Control 2527 e Ed E e Ed E222








- Slides: 141
Control #: 2527 e. Ed. E#: e. Ed. E-222 (Shared Display) CAUDA EQUINA: EMBROYOLOGY, ANATOMY & PATHOLOGY: A SYSTEMATIC APPROACH PARVEZ MASOOD, MD JAWAD TSAY, MD VIRGINIA HILL, MD CLEVELAND CLINIC FOUNDATION
No disclosures • Parvez Masood, MD, Jawad Tsay, MD, and Virginia Hill, MD, have nothing to disclose.
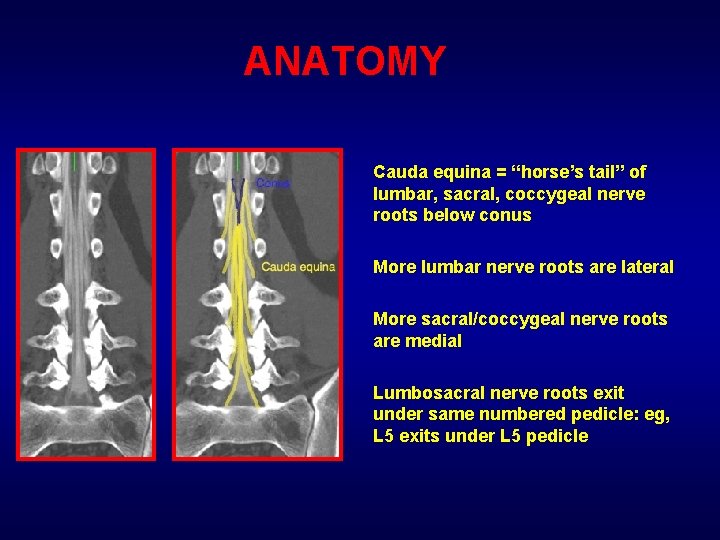
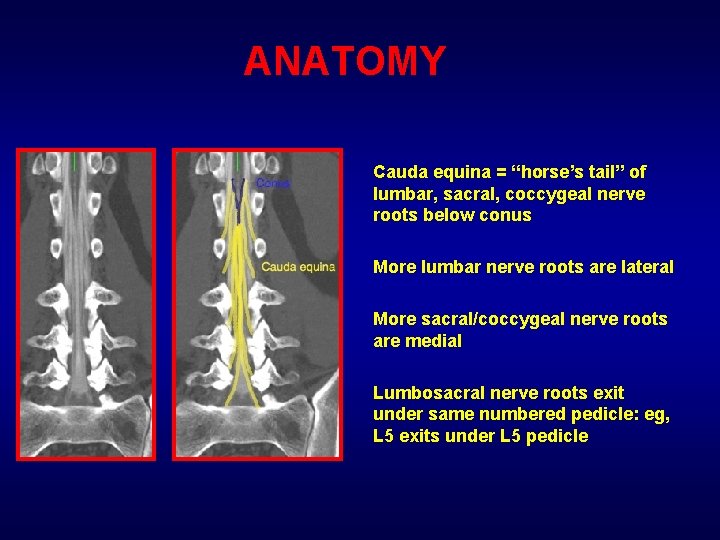
ANATOMY Cauda equina = “horse’s tail” of lumbar, sacral, coccygeal nerve roots below conus More lumbar nerve roots are lateral More sacral/coccygeal nerve roots are medial Lumbosacral nerve roots exit under same numbered pedicle: eg, L 5 exits under L 5 pedicle
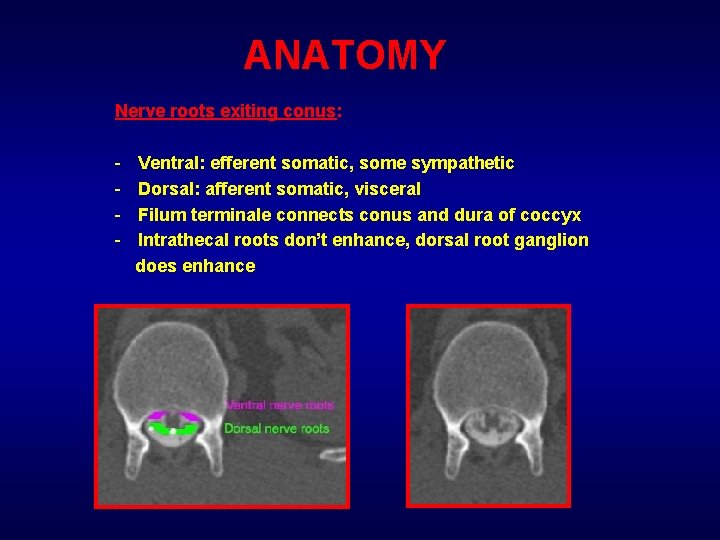
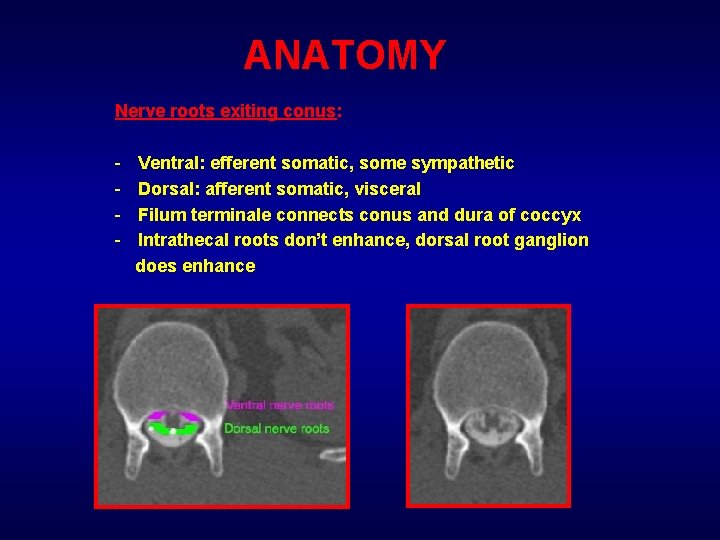
ANATOMY Nerve roots exiting conus: - Ventral: efferent somatic, some sympathetic Dorsal: afferent somatic, visceral Filum terminale connects conus and dura of coccyx Intrathecal roots don’t enhance, dorsal root ganglion does enhance
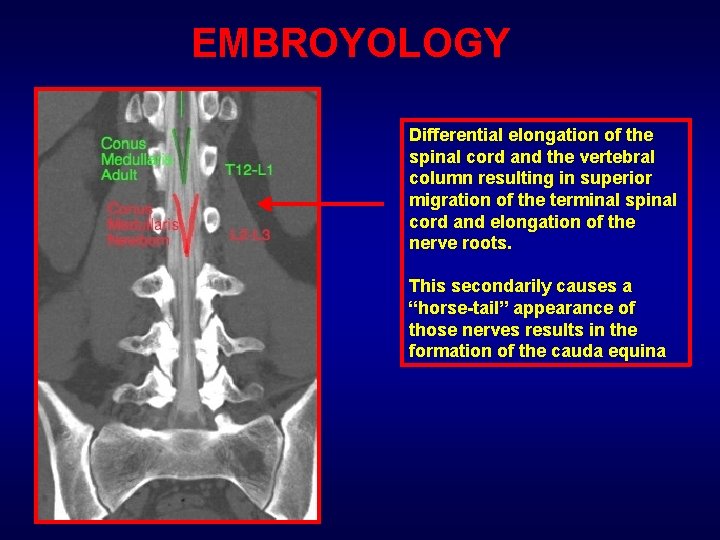
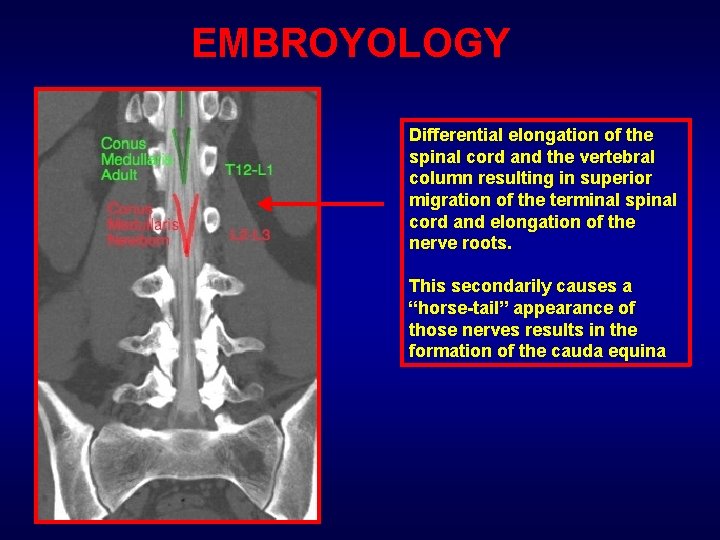
EMBROYOLOGY Differential elongation of the spinal cord and the vertebral column resulting in superior migration of the terminal spinal cord and elongation of the nerve roots. This secondarily causes a “horse-tail” appearance of those nerves results in the formation of the cauda equina
CONGENITAL ABNORMALITIES
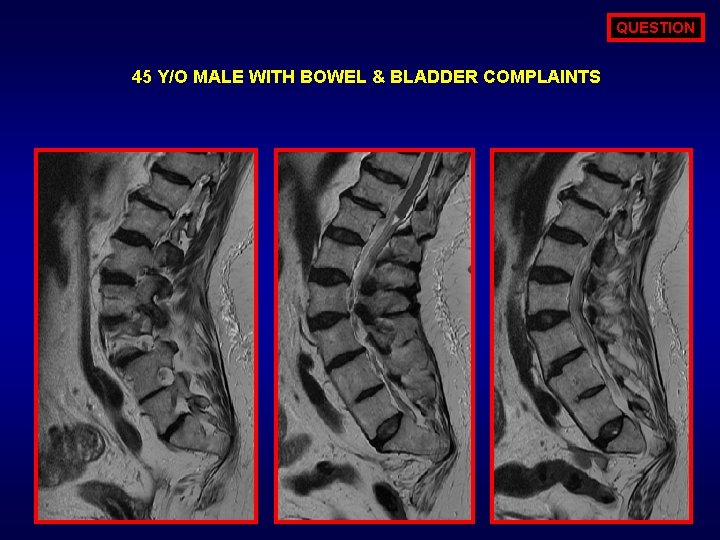
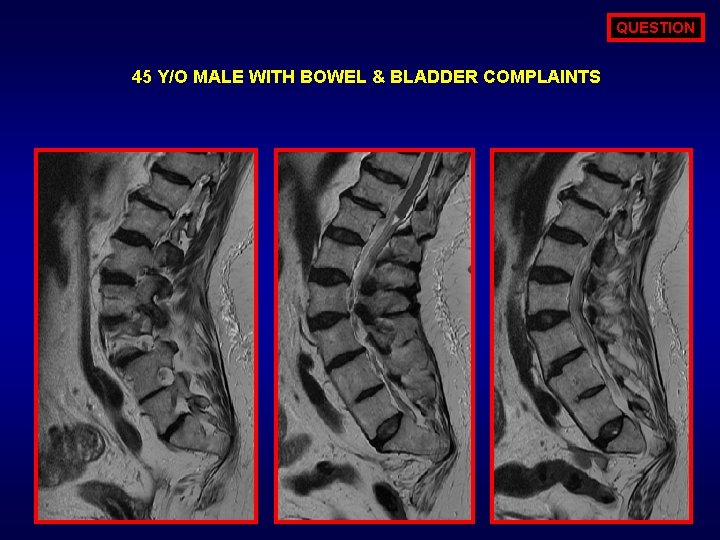
QUESTION 45 Y/O MALE WITH BOWEL & BLADDER COMPLAINTS
ANSWER OPTIONS MOST COMMON MATERNAL FACTOR ASSOCIATED WITH THIS ENTITY IS? 1. 2. 3. 4. FOLATE DEFICIENCY ALCOHOL ABUSE MATERNAL DIABETES TORCH INFECTION
ANSWER MATERNAL DIABETES: A. 15 -20% OF CHILDREN WITH CAUDAL REGRESSION SYNDROME ARE BORN TO DAIBATIC MOTHERS. ALSO B. 1% OF INFANTS OF DIABETIC MOTHERS ARE AFFECTED
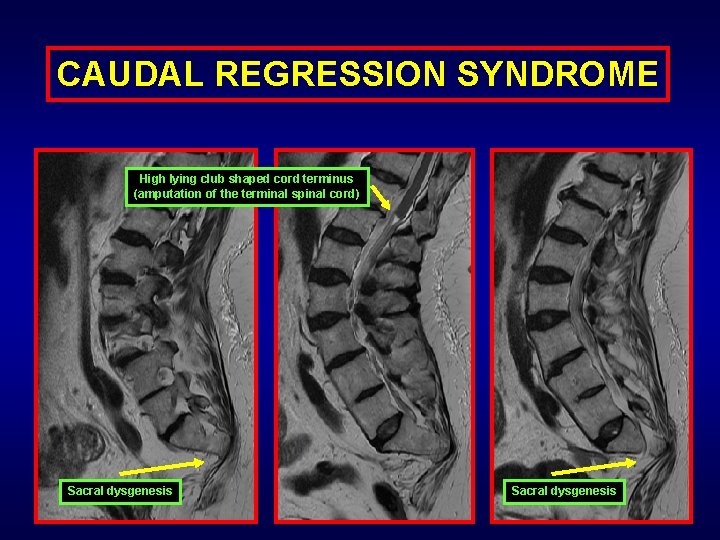
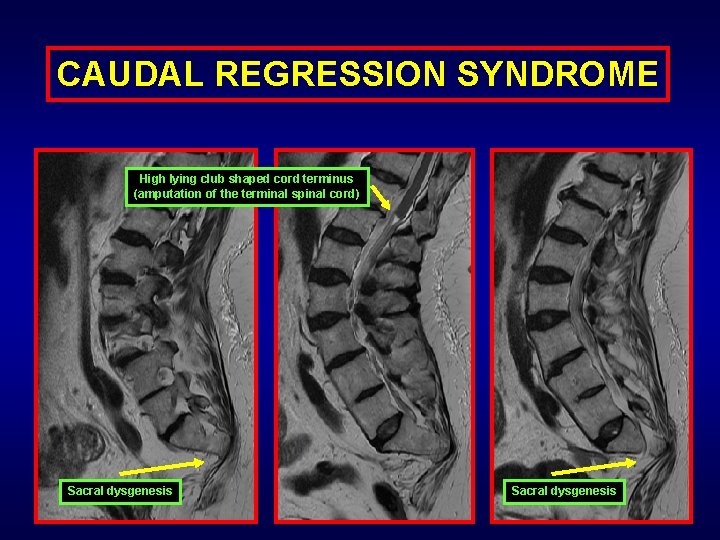
CAUDAL REGRESSION SYNDROME High lying club shaped cord terminus (amputation of the terminal spinal cord) Sacral dysgenesis
CAUDAL REGRESSION SYNDROME INTRODUCTION: A rare congenital anomaly assocaited with absent lower vertebral bodies, malformed genitalia, anal atresia and potential lower extremity anomaly (worst case scenario – sirenomyelia). CLINICAL PRESENTATION: Neurogenic urinary bladder dysfunction. Structural anomaly of lower extremity & sacrum Sacral dysgensis with high lying club shaped cord (Group I) CLASSIFICATION: Sacral dysgensis with low lying cord with associated tethered anomalies and lipo-myelo-meningo anomalies (Group II)
IMAGING HALLMARKS: 1. Lumbosacral dysgenesis (both with group I & II) 2. Amputated high lying spinal cord (Group I) 3. Tethered low lying cord with variable associated anomalies of the meninges – fat – skin. IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging TREATMENT PROGNOSIS: 1. With group II: Untethering with repair of associated anomalies 2. Surgery to improve lower extremity & bowel bladder function

QUESTION NEWBORN WITH DORSAL MENINGOCELE
ANSWER OPTIONS WHAT IS THE MOST COMMON MALFORMATION ASSOCIATED WITH THIS ENTITY? 1. 2. 3. 4. CHIARI DANDY WALKER CARDIAC SEPTAL DEFECTS SEPTO-OPTIC DYSPLASIA
ANSWER CHAIRI II: A. 15 -20% OF CHIARI MALFORMATION PATIENTS ARE ASSOCIATED WITH DIASTOMETAMYELIA.
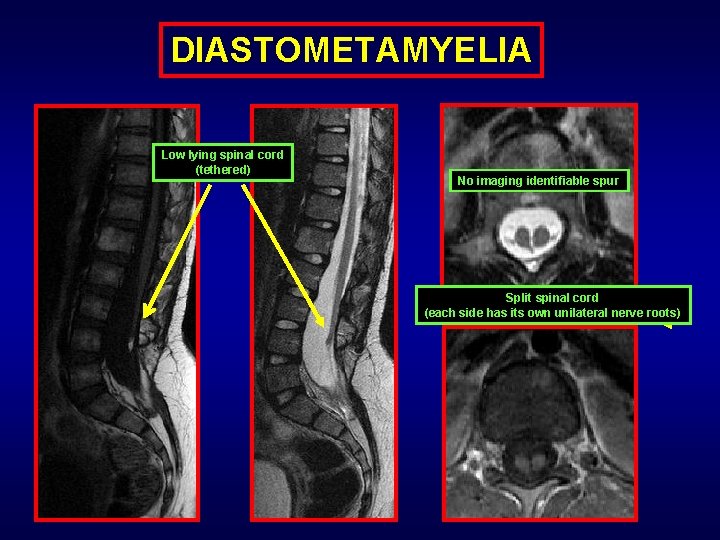
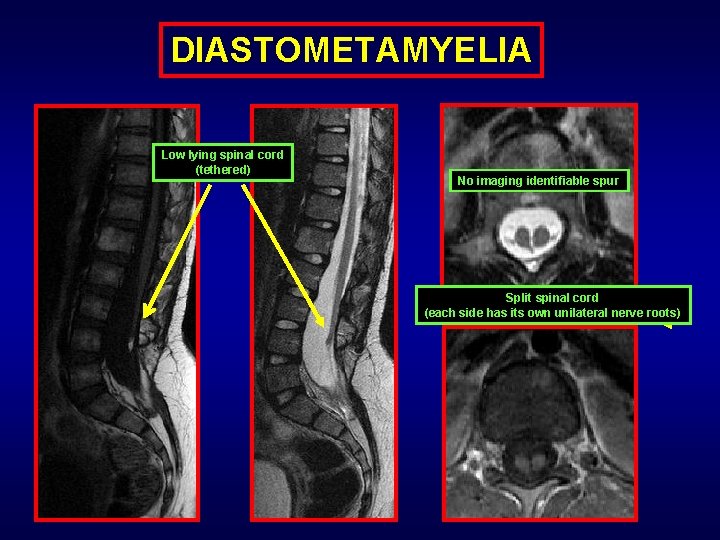
DIASTOMETAMYELIA Low lying spinal cord (tethered) No imaging identifiable spur Split spinal cord (each side has its own unilateral nerve roots)
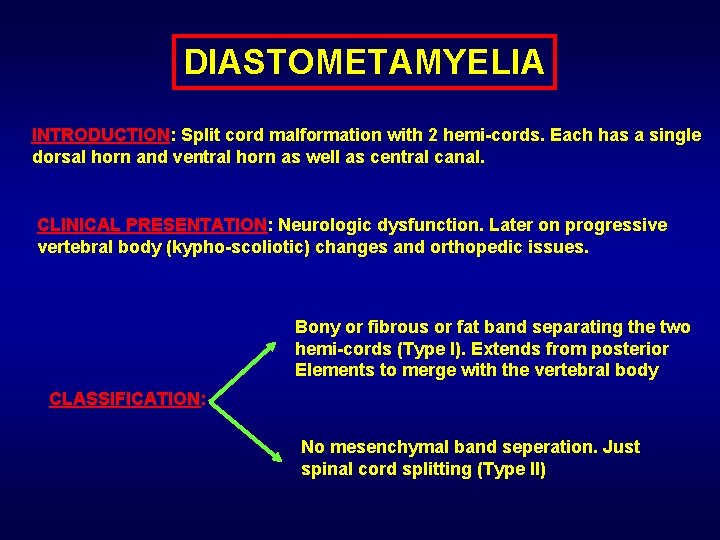
DIASTOMETAMYELIA INTRODUCTION: Split cord malformation with 2 hemi-cords. Each has a single dorsal horn and ventral horn as well as central canal. CLINICAL PRESENTATION: Neurologic dysfunction. Later on progressive vertebral body (kypho-scoliotic) changes and orthopedic issues. Bony or fibrous or fat band separating the two hemi-cords (Type I). Extends from posterior Elements to merge with the vertebral body CLASSIFICATION: No mesenchymal band seperation. Just spinal cord splitting (Type II)
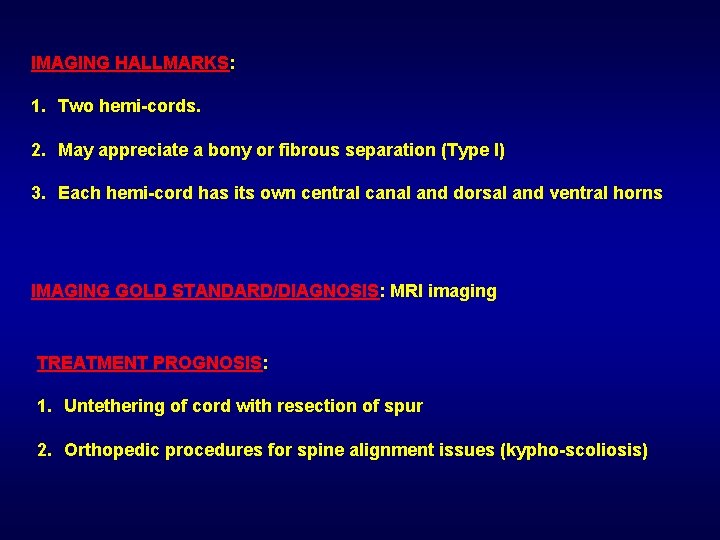
IMAGING HALLMARKS: 1. Two hemi-cords. 2. May appreciate a bony or fibrous separation (Type I) 3. Each hemi-cord has its own central canal and dorsal and ventral horns IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging TREATMENT PROGNOSIS: 1. Untethering of cord with resection of spur 2. Orthopedic procedures for spine alignment issues (kypho-scoliosis)
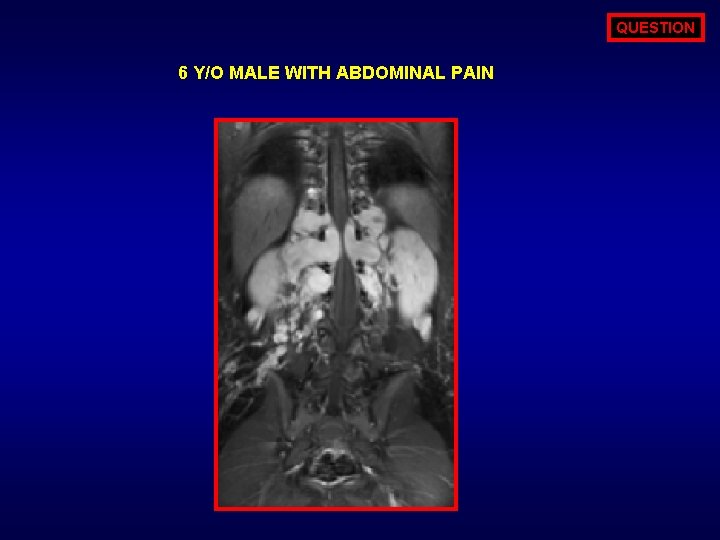
QUESTION 6 Y/O MALE WITH ABDOMINAL PAIN
ANSWER OPTIONS ALL OF THE FOLLOWING ARE CHARACTERSTIC FOR NF-1 EXCEPT? 1. 2. 3. 4. 5. PSEUDOARTHROSIS LATERAL MENINGOCELE PLEXIFORM NEUROFIBROMA SACRAL DYSPLASIA SPHENOID WING DYSPLASIA
ANSWER SACRAL DYSPLASIA: A. ALL OF THE AFOREMENTIONED ARE CHARACHTERSTICS OF NF-1 EXCEPT SACRAL DYSPLASIA. B. HALLMARK OF NF-1 IS PLEXIFORM NEUROFIBROMA. C. HALLMARK OFNF-2 IS VESTIBULAR SCHWANNOMA (BILATERAL).
