Chapter 32 Gastrointestinal Secretions 1 Exocrine of the


















- Slides: 79
Chapter 32 Gastrointestinal Secretions 1
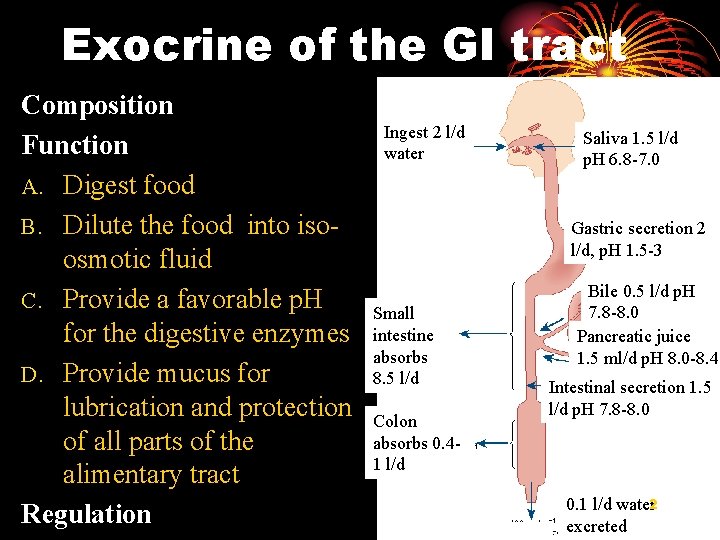
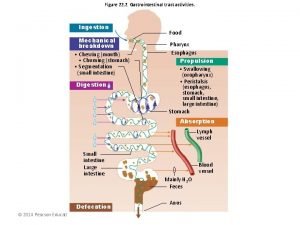
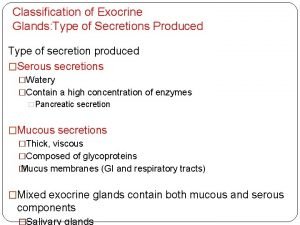
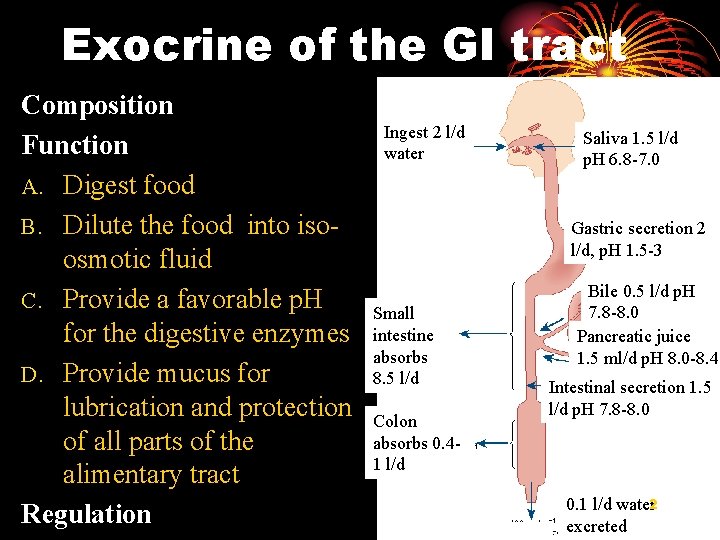
Exocrine of the GI tract Composition Function A. Digest food B. Dilute the food into isoosmotic fluid C. Provide a favorable p. H for the digestive enzymes D. Provide mucus for lubrication and protection of all parts of the alimentary tract Regulation Ingest 2 l/d water Saliva 1. 5 l/d p. H 6. 8 -7. 0 Gastric secretion 2 l/d, p. H 1. 5 -3 Small intestine absorbs 8. 5 l/d Colon absorbs 0. 41 l/d Bile 0. 5 l/d p. H 7. 8 -8. 0 Pancreatic juice 1. 5 ml/d p. H 8. 0 -8. 4 Intestinal secretion 1. 5 l/d p. H 7. 8 -8. 0 0. 1 l/d water 2 excreted
I. Salivary secretion 3
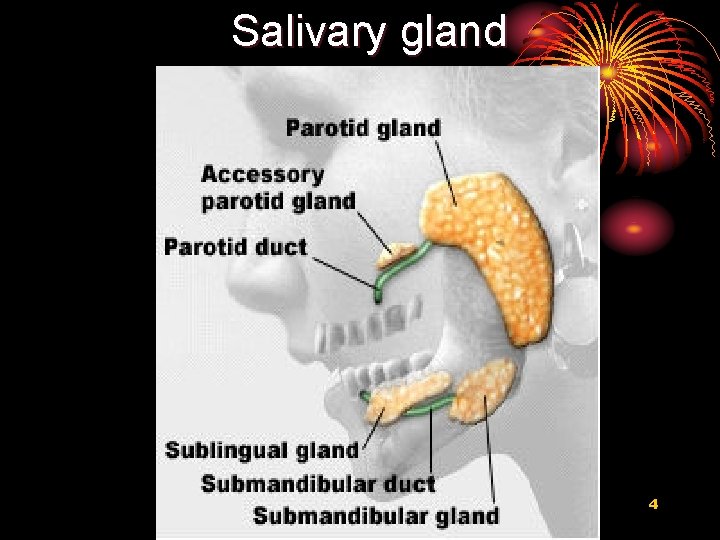
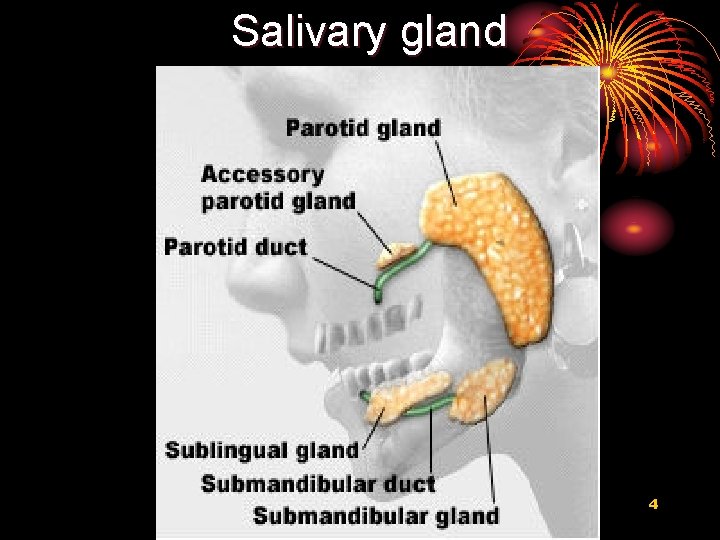
Salivary gland 4

Secretion Saliva: water, ions, mucus, enzymes Acinar Cells: 腺 泡细胞 5

Functions of secretion 1. Moisten food 2. Begin chemical digestion (a amylase, 淀 粉酶) 3. Adjust appetite 4. Bacteriostatic action (抑菌作用) (bacteriolysin, 溶菌素) 6
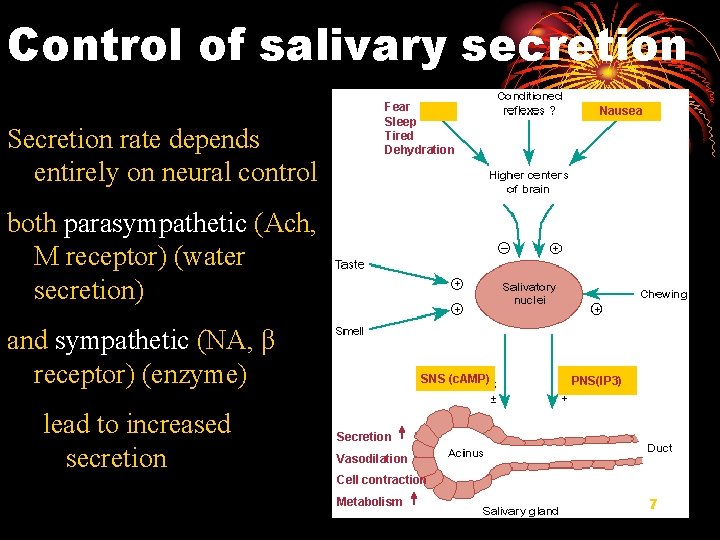
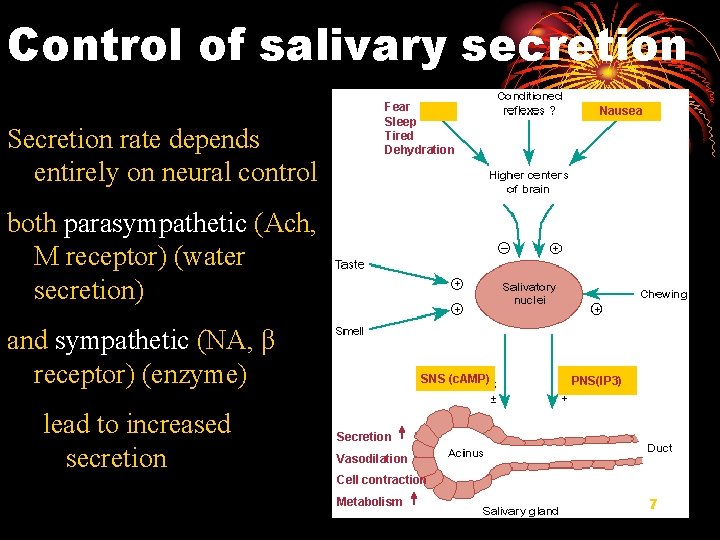
Control of salivary secretion Secretion rate depends entirely on neural control Fear Sleep Tired Dehydration Nausea both parasympathetic (Ach, M receptor) (water secretion) and sympathetic (NA, β receptor) (enzyme) lead to increased secretion SNS (c. AMP) PNS(IP 3) Secretion Vasodilation Cell contraction Metabolism 7

II. Gastric secretion 8
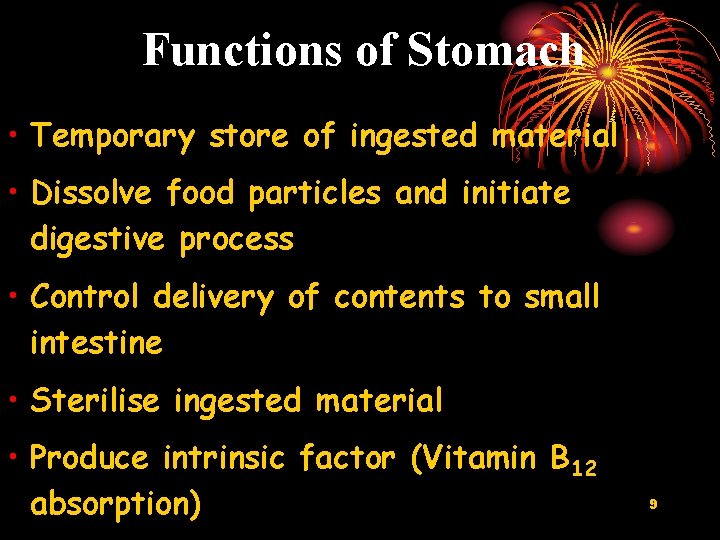
Functions of Stomach • Temporary store of ingested material • Dissolve food particles and initiate digestive process • Control delivery of contents to small intestine • Sterilise ingested material • Produce intrinsic factor (Vitamin B 12 absorption) 9
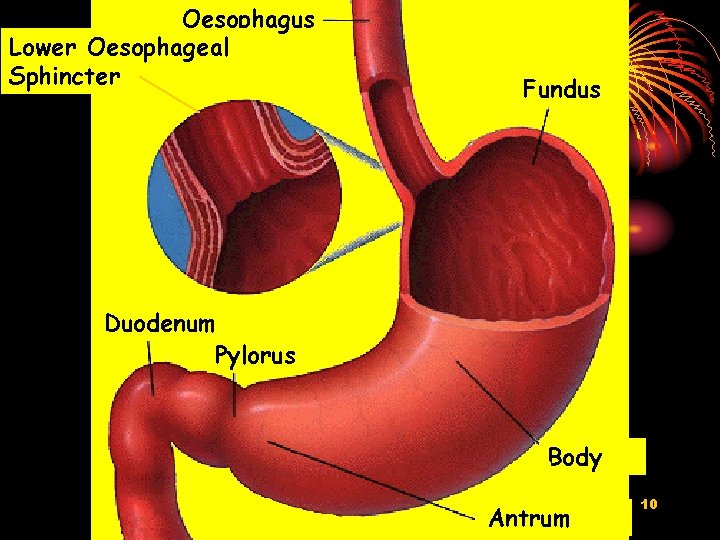
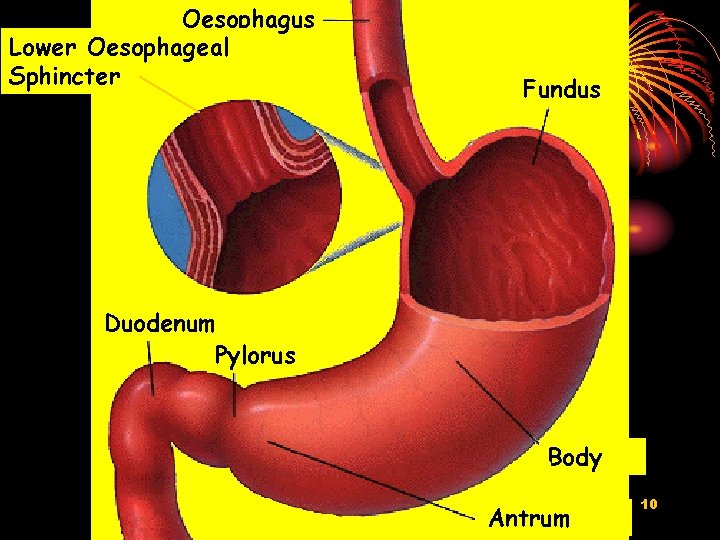
Oesophagus Lower Oesophageal Sphincter Fundus Duodenum Pylorus Body Antrum 10
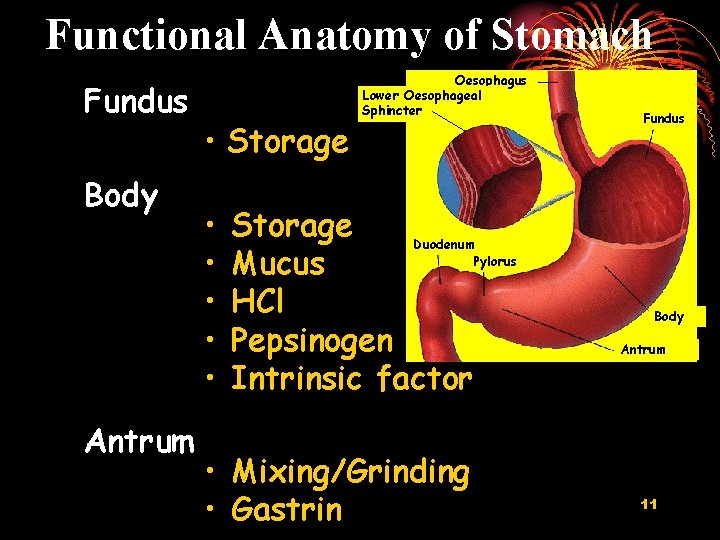
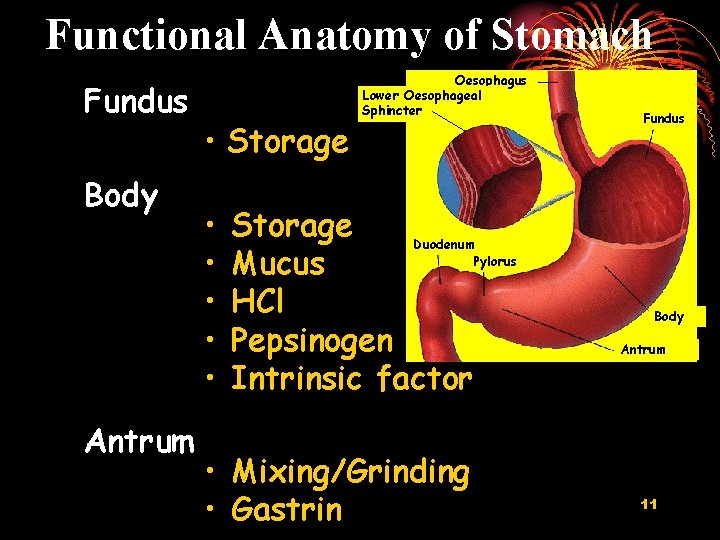
Functional Anatomy of Stomach Fundus Body Antrum • Storage • • • Oesophagus Lower Oesophageal Sphincter Storage Duodenum Pylorus Mucus HCl Pepsinogen Intrinsic factor • Mixing/Grinding • Gastrin Fundus Body Antrum 11

