Acute postinfectious glomerulonephritis APIG is the most common













- Slides: 75
Acute postinfectious glomerulonephritis APIG) is the most common renal pathology in underdeveloped countries
The clinical presentation of APIG varies from subclinical disease to acute renal failure, and is usually accompanied by transient hypocomplementemia. • Dark urine and suppression of urine output was a feared complication of the convalescent period of scarlet fever • The disease is characterized by sudden onset of nephritic signs, such as hematuria, edema, hypertension, oliguria, and azotemia.
Epidemiology • pyoderma In the tropics, M types 2, 47, 49, 55, 57, and 60 • moderate and cold climates, PSGN is a complication of upper respiratory tract infections (pharyngitis) M types 1, 2, 3, 4, 12, 25, and 45 •
• Group A streptococci divide into 2 groups based on presnce or absence of a lipoproteinase that causes serun to become opaque; each has characteristic group of M proteins: – Opacity factor negative(rheumatogenic strains) – Opacity factor positive(nephritigenic strains) So no association.
• The male : female ratio is up to 2 : 1 • when subclinical cases are included, male predominance disappears. • aged 3 to 12 years
• risk for developing PSGN after infection with a nephritogenic strain of GABHS is about 15%; for M type 49, it is 5% after pharyngeal infection and 25% after pyoderma. • streptococci from groups C and G (common nephritogenic antigen (endostreptosin)), • recent epidemic have been caused by Streptococcus zooepidemicus and associated with the consumption of unpasteurized milk from cows with mastitis
• cases occur in communities poor, with deficient hygienic conditions and with uneasy access to opportune medical care • Marked reduction in the incidence(pyoderma ) – easier and earlier access to competent medical treatment of streptococcal infections – the widespread use of fluorination of water
PATHOGENESIS • (1) deposition of circulating immune complexes containing nephritogenic antigen in glomeruli, • (2) implantation of the nephritogenic antigen into glomerular structures and in situ formation of immune • complexes, • (3) molecular mimicry between streptococcal antigens and normal glomerular antigens that react with antibodies against streptococcal antigens, • (4) direct activation of the complement system by implanted streptococcal antigens.
nephritogenic antigens • endostreptosin(ESS) • (1) ESS is an anionic antigen, and its implantation on the GBM is not explained, • (2) injections of ESS have never induced histological changes and clinical features compatible with PSGN. • (3) early in course,
nephritogenic antigens • antigens were responsible for immunopathogenesis of PSGN; • induce long-lasting antibody response • 1. streptococcal pyrogenic exotoxin (erythrotoxin) B (SPEB) and its zymogen precursor (z. SPEB). • 2. nephritis associated plasmin receptor (NAPlr), identified as glyceraldehyde 3 phosphate dehydrogenase (GAPDH)
SPEB • SPEB is co-localized in the glomeruli with complement and Ig deposits • is the only streptococcal antigen that has been localized within the electron dense subepithelial deposits (humps)
NAPlr • nephritogenic potential of the NAPlr may reside in its plasmin binding characteristics • it is not co-localized with either Ig or complement • Increased plasmin binding and degrading GBM by promoting the local inflammatory reactivity and facilitate the penetration of nephritogenic antigen-antibody complexes.
