Pediatric Syncope Nate Whittaker 032008 Template copyright 2005




- Slides: 70
Pediatric Syncope Nate Whittaker 03/20/08 Template copyright 2005 www. brainybetty. com

Pediatric Syncope • • Definition Epidemiology General Clinical Features Pathophysiology (4 broad categories) Specific Conditions (Ddx) Diagnosis Treatment Disposition Vasovagal Syncope 2 12/19/2021 Template copyright 2005 www. brainybetty. com 2
Definition - Syncope is the temporary loss of consciousness from reversible disruption of cerebral functioning and usually refers to inadequate cardiac output and cerebral hypoperfusion, depriving the brain of O 2. - Occurs when cerebral blood flow decreases below 30 -50% of baseline 12/19/2021 Template copyright 2005 www. brainybetty. com 3
Epidemiology • Experienced at least by 15 -25% of kids before the end of adolescence • Higher in females than in males • Peaks in adolescents aged 15 -19 • . 05 % of pediatric ED visits 12/19/2021 Template copyright 2005 www. brainybetty. com 4
Clinical Features of Syncope • • Sudden onset of falling with a brief LOC 2/3 have lightheadedness before the event vertigo is much less common. Involuntary movements occur with all types of syncope, but are more common with seizures. • Stokes-Adams syndrome - cardiac syncope with very brief tonic or clonic motor activity 12/19/2021 Template copyright 2005 www. brainybetty. com 5
Pathophysiology • • Neurally Mediated Syncope (NMS) Structural Cardiac Disease Cardiac Dysrhythmias Non. Cardiovascular 12/19/2021 Template copyright 2005 www. brainybetty. com 6
Neurally Mediated Syncope (NMS) • Most common cause of syncope in children (61 -80%) • Generally benign • Includes vasovagal, vasodepressor, neurocardiogenic, reflex syncopes, and the simple faint. • Due to vasodilatation, vagal stimulation, or both 12/19/2021 Template copyright 2005 www. brainybetty. com 7
NMS & the Bezold-Jarisch Reflex Extreme overshoot of response to hypotension: • Pooling of blood in Lower Extremities • Drop in intracardiac volume • Increased HR and vigorous contractility • Receptors in atria and ventricle sense high pressure • Paradoxical bradycardia, sudden arterial hypotension SYNCOPE 12/19/2021 Template copyright 2005 www. brainybetty. com 8
NMS Preceded by: -a sensation of warmth -nausea -lightheadedness -visual grayout -tunneling of vision • Lasts less than 1 min 12/19/2021 Template copyright 2005 www. brainybetty. com 9
NMS Precipitated by: • Prolonged recumbence just before standing or prolonged standing • Sight of blood or disfiguring injury (e. g. , fractures or soft tissue injuries) • Emotional upset • Mild physical trauma or pain (Combing) • Physical exertion – blood shifted peripherally • Hot or crowded conditions-vasodilation and water loss. 12/19/2021 Template copyright 2005 www. brainybetty. com 10
NMS Other contributing factors include: • Hypovolemia • Anemia • Dehydration • Pregnancy 12/19/2021 Template copyright 2005 www. brainybetty. com 11
NMS also can occur with: • Stretch with neck hyperextension – Valsalva +/vertebral & PCA compression • Swallowing - vasovagal • Urination – less frequent in kids • Defecation - vasovagal • Coughing – asthma or CF • Medications – BBs, CCBs, Diuretics –wrestlers • Breath-holding spells are a variant of this form of syncope 12/19/2021 Template copyright 2005 www. brainybetty. com 12
