Congenital Muscular Torticollis Differential Diagnosis and Physical Therapy



- Slides: 67
Congenital Muscular Torticollis: Differential Diagnosis and Physical Therapy Management Carol Daly, PT, DPT, PCS
Outline of the Presentation • Objectives • Algorithms for clinical decision making in CMT • Physical therapy evidence based plan of care in CMT • Post-Test and Certificate of Completion 9/10/2021 © 2014 C. Daly, G. Neslund 2
Part 2 Objectives • Upon completion of this course, participants will Ø Understand the use of algorithms for the management of CMT Ø Identify the physical therapy diagnosis and prognosis associated with CMT Ø Describe “keep, consult, and refer” decisions associated with CMT evaluation Ø Describe evidence based physical therapy interventions for CMT Ø Understand evidence based dosing for physical therapy management of CMT Ø Identify appropriate outcome measures for assessment of the PT plan of care for infants with CMT 9/10/2021 © 2014 C. Daly, G. Neslund 3
Part 1 Review • Torticollis posture • Differential diagnosis of CMT • Clinical decisions to “Keep, Consult, or Refer” 9/10/2021 © 2014 C. Daly, G. Neslund 4
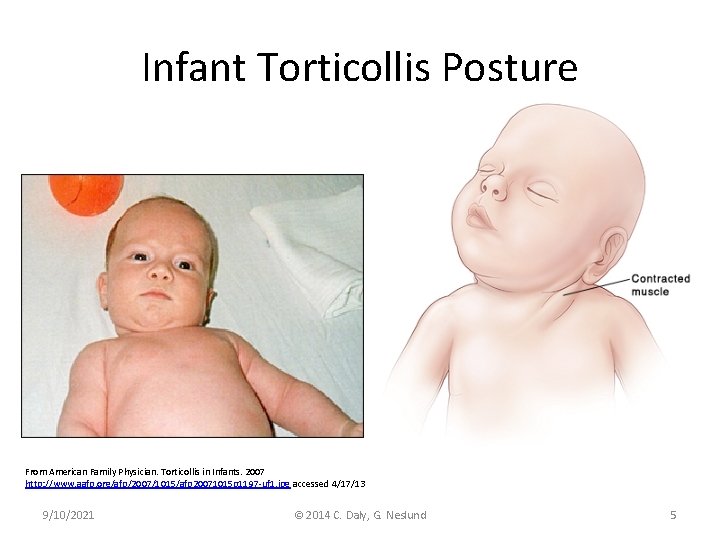
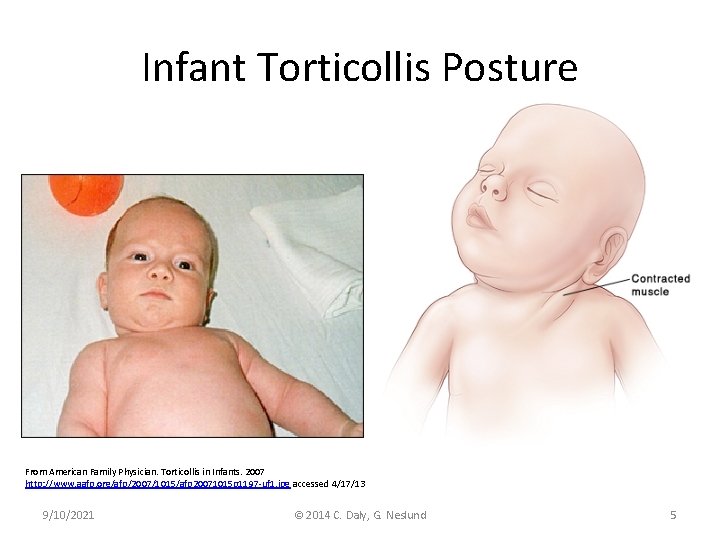
Infant Torticollis Posture From American Family Physician. Torticollis in Infants. 2007 http: //www. aafp. org/afp/2007/1015/afp 20071015 p 1197 -uf 1. jpg accessed 4/17/13 9/10/2021 © 2014 C. Daly, G. Neslund 5
Torticollis (Gray & Tasso, 2009; Karmel-Ross, 2012) • Differing origins of torticollis posture in infants – Congenital muscular torticollis (CMT) • Postural • Muscular • SCM mass – Non-muscular torticollis • Ocular • Osseous – Occipito-cervical – Cervical-vertebral • Neurologic 9/10/2021 © 2014 C. Daly, G. Neslund 6
Types of CMT (Kaplan, Coulter, Fetters, 2013) • Postural – Infant presents with strong postural preference – No restriction in cervical PROM • Muscular – SCM tightness noted on examination – Limitation in cervical PROM • SCM mass – Fibrotic thickening of the SCM – Limitation in cervical PROM 9/10/2021 © 2014 C. Daly, G. Neslund 7
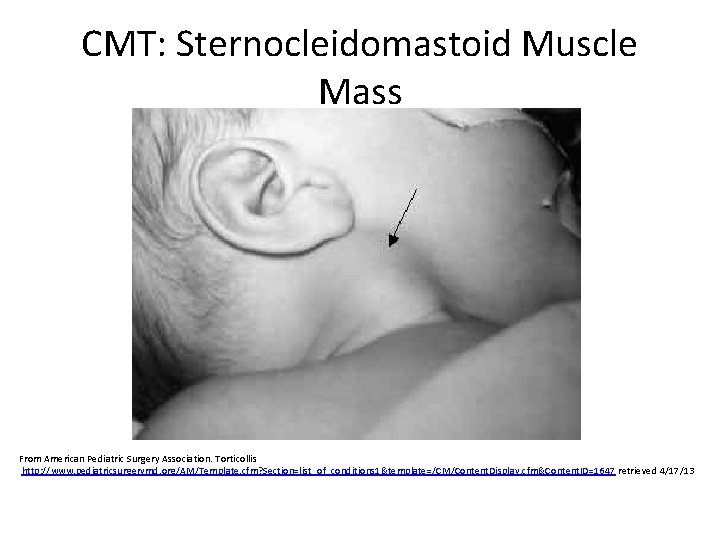
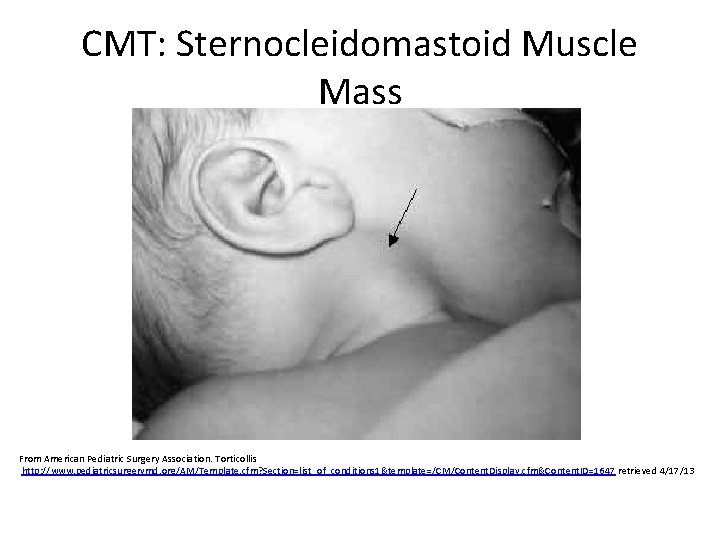
CMT: Sternocleidomastoid Muscle Mass From American Pediatric Surgery Association. Torticollis http: //www. pediatricsurgerymd. org/AM/Template. cfm? Section=list_of_conditions 1&template=/CM/Content. Display. cfm&Content. ID=1647 retrieved 4/17/13
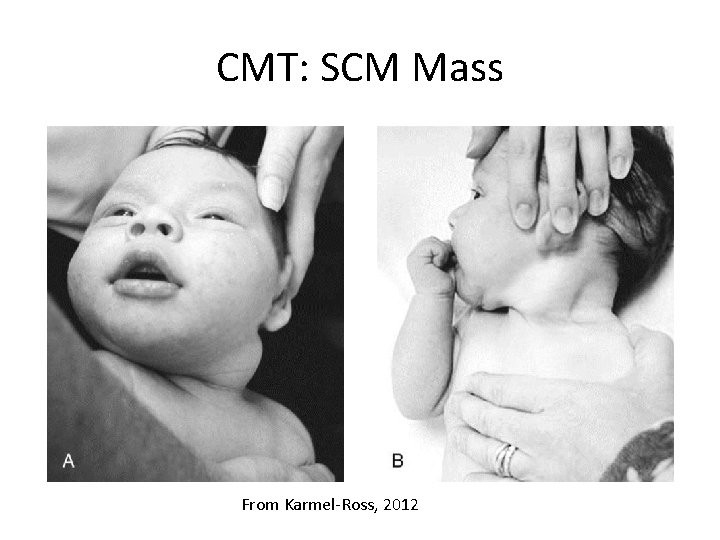
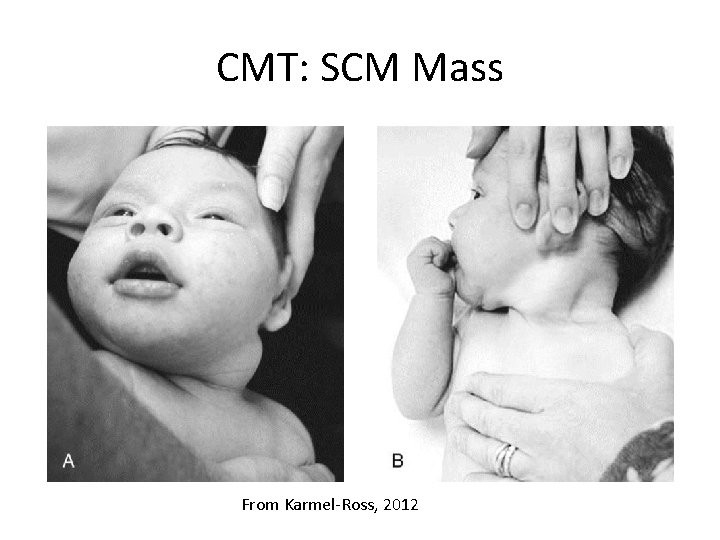
CMT: SCM Mass From Karmel-Ross, 2012
Type of CMT and Prognosis (Kaplan, Coulter, Fetters, 2013) • Type of CMT combined with age at time of diagnosis is predictive of the amount of time required to resolve the torticollis posture – An infants identified early with postural CMT is expected to have the shortest treatment episode – Infants identified after 3 -6 months of age with SCM mass CMT have the longest episodes of conservative treatment and may require more invasive interventions 9/10/2021 © 2014 C. Daly, G. Neslund 10
CMT: Associated Conditions (Kaplan, Coulter, Fetters, 2013) • • • Developmental hip dysplasia Foot deformity Brachial plexus injury Plagiocephaly Pelvic asymmetry Scoliosis