• M serotypes ; do not confer life immunity; not in zooepidemics (C) • Autoimmunogenic streptococcal-altered Ig. G by neuraminidase; rheumatogenic and nephritogenic strains • Nephritis strain-assotiated protein (NSAP) • Streptokinase deposition; NZ 131 strains
• Immune complexes deposited from the circulation or formed in situ activate the complement cascade that leads to production of various cytokines and other cellular immunity factors that initiate an inflammatory response manifested by cellular proliferation and edema of the glomerular tuft
• Complement activation occurs preferentially by the alternate pathway. • Ig-binding proteins in streptococcal surface interfere with the classical pathway of complement activation. • Recent investigations have shown that the lectin pathway of complementmay also be activated in APSGN by the recognition of glucosamine residues • cell-mediated mechanisms are also involved in the development of APSGN. Glomerular infiltration of lymphocytes and macrophages
• A number of autoimmune findings have been reported in APSGN • rheumatoid factor, cryoglobulins, and antineutrophil cytoplasmic antibodies
• Cryoglobulins are high titers of rheumatoid factor • present in about two-third of the patients in the first week of the disease; • The anti-Ig. G reactivity may be the result of autoantigenic modification of Ig that occurs with its desialization caused by streptococcal neuraminidase. • ANCA has been found in two-third of the patients with azotemia and 70% of the patients with APSGN that develop crescentic glomerulonephritis

PATHOLOGY • Biopsy findings in APSGN are those of endocapillary proliferative glomerulonephritis • light microscopy: • 1. diffuse enlargement of all glomeruli due to hypercellularity • 2. swelling of the endothelial cells that leads to the obliteration of the capillary loops
• mesangial cells is increased. • There is recruitment of numerous inflammatory cells in the glomeruli, mainly polymorphonuclear leukocytes and monocytes; exudative proliferative glomerulonephritis. • Glomerular basement membrane is normal • Capillary walls are not thickened. Arterioles and tubules are not affected
• Edema of the interstitium and infiltration with inflammatory cells may be found. • Rarely, proliferation of parietal cells of Bowman’s capsule may result in the formation of crescents; • if the proportion of crescents is high, the disease may run a rapidly progressive course.

immunofluorescent study, • irregular granular deposits of complement and immunoglobulins • C 3 and Ig. G, but C 4, C 1 q, Ig. M, fibrinogen, and factor B may be found. • mesangium or in the GBM or in both • Recent studies have co-localized SPEB deposits with complement and Ig. G and NAPlr with plasmin activity in the glomeruli
• 1. starry sky (discrete mesangial and basement membrane deposits, usually of complement) • fine granular deposition of C 3 and Ig. G along the capillary walls in the first week of the disease • 2. Mesangial pattern is found between the 4 th and 6 th week after disease onset; the only immune reactant is C 3, which is found in mesangial location. • with features of the acute nephritic syndrome. • 3. Garland type is characterized by dense, confluent deposits along the capillary loops in the basement membrane. • mesangial and endocapillary locations are preserved…. • with massive proteinuria


electron microscopy • deposits on the subepithelial side of the GBM (humps) • These deposits disappear after the 6 th week from disease onset. • characteristic lesion is not pathognomonic of APSGN since it may also be found in other immune complex glomerulonephritis, notably lupus nephritis.


• The resolution of the proliferative changes is by apoptosis • Prolonged oliguria or oligoanuria has been associated with mesangiolysis (44). • Follow-up studies performed several years after the initial episode of acute poststreptococcal glomerulonephritis, have revealed immune deposits and a variable degree of mesangial sclerosis and obliteration, even in the absence of clinical manifestations of renal disease
CLINICAL FEATURES • rare below the age of 2 and above the age of 20 • twice more frequent in males than in females. • The usual sites of antecedent infection are the skin and the throat • Sites of infection: – pneumonia, – meningitis (particularly with infected ventriculo-atrial or ventriculo-peritoneal shunts), – sepsis, – infected endocarditis(SBE)
• Three phases: – Latent – Acute – Recovery

• The latent period is usually 10 to 14 days after pharyngitis or 2 to 3 weeks after pyoderma. • One-third of APSGN patients develop discrete microscopic hematuria and/or proteinuria in the latent period. • clinical PSGN represents only 10% of all cases, while 90% of cases develop subclinical disease and thus escape medical attention due to absence of symptoms.
Subclinical disease • characterized by a reduction of serum complement, microscopic hematuria and normal or increased blood pressure in asymptomatic patients • In epidemic conditions occurs 1. 5 times more frequently than clinically apparent disease • in non-epidemic situations the patients without symptoms are 4– 5 times more frequent than symptomatic patients • One report: PSAGN in 20% of a. Sx family of pt.
CLINICAL FEATURES • sudden onset with development of nephritic syndrome (edema, oliguria, azotemia, hematuria, hypertension) • initial nonspecific symptoms(as pallor, malaise, low-grade fever, lethargy, anorexia, and headache)
Hematuria • Gross hematuria is present in one-third of (30% to 70% ) • microscopic hematuria is present in all patients. • smoky, cola colored, tea colored, or rusty. • Gross hematuria may last a few hours during the day. • Usually it resolves after 1 to 2 weeks and transforms into microscopic hematuria. • Once gross hematuria has resolved, relapses may appear after physical exercise or intercurrent infections • dysmorphic red blood cells and casts.
