Cardiac causes of cardiac arrest Learning outcomes This
- Slides: 28
Cardiac causes of cardiac arrest
Learning outcomes This lecture should enable you to: • describe the different types of ACS • explain how to recognise and assess an ACS • list the relevant immediate treatment for each type of ACS • discuss how to recognise and respond to other cardiac conditions that may cause cardiac arrest
Acute coronary syndromes Clinical syndromes caused by the same disease process: • unstable angina • non-ST-elevation myocardial infarction • ST-elevation myocardial infarction
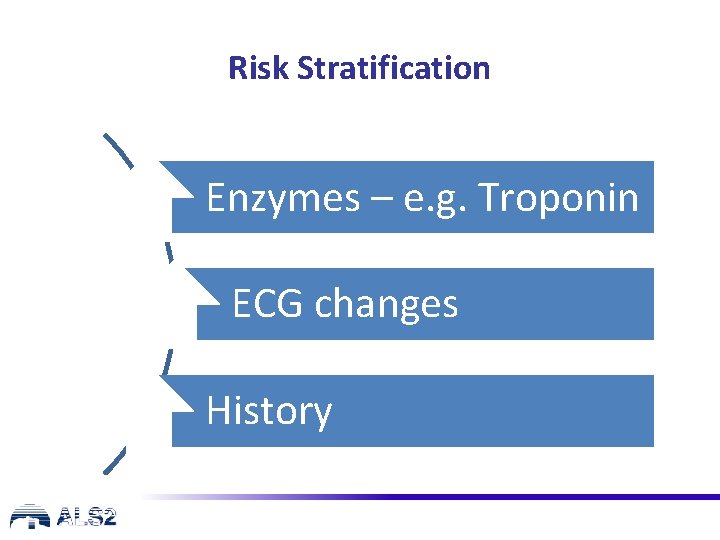
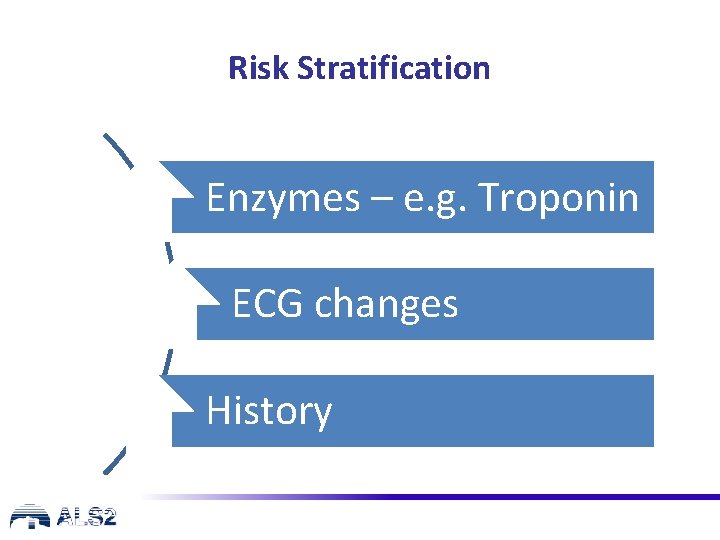
Risk Stratification Enzymes – e. g. Troponin ECG changes History
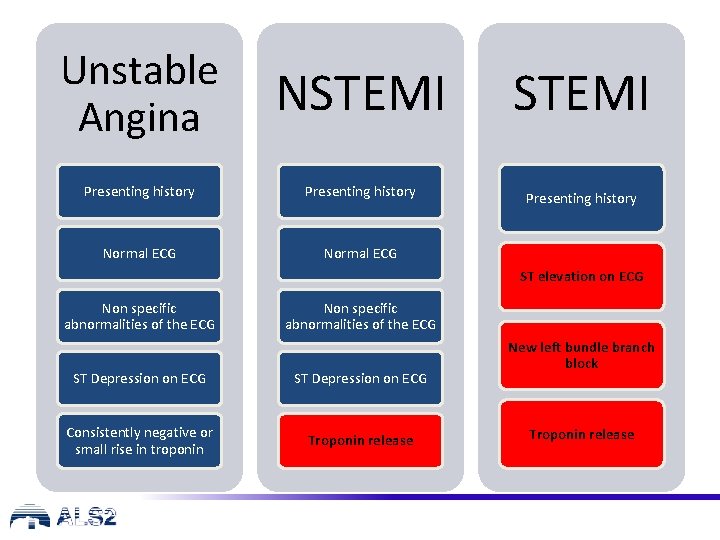
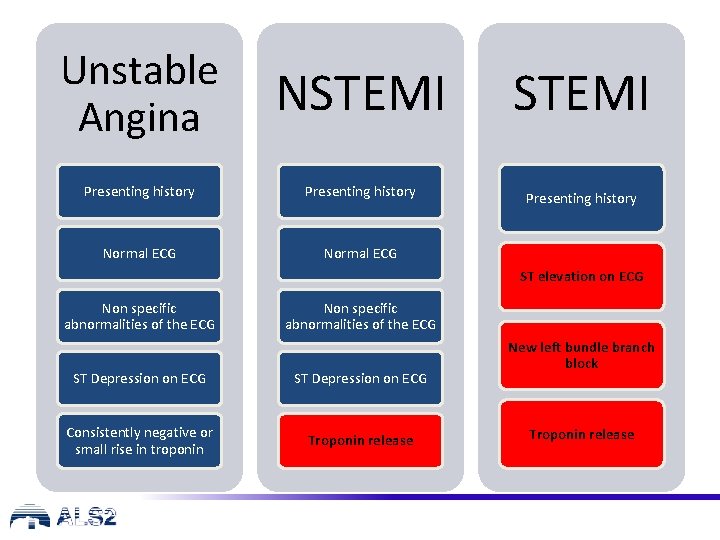
Unstable Angina NSTEMI Presenting history Normal ECG ST elevation on ECG Non specific abnormalities of the ECG ST Depression on ECG Consistently negative or small rise in troponin Troponin release New left bundle branch block Troponin release
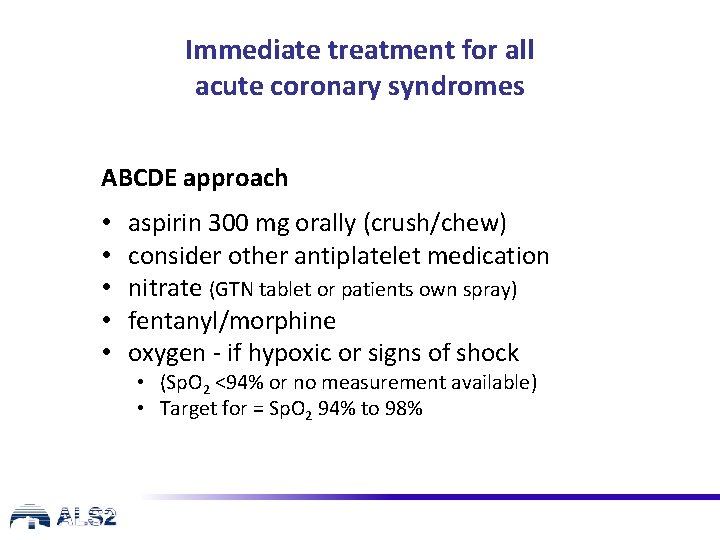
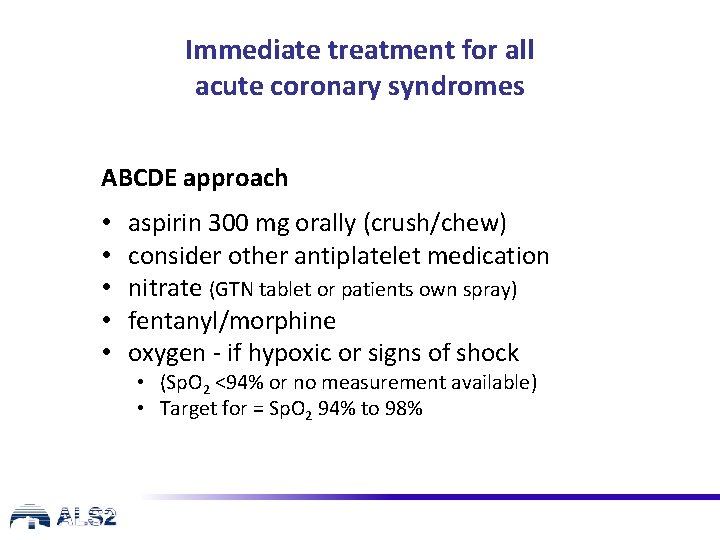