Non-Muscular Torticollis: Neurologic Causes • Acquired torticollis secondary to neurologic causes: – Arnold-Chiari malformation – Syringomyelia – Post-encephalitis syndromes – Posterior fossa tumor – Brain stem, cerebellar, and spinal cord tumors • Associated symptoms may include nausea, vomiting, and positive neurologic signs
Non-Muscular Torticollis: Ocular Causes • Acquired torticollis due to ocular involvement – Unilateral impairment of extra-ocular muscles or defects in visual field lead to abnormal head posture in order to achieve clear binocular vision and/or avoid diplopia – Typically occurs after the infant has developed head control and binocular vision – Associated with full cervical PROM
Non-Muscular Torticollis: Orthopedic Causes • Osseous torticollis – Congenital torticollis posture with abnormal radiographs • • Klipel-Feil syndrome Hemi-vertebrae Atlanto-axial disassociation C 1 -C 2 subluxation (Grisel's syndrome)
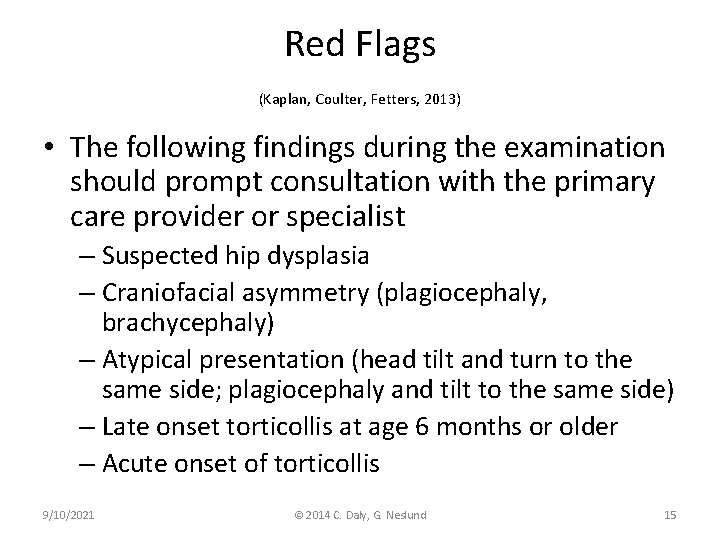
Red Flags (Kaplan, Coulter, Fetters, 2013) • The following findings during the examination should prompt consultation with the primary care provider or specialist – Suspected hip dysplasia – Craniofacial asymmetry (plagiocephaly, brachycephaly) – Atypical presentation (head tilt and turn to the same side; plagiocephaly and tilt to the same side) – Late onset torticollis at age 6 months or older – Acute onset of torticollis 9/10/2021 © 2014 C. Daly, G. Neslund 15
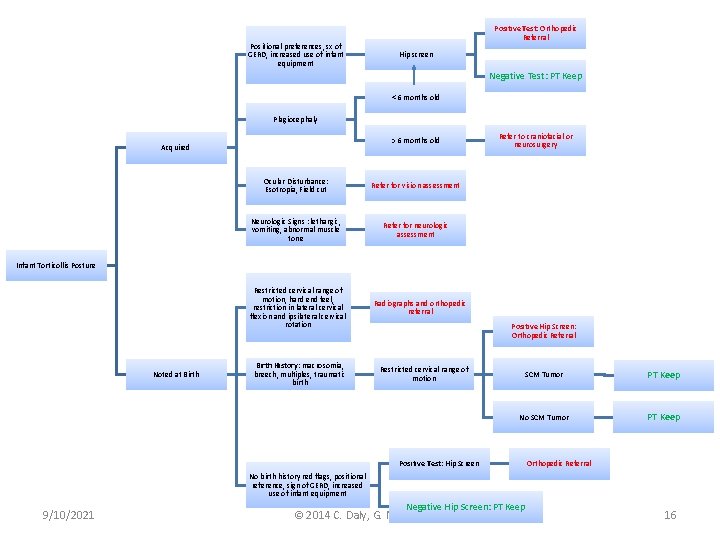
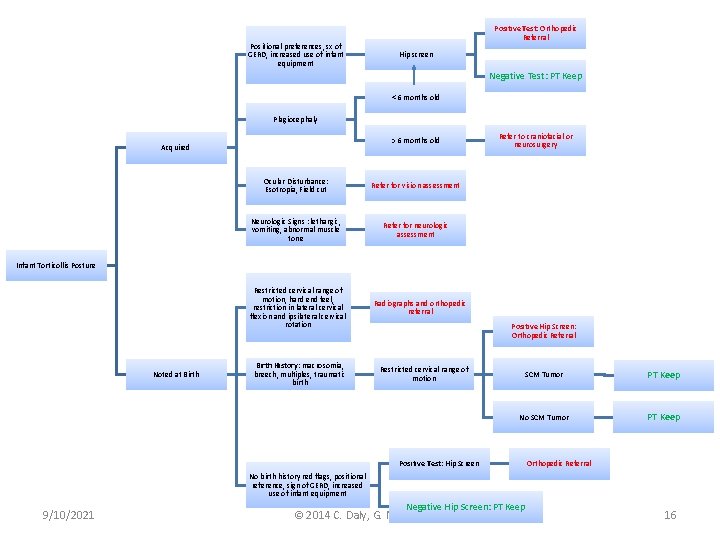
Positional preferences, sx of GERD, increased use of infant equipment Positive Test: Orthopedic Referral Hip screen Negative Test: PT Keep < 6 months old Plagiocephaly > 6 months old Acquired Ocular Disturbance: Esotropia, Field cut Refer for vision assessment Neurologic Signs : lethargic, vomiting, abnormal muscle tone Refer for neurologic assessment Refer to craniofacial or neurosurgery Infant Torticollis Posture Noted at Birth Restricted cervical range of motion, hard end feel, restriction in lateral cervical flexion and ipsilateral cervical rotation Radiographs and orthopedic referral Birth History: macrosomia, breech, multiples, traumatic birth Restricted cervical range of motion Positive Hip Screen: Orthopedic Referral SCM Tumor PT Keep No SCM Tumor PT Keep Positive Test: Hip Screen Orthopedic Referral No birth history red flags, positional reference, sign of GERD, increased use of infant equipment 9/10/2021 Negative Hip Screen: PT Keep © 2014 C. Daly, G. Neslund 16
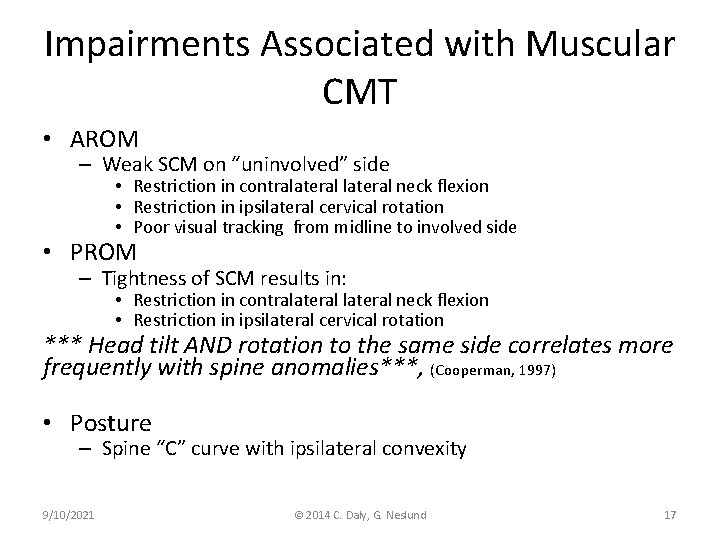
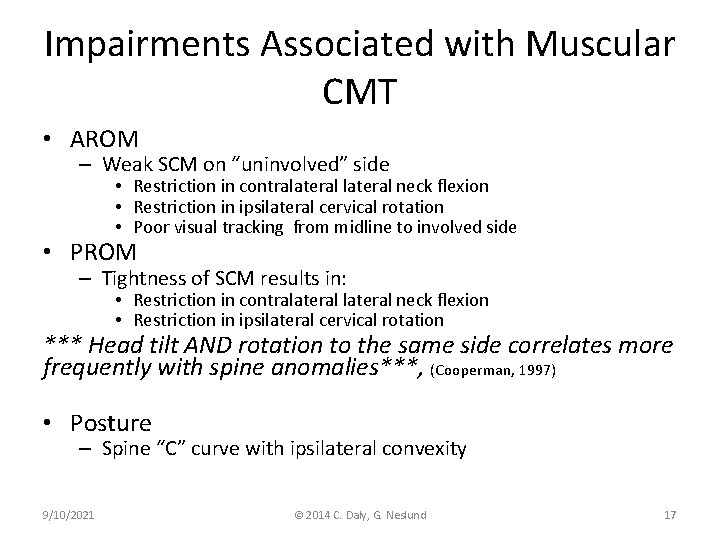
Impairments Associated with Muscular CMT • AROM – Weak SCM on “uninvolved” side • Restriction in contralateral neck flexion • Restriction in ipsilateral cervical rotation • Poor visual tracking from midline to involved side • PROM – Tightness of SCM results in: • Restriction in contralateral neck flexion • Restriction in ipsilateral cervical rotation *** Head tilt AND rotation to the same side correlates more frequently with spine anomalies***, (Cooperman, 1997) • Posture – Spine “C” curve with ipsilateral convexity 9/10/2021 © 2014 C. Daly, G. Neslund 17
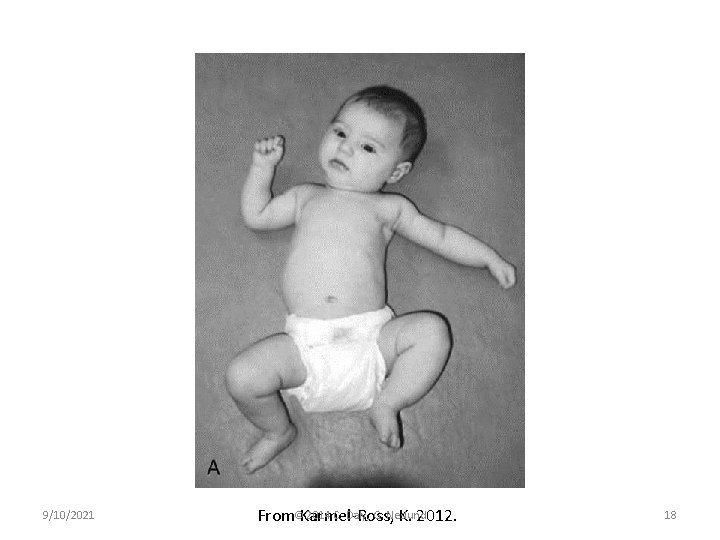
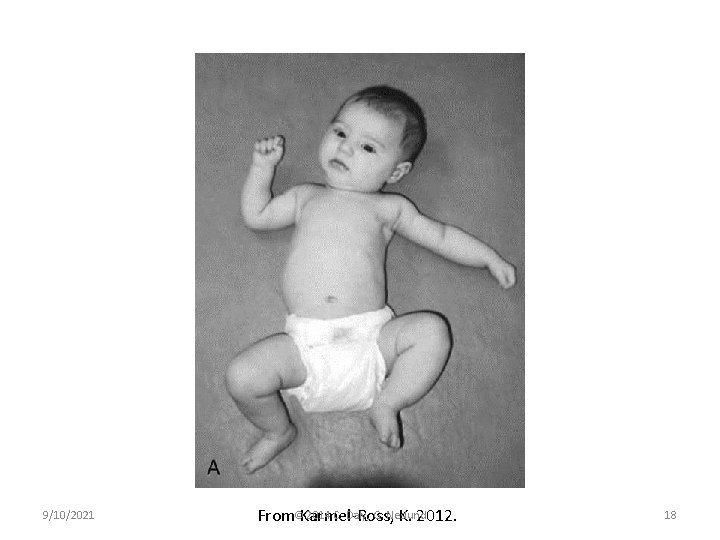
9/10/2021 2014 C. Daly, G. Neslund From©Karmel-Ross, K. 2012. 18
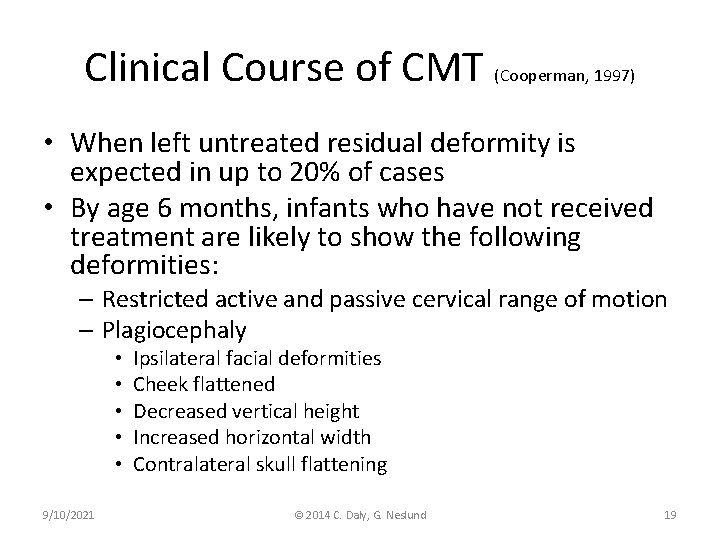
