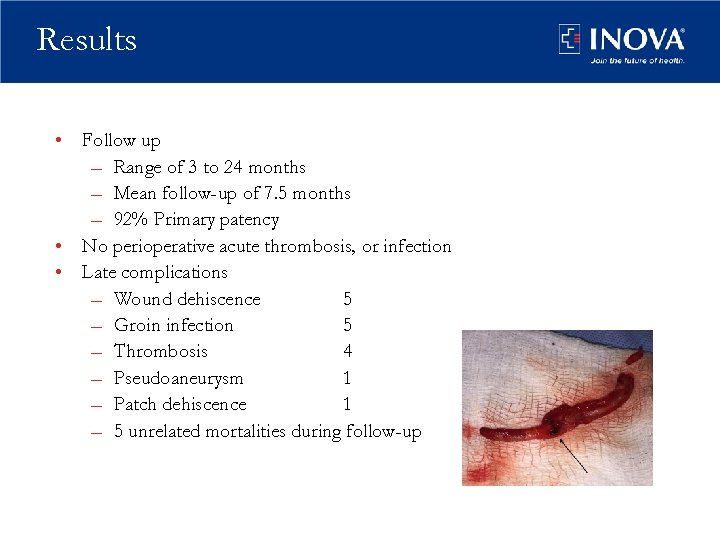
Results • Follow up – Range of 3 to 24 months – Mean follow-up of 7. 5 months – 92% Primary patency • No perioperative acute thrombosis, or infection • Late complications – Wound dehiscence 5 – Groin infection 5 – Thrombosis 4 – Pseudoaneurysm 1 – Patch dehiscence 1 – 5 unrelated mortalities during follow-up
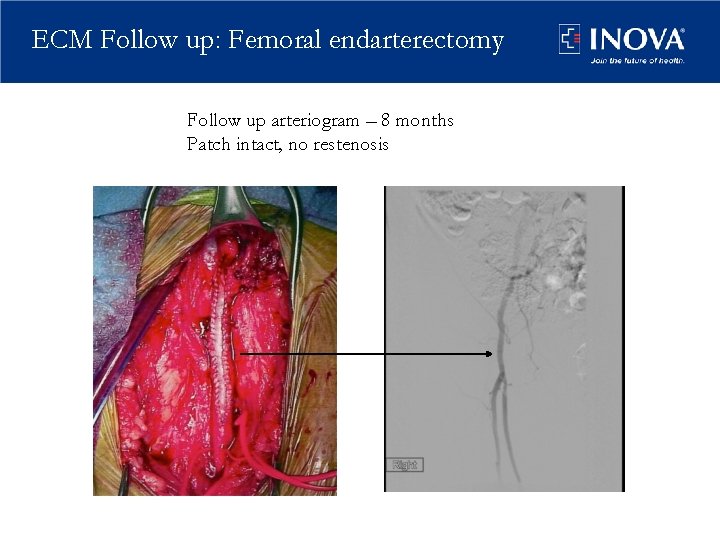
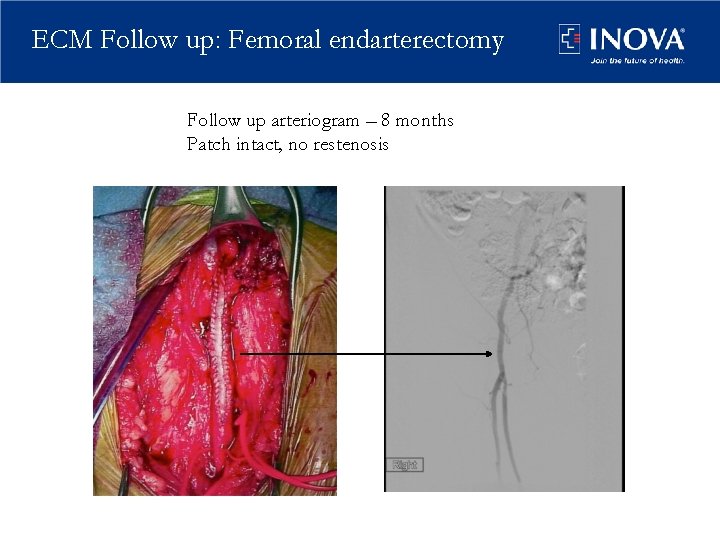
ECM Follow up: Femoral endarterectomy Follow up arteriogram – 8 months Patch intact, no restenosis
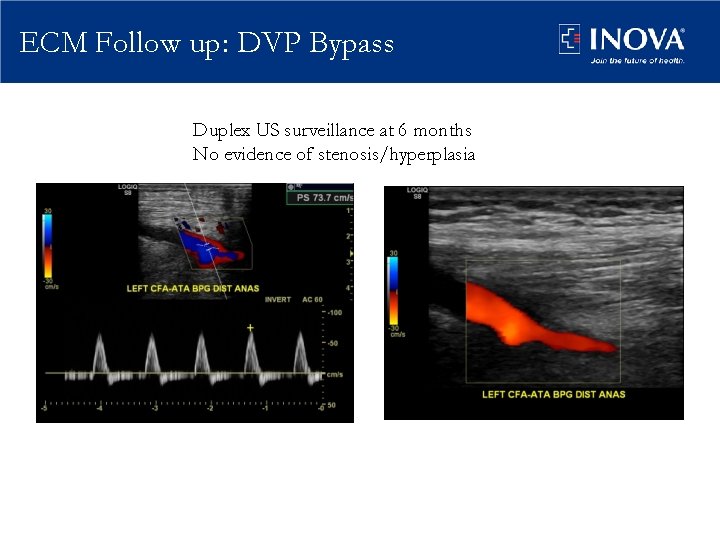
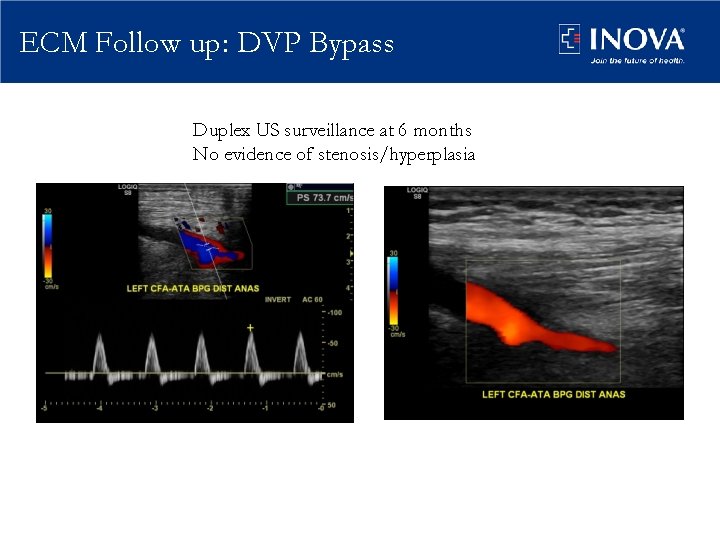
ECM Follow up: DVP Bypass Duplex US surveillance at 6 months No evidence of stenosis/hyperplasia
