Motor Learning Process of acquiring or modifying motor











- Slides: 104
Motor Learning Process of acquiring or modifying motor skills through practice Leads to a relatively permanent change After CNS injury, relies on plasticity (CNS adaptation)
Factors that affect Motor Learning CNS arousal / multisensory approach Attention to task Patient motivation Type of memory needed Level / degree of movement required Type / timing of reinforcement Practice schedule Type of practice Environmental context
Stages of Motor Learning SKILL ACQUISITION Patient is getting the idea Many errors Performance inconsistent Frequent repetition and feedback needed Regular practice schedule needed
Stages of Motor Learning SKILL REFINEMENT Decrease in number / degree of errors Increase in consistency / efficiency of movement Distributed practice schedule often used in this stage
Stages of Motor Learning SKILL RETENTION Patient able to perform movement Patient able to achieve functional goals Objective to retain skill and transfer it to different settings Utilize motor problem-solving Random practice schedule useful
Measures of Learning The structure and quality of practice and feedback about performance influence the transfer of skills.
Types of Practice RANDOM Best if several tasks are planned Allows for problem-solving motor problems which aids retention
Types of Practice BLOCKED Repeated performance of the same motor skill Good during early learning or with confused patients
Types of Practice PRACTICE CONTEXTS Facilitates generalization of learning Change environments / conditions yet retain the motor skills required for the task Training should be realistic and in an appropriate environment
Feedback / Reinforcement INTRINSIC FEEDBACK Information received from the learner after performing the task Arises from sensory stimulation to tactile receptors, proprioceptors, and visual and vestibular systems May be limited in patients with sensory, perceptual or cognitive impairments
Feedback / Reinforcement EXTRINSIC FEEDBACK Information received from outside source Augments intrinsic feedback Can provide information on performance and/or results
Feedback / Reinforcement Use performance feedback vs. results feedback in treatment Give feedback more in the early stages and taper off when the patient can correct errors in movement Does frequent extrinsic feedback delay the development of intrinsic feedback?

13 13
Weight Management National Institutes of Health 68% of American adults are overweight More than 33. 8% of American adults are obese In 2007 -2008, 32. 3% of adult men and 35. 5% of adult women were obese 14 Weight Management
Basic Concepts of Weight Management Body Composition Fat-free mass and body fat ○ Fat-free mass: bone, water, muscle, connective tissue, organ tissues, and teeth Body Fat Essential fat: necessary for body to function ○ 3 -5% of total fat in men, 8 -12% in women Fat Storage Adipose tissue: connective tissue in which fat is stored Subcutaneous fat: Located under the skin Visceral Fat (intra-abdominal fat): Located around major organs Factors Affecting Body Composition Genetically determined number of fat cells Cells can increase or decrease in size depending on ○ Age ○ ○ Sex Metabolism Diet Activity level 1 pound of fat = 3500 calories Weight Management 15
Energy Balance Energy balance is key to keeping a healthy ratio of fat and fat-free mass You take in energy (calories) You use up energy (calories) Energy in = energy out, you maintain your current weight Energy in > energy out, you gain weight Energy in < energy out, you lose weight Weight Management 16