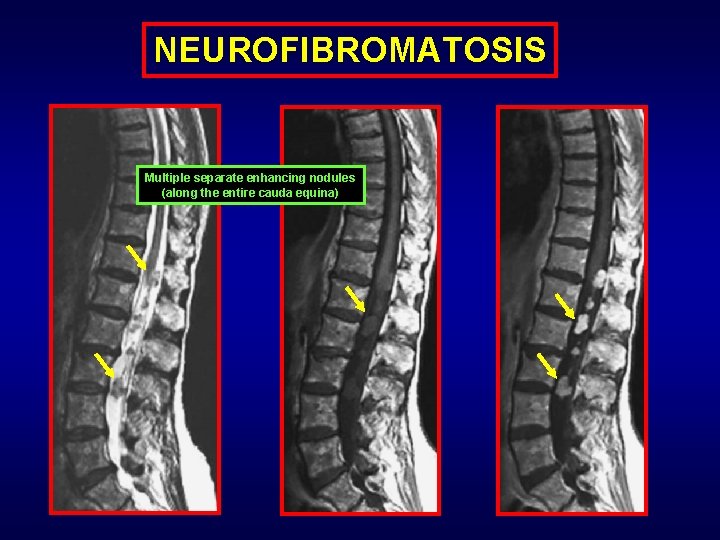
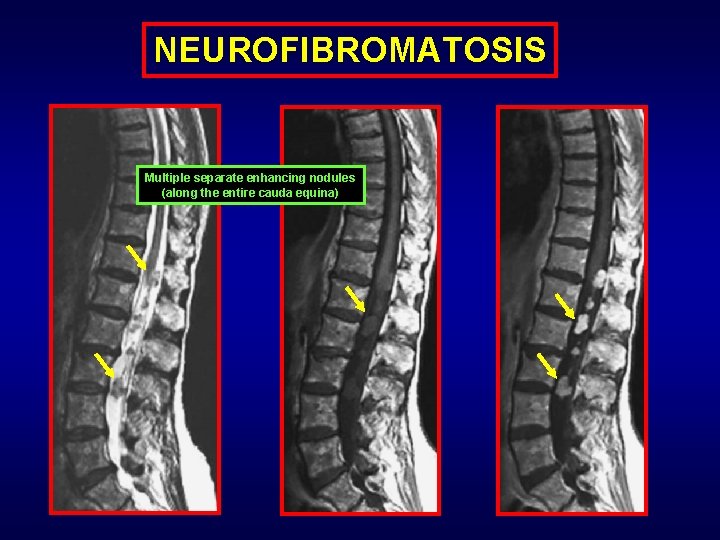
NEUROFIBROMATOSIS Multiple separate enhancing nodules (along the entire cauda equina)
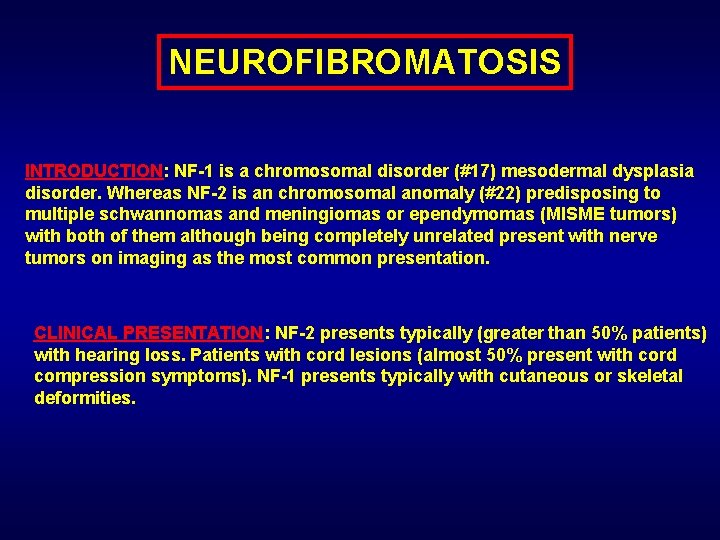
NEUROFIBROMATOSIS INTRODUCTION: NF-1 is a chromosomal disorder (#17) mesodermal dysplasia disorder. Whereas NF-2 is an chromosomal anomaly (#22) predisposing to multiple schwannomas and meningiomas or ependymomas (MISME tumors) with both of them although being completely unrelated present with nerve tumors on imaging as the most common presentation. CLINICAL PRESENTATION: NF-2 presents typically (greater than 50% patients) with hearing loss. Patients with cord lesions (almost 50% present with cord compression symptoms). NF-1 presents typically with cutaneous or skeletal deformities.
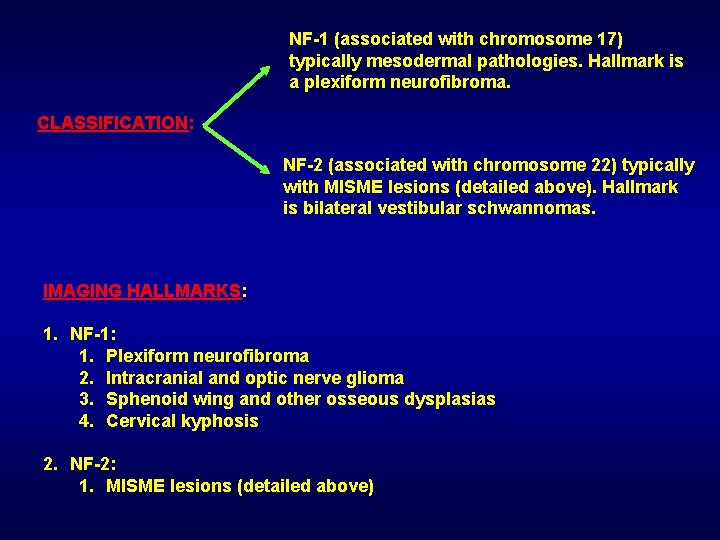
NF-1 (associated with chromosome 17) typically mesodermal pathologies. Hallmark is a plexiform neurofibroma. CLASSIFICATION: NF-2 (associated with chromosome 22) typically with MISME lesions (detailed above). Hallmark is bilateral vestibular schwannomas. IMAGING HALLMARKS: 1. NF-1: 1. Plexiform neurofibroma 2. Intracranial and optic nerve glioma 3. Sphenoid wing and other osseous dysplasias 4. Cervical kyphosis 2. NF-2: 1. MISME lesions (detailed above)
IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging of brain and spine TREATMENT PROGNOSIS: 1. Resection of symptomatic tumors 2. Orthopedic procedures for spine alignment issues (kypho-scoliosis)
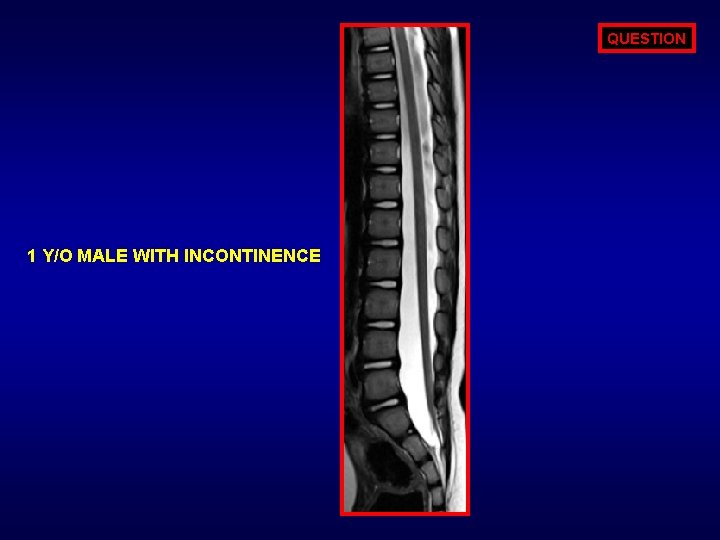
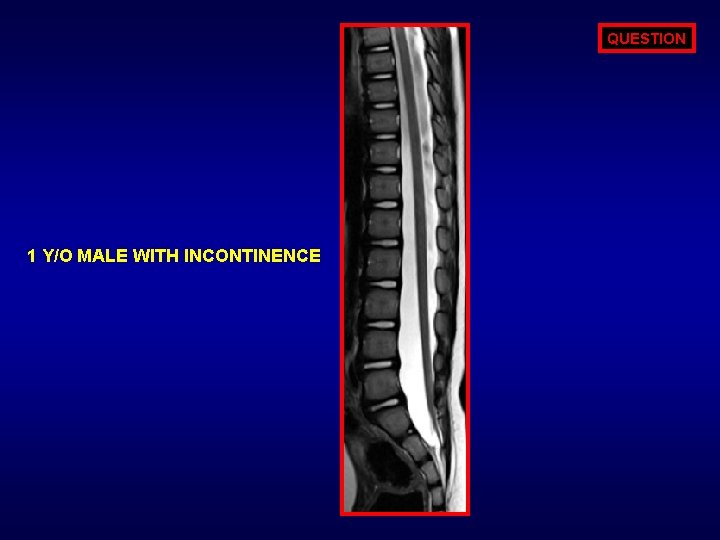
QUESTION 1 Y/O MALE WITH INCONTINENCE
ANSWER OPTIONS NORMAL LOCATION OF CONUS? 1. 2. 3. 4. 5. L 1 -2 L 2 -3 L 3
ANSWER AT OR ABOVE L 2 -3 LEVEL:
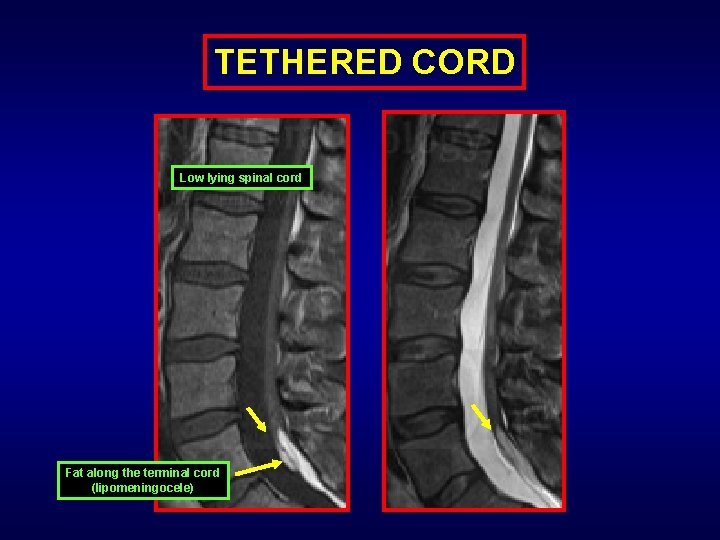
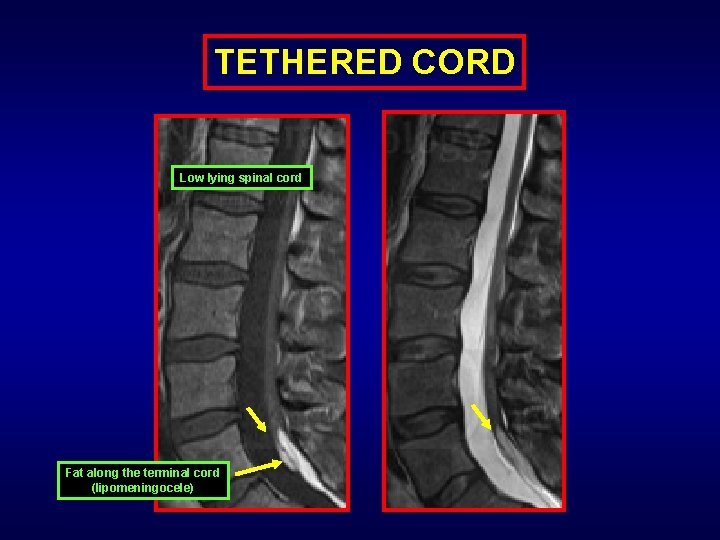
TETHERED CORD Low lying spinal cord Fat along the terminal cord (lipomeningocele)
TETHERED CORD INTRODUCTION: Low lying terminal spinal cord below inferior L 2 which may or may not be associated with a soft tissue – fatty mass or may not be adherent to the posterior spinal canal. CLINICAL PRESENTATION: Neurologic dysfunction. Low back and leg pain. May be associated with gait disturbance. IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging
IMAGING HALLMARKS: 1. Conus ends below inferior L 2. 2. Thickened filum (greater than 2 mm at L 5 -S 1 on MRI). 3. May or may not be associated with spectrum of spinal dysraphisms TREATMENT PROGNOSIS: 1. Untethering of cord 2. May be followed with CSF flow study to look for re-tethering (Caveat: return of normal CSF flow is seen in less 1/3 of patients even if symptoms resolve) 3. Re-tethering is based mainly on clinical grounds
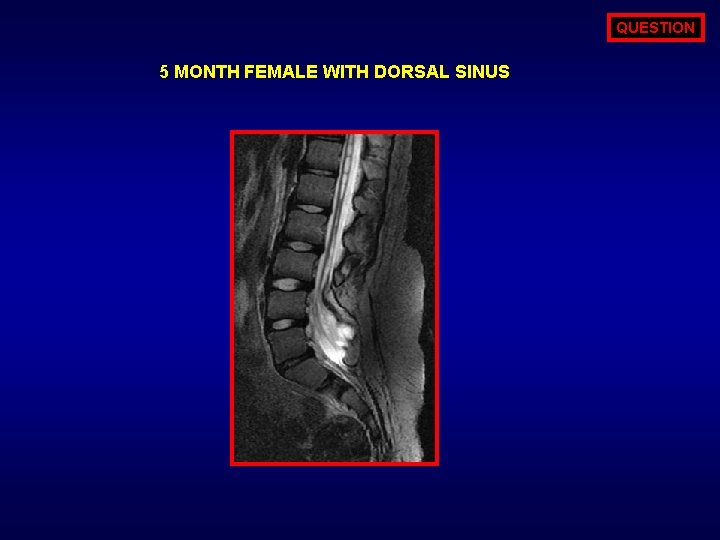
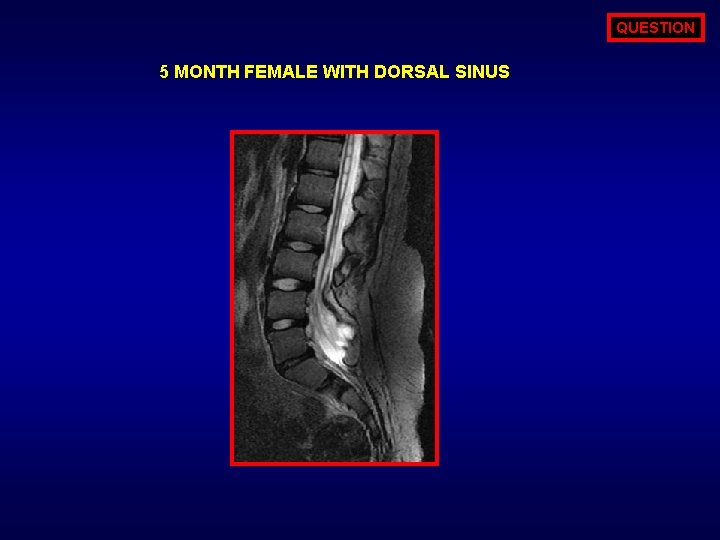
QUESTION 5 MONTH FEMALE WITH DORSAL SINUS
ANSWER OPTIONS WHICH NEUTRITIONAL DEFICIENCY IS ASSOCIATED WITH THIS ENTITY? 1. 2. 3. 4. 5. Thiamine Riboflavin Folic acid Leucine Cholecalciferol
ANSWER FOLIC ACID:
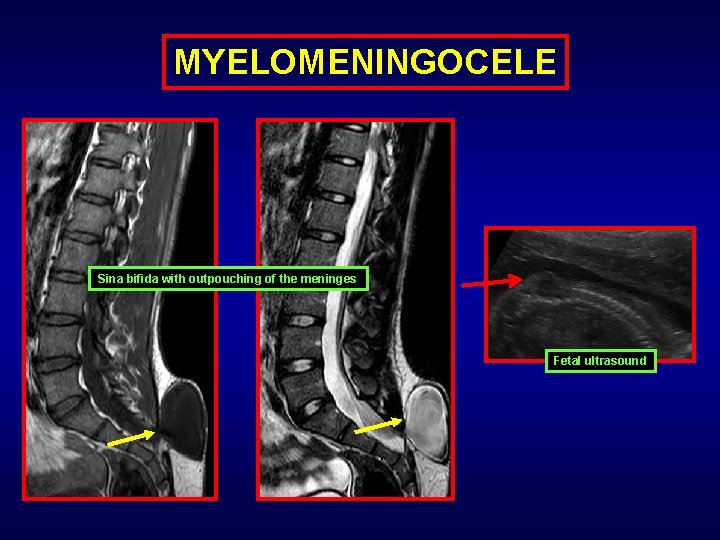
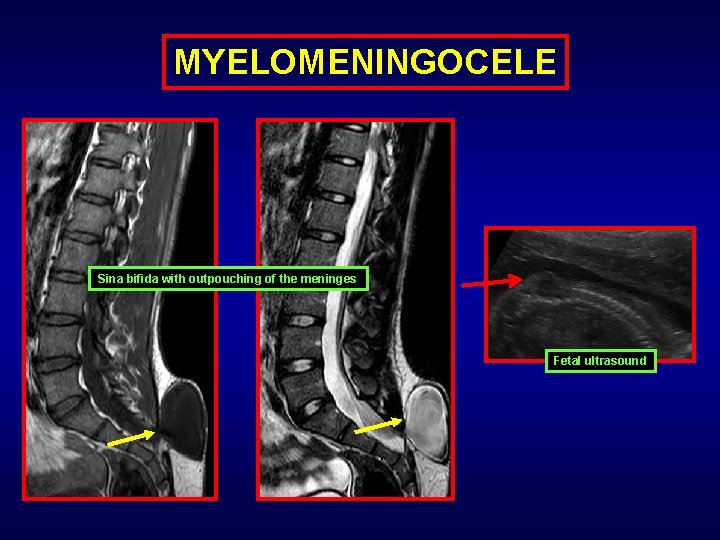
MYELOMENINGOCELE Sina bifida with outpouching of the meninges Fetal ultrasound
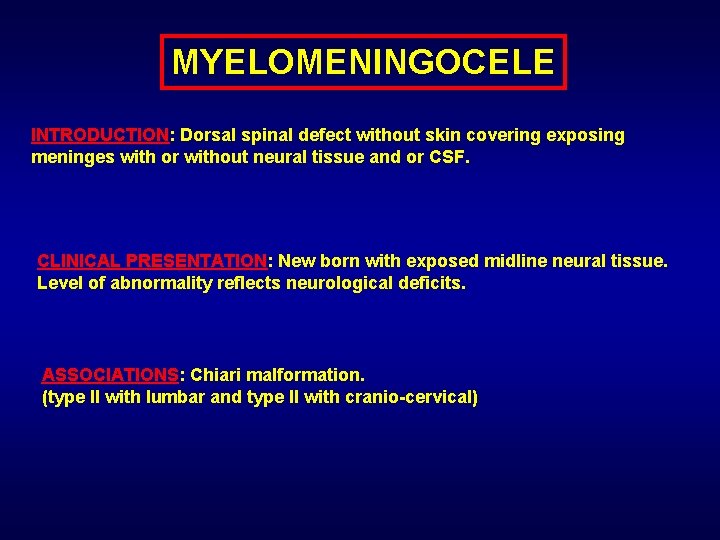
MYELOMENINGOCELE INTRODUCTION: Dorsal spinal defect without skin covering exposing meninges with or without neural tissue and or CSF. CLINICAL PRESENTATION: New born with exposed midline neural tissue. Level of abnormality reflects neurological deficits. ASSOCIATIONS: Chiari malformation. (type II with lumbar and type II with cranio-cervical)
IMAGING HALLMARKS: 1. Open spinal dysraphism 2. Low lying spinal cord 3. Open neural arch 4. Intracranial Chiari findings IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging TREATMENT PROGNOSIS: 1. Prevention (Folate supplementation for conceiving & pregnant women) 2. In-utero surgery if possible 3. Repair of the meningomyelocele in early neonate period
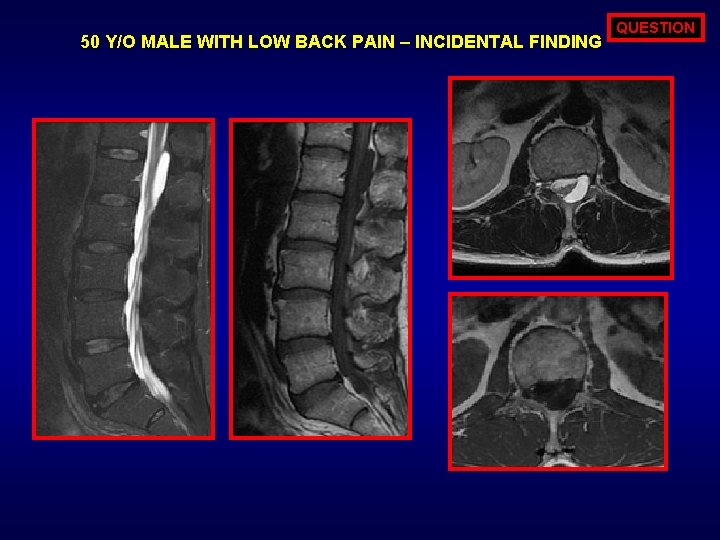
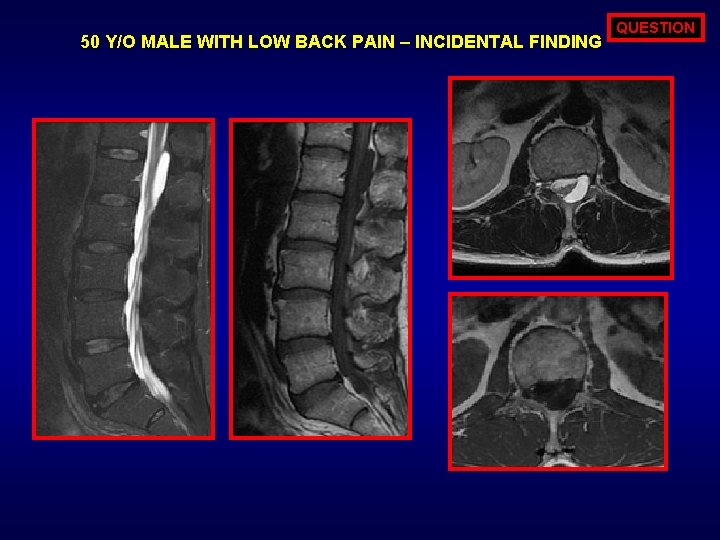
50 Y/O MALE WITH LOW BACK PAIN – INCIDENTAL FINDING QUESTION
ANSWER OPTIONS ALL THE FOLLOWNG RESTRIC DIFFUSION EXCEPT? 1. 2. 3. 4. EPIDERMOID ARACHNOID CYST ABSCESS INTRACRANIAL PNET
ANSWER ARACHNOID CYST: Follows CSF intensity (density) on all imaging parameters
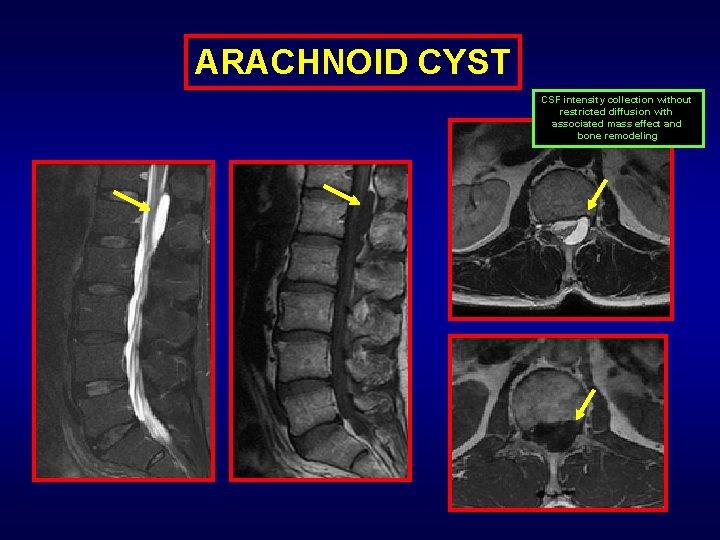
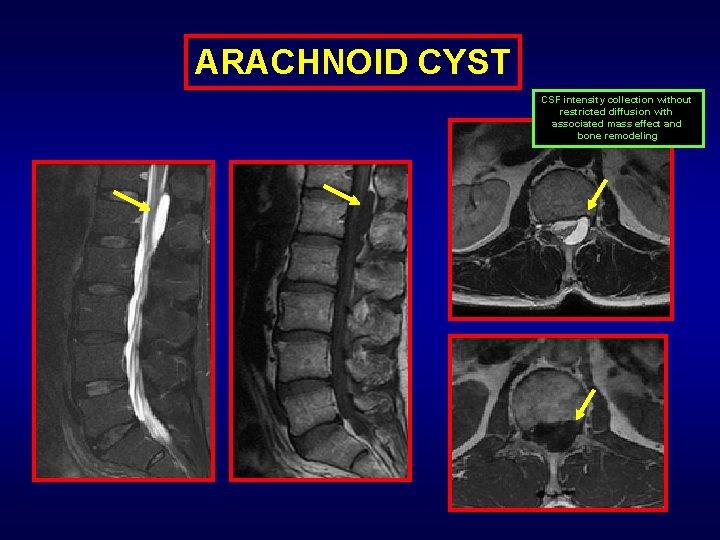
ARACHNOID CYST CSF intensity collection without restricted diffusion with associated mass effect and bone remodeling
ARACHNOID CYST INTRODUCTION: Extramedullary intraspinal CSF collection. CLINICAL PRESENTATION: Most patients are incidentally detected. Presentation may be in relation to mass effect and compression of cauda equina, especially if present in sacral region. Intradural. CLASSIFICATION: Extradural (herniating thru the dura)
IMAGING HALLMARKS: 1. CSF intensity circumscribed collection 2. Mass effect (bone scalloping & compression of cauda equina – thecal sac) (bone remodeling is more common with extradural form) 3. Cap sign: Seen with extradural type – epidural fat at superior & inferior aspect IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging TREATMENT - PROGNOSIS: 1. Only if symptomatic (nerve or cord compression) 2. Decompression – fenestration of the arachnoid cyst

TRAUMA - IATROGENIC ABNORMALITIES
QUESTION MOST COMMON PRESENTATION OF CHRONIC SPINE SUBARACHNOID HEMORRHAGE IS? 1. 2. 3. 4. Headache Hearing loss Vomiting Back pain
ANSWER HEARING LOSS: Due to cortical superficial siderosis (most common extra spinal presentation of myxopapillary ependymoma).
