PEDIATRIC DISASTER TRIAGE UTILIZING THE JUMPSTART METHOD MARCH




- Slides: 109
PEDIATRIC DISASTER TRIAGE UTILIZING THE JUMPSTART © METHOD MARCH 2016 (4 TH EDITION) Illinois Emergency Medical Services for Children is a collaborative program between the Illinois Department of Public Health and Loyola University Chicago
Disclaimer This slide set and all related training information provided in this session is in accordance with current practice at the time that this program was developed.
Acknowledgements • This 4 th edition education program was developed under the direction and guidance of the Illinois Pediatric Preparedness Workgroup. The original program was adapted in 2006 from a module developed by Children’s Memorial Hospital (now Ann & Robert H. Lurie Children’s Hospital of Chicago). • This program was developed from an Assistant Secretary for Preparedness and Response (ASPR) Hospital Preparedness Program (HPP) grant. All training materials are considered under public domain and can be utilized by others in the conduction of similar educational programs, provided there is acknowledgement of the source of these materials.
Objectives • Identify unique characteristics that make children more vulnerable in a disaster • Discuss mass casualty triage and the pediatric patient • Review START and Jump. START© Triage Tools and the SMART Triage Pacs™ • Demonstrate the use of the START and Jump. START© Triage Tool
Objectives (continued) • Discuss the instructor role for Jump. START© Triage Training • Identify Healthcare Professionals in your EMS Region to target for Jump. START© Triage training • Discuss the necessary steps to teach a Jump. START© Provider and Instructor Class • Review the training materials that are necessary to teach a Jump. START© Provider and Instructor Class
Introduction
Background Illinois Emergency Medical Services for Children (EMSC) 1984: National EMSC Program established through federal legislation • Jointly sponsored by • Maternal & Child Health Bureau • National Highway Traffic Safety Administration • States are charged with enhancing the pediatric component of their Emergency Medical Services (EMS) systems. 1994: Illinois EMSC was established.
Illinois EMSC Pediatric Disaster Preparedness • 2002: • Illinois Pediatric Bioterrorism Workgroup convened • Name changed in 2011 to Pediatric Preparedness Workgroup to ensure a more all-hazards approach. • Reports to EMSC Advisory Board and Illinois Terrorism Task Force • Assists in assuring that the special needs of children are addressed during a disaster or terrorist event by: • Enhancing awareness of pediatric needs • Identifying/sharing best practices • Developing resource documents, tools, and guidelines • Integrating disaster preparedness into existing state initiatives
Illinois Communities • Illinois is the 5 th most populous state with a population of 12. 9 million • Almost 3 million children <18 years of age • Approximately 800, 000 are age five and younger.
Children and Disasters
Disaster “A medical disaster occurs when the destructive effects of natural or man made forces overwhelm the ability of a given area or community to meet the demand for health care. ” (Source: ACEP Disaster Medical Services Policy Statement, 2006)
