Opthalmologic Emergencies Dave Dyck R 3 Preceptor Dr
















































- Slides: 143
Opthalmologic Emergencies Dave Dyck R 3 Preceptor: Dr. Bryan Young Sept. 26/02
Objectives: • Briefly review ocular anatomy and exam • Recognize pathology (yeah – pictures!) • Discuss treatment options • Discuss areas of controversy • Slit lamp review
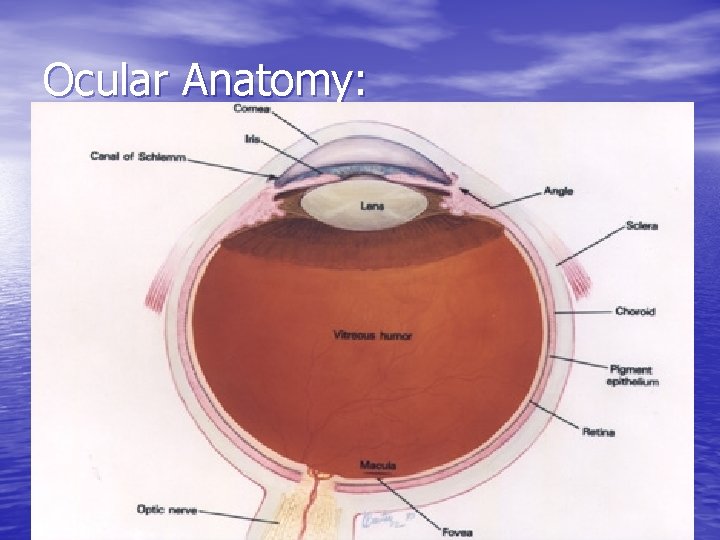
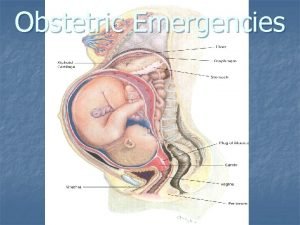
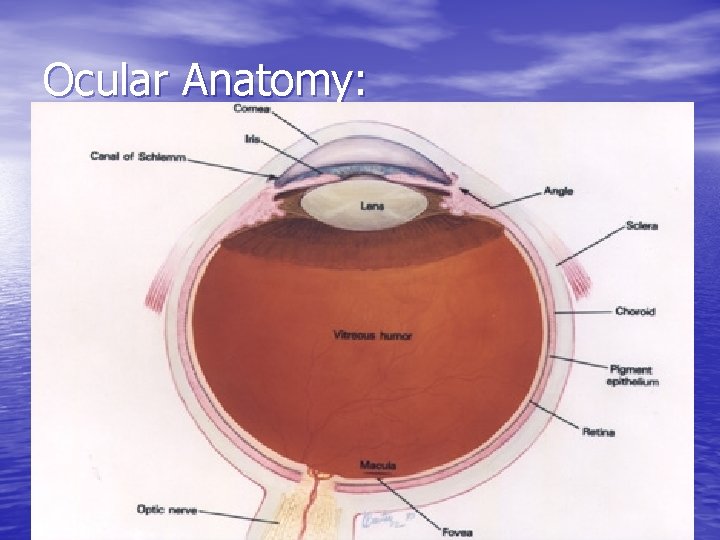
Ocular Anatomy:


Eye Exam: • Visual acuity • Pupils • Motility • Confrontation visual fields • Anterior segment • Posterior segment • Intraocular pressure
Visual Acuity: • Perform at 20 feet (6 meters) • Range from 20/15 to 20/400 then counting • • • fingers, hand movements, light perception, and no light perception Near vision uses a reading card at 14 inches OD= right eye; OS= left eye; OU= both eyes If vision< 20/20 use pinhole to check for correctable refractive errors
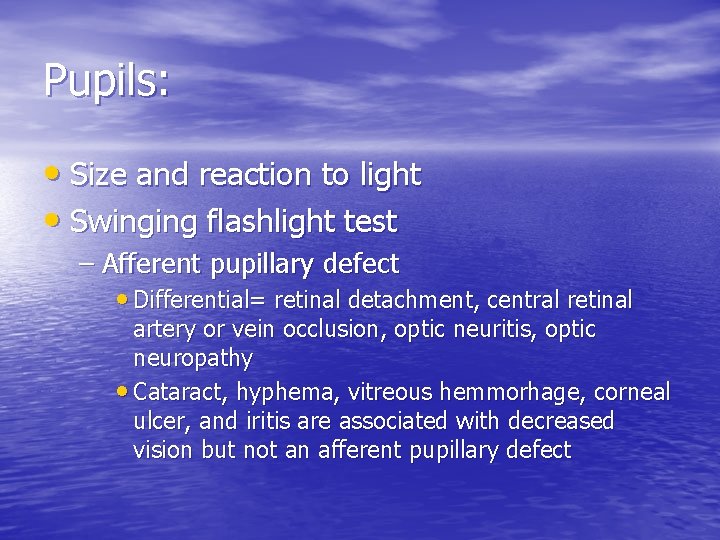
Pupils: • Size and reaction to light • Swinging flashlight test – Afferent pupillary defect • Differential= retinal detachment, central retinal artery or vein occlusion, optic neuritis, optic neuropathy • Cataract, hyphema, vitreous hemmorhage, corneal ulcer, and iritis are associated with decreased vision but not an afferent pupillary defect
Pupils cont. • Dilated – Third nerve palsy – Trauma – Adie’s pupil – Drug induced (dilating drops) – Acute glaucoma
Pupils cont. • Constricted – Drug induced – Iritis – Horner’s syndrome * Anisocoria >4 mm seen in 19% of normals
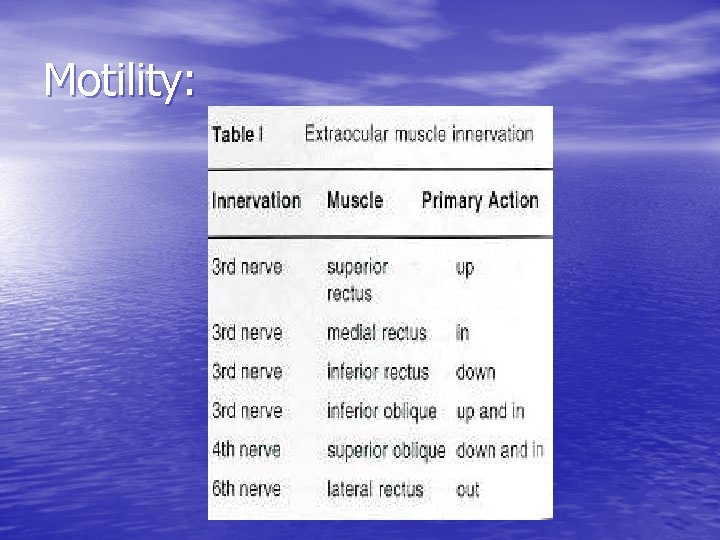
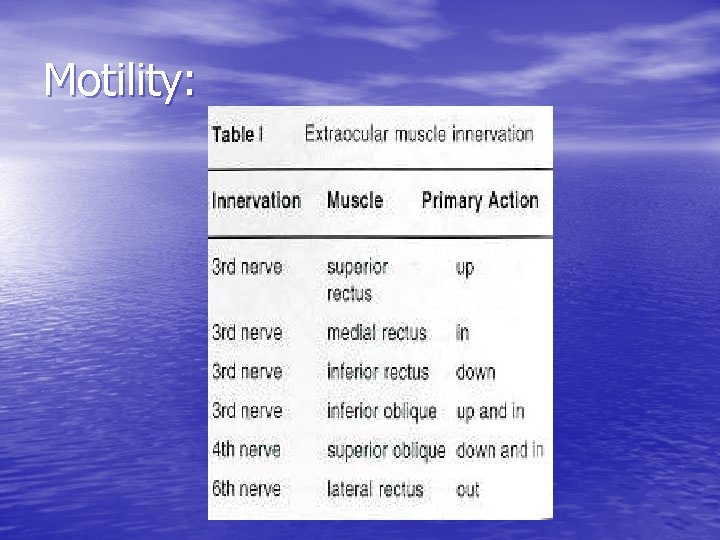
Motility:
Confrontation Visual Fields: To help localize lesions to the retina, optic nerve, optic chiasm, or visual cortex
Anterior Segment: • Lids, puncta, conjunctiva, sclera, cornea, anterior chamber, and lens • Fluorescein – Remove contact lenses

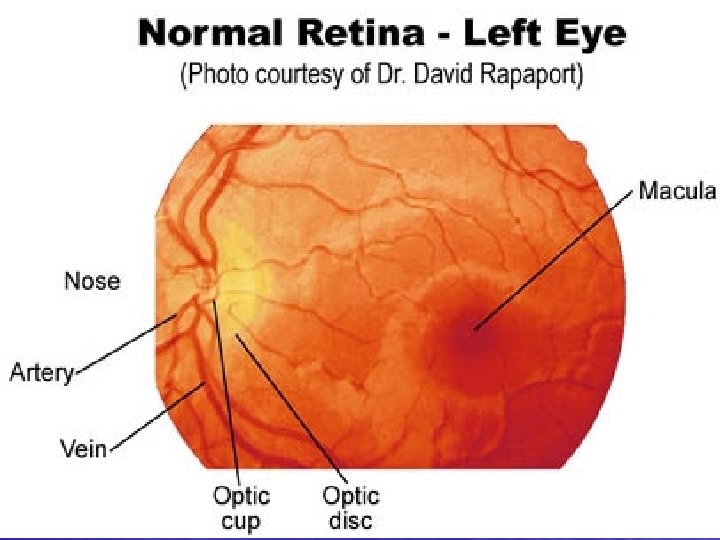
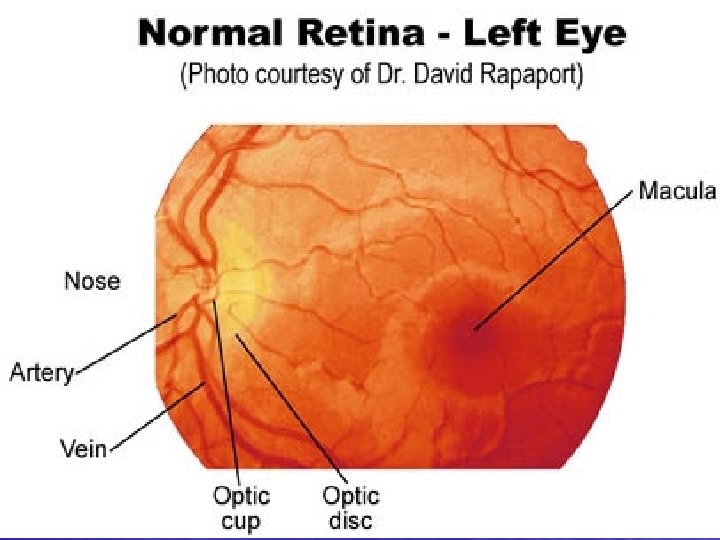
Posterior Segment: • Vitreous, disc, vessels, macula, and peripheral retina • Through dilated pupil UNLESS shallow anterior chamber (or hx of angle closure glaucoma), iris supported intraocular lens (rare), head injury, ruptured globe
Optic Disc: • Normally slightly oval in the vertical meridian, central depression (cup), various pigmentation • Cup-to-disc ratio <0. 5 • Distinct disc margins
Intraocular Pressure: • Normal < 23 mm. Hg. • Acute angle glaucoma often > 40 mm. Hg. • Tonopen- easy • Schiotz tonometry (Roberts) • Applanation tonometry • Air-puff tonometry
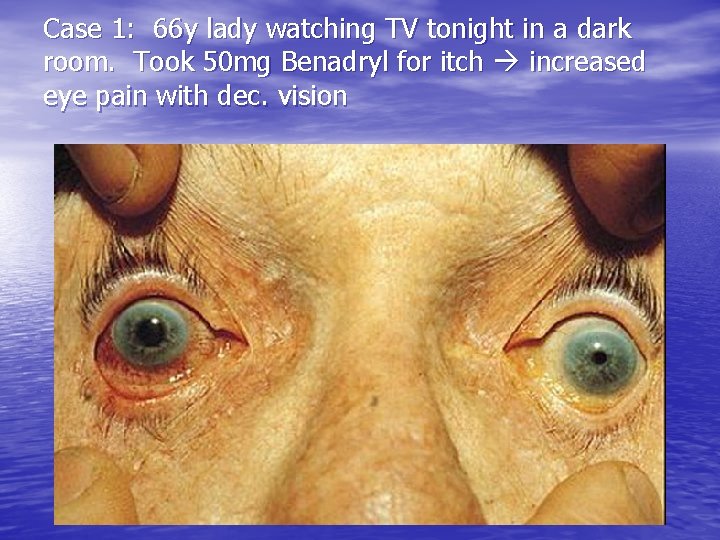
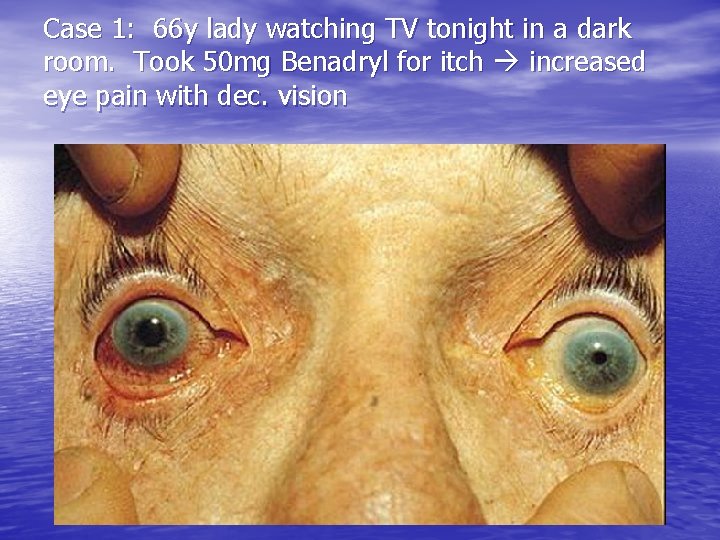
Case 1: 66 y lady watching TV tonight in a dark room. Took 50 mg Benadryl for itch increased eye pain with dec. vision