NMS Breath-holding spells (BHSs): • Involuntary, occur in healthy children. • After a few cries, the child becomes silent and apneic pallor or cyanosis. • Simple BHSs resolve with no associated syncope or postural change. • Severe BHSs LOC and a change in postural tone with occasional myoclonic jerks. • Lasts seconds to a minute • End with a deep inspiration. • Vagus mediated 12/19/2021 Template copyright 2005 www. brainybetty. com 13

Pediatric Syncope Most cases result from the before mentioned benign etiologies and have complete resolution in 1 or 2 years. BUT, sometimes syncope can be a warning sign for a more serious condition. Save Sudden Cardiac Death Victims 12/19/2021 Template copyright 2005 www. brainybetty. com 14
Pediatric Syncope • Miklós "Miki" Fehér died from ventricular fibrillation brought on by hypertrophic cardiomyopathy at the age of 24. • Up to 25 percent of children who die suddenly have a history of at least one prior syncopal event. • Some reports have found heart disease present in 10 -28% of pediatric syncope patients. 12/19/2021 Template copyright 2005 www. brainybetty. com 15
Pediatric Syncope • Many of the diseases that cause syncope also cause sudden death in children. • Hypertrophic cardiomyopathy and myocarditis are the two most common causes of sudden cardiac death among children with no known cardiac disease. • The greatest risk for sudden cardiac death is among patients with congenital or acquired structural cardiac disease, including postoperative congenital heart disease. 12/19/2021 Template copyright 2005 www. brainybetty. com 16
The most common causes of sudden cardiac death in children • • • Acute myocarditis Cardiomyopathy Cyanotic and noncyanotic congenital heart disease Valvular heart disease Congenital complete heart block Wolff-Parkinson-White syndrome Long QT syndrome (LQTS), Marfan syndrome Coronary artery disease Anomalous coronary arteries 12/19/2021 Template copyright 2005 www. brainybetty. com 17
Risk Factors for a Serious Cause of Syncope • Exertion preceding the event • History of cardiac disease in the patient • Family history of sudden death, deafness, or cardiac disease • Recurrent episodes • Recumbent episode • Prolonged loss of consciousness • Associated chest pain or palpitations • Medications that can alter cardiac conduction 12/19/2021 Template copyright 2005 www. brainybetty. com 18
Structural Cardiac Disease Hypertrophic Cardiomyopathy • AKA idiopathic hypertrophic subaortic stenosis • Exertional syncope, infants CHF & cyanosis. • Greatest risk with earliest onset • 10 -year mortality rate is 50 percent for children diagnosed before 14 years of age • Syncope 2/2 blood flow obstruction, diastolic dysfunction, or A/V arrhythmias • An echocardiogram is necessary to exclude or confirm this diagnosis. • Implantable cardiac defibrillators in children 12/19/2021 Template copyright 2005 www. brainybetty. com 19
Structural Cardiac Disease Dilated Cardiomyopathy • Unusual in children • Three general mechanisms: idiopathic, congenital heart disease, or after myocarditis • Syncope and death are thought to be caused by ventricular dysrhythmias, AV conduction delays or severe myocardial dysfunction • Syncope=high risk of sudden death Defib 12/19/2021 Template copyright 2005 www. brainybetty. com 20
