Penetrating Neck Trauma Nate Whittaker 121307 Penetrating Neck


- Slides: 56
Penetrating Neck Trauma Nate Whittaker 12/13/07
Penetrating Neck Trauma l Intro l Anatomy l ABCs l Physical Exam l Diagnosis & Management
Penetrating Neck Trauma l Missile or sharp object penetrating the skin and violating the platysma (GSW, Stab, Puncture wounds, and Impalement Injuries). l 30% of cases are accompanied by injury outside of the neck zones l 5 -10% of all traumas presenting to the ED
Penetrating Neck Trauma l Higher mortality rates with injuries to large vessels (carotid or subclavian arteries and veins) l Civilian mortality rate ranges from 3 -6%
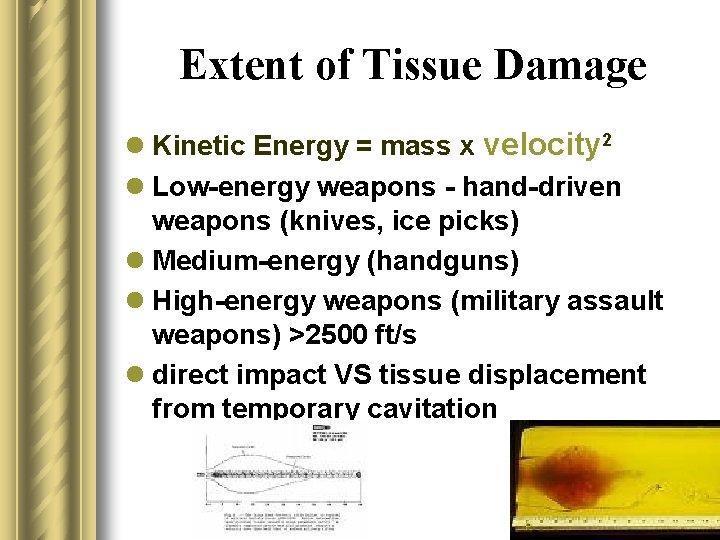
Extent of Tissue Damage l Kinetic Energy = mass x velocity 2 l Low-energy weapons - hand-driven weapons (knives, ice picks) l Medium-energy (handguns) l High-energy weapons (military assault weapons) >2500 ft/s l direct impact VS tissue displacement from temporary cavitation
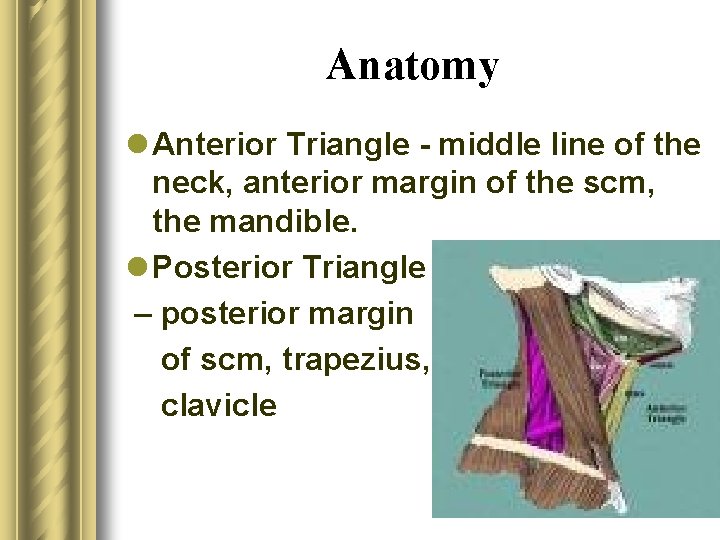
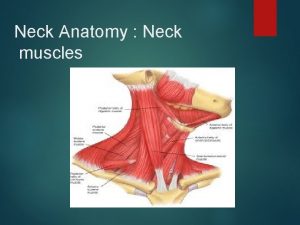
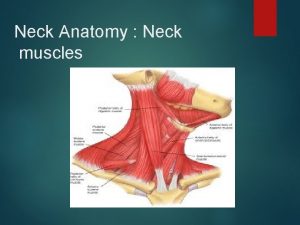
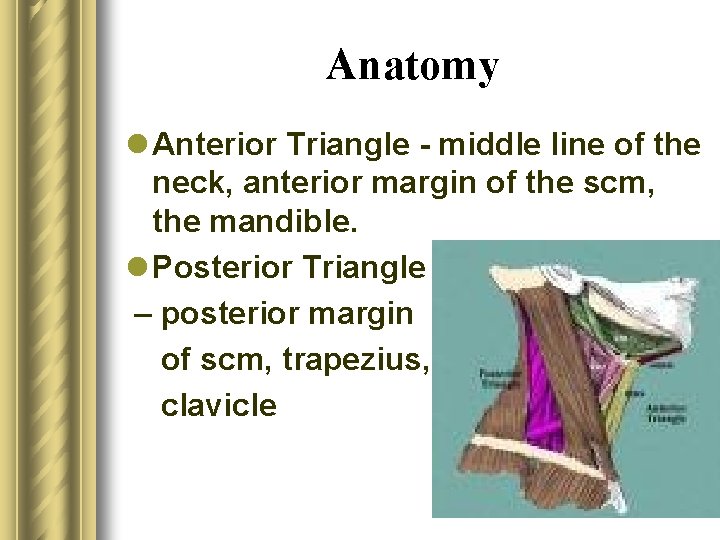
Anatomy l Anterior Triangle - middle line of the neck, anterior margin of the scm, the mandible. l Posterior Triangle – posterior margin of scm, trapezius, clavicle
Anatomy
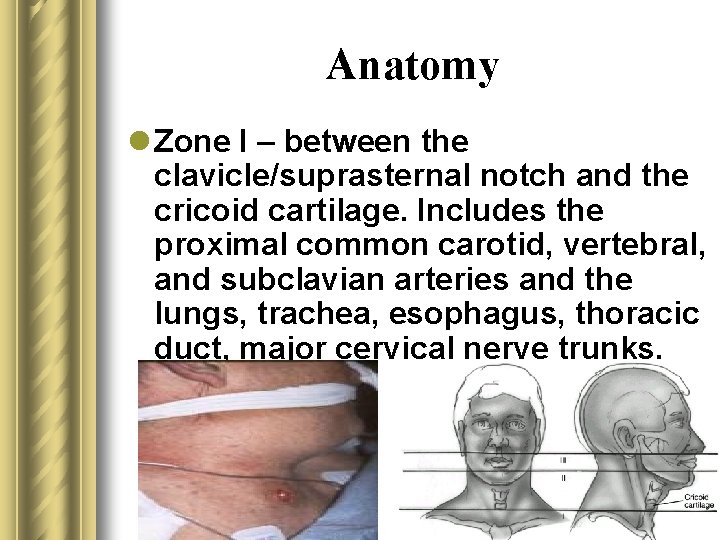
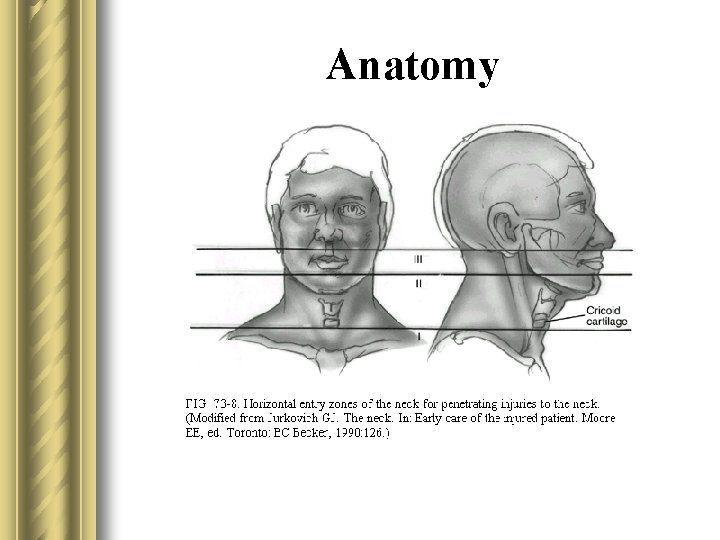
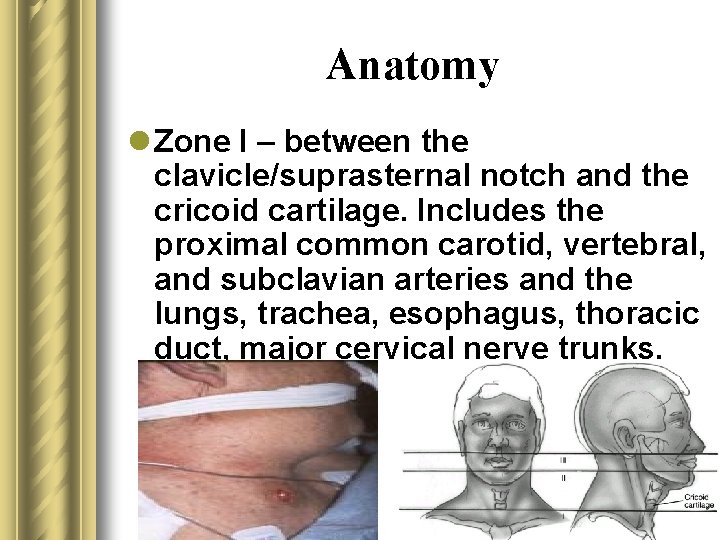
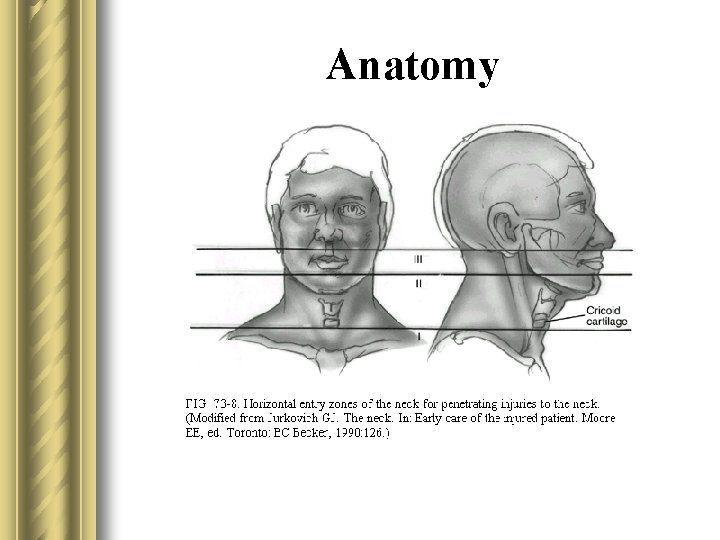
Anatomy l Zone I – between the clavicle/suprasternal notch and the cricoid cartilage. Includes the proximal common carotid, vertebral, and subclavian arteries and the lungs, trachea, esophagus, thoracic duct, major cervical nerve trunks.