Glaucoma: • Imbalance of aqueous humor production and drainage leading to increased intraocular pressure optic neuropathy
Types: • Primary angle closure glaucoma • Secondary angle closure glaucoma • Primary open angle glaucoma • Secondary open angle glaucoma
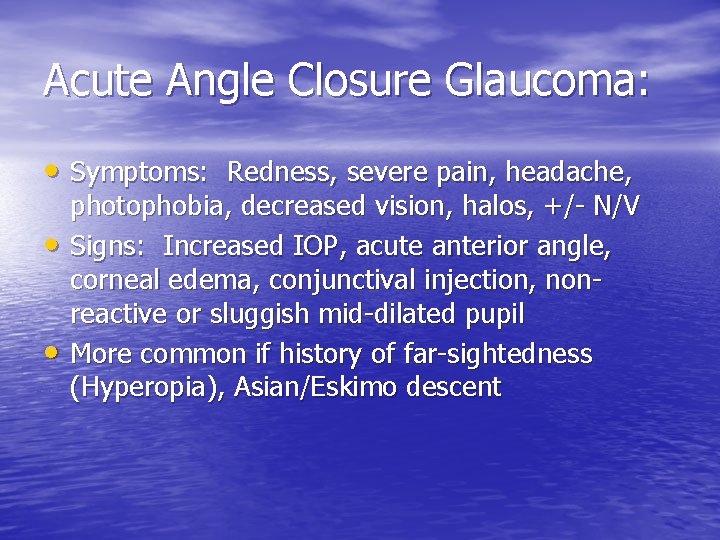
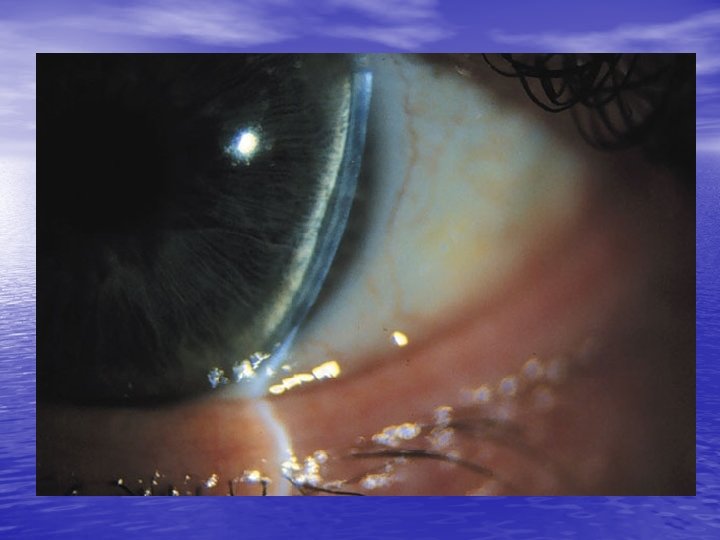
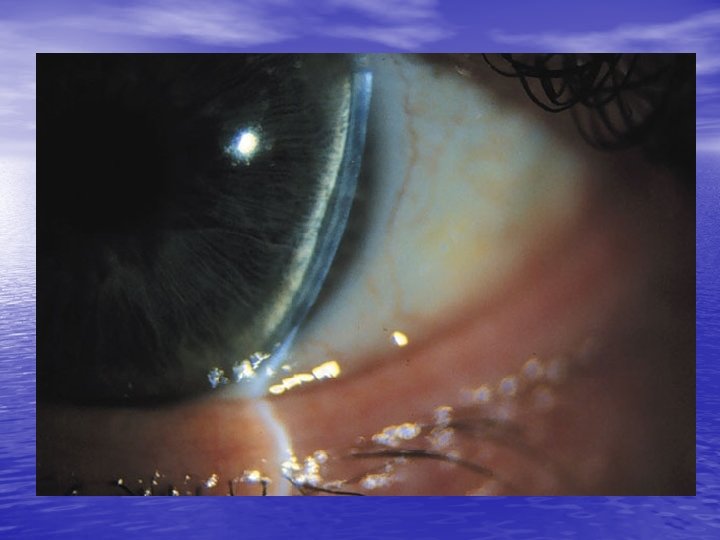
Acute Angle Closure Glaucoma: • Symptoms: Redness, severe pain, headache, • • photophobia, decreased vision, halos, +/- N/V Signs: Increased IOP, acute anterior angle, corneal edema, conjunctival injection, nonreactive or sluggish mid-dilated pupil More common if history of far-sightedness (Hyperopia), Asian/Eskimo descent
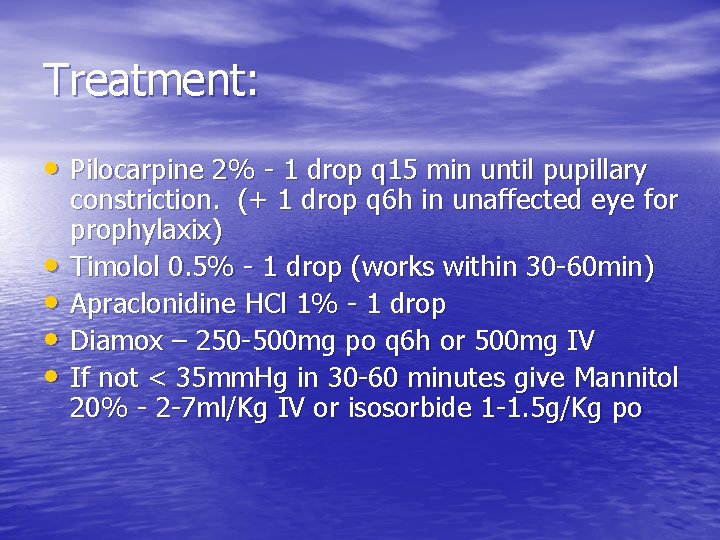
Treatment: • Pilocarpine 2% - 1 drop q 15 min until pupillary • • constriction. (+ 1 drop q 6 h in unaffected eye for prophylaxix) Timolol 0. 5% - 1 drop (works within 30 -60 min) Apraclonidine HCl 1% - 1 drop Diamox – 250 -500 mg po q 6 h or 500 mg IV If not < 35 mm. Hg in 30 -60 minutes give Mannitol 20% - 2 -7 ml/Kg IV or isosorbide 1 -1. 5 g/Kg po
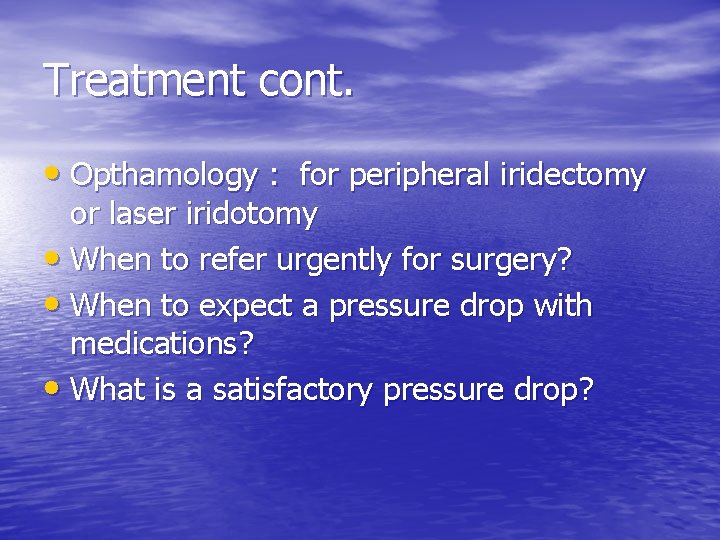
Treatment cont. • Opthamology : for peripheral iridectomy or laser iridotomy • When to refer urgently for surgery? • When to expect a pressure drop with medications? • What is a satisfactory pressure drop?
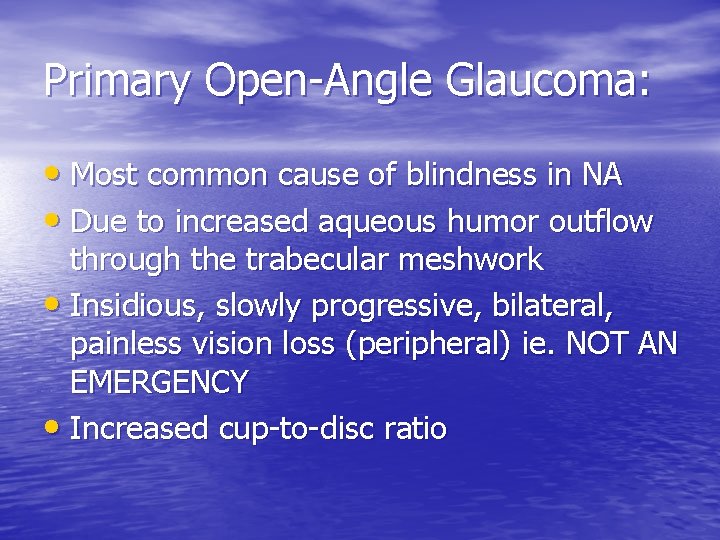
Primary Open-Angle Glaucoma: • Most common cause of blindness in NA • Due to increased aqueous humor outflow through the trabecular meshwork • Insidious, slowly progressive, bilateral, painless vision loss (peripheral) ie. NOT AN EMERGENCY • Increased cup-to-disc ratio


Fundoscopic lesions:
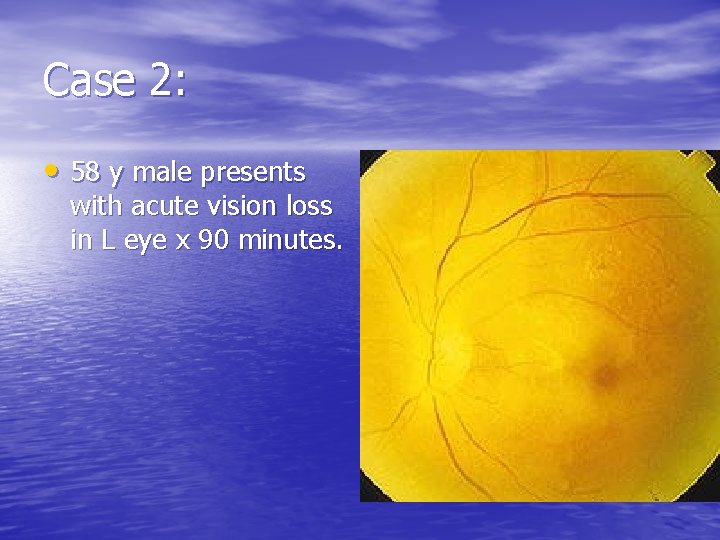
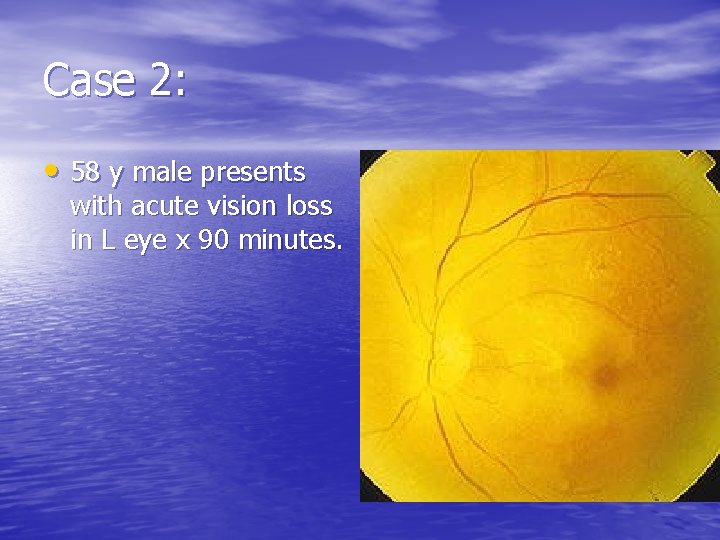
Case 2: • 58 y male presents with acute vision loss in L eye x 90 minutes.

