SERVICE EXCELLENCE another name for Customer Service Excellence

















- Slides: 108
SERVICE EXCELLENCE …another name for Customer Service Excellence is not just a good attitude, it’s a great one… Service Excellence is a way of working, a way of interacting and a way of thinking about our jobs as we work together with others to create positive patient experiences.
WHY SERVICE EXCELLENCE MATTERS • Service Excellence is about the patient’s impression and perception, we get one chance to make a first impression. • It is about making a difference in the patient experience. • It is about quality patient care. To ensure a positive experience, remember…. Every person has a role – direct care givers and support departments – both are equally important. • We need to provide a consistent product – with every patient, every time! • We are here for the patient, they come first!
TO PROVIDE GREAT SERVICE EXCELLENCE…. • Let the patient know that we are a team • Put yourself in the role of the patient • Treat the patient as you would want caregivers to treat you or your family member • Ask yourself have you done as much as you could to make this patient’s experience a positive one • REMEMBER to adhere to the essential components of our RUMC Service Excellence Program…
Essential Components of our Service Excellence Program • RUMC Standards-WE CARE • Employee Recognition • The Chronicle • Expressions of Appreciation • HCAHPS • AIDET • Visitor Courtesy

More Essential Components • Telephone Etiquette • White Boards • Hourly Rounding • Service Recovery • Quiet Campaign SERV IC E

Welcoming Energized Compassion Advocacy Respect Excellence RUMC STANDARDS
WELCOMING We are the ambassadors of our hospital • We do A-I-D-E-T Acknowledge our patients Introduce ourselves and our skills Describe the Duration of the test Explain the procedure and how we do things for their safety – Thank you for choosing our hospital. – –
ENERGIZED We are proud to use our energy performing purposeful work. • • We follow through, follow-up. We show confidence in our ability to provide care. We keep up with continuing education. We contribute new ideas, input, new initiatives to improve care.

COMPASSIONATE We care for our patients as if they are our own family. • We listen carefully to our clients, their families and each other and to respond quickly and appropriately to needs expressed. • We spontaneously offer assistance. • We are empathetic by putting ourselves in each patient’s situation and taking action.
ADVOCACY We support our patients, our community and each other. • We help our patients and their families resolve problems and concerns. • We are the voices of our patients when needed. We take our voices as employees a step further when we can. • We educate patients about their rights, how to consider appropriate choices and achieve positive outcomes.

RESPECT We treat others as we want to be treated. • We provide privacy for our patients and their families. • We follow HIPAA rules of confidentiality. • We treat all with dignity. • We give patients our full attention, keeping side conversations to a minimum during patient care activities.
EXCELLENCE We make every encounter, every day, excellent through consistent service. • We show confidence in our abilities. • We assess and know the customers needs versus expectations. • We are thorough and comprehensive including having sensitivity to cultural and spiritual needs. • We adhere to all hospital policies including dress code.
What is HCAHPS? (Hospital Consumer Assessment of Healthcare Providers & Systems) • Survey created by CMS to consistently measure patient’s perspectives of care • Mandatory participation for all U. S. hospitals • Questions focus on frequency of specific behaviors and actions • Survey results are publicly reported along with other clinical measures (core measures) • Part of our CMS reimbursement will be based on these measures
Dress Code • Beards and mustaches • Your appearance and must be neat and well manner are reflective of trimmed. Hair must be our values to our patients, properly groomed. visitors, and the communities we serve and • Head-ties/ Doo rags/Skull caps/ Hats are not to each other. appropriate. • Your appearance is an expression of our collective • Fingernails must be neat and comply with infection commitment to treat everyone with RESPECT and control standards. Heavy perfumes, colognes, or to continually strive to achieve EXCELLENCE in the other strong odors are not acceptable. quality of the service we • ID badges will be worn at provide. all times so that the • Body piercing or tattoos information is easily should not be apparent visible to patients and should be covered visitors. where possible.
Annual Physicals • All employees are responsible to have their annual physical during the month of their birthday. Even if their birth month falls less than a year from their start date. • Staff are responsible for ensuring that they visit Personnel Health Services, complete their annual health assessment form and have their PPD placed and read before the end of their birth month. • Failure to comply may lead to removal from duty.
DISCRIMINATION AND HARASSMENT • Any behavior, including verbal or physical conduct that constitutes, in any form, discrimination against or harassment of any member or guest of the Medical Center is prohibited. Retaliation in any form against a person because he or she complained about an act of discrimination or harassment is prohibited. • Discrimination is: any behavior (however manifested, and whether anonymous or overt) that limits, segregates or classifies an individual or group in such a way that might deprive them of the opportunity fully to function and participate as a member of the Medical Center. Discrimination includes any behavior that might reasonably be considered unlawful discrimination under applicable NYS and/or federal law. • Harassment is: any behavior (however manifested, and whether anonymous or overt) that is intended to cause or could reasonably be expected to cause an individual or group to feel intimidated, demeaned, or abused, or fear or have concern for their personal safety. Harassment includes any behavior that might reasonably be considered unlawful harassment under applicable NYS and/or federal law.
IT IS CRUCIAL TO REMEMBER • If you feel you are being discriminated against or harassed, you should take action which may include any/all of the following: • Speak with the individual and let him or her know that the behavior is unwelcome and unacceptable. • Talk with your supervisor/manager. • Contact Human Resources, or call the Corporate Compliance Hotline (800 -826 -6762).
Diversity At RUMC, diversity means that we believe everyone is unique and has different talents and abilities. All of us contribute in various ways to provide our customers, the organization, and the community with excellent service. When we value diversity we can fulfill our highest potential as a team and as individuals. To meet the needs of each person we interact with, we must be trained to understand the complex dimensions of diversity. These include, but are not limited to: Age, Physical or mental abilities, Race, Culture, Ethnicity, Sexual orientation, Gender, Learning abilities.
Diversity By examining our own attitudes, values, and behavior (as well as those of others), we begin to achieve real understanding. Teamwork is essential in a diverse work force. Qualified and diverse team members learn to respect each other’s differences. Job satisfaction will be greatly increased if each employee is valued and treated with respect. Every employee will become empowered to build strength for our team. When each member of a team has high morale, the productivity of the organization and the quality of service will be enhanced. This leads to increased customer satisfaction and improved community relations. It is up to each of us to learn about others and address individual needs so we can work together to serve our customers. We are stronger through diversity.
Diversity Inclusion means creating an organizational environment and culture where every employee feels valued and is able to function at his or her best. The key to inclusion is harnessing the talents, strengths and personal motivation of each individual in our diverse workforce and aligning each person’s talents, abilities and skills with the organization’s goals, mission and values. IT IS CRUCIAL TO REMEMBER: Our workforce is diverse; we must respect differences and make them work for us. Interpersonal relations and organizational effectiveness are improved through encouraging new ideas and perspectives.
Diversity Stereotypical views of others limit our ability to understand those different from us. Every human being is unique; we need to create an environment where all employees feel they can contribute to their fullest potential.
• Replaces all other incident reports • Allows for immediate reporting of an event • Mandates investigation into each event • Encompasses actual events and near misses.
One Consolidated Form Replaces Employee Incident Report Safe Medication Event Form Workplace Violence Form Memo to Quality Assurance Form Safety Report
Timely Reporting & Follow up Two part form allows for immediate notification to various departments such as Risk, Employee Health, Quality, Pharmacy. This will allow for appropriate and timely reporting to external authorities if necessary. External authorities include: NYPORTS; DOH; OMH; OSHA; and Insurance Carriers. Failure to report within a timely manner can lead to citations and fines. Investigation to event can then be carried out as appropriate and will “catch up” with initial notification.
Actual Events & Near Misses Actual events are those that happen – a fall, a medication error, a back sprain, a theft. A near miss – is a potential event that is caught because of an internal mechanism of checks and balances or by chance – for example wrong medication is delivered to the unit but not received by the patient.
Event Reporting Guidelines • The hospital investigates all Events: including occurrences, incidents, sentinel events, or near misses, to understand the causes that underlie the event and to make changes to the hospital’s systems and processes in order to prevent the probability of recurrence of the event. • It is the policy of the Medical Center to ensure that proper actions are taken, adequate documentation, and notification to the appropriate persons or regulatory bodies is made when an event happens.
