GASTROINTESTINAL DISORDER ISLAMIC University Nursing College Gastrointestinal Tract



- Slides: 71
GASTROINTESTINAL DISORDER ISLAMIC University Nursing College
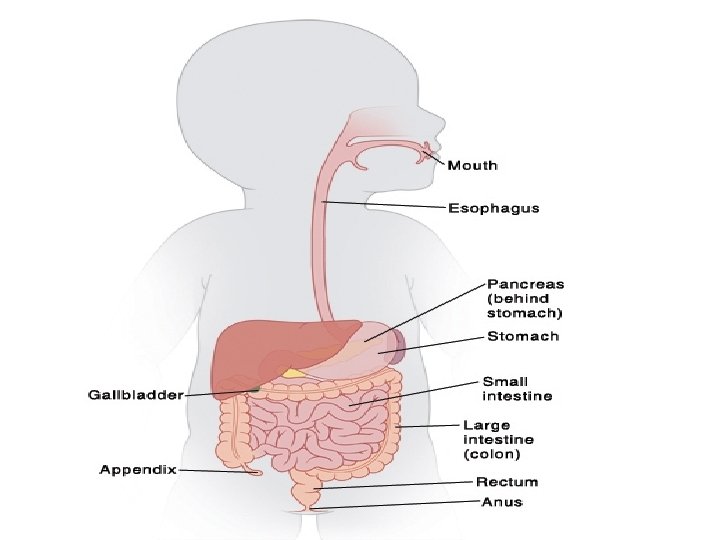
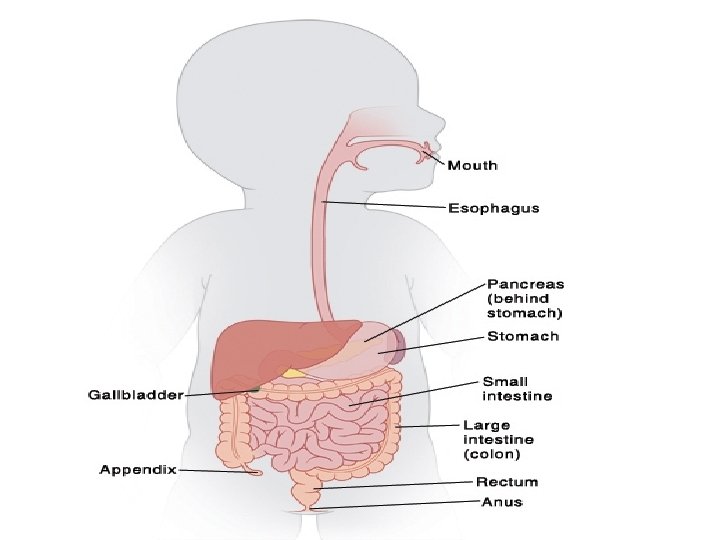
Gastrointestinal Tract � GI tract consists of a hollow muscular tube starting from the oral cavity, going through the rectum and is ended at the anus, where food is expelled. � Main function GI is turning food into nutrients which can be absorbed by the human body to provide energy needed for survival � Accessory organs that assist the tract by secreting enzymes to help break down food into its component nutrients (salivary glands, liver, pancreas and gall bladder)
Gastrointestinal Tract: Assessment � Health history Gestational age and birth weight. Nutritional history (length of BF, introduction of solid food). Neonatal & infancy GI problems. Family factors (life style, hereditary problems. present changes in child’s life (start schooling, new sibling or death in the family) Assessment of the digestive function in a 24 hr (food intake and elimination)

Gastrointestinal Tract: Physical Exam � physical parameter (Wt and Ht) � Skin Color � Inspection of oral cavity � S & S of dehydration � Abdominal and rectal assessment Peristalsis Abdominal Tenderness Distended abdomen � Displaced heart (diaphragmatic hernia) � Hair (loss of pigment or brittle)
Gastrointestinal Tract: Problems Regurgitation(spitting-up) Vomiting. � Mechanical due to obstruction � Reflexive due to infection or allergy � Central due to CNS involvement (meningitis) or sepsis Vomitous assessment includes: Onset & frequency Quantity Degree of forcefulness Presence of bile
Gastrointestinal Tract: Problems Abdominal distention may be due to: � Accumulation � Congenital of fluid or gases malformation � Constipation � Hernia � GI perforation � Cirrhosis Abdominal pain
Gastrointestinal Tract: Problems Diarrhea �Acute due to: Infection. Stress. Drug reaction. �Chronic due to: Chronic infection Malabsorption Obstruction inflammatory bowel disease.
Gastrointestinal Tract: Problems Assessment of Diarrhea � Onset � � Frequency Consistency & Quantity � Odor, presence of blood mucus � Combining factors (food, medication. . etc)
Gastrointestinal Tract: Diagnostic tests CBC, ESR, Electrolytes Liver enzymes Pancreatic enzymes (amylase) Bilirubin Serum ammonia Stool testes � Stool culture/occult blood � Stool fat � Stool p. H

Gastrointestinal Tract: Diagnostic procedures Gastric Analysis � Specimen is taken using NG tube � pt should be NPO after midnight �Stomach contents are examined for: Hydrochloric Occult acid blood Malignant cells Bacteria/parasites
Gastrointestinal Tract: Diagnostic procedures Barium Swallow �Visualize esophagus, stomach and duodenum in upright position behind fluoroscopic screen �Pt should be NPO after midnight �Post-care Encourage fluid intake to White stools up to 72 hrs prevent constipation
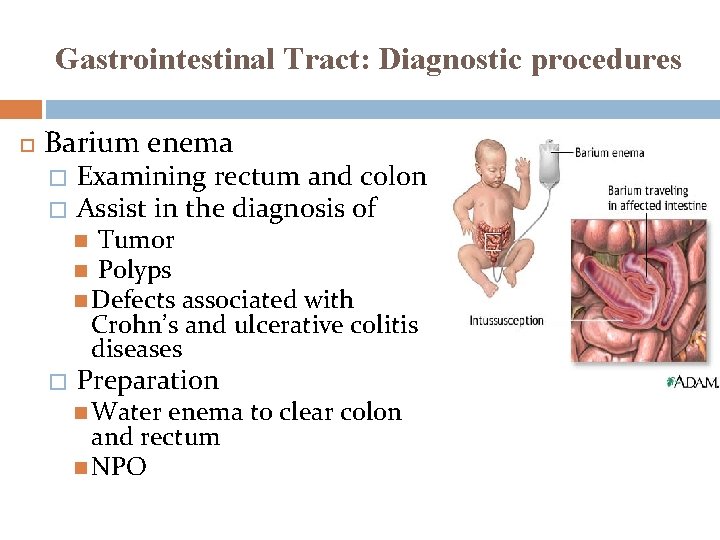
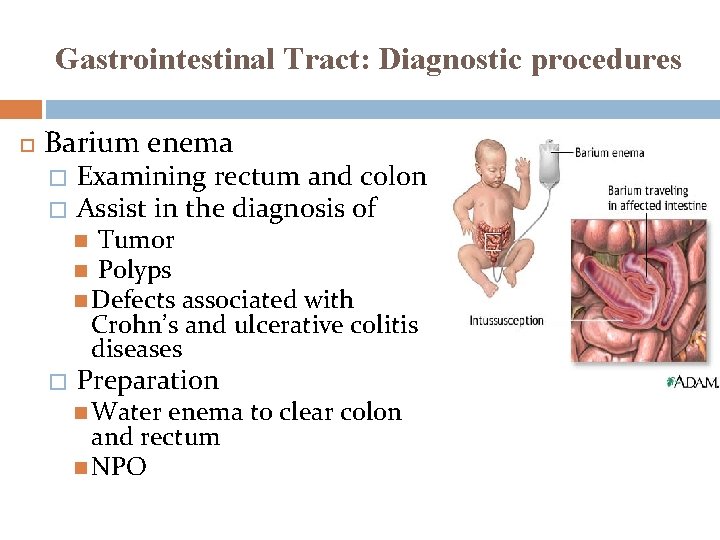
Gastrointestinal Tract: Diagnostic procedures Barium enema � � Examining rectum and colon Assist in the diagnosis of Tumor Polyps Defects associated with Crohn’s and ulcerative colitis diseases � Preparation Water enema to clear colon and rectum NPO
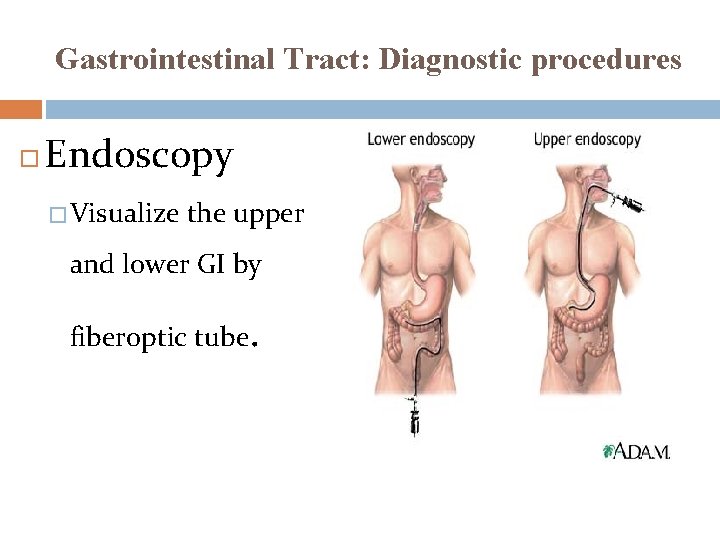
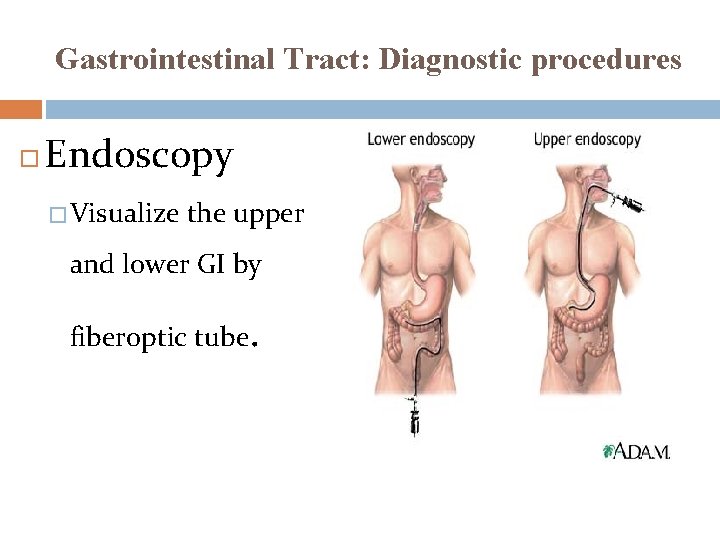
Gastrointestinal Tract: Diagnostic procedures Endoscopy � Visualize the upper and lower GI by fiberoptic tube.