Edema • Results from retention of salt and water • is the chief complaint more frequently in children (90%) than in adult patients (75%). • Younger children tend to have more often anasarca. • ascities is uncommon, except in the cases with nephrotic syndrome. • mild morning periorbital , pretibial area , generalized (anasarca) with presence of pleural effusion and ascites. • restriction of water and salt
Hypertension • third cardinal sign in PSGN, • found in up to 70% of hospitalized children. • Hypertension in PSGN is the low-renin type due to retention of water and salt, which leads to expansion of the extracellular fluid volume with consequent suppression of the renin-angiotensin-aldosterone axis. • Usually it is mild and has a biphasic character. • If hypertension is severe and associated with retinal changes, preexisting renal disease should be suspected. • Normalization of the blood pressure correlates with increased diuresis and recovery of renal function.
Recovery phase • Edema and hypertension typically disappear in 5– 10 days with resolution of fluid overload with diuresis(spontaneous or induced), with resolution of proteinuria and gross hematuria. • If elevated blood pressure persists 4 weeks after disease onset, rapidly progressive disease or chronic glomerulonephritis should be suspected
CLINICAL FEATURES • Oliguria is referred on admission by the patient or their family in less than half of the patients • Massive proteinuria with or without other features of the nephrotic syndrome : 2– 4% – It usually resolves within 2 to 3 weeks – its persistence is a risk factor for progression to chronic renal disease. • Azotemia occurs in 25– 30% of the patients but the need of dialysis is infrequent. • A rapidly progressive azotemia occurs in less than 0. 5% of the case due to the development of crescentic glomerulonephritis. •
Pathophysiology of the Acute Nephritic Syndrome • reduction of the glomerular filtration rate caused by the inflammatory reaction in the glomeruli. • renal blood flow it is usually normal. • the filtration fraction is depressed, frequently below 1%. • Fractional excretion of Na less than 1%(pre renal azotemia) • The reabsorption is appropriately reduced in the proximal tubule and assumed to be maintained at the distal areas. •
Pathophysiology • the reduction in glomerular filtration has long been assigned a central role in the fluid retention in acute glomerulonephritis, • severe fluid retention may some times occur in association with mild reduction in glomerular filtration rate • reduction of glomerular filtration is a feature of renal conditions that are not necessarily associated with fluid retention • Potential influences that may modulate sodium and fluid retention at more distal levels are – endothelial or mesangial factors released by glomerular injury – overexpression of the epithelial sodium channel – interstitial inflammatory cells capable of maintaining an increased intrarenal angiotensin activity.
Pathophysiology • sodium and water retention that results in expansion of the extracellular volume, edema and hypertension. • The potential additional effects of hypoalbuminemia are not present in the acute nephritc syndrome , so the plasma levels of hormones that regulate the extracellular volume (renin-angiotensin, aldosterone and atrial natriuretic peptide) show an appropriate response for an expanded extracellular volume. • The suppression of plasma renin activity and aldosterone and the stimulation of atrial natriuretic peptide are correlated with the severity of edema. • Renal prostaglandin and kallikrein activities are suppressed. • improvement of volume retention • development of spontaneous or induced diuresis results in a prompt reduction of the edema and correction of the hypertension
COMPLICATIONS • Circulatory congestion(since children and youths typically have healthy cardiovascular systems, cardiac failure is rarely seen) • acute renal failure characterized by oliguria to anuria, severe azotemia, and acid–base and electrolyte disturbances • cutaneous and gastrointestinal vasculitis reported, may mimic HSP • acute thrombocytopenic purpura reported. autoantibodies crossreactive against GABHS platelets. • In a very few cases, PSGN with rheumatic fever.
Neurological complication • hypertensive encephalopathy – 0. 5% to 10% of hospitalized patients. – nausea, vomiting, headache, impairment of consciousness (somnolence to coma), seizures, hemiparesis, amaurosis, and aphasia. – Presntation without typical urinary findings(reported) – sudden elevation of the blood pressure, which impairs cerebral autoregulation leading to vasogenic edema • abnormal serum biochemistry • cerebral vasculitis • Nuclear MRI : posterior white matter alteration reversible posterior leukoencephalopathy syndrome •
LABORATORY FINDINGS • hematuria in almost all patients with PSGN. • red blood cell casts and dysmorphic erythrocytes; glomerular origin. • In a few patients, minimal urinary findings contrast with the severe clinical presentation • Proteinuria • mild dilutional anemia • Thrombocytopenia (SLE, HUS) • hyperkalemia, uremia, and acidosis. • Hypoproteinemia, hypoalbuminema, and hyperlipidemia (nephrotic syndrome).
