Musculoskeletal fractures Nancy Lin RN MS Adapted from


- Slides: 78
Musculoskeletal- fractures Nancy Lin, RN, MS Adapted from Kara Potter
SLO’s ¡ Compare and contrast clinical manifestations, pathophysiology, clinical treatments and management of pediatric clients with congenital and acquired musculoskeletal conditions
SLO’s ¡ ¡ Compare and contrast clinical manifestations, pathophysiology, clinical treatment and nursing management of pediatric and adult clients with acquired musculoskeletal conditions. Analyze the nursing process for clients with musculoskeletal conditions.
FUNCTIONS OF THE SKELETAL SYSTEM ¡ ¡ ¡ SUPPORT PROTECTION MOVEMENT HEMATOPORESIS MINERAL STORAGE
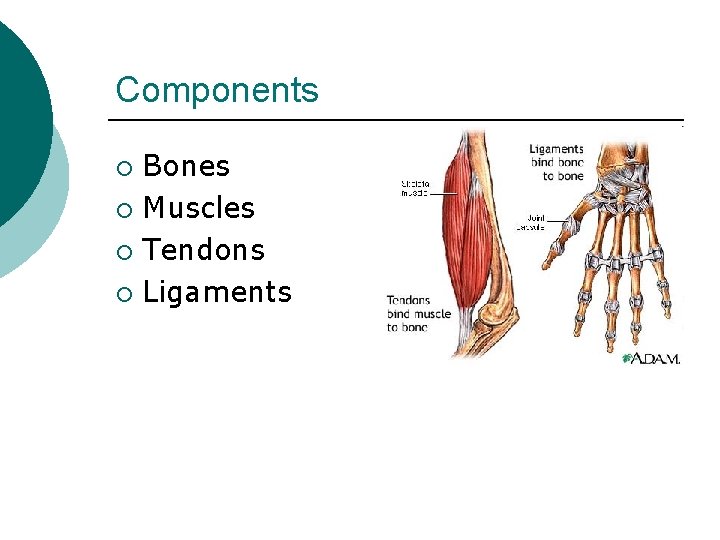
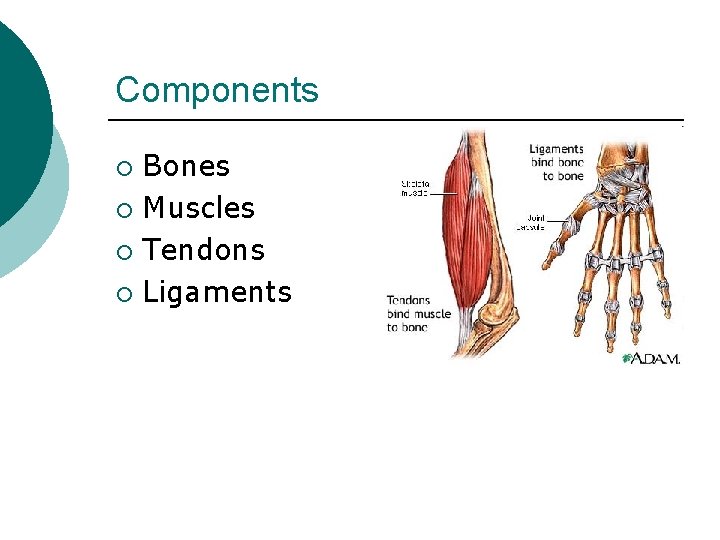
Components Bones ¡ Muscles ¡ Tendons ¡ Ligaments ¡
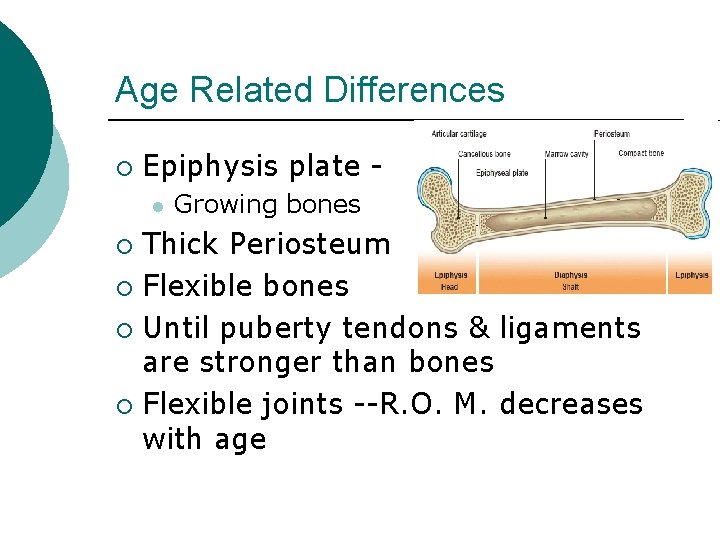
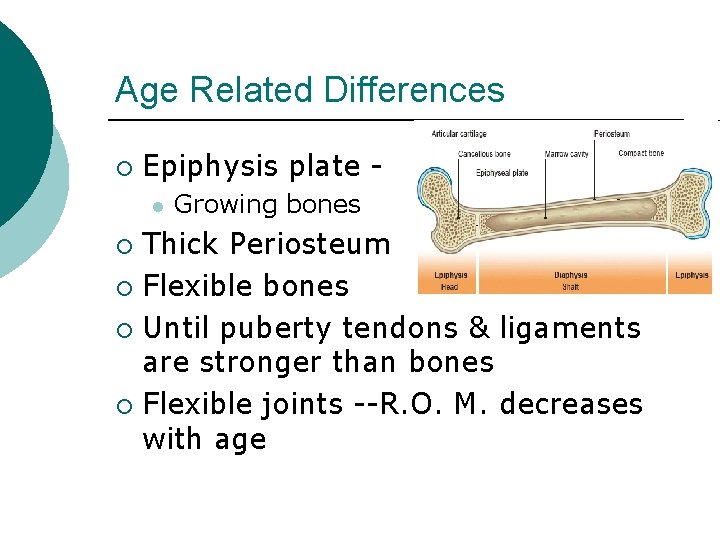
Age Related Differences ¡ Epiphysis plate l Growing bones Thick Periosteum ¡ Flexible bones ¡ Until puberty tendons & ligaments are stronger than bones ¡ Flexible joints --R. O. M. decreases with age ¡
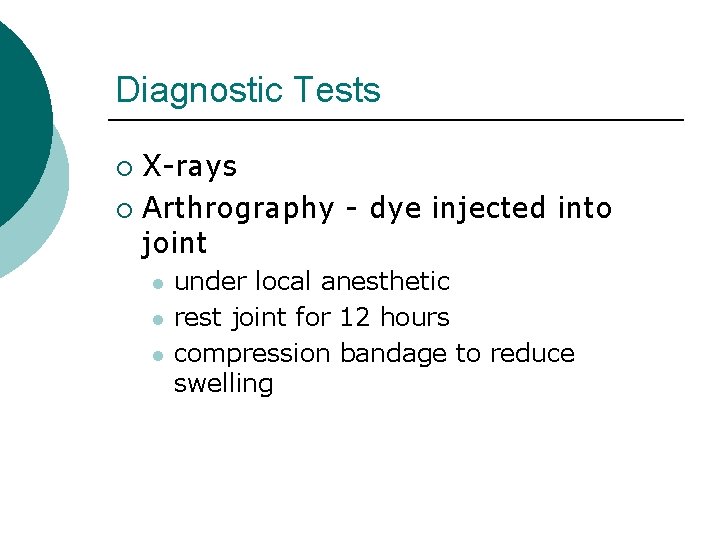
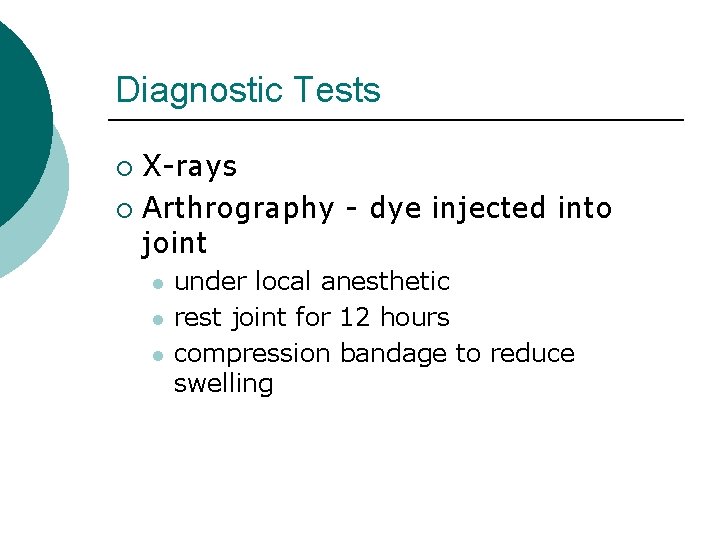
Diagnostic Tests X-rays ¡ Arthrography - dye injected into joint ¡ l l l under local anesthetic rest joint for 12 hours compression bandage to reduce swelling
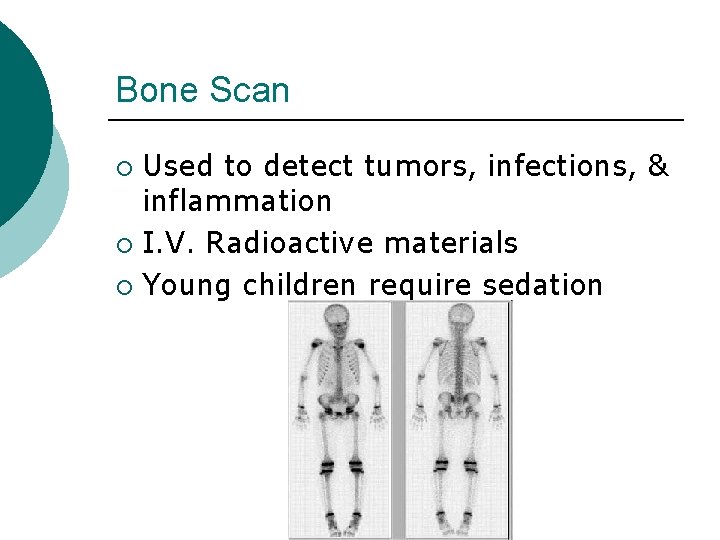
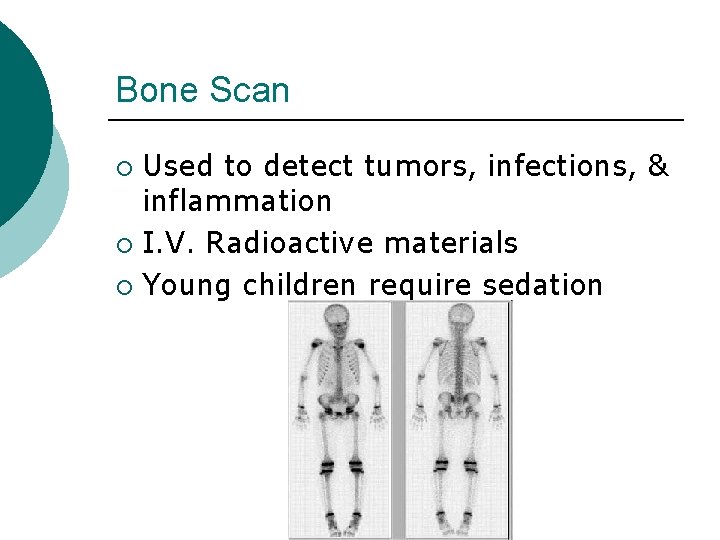
Bone Scan Used to detect tumors, infections, & inflammation ¡ I. V. Radioactive materials ¡ Young children require sedation ¡
Computed Tomography Scan (CAT) Used to visualize anatomic details ¡ Narrow x ray beam - 3 D cross section ¡ Contrast dye may be used ¡ Painless but frightening ¡ Youngsters may require sedation ¡
MRI Organ structures clearly defined ¡ Often used to diagnose ligament and muscle tears ¡ Unrestricted food & fluid ¡ Length of test - one hour or more ¡ Sedation may be needed ¡
Fractures Disruption or break in continuity of the structure of bone ¡ Majority of fractures from traumatic injuries ¡ Some fractures secondary to disease process ¡ l Cancer or osteoporosis
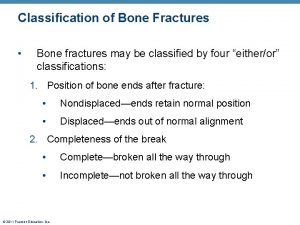
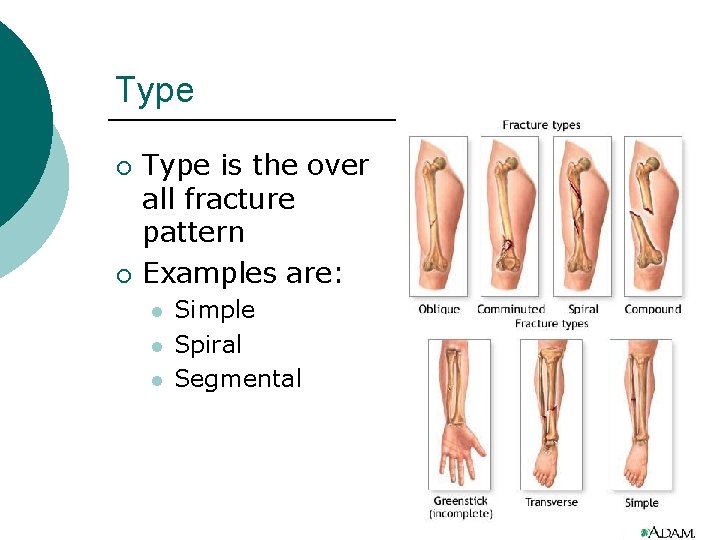
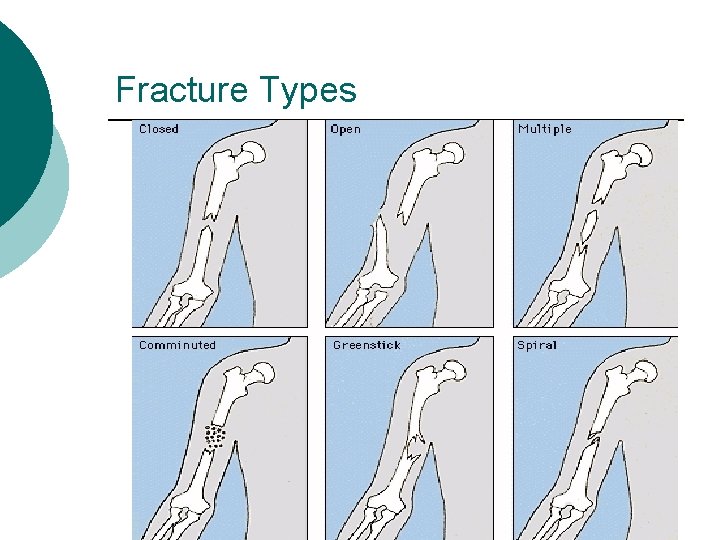
Classification ¡ Fractures are described and classified according to l l l Type Comminution Anatomic location of fracture on involved bone
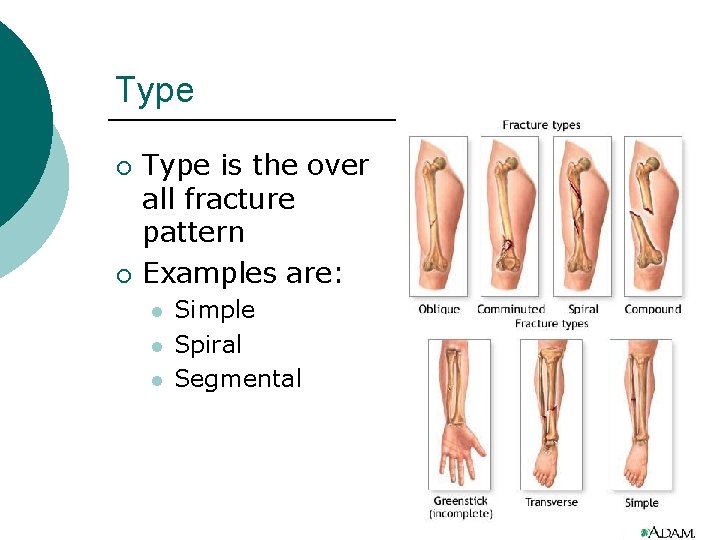