Clinical Course of CMT (Cooperman, 1997) • When left untreated residual deformity is expected in up to 20% of cases • By age 6 months, infants who have not received treatment are likely to show the following deformities: – Restricted active and passive cervical range of motion – Plagiocephaly • • • 9/10/2021 Ipsilateral facial deformities Cheek flattened Decreased vertical height Increased horizontal width Contralateral skull flattening © 2014 C. Daly, G. Neslund 19
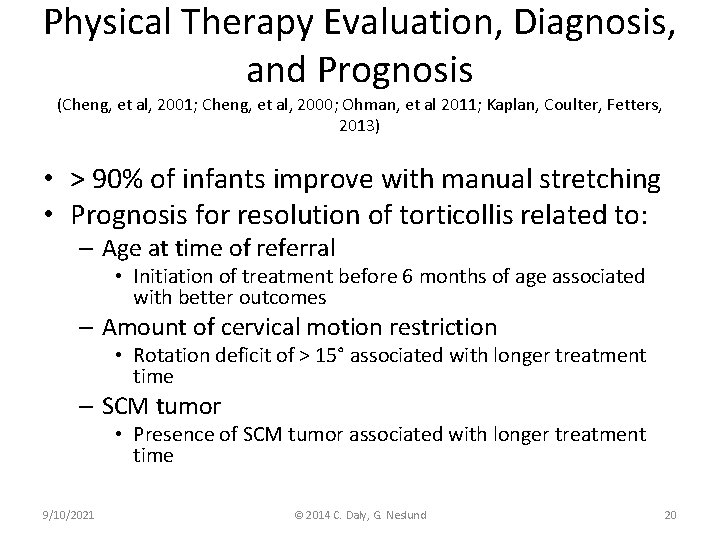
Physical Therapy Evaluation, Diagnosis, and Prognosis (Cheng, et al, 2001; Cheng, et al, 2000; Ohman, et al 2011; Kaplan, Coulter, Fetters, 2013) • > 90% of infants improve with manual stretching • Prognosis for resolution of torticollis related to: – Age at time of referral • Initiation of treatment before 6 months of age associated with better outcomes – Amount of cervical motion restriction • Rotation deficit of > 15° associated with longer treatment time – SCM tumor • Presence of SCM tumor associated with longer treatment time 9/10/2021 © 2014 C. Daly, G. Neslund 20
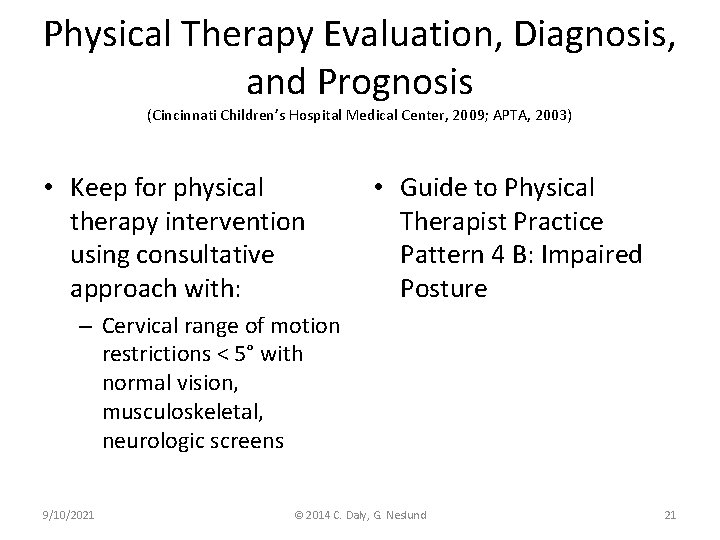
Physical Therapy Evaluation, Diagnosis, and Prognosis (Cincinnati Children’s Hospital Medical Center, 2009; APTA, 2003) • Keep for physical therapy intervention using consultative approach with: • Guide to Physical Therapist Practice Pattern 4 B: Impaired Posture – Cervical range of motion restrictions < 5° with normal vision, musculoskeletal, neurologic screens 9/10/2021 © 2014 C. Daly, G. Neslund 21
Physical Therapy Evaluation, Diagnosis, and Prognosis (Cincinnati Children’s Hospital Medical Center, 2009; APTA, 2003) • Keep for physical therapy intervention with: – Cervical range of motion restrictions > 5° with normal vision, musculoskeletal, neurologic screens 9/10/2021 • Guide to Physical Therapist Practice Pattern 4 B: Impaired Posture © 2014 C. Daly, G. Neslund 22
Physical Therapy Evaluation, Diagnosis, and Prognosis (Kapalan, et al, 2013; Tessmer, Mooney, Pelland, 2010; Freed & Coulter-O’Berry, 2004) • Association between CMT and early motor developmental delay – Motor delay typically resolves by toddler age • No long term effect on perceptual or cognitive development • Positioning, passive manual stretching, cervical muscle strengthening, and developmentally supportive interventions associated with positive outcomes 9/10/2021 © 2014 C. Daly, G. Neslund 23
Goals and Expected Outcomes • Long term goals: 3 – 6 months – Active and passive cervical range of motion that is restricted by no more than 5° – Age appropriate motor skills • Short term goals: 30 days – Goal attainment scaling of LTG 9/10/2021 © 2014 C. Daly, G. Neslund 24
Physical Therapy Plan of Care: Interventions (Kaplan, et al, 3013; Christensen, et al, 2013; Cincinnati Children’s Hospital Medical Center, 2009; Luxford, Hale, & Piggot, 2009) • Primary evidence based interventions – Parent/caregiver education – Environmental adaptations • Positioning in midline – Gentle manual stretching multiple times/day • Carry positions • Cervical PROM – achieved without resistance, pain or crying! – Neck and trunk AROM • Cervical lateral flexor muscle strengthening for infants > 4 m – Development of symmetrical movement 9/10/2021 © 2014 C. Daly, G. Neslund 25