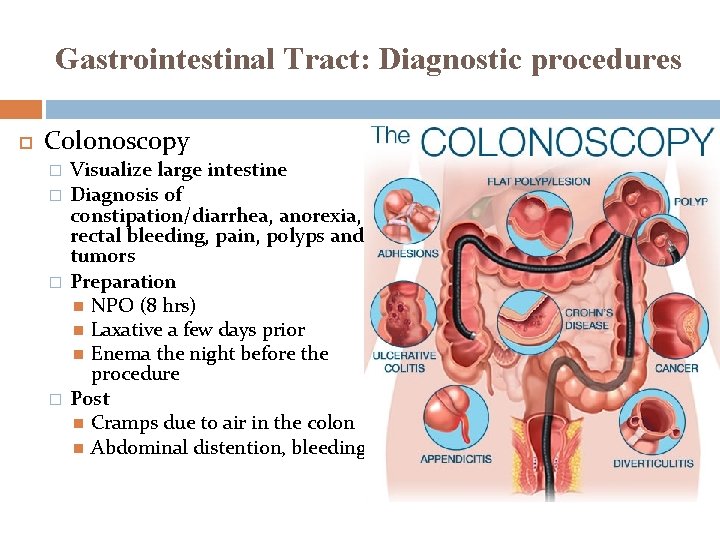
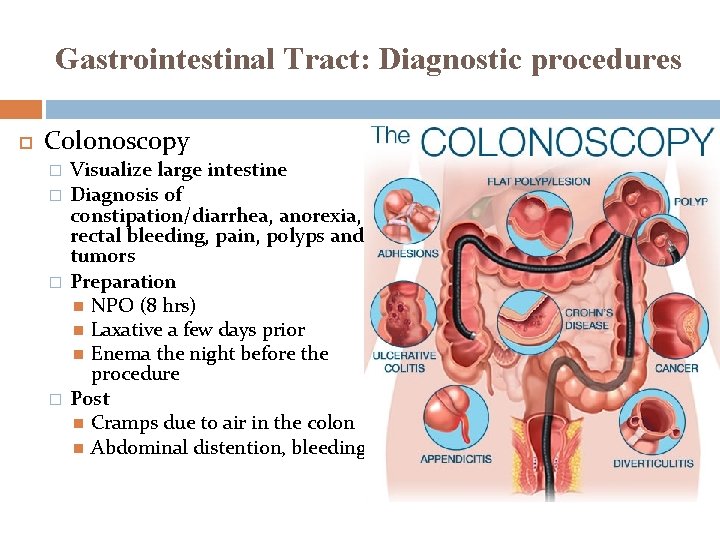
Gastrointestinal Tract: Diagnostic procedures Colonoscopy � � Visualize large intestine Diagnosis of constipation/diarrhea, anorexia, rectal bleeding, pain, polyps and tumors Preparation NPO (8 hrs) Laxative a few days prior Enema the night before the procedure Post Cramps due to air in the colon Abdominal distention, bleeding
Gastrointestinal Tract: Nursing Care Monitoring � Caloric intake � Daily wt � Abdominal girth � Intake and output � Stool chart Help family for lifetime adjustment to the disease by; � Encouraging early family involvement in child’s care � Educating family about the consequence of GI alteration on child’s health and life style ( decrease oral gratification and availability of energy for mobility
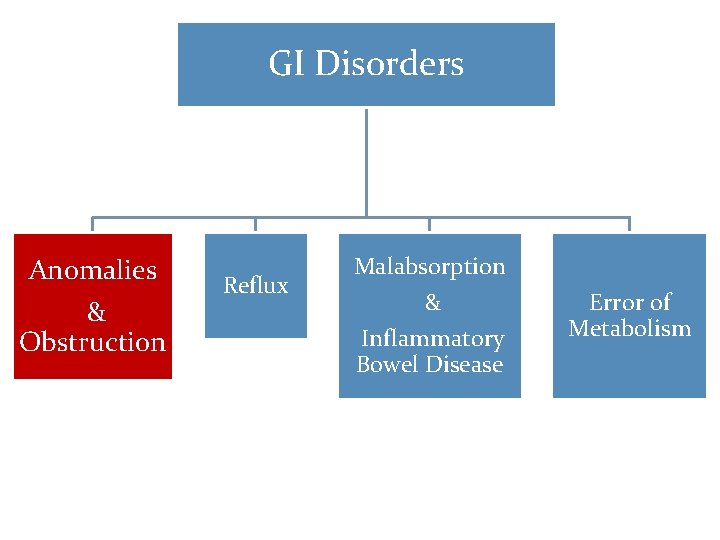
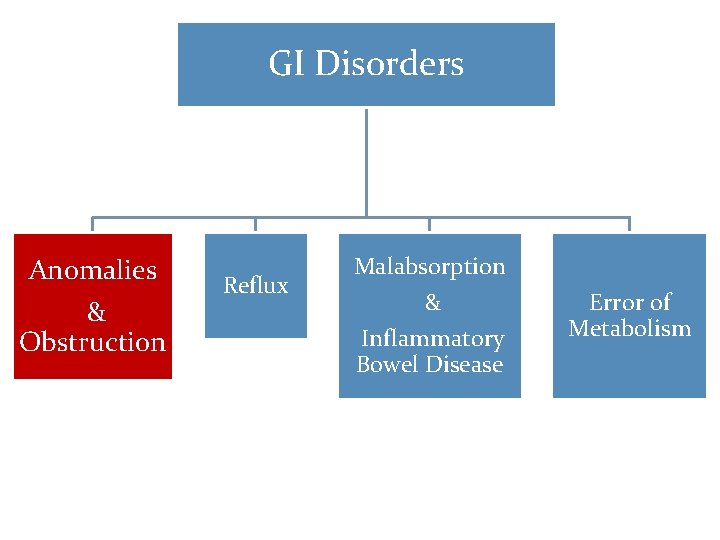
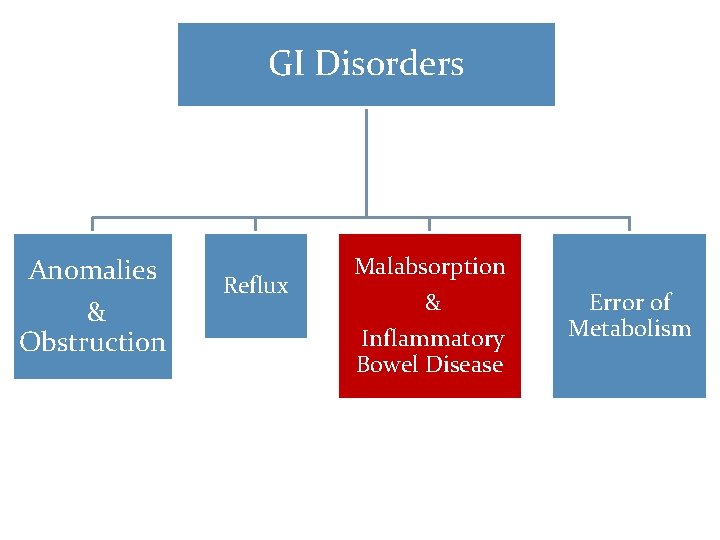
GI Disorders Anomalies & Obstruction Reflux Malabsorption & Inflammatory Bowel Disease Error of Metabolism
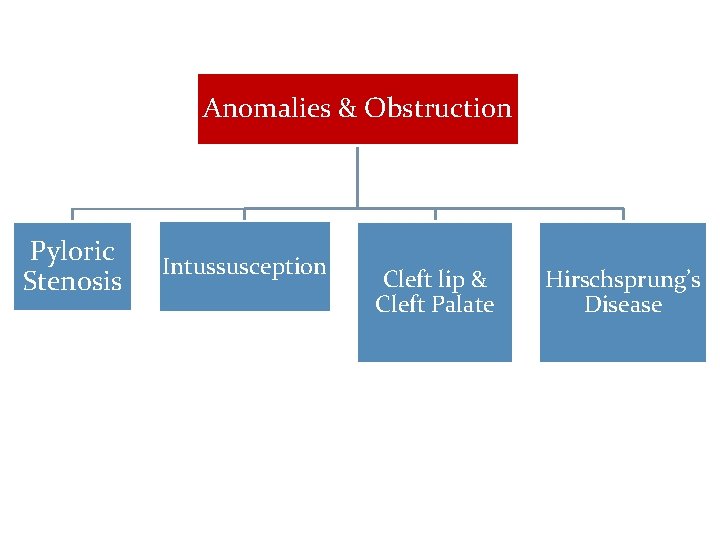
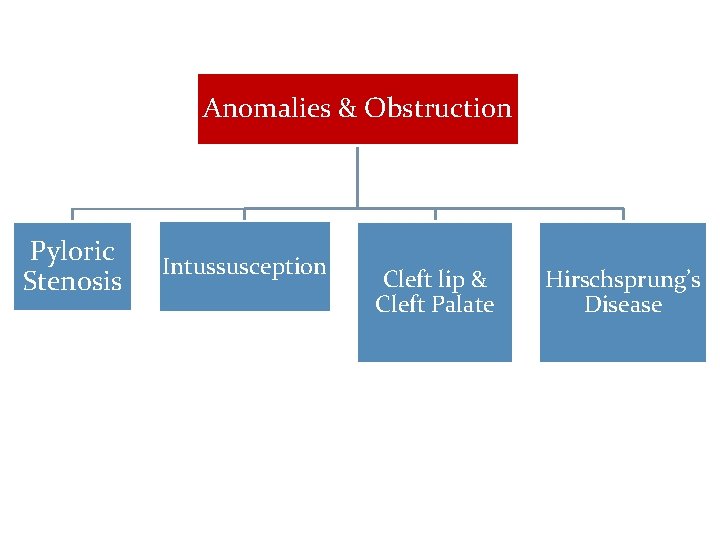
Anomalies & Obstruction Pyloric Stenosis Intussusception Cleft lip & Cleft Palate Hirschsprung’s Disease
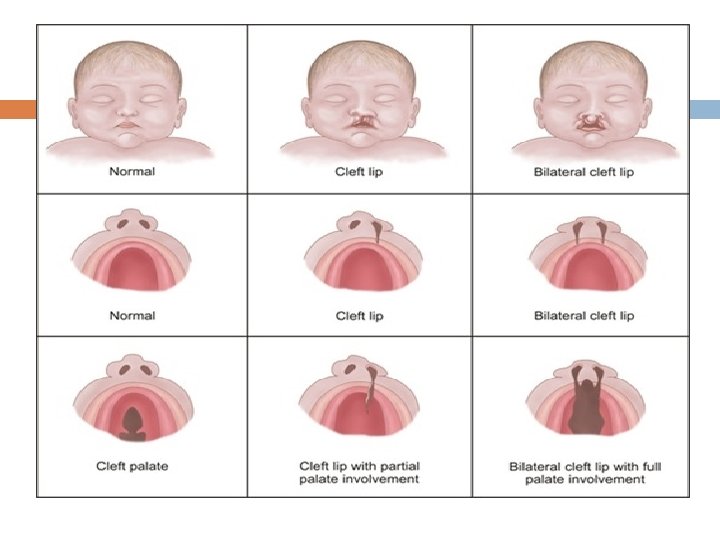
Cleft Lip & Cleft Palate Incomplete fusion of the embryonic structure surrounding the primitive oral cavity Among the most common facial anomalies Genetic basis is present (family history for presence of the defect in other siblings) Incidence rate of cleft lip is 1: 7800 Incidence rate of cleft palate alone in 1: 2000 May result in communication between the nasal and oral cavities