Structural Cardiac Disease ARRHYTHMOGENIC RIGHT VENTRICULAR DYSPLASIA • Rare in the US but, common cause of adolescent death in Italy. • More common in older adolescents/adults. • Present with CHF, cardiomegaly, and syncope or sudden death from a dysrhythmia. • EKG abnormalities - LBBB and T-wave inversion, but may have a normal ECG. 12/19/2021 Template copyright 2005 www. brainybetty. com 21
Structural Cardiac Disease CONGENITAL CYANOTIC AND NONCYANOTIC HEART DISEASE • Hypercyanotic spells may progress to syncope in tetralogy of Fallot, tricuspid atresia, TGA, and Eisenmenger syndrome • Children with structural heart disease are also prone to ventricular dysrhythmias and AV block. • In most cases you will know of a hx of a heart defect. 12/19/2021 Template copyright 2005 www. brainybetty. com 22
Structural Cardiac Disease VALVULAR DISEASES • Degree of valve dysfunction correlates with the risk of sudden death. • Aortic stenosis - most identified by the presence of a murmur, exertional syncope, chest pain, dyspnea on exertion, and poor exercise tolerance (Mean projected survival time of only 27 months after 1 st syncope if untreated) • Mitral Valve Prolapse (MVP) • Ebstein malformation of the tricuspid valve 12/19/2021 Template copyright 2005 www. brainybetty. com 23
Structural Cardiac Disease PULMONARY HYPERTENSION (PH) • Primary PH - associated with dyspnea on exertion, SOB, exercise intolerance, syncope. • Eisenmenger syndrome - left-to-right shunt reverses due to an increase in pulmonary resistance cyanosis. • ½ of patients with PH develop syncope, which is a poor prognostic sign. • Exam - increased ventricular impulse, a loud second heart sound, and cyanosis. • Syncope/sudden death in these patients usually are related to a dysrhythmia. 12/19/2021 Template copyright 2005 www. brainybetty. com 24
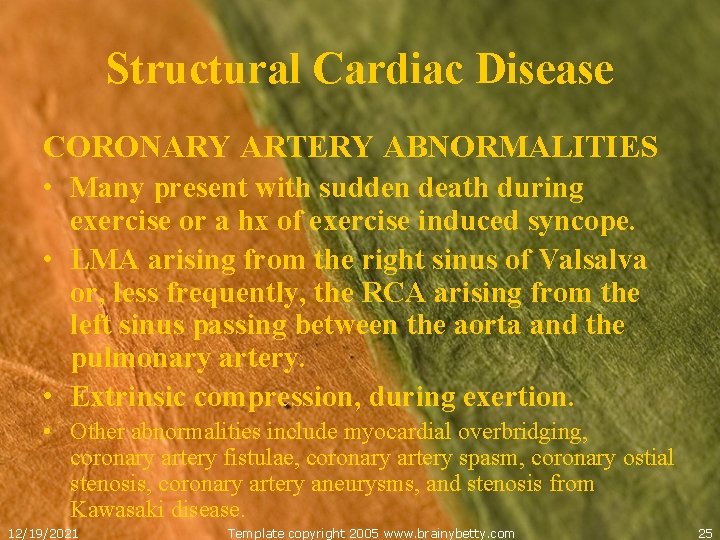
Structural Cardiac Disease CORONARY ARTERY ABNORMALITIES • Many present with sudden death during exercise or a hx of exercise induced syncope. • LMA arising from the right sinus of Valsalva or, less frequently, the RCA arising from the left sinus passing between the aorta and the pulmonary artery. • Extrinsic compression, during exertion. • Other abnormalities include myocardial overbridging, coronary artery fistulae, coronary artery spasm, coronary ostial stenosis, coronary artery aneurysms, and stenosis from Kawasaki disease. 12/19/2021 Template copyright 2005 www. brainybetty. com 25
Cardiac Dysrythmias • Suspect if syncope is associated with an intense sympathetic stimulus, such as anger, surprise, physical exertion, or fright. devil cat • Usually starts and ends abruptly, in contrast to hypoglycemia or seizures, which are more gradual. • May feel palpitations. • Holter monitoring identifies the cause of syncope in only 3 percent of pediatric patients. 12/19/2021 Template copyright 2005 www. brainybetty. com 26
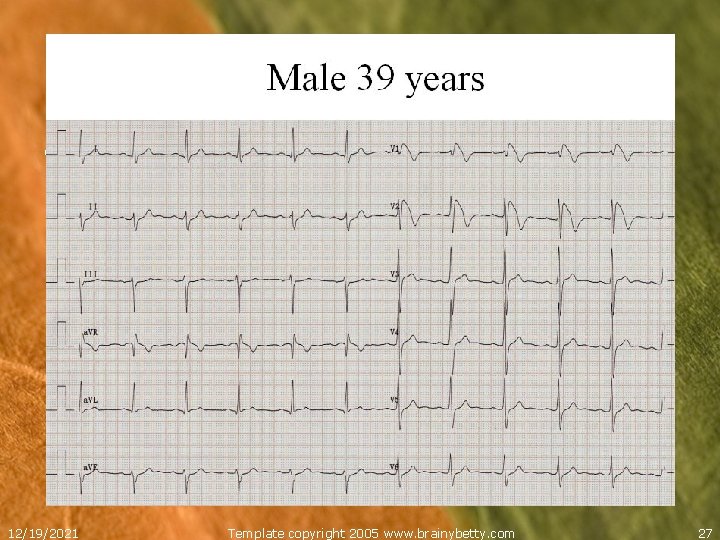
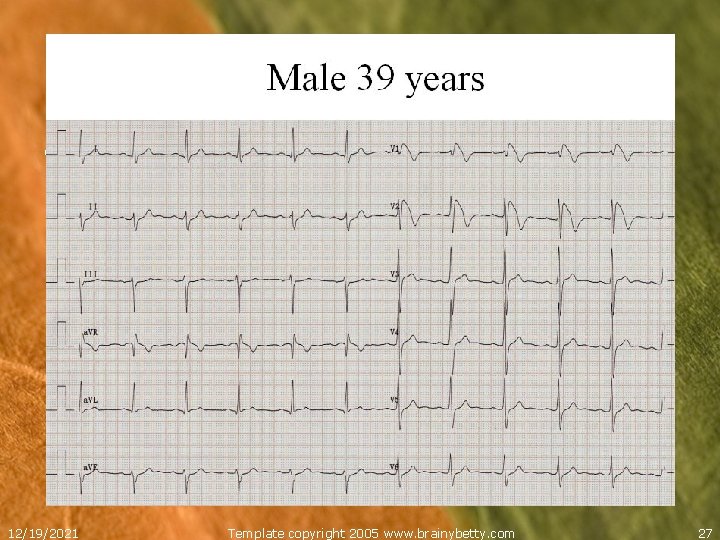
• 12/19/2021 Template copyright 2005 www. brainybetty. com 27
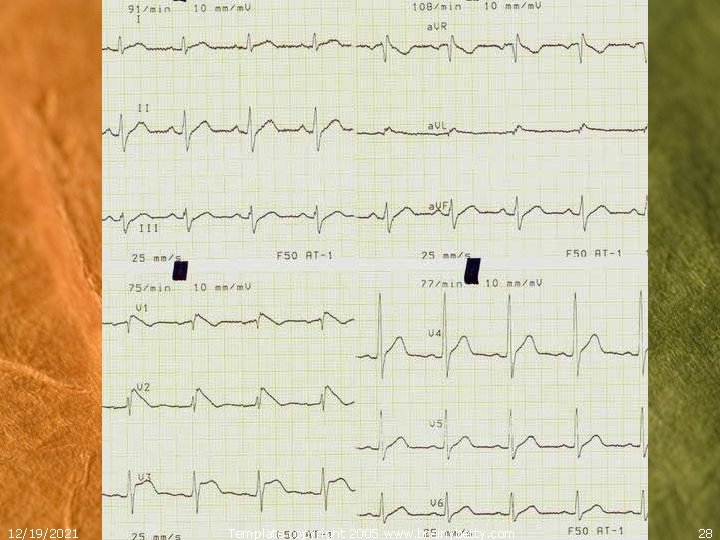
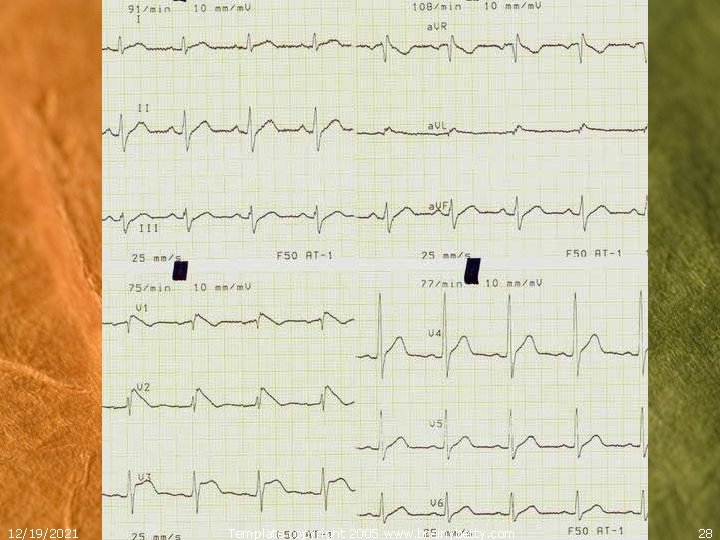
12/19/2021 Template copyright 2005 www. brainybetty. com 28