Evaluating Body Weight and Body Composition Overweight: Total body weight above recommended range for good health Obesity: A more serious degree of overweight Body Mass Index (BMI) Based on the concept that weight should be proportional to height Does not distinguish between fat weight and fat-free weight 17 Weight Management
Body Composition Analysis Most accurate and direct way to determine percent body fat Hydrostatic (underwater) weighing and Bod Pod Skinfold measurements Thickness of fat under the skin Electrical impedance analysis Electricity prefers fat-free tissue 18 Weight Management
Excess Body Fat and Wellness The health risks of excess body fat Reduces life expectancy by 10 -20 years Associated with: Unhealthy cholesterol and triglyceride levels, impaired heart function, and death from cardiovascular disease Other health factors: hypertension, cancer, impaired immune function, gallbladder and kidney disease, skin problems, impotence, sleep and breathing disorders, back pain, arthritis, bone and joint disorders Strong association with diabetes mellitus: a disease that disrupts normal metabolism 19 Weight Management

Body Fat Distribution and Health Apple shape Pear shape Assessed by measuring waist circumference Total waist measurement of more than 40 inches for men and 35 inches for women is associated with increased risk of disease Large waist circumference can be a marker for increased risk of diabetes, high blood pressure, and CVD, even in people with a BMI in the normal range 20 Weight Management
Body Image Collective picture of the body as seen through the mind’s eye Perceptions Images Thoughts Attitudes Emotions 21 Weight Management
Problems Associated with Very Low Levels of Body Fat Very low body fat is less than 8 -12% for women and less than 3 -5% for men Extreme leanness has been linked to problems with Reproductive disorders Circulatory disorders Immune system disorders Female Athlete Triad 1. 2. 3. Abnormal eating patterns Amenorrhea Decreased bone density 22 Weight Management
Factors Contributing To Excess Body Fat Genetic Factors 25% to 40% of an individual’s body fat The tendency to develop weight is inherited, what you do does matter Physiological Factors Metabolism ○ Resting metabolic rate (RMR): the energy required to maintain vital body functions while the body is at rest 23 Weight Management
Lifestyle Factors Eating Physical activity Psychosocial factors Emotions ○ Distraction from difficult feelings ○ Helps regulate emotions ○ Coping strategies Socioeconomic status Family and culture 24 Weight Management

Adopting A Healthy Lifestyle For Successful Weight Management Diet and eating habits Total calories ○ My. Pyramid suggestions ○ Best approach for weight loss is combining an increase of exercise with moderate calorie restriction Portion Sizes Energy (Calorie) Density Eating Habits Small, frequent meals Set rules to govern your food choices Eat in moderation 25 Weight Management

Physical Activity and Exercise Increasing physical activity is a better approach to losing weight than cutting food intake Regular physical activity: Protects against weight gain Maintains weight loss Improves quality of life 26 Weight Management
Thinking and Emotions Low self-esteem “Ideal self” “Self-talk” can either be self-deprecating or motivating Realistic beliefs and goals 27 Weight Management