Event Reporting Guidelines • This event may involve a patient, visitor, volunteer, employee or property or may be an actual or potential interruption of services necessary to the continued safe operation of the hospital. • Many of these events are reported for tracking purposes only. Reporting is not meant to imply negligence, wrong doing, or place blame. • Every effort must be made to report and investigate as quickly as possible. Any lag deters from the investigation and provides a window for recurrence.
Types of Events to Be Reported • An unexpected event or situation related to a patient, visitor, or staff irrespective of outcome * fall, med error, test on wrong patient • An unexpected occurrence which leads to serious harm or death or has the potential for same * rape, amputation, wrong surgery • Work related employee illness or injury or potential for same • An unexpected event not necessarily associated with a person * Code Red • Act of commission or omission that could have resulted in harm • Workplace violence
Event Reporting Guidelines Actions • Stabilize the situation. Perform immediate actions to decrease harm and protect. • Assess the person and render appropriate care. Documentation • All patient events that reach the patient should be fully documented in the patients medical record by the staff identifying the event, the clinical staff assessing the patient, and staff carrying out the interventions-if necessary. The entry must be objective, stating the facts only.
Event Reporting Guidelines Documentation (continued) • An event report should be initiated as soon as possible after the event by the person with the best knowledge of the event, typically this is the individual who first discovers the situation. • Do not reference the event report in the medical record or during conversation with the patient and/or family. Disclosure • Disclosure of events should occur ideally by the attending physician and after consultation with the Quality/Risk Management Leadership.
Event Reporting Guidelines Investigation • The manager is responsible for taking the lead in investigating the who, what, when, where, and why of the events. • This investigation along with any corrective action is reviewed with the Senior Leader for the area.
Event Reporting Form Guidelines The event report should be initiated by the person who has direct knowledge of the situation • Place patient label in the identification box if a patient event. If visitor, staff, or other person document demographic information. • Identify if the event is an incident, sentinel event, or near miss only if the determination can be made at the time. If it is believed that a sentinel event has occurred- immediate notification to the Quality/Risk management or the ADN must occur. • In the event of work place violence, security and/ or the ADN must be notified.
Event Reporting Form Guidelines • Document the date, time (military) and location of the event. Be as specific as possible. • Document the nature of the event If a category does not exist, use the other selection in the first column. • Identify a potential cause of the event if possible. • For blood borne pathogen exposures, identify the device utilized. Specifically indicate the brand, model number and any other identifying information. Every effort should be made to retain the device in a safe manner.
Event Reporting Form Guidelines • Describe the event. 1. Include the who, what, where, and how 2. Identify equipment by brand, model, and serial number. Every effort should be made to secure any equipment that is believed to have contributed to the event. This may be essential to the investigation. • Identify any witnesses • Indicate any initial treatment rendered • Identify the specific outcomes and disposition of the involved party
Event Reporting Form Guidelines • Indicate to whom notifications were made. Include name, badge number, report number, when possible. • Signatures- The person initiating the form The physician evaluating the individual The supervisor on duty Distribution: • Send one copy of page 1 immediately to Quality/Risk Management Villa Building • Send the second copy of page 1 to: • Personal Health if an employee event • Pharmacy if a medication event • Forward all remaining forms to your immediate supervisor further investigation
FAMILY HEALTH CARE DECISIONS ACT (FHCDA) New York State Family Health Care Decisions Act June 1, 2010
FHCDA OVERVIEW • Applies to patients in hospitals and nursing homes in New York State • Empowers families and close friends to make treatment decisions for patients without capacity • Overcomes legal barriers by permitting those closest to patient to make decisions based on patient’s known wishes and/or in the patient’s best interest • Does not apply to patients who have a Health Care Proxy
FHCDA HIGHLIGHTS • Provides a list of surrogates in order of priority who have authority to make decisions when patients no longer have capacity • Does away with clear and convincing evidence for end-of-life decisions • Makes it possible to provide care and to withhold or withdraw life-sustaining treatment from patients without capacity or with no surrogate • Permits artificial nutrition and hydration to be withdrawn whether or not patient has discussed wishes
FHCDA Modifications to Hospital Policies • New and revised policies • Eight (8) new forms – FHCDA Hospital Form 1 -7 – Withhold/Withdraw/Refusal of Treatment Consent Form • Eliminates DNR Form 2 -7

INFECTION CONTROL
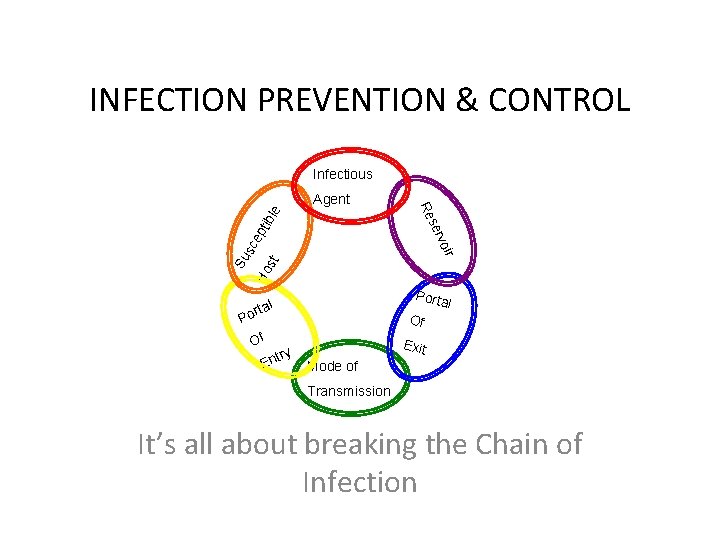
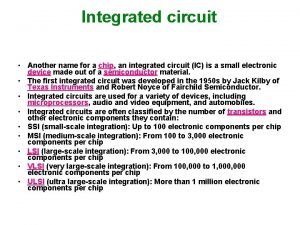
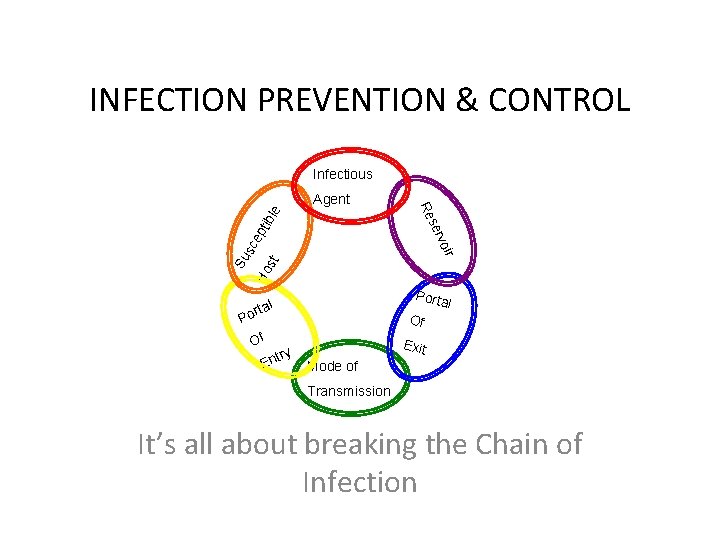
INFECTION PREVENTION & CONTROL Infectious ble pti sc e st Ho Su r voi P ser Re Agent Porta l al ort Of E y ntr Of Exit Mode of Transmission It’s all about breaking the Chain of Infection
How do we break the chain of infection? Handwashing is the single most effective way of stopping the spread of infections!