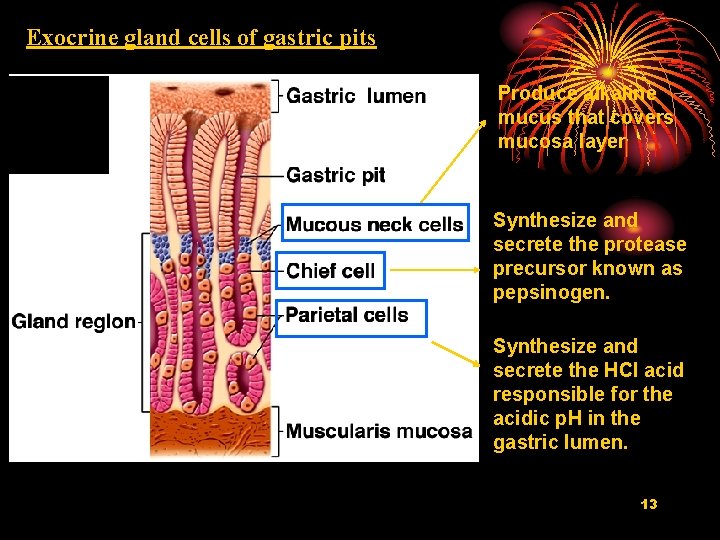
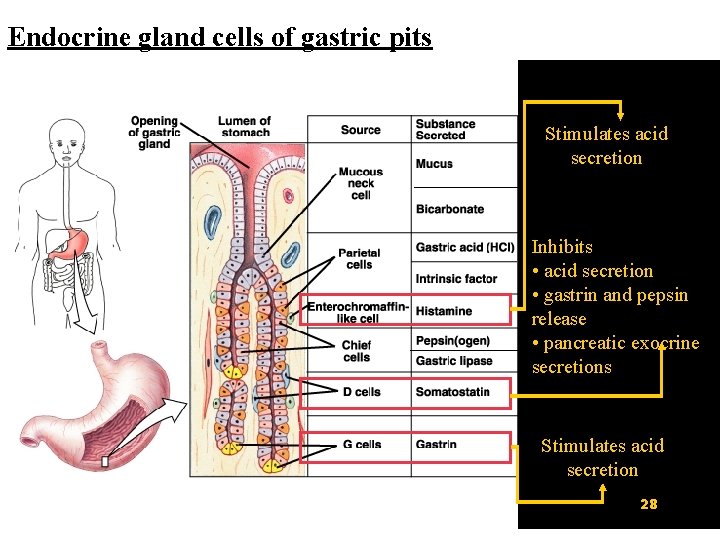
II. 1 Gastric gland cells 1. Oxyntic gland (泌酸 腺) Parietal cell Chief cell Mucous neck cell 2. Pyloric gland Mucus cell 3. Cardiac gland Mucus cell 4. Endocrine cells (G, D, ECL) ECL: enterochromaffin-like cell 12
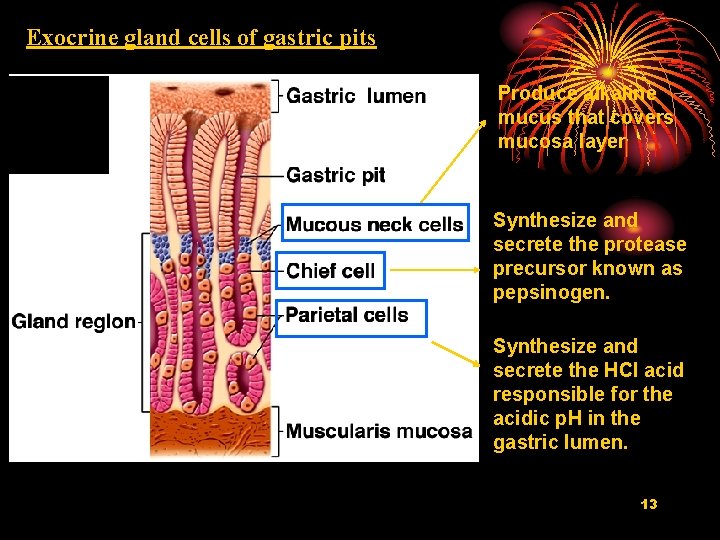
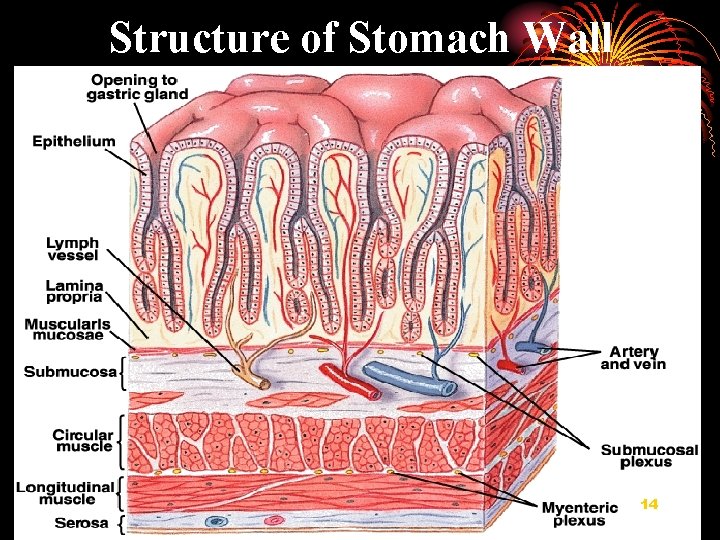
Exocrine gland cells of gastric pits Produce alkaline mucus that covers mucosa layer Synthesize and secrete the protease precursor known as pepsinogen. Synthesize and secrete the HCl acid responsible for the acidic p. H in the gastric lumen. 13
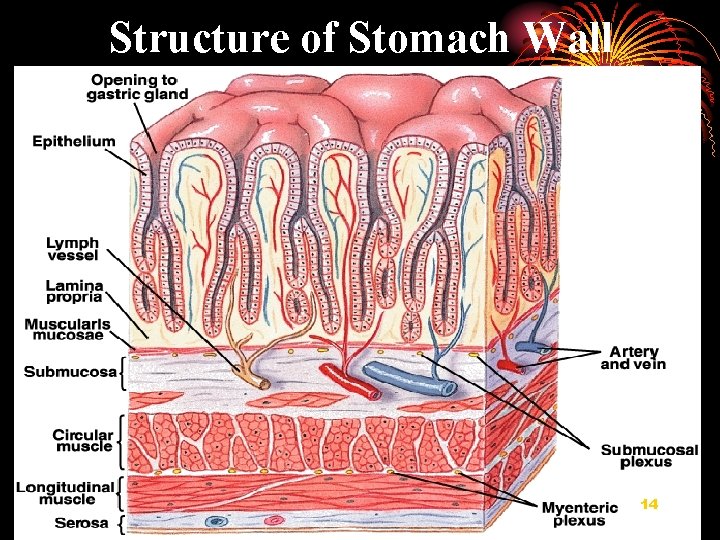
Structure of Stomach Wall 14

II. 2 Composition and function of gastric secretions 1. HCl Ø converts pepsinogen to pepsin for chemical digestion Ø provides optimal p. H environment for pepsin Ø destroys some bacteria Ø stimulates the small intestinal mucosa to release secretinand CCK Ø promotes the absorption of Ca and Fe in small 15 intestine
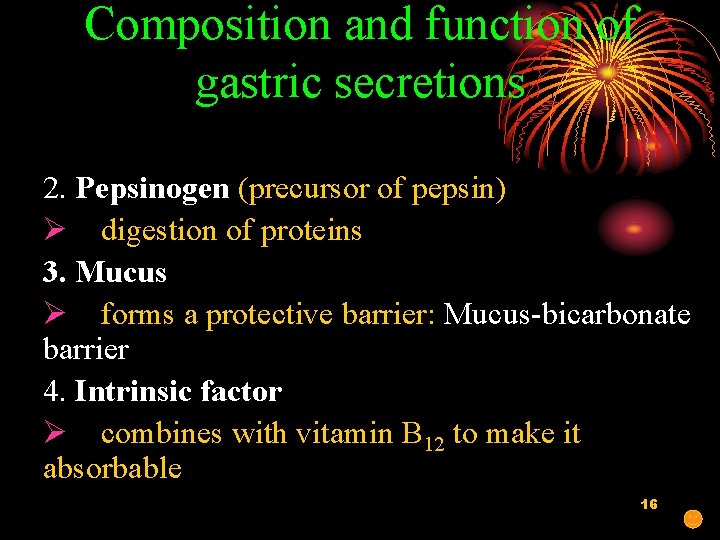
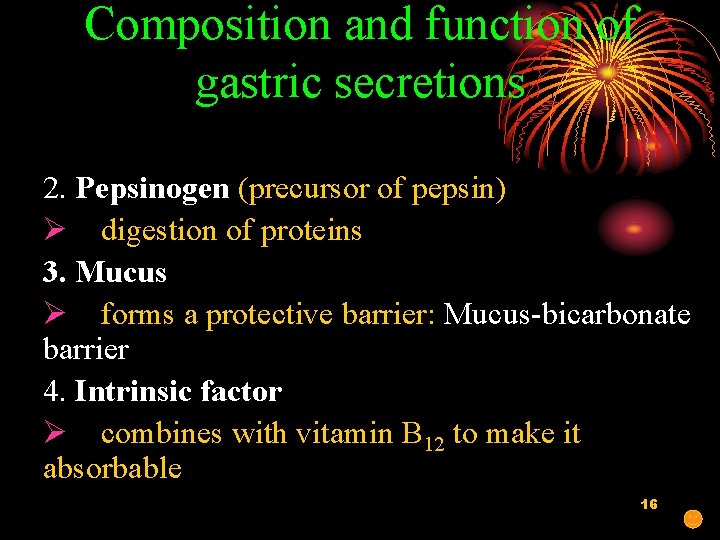
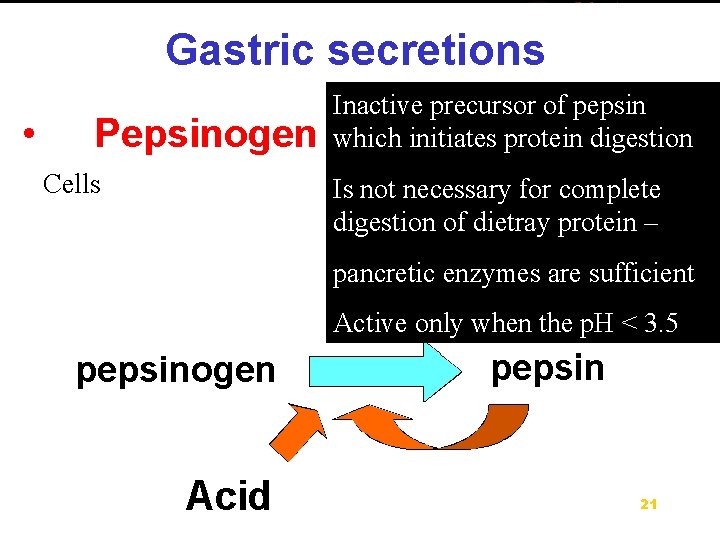
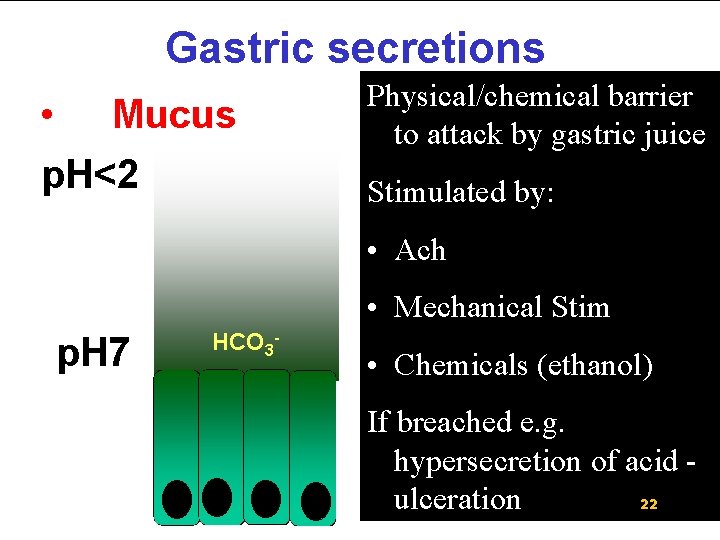
Composition and function of gastric secretions 2. Pepsinogen (precursor of pepsin) Ø digestion of proteins 3. Mucus Ø forms a protective barrier: Mucus-bicarbonate barrier 4. Intrinsic factor Ø combines with vitamin B 12 to make it absorbable 16
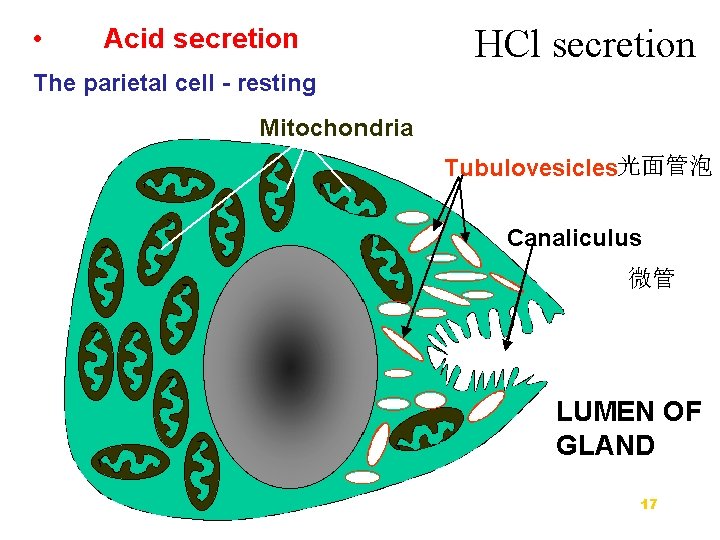
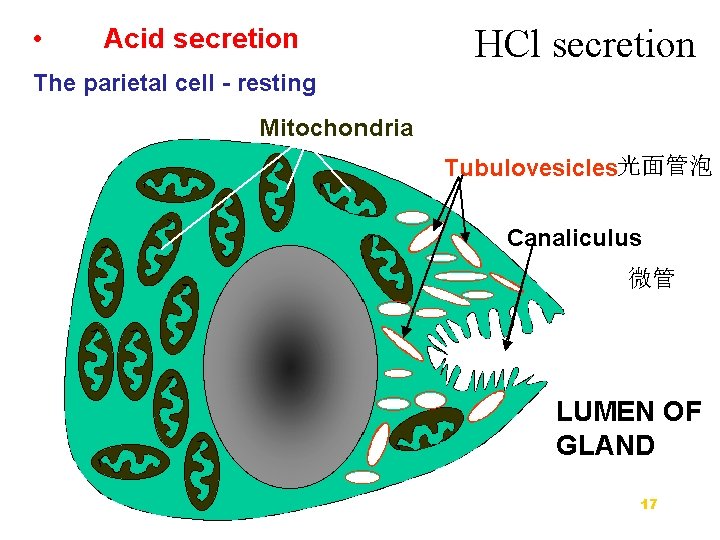
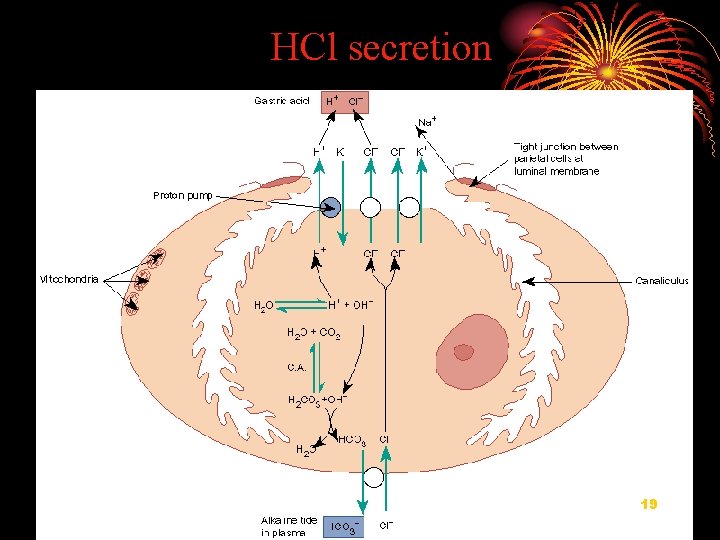
HCl secretion 光面管泡 微管 17
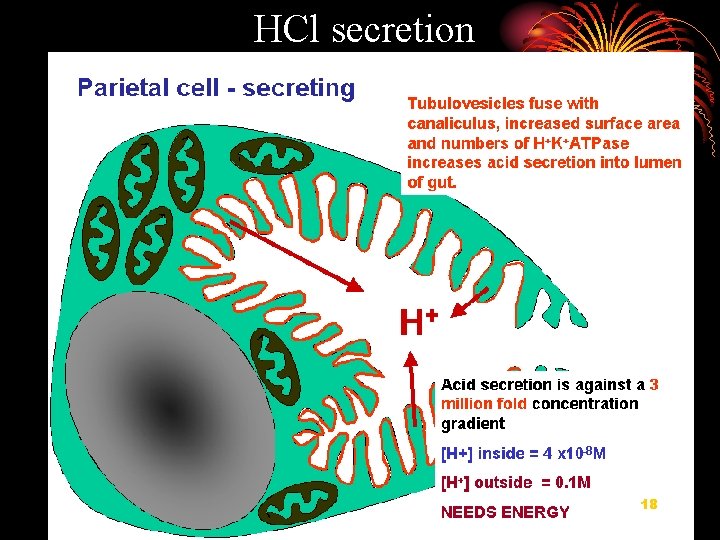
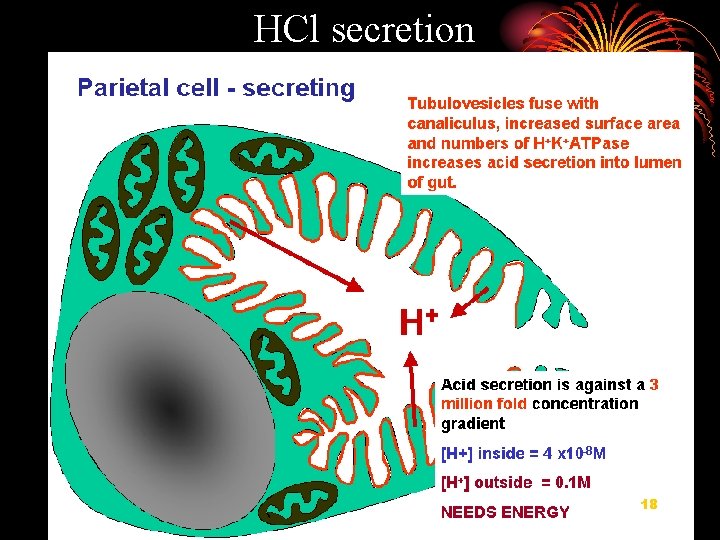
HCl secretion 18
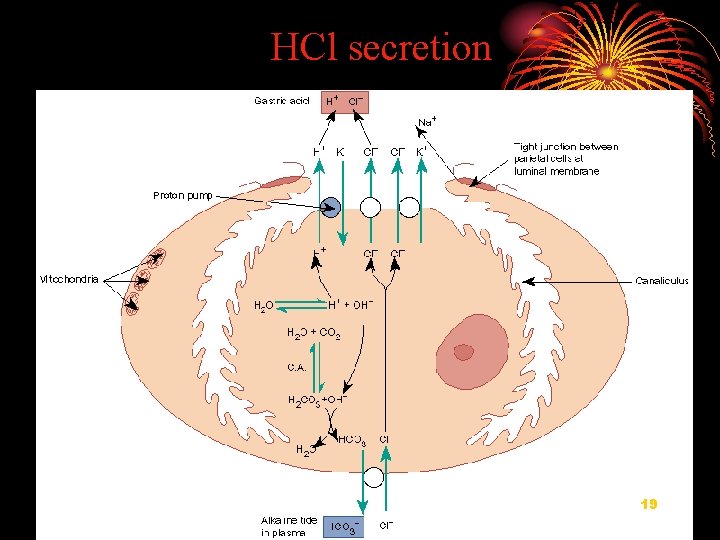
HCl secretion 19
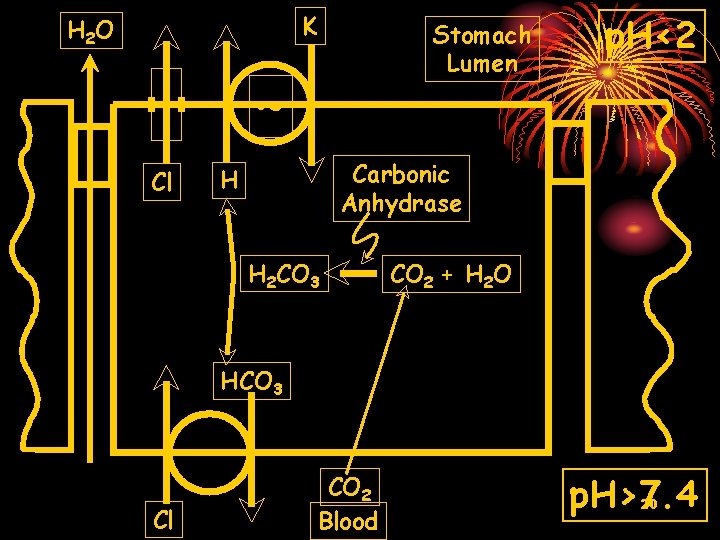
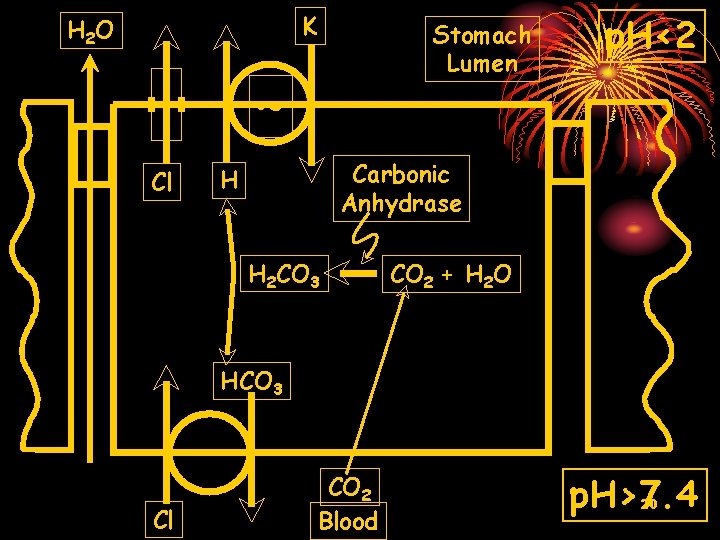
K H 2 O Stomach Lumen ~ Cl p. H<2 Carbonic Anhydrase H H 2 CO 3 CO 2 + H 2 O HCO 3 Cl CO 2 Blood p. H>7. 4 20
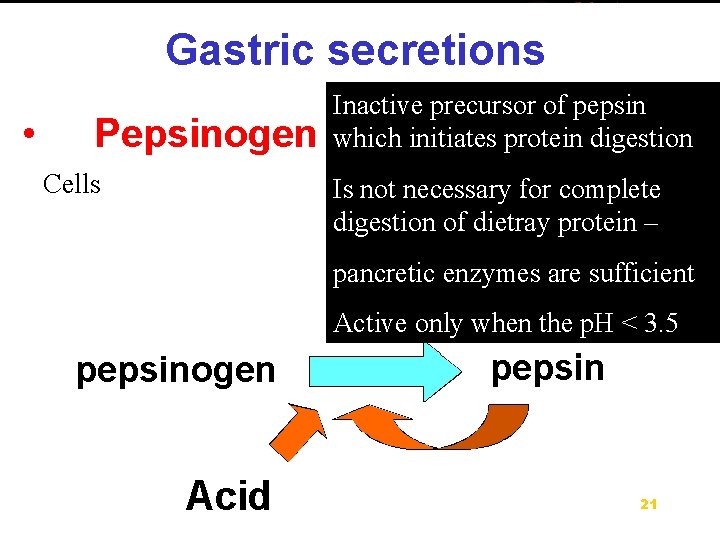
Inactive precursor of pepsin which initiates protein digestion Cells Is not necessary for complete digestion of dietray protein – pancretic enzymes are sufficient Active only when the p. H < 3. 5 21
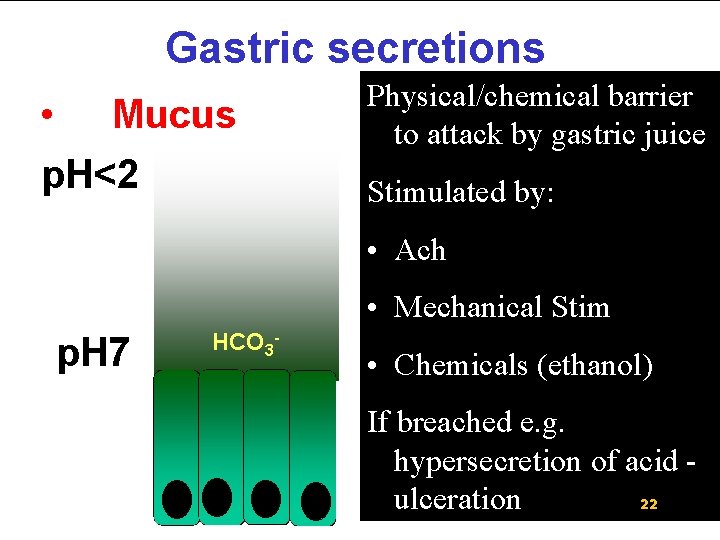
Physical/chemical barrier to attack by gastric juice Stimulated by: • Ach • Mechanical Stim • Chemicals (ethanol) If breached e. g. hypersecretion of acid 22 ulceration
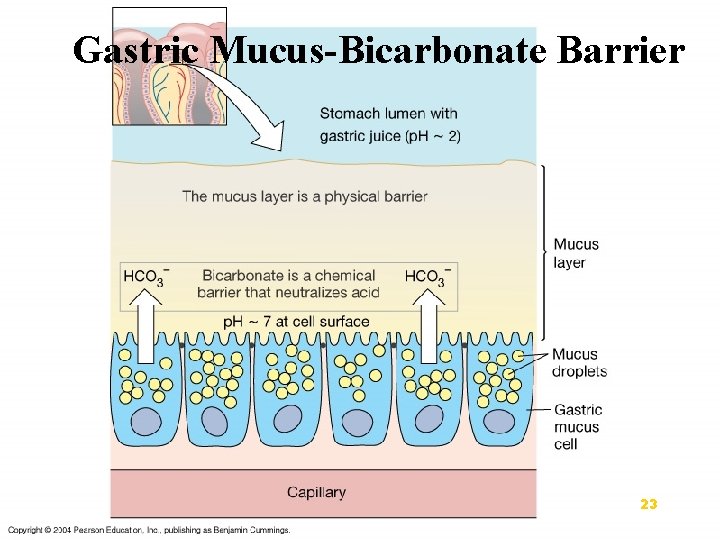
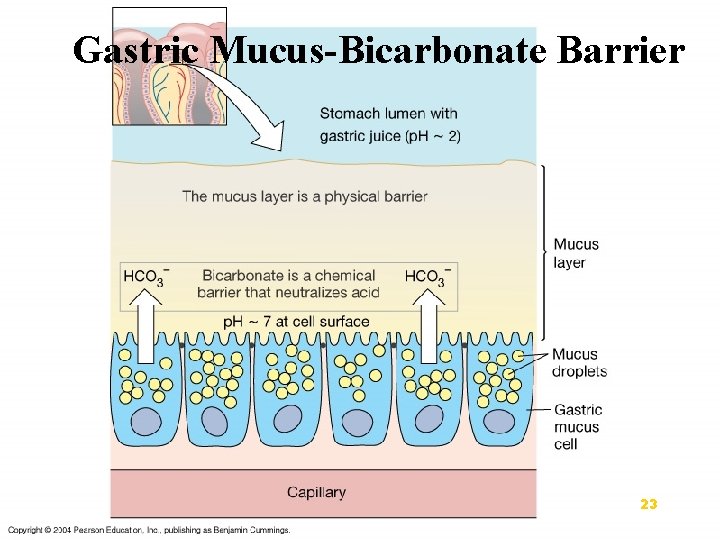
Gastric Mucus-Bicarbonate Barrier 23
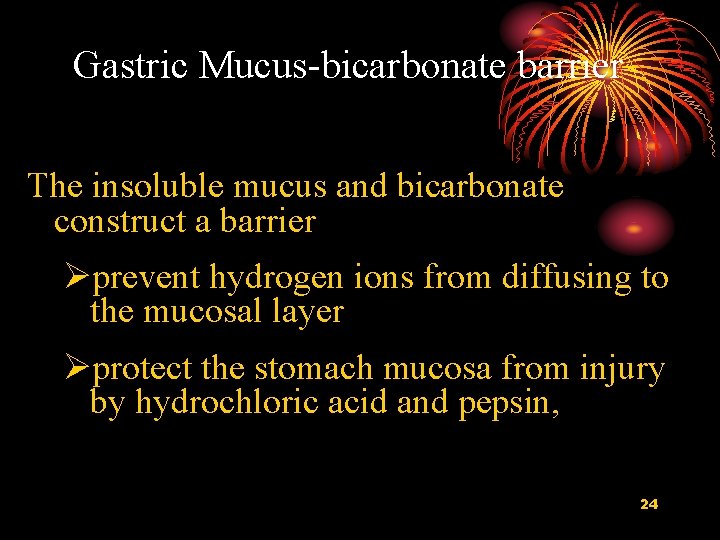
Gastric Mucus-bicarbonate barrier The insoluble mucus and bicarbonate construct a barrier Øprevent hydrogen ions from diffusing to the mucosal layer Øprotect the stomach mucosa from injury by hydrochloric acid and pepsin, 24
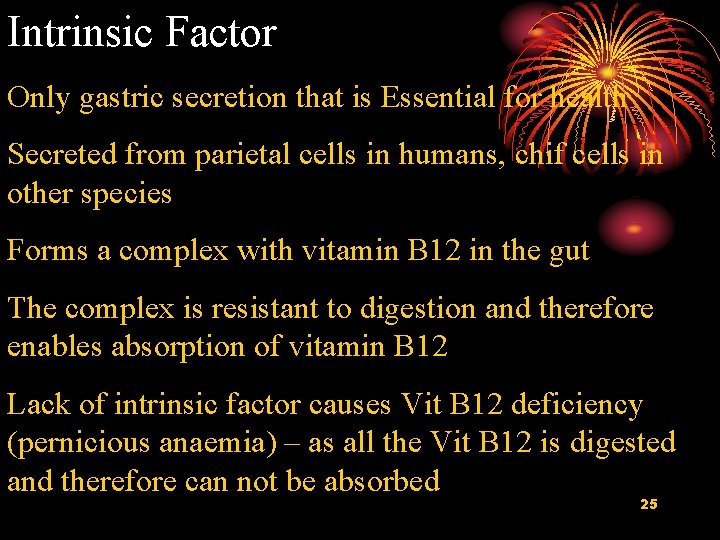
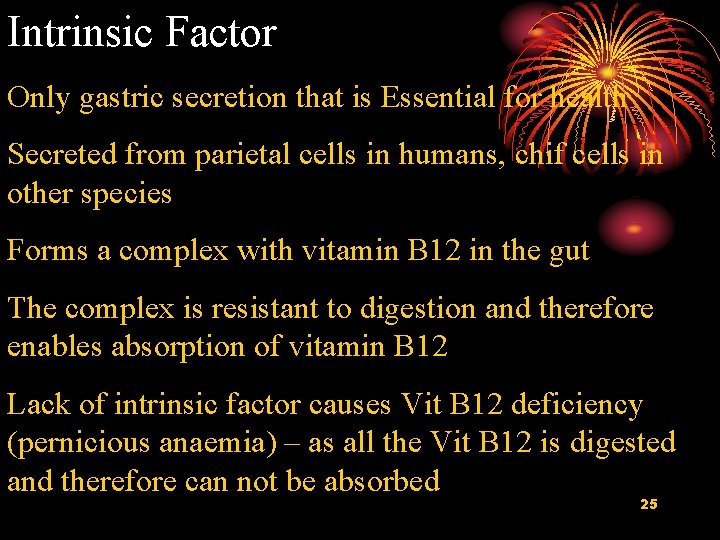
Intrinsic Factor Only gastric secretion that is Essential for health Secreted from parietal cells in humans, chif cells in other species Forms a complex with vitamin B 12 in the gut The complex is resistant to digestion and therefore enables absorption of vitamin B 12 Lack of intrinsic factor causes Vit B 12 deficiency (pernicious anaemia) – as all the Vit B 12 is digested and therefore can not be absorbed 25