Coping Strategies Appropriate coping strategies help you deal with the stresses of life and help with weight management Overeating is not an appropriate coping strategy Use food appropriately To fuel life activities Foster growth Bring pleasure Find new coping strategies Weight Management 28
Approaches to Overcoming A Weight Problem Doing it yourself ○ Lose 0. 5 -2. 0 pounds per week ○ Initial weight loss occurs from fluid loss ○ Smaller, mostly fat, losses later in the diet are better than initial larger, mostly fluid, losses ○ Reasonable weight loss: 8 -10% of body weight over 6 months Dietary supplements and diet aids ○ Formula drinks and food bars ○ Herbal supplements ○ Other supplements 29 Weight Management
Prescription Drugs Appetite suppressants All prescription weight-loss drugs have potential side effects Recommended only for people who have been unable to lose weight with nondrug options or who have a BMI over 30 Weight Management
Surgery Treatment of last resort Only for severely obese 5. 7% of American adults qualify as severely, or morbidly, obese NIH recommends gastric bypass for individuals with a BMI of 40 or higher 31 Weight Management
Eating Disorders Problems with body weight and weight control Characterized by severe disturbances in body image, eating patterns, and eatingrelated behaviors Disordered eating affects an estimated 10 million American females and 1 million males About 90% of eating disorders begin during adolescence. Some begin as young as 8 32 Weight Management
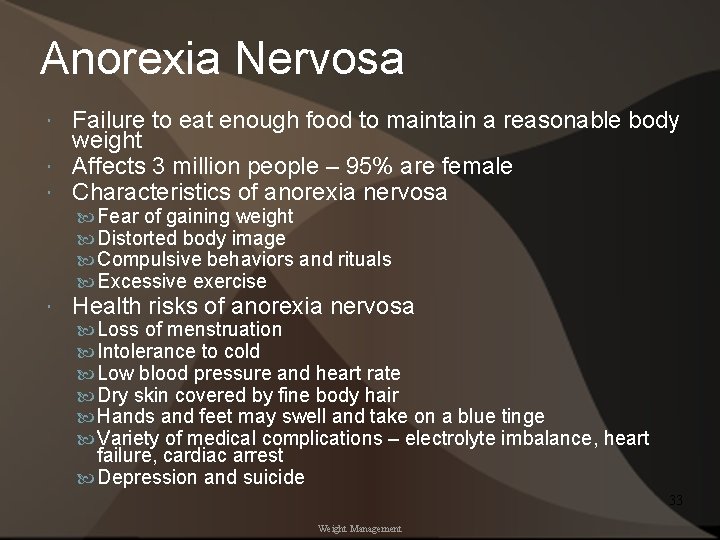
Anorexia Nervosa Failure to eat enough food to maintain a reasonable body weight Affects 3 million people – 95% are female Characteristics of anorexia nervosa Fear of gaining weight Distorted body image Compulsive behaviors and rituals Excessive exercise Health risks of anorexia nervosa Loss of menstruation Intolerance to cold Low blood pressure and heart rate Dry skin covered by fine body hair Hands and feet may swell and take on a blue tinge Variety of medical complications – electrolyte imbalance, heart failure, cardiac arrest Depression and suicide 33 Weight Management
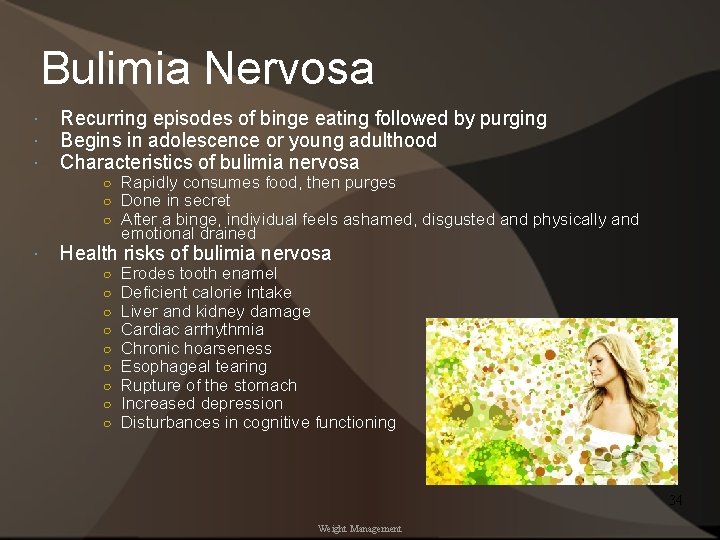
Bulimia Nervosa Recurring episodes of binge eating followed by purging Begins in adolescence or young adulthood Characteristics of bulimia nervosa ○ Rapidly consumes food, then purges ○ Done in secret ○ After a binge, individual feels ashamed, disgusted and physically and emotional drained Health risks of bulimia nervosa ○ ○ ○ ○ ○ Erodes tooth enamel Deficient calorie intake Liver and kidney damage Cardiac arrhythmia Chronic hoarseness Esophageal tearing Rupture of the stomach Increased depression Disturbances in cognitive functioning 34 Weight Management
Other Eating Disorders Binge-Eating Similar to bulimia, except no purging behavior Likely to be obese Increased health risks Higher rates of depression and anxiety Borderline Disordered Eating Have some symptoms of eating disorders but do not meet full diagnostic criteria for eating disorder 35 Weight Management
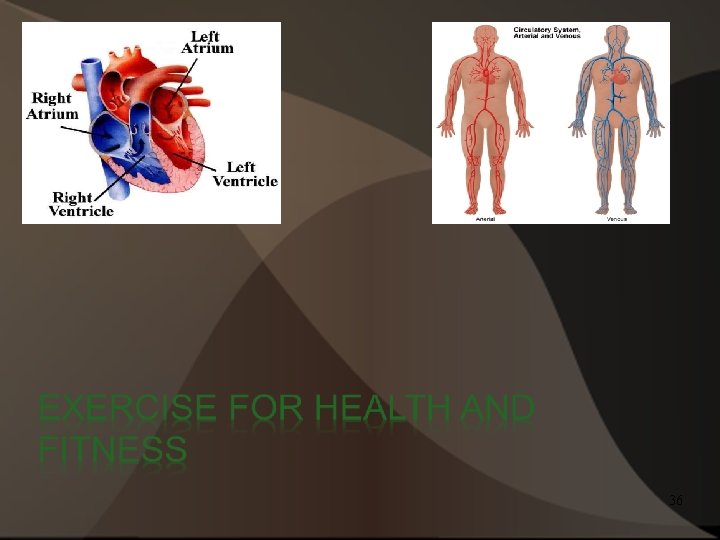
36
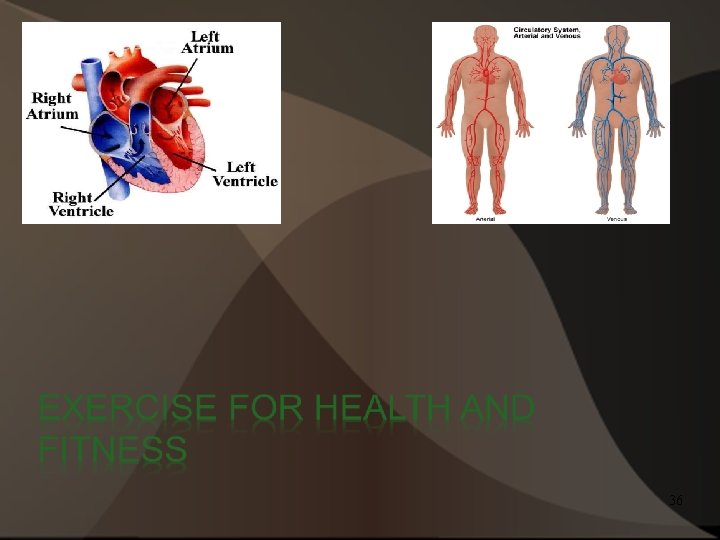
Why Exercise * Increased energy level * Increased cardiovascular fitness * Increased HDL levels * Overall wellness * Better quality of life * Decreased mortality rates due to preventable illnesses (Diabetes, Osteoporosis, some cancers (Colon/Breast), and Cardiovascular disease) 37
What is Physical Fitness? The body’s ability to respond or adapt to the demands and stress of physical effort Health-related fitness: 5 components Cardiorespiratory endurance Muscular strength Muscular endurance Flexibility Body composition 38