Natural Disasters • Earthquake • Flood • Snow/ice storm • Tornado • Others
Human Caused Disasters • Terrorist Events • Arson • Bombings • Shootings • Use of chemical, biological or nuclear agents • Hazmat incidents
Terrorist Events and the Pediatric Population Myth Kids are secondary victims of terrorism and inadvertently targeted Fact Children may be intentionally targeted
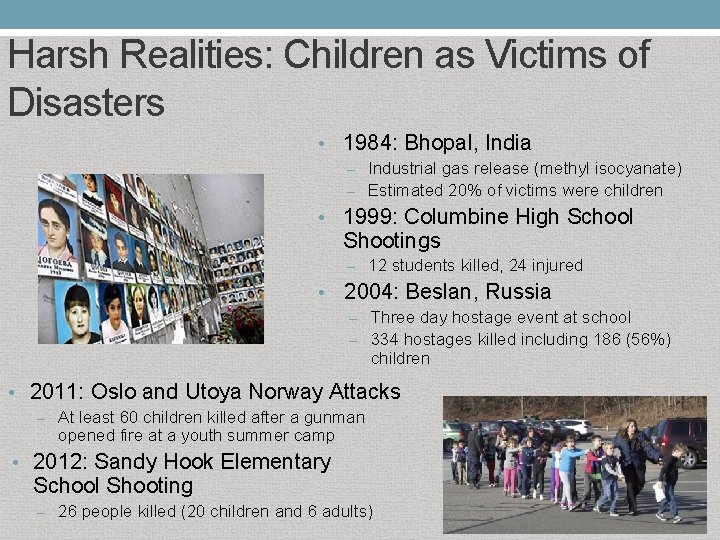
Harsh Realities: Children as Victims of Disasters • 1984: Bhopal, India – Industrial gas release (methyl isocyanate) – Estimated 20% of victims were children • 1999: Columbine High School Shootings – 12 students killed, 24 injured • 2004: Beslan, Russia – Three day hostage event at school – 334 hostages killed including 186 (56%) children • 2011: Oslo and Utoya Norway Attacks – At least 60 children killed after a gunman opened fire at a youth summer camp • 2012: Sandy Hook Elementary School Shooting – 26 people killed (20 children and 6 adults)
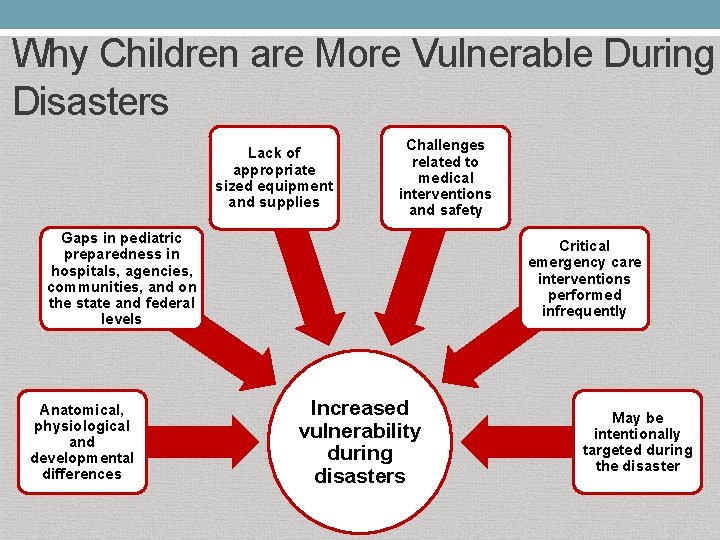
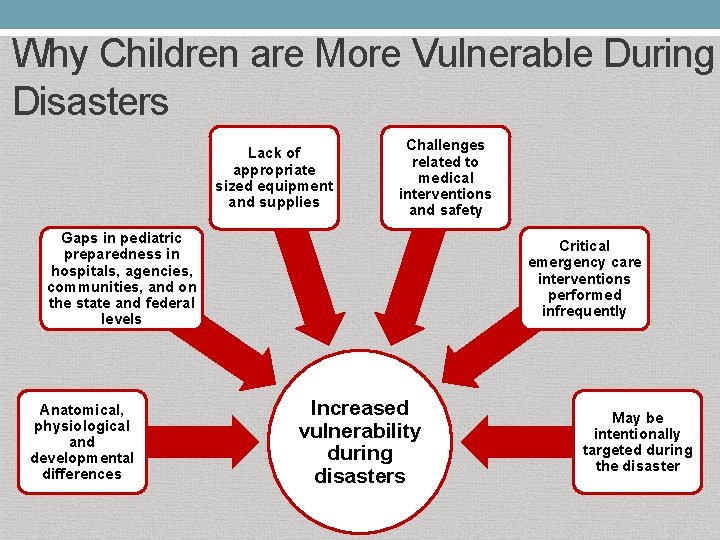
Why Children are More Vulnerable During Disasters Lack of appropriate sized equipment and supplies Challenges related to medical interventions and safety Gaps in pediatric preparedness in hospitals, agencies, communities, and on the state and federal levels Anatomical, physiological and developmental differences Critical emergency care interventions performed infrequently Increased vulnerability during disasters May be intentionally targeted during the disaster
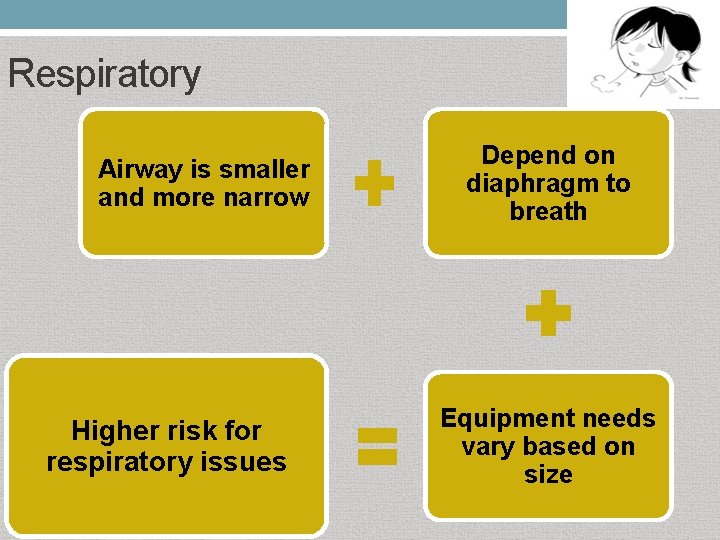
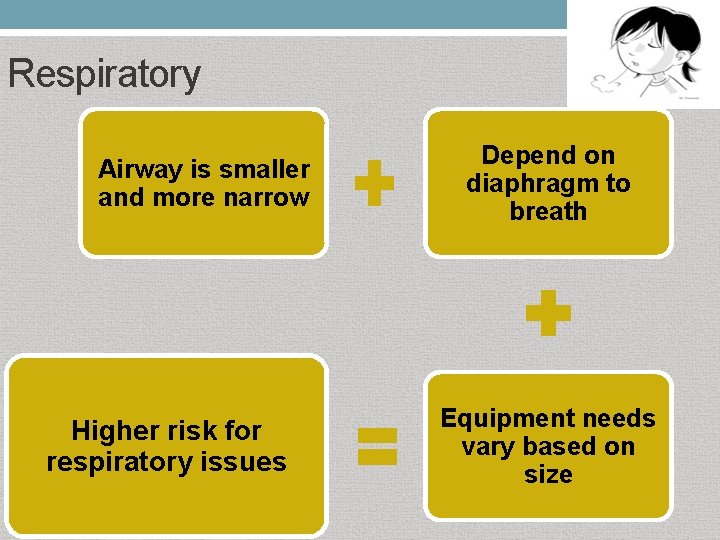
Respiratory Airway is smaller and more narrow Higher risk for respiratory issues Depend on diaphragm to breath Equipment needs vary based on size
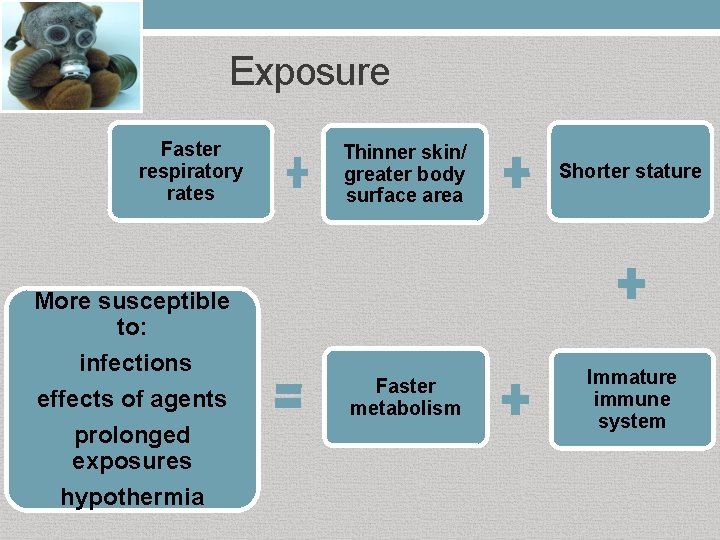
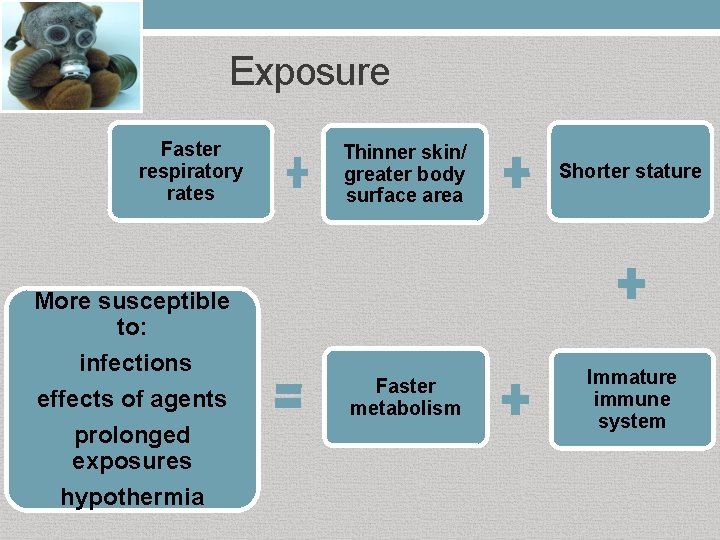
Exposure Faster respiratory rates More susceptible to: infections effects of agents prolonged exposures hypothermia Thinner skin/ greater body surface area Shorter stature Faster metabolism Immature immune system
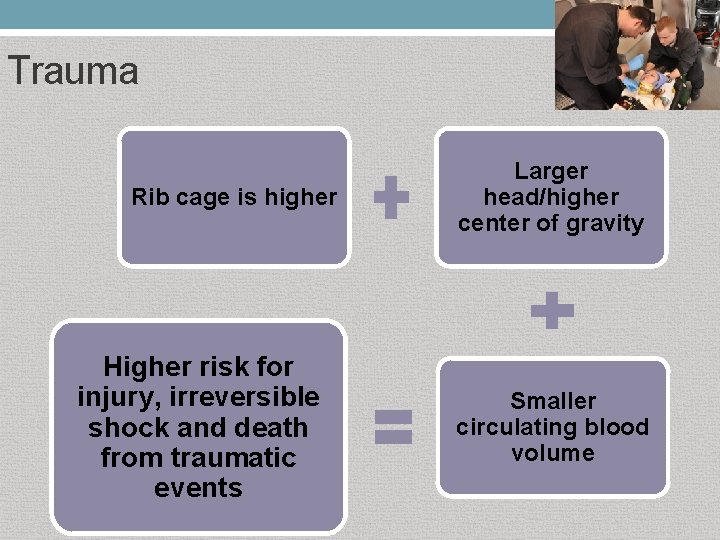
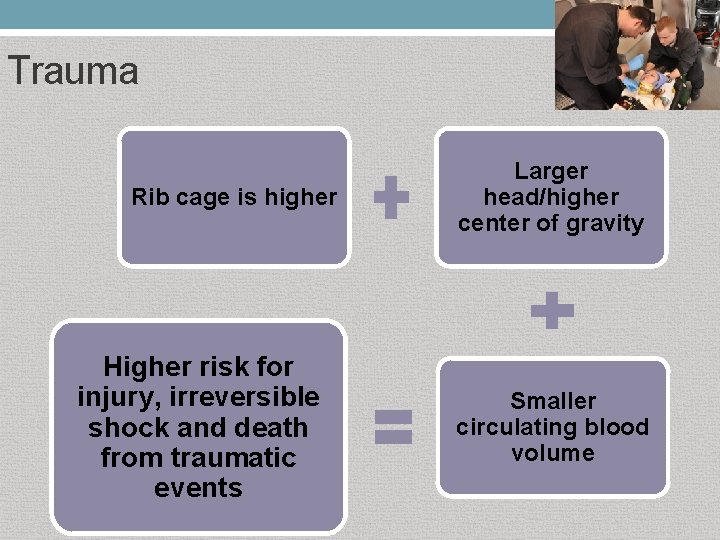
Trauma Rib cage is higher Higher risk for injury, irreversible shock and death from traumatic events Larger head/higher center of gravity Smaller circulating blood volume
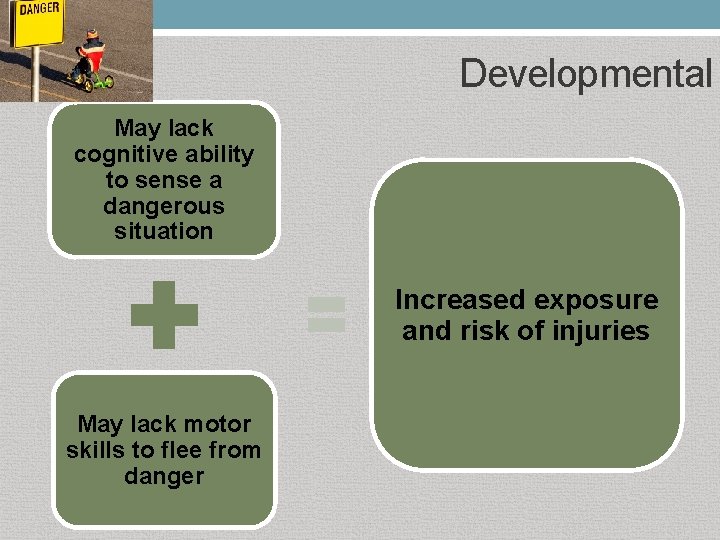
Developmental May lack cognitive ability to sense a dangerous situation Increased exposure and risk of injuries May lack motor skills to flee from danger
Developmental May be nonverbal or not know personal information Age & developmental level influences response to stressful events May be uncooperative Unable to help with reunification Long term psychological effects are possible
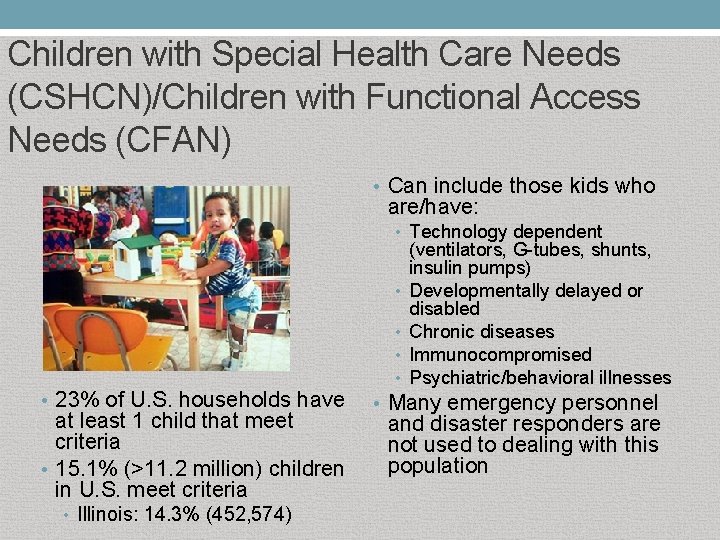
Children with Special Health Care Needs (CSHCN)/Children with Functional Access Needs (CFAN) • Can include those kids who are/have: • Technology dependent • • • 23% of U. S. households have at least 1 child that meet criteria • 15. 1% (>11. 2 million) children in U. S. meet criteria • Illinois: 14. 3% (452, 574) (ventilators, G-tubes, shunts, insulin pumps) Developmentally delayed or disabled Chronic diseases Immunocompromised Psychiatric/behavioral illnesses • Many emergency personnel and disaster responders are not used to dealing with this population