Central Retinal Artery Occlusion: • Painless, ages 50 -70, vasculopathic hx • R/O glaucoma • Signs= Decreased visual acuity, afferent pupillary defect, pale fundus with cherryred fovea • Experimentally, 100 min until irreversible ischemia
Treatment: • Digital global massage (5 sec on – 5 sec off) • Increase PCO 2 by breathing into paper bag for 10 min every hour vs Carbogen • IV acetozolamide + ASA • R/O and Treat glaucoma • Emergent Opthamology referral and outpatient Cardiology • R/O neuritis 2% (ESR, hx, etc)
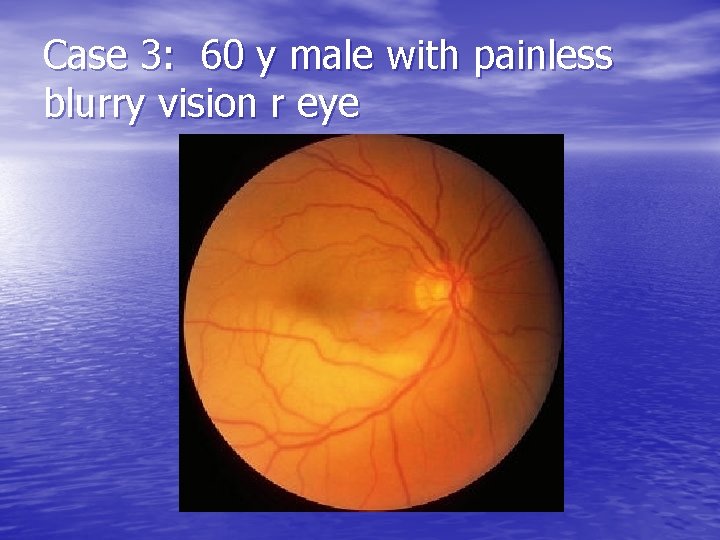
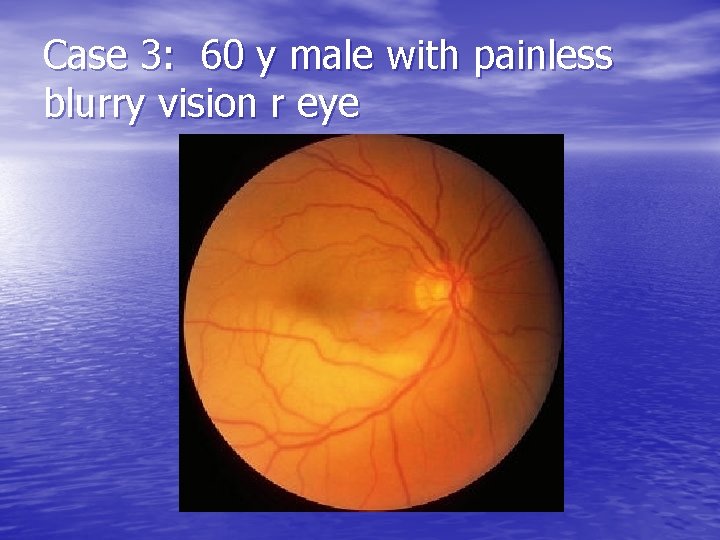
Case 3: 60 y male with painless blurry vision r eye

Branch Retinal Artery Occlusion: • Same treatment as for CRAO

Case 4: • 60 y female with vision loss L eye

Central/Branch Retinal Vein Occlusion: • Symptoms: variable vision loss, usually painless • Signs: ischemic (neovascular glaucoma) or non-ischemic (macular edema with leaking capillaries) Dilated tortuous veins, retinal hemmorhages and disc edema
Treatment: • Expectant • Referral to Opthomology within 24 hrs to R/O neovascular glaucoma
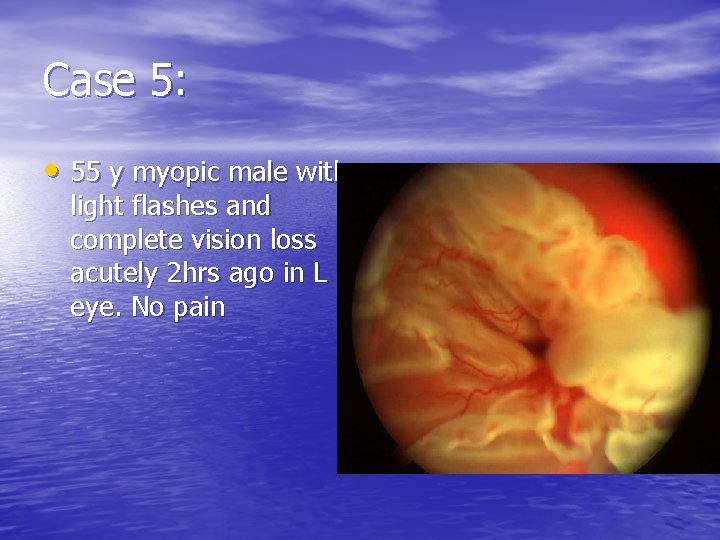
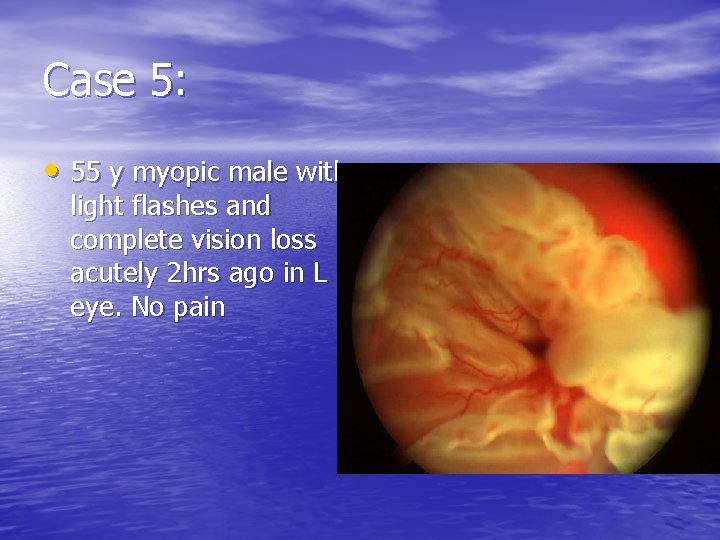
Case 5: • 55 y myopic male with light flashes and complete vision loss acutely 2 hrs ago in L eye. No pain
Retinal Detachment: • Separation of the inner neuronal retina layer from the outer retinal pigment epithelial layer • 3 types: – i. rhegmatogenous – ii. Exudative – iii. Tractional
Rhegmatogenous: • Due to tear/hole in the neuronal layer causing vitreous fluid to enter and separate the 2 retinal layers • Often due to vitreous gel pulling on retina as one ages or related to trauma • Men, myopia, age>45
Exudative: • From blood/fluid leakage from vessels within the retina • HT, eclampsia, CRVO, papilledema, vasculitis, choroid tumor
Tractional: • Due to fibrous band formation in the vitreous and the contraction of these bands

Retinal Detachment: • Symptoms: light flashes, floaters, variable vision loss depending on macular involvement (cloudy or curtainlike), painless • Signs: area out of focus on fundoscopy • Cannot be ruled out by direct fundoscopy

Treatment: • Emergent opthamologic consultation • When?
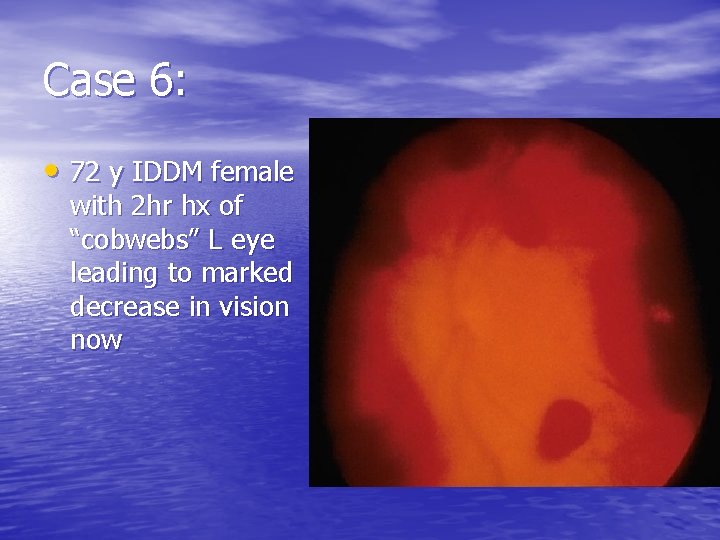
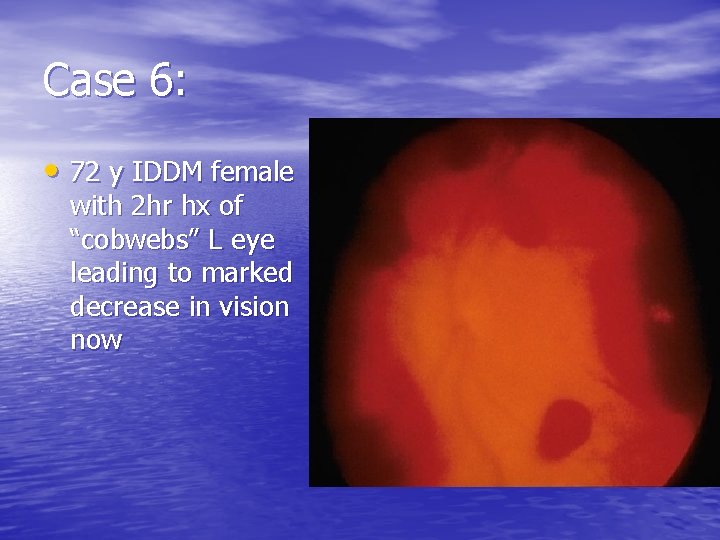
Case 6: • 72 y IDDM female with 2 hr hx of “cobwebs” L eye leading to marked decrease in vision now
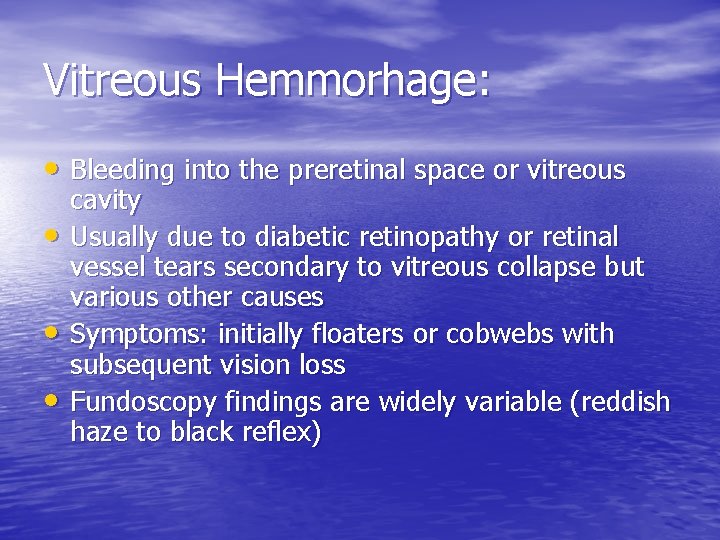
Vitreous Hemmorhage: • Bleeding into the preretinal space or vitreous • • • cavity Usually due to diabetic retinopathy or retinal vessel tears secondary to vitreous collapse but various other causes Symptoms: initially floaters or cobwebs with subsequent vision loss Fundoscopy findings are widely variable (reddish haze to black reflex)
Vitreous hemmorhage: • If afferent pupillary defect present retinal detachment likely behind hemmorhage • Treatment: bedrest, elevate HOB, avoid ASA and refer to opthomology