Evidence for previous streptococcal infection • Cultures from the throat or skin. • positive cultures 20– 25% , except epidemics. • rising titers against streptococcal antigens (antistreptolysin O, antihyaluronidase, anti. DNA-se B titer), or a combination of antigens (streptozyme) measured serially • Serial measurement of ASOTiter over 4 weeks. Antistreptolysin O titers and anti-DNAse B titers are the most frequently elevated antibody titers after streptococcal throat infections and after streptococcal impetigo, respectively.
• Anti-z. SPEB/SPEB serum best markers of nephritogenic(not available for routine practice) • Ig. G and Ig. M serum levels elevated 80– 90%. • Two-thirds in the first week of the disease present cryoglobulins and elevated Ig. Ganti. Ig. G rheumatoid factor titers. •
Complement Studies • reduction in more than 90% • marked depression of serum hemolytic component CH 50 and C 3 ; activation of the alternative pathway • Depression of C 3 precedes the onset of heamaturia. • depression of C 2 and C 4 fractions (classical) • anti–C 1 q-positive; severe clinical presentation with hypertension, proteinuria, and unfavorable resolution of the disease • normalize in 6 to 8 weeks( 3 months)
Diagnosis • a child of 4– 15 years who suddenly develops dark and scanty urine and swelling of the face and legs. • high blood pressure and the absence of a systemic illness • history of a precedent upper respiratory infection and/or skin infections
• diagnosis of active skin infection is usually straight forward • clinical judgment may miss half of the streptococal pharyngitis and may incorrectly diagnose a sore throat as due to streptococcal infection in 20– 40% of the cases
• score has a range from 0 to 4 and incorporates age as one of the criteria. ( Mc. Isaac) • +1 to each one of the following: – 1. temperature >38°C, – 2. cervical adenopathy, – 3. no cough, – 4. tonsillar exudate – 5. age between 3 and 14 years. – 6. Age > 44 years is assigned − 1 point. • Sensitivity and specificity of the score is 85 and 95%, respectively. • Antibiotic treatment is recommended (without culture confirmation) when the score is 4, • antibiotic treatment is not indicated (and cultures unnecessary) when scores are 0– 1.
Diagnosis • Positive streptococcal cultures are frequent in epidemic conditions but in less than 25% of the sporadic cases. • rising titer of serum antistreptococcal antibodies. • Anti-NAPlr and anti. SPEB-z. SPEB titers • Streptozyme test which includes four antigens (DNAse B, Streptolysin O, hyaluronidase and streptokinase) positive in more than 80% of the cases.