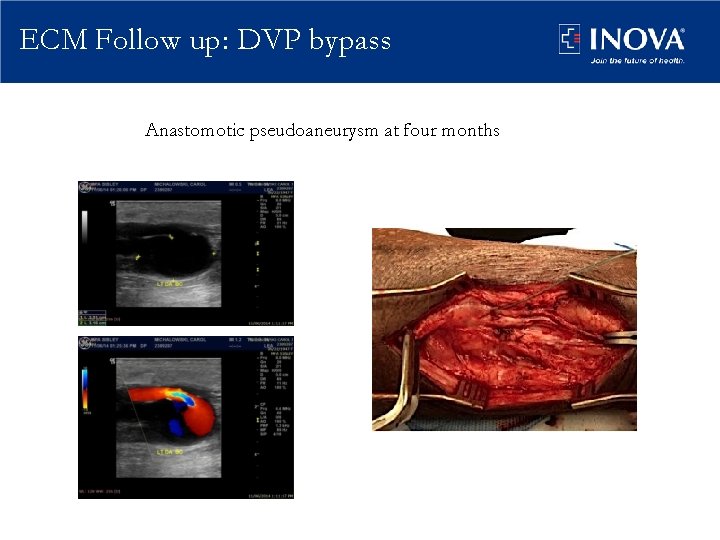
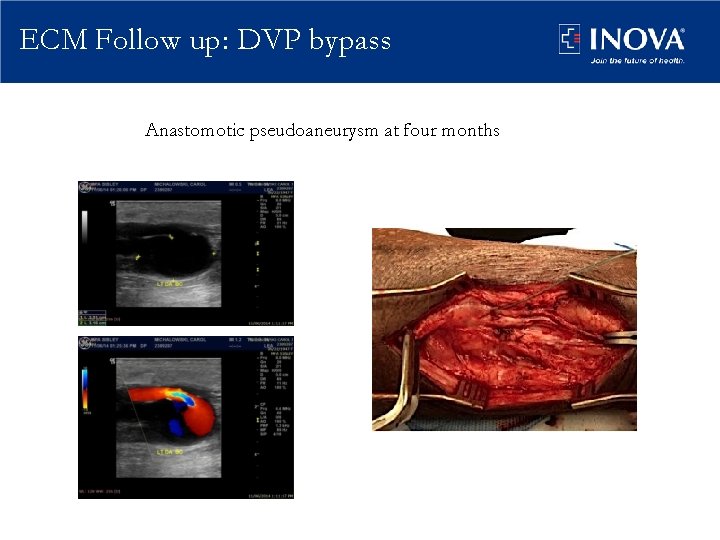
ECM Follow up: DVP bypass Anastomotic pseudoaneurysm at four months
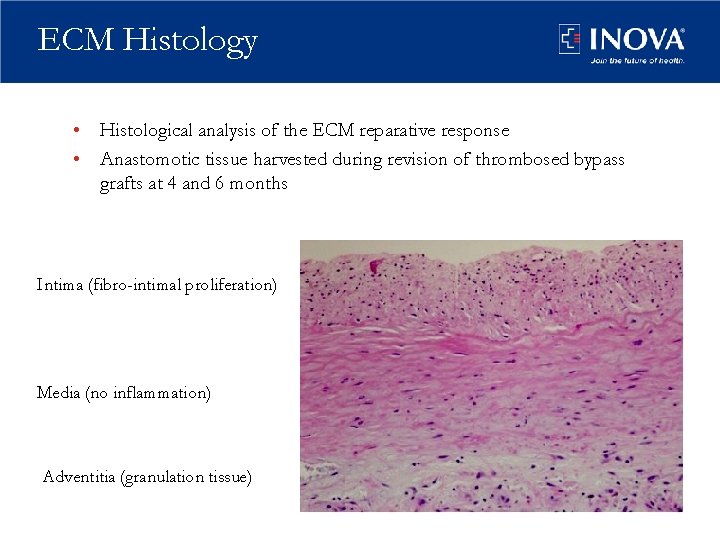
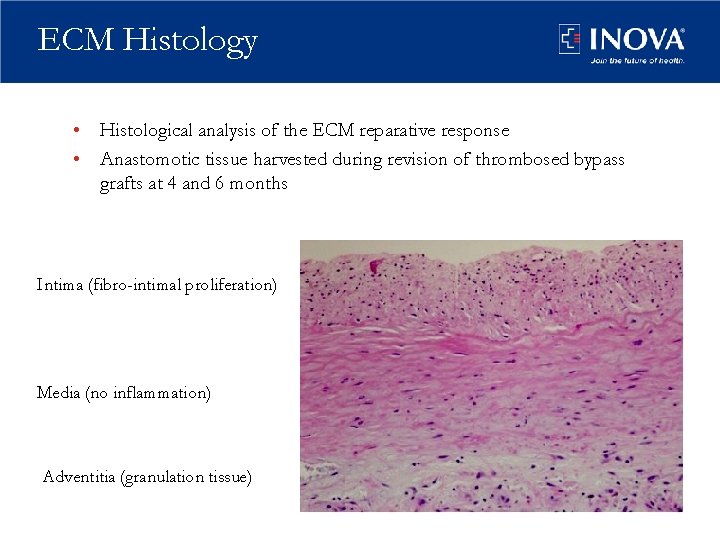
ECM Histology • Histological analysis of the ECM reparative response • Anastomotic tissue harvested during revision of thrombosed bypass grafts at 4 and 6 months Intima (fibro-intimal proliferation) Media (no inflammation) Adventitia (granulation tissue)
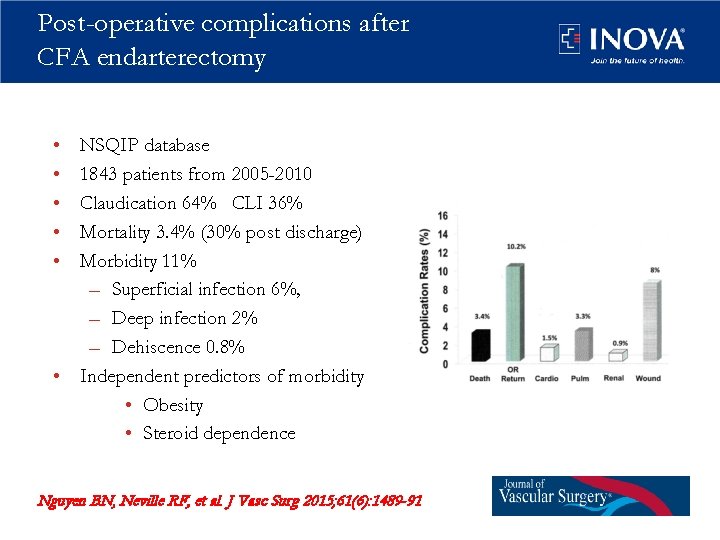
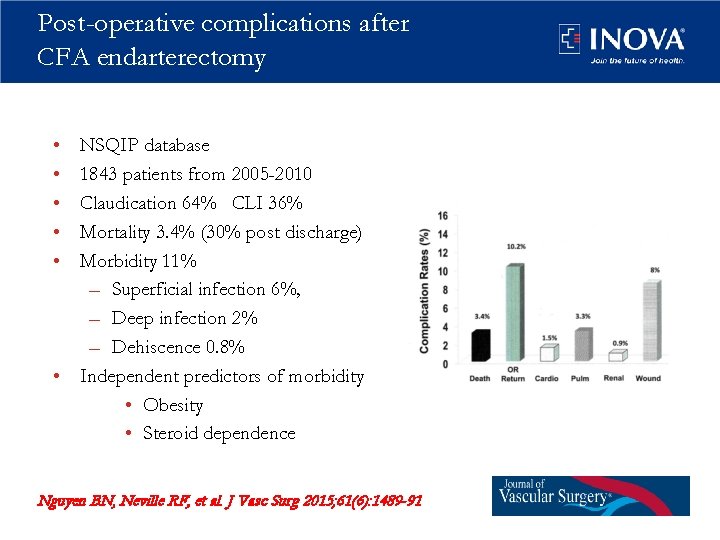