What is Physical Fitness? Cardiorespiratory Endurance - ability to perform prolonged, large- muscle, dynamic exercise at moderate to high intensity Muscular Strength - amount of force a muscle can produce with a single maximum effort Muscular Endurance - ability to resist fatigue and sustain a given level of muscle tension - ability of joints to move through their full range of motion Flexibility Body Composition – proportion of fat and fat-free mass (muscle, bone, and water) in the body Skill-Related Components of Fitness – speed, power, agility, balance, coordination and reaction time. Tends to be sport specific 39
Physical Activity and Exercise for Health and Fitness The Centers for Disease Control and Prevention (CDC) recent statistics about American adults: About 31% participate in some leisure-time physical activity Between 2003 and 2009, that leisure-type physical activity decreased by nearly 6% Physical activity levels are higher in men than in women but decline with age in both Levels are lower in Hispanics, American Indians, and blacks than in whites People with higher levels of education are more active. 54% of college grads exercise regularly compared to 31% of high school dropouts 40
The Benefits of Exercise Improved cardiorespiratory functioning More efficient metabolism and improved cell health Improved body composition Reduced risk of premature death 41
Disease Prevention and Management Cardiovascular Prevention Disease = Exercise Improves cholesterol levels Improves blood pressure Improves insulin resistance Interferes with the disease itself Lowers risk of heart disease and stroke Cancer Osteoporosis Type 2 Diabetes 42
Improved Psychological and Emotional Wellness Reduced anxiety and depression Improved sleep Reduced stress Enhanced self-esteem and sense of self-efficacy Enhanced creativity and intellectual functioning Improved interpersonal wellness 43

Physical Activity and Exercise for Health and Fitness Improved immune function Prevention of injures and low-back pain Improved wellness for life 44
Designing Your Exercise Program: First Steps Medical clearance Men over 40 and women over 50 Basic principles of physical training Specificity Progressive overload Frequency Intensity Time Type Reversibility Individual differences Selecting activities 45
Cardiorespiratory Endurance Exercises Frequency - 3 -5 days per week Intensity Maximal oxygen consumption (VO 2 max) Target heart rate range Duration - 20 -60 minutes per workout Type The warm-up and cool-down 46
Developing Muscular Strength and Endurance Types of strength training exercise Resistance exercise Isometric (static) exercise Isotonic (dynamic) exercise Choosing equipment Choosing exercises Frequency Intensity and time A caution about supplements 47
Flexibility Exercises Proper stretching technique Statically Ballistic (bouncing) is dangerous Active Passive Frequency Intensity and time 48
Getting Started and Staying on Track Selecting instructors, equipment, and facilities Finding help and advice about exercise Selecting equipment Choosing a fitness center Eating and drinking for exercise Balanced diet Drink before and during exercise 2 cups, 2 hours before Manage your fitness program Start slowly, get in shape gradually Exercising consistently Assessing your fitness Preventing and managing athletic injuries Staying with your program 49