low complement: • • • 1. APSGN, 2. Lupus nephritis, 3. shunt nephritis, 4. endocarditis, 5. cryoglobulinemia, 6. hypocomplementemic membranoproliferative glomerulonephritis
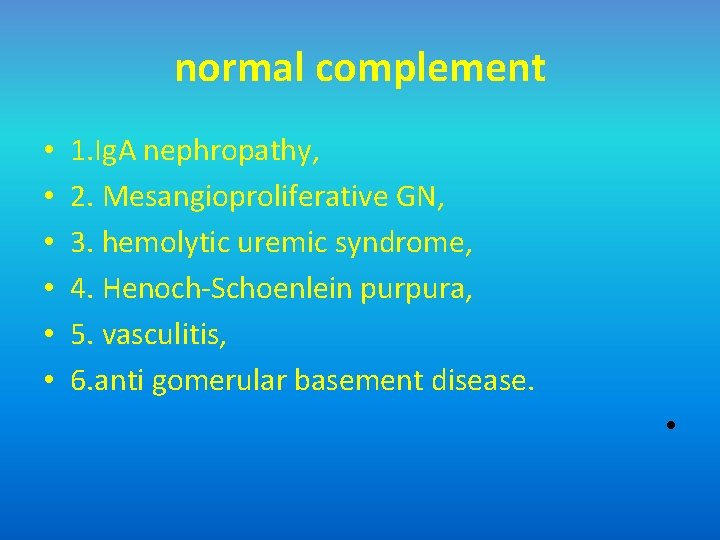
normal complement • • • 1. Ig. A nephropathy, 2. Mesangioproliferative GN, 3. hemolytic uremic syndrome, 4. Henoch-Schoenlein purpura, 5. vasculitis, 6. anti gomerular basement disease. •
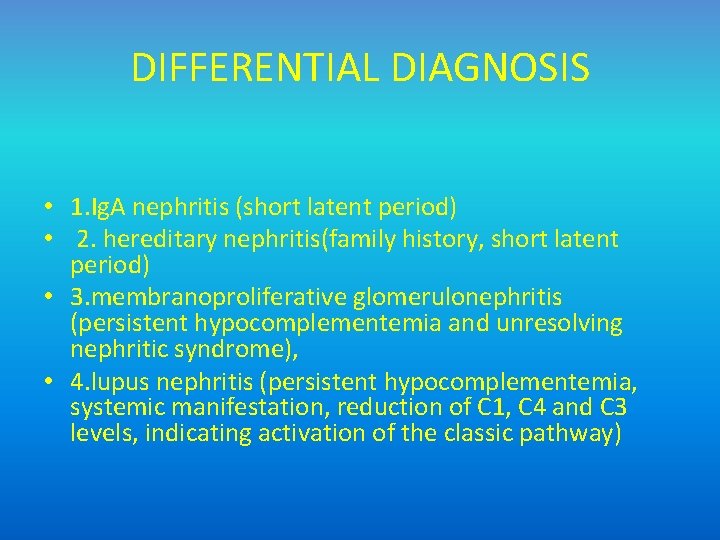
DIFFERENTIAL DIAGNOSIS • 1. Ig. A nephritis (short latent period) • 2. hereditary nephritis(family history, short latent period) • 3. membranoproliferative glomerulonephritis (persistent hypocomplementemia and unresolving nephritic syndrome), • 4. lupus nephritis (persistent hypocomplementemia, systemic manifestation, reduction of C 1, C 4 and C 3 levels, indicating activation of the classic pathway)
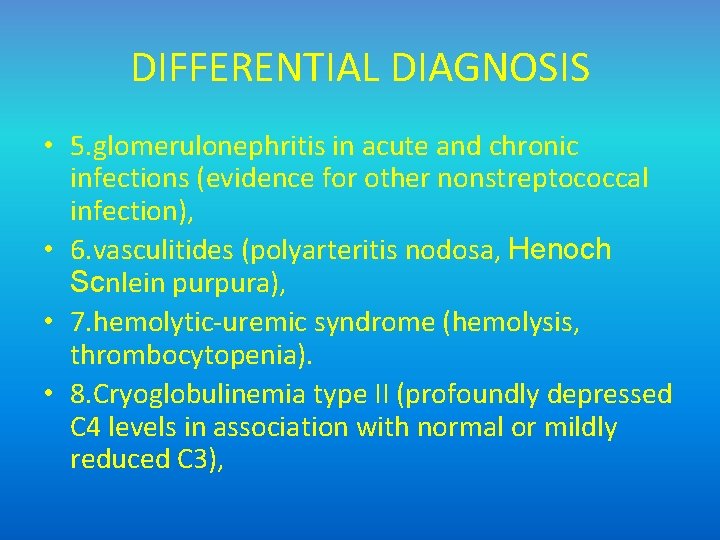
DIFFERENTIAL DIAGNOSIS • 5. glomerulonephritis in acute and chronic infections (evidence for other nonstreptococcal infection), • 6. vasculitides (polyarteritis nodosa, Henoch Scnlein purpura), • 7. hemolytic-uremic syndrome (hemolysis, thrombocytopenia). • 8. Cryoglobulinemia type II (profoundly depressed C 4 levels in association with normal or mildly reduced C 3),
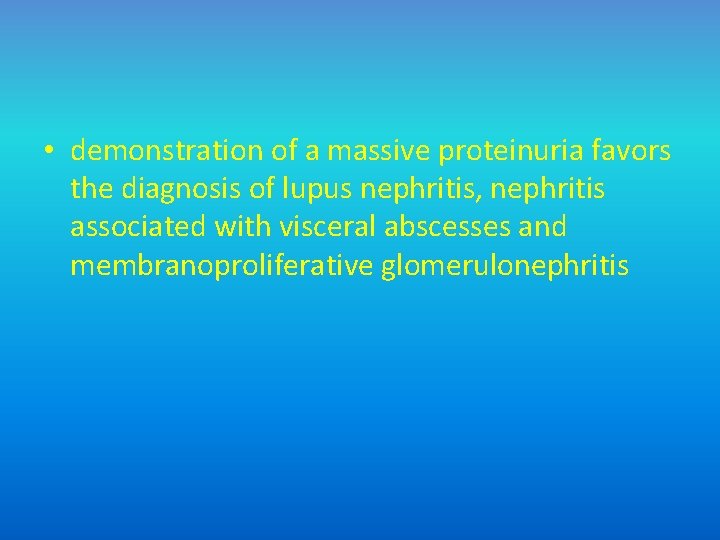
• demonstration of a massive proteinuria favors the diagnosis of lupus nephritis, nephritis associated with visceral abscesses and membranoproliferative glomerulonephritis

TREATMENT • Bed rest and limited activity are indicated in the early stage (particularly circulatory overload and hypertension) • no evidence that prolonged bed rest hastens recovery. • In most cases, fluid and salt restriction are sufficient to prevent edema and hypertension. • Salt intake less than 1. 0 g/day. • protein intake limited to 1. 0 g/kg/day. • marked azotemia, calories provided from carbohydrates and fats. • Diuresis and body weight should be monitored every day.
Diuretics • Loop diuretics (furosemide 1 -2 mg/kg/ day) in moderate circulatory congestion. • Higher doses up to 5 mg/kg (IV) dose in pulmonary edema. • Other diuretics are without effect (thiazide diuretics) or dangerous ( hyperkalemia ; aldosterone antagonists). • Digitalis : ineffective ; intoxication.
hypertension • Moderate hypertension : diuretics and oral antihypertensive drugs (vasodilators; nifedipine, hydralazine, prazosin). • captopril ; hyperkalemia. • hypertensive emergency, : the drug of choice is – labetalol 0. 5 -1. 0 mg/kg/hour IV. – diazoxide 2 -3 mg/kg IV slowly over 30 minutes – Nitroprusside 0. 5 -2 mcg/kg/min IV.