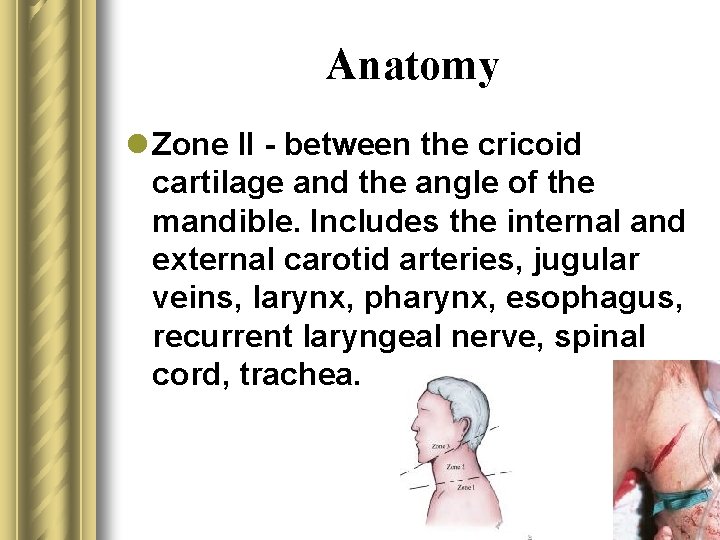
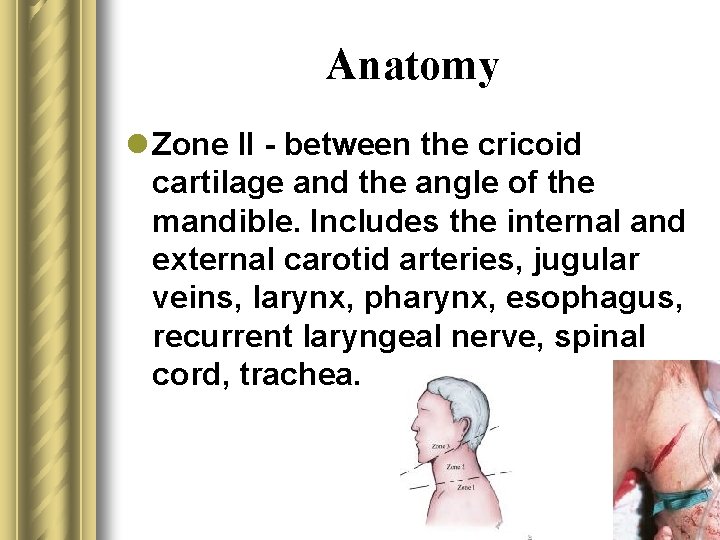
Anatomy l Zone II - between the cricoid cartilage and the angle of the mandible. Includes the internal and external carotid arteries, jugular veins, larynx, pharynx, esophagus, recurrent laryngeal nerve, spinal cord, trachea.
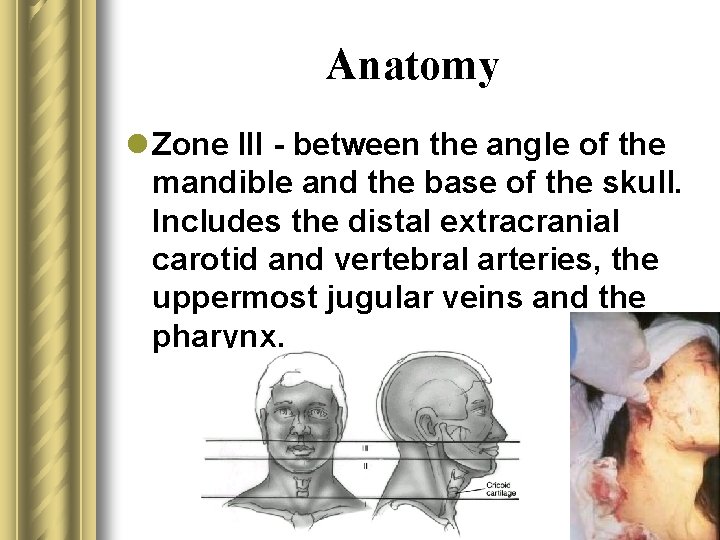
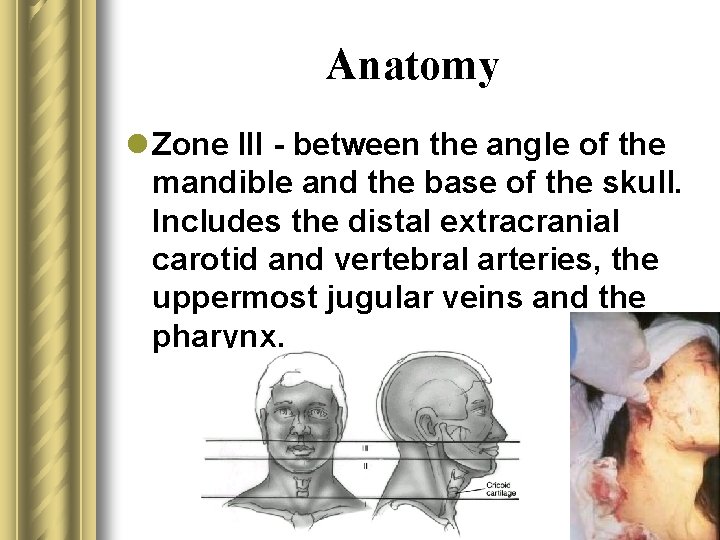
Anatomy l Zone III - between the angle of the mandible and the base of the skull. Includes the distal extracranial carotid and vertebral arteries, the uppermost jugular veins and the pharynx.
