Renal pulmonar and cardiac failure and nutritio M


- Slides: 50

Renal pulmonar and cardiac failure and nutritio M. safarian, MSc, MD, Ph. D Mashhad University of Medical Sciences, Nutrition Department
Nutrition & Pulmonary function �Dietary habits influence lung function and the tendency to common lung diseases, such as asthma, chronic obstructive pulmonary disease (COPD), and lung cancer. �Optimal nutrition throughout life promotes anatomic development and physiologic function of the pulmonary system. �Nutrition affects lung immune defense mechanisms. 3
Malnutrition & Lung function �Malnutrition adversely affects: �lung structure, elasticity, and function �respiratory muscle mass, strength, and endurance �lung immune defense mechanisms �control of breathing 4
Malnutrition & Lung function Malnutrition impairs �Respiratory muscle function �Ventilatory drive �Response to hypoxia �Pulmonary defense mechanisms
Chronic Pulmonary Disorders �Bronchopulmonary displasia �Cystic fibrosis �Tuberculosis �Bronchial asthma �Chronic obstructive pulmonary disease (COPD)
Acute Pulmonary Disorders �Pulmonary aspiration �Pneumonia �Tuberculosis �Cancer of the lung �Acute respiratory distress syndrome �Pulmonary failure
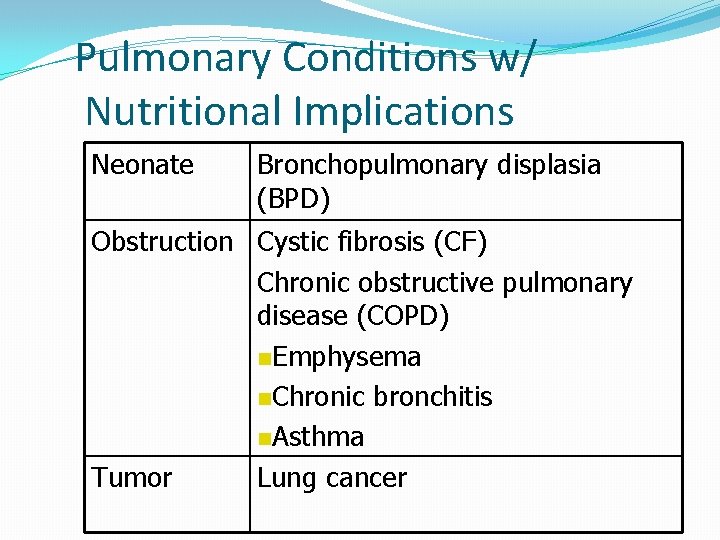
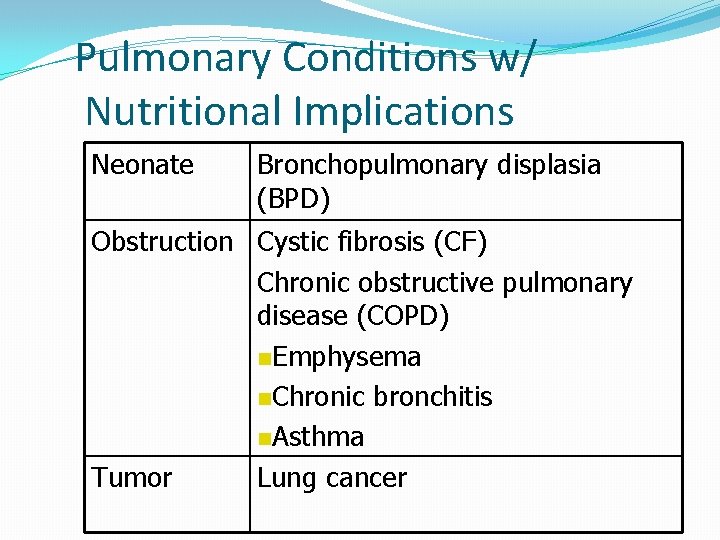