II. 3 Regulation of Secretion 26
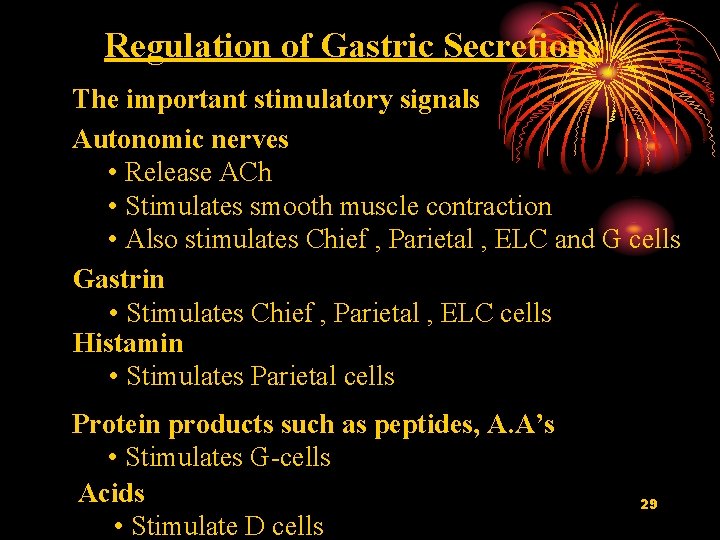
Control of Gastric Acid Secretion Gastric acid secretion is controlled by three mechanisms: • Neurocrine (vagus/local reflexes) • Endocrine (gastrin) • Paracrine (histamine) 27
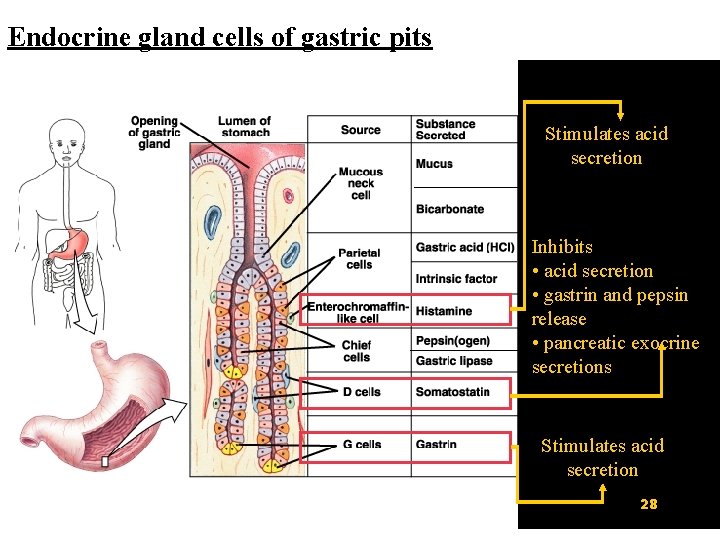
Endocrine gland cells of gastric pits Stimulates acid secretion Inhibits • acid secretion • gastrin and pepsin release • pancreatic exocrine secretions Stimulates acid secretion 28
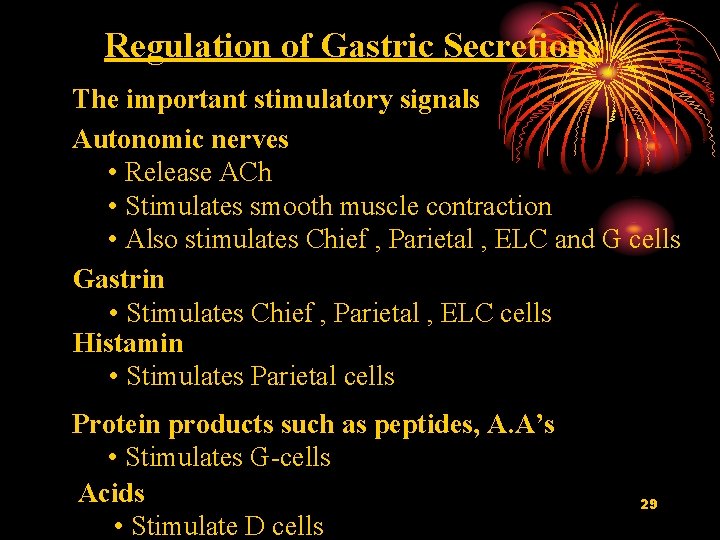
Regulation of Gastric Secretions The important stimulatory signals Autonomic nerves • Release ACh • Stimulates smooth muscle contraction • Also stimulates Chief , Parietal , ELC and G cells Gastrin • Stimulates Chief , Parietal , ELC cells Histamin • Stimulates Parietal cells Protein products such as peptides, A. A’s • Stimulates G-cells Acids • Stimulate D cells 29
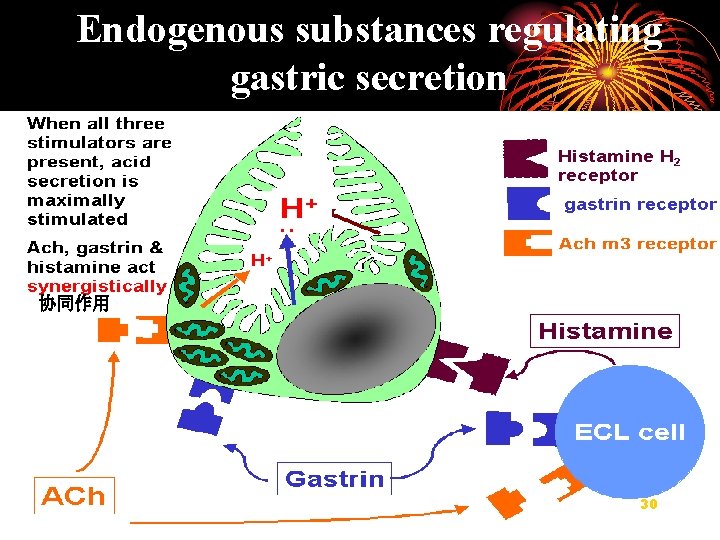
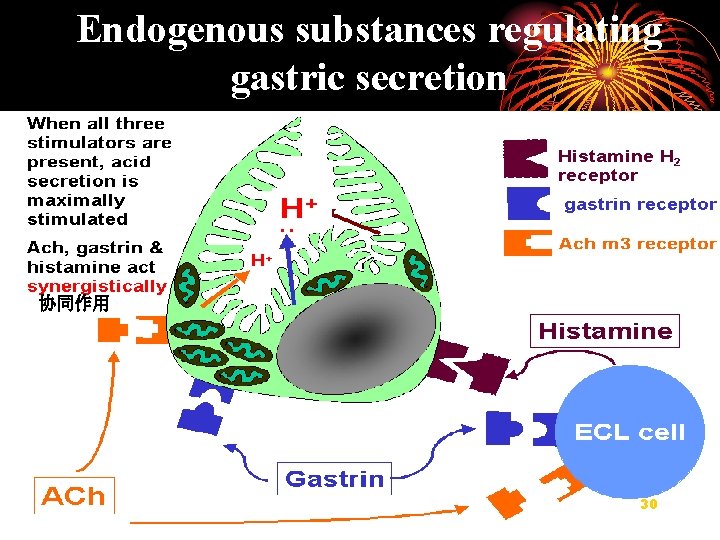
Endogenous substances regulating gastric secretion 协同作用 30
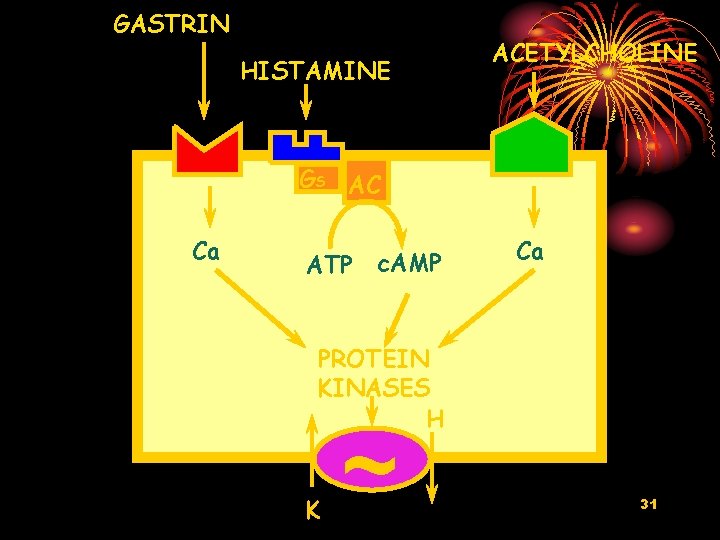
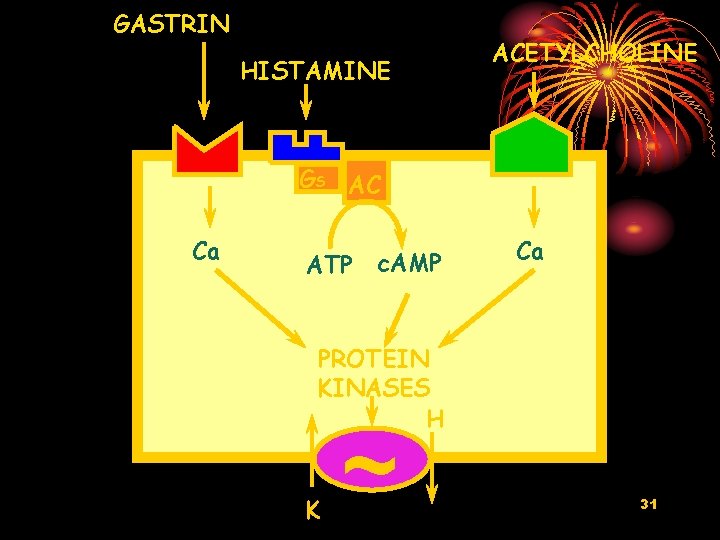
GASTRIN HISTAMINE ACETYLCHOLINE GS AC Ca ATP c. AMP Ca PROTEIN KINASES H K ~ 31