Type ¡ ¡ Type is the over all fracture pattern Examples are: l l l Simple Spiral Segmental
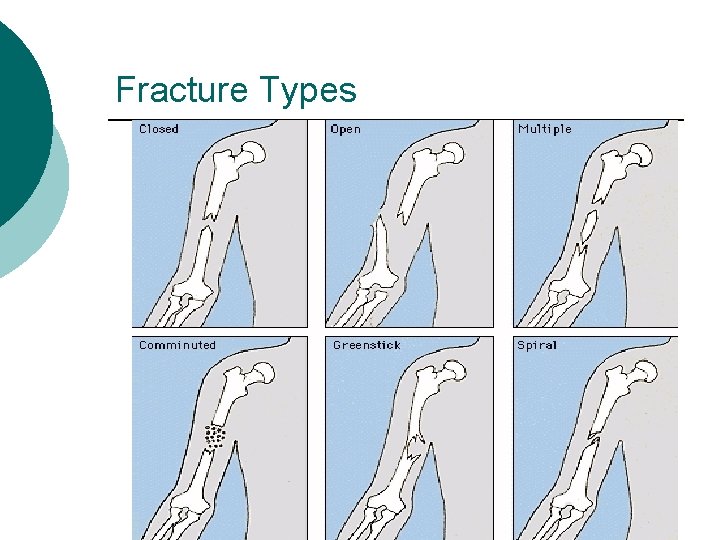
Fracture Types
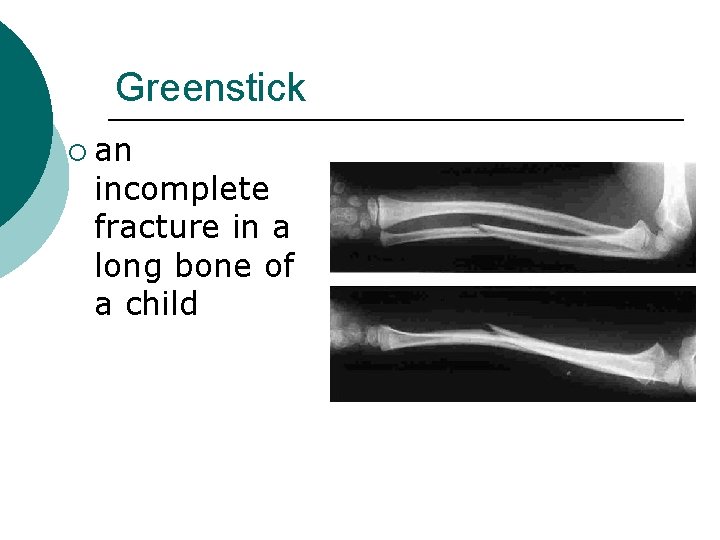
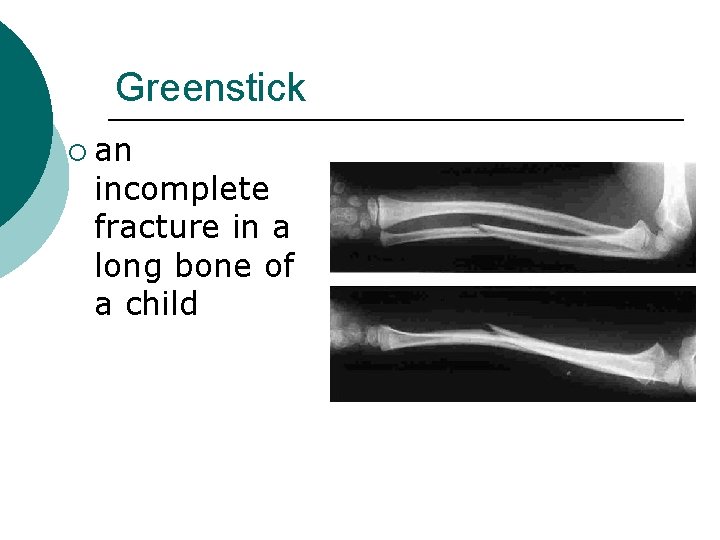
Greenstick ¡ an incomplete fracture in a long bone of a child
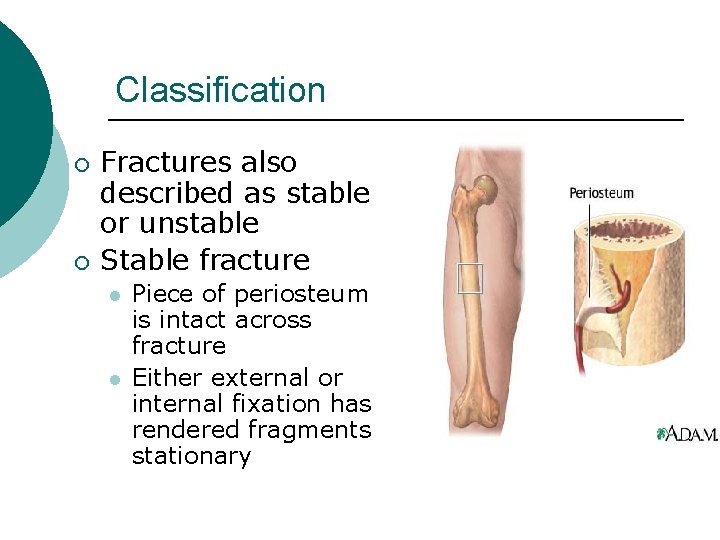
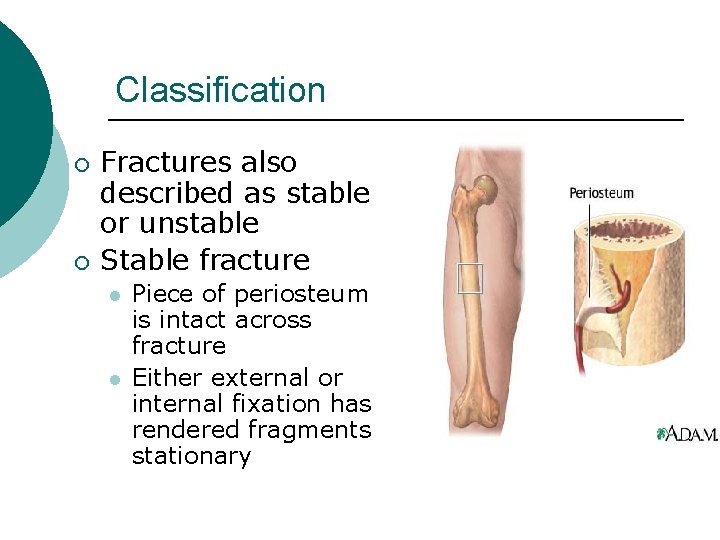
Classification ¡ ¡ Fractures also described as stable or unstable Stable fracture l l Piece of periosteum is intact across fracture Either external or internal fixation has rendered fragments stationary
Classification ¡ Unstable fracture Grossly displaced during injury l Site of poor fixation l Usually comminuted or oblique l
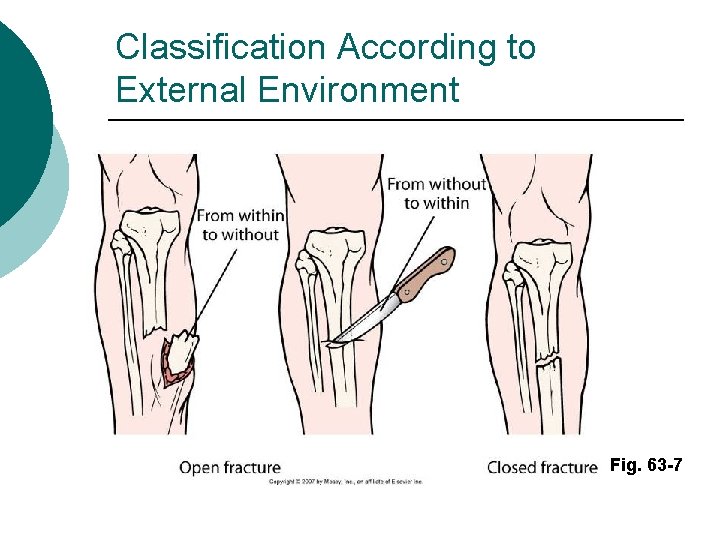
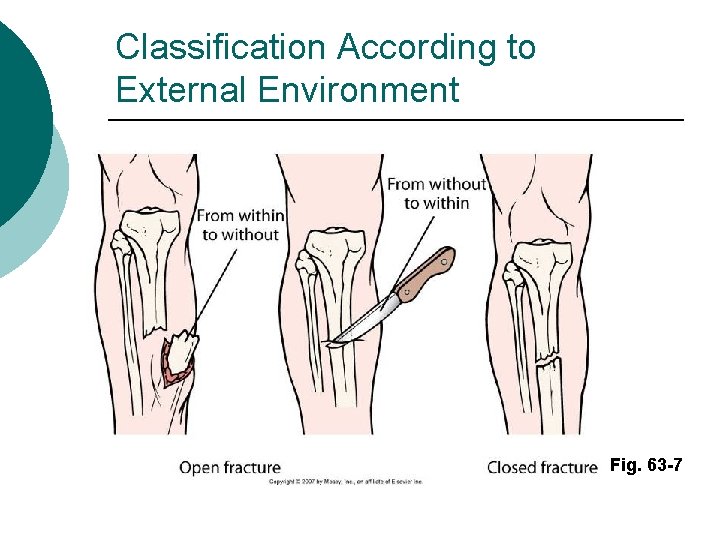
Classification According to External Environment Fig. 63 -7
Anatomic description Comminution is the measure of the number of pieces of broken bone that there are. ¡ Examples: ¡ l l l non-comminuted mildly comminuted severely comminuted
Anatomic description - Location Anatomic location of fracture usually described by giving the bone involved and location on the bone ¡ Examples: distal radial shaft, proximal 1/3 humeral shaft, intraarticular distal tibial ¡
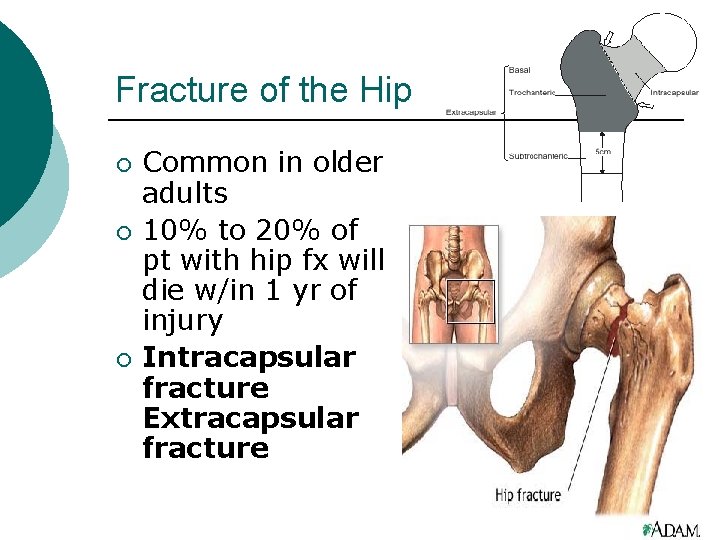
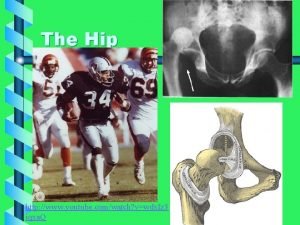
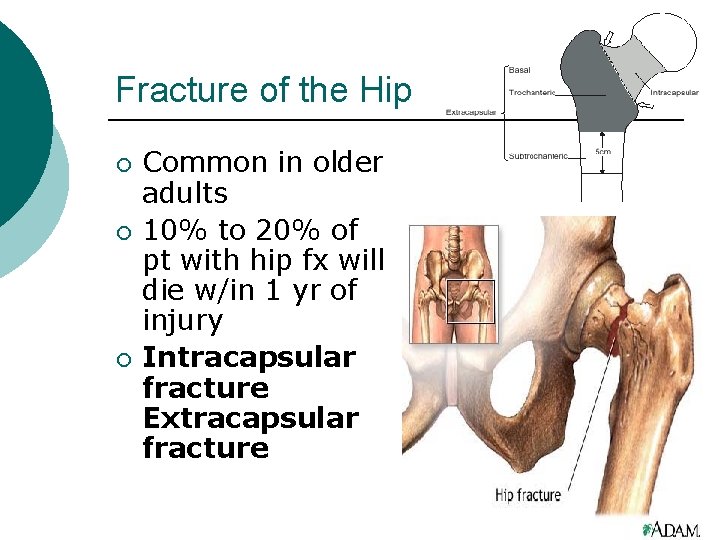
Fracture of the Hip ¡ ¡ ¡ Common in older adults 10% to 20% of pt with hip fx will die w/in 1 yr of injury Intracapsular fracture Extracapsular fracture
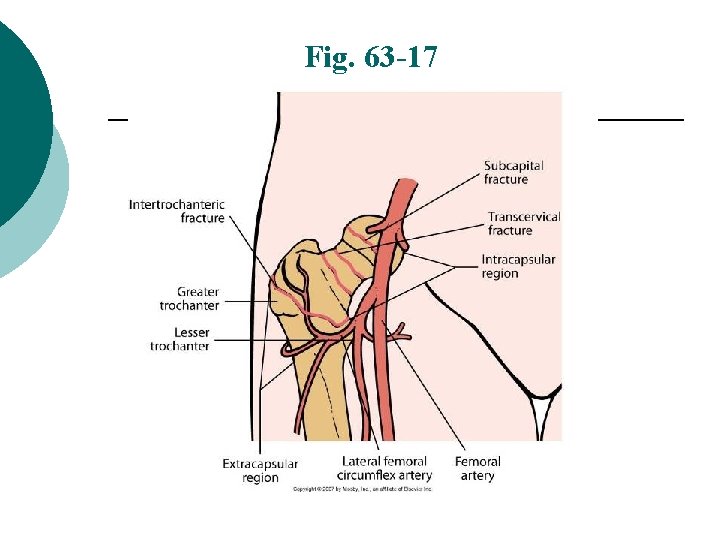
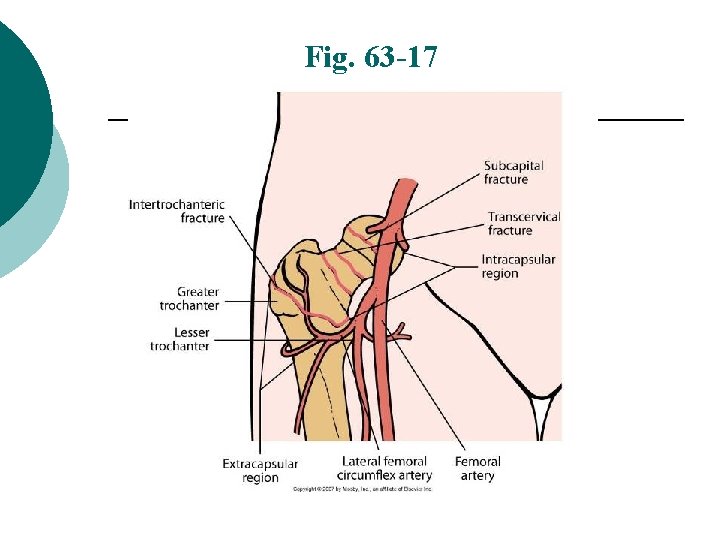
Fig. 63 -17
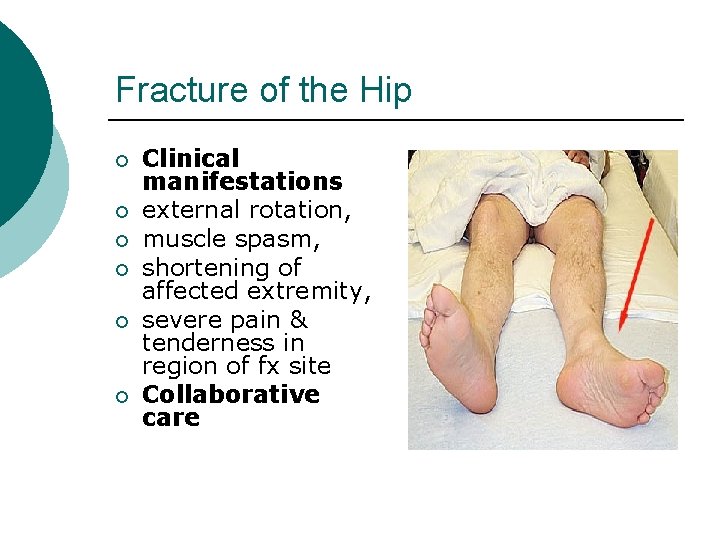
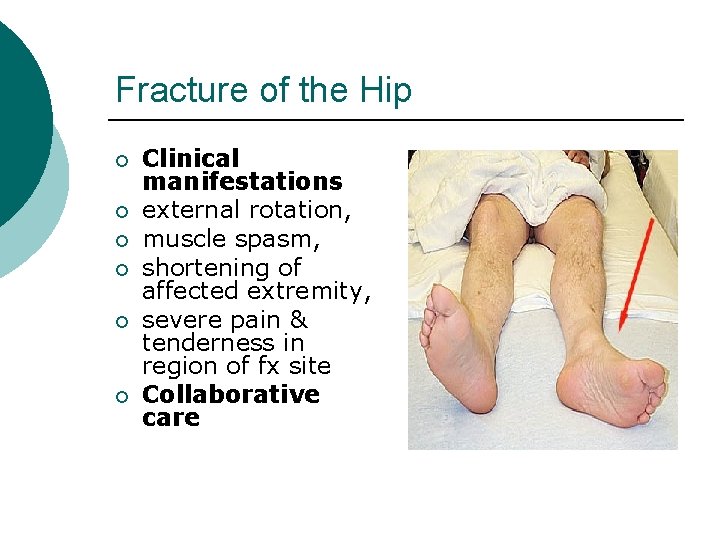
Fracture of the Hip ¡ ¡ ¡ Clinical manifestations external rotation, muscle spasm, shortening of affected extremity, severe pain & tenderness in region of fx site Collaborative care
Gerontology Considerations Hip Fracture ¡ ¡ ¡ Inadequacy of local tissue shock absorbers Underlying skeletal strength Interventions to reduce hip fx in elderly: - Calcium & Vit D supplementation - estrogen replacement - bisphonate drug therapy
Hip Fx Treatment ORIF ¡ Preoperative management ¡ Postoperative management ¡
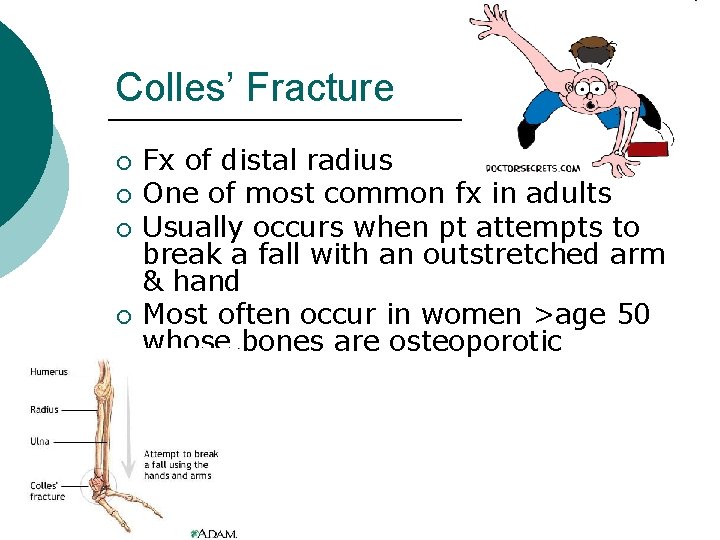
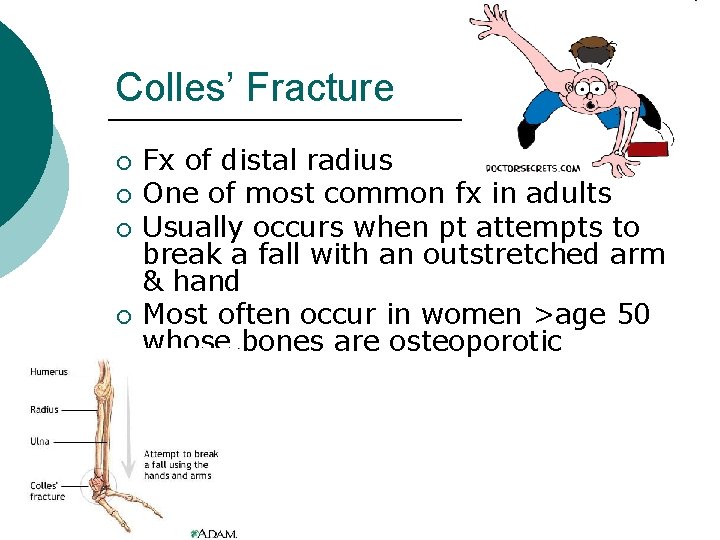
Colles’ Fracture ¡ ¡ Fx of distal radius One of most common fx in adults Usually occurs when pt attempts to break a fall with an outstretched arm & hand Most often occur in women >age 50 whose bones are osteoporotic