Pulmonary Conditions w/ Nutritional Implications Neonate Bronchopulmonary displasia (BPD) Obstruction Cystic fibrosis (CF) Chronic obstructive pulmonary disease (COPD) n. Emphysema n. Chronic bronchitis n. Asthma Tumor Lung cancer
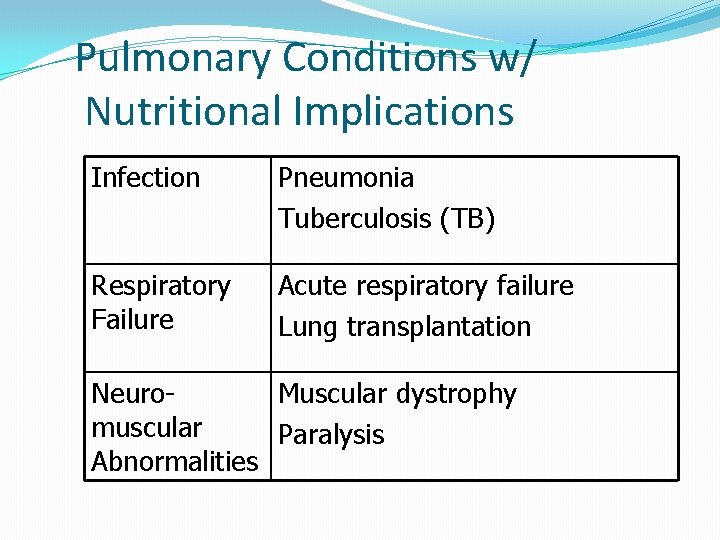
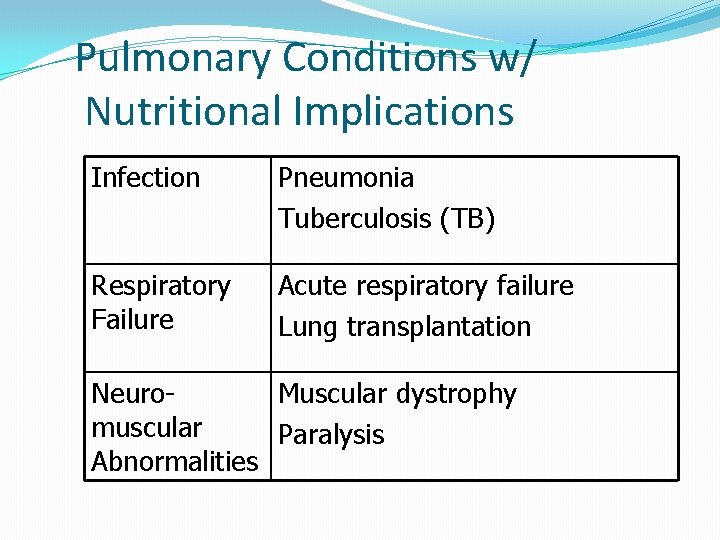
Pulmonary Conditions w/ Nutritional Implications Infection Pneumonia Tuberculosis (TB) Respiratory Failure Acute respiratory failure Lung transplantation Neuro. Muscular dystrophy muscular Paralysis Abnormalities
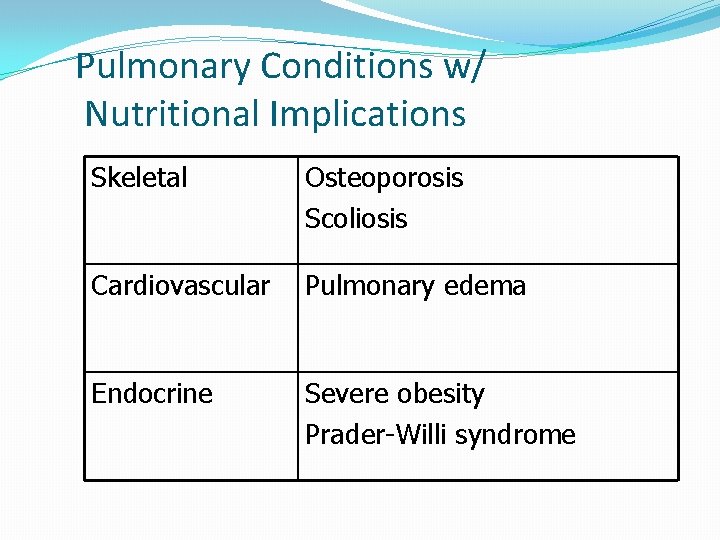
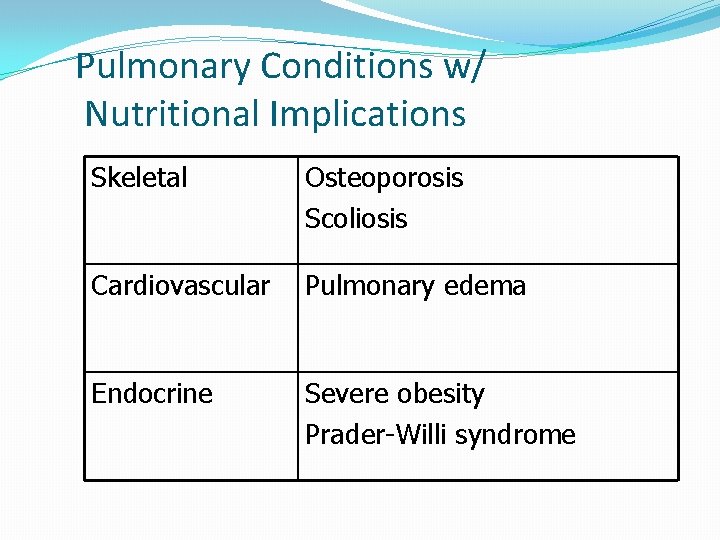
Pulmonary Conditions w/ Nutritional Implications Skeletal Osteoporosis Scoliosis Cardiovascular Pulmonary edema Endocrine Severe obesity Prader-Willi syndrome
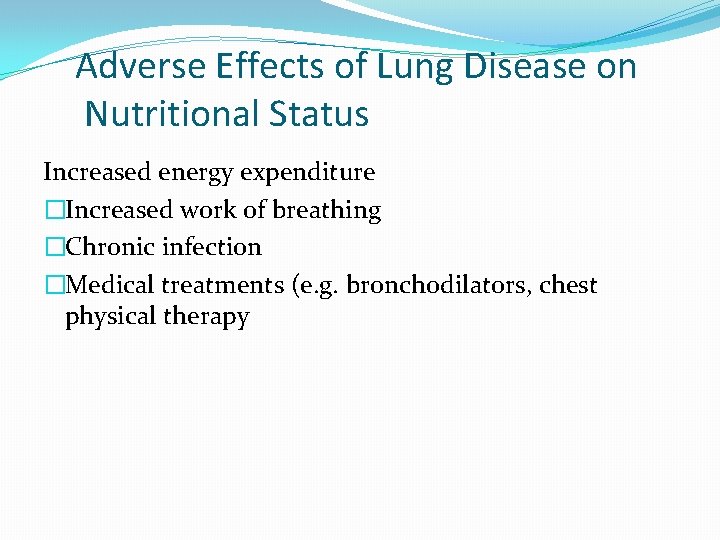
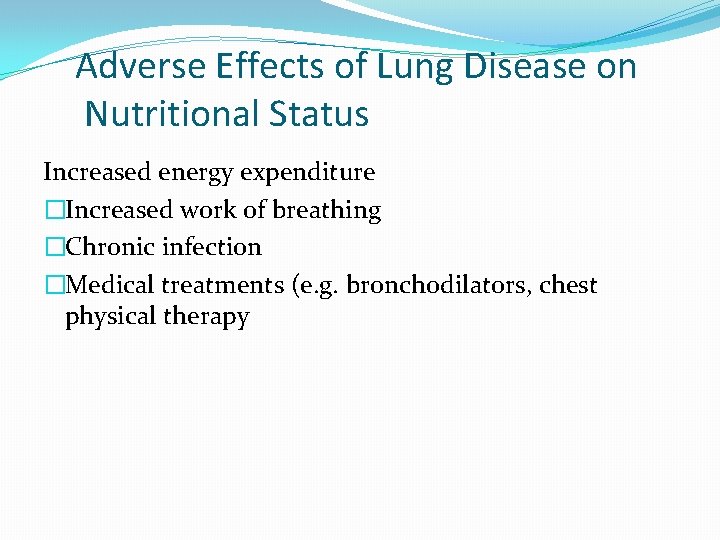
Adverse Effects of Lung Disease on Nutritional Status Increased energy expenditure �Increased work of breathing �Chronic infection �Medical treatments (e. g. bronchodilators, chest physical therapy
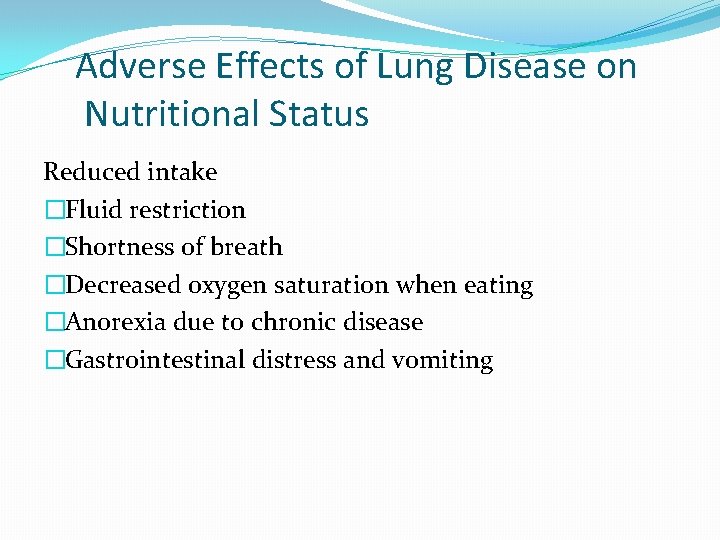
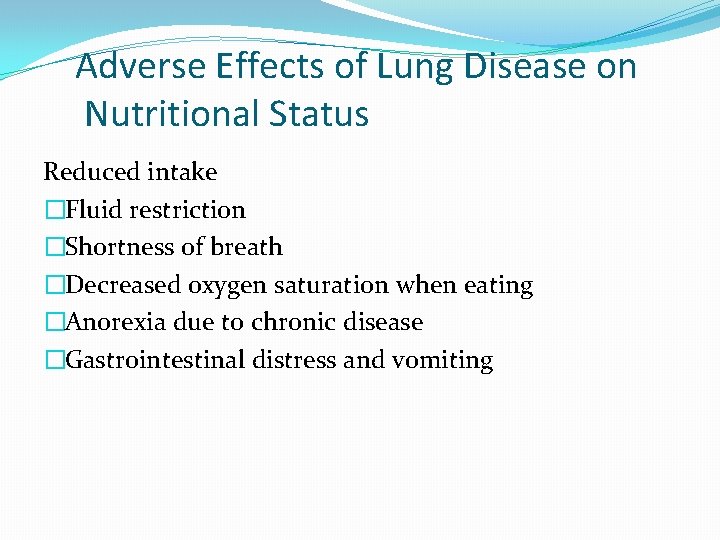
Adverse Effects of Lung Disease on Nutritional Status Reduced intake �Fluid restriction �Shortness of breath �Decreased oxygen saturation when eating �Anorexia due to chronic disease �Gastrointestinal distress and vomiting