Immediate treatment for all acute coronary syndromes ABCDE approach • • • aspirin 300 mg orally (crush/chew) consider other antiplatelet medication nitrate (GTN tablet or patients own spray) fentanyl/morphine oxygen - if hypoxic or signs of shock • (Sp. O 2 <94% or no measurement available) • Target for = Sp. O 2 94% to 98%
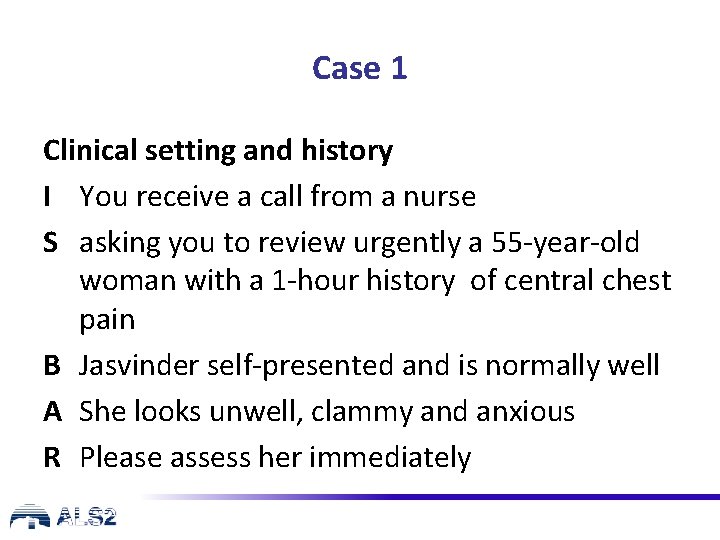
Case 1 Clinical setting and history I You receive a call from a nurse S asking you to review urgently a 55 -year-old woman with a 1 -hour history of central chest pain B Jasvinder self-presented and is normally well A She looks unwell, clammy and anxious R Please assess her immediately
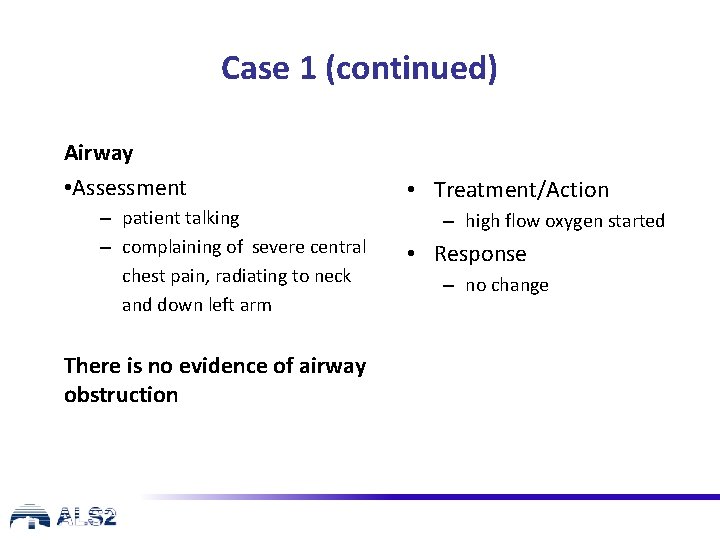
Case 1 (continued) Airway • Assessment – patient talking – complaining of severe central chest pain, radiating to neck and down left arm There is no evidence of airway obstruction • Treatment/Action – high flow oxygen started • Response – no change
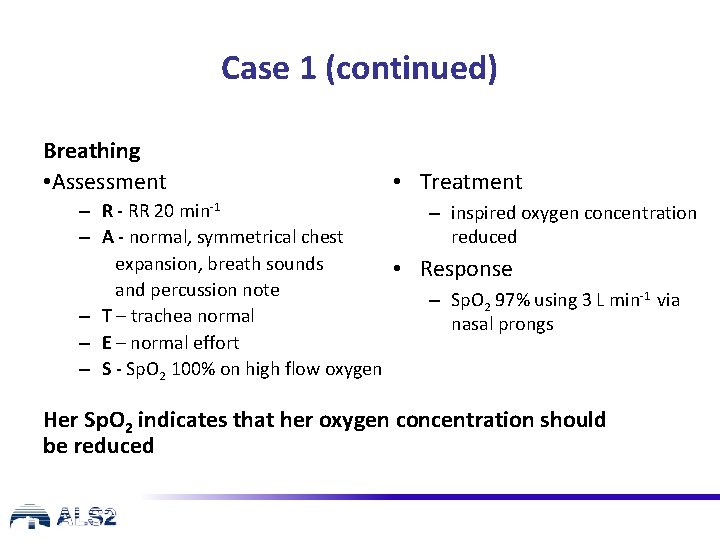
Case 1 (continued) Breathing • Assessment • Treatment – R - RR 20 min-1 – inspired oxygen concentration reduced – A - normal, symmetrical chest expansion, breath sounds • Response and percussion note – Sp. O 2 97% using 3 L min-1 via – T – trachea normal nasal prongs – E – normal effort – S - Sp. O 2 100% on high flow oxygen Her Sp. O 2 indicates that her oxygen concentration should be reduced