Gastric secretion during digesting food 32
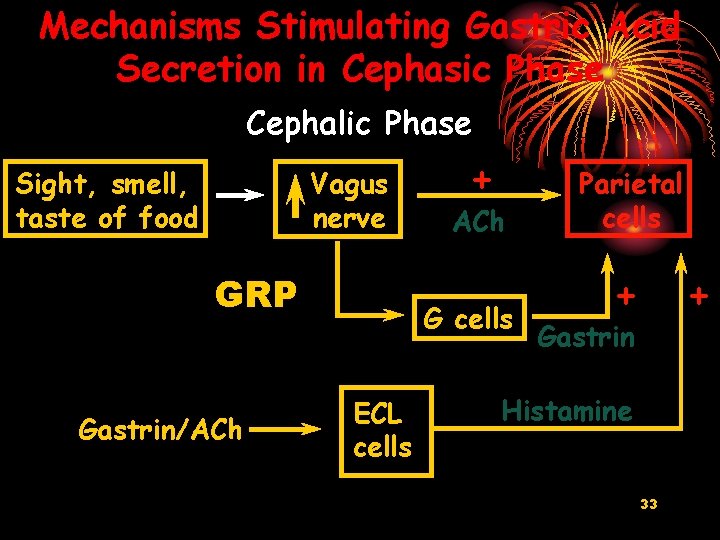
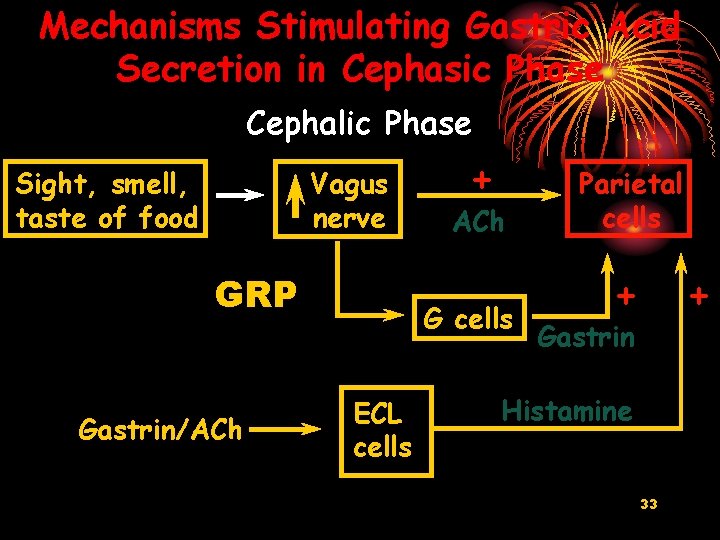
Mechanisms Stimulating Gastric Acid Secretion in Cephasic Phase Cephalic Phase Sight, smell, taste of food Vagus nerve GRP Gastrin/ACh + ACh G cells ECL cells Parietal cells + + Gastrin Histamine 33
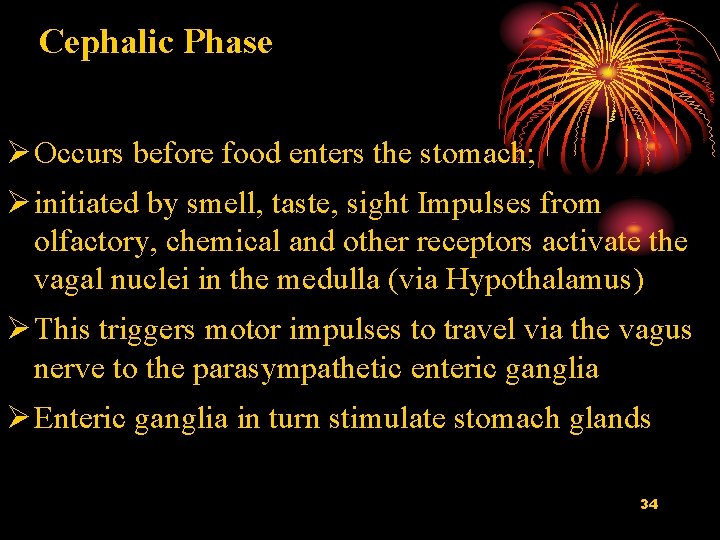
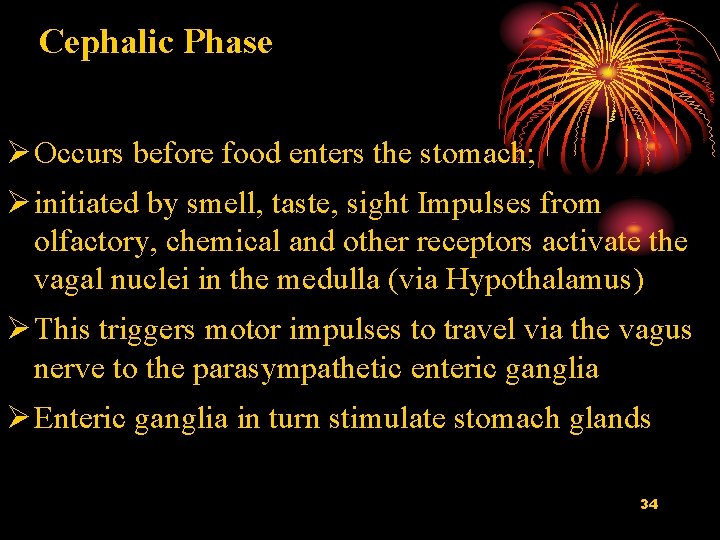
Cephalic Phase 1. Cephalic phase Ø Occurs before food enters the stomach; Ø initiated by smell, taste, sight Impulses from olfactory, chemical and other receptors activate the vagal nuclei in the medulla (via Hypothalamus) Ø This triggers motor impulses to travel via the vagus nerve to the parasympathetic enteric ganglia Ø Enteric ganglia in turn stimulate stomach glands 34
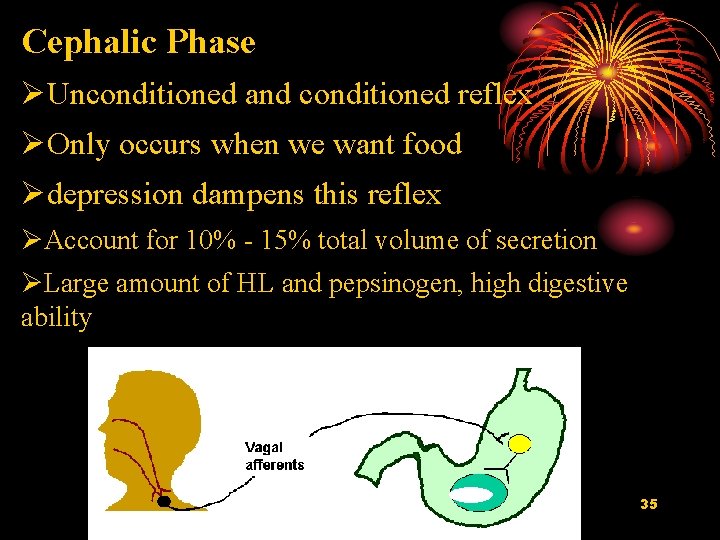
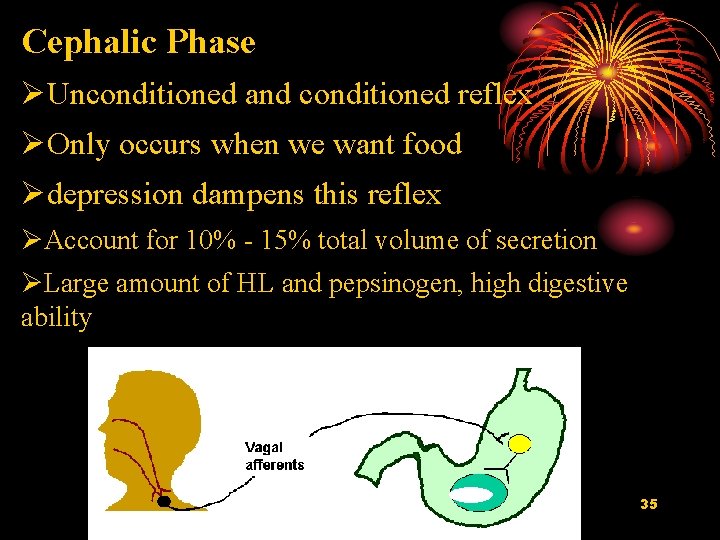
Cephalic Phase ØUnconditioned and conditioned reflex ØOnly occurs when we want food Ødepression dampens this reflex ØAccount for 10% - 15% total volume of secretion ØLarge amount of HL and pepsinogen, high digestive ability 35
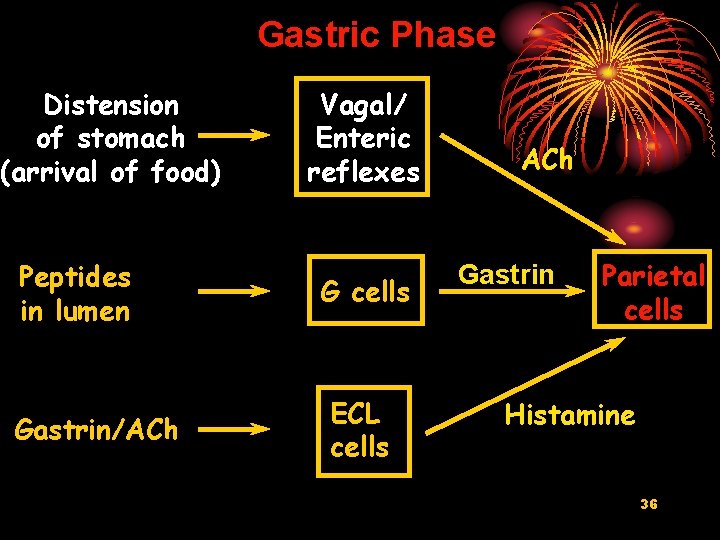
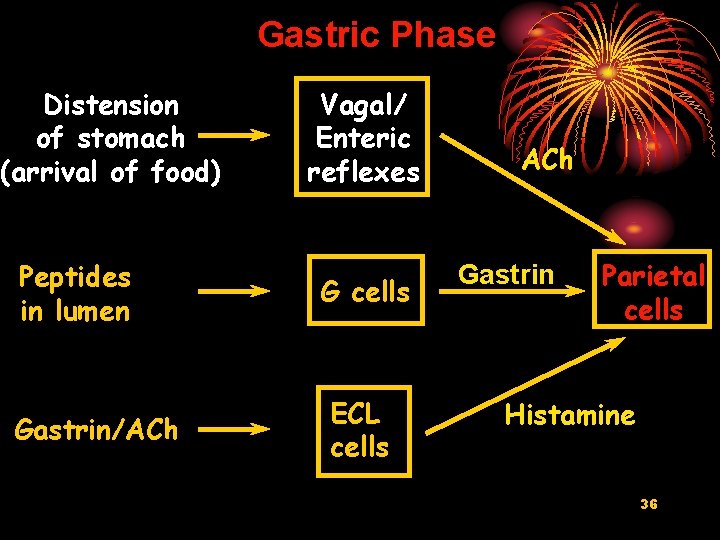
Gastric Phase Distension of stomach (arrival of food) Peptides in lumen Gastrin/ACh Vagal/ Enteric reflexes G cells ECL cells ACh Gastrin Parietal cells Histamine 36
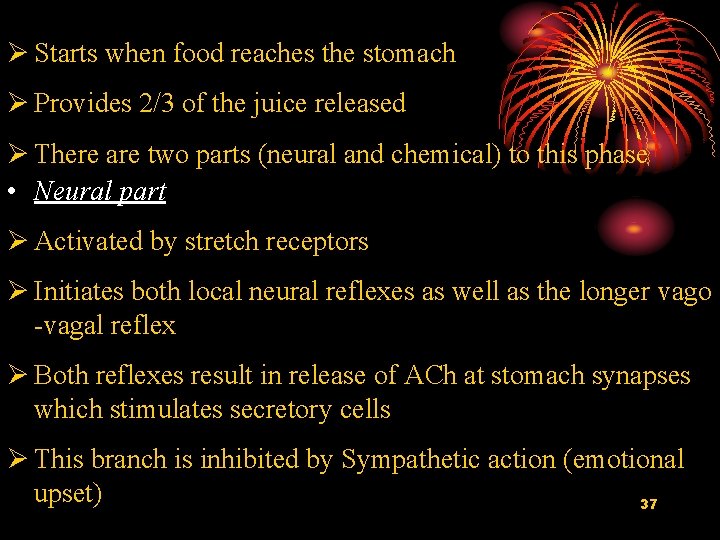
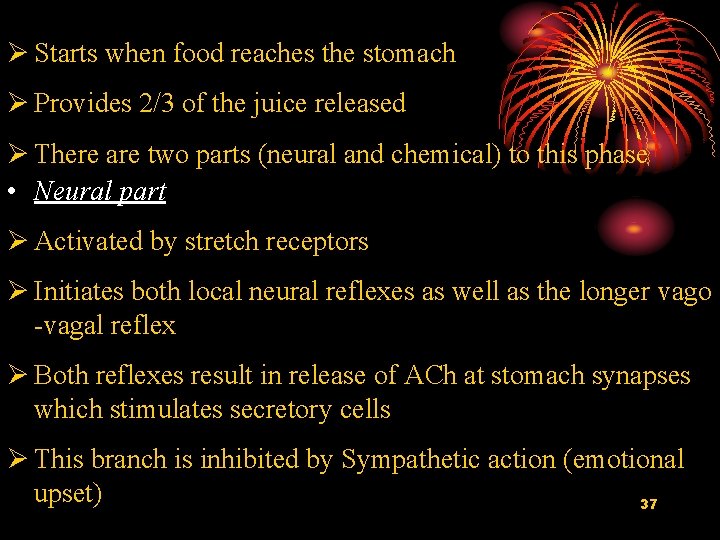
Ø Starts when food reaches the stomach Ø Provides 2/3 of the juice released Ø There are two parts (neural and chemical) to this phase • Neural part Ø Activated by stretch receptors Ø Initiates both local neural reflexes as well as the longer vago -vagal reflex Ø Both reflexes result in release of ACh at stomach synapses which stimulates secretory cells Ø This branch is inhibited by Sympathetic action (emotional upset) 37