Bronchopulmonary Dysplasia: Pathophysiology �Chronic lung condition in newborns that often follows respiratory distress syndrome (RDS) and treatment with oxygen �Characterized by broncheolar metaplasia and interstitial fibrosis �Occurs most frequently in infants who are premature or low birth weight
BPD: Signs and Symptoms �Hypercapnea (CO 2 retention) �Tachypnea �Wheezing �Dyspnea �Recurrent respiratory infections �Cor pulmonale (right ventricular enlargement of the heart)
Growth Failure in BPD �Increased energy needs �Inadequate dietary intake �Gastroesophageal reflux �Emotional deprivation �Chronic hypoxia
Goals of Nutritional Management in BPD �Meet nutritional needs �Promote linear growth �Develop age-appropriate feeding skills �Maintain fluid balance
Energy Needs in BPD �REE in infants with BPD is 25 -50% higher than in age -matched controls �Babies with growth failure may have needs 50% higher �Energy needs in acute phase (PN, controlled temperature) 50 -85 kcals/kg �Energy needs in convalescence (oral feeds, activity, temperature regulation) as high as 120 -130 kcals/kg
Protein Needs in Babies with BPD �Protein: within advised range for infants of comparable post-conceptional age �As energy density of the diet is increased by the addition of fat and carbohydrate, protein should still provide 7% or more of total kcals