Parent/Caregiver Education (Kaplan, Coulter, Fetters, 20130 • Parents should be informed about the importance of – “Tummy time” prone positioning – Positioning and handling for symmetrical posture – Alternating feedings to both sides – Minimizing time spent in car seats and carriers 9/10/2021 © 2014 C. Daly, G. Neslund 26
9/10/2021 © 2014 C. Daly, G. Neslund 27
Environmental Adaptations (Kaplan, Coulter, Fetters, 2013) • Parents and caregivers should be encouraged to use the following environmental adaptations: – Alternating head of bed and changing table – Adapting car seat with head, trunk, and hip rolls to encourage symmetrical posture – Placing toys overhead and/or to the non-preferred side 9/10/2021 © 2014 C. Daly, G. Neslund 28
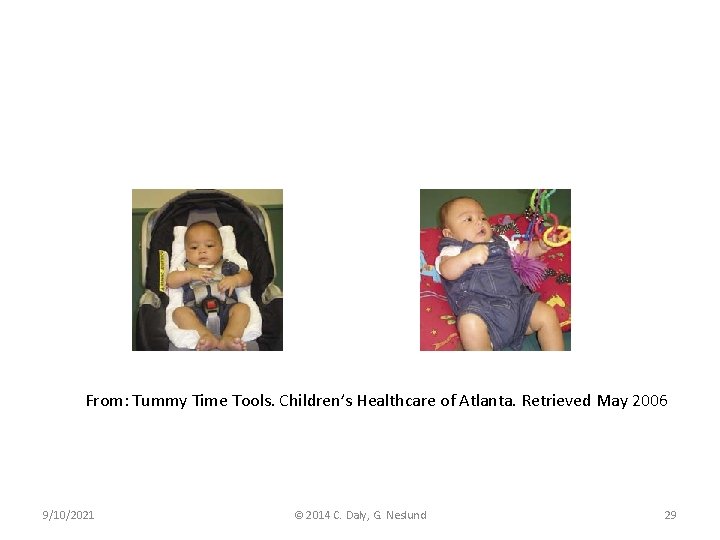
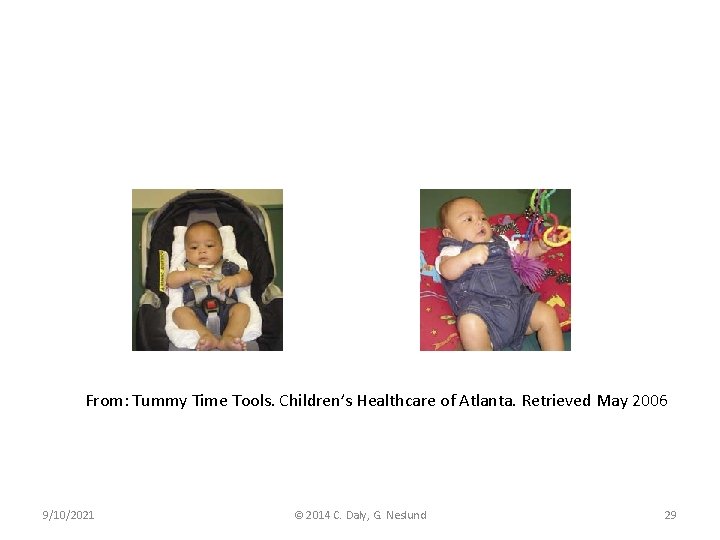
From: Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved May 2006 9/10/2021 © 2014 C. Daly, G. Neslund 29
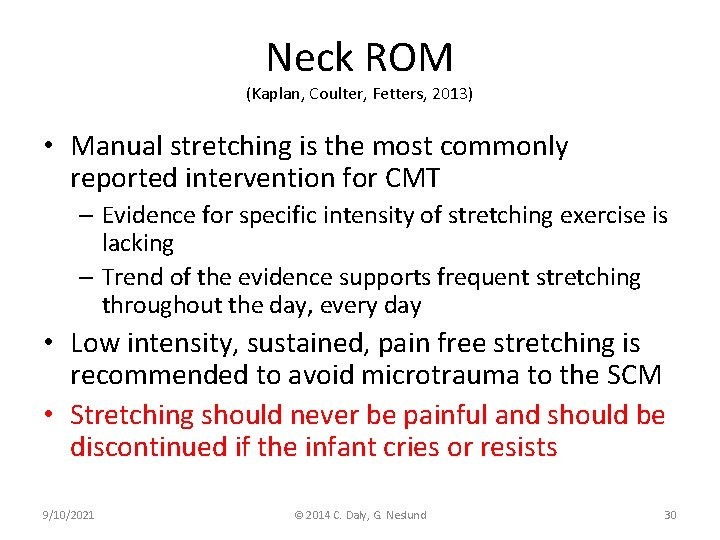
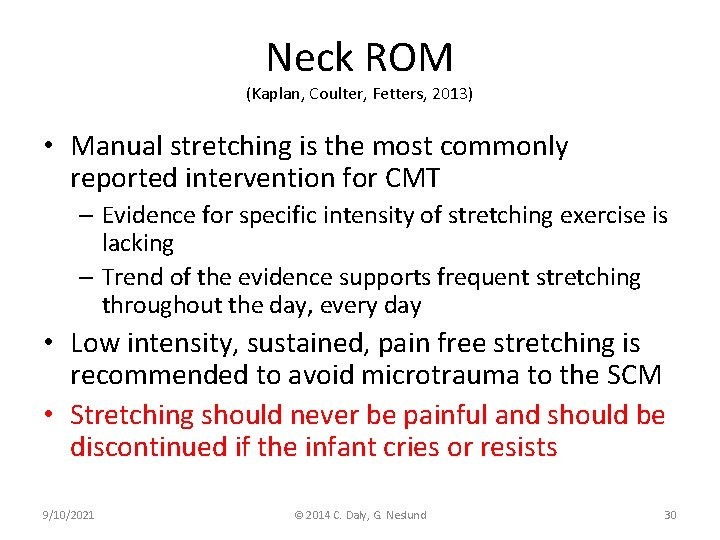
Neck ROM (Kaplan, Coulter, Fetters, 2013) • Manual stretching is the most commonly reported intervention for CMT – Evidence for specific intensity of stretching exercise is lacking – Trend of the evidence supports frequent stretching throughout the day, every day • Low intensity, sustained, pain free stretching is recommended to avoid microtrauma to the SCM • Stretching should never be painful and should be discontinued if the infant cries or resists 9/10/2021 © 2014 C. Daly, G. Neslund 30
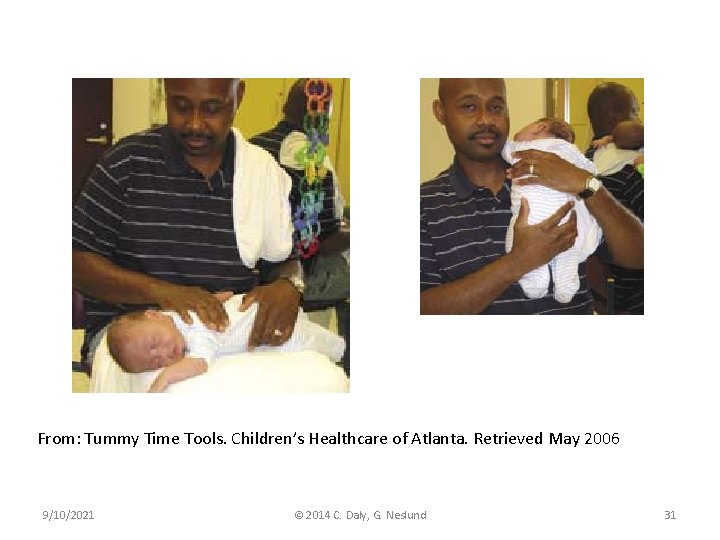
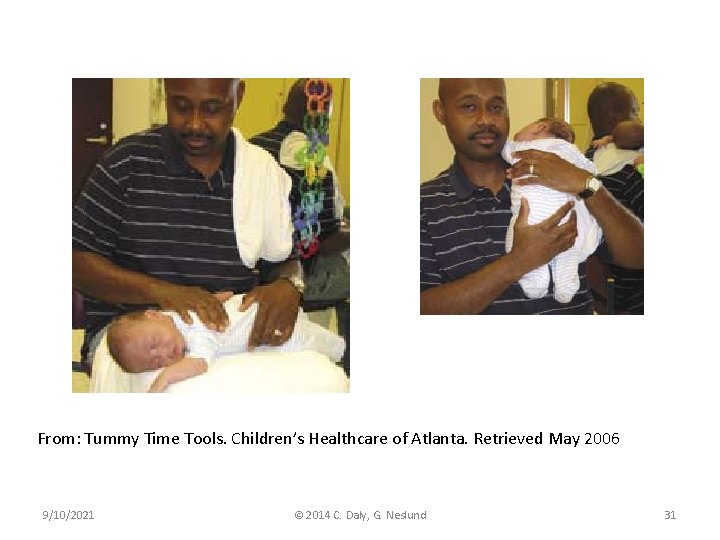
From: Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved May 2006 9/10/2021 © 2014 C. Daly, G. Neslund 31
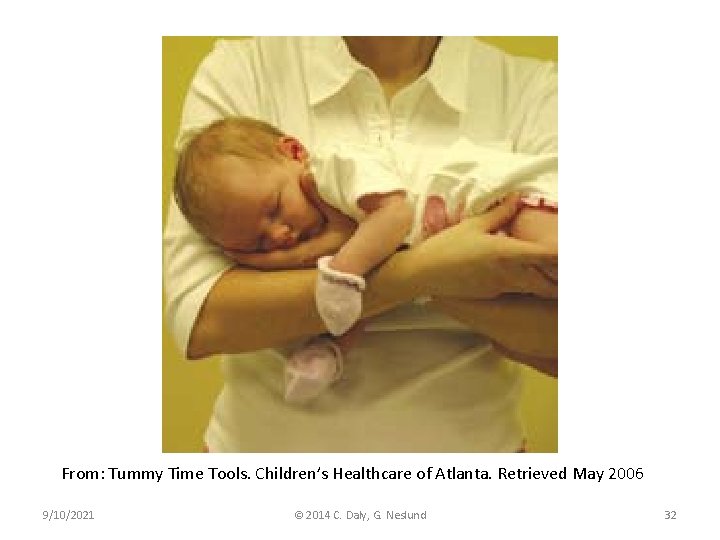
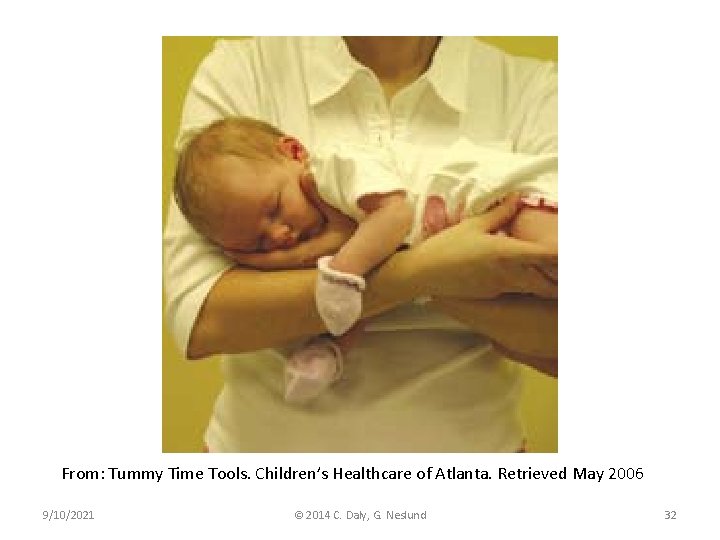
From: Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved May 2006 9/10/2021 © 2014 C. Daly, G. Neslund 32
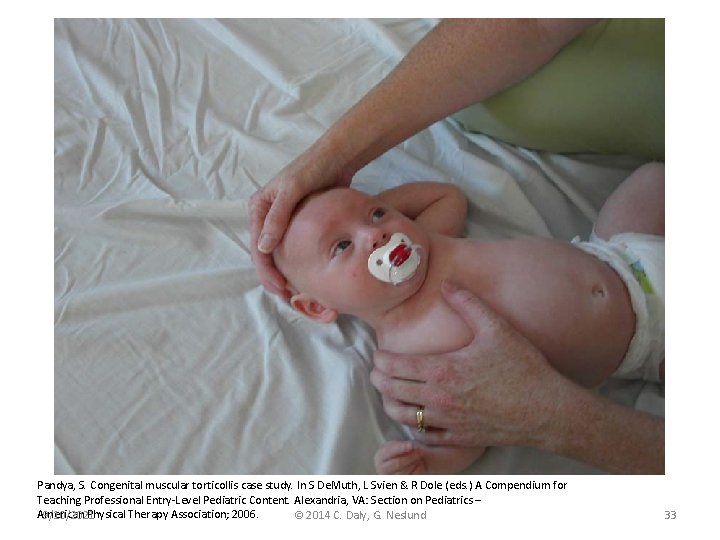
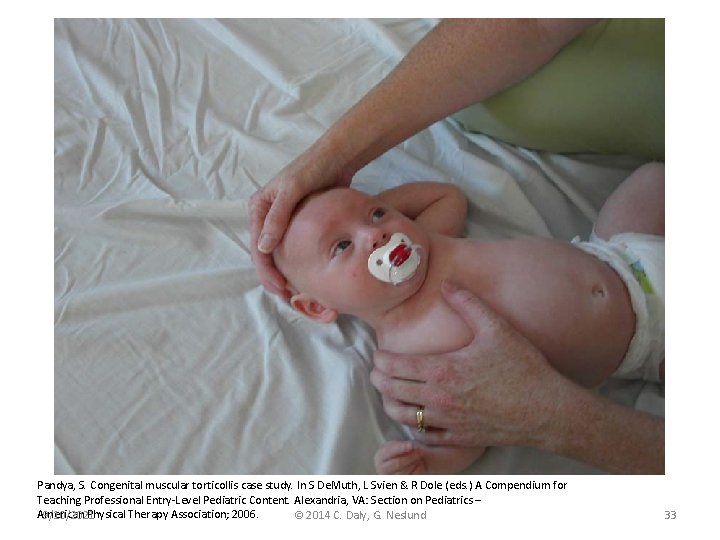
Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for Teaching Professional Entry-Level Pediatric Content. Alexandria, VA: Section on Pediatrics – American Physical Therapy Association; 2006. 9/10/2021 © 2014 C. Daly, G. Neslund 33
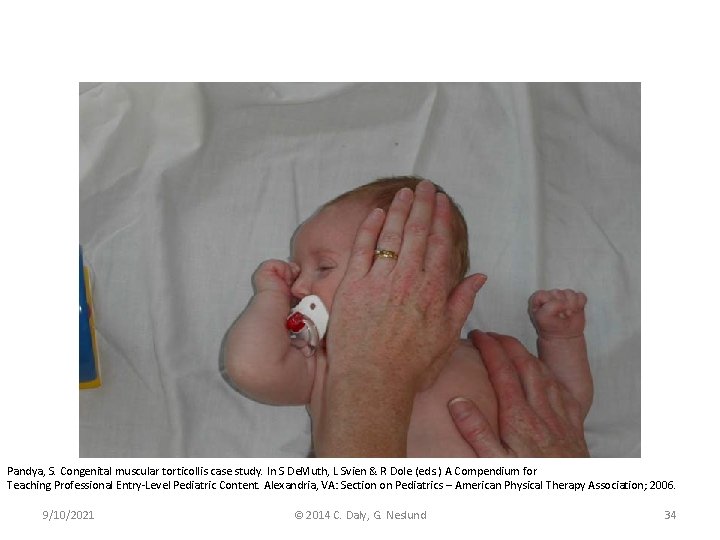
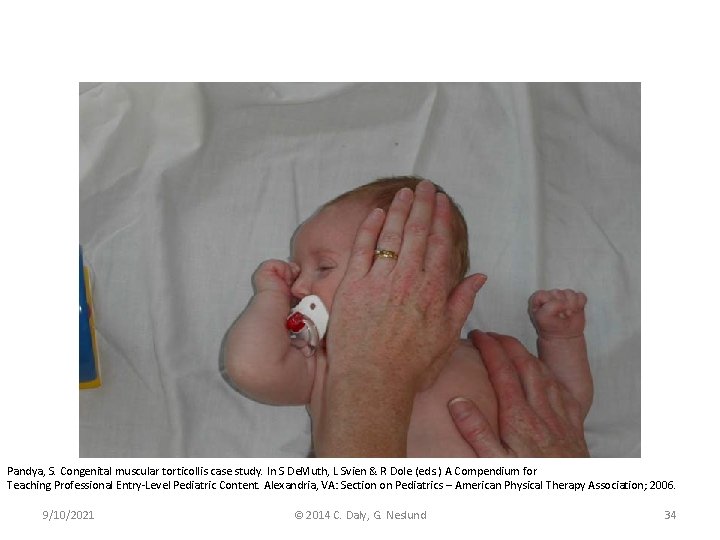
Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for Teaching Professional Entry-Level Pediatric Content. Alexandria, VA: Section on Pediatrics – American Physical Therapy Association; 2006. 9/10/2021 © 2014 C. Daly, G. Neslund 34
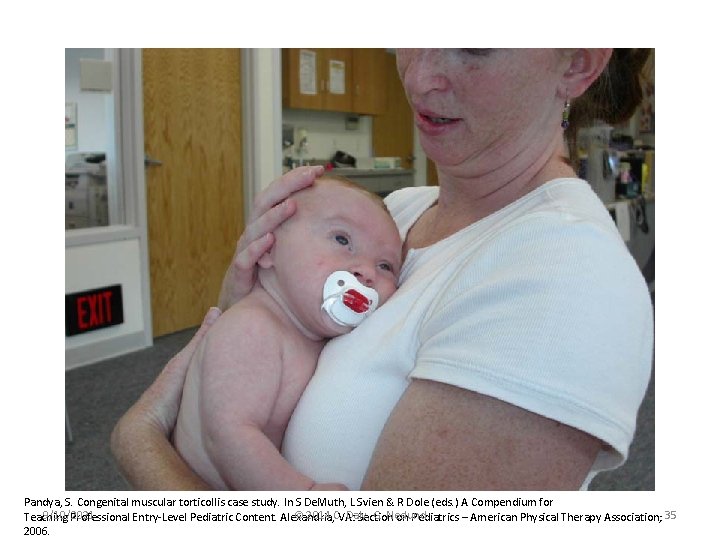
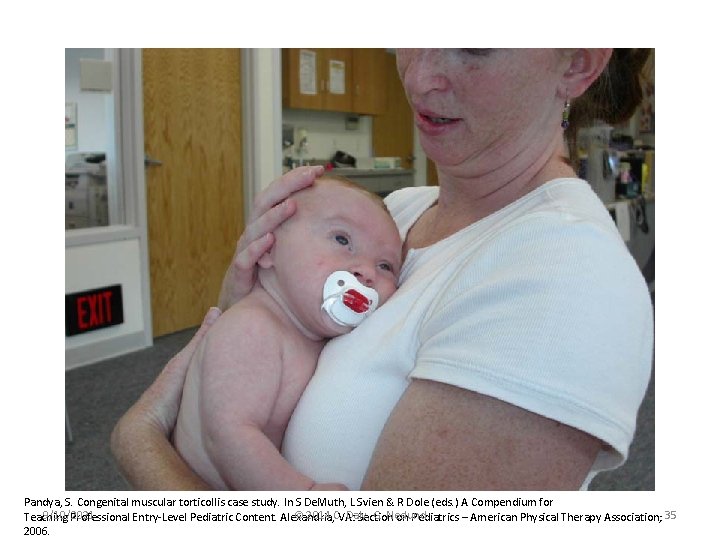
Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for 9/10/2021 © 2014 C. VA: Daly, G. Neslund Teaching Professional Entry-Level Pediatric Content. Alexandria, Section on Pediatrics – American Physical Therapy Association; 35 2006.
Neck / Trunk Strengthening and Development of Symmetrical Movement (Kaplan, Coulter, Fetters, 2013) • Active head turning to the non-preferred side • Activate righting reactions in upright postures: – Rolling – Side lying – Sitting 9/10/2021 © 2014 C. Daly, G. Neslund 36

Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for Teaching Professional Entry-Level Pediatric Content. Alexandria, VA: Pediatrics – American Physical Therapy Association; 2006 9/10/2021 © 2014 C. Section Daly, G. on Neslund 37.