Post-operative complications after CFA endarterectomy • • • NSQIP database 1843 patients from 2005 -2010 Claudication 64% CLI 36% Mortality 3. 4% (30% post discharge) Morbidity 11% – Superficial infection 6%, – Deep infection 2% – Dehiscence 0. 8% • Independent predictors of morbidity • Obesity • Steroid dependence Nguyen BN, Neville RF, et al. J Vasc Surg 2015; 61(6): 1489 -91
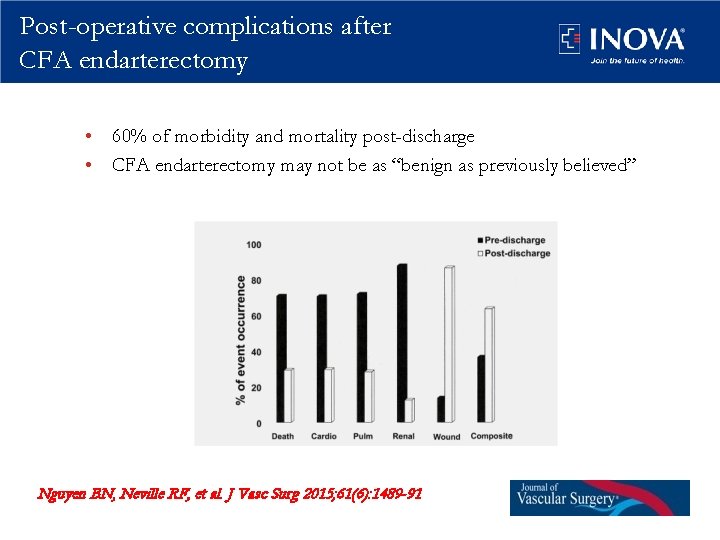
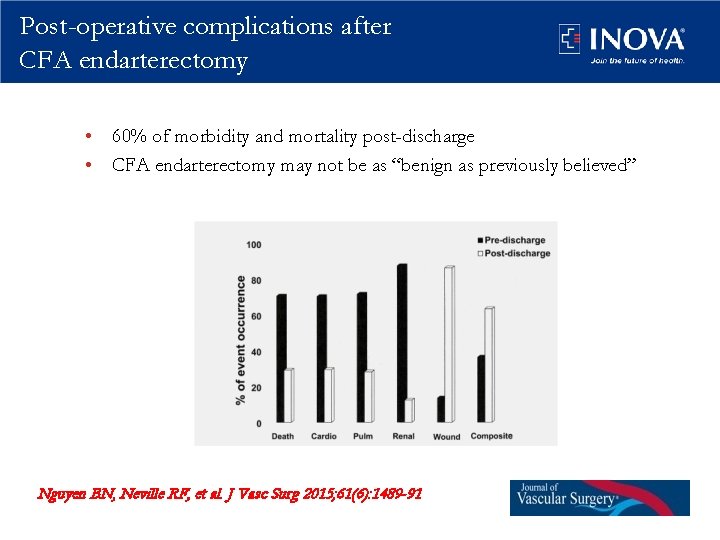
Post-operative complications after CFA endarterectomy • 60% of morbidity and mortality post-discharge • CFA endarterectomy may not be as “benign as previously believed” Nguyen BN, Neville RF, et al. J Vasc Surg 2015; 61(6): 1489 -91
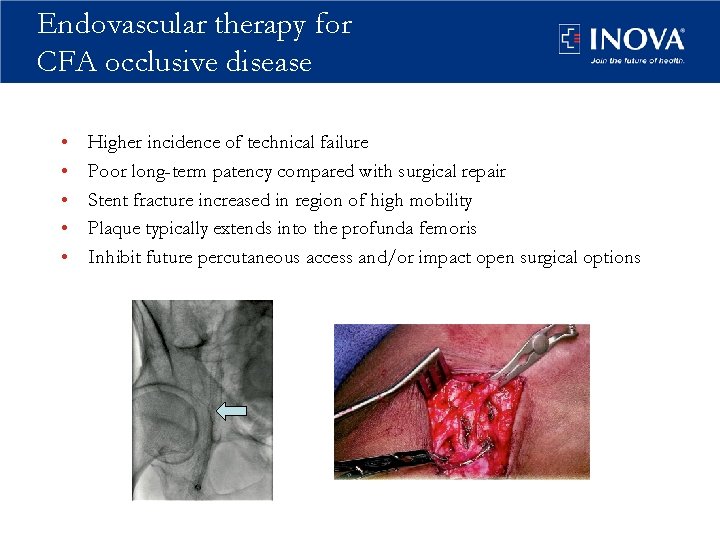