Triage
Triage • • • Sorting and prioritizing patients Looks at the medical needs and urgency of each individual patient Conventional Triage • • Do the best for each individual Disaster/MCI Triage Do the greatest good for the greatest number • Based on physiology • Provides an objective framework for stressful and emotional decisions • Helps in resource allocation •
Triage • Primary Triage • • Typically performed at the scene of the incident Helps prioritize patients for evacuation/transport Can occur at a hospital Secondary Triage • • • Performed to re-evaluate the patient after primary triage has been completed Typically done once the patient arrives at the hospital. Can also take place at an alternate care site or at the scene of the incident if prolonged scene time or in casualty collection areas
Mass Casualty Incident Any incident in which there are more patients than rescuers (Source: newyearseve. com)
~80% of casualties self or buddy transport to the closest hospital
MCI Triage • All victims must have equal importance at the time of primary triage • Sort patients based on the need for immediate care • Be able to recognize futility • No patient group can receive special consideration other than that dictated by their physiologic state This includes children! (Source: Dr. Lou Romig-slide presentation: Jump. START Pediatric Multi-casualty Triage System)
MCI Triage Categories • IMMEDIATE = Emergent IMMEDIATE • DELAYED = Urgent DELAYED • MINOR = Non-urgent/walking MINOR wounded • EXPECTANT/DECEASED = Dead/little to no hope of survival

IMMEDIATE Severely ill/injured but treatable and able to be saved with relatively quick treatment and transport • Examples: • Severe bleeding • Shock • Open chest or abdominal wounds • Severe respiratory distress • Emotionally out of control (Source: Optimistworld. com/anaphylaxis)
DELAYED Injured/ill and unable to walk on their own; Potentially serious injuries/illnesses but stable enough to wait a short while for medical treatment • Examples • Burns with no respiratory distress • Spinal injuries • Moderate blood loss • Conscious with head injury (Source: Chemaxx. com)
MINOR Minor injuries/illnesses that can wait for a longer period of time for treatment • Examples • Minor fractures • Minor bleeding • Minor lacerations
EXPECTANT/DECEASED Dead or obviously dying; May have signs of life but injuries are incompatible with survival • Examples • Cardiac arrest • Respiratory arrest with a pulse • Massive head injury
Triaging Expectant/Deceased Patients • Can be psychologically difficult to tag a child as Expectant/Deceased • Can be hard to resist the tendency to assign pediatric patients a higher triage category just because they are children • Using a MCI triage tool especially with children can help to eliminate the role of emotions in the triage process • Objective triage criteria during an MCI can provide emotional support for triage personnel forced to make life or death decisions for children