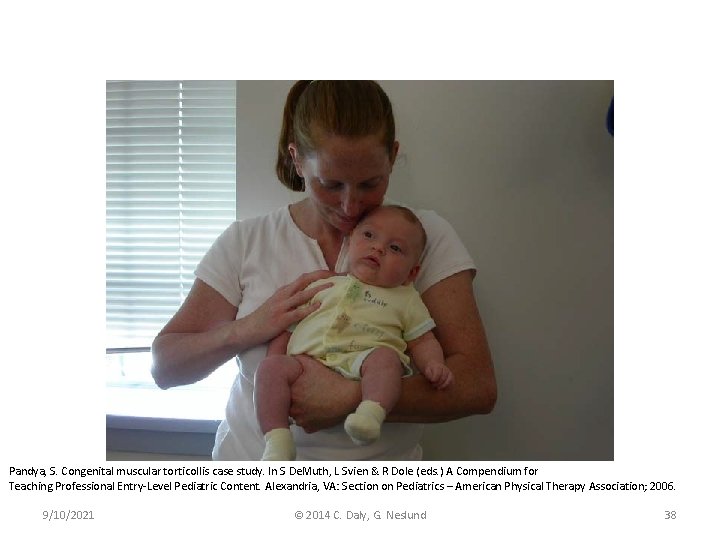
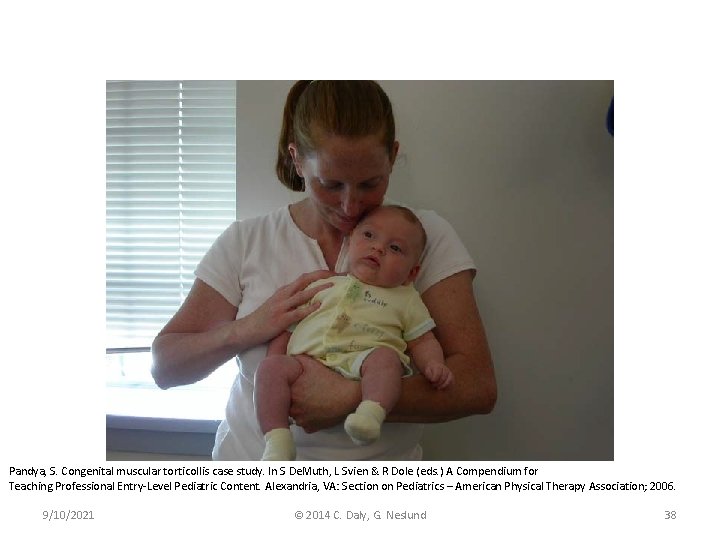
Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for Teaching Professional Entry-Level Pediatric Content. Alexandria, VA: Section on Pediatrics – American Physical Therapy Association; 2006. 9/10/2021 © 2014 C. Daly, G. Neslund 38
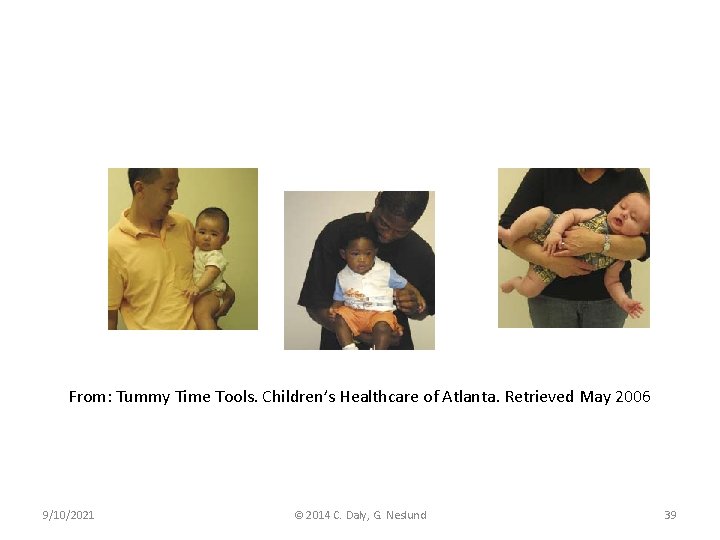
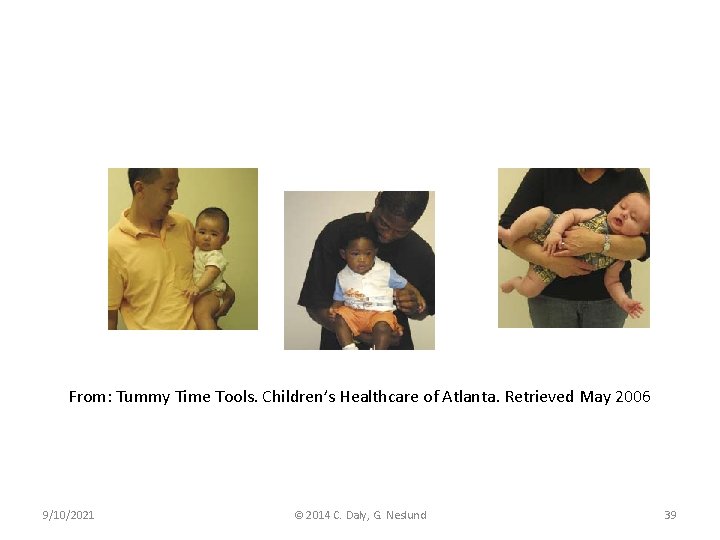
From: Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved May 2006 9/10/2021 © 2014 C. Daly, G. Neslund 39
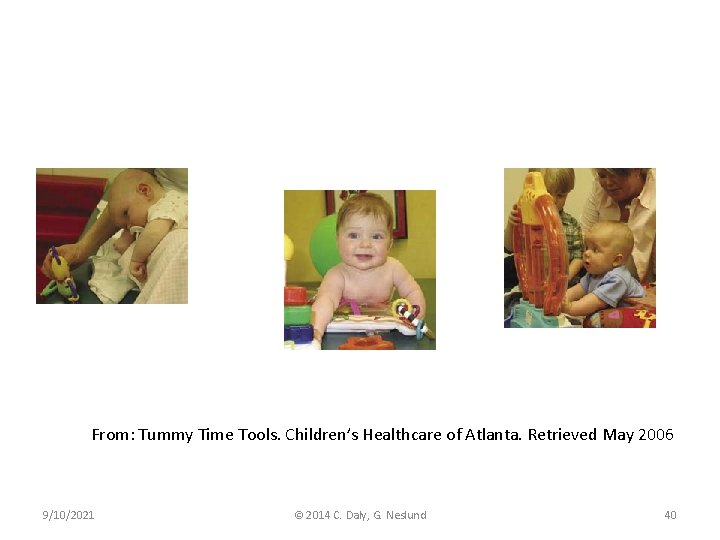
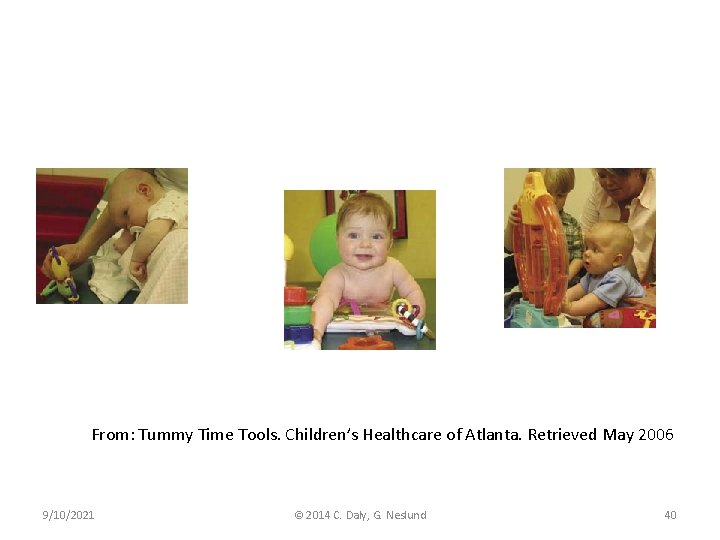
From: Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved May 2006 9/10/2021 © 2014 C. Daly, G. Neslund 40
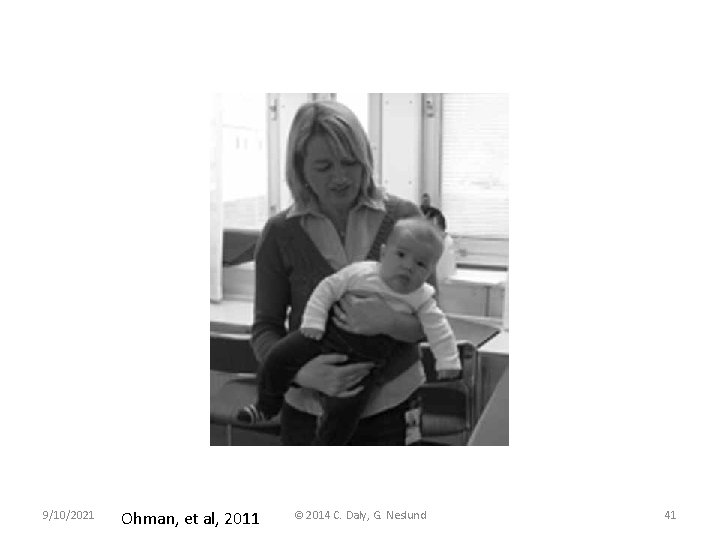
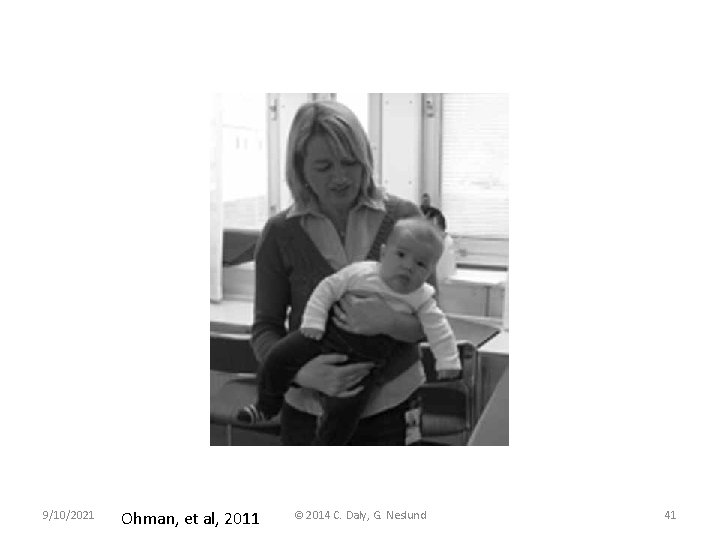
9/10/2021 Ohman, et al, 2011 © 2014 C. Daly, G. Neslund 41
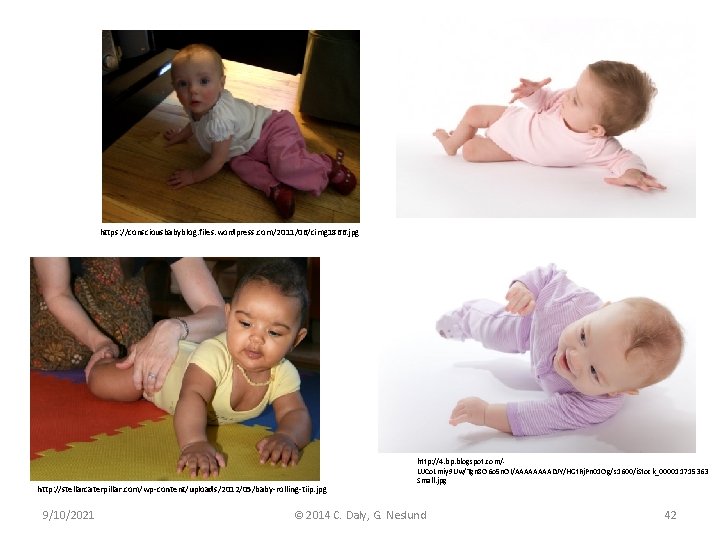
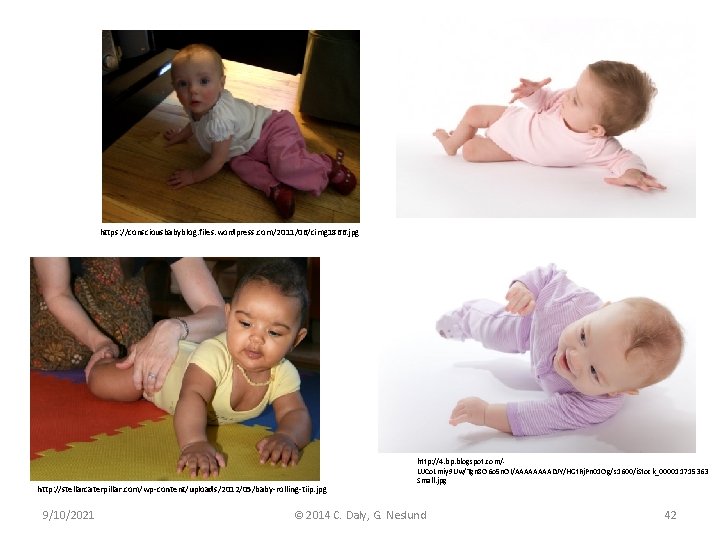
https: //consciousbabyblog. files. wordpress. com/2011/06/cimg 1866. jpg http: //stellarcaterpillar. com/wp-content/uploads/2012/05/baby-rolling-tiip. jpg 9/10/2021 http: //4. bp. blogspot. com/UJCo. Lmiy 9 Uw/Tgn 8 O 6 o 5 n. OI/AAAADJY/HGt. Rj. Pn 01 Og/s 1600/i. Stock_000011715363 Small. jpg © 2014 C. Daly, G. Neslund 42
• Video of PROM, carry positions, cervical ms. strengthening? 9/10/2021 © 2014 C. Daly, G. Neslund 43
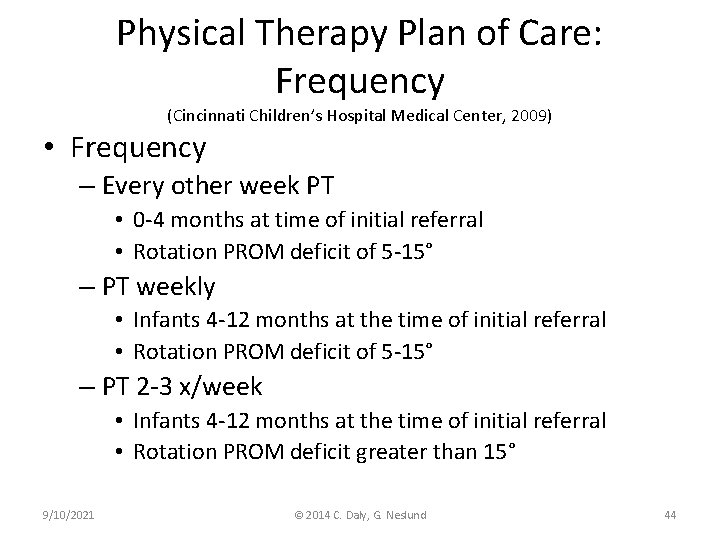
Physical Therapy Plan of Care: Frequency (Cincinnati Children’s Hospital Medical Center, 2009) • Frequency – Every other week PT • 0 -4 months at time of initial referral • Rotation PROM deficit of 5 -15° – PT weekly • Infants 4 -12 months at the time of initial referral • Rotation PROM deficit of 5 -15° – PT 2 -3 x/week • Infants 4 -12 months at the time of initial referral • Rotation PROM deficit greater than 15° 9/10/2021 © 2014 C. Daly, G. Neslund 44
Physical Therapy Re-examination (Cincinnati Children’s Hospital Medical Center, 2009) • Re-examination at each visit • Re-assess: – Passive and active cervical ROM – Cervical muscle strength – Developmental skills • Symmetry of postural control • At each visit review and update HEP 9/10/2021 © 2014 C. Daly, G. Neslund 45

Physical Therapy Re-examination (Cincinnati Children’s Hospital Medical Center, 2009) • At each visit re-evaluate frequency – Decrease to every other week good compliance with HEP, improved ROM, improved developmental skills – Short trial of increase to 2 x/week if child is not progressing • Refer back to MD if trial does not improve with increased frequency of PT 9/10/2021 © 2014 C. Daly, G. Neslund 46
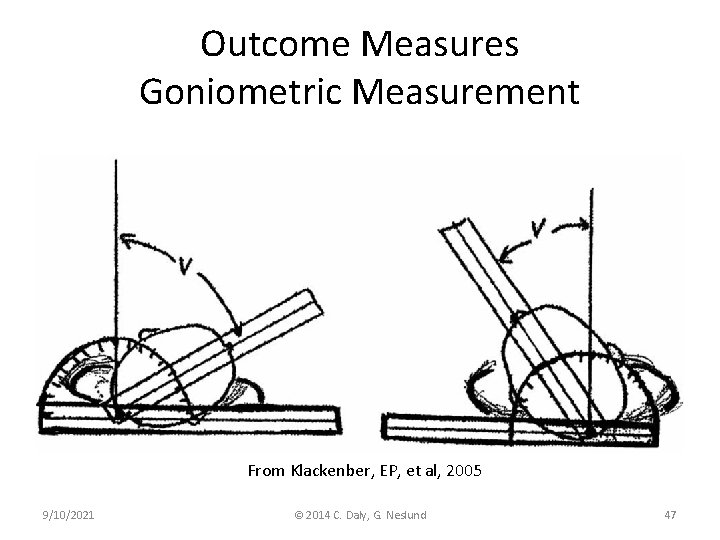
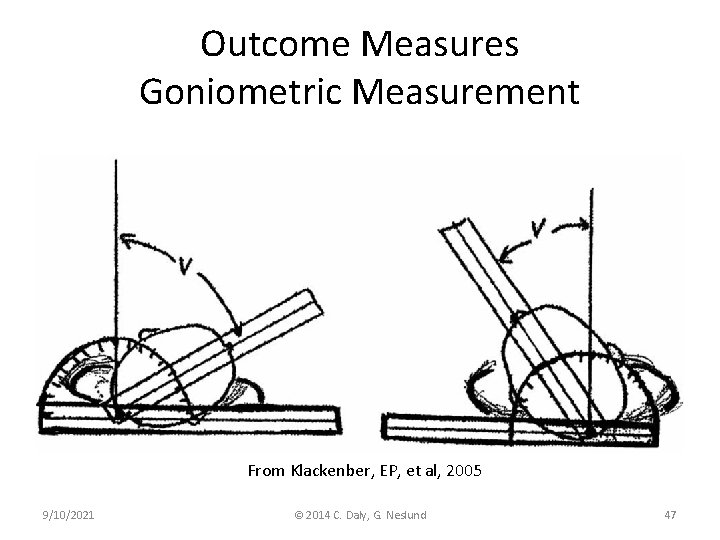
Outcome Measures Goniometric Measurement From Klackenber, EP, et al, 2005 9/10/2021 © 2014 C. Daly, G. Neslund 47
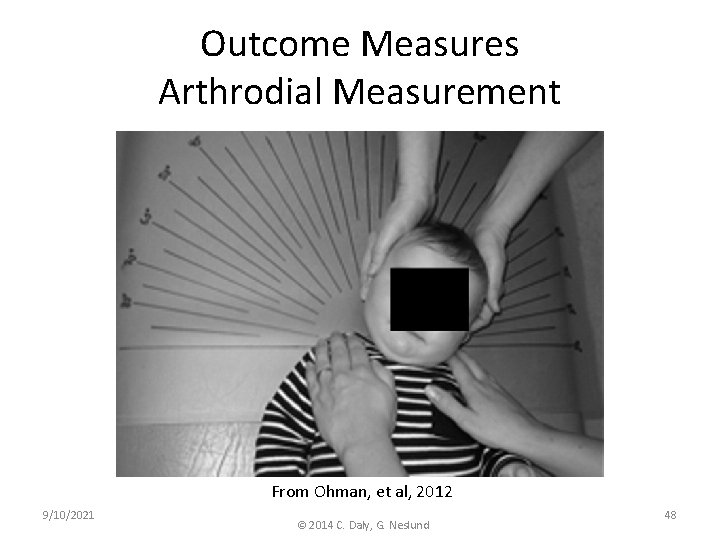
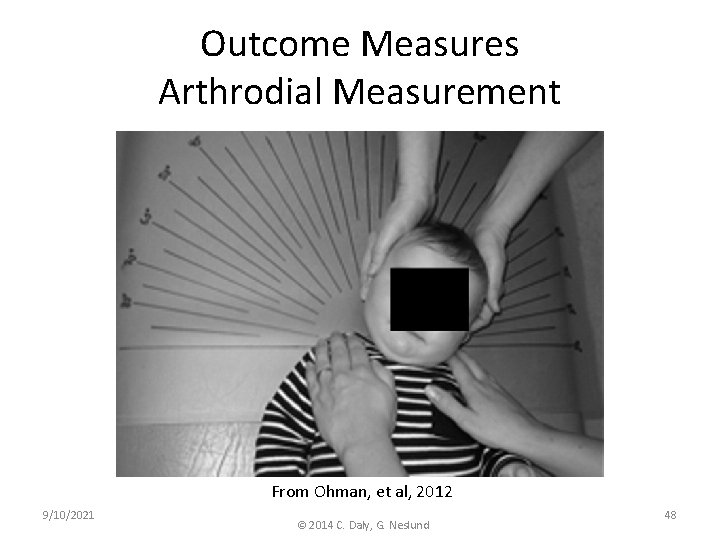
Outcome Measures Arthrodial Measurement From Ohman, et al, 2012 9/10/2021 © 2014 C. Daly, G. Neslund 48
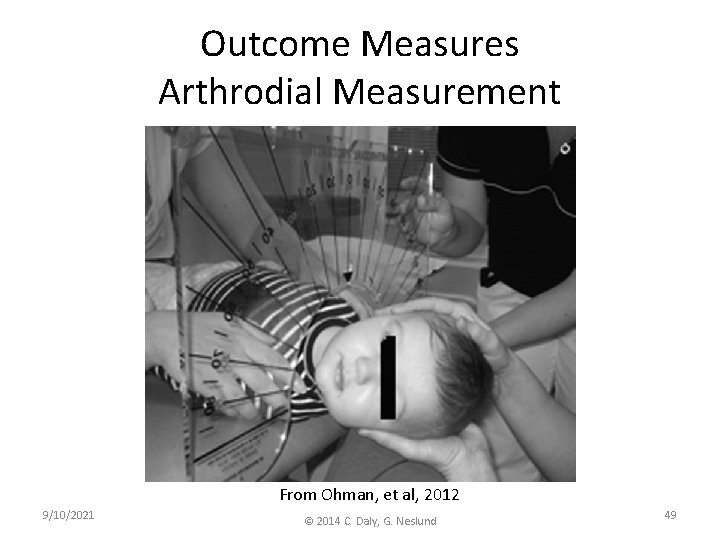
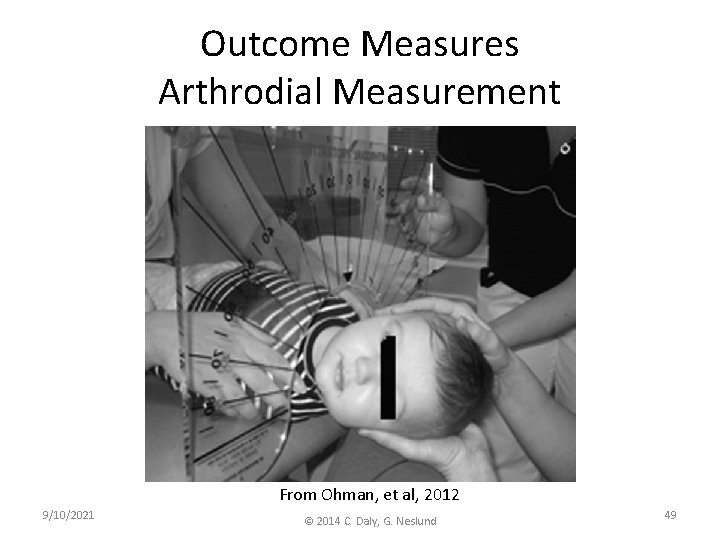
Outcome Measures Arthrodial Measurement From Ohman, et al, 2012 9/10/2021 © 2014 C. Daly, G. Neslund 49
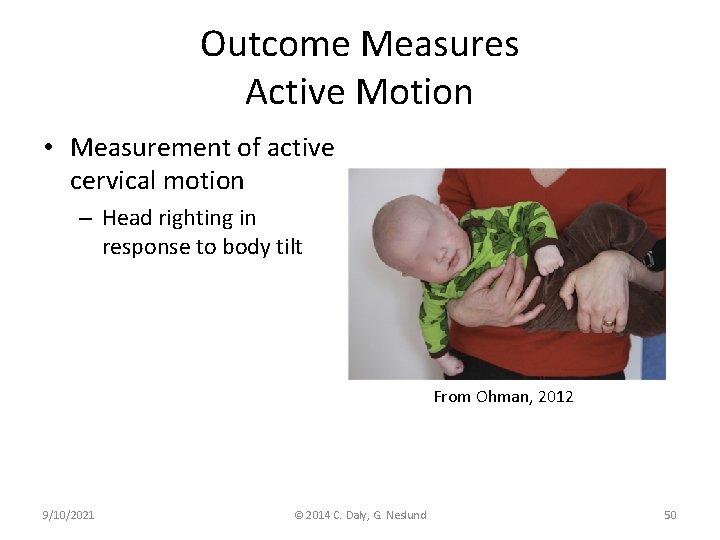
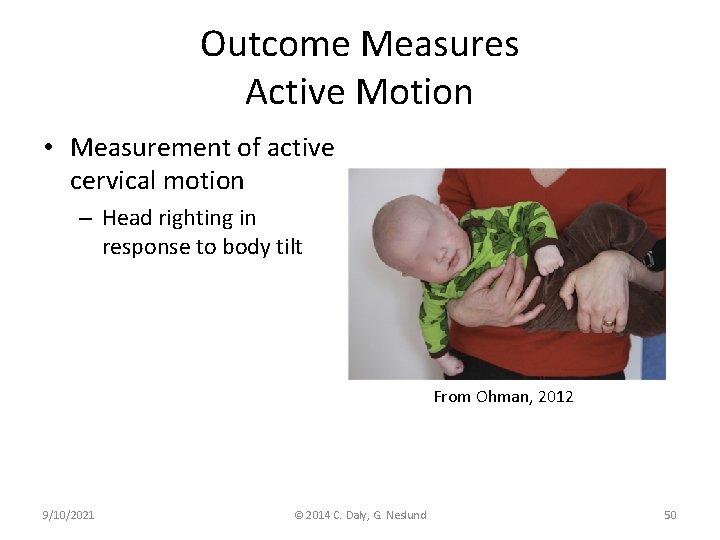
Outcome Measures Active Motion • Measurement of active cervical motion – Head righting in response to body tilt From Ohman, 2012 9/10/2021 © 2014 C. Daly, G. Neslund 50
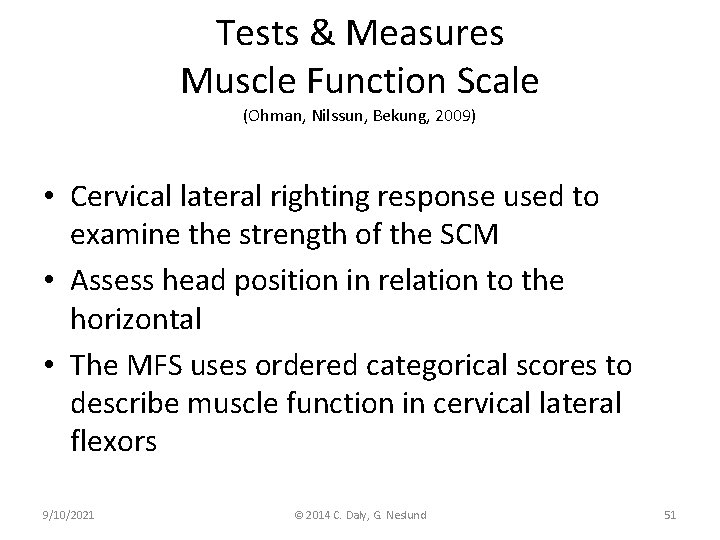
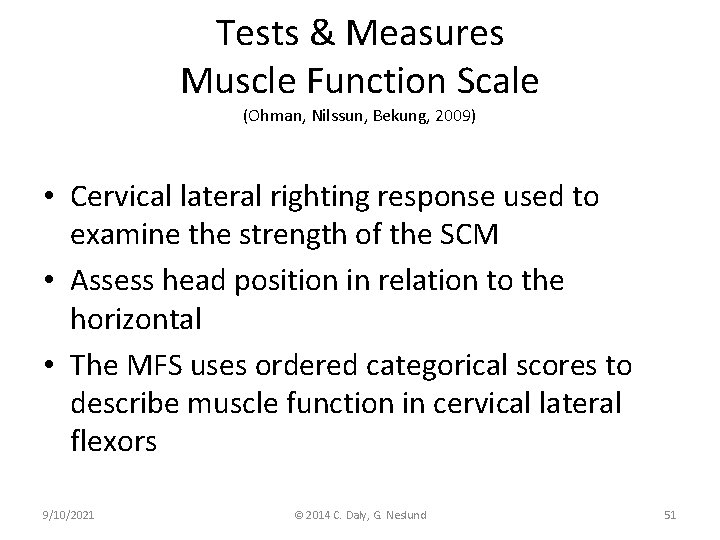
Tests & Measures Muscle Function Scale (Ohman, Nilssun, Bekung, 2009) • Cervical lateral righting response used to examine the strength of the SCM • Assess head position in relation to the horizontal • The MFS uses ordered categorical scores to describe muscle function in cervical lateral flexors 9/10/2021 © 2014 C. Daly, G. Neslund 51

9/10/2021 © 2014 C. Daly, G. Neslund 52 Ohman, Nilssen, Bekung, 2009