• Severe hyperkalemia, azotemia, acidosis, uncontrolled hypertension, cardiovascular insufficiency, and pulmonary edema are indications for immediate dialysis. • When there is acute renal failure and crescents on biopsy, corticosteroids, methylprednisolone pulses, and cyclophosphamide may be beneficial. •
Antibiotic therapy • signs of streptococcal infection (pharyngitis, pyoderma) • patients have a positive throat or skin culture. • Early administration of penicillin is reported to prevent or ameliorate the severity of acute glomerulonephritis…not proven. • at least one report suggests that APSGN patients that receive antibiotic treatment have a milder clinical course • Oral penicillin V (or erythromycin for allergic patients) FOR 7 TO 10 DAYS or parenteral treatment.
• If infection is not apparent at the time of diagnosis, antibiotic treatment should be given anyway because positive cultures are sometimes obtained in apparently healthy patients and cross infection of household members and siblings of index cases is very high • Antibiotic treatment does not alter the course of the disease, but it is very important in preventing the spread of nephritogenic strains of GABHS to close contacts
Preventive antibiotic treatment • indicated in epidemic situations and to household members of index cases in non-epidemic conditions since most of them present evidence of recent infection and about one-third of them develop nephritis. • In high risk communities the strategy of treating household contacts has resulted in a decrease in the number of cases of PSGN. • Long-term antibiotic prophylaxis is not justified since second attacks of PSGN are very rare. •
PROGNOSIS • the prognosis of PSGN in children in the acute phase is excellent, with mortality of less than 1% due to improved conservative management and availability of dialysis • only clinical cases (10%) are included in the analysis, while those with subclinical and mild disease may escape clinicians’ attention. • prognosis of PSGN caused by group C Streptococcus zooepidemicus is not as promising
risk factors for an unfavorable outcome • • older age, high serum creatinine at presentation nephrotic syndrome crescents on renal biopsy
• Even after initial normalization of renal function, impairment of the GFR may ensue many years after disease onset; thus, children who present with crescents need indefinite follow-up. • APSGN followed for 10– 20 years present frequently abnormal urine analysis (20%) but azotemia occurs in less than 1% of the patients.

THANK YOU