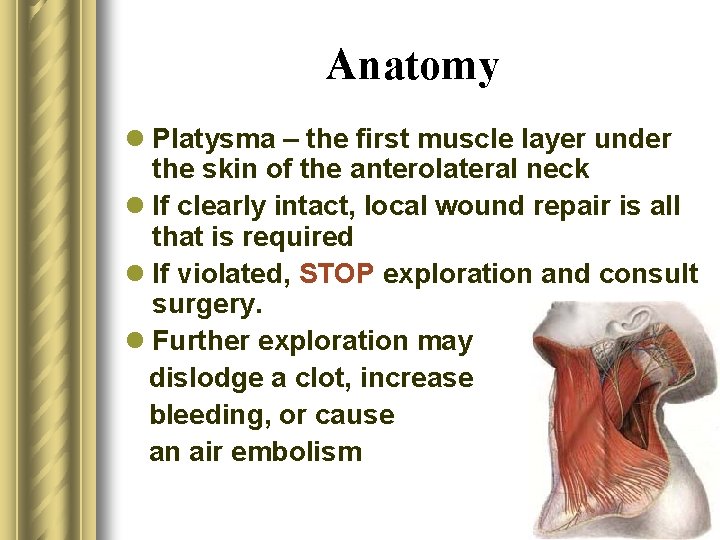
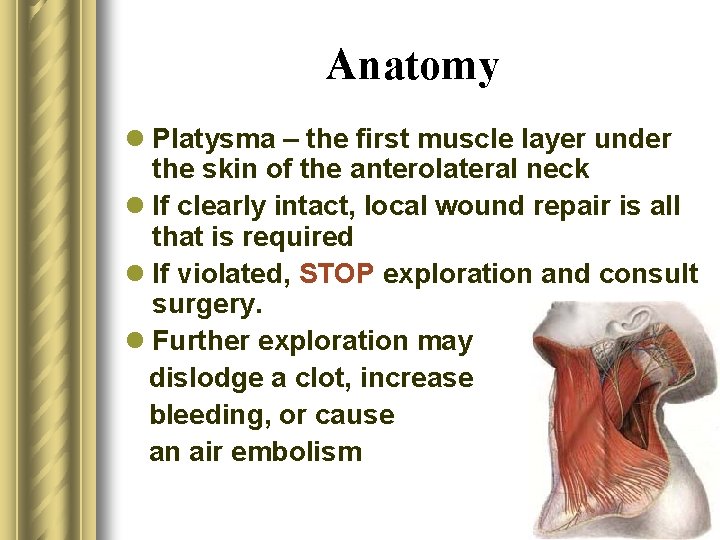
Anatomy l Platysma – the first muscle layer under the skin of the anterolateral neck l If clearly intact, local wound repair is all that is required l If violated, STOP exploration and consult surgery. l Further exploration may dislodge a clot, increase bleeding, or cause an air embolism
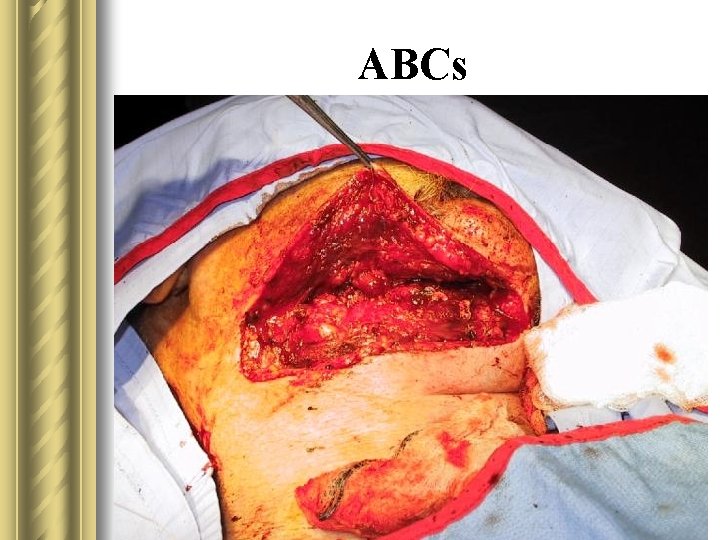
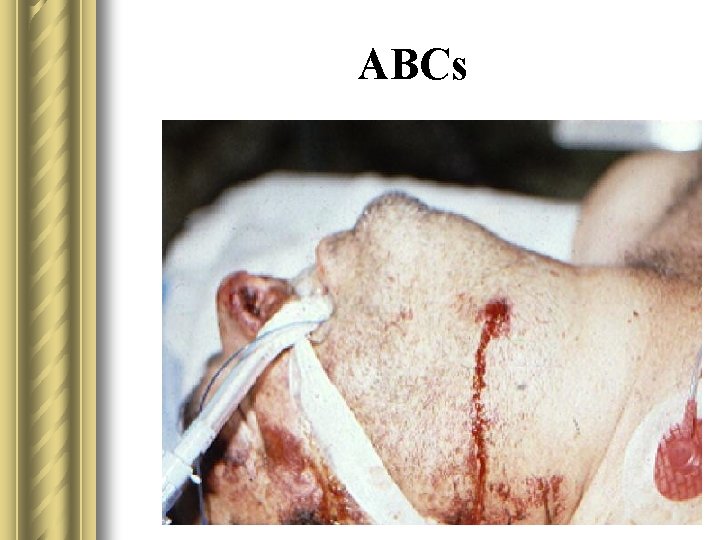
ABCs
ABCs
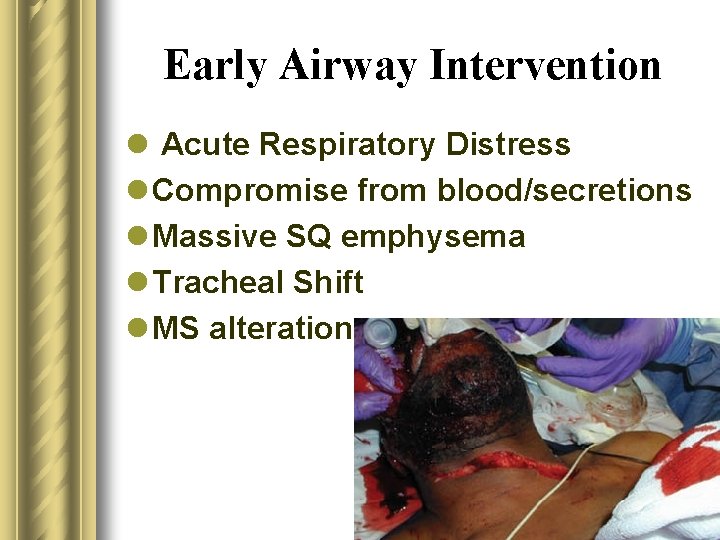
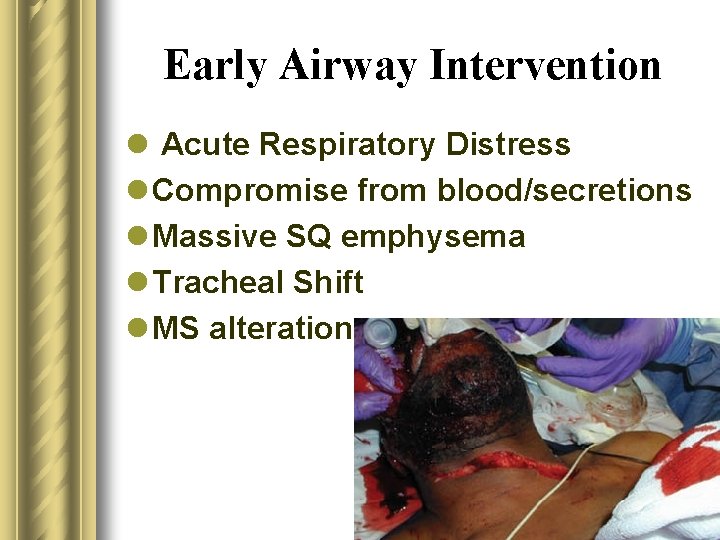
Early Airway Intervention l Acute Respiratory Distress l Compromise from blood/secretions l Massive SQ emphysema l Tracheal Shift l MS alteration
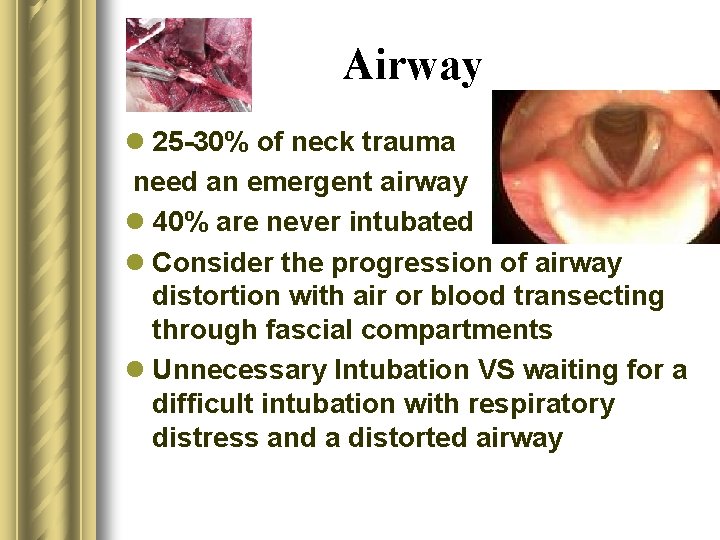
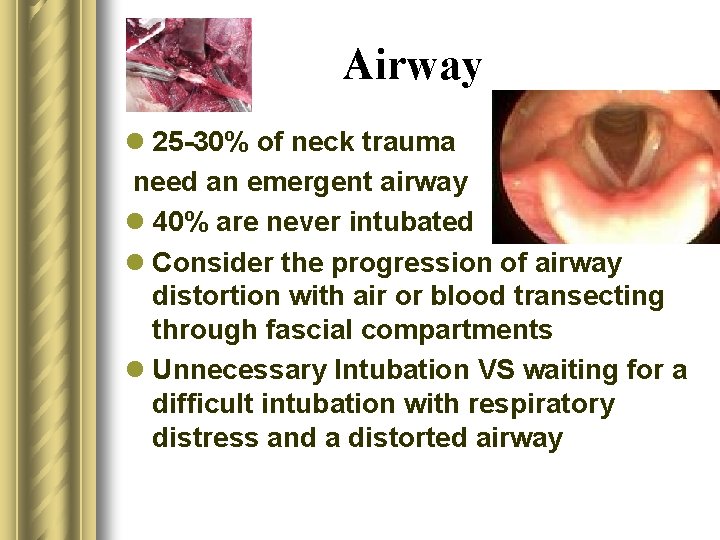
Airway l 25 -30% of neck trauma need an emergent airway l 40% are never intubated l Consider the progression of airway distortion with air or blood transecting through fascial compartments l Unnecessary Intubation VS waiting for a difficult intubation with respiratory distress and a distorted airway
Airway l RSI l Gum Elastic Bougie l Blind Nasotracheal – perceived high failure and complication rates l Fiberoptic l Retrograde tracheal intubation l Cricothyrotomy l Tracheostomy
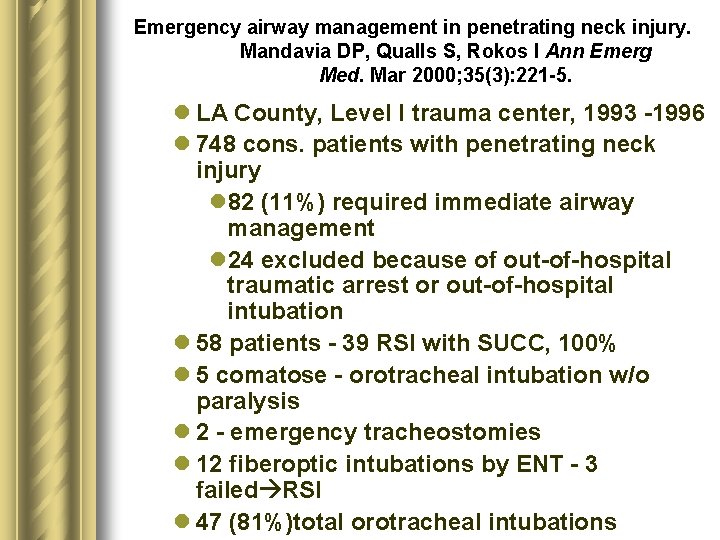
Emergency airway management in penetrating neck injury. Mandavia DP, Qualls S, Rokos I Ann Emerg Med. Mar 2000; 35(3): 221 -5. l LA County, Level I trauma center, 1993 -1996 l 748 cons. patients with penetrating neck injury l 82 (11%) required immediate airway management l 24 excluded because of out-of-hospital traumatic arrest or out-of-hospital intubation l 58 patients - 39 RSI with SUCC, 100% l 5 comatose - orotracheal intubation w/o paralysis l 2 - emergency tracheostomies l 12 fiberoptic intubations by ENT - 3 failed RSI l 47 (81%)total orotracheal intubations
Blind nasotracheal intubation for patients with penetrating neck trauma. Weitzel N, Kendall J, Pons P. J Trauma. May 2004; 56(5): 1097101 l Denver, Colorado, 1993 - 2001 l 240 patients with penetrating neck trauma l 89 (37%) required emergent airway management l 40 (17%) prehospital blind nasotracheal intubation l. Success rate - 90% l. Mean # of attempts was 1. 16 (range, 1 -4) l. Paramedics very experienced at blind nasotracheal intubation