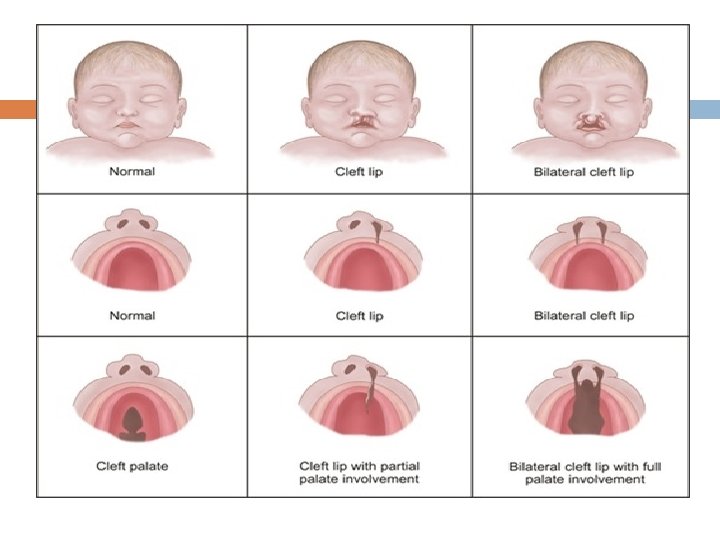
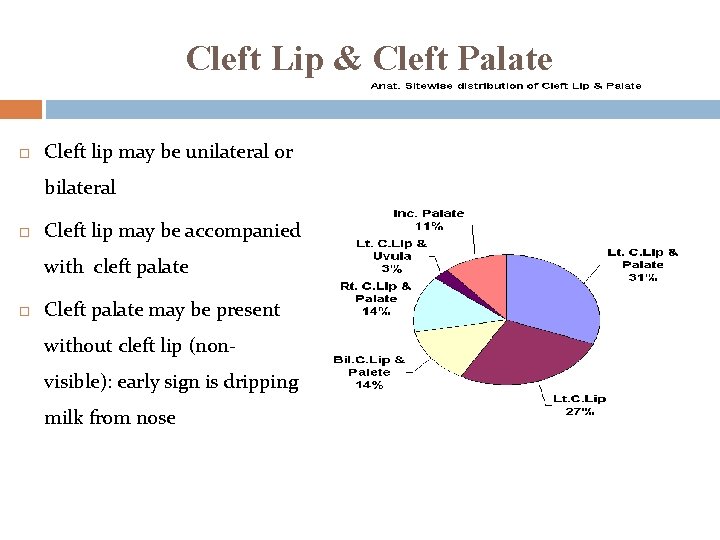
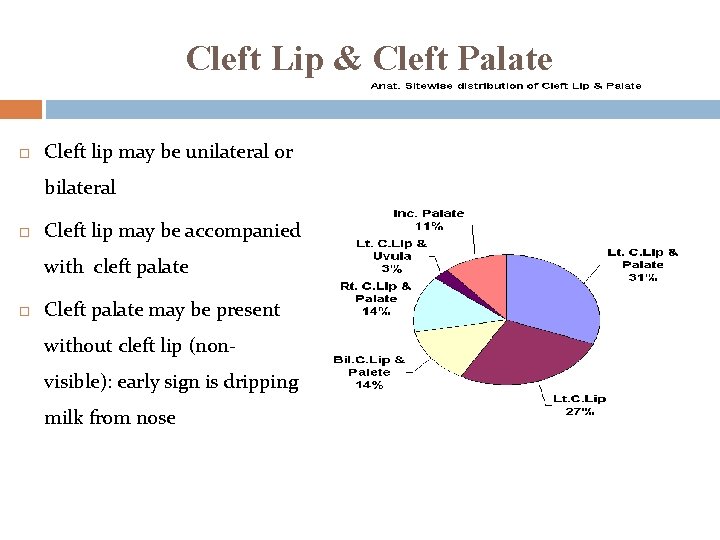
Cleft Lip & Cleft Palate Cleft lip may be unilateral or bilateral Cleft lip may be accompanied with cleft palate Cleft palate may be present without cleft lip (nonvisible): early sign is dripping milk from nose
Cleft Lip & Cleft Palate Assessment should be focused on; � In newborn: compromised sucking ability �Respiratory status �Family reaction
Cleft Lip & Cleft Palate Management �Surgical repair for cleft lip during the first few weeks of life �Initial repair for cleft palate during 4 -6 months of age and the surgical correction between 6 -18 months
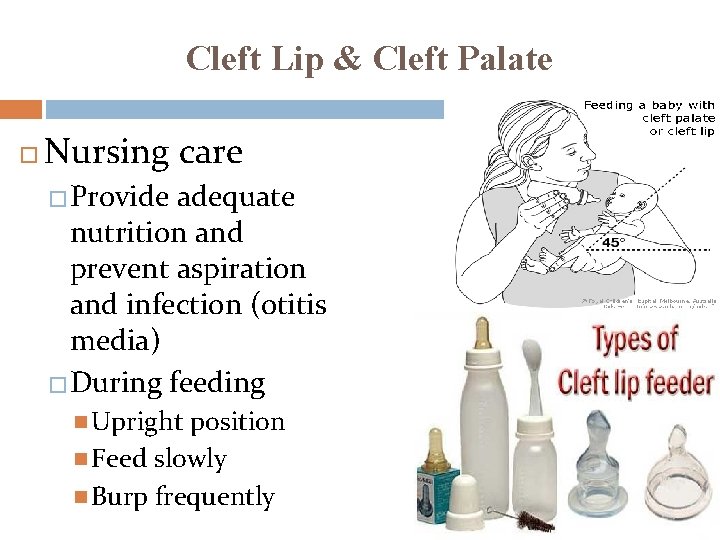
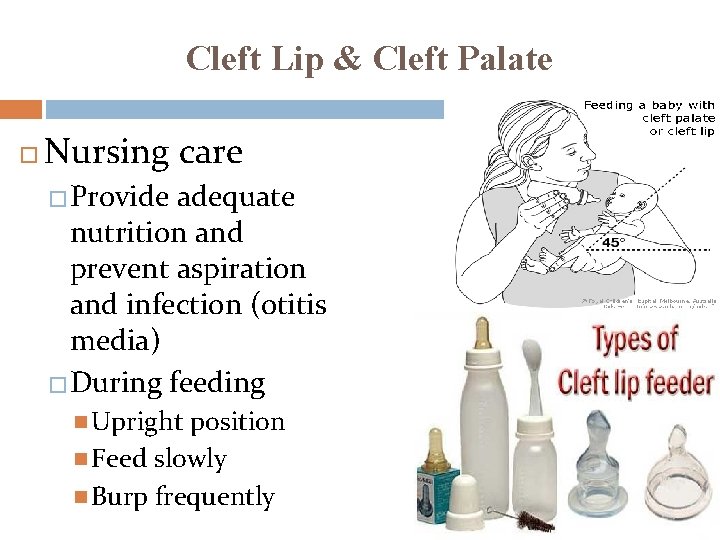
Cleft Lip & Cleft Palate Nursing care �Provide adequate nutrition and prevent aspiration and infection (otitis media) �During feeding Upright position Feed slowly Burp frequently
Cleft Lip & Cleft Palate After the surgical operation �Restrains may be necessary to prevent disturbance of the surgical site �No straws, tooth brushing �Prevent infection � follow-up assessment of Growth Speech Teeth development
Cleft Lip & Cleft Palate Complications �Makes sucking weaker: altered nutrition �Speech difficulties �May affect development of teeth and jaw �Affect the bite �More frequent ear infection
Cleft Lip & Cleft Palate Nursing diagnosis: �Altered nutrition related to physical defect / difficulty eating �Risk for aspiration �Risk for infection �Risk for impaired verbal communication �Altered family process
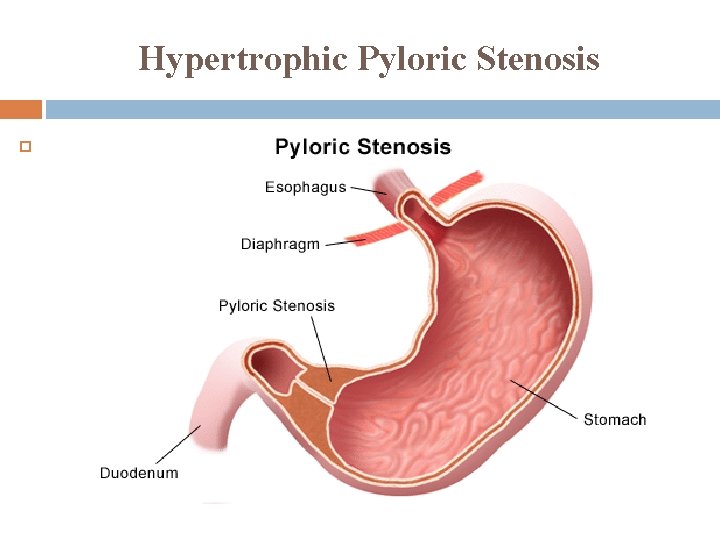
