Cardiac Arrest Arrhythmias Terry White RN Cardiac Arrest
- Slides: 34
Cardiac Arrest Arrhythmias Terry White, RN
Cardiac Arrest u. Mechanisms v. Ventricular Fibrillation v. Pulseless Ventricular Tachycardia v. Asystole v. Pulseless Electrical Activity (PEA) u. A condition; Not an ECG rhythm
Cardiac Arrest u. Most common rhythms v. Adults: ventricular fibrillation v. Children: Asystole, Bradycardic PEA v. Pediatric V-fib suggests: u. Drug toxicity u. Electrolyte imbalance u. Congenital heart disease
Cardiac Arrest u ABCs come first! v Airway - unobstructed? manually open v Breathing - no or inadequate ventilate v Circulation - no pulse in 5 sec chest compressions u Do NOT wait on equipment u Assure effective BLS before going to ALS v Rise and fall of chest v Air movement in lung fields v Pulse with compressions
Cardiac Arrest u. First ALS priority is defibrillation v. Only cure for v-fib is defib v. The quicker the better u. Probability of resuscitation decreases 7 -10% with each passing minute
Cardiac Arrest u Vascular access v Antecubital space u. Arm, EJ, Foot (last resort) u. IO in peds < 6 y/o v 14 or 16 gauge v LR or NS v 30 sec - 60 sec of CPR to circulate drug