QUESTION MOST COMMON CAUSE OF EPIDURAL HEMATOMA IN SPINE IS? 1. 2. 3. 4. Coagulopathies Trauma Spontaneous Iatrogenic

ANSWER SPONTANEOUS EPIDURAL HEMTOMA:
QUESTION DESIRED LOCATION OF COLLECTION IN CSF LEAK BLOOD PATCH IS: 1. Subdural 2. Epidural 3. Subarachnoid
ANSWER EPIDURAL - BLOOD PATCH
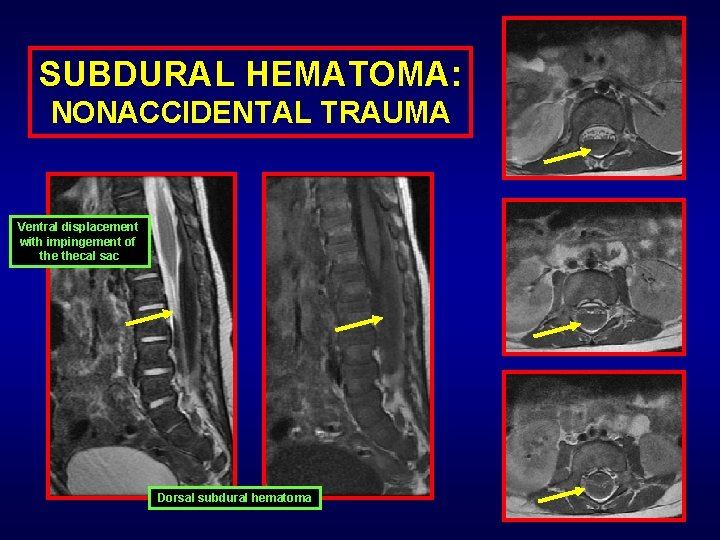
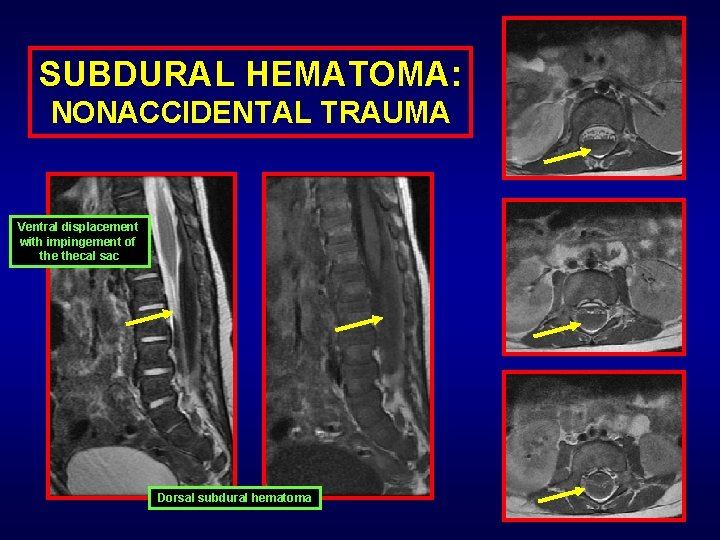
SUBDURAL HEMATOMA: NONACCIDENTAL TRAUMA Ventral displacement with impingement of thecal sac Dorsal subdural hematoma
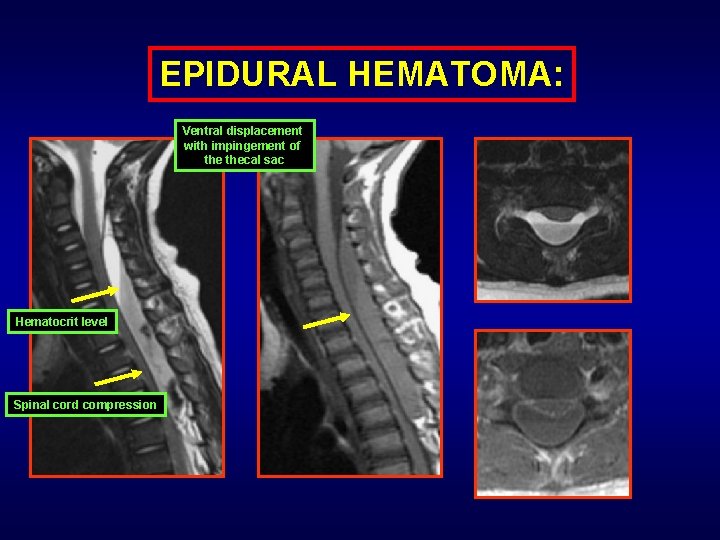
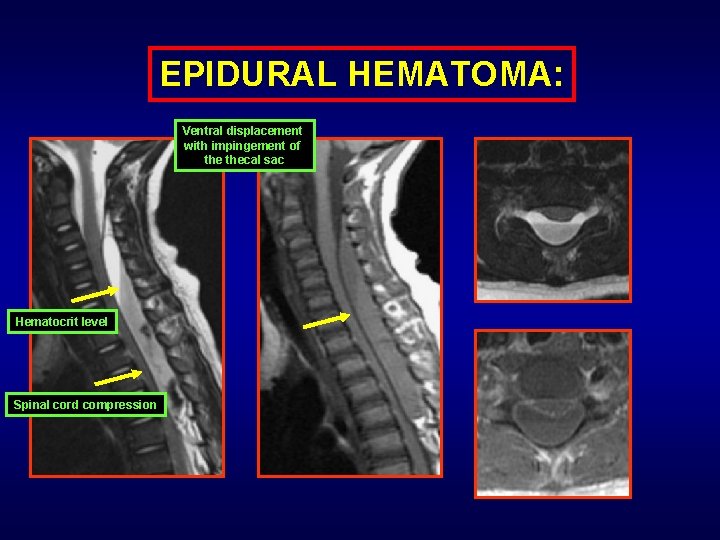
EPIDURAL HEMATOMA: Ventral displacement with impingement of thecal sac Hematocrit level Spinal cord compression
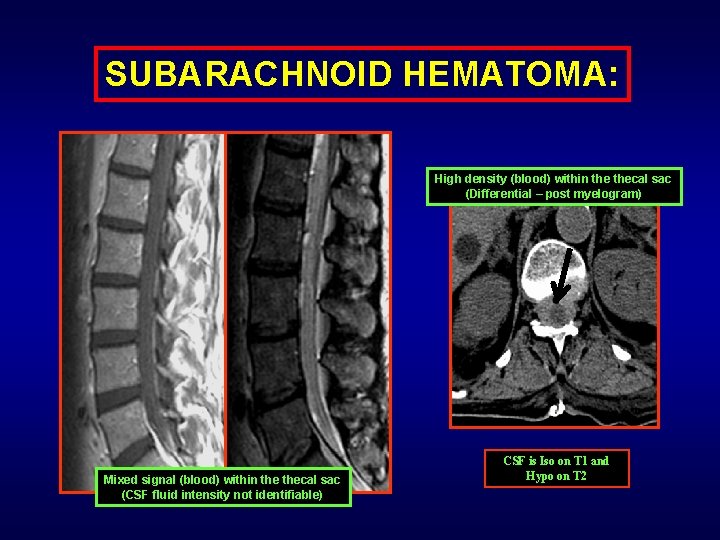
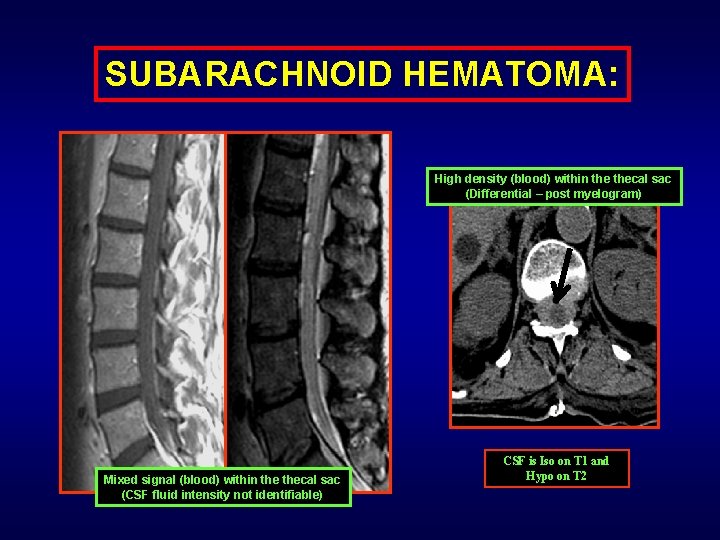
SUBARACHNOID HEMATOMA: High density (blood) within thecal sac (Differential – post myelogram) Mixed signal (blood) within thecal sac (CSF fluid intensity not identifiable) CSF is Iso on T 1 and Hypo on T 2
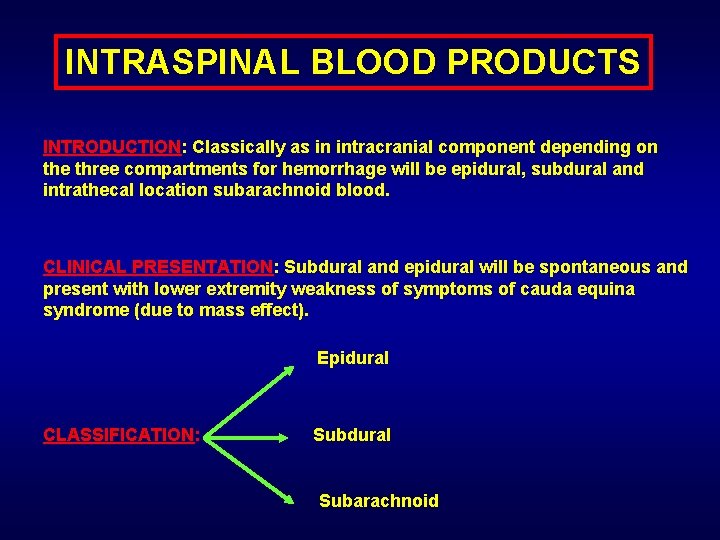
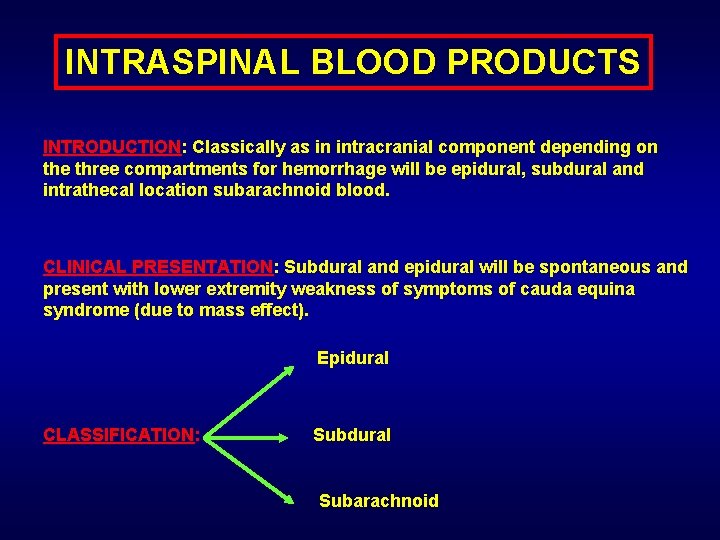
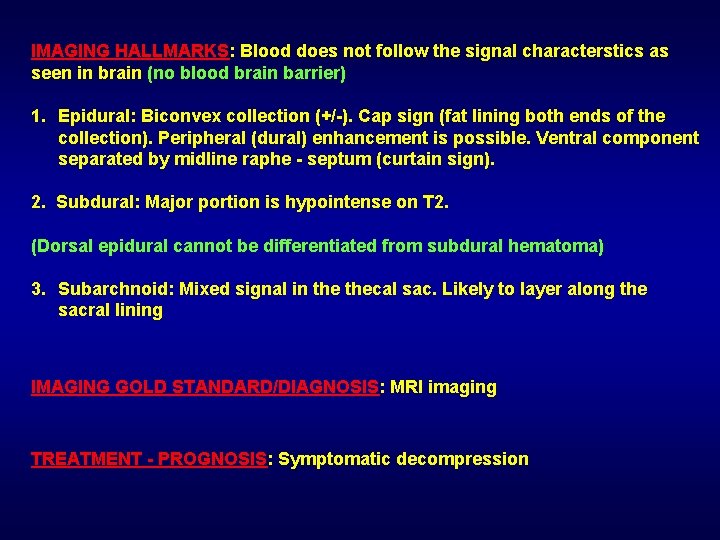
INTRASPINAL BLOOD PRODUCTS INTRODUCTION: Classically as in intracranial component depending on the three compartments for hemorrhage will be epidural, subdural and intrathecal location subarachnoid blood. CLINICAL PRESENTATION: Subdural and epidural will be spontaneous and present with lower extremity weakness of symptoms of cauda equina syndrome (due to mass effect). Epidural CLASSIFICATION: Subdural Subarachnoid
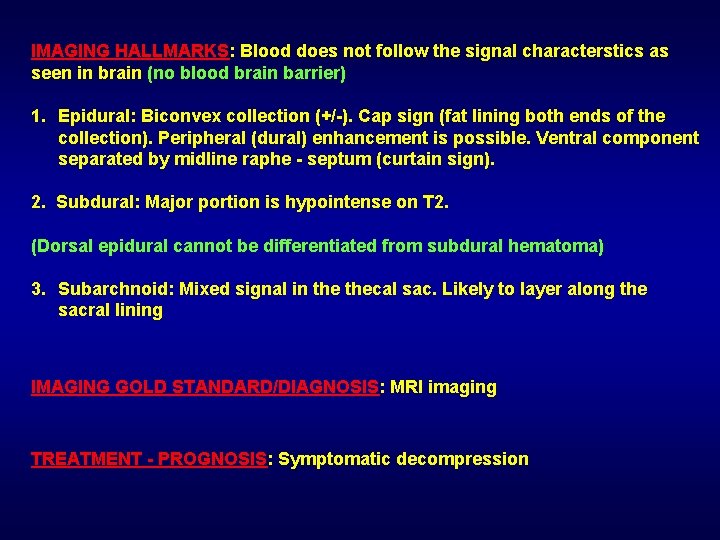
IMAGING HALLMARKS: Blood does not follow the signal characterstics as seen in brain (no blood brain barrier) 1. Epidural: Biconvex collection (+/-). Cap sign (fat lining both ends of the collection). Peripheral (dural) enhancement is possible. Ventral component separated by midline raphe - septum (curtain sign). 2. Subdural: Major portion is hypointense on T 2. (Dorsal epidural cannot be differentiated from subdural hematoma) 3. Subarchnoid: Mixed signal in thecal sac. Likely to layer along the sacral lining IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging TREATMENT - PROGNOSIS: Symptomatic decompression
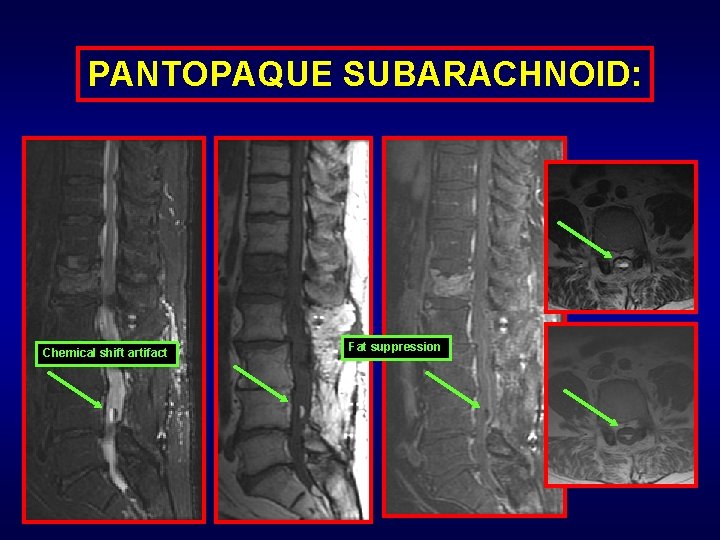
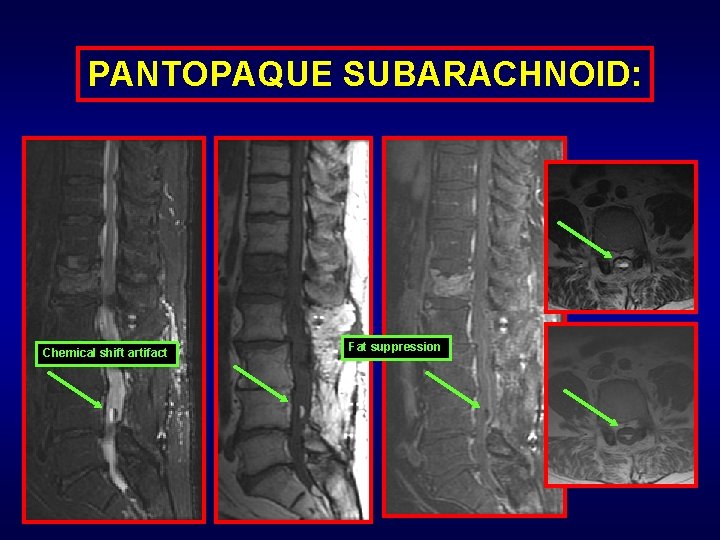
PANTOPAQUE SUBARACHNOID: Chemical shift artifact Fat suppression
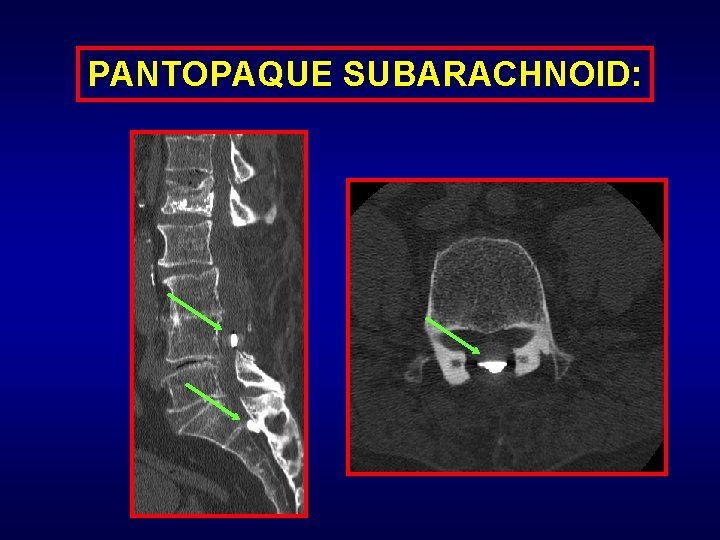
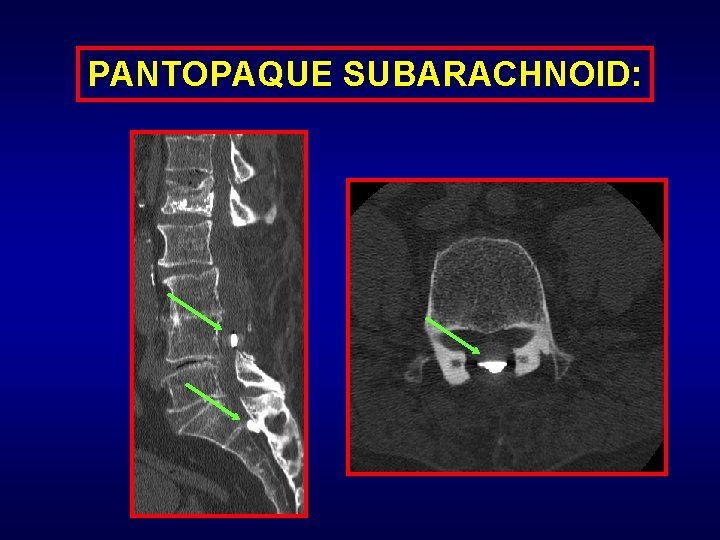
PANTOPAQUE SUBARACHNOID:

INFLAMMATORY AUTOIMMUNE GRANULOMATOUS:
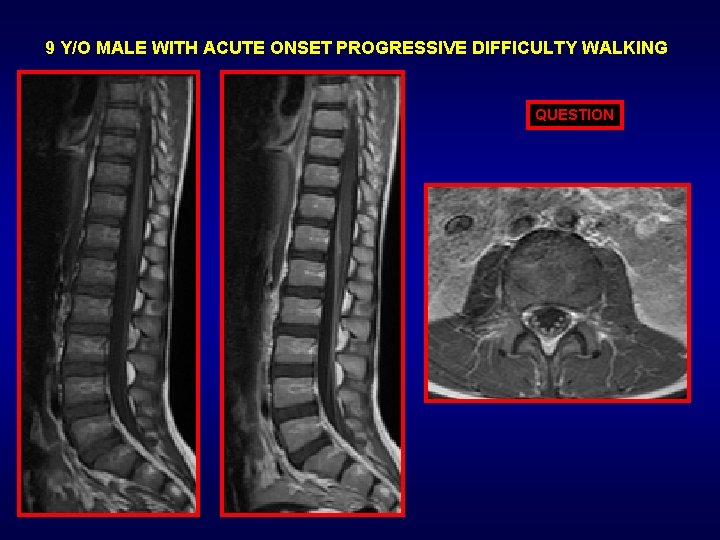
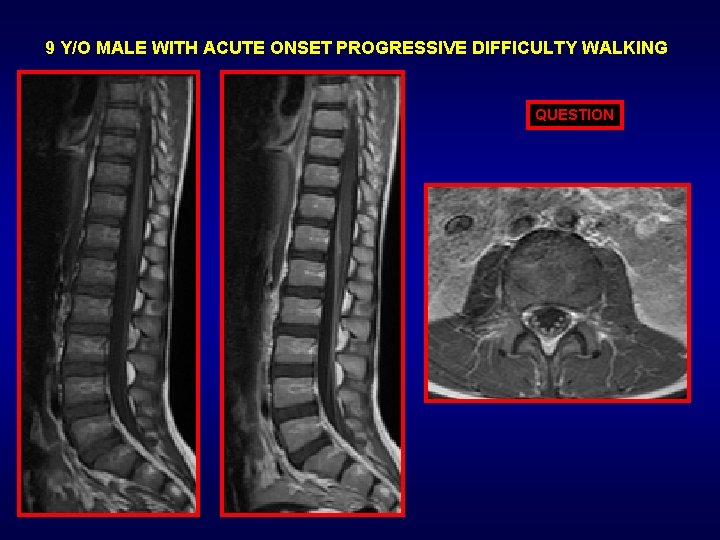
9 Y/O MALE WITH ACUTE ONSET PROGRESSIVE DIFFICULTY WALKING QUESTION
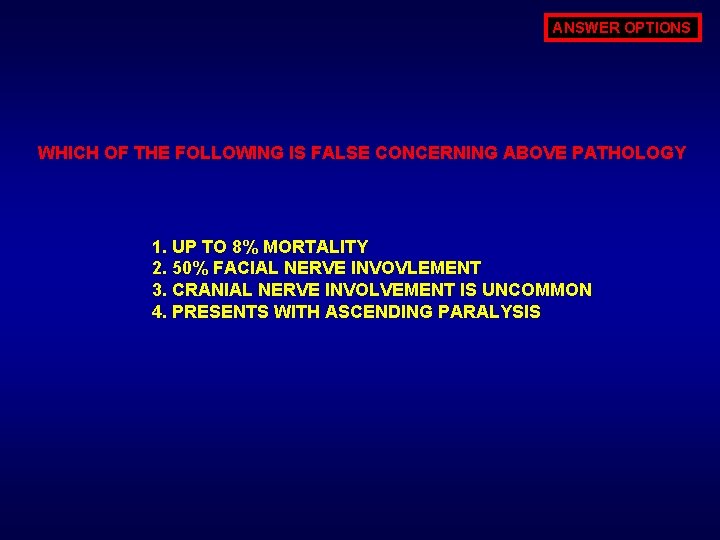
ANSWER OPTIONS WHICH OF THE FOLLOWING IS FALSE CONCERNING ABOVE PATHOLOGY 1. UP TO 8% MORTALITY 2. 50% FACIAL NERVE INVOVLEMENT 3. CRANIAL NERVE INVOLVEMENT IS UNCOMMON 4. PRESENTS WITH ASCENDING PARALYSIS
ANSWER CRANIAL NERVE INVOLVEMENT IS UNCOMMON: Cranial nerve is common. In fact facial nerve is invovled almost upto 50%
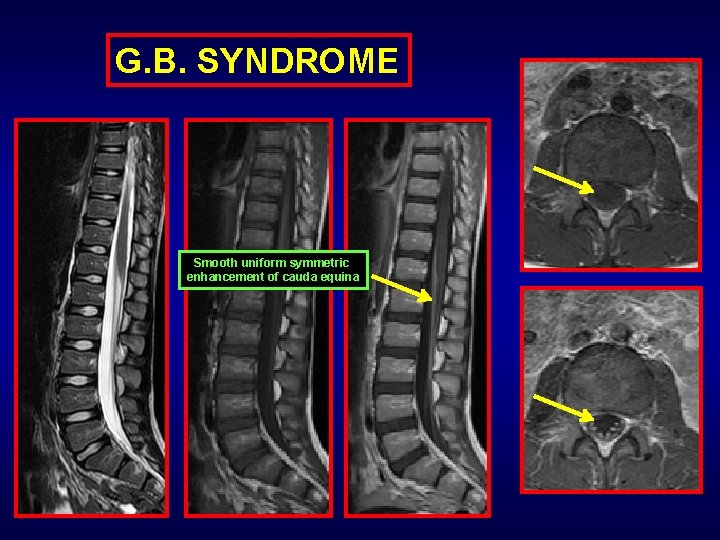
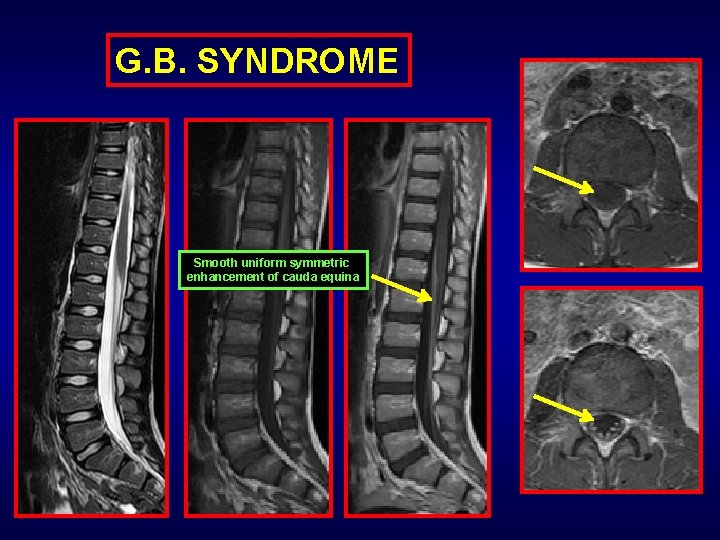
G. B. SYNDROME Smooth uniform symmetric enhancement of cauda equina
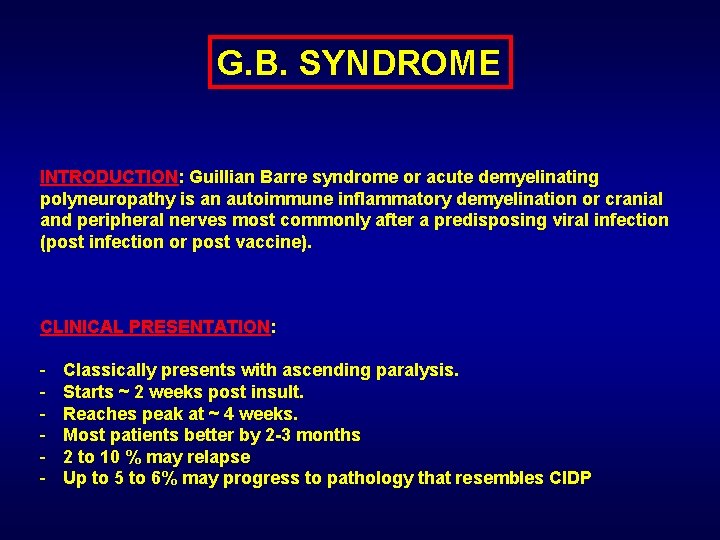
G. B. SYNDROME INTRODUCTION: Guillian Barre syndrome or acute demyelinating polyneuropathy is an autoimmune inflammatory demyelination or cranial and peripheral nerves most commonly after a predisposing viral infection (post infection or post vaccine). CLINICAL PRESENTATION: - Classically presents with ascending paralysis. Starts ~ 2 weeks post insult. Reaches peak at ~ 4 weeks. Most patients better by 2 -3 months 2 to 10 % may relapse Up to 5 to 6% may progress to pathology that resembles CIDP
IMAGING HALLMARKS: (CT is non diagnostic) - Smooth + uniform +/- minimally enlarged (typically not) nerve roots - No nodularity of the nerve roots - Avid enhancement of the cauda equina (+/- cranial nerves) - Variable enhancement of the pial lining of conus - Some sources claim (? ? ? ) – more prominent ventral nerve root enhancement.
IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging (final diagnosis by CSF evaluation) TREATMENT - PROGNOSIS: - Plasma exchange or IV Gamma-globulin - No proven data that steroids help - Some time supportive (breathing) therapy in severe cases - 2 to 10% may replase Up to 8% patient mortality 6% may progress to condition similar to CIDP

53 Y/O MALE WITH LOWER EXTRIMITY PARESTHESIAS QUESTION
ANSWER OPTIONS DIFFERNTIAL FOR THE ABOVE IMAGES INCLUDES ALL OF THE FOLLOWING EXCEPT? 1. LYMPHOMA 2. METASTASIS 3. GUILLIAN BARRE SYNDROME 4. SARCOID 5. ATYPICAL INFECTION (TUBERCULOSIS)
ANSWER GUILLIAN BARRE SYNDROME: G. B. syndrome typically presents as smooth, non-nodular, homogenous avid enhancement of the cauda equina and cranial nerves and not thickened nodular enhancement as in the images above
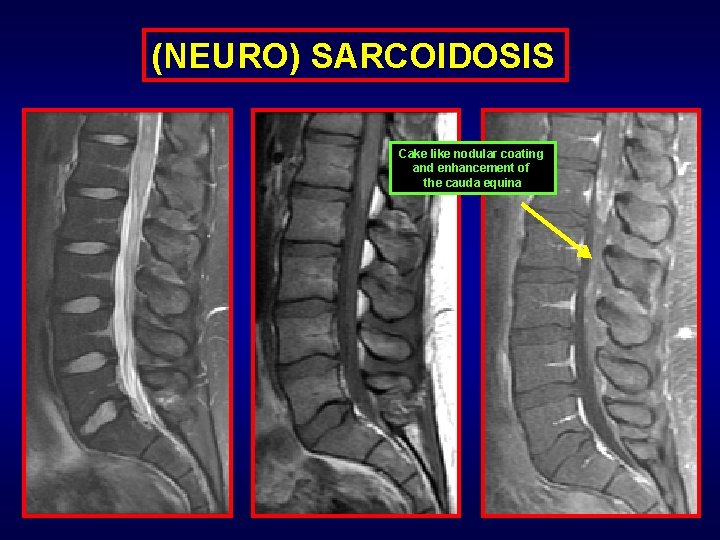
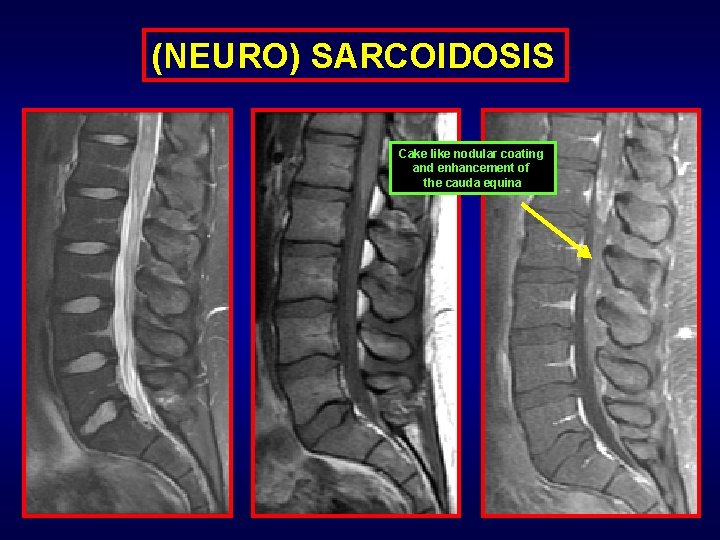
(NEURO) SARCOIDOSIS Cake like nodular coating and enhancement of the cauda equina
(NEURO) SARCOIDOSIS INTRODUCTION: Noncaseating granulomatous disease involving any organ system with almost 5% involvement of the central nervous system. CLINICAL PRESENTATION: - Lower extremity weakness - Paresthesias – radiculopathy - Bowel – bladder abnormalities (Essentially nonspecific neurological symptomatology) - Exclusive CNS involvement in only 1. 5% patients of sarcoid - 15 to 25% of sarcoid patients have CNS invovlemnt (on Autopsy findings)
IMAGING HALLMARKS: - Wide spectrum imaging findings (mimicking other disease processes) - When it involves cord: Long segment patchy mass like cord/conus enhancement - Nodular (but on rare occasions may be smooth) enhancement - Intramedullary as well as pial/surface enhancement - Cauda equina: Mass like or nodular (or on rare occasions smooth) patchy or diffuse cauda equina enhancement - Almost certain systemic disease involvement provides for better diagnosis and easy biopsy source When an enhancing pathology in any organ system spreads without respect to fat or tissue planes then differential would include but not be limited to sarcoidosis or lymphoma/leukemia or atypical granulomatous infections (like tuberculosis and fungal infections)
IMAGING GOLD STANDARD/DIAGNOSIS: MRI imaging (final diagnosis by CSF evaluation) TREATMENT - PROGNOSIS: - IV (+/- oral) corticosteroids. Immunosuppression therapy (Rarely) radiation therapy - Prognosis: Majority (roughly 60% patients) have a good response to steroid therapy Approximately 30% of the patients will have a relapse -
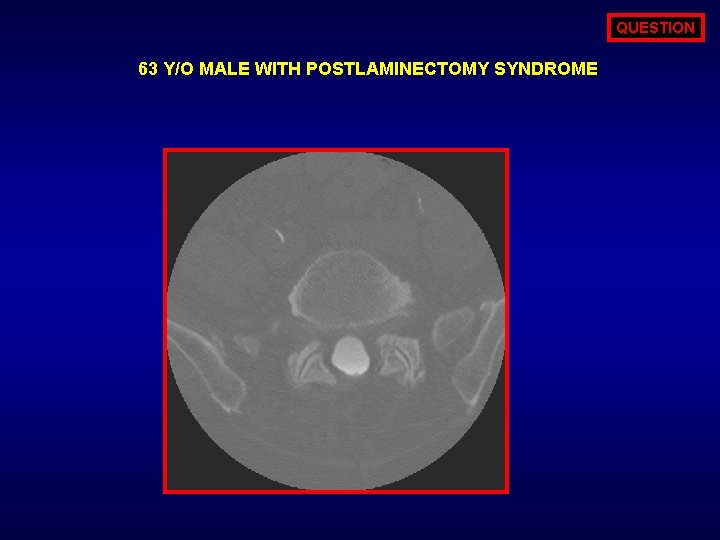
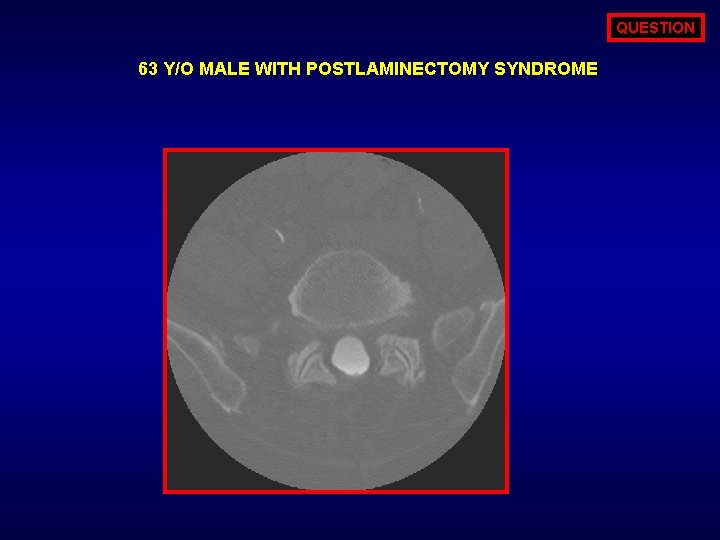
QUESTION 63 Y/O MALE WITH POSTLAMINECTOMY SYNDROME
ANSWER OPTIONS DIFFERNTIAL FOR THE ABOVE IMAGES INCLUDES ALL OF THE FOLLOWING EXCEPT? 1. LYMPHOMA 2. METASTASIS 3. GUILLIAN BARRE SYNDROME 4. SARCOID 5. ATYPICAL INFECTION (TUBERCULOSIS)
ANSWER GUILLIAN BARRE SYNDROME: G. B. syndrome typically presents as smooth, non-nodular, homogenous avid enhancement of the cauda equina and cranial nerves and not thickened nodular enhancement as in the images above
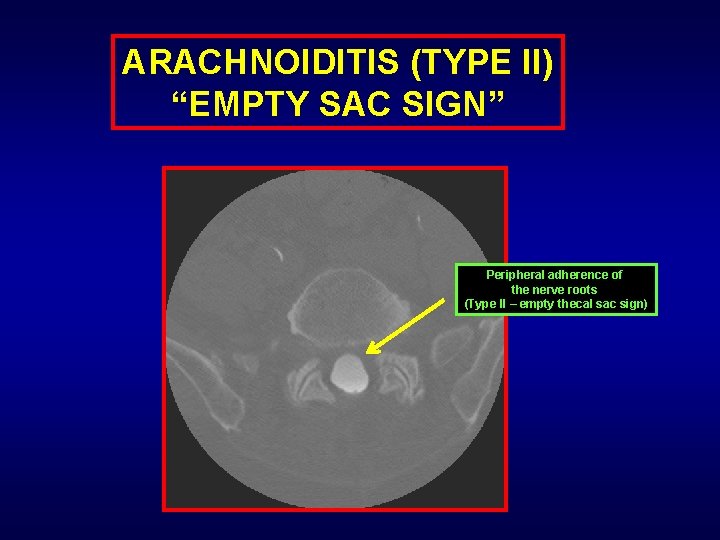
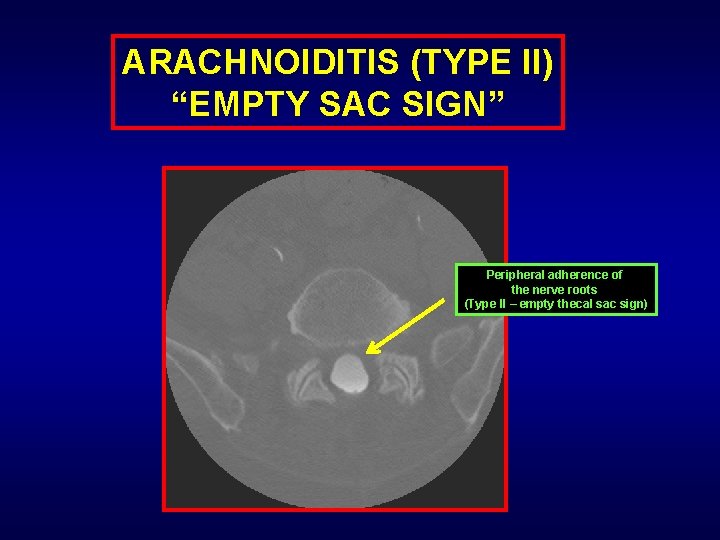
ARACHNOIDITIS (TYPE II) “EMPTY SAC SIGN” Peripheral adherence of the nerve roots (Type II – empty thecal sac sign)
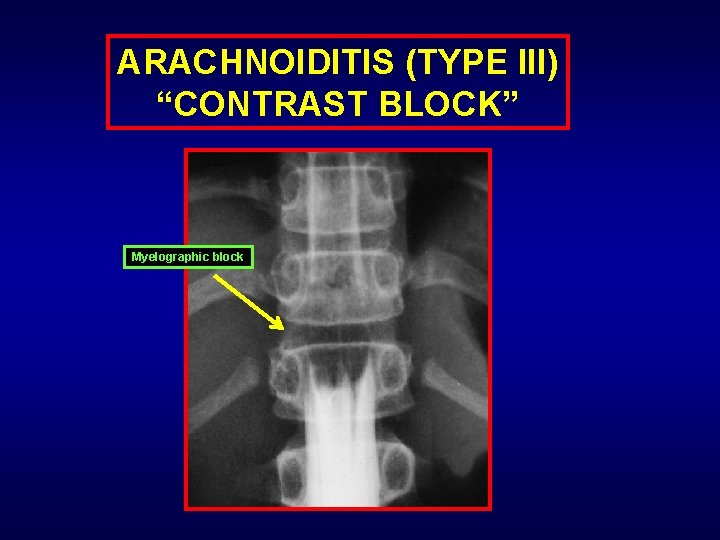
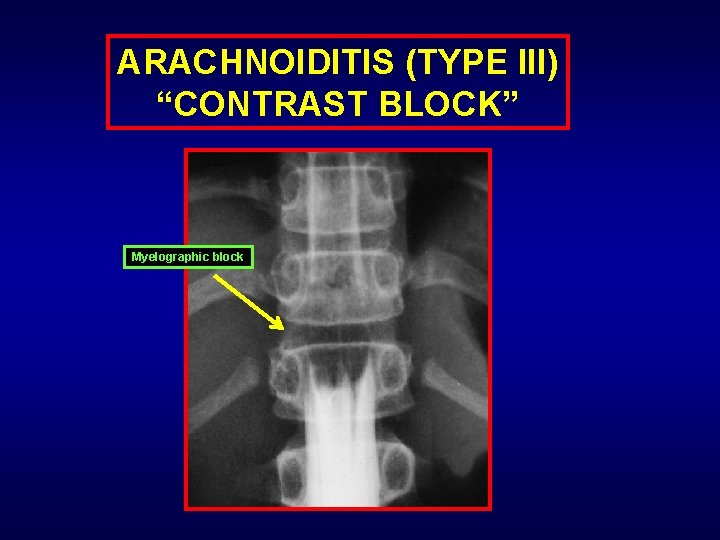
ARACHNOIDITIS (TYPE III) “CONTRAST BLOCK” Myelographic block
ARACHNOIDITIS INTRODUCTION: Post iatrogenic or infectious inflammatory scarring +/- adhesions or clumping of the nerve roots (cauda equina). CLINICAL PRESENTATION: Low back pain +/- lower extremity pain and paresthesias mimicking spinal stenosis or neurogenic claudication from spinal stenosis. Sometimes imaging findings may be present without clinical symptoms.