MCI Triage Considerations Scene Safety • Ensure the scene is safe before entering • Assess for need for decontamination Designate Treatment Areas • Establish areas for each triage color category • Triaged patients should be moved to designated areas Incident command (IC) • Process what you see and hear in 30 seconds and paint as accurate a picture as you can in your report to IC
MCI TRIAGE TOOLS

MCI Triage Tools • START Algorithm • Jump. START© Algorithm • SMART Triage Pacs™
START TRIAGE
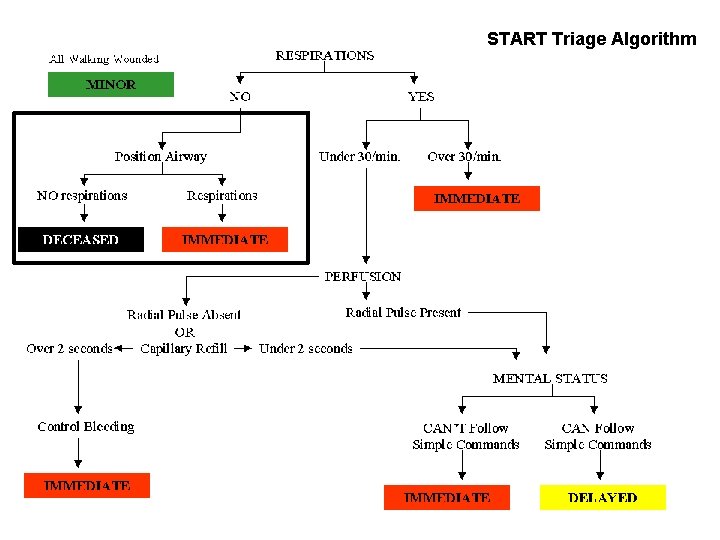
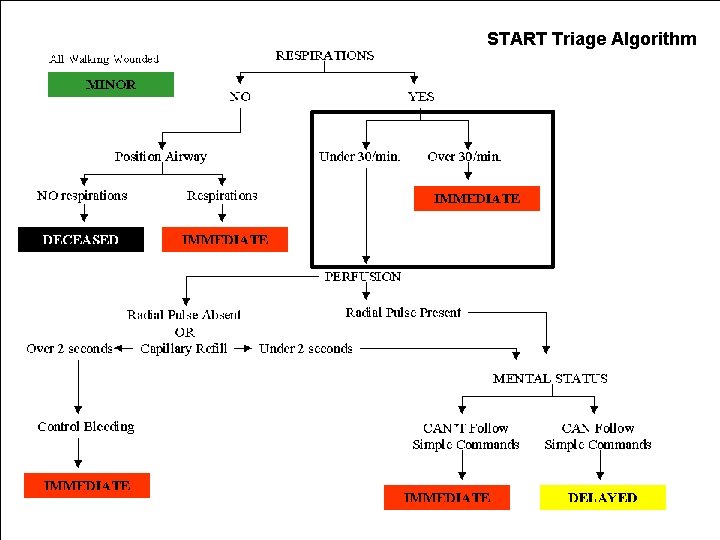
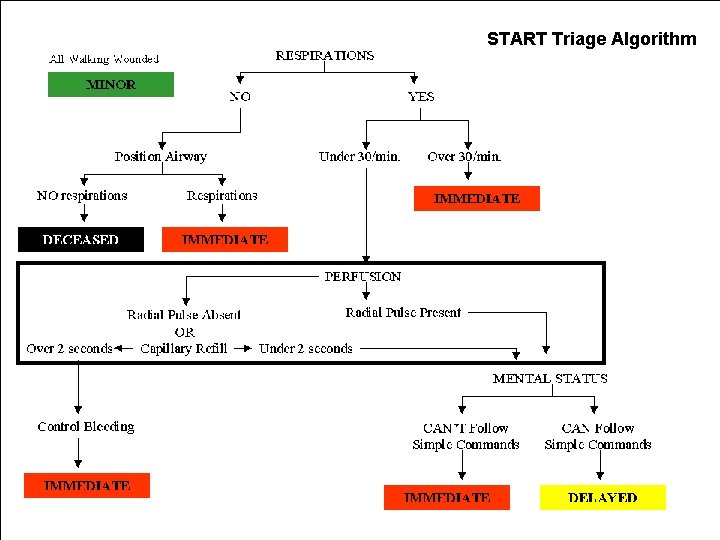
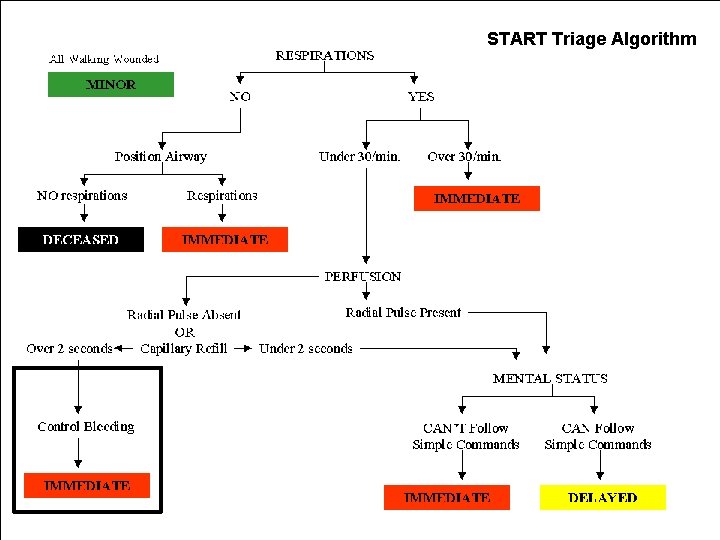
START • Simple Triage And Rapid Treatment • Joint development by the Fire & Marine Department and Hoag Hospital in New Port Beach, California • Gold standard for field adult MCI triage in U. S. and numerous other countries • Utilizes the standard four color triage categories • Used for primary triage • More information at www. start-triage. com
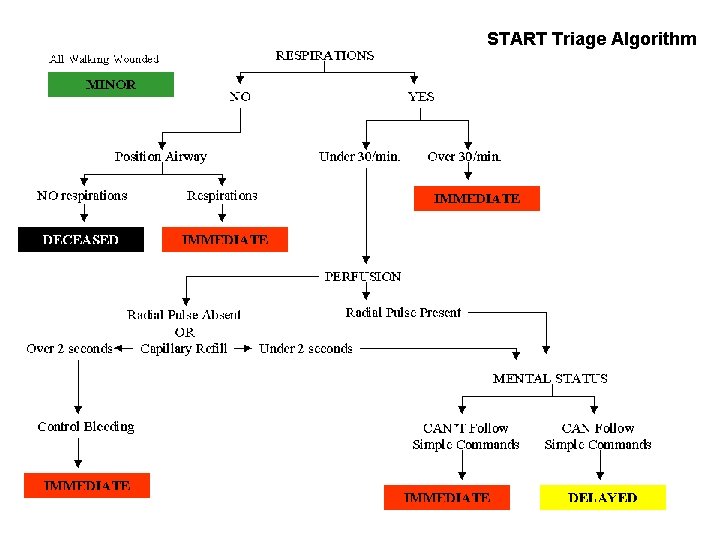
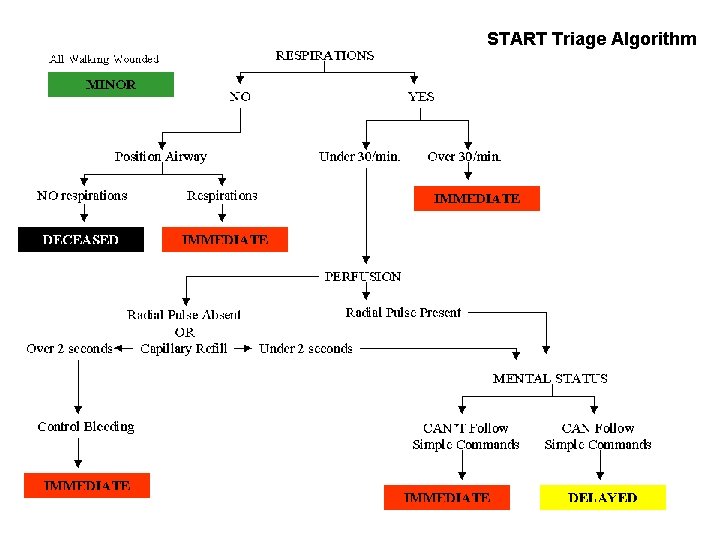
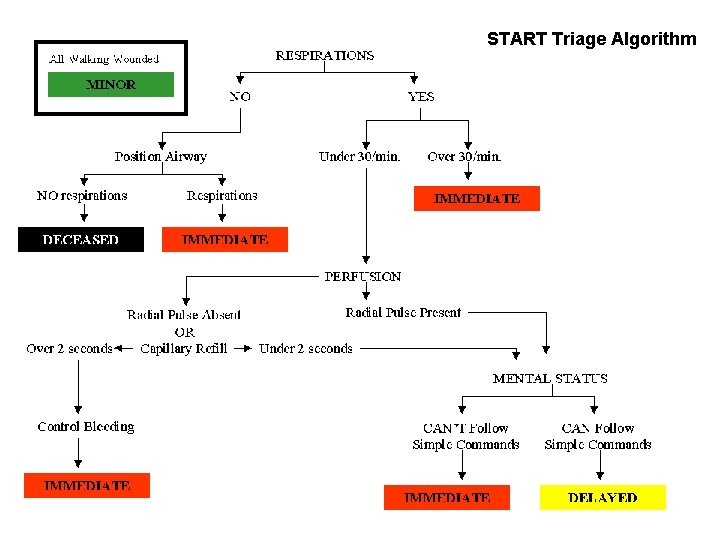
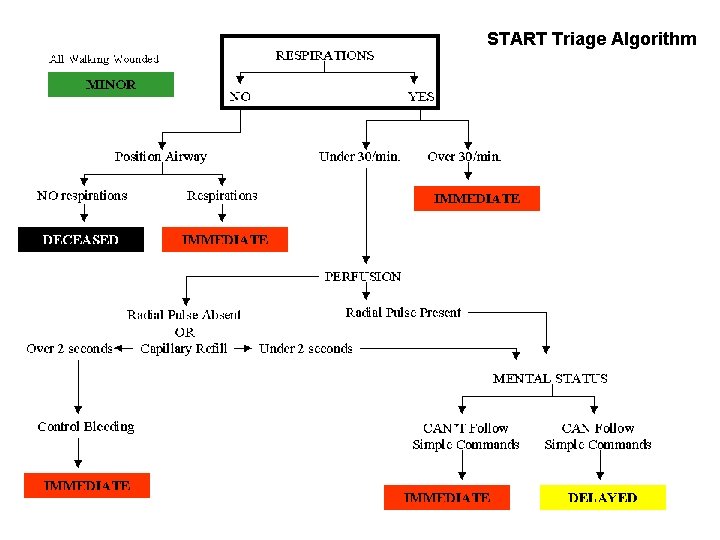
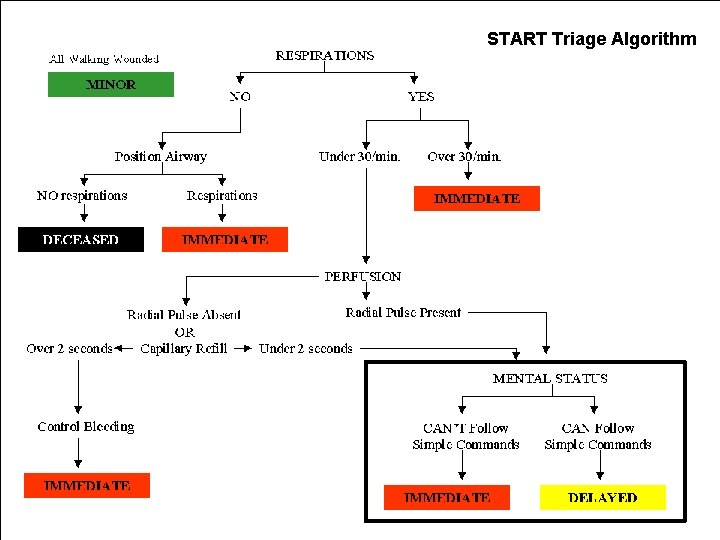
START Triage Algorithm
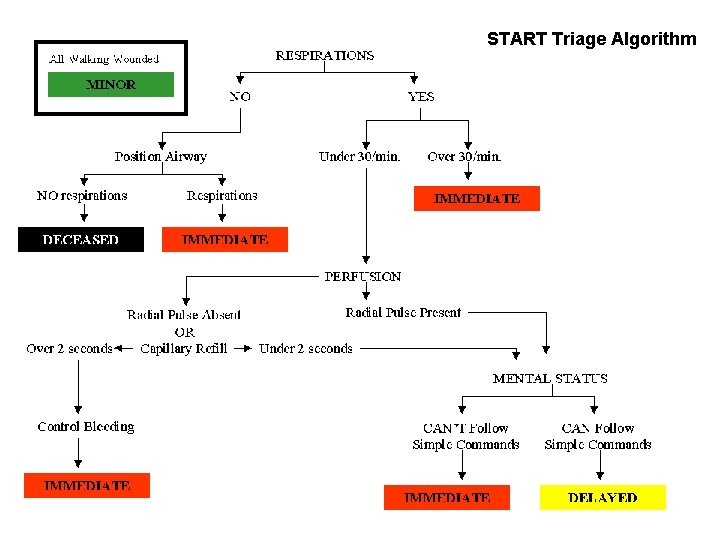
START Triage Algorithm
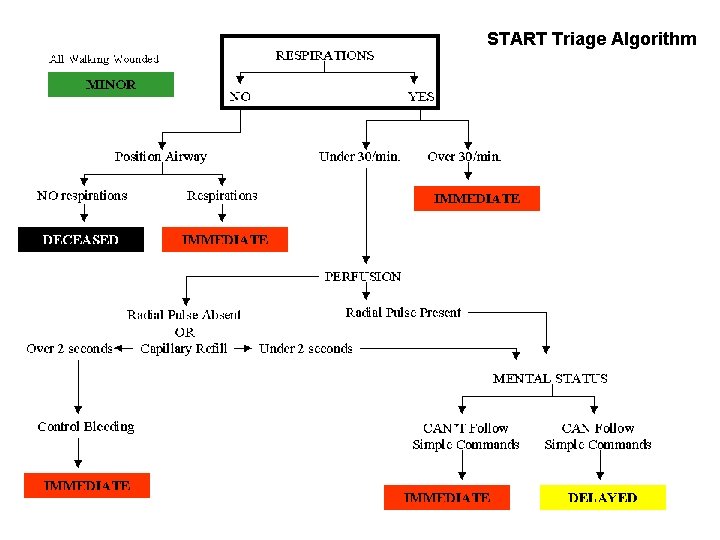
START Triage Algorithm
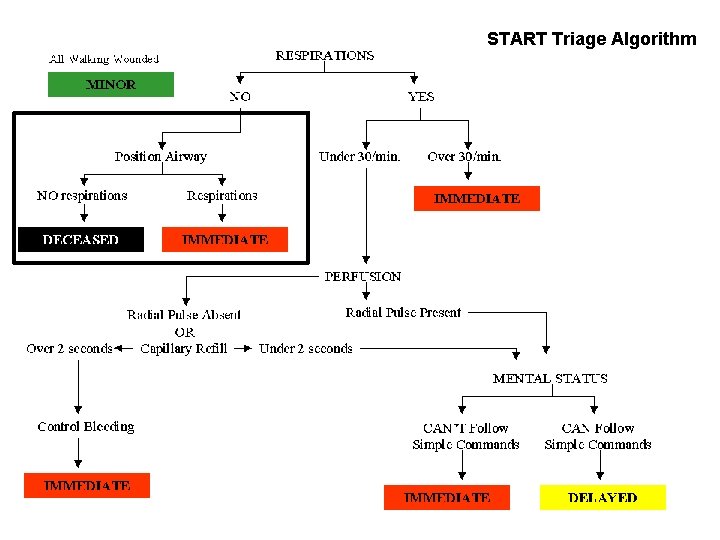
START Triage Algorithm
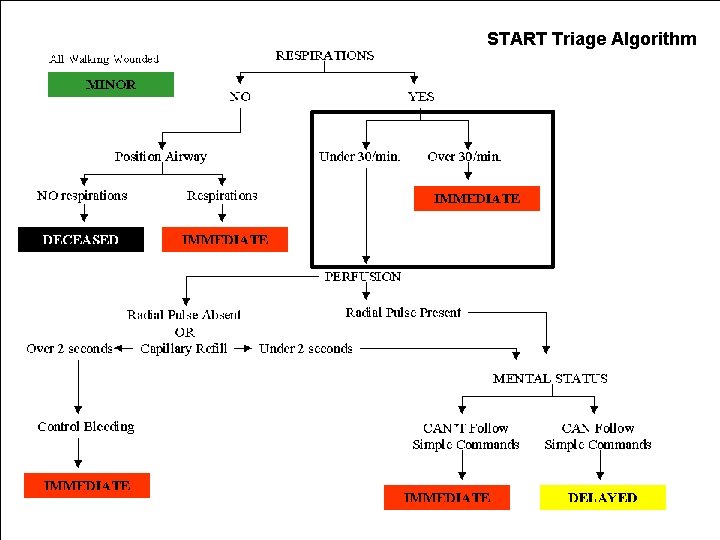
START Triage Algorithm
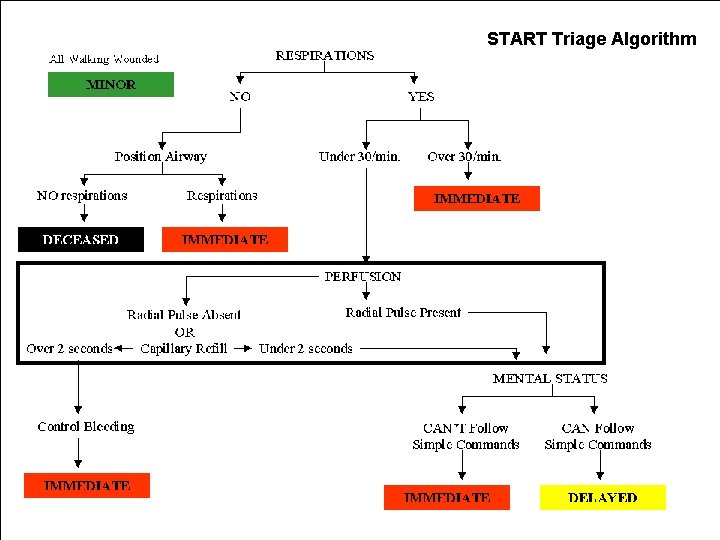
START Triage Algorithm
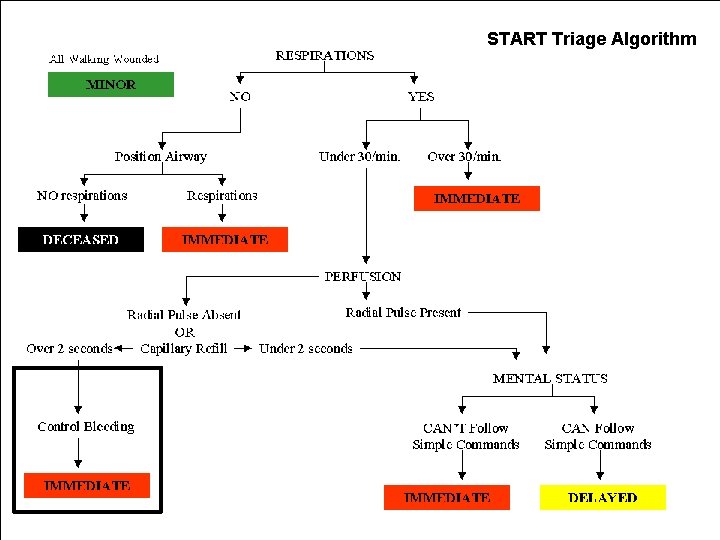
START Triage Algorithm
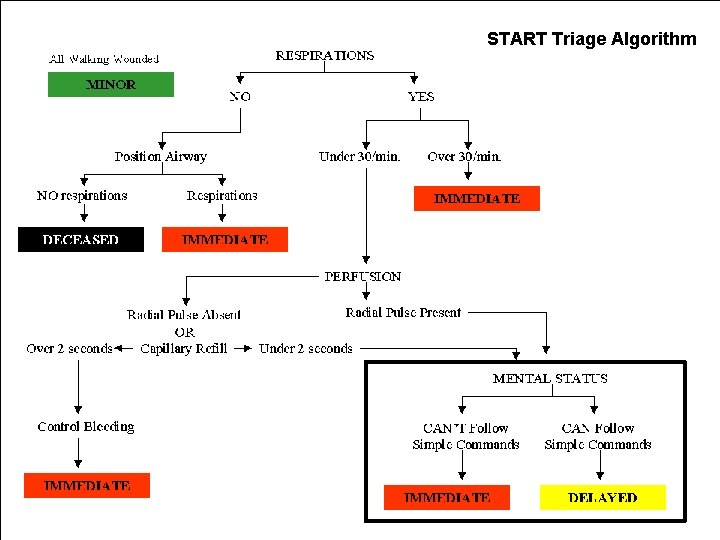
START Triage Algorithm
Jump. START© Triage
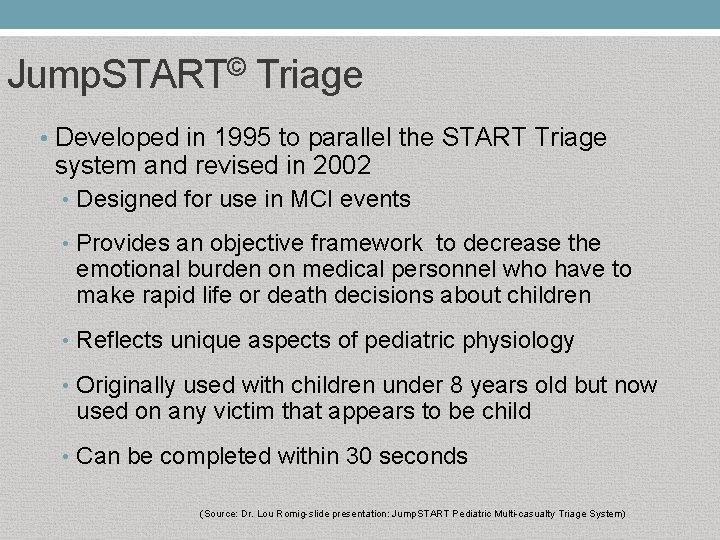
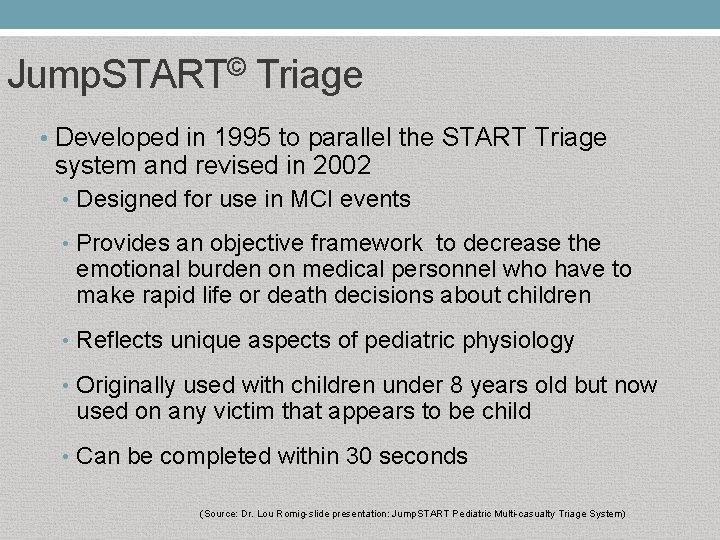
Jump. START© Triage • Developed in 1995 to parallel the START Triage system and revised in 2002 • Designed for use in MCI events • Provides an objective framework to decrease the emotional burden on medical personnel who have to make rapid life or death decisions about children • Reflects unique aspects of pediatric physiology • Originally used with children under 8 years old but now used on any victim that appears to be child • Can be completed within 30 seconds (Source: Dr. Lou Romig-slide presentation: Jump. START Pediatric Multi-casualty Triage System)
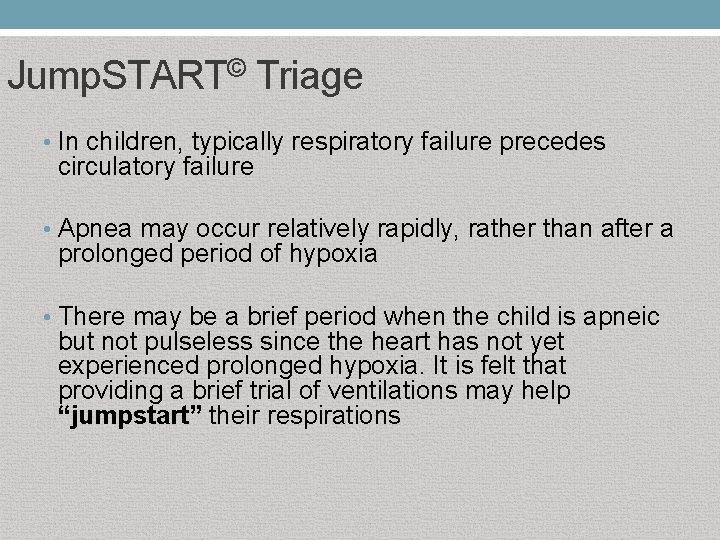
Jump. START© Triage • In children, typically respiratory failure precedes circulatory failure • Apnea may occur relatively rapidly, rather than after a prolonged period of hypoxia • There may be a brief period when the child is apneic but not pulseless since the heart has not yet experienced prolonged hypoxia. It is felt that providing a brief trial of ventilations may help “jumpstart” their respirations
Jump. START© Triage and Age What age defines the pediatric patient?
Jump. START© Triage and Age It can be difficult to discern the age of a child especially preteen and early teen years, and which triage tool to use. If a victim appears to be a CHILD, use Jump. START© If a victim appears to be a YOUNG ADULT, use START (Source: Dr. Lou Romig-slide presentation: Jump. START Pediatric Multi-casualty Triage System)