When Do You Wash Your Hands? • Before eating or handling food • After using the restroom • Before and after each patient contact • Before handling clean equipment • Before and after performing procedures • After removing a used pair of gloves
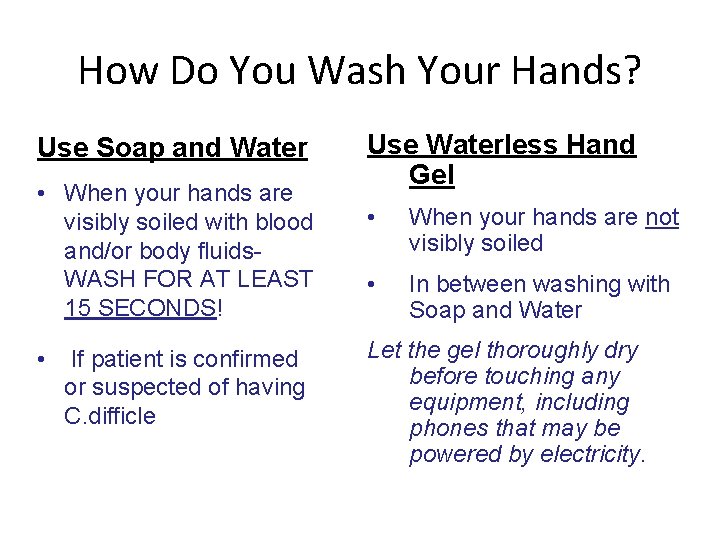
How Do You Wash Your Hands? Use Soap and Water • When your hands are visibly soiled with blood and/or body fluids. WASH FOR AT LEAST 15 SECONDS! • If patient is confirmed or suspected of having C. difficle Use Waterless Hand Gel • When your hands are not visibly soiled • In between washing with Soap and Water Let the gel thoroughly dry before touching any equipment, including phones that may be powered by electricity.
Hand Hygiene • Keep natural nails less than ¼ inch long • Artificial nails, extenders, tip, wraps, permanent French, etc. MUST NOT be worn by all personnel assigned to an acute inpatient unit and/or staff performing patient related procedures, or preparing equipment or supplies for patient use.
How do we break the chain of infection? Standard and Transmission Based Precautions – CDC Guidelines – Established to control the spread of communicable diseases and protect against unknown organisms. Always notify Infection Control Ext# 3134 when placing someone on Isolation
Standard Precautions • Practices that apply to all patients in any setting – Hand Hygiene – Use of Personal Protective Equipment (PPE) • gloves, gown, mask, eye protection, or face shield, depending on the anticipated exposure – Safe Injection Practices • All Blood & Body Fluids Treated as Infectious: (Blood, Body Fluids (Except Sweat), Non-intact Skin, Mucous Membranes
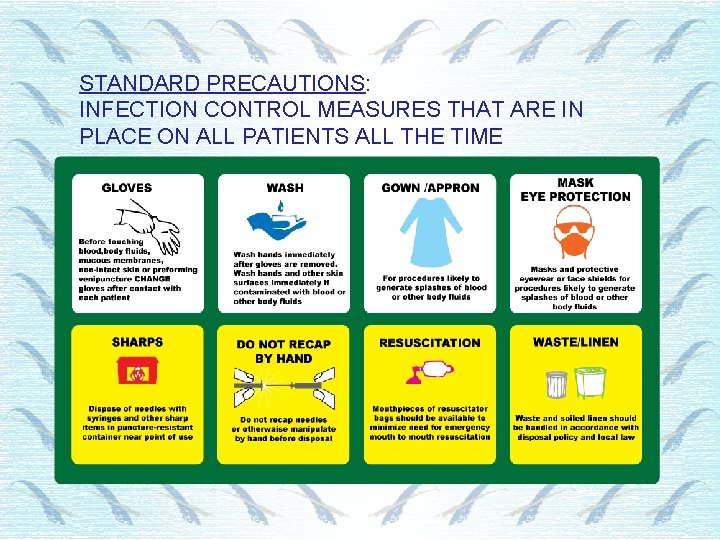
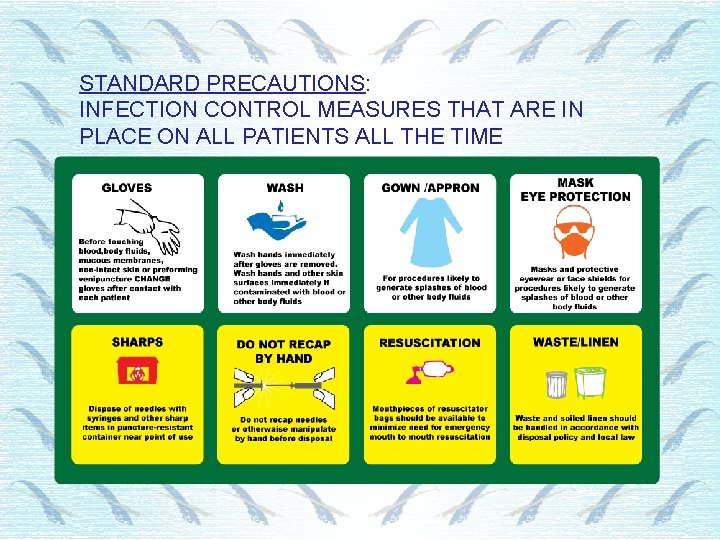
STANDARD PRECAUTIONS: INFECTION CONTROL MEASURES THAT ARE IN PLACE ON ALL PATIENTS ALL THE TIME
Caught in the act! Personal Protective Equipment (PPE) (shoe and head covers, gloves, gowns, etc. ) must be disposed of in a proper receptacle before exiting the work area. This is especially important for employees working with patients at high risk for cross-contamination (OR, L&D, NICU). No employees are exempt. Thank you for every effort you undertake to make RUMC a more patient-centered environment.
Transmission Based Precautions • Extra Precautions • Used in addition to Standard Precautions • Used with highly transmissible or contagious pathogens

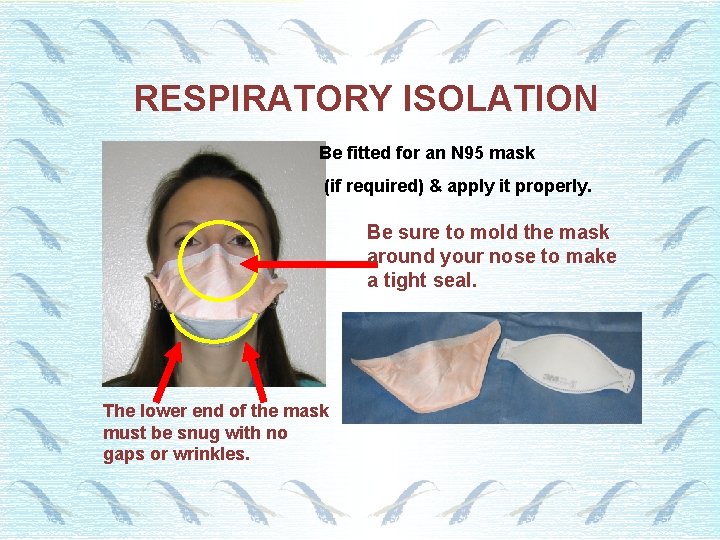
Transmission Based Precautions: Airborne Precautions • To be used for diseases that are transmitted by small particles circulating in the air and in air vent systems. • N 95 respirator mask must be worn correctly to enter this room. • Room must have Negative Pressure ventilation system with monitor system in operation • Door must remain closed
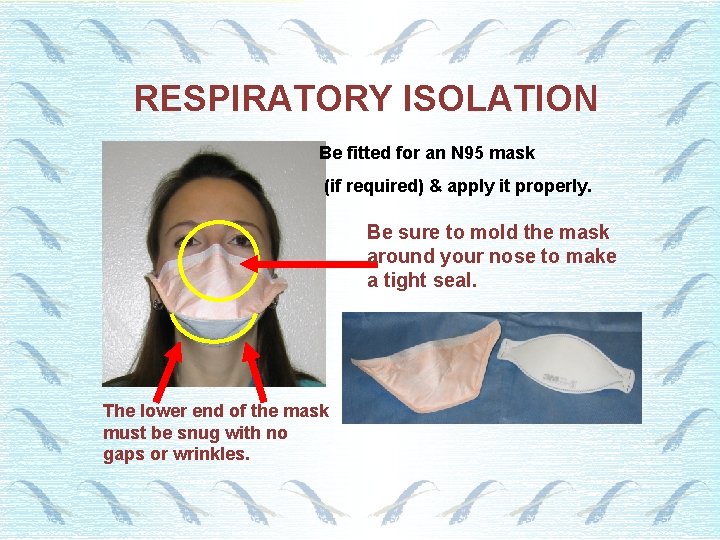
RESPIRATORY ISOLATION Be fitted for an N 95 mask (if required) & apply it properly. Be sure to mold the mask around your nose to make a tight seal. The lower end of the mask must be snug with no gaps or wrinkles.