Outcome Measures Gross Motor Development • Motor Skills – Assess posture and function in supine, prone, and sitting – Assess mid-line motor control in all positions – Assess head righting – Assess age expected motor development: Alberta Infant Motor Scale (AIMS) 9/10/2021 © 2014 C. Daly, G. Neslund 53
Outcome Measures Gross Motor Development Alberta Infant Motor Scale 9/10/2021 • Norm referenced observational assessment of gross motor development from 0 -18 months • Reliability >0. 90 • Predictive validity for identifying motor developmental delay at 18 m. using cut score of 10% at 4 months and 5% at 8 months © 2014 C. Daly, G. Neslund 54
Goal Attainment Scaling (Westcott & Goulet, 2005) • GAS is a system that assists with the development of specific objectives for an individual • Objectives can be at the body structure and function, activity, and/or participation levels • GAS allows therapist to code progress related to those objectives using a point system 9/10/2021 © 2014 C. Daly, G. Neslund 55
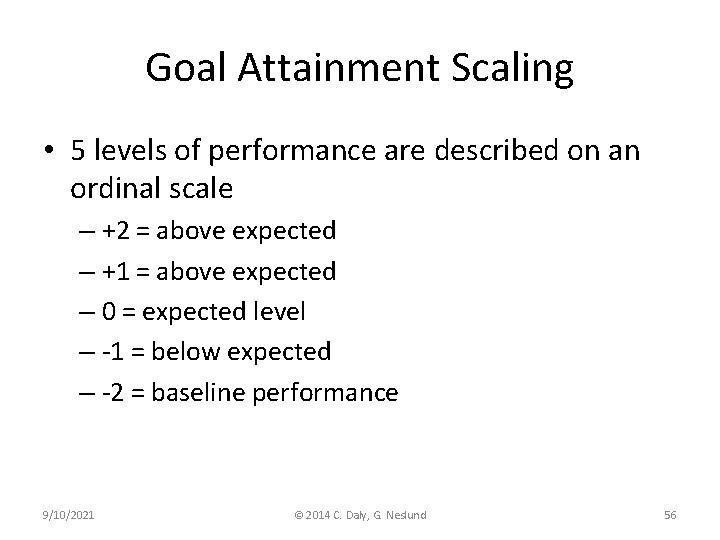
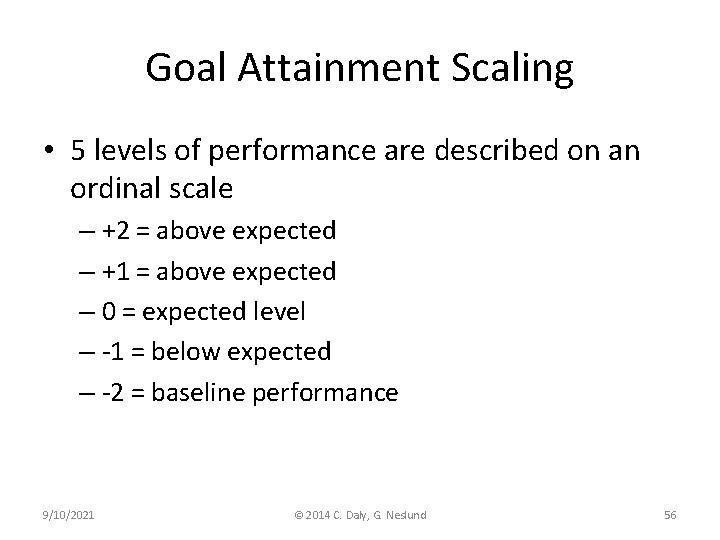
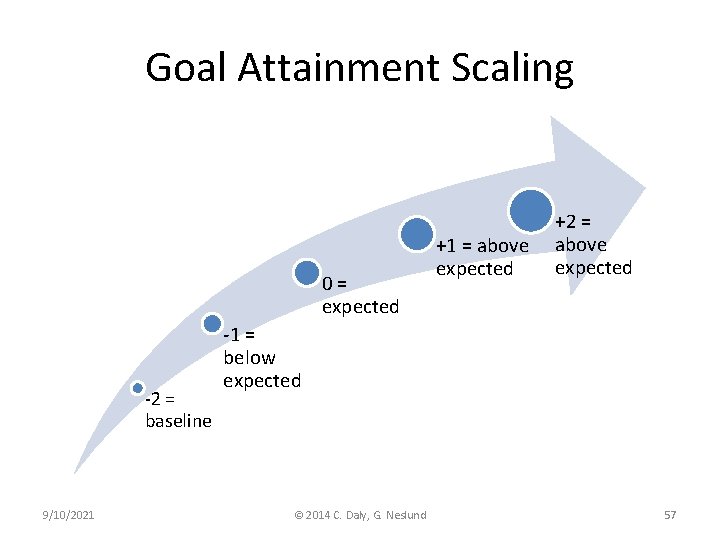
Goal Attainment Scaling • 5 levels of performance are described on an ordinal scale – +2 = above expected – +1 = above expected – 0 = expected level – -1 = below expected – -2 = baseline performance 9/10/2021 © 2014 C. Daly, G. Neslund 56
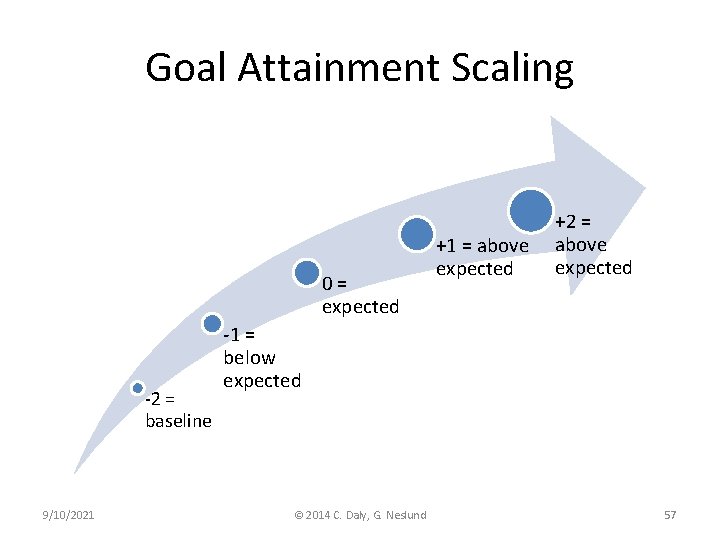
Goal Attainment Scaling 0= expected -2 = baseline 9/10/2021 +1 = above expected +2 = above expected -1 = below expected © 2014 C. Daly, G. Neslund 57
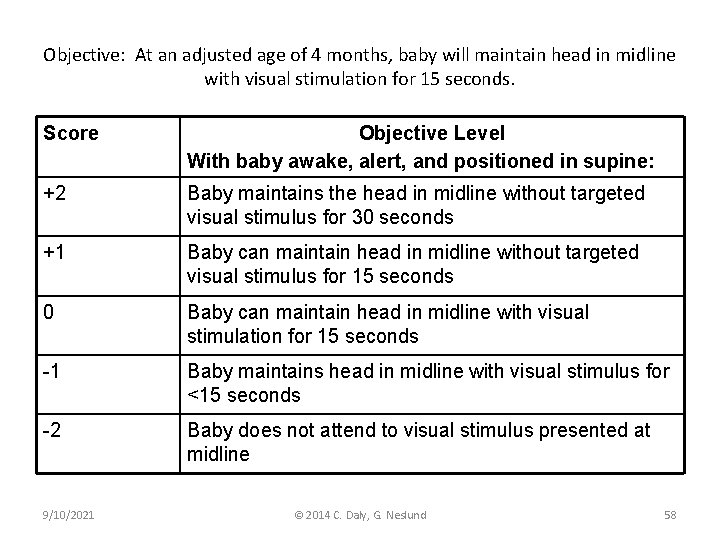
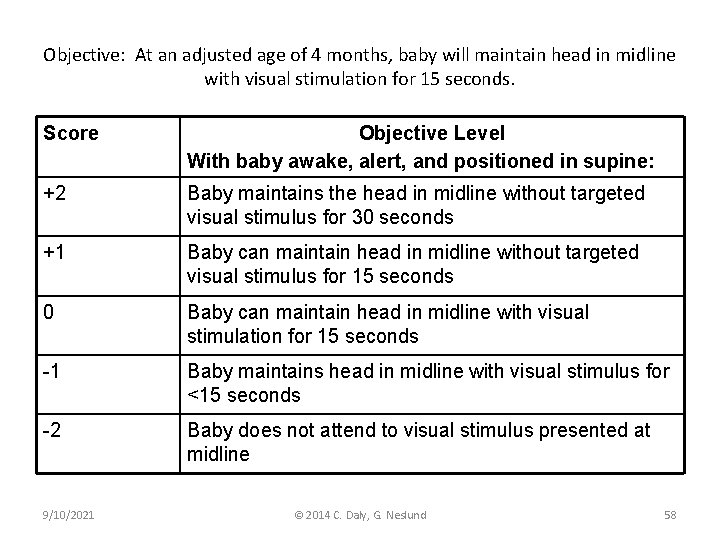
Objective: At an adjusted age of 4 months, baby will maintain head in midline with visual stimulation for 15 seconds. Score Objective Level With baby awake, alert, and positioned in supine: +2 Baby maintains the head in midline without targeted visual stimulus for 30 seconds +1 Baby can maintain head in midline without targeted visual stimulus for 15 seconds 0 Baby can maintain head in midline with visual stimulation for 15 seconds -1 Baby maintains head in midline with visual stimulus for <15 seconds -2 Baby does not attend to visual stimulus presented at midline 9/10/2021 © 2014 C. Daly, G. Neslund 58
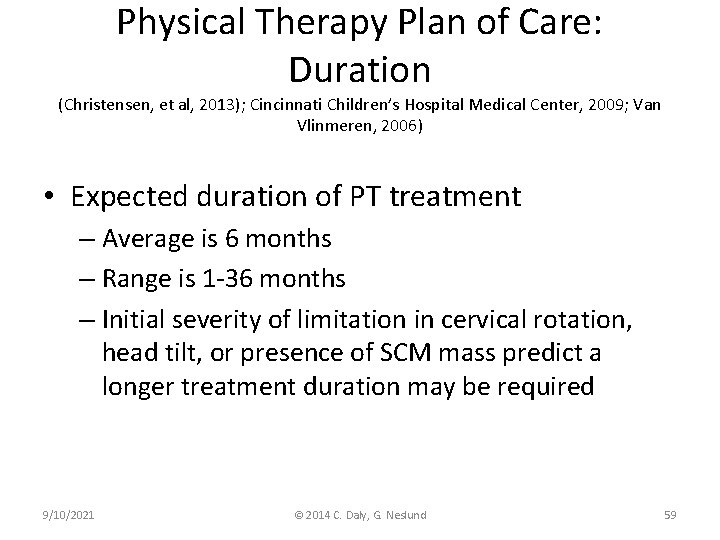
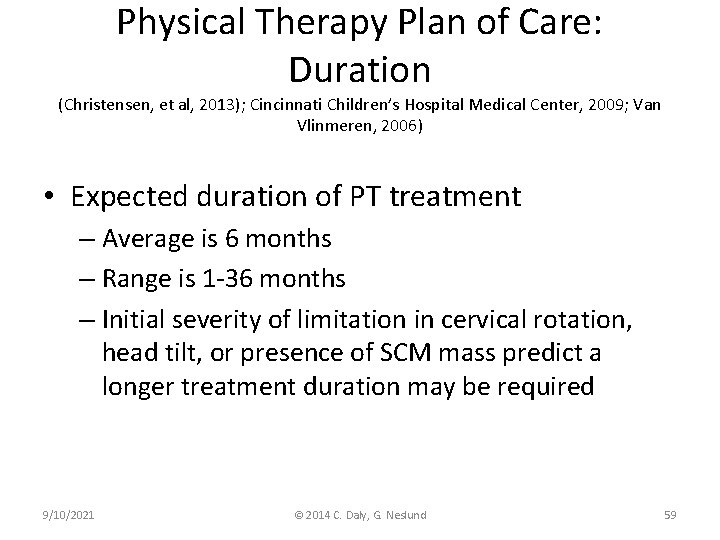
Physical Therapy Plan of Care: Duration (Christensen, et al, 2013); Cincinnati Children’s Hospital Medical Center, 2009; Van Vlinmeren, 2006) • Expected duration of PT treatment – Average is 6 months – Range is 1 -36 months – Initial severity of limitation in cervical rotation, head tilt, or presence of SCM mass predict a longer treatment duration may be required 9/10/2021 © 2014 C. Daly, G. Neslund 59
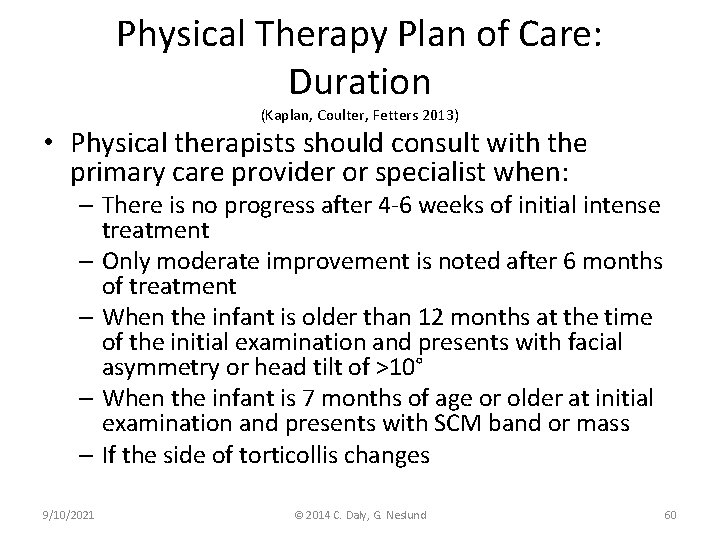
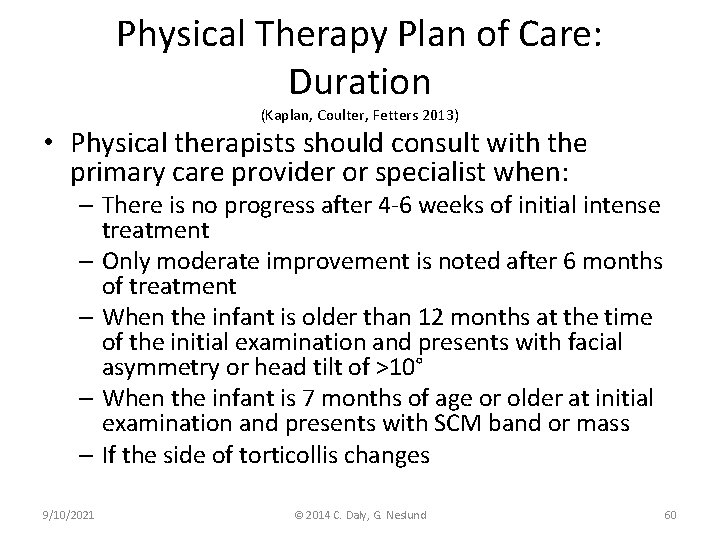
Physical Therapy Plan of Care: Duration (Kaplan, Coulter, Fetters 2013) • Physical therapists should consult with the primary care provider or specialist when: – There is no progress after 4 -6 weeks of initial intense treatment – Only moderate improvement is noted after 6 months of treatment – When the infant is older than 12 months at the time of the initial examination and presents with facial asymmetry or head tilt of >10° – When the infant is 7 months of age or older at initial examination and presents with SCM band or mass – If the side of torticollis changes 9/10/2021 © 2014 C. Daly, G. Neslund 60
Outcomes Achieved Follow-Up Screening (Kaplan, Coulter, Fetters, 2013) • When outcomes are achieved follow-up screening should be completed 3 -12 months post discharge or when the infant initiates walking • The following areas should be screened: – Positional preference – Neck and trunk PROM and AROM – Structural symmetry of the face and skull – Movement symmetry of the neck, trunk, and extremities – Gross motor developmental milestones 9/10/2021 © 2014 C. Daly, G. Neslund 61
Action When Outcomes Not Achieved (Kaplan, Coulter, Fetters, 2013) • Evaluate appropriateness of supplemental interventions – See Kaplan, Couter, Fetters, 2013 p. 383 • Modify frequency and intensity • Refer for specialist consultation 9/10/2021 © 2014 C. Daly, G. Neslund 62