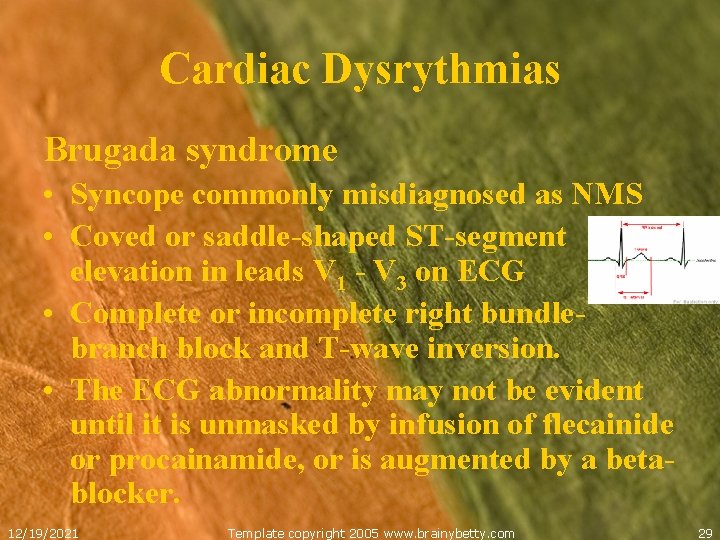
Cardiac Dysrythmias Brugada syndrome • Syncope commonly misdiagnosed as NMS • Coved or saddle-shaped ST-segment elevation in leads V 1 - V 3 on ECG • Complete or incomplete right bundlebranch block and T-wave inversion. • The ECG abnormality may not be evident until it is unmasked by infusion of flecainide or procainamide, or is augmented by a betablocker. 12/19/2021 Template copyright 2005 www. brainybetty. com 29
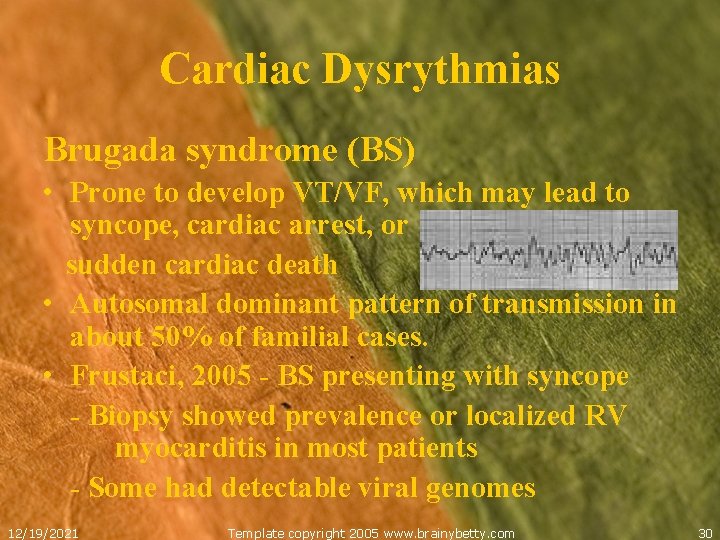
Cardiac Dysrythmias Brugada syndrome (BS) • Prone to develop VT/VF, which may lead to syncope, cardiac arrest, or sudden cardiac death • Autosomal dominant pattern of transmission in about 50% of familial cases. • Frustaci, 2005 - BS presenting with syncope - Biopsy showed prevalence or localized RV myocarditis in most patients - Some had detectable viral genomes 12/19/2021 Template copyright 2005 www. brainybetty. com 30
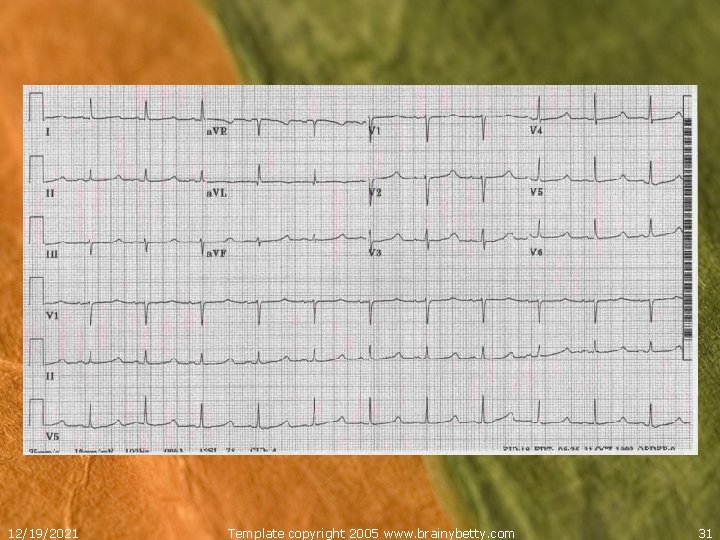
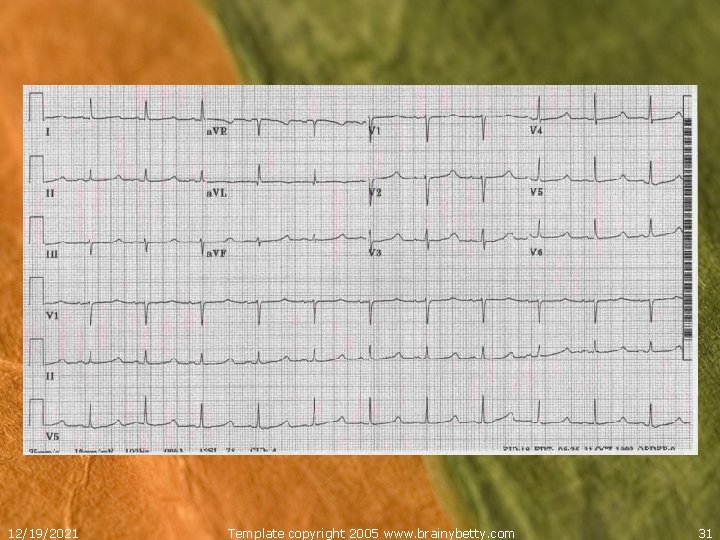
12/19/2021 Template copyright 2005 www. brainybetty. com 31
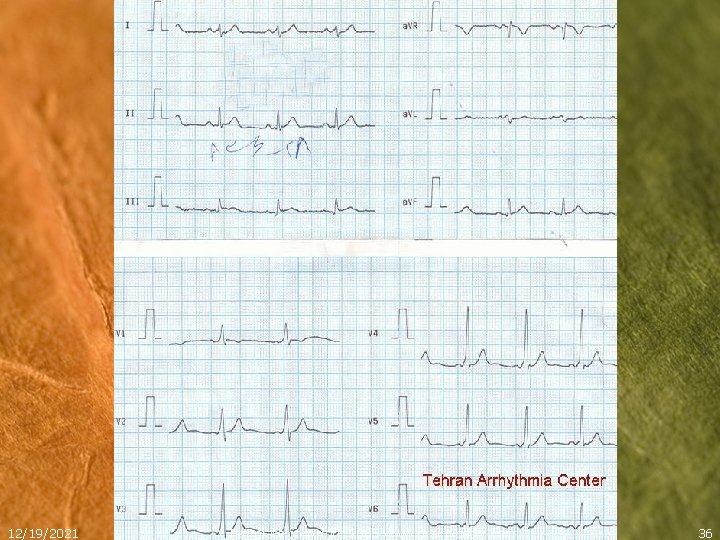
Cardiac Dysrythmias LONG QT SYNDROME • Inherited (Jervell, Lange-Nielsen & Romano-Ward syndromes) or acquired - prolonged QT interval on the ECG. • Incidence - 1 in 5000 births, but LQTS is associated with hypertrophic cardiomyopathy • The corrected QT interval is > 0. 44 s. • Other abnormalities on the ECG associated with LQTS include torsade de pointes, T-wave alternans, notched T waves in three leads, and prominent U waves. 12/19/2021 Template copyright 2005 www. brainybetty. com 32
Cardiac Dysrythmias LONG QT SYNDROME • Syncope = aborted sudden death from Td. P -Sudden (no warning) - Td. P initiated by one PVC -Commonly misdiagnosed as NMS • Pts with a LQTS may have a normal ECG • These patients may be diagnosed by a history of LQTS in a family member (familial LQTS), stress testing (exertional LQTS), or Holter monitoring (intermittent LQTS). • May be using meds that prolong the QT interval. 12/19/2021 Template copyright 2005 www. brainybetty. com 33
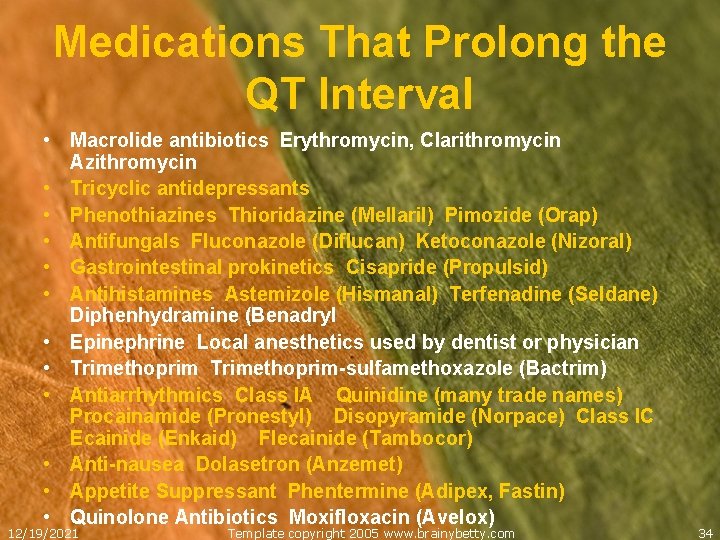
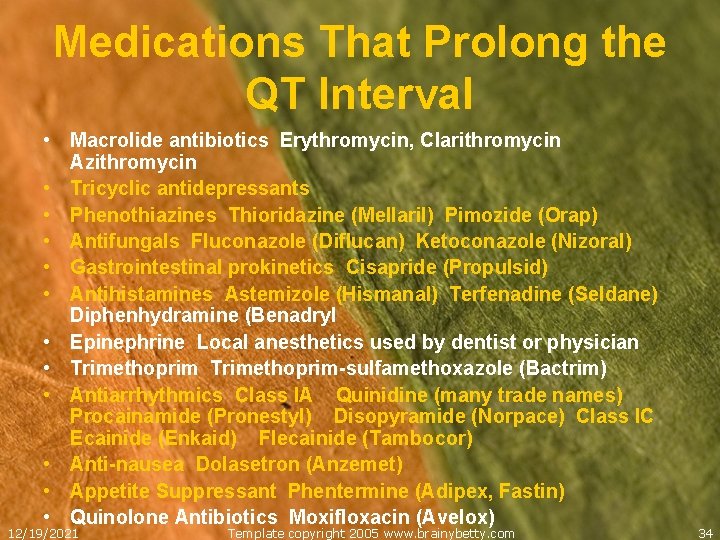
Medications That Prolong the QT Interval • Macrolide antibiotics Erythromycin, Clarithromycin Azithromycin • Tricyclic antidepressants • Phenothiazines Thioridazine (Mellaril) Pimozide (Orap) • Antifungals Fluconazole (Diflucan) Ketoconazole (Nizoral) • Gastrointestinal prokinetics Cisapride (Propulsid) • Antihistamines Astemizole (Hismanal) Terfenadine (Seldane) Diphenhydramine (Benadryl • Epinephrine Local anesthetics used by dentist or physician • Trimethoprim-sulfamethoxazole (Bactrim) • Antiarrhythmics Class IA Quinidine (many trade names) Procainamide (Pronestyl) Disopyramide (Norpace) Class IC Ecainide (Enkaid) Flecainide (Tambocor) • Anti-nausea Dolasetron (Anzemet) • Appetite Suppressant Phentermine (Adipex, Fastin) • Quinolone Antibiotics Moxifloxacin (Avelox) 12/19/2021 Template copyright 2005 www. brainybetty. com 34
Cardiac Dysrythmias LONG QT SYNDROME • The 10 -year mortality rate can be reduced from 70 to 4 percent by appropriate treatment. • Treatment with BBs in the asymptomatic and ICDs in the symptomatic 12/19/2021 Template copyright 2005 www. brainybetty. com 35
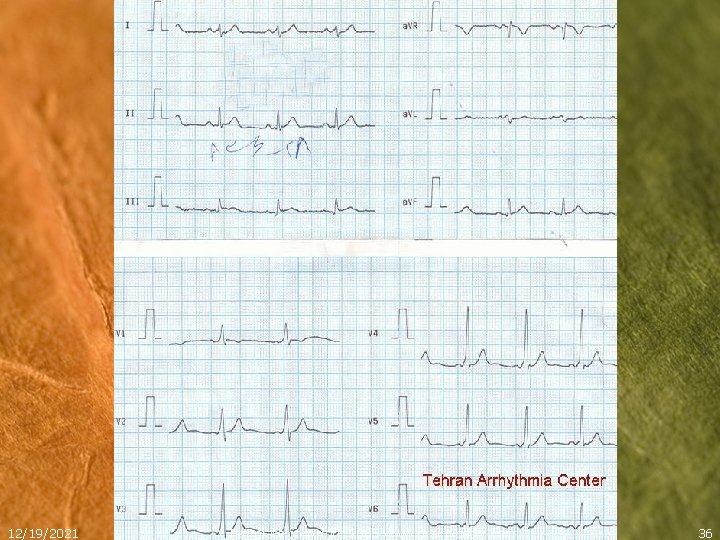