Use of a gum elastic bougie (GEB) in a zone II penetrating neck trauma: a case report. Steinfeldt J, Bey TA, Rich JM. J Emerg Med 2003; 24: 267 -70 l Self inflicted 5 cm deep slash wound in zone II w/ transection of his pharynx l Blind intubation through the wound failed x 3 2/2 constant blood blow l Bougie used to intubate trachea with confirmatory clicking on tracheal rings l ET tube successfully placed over bougie into trachea
Cricothyrotomy l Favored surgical back up if RSI fails l Have kit opened and neck prepped before RSI in tenuous circumstances l Risk of disrupting stable hematoma in some trauma patients obscuring operative field and significant hemorrhage l If integrity of larynx is questionable, tracheostomy may be the best option
Airway l C-spine – maintain the best you can – No reports of unstable c-spine injuries from stab wounds (not enough force) – GSW – instability = fx in 2 columns, requiring the bullet to traverse the spinal cord neurological symptoms – Airway takes priority • Remove the collar – Use in-line cervical traction for c-spine stabilization.
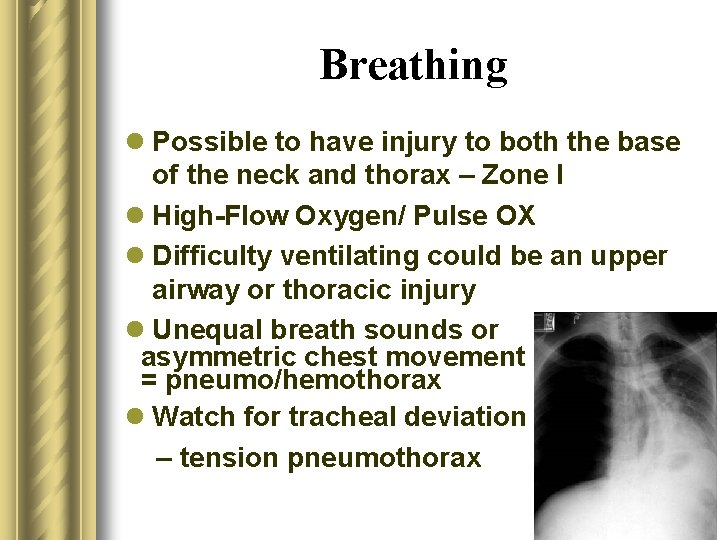
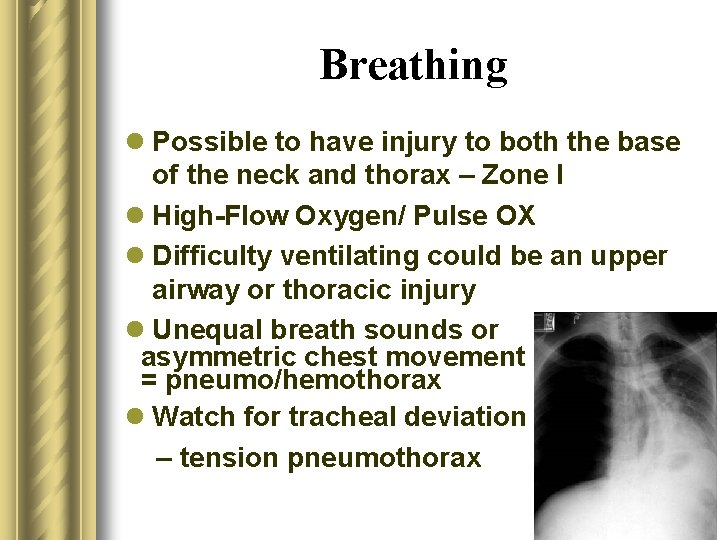
Breathing l Possible to have injury to both the base of the neck and thorax – Zone I l High-Flow Oxygen/ Pulse OX l Difficulty ventilating could be an upper airway or thoracic injury l Unequal breath sounds or asymmetric chest movement = pneumo/hemothorax l Watch for tracheal deviation – tension pneumothorax
Circulation l Hard signs of Vascular Injury • • Bruit or Thrill Expanding or Pulsatile Hematoma Pulsatile or Severe Hemorrhage Pulse Deficit l Soft signs of Vascular Injury • Hypotension and Shock • Stable, nonpulsatile hematoma • Central or Peripheral nervous system ischemia • Proximity to a major vascular structure
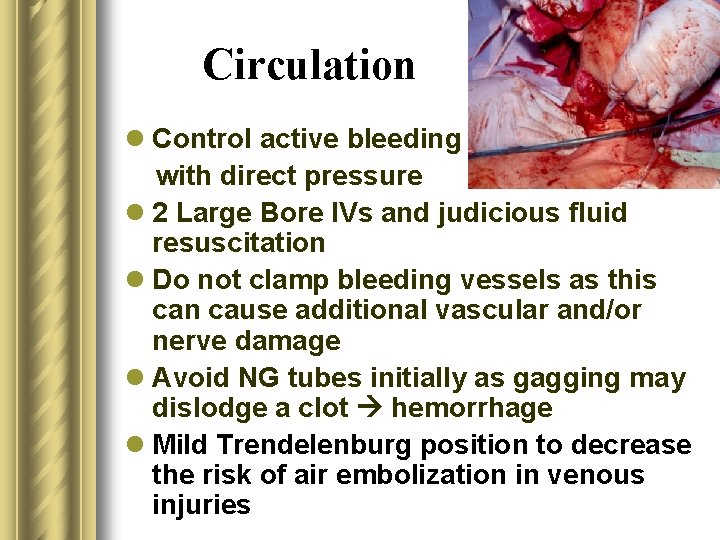
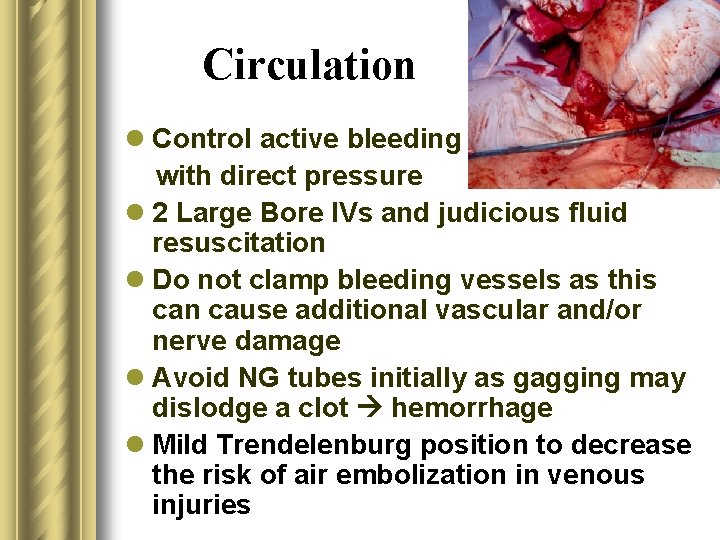
Circulation l Control active bleeding with direct pressure l 2 Large Bore IVs and judicious fluid resuscitation l Do not clamp bleeding vessels as this can cause additional vascular and/or nerve damage l Avoid NG tubes initially as gagging may dislodge a clot hemorrhage l Mild Trendelenburg position to decrease the risk of air embolization in venous injuries
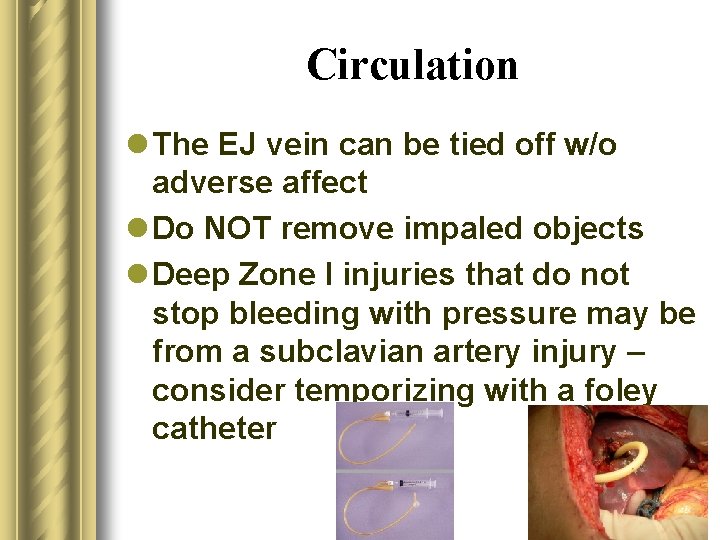