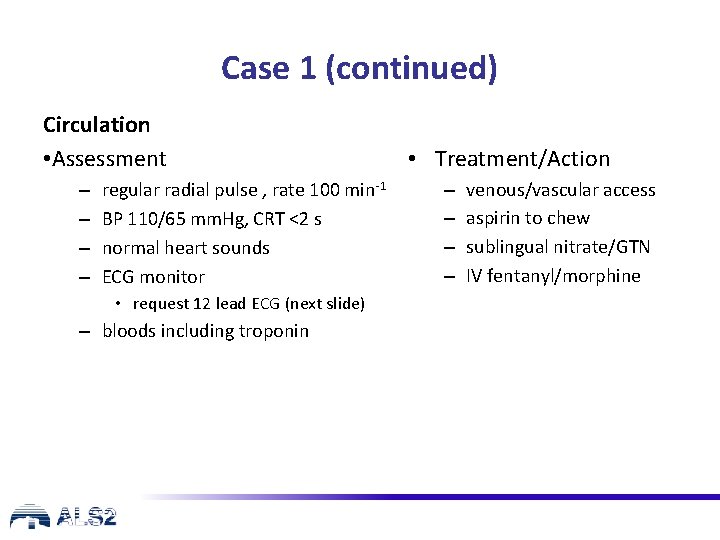
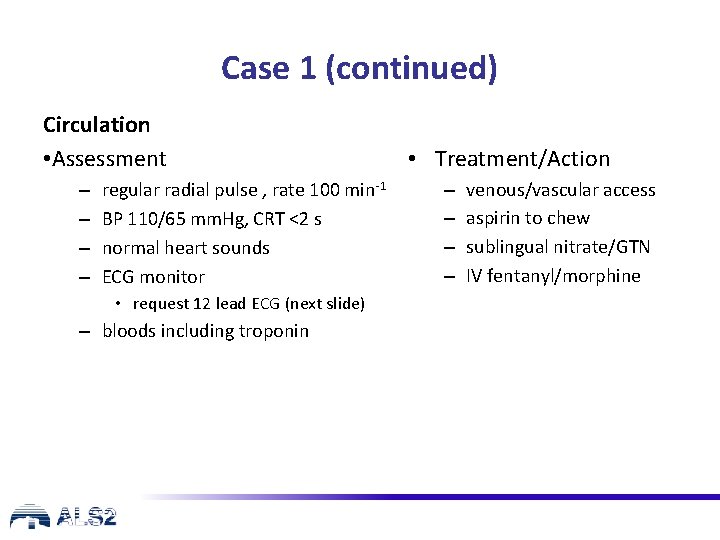
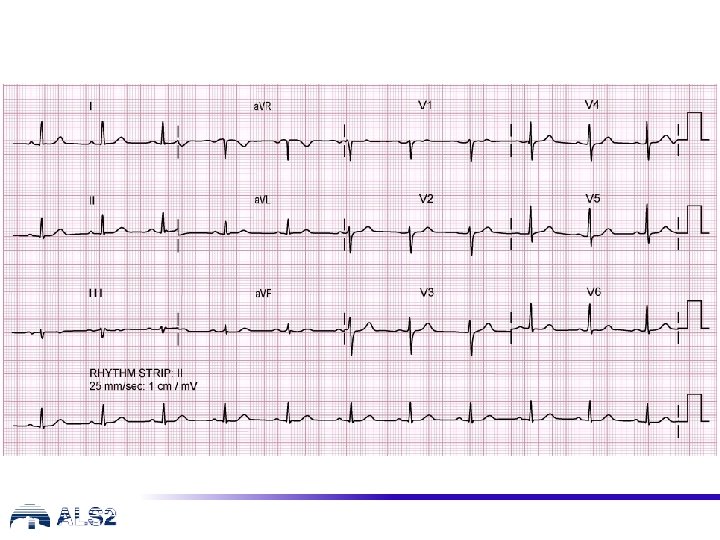
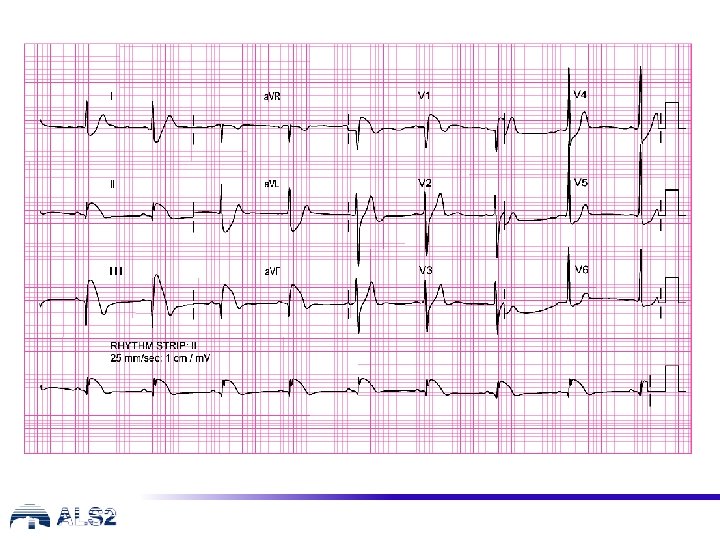
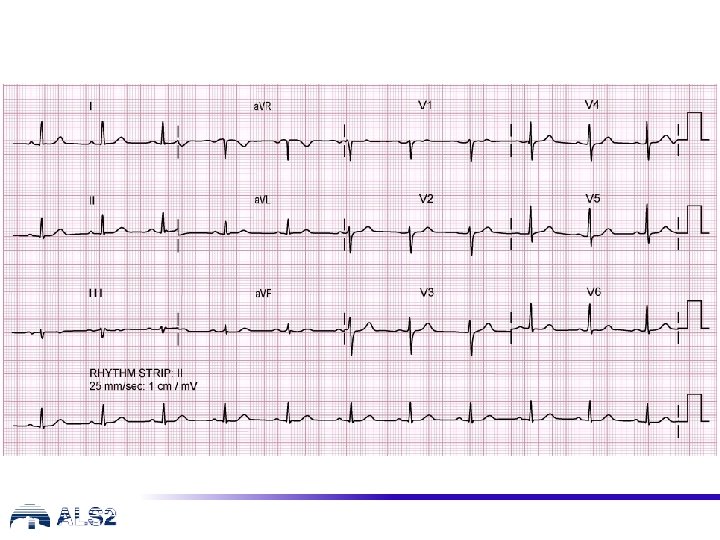
Case 1 (continued) Circulation • Assessment – – regular radial pulse , rate 100 min-1 BP 110/65 mm. Hg, CRT <2 s normal heart sounds ECG monitor • request 12 lead ECG (next slide) – bloods including troponin • Treatment/Action – – venous/vascular access aspirin to chew sublingual nitrate/GTN IV fentanyl/morphine
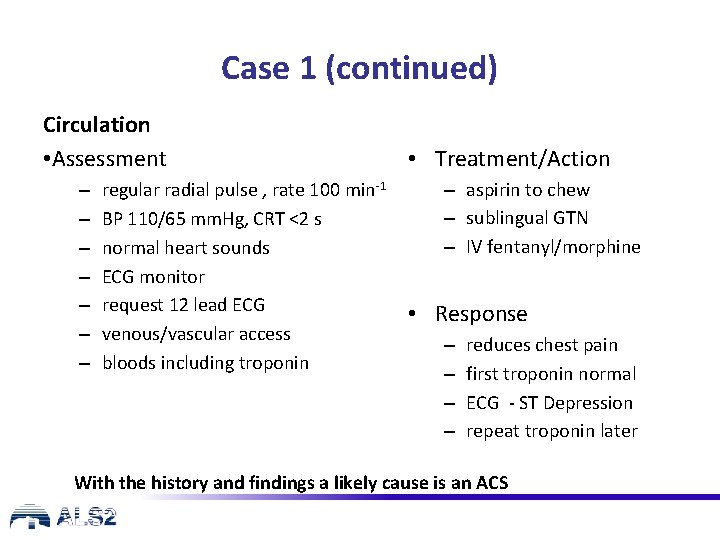
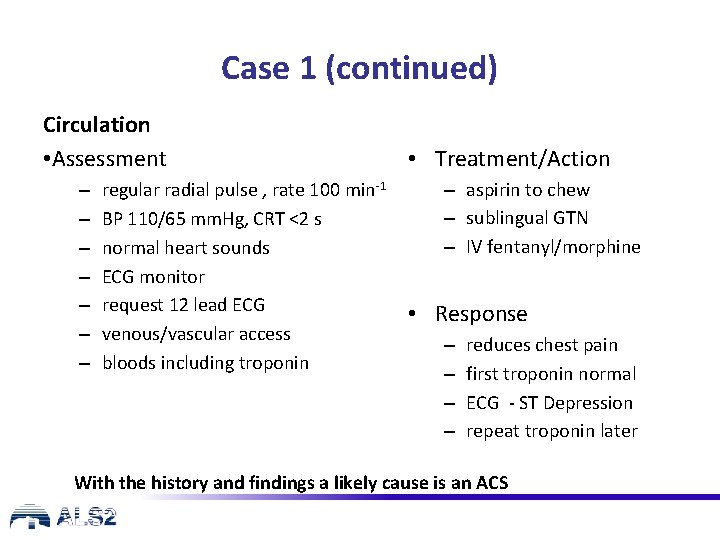
Case 1 (continued) Circulation • Assessment – – – – regular radial pulse , rate 100 min-1 BP 110/65 mm. Hg, CRT <2 s normal heart sounds ECG monitor request 12 lead ECG venous/vascular access bloods including troponin • Treatment/Action – aspirin to chew – sublingual GTN – IV fentanyl/morphine • Response – – reduces chest pain first troponin normal ECG - ST Depression repeat troponin later With the history and findings a likely cause is an ACS
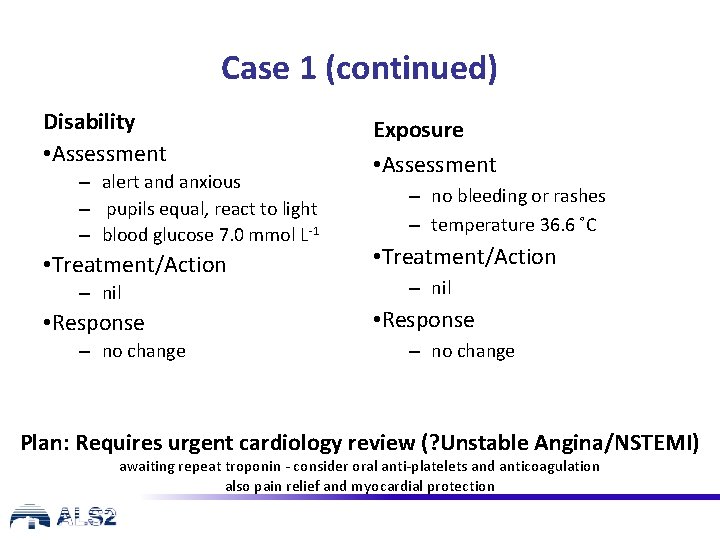
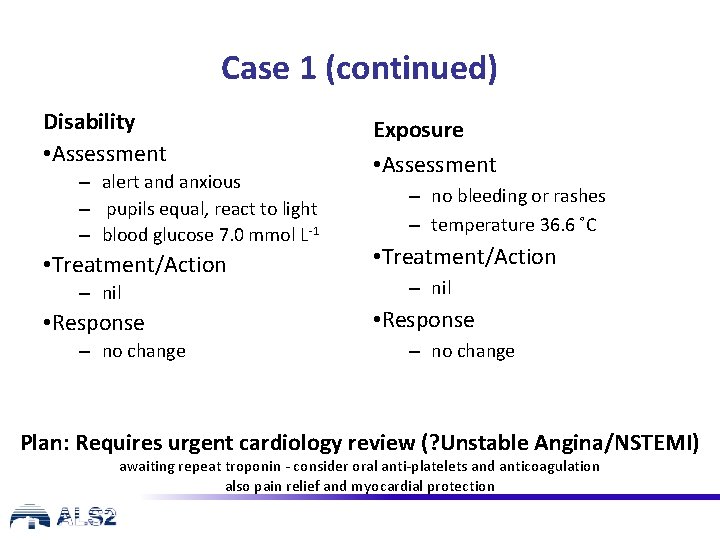