Macronutrient Mix in BPD �Fat and carbohydrate should be added to formula only after it has been concentrated to 24 kcals/oz to keep protein high enough �Fat provides EFA and energy when tolerance for fluid and carbohydrate is limited �Excess CHO increases RQ and CO 2 output
Fluid in BPD �Infants with BPD may require fluid restriction, sodium restriction, and long term treatment with diuretics �Use of parenteral lipids or calorically dense enteral feeds may help the infant meet energy needs
Mineral Needs in BPD �Often driven by the baby’s premature status �Lack of mineral stores as a result of prematurity (iron, zinc, calcium) �Growth delay �Medications: diuretics, bronchodilators, antibiotics, cardiac antiarrhythmics, corticosteroids associated with loss of minerals including chloride, potassium, calcium
Vitamin Needs in BPD �Interest in antioxidants, including vitamin A for role in developing epithelial cells of the respiratory tract �Provide intake based on the DRI, including total energy, to promote catchup growth
Feeding Strategies in BPD �Calorically dense formulas or boosted breast milk (monitor fluid status and urinary output) �Small, frequent feedings �Use of a soft nipple �Nasogastric or gastrostomy tube feedings
Cystic Fibrosis �Inherited autosomal recessive disorder � 2 -5% of the white population are heterozygous �CF incidence of 1: 2500 live births � 30, 000 people treated at CF centers in the U. S. �Survival is improving; median age of patients has exceeded 30 years