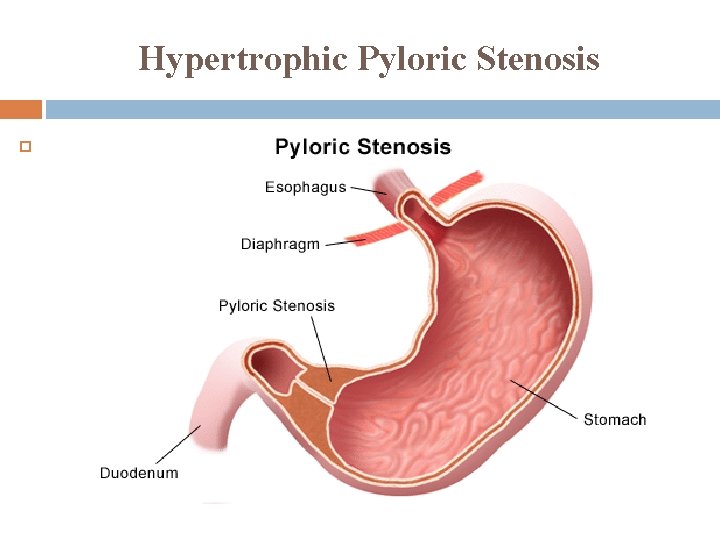
Hypertrophic Pyloric Stenosis
Hypertrophic Pyloric Stenosis An overgrowth of the circular muscle of the pylorus, results in obstruction/ partially / narrowing of the pyloric sphincter Cause is unknown, however there is a hereditary component The stomach contractions increase in frequency and force to empty the stomach content.
Hypertrophic Pyloric Stenosis Usually develops in the first few weeks of life Clinical Manifestation: � Regurgitation small amounts of milk immediately after feeding. � Projectile vomiting. � Vomiting may occur during feeding or shortly after feeding � Vomitus contain NO bile � Gastritis due to prolonged stay of stomach content � Wt loss and dehydration � Metabolic alkalosis � Failure to thrive
Hypertrophic Pyloric Stenosis Assessment �Olive-like mass at right epigastrium under the edge of the liver. �Peristaltic waves can be noted after feeding moving from left to right. �Ultrasoundgraphy. Treatment is by surgery: to allow better passage of milk.
Hypertrophic Pyloric Stenosis Nursing diagnosis: �Fluid volume deficit. Nursing Care: Monitor intake and output. Assess vomitus. Prevent dehydration. Monitor Wt and Ht.
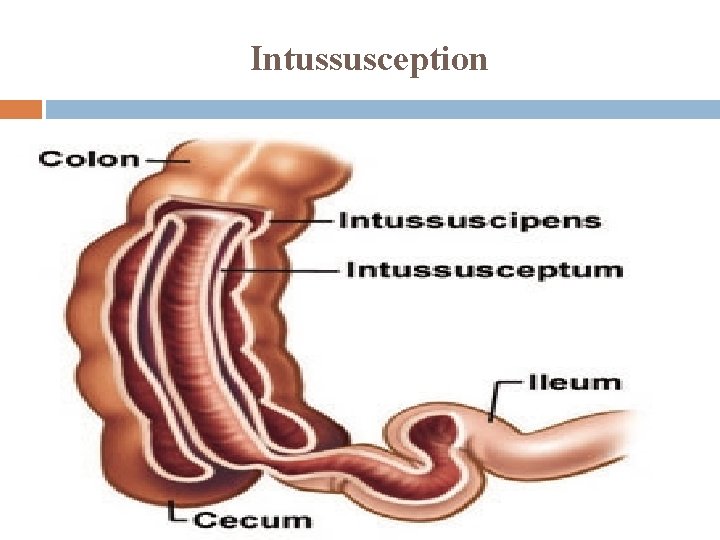
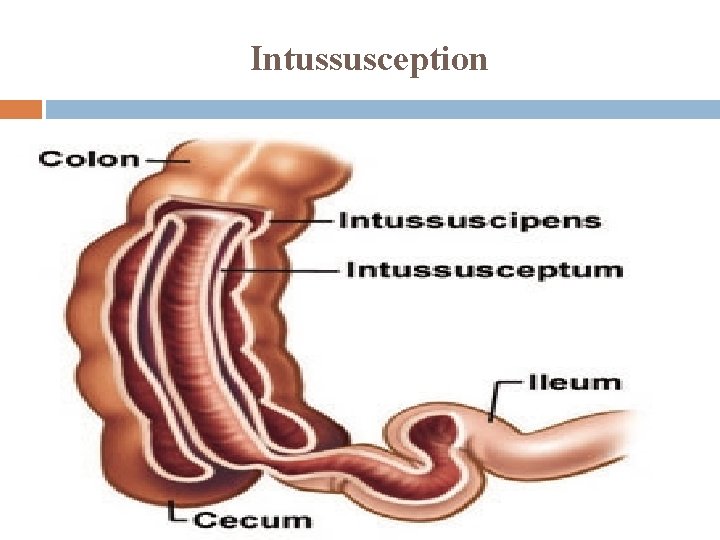
Intussusception
Intussusception Is an invagination of part of the intestine into an adjacentdistal portion of the intestine. Occurs in healthy infants around 6 months of age and rarely occur before 3 months or after 3 -years of age More common in male infants The cause is unknown. The most common type is near the ileocecal valve pushing into the cecum and onto the colon.