12/19/2021 Template copyright 2005 www. brainybetty. com 36
Cardiac Dysrythmias WOLFF-PARKINSON-WHITE SYNDROME • Characterized by antegrade conduction through an accessory pathway reentrant SVT. • Symptomatic when accessory pathway conduction occurs rapidly reentrant SVT. • ECG- delta wave & short PR <. 12; may be normal • Affects 0. 1% of the general population, but more common in Ebstein malformation, corrected transposition of the great arteries (levo-TGA), and hypertrophic cardiomyopathy. 12/19/2021 Template copyright 2005 www. brainybetty. com 37
Cardiac Dysrythmias WOLFF-PARKINSON-WHITE SYNDROME • Greatest risk for sudden death and syncope occur in patients who have A-fib or A-flutter. • Patients at greatest risk for death are those who conduct antegrade over the accessory pathway, allowing 1: 1 conduction of an atrial dysrhythmia. • Atrial fibrillation and atrial flutter are rare before adolescence. 12/19/2021 Template copyright 2005 www. brainybetty. com 38
Cardiac Dysrythmias ATRIOVENTRICULAR BLOCK • Most common in children with congenital heart disease after surgery, but also occurs as a rare congenital disorder. • Also occurs with acquired heart disease, such as hypertrophic cardiomyopathy, myocarditis (Chagas, RF, Lyme, transient viruses), and muscular dystrophy. • Lyme disease - AV block occurs in 87 percent of children with carditis. 12/19/2021 Template copyright 2005 www. brainybetty. com 39
Cardiac Dysrythmias ATRIOVENTRICULAR BLOCK • The risk of death is highest in infants, but asymptomatic children may also die in adolescence. • Prophylactic pacemaker insertion is routinely performed in children with acquired or congenital AV block. 12/19/2021 Template copyright 2005 www. brainybetty. com 40
Cardiac Dysrythmias SICK SINUS SYNDROME • AKA tachycardia-bradycardia syndrome. . • Mostly associated with prior heart surgery, such as for transposition of the great vessels. • Syncope and sudden death can occur after pacemaker placement, because the pacemaker will prevent bradycardia but not tachycardia. 12/19/2021 Template copyright 2005 www. brainybetty. com 41
Cardiac Dysrythmias SUPRAVENTRICULAR TACHYCARDIA • Any cause of SVT can lead to syncope while recumbent if the heart rate is high enough to inhibit cardiac filling or if coincident vasomotor abnormalities occur. • WPW syndrome and A-fib are the most common causes, but primary SVT can also occur. 12/19/2021 Template copyright 2005 www. brainybetty. com 42
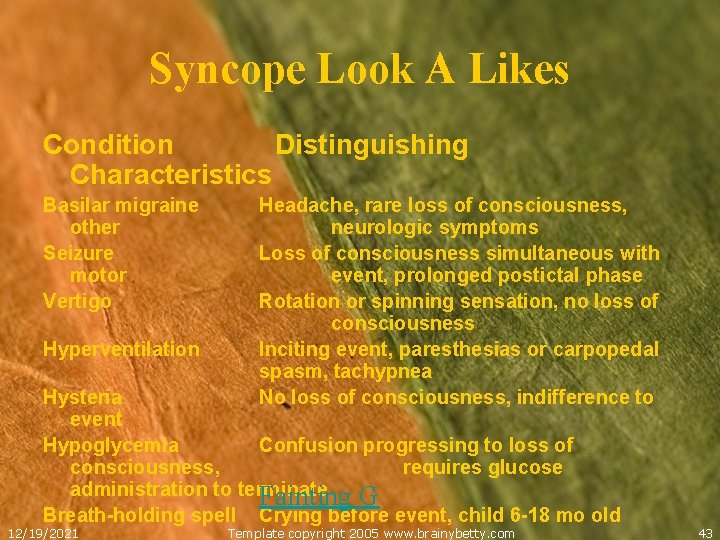
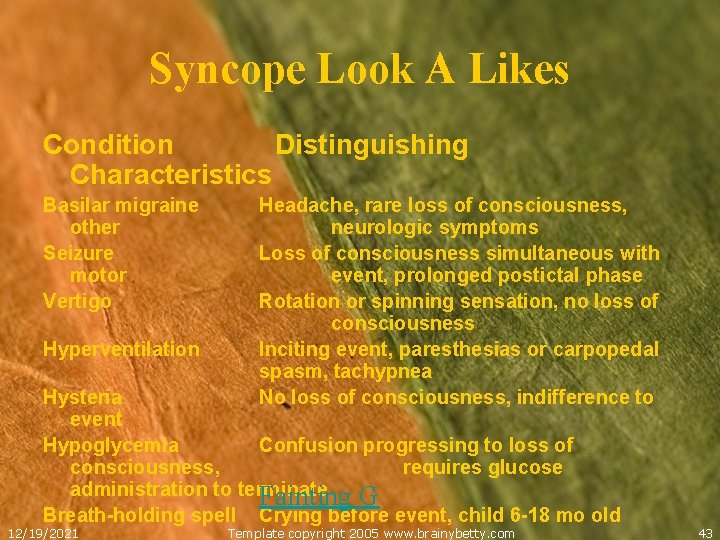
Syncope Look A Likes Condition Distinguishing Characteristics Basilar migraine other Seizure motor Vertigo Hyperventilation Headache, rare loss of consciousness, neurologic symptoms Loss of consciousness simultaneous with event, prolonged postictal phase Rotation or spinning sensation, no loss of consciousness Inciting event, paresthesias or carpopedal spasm, tachypnea No loss of consciousness, indifference to Hysteria event Hypoglycemia Confusion progressing to loss of consciousness, requires glucose administration to terminate Fainting G Breath-holding spell Crying before event, child 6 -18 mo old 12/19/2021 Template copyright 2005 www. brainybetty. com 43