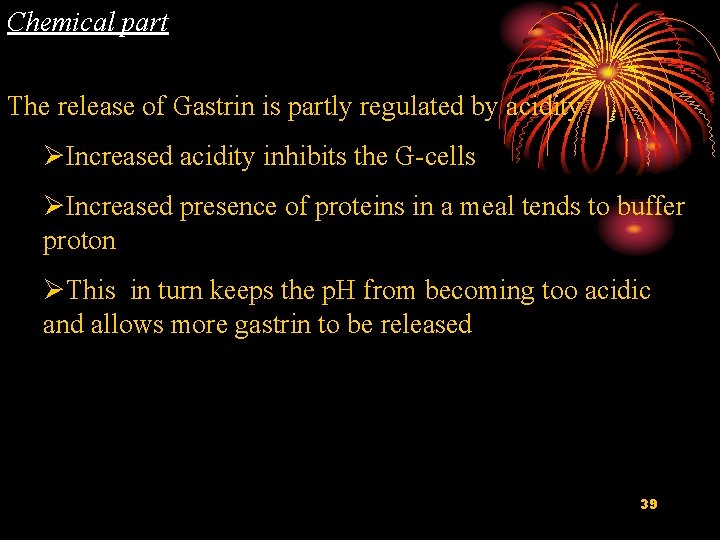
Chemical part ØAn increase in p. H (thus, ‘less’ acidity), presence of peptides, caffeine activate the G-cells ØThis results in Gastrin being released ØGastrin acts on Parietal cells that start secreting HCl ØGastrin also stimulates Histamine release, which in turn stimulates Parietal cells ØThe increase in HCl promotes pepsin production and protein degradation 38
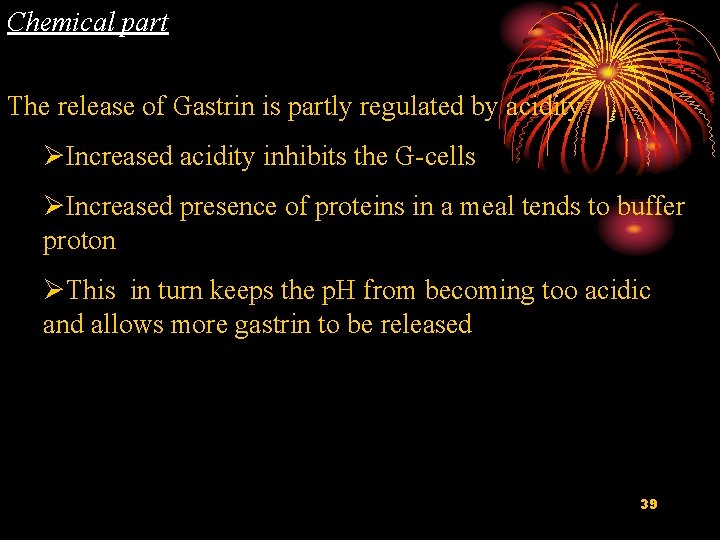
Chemical part The release of Gastrin is partly regulated by acidity ØIncreased acidity inhibits the G-cells ØIncreased presence of proteins in a meal tends to buffer proton ØThis in turn keeps the p. H from becoming too acidic and allows more gastrin to be released 39
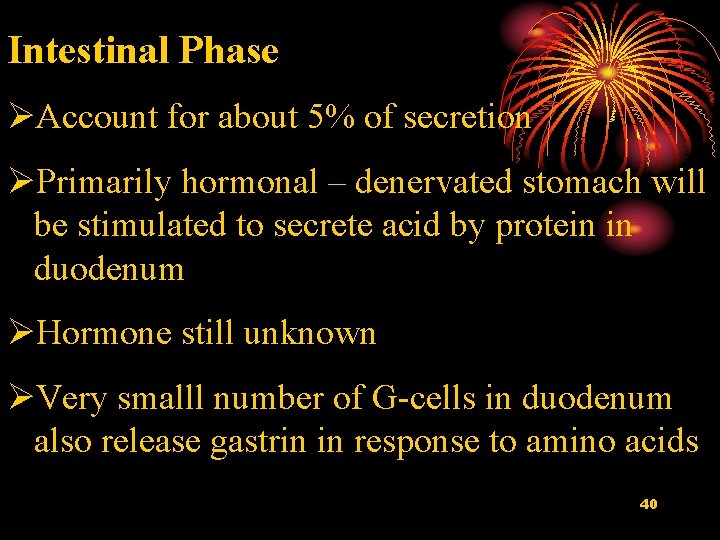
Intestinal Phase ØAccount for about 5% of secretion ØPrimarily hormonal – denervated stomach will be stimulated to secrete acid by protein in duodenum ØHormone still unknown ØVery smalll number of G-cells in duodenum also release gastrin in response to amino acids 40
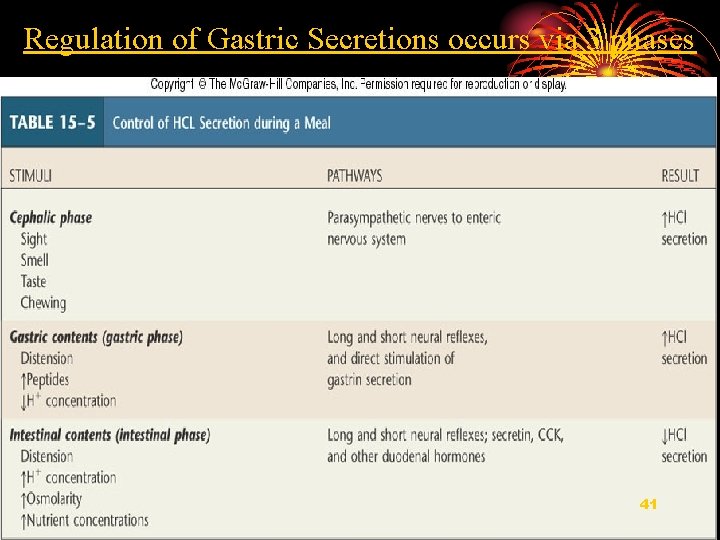
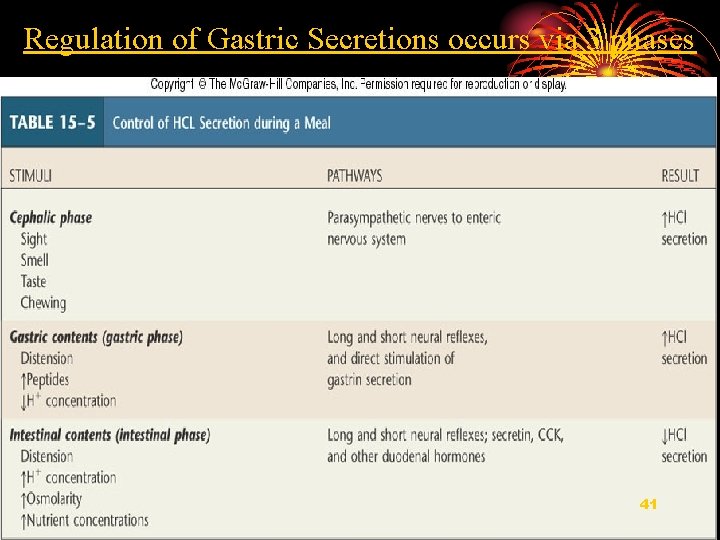
Regulation of Gastric Secretions occurs via 3 phases 41
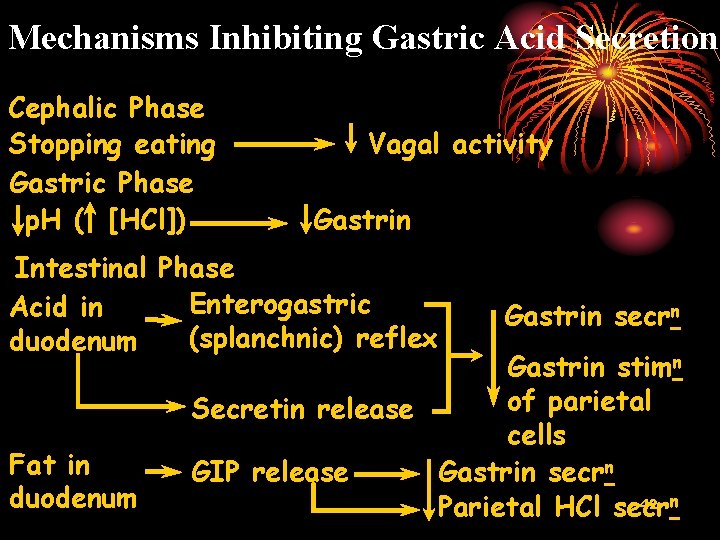
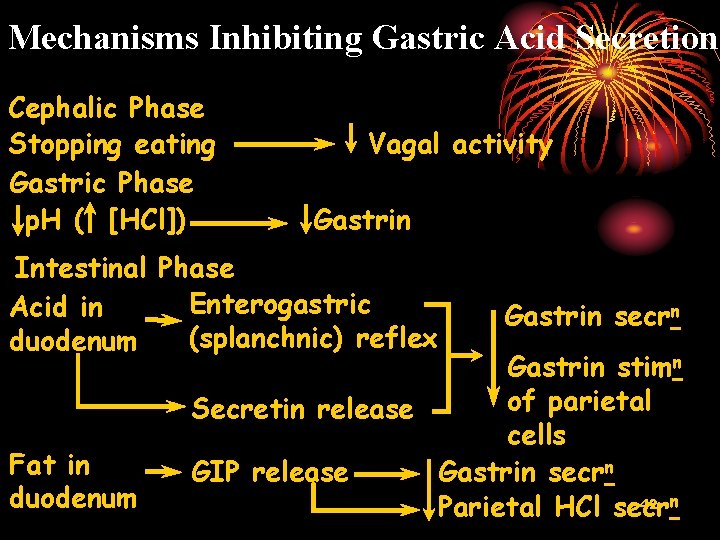
Mechanisms Inhibiting Gastric Acid Secretion Cephalic Phase Stopping eating Gastric Phase p. H ( [HCl]) Vagal activity Gastrin Intestinal Phase Enterogastric Acid in (splanchnic) reflex duodenum Fat in duodenum Gastrin secrn Gastrin stimn of parietal Secretin release cells GIP release Gastrin secrn 42 n Parietal HCl secr
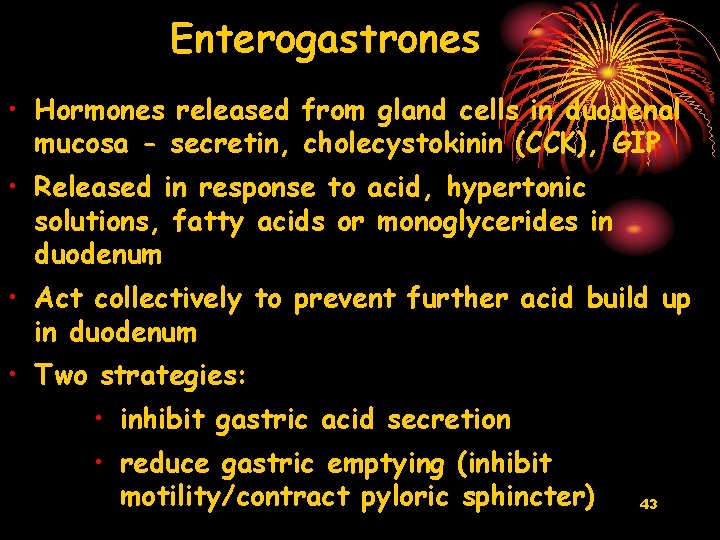
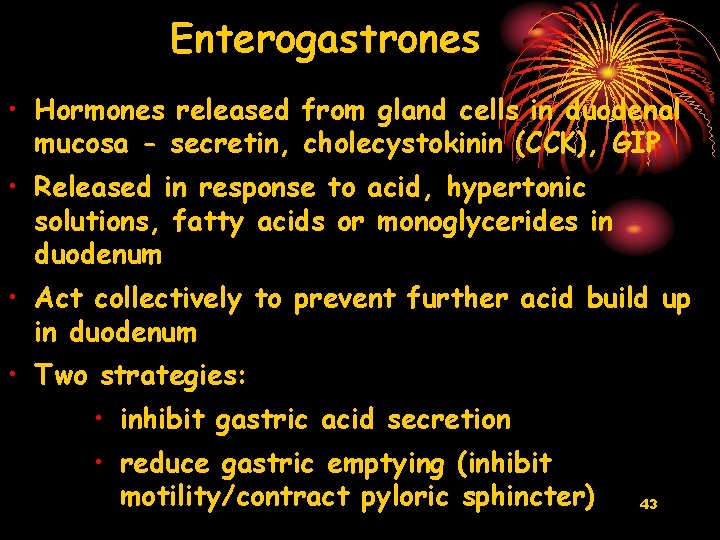
Enterogastrones • Hormones released from gland cells in duodenal mucosa - secretin, cholecystokinin (CCK), GIP • Released in response to acid, hypertonic solutions, fatty acids or monoglycerides in duodenum • Act collectively to prevent further acid build up in duodenum • Two strategies: • inhibit gastric acid secretion • reduce gastric emptying (inhibit motility/contract pyloric sphincter) 43

Regulation of gastric secretion Hyperosmotic solution Mechanical stimulation Entero-oxyntin Fatty acids HCl Secretion of Ach or other transmitters by nerve endings D Gastric gland 44

III. Secretion of the pancreas 45
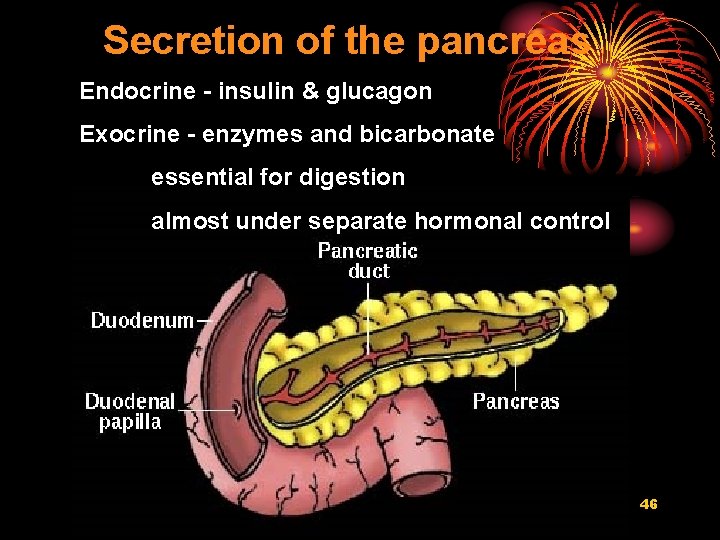
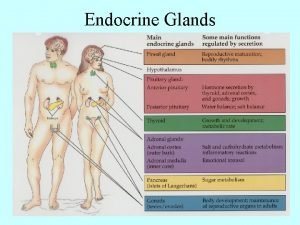
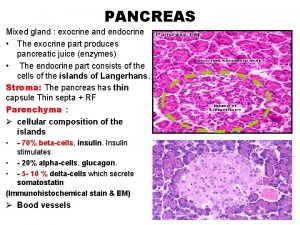
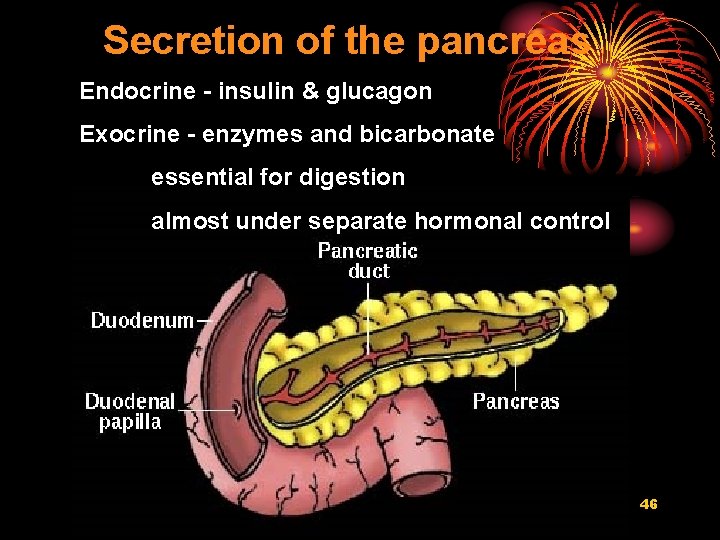
Secretion of the pancreas Endocrine - insulin & glucagon Exocrine - enzymes and bicarbonate essential for digestion almost under separate hormonal control 46

Gall bladder Sphincter of Oddi 47
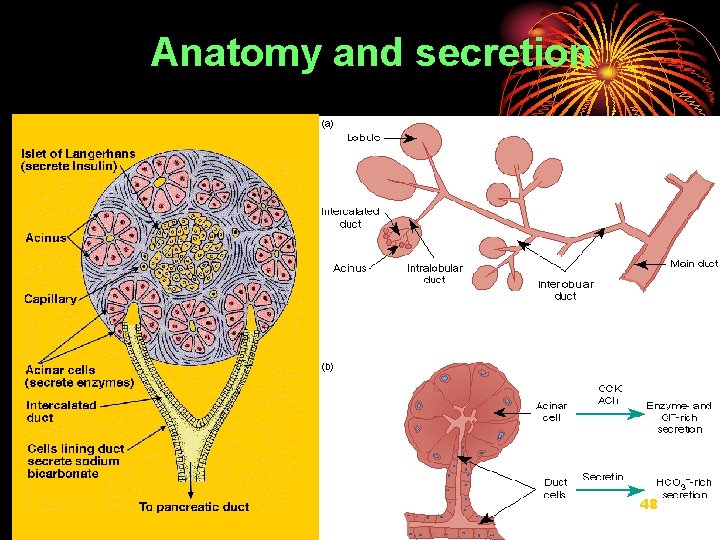
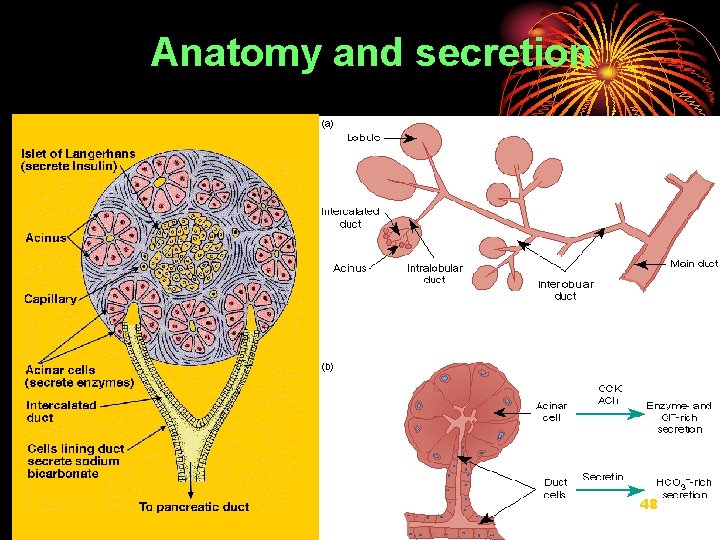
Anatomy and secretion 48

Islet of Langerhans (secrete insulin) Acinus Capillary Acinar cells (secrete enzymes) Intercalated duct Duct cells (secrete HCO 3) 49 To pancreatic duct
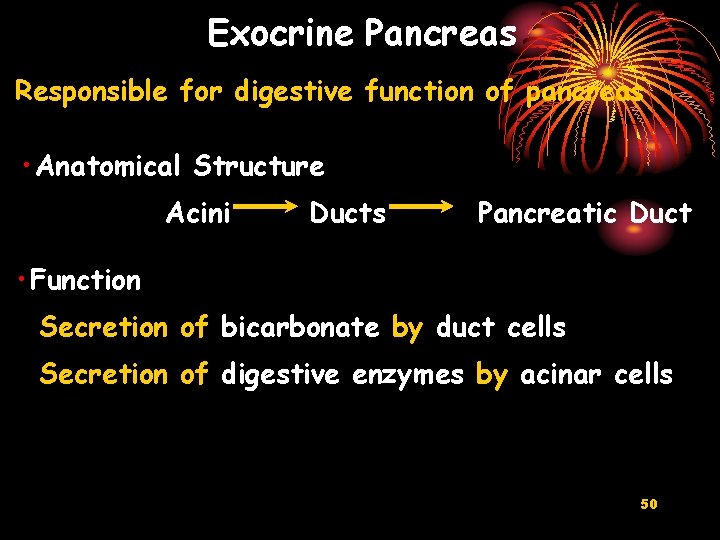
Exocrine Pancreas Responsible for digestive function of pancreas • Anatomical Structure Acini Ducts Pancreatic Duct • Function Secretion of bicarbonate by duct cells Secretion of digestive enzymes by acinar cells 50

Zymogens • Acinar cells contain digestive enzymes stored as inactive zymogen granules • Prevents autodigestion of pancreas • Enterokinase (bound to brush border of duodenal enterocytes) converts trypsinogen to trypsin • Trypsin converts all other zymogens to active forms Duodenum 51
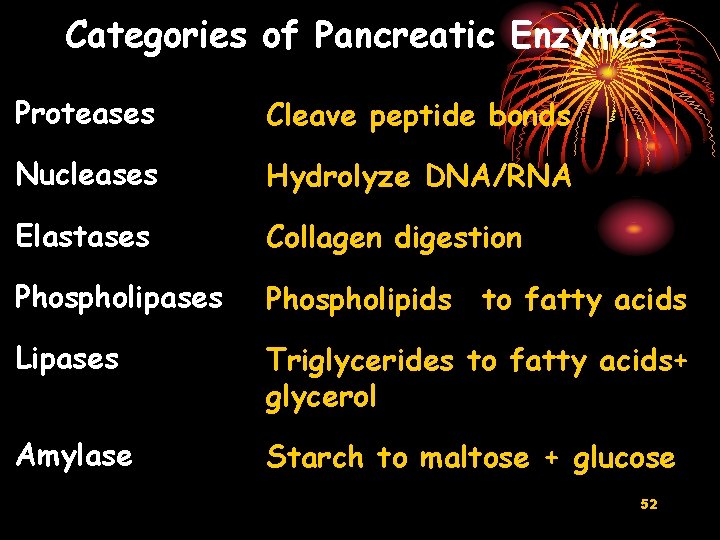
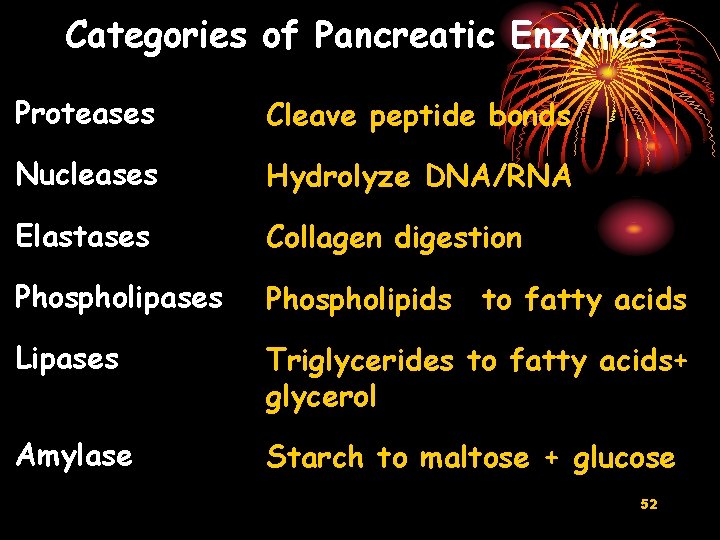
Categories of Pancreatic Enzymes Proteases Cleave peptide bonds Nucleases Hydrolyze DNA/RNA Elastases Collagen digestion Phospholipases Phospholipids Lipases Triglycerides to fatty acids+ glycerol Amylase Starch to maltose + glucose to fatty acids 52