Intussusception The involved intestine become inflamed and edematous with bleeding from the mucosa Untreated intussusception can lead to intestinal gangrene, peritonitis and death Diagnosis by barium enema ( if there is intraperitoneal air from a bowel perforation thus enema is contraindicated)
Intussusception Assessment is focused on: �Stool inspection (currant-jelly stools) � CM such as Pain �Abdominal palpation
Intussusception Early symptoms � Crampy abdominal pain and a drawing up of the knees to the chest � periods of apathy � Poor feeding and vomiting Late symptoms � Worsening vomiting, becoming bilious � Abdominal distension/ Palpable abd. Mass (sausage-shaped) � Heme positive stools � Followed by “currant jelly” stools: Jelly stools due to leaking of blood and mucus into the intestinal lumen as a result of venous engorgement � Dehydration � If untreated, necrosis and perforation are possible
Intussusception Treatment � Supportive therapy (Fluid; Antibiotics) � Hydrostatic barium � Operation Manual Resection and reanastamosis
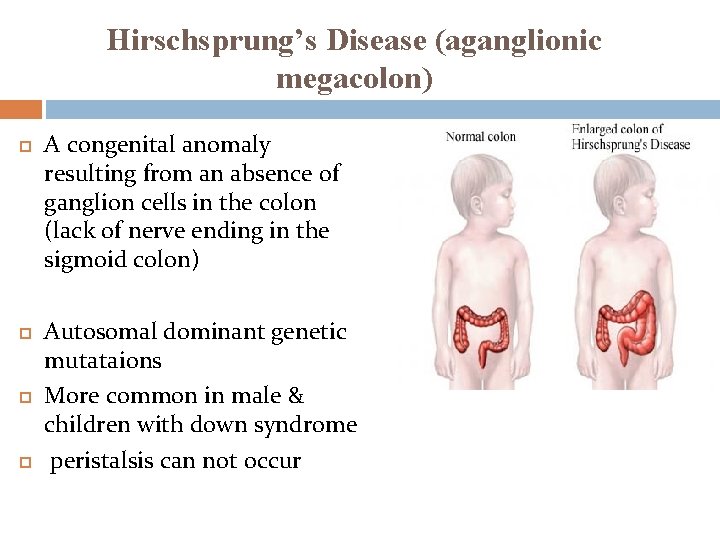
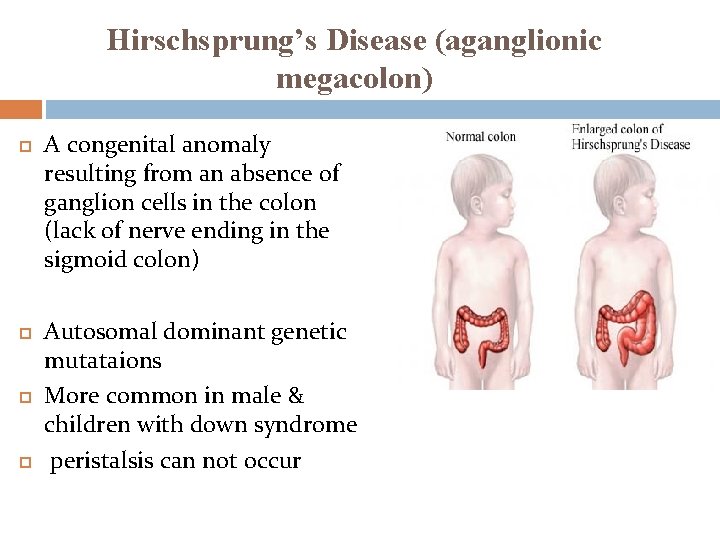
Hirschsprung’s Disease (aganglionic megacolon) A congenital anomaly resulting from an absence of ganglion cells in the colon (lack of nerve ending in the sigmoid colon) Autosomal dominant genetic mutataions More common in male & children with down syndrome peristalsis can not occur
Hirschsprung’s Disease (aganglionic megacolon) CM � Newborn: failure to pass meconium after birth (during the firs t 24 hr) Poor feeding and spitting up Visible bowel loops Bile-stained vomitus Abdominal distention � Infancy Failure to thrive Constipation & Abdominal distention Diarrhea & vomiting/ Explosive watery stool fever
Hirschsprung’s Disease (aganglionic megacolon) CM � Childhood (more chronic: constipation Ribbon-like & foul smelling stools Abdominal distention Palpable fecal masses Poorly nourished Lethargy, nausea and anorexia Treatment by surgery (removal of non-motile part) Colostomy/ileostomy care after surgery After surgery high fiber diet is established Prevent enterocolitis
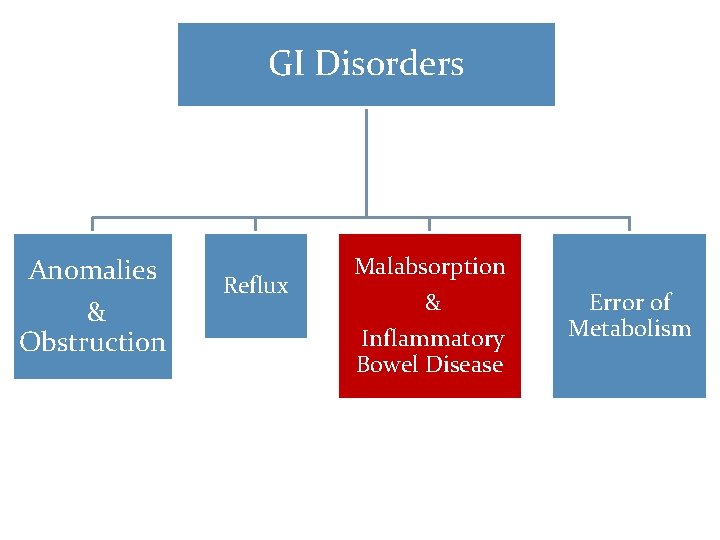
GI Disorders Anomalies & Obstruction Reflux Malabsorption & Inflammatory Bowel Disease Error of Metabolism
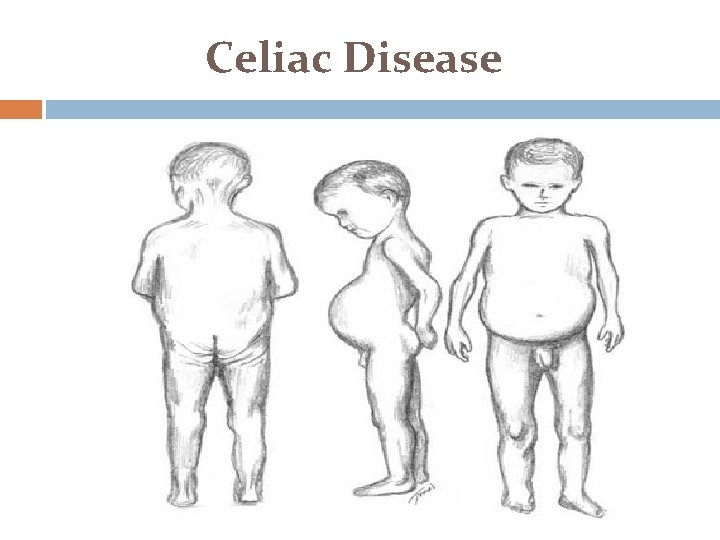
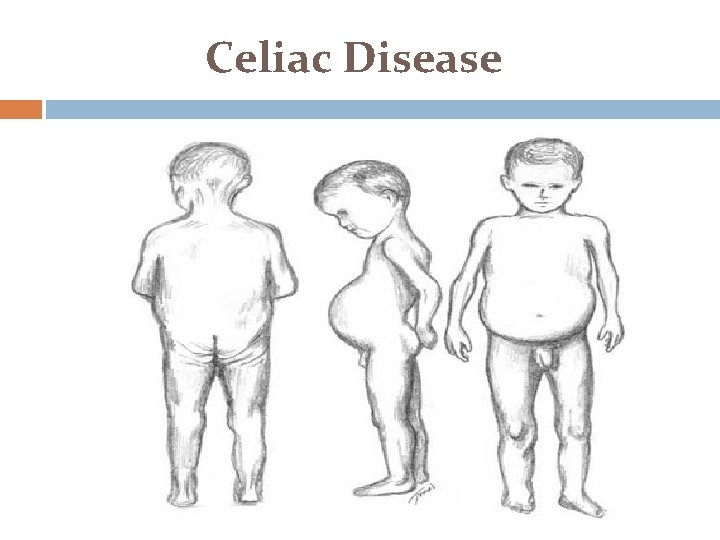
Celiac Disease
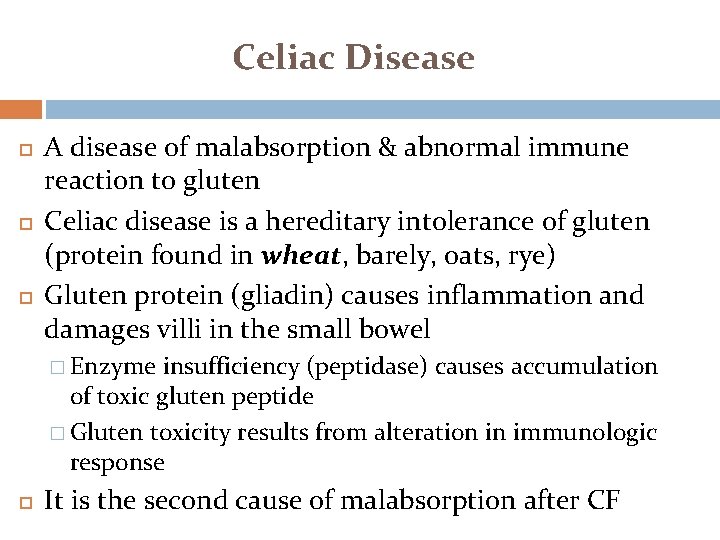
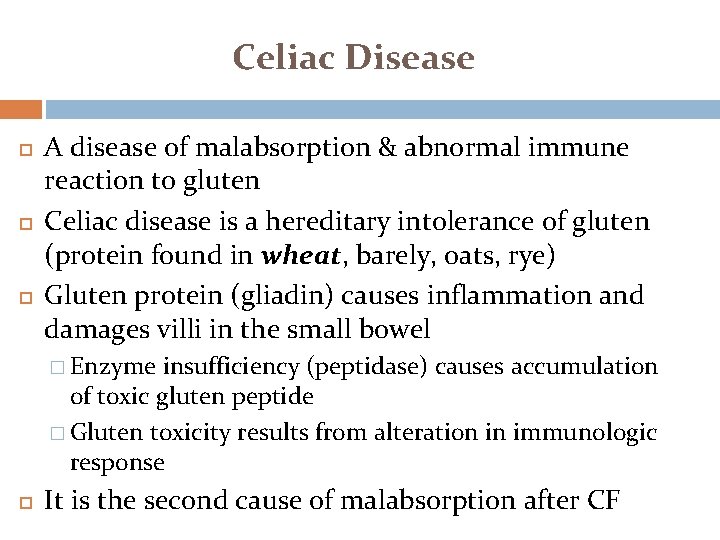
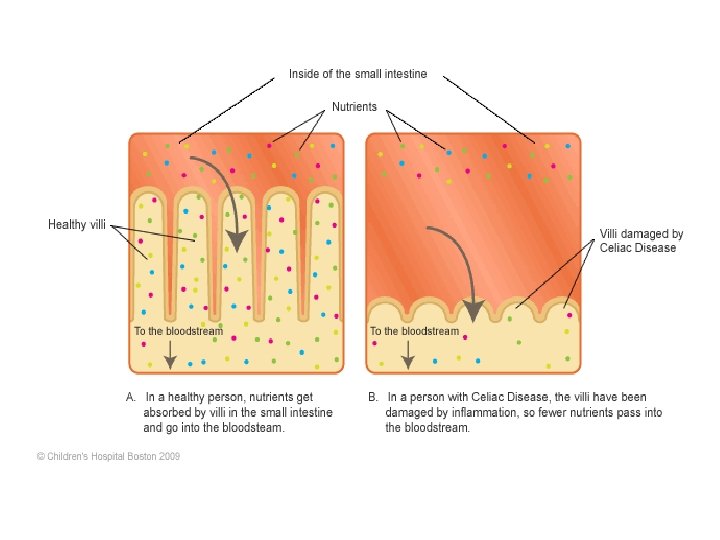
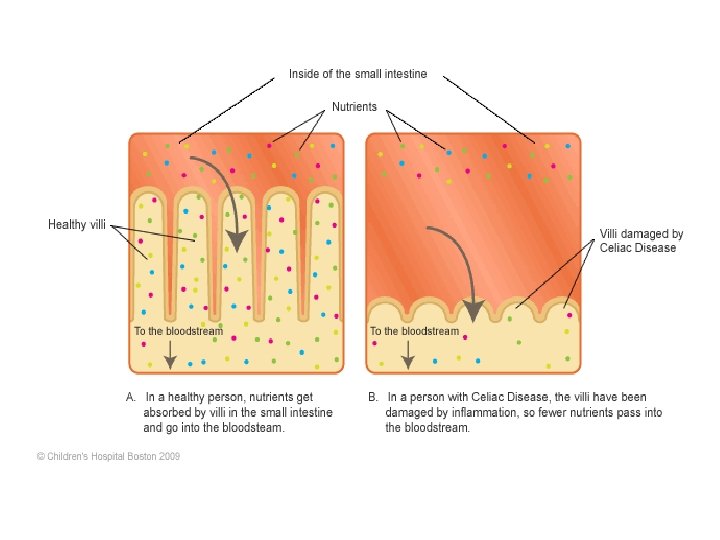
Celiac Disease A disease of malabsorption & abnormal immune reaction to gluten Celiac disease is a hereditary intolerance of gluten (protein found in wheat, barely, oats, rye) Gluten protein (gliadin) causes inflammation and damages villi in the small bowel � Enzyme insufficiency (peptidase) causes accumulation of toxic gluten peptide � Gluten toxicity results from alteration in immunologic response It is the second cause of malabsorption after CF
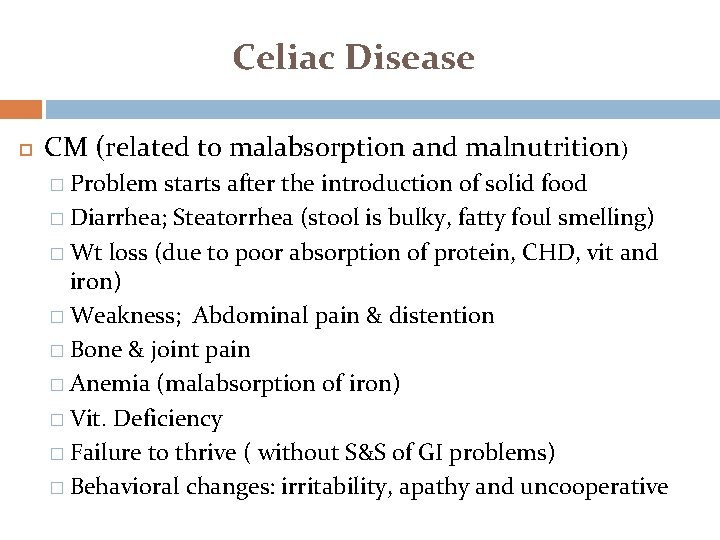
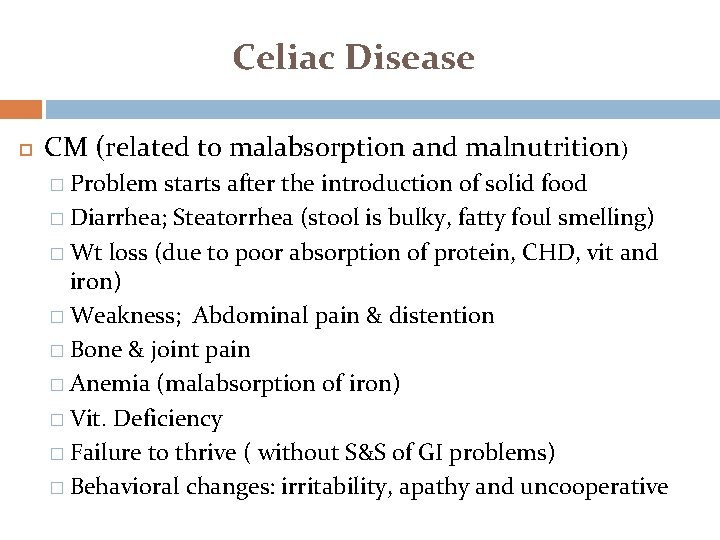
Celiac Disease CM (related to malabsorption and malnutrition) � Problem starts after the introduction of solid food � Diarrhea; Steatorrhea (stool is bulky, fatty foul smelling) � Wt loss (due to poor absorption of protein, CHD, vit and iron) � Weakness; Abdominal pain & distention � Bone & joint pain � Anemia (malabsorption of iron) � Vit. Deficiency � Failure to thrive ( without S&S of GI problems) � Behavioral changes: irritability, apathy and uncooperative
