Cardiac Causes of Pediatric Syncope Finding the Needle


- Slides: 46
Cardiac Causes of Pediatric Syncope: Finding the Needle in the Haystack Eric Johnson, MD April 18, 2019
Disclosures § None
Objectives § List the most common causes of syncope in pediatric patients § Describe the mechanism of vasovagal syncope in one sentence § Know what to do if you suspect an arrhythmia (such as SVT) § Identify features that may be related to a lifethreatening cardiac cause
Outline § § Cases Definition Epidemiology Causes – Dysautonomia – Cardiac § Clinical evaluation § When to consider referral
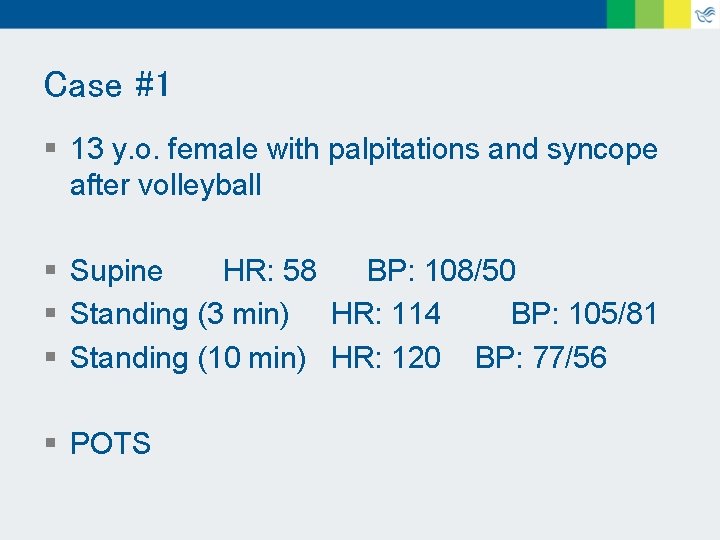
Case #1 § 13 y. o female § Unremarkable medical history § Just finished tryouts for volleyball, was standing in a circle during announcement of who made the varsity team § Felt dizzy and lightheaded, rapid palpitations, and “slumped to the floor, ” losing consciousness for 1 minute § Afterward, she felt weak and had shaky hands for about 15 minutes
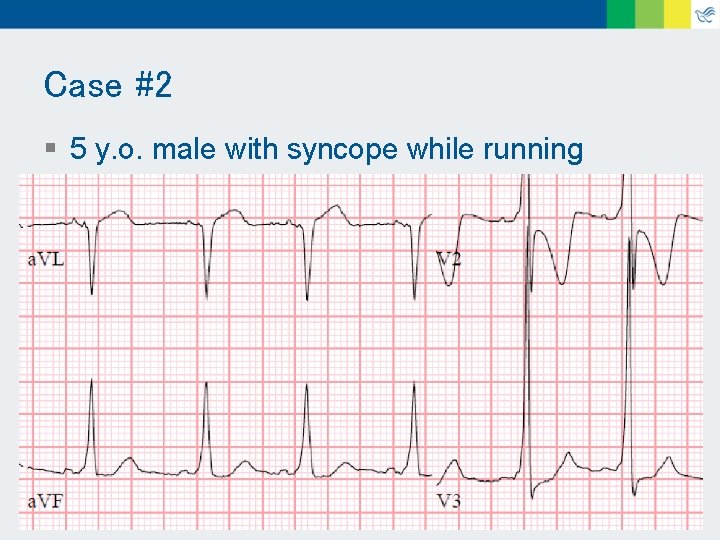
Case #2 § 5 y. o. male § At age 2, he was running during recess, collapsed, neck extended, eyes “rolled back, ” appeared to stop breathing, had fine movements of shoulders and arms, and turned “purple” § Unconscious for 1 minute, seemed confused for a few seconds, then back to baseline § Since then, similar episodes about once a year
Definition § A sudden and transient loss of consciousness and postural tone that reverses without intervention.