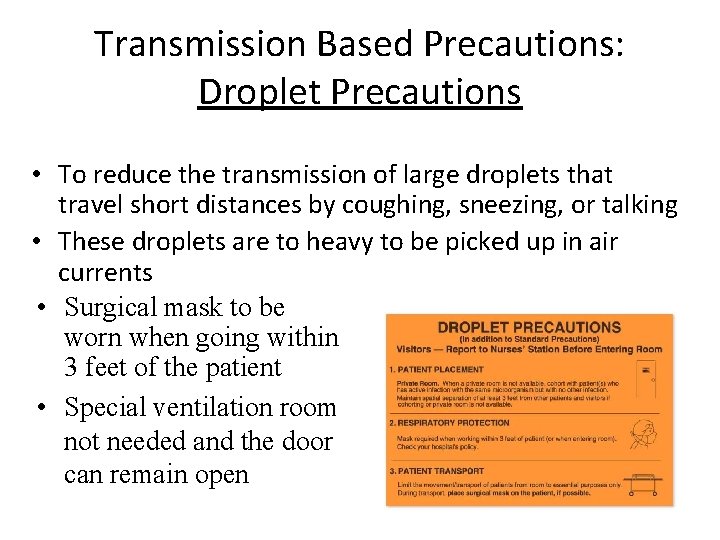
Transmission Based Precautions: Droplet Precautions • To reduce the transmission of large droplets that travel short distances by coughing, sneezing, or talking • These droplets are to heavy to be picked up in air currents • Surgical mask to be worn when going within 3 feet of the patient • Special ventilation room not needed and the door can remain open
Transmission Based Precautions: Contact Precautions • To be used for diseases and/or organisms transmitted by person to person skin contact and/or by sharing of equipment • Known or suspect infection or colonization of microorganism, usually resistant to antibiotics • Gloves & Gowns MUST be worn before entering the room
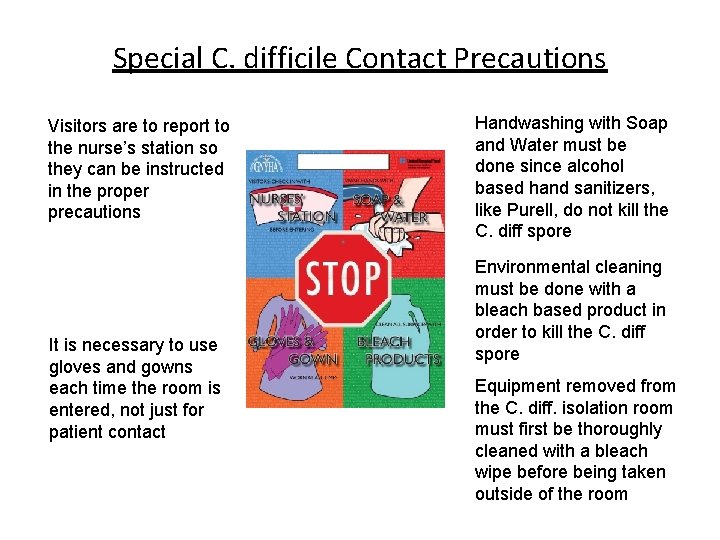
Transmission Based Precautions: Special C. difficile Contact Precautions Clostridium difficile (C. diff. ) • Causes serious illness in • A spore forming Gram patients with severely Positive bacteria that is weakened or immature difficult to kill when in its immune systems with spore form diarrhea as a primary symptom • An organism that is easy to spread from person to person by direct or indirect contact with contaminated patients or equipment.
Special C. difficile Contact Precautions • Identify patients at risk early • Diarrhea is often an early symptom • Patients receiving antibiotic therapy may develop C. diff infection as early as 1 -10 days after antibiotics have been initiated. • Place patient on C. Difficile Isolation as soon as you suspect C. Diff. • Notify Infection Control ext. : 3134 • If the patient shares a room, designate the bathroom for use by the C. Diff. Toxin positive patient. • If the patient is not able to maintain good hygiene (I. e. soiling the environment), place patient in a private room. • Do not share equipment (commodes, etc. )
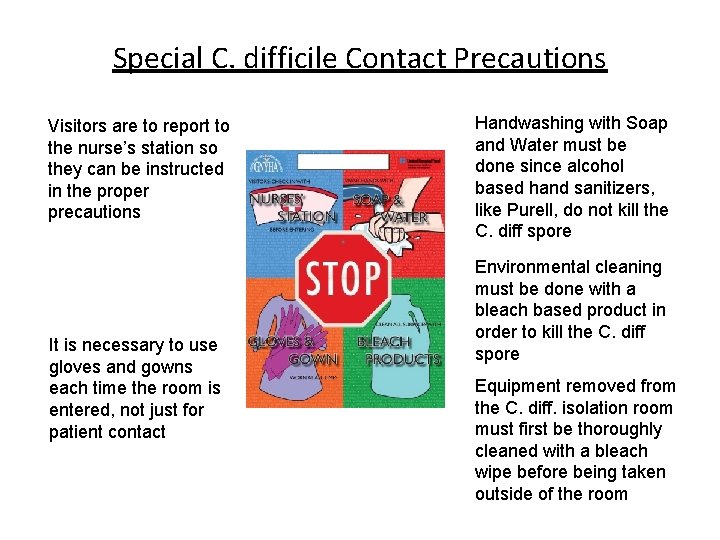
Special C. difficile Contact Precautions Visitors are to report to the nurse’s station so they can be instructed in the proper precautions It is necessary to use gloves and gowns each time the room is entered, not just for patient contact Handwashing with Soap and Water must be done since alcohol based hand sanitizers, like Purell, do not kill the C. diff spore Environmental cleaning must be done with a bleach based product in order to kill the C. diff spore Equipment removed from the C. diff. isolation room must first be thoroughly cleaned with a bleach wipe before being taken outside of the room
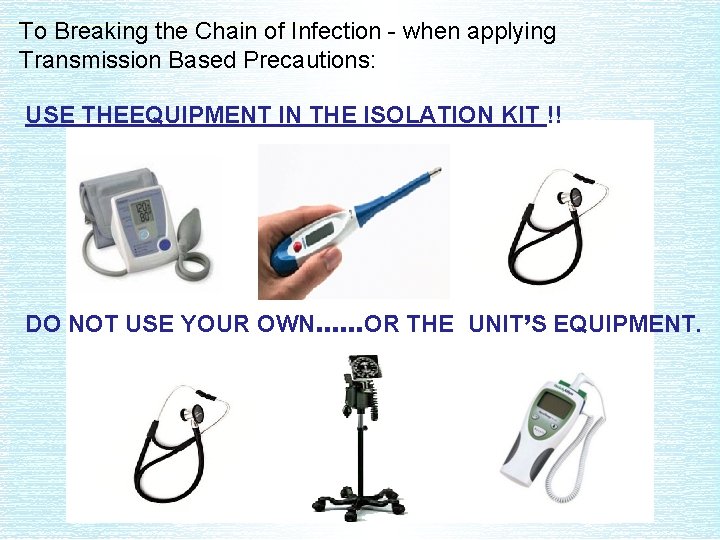
To Breaking the Chain of Infection - when applying Transmission Based Precautions: USE THEEQUIPMENT IN THE ISOLATION KIT !! DO NOT USE YOUR OWN……OR THE UNIT’S EQUIPMENT.