Case 7: • 75 y male with progressive vision loss x years with acute worsening central vision today. No pain.
Macular Hemmorhage: • Refer to opthomology
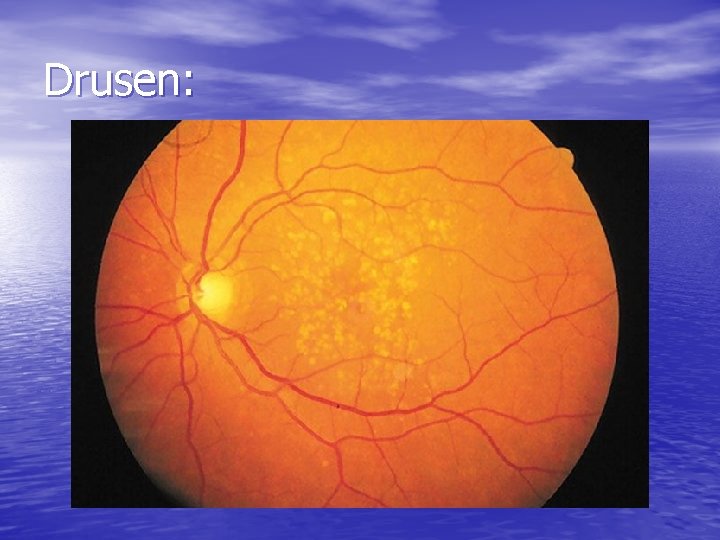
Macular Disorders: • Loss of central vision with preservation of • • peripheral vision, central vision distortion, abnormal retinal changes at macula Due to trauma, radiation, inflammation, vascular disease, toxins, genetics, idiopathic Drusen Neovascularization *no afferent defect and optic nerve normal
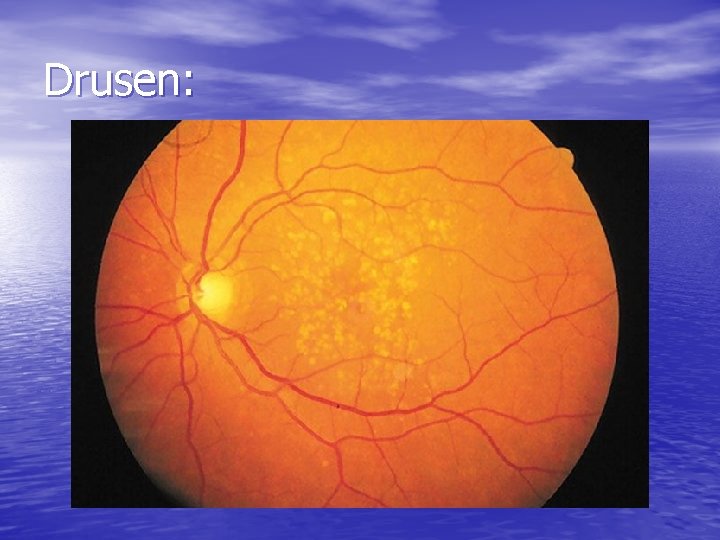
Drusen:

Macular Star:
ER role: • Recognition primarily and referral to opthamology for fluorescein angiogram within 24 -48 hrs
Non-Penetrating Ocular Trauma: • Orbit and globe • Cornea and conjunctiva • Anterior chamber and iris • Lens • Posterior Segment
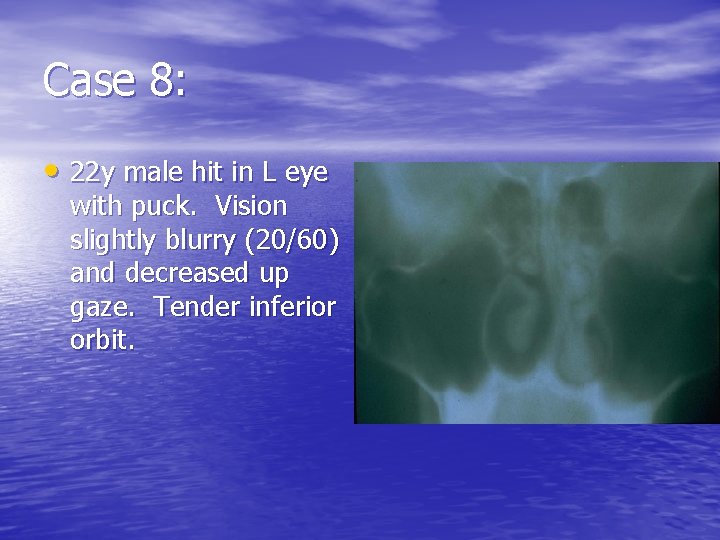
Case 8: • 22 y male hit in L eye with puck. Vision slightly blurry (20/60) and decreased up gaze. Tender inferior orbit.

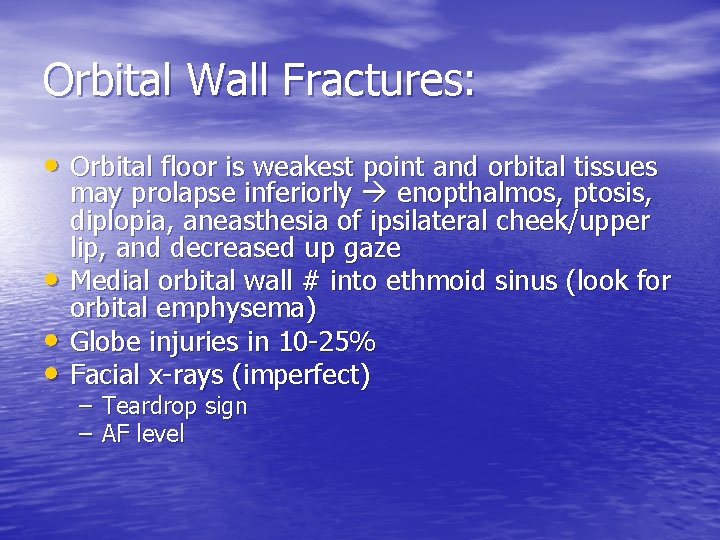
Orbital Wall Fractures: • Orbital floor is weakest point and orbital tissues • • • may prolapse inferiorly enopthalmos, ptosis, diplopia, aneasthesia of ipsilateral cheek/upper lip, and decreased up gaze Medial orbital wall # into ethmoid sinus (look for orbital emphysema) Globe injuries in 10 -25% Facial x-rays (imperfect) – Teardrop sign – AF level
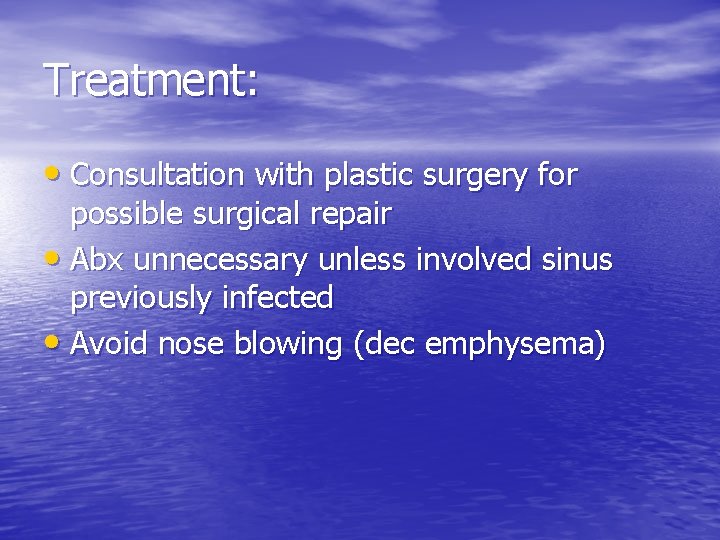
Treatment: • Consultation with plastic surgery for possible surgical repair • Abx unnecessary unless involved sinus previously infected • Avoid nose blowing (dec emphysema)
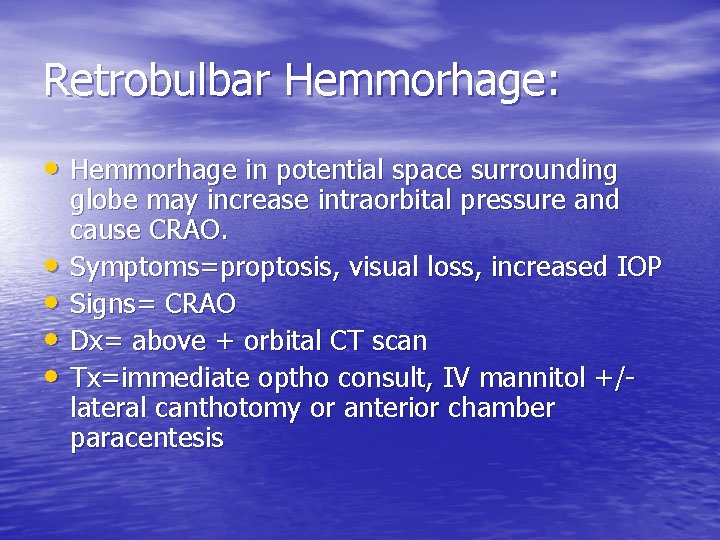
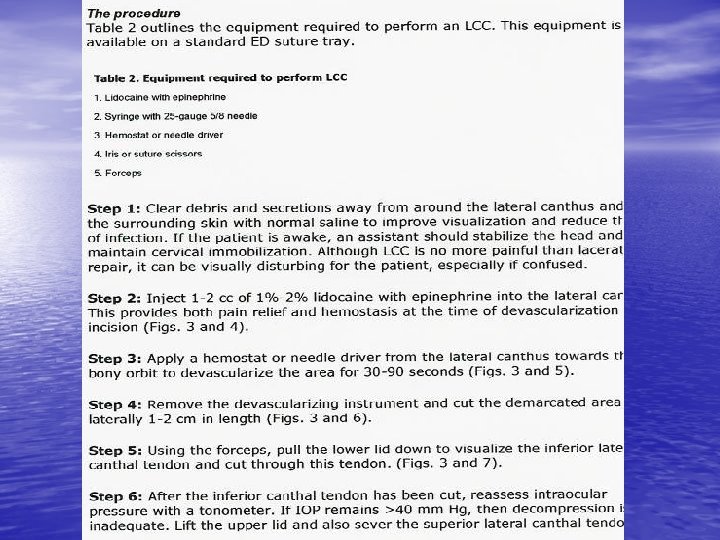
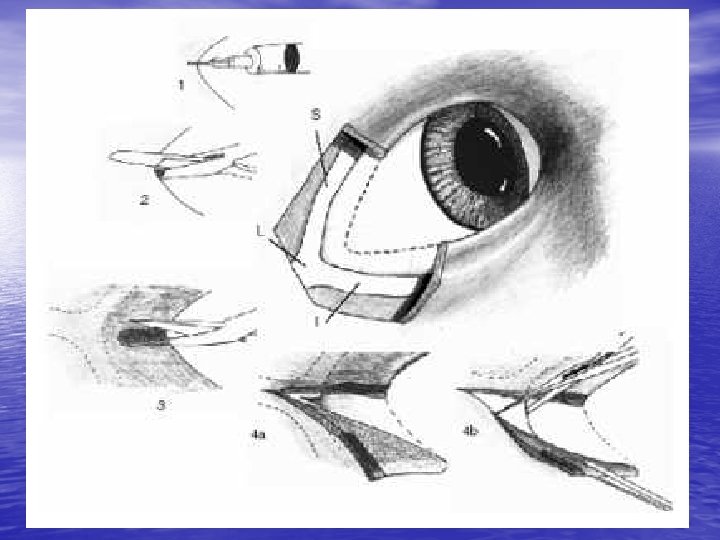
Retrobulbar Hemmorhage: • Hemmorhage in potential space surrounding • • globe may increase intraorbital pressure and cause CRAO. Symptoms=proptosis, visual loss, increased IOP Signs= CRAO Dx= above + orbital CT scan Tx=immediate optho consult, IV mannitol +/lateral canthotomy or anterior chamber paracentesis


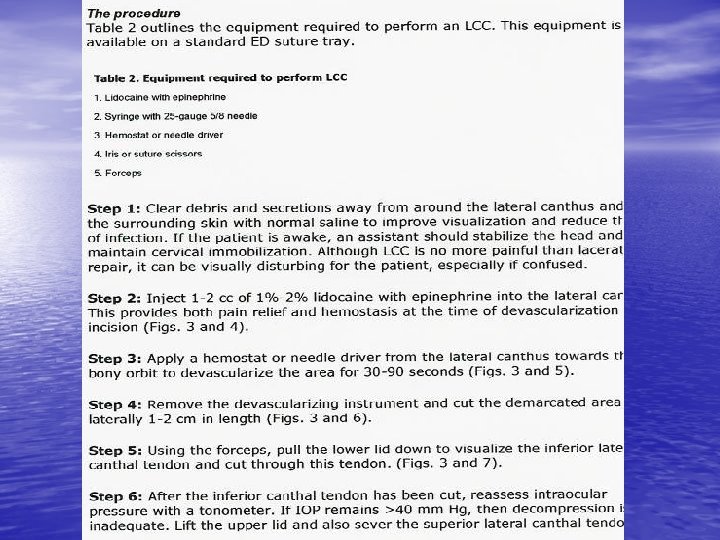





Complications: • Infection, hemmorhage, injury to globe • Rare • Canthotomy wounds heal well without suturing or significant scarring