Circulation l The EJ vein can be tied off w/o adverse affect l Do NOT remove impaled objects l Deep Zone I injuries that do not stop bleeding with pressure may be from a subclavian artery injury – consider temporizing with a foley catheter
Foley catheter balloon tamponade for life-threatening hemorrhage in penetrating neck trauma. Navsaria P, Thoma M, Nicol A. World J Surg. Jul 2006; 30(7): 1265 -8 l Cape Town, South Africa 07/04 – 06/05 l 220 penetrating neck traumas l 17/18 successfully txed with foley tamponade l Foley filled with 5 ml of h 20 or until resistance felt l Zone I – 3, Zone II – 8, Zone III – 1, Posterior triangle – 5

Disability Spinal Cord Phrenic Recurrent Laryngeal Cranial Nerves IX-XII Brachial Plexus Focal neurological deficits from damage to the carotid or vertebral artery CNS Ischemia
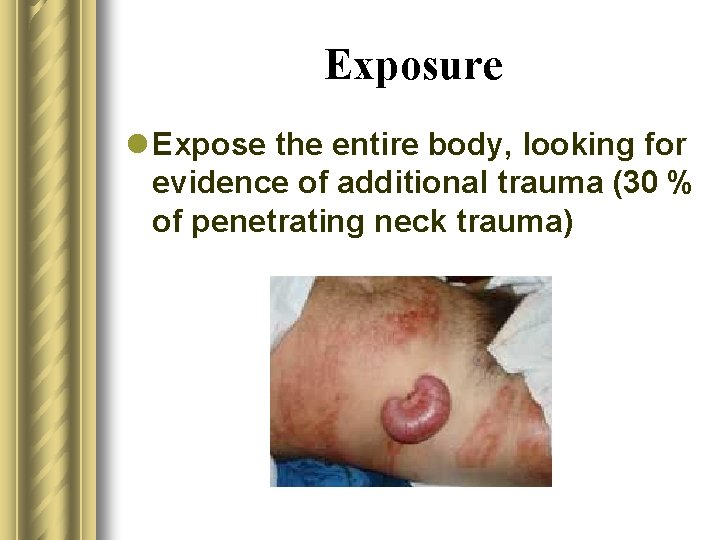
Exposure l Expose the entire body, looking for evidence of additional trauma (30 % of penetrating neck trauma)
ED Stand-up l www. youtube. com/watch? v=k 9 m 2 F LHl. Ew. A
Who goes emergently to the OR ? l Absolute Criteria: – – – Shock Uncontrolled Bleeding No Radial Pulse Rapidly Expanding or Pulsatile Hematoma Respiratory Distress l Relative Criteria: – Air Bubbles from Wound – Hemoptysis – Crepitus
Physical Exam l Controversial how much weight should be placed on physical exam l Regardless, the more we gather from the PE, the more appropriate and timely our w/u and management will be l Demetriades et al, Los Angeles (OR full, stock in PE, chart)
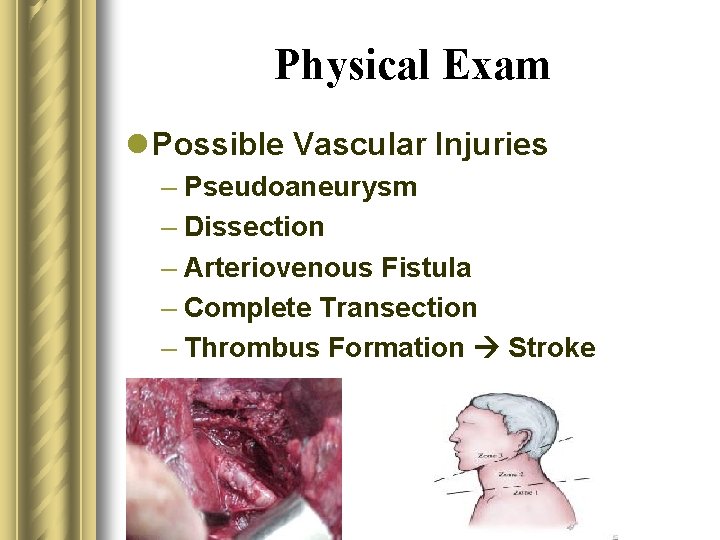
Physical Exam l Vascular – 25 – 50% of cases – Active Bleeding (w/ direct pressure) • Degree – Hypotension • >100, 60 -90, <60 – Peripheral Pulses (brachial, radial) • Diminished, absent – Bruit – heard in 50% of carotid injuries • where – Hematoma (size, expanding? )
Physical Exam l Possible Vascular Injuries – Pseudoaneurysm – Dissection – Arteriovenous Fistula – Complete Transection – Thrombus Formation Stroke
Physical Exam l Larynx/Trachea – 10 % of cases – Hemoptysis (ask pt to cough) – Air bubbling though the wound (ask pt to cough) – Subcutaneous emphysema – Crepitation – Hoarseness – Trachea Midline
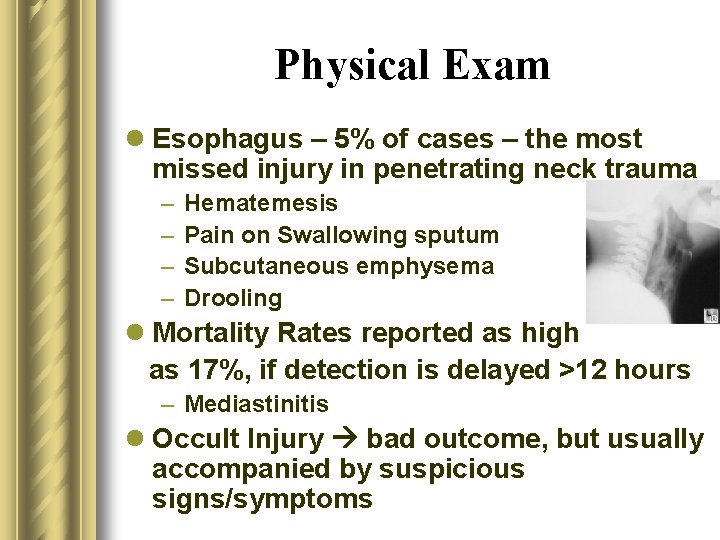
Physical Exam l Esophagus – 5% of cases – the most missed injury in penetrating neck trauma – – Hematemesis Pain on Swallowing sputum Subcutaneous emphysema Drooling l Mortality Rates reported as high as 17%, if detection is delayed >12 hours – Mediastinitis l Occult Injury bad outcome, but usually accompanied by suspicious signs/symptoms