References • American Physical Therapy Association. 2003. Guide to Physical Therapist Practice, Revised 2 nd Ed. Alexandria, VA: APTA. • Bialocerkowski, AE, Vladusic, SL, Ng, CW. 2008. Prevalence, risk factors, and natural progression of positional plagiocephaly: a systematic review. Developmental Medicine and Child Neurology; 50: 577 -586. • Cheng, JYC, et al. 2000. Clinical presentation and outcome of treatment of congenital muscular torticollis in infants – A study of 1, 086 cases. Journal of Pediatric Surgery; 35 (7): 1091 -1096. • Cheng, JCY, et al. 2001. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. Journal of Bone and Joint Surgery; 83(5): 679. • Christensen, C, et al. 2013. Conservative management of congenital muscular torticollis: an evidence-based algorithm and preliminary treatment parameter recommendations. Physical and Occupational Therapy in Pediatrics; Early Online: 1 -14. 9/10/2021 © 2014 C. Daly, G. Neslund 63
References • Cincinnati Children’s Hospital Medical Center. 2009. Evidence-based care guideline for management of congenital muscular torticollis in children age 0 -36 months. Retrieved 4/11/13 from http: //www. cincinnatichildrens. org/service/j/andersoncenter/evidence-based-care/recommendations/default/ • • Cooperman, D. 1997. Differential diagnosis of torticollis in children. Physical & Occupational Therapy in Pediatrics; 17: 1 -11. Coulter-O’Berry, C. & Lima, D. 2007. Tummy Time Tools. Children’s Healthcare of Atlanta. Retrieved 4/15/13 from http: //www. choa. org/childrens-hospitalservices/orthopaedics/programs-services/orthotics-and-prosthetics/tummy-timetools • Do, TT. 2006. Congenital muscular torticollis: Current concepts and review of treatment. Current Opinion in Pediatrics; 18: 26 -29. • De Chalain, T. , Park, S. (2005). Torticollis associated with positional plagiocephaly: a growing epidemic. The Journal of Craniofacial Surgery, 16(3), 411 -418 Darrah, J. et al. (1998). Assessment of gross motor skills of at-risk infants: Predictive validity of the Alberta Infant Motor Scale. Developmental Medicine and Child Neurology, 40, 485 -491. © 2014 C. Daly, G. Neslund 9/10/2021 64 •
References • Freed, SS & Coulter-O’Berry, C. 2004. Identification and treatment of congenital muscular torticollis in infants. Journal of Prosthetics and Orthotics; 16(4 S): 18 • Kaplan SL, Coulter C, Fetters L. 2013. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline. Pediatric Physical Therapy; 25: 348 -394. • Karmel-Ross, K. (2012). Congenital muscular torticollis. In S. K. Campbell, R. J. Palisano, M. Orlin (Eds. ), Physical Therapy for Children, 4 th Ed. , pp 292 -312. St. Louis, MO: Saunders Elsevier. • Klackenberg, EP, et al. 2005. Intra-rater reliability in measuring range of motion in infants with congenital muscular torticollis. Advances in Physiotherapy; 7: 84 -91. • Looman, WS. & Flannery, ABK. 2012. Evidence-based care of the child with deformational plagiocephaly, Part 1: Assessment and diagnosis. Journal of Pediatric Health Care; 26(4): 242 -250. 9/10/2021 © 2014 C. Daly, G. Neslund 65
References • • Luxford, BK. , Hale, L. , Piggot, J. 2009. The physiotherapy management of infants with congenital muscular torticollis: a survey of current practice in New Zealand Journal of Physiotherapy; 37(3): 127 -135. Ohman, AM, Nilssen, S, Bekung, ERE. 2009. Validity and reliability of the muscle function scale, aimed to assess the lateral flexors of the neck in infants. Physiotherapy Theory & Practice; 25(2): 29 -137. Pandya, S. Congenital muscular torticollis case study. In S De. Muth, L Svien & R Dole (eds. ) A Compendium for Teaching Professional Entry-Level Pediatric Content. Alexandria, VA: Section on Pediatrics – American Physical Therapy Association; 2006. Persing, J. et al. (2003). Prevention and management of positional skull deformities in infants. Pediatrics, 112(1), 199 -202. 9/10/2021 © 2014 C. Daly, G. Neslund 66