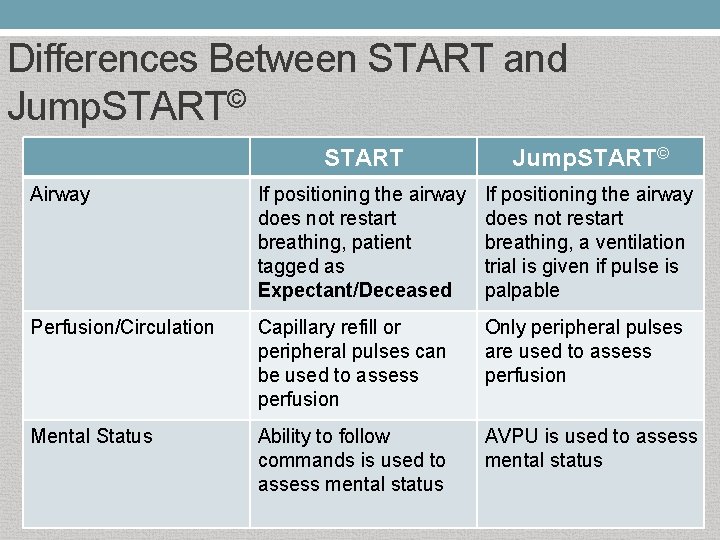
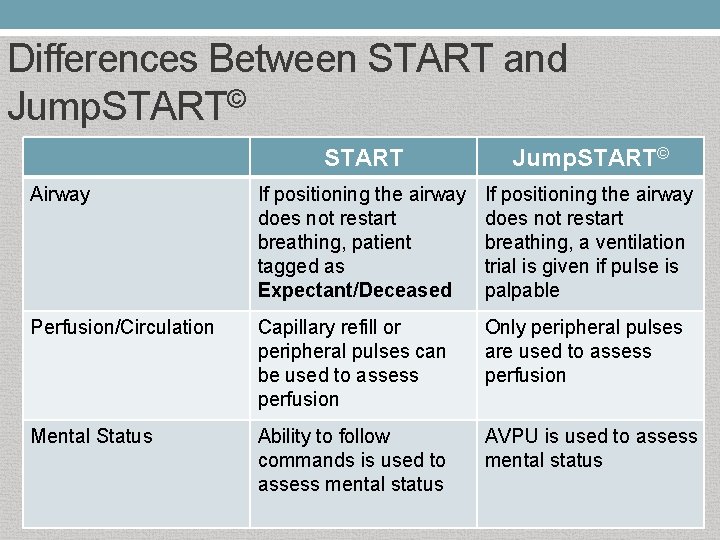
Differences Between START and Jump. START© START Jump. START© Airway If positioning the airway does not restart breathing, patient tagged as Expectant/Deceased If positioning the airway does not restart breathing, a ventilation trial is given if pulse is palpable Perfusion/Circulation Capillary refill or peripheral pulses can be used to assess perfusion Only peripheral pulses are used to assess perfusion Mental Status Ability to follow commands is used to assess mental status AVPU is used to assess mental status
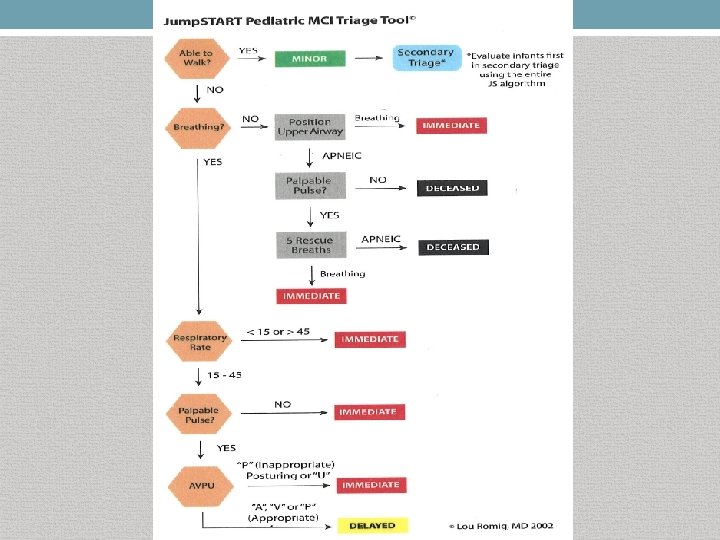
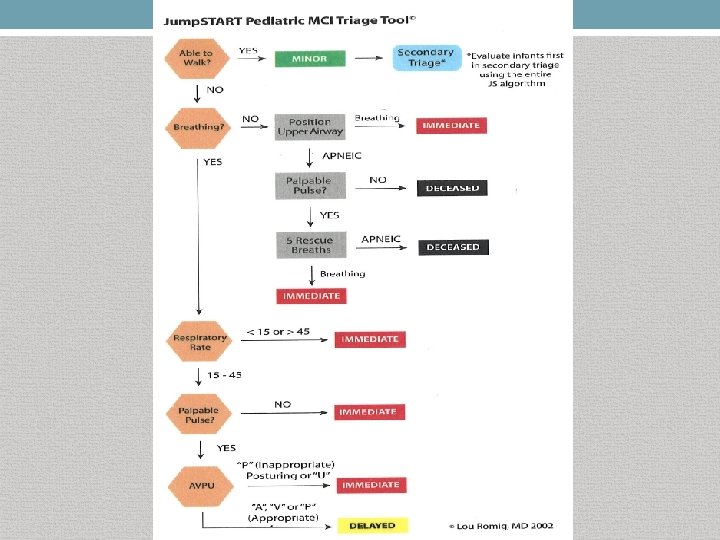
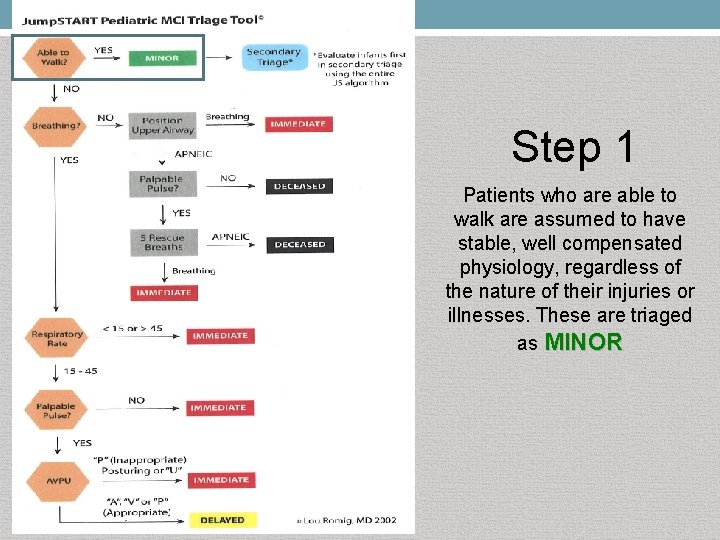
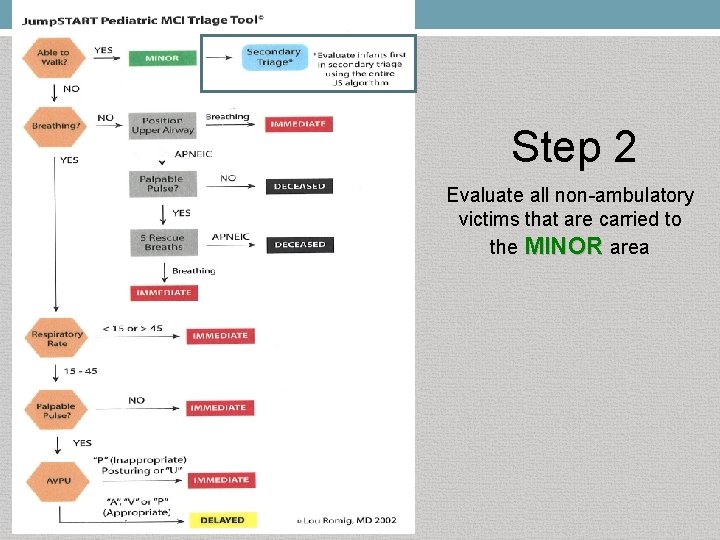
Step 1 Patients who are able to walk are assumed to have stable, well compensated physiology, regardless of the nature of their injuries or illnesses. These are triaged as MINOR
Step 2 Evaluate all non-ambulatory victims that are carried to the MINOR area
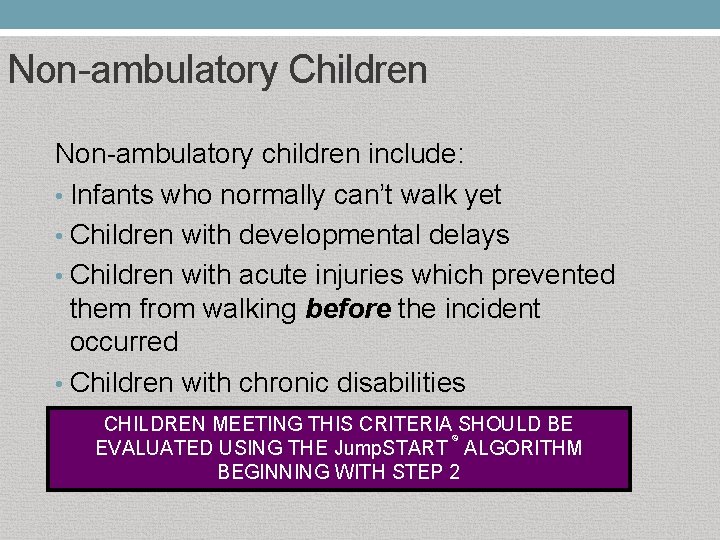
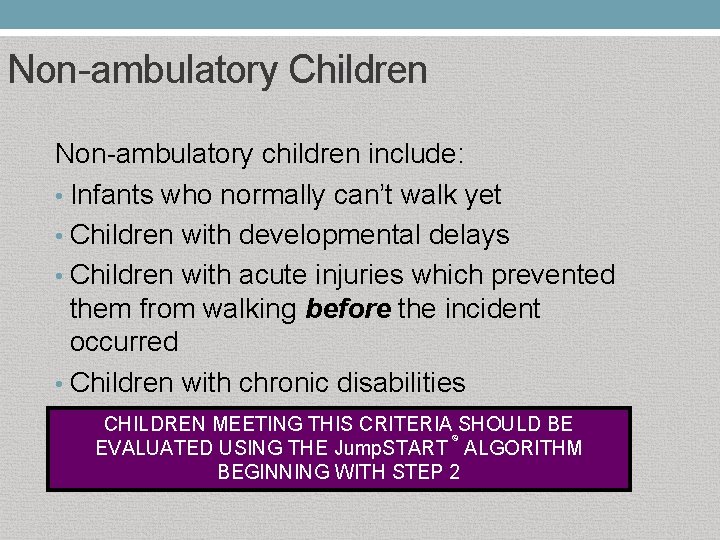
Non-ambulatory Children Non-ambulatory children include: • Infants who normally can’t walk yet • Children with developmental delays • Children with acute injuries which prevented them from walking before the incident occurred • Children with chronic disabilities CHILDREN MEETING THIS CRITERIA SHOULD BE © EVALUATED USING THE Jump. START ALGORITHM BEGINNING WITH STEP 2
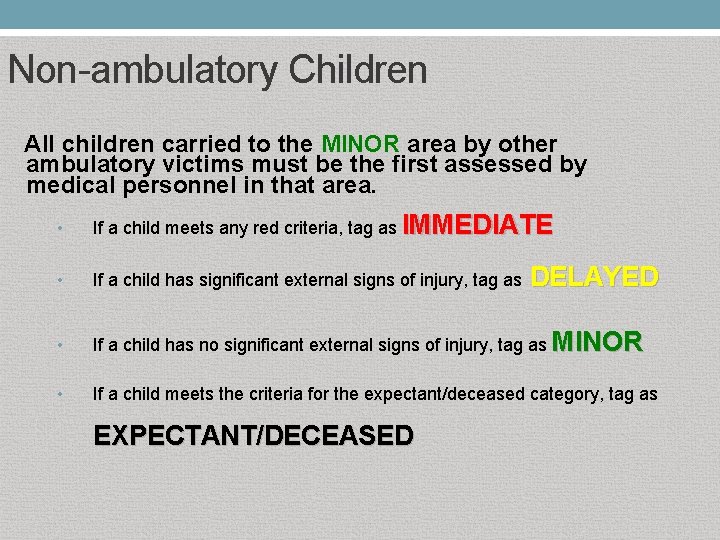
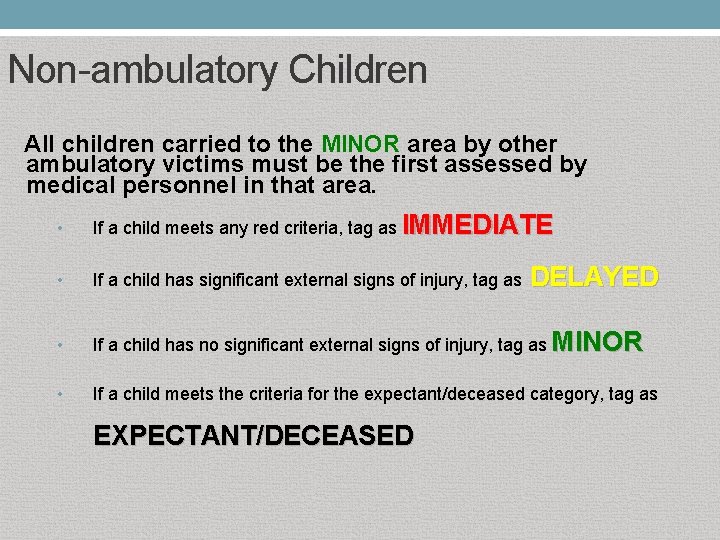
Non-ambulatory Children All children carried to the MINOR area by other ambulatory victims must be the first assessed by medical personnel in that area. • If a child meets any red criteria, tag as IMMEDIATE • If a child has significant external signs of injury, tag as DELAYED • If a child has no significant external signs of injury, tag as MINOR • If a child meets the criteria for the expectant/deceased category, tag as EXPECTANT/DECEASED
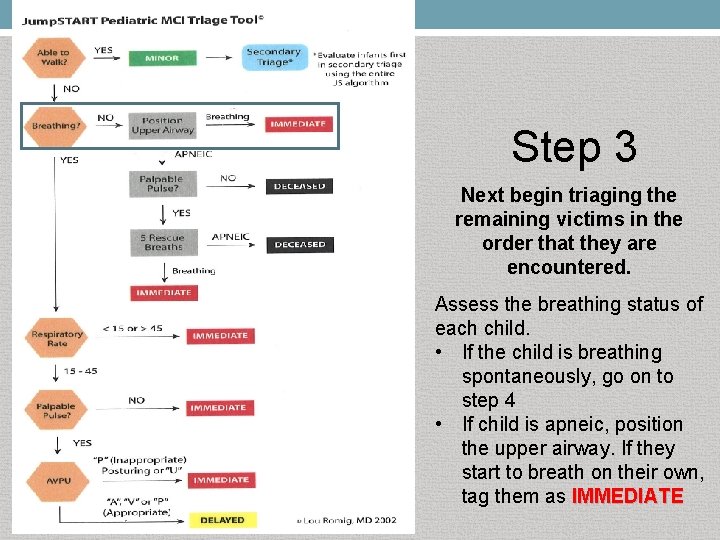
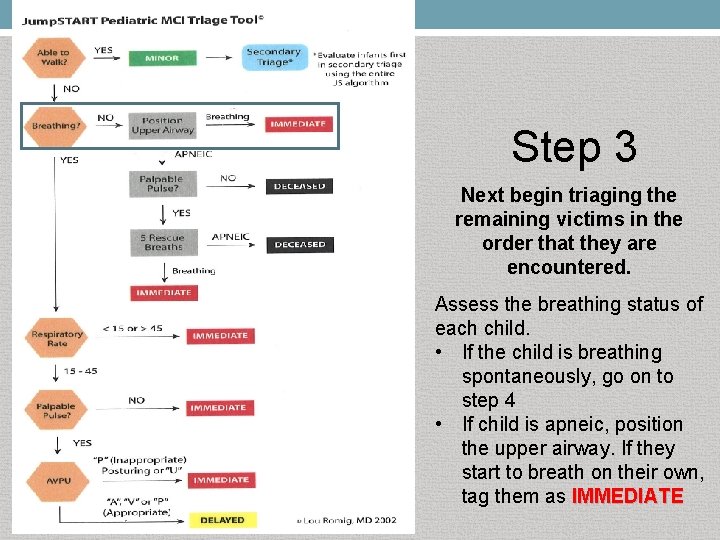
Step 3 Next begin triaging the remaining victims in the order that they are encountered. Assess the breathing status of each child. • If the child is breathing spontaneously, go on to step 4 • If child is apneic, position the upper airway. If they start to breath on their own, tag them as IMMEDIATE
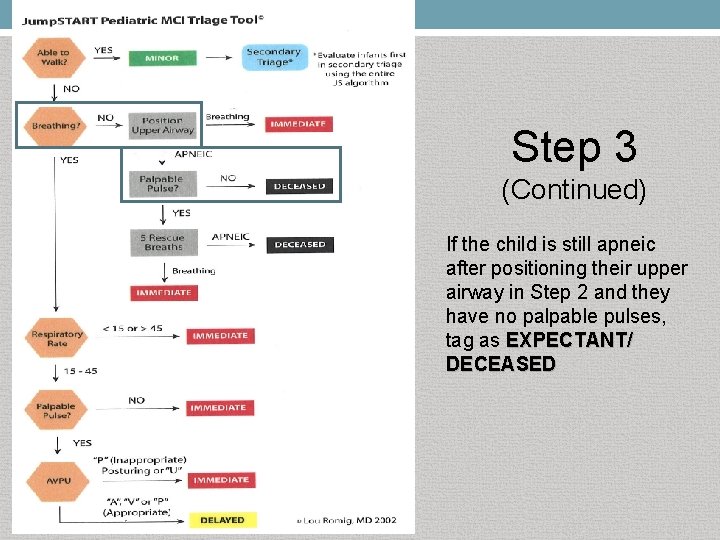
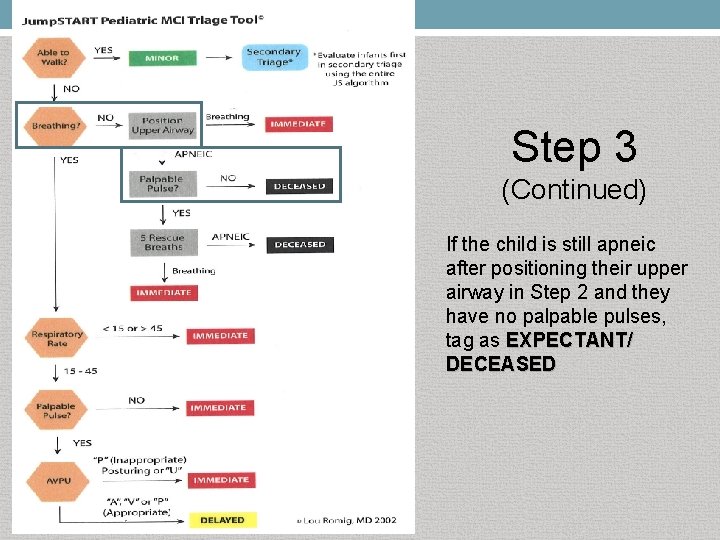
Step 3 (Continued) If the child is still apneic after positioning their upper airway in Step 2 and they have no palpable pulses, tag as EXPECTANT/ DECEASED
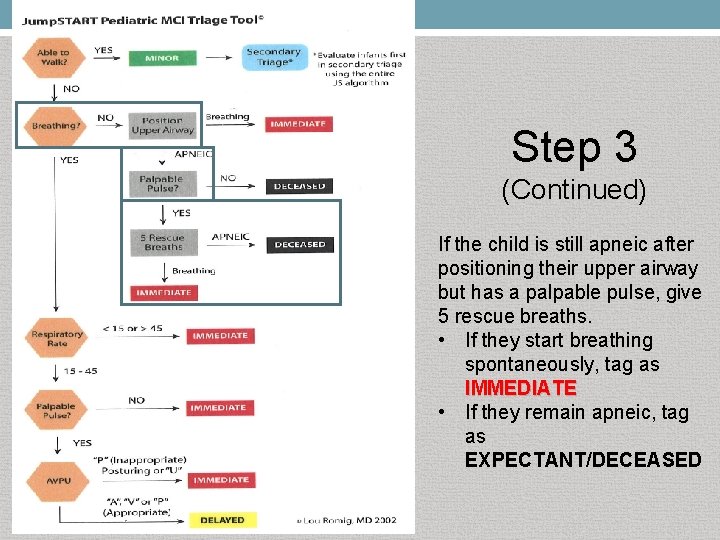
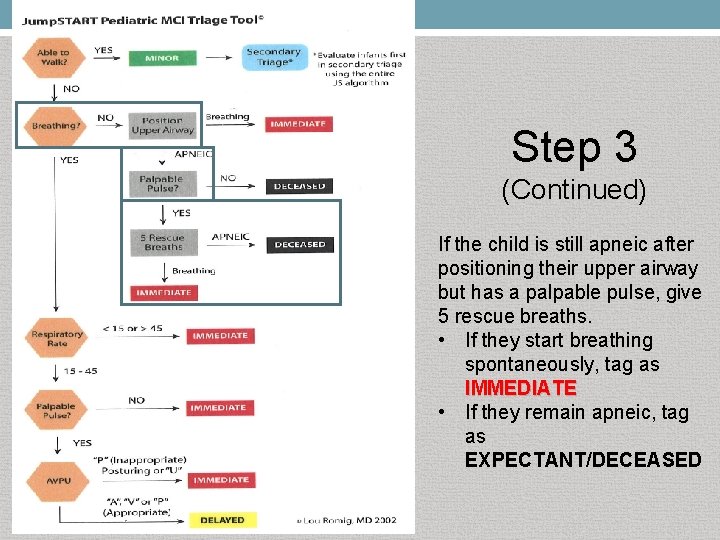
Step 3 (Continued) If the child is still apneic after positioning their upper airway but has a palpable pulse, give 5 rescue breaths. • If they start breathing spontaneously, tag as IMMEDIATE • If they remain apneic, tag as EXPECTANT/DECEASED
FOR THOSE CHILDREN WHO REMAIN APNEIC AFTER 5 RESCUE BREATHS, DO NOT CONTINUE TO VENTILATE THE PATIENT RESUME TRIAGE DUTIES.