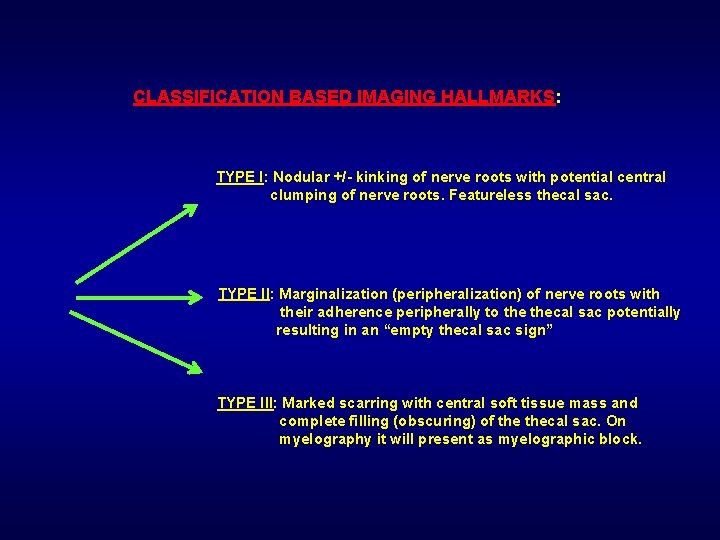
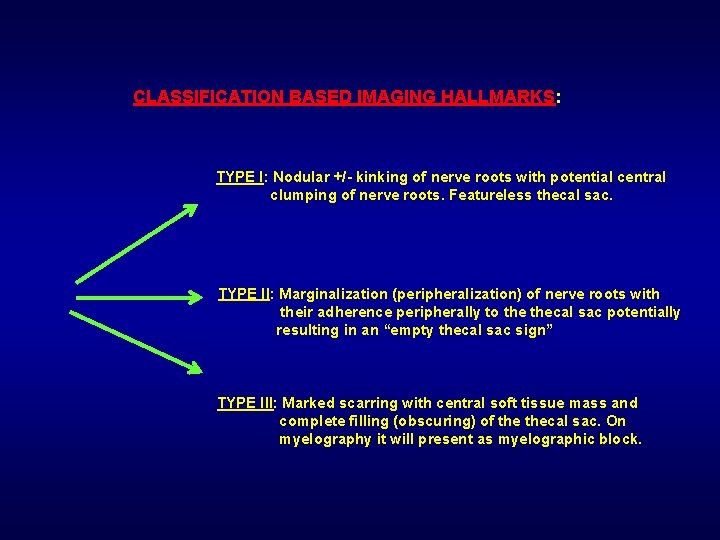
CLASSIFICATION BASED IMAGING HALLMARKS: TYPE I: Nodular +/- kinking of nerve roots with potential central clumping of nerve roots. Featureless thecal sac. TYPE II: Marginalization (peripheralization) of nerve roots with their adherence peripherally to thecal sac potentially resulting in an “empty thecal sac sign” TYPE III: Marked scarring with central soft tissue mass and complete filling (obscuring) of thecal sac. On myelography it will present as myelographic block.
IMAGING GOLD STANDARD/DIAGNOSIS: CT myelogram TREATMENT - PROGNOSIS: - No good treatment or cure Pain management is the approach: - Intrathecal steroid injections Spinal cord stimulators If possible release/lysis of adhesions If calcific/ossific arachnoiditis: Surgical resection of the portion (mostly not effective)
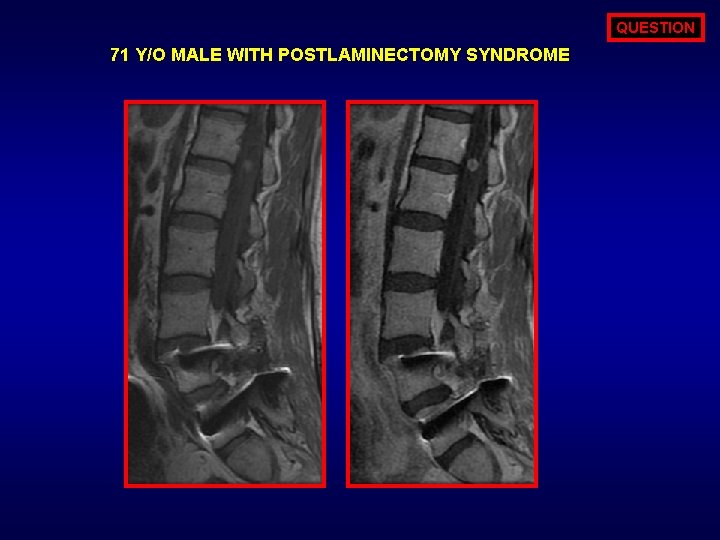
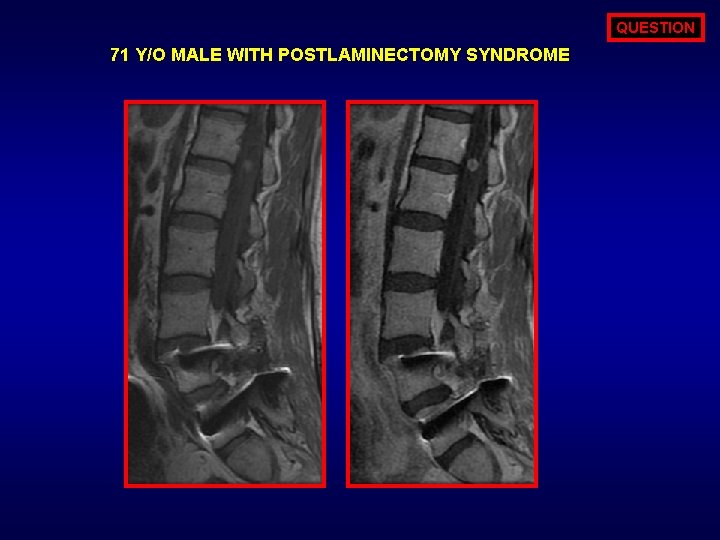
QUESTION 71 Y/O MALE WITH POSTLAMINECTOMY SYNDROME
ANSWER OPTIONS DIFFERNTIAL FOR THE ABOVE IMAGES INCLUDES ALL OF THE FOLLOWING EXCEPT? 1. SCHWANNOMA 2. METASTASIS (DROP) 3. NEUROFIBROMA 4. CIDP 5. MYXOPAILLARY EPENDYMOMA
ANSWER CIDP: Typically associated with diffuse cauda equina involvement with multiple bilateral nerve root marked thickening with +/- patchy enhancement
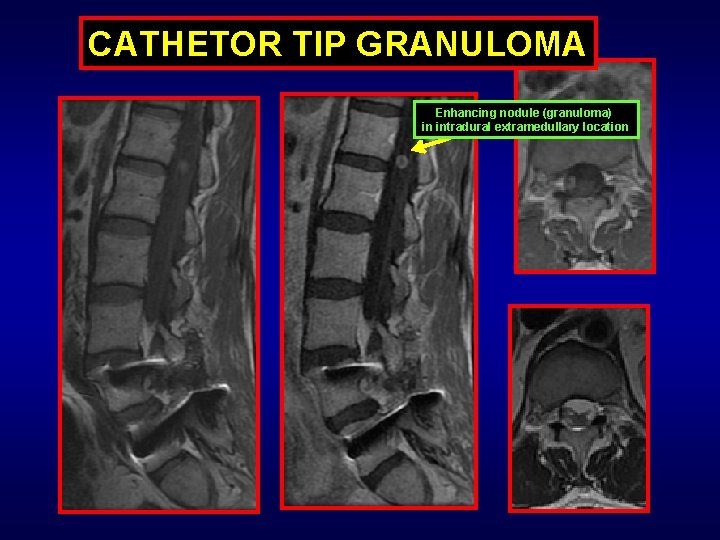
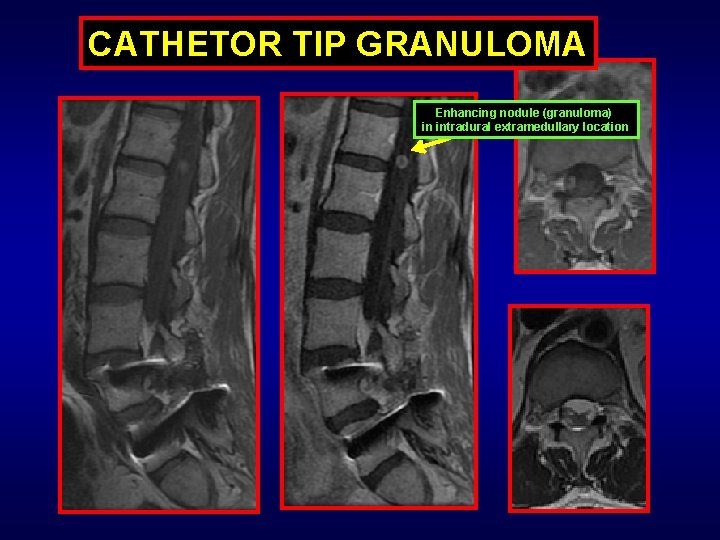
CATHETOR TIP GRANULOMA Enhancing nodule (granuloma) in intradural extramedullary location
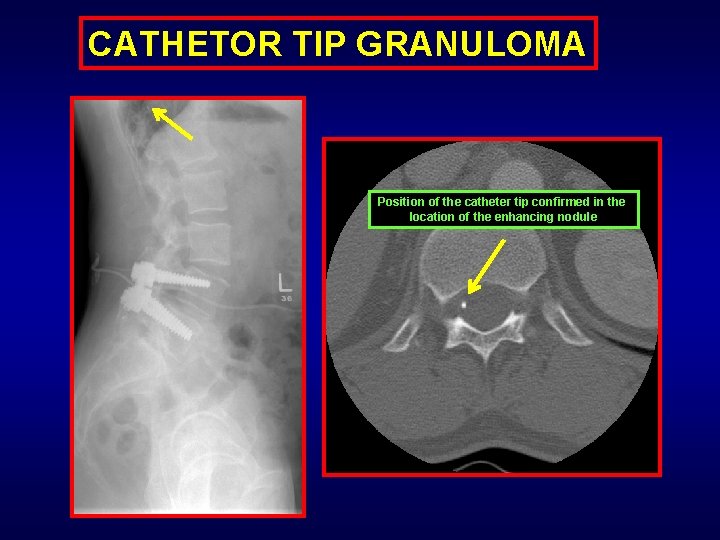
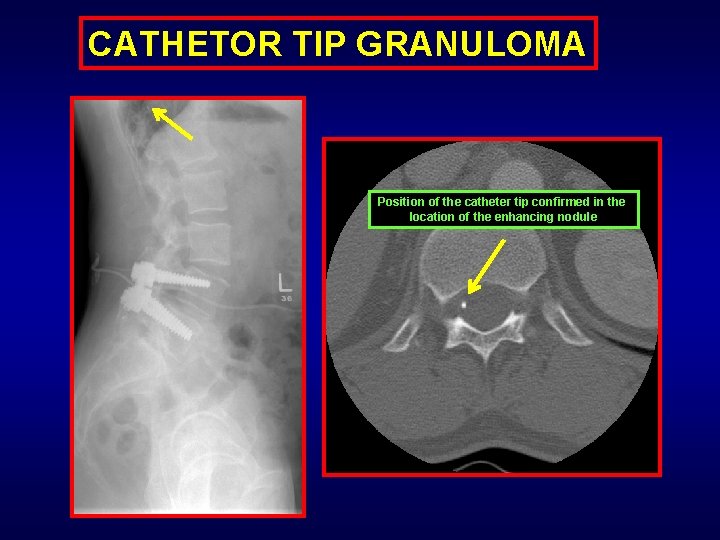
CATHETOR TIP GRANULOMA Position of the catheter tip confirmed in the location of the enhancing nodule
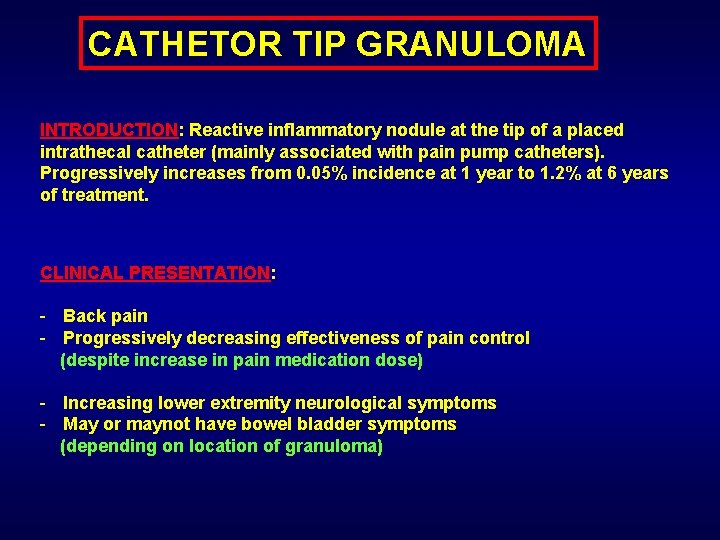
CATHETOR TIP GRANULOMA INTRODUCTION: Reactive inflammatory nodule at the tip of a placed intrathecal catheter (mainly associated with pain pump catheters). Progressively increases from 0. 05% incidence at 1 year to 1. 2% at 6 years of treatment. CLINICAL PRESENTATION: - Back pain - Progressively decreasing effectiveness of pain control (despite increase in pain medication dose) - Increasing lower extremity neurological symptoms - May or maynot have bowel bladder symptoms (depending on location of granuloma)
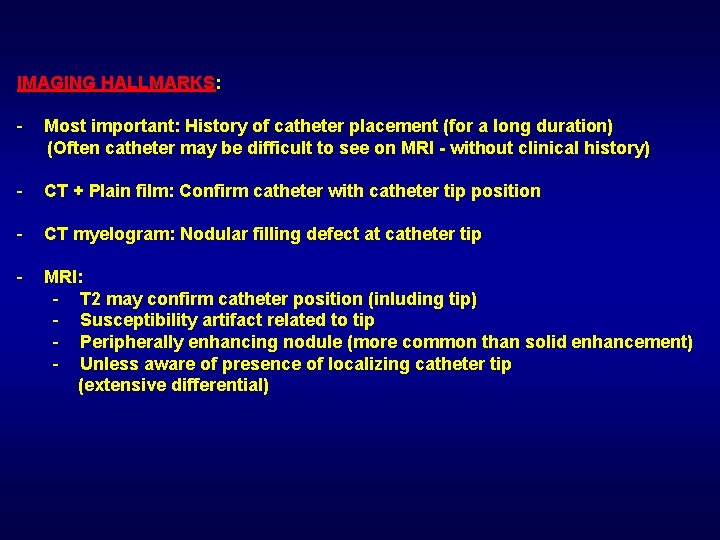
IMAGING HALLMARKS: - Most important: History of catheter placement (for a long duration) (Often catheter may be difficult to see on MRI - without clinical history) - CT + Plain film: Confirm catheter with catheter tip position - CT myelogram: Nodular filling defect at catheter tip - MRI: - T 2 may confirm catheter position (inluding tip) - Susceptibility artifact related to tip - Peripherally enhancing nodule (more common than solid enhancement) - Unless aware of presence of localizing catheter tip (extensive differential)
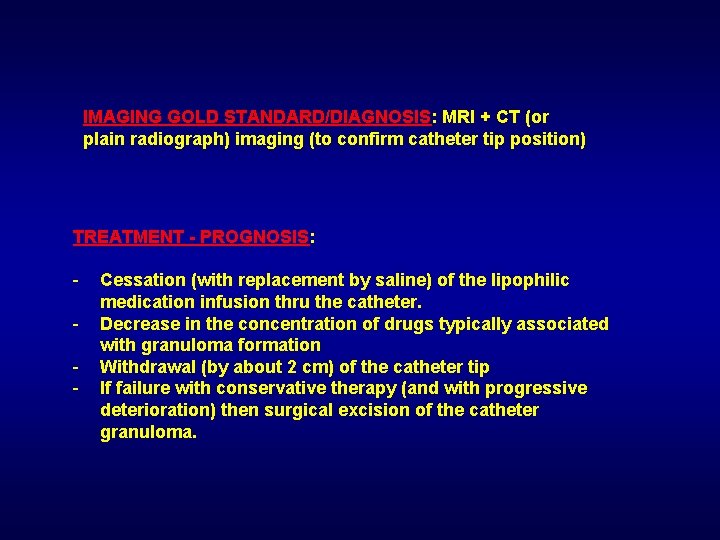
IMAGING GOLD STANDARD/DIAGNOSIS: MRI + CT (or plain radiograph) imaging (to confirm catheter tip position) TREATMENT - PROGNOSIS: - Cessation (with replacement by saline) of the lipophilic medication infusion thru the catheter. Decrease in the concentration of drugs typically associated with granuloma formation Withdrawal (by about 2 cm) of the catheter tip If failure with conservative therapy (and with progressive deterioration) then surgical excision of the catheter granuloma.
NEOPLASM - TUMOR:
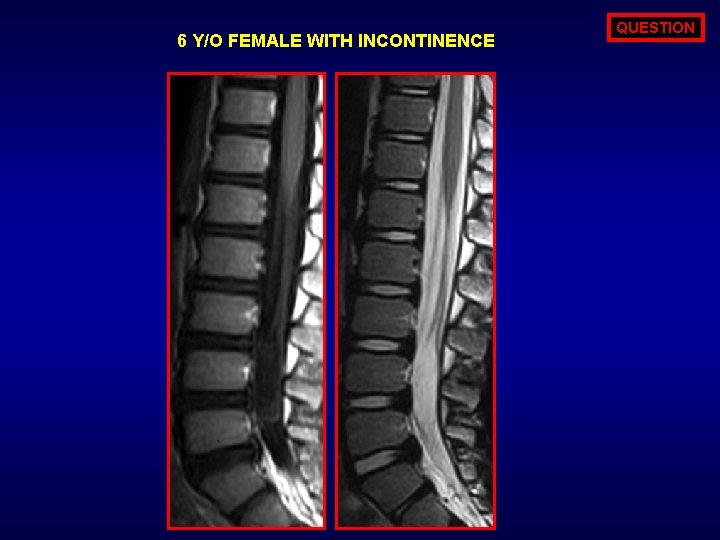
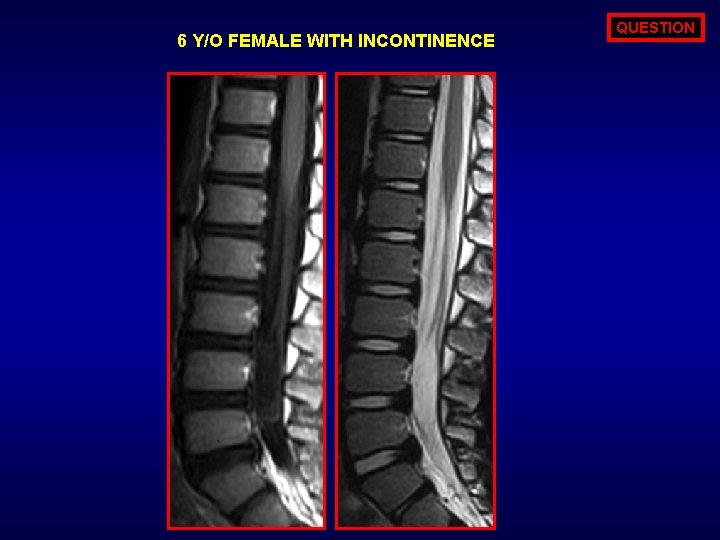
6 Y/O FEMALE WITH INCONTINENCE QUESTION
ANSWER OPTIONS ALL OF THE FOLLOWING ARE ASSOCIATED WITH THE DEPICTED ABNORMALITY EXCEPT? 1. DERMAL SINUS 2. STRUCTURAL VERTEBRAL BODY ANOMALIES 3. INTENSE ENHANCEMENT 4. RESTRICTED DIFFUSION
ANSWER ENHANCEMENT: Epidermoid (shown above) as well as dermoid will have minimal to no enhancement. All of the remaining are associations for an epidermoid which is shown above.
QUESTION ALL OF THE FOLLOWING ARE EXCLUSIVELY CONGENITAL IN ORIGIN EXCEPT? 1. DERMOID CYST 2. EPIDERMOID CYST 3. NEUROENTERIC CYST 4. LIPOMENIGOCELE CYST
EPIDERMOID CYST: Greater than 50% of the epidermoid cysts are congenital in nature with up to 40% of the cysts being acquired (from iatrogenic reasons).