Case 9: 22 y male in MVA
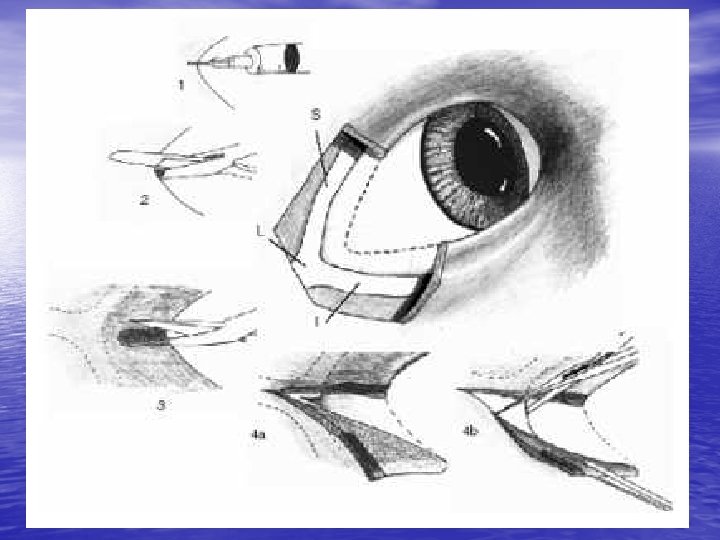
Globe Rupture: • Most common at EOM insertions into sclera or at limbus • Pain and decreased vision • Examination: various = teardrop pupil (iris plugging limbal hole), distortion of anterior chamber, others
Diagnosis: • Hx/Px +/- CT or U/S • Fluorescein • Avoid tonometry
Treatment: • Protective shield, avoid manipulation, NPO, tetanus, IV Abx, urgent opthalmology • Avoid succ or use defasciculator if must use it
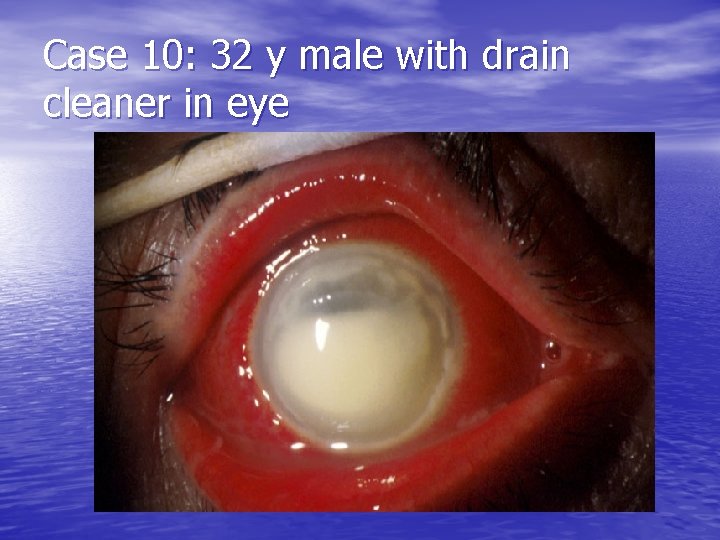
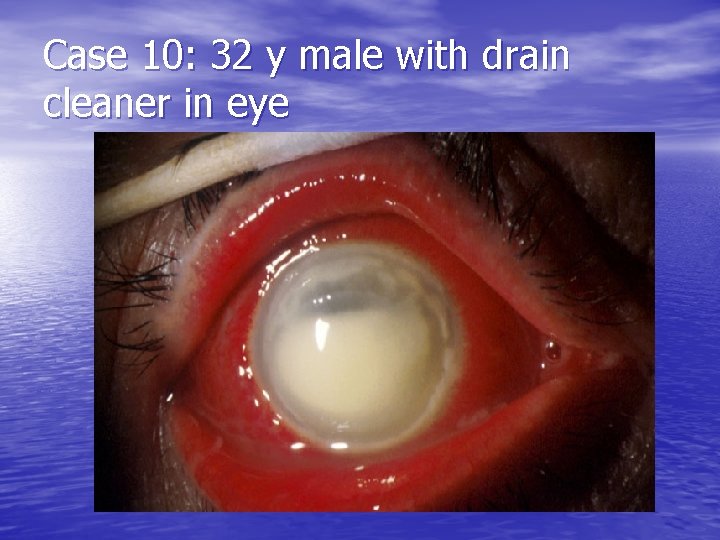
Case 10: 32 y male with drain cleaner in eye
Alkali burns: • Liquefaction necrosis • Severe injury= (severity judged by degree of corneal whitening)

Treatment: • Prehospital- copious irrigation with clean water x 15 min prior to transport. Bring in chemical • Hospital- topical anaesthesia, lid retraction and 2 L continuous irrigation NS. Continue until p. H=7. 4 -7. 6. Remove foreign bodies. Urgent optho consult.
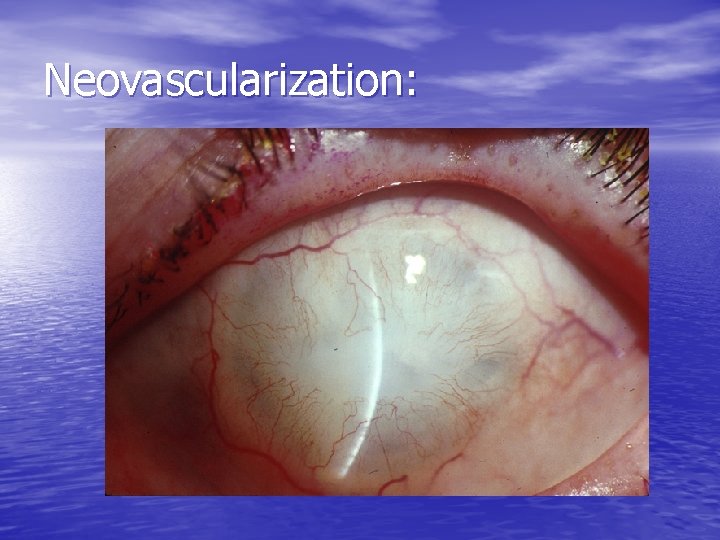
Complications: • Perforation, scarring and corneal neovascularization. Lid adhesions, glaucoma, cataracts, and retinal damage
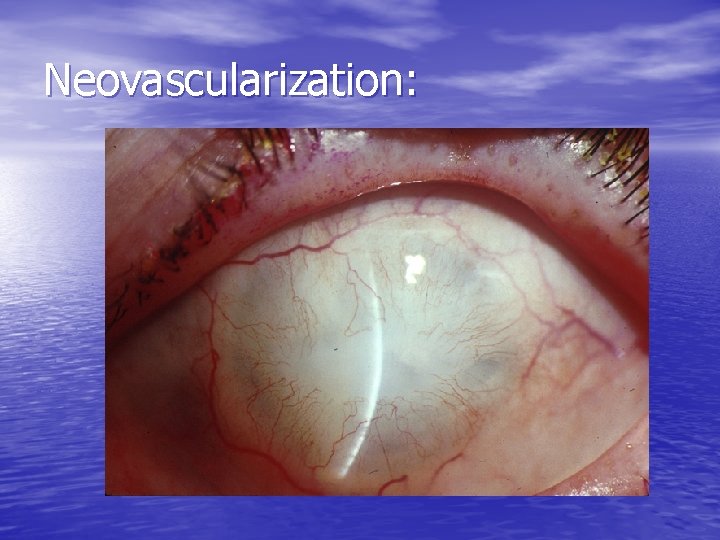
Neovascularization:

Acid burns: • Less devastating • Coagulation necrosis precipitates tissue proteins to limit depth of injury • If p. H>2 usually min damage unless very high concentration or long duration of exposure • Treatment as for alkali burns
Miscellaneous exposures: • Treat as if acid/alkali • Superglue= If eyelids sealed shut in normal position leave alone. If eyelids in abnormal position may require surgery. Optho should see both in consultation
Thermal Burns: • Eyelid usually worse than globe • If superficial treat with irrigation and Abx ointment. If deeper as above + involve optho
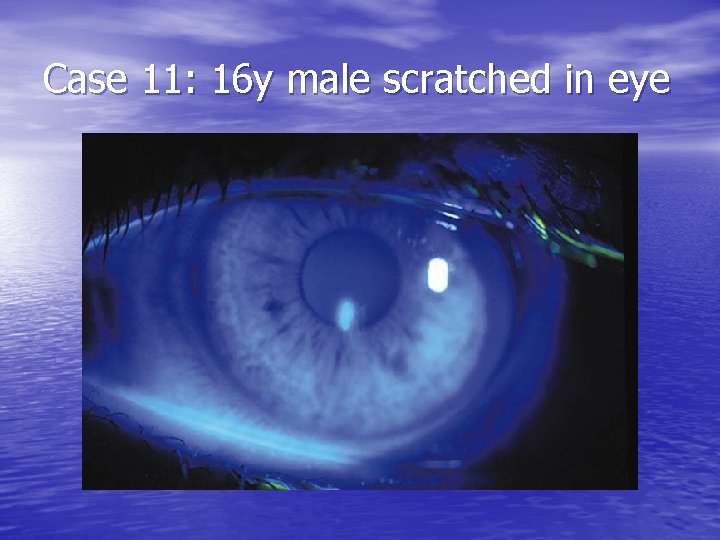
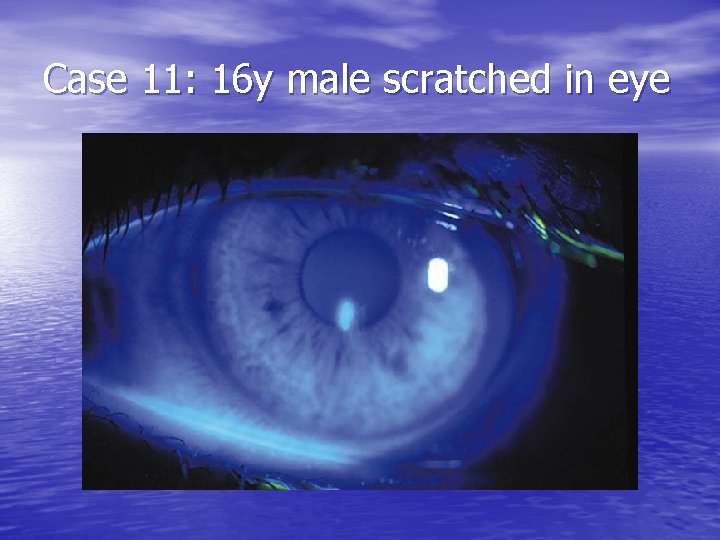
Case 11: 16 y male scratched in eye
Corneal Abrasion: • Symptoms: pain, photophobia, foreign body sensation, dec vision. • Signs: injected conjunctiva, fluorescein defect

Treatment: • R/O foreign body and herpes keratitis (evert lids, • • • use slit lamp) Refer immed if pain not relieved with top anaesthetics or if large abrasion esp if in central field of vision Cycloplegics (cyclogyl 1%) Abx drops (sulfacetamide 10%, polytrim, ocuflox, etc) Patch vs no patch (Kaiser 1995; Hart 1997; Patterson 1996) If no patch give topical NSAID for pain control eg ketorolac 0. 5% QIDx 3 d