Celiac Disease Assessment � Family history � Child’s dietary history Diagnostic test � anti-tissue transglutaminase antibodies (t. TGA) or antiendomysium antibodies (EMA). � Malabsorption test � CBC � Biopsy of jejunal (atrophy of villi) � Serum protein & immunoglobulin decreased
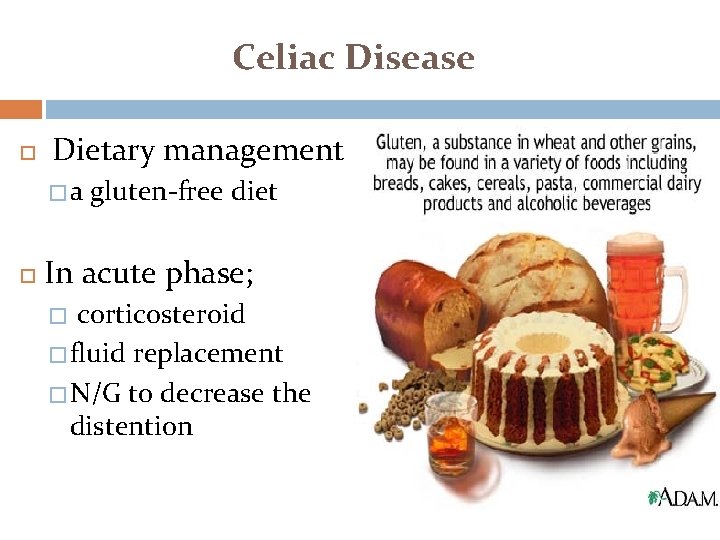
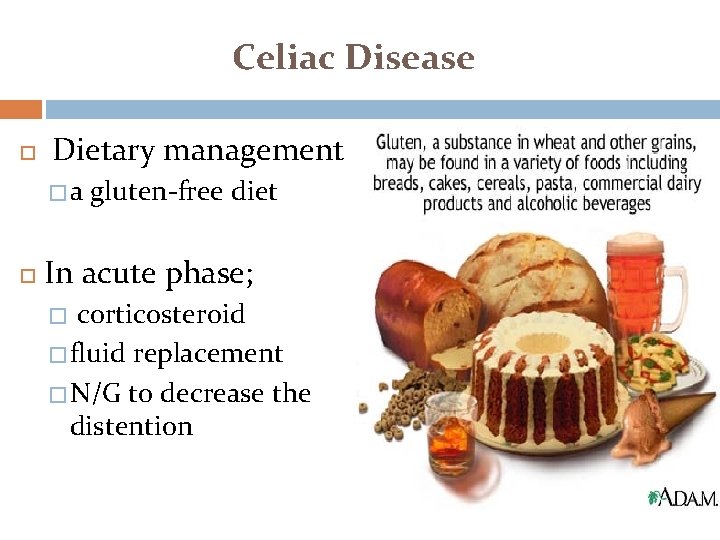
Celiac Disease Dietary management �a gluten-free diet In acute phase; corticosteroid � fluid replacement � N/G to decrease the distention �
Celiac Disease Family education: � � � Diet regimen: free of wheat and barley Monitor growth and development Complications (if not treated) Iron deficiency anemia Osteoporosis infertility or recurrent miscarriage depression or anxiety tingling numbness in the hands and feet seizures
Inflammatory bowel diseases: Ulcerative colitis & Crohn’s disease Inflammatory bowel disease (IBD) refers to chronic conditions that cause inflammation in some part of the intestines. The intestinal walls become swollen, inflamed, and develop ulcers IBD can cause discomfort and serious digestive problems Symptoms depend on which part of the digestive tract is involved
Inflammatory bowel diseases: Ulcerative colitis & Crohn’s disease Causes of the inflammation in IBD involves a complex interaction of several factors: the genes the patient has inherited, � the environment and the immune system. antigens in the environment may cause of the inflammation or they may stimulate the body's defenses to produce inflammation �
Inflammatory bowel diseases: Ulcerative colitis & Crohn’s disease Symptoms of IBD The symptoms of ulcerative colitis and Crohn's disease are similar: � Abdominal pain or cramping � Diarrhea multiple times per day � Bloody stools � Weight loss � Mouth sores and skin problems � Arthritis � Eye problems that affect vision
Inflammatory bowel diseases: Crohn’s disease Crohn's Disease is characterized by a chronic inflammatory process that may affect any segment of the gastrointestinal tract, from mouth to anus. The inflammatory process usually extends through all layers of the intestinal wall Skip lesions Treated by medication to decrease inflammation and usually control the symptoms but does not provide a cure
Inflammatory bowel diseases: Ulcerative colitis Ulcerative Colitis is characterized by continuous inflammation confined to the large intestine. Inflammation is limited primarily to the mucosa and does not extend through all layers. Treated by; � � The primary treatment options are medications that decrease the abnormal inflammation in the colon lining and control the symptoms. . Ulcerative colitis is potentially curable if the colon is removed
Inborn errors of metabolism 55 Galactosemia �Phenylketonuria �Congenital hypothyroidism �

Inborn errors of metabolism 56 � Clinical manifestations � Neurological symptoms ( lethargy, poor feeding, vomiting and irritability) � In severe cases coma, seizure � Unexplained metabolic acidosis � Episodes of hypoglycemia/ hyperglycemia, ketonuria � Heart failure � Liver disease � Dysmorphic features � Developmental delay
Inborn error of metabolism: Galactosemia 57 Lack of galactose-1 -phosphate uridyl-transferase enzyme. Inherited as autosomal recessive. Failure of conversion of galactose to glucose, accumulation of galactose leads to damage of the liver & brain. Should be suspected in any infant who vomits, refuses feeds, fails to thrive & become jaundiced in the first week Long term effect: ovaries damage, speech delay, learning difficulties Treatment may include stopping BF & replacement by a special low-lactose milk.
Inborn error of metabolism: Phenylketonuria 58 autosomal recessive genetic disorder causing mutation of the gene that producing phenylalanine hydroxylase enzyme that is necessary to metabolize the amino acid phenylalanine to tyrosine. Phenylalanine is converted into phenylketone which is detected in the urine the disease may present clinically with � � � Seizures excessively fair hair and skin "musty odor" to the baby's sweat and urine
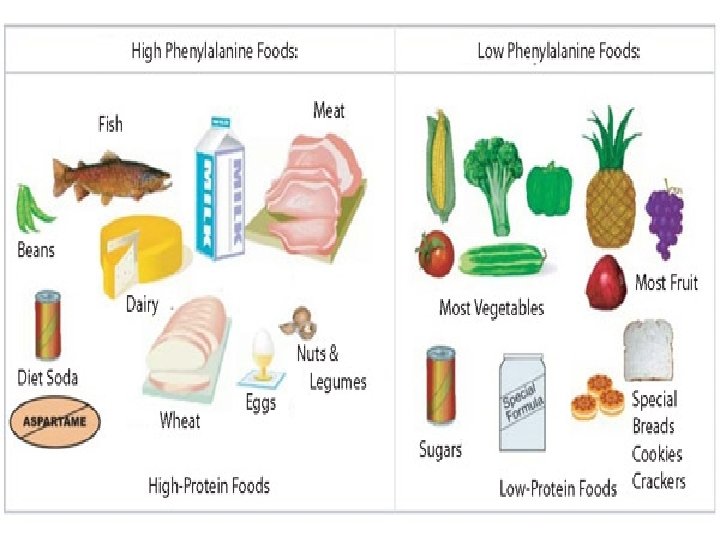
Inborn error of metabolism: Phenylketonuria 59 Early cases of PKU were treated with a lowphenylalanine diet. � Children with PKU must adhere to a special diet low in Phe for optimal brain development. � The diet requires severely restricting or eliminating foods high in Phe, such as meat, chicken, fish, eggs, nuts, cheese, milk & dairy products. If PKU is left untreated, it can cause problems with brain development, including mental retardation, brain damage and seizures.
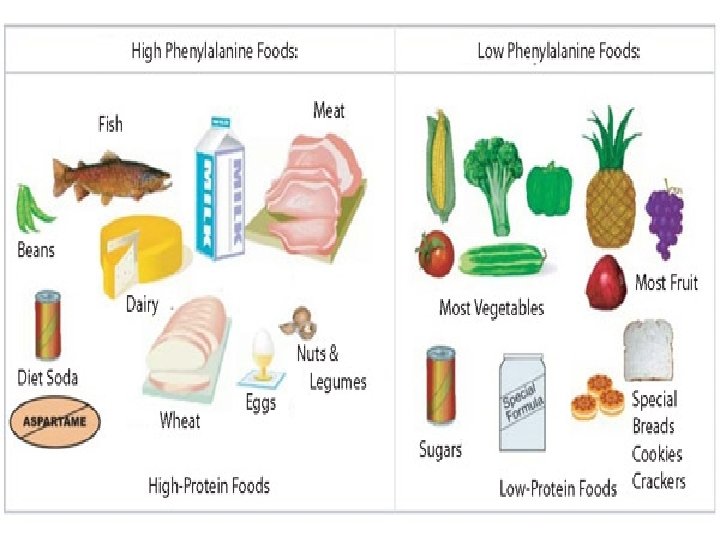
Inborn error of metabolism: Phenylketonuria 60
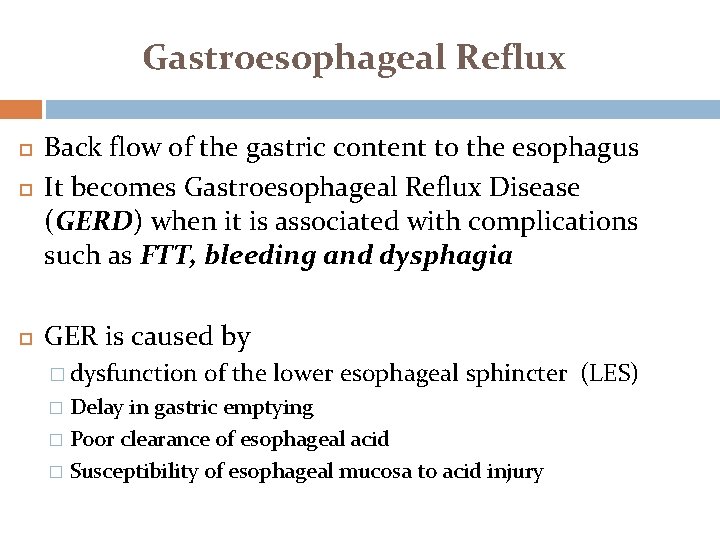
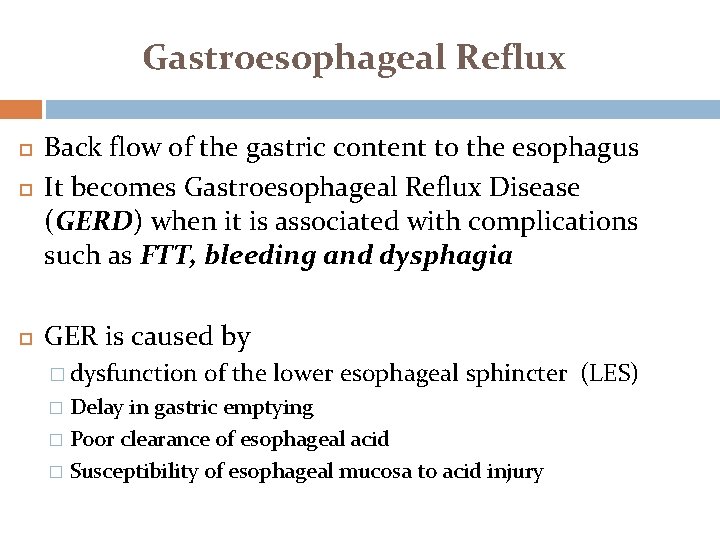
Gastroesophageal Reflux Back flow of the gastric content to the esophagus It becomes Gastroesophageal Reflux Disease (GERD) when it is associated with complications such as FTT, bleeding and dysphagia GER is caused by � dysfunction of the lower esophageal sphincter (LES) Delay in gastric emptying � Poor clearance of esophageal acid � Susceptibility of esophageal mucosa to acid injury �
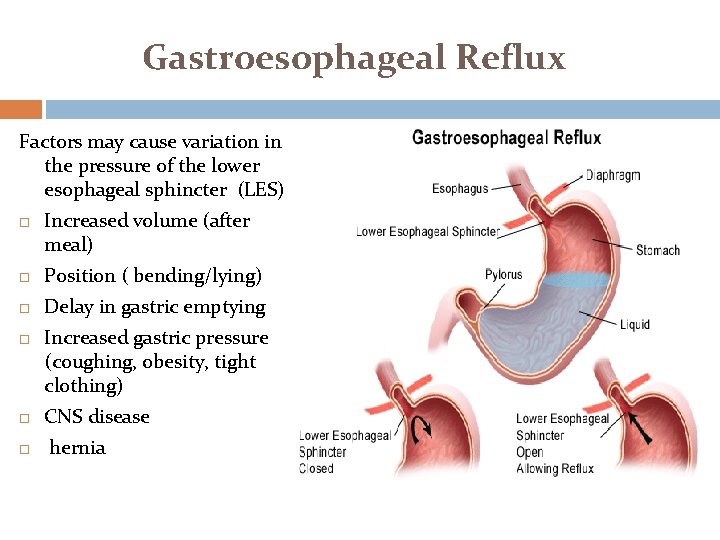
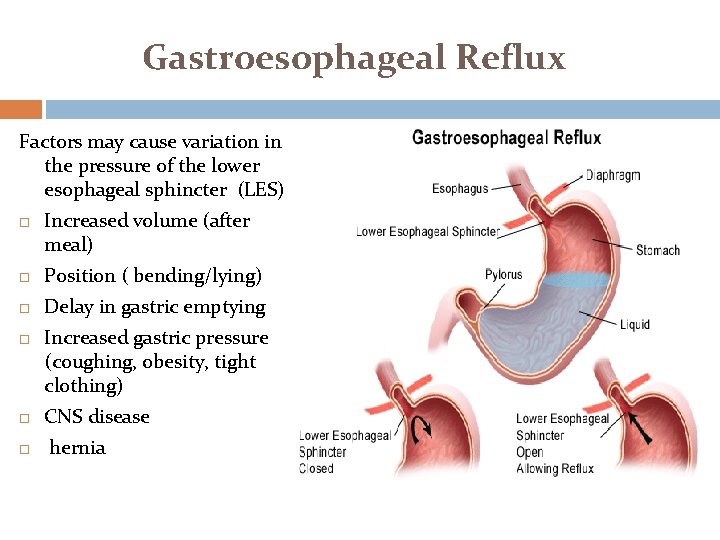
Gastroesophageal Reflux Factors may cause variation in the pressure of the lower esophageal sphincter (LES) Increased volume (after meal) Position ( bending/lying) Delay in gastric emptying Increased gastric pressure (coughing, obesity, tight clothing) CNS disease hernia
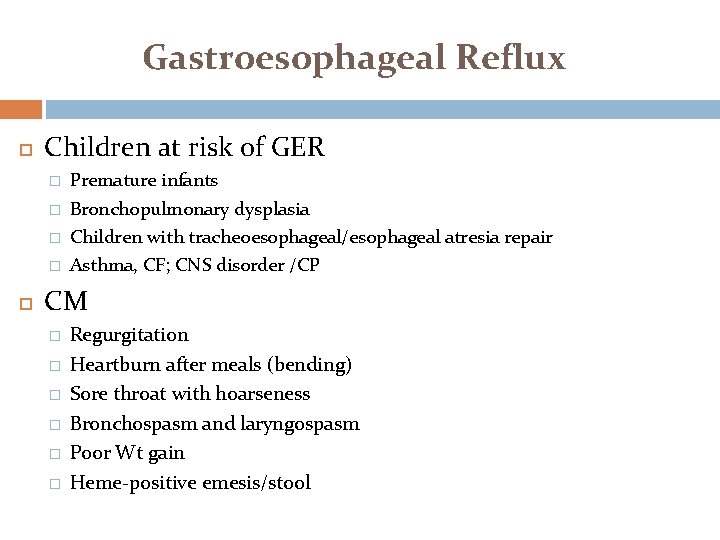
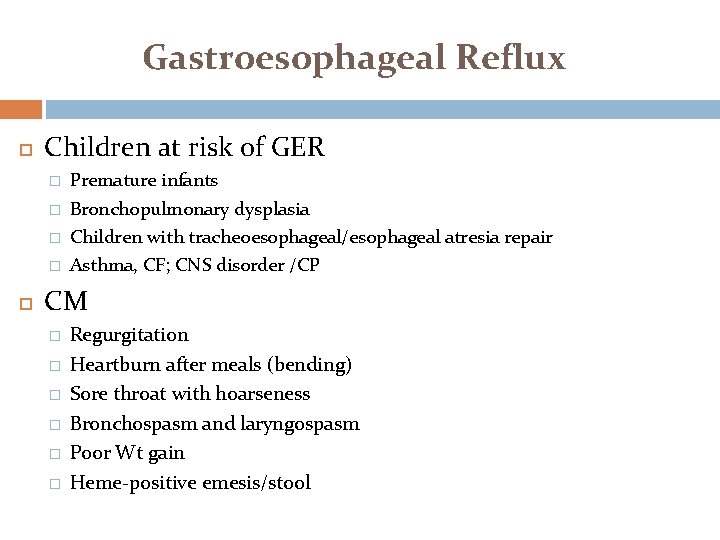
Gastroesophageal Reflux Children at risk of GER � � Premature infants Bronchopulmonary dysplasia Children with tracheoesophageal/esophageal atresia repair Asthma, CF; CNS disorder /CP CM � � � Regurgitation Heartburn after meals (bending) Sore throat with hoarseness Bronchospasm and laryngospasm Poor Wt gain Heme-positive emesis/stool
Gastroesophageal Reflux Diagnostic test � 24 -hour p. H monitoring � Barium swallow � Upper endoscopy Management � Medication: antiacids; maalox 0 H 2 receptor blocker ; decrease acid production (ranitidine) Reduce gastric secretion ( omeprazole (prilosec)) Pro-motility agent (metoclopramide( reglan))
Gastroesophageal Reflux Diet modifications � � Eliminate acid food (citrus juice, tomatoes, carbonated fluid) Avoid food that relax esophageal sphincter (fatty foods, peppermint, chocolate) thickened formula & Small meals Elevate the head of the bed when sleeping (infant in prone position) Avoid feeding at bedtime Wear loss cloth Maintain ideal body weight Surgery to tighten the lower esophageal sphincter
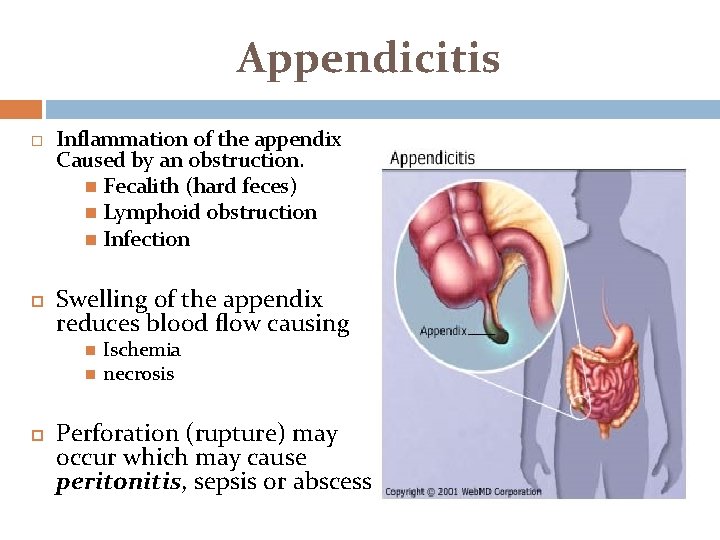
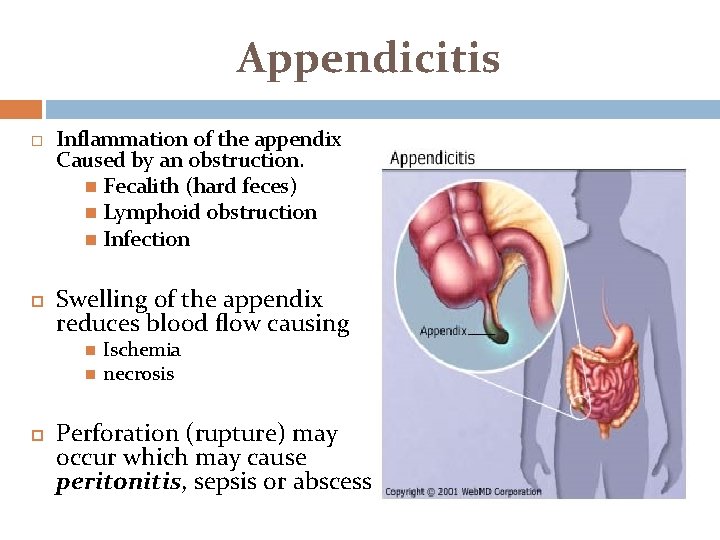
Appendicitis Inflammation of the appendix Caused by an obstruction. Fecalith (hard feces) Lymphoid obstruction Infection Swelling of the appendix reduces blood flow causing Ischemia necrosis Perforation (rupture) may occur which may cause peritonitis, sepsis or abscess
Appendicitis CM � PAIN (pain is the first sign) starts around the belly and moves to the lower right quadrant of the abdomen Right lower quadrant localized tenderness Right � fever, lower quadrant rebound tenderness nausea, vomiting & diarrhea � WBC over 15, 000 � Elevated C-reactive protein
Appendicitis CM � In neonate (non specific) Irritability/ lethargy Abdominal distention & abdominal mass Vomiting � In infants and older children Vomiting & diarrhea; Pain & fever
Appendicitis S & S of appendix perforation � Fever � Sudden relief from pain � Subsequent increase in pain and rigidity guarding of the abdomen � Progressive abdominal distention � Tachycardia, rapid-shallow breathing � Pallor , chills and irritability
Appendicitis Nursing Diagnosis � Pain R/T inflammation process � Risk for fluid volume deficit R/T decrease intake (loss of appetite) and excessive loss via vomiting � Risk for infection ( possibility of rupture)
Appendicitis Nursing care (pre-op care) � Avoid administering laxative, enema or heat application to avoid increase the bowel motility which may lead to perforation � Cold packs on the abdomen/pain killer � Monitor I & O � IV fluid � Monitor S & S of appendix rupture/peritonitis � Post operative care