Epidemiology § 15 – 25% experience syncope before adulthood § Disproportionately affects teenage females § 3% of all pediatric ED visits § Most cases are benign § Rarely, syncope is a harbinger of a lifethreatening condition, usually cardiac
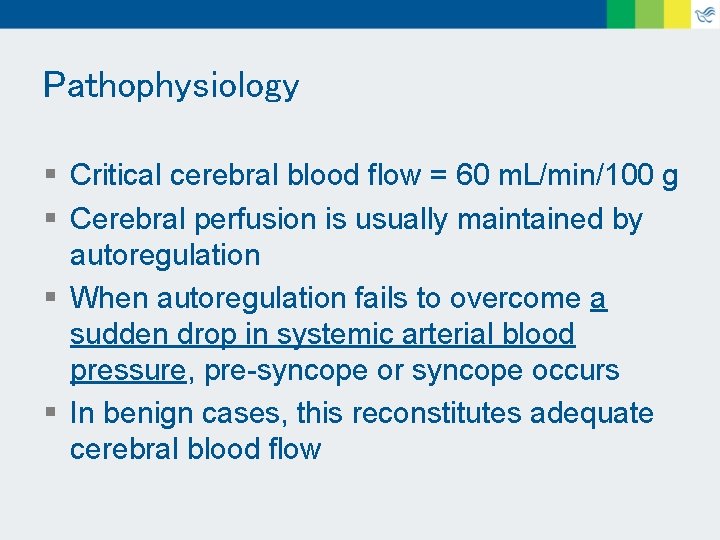
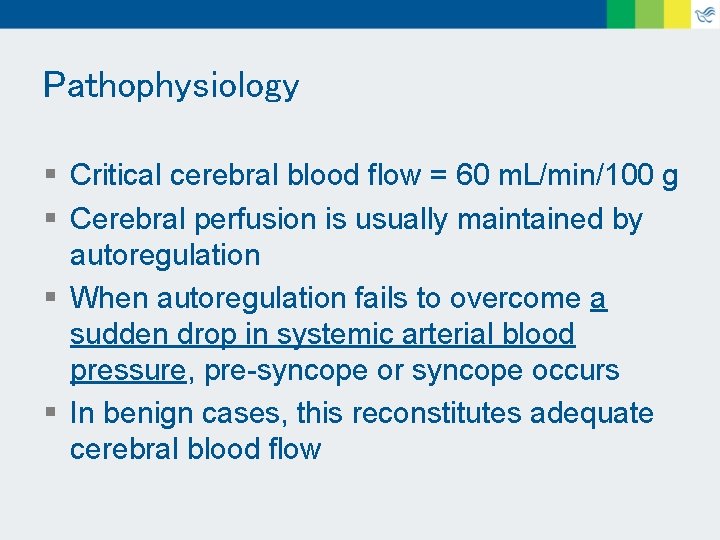
Pathophysiology § Critical cerebral blood flow = 60 m. L/min/100 g § Cerebral perfusion is usually maintained by autoregulation § When autoregulation fails to overcome a sudden drop in systemic arterial blood pressure, pre-syncope or syncope occurs § In benign cases, this reconstitutes adequate cerebral blood flow

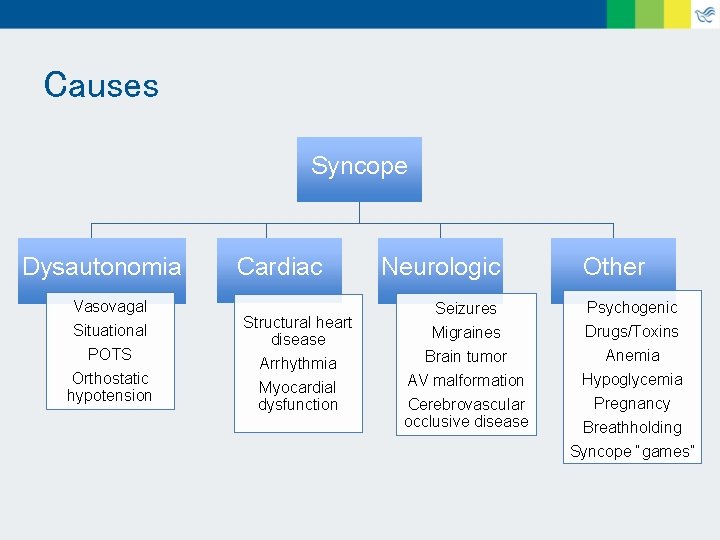
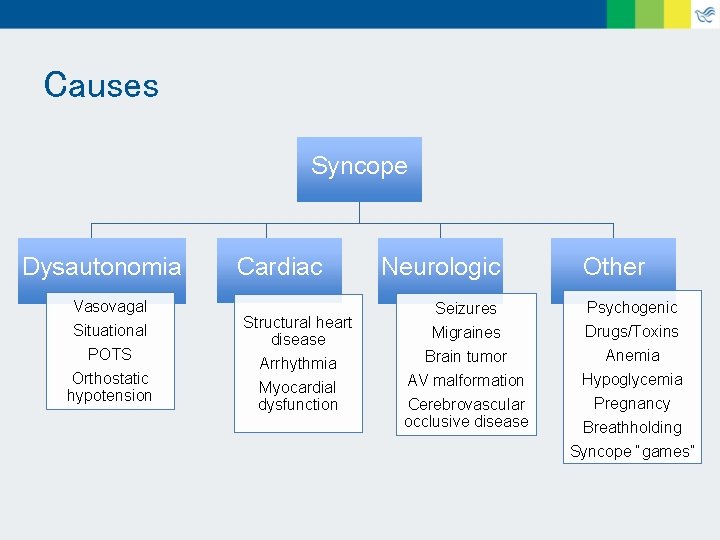
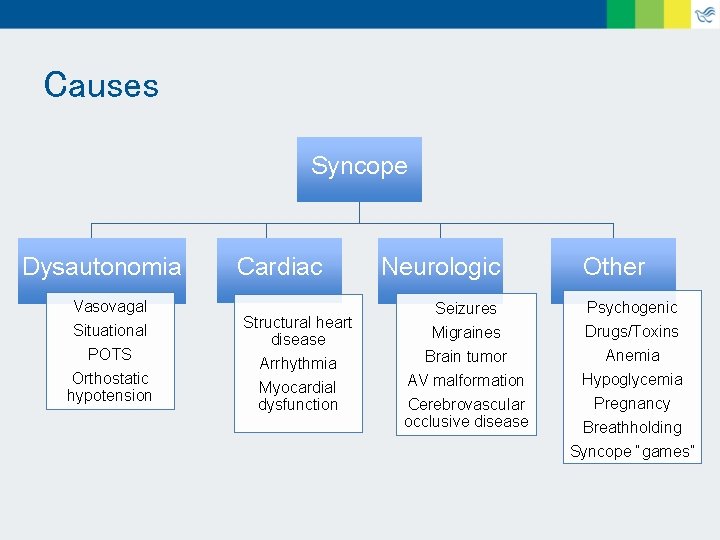
Causes Syncope Dysautonomia Vasovagal Situational POTS Orthostatic hypotension Cardiac Structural heart disease Arrhythmia Myocardial dysfunction Neurologic Other Seizures Migraines Psychogenic Drugs/Toxins Brain tumor AV malformation Cerebrovascular occlusive disease Anemia Hypoglycemia Pregnancy Breathholding Syncope “games”
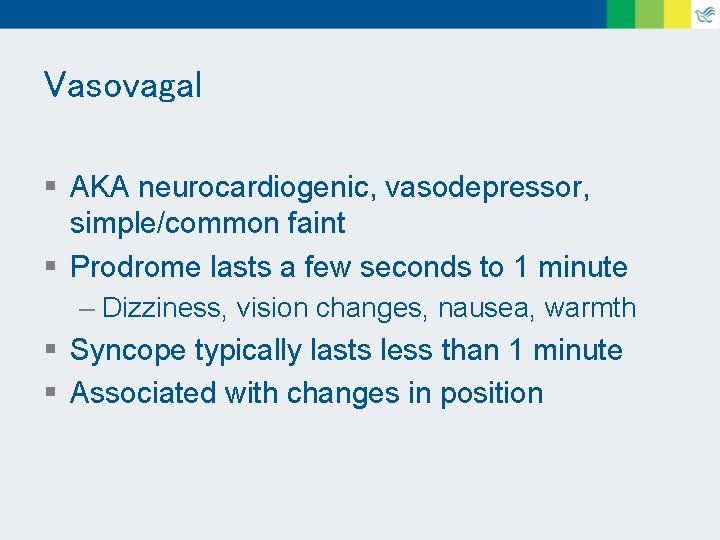
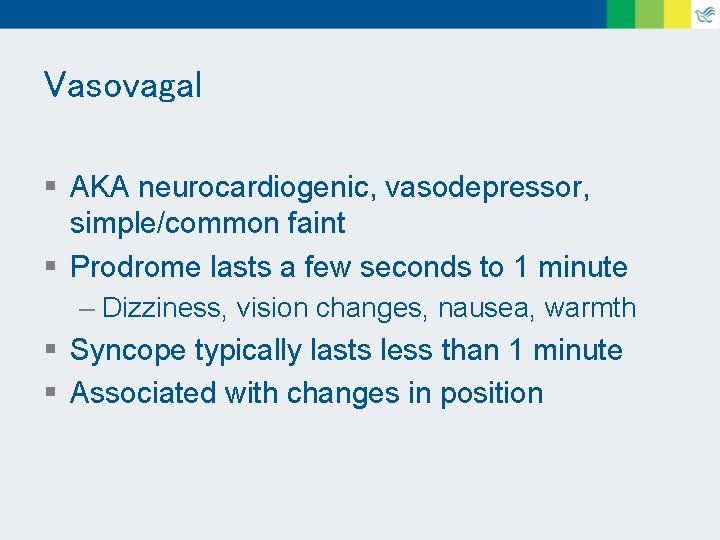
Vasovagal § AKA neurocardiogenic, vasodepressor, simple/common faint § Prodrome lasts a few seconds to 1 minute – Dizziness, vision changes, nausea, warmth § Syncope typically lasts less than 1 minute § Associated with changes in position
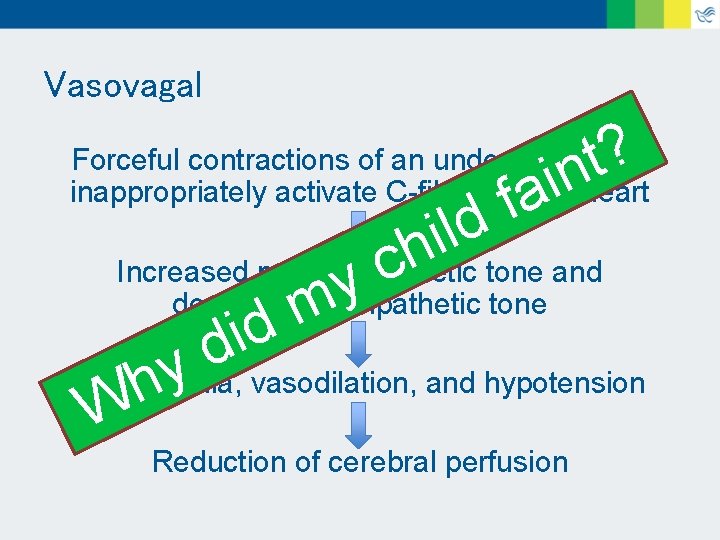
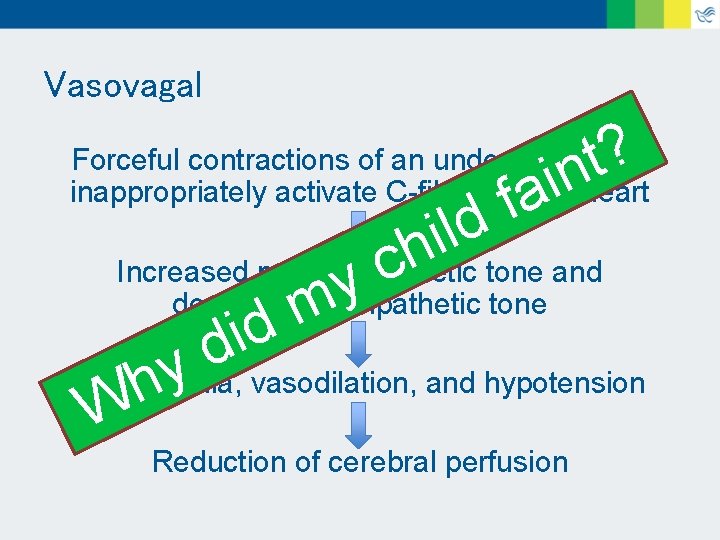
Vasovagal ? t in Forceful contractions of an underfilled heart inappropriately activate C-fibers in the heart a f ld i h tone and Increased parasympathetic c y decreased sympathetic tone m d i d y vasodilation, and hypotension Bradycardia, h W Reduction of cerebral perfusion