Endovascular therapy for CFA occlusive disease • • • Higher incidence of technical failure Poor long-term patency compared with surgical repair Stent fracture increased in region of high mobility Plaque typically extends into the profunda femoris Inhibit future percutaneous access and/or impact open surgical options
Endovascular therapy for CFA occlusive disease: success? • Ahn, et al (DFW Vascular Group, Dallas, Texas) – 61 patients – 19% procedural failures – 33% thrombosis at 12 months • Bonvini et al (Bad Krozingen, Germany; Geneva, Switzerland) – 360 patients – 37% with stenting due to suboptimal PTA – 28% restenosis at 1 year • Paris et al(Ochsner Clinic) – 29 lesions treated with CFA stenting (10% for hemorrhage) – 100% procedural success – 93% with symptomatic improvement in follow up
Should we change the paradigm for treatment of CFA occlusive disease? • The number of study limitations must be addressed. • Although 1 -year results are often acceptable, the long-term outcomesare not as promising. • Kaplan-Meier curves for restenosis and TLR reveal a significant drop-off in patency after 1 year, with frequent need for re-intervention. • 5 -year primary patency is approximately 50%. These long-term results are inferior to those achieved with endarterectomy and patch angioplasty. John R. Laird, MD, J Am Coll Cardiol. 2011; 58(8): 799 -800.