Colles’ Fracture ¡ Clinical Manifestations: • Complications: - vascular insufficiency - carpal tunnel syndrome • Management:
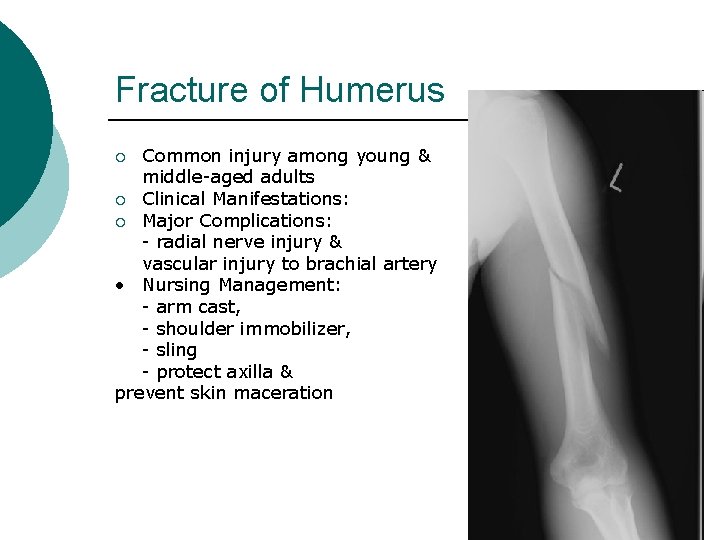
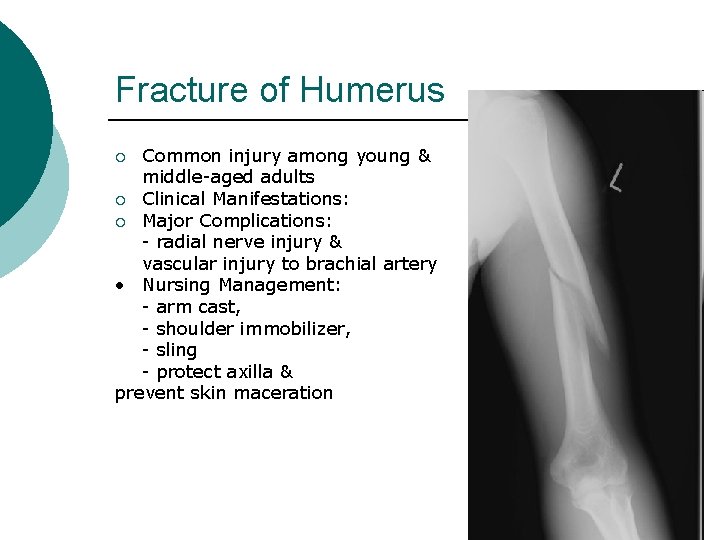
Fracture of Humerus Common injury among young & middle-aged adults ¡ Clinical Manifestations: ¡ Major Complications: - radial nerve injury & vascular injury to brachial artery • Nursing Management: - arm cast, - shoulder immobilizer, - sling - protect axilla & prevent skin maceration ¡
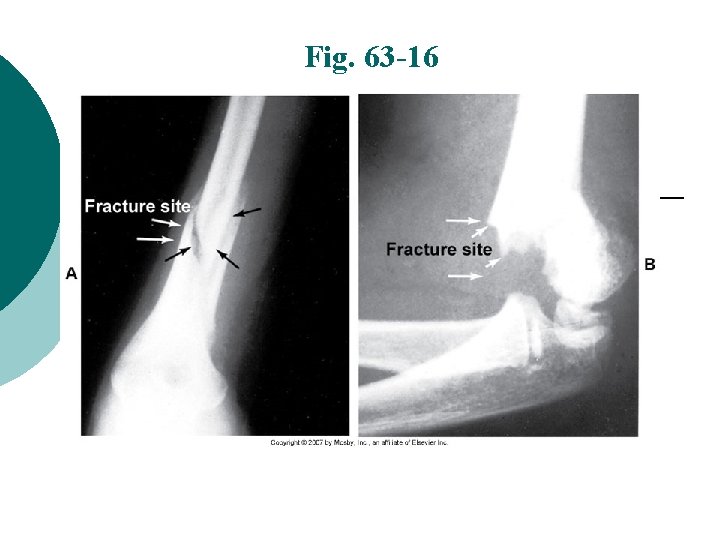
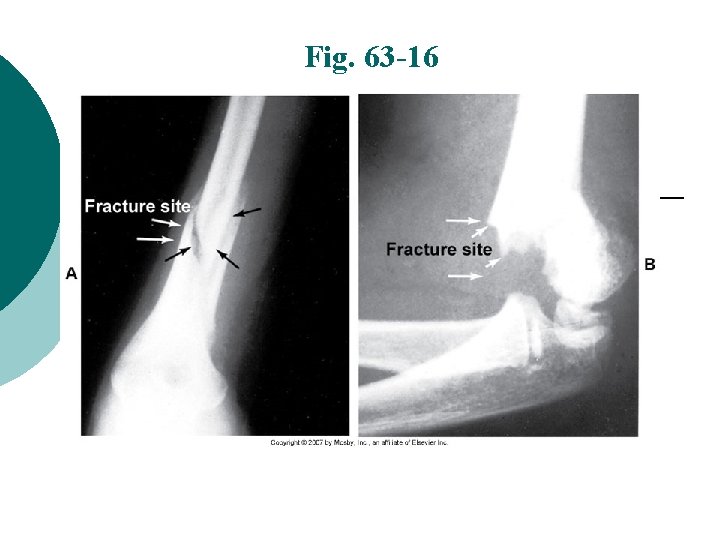
Fig. 63 -16
Pelvis Fracture ¡ ¡ Pelvic fx range from benign to life threatening Small percentage of all fx are pelvic fractures, associated with highest mortality rate May cause serious intraabdominal inj Patients may survive initial pelvic injury, only to die from sepsis, FES, or DVT complications
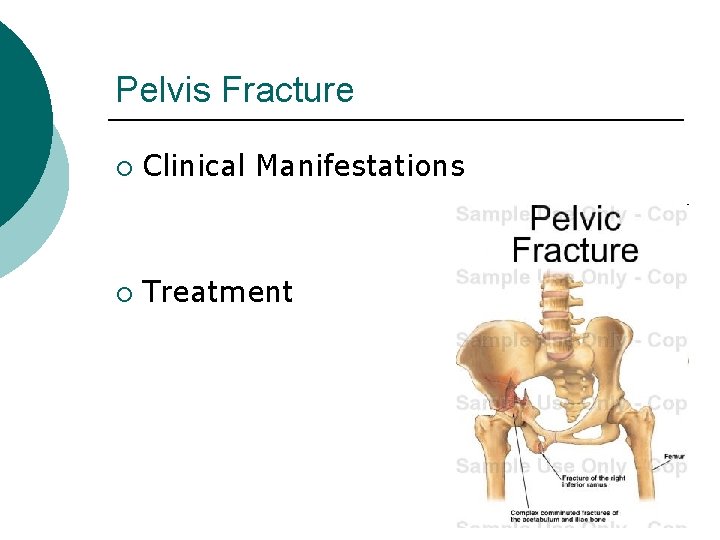
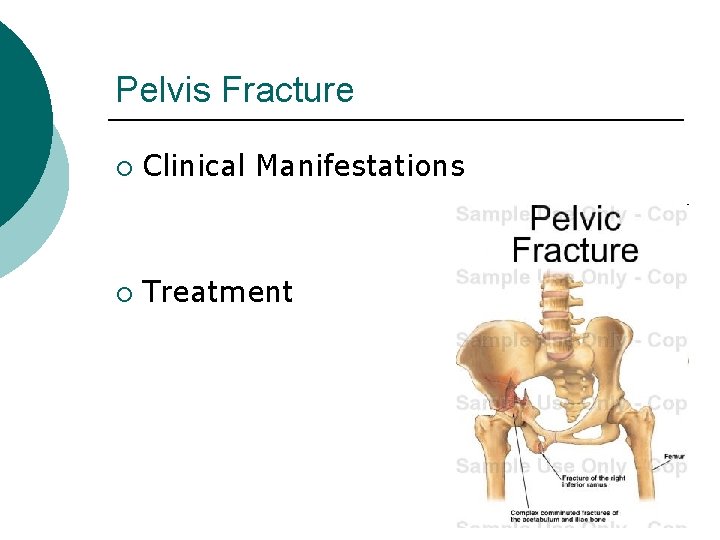
Pelvis Fracture ¡ Clinical Manifestations ¡ Treatment
Stable Vertebral Fractures ¡ Fracture or fragment not likely to move or cause spinal cord damage l ¡ ¡ Often in lumbar regions Vertebral bodies usually protected from displacement by intact spinal ligaments All spinal injuries should initially be considered unstable & potentially serious until tests are performed & fx is determined to be stable
Facial Fractures ¡ Primary concern: - establish & maintain patent airway - provide adequate ventilation by removal of foreign material & blood - alternative airway may be needed if patent airway cannot be maintained - all patients with facial injuries should be ruled out for cervical injury
Fracture Clinical Manifestations ¡ Mechanism of injury associated with numerous signs and symptoms Edema & Swelling l Pain & Tenderness l Muscle Spasm l Deformity l Ecchymosis/Contusion l Loss of Function l Crepitation l
Fracture Clinical Manifestations Fracture may not be accompanied by obvious bone deformity ¡ Immobilize extremity if fracture is suspected ¡ Unnecessary movement l Increases soft tissue damage l May convert a closed fracture to open ¡
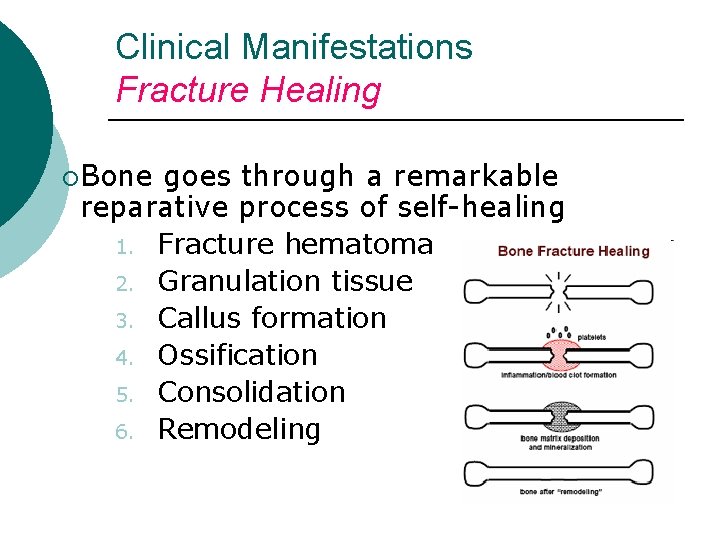
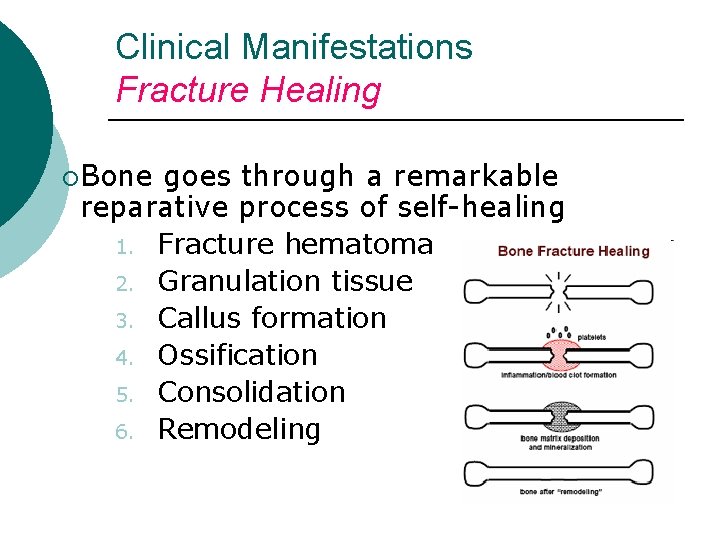
Clinical Manifestations Fracture Healing ¡Bone goes through a remarkable reparative process of self-healing 1. Fracture hematoma 2. Granulation tissue 3. Callus formation 4. Ossification 5. Consolidation 6. Remodeling