Cystic Fibrosis �Epithelial cells and exocrine glands secrete abnormal mucus (thick) �Affects respiratory tract, sweat, salivary, intestine, pancreas, liver, reproductive tract
Diagnosis of Cystic Fibrosis �Neonatal screening provides opportunity to prevent malnutrition in CF infants �Sweat test (Na and Cl >60 m. Eq/L) �Chronic lung disease �Failure to thrive �Malabsorption �Family history
Nutritional Implications of CF �Infants born with meconium ileus are highly likely to have CF � 85% of persons with CF have pancreatic insufficiency �Plugs of mucus reduce the digestive enzymes released from the pancreas causing maldigestion of food and malabsorption of nutrients
Nutritional Implications of CF �Decreased bicarbonate secretion reduces digestive enzyme activity �Decreased bile acid reabsorption contributes to fat malabsorption �Excessive mucus lining the GI tract prevents nutrient absorption by the microvilli
Gastrointestinal Complications of CF �Bulky, foul-smelling stools �Cramping and intestinal obstruction �Rectal prolapse �Liver involvement �Pancreatic damage causes impaired glucose tolerance (50% of adults with CF) and development of diabetes (15% of adults with CF)
Nutritional Care Goals �Control malabsorption �Provide adequate nutrients for growth or maintain weight for height or pulmonary function �Prevent nutritional deficiencies
Common Treatments �Pancreatic enzyme replacement �Adjust macronutrients for symptoms �Nutrients for growth �Meconium ileus equivalent: intestinal obstruction (enzymes, fiber, fluids, exercise, stool softeners)
Nutrition and Renal failure
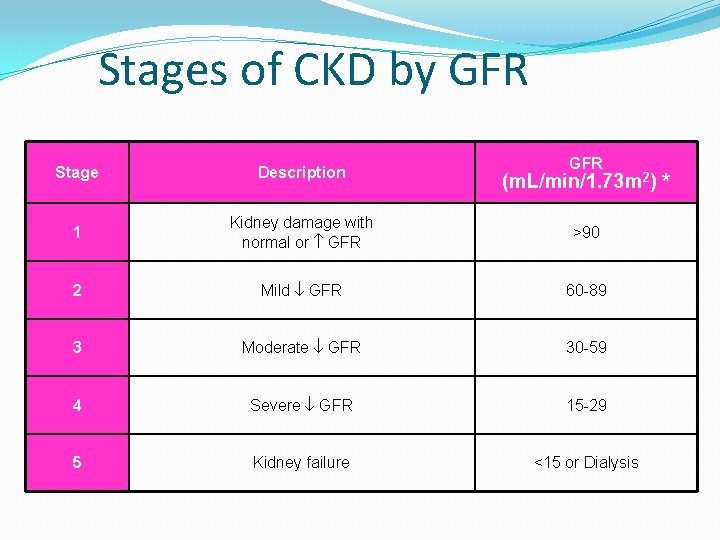
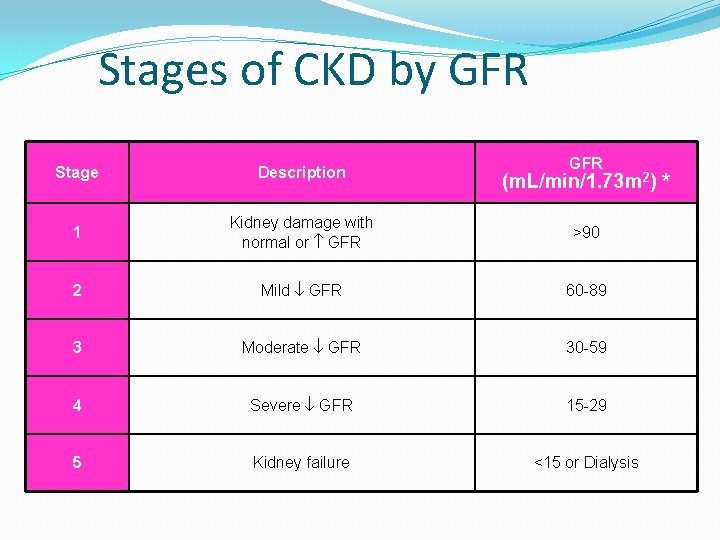
Stages of CKD by GFR Stage Description 1 Kidney damage with normal or GFR >90 2 Mild GFR 60 -89 3 Moderate GFR 30 -59 4 Severe GFR 15 -29 5 Kidney failure <15 or Dialysis (m. L/min/1. 73 m 2) *
Types of renal failure There are two different types of renal failure -acute renal failure (ARF) - chronic renal failure (ESRD)
Acute Renal Failure Acute renal failure occurs suddenly and may last a few days to a few weeks. Caused by another medical problem such as a serious burn, a crushing injury, or cardiac arrest immunologic causes etc. 35
Chronic Renal Failure Develops slowly, number of functioning nephrons constantly diminishing. Uremia is a result Symptoms: nausea, headache, coma, convulsions. Severe renal failure will result in death unless dialysis used. 36
Categories of Acute Renal Failure � prerenal (hypoperfusion of kidney), � intrarenal (actual damage to kidney tissue), �postrenal (obstruction to urine flow).