Non. Cardiovascular ATYPICAL MIGRAINE • Basilar artery migraines - syncope due to poor cerebral circulation during vasospasm. • Headache, a family hx of migraines, and a normal HR and BP during the event. • Posterior cerebral circulation symptoms: -visual changes -dysarthria -tinnitus -vertigo -ataxia 12/19/2021 Template copyright 2005 www. brainybetty. com 44
Non. Cardiovascular SEIZURES • Not true syncope, but confused with syncope • Often have little or no prodrome and are associated with LOC. • Tongue biting and loss of bowel or bladder control can be seen • Postictal phase - most syncopal events lack. • Onset while supine, convulsions immediately with LOC, and a warm, flushed, or cyanotic skin color. 12/19/2021 Template copyright 2005 www. brainybetty. com 45
Non. Cardiovascular SEIZURES • Many patients who are diagnosed with a syncopal event in the ED are later found to have a seizure disorder. • Up to 71 percent of syncopal events may have associated behavior that could be called a seizure. 12/19/2021 Template copyright 2005 www. brainybetty. com 46
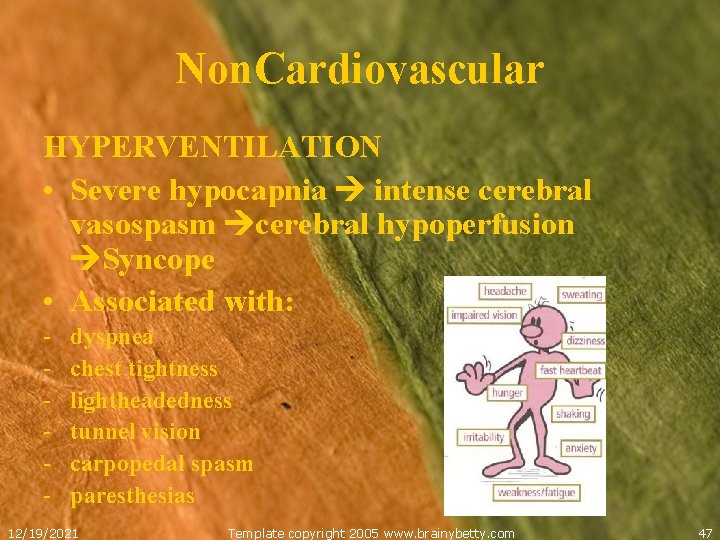
Non. Cardiovascular HYPERVENTILATION • Severe hypocapnia intense cerebral vasospasm cerebral hypoperfusion Syncope • Associated with: - dyspnea chest tightness lightheadedness tunnel vision carpopedal spasm paresthesias 12/19/2021 Template copyright 2005 www. brainybetty. com 47
Non. Cardiovascular HYSTERIA • Appearance of syncope, but not true syncope • Often in front of an audience • Independent of posture • Fall gracefully to the floor without injury • Pt. may describe the event, indifferently or unconcerned, indicating no LOC. 12/19/2021 Template copyright 2005 www. brainybetty. com 48
Non. Cardiovascular HYPOGLYCEMIA • Syncope is usually gradual • Diaphoresis, tachycardia, hunger, and generalized weakness • Resolves with glucose • Does not usually resolve with recumbency • Usually a hx of diabetes 12/19/2021 Template copyright 2005 www. brainybetty. com 49
Diagnosis • No clinical or historical features reliably distinguish vasovagal syncope from other causes. • The event hx from the pt. and observations of witnesses are critical for the Ddx, w/u, and management. • A pt. s historical features and a careful H&P will increase suspicion of a serious cause. . 12/19/2021 Template copyright 2005 www. brainybetty. com 50
Diagnosis • Particularly pay attention to the CV exam. • The PE will often be completely normal. • An ECG should be obtained for almost all children - usually normal. • Children who have an unmistakable episode of vasovagal syncope do not need an ECG. 12/19/2021 Template copyright 2005 www. brainybetty. com 51
Diagnosis History • Interview witnesses who were with the child just before the event. • Events leading up to the incident and any apparent change in behavior or symptoms and episode duration should be described. • Syncope without warning suggests more malignant cardiac causes and increased injury • Intake of meds, drugs, fluids, and food should be noted. 12/19/2021 Template copyright 2005 www. brainybetty. com 52
Diagnosis History • Note the pt. position when syncope occurred • A history of syncope during exertion or exercise increases the likelihood of the more serious etiologies. • The sequence and timing of motor movements, level of consciousness, and postural positioning will help to differentiate primary seizures from true causes of syncope. 12/19/2021 Template copyright 2005 www. brainybetty. com 53