Case 1 (continued) Disability • Assessment – alert and anxious – pupils equal, react to light – blood glucose 7. 0 mmol L-1 • Treatment/Action – nil • Response – no change Exposure • Assessment – no bleeding or rashes – temperature 36. 6 ˚C • Treatment/Action – nil • Response – no change Plan: Requires urgent cardiology review (? Unstable Angina/NSTEMI) awaiting repeat troponin - consider oral anti-platelets and anticoagulation also pain relief and myocardial protection
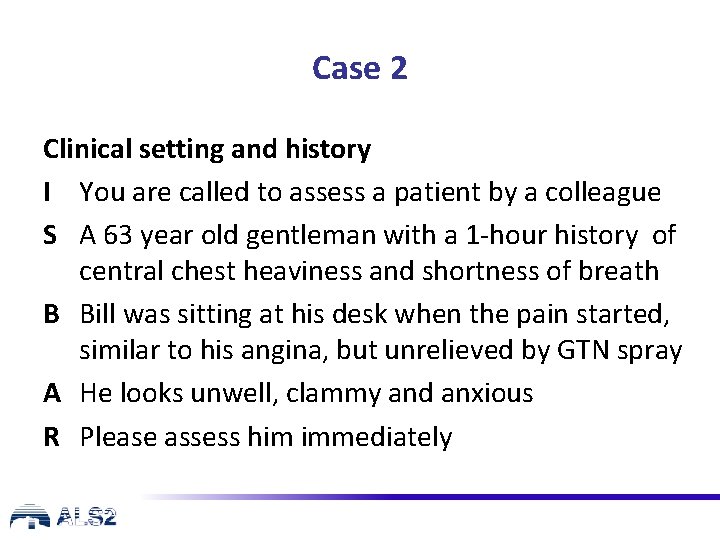
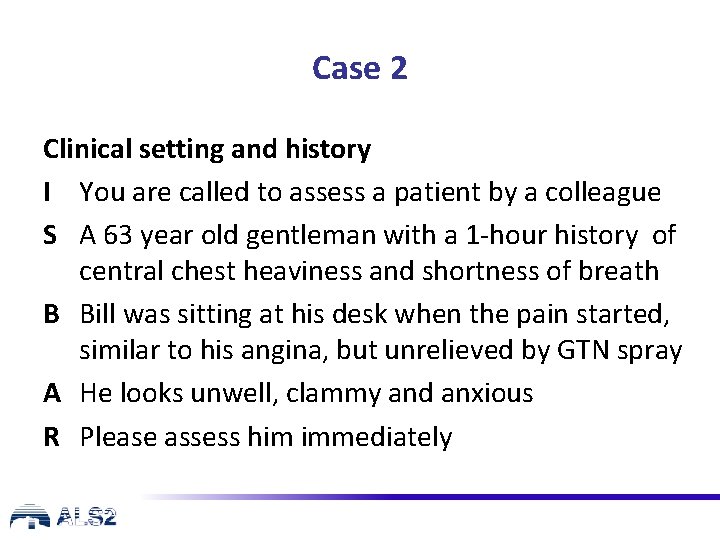
Case 2 Clinical setting and history I You are called to assess a patient by a colleague S A 63 year old gentleman with a 1 -hour history of central chest heaviness and shortness of breath B Bill was sitting at his desk when the pain started, similar to his angina, but unrelieved by GTN spray A He looks unwell, clammy and anxious R Please assess him immediately
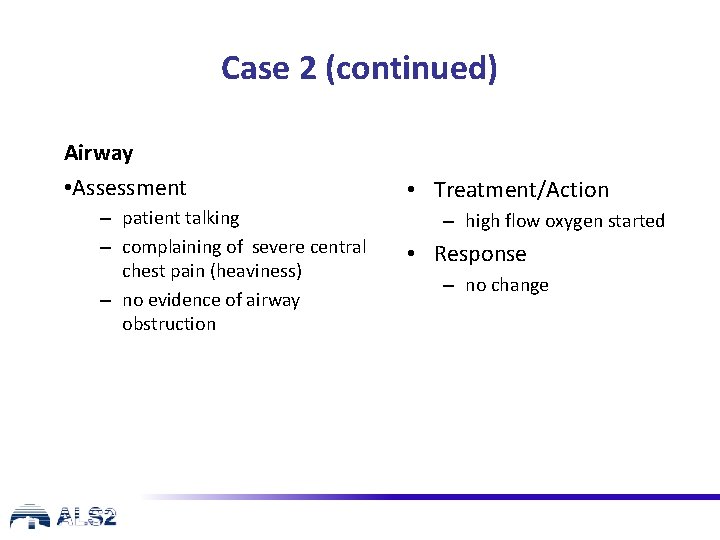
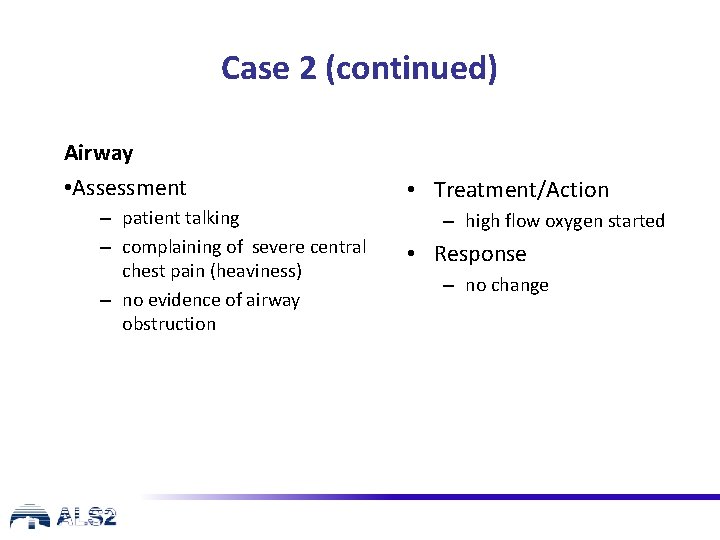
Case 2 (continued) Airway • Assessment – patient talking – complaining of severe central chest pain (heaviness) – no evidence of airway obstruction • Treatment/Action – high flow oxygen started • Response – no change
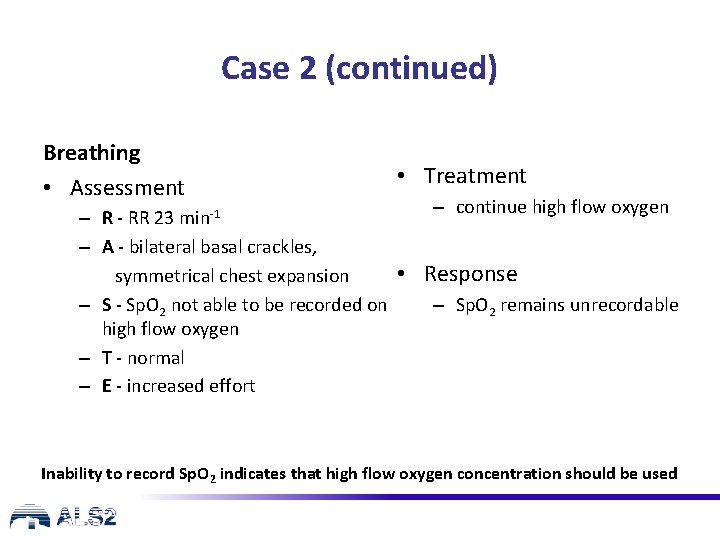
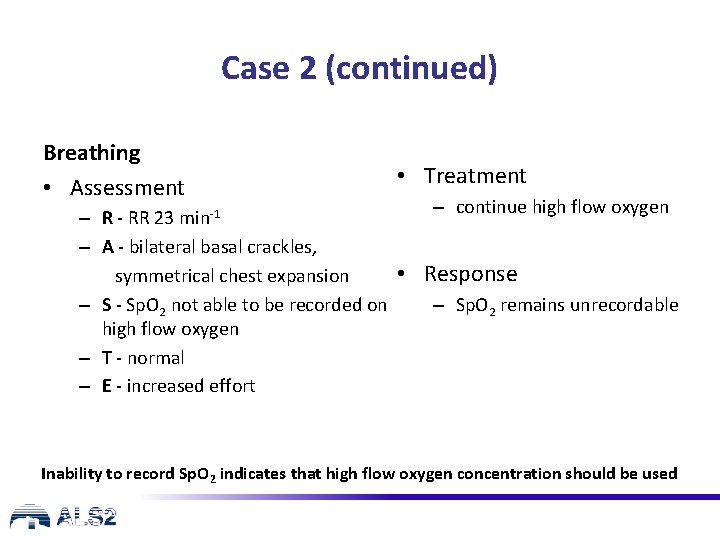