Points to remember Functional performance directly affects, occupational performance (ADL’s, IADL’s, etc. ), performance skills (energy, endurance, etc. ), and performance patterns (roles, habits, etc. ) Physical exercise has been shown to have a significant impact on functional performance as individuals begin to age. 50

The Challenge of Aging 51
The Challenge of Aging – Normal process of development that occurs throughout life • Generating vitality as you age – Biological aging: the normal, progressive, irreversible changes to one’s body that begin at birth and continue until death – Psychological and social aging: more abrupt changes in circumstances and emotion – Successful aging requires preparation • What happens as you age? – Characteristics associated with aging are not due to aging at all • Result of neglect and abuse of our bodies and minds 52
Life-Enhancing Measures: Age-Proofing • Challenge your mind – Older adults who stay mentally active have a lower risk of developing dementia • Develop physical fitness – Enhances both psychological and physical health • Eat wisely – Eat a varied diet full of nutrient-rich foods – Guidelines for older adults: • • Get enough vitamin B-12 and vitamin D Limit sodium intake and get enough potassium Consume foods rich in dietary fiber and drink plenty of water Pay special attention to food safety 53
Life-Enhancing Measures: Age-Proofing • Maintain a healthy weight • Control drinking and overdependence on medications • Don’t smoke • Schedule screenings and physical examinations to detect treatable diseases • Recognize and reduce stress 54
Dealing With The Changes Of Aging • Planning for social changes – Changing roles and relationships • Major feature of life – Increased leisure time • Many people do not know how to enjoy their free time – The economics of retirement • Financial planning should begin early in life 55
Adapting to Physical Changes • Hearing loss • Vision changes – Age-related macular degeneration (AMD) – Presbyopia – Cataracts • Arthritis – Osteoarthritis (OA) is the most common type of arthritis • Menopause – Usually occurs during a woman’s 40 s or 50 s – Perimenopause • Osteoporosis 56
Handling Psychological and Mental Changes • Grief – Dealing with grief and mourning – Aging is associated with loss • Depression – Unresolved grief can lead to depression, a common problem in older adults 57
Aging And Life Expectancy • Life expectancy – Average length of time we can expect to live – In 2006, life expectancy for the total population was 78. 1 years – Those who reach age 65 can expect to live even longer, 18 years or more longer – Women have longer life expectancy than men 58
Aging and Life Expectancy • America’s aging minority – People 65 and over are a large minority of American population • Over 37. 3 million people • About 12% of the total population in 2006 • Expected to double by 2030 – Social Security benefits • 90% of total income for one-third of Americans over age 65 59
Family and Community Resources for Older Adults • 66% of noninstitutionalized older Americans live with a spouse or family member • 30% live alone • Only 4% live in institutional settings • Of those over the age of 85, about 15% live in a nursing home 60
Coping With Loss • Experiencing grief – Bereavement – Mourning • Tasks of mourning 1. Accepting reality 2. Working through the pain 3. Adjusting to a changed environment 4. Emotionally relocating the deceased and moving on with life • The course of grief – Complicated grief • Supporting a grieving person • Coming to terms with death 61