Vasovagal § “The nerves that help regulate your child’s heart rate and blood pressure were not working properly, which led to a temporary decrease in blood flow to the brain, and subsequent loss of consciousness. ”
Situational § Pathophysiology and clinical presentation is similar to vasovagal § A specific trigger initiates the cascade of autonomic events leading to syncope § Sight of blood, pain, fear, hair brushing, urination
POTS § Postural orthostatic tachycardia syndrome § Within 10 minutes of assuming an upright position. . . – HR increase 30 -40, or > 120 beats/min § Associated with exercise intolerance, chronic fatigue, GI problems, headaches, poor sleep, difficulty concentrating, psychological problems § Female: male = 5: 1
Orthostatic hypotension § Within 3 minutes of assuming an upright position. . . – Decrease in systolic BP > 20 mm. Hg – Decrease in diastolic BP > 10 mm. Hg § Normal adrenergic vasoconstriction is inadequate § Associated with prolonged bed rest or standing
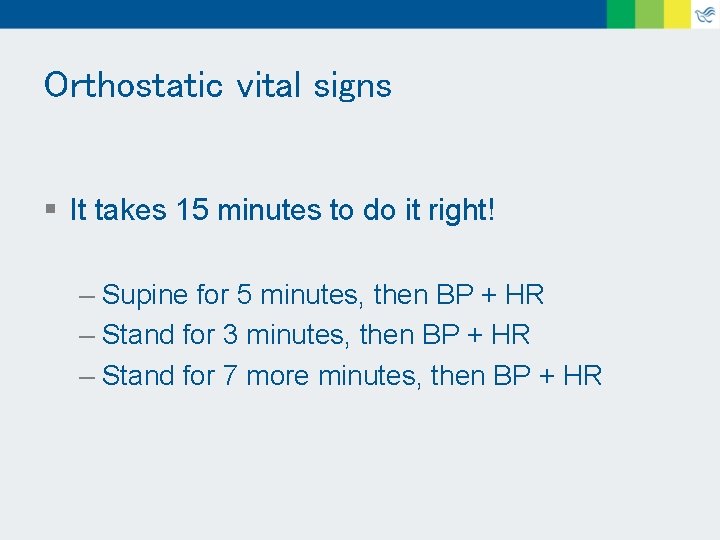
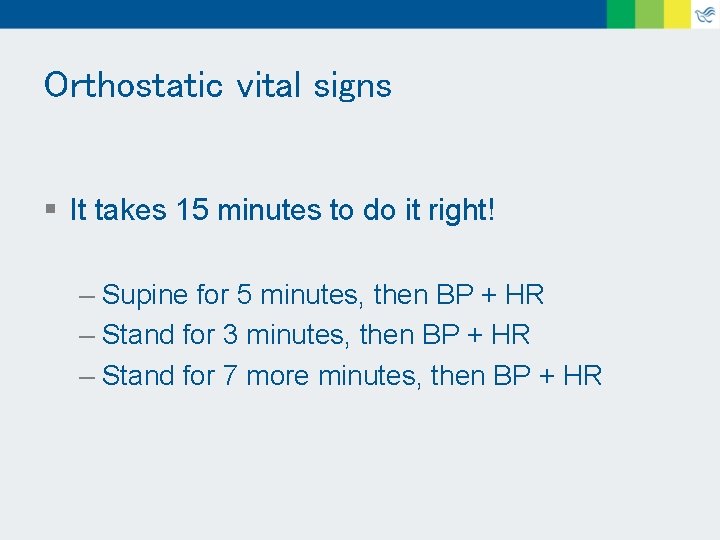
Orthostatic vital signs § It takes 15 minutes to do it right! – Supine for 5 minutes, then BP + HR – Stand for 3 minutes, then BP + HR – Stand for 7 more minutes, then BP + HR
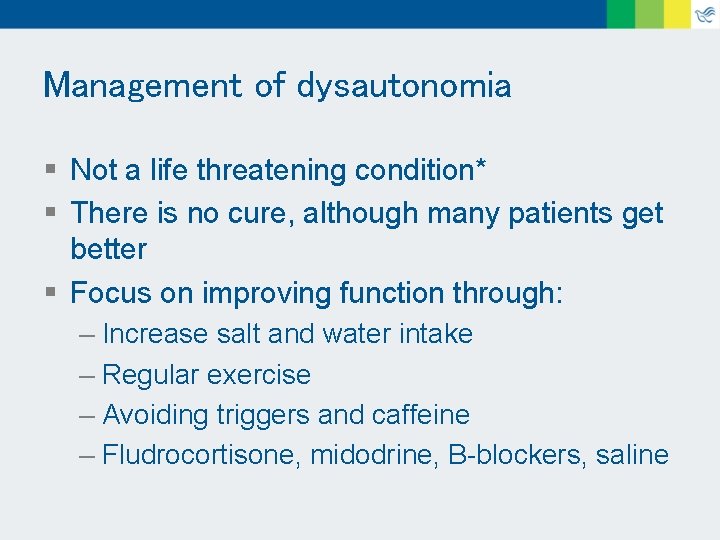
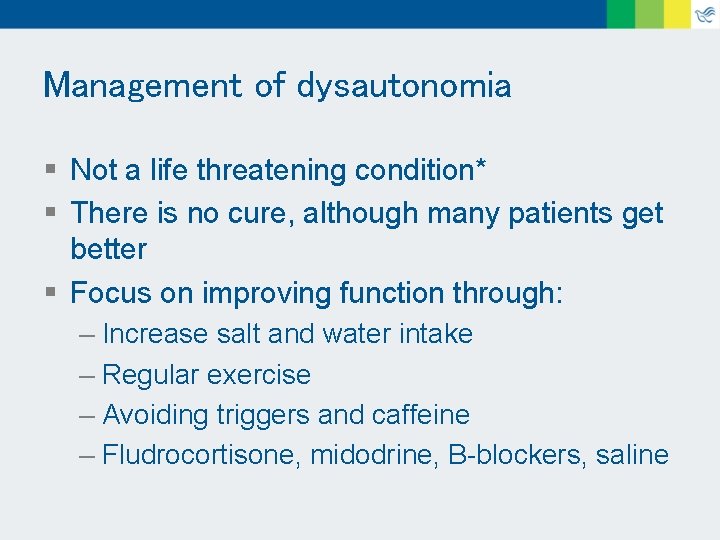