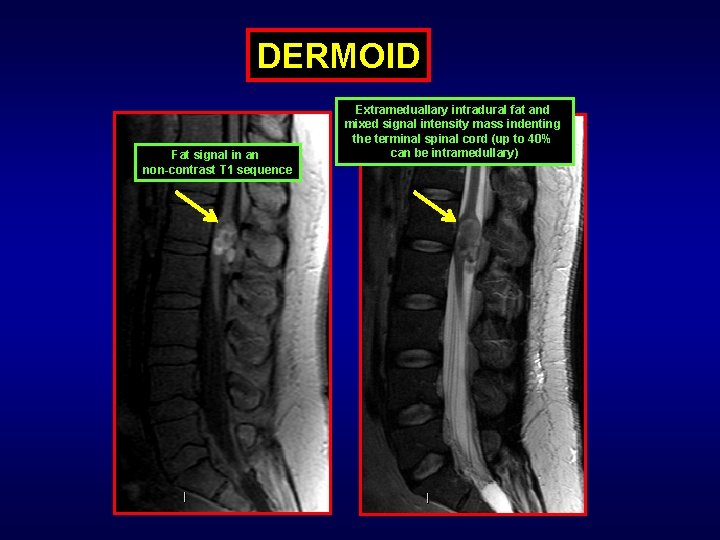
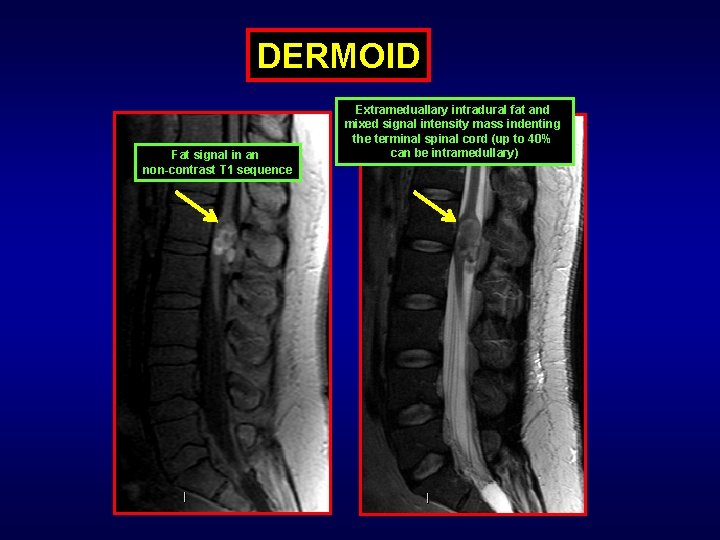
DERMOID Fat signal in an non-contrast T 1 sequence Extrameduallary intradural fat and mixed signal intensity mass indenting the terminal spinal cord (up to 40% can be intramedullary)
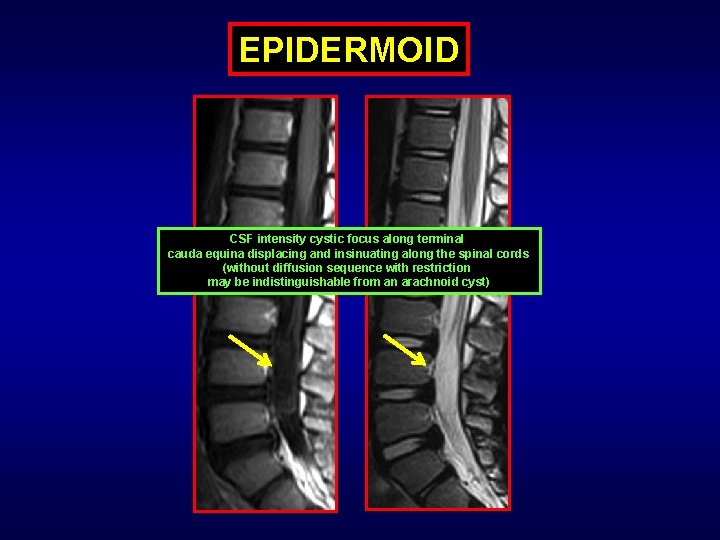
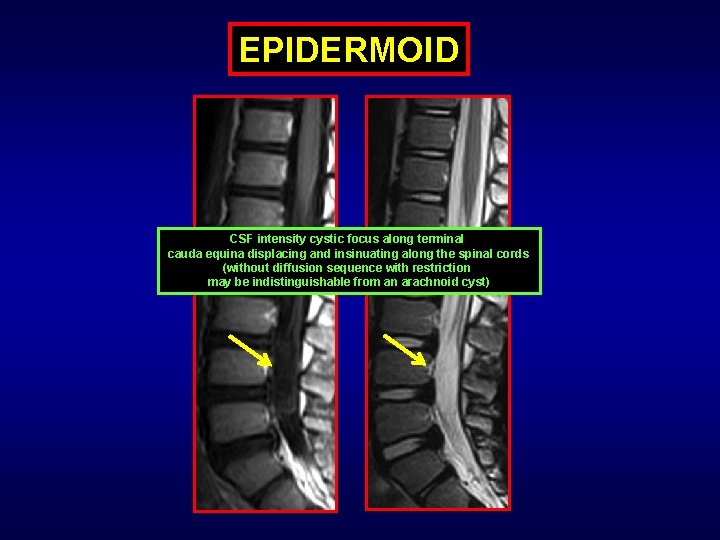
EPIDERMOID CSF intensity cystic focus along terminal cauda equina displacing and insinuating along the spinal cords (without diffusion sequence with restriction may be indistinguishable from an arachnoid cyst)
DERMOID – EPIDERMOID - TERATOMA INTRODUCTION: Tumors of ectodermal origin which may arise mainly along the midline or para-midline region from inclusion rest cells progressing to mass like nodular formation that tend to remain benign. CLINICAL PRESENTATION: - Frequently asymptomatic with incidental detection - Gradually increasing radiculopathy/myelopathy (Due to mass effect) - Late: Cauda equina syndrome - Chemical meningitis (with dermoid secondary to rupture) - Infectious meningitis (if associated with dermal sinus)
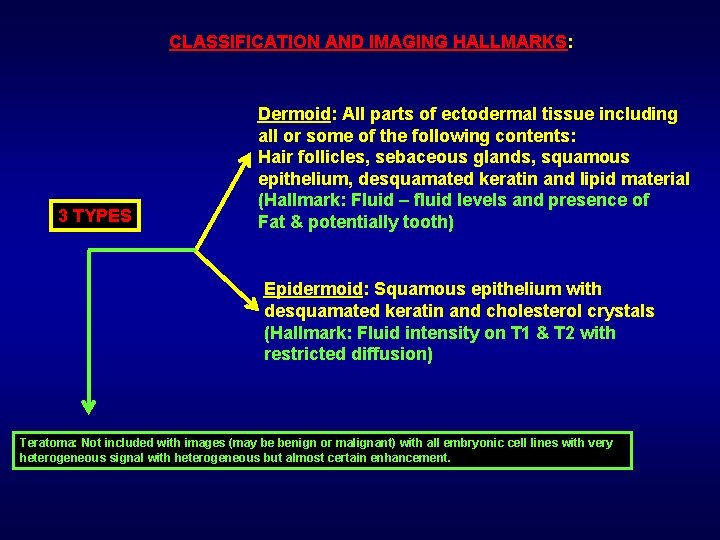
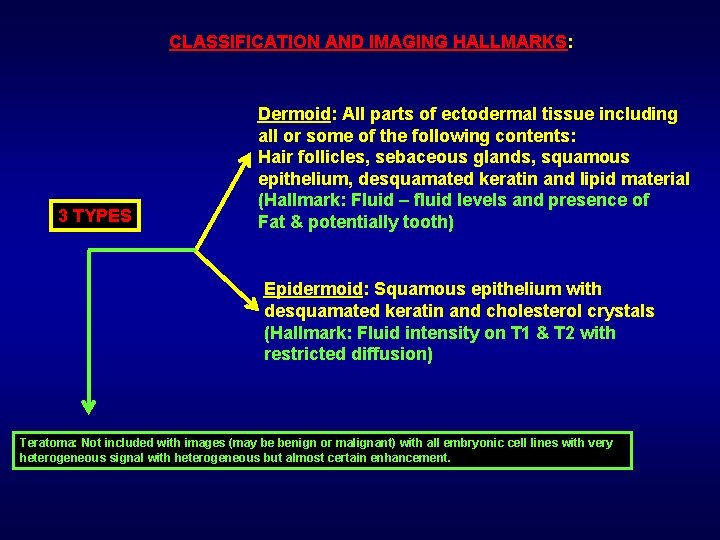
CLASSIFICATION AND IMAGING HALLMARKS: 3 TYPES Dermoid: All parts of ectodermal tissue including all or some of the following contents: Hair follicles, sebaceous glands, squamous epithelium, desquamated keratin and lipid material (Hallmark: Fluid – fluid levels and presence of Fat & potentially tooth) Epidermoid: Squamous epithelium with desquamated keratin and cholesterol crystals (Hallmark: Fluid intensity on T 1 & T 2 with restricted diffusion) Teratoma: Not included with images (may be benign or malignant) with all embryonic cell lines with very heterogeneous signal with heterogeneous but almost certain enhancement.
IMAGING GOLD STANDARD/DIAGNOSIS: MRI TREATMENT - PROGNOSIS: - Surgical complete resection If incomplete resection: Will recur
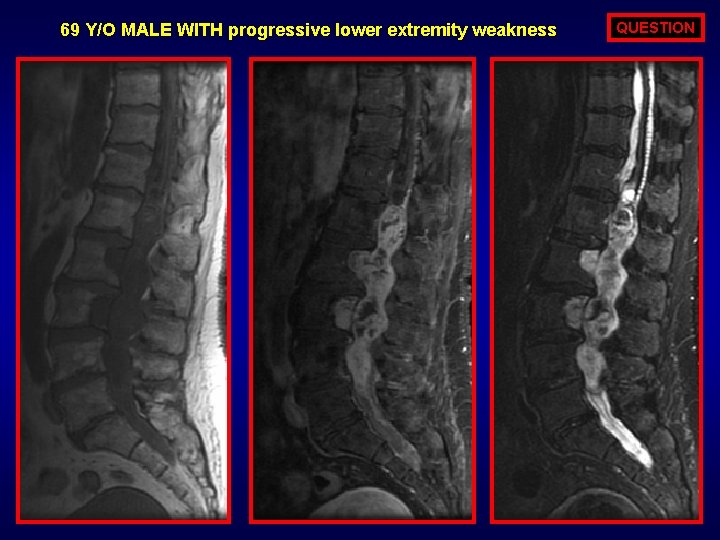
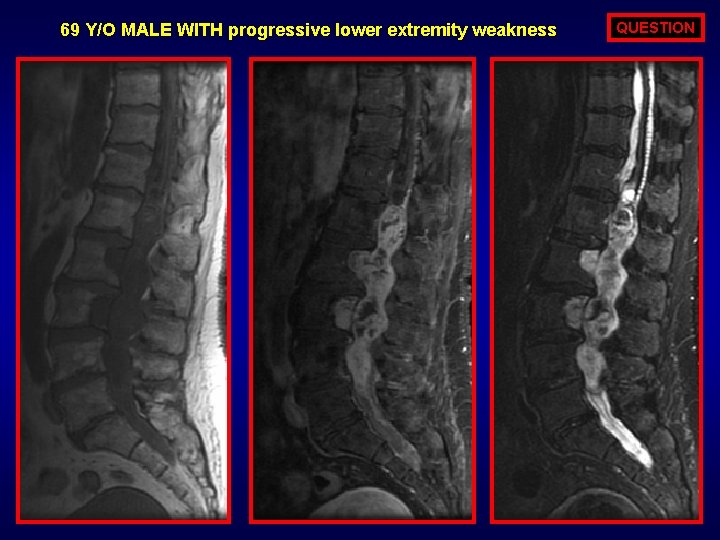
69 Y/O MALE WITH progressive lower extremity weakness QUESTION
ANSWER OPTIONS SPINAL ENTITY DEPICTED ABOVE IS MORE COMMON IN FEMALES? 1. TRUE 2. FALSE
ANSWER FALSE: Shown entity is an myxopapillary ependymoma which is (2: 1 preponderance) more common in males.
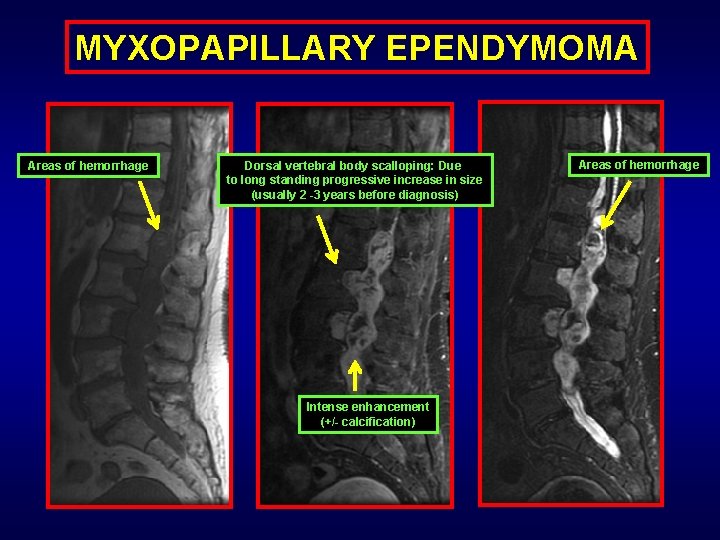
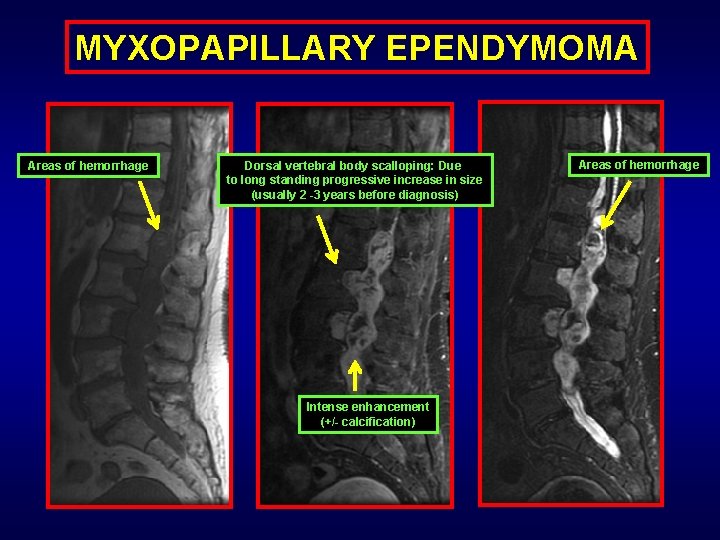
MYXOPAPILLARY EPENDYMOMA Areas of hemorrhage Dorsal vertebral body scalloping: Due to long standing progressive increase in size (usually 2 -3 years before diagnosis) Intense enhancement (+/- calcification) Areas of hemorrhage
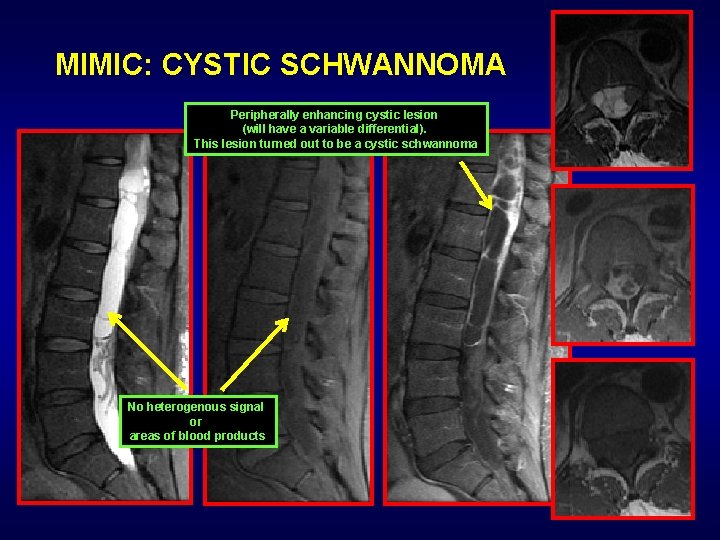
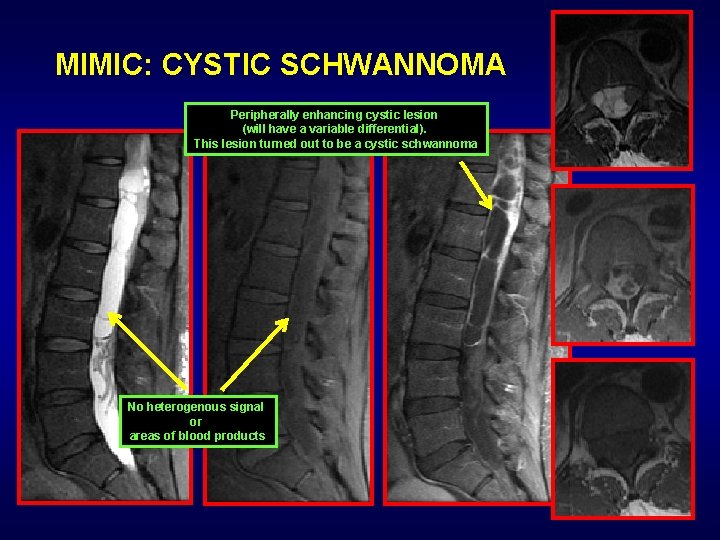
MIMIC: CYSTIC SCHWANNOMA Peripherally enhancing cystic lesion (will have a variable differential). This lesion turned out to be a cystic schwannoma No heterogenous signal or areas of blood products
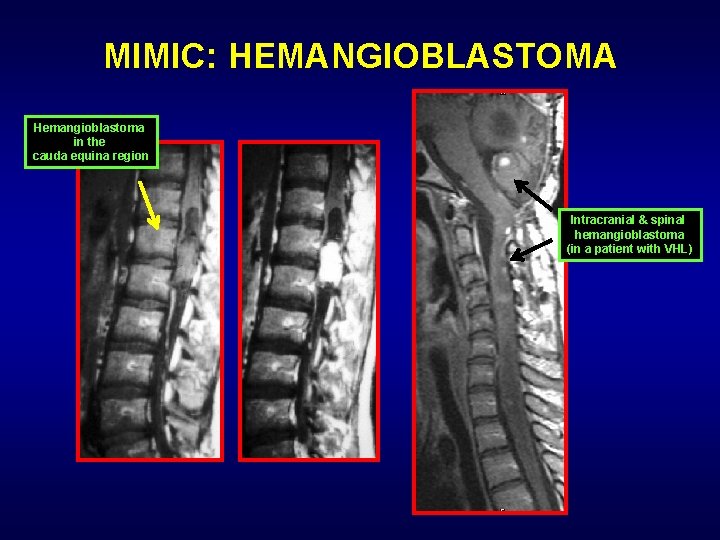
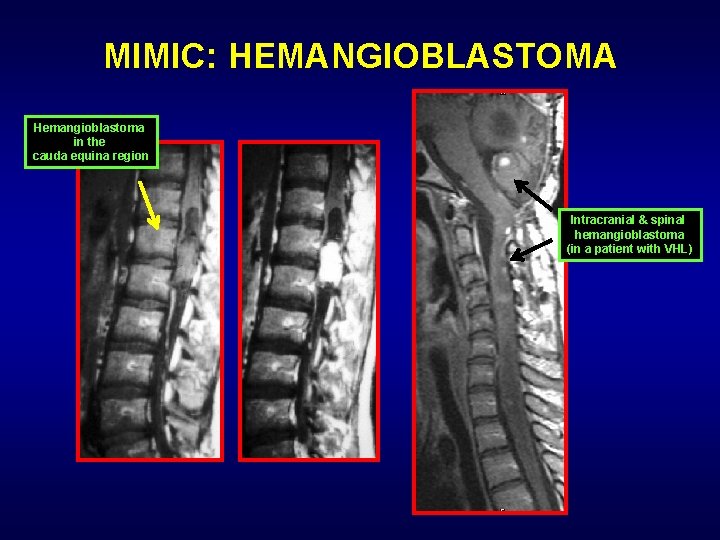
MIMIC: HEMANGIOBLASTOMA Hemangioblastoma in the cauda equina region Intracranial & spinal hemangioblastoma (in a patient with VHL)
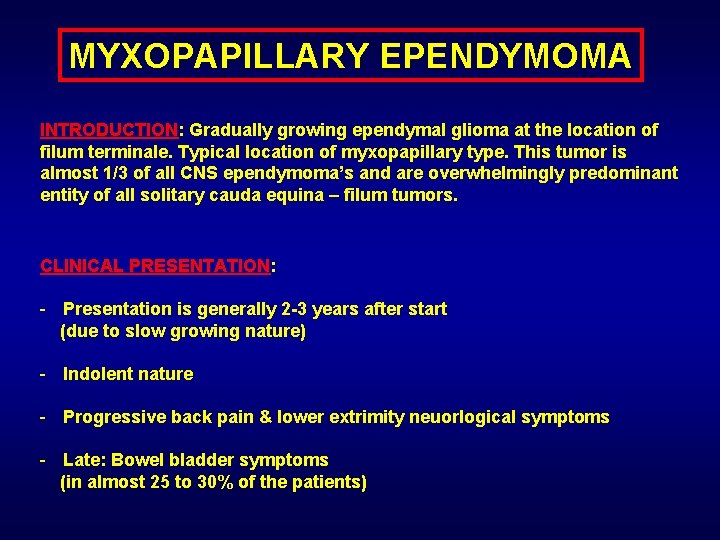
MYXOPAPILLARY EPENDYMOMA INTRODUCTION: Gradually growing ependymal glioma at the location of filum terminale. Typical location of myxopapillary type. This tumor is almost 1/3 of all CNS ependymoma’s and are overwhelmingly predominant entity of all solitary cauda equina – filum tumors. CLINICAL PRESENTATION: - Presentation is generally 2 -3 years after start (due to slow growing nature) - Indolent nature - Progressive back pain & lower extrimity neuorlogical symptoms - Late: Bowel bladder symptoms (in almost 25 to 30% of the patients)
IMAGING HALLMARKS: - Heterogenously avidly enhancing soft tissue insinuating mass - Intradural and extramedullary in location - Usually spans > 2 vertebral bodies (at presentation) - Can see (+/-) flow voids - May have terminal cord signal changes - Common to have hemorrhage - Dorsal vertebral body scalloping with larger lesions

IMAGING GOLD STANDARD/DIAGNOSIS: MRI + Contrast TREATMENT - PROGNOSIS: - Surgical resection - Radiotherapy for recurrence and residual tumors

QUESTION 30 Y/O MALE with melanoma for staging
ANSWER OPTIONS DROP METASTASIS ARE SEEN CLASICALLY WITH? 1. 2. 3. 4. ANAPLASTIC ASTROCYTOMA MEDULLOBLASTOMA DYSEMBROPLASTIC INFANTILE GLIOMA MENINGIOMA
ANSWER MEDULLOBLASTOMA: High grade exophytic tumors of intracranial location can be associated with drop metastasis. Typically seen with ependymoma and medulloblastoma and choroid plexus papillary carcinoma.