Activation of pancreatic proteases Enterokinase Trypsinogen Chymotrypsinogen Proelastase Procarboxypeptidase Trypsin Chymotrypsin Elastase Carboxypeptidase 53
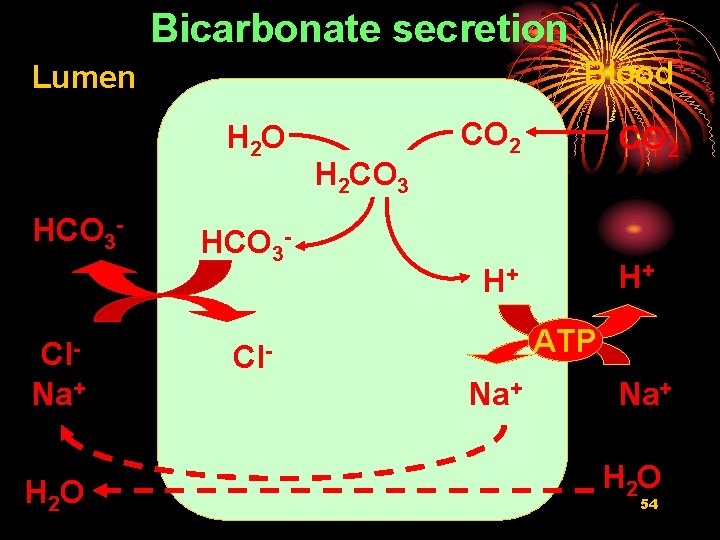
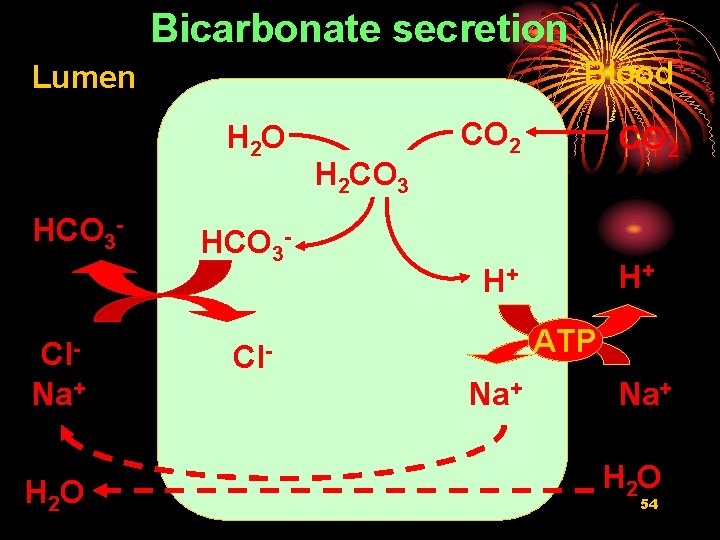
Bicarbonate secretion Blood Lumen H 2 O HCO 3 - Cl. Na+ H 2 O HCO 3 - H 2 CO 3 CO 2 H+ H+ ATP Cl. Na+ H 2 O 54
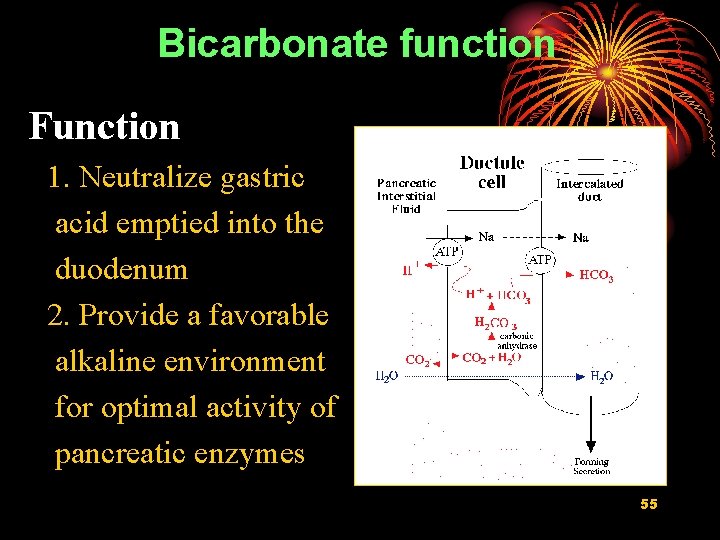
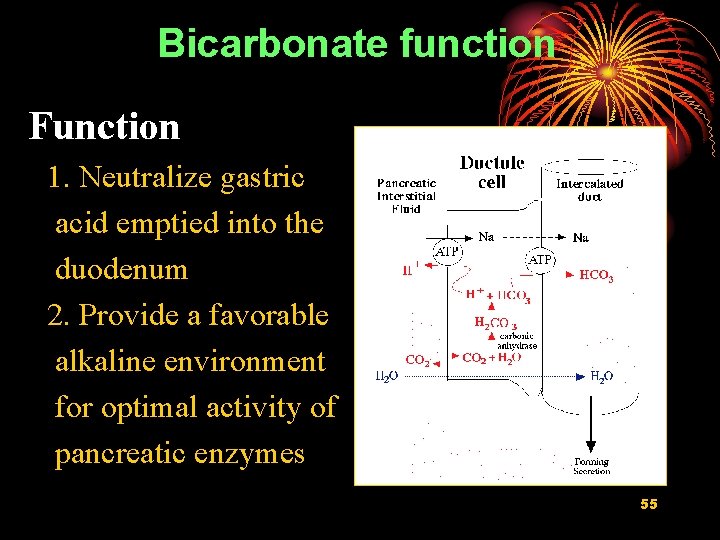
Bicarbonate function Function 1. Neutralize gastric acid emptied into the duodenum 2. Provide a favorable alkaline environment for optimal activity of pancreatic enzymes 55
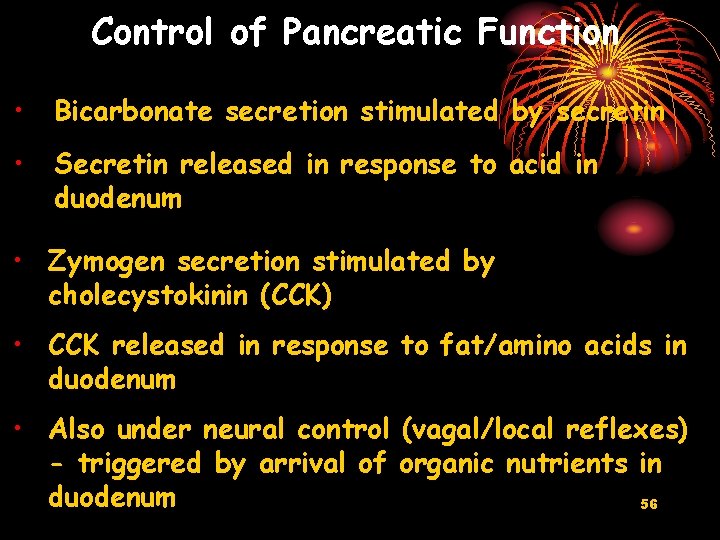
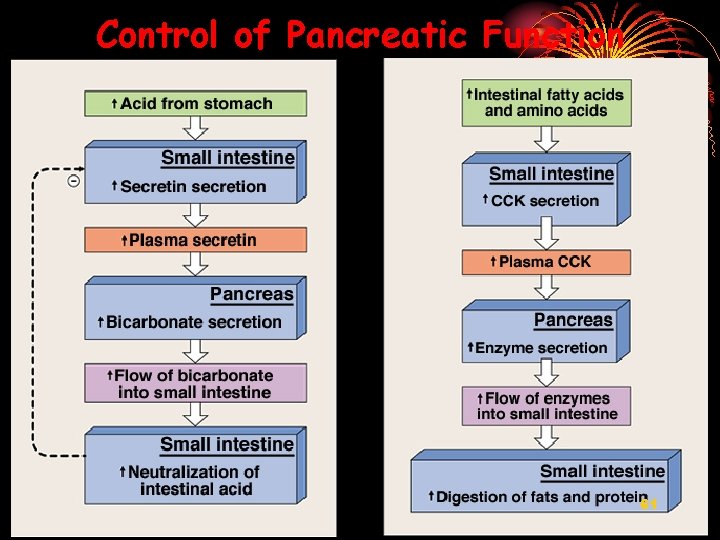
Control of Pancreatic Function • Bicarbonate secretion stimulated by secretin • Secretin released in response to acid in duodenum • Zymogen secretion stimulated by cholecystokinin (CCK) • CCK released in response to fat/amino acids in duodenum • Also under neural control (vagal/local reflexes) - triggered by arrival of organic nutrients in duodenum 56
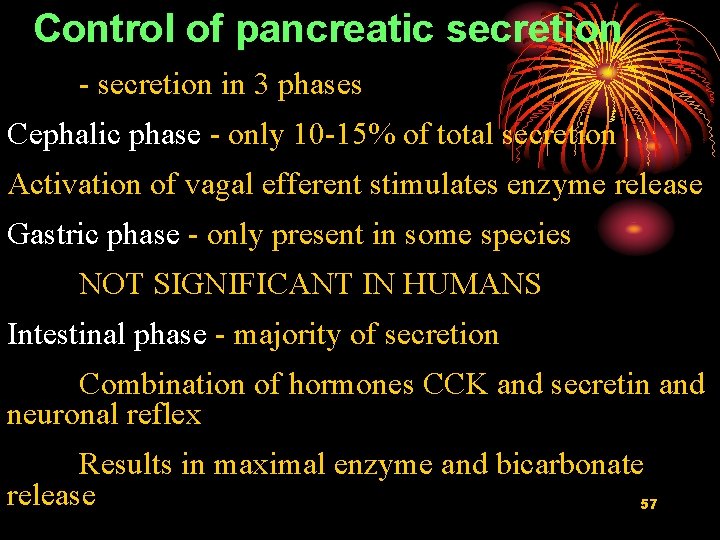
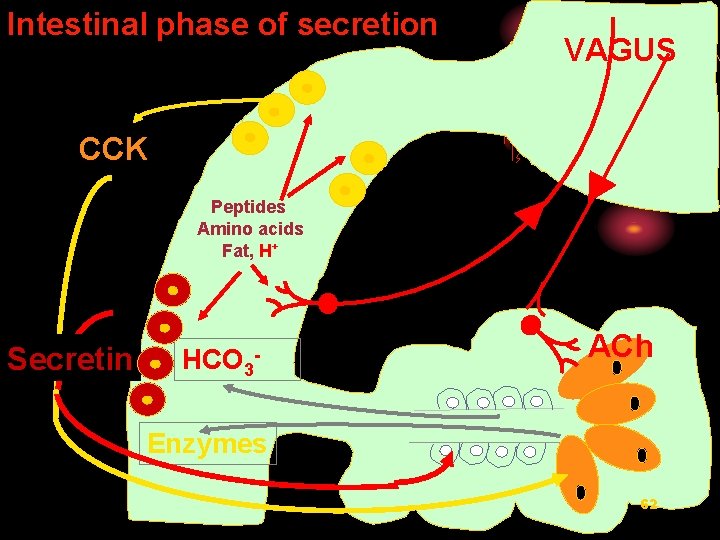
Control of pancreatic secretion - secretion in 3 phases Cephalic phase - only 10 -15% of total secretion Activation of vagal efferent stimulates enzyme release Gastric phase - only present in some species NOT SIGNIFICANT IN HUMANS Intestinal phase - majority of secretion Combination of hormones CCK and secretin and neuronal reflex Results in maximal enzyme and bicarbonate release 57
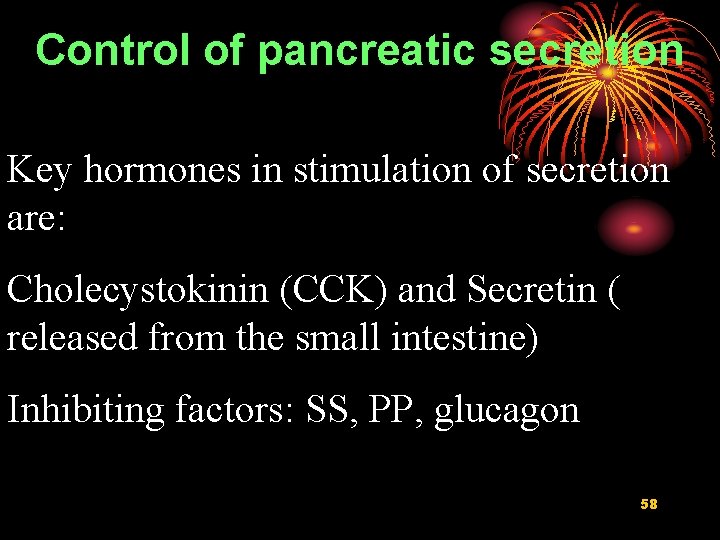
Control of pancreatic secretion Key hormones in stimulation of secretion are: Cholecystokinin (CCK) and Secretin ( released from the small intestine) Inhibiting factors: SS, PP, glucagon 58
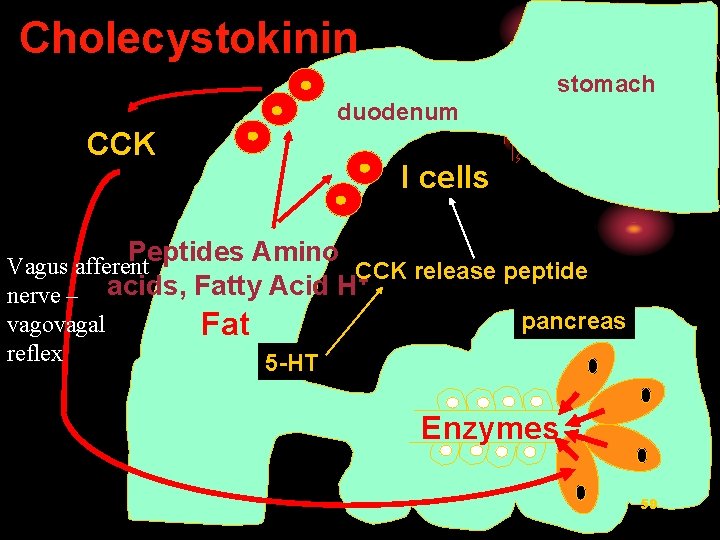
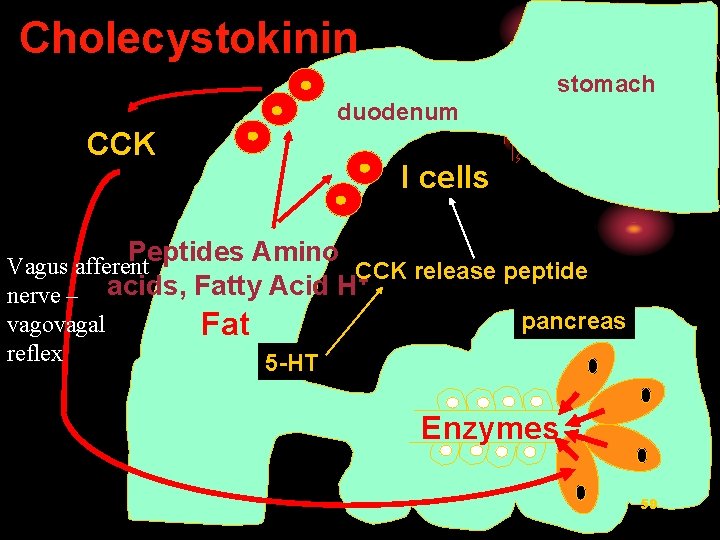
Cholecystokinin stomach duodenum CCK I cells Peptides Amino Vagus afferent CCK release peptide + nerve – acids, Fatty Acid H pancreas vagovagal Fat reflex 5 -HT Enzymes 59
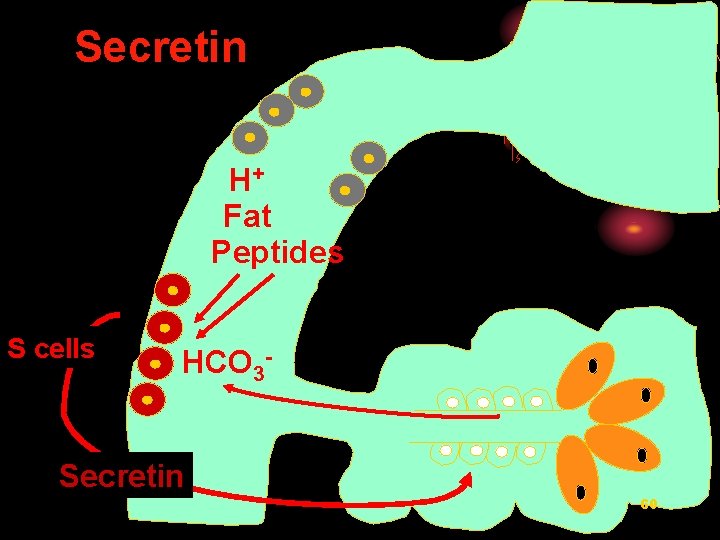
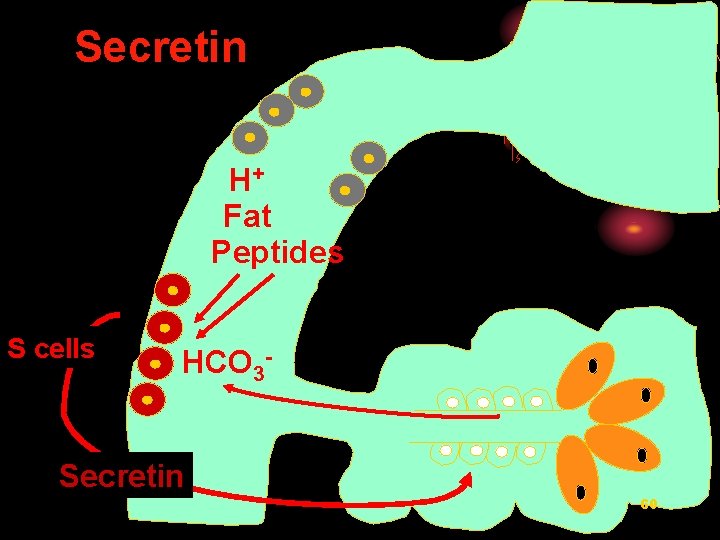
Secretin H+ Fat Peptides S cells HCO 3 - Secretin 60
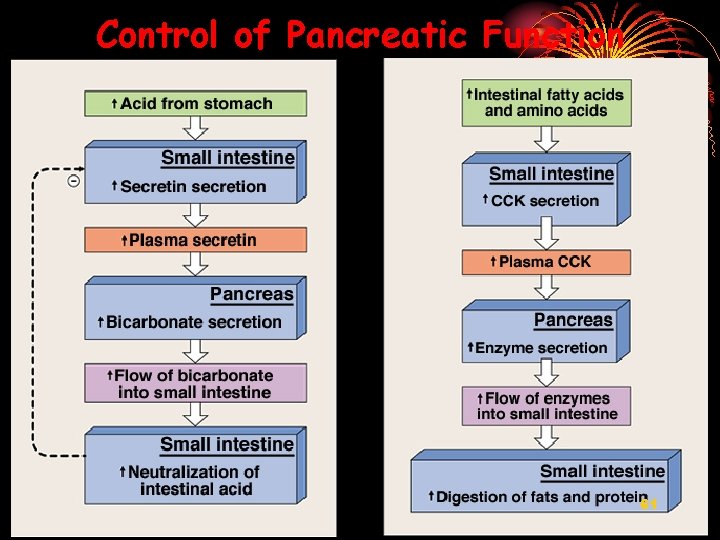
Control of Pancreatic Function 61
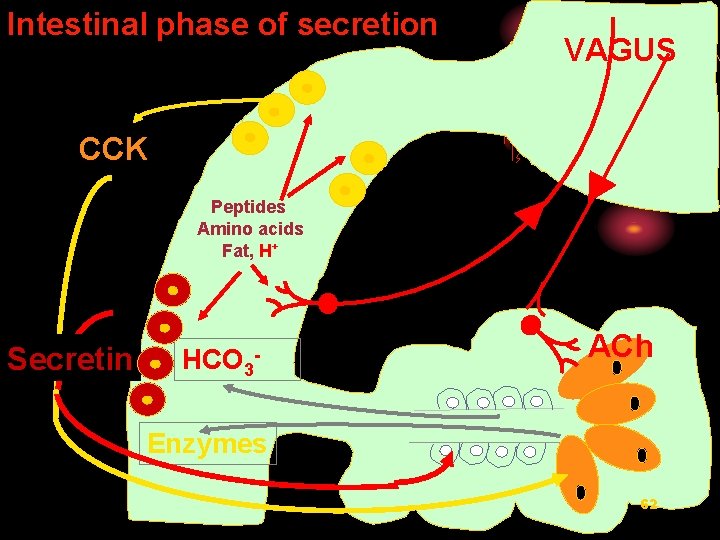
Intestinal phase of secretion VAGUS CCK Peptides Amino acids Fat, H+ Secretin HCO 3 - ACh Enzymes 62