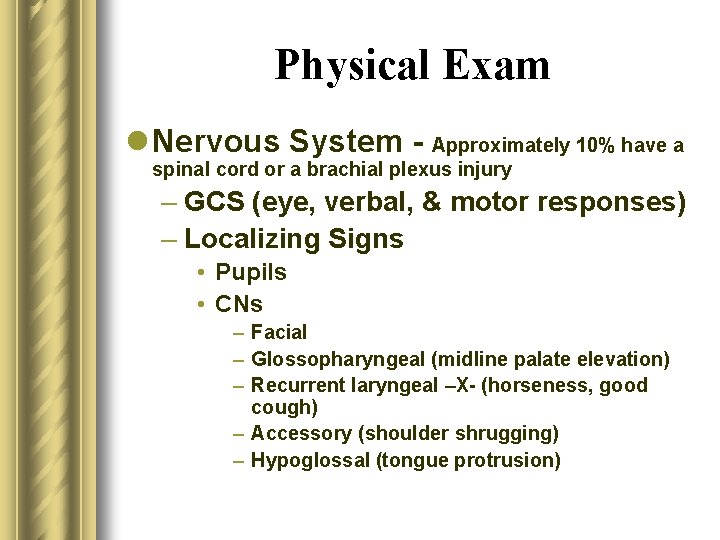
Physical Exam l Nervous System - Approximately 10% have a spinal cord or a brachial plexus injury – GCS (eye, verbal, & motor responses) – Localizing Signs • Pupils • CNs – Facial – Glossopharyngeal (midline palate elevation) – Recurrent laryngeal –X- (horseness, good cough) – Accessory (shoulder shrugging) – Hypoglossal (tongue protrusion)
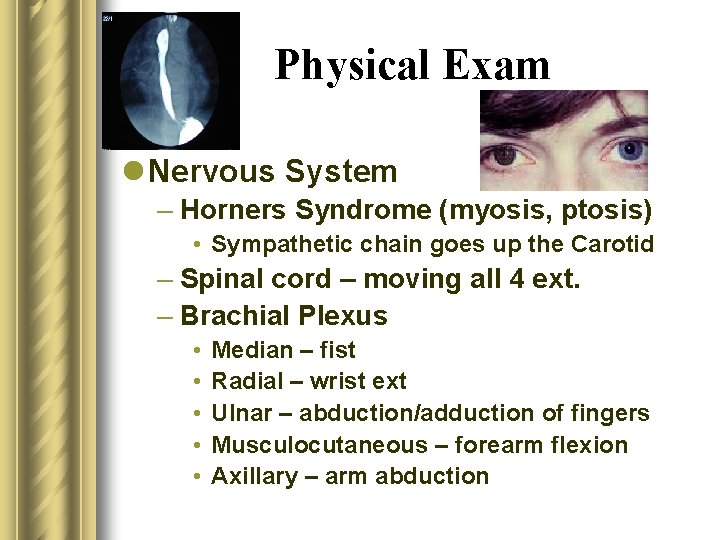
Physical Exam l Nervous System – Horners Syndrome (myosis, ptosis) • Sympathetic chain goes up the Carotid – Spinal cord – moving all 4 ext. – Brachial Plexus • • • Median – fist Radial – wrist ext Ulnar – abduction/adduction of fingers Musculocutaneous – forearm flexion Axillary – arm abduction
Physical Exam l Obvious signs/symptoms suggestive of major vascular or aerodigestive injuries require emergent or urgent operative intervention
Who goes emergently to the OR ? l Absolute Criteria: – – – Shock Uncontrolled Bleeding No Radial Pulse Rapidly Expanding or Pulsatile Hematoma Respiratory Distress l Relative Criteria: – Air Bubbles from Wound – Hemoptysis – Crepitus
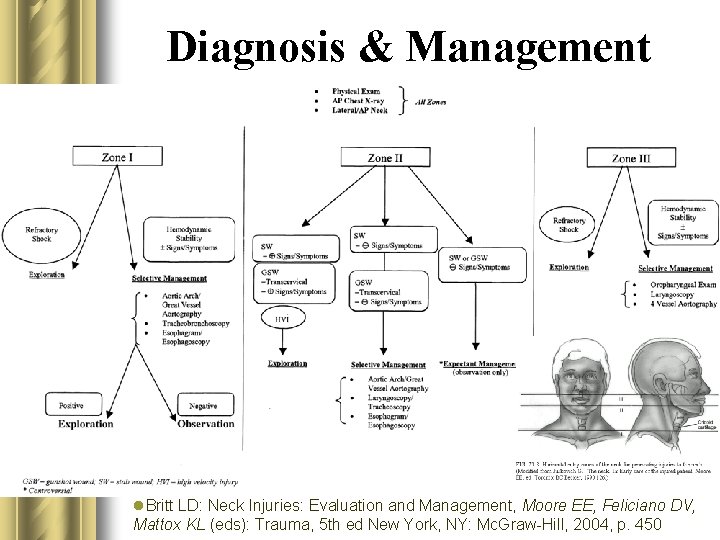
Diagnosis & Management l Institution, Resource, and Surgeon dependant l All hemodynamically unstable patients or those with obvious aerodigestive injuries should go immediately to the OR l Everybody gets a an AP CXR & a Lateral/AP Neck l Type and Cross l Consider LA, base deficit, or bicarb
Diagnosis & Management l Historically, after WWII, routine surgical exploration of Zone II penetrating wounds was accepted l Studies in the 1980 s demonstrated a high rate of negative exploration encouraging a more selective approach to surgical management l Since then, the greatest controversy has been over how to w/u stable Zone II trauma pts without evidence of Aerodigestive injury
Diagnosis & Management l Unless hemodynamically unstable or there is evidence of aerodigestive tract injuries, surgeons prefer the selective approach in Zone I & III, given difficulty of exposure l Operative management of Zone I may require a median sternotomy or a thoracic approach and Zone III may require disarticulation of the mandible or resection of the styloid or mandible angle.