Cardiac Arrest u. Intubation as time allows v. Less emphasis today as compared to past v. Epi, atropine, lidocaine may be administered down tube u 2 x IV dose u. IV is preferred
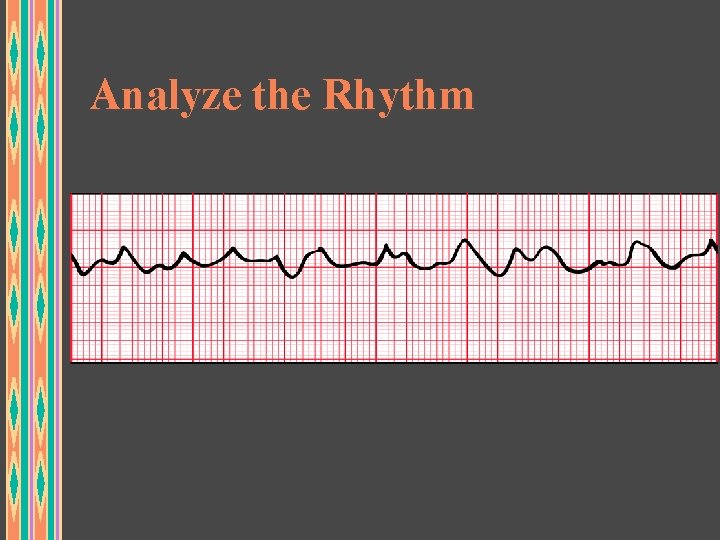
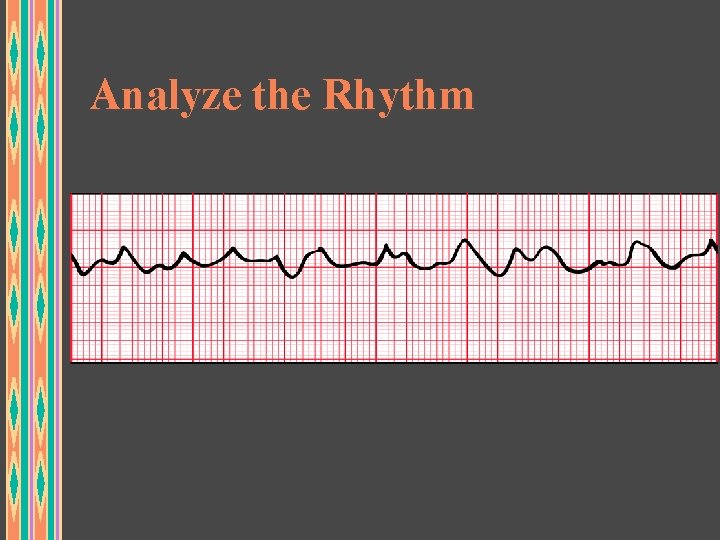
Analyze the Rhythm
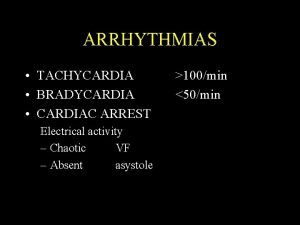
Ventricular Fibrillation (VF) u Characteristics v Chaotic, irregular, ventricular rhythm v Wide, variable, bizarre complexes v Fast rate of activity v Multiple ventricular foci v No cardiac output v Terminal rhythm if not corrected quickly v Most common rhythm causing sudden cardiac death in adults
Ventricular Fibrillation (VF) Treatment u ABC’s u Witnessed arrest: Precordial thump v Little demonstrated value but worth a try u CPR until defibrillator available u Quick Look for VF or pulseless VT v Treat pulseless VT as if it were VF u Defibrillate v 200 J, 360 J v Quickly and in rapid succession u Identify cause if possible
Ventricular Fibrillation Treatment u If still in VF/VT arrest, continue CPR for 1 minute u Establish IV access and Intubate v If sufficient personnel, attempt both simultaneously v If not, quick attempt at IV access then attempt ETT u Vasopressor Medication v Epinephrine 1 mg 1: 10, 000 IVP u Repeat every 3 -5 mins as long as arrest persists u v Vasopressin (alternative to Epinephrine) u 40 units IVP one time only