Contact lens related abrasions: -remove contact lens -gram neg coverage (gentamycin, ocuflox) -cycloplegic -don’t patch -may require opth follow-up so that a corneal ulcer doesn’t develop
Follow-up: • Bring back in 24 hrs or not? • Optho follow-up?
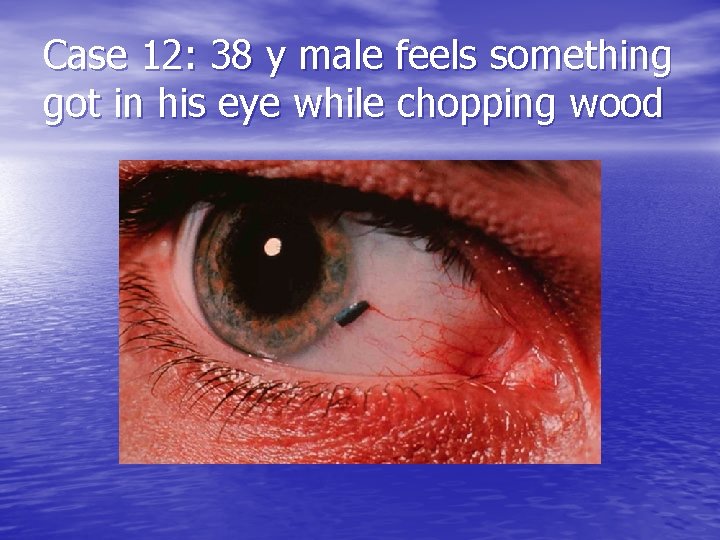
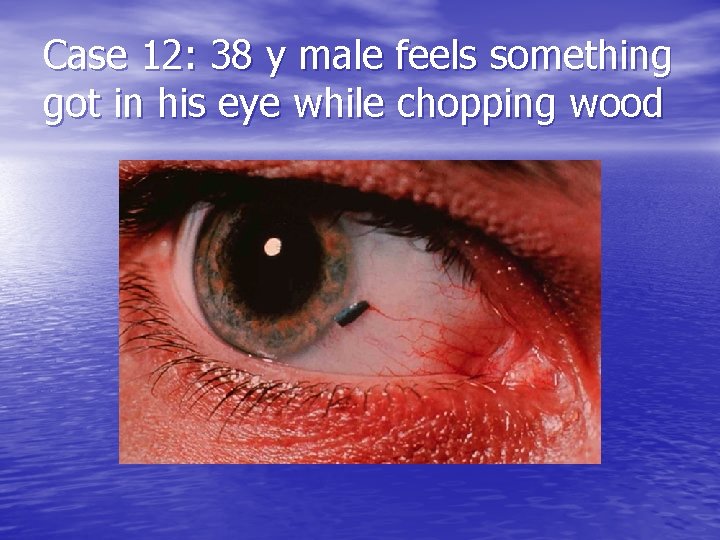
Case 12: 38 y male feels something got in his eye while chopping wood
Corneal foreign body: • Dx. =topical aneasthetic and slit lamp exam • r/o intraocular foreign body • Treatment= irrigation or needle removal (25 guage) and then as for abrasion • Rust ring removal
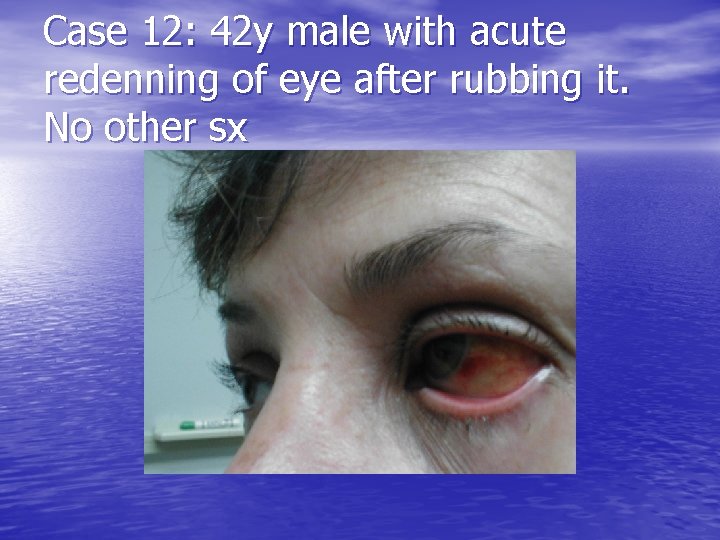
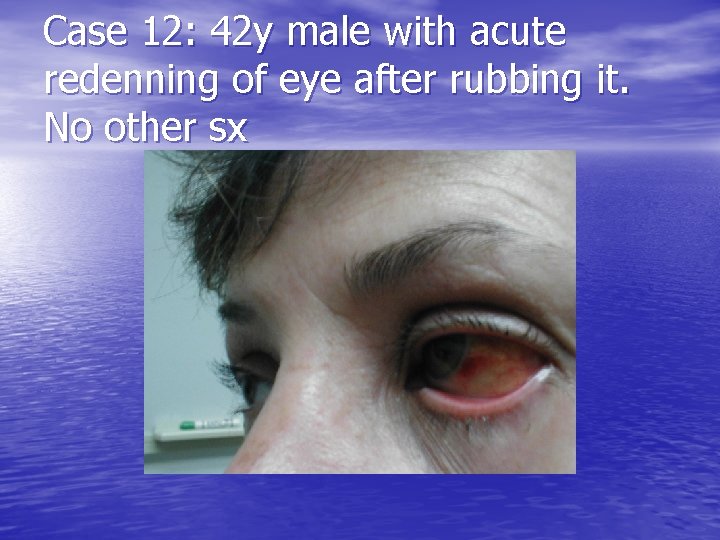
Case 12: 42 y male with acute redenning of eye after rubbing it. No other sx

Subconjunctival Hemmorhage: • Treatment= reassurance, cool compresses • Resolves in 2 -3 weeks
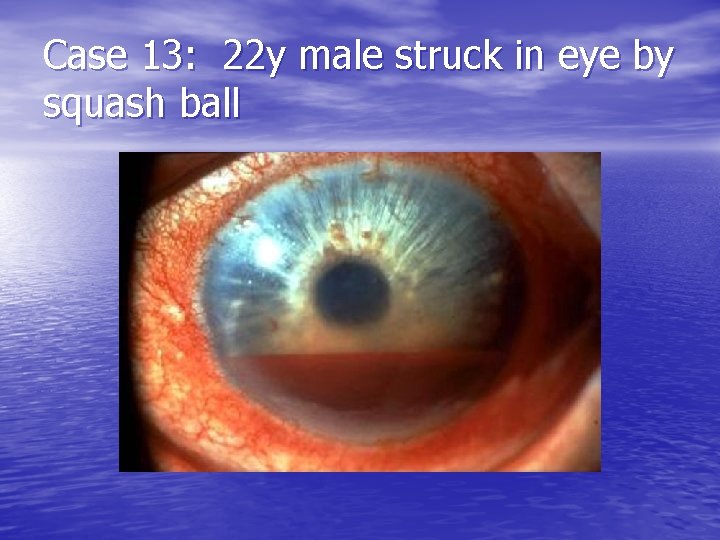
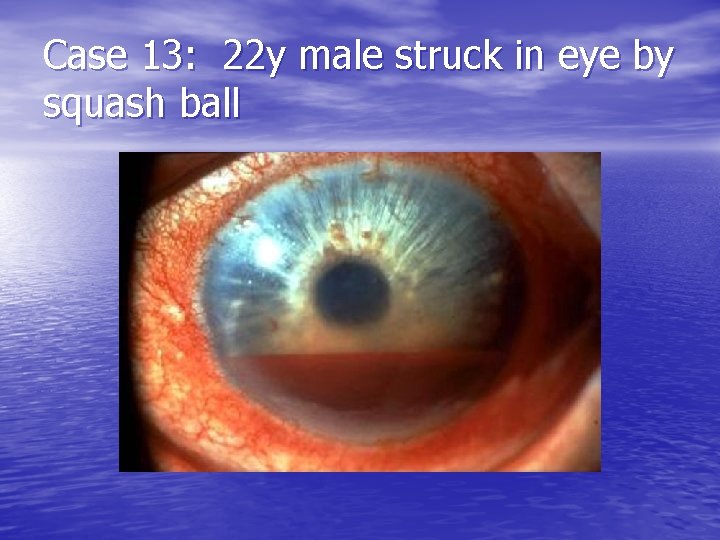
Case 13: 22 y male struck in eye by squash ball
Hyphema: • Blood in anterior chamber • Due to disruption of blood vessels in the iris or • • ciliary body (trauma or spontaneous) Typically lasts 4 -6 days if uncomplicated Classification: – – Grade 1 = less than 1/3 of ant chamber filled (72%) Grade 2 = 1/3 to ½ (20%) Grade 3 = greater than ½ (5%) Grade 4 = complete filling of ant chamber (3%) v “eight ball hyphema”
Complications • Glaucoma 1/3 (esp if Sickle Cell Anemia) • Rebleeding 4 -38% usually at 2 -5 days • Corneal staining 2 -5%
Management: • Document VA, pupils, IOP, aff pupillary defect (eight ball) • Slit lamp and complete eye exam to r/o other injuries
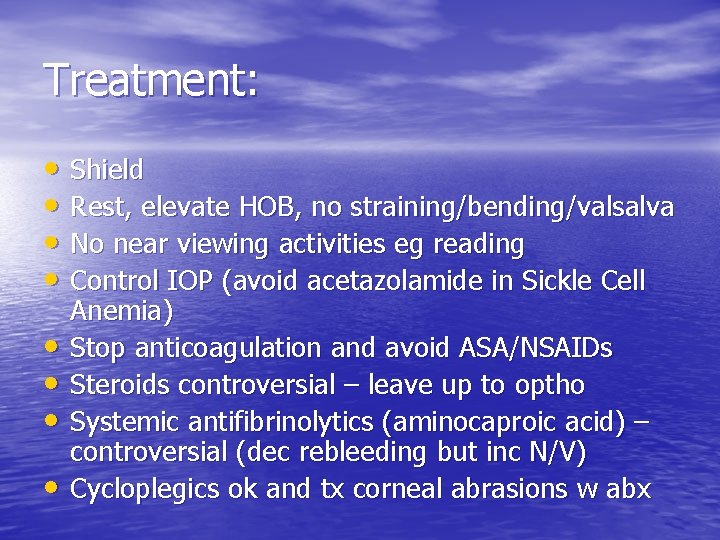
Treatment: • Shield • Rest, elevate HOB, no straining/bending/valsalva • No near viewing activities eg reading • Control IOP (avoid acetazolamide in Sickle Cell • • Anemia) Stop anticoagulation and avoid ASA/NSAIDs Steroids controversial – leave up to optho Systemic antifibrinolytics (aminocaproic acid) – controversial (dec rebleeding but inc N/V) Cycloplegics ok and tx corneal abrasions w abx
Treatment: • To admit or not? – No answer in literature – Growing opinion to allow grade 1 -11 hyphemas with controlled IOP to be treated at home with close optho follow-up daily
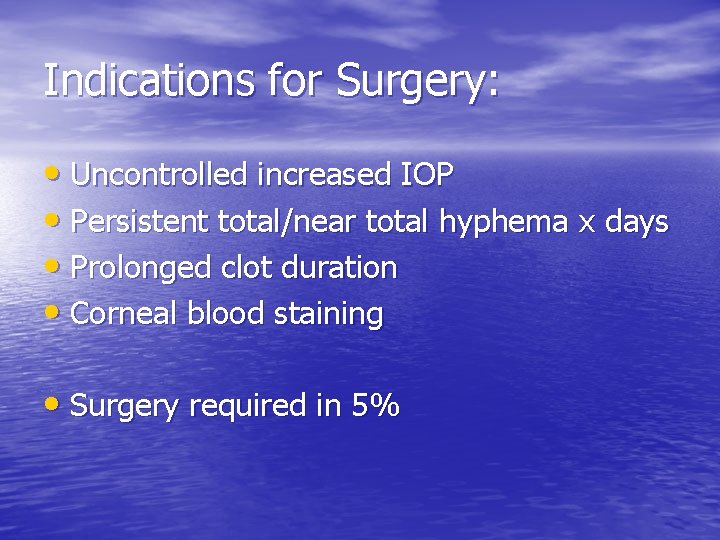
Indications for Surgery: • Uncontrolled increased IOP • Persistent total/near total hyphema x days • Prolonged clot duration • Corneal blood staining • Surgery required in 5%
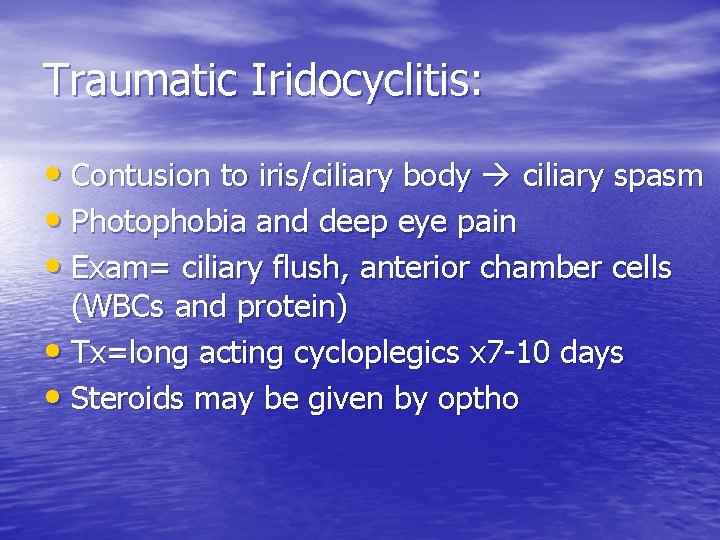
Traumatic Iridocyclitis: • Contusion to iris/ciliary body ciliary spasm • Photophobia and deep eye pain • Exam= ciliary flush, anterior chamber cells (WBCs and protein) • Tx=long acting cycloplegics x 7 -10 days • Steroids may be given by optho
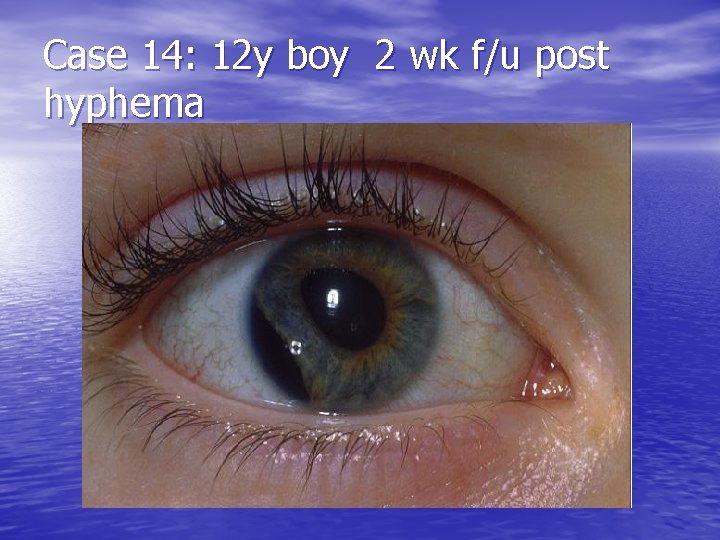
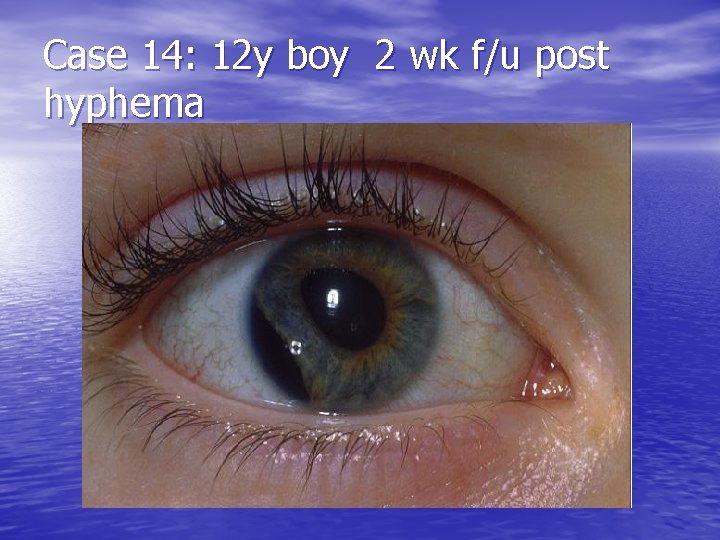
Case 14: 12 y boy 2 wk f/u post hyphema