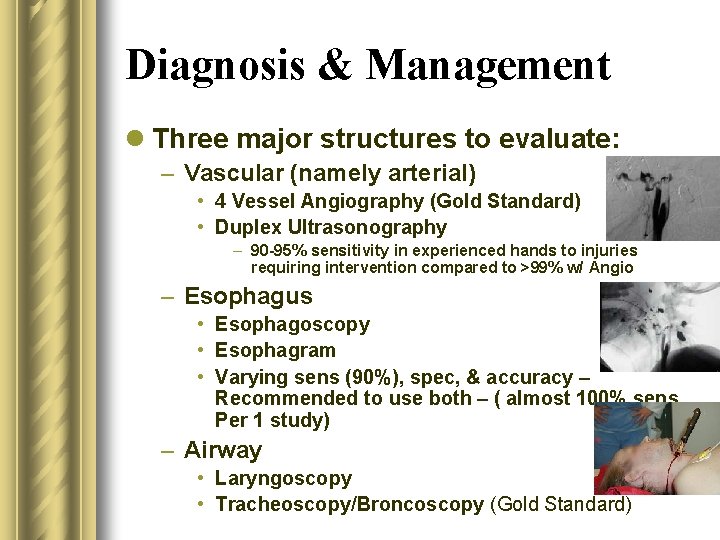
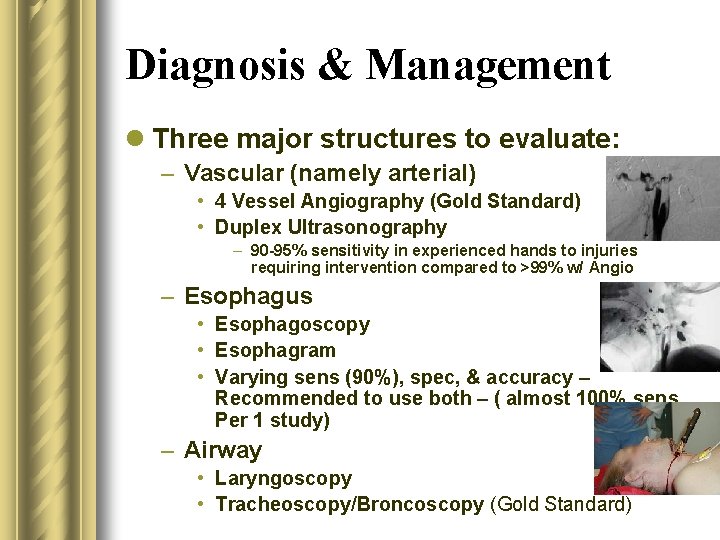
Diagnosis & Management l Three major structures to evaluate: – Vascular (namely arterial) • 4 Vessel Angiography (Gold Standard) • Duplex Ultrasonography – 90 -95% sensitivity in experienced hands to injuries requiring intervention compared to >99% w/ Angio – Esophagus • Esophagoscopy • Esophagram • Varying sens (90%), spec, & accuracy – Recommended to use both – ( almost 100% sens. Per 1 study) – Airway • Laryngoscopy • Tracheoscopy/Broncoscopy (Gold Standard)
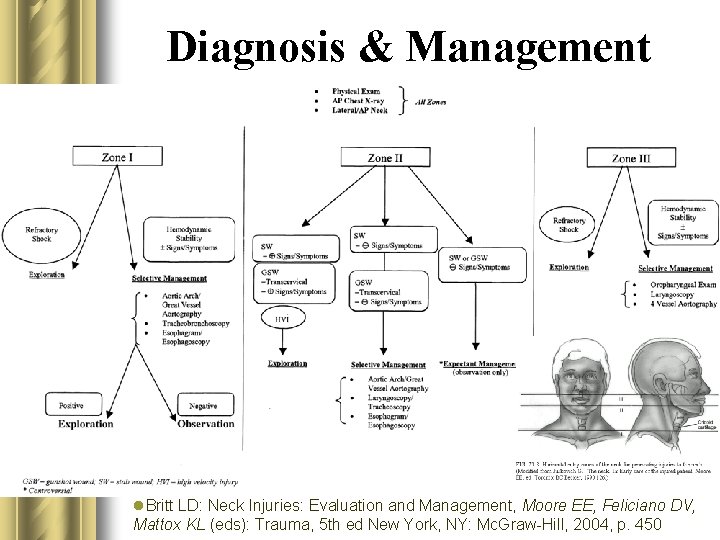
Diagnosis & Management l l. Britt LD: Neck Injuries: Evaluation and Management, Moore EE, Feliciano DV, Mattox KL (eds): Trauma, 5 th ed New York, NY: Mc. Graw-Hill, 2004, p. 450
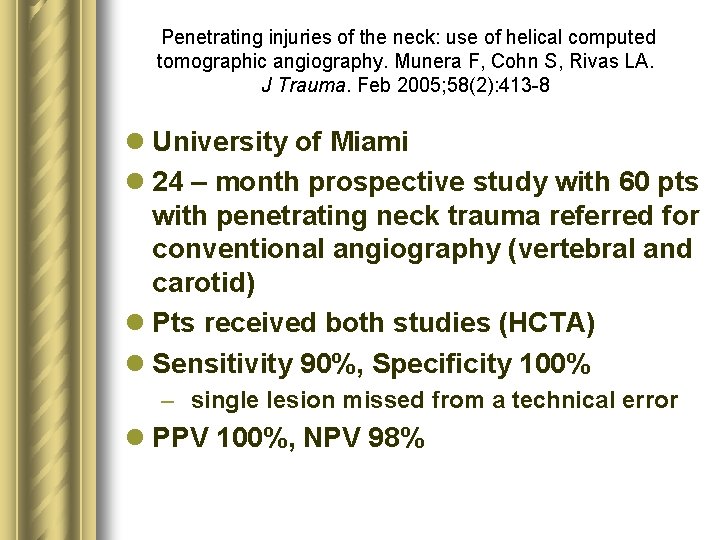
Penetrating injuries of the neck: use of helical computed tomographic angiography. Munera F, Cohn S, Rivas LA. J Trauma. Feb 2005; 58(2): 413 -8 l University of Miami l 24 – month prospective study with 60 pts with penetrating neck trauma referred for conventional angiography (vertebral and carotid) l Pts received both studies (HCTA) l Sensitivity 90%, Specificity 100% – single lesion missed from a technical error l PPV 100%, NPV 98%
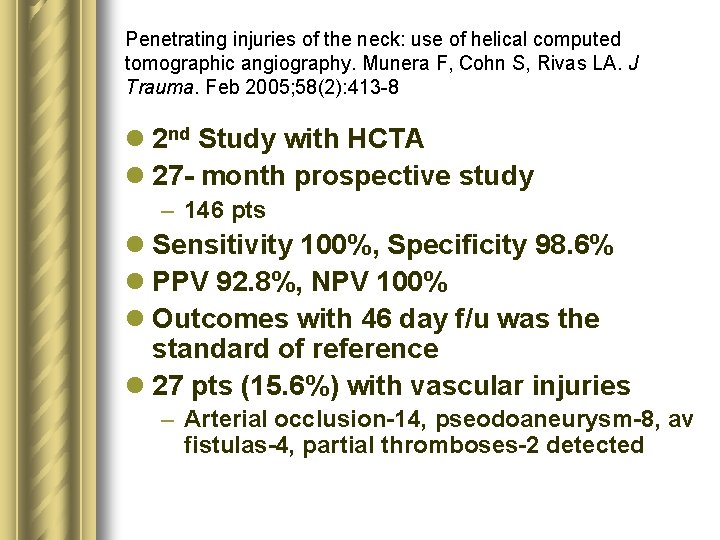
Penetrating injuries of the neck: use of helical computed tomographic angiography. Munera F, Cohn S, Rivas LA. J Trauma. Feb 2005; 58(2): 413 -8 l 2 nd Study with HCTA l 27 - month prospective study – 146 pts l Sensitivity 100%, Specificity 98. 6% l PPV 92. 8%, NPV 100% l Outcomes with 46 day f/u was the standard of reference l 27 pts (15. 6%) with vascular injuries – Arterial occlusion-14, pseodoaneurysm-8, av fistulas-4, partial thromboses-2 detected
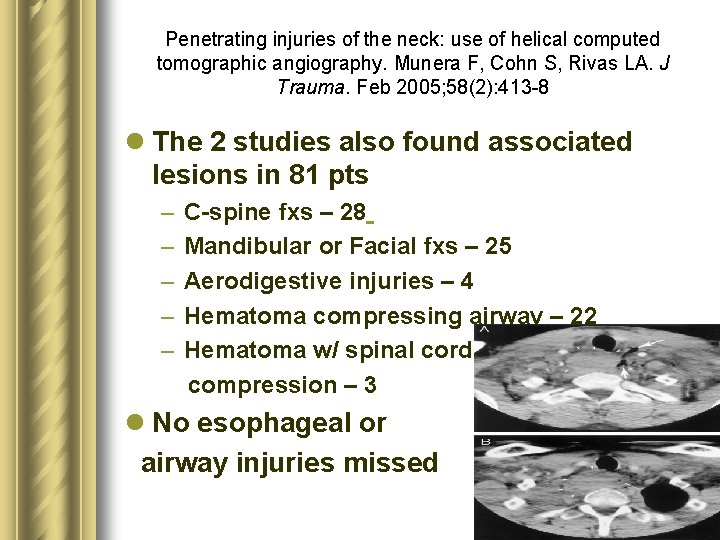
Penetrating injuries of the neck: use of helical computed tomographic angiography. Munera F, Cohn S, Rivas LA. J Trauma. Feb 2005; 58(2): 413 -8 l The 2 studies also found associated lesions in 81 pts – – – C-spine fxs – 28 Mandibular or Facial fxs – 25 Aerodigestive injuries – 4 Hematoma compressing airway – 22 Hematoma w/ spinal cord compression – 3 l No esophageal or airway injuries missed

CT Angiography in Penetrating Neck Trauma Reduces the Need for Operative Neck Exploration. Woo K et al. American Surgeon. 71(9): 754 -8, 2005 Sep. l Conclusions from this study recommend HCTA as a screening test, as the tract of injury can be seen – 1. Tract seen, no injuries NO surgery – 2. Injury to vascular or aerodigestive structure surgery – 3. Indeterminate scan further eval.