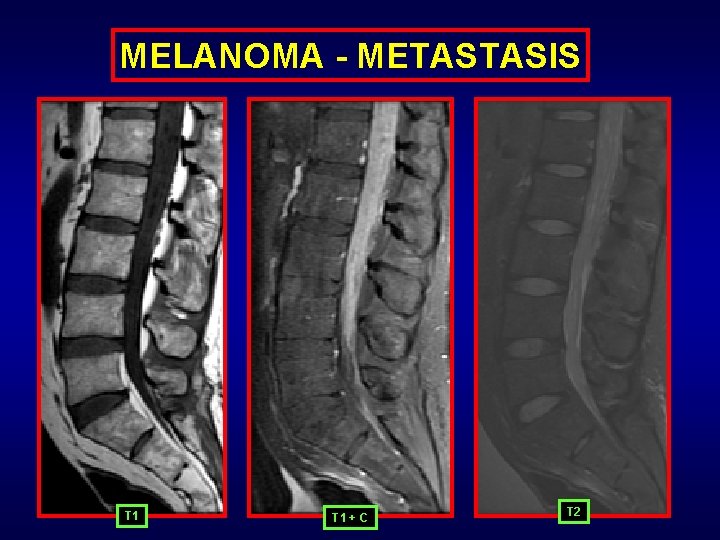
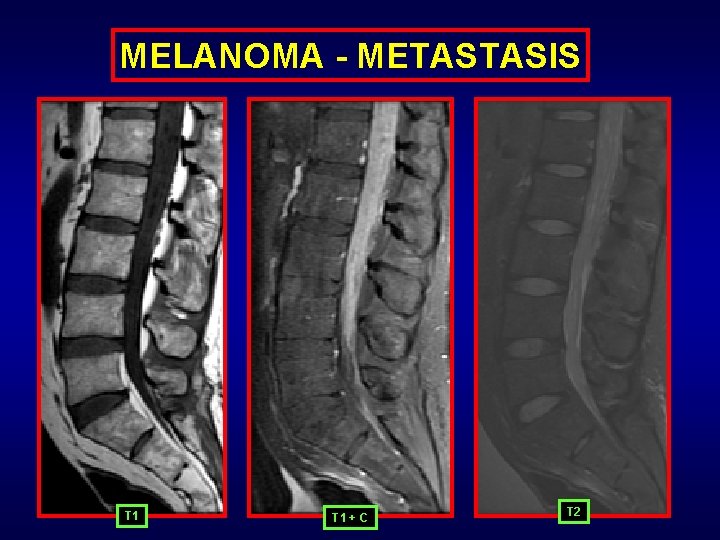
MELANOMA - METASTASIS T 1 + C T 2
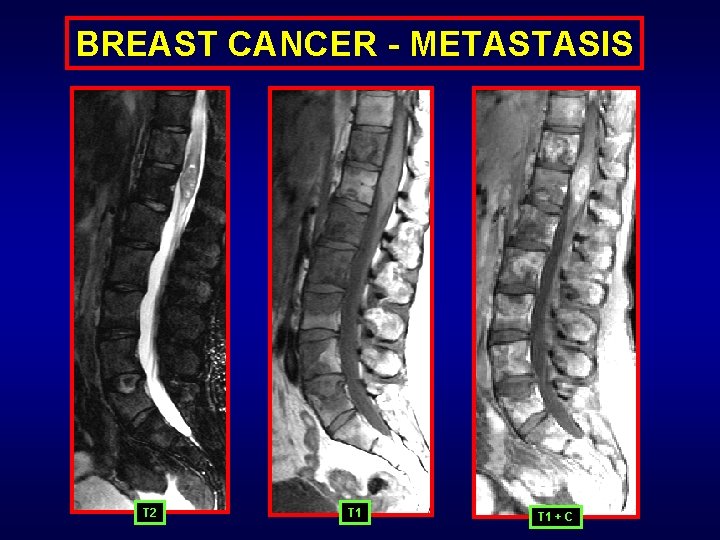
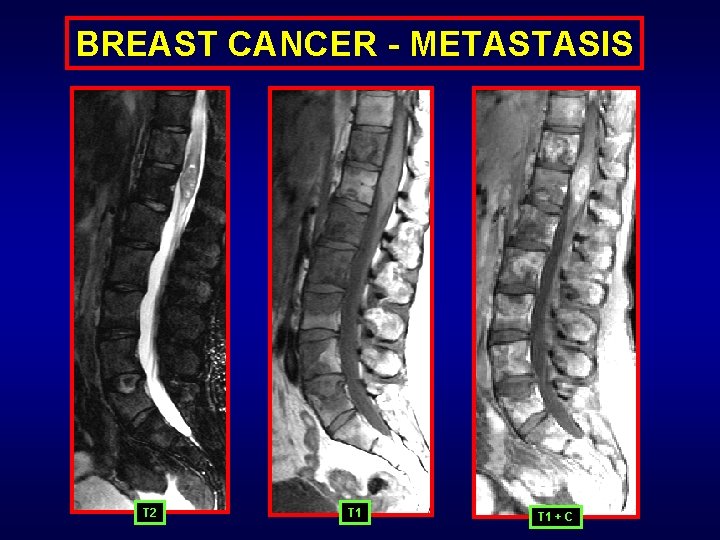
BREAST CANCER - METASTASIS T 2 T 1 + C
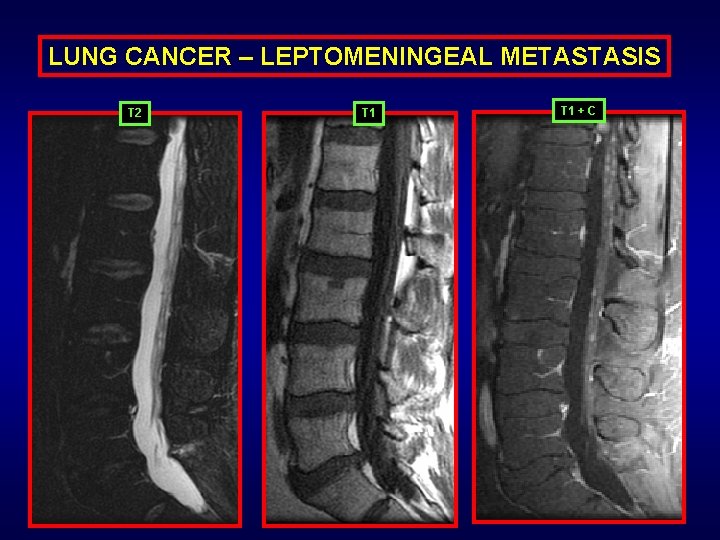
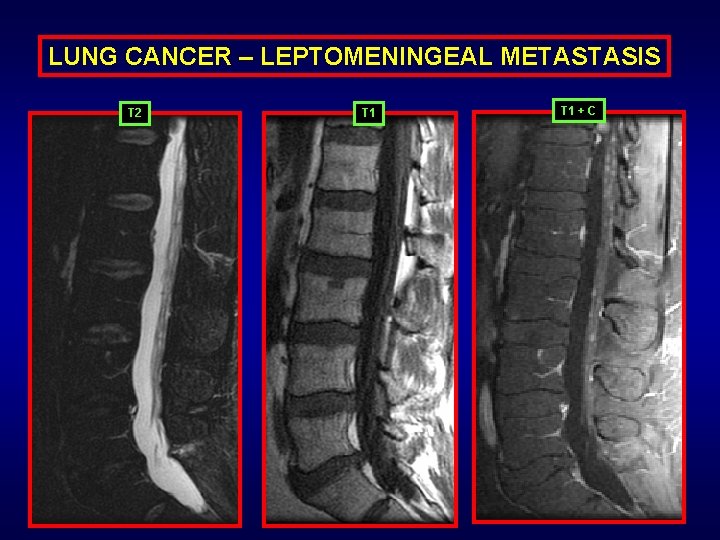
LUNG CANCER – LEPTOMENINGEAL METASTASIS T 2 T 1 + C
FILUM METASTATIC DISEASE INTRODUCTION: Intradural metastasis can spread via hematomgenous route or contiguous route or as drop CSF dissemination from intracranial tumors. Once it lodges to the pia-arachnoid or dural ling it drops the prognosis of the patient (even with treatment) significantly. Alternatively vertebral body (extradural – extramedullary [extra osseous] cancer – metastasis may affect the cauda equina with compression due to vertebral collapse or soft tissue component with epidural extension. CLINICAL PRESENTATION: - Mainly detected on staging - Rare to primarily present with cauda equina metastasis
IMAGING HALLMARKS: - Smooth or nodular (typically) enhancement of the cauda equina and the cord surface - May or may not be associated with underlying cord edema - Frequently associated with metastasis of the vertebral bodies, retroperitoneum, intracranial region as well as the spinal cord - Biggest indicator: Multiplicity of lesions EXTENSIVE DIFERENTIAL: - Hematogenous spread of infection - Granulomatous disease - Lymphoma/leukemia - Multiple nerve sheath tumors
IMAGING GOLD STANDARD/DIAGNOSIS: 1. LP and CSF evaluation are the gold standard. 2. Imaging gold standard will be MRI with contrast. TREATMENT - PROGNOSIS: - Intrathecal rounds of chemotherapy - Radiation PROGNOSIS: Extremely poor: Terminal stage of cancer with 5% patients presenting with it. Survival of less than ~3 months with aggressive treatment.
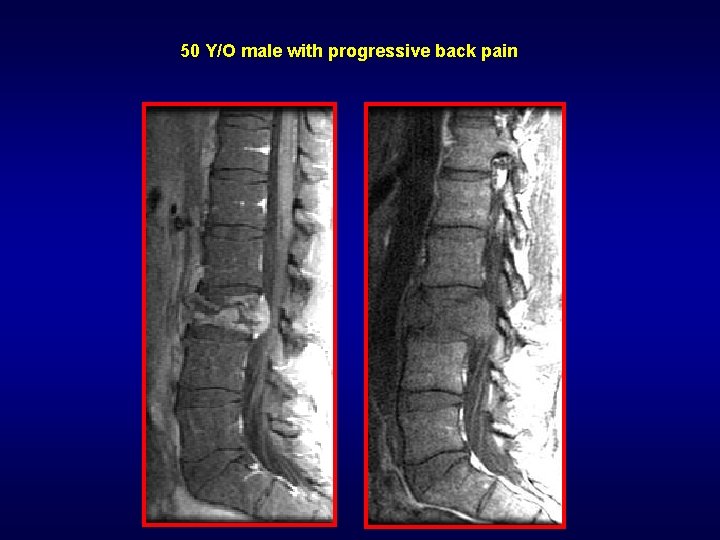
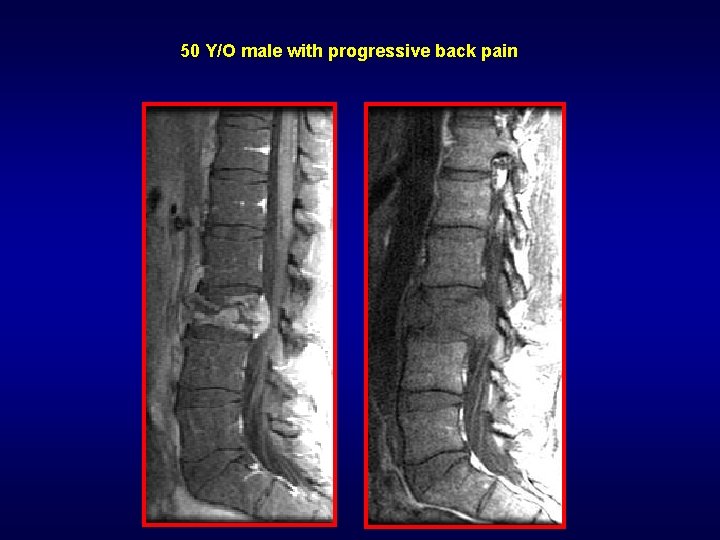
50 Y/O male with progressive back pain
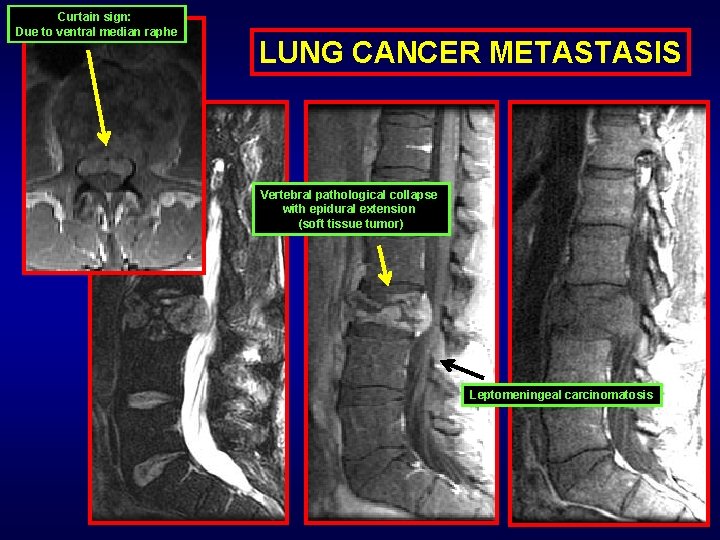
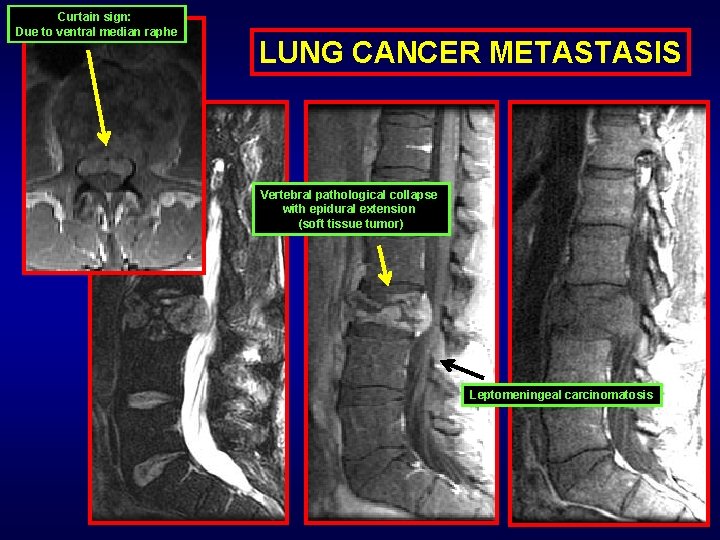
Curtain sign: Due to ventral median raphe LUNG CANCER METASTASIS Vertebral pathological collapse with epidural extension (soft tissue tumor) Leptomeningeal carcinomatosis
VASCULAR:
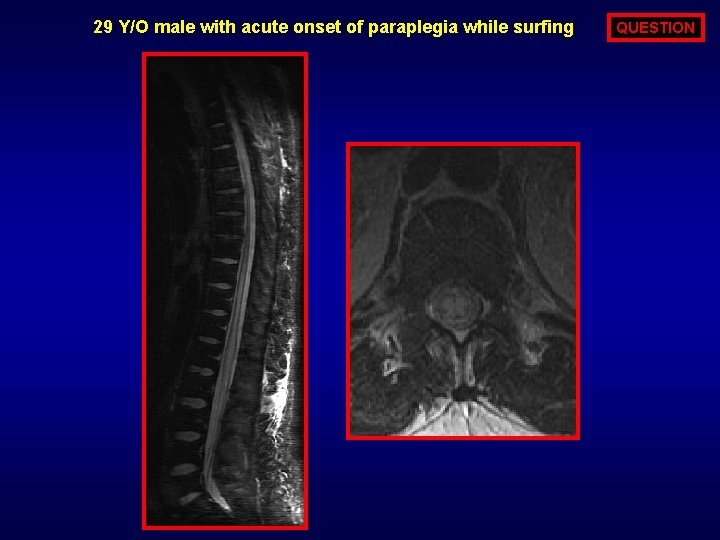
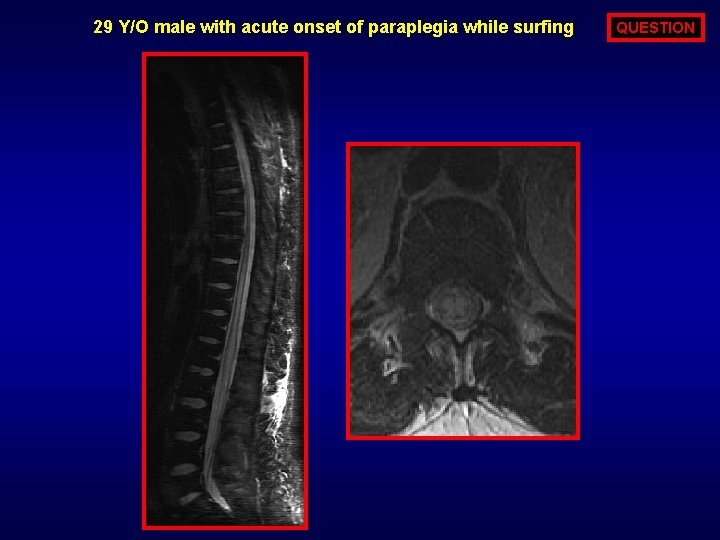
29 Y/O male with acute onset of paraplegia while surfing QUESTION
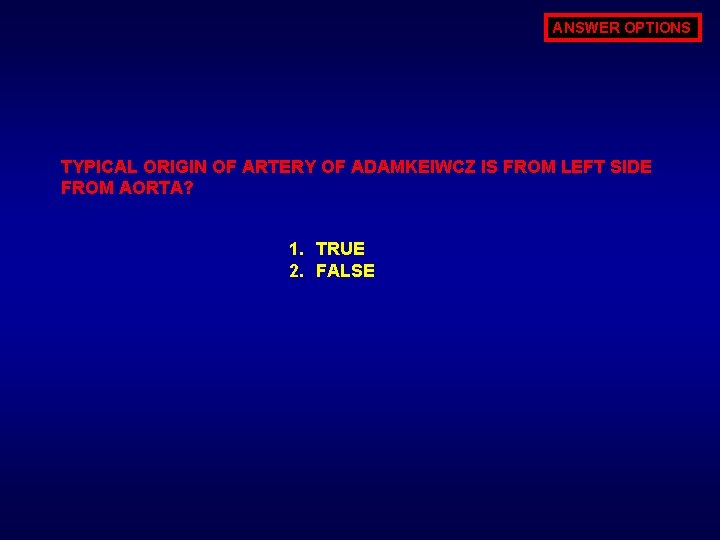
ANSWER OPTIONS TYPICAL ORIGIN OF ARTERY OF ADAMKEIWCZ IS FROM LEFT SIDE FROM AORTA? 1. TRUE 2. FALSE
ANSWER TRUE: Artery of Adamkeiwcz typically arises from left side of aorta between T 9 to T 12 levels from the left side with a classic hair-pin “U” turn of the vessel at its entry into the spinal canal
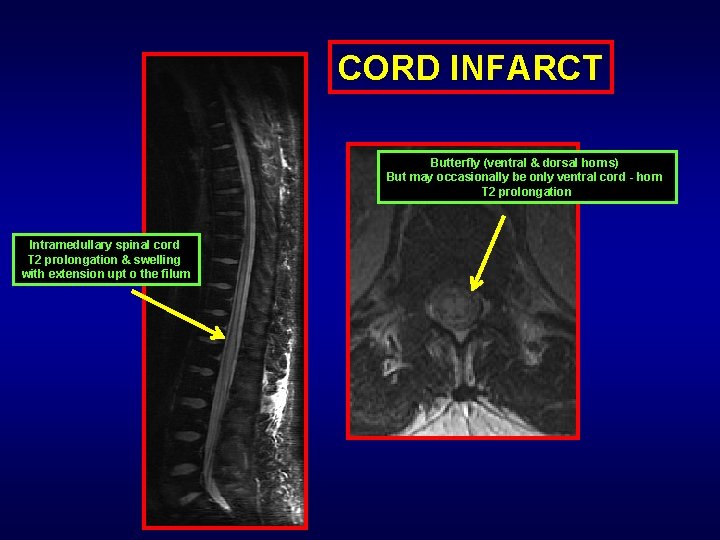
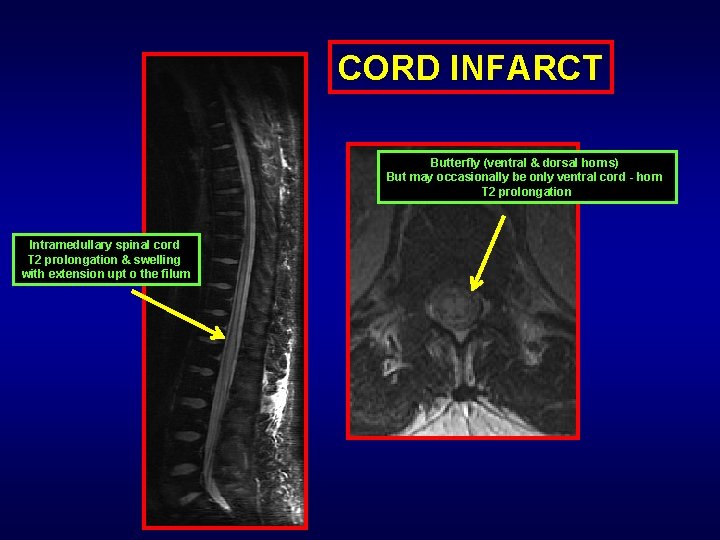
CORD INFARCT Butterfly (ventral & dorsal horns) But may occasionally be only ventral cord - horn T 2 prolongation Intramedullary spinal cord T 2 prolongation & swelling with extension upt o the filum
CORD INFARCT INTRODUCTION: Abrupt vascular occlusion or cutoff involving spinal cord from aortic dissection or iatrogenic or vascular avulsion leading to cord infarct or necrosis. CLINICAL PRESENTATION: - Acute onset paraplegia or paraparesis - Symptoms peak within couple hours of onset
IMAGING HALLMARKS: - Long segment central cord T 2 hyperintensity - Cord swelling in acute state volume decrease in chronic (if patient survives) - Ventral & dorsal horn (butterfly appearance) or more preponderance of ventral horn involvement - Restricted diffusion in acute state and enhancement in subacute state - Most commonly distal thoracic spinal cord extending to conus - Contiguous T 2 signal abnormality Differential: Cord edema due to inherent cord disease from tumor or infection or inflammation or the waste basket transverse myelitis. to be differentiated from discontinuous cord multiple sclerosis
IMAGING GOLD STANDARD/DIAGNOSIS: 1. MRI 2. Followed by angiography for vascular occlusion TREATMENT - PROGNOSIS: - Supportive - Treatment of underlying vascular cause (like aortic dissection or aneurysm) PROGNOSIS: Poor: Nearly quarter of the patient die within the acute hospital stay.