Clinical pathophysioloy �Metabolic acidosis: result in; �Muscle breakdown �Bone dissolving �Hyperkalemia �Hypertension �Negative N balance �Insulin resistance �Hyperphosphatemia �Anemia
Phases of Acute Renal Failure �There are four clinical phases of ARF: initiation, oliguria, diuresis, and recovery
�The initiation period begins with the initial insult and ends when oliguria develops. �The oliguria period is accompanied by an increase in the serum concentration of substances usually excreted by the kidneys (urea, creatinine, uric acid, organic acids, and the intracellular cations [potassium and magnesium]).
�The diuresis period is marked by a gradual increase in urine output, which signals that glomerular filtration has started to recover. Laboratory values stop increasing and eventually decrease. Although the volume of urinary output may reach normal or elevated levels, renal function may still be markedly abnormal.
Treatment Goals for Renal Failure �Correct electrolytes �Control acidosis �Treat significant hyperphosphatemia �Treat symptomatic anemia �Initiate dialysis for hyperkalemia or acidosis not controlled, fluid overload, ↑ in BUN>20 mg/dl/24 hours or BUN>100 mg/dl �Evaluate drugs for renal effect �Avoid/treat infection
Calcium �In children with CRI, both dietary Ca uptake and urinary Ca excretion are �GI Ca absorption is as a result of circulating 1, 25 hydroxy Vitamin D levels � PTH increases both bone Ca release and renal Ca reabsorption
Calcium �In severe renal failure, total urinary Ca excretion remains low and Fe. Ca �When Vitamin D is given to prevent renal osteodystrophy, hypercalcemia, hypercalciuria and decreased GFR may occur
Phosphorus �Serum phosphorus levels are maintained WNL until GFR decreases to about 25% of normal �If phosphorus intake remains high, the release of phosphate is in patients with CRI �The Fe. PO 4 �It is proposed that a decrease in renal phosphate excretion secretion of PTH
Phosphorus � PTH levels cause an increase in fractional excretion of phosphorus �The Fe. PO 4 does not depend on hyperpara, as it can occur in parathyroidectomized animals in which PTH is absent or at base-line level
Growth and Development Malnutrition �Anorexia is a major c/o (? Taste sensation altered) �When diet <80% RDA = growth retardation �Catch up growth does not catch up to peers �Calorie use less efficient in CRF ? �Intakes > 100% RDA are not desirable
Vitamins in ARF �Vitamin A: elevated vitamin A levels are known to occur with RF �Vitamin B – prevent B 6 deficiency by giving 10 mg pyridoxine hydrochloride/day �Folate and B 6: supplement when homocysteine levels are high �Vitamin C: <200 mg/day to prevent ↑ oxalate �Activated vitamin D �Vitamin K: give Vitamin K especially to pts on antibiotics that suppress gut production of K
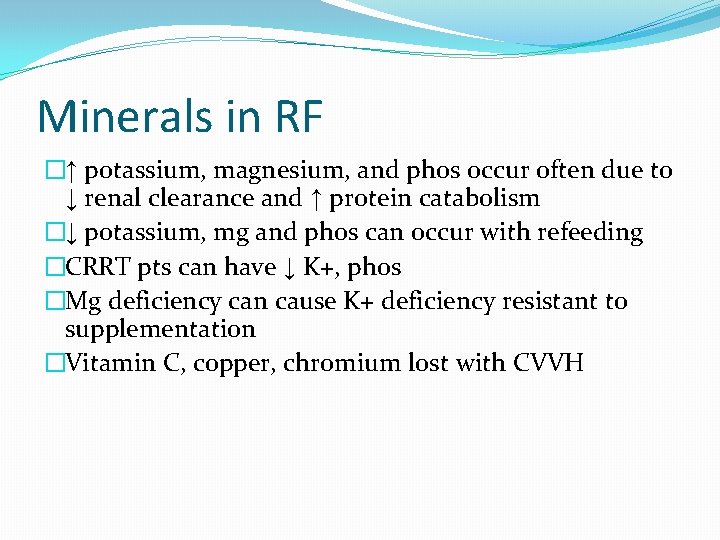