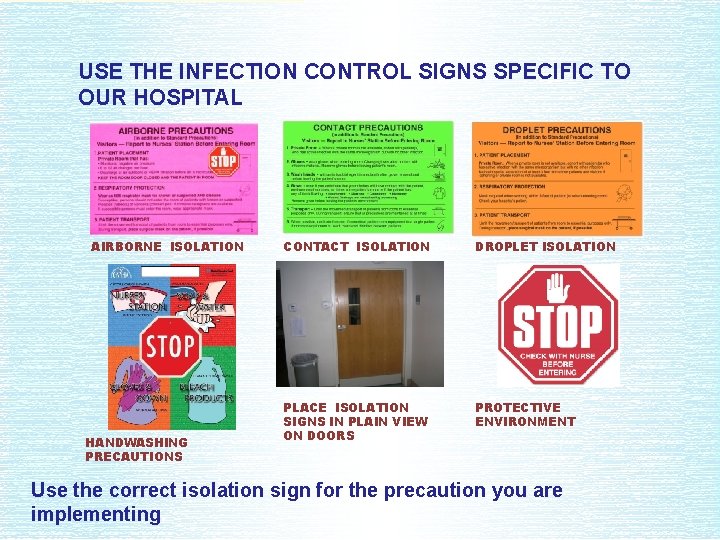
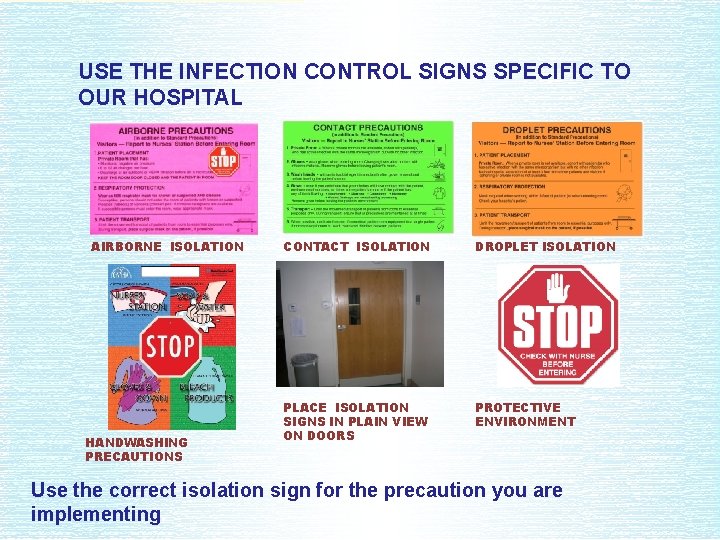
USE THE INFECTION CONTROL SIGNS SPECIFIC TO OUR HOSPITAL AIRBORNE ISOLATION HANDWASHING PRECAUTIONS CONTACT ISOLATION DROPLET ISOLATION PLACE ISOLATION SIGNS IN PLAIN VIEW ON DOORS PROTECTIVE ENVIRONMENT Use the correct isolation sign for the precaution you are implementing.
Protective Environment Precautions: Always place a visitor-stop sign on the door when protective environment precautions are in place. Teach visitors to put on and remove PPE and show and when to perform hand hygiene.
To Breaking the Chain of Infection - when applying Transmission Based Precautions: PPE used for isolation must be removed and discarded before leaving a patient’s room. Do not risk cross contamination. Think infection control instead. Caught in the act!
IT TAKES FIFTEEN SECONDS! If a three-year-old can wash his hands, you can, too! Numerous studies show that proper hand hygiene reduces the spread of bacteria in various healthcare settings.
Richmond University Medical Center Responsible Use Acknowledgement Statement This acknowledgement is to certify that I have read and understand the guidelines set forth within the Richmond University Medical Center’s Information Security Policies. As an employee or agent of Richmond University Medical Center or its subsidiaries, I will comply with the policy and guidelines. I understand that these guidelines may be modified by Richmond University Medical Center at any time and that I will be advised of such modifications as far in advance as reasonably possible. I realize privacy is not guaranteed on the company network, Internet/Intranet, and E-mail, and any transmission is subject to review. My use of company provided Email, Internet or Intranet services will constitute acceptance of the guideline, and consent to monitoring while using the services. I understand that I am personally liable for my misuse of E-mail, Internet or Intranet services provided by Richmond University Medical Center. In general personal Use is prohibited. I also understand failure to adhere to this policy may result in disciplinary action up to and including termination. **By completing the mandatory test, I certify that I have read, understand agree to the above**

RICHMOND UNIVERSITY MEDICAL CENTER • MISSION STATEMENT • PATIENT RIGHTS • LANGUAGE SERVICES • ADVANCE DIRECTIVES • PASTORAL CARE/SPIRITUAL CARE
MISSION STATEMENT The Medical Center is a not-for-profit health care provider serving the ethnically diverse community of Staten Island its neighborhood. We provide premier quality patient care through a full spectrum of emergent, acute, primary, behavioral health and educational services. We do this in an environment that promotes the highest satisfaction among patient, families, physicians and staff.
PATIENT BILL OF RIGHTS NYS DOH - BILL OF RIGHTS (19) • Right to receive treatment without discrimination • Right to care in a clean and safe environment • Right to know names and position of staff • Right to receive information & make an informed consent to treatment, DNR, Health Care Proxy, which includes a right to an Interpreter if needed • Right to privacy, confidentiality (HIPPA laws) • Right to file a complaint without fear of reprisal • Right to refuse treatment • Right to a no-smoking environment
Patient-related privacy is federally regulated under HIPAA. Patients deserve privacy. Do not share medical information with people who are not part of the treatment team. A health information violation can cost the hospital $50, 000 - $250, 000 in fines.
What can you do? Make information privacy a priority. Speak quietly while discussing a patient’s health information in public areas. Provide a quiet, private area for sensitive information exchange. Avoid using names or other identifying information when conversing if possible.
Privacy Tips When using the telephone: 1. Try to conduct the conversation so that you are not overheard. 2. Before giving out medical information, the other person’s identity must be confirmed. When dealing with paper, copiers and faxes: • Be careful not to leave information out in the open (such as the counter at a nurses’ station). • Sensitive information needs to be shredded, don’t just toss it in the trash. Place in confidencial paper bins. • Only fax to known locations.
PATIENT RIGHTS: USING AN INTERPRETER RUMC has qualified or certified Medical Interpreters and native speakers for on-site Language Interpretation. We also utilize a Telephonic Language Phone (Language Line Services), where interpreters are available in minutes over the phone. Ask your manager or supervisor for the contact information, or call Patient Relations at ext. 4340 or the Operator.
Who can be used as a medical interpreter? • Staff member that is hospital approved in Language Bank • Over-the-telephone interpreter through Language Line Services, in over 150 languages • Staff member who is bilingual and learned language other than English in native country (native speaker)
SIGN LANGUAGE INTERPRETATION FOR THE DEAF • Provide a Sign Interpreter for deaf patients • Assess if patient knows American Sign Language • A Sign Interpreter must be present for all medical interpretations and medical appointments if requested REQUEST A SIGN INTERPRETER: • Call Patient Relations to request Sign Interpreter, M-F, 9 -5 P • Call Operator during all other hours
Assistance for the Visually Impaired • The hospital offers assistance to the visually impaired by providing staff members to read forms, documents and consents to patients, as well as access to large button telephones and magnifying glasses. The Patient Bill of Rights is available on audiocassette. All requests should be referred to the Patient Relations Department during normal business hours and the Assistant Director of Nursing on duty during all other hours.

Health Care Proxy Healthcare professionals should help patients understand reach decisions about lifesustaining treatment such as CPR.
ADVANCE DIRECTIVES A person over the age of 18 years old can complete documents stating their health care wishes or he/she can appoint someone to make decisions when he/she is unable to make decisions Types of Advance Directives include: • Health Care Proxy • Living Will • DNR • Organ Donation
Providing Spiritual Support • Staff have the responsibility to ensure that the patient’s spiritual needs are met, either through direct interventions or by arranging access to individuals who can provide spiritual care. • Pastoral Care can be reached at extension 2062 or through the operator.

The Bikur Cholim room is now located on the 1 st floor Room 1 -28.
Employee Lactation Room is available on the 4 th floor near main elevators. The key can be obtained from the nursing office.