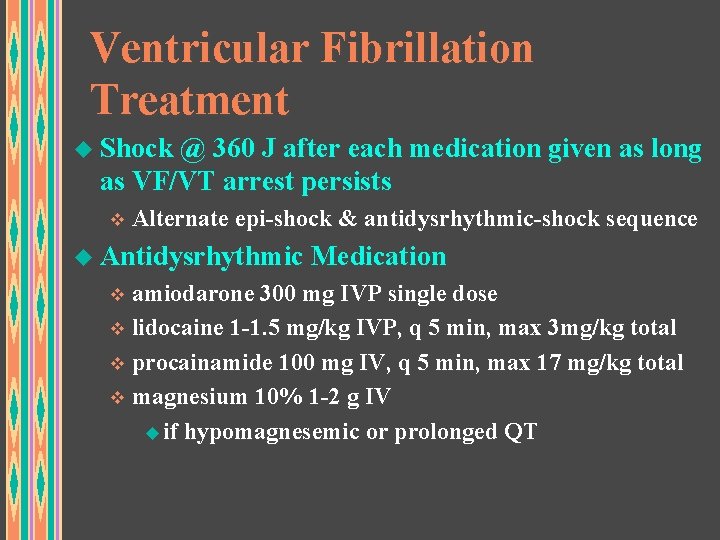
Ventricular Fibrillation Treatment u Shock @ 360 J after each medication given as long as VF/VT arrest persists v Alternate epi-shock & antidysrhythmic-shock sequence u Antidysrhythmic Medication v amiodarone 300 mg IVP single dose v lidocaine 1 -1. 5 mg/kg IVP, q 5 min, max 3 mg/kg total v procainamide 100 mg IV, q 5 min, max 17 mg/kg total v magnesium 10% 1 -2 g IV u if hypomagnesemic or prolonged QT
Ventricular Fibrillation Treatment u Consider Na. HCO 3 if prolonged v Only after effective ventilations u In many EMS systems, consider terminating resuscitation efforts in consult with med control
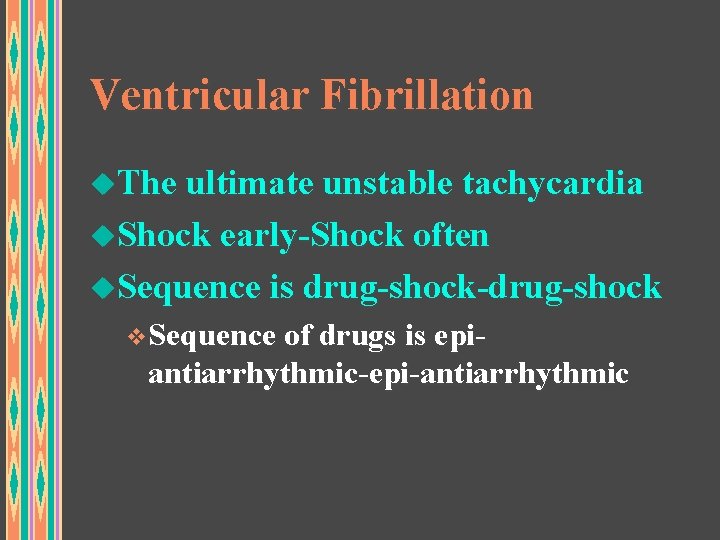
Ventricular Fibrillation u. The ultimate unstable tachycardia u. Shock early-Shock often u. Sequence is drug-shock-drug-shock v. Sequence of drugs is epi- antiarrhythmic-epi-antiarrhythmic
Analyze the Rhythm
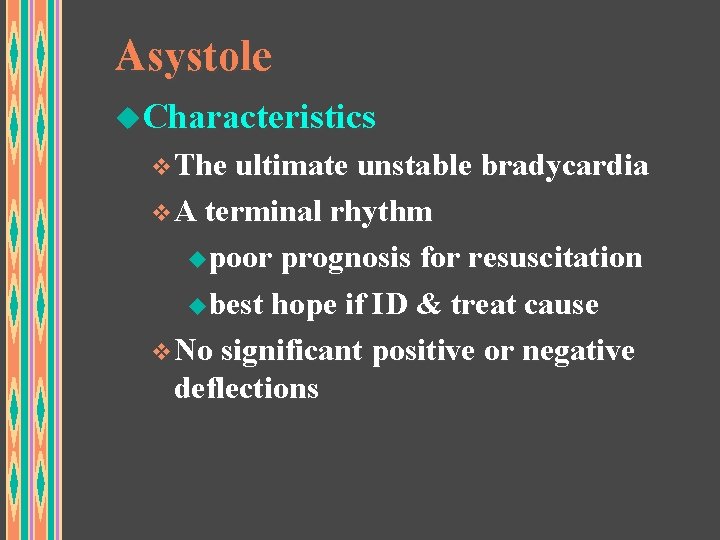
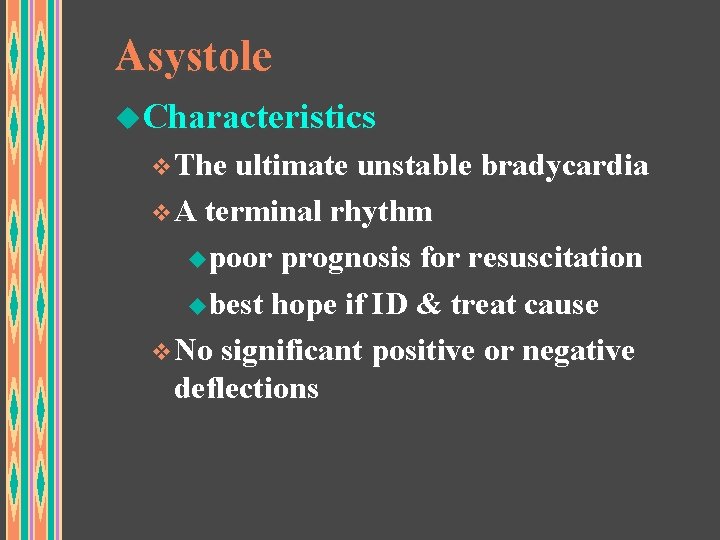
Asystole u. Characteristics v. The ultimate unstable bradycardia v. A terminal rhythm upoor prognosis for resuscitation ubest hope if ID & treat cause v. No significant positive or negative deflections
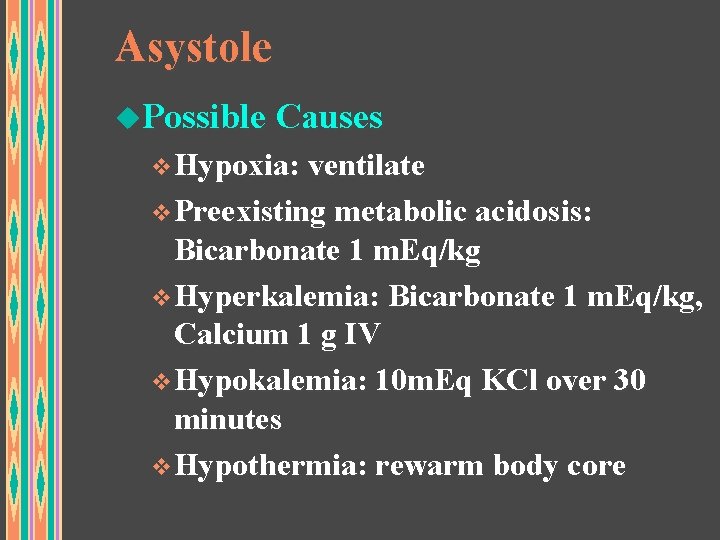