Case 2 (continued) Breathing • Assessment • Treatment – continue high flow oxygen – R - RR 23 min-1 – A - bilateral basal crackles, • Response symmetrical chest expansion – Sp. O 2 remains unrecordable – S - Sp. O 2 not able to be recorded on high flow oxygen – T - normal – E - increased effort Inability to record Sp. O 2 indicates that high flow oxygen concentration should be used
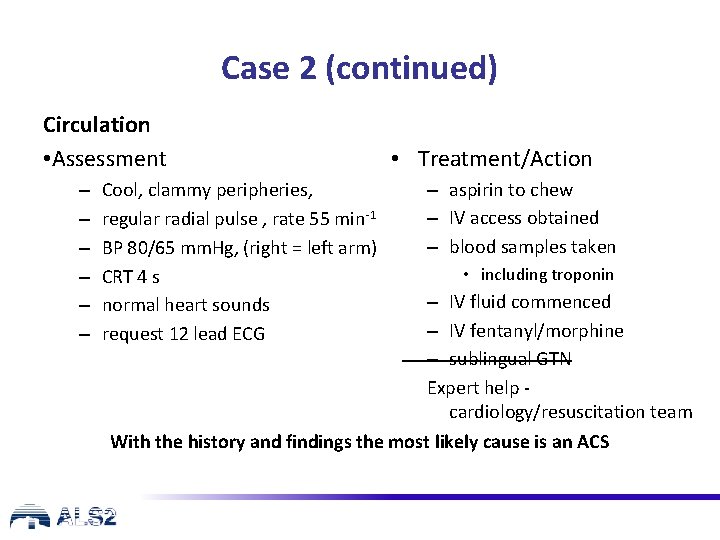
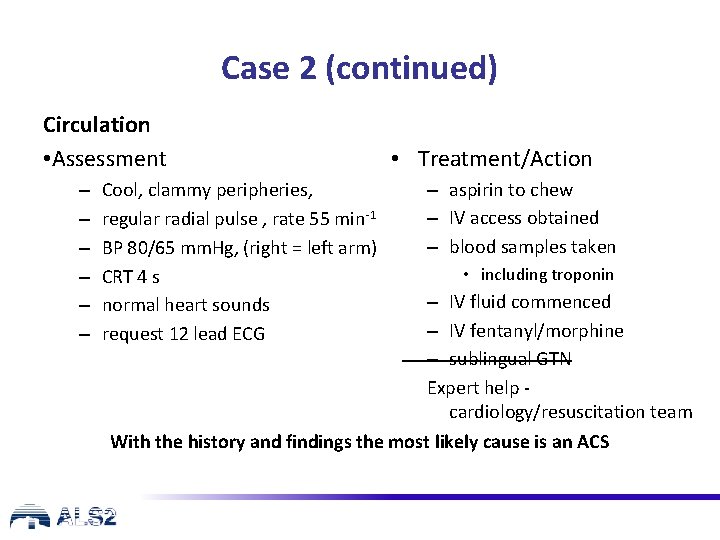
Case 2 (continued) Circulation • Assessment – – – Cool, clammy peripheries, regular radial pulse , rate 55 min-1 BP 80/65 mm. Hg, (right = left arm) CRT 4 s normal heart sounds request 12 lead ECG • Treatment/Action – aspirin to chew – IV access obtained – blood samples taken • including troponin – IV fluid commenced – IV fentanyl/morphine – sublingual GTN Expert help cardiology/resuscitation team With the history and findings the most likely cause is an ACS
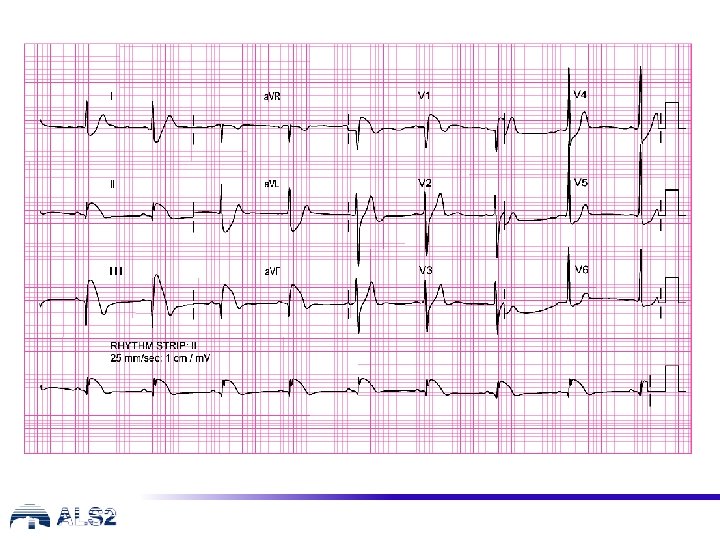
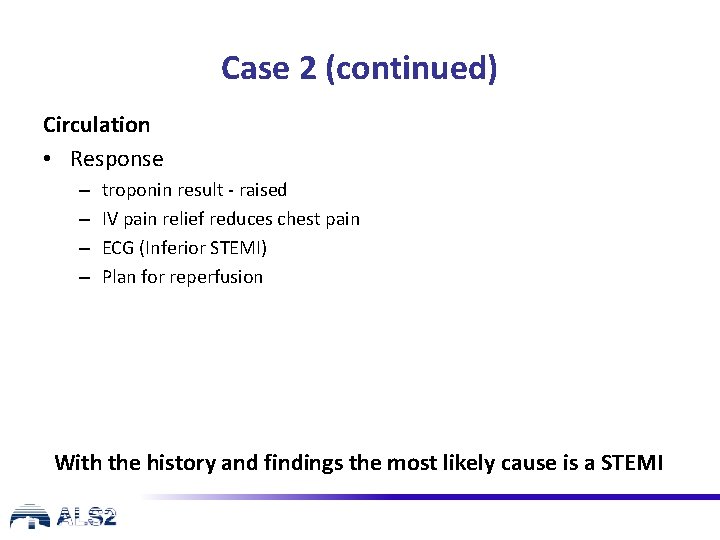
Case 2 (continued) Circulation • Response – – troponin result - raised IV pain relief reduces chest pain ECG (Inferior STEMI) Plan for reperfusion With the history and findings the most likely cause is a STEMI
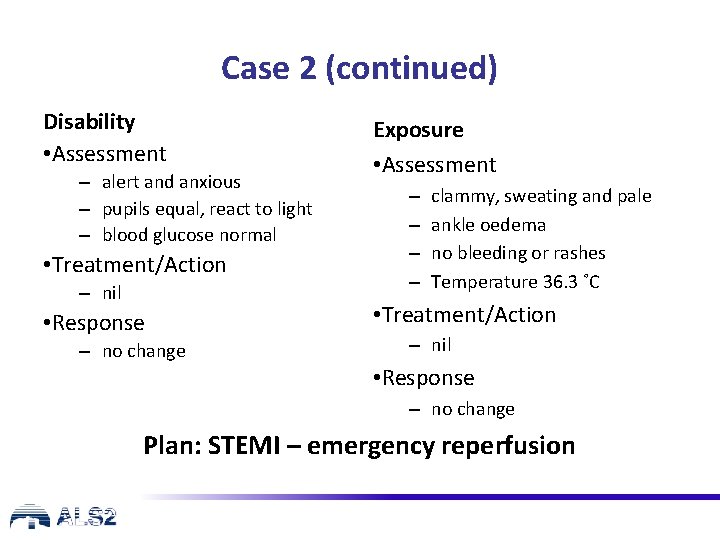
Case 2 (continued) Disability • Assessment – alert and anxious – pupils equal, react to light – blood glucose normal • Treatment/Action – nil • Response – no change Exposure • Assessment – – clammy, sweating and pale ankle oedema no bleeding or rashes Temperature 36. 3 ˚C • Treatment/Action – nil • Response – no change Plan: STEMI – emergency reperfusion
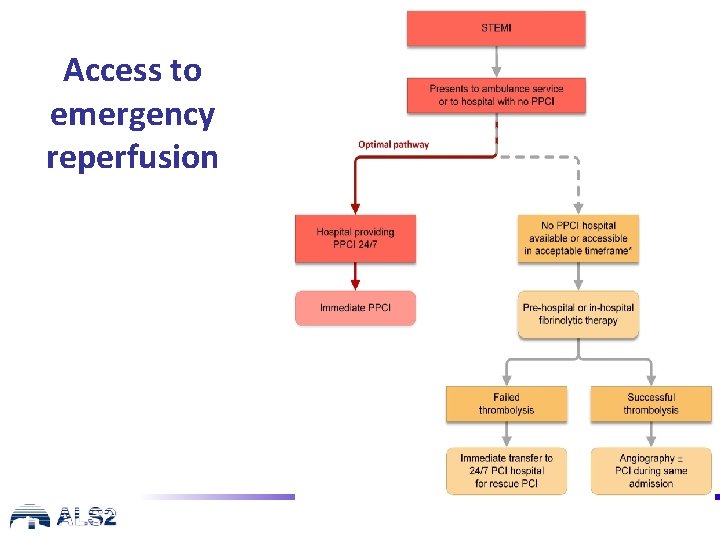
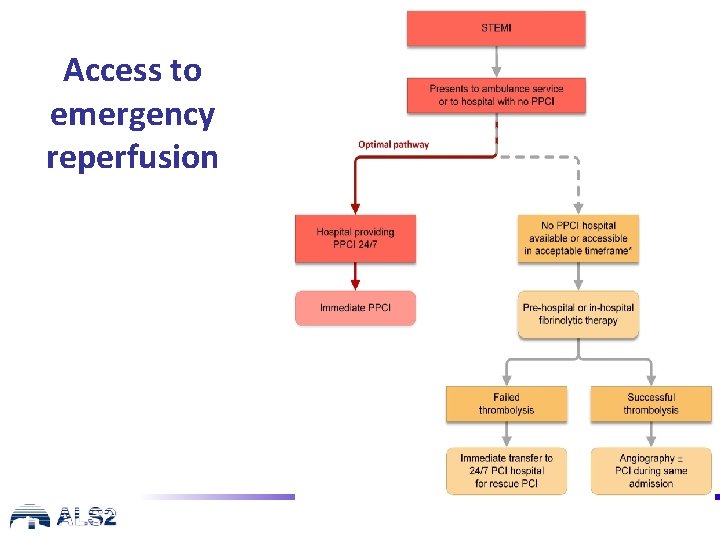
Access to emergency reperfusion
Other cardiac causes of cardiac arrest • in any cardiac arrest look for evidence of the cause • not all cardiac arrests are due to ACS • other causes may be ‘structural’ or ‘electrical’ • some are inherited, some acquired, some congenital
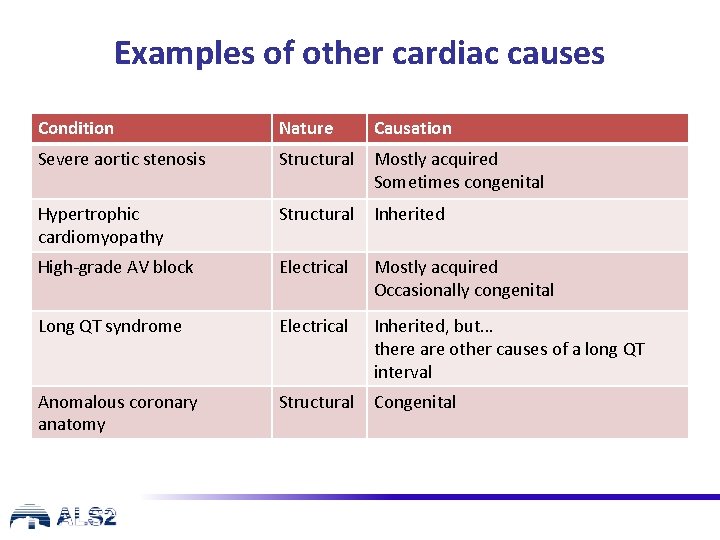
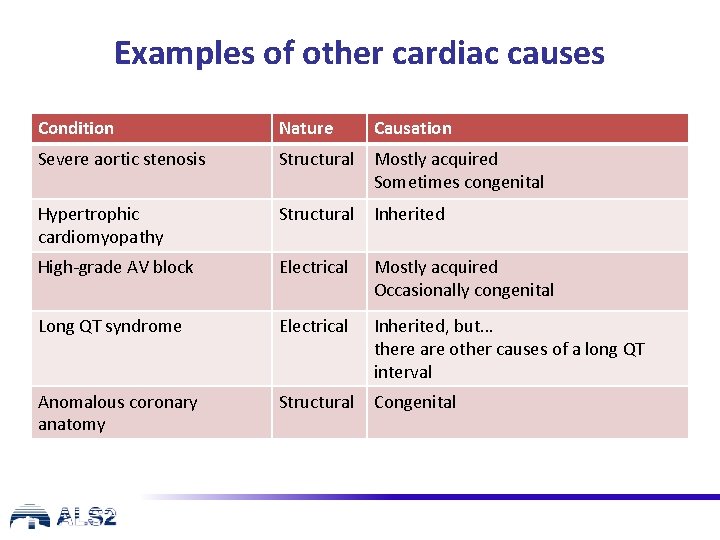
Examples of other cardiac causes Condition Nature Causation Severe aortic stenosis Structural Mostly acquired Sometimes congenital Hypertrophic cardiomyopathy Structural Inherited High-grade AV block Electrical Mostly acquired Occasionally congenital Long QT syndrome Electrical Inherited, but… there are other causes of a long QT interval Anomalous coronary anatomy Structural Congenital
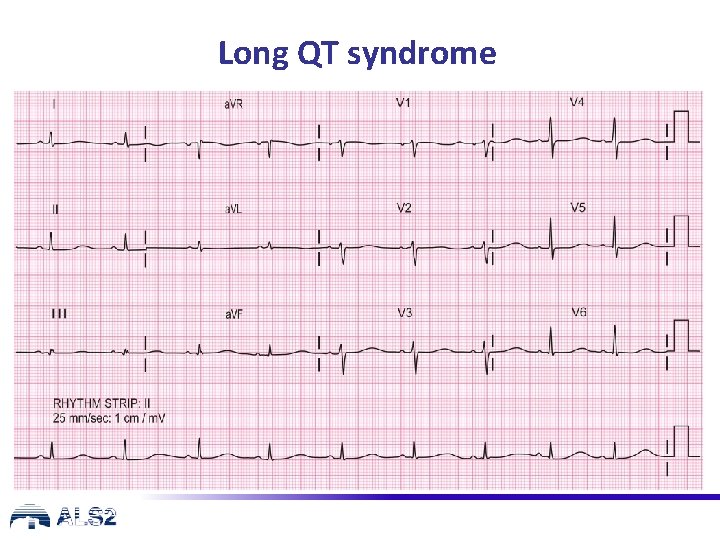
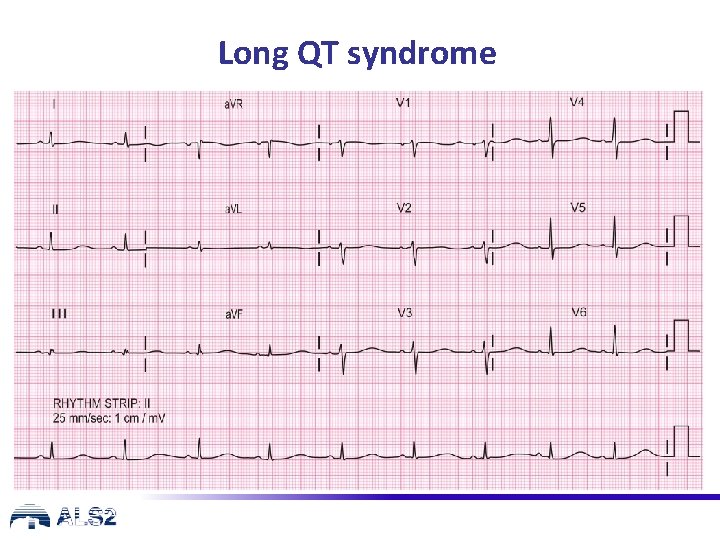
Long QT syndrome
Other cardiac causes: preventing cardiac arrest • be alert for warning symptoms (e. g. unexplained syncope) • arrange urgent specialist assessment and treatment (including genetic family) • with inherited conditions, don’t forget the family
Any questions?
Summary • • • recognise the different presentations of ACS use the ABCDE approach start appropriate immediate treatment arrange immediate PPCI when appropriate be aware of other cardiac causes of arrest requiring different management
Advanced Life Support Level 2 Course Slide set All rights reserved © Australian Resuscitation Council (August 2018)
 Causes of cardiac arrest
Causes of cardiac arrest Cause of cardiac arrest
Cause of cardiac arrest Classification of antiarrhythmic drugs with examples
Classification of antiarrhythmic drugs with examples Pediatric assesment triangle
Pediatric assesment triangle Code pink hospital
Code pink hospital In hospital cardiac arrest chain of survival
In hospital cardiac arrest chain of survival The power of the church chapter 13 section 4
The power of the church chapter 13 section 4 Otto invades italy on pope's behalf causes and outcomes
Otto invades italy on pope's behalf causes and outcomes Example of learning outcomes
Example of learning outcomes Water cycle learning outcomes
Water cycle learning outcomes Lesson plan for notice writing
Lesson plan for notice writing Swot analza
Swot analza Learning outcomes of rhymes
Learning outcomes of rhymes Planning goals and learning outcomes
Planning goals and learning outcomes What is photolysis in photosynthesis
What is photolysis in photosynthesis Learning outcomes of photosynthesis
Learning outcomes of photosynthesis 7 domain of ncbts
7 domain of ncbts Learning outcomes of linear equations in one variable
Learning outcomes of linear equations in one variable Learning outcome generator
Learning outcome generator Reported speech objectives
Reported speech objectives Purpose of learning outcomes
Purpose of learning outcomes Output devices purpose
Output devices purpose Ib psychology learning outcomes
Ib psychology learning outcomes Essay writing learning outcomes
Essay writing learning outcomes Learning outcomes of holy week
Learning outcomes of holy week Learning outcomes of holy week
Learning outcomes of holy week Headstart early learning outcomes framework
Headstart early learning outcomes framework Learning objectives of fruits and vegetables
Learning objectives of fruits and vegetables Gagne learning outcomes
Gagne learning outcomes