Patient’s Right to Opt Out of Being Listed in Facility Directory Patient Requests Directory Opt Out Upon Registration 1. A patient’s request to opt out must be provided in writing using a Directory Opt Out Form. 2. Registration notifies security immediately upon patient request. 3. Security reviews the form with the patient and makes certain the patient fully understands the consequences of opting out of the directory (language is included in the form). 4. Security manager immediately notifies registration who enters flag in the patient demographic screen. 5. Security must distribute the signed copies of the Directory Opt Out Form to the following: a. The Director/Designee of HIM b. One copy is given to the patient c. One copy is retain by the security desk, main lobby desk and Switchboard
Patient’s Right to Opt Out of Being Listed in Facility Directory Patient Requests Directory Opt Out While On A Nursing Unit 1. Appropriate hospital representative (e. g. , Nurse, Unit clerk, patient care representative, etc. ) provides the patient with a copy of the Directory Opt Out form. 2. Hospital representative notifies security immediately upon patient request. 3. Security reviews the form with the patient and makes certain the patient fully understands the consequences of opting out of the directory (language is included in the form). 4. Directory Opt Out from is signed by the patient 5. Security manager immediately notifies admitting who enters flag in the patient demographic screen
Patient’s Right to Opt Out of Being Listed in Facility Directory Patient Requests Directory Opt Out While On A Nursing Unit 6. Security must distribute the form as follows: a. Security places original document within the patient’s medical record b. One copy is given to the patient c. One copy is immediately faxed to the security department, main lobby desk and switchboard
Rescinding the Directory Opt Out 1. 2. 3. 4. 5. 6. • • • Only the individual, usually the patient, who has originally requested the Directory Opt Out, can rescind the Directory Opt Out. Patient will notify an appropriate hospital representative, e. g. nurse, patient representative, clerk, etc. Hospital representative notifies security immediately upon patient request Security reviews the form with the patient and makes certain the patient fully understands Security will notify admitting to remove the flag Security must distribute the signed copies of the Directory Opt Out Form to the following: Security places original within the patient’s medical record One copy is given to the patient One copy is retained by the Front desk/security desk
Internal Notification of Directory Opt Out A daily schedule report listing the patients who have opted out of the directory will be printed to the following departments: a. Security b. Patient Information c. Switchboard d. Admitting







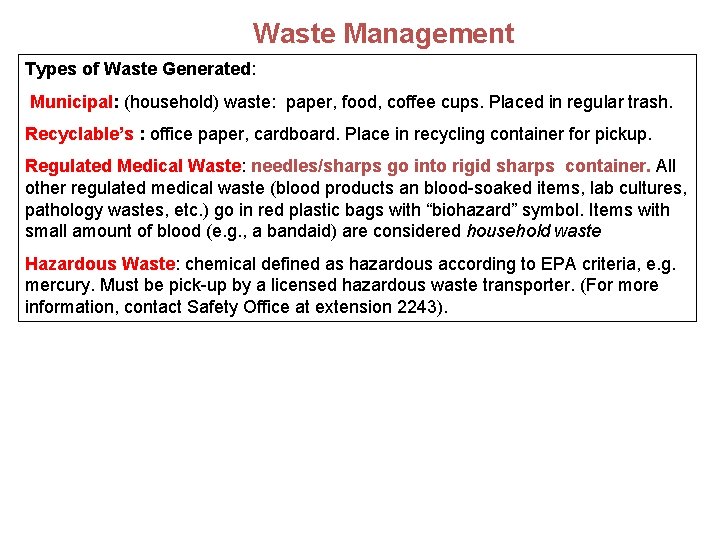
Waste Management Types of Waste Generated: Municipal: (household) waste: paper, food, coffee cups. Placed in regular trash. Recyclable’s : office paper, cardboard. Place in recycling container for pickup. Regulated Medical Waste: needles/sharps go into rigid sharps container. All other regulated medical waste (blood products an blood-soaked items, lab cultures, pathology wastes, etc. ) go in red plastic bags with “biohazard” symbol. Items with small amount of blood (e. g. , a bandaid) are considered household waste Hazardous Waste: chemical defined as hazardous according to EPA criteria, e. g. mercury. Must be pick-up by a licensed hazardous waste transporter. (For more information, contact Safety Office at extension 2243).
SMOKE-FREE CAMPUS, INSIDE AND OUT • As a provider of health care and promoter for the physical well-being of the community, smoking and the sale of smoking materials is prohibited in all areas of the Medical Center campus. Smoking by faculty, staff, volunteers, students, patients and visitors is prohibited. A smoking perimeter is established for the exterior surrounding property. Smoking is prohibited inside the outlined perimeter including parking lots/areas. Smoking in personal vehicles within the perimeter area is not allowed. • ALL faculty and staff are expected to achieve a smoke free campus.
Let’s be good Neighbors Please remember: - Don’t throw trash or cigarette butts on the ground or on private property - No milling around private homes or businesses - Be conscious of your surroundings and act accordingly - You represent the hospital, so please be courteous
The Colors Of Safety • The Colors of Safety Across the Continuum of Care initiative is intended to enhance patient safety by standardizing the colorcoding of specific alert conditions across acute & long term care settings. The initiative seeks to spread awareness about these standardized identifiers among clinical & non-clinical staff in health care settings as well as to patients, residents, and their families.
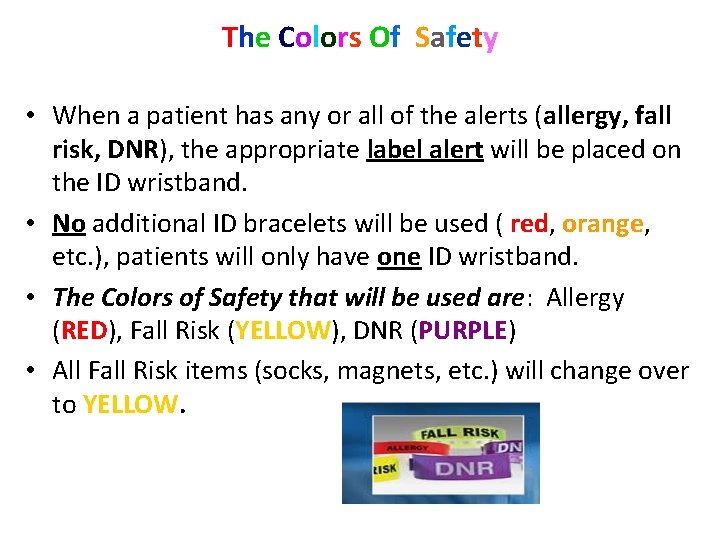
The Colors Of Safety • When a patient has any or all of the alerts (allergy, fall risk, DNR), the appropriate label alert will be placed on the ID wristband. • No additional ID bracelets will be used ( red, orange, etc. ), patients will only have one ID wristband. • The Colors of Safety that will be used are: Allergy (RED), Fall Risk (YELLOW), DNR (PURPLE) • All Fall Risk items (socks, magnets, etc. ) will change over to YELLOW.
Employees have the right to report issues to regulatory agencies such as The Joint Commission “TJC” or the Department of Health “DOH”. The Joint Commission website for complaints is jointcommission. org. or fax to The Joint Commission @1 -630 -792 -5636. The NYS Department of Health @1 -800 -804 -5447 Or You can contact the RUMC Compliance Hotline @1 -800 -826 -6762
Workplace Violence • Richmond University Medical Center strives for a safe and violence-free environment. Acts or threats of violence are serious and will not be tolerated. • The signs of potential violence (what you might see or hear): • Visible stress, tense muscles, fidgeting, glaring, pacing, threats, loud, fast speech, demanding, blaming statements, refusal to follow rules, throwing, slamming objects, verbal outbursts, unrealistic expectations • How to respond to potential violence: • If a threat is immediate, call: 1100 • If a threat is not imminent, notify your supervisor/manager and appropriate security.