IV Biliary secretion 63
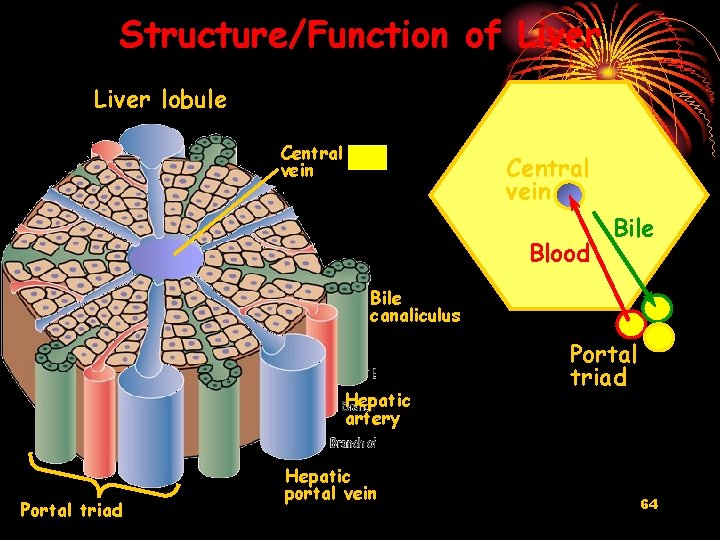
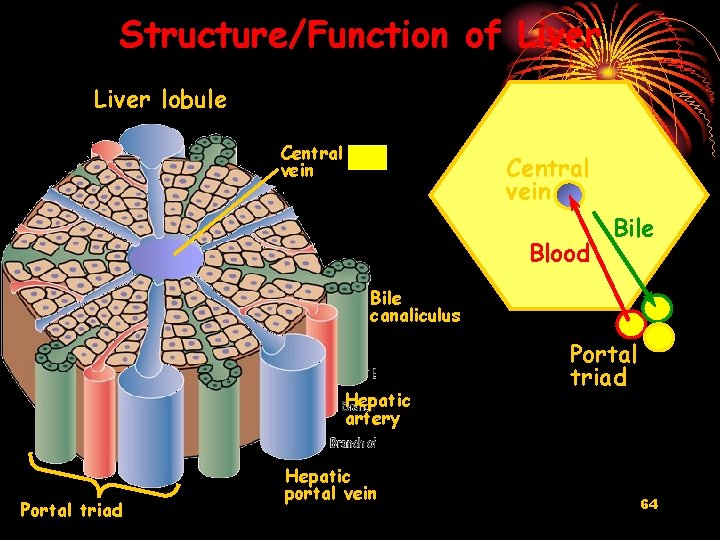
Structure/Function of Liver lobule Central vein Blood Bile canaliculus Hepatic artery Portal triad Hepatic portal vein Portal triad 64

65
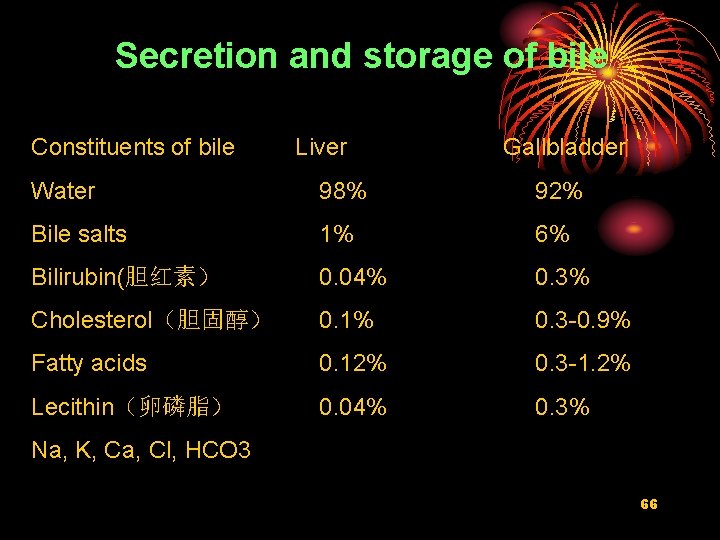
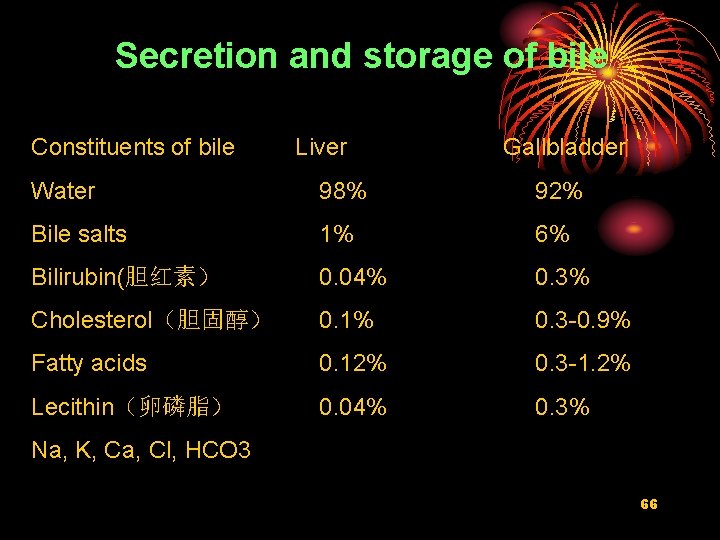
Secretion and storage of bile Constituents of bile Liver Gallbladder Water 98% 92% Bile salts 1% 6% Bilirubin(胆红素) 0. 04% 0. 3% Cholesterol(胆固醇) 0. 1% 0. 3 -0. 9% Fatty acids 0. 12% 0. 3 -1. 2% Lecithin(卵磷脂) 0. 04% 0. 3% Na, K, Ca, Cl, HCO 3 66

Functions of bile ØEmulsification of fats ØIncreased absorption of lipids into enterocytes (include vitamin A, D, E, K) ØIncreased synthesis and secretion of bile ØCholesterol excretion (only route) ØExcretion of breakdown products of haemoglobin (bilirubin,胆红素) 67
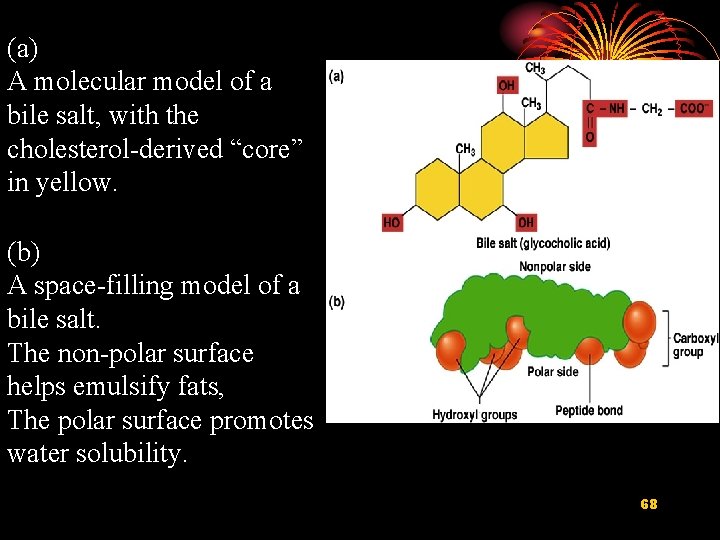
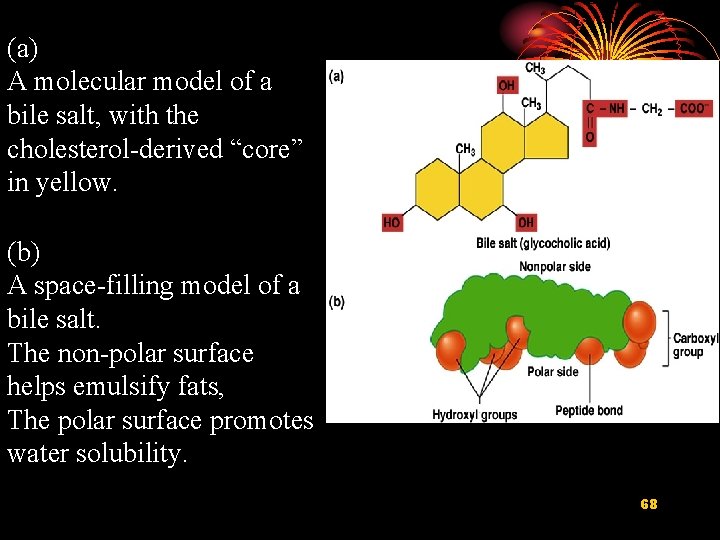
(a) A molecular model of a bile salt, with the cholesterol-derived “core” in yellow. (b) A space-filling model of a bile salt. The non-polar surface helps emulsify fats, The polar surface promotes water solubility. 68
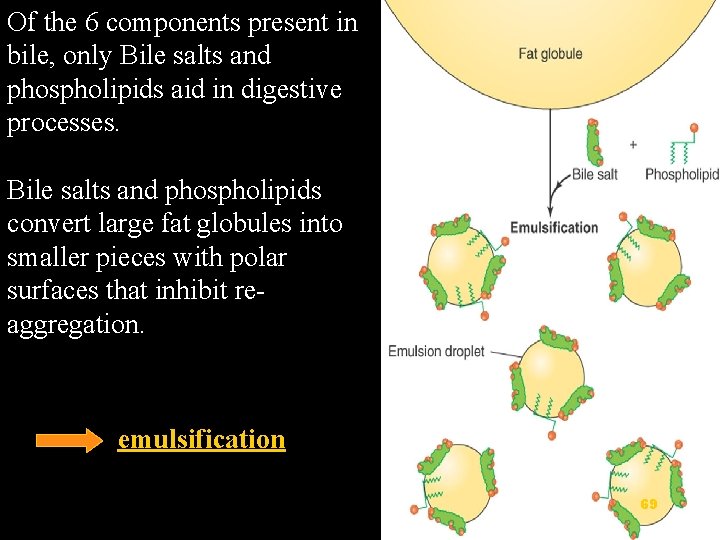
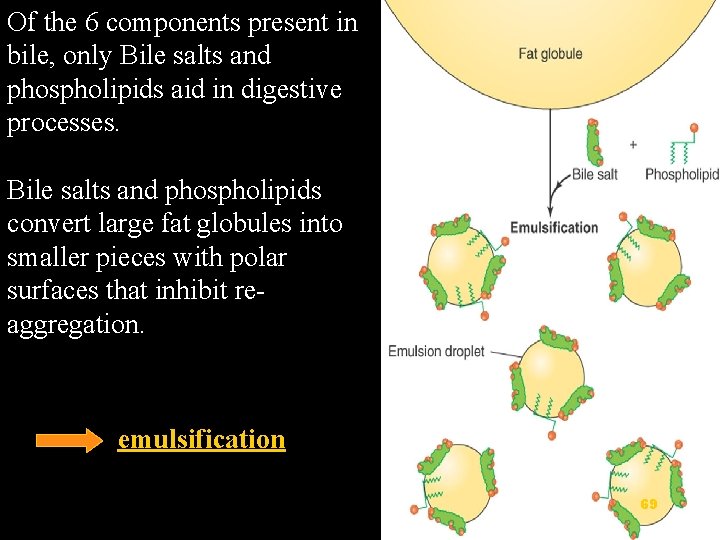
Of the 6 components present in bile, only Bile salts and phospholipids aid in digestive processes. Bile salts and phospholipids convert large fat globules into smaller pieces with polar surfaces that inhibit reaggregation. emulsification 69
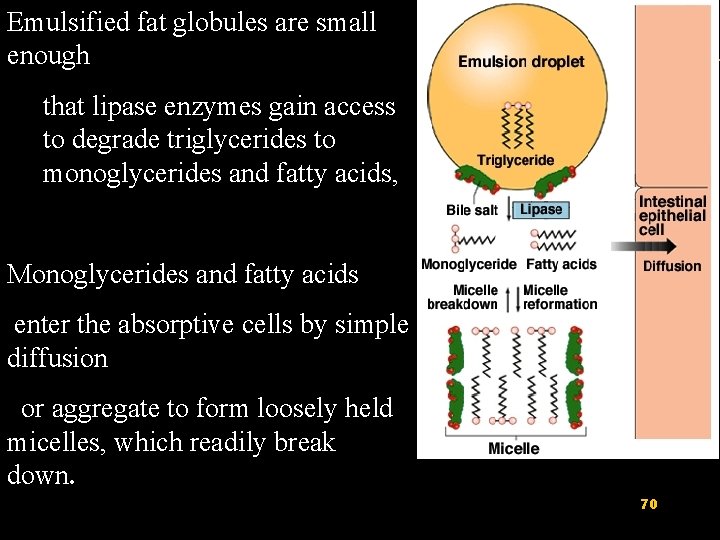
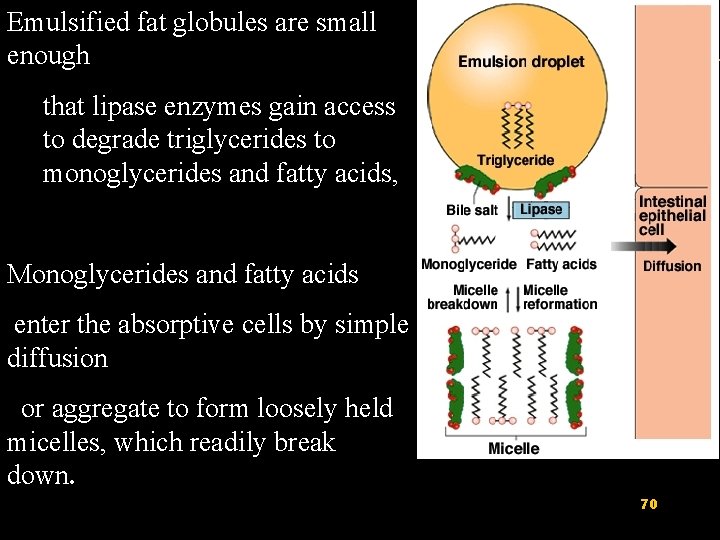
Emulsified fat globules are small enough that lipase enzymes gain access to degrade triglycerides to monoglycerides and fatty acids, Monoglycerides and fatty acids enter the absorptive cells by simple diffusion or aggregate to form loosely held micelles, which readily break down. 70
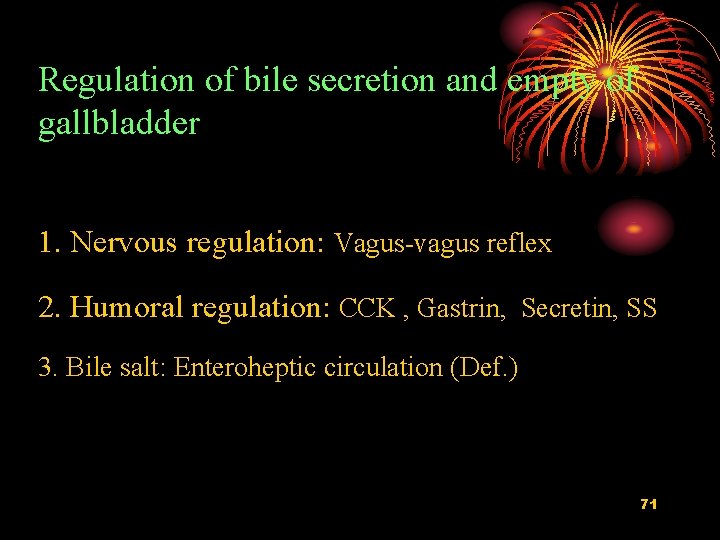
Regulation of bile secretion and empty of gallbladder 1. Nervous regulation: Vagus-vagus reflex 2. Humoral regulation: CCK , Gastrin, Secretin, SS 3. Bile salt: Enteroheptic circulation (Def. ) 71
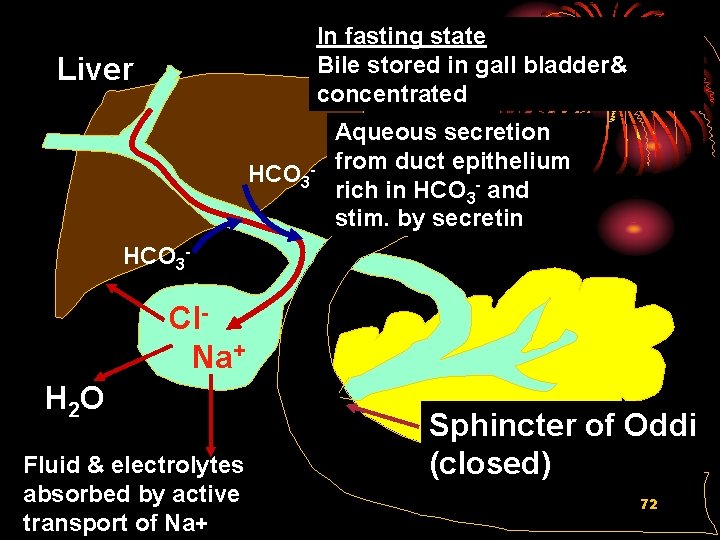
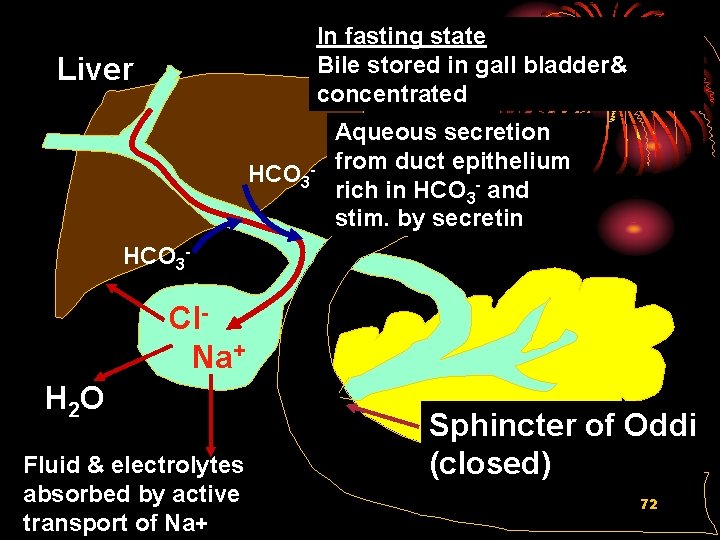
In fasting state Bile stored in gall bladder& concentrated Liver HCO 3 - Aqueous secretion from duct epithelium rich in HCO 3 - and stim. by secretin HCO 3 - Cl. Na+ H 2 O Fluid & electrolytes absorbed by active transport of Na+ Sphincter of Oddi (closed) 72