Management of dysautonomia § Not a life threatening condition* § There is no cure, although many patients get better § Focus on improving function through: – Increase salt and water intake – Regular exercise – Avoiding triggers and caffeine – Fludrocortisone, midodrine, B-blockers, saline
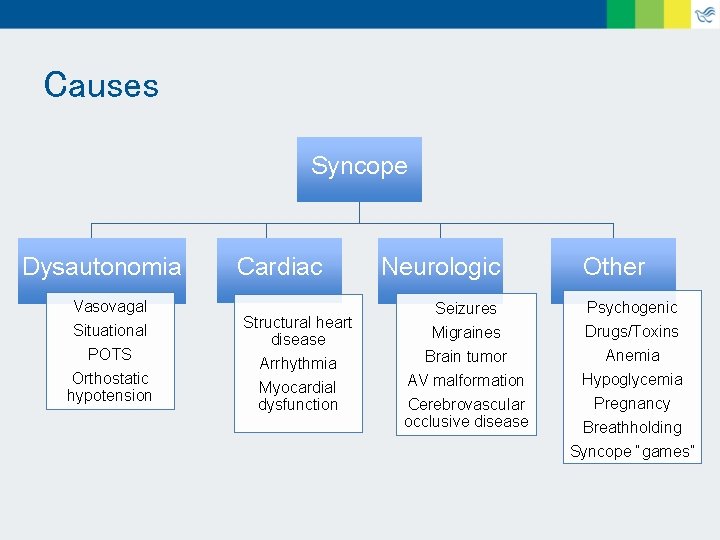
Causes Syncope Dysautonomia Vasovagal Situational POTS Orthostatic hypotension Cardiac Structural heart disease Arrhythmia Myocardial dysfunction Neurologic Other Seizures Migraines Psychogenic Drugs/Toxins Brain tumor AV malformation Cerebrovascular occlusive disease Anemia Hypoglycemia Pregnancy Breathholding Syncope “games”
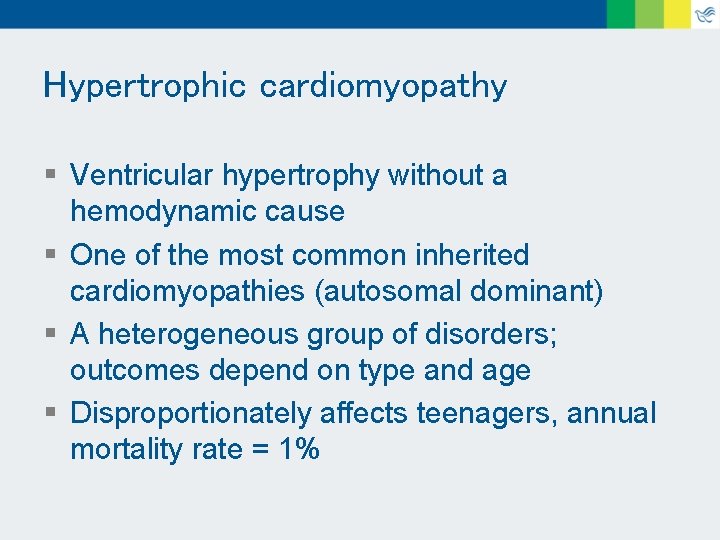
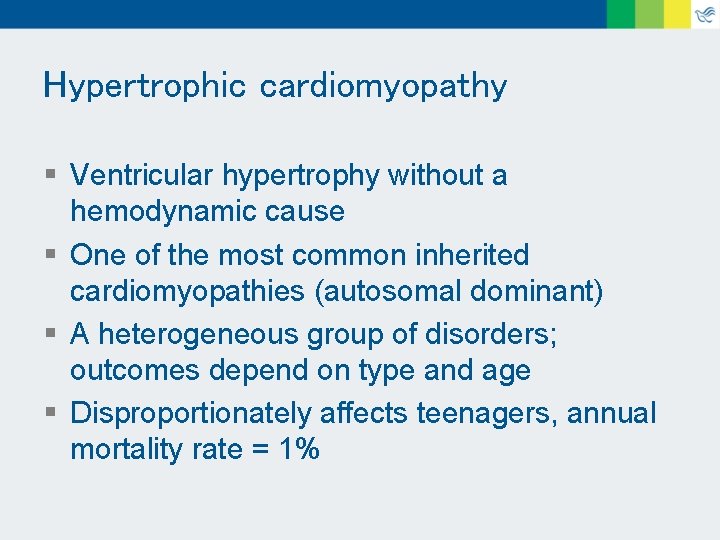
Hypertrophic cardiomyopathy § Ventricular hypertrophy without a hemodynamic cause § One of the most common inherited cardiomyopathies (autosomal dominant) § A heterogeneous group of disorders; outcomes depend on type and age § Disproportionately affects teenagers, annual mortality rate = 1%
Hypertrophic cardiomyopathy § History: – Heart failure (primarily dyspnea on exertion), chest pain (both at rest or with exertion), arrhythmias (both atrial and ventricular), syncope (15 -25% of patients), or sudden death § Exam: – Systolic ejection murmur (the less full the ventricle, the louder the murmur) – Systolic regurgitant murmur
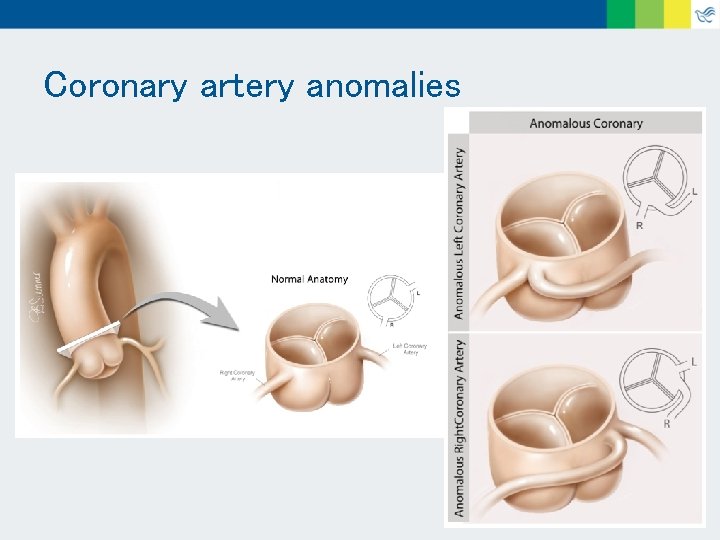
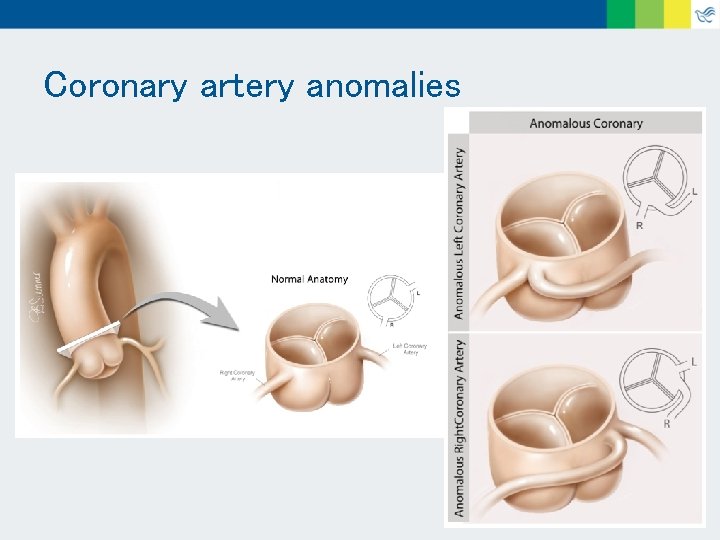
Coronary artery anomalies
Coronary artery anomalies § Many variations § Incidence of both coming off the same sinus of Valsalva ~ 0. 1 to 0. 3% of births § The left coronary coming off the right sinus has higher mortality