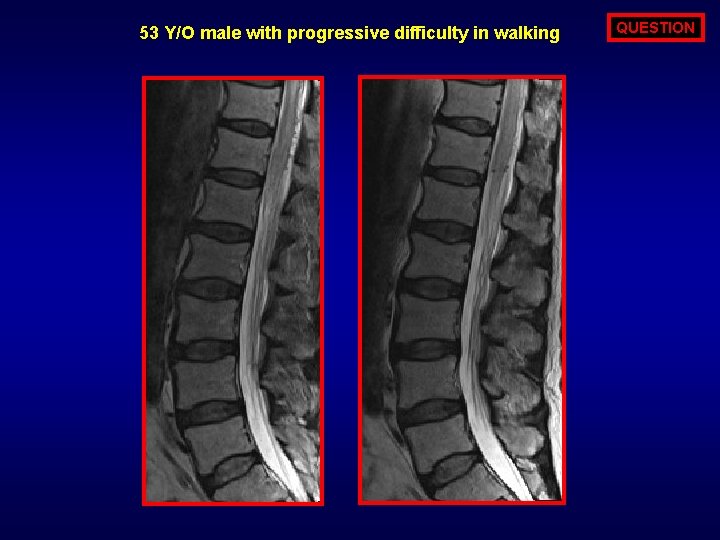
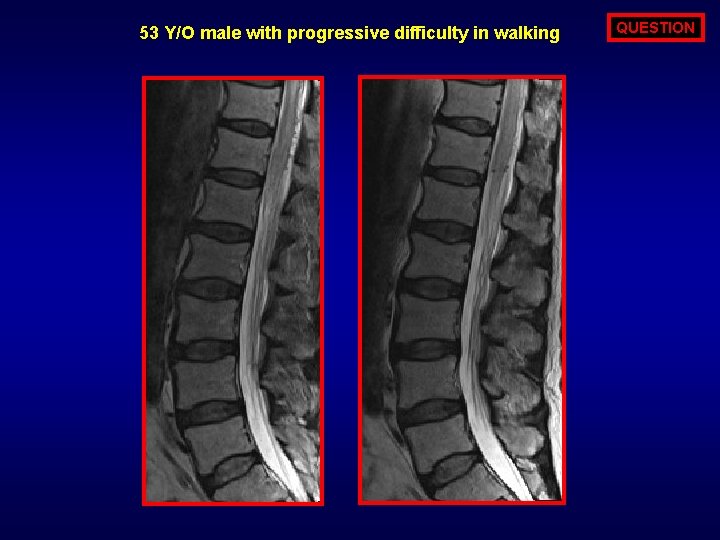
53 Y/O male with progressive difficulty in walking QUESTION
ANSWER OPTIONS MOST COMMON SPINAL CORD VASCULAR MALFORMATION - FISTULA IS? 1. 2. 3. 4. TYPE III TYPE IV
ANSWER TYPE I: 75 TO 85% IS THE FORMAINAL DURAL FISTULA (TYPE I) ABNORMALITY. ALSO 75 TO 85% OF THE PATIENTS WITH VASCULAR CHANNEL ABNORMALITY ARE MEN.
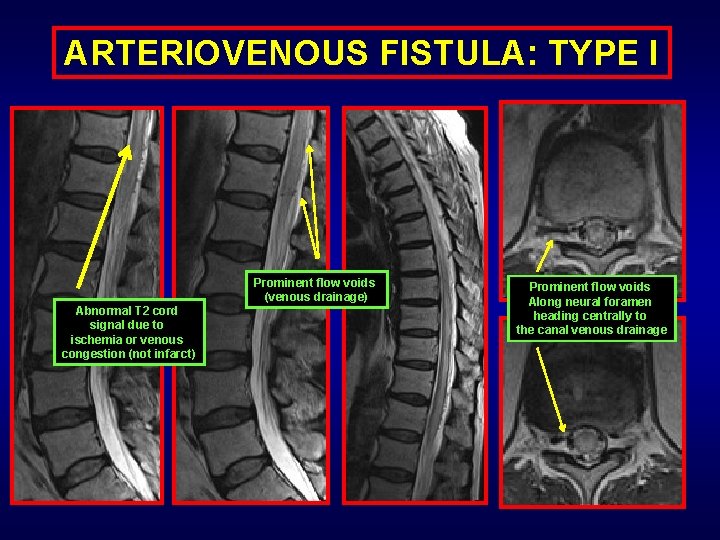
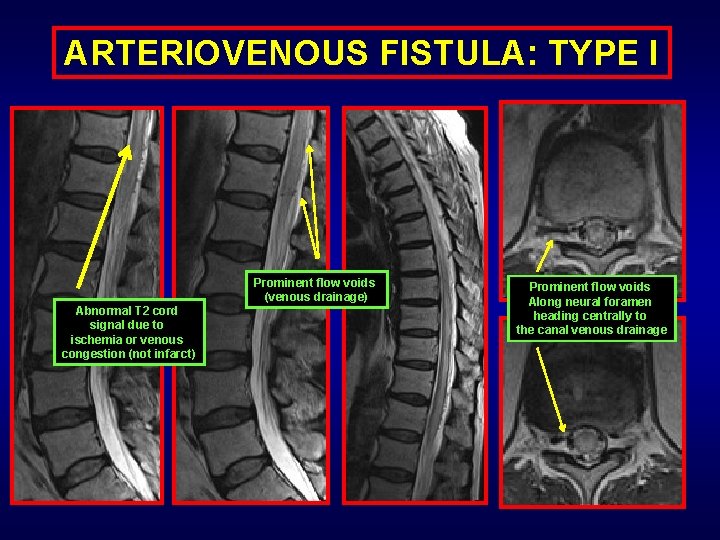
ARTERIOVENOUS FISTULA: TYPE I Prominent flow voids (venous drainage) Abnormal T 2 cord signal due to ischemia or venous congestion (not infarct) Prominent flow voids Along neural foramen heading centrally to the canal venous drainage
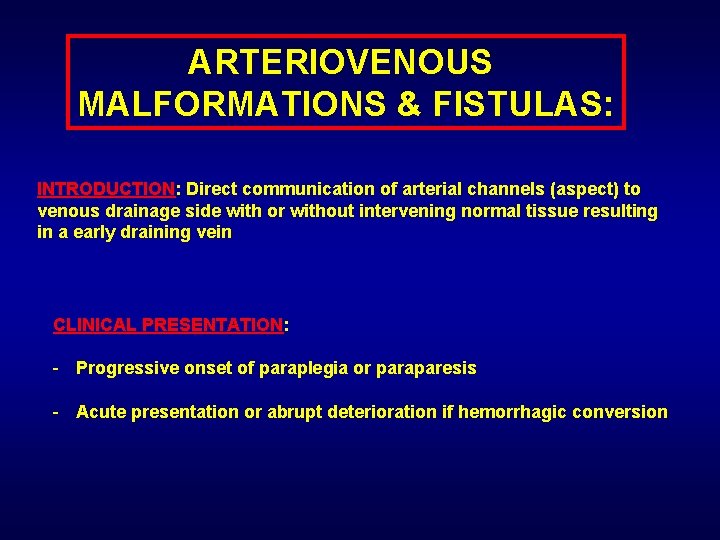
ARTERIOVENOUS MALFORMATIONS & FISTULAS: INTRODUCTION: Direct communication of arterial channels (aspect) to venous drainage side with or without intervening normal tissue resulting in a early draining vein CLINICAL PRESENTATION: - Progressive onset of paraplegia or paraparesis - Acute presentation or abrupt deterioration if hemorrhagic conversion
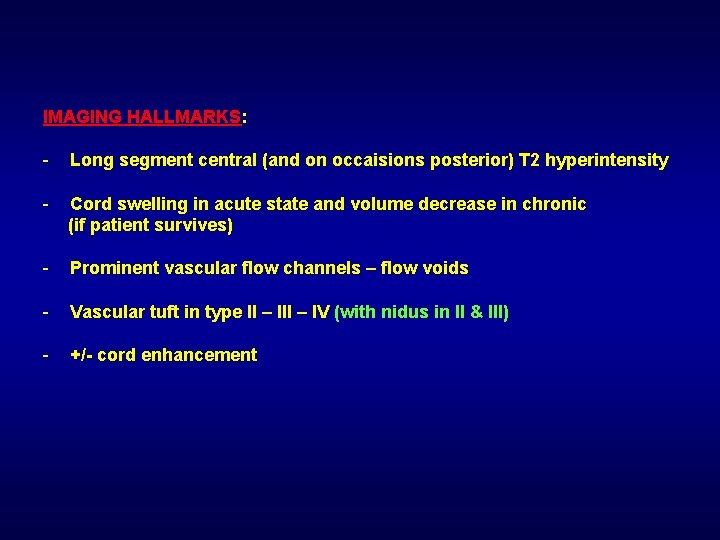
IMAGING HALLMARKS: - Long segment central (and on occaisions posterior) T 2 hyperintensity - Cord swelling in acute state and volume decrease in chronic (if patient survives) - Prominent vascular flow channels – flow voids - Vascular tuft in type II – IV (with nidus in II & III) - +/- cord enhancement
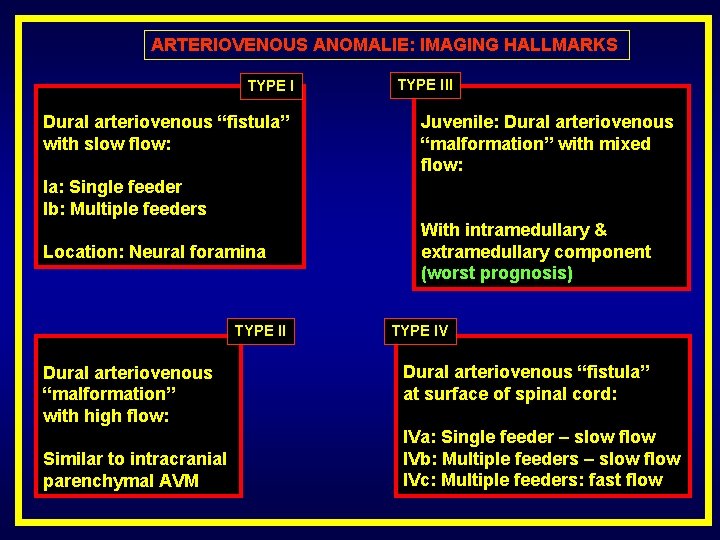
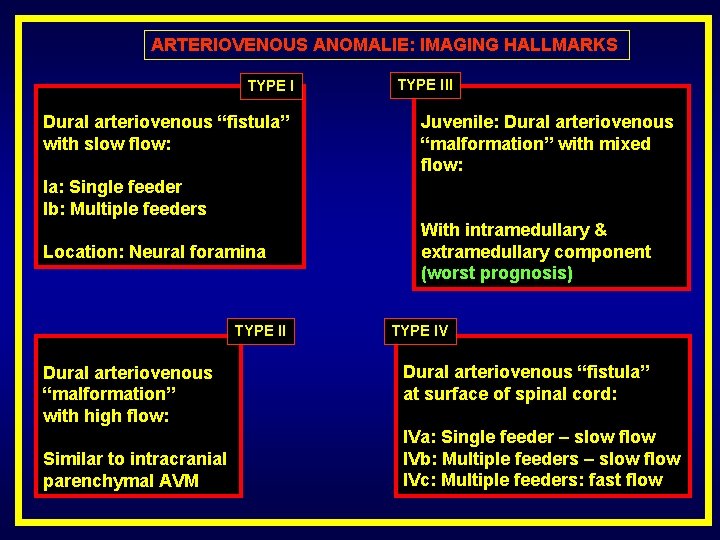
ARTERIOVENOUS ANOMALIE: IMAGING HALLMARKS TYPE I Dural arteriovenous “fistula” with slow flow: TYPE III Juvenile: Dural arteriovenous “malformation” with mixed flow: Ia: Single feeder Ib: Multiple feeders Location: Neural foramina TYPE II Dural arteriovenous “malformation” with high flow: Similar to intracranial parenchymal AVM With intramedullary & extramedullary component (worst prognosis) TYPE IV Dural arteriovenous “fistula” at surface of spinal cord: IVa: Single feeder – slow flow IVb: Multiple feeders – slow flow IVc: Multiple feeders: fast flow
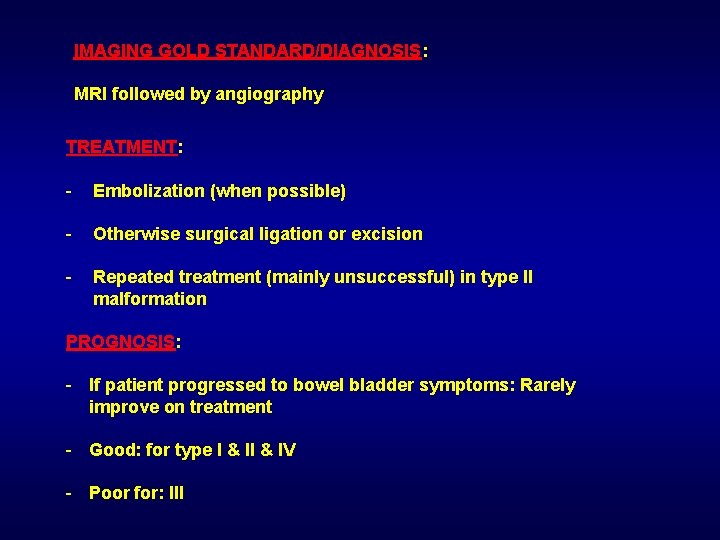
IMAGING GOLD STANDARD/DIAGNOSIS: MRI followed by angiography TREATMENT: - Embolization (when possible) - Otherwise surgical ligation or excision - Repeated treatment (mainly unsuccessful) in type II malformation PROGNOSIS: - If patient progressed to bowel bladder symptoms: Rarely improve on treatment - Good: for type I & IV - Poor for: III
MISCELLANOUS:
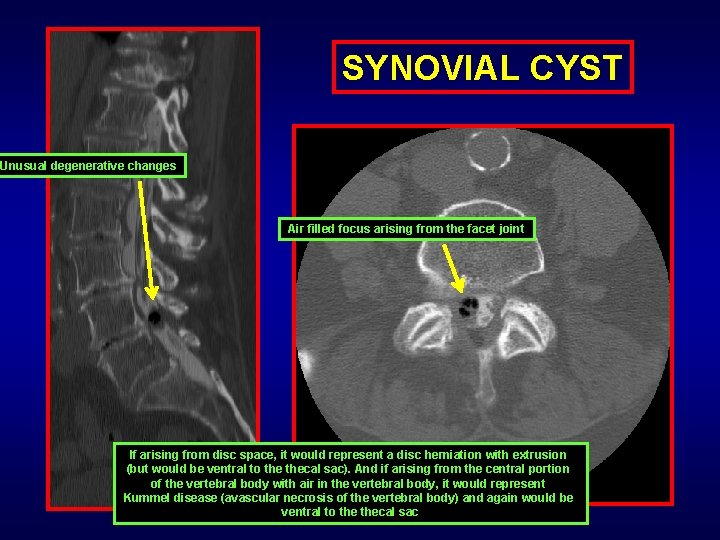
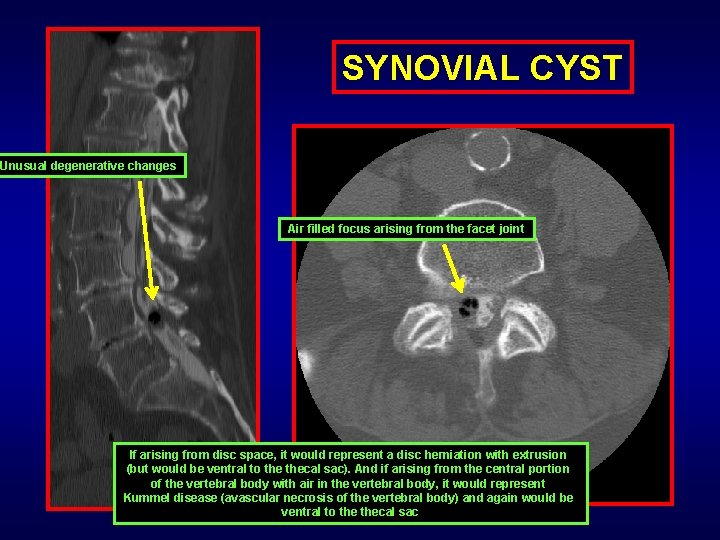
SYNOVIAL CYST Unusual degenerative changes Air filled focus arising from the facet joint If arising from disc space, it would represent a disc herniation with extrusion (but would be ventral to thecal sac). And if arising from the central portion of the vertebral body with air in the vertebral body, it would represent Kummel disease (avascular necrosis of the vertebral body) and again would be ventral to thecal sac
SIMPLISTIC APPROACH TO CAUDA EQUINA AND CORD PATHOLOGY:
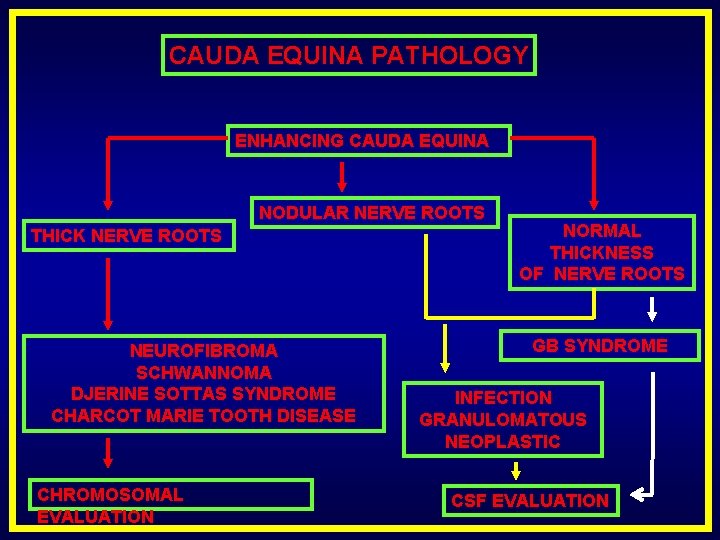
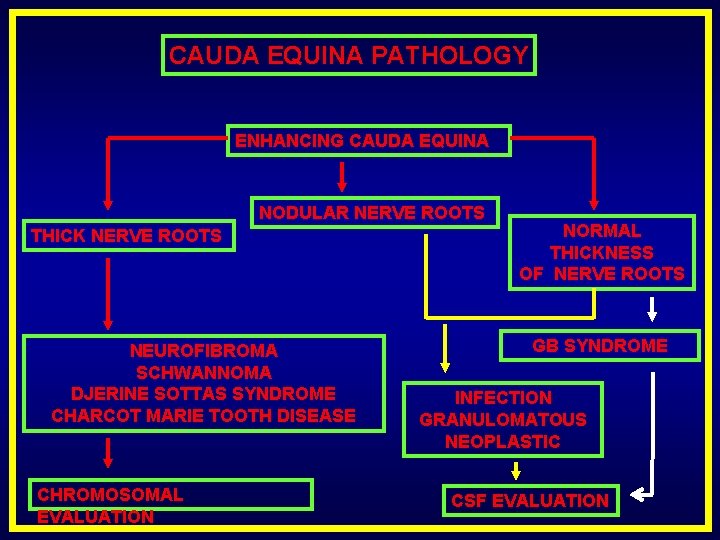
CAUDA EQUINA PATHOLOGY ENHANCING CAUDA EQUINA NODULAR NERVE ROOTS THICK NERVE ROOTS NEUROFIBROMA SCHWANNOMA DJERINE SOTTAS SYNDROME CHARCOT MARIE TOOTH DISEASE CHROMOSOMAL EVALUATION NORMAL THICKNESS OF NERVE ROOTS GB SYNDROME INFECTION GRANULOMATOUS NEOPLASTIC CSF EVALUATION
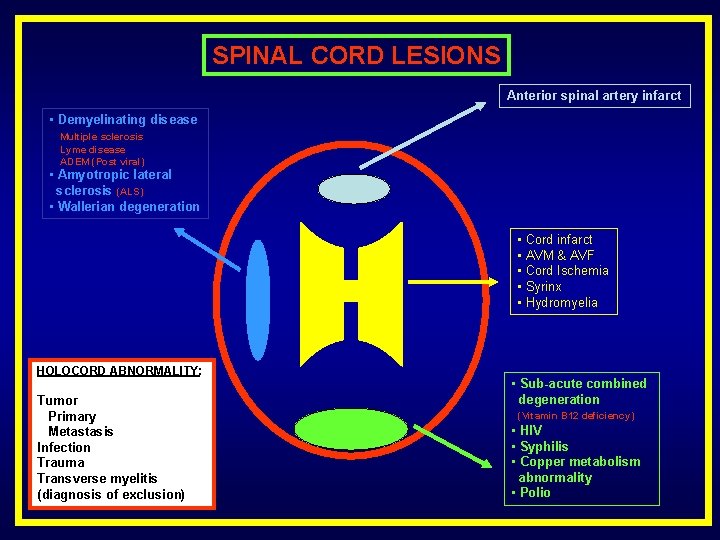
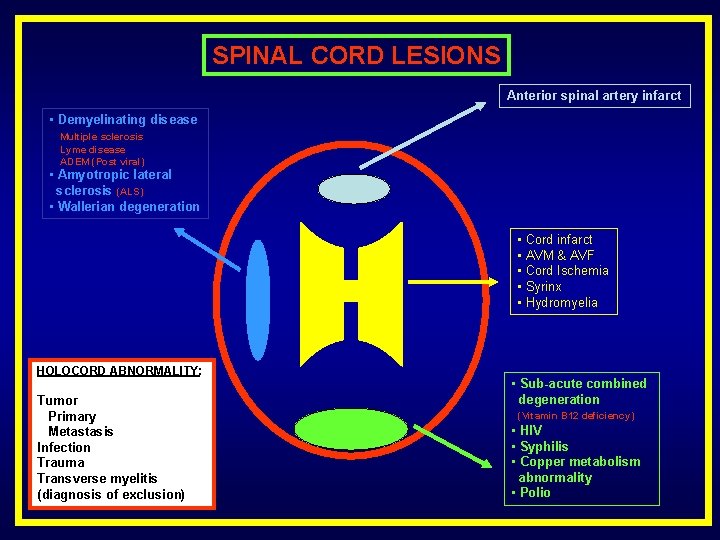
SPINAL CORD LESIONS Anterior spinal artery infarct • Demyelinating disease Multiple sclerosis Lyme disease ADEM (Post viral) • Amyotropic lateral sclerosis (ALS) • Wallerian degeneration • Cord infarct • AVM & AVF • Cord Ischemia • Syrinx • Hydromyelia HOLOCORD ABNORMALITY: Tumor Primary Metastasis Infection Trauma Transverse myelitis (diagnosis of exclusion) • Sub-acute combined degeneration (Vitamin B 12 deficiency) • HIV • Syphilis • Copper metabolism abnormality • Polio

THANK YOU