Minerals in RF �↑ potassium, magnesium, and phos occur often due to ↓ renal clearance and ↑ protein catabolism �↓ potassium, mg and phos can occur with refeeding �CRRT pts can have ↓ K+, phos �Mg deficiency can cause K+ deficiency resistant to supplementation �Vitamin C, copper, chromium lost with CVVH

52 Thank you
 Res extra commercium
Res extra commercium Teoria do nefron intacto
Teoria do nefron intacto Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries Edema lesion
Edema lesion Earthy look in chronic renal failure
Earthy look in chronic renal failure Urinalysis
Urinalysis Acute glomerulonephritis pathophysiology
Acute glomerulonephritis pathophysiology Renal failure
Renal failure Failure to capture vs failure to sense ecg
Failure to capture vs failure to sense ecg Supparerk vision center
Supparerk vision center Brittle failure vs ductile failure
Brittle failure vs ductile failure Lobule of kidney
Lobule of kidney Maintenance dose formula
Maintenance dose formula Urinary bladder histology
Urinary bladder histology Function of nephron in points
Function of nephron in points Diferença entre volume e capacidade
Diferença entre volume e capacidade Signo de empastamiento gemelar
Signo de empastamiento gemelar Tuberculosis patogenia
Tuberculosis patogenia Tratamiento para tromboembolismo pulmonar
Tratamiento para tromboembolismo pulmonar Sistema circulatorio cerrado
Sistema circulatorio cerrado Traquea
Traquea Circulação pulmonar e sistemica
Circulação pulmonar e sistemica Circulação pulmonar e sistemica
Circulação pulmonar e sistemica Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Scifosis
Scifosis Foco aortico
Foco aortico Focos cardiacos de auscultacion
Focos cardiacos de auscultacion Tbc pulmonar
Tbc pulmonar Vascularizatia toracelui
Vascularizatia toracelui Volume e capacidade pulmonar
Volume e capacidade pulmonar Veia pulmonar sangue arterial
Veia pulmonar sangue arterial Impneding
Impneding Patron de arbol en gemacion
Patron de arbol en gemacion Gangrena pulmonara
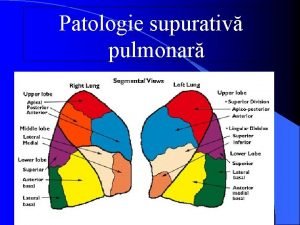
Gangrena pulmonara Etiologia de absceso pulmonar
Etiologia de absceso pulmonar Parametros gasometria
Parametros gasometria Infarto pulmonar
Infarto pulmonar Miocardio
Miocardio Htp pulmonar
Htp pulmonar Embolismo pulmonar radiografia
Embolismo pulmonar radiografia Excrecion pulmonar
Excrecion pulmonar Pseudoquilotorax
Pseudoquilotorax Presion de la circulacion pulmonar
Presion de la circulacion pulmonar Infarto pulmonar
Infarto pulmonar Displasia broncopulmonar
Displasia broncopulmonar Diafragma
Diafragma Cord pulmonar acut
Cord pulmonar acut Inhomogeneidad
Inhomogeneidad Pressão sistólica da artéria pulmonar valores normais
Pressão sistólica da artéria pulmonar valores normais Chistul hidatic pulmonar
Chistul hidatic pulmonar Complacência pulmonar calculo
Complacência pulmonar calculo