Clinical Manifestations Fracture Healing ¡ Factors influencing healing ¡Age ¡Initial displacement ¡Immobilization ¡Implants ¡Site ¡Infection ¡Hormones ¡Blood supply to area
Clinical Manifestations Fracture Healing ¡ ¡ Fracture healing may l Not occur in the expected time ¡ Delayed union l Not occur at all ¡ Nonunion Healing time of fractures increases with age
Collaborative Care ¡ Overall goals of fracture treatment Anatomic realignment of bone fragments l Immobilization to maintain realignment l Restoration of normal or nearnormal function of injured parts l
Nursing Management Nursing Assessment ¡ Initial treatment Splint joints l Check neurovascular status l Elevate l Do not attempt to straighten fractured or dislocated joint l Do not manipulate protruding bone ends l
Nursing Management Nursing Assessment ¡ ¡ ¡ ¡ ¡ Monitor for 5 P’s Deformity of affected limb Edema and ecchymoses Muscle spasm Tenderness and pain Loss of function Numbness, tingling, loss of distal pulse Grating (crepitus) Open wound over injured site, exposure of bone
Nursing Management Nursing Assessment ¡ Initial treatment ice packs l x-rays l Mark location of pulses l Splint fracture site l Elevate l
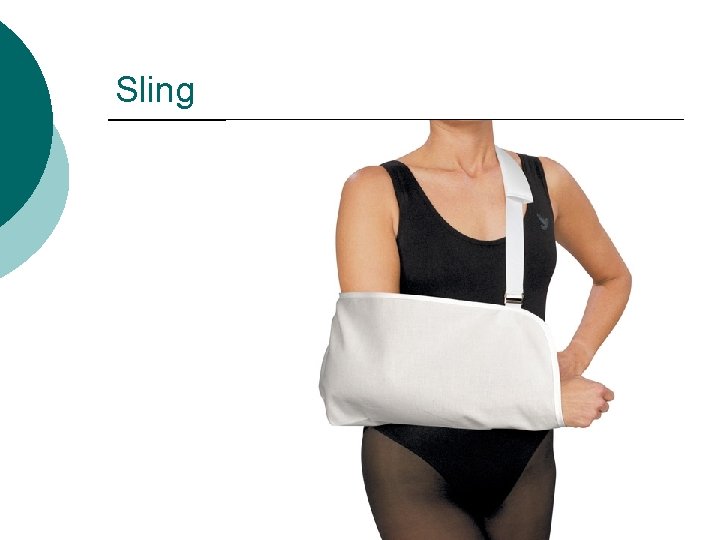
Initial Care ¡ Immobilize +Maintain alignment l l ¡ Splints Slings Cast Manual Traction Elevate

Splint
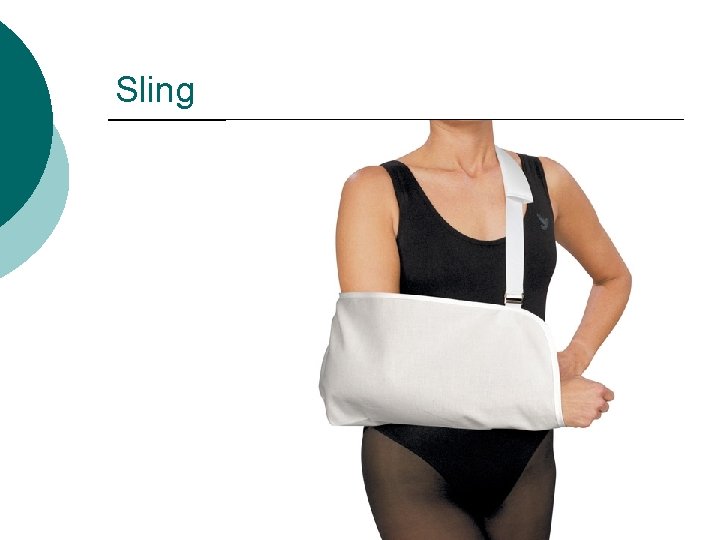
Sling
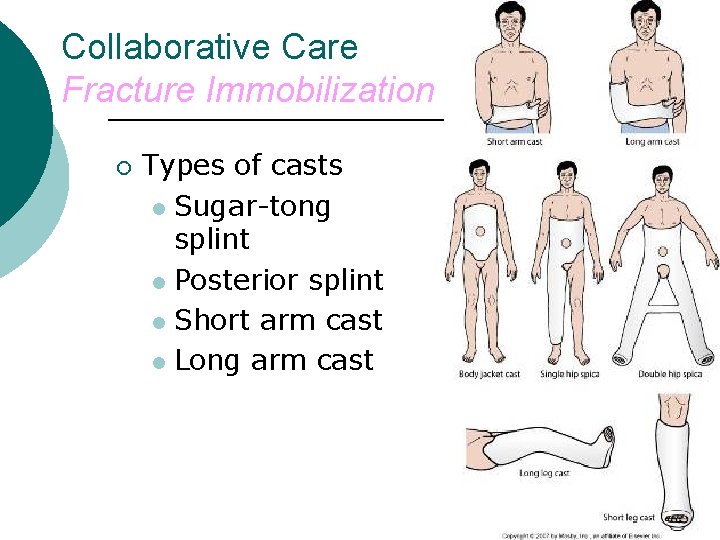
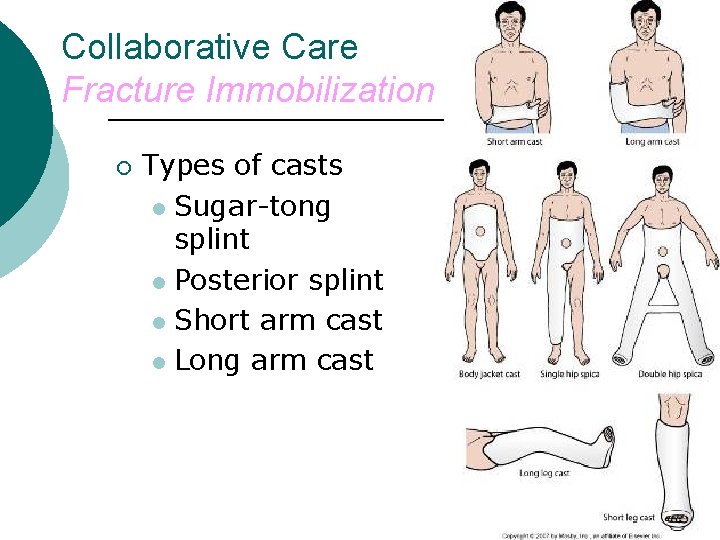
Collaborative Care Fracture Immobilization ¡ Types of casts l Sugar-tong splint l Posterior splint l Short arm cast l Long arm cast
Collaborative Care Traction Application of a pulling force to an injured part of body or extremity while counter traction pulls in opposite direction ¡ Purpose of any traction ¡ l l Prevent or ↓ muscle spasm Immobilize joint or part of body ↓ a fracture or dislocation Treat a pathologic joint condition
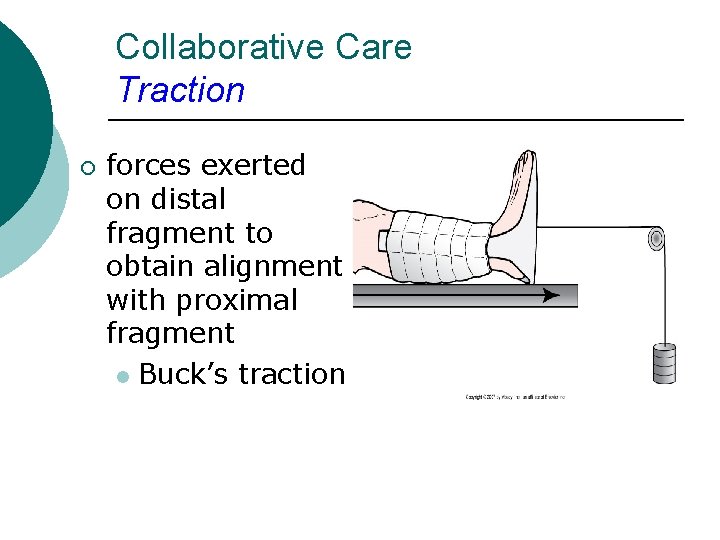
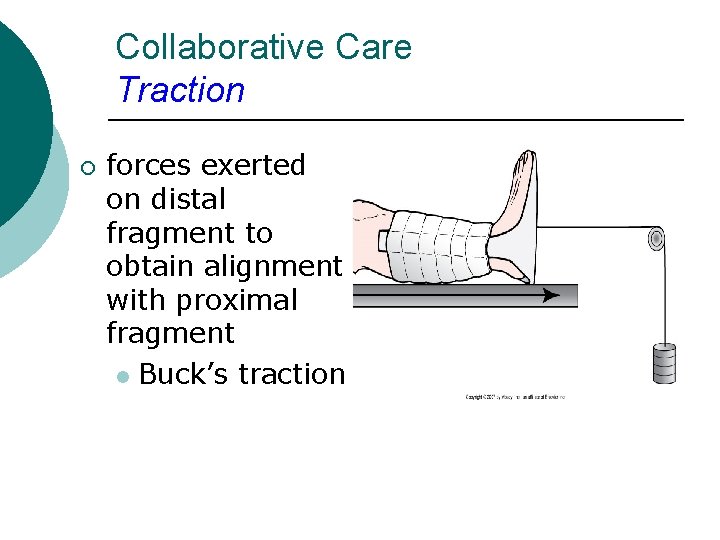
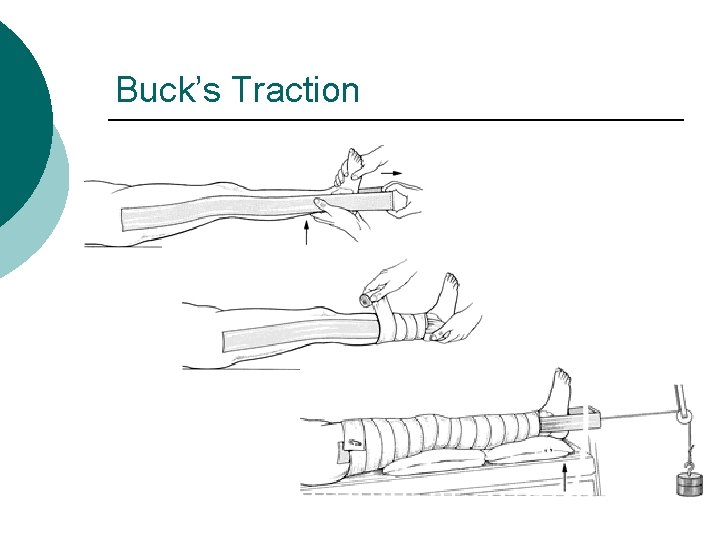
Collaborative Care Traction ¡ forces exerted on distal fragment to obtain alignment with proximal fragment l Buck’s traction
Traction
Collaborative Care Traction ¡ Traction also indicated to l l l Provide immobilization Reduce muscle spasm Expand a joint space During arthroscopic procedures ¡ Before major joint reconstruction ¡
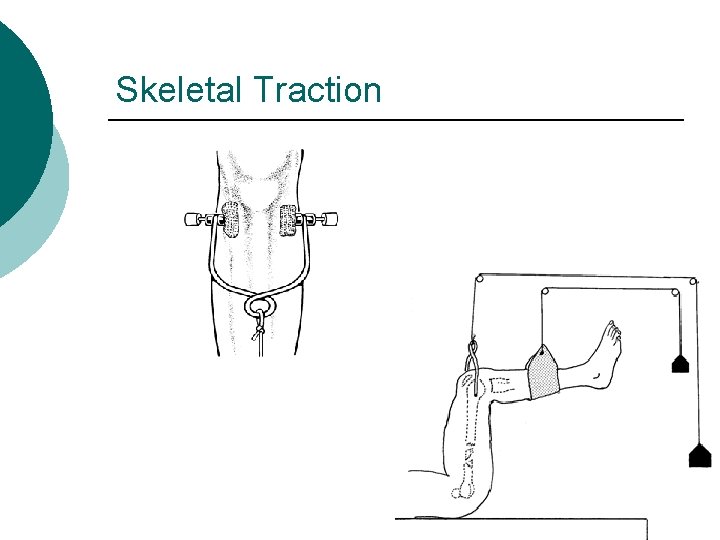
Collaborative Care Traction ¡ Two most common types of traction l l Skin traction Skeletal traction
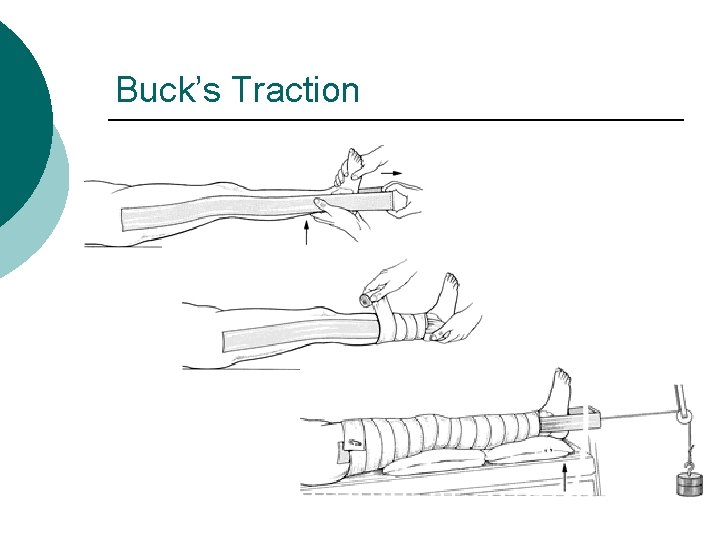
Buck’s Traction
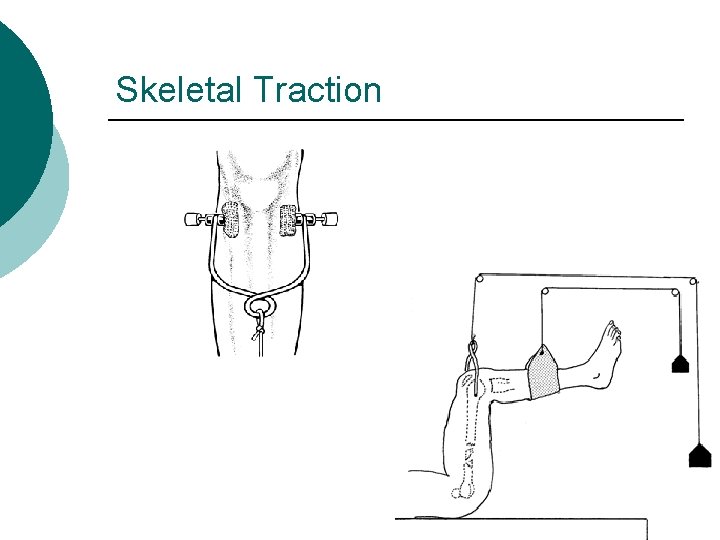
Skeletal Traction
Application of Skin Traction ¡ http: //www. youtube. com/watch? v= 2 ZEWz_Ps 7 vo&feature=related
Collaborative Care Fracture Reduction ¡ Closed l l reduction manual realignment of bone without surgery Traction and counter-traction Performed while patient is under local or general anesthesia Need to be splinted or casted after
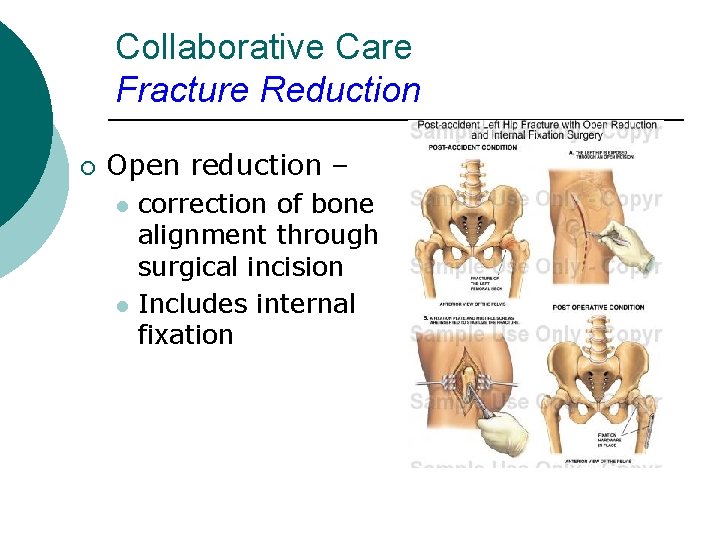
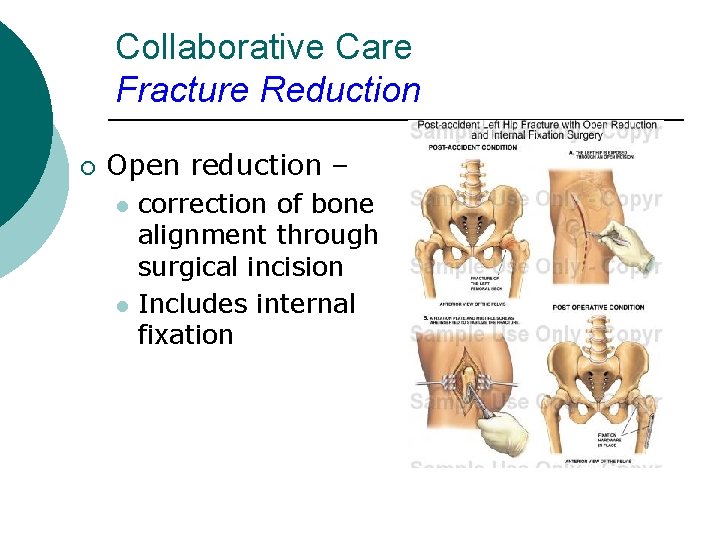
Collaborative Care Fracture Reduction ¡ Open reduction – l l correction of bone alignment through surgical incision Includes internal fixation
Collaborative Care Fracture Immobilization ¡ Internal fixation devices: surgically inserted at time of realignment l l l Pins Plates Screws Wires Rods Nails
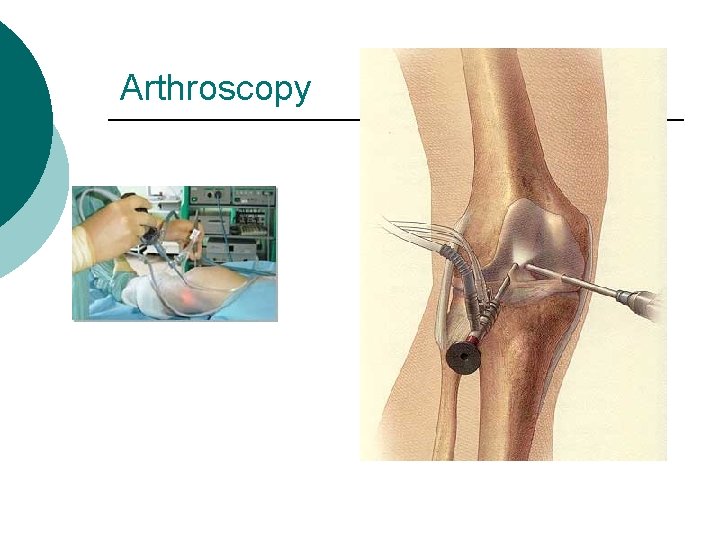
Arthroscopy For visualization inside the joint ¡ Dx or repair ¡ Local or may be general anesthesia ¡ NPO 8 hours pre op ¡ Antibiotics - prn ¡
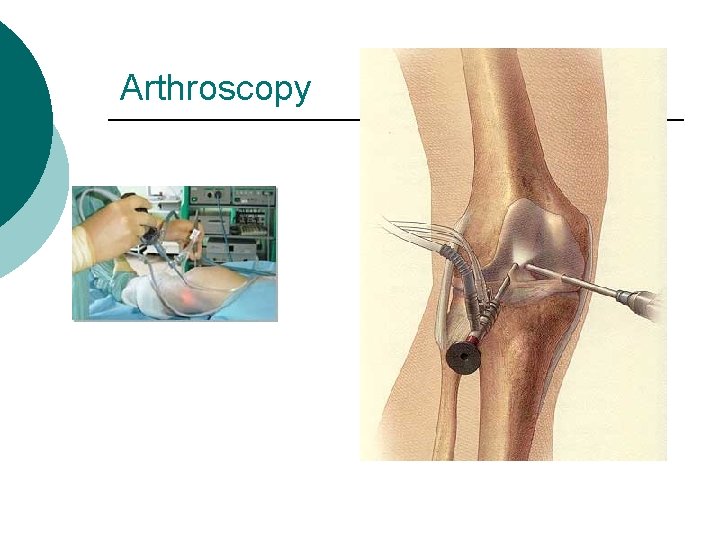
Arthroscopy
Nursing Assessments Fracture ¡ CSMT’s l l l ¡ AKA neurovascular checks Circulation Sensation Motion temperature Pin sites with traction
Collaborative Care Nutritional Therapy ¡ ¡ ¡ Patient’s dietary requirements must include l Ample protein l Vitamins l Calcium, Phosphorus, Magnesium Adequate fluid intake: 2000 to 3000 ml/day High-fiber diet with fruits and vegetables
Collaborative Care Drug Therapy up to date with Tetanus ¡ Open fracture need bonepenetrating abx: ¡ cephalosporins – ¡ l kefzol, ancef
Complications of Fractures Majority heal without complication ¡ If death occurs, usually result of ¡ l l ¡ Damage to underlying organs and vascular structures Complications of fracture or immobility May be either direct or indirect
Complications of Fractures ¡ Direct complications l Problems with bone infection l Bone union l Avascular necrosis ¡ Fat embolism ¡ Traumatic or hypovolemic shock ¡ Indirect complications l Blood vessels and nerve damage ¡ Compartment syndrome ¡ Deep vein thrombosis
Complications of Fractures ¡ Infection l l l High incidence in open fractures and soft tissue injuries Massive or blunt soft tissue injury often has more serious consequences than fractures Devitalized and contaminated tissue: ideal medium for pathogens Costly Treatment Osteomyelitis may become chronic
Collaborative Care Open fractures require aggressive surgical debridement ¡ Extent of soft tissue damage determines whether ¡ l l l Wound will be closed at time of surgery Drainage may be necessary Skin grafting may be needed
Compartment Syndrome ¡ http: //www. youtube. com/watch? v= 4 l. KKBWWEr. HM
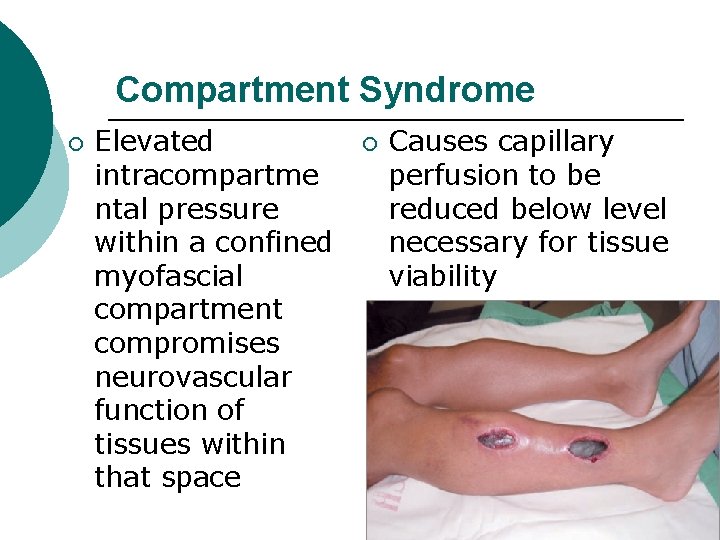
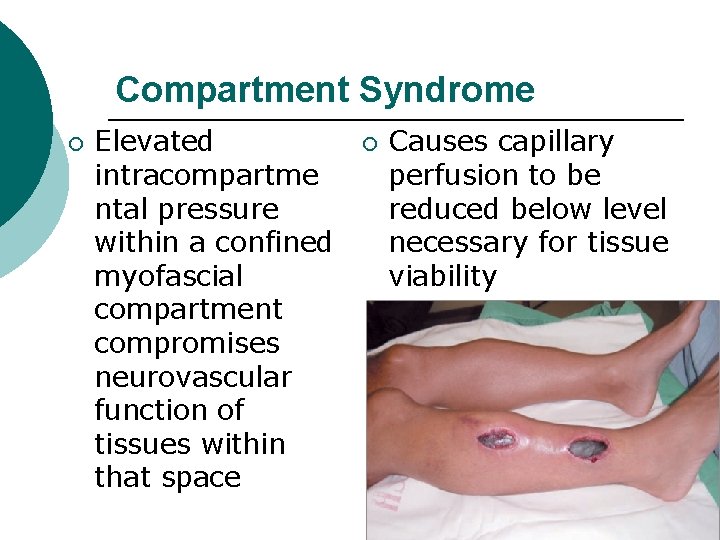
Compartment Syndrome ¡ Elevated intracompartme ntal pressure within a confined myofascial compartment compromises neurovascular function of tissues within that space ¡ Causes capillary perfusion to be reduced below level necessary for tissue viability
Compartment Syndrome ¡ Two types include: - ↓ compartment size resulting from restrictive dressings, splints, casts, excessive traction, or premature closure of fascia - ↑ compartment content related to bleeding, edema, chemical response to snakebite, or IV infiltration
Compartment Syndrome ¡ Associated with trauma - fractures - extensive soft tissue damage - crush injury - reperfusion syndrome - severe burns - venomous snakebite - following knee or leg surgery - prolonged pressure on a muscle compartment - massive infiltration of IV fluids -
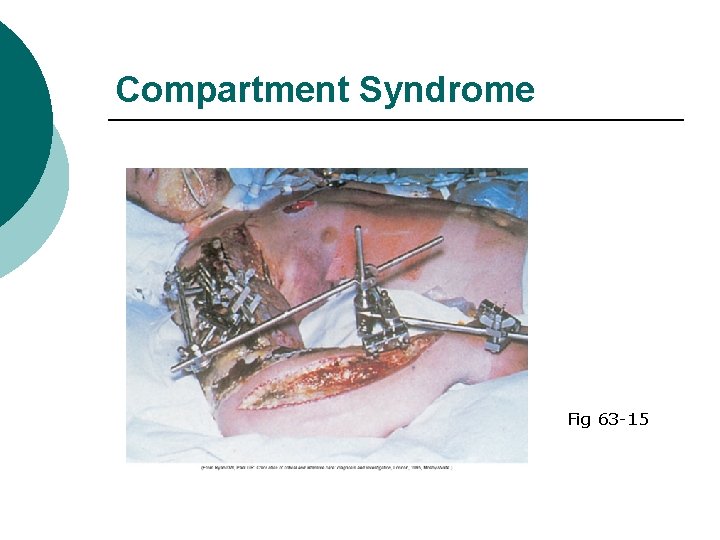
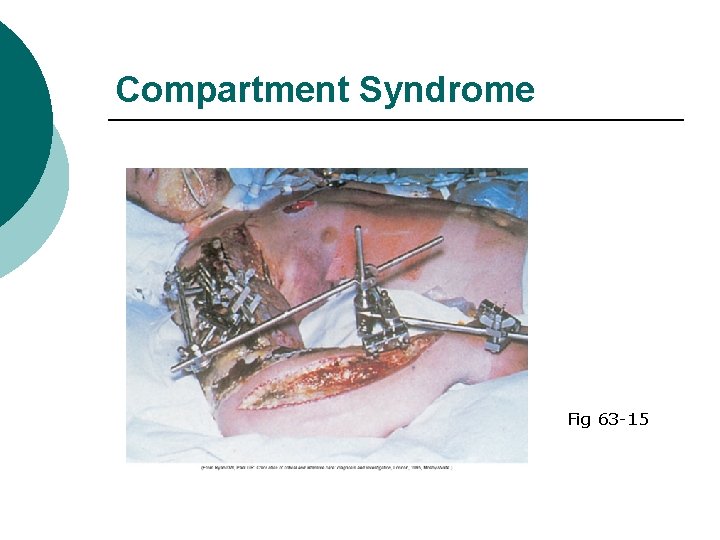
Compartment Syndrome Fig 63 -15
Compartment Syndrome Clinical Manifestations & Nsg Management Early recognition and treatment essential ¡ Ischemia can occur within 4 to 12 hours after onset ¡ Regular neurovascular assessments ¡
Compartment Syndrome Clinical Manifestations ¡ Six Ps are characteristic of impending compartment syndrome 1. 2. 3. 4. 5. 6. P P P
Compartment Syndrome Clinical Manifestations & Nsg Mgt Assess urine output ¡ Acute renal failure ¡ Myoglobin released can obstruct renal tubules ¡ Common signs of myoglobinuria ¡ l l Dark reddish brown urine Clinical manifestations associated with acute renal failure
Compartment Syndrome Collaborative Care ¡ ¡ ¡ Extremity SHOULD NOT be elevated above heart level DO NOT apply cold compresses Remove or loosen bandage or bivalve cast Reduction in traction weight may ↓ external circumferential pressures Surgical decompression may be necessary Severe compartment syndrome may require amputation
Venous Thrombosis ¡ Precipitating factors l ¡ ¡ Venous stasis Aggravated by inactivity of muscles that normally assist in pumping action of venous blood Instruct patient to l l Wear compression gradient stockings Move fingers or toes of affected extremity against resistance and perform ROM exercises