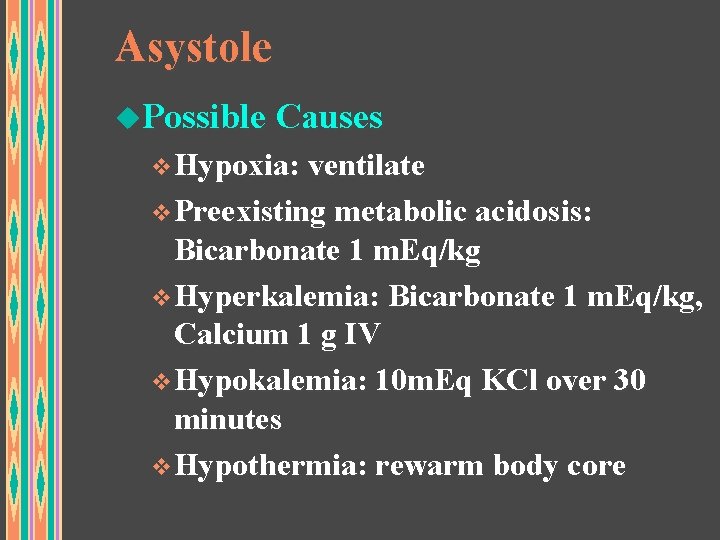
Asystole u. Possible Causes v. Hypoxia: ventilate v. Preexisting metabolic acidosis: Bicarbonate 1 m. Eq/kg v. Hyperkalemia: Bicarbonate 1 m. Eq/kg, Calcium 1 g IV v. Hypokalemia: 10 m. Eq KCl over 30 minutes v. Hypothermia: rewarm body core
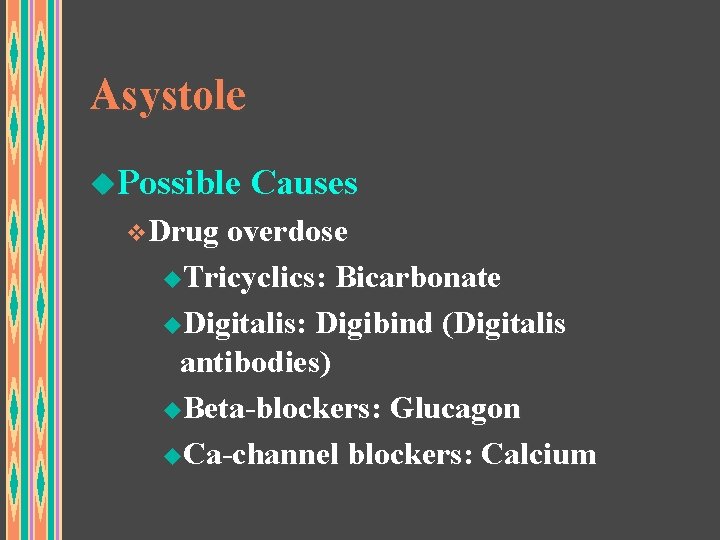
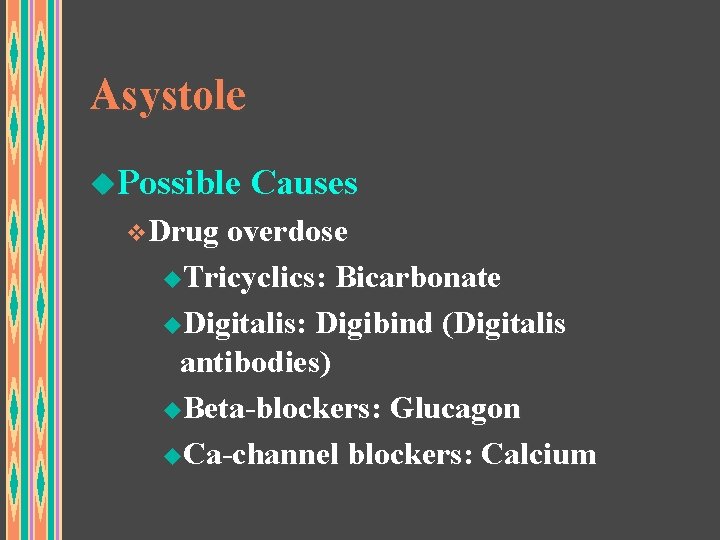
Asystole u. Possible Causes v. Drug overdose u. Tricyclics: Bicarbonate u. Digitalis: Digibind (Digitalis antibodies) u. Beta-blockers: Glucagon u. Ca-channel blockers: Calcium
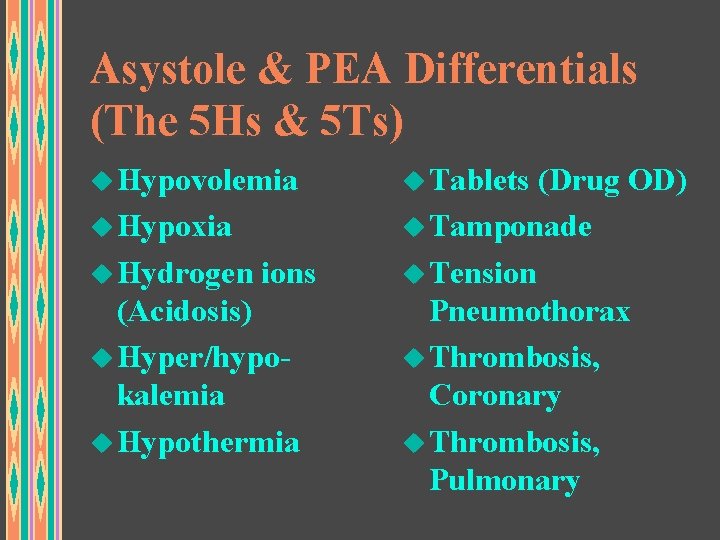
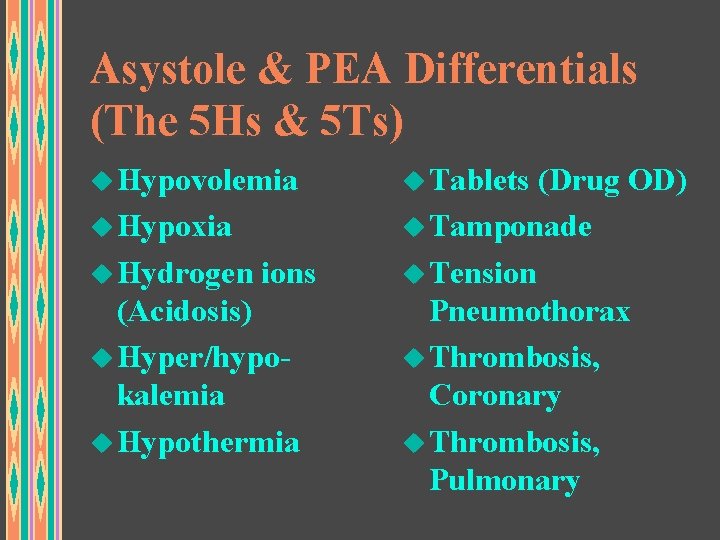
Asystole & PEA Differentials (The 5 Hs & 5 Ts) u Hypovolemia u Tablets (Drug OD) u Hypoxia u Tamponade u Hydrogen ions u Tension (Acidosis) u Hyper/hypokalemia u Hypothermia Pneumothorax u Thrombosis, Coronary u Thrombosis, Pulmonary
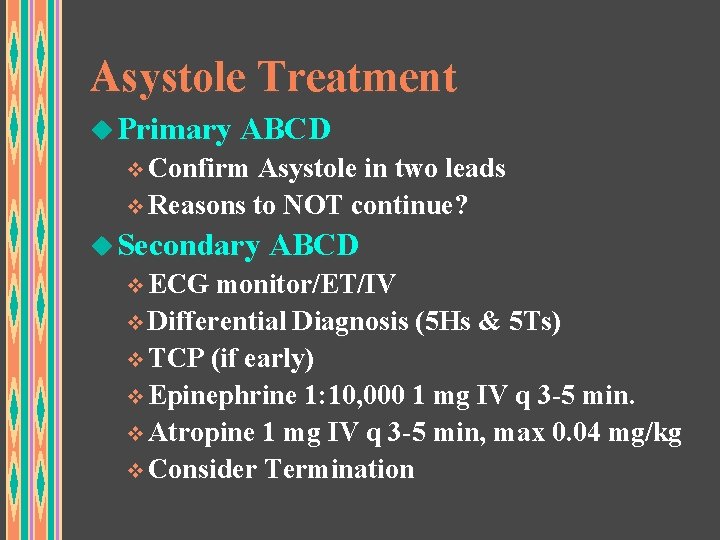
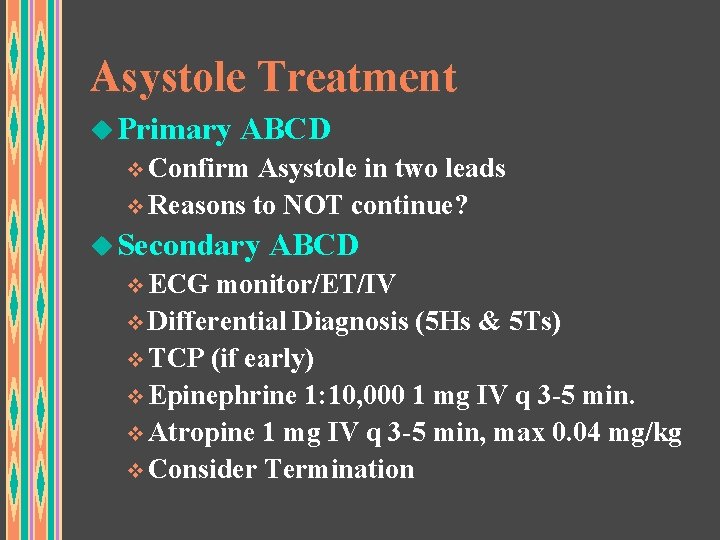
Asystole Treatment u Primary ABCD v Confirm Asystole in two leads v Reasons to NOT continue? u Secondary ABCD v ECG monitor/ET/IV v Differential Diagnosis (5 Hs & 5 Ts) v TCP (if early) v Epinephrine 1: 10, 000 1 mg IV q 3 -5 min. v Atropine 1 mg IV q 3 -5 min, max 0. 04 mg/kg v Consider Termination