Diagnosis History • Hx of previous syncopal events? • Medical Hx? (Cardiac diseases, diabetes, seizures, meds or drug use, or Psych problems). • Fam. history of structural cardiac disease, dysrhythmias, sudden death, migraines, or seizures. basketball 12/19/2021 Template copyright 2005 www. brainybetty. com 54
Diagnosis Physical Exam • Complete CV, neurologic, and pulmonary examinations are crucial, but usually normal, despite the etiology. • Neurologic examination should include deep tendon reflex, gait, and coordination testing. 12/19/2021 Template copyright 2005 www. brainybetty. com 55
Diagnosis Physical Exam • Assess BP, HR, O 2 sat. , RR, pulse quality in all extremities, orthostatics. • Auscultate for murmurs, arrhythmias, and abnormalities in heart sounds. • CV abnormality = in depth cardiac evaluation. 12/19/2021 Template copyright 2005 www. brainybetty. com 56
Diagnosis Work UP • Syncope = ECG, unless unmistakable vasovagal episode • EKG abnormalities may not have caused syncope and EKG may not pick up arrhythmia • Lab tests determined by clinical suspicion (e. g. , a Hgb for possible anemia or glucose in a diabetic). 12/19/2021 Template copyright 2005 www. brainybetty. com 57
Diagnosis Work UP • Routine lab studies not needed in a clear episode of vasovagal syncope. • However, atypical presentation or worrisome associated symptoms BMP, CBC, thyroid, CXR, and ECG in the ED. • Hyperthyroidism SVTs. • In adolescents, ETOH and UDS should be considered 12/19/2021 Template copyright 2005 www. brainybetty. com 58
Diagnosis Work UP Known or suspected cardiac disease = Cardiac Echo in ED or inpatient -abnormal heart sounds -cardiac murmurs -cardiac chamber enlargement on ECG -repolarization abnormalities on ECG 12/19/2021 Template copyright 2005 www. brainybetty. com 59
Diagnosis Echocardiography– looking at: • • • coronary anatomy right and left ventricular size and function free wall and septal thickness left ventricular outflow tract obstruction presence of cardiac tumors pulmonary artery pressure 12/19/2021 Template copyright 2005 www. brainybetty. com 60
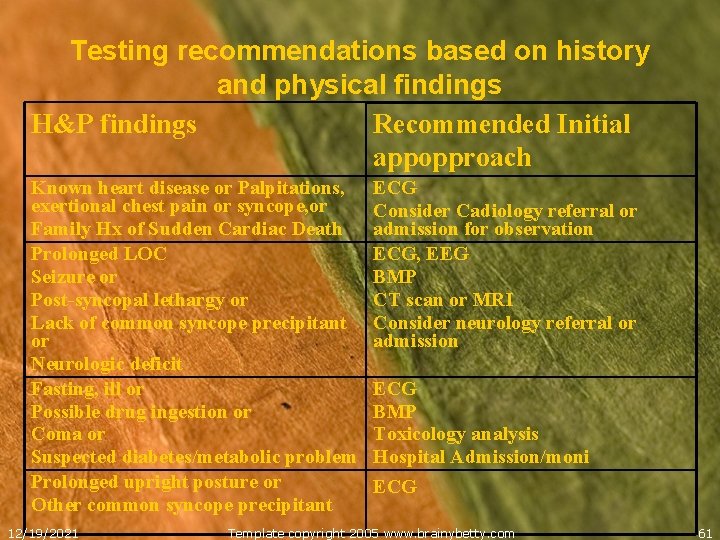
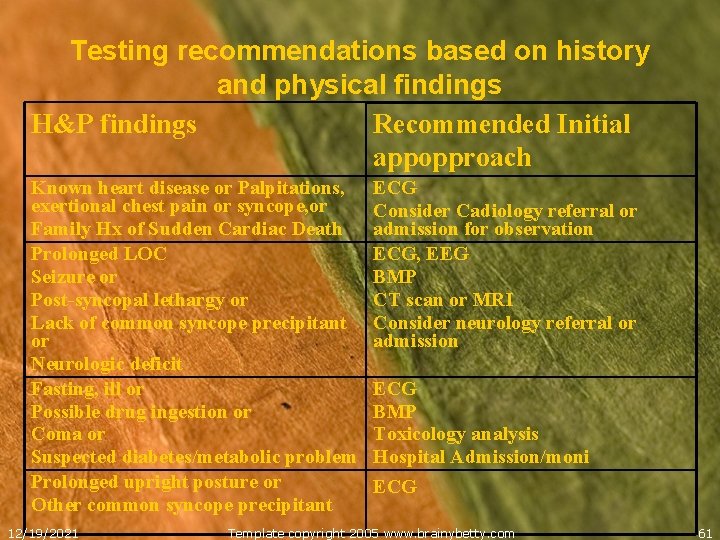
Testing recommendations based on history and physical findings H&P findings Recommended Initial appopproach Known heart disease or Palpitations, exertional chest pain or syncope, or Family Hx of Sudden Cardiac Death Prolonged LOC Seizure or Post-syncopal lethargy or Lack of common syncope precipitant or Neurologic deficit Fasting, ill or Possible drug ingestion or Coma or Suspected diabetes/metabolic problem Prolonged upright posture or Other common syncope precipitant 12/19/2021 ECG Consider Cadiology referral or admission for observation ECG, EEG BMP CT scan or MRI Consider neurology referral or admission ECG BMP Toxicology analysis Hospital Admission/moni ECG Template copyright 2005 www. brainybetty. com 61
Diagnosis A pediatric cardiologist may order the following further work up: -stress tests -tilt-table tests -electrophysiologic studies -cardiac catheterization 12/19/2021 Template copyright 2005 www. brainybetty. com 62