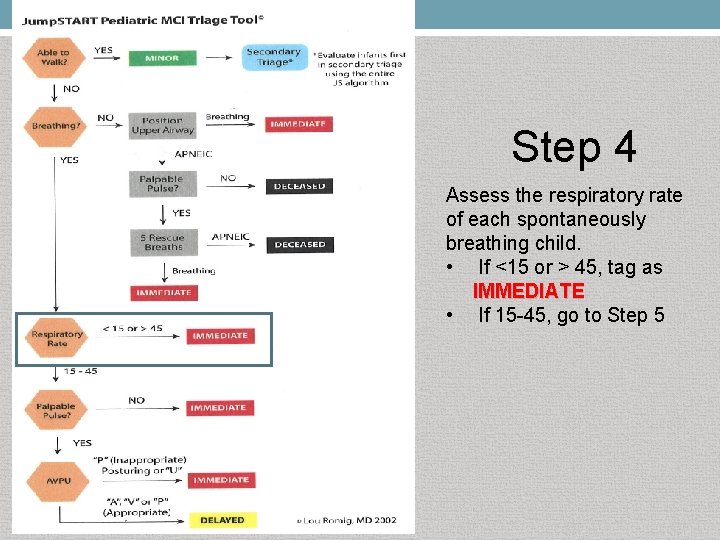
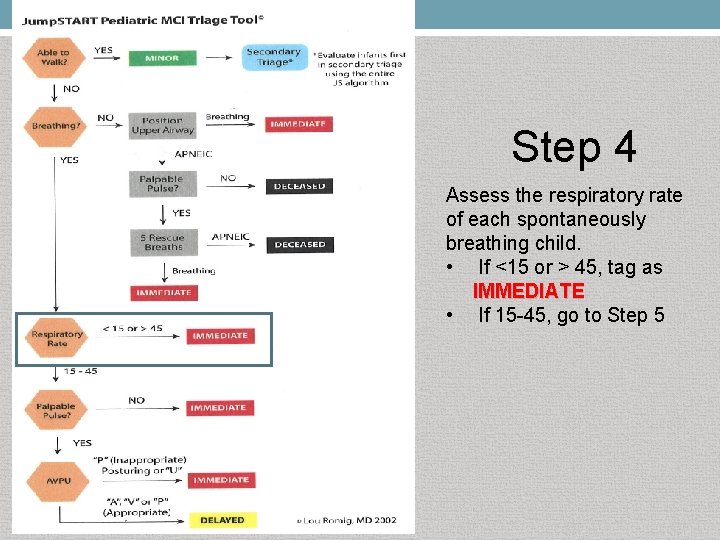
Step 4 Assess the respiratory rate of each spontaneously breathing child. • If <15 or > 45, tag as IMMEDIATE • If 15 -45, go to Step 5
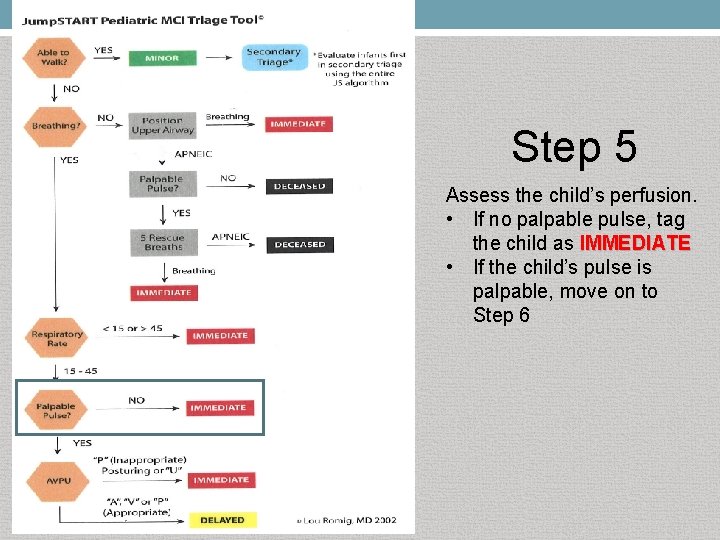
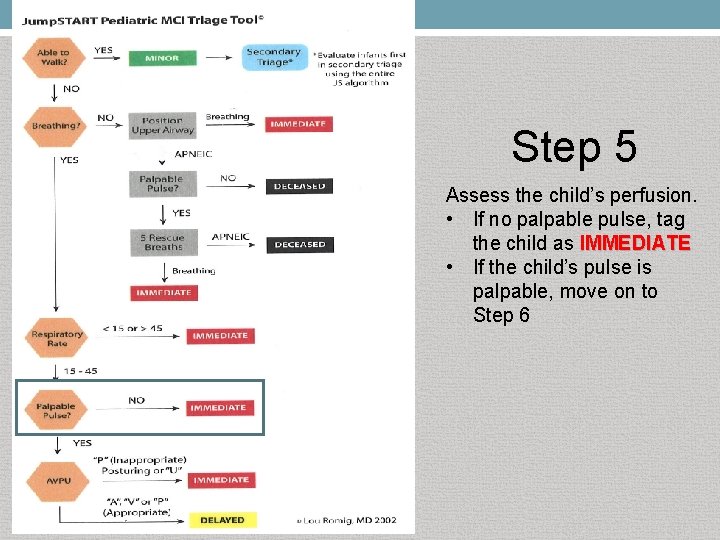
Step 5 Assess the child’s perfusion. • If no palpable pulse, tag the child as IMMEDIATE • If the child’s pulse is palpable, move on to Step 6
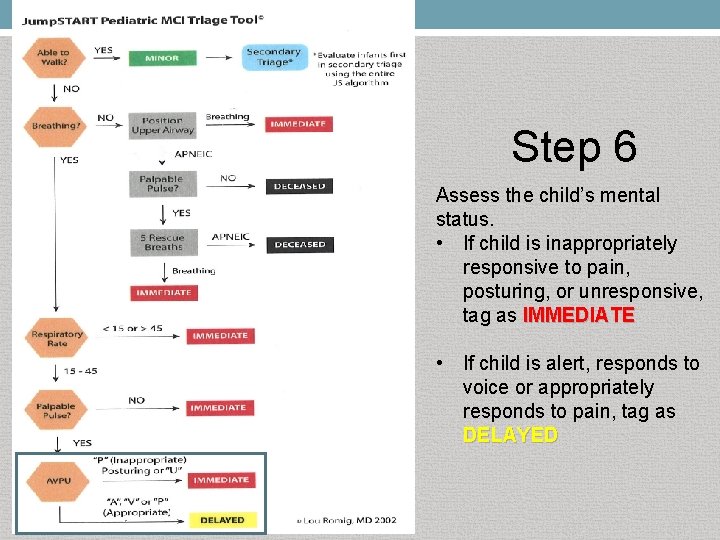
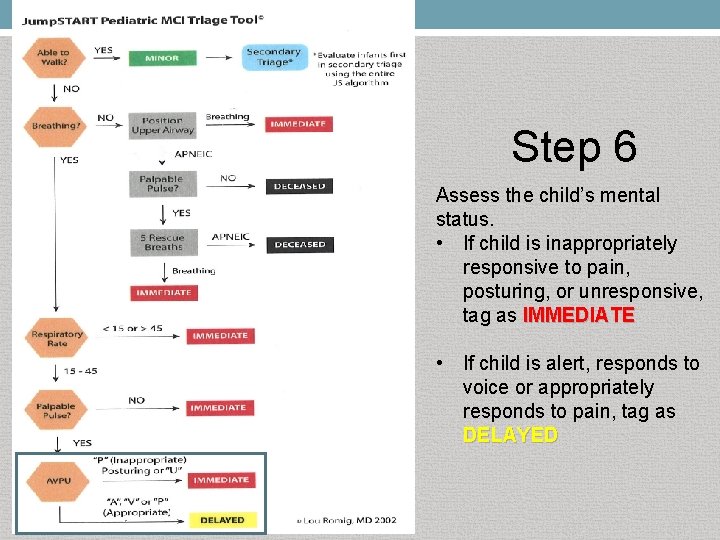
Step 6 Assess the child’s mental status. • If child is inappropriately responsive to pain, posturing, or unresponsive, tag as IMMEDIATE • If child is alert, responds to voice or appropriately responds to pain, tag as DELAYED
SMART TRIAGE TAG SYSTEM
State Mass Casualty Triage System • 2004 - State committee identified need for consistency in MCI triaging throughout Illinois � Various MCI triage systems reviewed � Endorsement of SMART Incident Command System™ for use in Illinois • 2007 -Statewide distribution of SMART Triage Pacs™ • Illinois Custom-Designed SMART Pacs™ � Contains a START and Jump. START© algorithm card � Does not have the SMART Pediatric Tape (tape not approved for use in Illinois)
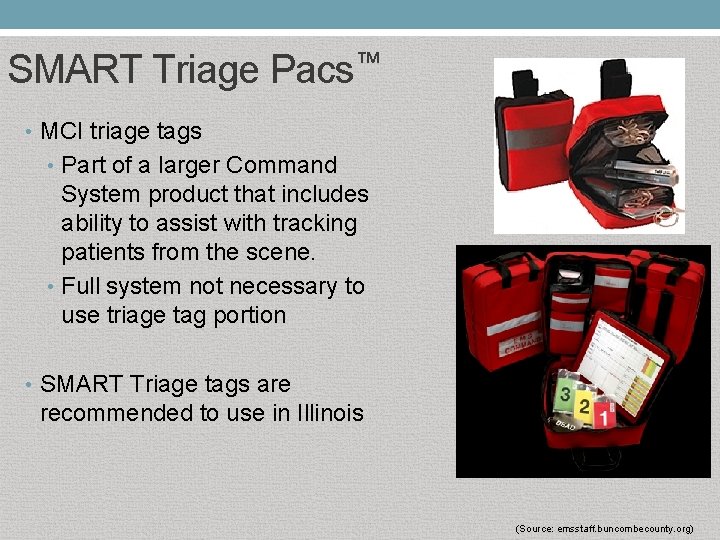
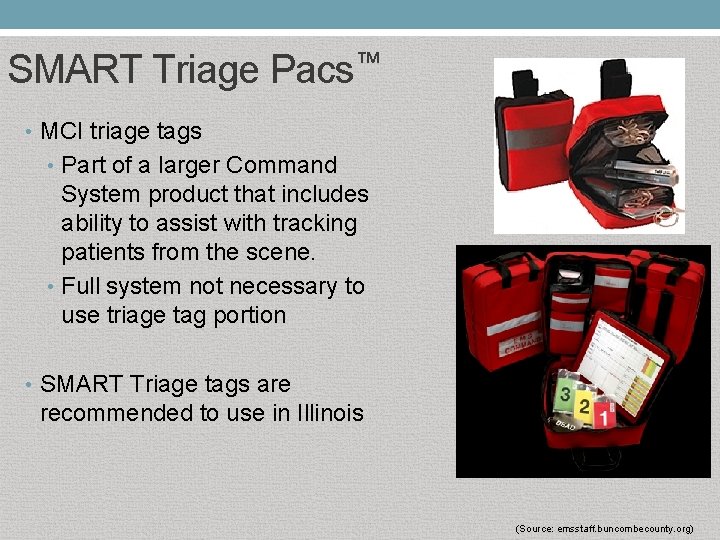
SMART Triage Pacs™ • MCI triage tags • Part of a larger Command System product that includes ability to assist with tracking patients from the scene. • Full system not necessary to use triage tag portion • SMART Triage tags are recommended to use in Illinois (Source: emsstaff. buncombecounty. org)

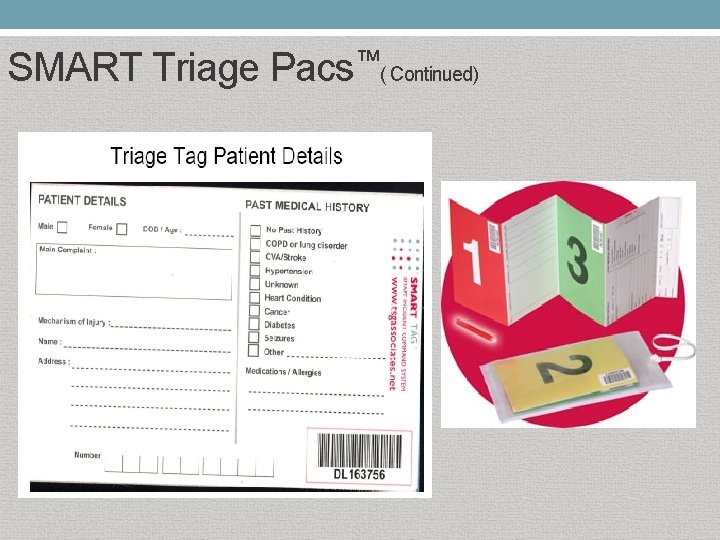
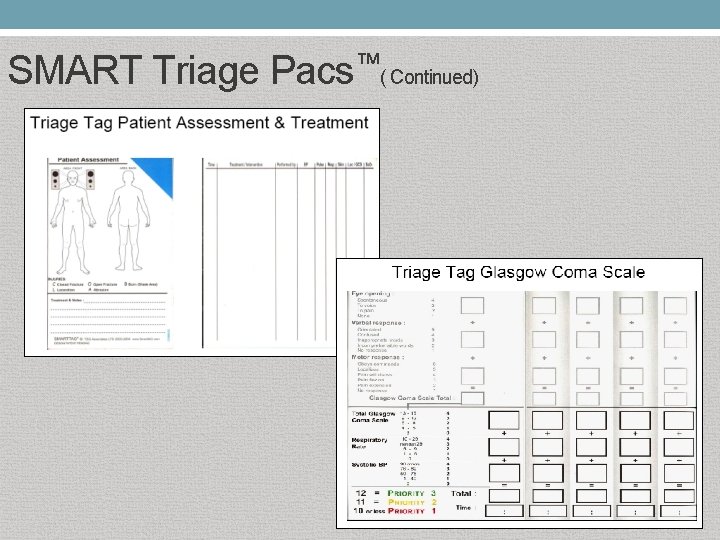