Hybrid procedures: CFA endaterectomy with endovascular Rx • • • Femoral endarterectomy with proximal/distal endovascular revascularization Multilevel revascularization through one point Iliac endovascular interventions possible Femoral-popliteal interventions possible Decrease in morbidity and Length of Stay Doslouglu H, et al, Vasc Endovasc Surg Sharafuddin MJ, et al. Vasc Endovasc Surg Chang RW, et al. J Vasc Surg.
Summary: CFA endarterectomy in current vascular practice • Common femoral endarterectomy remains the “gold standard” for femoral stenosis – Liberal use of profundaplasty – Liberal use of patch closure – ECM material • Favorable healing, reparative characteristics • Further clinical and basic research is warranted • Hybrid procedures are increasing • Role for endovascular therapy – Patient related: Morbidly obese, infected groin, steroid use – Lesion related: focal, not involving the PFA, thrombus – Device choice: PTA, avoid stenting, Atherectomy/debulking?
Thank you
 Subsartorial canal
Subsartorial canal Femoral triangle contents
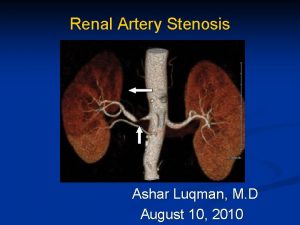
Femoral triangle contents Artery stenosis
Artery stenosis Pyloric stenosis adults treatment
Pyloric stenosis adults treatment Termination of femoral artery
Termination of femoral artery Profunda artery
Profunda artery Popliteal fossa pulse
Popliteal fossa pulse Popliteal pulsation
Popliteal pulsation Femoral artery
Femoral artery Sternal border
Sternal border Lower extremity arteries and veins
Lower extremity arteries and veins Deep veins of the leg
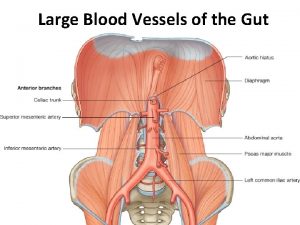
Deep veins of the leg Branches of sma
Branches of sma Common femoral vein
Common femoral vein Getting nerdy llc
Getting nerdy llc Hepatic portal vein model
Hepatic portal vein model Branches of celiac trunk
Branches of celiac trunk Aorta branches
Aorta branches Left renal vein
Left renal vein Portacaval anastomosis
Portacaval anastomosis Encoding
Encoding Teljes nagyér transpositio
Teljes nagyér transpositio Mitral stenosis chest x ray
Mitral stenosis chest x ray Pyloric stenosis nursing diagnosis
Pyloric stenosis nursing diagnosis Somatotopické uspořádání
Somatotopické uspořádání Choanal atresia,
Choanal atresia, Valve resistance formula
Valve resistance formula Define mitral stenosis
Define mitral stenosis Laryngotracheal stenosis
Laryngotracheal stenosis