Vital Signs 62
Assessing Vital Signs Necessary equipment: Quiet environment (quiet as possible) Yourself (of course) Stethoscope Sphygmomanometer (blood pressure cuff) BP cuff which is too small will give abnormally high reading Can use automated or automatic BP, read manual and confirm accuracy of equipment. 63
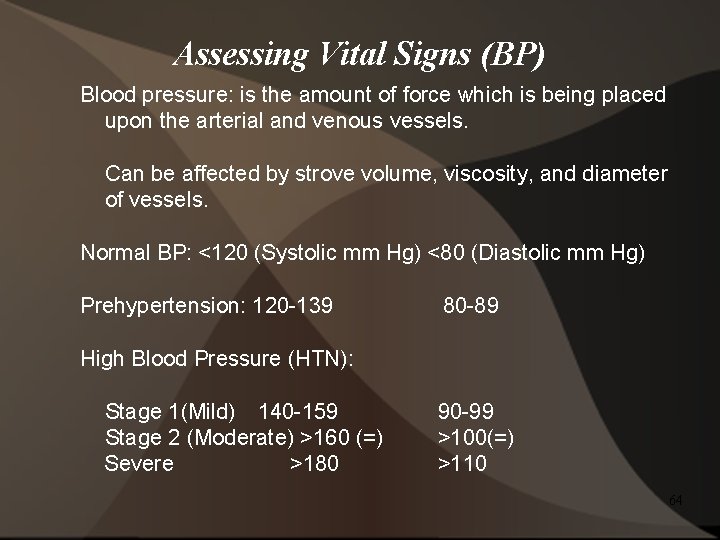
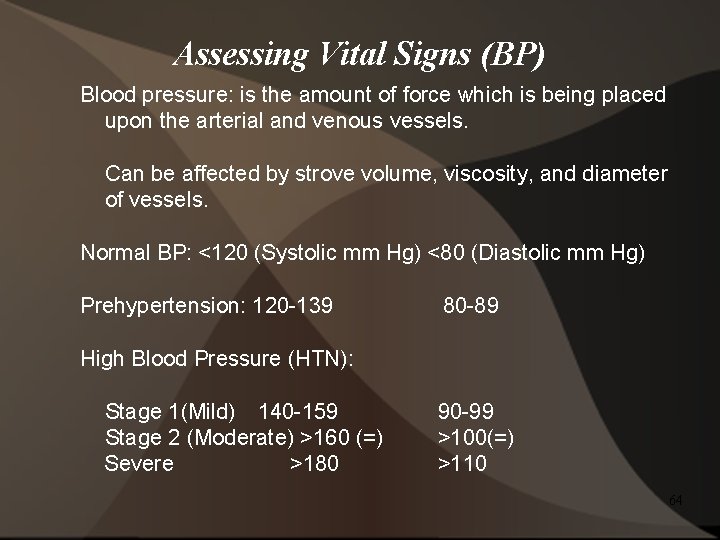
Assessing Vital Signs (BP) Blood pressure: is the amount of force which is being placed upon the arterial and venous vessels. Can be affected by strove volume, viscosity, and diameter of vessels. Normal BP: <120 (Systolic mm Hg) <80 (Diastolic mm Hg) Prehypertension: 120 -139 80 -89 High Blood Pressure (HTN): Stage 1(Mild) 140 -159 Stage 2 (Moderate) >160 (=) Severe >180 90 -99 >100(=) >110 64
Assessing Vitals (BP) Procedure: Inflate BP cuff to 200 (sometimes may have to go a little higher with some patients) Slowly release at 2 to 3 mm Hg/sec. Listen for first Korotkoff sound (Systolic/contraction) Cont. listening for last Korotkoff Sound (Diastolic/relaxation) 65
Assessing Vitals (BP) Positioning: In a upright seated position and relaxed. Do not cross legs (at knee/in general), create an increase in BP (false reading). BP cuff should be ~2. 5 cm above cubital fossa. Should be snug but not too tight around upper arm. Aneroid dial should be facing examiner. 66
Assessing Vitals (Pulse/HR) Pulse is described by: Rate, force, and rhythm Rate: Bradycardia <60 beats/min Tachycardia >100 beats/min Force: Bounding/Increased/Normal/ weak/absent Rhythm: speed up slow down with inspiration expiration Normal resting HR can range from 60 -72 (beats/min) 67
Assessing Vitals (Pulse/HR) Procedure: Have person in a relaxed and comfortable position (seated) Locate Radial, carotid, dorsal pedal, posterior tibial, popliteal, and brachial pulse Place pads of index/middle finger on location Count pulse for 15 seconds and multiply by 4 (1 minute total) (start with 0) 68
Assessing Vitals (Pulse/HR) Pulse locations: Radial: on radial and ventral side of wrist Brachial: medial to biceps tendon Carotid: cervical, medial and below the angel of the jaw Popliteal: Popliteal fossa (posterior knee) Posterior tibial: posterior and inferior to medial malleolus Dorsal pedis(al): medial side of the dorsum of foot 69

Assessing Vitals (Respiration) Involves: Rate, effort, depth of inspiration, and ratio of inspirations/expirations. Rate: number of respirations per minute. Normal respiration rate for an adult is 12 -20 breaths/min. Asses by watching individual breath. Relaxed seated position 70
Assessing Vitals (Temperature) Equipment: Glass, electronic, or Tympanic thermometer Typical Locations: Sub lingual, auditory canal, rectal, and axillary region Tympanic temperatures are typically 0. 8°C/1. 4°F higher than oral Rectal temperatures vary by 0. 4° to 0. 5° C higher than oral Rectal temp. most accurate for core body temperature Axillary temperatures are typically 0. 5°/1°F lower than oral (Not as accurate as either oral/rectal) Normal core body temperature: Oral 98. 6°F (37°C) However, normal may vary from depending upon time of day, earlier maybe lower(35. 8°C/96. 4°F) and evening maybe higher (37. 3°C/99. 1°F) Note: If there is not a reason to suspect fever, assessing temperature may be omitted. Monitor activity levels 71