Coronary artery anomalies § History: – Exertional chest pain, syncope, or sudden death § Exam: – Unrevealing
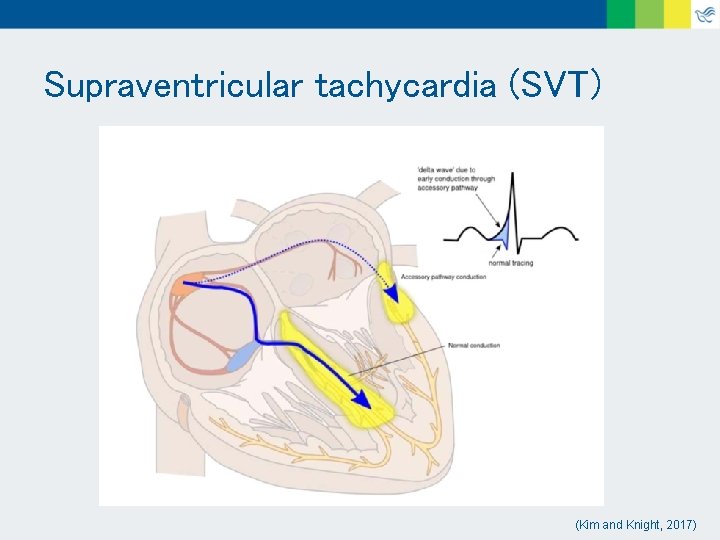
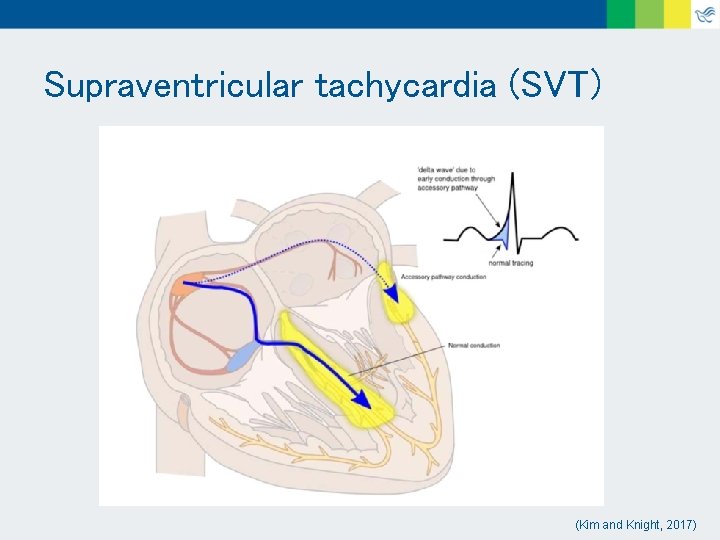
Supraventricular tachycardia (SVT) (Kim and Knight, 2017)
SVT § History – Palpitations (due to an atrial arrhythmia), lightheadedness, dizziness, syncope, chest pain, sudden death § Exam – Unrevealing

SVT § If a patient is having an episode of likely SVT (heart rate > 150 beats/min at rest, can be much higher): – Take blood pressure if able, consider calling pediatric cardiologist – If doing fine, get an ECG – If not, try vagal maneuvers (such as Valsalva) – Or consider local ED / 911
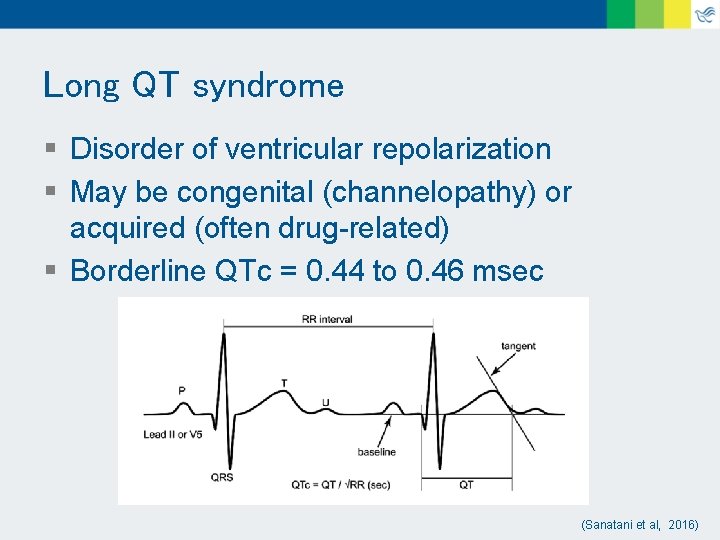
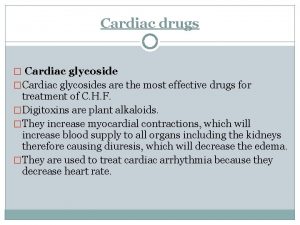
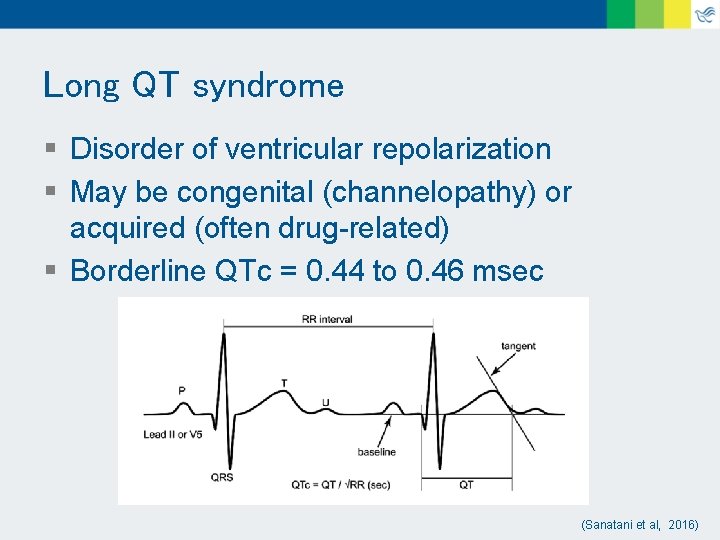
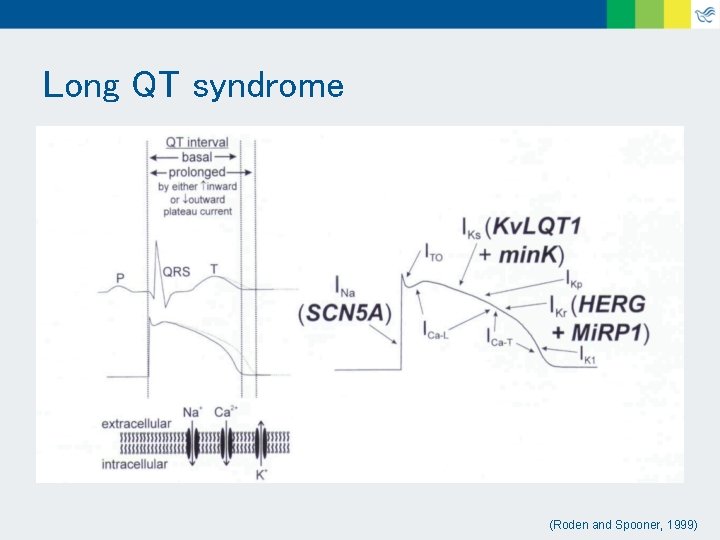
Long QT syndrome § Disorder of ventricular repolarization § May be congenital (channelopathy) or acquired (often drug-related) § Borderline QTc = 0. 44 to 0. 46 msec (Sanatani et al, 2016)
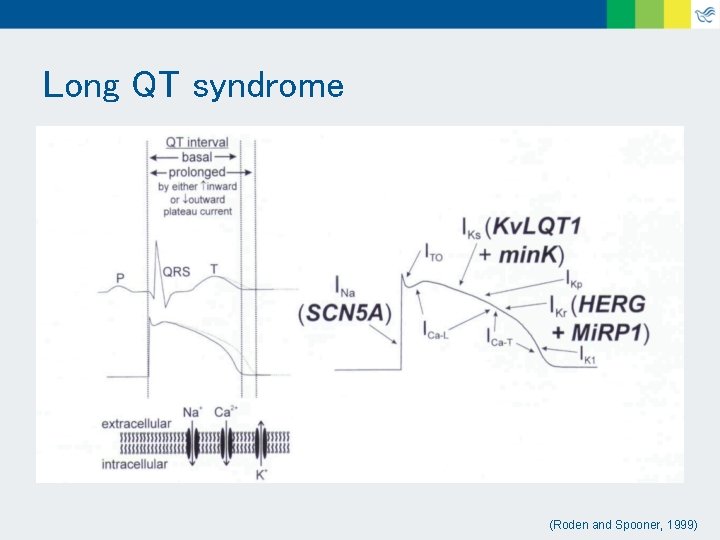
Long QT syndrome (Roden and Spooner, 1999)
Long QT syndrome § History: – Palpitations, syncope, cardiac arrest, sudden death – Family history of congenital deafness, drownings, or accidents without precipitating factors § Exam: – Unrevealing
Acute myocarditis § Inflammation of the myocardium § Pediatric patients can present with acute or fulminant disease § Most common etiology is viral infection – Coxsackie A and B, and adenovirus § Syncope may be due to ventricular dysfunction or arrhythmia