Venous Thrombosis Prophylactic anticoagulant drugs may be ordered ¡ Low-molecular-weight heparin (lovenox) frequently used ¡ Newer class of antithrombotic drugs - fondaparinux (arixtra) ¡
References Hockenberry, M. J. & Wilson, D. (2015). Wong’s Nursing care of infants and children (10 th ed. ). St. Louis, MO: Mosby. Lewis, S. , Heitkemper, M. & Dirksen, S. (2014). Medical Surgical Nursing: Assessment and Management of Clinical Problems (9 th ed. ). St. Louis, MO: Mosby Potter, K (2009) Musculoskeletal. Presented at Evergreen Valley College Touhy, T. & Jett, K. (2014). Ebersole & Hess’ Gerontological Nursing Healthy Aging (4 th Ed. ) St. Louis: Mosby/Elsevier
 Skeletal traction femur
Skeletal traction femur Late complications of fracture
Late complications of fracture Classification of open fractures
Classification of open fractures Fracture supracondylienne coude
Fracture supracondylienne coude Youtube
Youtube Panfacial fractures sequencing
Panfacial fractures sequencing Radial fractures glass
Radial fractures glass Pronation main
Pronation main Types of fractures with pictures
Types of fractures with pictures Classification fracture du bassin
Classification fracture du bassin Acetabulum ossification
Acetabulum ossification Classification of open fractures
Classification of open fractures Glass fracture analysis
Glass fracture analysis Weber classification
Weber classification Types of fractures with pictures
Types of fractures with pictures Chest tube water seal vs suction
Chest tube water seal vs suction Types of glass fractures
Types of glass fractures Dr sukhpal singh
Dr sukhpal singh Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Types of fractures with pictures
Types of fractures with pictures Primary bone vs secondary bone
Primary bone vs secondary bone Olecranon fractures irving
Olecranon fractures irving How have plants adapted to the rainforest
How have plants adapted to the rainforest Red blood cells are
Red blood cells are How are giraffes long necks adapted to their lifestyle
How are giraffes long necks adapted to their lifestyle The two brothers adapted
The two brothers adapted Chaparral biomass
Chaparral biomass What are spermopsida
What are spermopsida Adapted with permission from
Adapted with permission from Adapted from the internet
Adapted from the internet Adaptation of camel in points