Treatment • Most children with syncope will be fully recovered by the time they arrive in the ED. • Continued altered level of consciousness should prompt an evaluation for causes other than syncope. • Immediately address signs of compromised oxygenation, ventilation, or circulation • Hook pt. up to a cardiac monitor to document any transient dysrhythmias. 12/19/2021 Template copyright 2005 www. brainybetty. com 63
Treatment • Unless obvious vasovagal event, place IV and draw blood. • Treatment is targeted to specific identified etiologies for the syncopal event • NMS – Reassurance, avoidance of deydration and postural hypotension - salt intake, mineralcorticoids, BB • Ongoing cardiac dysrhythmias or seizures should be managed as appropriate. 12/19/2021 Template copyright 2005 www. brainybetty. com 64
Treatment Out-of-Hospital Cardiac Arrest Survival • Rapidly stabilized following principles of pediatric advanced life support • Cardiovert unstable ventricular or supraventricular rhythms • If LQTS is suspected, treat wide QRScomplex tachydysrhythmias with Class IB drugs (amiodarone). Class 1 A agents (procainamide and quinidine), prolong the QT interval. • Admit to PICU 12/19/2021 Template copyright 2005 www. brainybetty. com 65
Disposition • Difficult when etiology is unknown • Any child with a dysrhythmia documented by prehospital providers or on the ECG in the ED must be admitted. • Children with any high risk factors should be admitted in consultation with a pediatric cardiologist. 12/19/2021 Template copyright 2005 www. brainybetty. com 66
Risk Factors for a Serious Cause of Syncope • History of cardiac disease in the patient • Exertion preceding the event • Family history of sudden death, deafness, or cardiac disease • Recurrent episodes • Recumbent episode • Prolonged loss of consciousness • Associated chest pain or palpitations • Medications that can alter cardiac conduction 12/19/2021 Template copyright 2005 www. brainybetty. com 67
Disposition • If thorough Hx, PE, EKG, labs are Neg. D/C home with close F/U by PCP or cardiologist. • Most pediatric patients without cardiac risk factors or exercise-induced symptoms may be safely evaluated as outpatients. • Many of these kids will have additional tests as outpatients, including portable rhythm monitoring, tilt-table testing, and stress testing. 12/19/2021 Template copyright 2005 www. brainybetty. com 68
References • • • Vincent GM: The Long QT and Brugada Syndromes: Causes of Unexpected Syncope and Sudden Cardiac Death in Chinldren and Young Adults. Semin Pediatr Neurol 2005; 12: 15 -24, Massin MM, Malekzadeh-Milani S, Benatar A: Cardiac Syncope in Pediatric Patients. Clin. Cardiol. 81 -85 (2007). Goble MM et al. ED management of pediatric syncope: searching for a rationale. American Journal of Emergency Medicine (2008) 26, 66 -70 Johnsrude CL. Current approach to pediatric syncope. Pediatr Cardiol. Nov. Dec 2000; 21(6): 522 -31 http: //www. emedicine. com/ped/topic 2188. htm Hornstein MS, Hamilton, R. Syncope Tintinalli, J. E. , Kelen, G. D. , and Stapczynski, J. S. (Eds. ) (2004): Syncope and Sudden Death: Chapter 131. Emergency Medicine: A Comprehensive Study Guide, 6 th Edition. Mc. Graw-Hill. 12/19/2021 Template copyright 2005 www. brainybetty. com 69

Church Moments 12/19/2021 Template copyright 2005 www. brainybetty. com 70