SMART Triage Pacs™ • Triage tags • Equipment used to perform START and Jump. START© triage • Have standard barcodes for tracking patients • Card folds to the assigned color and only shows one color at a time • Allows patients to be re-triaged to another color classification without having to replace the tag and reassessment can be documented on the same tag • Separate tags for Expectant/Deceased category (Source: emsstaff. buncombecounty. org)
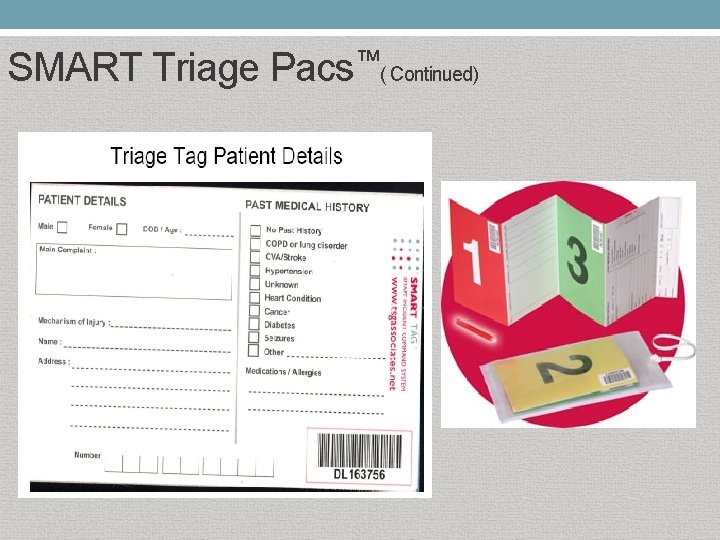
SMART Triage Pacs™( Continued)
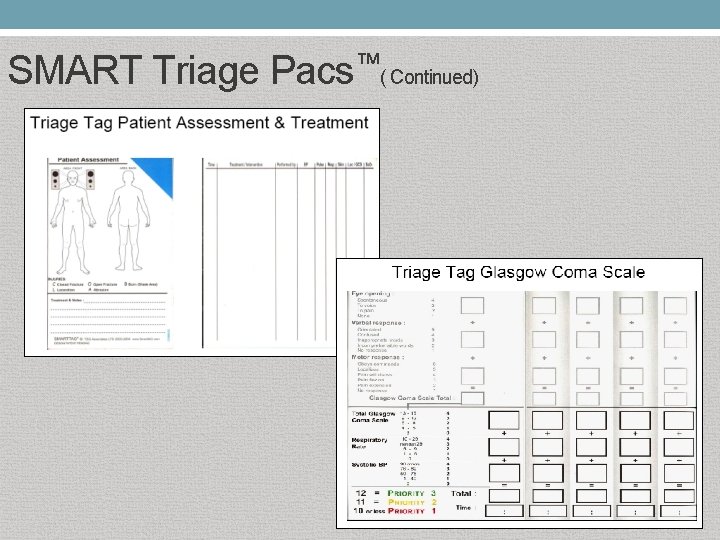
SMART Triage Pacs™( Continued)
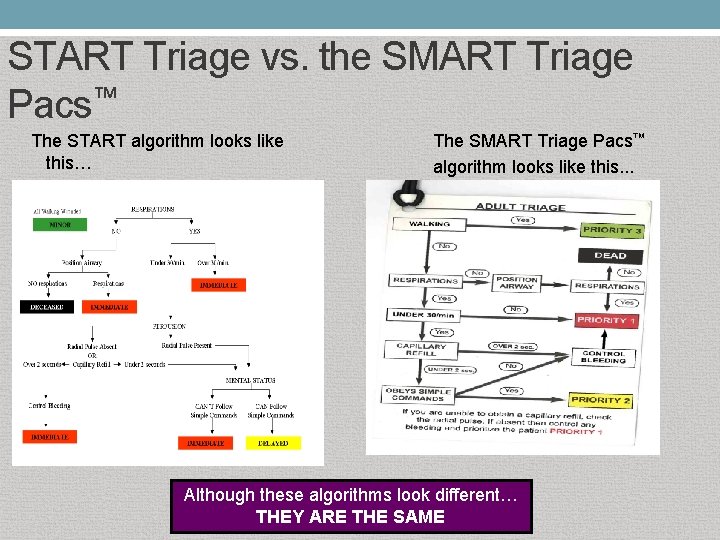
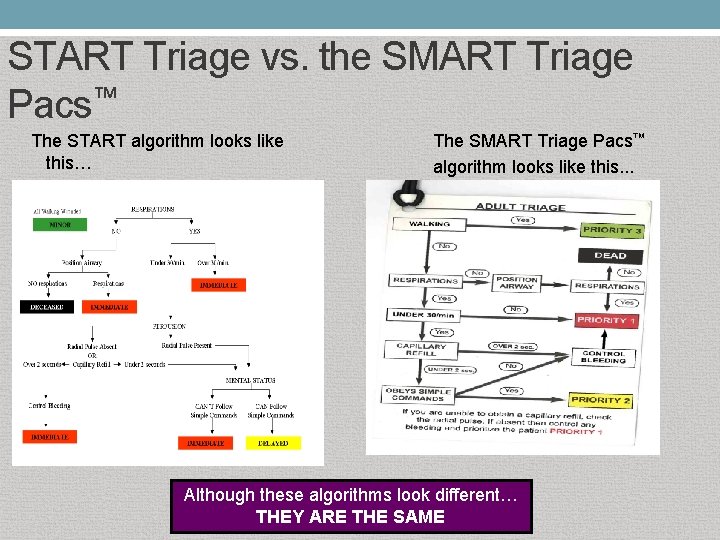
START Triage vs. the SMART Triage Pacs™ The START algorithm looks like this… The SMART Triage Pacs™ algorithm looks like this. . . Although these algorithms look different… THEY ARE THE SAME
Scenarios
Scenario 1: Bus Crash It’s 7 pm on a summer night when a bus returning from a day camp collides with a train on a remote road. You are the first responder and you find 20 + kids. Some are still in the bus and train while some are lying about the road.
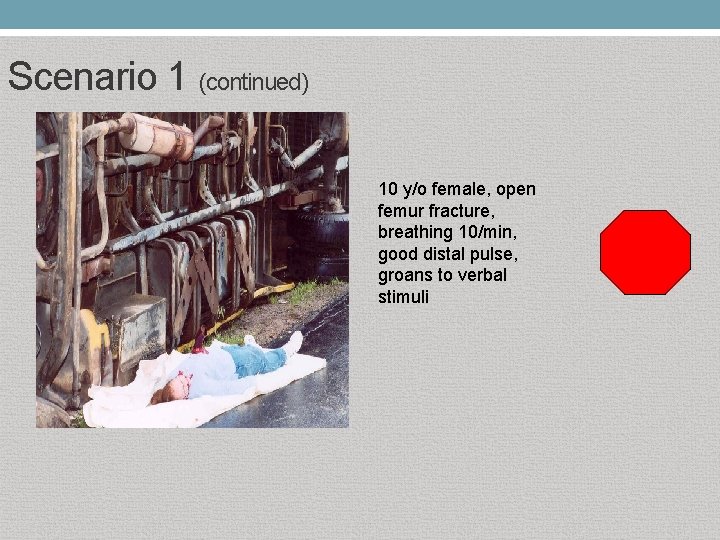
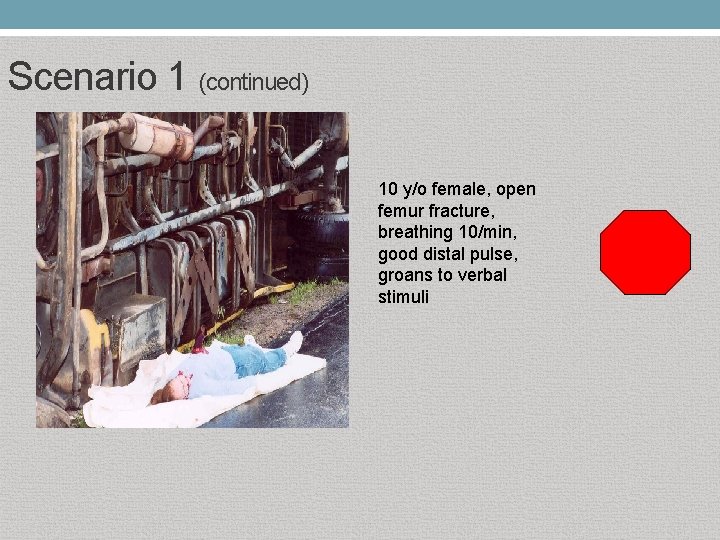
Scenario 1 (continued) 10 y/o female, open femur fracture, breathing 10/min, good distal pulse, groans to verbal stimuli
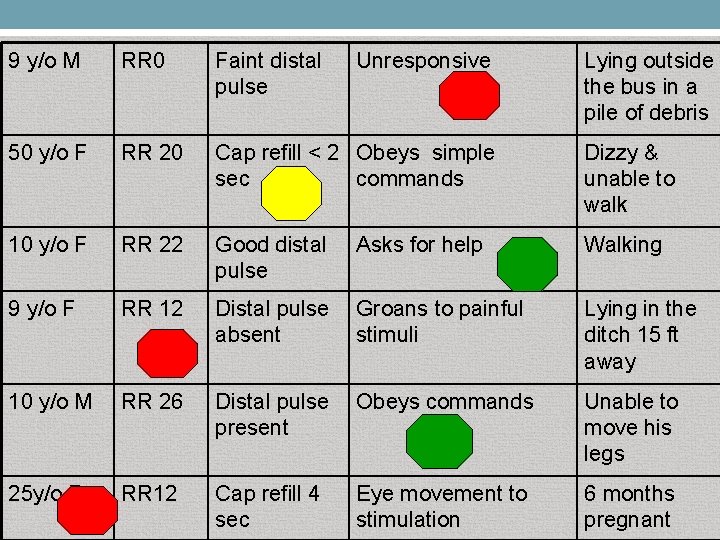
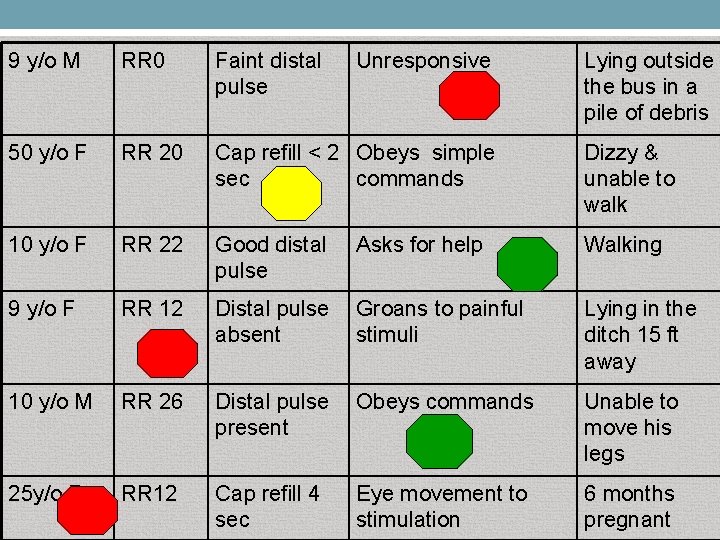
9 y/o M RR 0 Faint distal pulse Unresponsive 50 y/o F RR 20 Cap refill < 2 Obeys simple sec commands Dizzy & unable to walk 10 y/o F RR 22 Good distal pulse Walking 9 y/o F RR 12 Distal pulse Groans to painful absent stimuli Lying in the ditch 15 ft away 10 y/o M RR 26 Distal pulse Obeys commands present Unable to move his legs 25 y/o F RR 12 Cap refill 4 sec 6 months pregnant Asks for help Eye movement to stimulation Lying outside the bus in a pile of debris
Scenario 2: F 5 Tornado An F 5 tornado has struck within your city/town. It occurred at 3 pm while school was letting out. The tornado touched down near 3 schools and a shopping mall.