Assessing Vitals (Temperature) Sub lingual: Maintain contact for 3 -5 minutes (glass thermometer) Electronic requires 10 -15 seconds Glass thermometer shake down mercury to 35°C/96°F Auditory Canal: contact time 2 -3 seconds (ear canal free of excessive cerumen) Rectal: contact time requirement 3 minutes (unconscious person or suspected heat related illness/use Petroleum/KY jelly or approved lubricant) Axillary region; contact time 10 minutes 72
Assessing Vitals (Sanitation) Make sure all equipment is clean and sanitized before/after use Use alcohol swabs to clean stethoscope, BP cuff, and thermometer Use plastic covers for electronic thermometers. Still clean afterwards and before Makes sure hands are washed/sanitized before and after contact with client Alcohol or any pre-approved cleaning medium Treat everyone the same as if they have an infectious/contagious disease 73
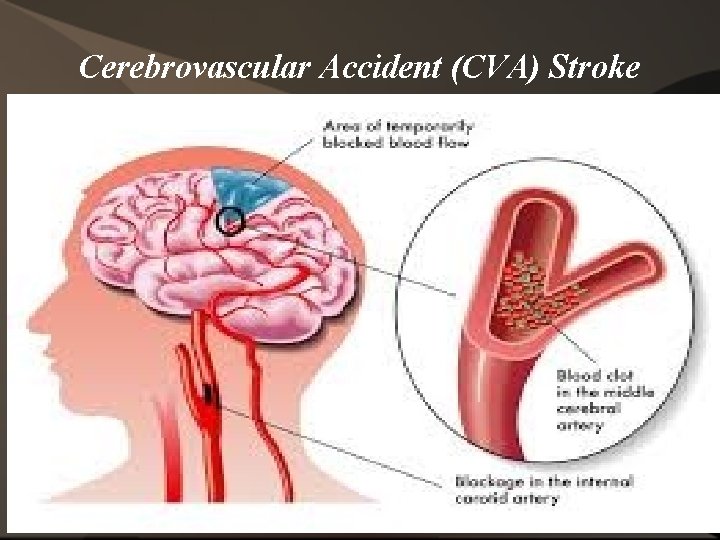
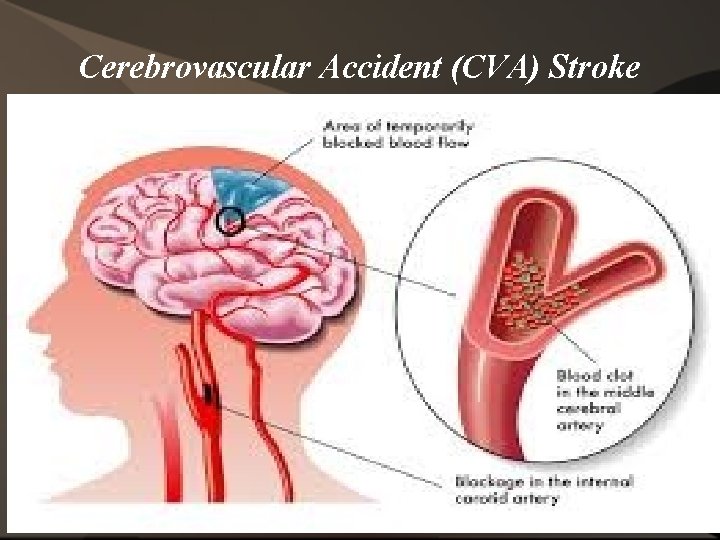
Cerebrovascular Accident (CVA) Stroke 74
Cerebrovascular Accident (CVA) Stroke Types: Ischemic/Hemorrhagic Ischemic: lack of blood perfusion to the brain and a stenotic environment Monitor: DM, HTN, other CVD, smoking, obesity, etc. Hemorrhagic: (has many causes) Primary is a bleeding(ruptures/aneurysms/arteriovenous) in the brain which causes pressure Accounts for 15% to 25% of total strokes Transient Ischemic Attacks (TIAs) Mild and isolated event, can be repetitive (Develops suddenly/last 24 hours/no residual effects) Sign of impending CVA 75
CVA (Signs) Client will be unresponsive: May have a blank stare Face Drooping – Does one side of the face droop or is it numb? Ask the person to smile. Is the person's smile uneven? Arm Weakness – Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward? Speech Difficulty – Is speech slurred? Is the person unable to speak or hard to understand? Ask the person to repeat a simple sentence, like "The sky is blue. " Is the sentence repeated correctly? Time to call 9 -1 -1 – If someone shows any of these symptoms, even if the symptoms go away, call 9 -1 -1 and get the person to the hospital immediately. Check the time so you'll know when the first symptoms appeared. 76
Residual Effects (CVA) Broca's/Expressive aphasia: ability to comprehend (except with rapid speech, lengthy information, or grammatically complex but not verbalize Wernicke's aphasia: ability to verbalize, thought process is compromised (impaired auditory comprehension and feedback) Muscular weakness/increased spasticity/flaccidity (absence of muscle tone) Visual impairment Ambulatory and balance impairments Memory integrity compromised Variety of effects, contingent upon location of the attack 77
Dementia/Alzheimer's 78
Dementia/Alzheimer's Dementia: decrease in cognition General term Slow to develop/progressive/degenerative Effects: Short term memory loss (especially recent events) Decline in functional tasks (IADLs/ADLs) Decreased awareness of functional decline 79
Dementia/Alzheimer's Disease (AD): Most common form of dementia Progressive neurological disorder Several stages (early/middle/late one example/1 -7), increasing in severity of the effects Approximately 6%-8% of people 65 or older have AD (~ 4 million people in US) Incidence of AD doubles every 5 years after age 65 80
Dementia/Alzheimer's Risk factors of AD: • Age • Family hx (history) Head trauma Lower education levels Gender (Females) 81
Dementia/Alzheimer's Etiology of AD: There is not an exact know cause Result of degenerative changes in CNS Plaques and tangles in the brain Protein build up in the brain 82