Acute myocarditis § History – Ranges from subclinical to sudden death – Often with viral prodrome – Heart failure: dyspnea, exercise intolerance, gastrointestinal symptoms § Exam – Tachypnea, tachycardia, rales, gallop, regurgitant murmur, friction rub, hepatomegaly
Clinical evaluation - History § Details about all of the events surrounding the episode are critical § Was it presyncope vs true syncope? § Are there risk factors for dehydration? § How long was the patient unconscious? § Family history of vasovagal episodes, cardiomyopathy, ICD, long QT, sudden death
§ Cross sectional study of 3, 445 patients (age < 18) § Presented with syncope or near-syncope to 2 EDs in Atlanta from 2009 to 2013
§ 0. 1% (n=3) were due to a previously undiagnosed cardiac etiology – 2 were SVT and 1 was myocarditis
§ The presence of 2 out of 4 of the following historical features was 100% sensitive and 100% specific – Absence of a prodrome – Chest pain leading up to syncope – Palpitations leading up to syncope – Syncope during exercise
Clinical evaluation - Exam § § Distressed? Pale? Count a heart rate (a key skill!) A heart rate >150 at rest may be SVT, and >220 at rest is SVT until proven otherwise § If possible, take a blood pressure § If possible listen for a heart murmur
Referral is indicated for patients who: § received CPR* § were cardioverted (external or ICD)* § have findings consistent with a cardiac cause for syncope § have recurrent episodes consistent with dysautonomia § would benefit from parental reassurance
Case #1 § 13 y. o. female with palpitations and syncope after volleyball § Supine HR: 58 BP: 108/50 § Standing (3 min) HR: 114 BP: 105/81 § Standing (10 min) HR: 120 BP: 77/56 § POTS
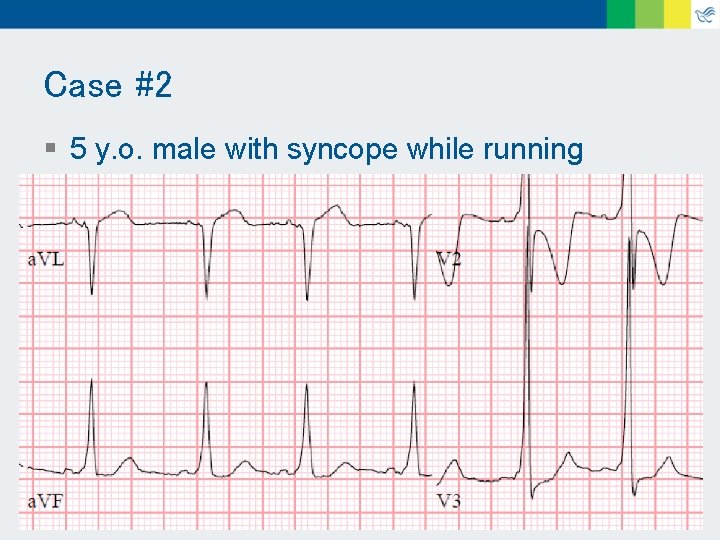
Case #2 § 5 y. o. male with syncope while running
Summary § Dysautonomia is the most common cause of syncope in pediatric patients § A thorough history is the key to distinguishing potentially dangerous etiologies § Practice counting high heart rates § Call us with concern for arrhythmia, or syncope with exercise/palpitations/chest pain (especially when there is no prodrome) § If a patient has known cardiovascular disease, make a written plan with family and/or provider
References § § § § § Allen, H. Syncope: Avoid the Knee-Jerk Echo. AAP Gateway Journals Blog. 2016 Apr 12. Cannon, B, and Wackel, P. Syncope. Pediatric in Review. 2016 Apr; 37(4): 159 -68. Hurst, D, et al. Syncope in the pediatric emergency department – can we predict cardiac disease based on history alone? J Emer Med. 2015; 49(1): 1 -7. Kim, S, and Knight, B. Long term risk of Wolff-Parkinson-White pattern and syndrome. Trends in Cardiovascular Medicine. Article in press. 2017 Reybrouck, T, and Ector, H. Syncope and Assessment of Autonomic Function in Children. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents, Chapter 12. Lippincott Williams & Wilkins. 2008. Roden, D, and Spooner, P. Inherited Long QT Syndromes. Journal of Cardiovascular Electrophysiology. 1999 Dec; 10(12): 1664 -83. Sanatani, S, et al. Canadian Cardiovascular Society and Canadian Pediatric Cardiology Association Position Statement on the Approach to Syncope in the Pediatric Patient. J CJC. Article in press. 2016. Up. To. Date, 2017. <https: //www. texaschildrens. org/departments/anomalous-aortic-origin-coronary-artery -aaoca>
Thank You
Pediatric Cardiology (541) 222 -6160 24/7/365 Misty Carlson, MD mcarlson 2@peacehealth. org • • Eric Johnson, MD ejohnson@peacehealth. org Outpatient clinic consultations Pediatric echocardiograms Pediatric ECGs and rhythm monitors Email or phone consultations
 Yong hoon kim
Yong hoon kim Causes of cardiac arrest
Causes of cardiac arrest Syncope
Syncope Syncope in the older patient is
Syncope in the older patient is Chess score syncope
Chess score syncope Syncope
Syncope Seizure mimics
Seizure mimics Snycope
Snycope Syncope
Syncope Syncope vs seizure
Syncope vs seizure Pulmonary embolism nursing care plan
Pulmonary embolism nursing care plan Basilaris migraine
Basilaris migraine Altruistic acts examples
Altruistic acts examples Proximate causation vs ultimate causation
Proximate causation vs ultimate causation Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Kể tên các môn thể thao
Kể tên các môn thể thao Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Dot
Dot Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Slidetodoc
Slidetodoc Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết Bảng số nguyên tố
Bảng số nguyên tố Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Glasgow thang điểm
Glasgow thang điểm ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Làm thế nào để 102-1=99
Làm thế nào để 102-1=99