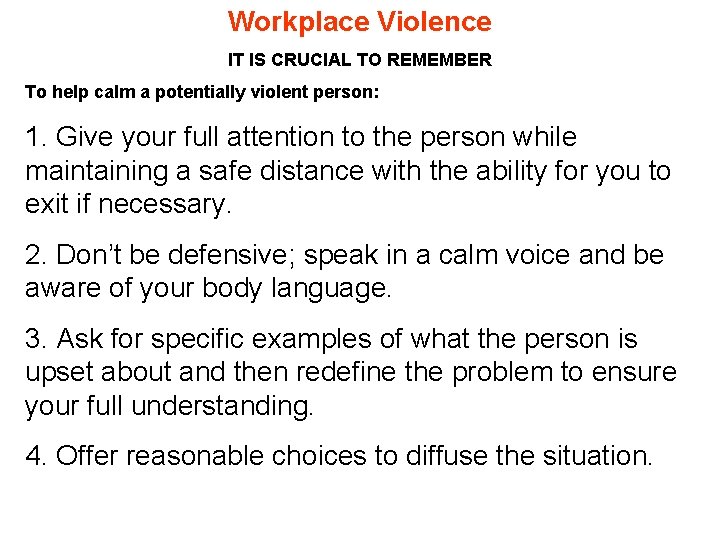
Workplace Violence IT IS CRUCIAL TO REMEMBER To help calm a potentially violent person: 1. Give your full attention to the person while maintaining a safe distance with the ability for you to exit if necessary. 2. Don’t be defensive; speak in a calm voice and be aware of your body language. 3. Ask for specific examples of what the person is upset about and then redefine the problem to ensure your full understanding. 4. Offer reasonable choices to diffuse the situation.
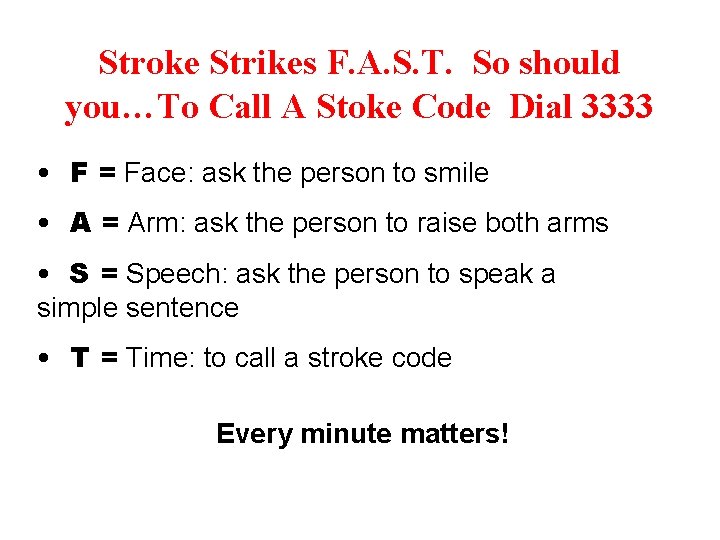
Stroke Strikes F. A. S. T. So should you…To Call A Stoke Code Dial 3333 • F = Face: ask the person to smile • A = Arm: ask the person to raise both arms • S = Speech: ask the person to speak a simple sentence • T = Time: to call a stroke code Every minute matters!
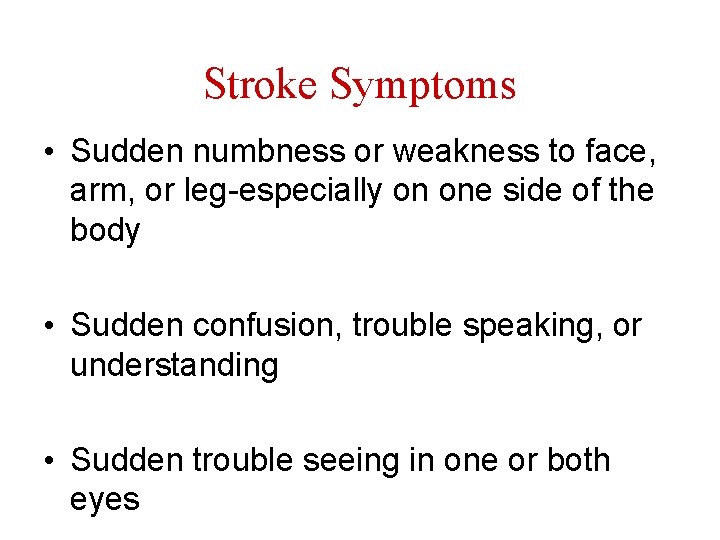
Stroke Symptoms • Sudden numbness or weakness to face, arm, or leg-especially on one side of the body • Sudden confusion, trouble speaking, or understanding • Sudden trouble seeing in one or both eyes
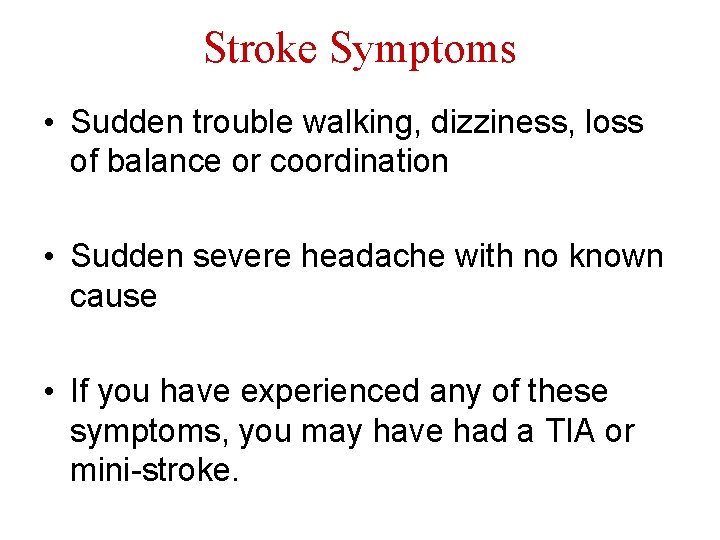
Stroke Symptoms • Sudden trouble walking, dizziness, loss of balance or coordination • Sudden severe headache with no known cause • If you have experienced any of these symptoms, you may have had a TIA or mini-stroke.
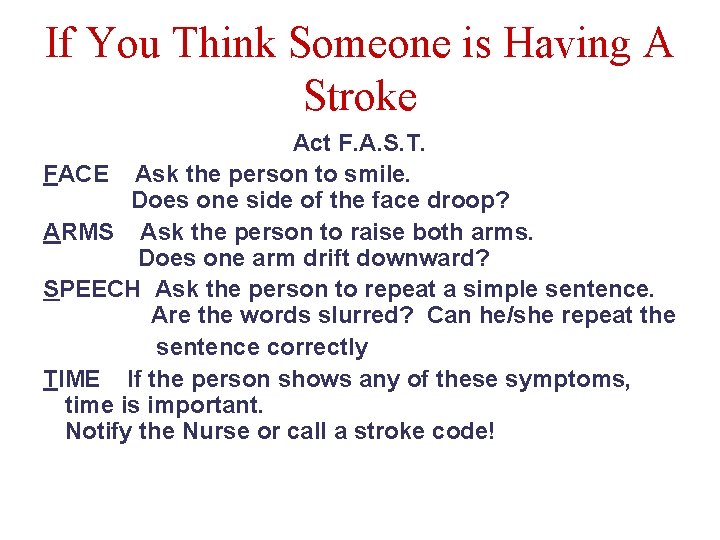
If You Think Someone is Having A Stroke Act F. A. S. T. FACE Ask the person to smile. Does one side of the face droop? ARMS Ask the person to raise both arms. Does one arm drift downward? SPEECH Ask the person to repeat a simple sentence. Are the words slurred? Can he/she repeat the sentence correctly TIME If the person shows any of these symptoms, time is important. Notify the Nurse or call a stroke code!