Iridodialysis: • Tearing of the iris root from the ciliary body • ED tx- only if hyphema present • May require non-urgent surgical correction

Case 16: Tall thin 32 y male presents with diplopic vision L eye after minor eye trauma
Lens subluxation/dislocation: • Due to trauma, Marfan’s, homocystinuria, and tertiary syphilis • Tx. = optho referral

Anterior chamber lens dislocation:

Penetrating Trauma:

Case 17: 18 y male hit in eye by TV remote
Lid lacerations: • What can ED do? – Simple horizontal and oblique partial thickness lacerations

Complex lid lacerations needing referral (24 hrs): • Lid margins • Canalicular system involvement (medial lower eyelid) • Levator or canthal tendon involvement • Lacs with tissue loss
Conjunctival, Corneal, Scleral lacerations and punctures: • Conjunctival lac: small, superficial no suturing, topical abx. O/W optho • Corneal lac: Dx. = fluorescein flow. Tx as for globe rupture. • Scleral lac: Dx and Tx as for globe rupture

Case 17:
Orbital and Intraocular Foreign Body: • May have normal physical exam. Therefore high index of suspicion is crucial. • Low threshold for plain orbital plain films or orbital CT scan if non radioopaque substance • Tx=optho

Case 18: 70 y male 3 days post L cataract surgery. Increased pain and dec. vision.
Endophthalmitis: • Infection involving the deep structures of the eye • Tx=early diagnosis, IV abx (Vanco + 3 rd gen antipseudomonal ceph. +/- clinda), prompt optho referral for intravitreal abx, vitreous tap/vitrectomy, and possible steroids.
Non-traumatic red eye (other than glaucoma)
Conjuncitivitis key points: • Bilateral findings less likely bacterial • Gonococcus only bacterial conjunctivitis with a preauricular node • Always fluorescein eyes to r/o herpes lesions • Never prescribe steroids from ER

Treatments: • Allergic: cool compresses, remove allergens, • • meds Viral (non-herpetic): cool compresses, reassurance, some advocate for prophylactic abx (adenovirus may take 3 weeks to resolve) Bacterial: warm compresses, Na Sulamyd, tobramycin, polymyxin, or erythro (chloramphenical); if o/w healthy avoid topical fluoroquinolones. Culture if non responders. (gonococcus systemic tx, ocular lavage, topical erythro, notification).
Treatment cont. • No evidence comparing one abx to another, but good evidence that abx ameliorate symptoms faster than placebo. (Sheikh & Hurwitz, 2001)

Case 19:
Herpetic keratoconjunctivitis: • Tx. = trifluridine 1% 8 x/day, acyclovir 400 mg 5 x/day (no clinically significant evidence), new topical acyclovir ointment 5 x/day

Case 20:
Herpes Zoster Opthalmica: • PO acyclovir 600 -800 mg 5 x/day or famcyclovir 500 mg po tid. • Start within 72 hrs • +/- po prednisone under guidance of opthamology
Disorders of Lids and Ocular Soft Tissues:

Case 21:
Hordeolum: • Localized, nodular acute infection of an eyelid (staph aureus most common) • Can point to either skin or conjunctival side • Tx=warm compresses 4 -6 x/day, topical abx. I&D if large

Case 22:

Chalazion: • Chronic inflammatory process develops after incomplete resolution of a meibomian gland • Conjunctival or skin side • Non-tender • Tx as for hordeolum (most resolve on own) Sx if still present x 3 -4 wks

Case 23:
Dacrocystitis: • Acute infection of lacrimal sac from Nasolacrimal obstruction • Staph aur. • May express pus from puncta • Tx. Po abx and hot compresses, massage
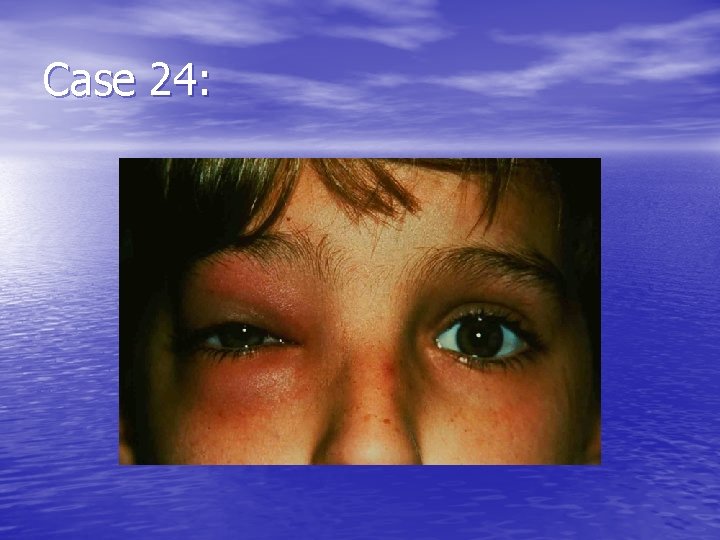
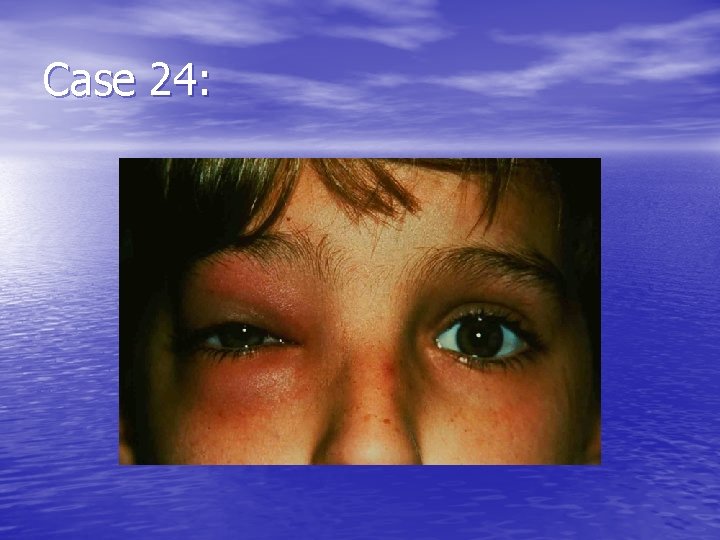
Case 24:
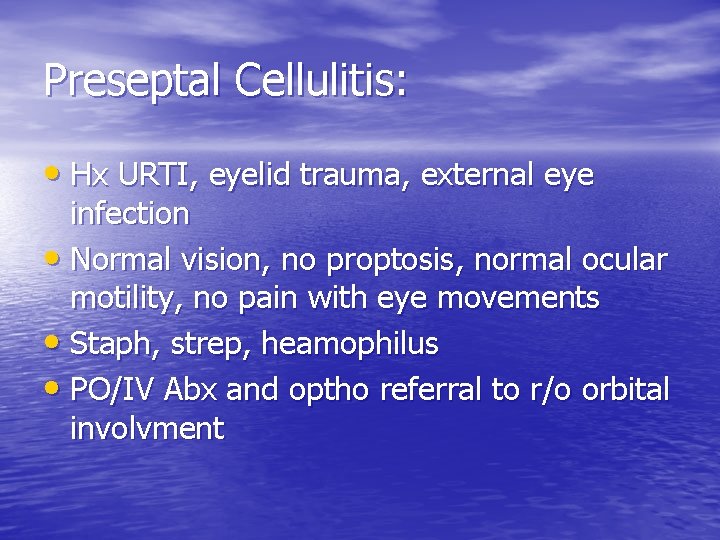
Preseptal Cellulitis: • Hx URTI, eyelid trauma, external eye infection • Normal vision, no proptosis, normal ocular motility, no pain with eye movements • Staph, strep, heamophilus • PO/IV Abx and optho referral to r/o orbital involvment

Case 25:
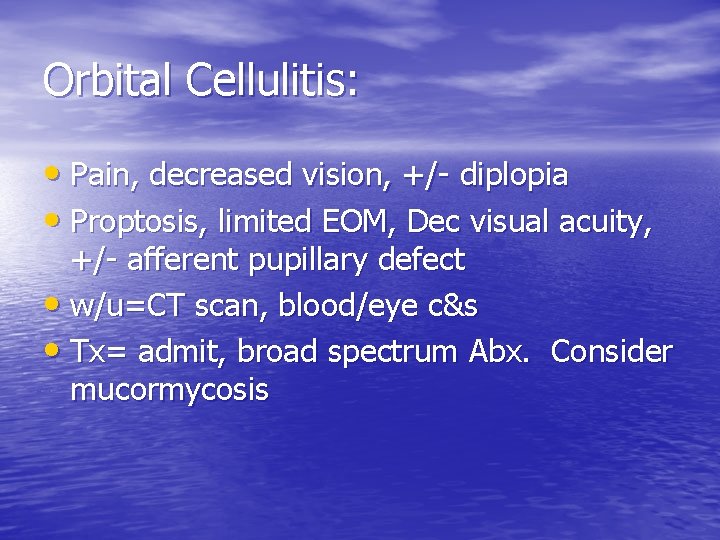
Orbital Cellulitis: • Pain, decreased vision, +/- diplopia • Proptosis, limited EOM, Dec visual acuity, +/- afferent pupillary defect • w/u=CT scan, blood/eye c&s • Tx= admit, broad spectrum Abx. Consider mucormycosis
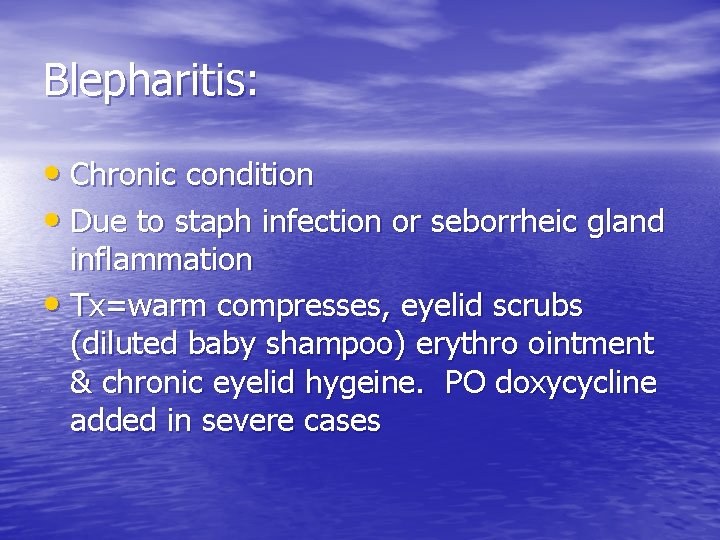
Blepharitis: • Chronic condition • Due to staph infection or seborrheic gland inflammation • Tx=warm compresses, eyelid scrubs (diluted baby shampoo) erythro ointment & chronic eyelid hygeine. PO doxycycline added in severe cases