HCTA/MDCT l Limitations – Artifact from bullet fragments or other metallic foreign bodies and shoulders of large pts – Inability to perform endovascular therapy simultaneously – Not in real time
HCTA/MDCT l Benefits – Less expensive – Don’t have to call in the angio team – Less Invasive – 3 -D reconstruction – Can see trajectory of penetrating injury and proximity to structures
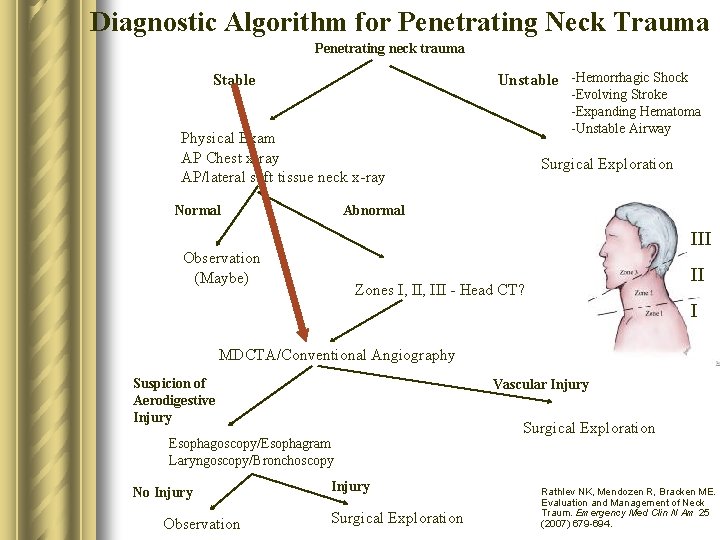
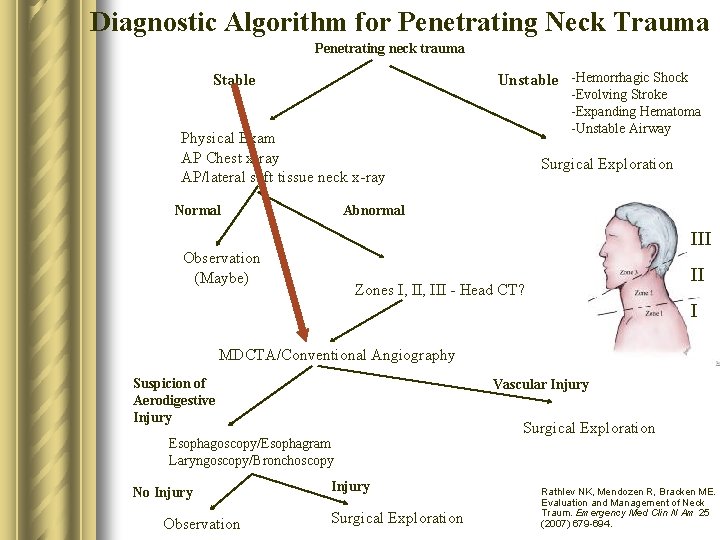
Diagnostic Algorithm for Penetrating Neck Trauma Penetrating neck trauma Unstable -Hemorrhagic Shock Stable -Evolving Stroke -Expanding Hematoma -Unstable Airway Physical Exam AP Chest x-ray AP/lateral soft tissue neck x-ray Normal Surgical Exploration Abnormal III Observation (Maybe) II Zones I, III - Head CT? I MDCTA/Conventional Angiography Suspicion of Aerodigestive Injury Vascular Injury Esophagoscopy/Esophagram Laryngoscopy/Bronchoscopy No Injury Observation Injury Surgical Exploration Rathlev NK, Mendozen R, Bracken ME. Evaluation and Management of Neck Traum. Emergency Med Clin N Am 25 (2007) 679 -694.
Moonlighting l Soooo…. What do you do when you are moonlighting in Marlette and a Penetrating Neck Injury walks in? l Is the platysma violated? l What would you do even if you had a HCT scanner and you found an injury? l What is your on call surgeon comfortable with?
Summary l ABCs l RSI with a back up (cric. ) l Does it penetrate the platysma l All unstable patients immediately go to the OR l Good Physical Exam l Don’t miss the esophageal Injury l If stable, consider MDCTA as a screening evaluation
References l l l Britt LD: Neck Injuries: Evaluation and Management, Moore EE, Feliciano DV, Mattox KL (eds): Trauma, 5 th ed New York, NY: Mc. Graw-Hill, 2004, p. 445 Mandavia DP, Qualls S, Rokos I. Emergency airway management in penetrating neck injury. Ann Emerg Med. Mar 2000; 35(3): 221 -5 Weitzel N, Kendall J, Pons P. Blind nasotracheal intubation for patients with penetrating neck trauma. J Trauma. May 2004; 56(5): 1097 -101 Steinfeldt J, Bey TA, Rich JM. Use of a gum elastic bougie (GEB) in a zone II penetrating neck trauma: a case report. J Emerg Med 2003; 24: 267 -70 Tintinalli, J. E. , Kelen, G. D. , and Stapczynski, J. S. (Eds. ) (2004) Disaster Medical Services: Chapter 258. Emergency Medicine: A Comprehensive Study Guide, 6 th Edition. Mc. Graw-Hill. Levy D. Neck Trauma, Emedicine. Available at: www. emedicine. com/emerg/topic 331. htm Cheng E. Penetrating Neck Trauma, Emedicine. Available at: www. emedicine. com/med/topic 2802. htm Munera F, Cohn S, Rivas LA. Penetrating injuries of the neck: use of helical computed tomographic angiography. J Trauma. Feb 2005; 58(2): 413 -8. Woo K et al. CT Angiography in Penetrating Neck Trauma Reduces the Need for Operative Neck Exploration. American Surgeon. 71(9): 754 -8, 2005 Sep. Kuzniec S, Kauffman P, Molnar LJ, et al. Diagnosis of Limb and Neck Arterial Trauma using Duplex Ultrasonography, Cardiovasc Surg. 1998: 6: 358 -66 Rathlev NK, Mendozen R, Bracken ME. Evaluation and Management of Neck Traum. Emergency Med Clin N Am 25 (2007) 679 -694. Collucciello S. Neck Trauma (Soft Tissue Injuries). EMRAP: Emergency Medicine Reviews and Perspectives 2006 Aug.
l www. youtube. com/watch? v=UMHWkbn. Dfg&feature=related
 Ground penetrating radar
Ground penetrating radar Non penetrating glaucoma surgery
Non penetrating glaucoma surgery Civil engineering applications of ground penetrating radar
Civil engineering applications of ground penetrating radar Cell penetrating peptides
Cell penetrating peptides Nate parsley
Nate parsley Nate conger
Nate conger Justin sconza
Justin sconza Nate mantua
Nate mantua Nate bard
Nate bard The true living god
The true living god Nate plasch
Nate plasch Nate powers
Nate powers Queer
Queer Nate booth
Nate booth Naté dearden
Naté dearden Nate humphrey
Nate humphrey Nate ramirez
Nate ramirez Nate rifkin
Nate rifkin Bipartição
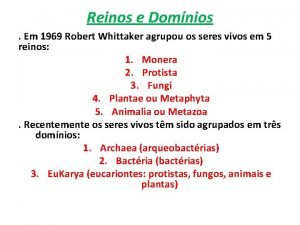
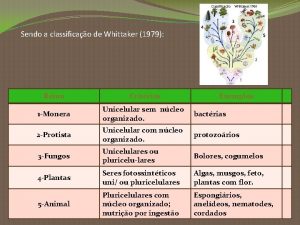
Bipartição Critérios de whittaker
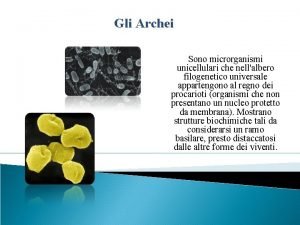
Critérios de whittaker Whittaker e woese
Whittaker e woese Milagro beanfield war summary
Milagro beanfield war summary 2cft
2cft Whittaker modificado
Whittaker modificado Whittaker
Whittaker Brad whittaker
Brad whittaker Sistema de whittaker modificado
Sistema de whittaker modificado Vaughn whittaker
Vaughn whittaker Classificazione di whittaker
Classificazione di whittaker Sistema de whittaker modificado
Sistema de whittaker modificado Libby whittaker
Libby whittaker Whittaker
Whittaker Curva rango abundancia
Curva rango abundancia Ace study score
Ace study score Ruptur ginjal grade
Ruptur ginjal grade Trauma yoga ausbildung
Trauma yoga ausbildung Psykoedukation ptsd
Psykoedukation ptsd Oliver hautmann
Oliver hautmann Trauma from occlusion
Trauma from occlusion Infermiere divisione in sillabe
Infermiere divisione in sillabe Trauma vascular
Trauma vascular 4 r's trauma informed care
4 r's trauma informed care Trauma informed care for foster youth
Trauma informed care for foster youth Trauma recovery and empowerment model
Trauma recovery and empowerment model Trauma gestig behindert
Trauma gestig behindert Cavitacion en trauma
Cavitacion en trauma What is trauma
What is trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Power to resist trauma
Power to resist trauma Ao trauma
Ao trauma Isi pikir
Isi pikir Trauma infromed
Trauma infromed Cinematica del trauma
Cinematica del trauma Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Choque medular
Choque medular Stan and ute lawrence
Stan and ute lawrence Pasg trauma
Pasg trauma