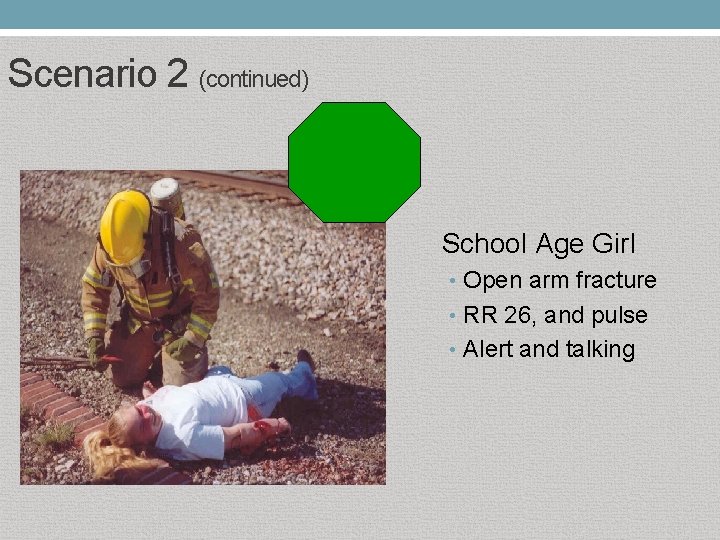
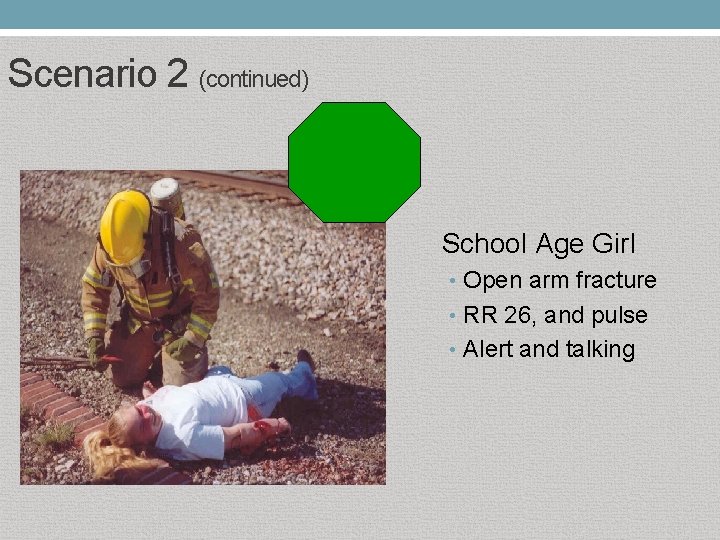
Scenario 2 (continued) School Age Girl • Open arm fracture • RR 26, and pulse • Alert and talking
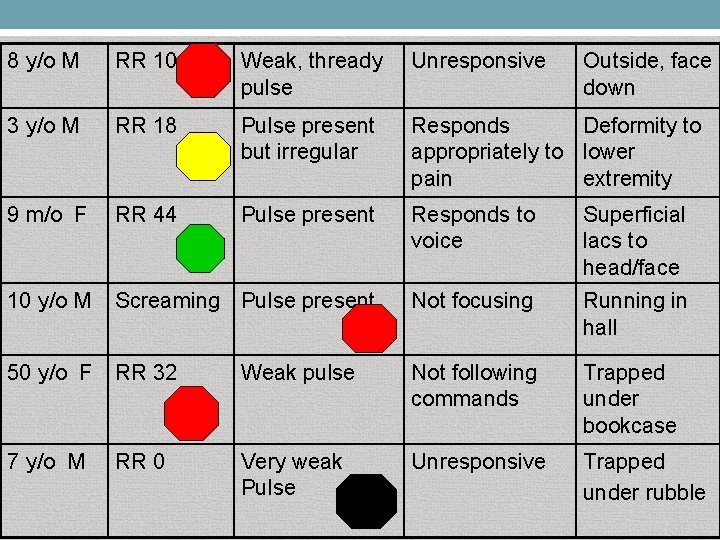
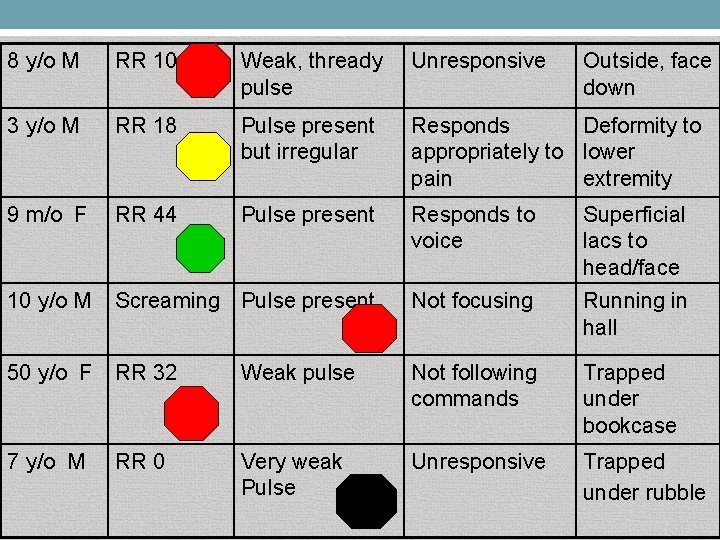
8 y/o M RR 10 Weak, thready pulse Unresponsive Outside, face down 3 y/o M RR 18 Pulse present but irregular Responds Deformity to appropriately to lower pain extremity 9 m/o F RR 44 Pulse present Responds to voice Superficial lacs to head/face 10 y/o M Screaming Pulse present Not focusing Running in hall 50 y/o F RR 32 Weak pulse Not following commands Trapped under bookcase 7 y/o M RR 0 Very weak Pulse Unresponsive Trapped under rubble
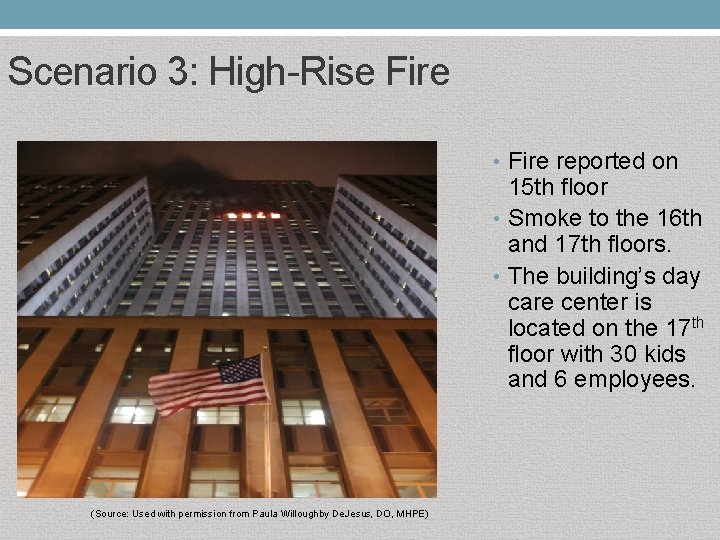
Scenario 3: High-Rise Fire • Fire reported on 15 th floor • Smoke to the 16 th and 17 th floors. • The building’s day care center is located on the 17 th floor with 30 kids and 6 employees. (Source: Used with permission from Paula Willoughby De. Jesus, DO, MHPE)
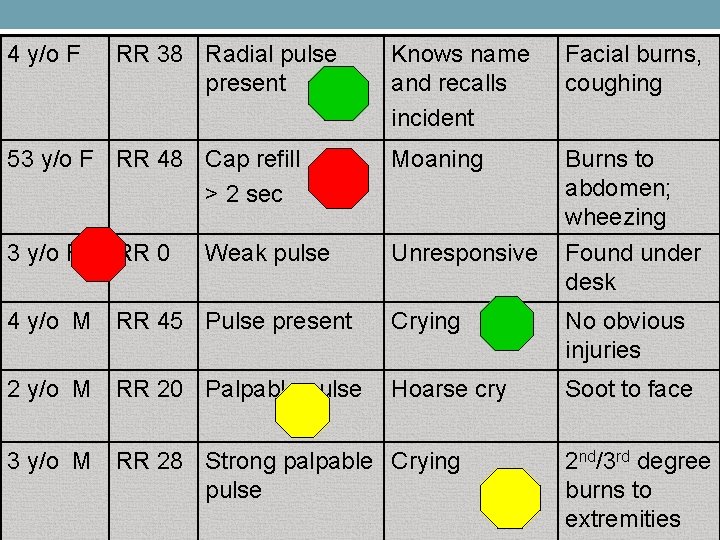
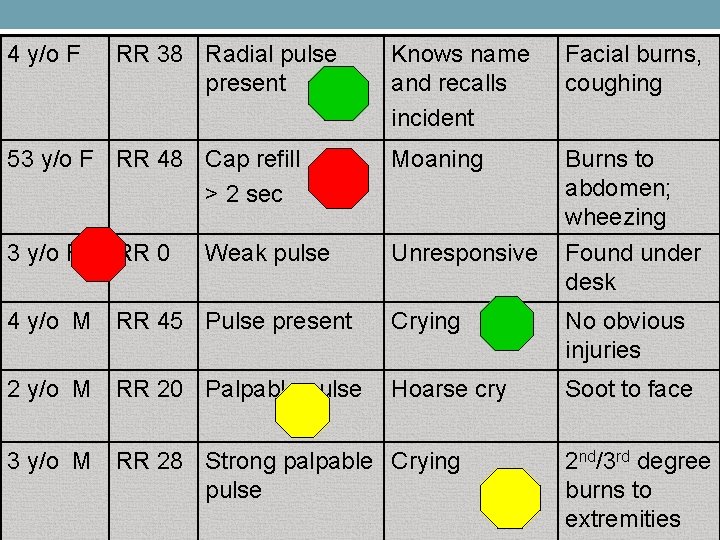
4 y/o F RR 38 Radial pulse present Knows name and recalls incident Facial burns, coughing 53 y/o F RR 48 Cap refill > 2 sec Moaning Burns to abdomen; wheezing 3 y/o F Unresponsive Found under desk 4 y/o M RR 45 Pulse present Crying No obvious injuries 2 y/o M RR 20 Palpable pulse Hoarse cry Soot to face RR 0 Weak pulse 3 y/o M RR 28 Strong palpable Crying pulse 2 nd/3 rd degree burns to extremities
Scenario 3 (continued) 5 kids are carried out, all being given CPR. As lead triage officer, what do you do? , (Source: Used with permission from Paula Willoughby De. Jesus DO, MHPE)
Recovery
Taking Care of Yourself After a critical event, rescue workers often struggle to get back to their daily lives and deal with their experiences • Can have difficulty coping and feeling back to normal • Look for mental health resources/professionals that may be available through your employer/organization or in your community • No one should feel alone in this process or that one has to get through this completely on their own
Conclusion • START/Jump. START are the MCI triage systems used in Illinois • SMART Triage Tags are recommended for use in Illinois • Jump. START incorporates unique aspects of pediatric physiology • Provide an objective framework to assist responders with making difficult life or death decisions during a disaster • Helps provide emotional support when responders know they followed the protocols
APPLYING START AND © JUMPSTART
Instructor Training
Trainer’s Role • Be an advocate for pediatric preparedness at your organization and within your region • Work within your EMS region to provide trainings • Conduct Jump. START© Provider courses • Conduct Jump. START© Train the Trainer Instructor courses
Jump. START© Pediatric Mass Casualty Triage Course Guidelines Course Participant Guidelines • Provider Course • Participants should ideally be healthcare professionals (i. e. physicians, registered nurses, EMTs, respiratory therapists) or other allied health personnel. • • Train-the-Trainer Course • Participants must be licensed healthcare professionals (i. e. physicians, registered nurses, EMTs, respiratory therapists) with current educator experience/background.
Jump. START© Pediatric Mass Casualty Triage Course Guidelines (continued) Course Instructor Guidelines • To teach a Provider Course • Instructors must: • Successfully complete a Jump. START© Train-the-Trainer course • Utilize current training materials available on the Illinois EMSC website • Submit a copy of the Training Completion form and Student Tracking Form (course roster) to the Illinois EMSC office after each course completion
Jump. START© Pediatric Mass Casualty Triage Course Guidelines (continued) Course Instructor Guidelines • To teach a Train-the-Trainer Course • Instructors must: • Successfully complete a Jump. START© Train-the-Trainer course • Have current role/responsibilities that includes providing adult healthcare related education • Have current background and experience in emergency medicine/disaster preparedness • Utilize current training materials available on the Illinois EMSC website • Submit a copy of the Training Completion form and Student Tracking Form (course roster) to the Illinois EMSC office after each course completion
Jump. START© Pediatric Mass Casualty Triage Course Guidelines (continued) Course Instructor Guidelines • Course Coordinators • Course coordinators are responsible for ensuring the overall coordination of the Jump. START© course by handling various responsibilities including but not limited to: • Securing the course location • Scheduling instructor • Obtaining course supplies/needs • Utilizing current training materials • Adhering to the course agenda • Completing appropriate documentation.
Who Needs Training in your Region? • Hospital Staff • EMS personnel • Fire department personnel • School nurses and school health personnel • Local clinics personnel • Local public health department personnel • Physician offices/groups
Course Overview • • 3 hours in length Composed of lecture, skills demonstration, question & answer session, and evaluation Course certificate upon completion CE hours EMS CE’s can be obtained through an IDPH code • Nursing CE’s • Apply as a region or an organization • Can be applied toward: • • EDAP, SEDP or PCCC Facility Recognition requirements ECRN TNS
Steps to Conduct a Class • Identify course coordinator • Identify target audience • Determine class size • Secure rooms at the location • Will need a lecture room and a skills station room • Promote the training • Develop a brochure • Template brochure available thru EMSC • Distribute brochure via email and/or mail
Steps to Conduct a Class (continued) • • • Coordinate course registrations Confirm course registration/details with participants Secure other instructors • • Typical instructor/student ratio is 1/6 for the skills demonstration component Gather necessary supplies and materials Conduct the class After course completion, forward Student Tracking Form (roster) and Training Completion Form to EMSC office
Course Content • Lecture • • Skills Demonstration Component • • Scenarios provided to trainers in the Disaster Preparedness Exercises Addressing the Pediatric Population document Question & Answer Component • • Power. Point Presentation provided in the course materials Post test provided to trainers Evaluation • Evaluation forms provided in the course materials
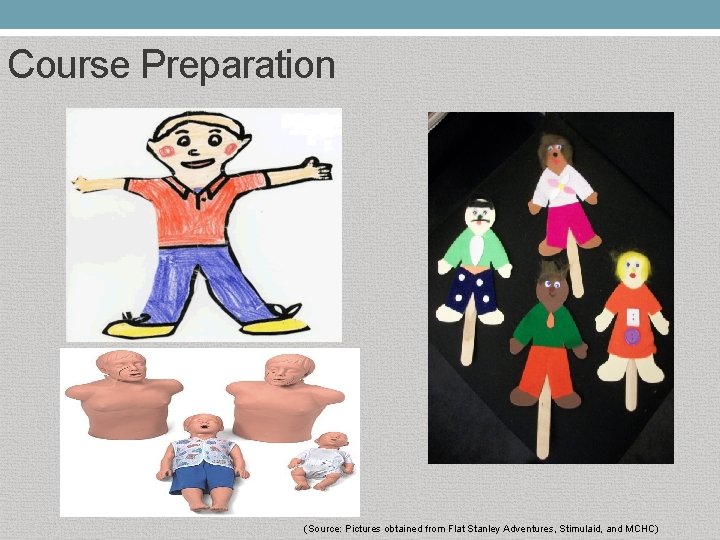
Course Preparation • • • Power point presentation with appropriate AV equipment Flat Stanleys, manikins, or other types of “victims” to use for skills demonstrations All forms: • • Student Tracking Form or other sign in sheet Certificate of Completion Evaluation Form Patient Tracking Form Post test Scenarios: Pediatric Disaster Triage Training Scenarios: Utilizing the Jump. START Method © START/Jump. START algorithm cards Consider if food/beverages will be provided
Course Preparation (Source: Pictures obtained from Flat Stanley Adventures, Stimulaid, and MCHC)
Course Preparation For Information Purposes Only BLUE Category in MCI Triage BLUE • Not universally accepted • Not used in START or Jump. START Triage Tools • Not part of the approved MCI Triage System for use in Illinois
Course Preparation For Information Purposes Only Other MCI Triage Systems • Examples: • Sacco Triage Method (STM) • http: //saccotriage. com/ • SALT MCI Triage Algorithm • http: //register. ndlsf. org/mod/page/view. php? id=2056 • Not universally accepted • Not part of the approved MCI Triage System for use in Illinois

Course Materials Jump. START© Algorithm • START Algorithm • Power. Point presentation • Pediatric Disaster Triage Training Scenarios: Utilizing the Jump. START Method •
Course Materials Certificate of Completion-Provider Certificate of Completion-Instructor Evaluation Form
Course Materials Patient Tracking Form Student Tracking Form
Course Materials Training Completion Form
Course Materials • SMART Triage Pac Illinois Order Form • SMART Triage Pac Illinois Order Form – Resupply
Conclusion • Use your available Resources! • EMSC • Can provide the START/Jump. START© algorithm cards • Can provide guidance, ideas, and answer questions • Obtain updated course materials • Connect with additional instructors • www. luhs. org/emsc • 708 -327 -3672 • www. jumpstarttriage. com • Other Jump. START instructors
ANY QUESTIONS?
THANK YOU! www. luhs. org/emsc