Case 26:
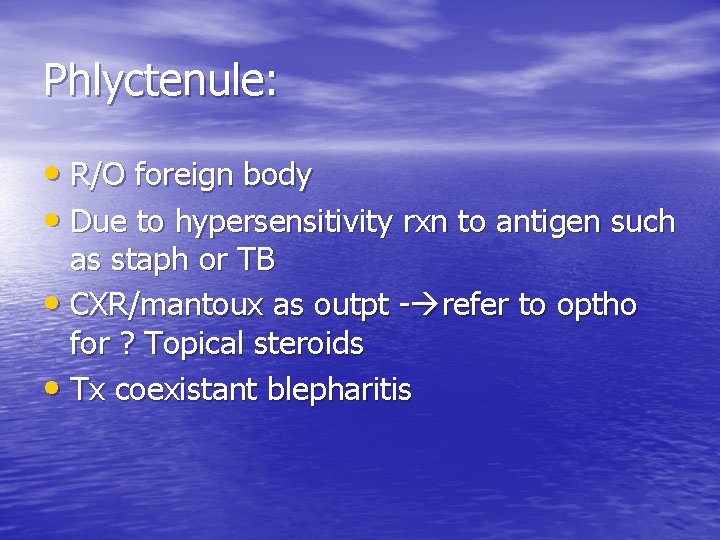
Phlyctenule: • R/O foreign body • Due to hypersensitivity rxn to antigen such as staph or TB • CXR/mantoux as outpt - refer to optho for ? Topical steroids • Tx coexistant blepharitis

Case 27:
Episcleritis: • “Salmon pink” hue of the superficial layer of the eye between conjunctiva/sclera • Usually idiopathic • 1/3 tender, 2/3 sectoral • Tx. Outpatient referral to optho for topical steroids only if severe.

Case 28:
Scleritis: • More painful, often bilateral • 50 % have systemic dx (Crohns, UC, collagen vasc dx, sarcoid, etc) • Simple vs nodular (immobile nodules with q tip) vs necrotizing • Tx: NSAIDs, Optho referral for steroids and systemic w/u
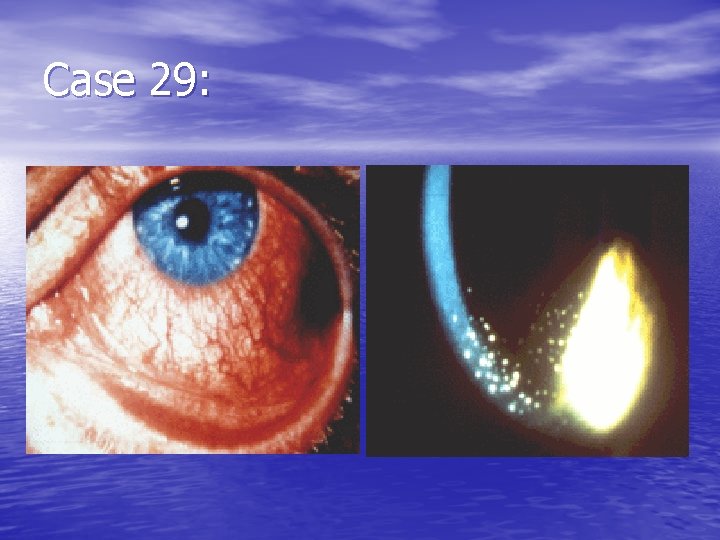
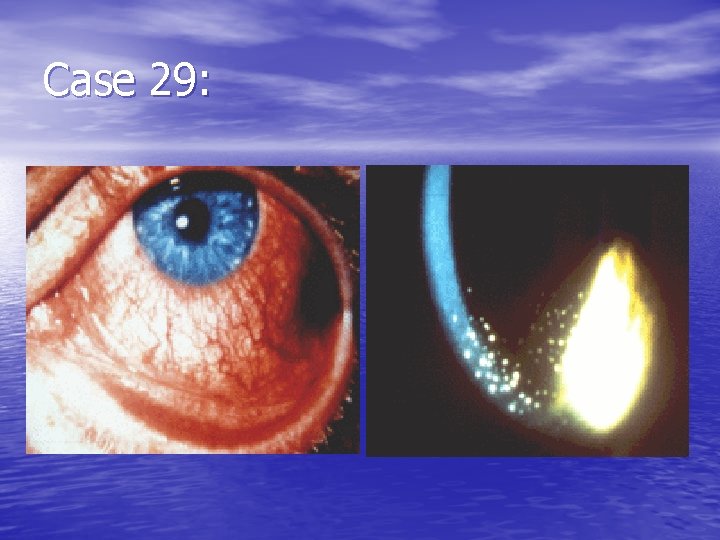
Case 29:
Iritis: • Redness, photophobia, tearing and decreased vision • Ciliary flush and pupillary constriction • Slit lamp= anterior chamber rxn with WBCs, flare (protein leakage), and keratic precipitates • Always fluorescein to r/o abrasion/herpes • Tx=cycloplegics & Topical NSAIDs and referral to optho for steroids
Dry Eyes:
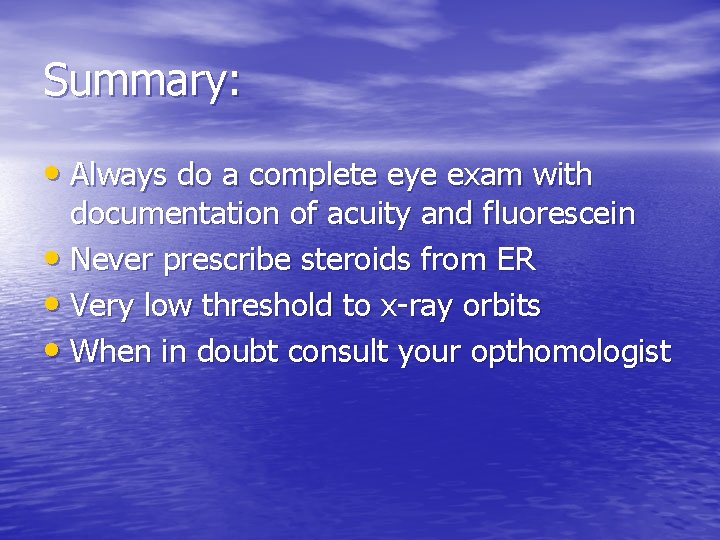
Summary: • Always do a complete eye exam with documentation of acuity and fluorescein • Never prescribe steroids from ER • Very low threshold to x-ray orbits • When in doubt consult your opthomologist

END
 Sportvoedingscoach
Sportvoedingscoach Gimmal compliance suite
Gimmal compliance suite Thank you judges
Thank you judges Preceptor de nero
Preceptor de nero A nurse preceptor is orienting
A nurse preceptor is orienting Preceptor
Preceptor One minute preceptor method
One minute preceptor method Bad preceptor
Bad preceptor Sanford avner
Sanford avner Thank you note to preceptor after orientation
Thank you note to preceptor after orientation Ambitos del pemce
Ambitos del pemce Preceptor evaluation
Preceptor evaluation Harvard preceptor
Harvard preceptor Preceptor ship
Preceptor ship Heartfulness trainer certification
Heartfulness trainer certification Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Chapter 13 handling emergencies
Chapter 13 handling emergencies Endocrine and hematologic emergencies
Endocrine and hematologic emergencies A diver is 30 metres/99 feet underwater
A diver is 30 metres/99 feet underwater Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Psychiatric emergencies
Psychiatric emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Lsu hematology oncology
Lsu hematology oncology Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Qut security contact number for emergencies
Qut security contact number for emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Gems diamond geriatric
Gems diamond geriatric Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Immunologic emergencies
Immunologic emergencies Chapter 28 lesson 1
Chapter 28 lesson 1 Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Solutions by dr dave
Solutions by dr dave Dave engels
Dave engels Dave britnell
Dave britnell Dave edinger
Dave edinger Flash detente winemaking
Flash detente winemaking Dave capstick
Dave capstick Dave ulrich three legged model
Dave ulrich three legged model Dave bockus
Dave bockus Dave kidney
Dave kidney Dave baranowski
Dave baranowski Kate whittemore
Kate whittemore Dave vizard
Dave vizard Dave brash
Dave brash Dave reed random
Dave reed random Dave dodson art of reading smoke
Dave dodson art of reading smoke Zetasizer nano
Zetasizer nano Dave eckhardt
Dave eckhardt Ucl careers service
Ucl careers service Indiana highway
Indiana highway Shuwen qiu
Shuwen qiu Dave joffe
Dave joffe Dave alfano
Dave alfano The amazing dave
The amazing dave Dave simpson rbc
Dave simpson rbc Windows nt vs unix
Windows nt vs unix David ward cisco
David ward cisco Dave wilson texas instruments
Dave wilson texas instruments Dave donut banner
Dave donut banner Dave thaler
Dave thaler Dave baldwin baseball
Dave baldwin baseball Dave bolt
Dave bolt Dave pearson star renewable energy
Dave pearson star renewable energy Daveloper
Daveloper Dave presotto
Dave presotto Dave
Dave Dave paris romeo and juliet
Dave paris romeo and juliet Will you stop dave
Will you stop dave Dave jaye
Dave jaye Dave probert
Dave probert Dave tarr
Dave tarr Dave stetzer
Dave stetzer Dave timecard
Dave timecard Dave paek death
Dave paek death Dave mawhinney
Dave mawhinney Dave and deann stone
Dave and deann stone Setuid
Setuid Dave ramsey fsbo letter
Dave ramsey fsbo letter Dave paige
Dave paige Ishan dave ucf
Ishan dave ucf Dave ulrich human resource champions
Dave ulrich human resource champions Dave cabrera
Dave cabrera Panaceauniversity.org hho
Panaceauniversity.org hho Dave malicke
Dave malicke Dave shattuck
Dave shattuck Skynet 6 service delivery wrap
Skynet 6 service delivery wrap Guys vs men dave barry
Guys vs men dave barry Ublt
Ublt Dave gault
Dave gault Dave grolsh
Dave grolsh Dave provenzano
Dave provenzano Dave thaler
Dave thaler Semil gp vc vc miamiharibhakti
Semil gp vc vc miamiharibhakti Dave brubeck unsquare dance
Dave brubeck unsquare dance Dave lebryk
Dave lebryk Dave stevens palo alto networks
Dave stevens palo alto networks Dave cutaia
Dave cutaia Dave touretzky
Dave touretzky Dave patten
Dave patten Dhiraj dave
Dhiraj dave Dave herald
Dave herald Dave sabben
Dave sabben The original markz twitch
The original markz twitch Dave rosenthal fbisd
Dave rosenthal fbisd Dave copeman
Dave copeman What occurs when a wave bounces off an object
What occurs when a wave bounces off an object Dave dockery
Dave dockery Dave touretzky
Dave touretzky Dave gorman bournemouth
Dave gorman bournemouth Dave paige
Dave paige Dave heaton
Dave heaton Dave feinberg
Dave feinberg Dave buys a baseball for $15 plus an 8 tax
Dave buys a baseball for $15 plus an 8 tax Dave pankow
Dave pankow Dave barach
Dave barach Dave abercrombie
Dave abercrombie Dave halverson
Dave halverson Dave clausen
Dave clausen Norman ackerman
Norman ackerman Dave touretzky
Dave touretzky Dave lin
Dave lin Dave barry colonoscopy pdf
Dave barry colonoscopy pdf Dave poulin db
Dave poulin db Dave kring
Dave kring Dave toback cosmos
Dave toback cosmos Code bases
Code bases Dave allard
Dave allard Psychomotor definition
Psychomotor definition Dave rosgen
Dave rosgen Jc manufacturing purchased inventory for $5 300
Jc manufacturing purchased inventory for $5 300 398712 + 436512 = 447212
398712 + 436512 = 447212 Dave woolf
Dave woolf Dave tolleris
Dave tolleris Dave adelson
Dave adelson Dave liniger net worth
Dave liniger net worth Texas instruments
Texas instruments Dave thimons
Dave thimons Dave galvin
Dave galvin