Why People Don’t Recognize and Respond to Symptoms • Don’t recognize symptoms • Denial • Think nothing can be done • Worry about cost • Think symptoms will go away • Fear or don’t trust hospitals
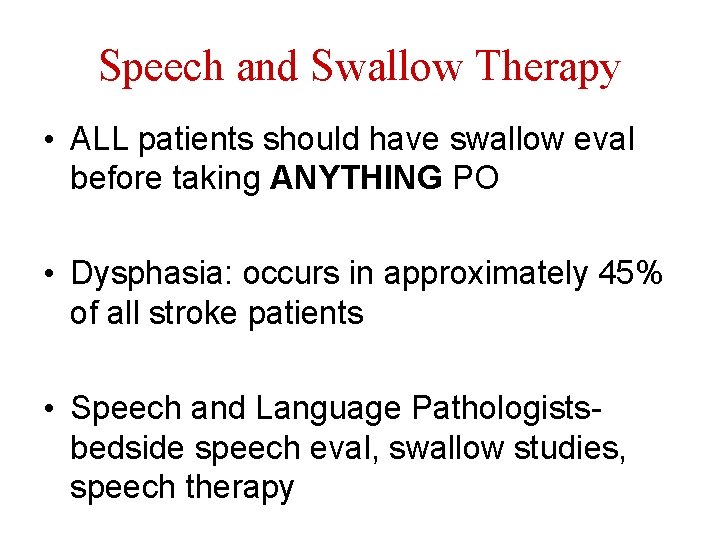
Speech and Swallow Therapy • ALL patients should have swallow eval before taking ANYTHING PO • Dysphasia: occurs in approximately 45% of all stroke patients • Speech and Language Pathologistsbedside speech eval, swallow studies, speech therapy
Primary Goals of Rehabilitation • Prevent complications • Minimize impairments • Maximize function • Return survivor to society with abilities to function by adapting to their deficit
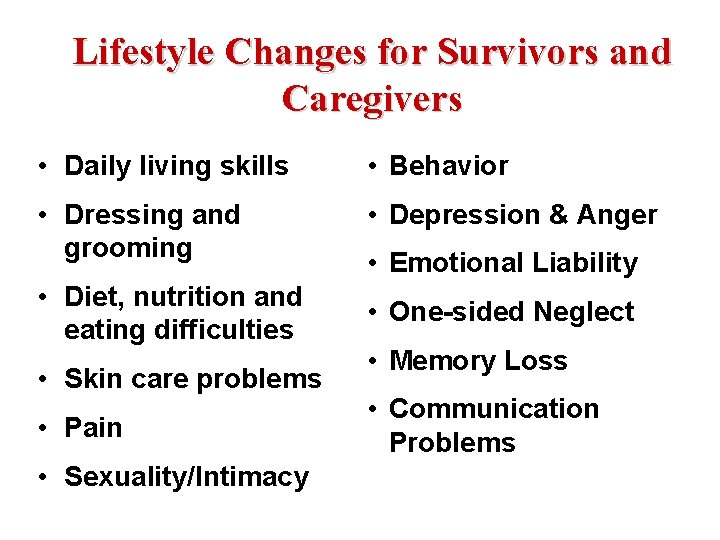
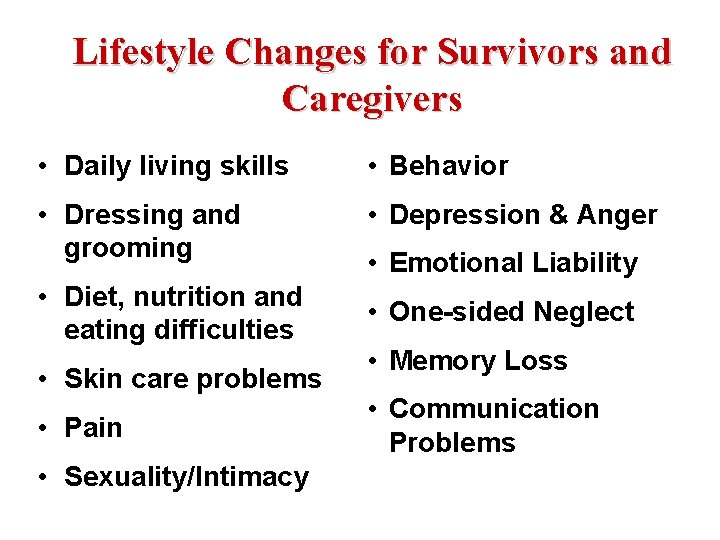
Lifestyle Changes for Survivors and Caregivers • Daily living skills • Behavior • Dressing and grooming • Depression & Anger • Diet, nutrition and eating difficulties • Skin care problems • Pain • Sexuality/Intimacy • Emotional Liability • One-sided Neglect • Memory Loss • Communication Problems
 Infection control isolation signs
Infection control isolation signs Perbedaan customer relation dan customer service
Perbedaan customer relation dan customer service Achieving operational excellence and customer intimacy
Achieving operational excellence and customer intimacy Operational excellence customer intimacy
Operational excellence customer intimacy Cva credential
Cva credential Project management center of excellence
Project management center of excellence Harris burdick
Harris burdick Adp employee self service portal
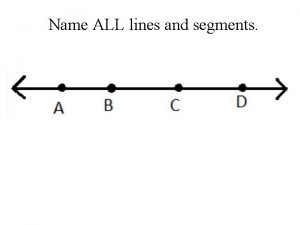
Adp employee self service portal Name three line segments
Name three line segments Managing marketing information
Managing marketing information Customer relationship management and customer intimacy
Customer relationship management and customer intimacy Beyond customer satisfaction
Beyond customer satisfaction Customer relationship management and customer intimacy
Customer relationship management and customer intimacy Customer relationship management and customer intimacy
Customer relationship management and customer intimacy Integrity service excellence
Integrity service excellence Integrity service excellence
Integrity service excellence Integrity excellence service
Integrity excellence service Four pillars of service excellence
Four pillars of service excellence Alr-69a block diagram
Alr-69a block diagram Accounting statement of financial position
Accounting statement of financial position Ozymandias greek
Ozymandias greek Another name for income statement
Another name for income statement Draw the six principal views
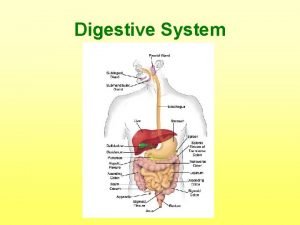
Draw the six principal views Protein digestion begins in the _____.
Protein digestion begins in the _____. Whats another name for the calvin cycle
Whats another name for the calvin cycle Another name for osseous tissue
Another name for osseous tissue Cross line headline
Cross line headline Drippy the raindrop
Drippy the raindrop National education commission is popularly known as
National education commission is popularly known as What is another name for the representative elements
What is another name for the representative elements What type of organism is the grass
What type of organism is the grass Ernst haeckel ecology
Ernst haeckel ecology What is the proper noun of movie
What is the proper noun of movie Selective set operation
Selective set operation Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Typiska novell drag
Typiska novell drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Personlig tidbok
Personlig tidbok A gastrica
A gastrica Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Debattinlägg mall
Debattinlägg mall Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Formel för lufttryck
Formel för lufttryck Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Jag har gått inunder stjärnor text
Jag har gått inunder stjärnor text Presentera för publik crossboss
Presentera för publik crossboss Argument för teckenspråk som minoritetsspråk
Argument för teckenspråk som minoritetsspråk Plats för toran ark
Plats för toran ark Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Epiteltyper
Epiteltyper Bästa kameran för astrofoto
Bästa kameran för astrofoto Cks
Cks Programskede byggprocessen
Programskede byggprocessen Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referatmarkering
Referatmarkering Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Stickprovsvariansen
Stickprovsvariansen Tack för att ni har lyssnat
Tack för att ni har lyssnat Steg för steg rita
Steg för steg rita Informationskartläggning
Informationskartläggning Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Toppslätskivling dos
Toppslätskivling dos Modell för handledningsprocess
Modell för handledningsprocess Egg för emanuel
Egg för emanuel Elektronik för barn
Elektronik för barn Plagg i gamla rom
Plagg i gamla rom Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Kung som dog 1611
Kung som dog 1611 Indikation för kejsarsnitt på moderns önskan
Indikation för kejsarsnitt på moderns önskan Romarriket tidslinje
Romarriket tidslinje Tack för att ni lyssnade
Tack för att ni lyssnade Större och mindre tecken
Större och mindre tecken Dikt rim
Dikt rim Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Fuktmätningar i betong enlig rbk
Fuktmätningar i betong enlig rbk Etik och ledarskap etisk kod för chefer
Etik och ledarskap etisk kod för chefer Kolopskopi
Kolopskopi Myndigheten för delaktighet
Myndigheten för delaktighet Trög för kemist
Trög för kemist Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Läkarutlåtande för livränta
Läkarutlåtande för livränta Karttecken kraftledning
Karttecken kraftledning Geometri för barn
Geometri för barn Shaktismen
Shaktismen Biologiska arvet
Biologiska arvet Bris för vuxna
Bris för vuxna Jätte råtta
Jätte råtta Contoh killer words
Contoh killer words End customer name
End customer name Lso customer service
Lso customer service Strengths lists
Strengths lists Susi login
Susi login