Analyze the Rhythm What are you going to do for this patient?
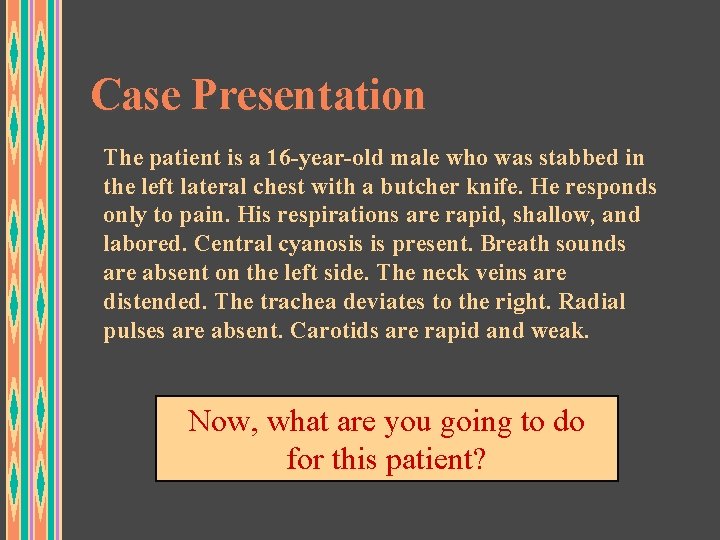
Case Presentation The patient is a 16 -year-old male who was stabbed in the left lateral chest with a butcher knife. He responds only to pain. His respirations are rapid, shallow, and labored. Central cyanosis is present. Breath sounds are absent on the left side. The neck veins are distended. The trachea deviates to the right. Radial pulses are absent. Carotids are rapid and weak. Now, what are you going to do for this patient?
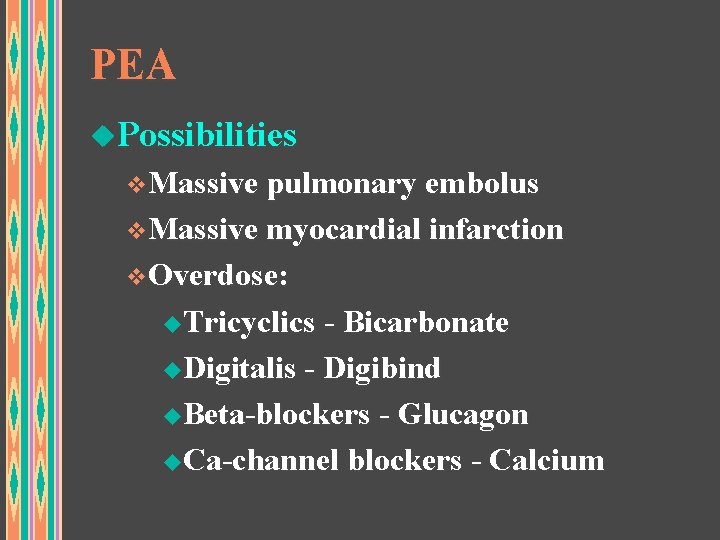
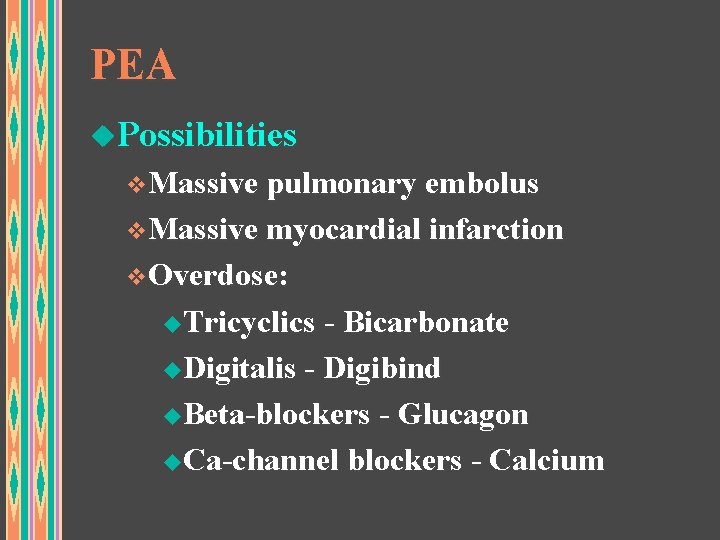
PEA u. Possibilities v. Massive pulmonary embolus v. Massive myocardial infarction v. Overdose: u. Tricyclics - Bicarbonate u. Digitalis - Digibind u. Beta-blockers - Glucagon u. Ca-channel blockers - Calcium
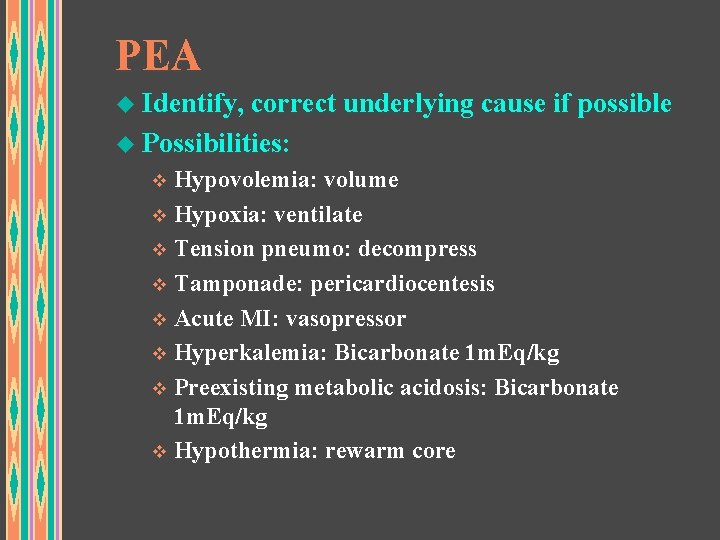
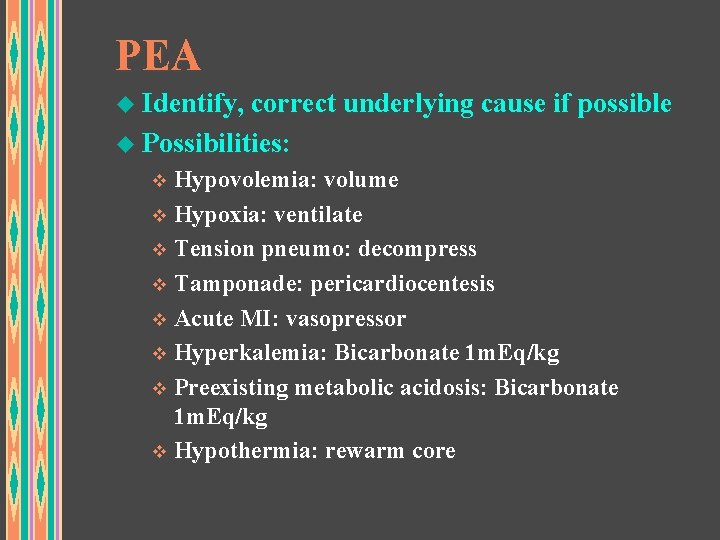
PEA u Identify, correct underlying cause if possible u Possibilities: v Hypovolemia: volume v Hypoxia: ventilate v Tension pneumo: decompress v Tamponade: pericardiocentesis v Acute MI: vasopressor v Hyperkalemia: Bicarbonate 1 m. Eq/kg v Preexisting metabolic acidosis: Bicarbonate 1 m. Eq/kg v Hypothermia: rewarm core
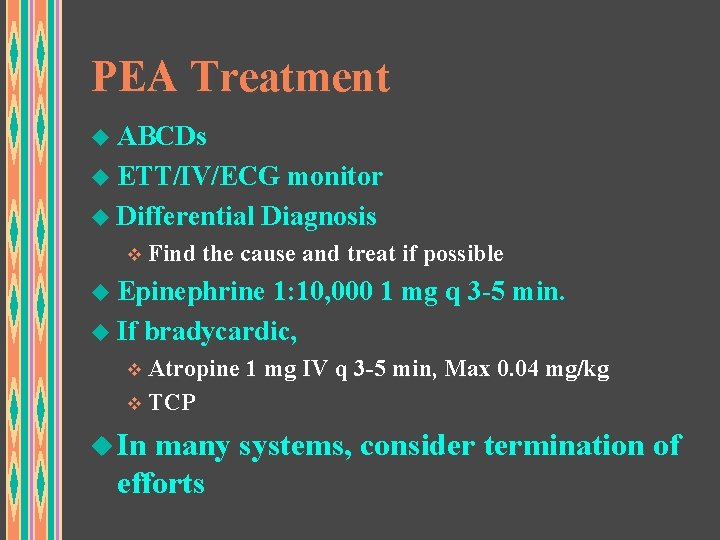
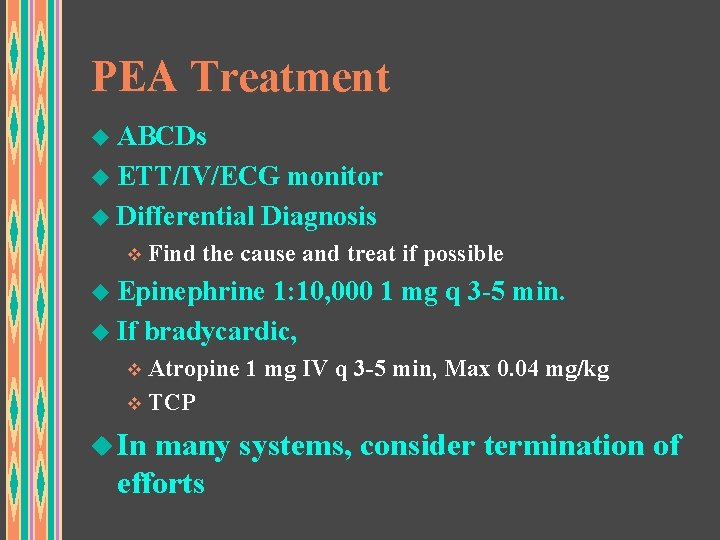
PEA Treatment u ABCDs u ETT/IV/ECG monitor u Differential Diagnosis v Find the cause and treat if possible u Epinephrine 1: 10, 000 1 mg q 3 -5 min. u If bradycardic, v Atropine 1 mg IV q 3 -5 min, Max 0. 04 mg/kg v TCP u In many systems, consider termination of efforts
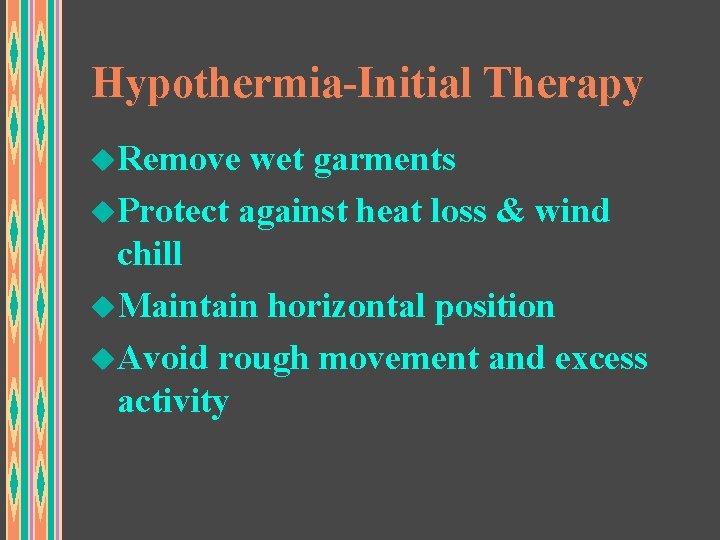
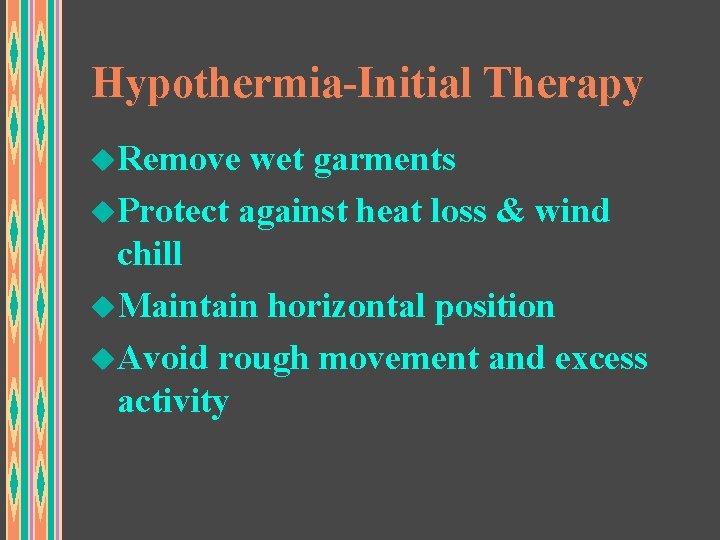
Hypothermia-Initial Therapy u. Remove wet garments u. Protect against heat loss & wind chill u. Maintain horizontal position u. Avoid rough movement and excess activity
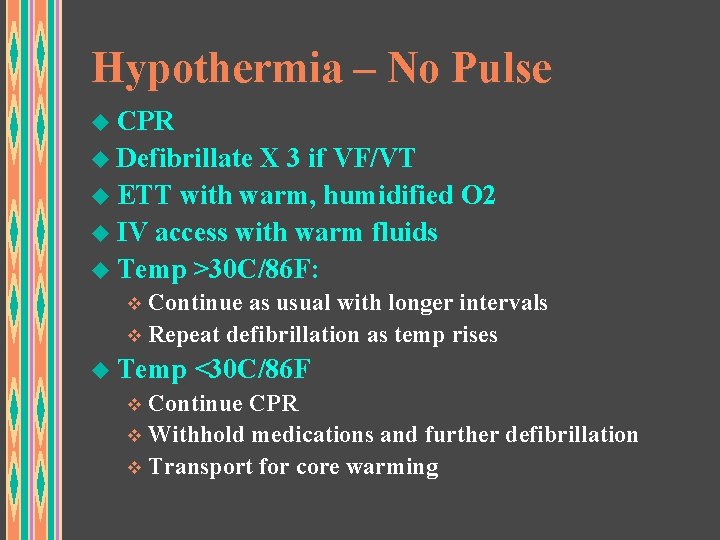
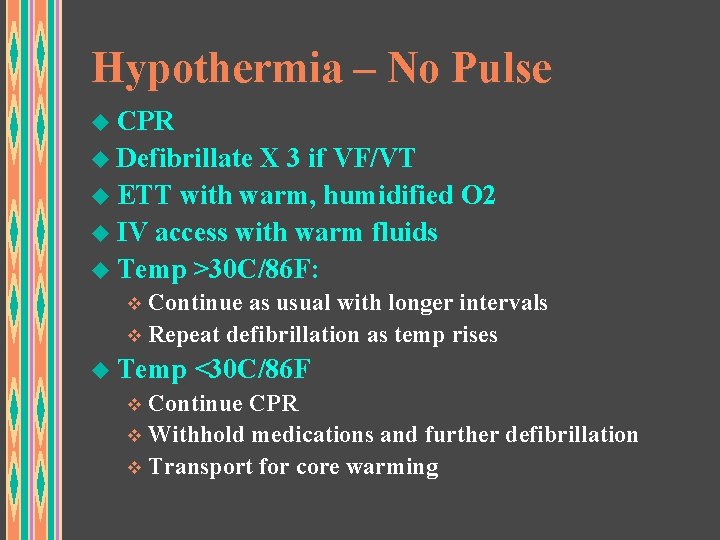
Hypothermia – No Pulse u CPR u Defibrillate X 3 if VF/VT u ETT with warm, humidified O 2 u IV access with warm fluids u Temp >30 C/86 F: v Continue as usual with longer intervals v Repeat defibrillation as temp rises u Temp <30 C/86 F v Continue CPR v Withhold medications and further defibrillation v Transport for core warming
Hypothermia – No Pulse Remember: A hypothermic patient is not dead until he is WARM & DEAD!!!
Managing Cardiac Arrest Check pulse after any treatment or rhythm change
Post-resuscitation Care u If pulse present: v. Assess breathing u. Present? u. Air moving adequately? u. Equal breath sounds? u. Possible flail chest?
Post-resuscitation Care u. If pulse present: v. Protect airway u. Position to prevent aspiration u. Consider intubation v 100% Oxygen via BVM or NRB v. Vascular access
Post-resuscitation Care u. Assess perfusion v. Evaluate u. Pulses u. Skin color u. Skin temperature u. Capillary refill u. BP v. Key is perfusion, not pressure
Post-resuscitation Care u. Management of Decreased Perfusion v. Fluid challenge v. Catecholamine infusion u. Dopamine, or u. Norepinephrine v. Titrate to BP ~ 90 to 100 systolic
Post-resuscitation Care u. Suppression of ventricular irritability v. If VT or VF converted before lidocaine given, lidocaine bolus and drip v. If lidocaine or bretylium worked, begin infusion v. Suppress irritability before giving vasopressors
 Pat pediatric assessment
Pat pediatric assessment Causes of cardiac arrest
Causes of cardiac arrest Hospital code colors
Hospital code colors In hospital cardiac arrest chain of survival
In hospital cardiac arrest chain of survival Amiodarone mechanism of action
Amiodarone mechanism of action Yong hoon kim
Yong hoon kim What is a nonsense poem
What is a nonsense poem Ellen g white biography
Ellen g white biography Amsta arrest
Amsta arrest Nabızsız elektriksel aktivite
Nabızsız elektriksel aktivite Advantage arrest
Advantage arrest Gary goulin arrest
Gary goulin arrest Dbi sala
Dbi sala Cipd arrest report
Cipd arrest report Gary goulin arrest
Gary goulin arrest Respiratory arrest definition
Respiratory arrest definition Hastane dışı kardiyak arrest
Hastane dışı kardiyak arrest Who was arrested in act 2 of the crucible
Who was arrested in act 2 of the crucible Chicago arrest search
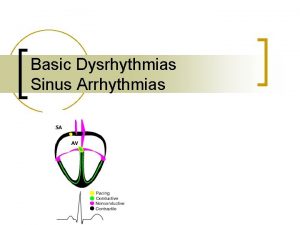
Chicago arrest search Sinuzal arrest
Sinuzal arrest Dka diagnosis
Dka diagnosis Ecg rhythm strip interpretation basic-lesson 7
Ecg rhythm strip interpretation basic-lesson 7 Fall protection methods
Fall protection methods How quickly did things get out of hand in salem
How quickly did things get out of hand in salem Bridget riley descending
Bridget riley descending Total sirkulatuar arrest
Total sirkulatuar arrest Dr douglas vaughan
Dr douglas vaughan Ketouria
Ketouria Sinus pause
Sinus pause Khadija diallo arrest
Khadija diallo arrest Kaushik arrest
Kaushik arrest Dasar dasar pengambilan keputusan menurut george r terry
Dasar dasar pengambilan keputusan menurut george r terry Dr. terry walker
Dr. terry walker Nttml-10
Nttml-10 Wsfcs atkins
Wsfcs atkins