Adaptation of camel in points The outsiders adapted for struggling readers
The outsiders adapted for struggling readers In what ways have the highland maya adapted to modern life?
In what ways have the highland maya adapted to modern life? Gallant
Gallant Sausage shaped organelles
Sausage shaped organelles This passage is adapted from jane austen
This passage is adapted from jane austen Entities antonym
Entities antonym Xerophytic adaptation
Xerophytic adaptation Thank you pictures for presentation
Thank you pictures for presentation ömpsq
ömpsq Musculoskeletal pronounce
Musculoskeletal pronounce Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Cochrane musculoskeletal group
Cochrane musculoskeletal group Muscle strength scale
Muscle strength scale Contoh soal koding icd 10
Contoh soal koding icd 10 Buck's extension traction
Buck's extension traction Musculoskeletal
Musculoskeletal Musculoskeletal
Musculoskeletal Medical term for top of foot
Medical term for top of foot Chapter 15 musculoskeletal system step by step
Chapter 15 musculoskeletal system step by step Mri
Mri Musculoskeletal system
Musculoskeletal system Musculoskeletal fitness assessment
Musculoskeletal fitness assessment The musculoskeletal system chapter 21
The musculoskeletal system chapter 21 Musculoskeletal integrity
Musculoskeletal integrity Musculoskeletal
Musculoskeletal Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Kode icd 10 fraktur vertebra thorakal
Kode icd 10 fraktur vertebra thorakal Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Objective data for musculoskeletal system
Objective data for musculoskeletal system West coast musculoskeletal
West coast musculoskeletal Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Musculoskeletal system
Musculoskeletal system Sathish srinivasan
Sathish srinivasan Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Chapter 40 musculoskeletal care modalities
Chapter 40 musculoskeletal care modalities Musculoskeletal system
Musculoskeletal system The vision of maya ying lin
The vision of maya ying lin Mot lin blinds
Mot lin blinds Chilin purse
Chilin purse Magistrala lin bmw
Magistrala lin bmw Lin donn
Lin donn Tul tevassut kasr ne demek
Tul tevassut kasr ne demek Lin mobile
Lin mobile Army ranger school packing list
Army ranger school packing list Suzanne lin
Suzanne lin Modelo logaritmico econometria
Modelo logaritmico econometria Yifei lin
Yifei lin V-lin
V-lin