Dementia/Alzheimer's Signs of which to be aware: Client may display an inability to attend to task Difficulty with concentrating (focusing) Issues with locating objects/items Inability to self-monitor Demonstrate poor insight/thought process Irritability/Confusion Aggression/anger 83
Mental Illness (Older Adults) 84
Mental Illness (Older Adults) There are many different mental health concerns within society Older adults: • • • Dementia/Alzheimer's Anxiety Depression Mania Psychosis Substance abuse 85
When to contact Physicians/Health care providers 86
When to contact Physicians/Health care providers BP is mild to moderate Abnormal temperature Client had a fall Whenever client is sent/goes to the hospital Abnormal respiration 87 Undocumented pulse irregularities
When to call “ 911” Client/patient/person is/has: Unconscious/loses consciousness CHF-severe fluid lower extremity(pitting edema), trouble with breathing Extremely high blood pressure (severe) Signs of stroke/cerebrovascular accident(CVA) Myocardial Infarction (MI) 88

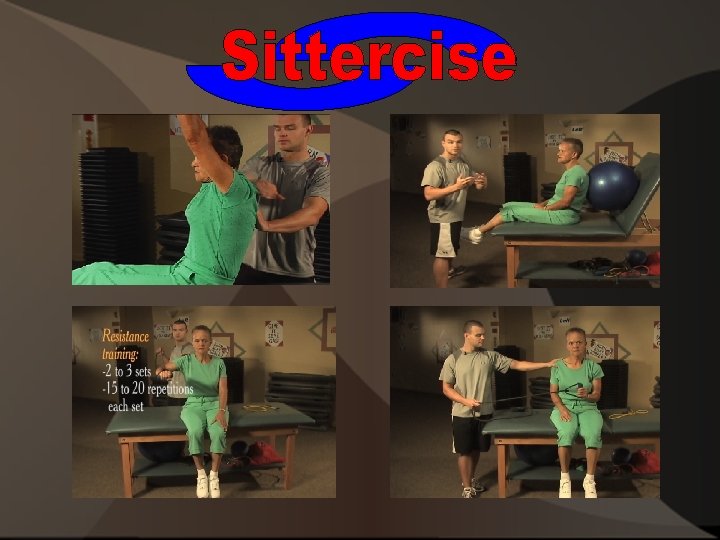
Sittercise Exercise Program 89
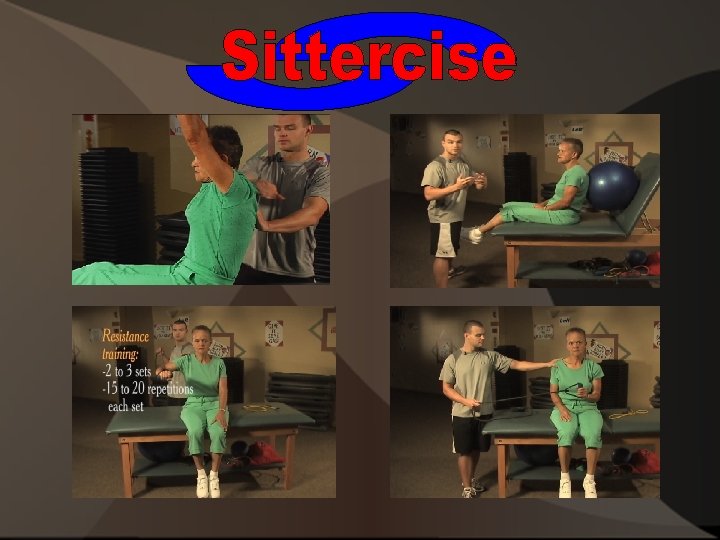
Sittercise Exercise Program Warm Up: (Dynamic) 1 -2 sets 15 -20 reps Ankle-bets (Draw alphabet with fee) Hip Crossovers (Hip rotation) Hip Abduction/adduction (side-lying/supine) Seated I's, Y's, and T's (prone) Cobra (superman) caution lumbar compression 90
Sittercise Exercise Program Resistance Exercises: (Tubing/bands/dumbbells) 2 -3 sets 15 -20 reps Chest press Seated Rows Shoulder (PNF D 1/PNF D 2) Draw the sword Shoulder ER/IR (adducted/or shoulder elbow 90°) Triceps Press (variations) Biceps Curl 91
Sittercise Exercise Program Flexibility/cool down: 1 -3 reps 20 -30 sec. /hold (pain free) Pectoralis (pec) stretch Cervical Strech (scalenes/SCM/Traps) Rotator Cuff (RC) Stretch Hamstring Stretch combination lumbar spine/calf (seated/prone) (Self/assisted) Quadriceps stretch (self/assisted) Hip flexors (rectus femoris/Iliopsoas/Pectineus/TFL) Back stretch (erector spinae/lumbar spine) 92
Exercise Cues (Verbal/Tactile) Caregiver or client stabilize Pelvic neutral Shoulder's back/back straight Core engaged Spinal alignment Pillow under lumbar spine for support Body positioning Do not go beyond pain tolerance 93
Proper Exercise given by Caring People Prevents Painful and Stressful Lifestyles

Product of Maintaining Life Health & Fitness
Slow down the process of Aging! STOP! Stop asking yourself if you are too old to start exercising or if your disability will get in the way.
Exercise Involvement • Increases functional fitness • Decreases the worsening of existing conditions
Ultimate Goals Improve mobility Self-efficacy Overall health Prolong Life
• Strengthens • Builds And • Restores Muscles, joints, and bones
The Sittercise program is designed to offer an at home exercise routine for the elderly and disable. Sittercise is structured in a way that the caretaker or family member can easily comprehend apply the steps that the DVD has to offer, without any confusion. Precautionary measures are highly recommended: - Consult with doctor prior to beginning the Sittercise program - Ensure patient or loved one is capable of performing exercises - Ensure caretaker is able to assist patient or loved one during Sittercise program - Follow instructions from Sittercise program video - Stop! at any signs of discomfort

Changing Lives ! Product of Maintaining Life Health & Fitness

Sittercise Training Are there any questions or concerns? Let's get ready for the exam and practical hands on session.