References • Westcott, SL. & Goulet, C. (2005). Neuromuscular System: Structures, Functions, Diagnoses, and Evaluation. In SK. Effgen, Meeting the physical therapy needs of children. (pp 185 -244). Philadelphia. F. A. Davis Co. • Van Vlimmeren, LA, et al. 2006. Torticollis and plagiocephaly in infancy: Therapeutic strategies. Pediatric Rehabilitation, 9(1), 40 -46. 9/10/2021 © 2014 C. Daly, G. Neslund 67
 Hyperkinesia
Hyperkinesia Plyometrics disadvantages
Plyometrics disadvantages What is the nursing process
What is the nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing diagnosis three parts
Nursing diagnosis three parts Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Muscular dystrophy definition
Muscular dystrophy definition Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Lymphedema differential diagnosis
Lymphedema differential diagnosis Melena stool
Melena stool Differential diagnosis of learning disabilities
Differential diagnosis of learning disabilities How many types of jaundice
How many types of jaundice Hormetonia
Hormetonia Describe
Describe Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Differential diagnosis red eye
Differential diagnosis red eye Vomiting case presentation
Vomiting case presentation Type 1 gastric ulcer
Type 1 gastric ulcer Haemtemesis
Haemtemesis Ulcer definition anatomy
Ulcer definition anatomy Jaundice physical exam
Jaundice physical exam Vitamin c differential diagnosis mnemonic
Vitamin c differential diagnosis mnemonic Polycythemia rubra vera
Polycythemia rubra vera Parkinson differential diagnosis
Parkinson differential diagnosis Differential diagnosis of stroke
Differential diagnosis of stroke Manchester staging of breast cancer
Manchester staging of breast cancer Non pitting edema
Non pitting edema Odd differential diagnosis
Odd differential diagnosis Differential diagnosis for pericarditis
Differential diagnosis for pericarditis Original source
Original source Jaundice
Jaundice Chicken pix los pinos menu
Chicken pix los pinos menu Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Osu lymphedema clinic
Osu lymphedema clinic Corte axial
Corte axial Brainstem stroke syndromes
Brainstem stroke syndromes Define demetia
Define demetia Latent nystagmus
Latent nystagmus Myelopathy vs radiculopathy
Myelopathy vs radiculopathy Normocytic hypochromic anemia differential diagnosis
Normocytic hypochromic anemia differential diagnosis Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Bakers cyst medscape
Bakers cyst medscape Osteochondrosis
Osteochondrosis Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Differential diagnosis for dysphagia
Differential diagnosis for dysphagia Carpal tunnel differential diagnosis
Carpal tunnel differential diagnosis Tocolytic drugs
Tocolytic drugs Differential diagnosis for premature rupture of membranes
Differential diagnosis for premature rupture of membranes Saw tooth appearance in lichen planus
Saw tooth appearance in lichen planus Epigastric pain differential diagnosis
Epigastric pain differential diagnosis Spotting differential diagnosis
Spotting differential diagnosis Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Leukocoria differential diagnosis
Leukocoria differential diagnosis Leukemia death rate
Leukemia death rate Polycythemia differential diagnosis
Polycythemia differential diagnosis Differentials for hydrocephalus
Differentials for hydrocephalus Dka in pregnancy
Dka in pregnancy Normal endometrial thickness postmenopausal
Normal endometrial thickness postmenopausal J
J Polymorphs pour out to sink to bottom of anterior chamber
Polymorphs pour out to sink to bottom of anterior chamber Differential diagnosis of vitiligo
Differential diagnosis of vitiligo Molar pregnancy differential diagnosis
Molar pregnancy differential diagnosis Differential diagnosis for leukoplakia
Differential diagnosis for leukoplakia Differential diagnosis of dysphagia
Differential diagnosis of dysphagia Profalam
Profalam Basamaklandırılmış öğretim yöntemi
Basamaklandırılmış öğretim yöntemi Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Normal bowel sound
Normal bowel sound