Digestion - fat in duodenum stimulates CCK release from I cells FAT CCK Gall bladder contraction BILE 73 Sphincter of Oddi relaxes
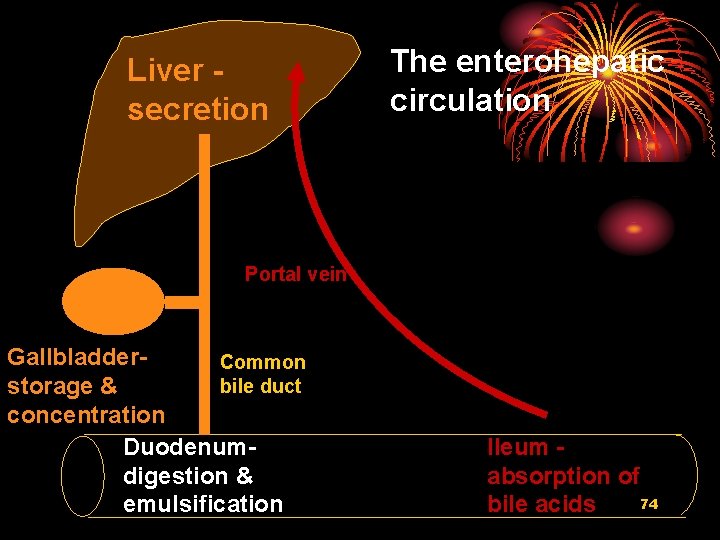
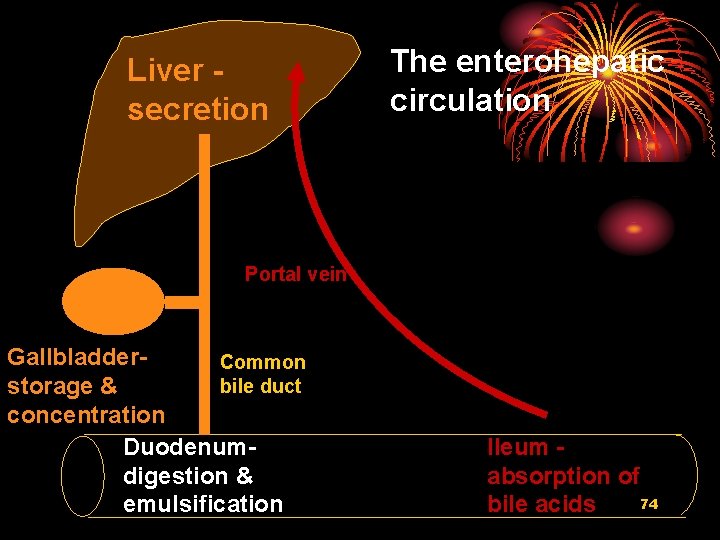
Liver secretion The enterohepatic circulation Portal vein Gallbladder. Common bile duct storage & concentration Duodenumdigestion & emulsification Ileum absorption of 74 bile acids
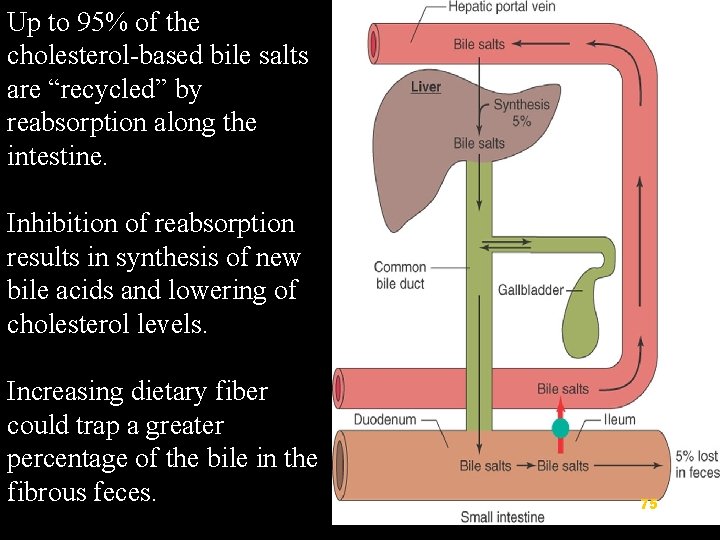
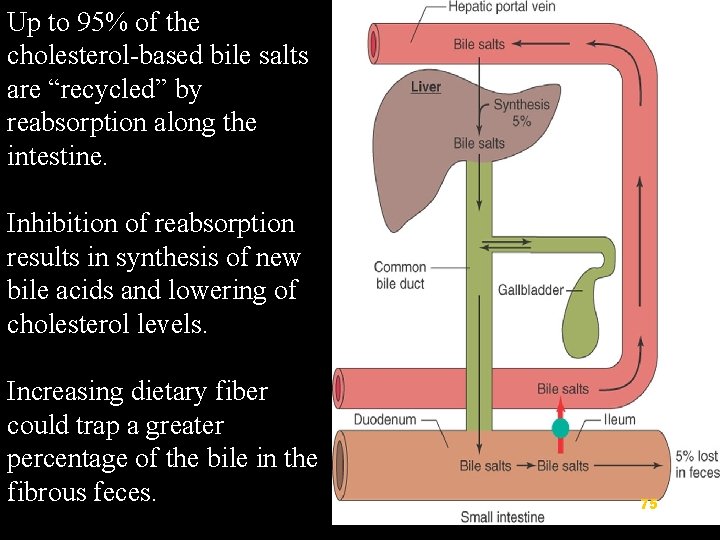
Up to 95% of the cholesterol-based bile salts are “recycled” by reabsorption along the intestine. Inhibition of reabsorption results in synthesis of new bile acids and lowering of cholesterol levels. Increasing dietary fiber could trap a greater percentage of the bile in the fibrous feces. 75
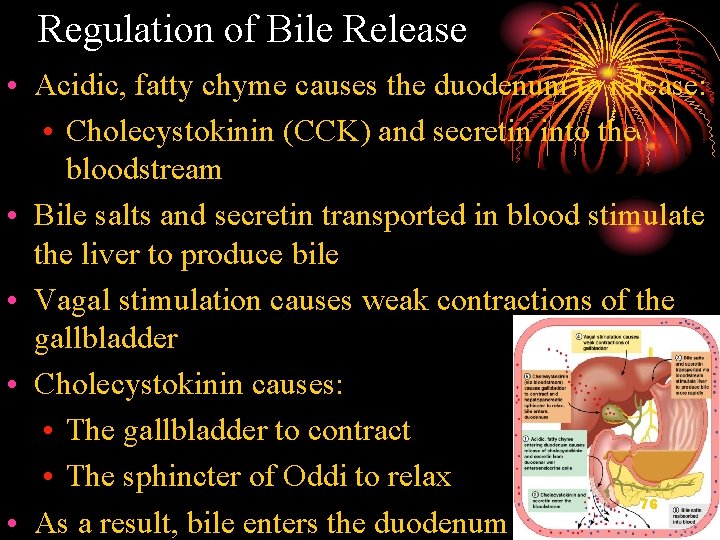
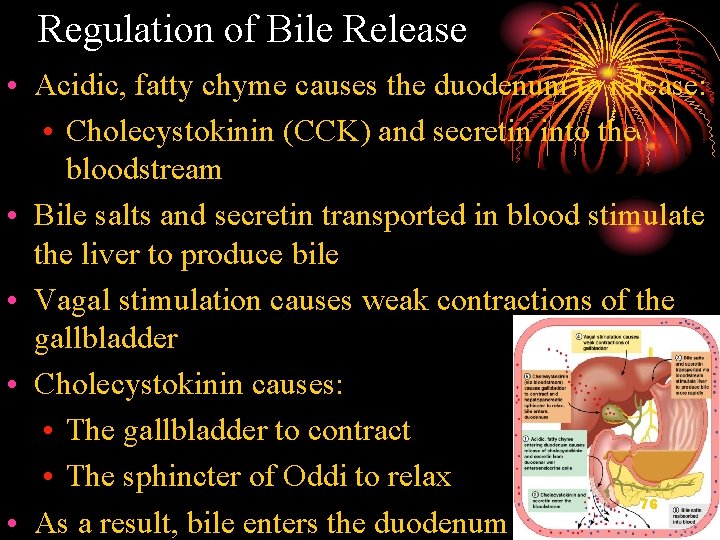
Regulation of Bile Release • Acidic, fatty chyme causes the duodenum to release: • Cholecystokinin (CCK) and secretin into the bloodstream • Bile salts and secretin transported in blood stimulate the liver to produce bile • Vagal stimulation causes weak contractions of the gallbladder • Cholecystokinin causes: • The gallbladder to contract • The sphincter of Oddi to relax 76 • As a result, bile enters the duodenum
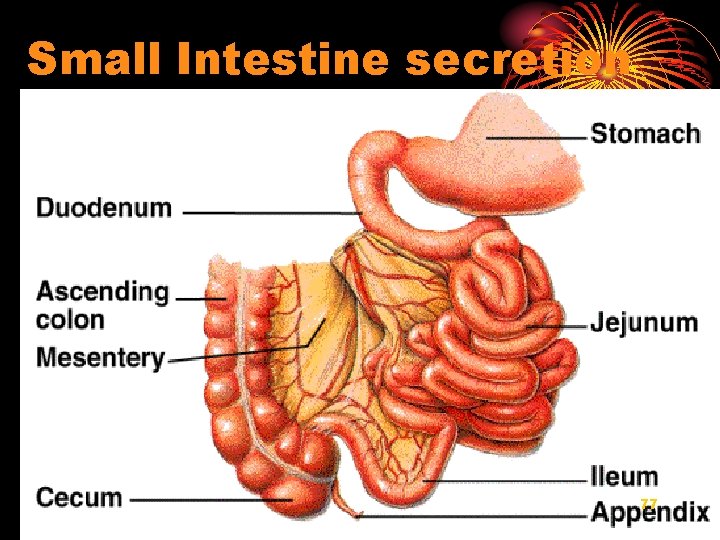
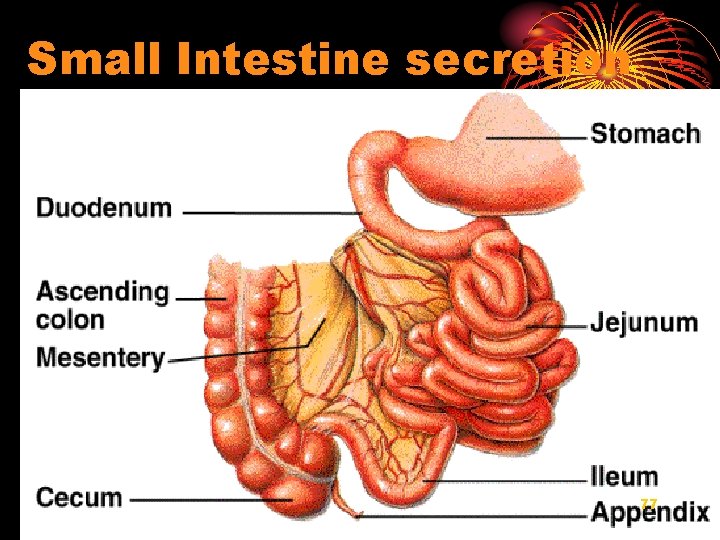
Small Intestine secretion 77
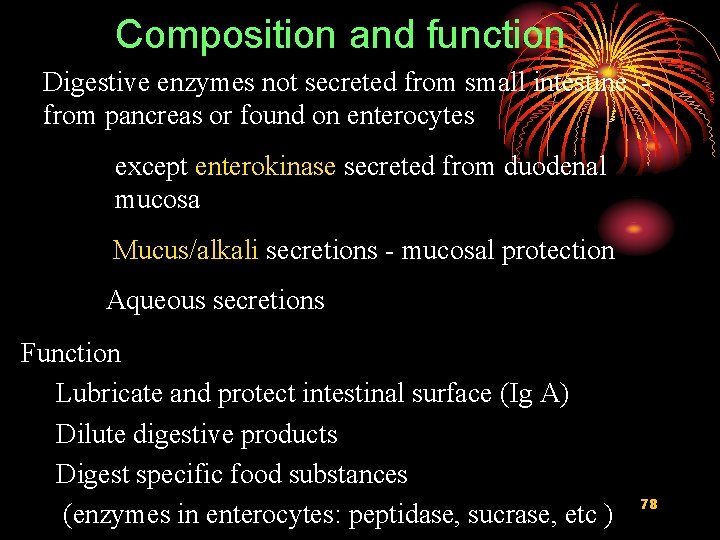
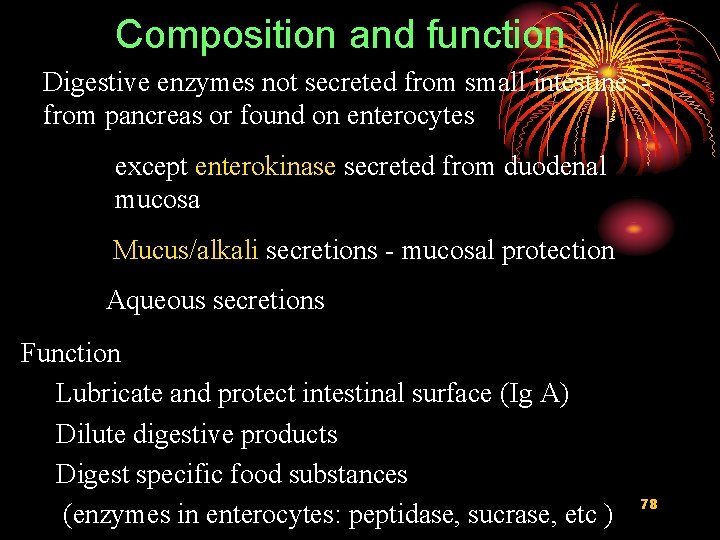
Composition and function Digestive enzymes not secreted from small intestine from pancreas or found on enterocytes except enterokinase secreted from duodenal mucosa Mucus/alkali secretions - mucosal protection Aqueous secretions Function Lubricate and protect intestinal surface (Ig A) Dilute digestive products Digest specific food substances (enzymes in enterocytes: peptidase, sucrase, etc ) 78
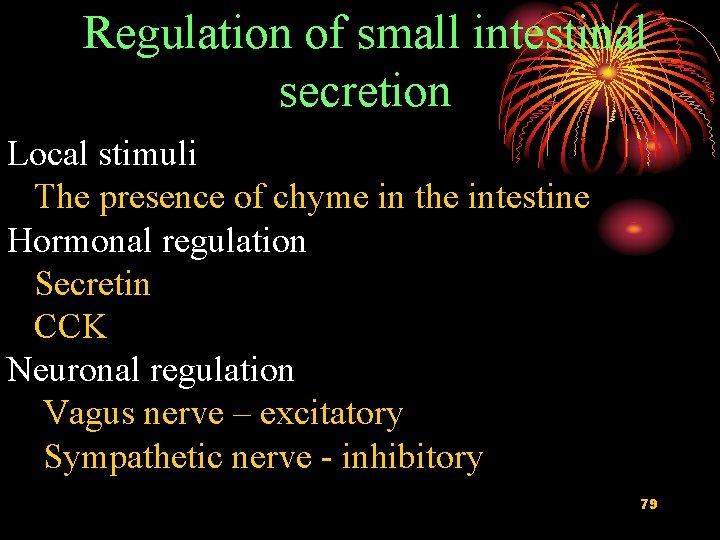
Regulation of small intestinal secretion Local stimuli The presence of chyme in the intestine Hormonal regulation Secretin CCK Neuronal regulation Vagus nerve – excitatory Sympathetic nerve - inhibitory 79
 Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Which is the largest gland of the body
Which is the largest gland of the body Hospice secretions medication
Hospice secretions medication Mobilizing secretions
Mobilizing secretions Git secretions
Git secretions Pooling of secretions
Pooling of secretions Chapter 15 digestive system
Chapter 15 digestive system Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Chemotrypsinogen
Chemotrypsinogen Gastrointestinal hormones
Gastrointestinal hormones Malrotasi traktus gastrointestinal
Malrotasi traktus gastrointestinal Livores violáceos
Livores violáceos Verner morrison sendromu
Verner morrison sendromu Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nutrition focused physical examination
Nutrition focused physical examination Derivatives of foregut
Derivatives of foregut Gastrointestinal tract
Gastrointestinal tract Motilidad gastrointestinal
Motilidad gastrointestinal Gastrointestinal diagram
Gastrointestinal diagram Função intestino delgado e grosso
Função intestino delgado e grosso Identificar
Identificar Ashraf radwan
Ashraf radwan Oral yol
Oral yol Intestinal villus
Intestinal villus Peristalsis and segmentation
Peristalsis and segmentation Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Which is not part of the alimentary canal
Which is not part of the alimentary canal Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Pathophysiology of intestinal obstruction
Pathophysiology of intestinal obstruction Four primary tissue types
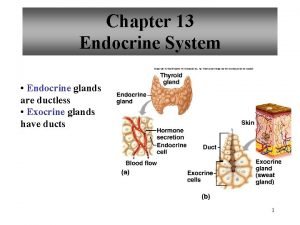
Four primary tissue types Kelenjar endokrin dan eksokrin
Kelenjar endokrin dan eksokrin Is bile in pancreatic juice
Is bile in pancreatic juice Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Are endocrine glands ductless
Are endocrine glands ductless Exocrine cell signaling
Exocrine cell signaling Endocrine exocrine
Endocrine exocrine Classification of exocrine glands
Classification of exocrine glands Papillary and reticular layers
Papillary and reticular layers General structure of exocrine glands
General structure of exocrine glands Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Endocrine exocrine
Endocrine exocrine Glande endocrine exocrine
Glande endocrine exocrine Simple cuboidal epithelium description
Simple cuboidal epithelium description Ipmn
Ipmn Exocrine glands function
Exocrine glands function Epi stool
Epi stool Endocrine vs exocrine
Endocrine vs exocrine Pycnotique
Pycnotique Simple acinar gland histology
Simple acinar gland histology Exocrine glands
Exocrine glands A multicellular exocrine gland consists of ______.
A multicellular exocrine gland consists of ______. Kliere
Kliere The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thang điểm glasgow
Thang điểm glasgow Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể