Gastrointestinal System Organ systems p p Gastrointestinal GI
![Organ systems p p Gastrointestinal (GI) tract [Alimentary canal] a continuous muscular digestive Organ systems p p Gastrointestinal (GI) tract [Alimentary canal] a continuous muscular digestive](https://slidetodoc.com/presentation_image_h/bd24c216406a57907790b0a8b309314b/image-2.jpg)



- Slides: 77
Gastrointestinal System
![Organ systems p p Gastrointestinal GI tract Alimentary canal a continuous muscular digestive Organ systems p p Gastrointestinal (GI) tract [Alimentary canal] a continuous muscular digestive](https://slidetodoc.com/presentation_image_h/bd24c216406a57907790b0a8b309314b/image-2.jpg)
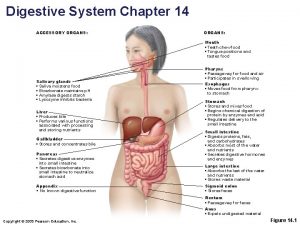
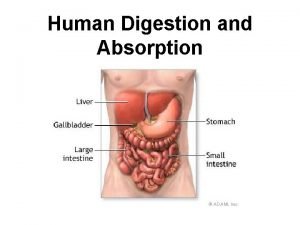
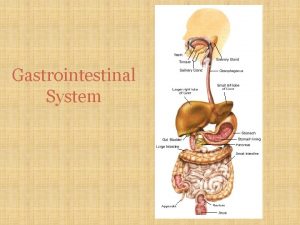
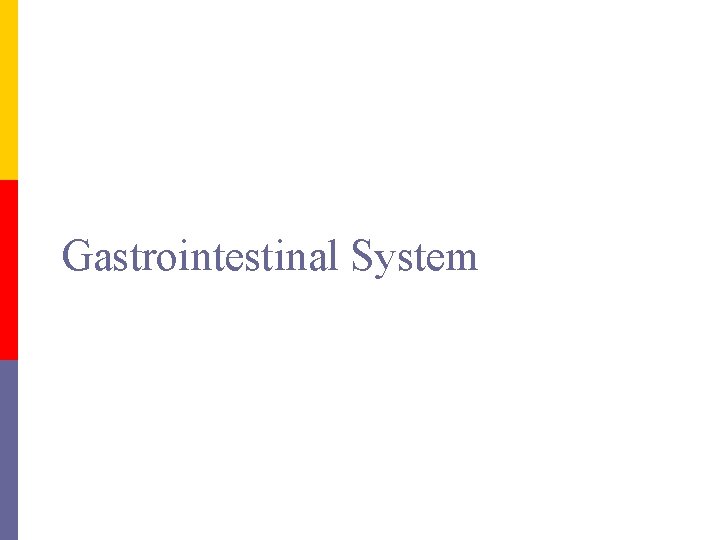
Organ systems p p Gastrointestinal (GI) tract [Alimentary canal] a continuous muscular digestive tube. The digestive system consists of group of organs working together to convert food to energy to feed the entire body. n Digests: p n Absorbs: p n breaks food into smaller fragments digested material is moved through mucosa into the blood Eliminates: p unabsorbed & secreted wastes.
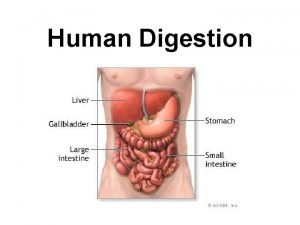
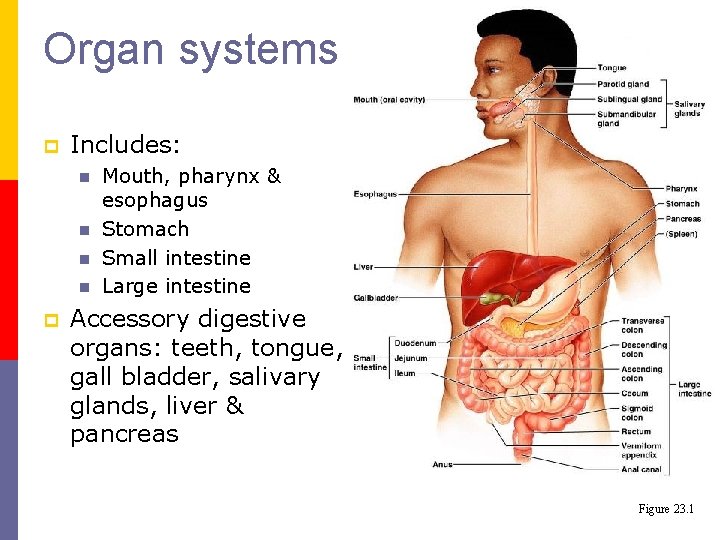
Organ systems p Includes: n n p Mouth, pharynx & esophagus Stomach Small intestine Large intestine Accessory digestive organs: teeth, tongue, gall bladder, salivary glands, liver & pancreas Figure 23. 1
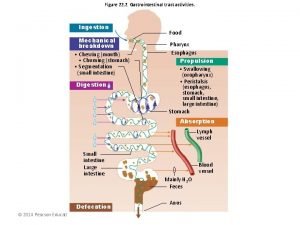
Processes Ingestion p Propulsion p Mechanical digestion p Chemical digestion p Absorption p Defecation p
Processes p p p Ingestion: obtaining food Propulsion: moves food along the GI tract by peristalsis (wave like muscular contraction) Mechanical digestion : n n n chewing & mixing with saliva mixing in stomach segmentation (local constriction in intestine to mix food & digestive juices)
Processes p Chemical digestion: breaks down food to molecular fragments (monomers) (Hydrolysis). n p p Begins in the mouth with saliva & continues into the small intestine. Absorption: movement of nutrients across the mucosal membrane into blood/lymph Defecation: eliminates unused/indigestible & secreted substances from the body
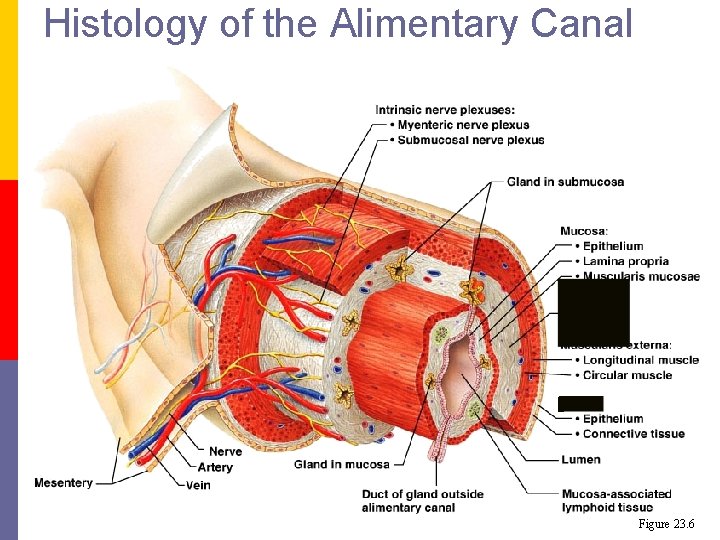
Histology p GI tract wall has 4 layers: n n Mucosa Submucosa Muscularis Externa Serosa or Adventitia
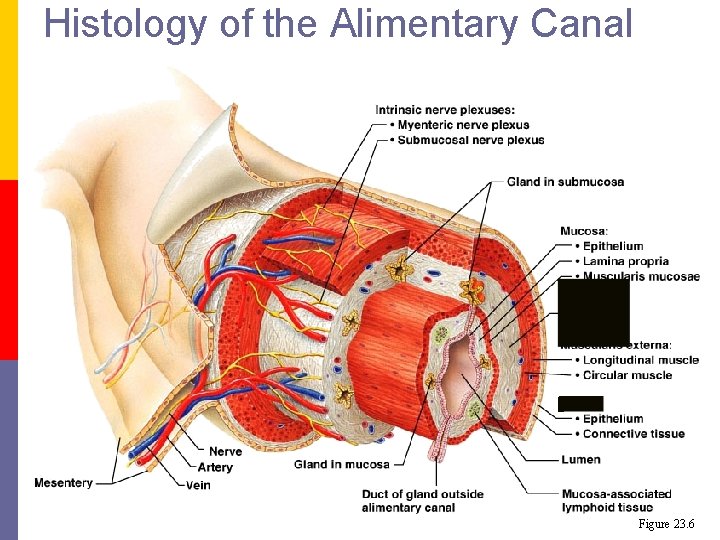
Histology of the Alimentary Canal Figure 23. 6
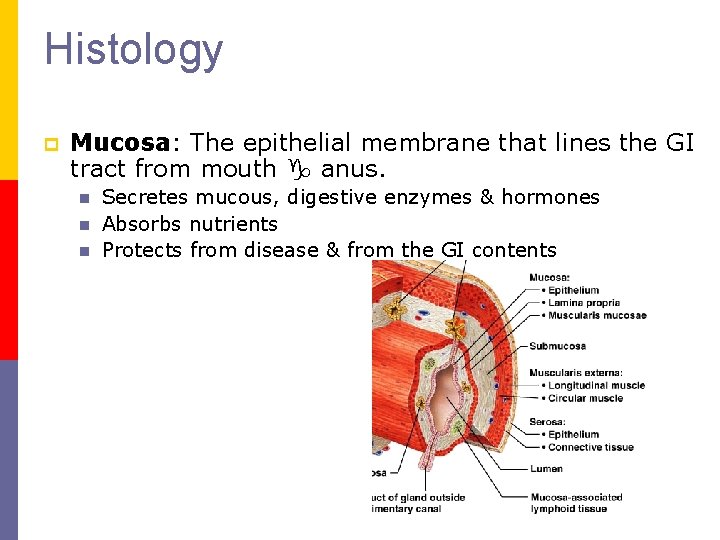
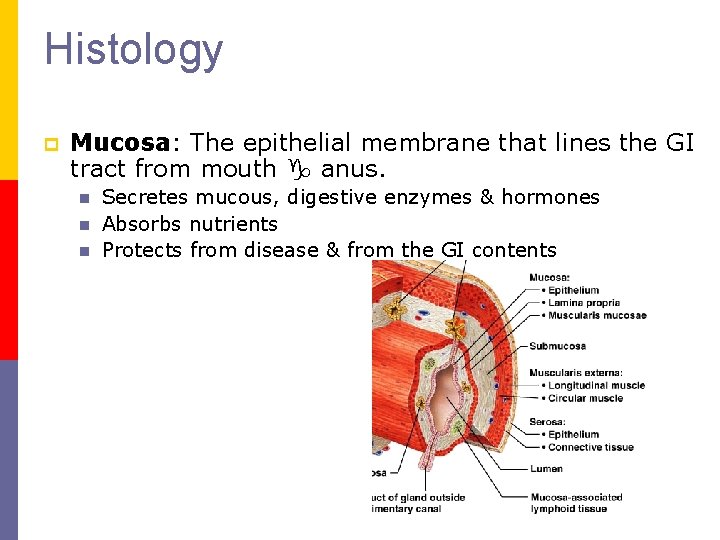
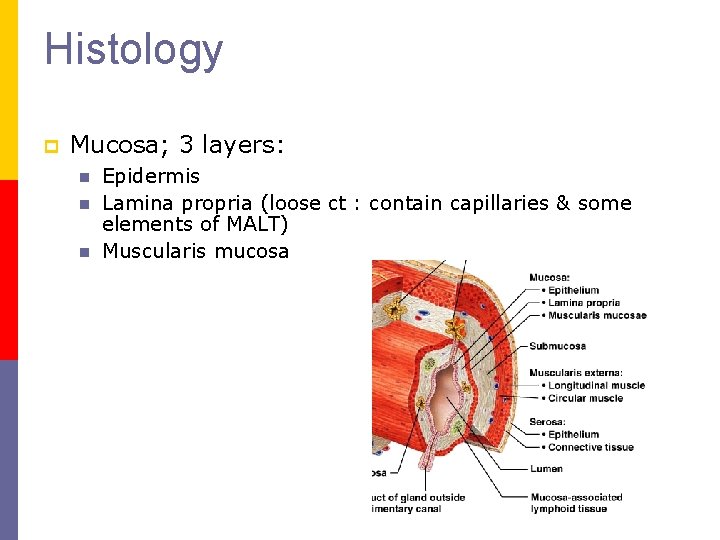
Histology p Mucosa: The epithelial membrane that lines the GI tract from mouth g anus. n n n Secretes mucous, digestive enzymes & hormones Absorbs nutrients Protects from disease & from the GI contents
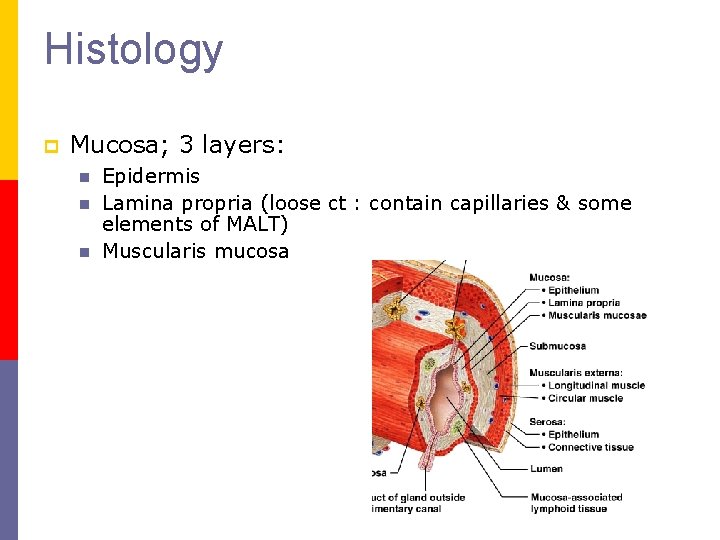
Histology p Mucosa; 3 layers: n n n Epidermis Lamina propria (loose ct : contain capillaries & some elements of MALT) Muscularis mucosa
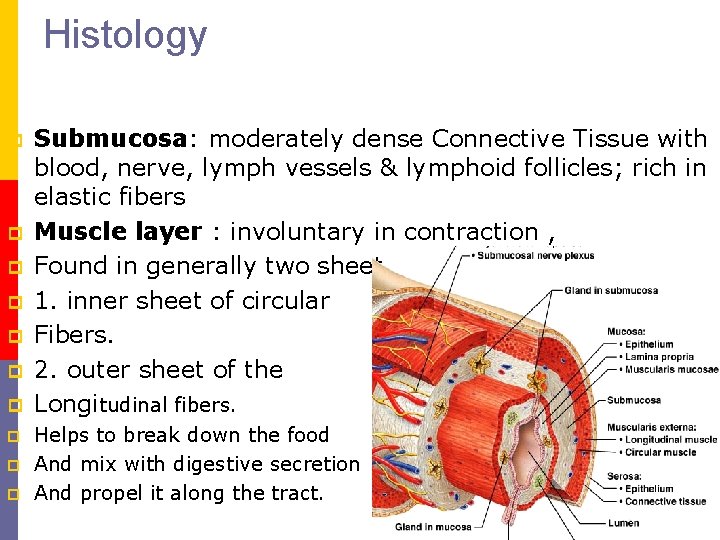
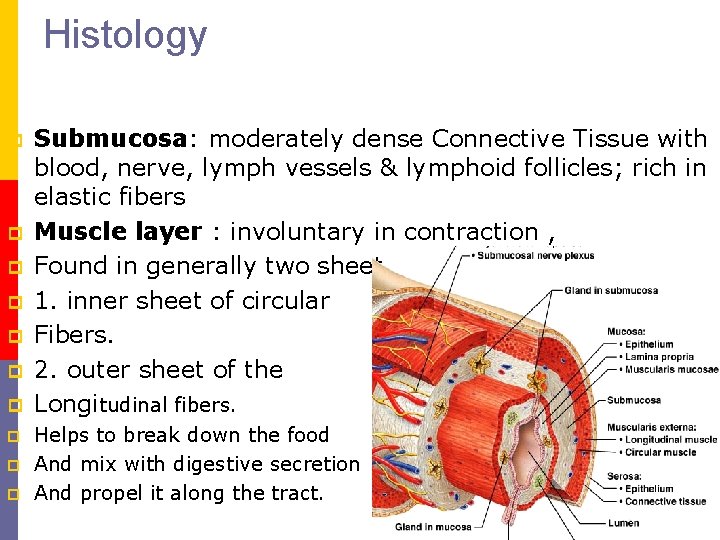
Histology p p p p p Submucosa: moderately dense Connective Tissue with blood, nerve, lymph vessels & lymphoid follicles; rich in elastic fibers Muscle layer : involuntary in contraction , Found in generally two sheet 1. inner sheet of circular Fibers. 2. outer sheet of the Longitudinal fibers. Helps to break down the food And mix with digestive secretion And propel it along the tract.

Adventica or outer covering It is a serous membrane , consist of closed sac containing a small amount of serous fluid , and richly supply with blood vessels and lymph vessels. p
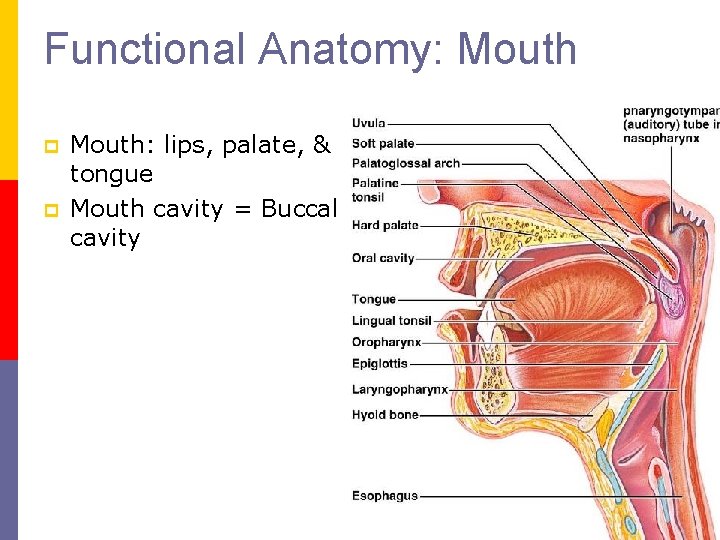
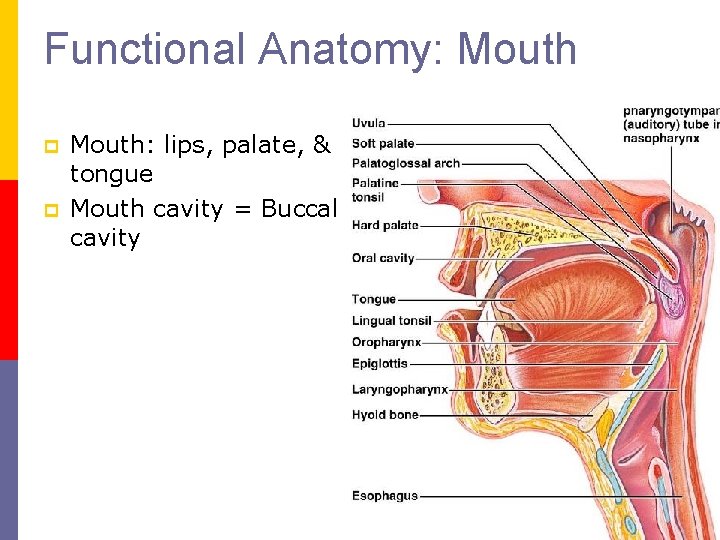
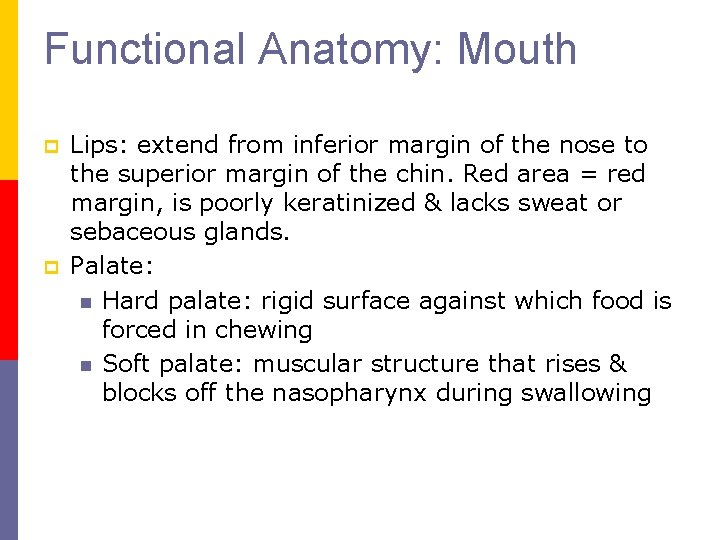
Functional Anatomy: Mouth p p Mouth: lips, palate, & tongue Mouth cavity = Buccal cavity
Functional Anatomy: Mouth p p Lips: extend from inferior margin of the nose to the superior margin of the chin. Red area = red margin, is poorly keratinized & lacks sweat or sebaceous glands. Palate: n Hard palate: rigid surface against which food is forced in chewing n Soft palate: muscular structure that rises & blocks off the nasopharynx during swallowing
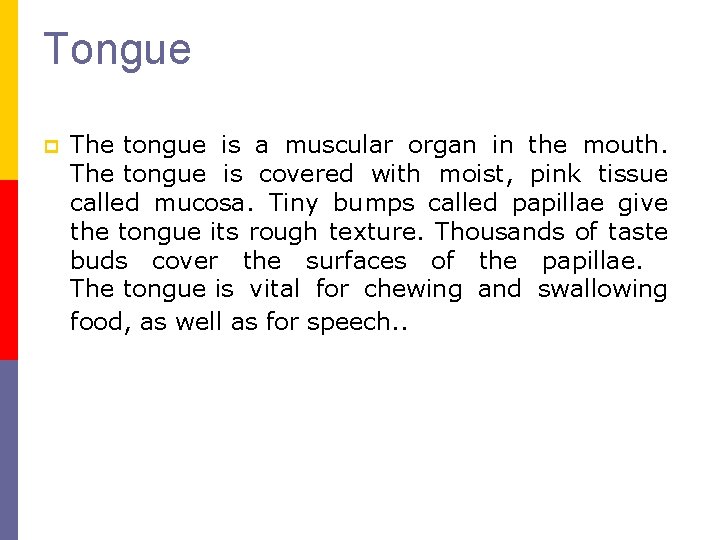
Tongue p The tongue is a muscular organ in the mouth. The tongue is covered with moist, pink tissue called mucosa. Tiny bumps called papillae give the tongue its rough texture. Thousands of taste buds cover the surfaces of the papillae. The tongue is vital for chewing and swallowing food, as well as for speech. .
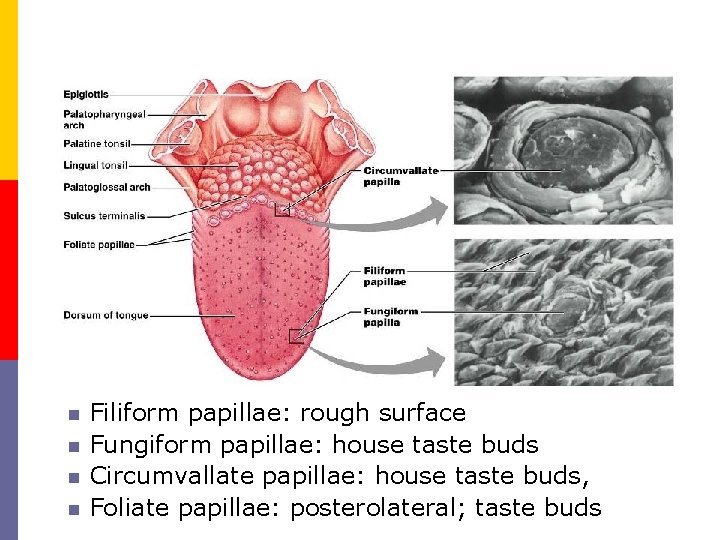
n n Filiform papillae: rough surface Fungiform papillae: house taste buds Circumvallate papillae: house taste buds, Foliate papillae: posterolateral; taste buds
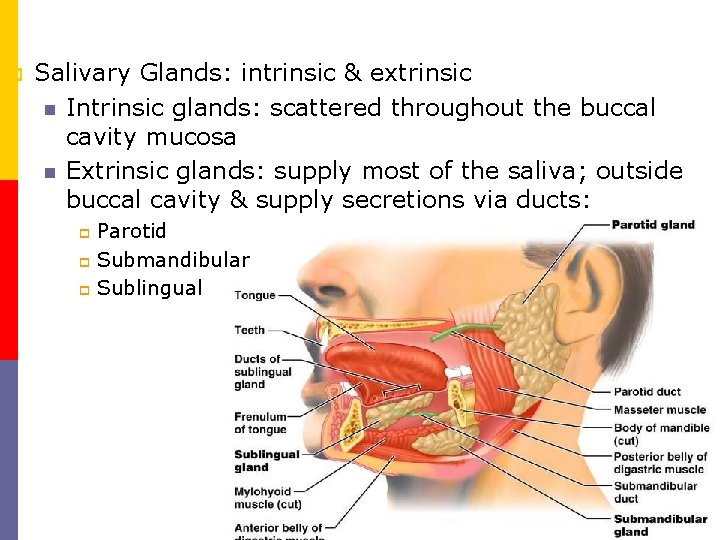
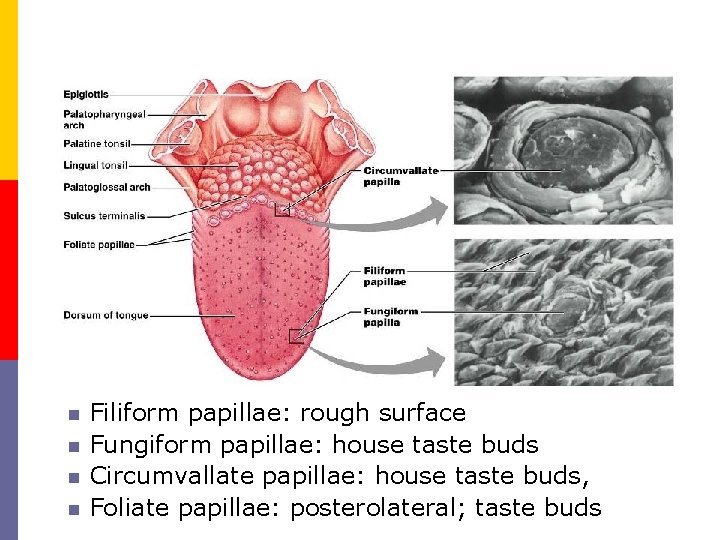
p Salivary Glands: intrinsic & extrinsic n Intrinsic glands: scattered throughout the buccal cavity mucosa n Extrinsic glands: supply most of the saliva; outside buccal cavity & supply secretions via ducts: Parotid p Submandibular p Sublingual p
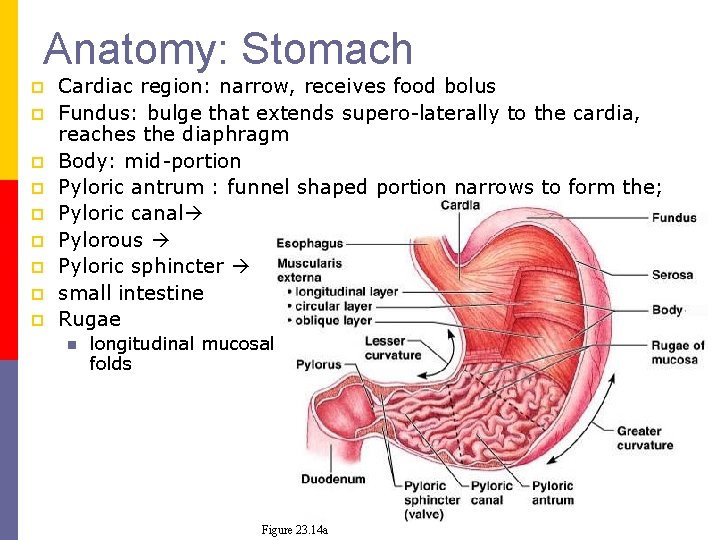
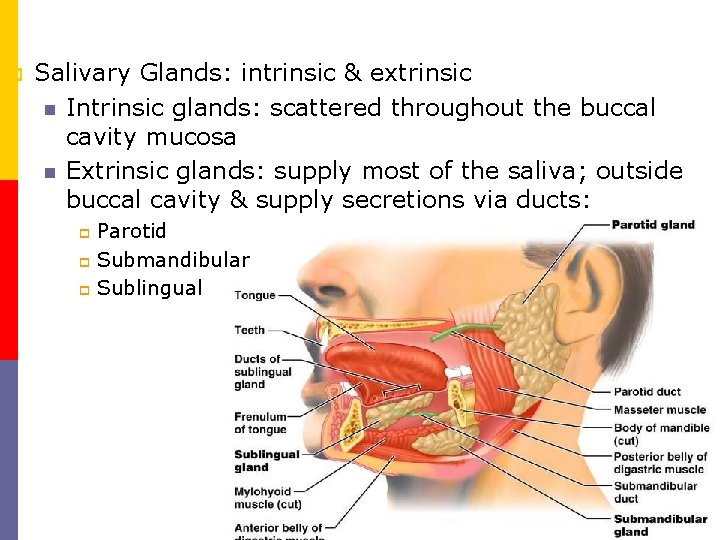
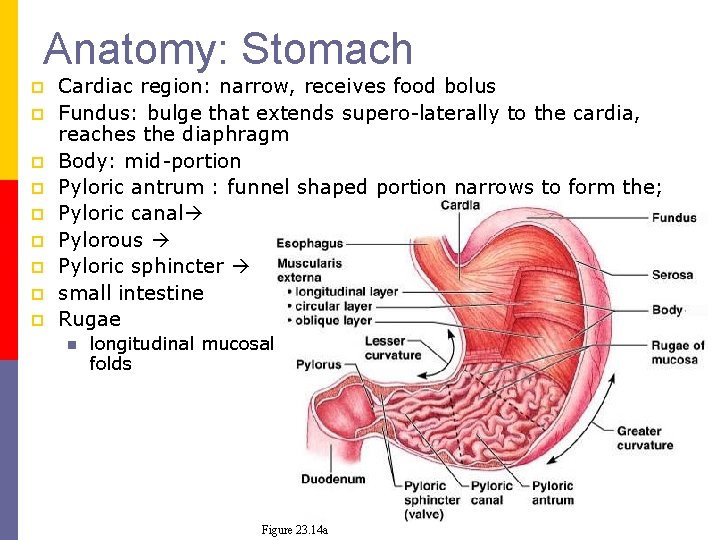
Anatomy: Stomach p p p p p Cardiac region: narrow, receives food bolus Fundus: bulge that extends supero laterally to the cardia, reaches the diaphragm Body: mid portion Pyloric antrum : funnel shaped portion narrows to form the; Pyloric canal Pylorous Pyloric sphincter small intestine Rugae n longitudinal mucosal folds Figure 23. 14 a
Stomach is the widest , most distensible part of the alimentary canal. p It connects esophagus to the duodenum. p The opening between esophagus and stomach is guarded by lower esophageal sphincter or cardiac sphincter p The opening between stomach and duodenum is guarded by pyloric sphincter. p
p Shape : J shape Location : Abdominal cavity , epigastric , umbilical and left hypochondriac region p Capacity : 1. 5 to 2 liters p Length : about 25 cm p
Curvatures p The stomach has two curvatures p The lesser curvature is short and lies in the medial border of stomach. p The greater curvature is long and lies in the lateral border of the stomach. p
Functions p Temporary storage organ: p It acts as a temporary storage organ. Because of this, the frequency of eating is reduced. p Secretory function : p It secretes HCl and pepsin(helps to digest protein) apart from other things including mucus. The G cells of pyloric region secrete gastrin hormone which is one of the GI tract hormones. p Digestive function is because of pepsin enzyme. It is a proteolytic enzyme.

Protective function is because of high acidic medium due to presence of HCl, many of the micro organisms die. Thereby it protects the GI tract from getting invaded by the microorganisms. p Hemopoietic function is because of the intrinsic factor which is secreted by gastric glands. Intrinsic factor is essential for absorption of vitamin B 12 in the ileum region. p Absorptive function is also one of the functions of stomach. Some amount of water and alcohol is absorbed in the stomach region p
Microscopic Anatomy : Stomach p p Mucous neck cells: in the duct portion Gastric glands secrete gastric juices n n n Mucous neck cells: in the duct portion Parietal cells: mid portion of glands secrete HCl & intrinsic factor Chief cells: base of gland; secretes pepsinogen a precursor molecule to pepsin (an enzyme that digests protein)
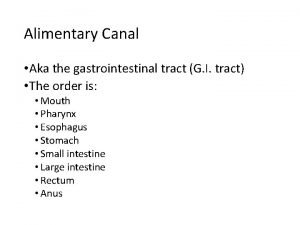
Small Intestine: Gross Anatomy 6 7 m long: from pyloric sphincter to the ileocecal valve p 3 subdivisions: p n n n Duodenum Jejunum Ileum
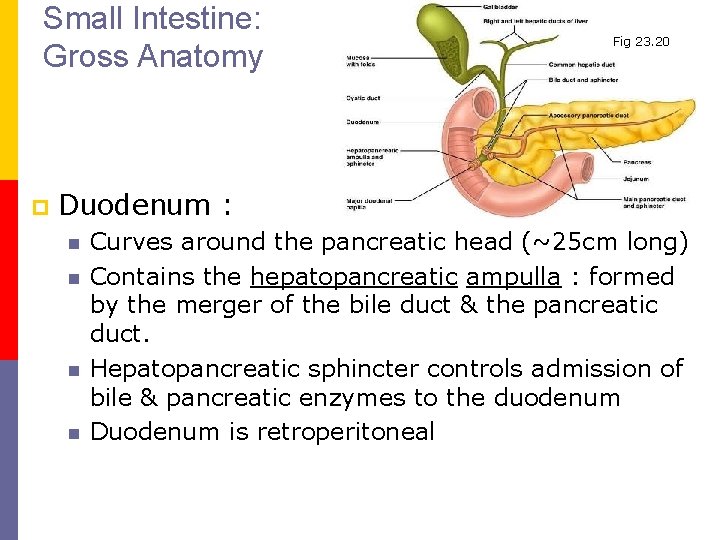
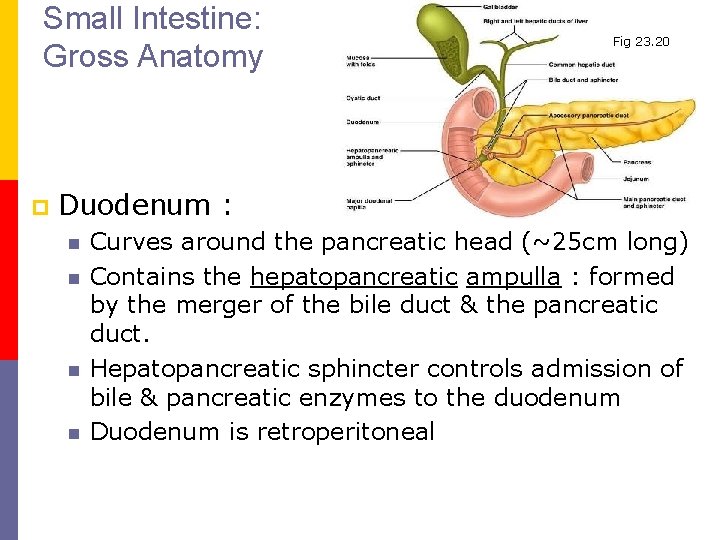
Small Intestine: Gross Anatomy p Fig 23. 20 Duodenum : n n Curves around the pancreatic head (~25 cm long) Contains the hepatopancreatic ampulla : formed by the merger of the bile duct & the pancreatic duct. Hepatopancreatic sphincter controls admission of bile & pancreatic enzymes to the duodenum Duodenum is retroperitoneal
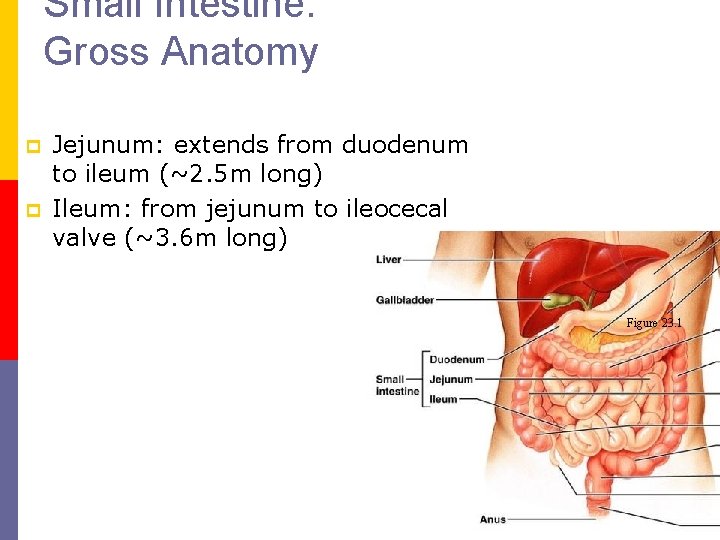
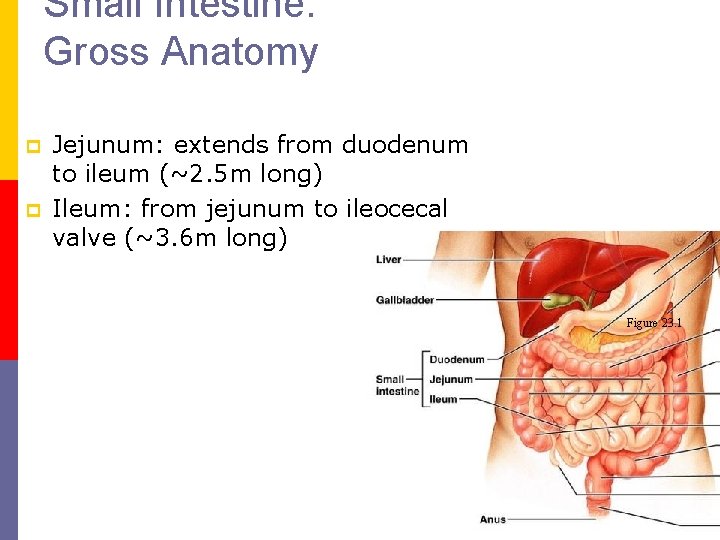
Small Intestine: Gross Anatomy p p Jejunum: extends from duodenum to ileum (~2. 5 m long) Ileum: from jejunum to ileocecal valve (~3. 6 m long) Figure 23. 1
Small Intestine: Gross Anatomy p Jejunum & Ileum function in absorption; n Intraperitoneal n Suspended from mesentery whose veins & lymph vessels carry nutrients away from small intestine
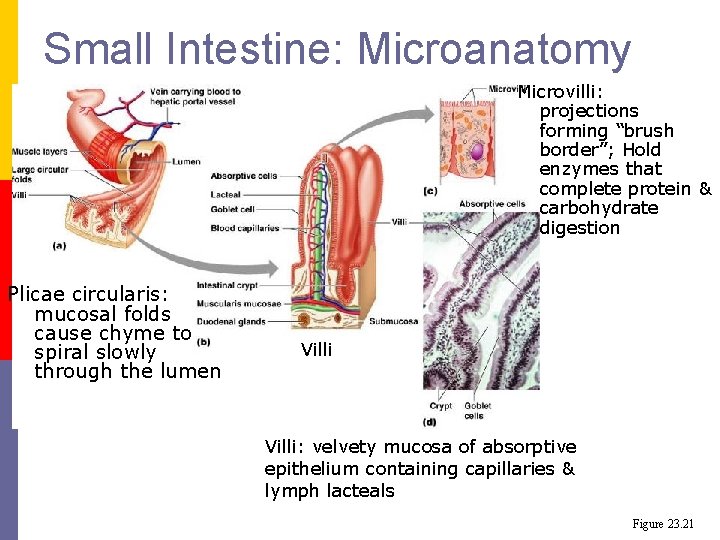
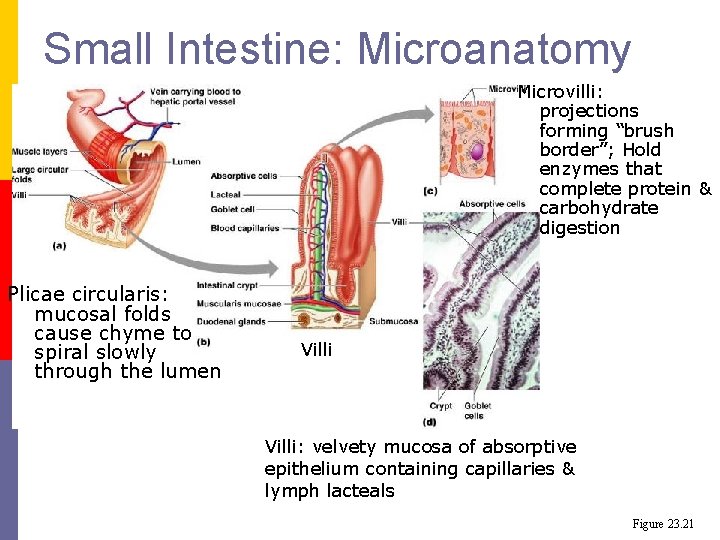
Small Intestine: Microanatomy Microvilli: projections forming “brush border”; Hold enzymes that complete protein & carbohydrate digestion Plicae circularis: mucosal folds cause chyme to spiral slowly through the lumen Villi: velvety mucosa of absorptive epithelium containing capillaries & lymph lacteals Figure 23. 21
Small intestine Wall p Cell types: n n p p Mostly absorptive cells Goblet (mucous) cells increase in number as the small intestine progresses Enteroendocrine cells T Lymphocytes Intestinal crypts with cells that secrete intestinal juice & contain Paneth cells that secrete protective lysozyme (antibacterial) Peyer’s Patches: lymphoid follicle in submucosa
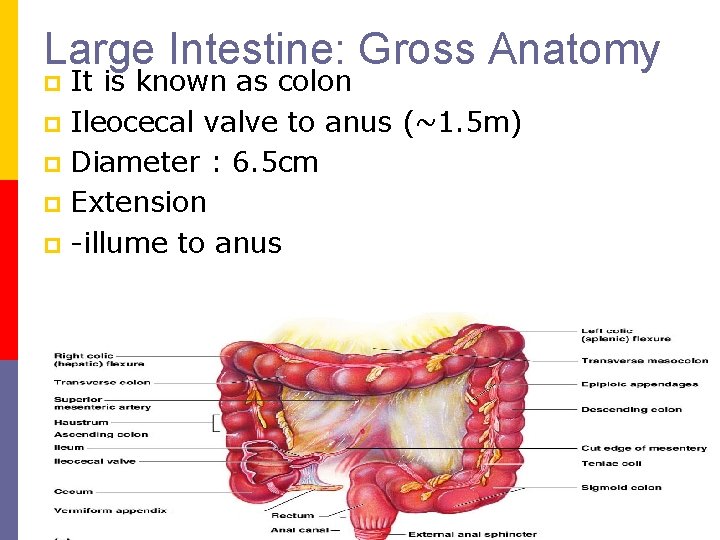
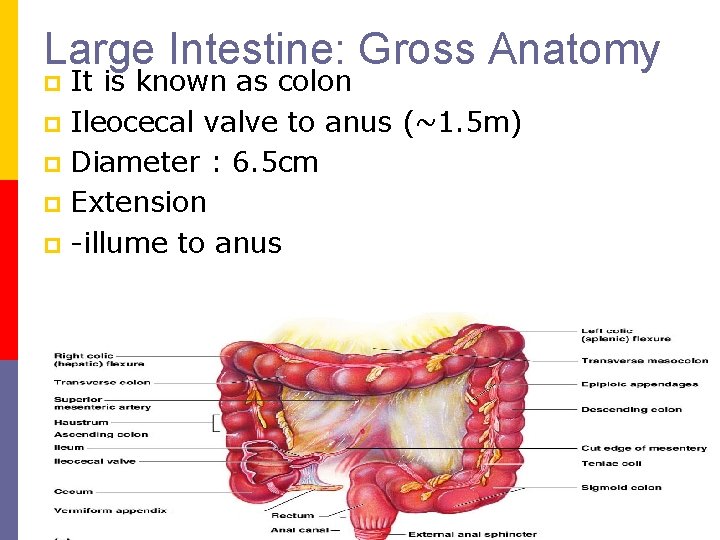
Large Intestine: Gross Anatomy It is known as colon p Ileocecal valve to anus (~1. 5 m) p Diameter : 6. 5 cm p Extension p illume to anus p

p p p Cecum: blind pouch (below ileocecal valve) Appendix: attached to cecum (lymphoid) Colon: ascending, transverse, descending, sigmoid n p p Transverse colon & sigmoid colon are intraperitoneal; anchored by mesentery. The rest of the colon is retroperitoneal Rectum Anal canal
Function of large intestine absorption of water , electrolyte and vitamins. p Act as a temporary reservoir of faeces. p Formation of faeces. p Excretion of faeces (defication). p The goblet cells form mucus which lubricates the faeces. p Hastral churning , peristalsis drive the content of the colon to the rectum. p
Large intestine is heavily colonize by bacteria (E. coli, streptococcus faecalis) p Bacteria in large intestine converts protein to amino acids and helps in the synthesis of vit k and folic acid. p
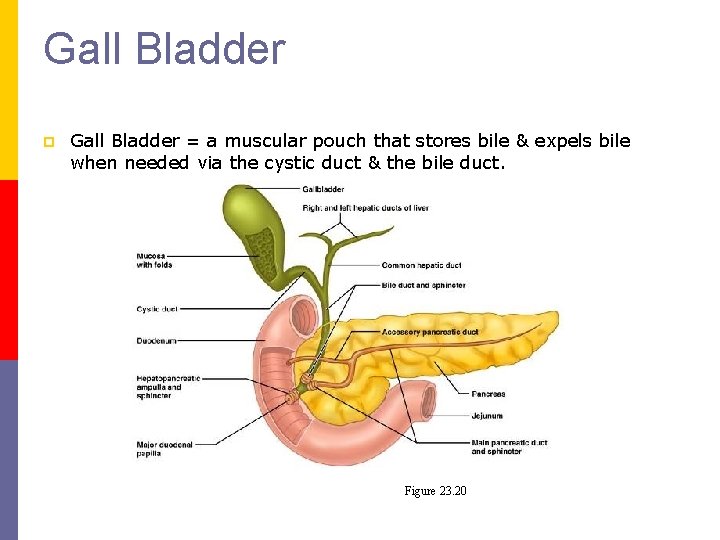
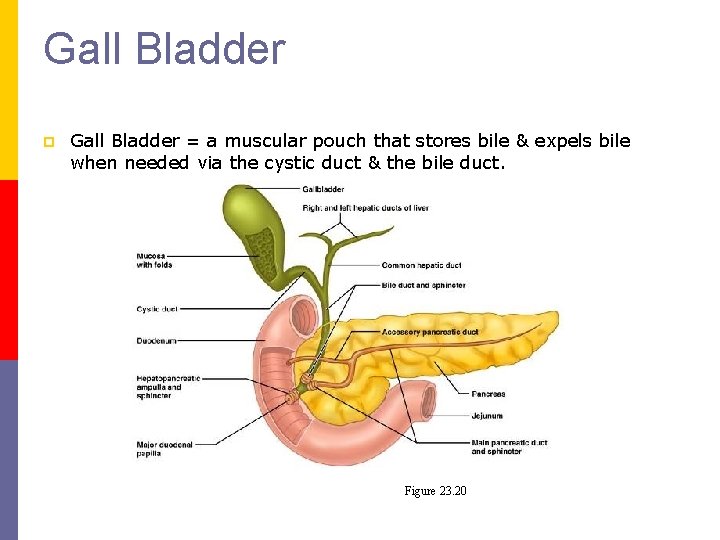
Gall Bladder p Gall Bladder = a muscular pouch that stores bile & expels bile when needed via the cystic duct & the bile duct. Figure 23. 20
Liver & Gall Bladder p p The gallbladder is a 4 inch long, pear shaped organ found under the liver in the upper right region of the abdomen. It stores bile, a compound produced by the liver to digest fat, and helps the body absorb fat soluble vitamins and nutrients. The gallbladder is a pear-shaped, hollow structure located under the liver and on the right side of the abdomen. Its primary function is to store and concentrate bile, a yellow-brown digestive enzyme produced by the liver. The gallbladder is part of the biliary tract.
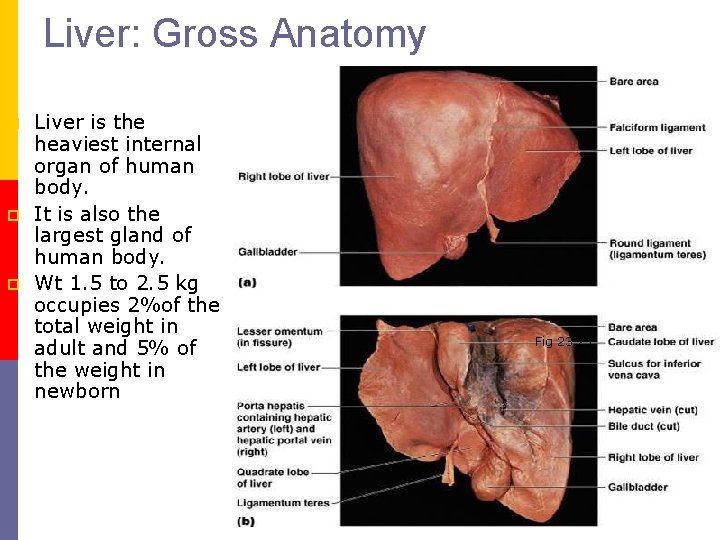
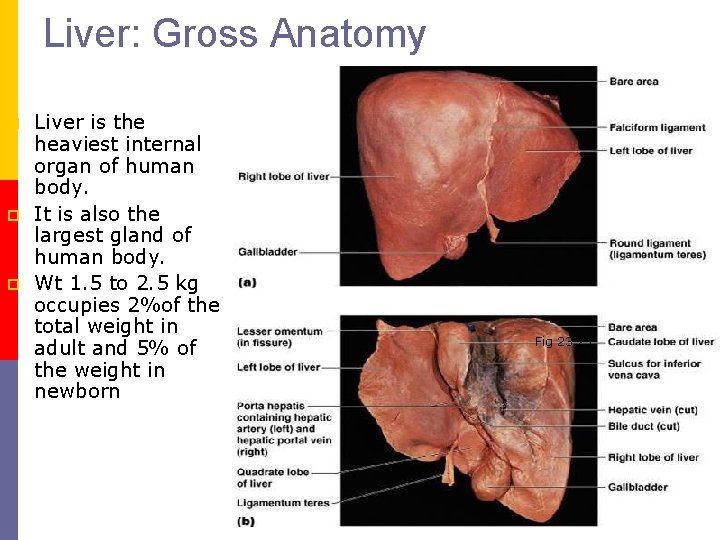
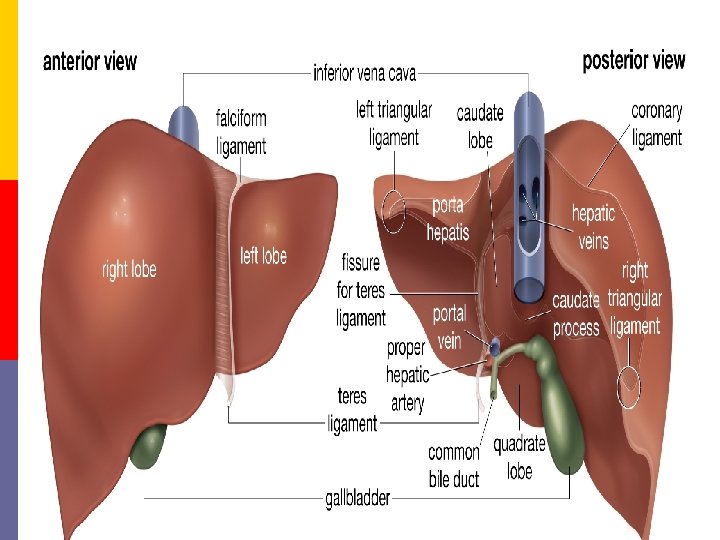
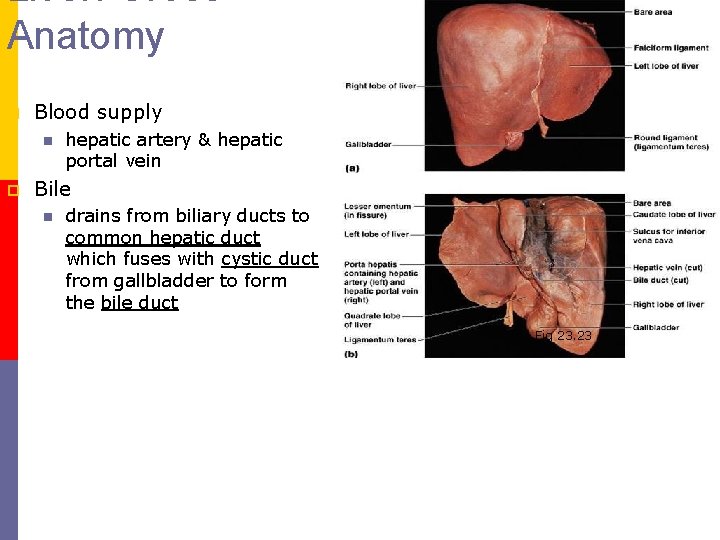
Liver: Gross Anatomy p p p Liver is the heaviest internal organ of human body. It is also the largest gland of human body. Wt 1. 5 to 2. 5 kg occupies 2%of the total weight in adult and 5% of the weight in newborn Fig 23. 23
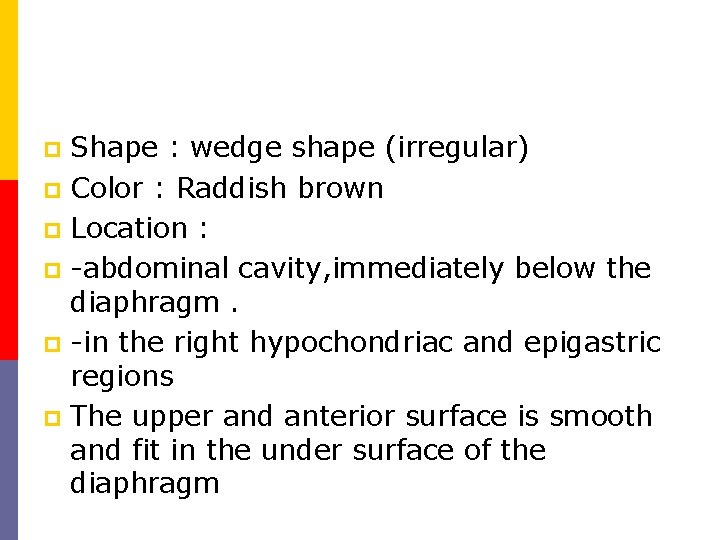
Shape : wedge shape (irregular) p Color : Raddish brown p Location : p abdominal cavity, immediately below the diaphragm. p in the right hypochondriac and epigastric regions p The upper and anterior surface is smooth and fit in the under surface of the diaphragm p
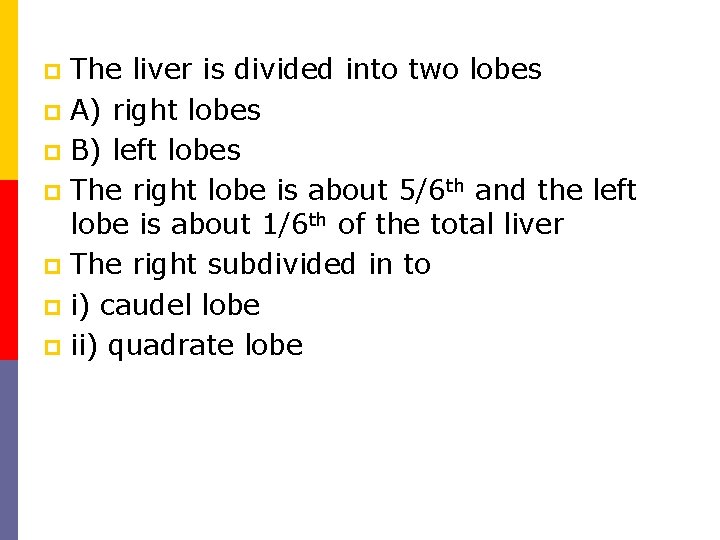
The liver is divided into two lobes p A) right lobes p B) left lobes p The right lobe is about 5/6 th and the left lobe is about 1/6 th of the total liver p The right subdivided in to p i) caudel lobe p ii) quadrate lobe p
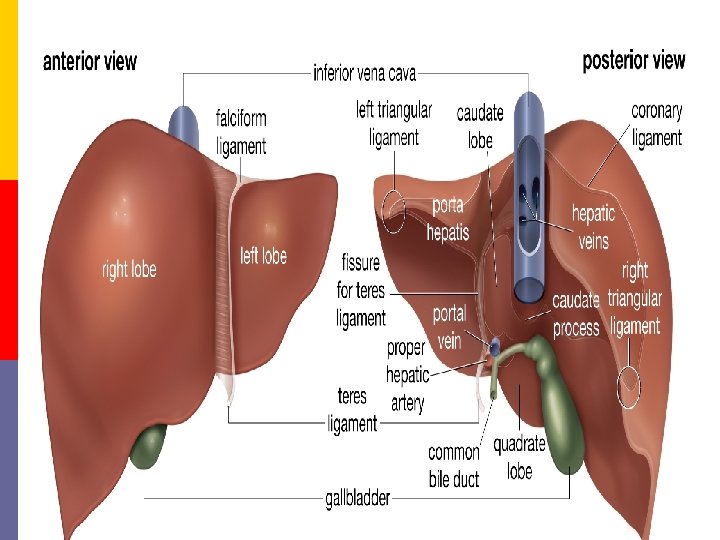
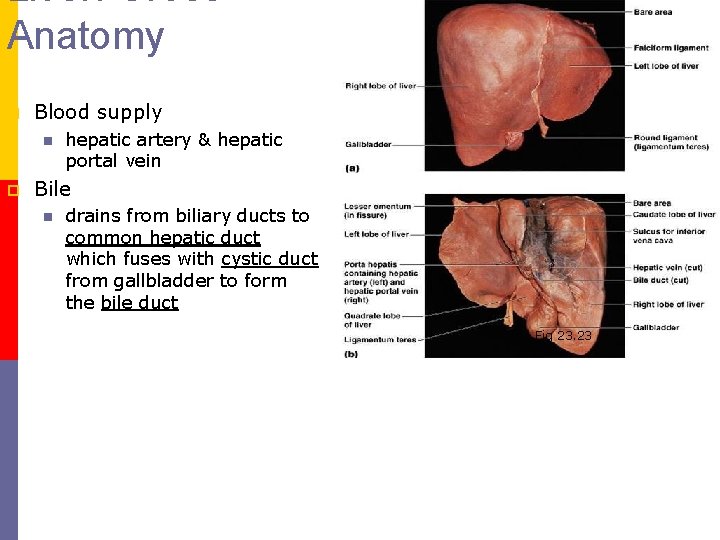
Liver: Gross Anatomy p Blood supply n p hepatic artery & hepatic portal vein Bile n drains from biliary ducts to common hepatic duct which fuses with cystic duct from gallbladder to form the bile duct Fig 23. 23
Liver & Gall Bladder p Composition of bile: Alkaline solution: Bile salts, bile pigments, cholesterol, fats & phospholipids n Bile salts & phospholipids participate in fat absorption
Liver & Gall Bladder p p Bile salts are conserved by enterohepatic circulation n Reabsorbed in the ileum n Return to Liver in hepatic portal blood n Re secreted by the Liver Bile pigments & bilirubin break down to urobilin then stercobilin
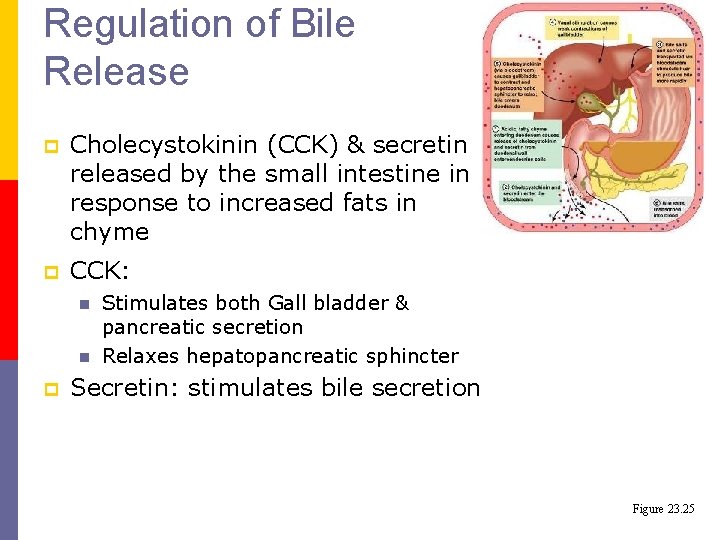
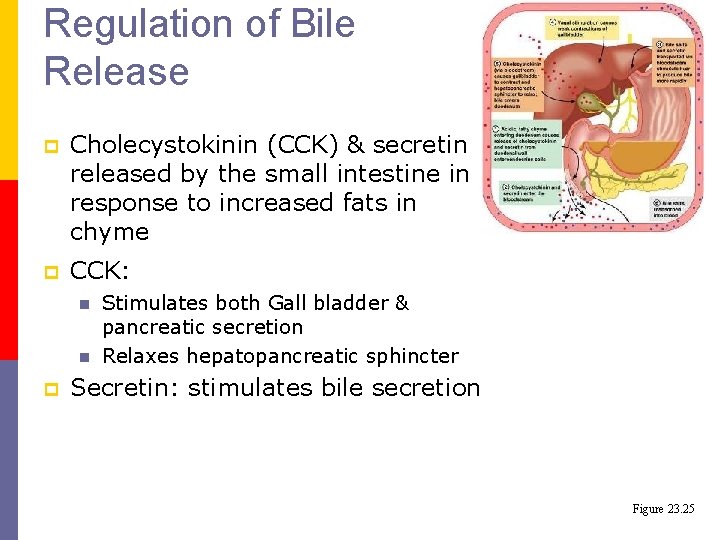
Regulation of Bile Release p p Cholecystokinin (CCK) & secretin released by the small intestine in response to increased fats in chyme CCK: n n p Stimulates both Gall bladder & pancreatic secretion Relaxes hepatopancreatic sphincter Secretin: stimulates bile secretion Figure 23. 25
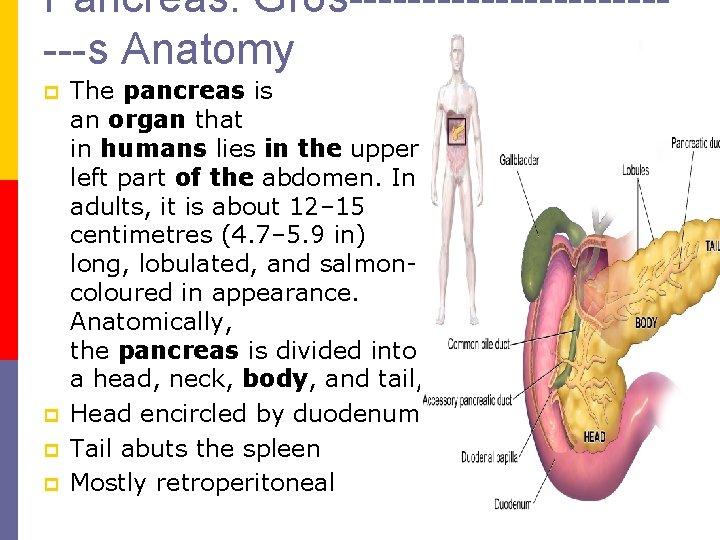
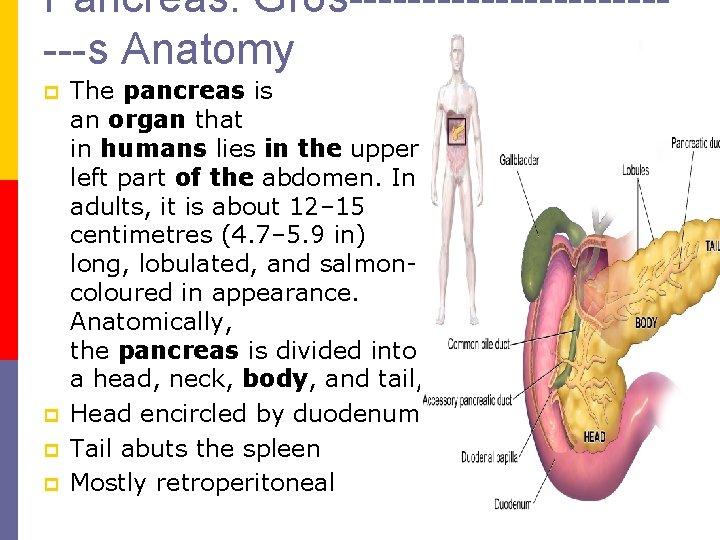
Pancreas: Gros------------s Anatomy p p The pancreas is an organ that in humans lies in the upper left part of the abdomen. In adults, it is about 12– 15 centimetres (4. 7– 5. 9 in) long, lobulated, and salmon coloured in appearance. Anatomically, the pancreas is divided into a head, neck, body, and tail, Head encircled by duodenum Tail abuts the spleen Mostly retroperitoneal
Pancreatic Juice p Pancreatic Juice: Alkaline, watery, contains enzymes & electrolytes
Pancreatic Juice p p Proteolytic enzymes are released as inactive forms then are activated in the duodenum n Trypsinogen g Trypsin by the brush border enzyme enterokinase n Trypsin activates precursors to form carboxypeptidase & chymotrypsin Amylase, lipase, & nuclease are released in their active forms
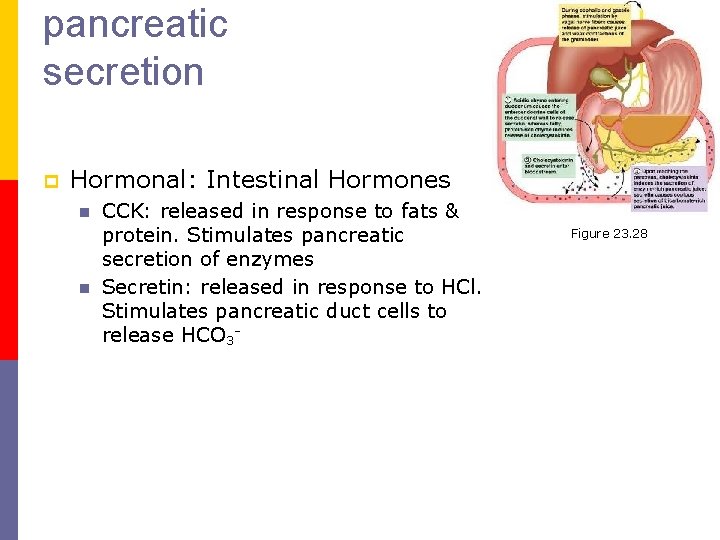
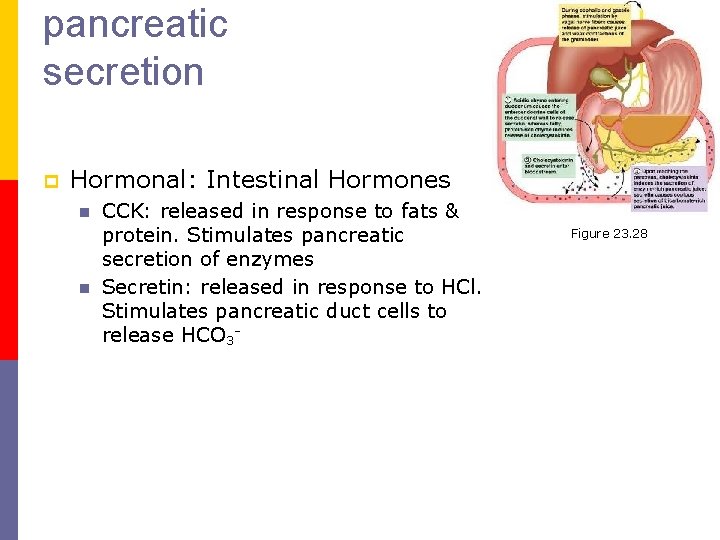
pancreatic secretion p Hormonal: Intestinal Hormones n n CCK: released in response to fats & protein. Stimulates pancreatic secretion of enzymes Secretin: released in response to HCl. Stimulates pancreatic duct cells to release HCO 3 Figure 23. 28
Digestive Processes : Small Intestine p Optimal digestion requires adequate motility & control of chemical composition
DEGLUTITON p The movement of food from the mouth into the stomach is achieved by the act of deglutition or swallowing. p Deglutition is facilitated by the secretion of saliva and mucous and involves mouth, pharynx and esophagus
It is initiated voluntary and completed involuntary. p It involves the following steps. The mouth is closed The voluntary muscle of the tongue and cheek pus the bolus in to the pharynx. The muscle of the pharynx are stimulated and this response is coordinated to medulla oblongata. Contraction of muscle of the pharynx propels the bolus into the oesophagus. The presence of bolus in the oesophagus stimulated a wave of peristalsis which propels the bolus to the stomach. p
The passage of solid or semisolid food from mouth to stomach takes 4 8 second p Very soft food and drink pass through in about 1 sec. p
Vomiting It is also called emesis p Vomiting is the forcible expulsion of upper GI content through the mouth. p The strong stimuli for vomiting are irritation and distension of stomach. p Nerve impulse are transmitted to the vomiting center in the medulla oblongata. p The returning impulses pass to the upper GI organ , diaphragm and abdominal muscles. p
p Vomiting involves the squeezing of the stomach between the diaphragm and abdominal muscle and expelling the contents through the mouth.
DAEFECTION It is the final act of digestion p It is the process of expelling faeces from the anal canal through the anus. p
Mechanism of daefecation Mass peristaltic movement propel the faecel matter from the pelvic colon to the rectum p This action is usually precipated by the entry of food into the stomach. p The entry of faeces into the rectum distends the wall of the rectum and causes the generation of impulses. p In the infant daefecation occurs by the reflexes (involuntary )action. p
In the age of 2 nd and 3 rd year of life the ability to override daefection reflexes develops. p The impulses pass along the parasympathic nerves to the brain where they arouse the conscious sensation of the desire to daefacate. p Under appropriate situation , the external anal spinture is relaxed voluntary and daefecation occur. p When the situation is not appropriate , daefection may be voluntarily postponed. p
When daefecation voluntarily postponed the felling of fullness and need to daefecate tends to fade until next mass movement occur and the reflex is initated again. p Repeated suppression of the reflex may led to constiption p Daefecation involves the following action relaxation of anal sphincters Contraction of muscles of rectum and pelvic floor Raising of intraabdominal pressure (by holding the breath and contracting the diaphragm and abdominal muscles ). p
Digestive Processes : Small Intestine p p. H: acidic chyme must be buffered to allow proper enzyme activity Osmolality: chyme is hypertonic & would pull H 2 O out of circulation; thus chyme is released in small amounts Liver & pancreatic function are required for appropriate delivery of bile salts & enzymes to the small intestine
Digestive Processes : Small Intestine p p Segmentation: moves intestinal contents back & forth to mix Duodenal rhythm for segmentation is greater than the rhythm in the ileum. n Contents move toward the ileum.
Digestive Processes : Small Intestine p p After most digestion has occurred, Peristalsis begins sweeping from duodenum distally n p Occurs in series with each peristaltic wave, originating more distally (migrating mobility complex) Ileocecal valve (sphincter) is relaxed by neural (gastroileal reflex) impulses from the stomach & hormonal (gastrin) secretion by the stomach
Chemical Digestion of Specific Food Groups p Chemical Digestion: Mechanism n n Catabolic process: break down of food molecules to monomeric form that can be absorbed Enzymes break molecules by hydrolysis (Adding H 2 O into a molecular bond)
Chemical Digestion: Carbohydrates p Carbohydrates (CHO): complex sugars are broken down to simple sugars (monomers) n Simple sugars (monosaccharides): glucose, fructose, & galactose can be absorbed n Disaccharides (not absorbed): sucrose, maltose, & lactose are hydrolyzed by sucrase, maltase, & lactase (brush border enzymes) into monosaccharides
Chemical Digestion: Carbohydrates p Polysaccharides: broken down to smaller & smaller oligosaccharides n n Salivary amylase: breaks starch into 2 8 linked monosaccharide Salivary amylase is denatured by HCl in the stomach
Chemical Digestion: Carbohydrates p Polysaccharides (cont) n n Pancreatic amylase: continues breakdown (mostly to maltose) Brush border enzymes act on oligosaccharides of more than 3 simple sugars (brush border) Sucrose, maltose & lactose are broken down by specific brush border enzymes (sucrase, maltase, & lactase) Monosaccharides are absorbed.
Chemical Digestion: Proteins p Proteins: broken down to amino acid monomers. Begins in the stomach. n n n Pepsinogen is activated to pepsin by HCL Pepsin: cleaves peptide bonds associated with tyrosine & phenylalanine forming polypeptides (+ a few amino acids). p Pepsin is inactivated by increased p. H in the duodenum Trypsin & chymotrypsin: pancreatic enzymes that further breakdown polypeptides.
Chemical Digestion: Proteins p Proteins (cont): n Carboxypeptidase (pancreatic & brush border enzyme): p Splits off single amino acid from the end of polypeptide chain that contains the carboxyl group n Aminopeptidase & dipeptidase (brush border n enzymes) release final amino acid monomers Figure 23. 34
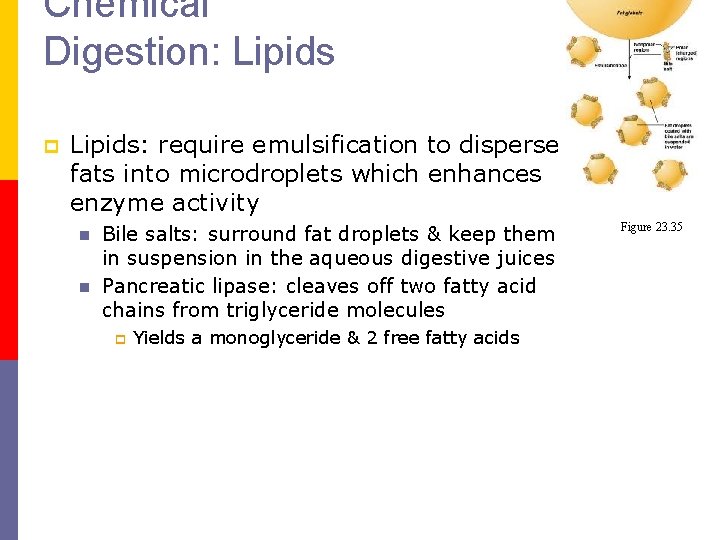
Chemical Digestion: Lipids p Lipids: require emulsification to disperse fats into microdroplets which enhances enzyme activity n n Bile salts: surround fat droplets & keep them in suspension in the aqueous digestive juices Pancreatic lipase: cleaves off two fatty acid chains from triglyceride molecules p Yields a monoglyceride & 2 free fatty acids Figure 23. 35
Chemical Digestion: Nucleic acids p Nucleic acids: small amounts occur in the diet n n Pancreatic nucleases: Hydrolyze nucleic acids to nucleotide monomers Nucleosidases & phosphatases (brush border) break down nucleotides
Absorption: Small Intestine p p Most nutrients are absorbed from chyme prior to the ileum (ileum primarily reabsorbs bile salts) Most nutrients cross the mucosa by active transport. n n Some products of lipid digestion are absorbed by diffusion. CHO, amino acids & nucleic acid remnants are actively transported into mucosal cells & then enter capillary blood
Absorption: Small Intestine (Fats) p Monoglycerides & free fatty acids are associated with bile salts & lecithin (a phospholipid) to form micelles n n n Micelles diffuse between microvilli The lipid substances leave the micelles & diffuse across the PM of microvilli Inside the intestinal epithelial cell, the components are reassembled into triglycerides
Absorption: Small Intestine (Fats) p Monoglycerides (cont) n n n Triglycerides are then packaged with cholesterol & phospholipids into chylomicrons Chylomicrons are exocytosed & diffuse to lymphatic lacteals to eventually be placed into blood by the lymphatic system Chylomicrons in the blood are hydrolyzed by lipoprotein lipase to free fatty acids & glycerol prior to tissue absorption § Fig. 23. 36
Absorption: Small Intestine p Vitamins n n n Some Vit. K & B complex vitamins are absorbed in the large intestine Dietary vitamins are absorbed in the small intestine Fat soluble vitamins (A, D, E, K) dissolve in dietary fats & are absorbed after being incorporated into micelles
Absorption: Small Intestine p p p Electrolytes: most ions are actively absorbed throughout small intestine Na+ is coupled to absorption of glucose & amino acids (cotransport) Cl actively transported into cells; exchange for HCO 3
Absorption: Small Intestine p p p K diffuses into the cells Iron is transported into cells & bound to ferritin Ca 2+ absorption regulated by blood Ca 2+ levels & Vit D p ( Vit D is a required cofactor for Ca 2+ absorption)
Absorption: Small Intestine p Water moves freely in both directions across the mucosa n n Active transport of solutes create an osmotic gradient & H 2 O follows H 2 O movement changes solute concentrations & effects absorption of substances that move by diffusion
Absorption: Small Intestine p Malabsorption: can result from n n n Disruption of secretion Mucosal damage Reduction of absorptive surface area
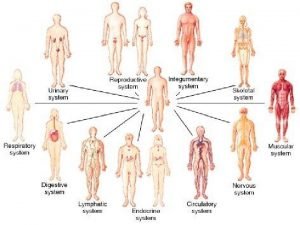
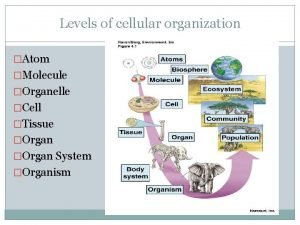
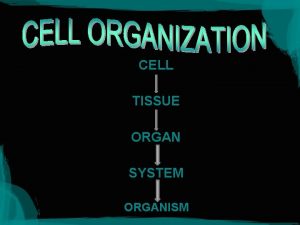
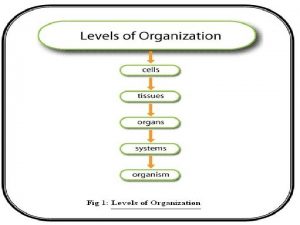
 Cell tissue organ organ system organism
Cell tissue organ organ system organism Tissue are grouped together to form various
Tissue are grouped together to form various Organ and organ system
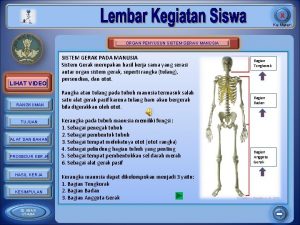
Organ and organ system Organ penyusun sistem gerak
Organ penyusun sistem gerak Tractus respiratorius
Tractus respiratorius Organ penyusun sistem transportasi
Organ penyusun sistem transportasi Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Third gender full body parts pictures
Third gender full body parts pictures 8 organ systems
8 organ systems Divisions of anatomy
Divisions of anatomy Muscle belly
Muscle belly John j. tyson
John j. tyson Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Gastrointestinal tract
Gastrointestinal tract Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Gastrointestinal hormones
Gastrointestinal hormones Sigid djuniawan
Sigid djuniawan Docimasia gastrointestinal
Docimasia gastrointestinal Gastrik inhibitör polipeptid
Gastrik inhibitör polipeptid Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nutrition focused physical examination
Nutrition focused physical examination Cloaca
Cloaca Composition of stomach
Composition of stomach Motilidad gastrointestinal
Motilidad gastrointestinal Dumping syndrome signs
Dumping syndrome signs Divisao anatomica do estomago
Divisao anatomica do estomago Anatomia rim
Anatomia rim Ashraf radwan
Ashraf radwan Oral yol
Oral yol Gastrointestinal structure
Gastrointestinal structure Peristalsis and segmentation
Peristalsis and segmentation Metformin and constipation
Metformin and constipation Alimentary canal diagram
Alimentary canal diagram Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Borborygmi
Borborygmi The human bodywhat is an organ system?
The human bodywhat is an organ system? Atom molecule cell
Atom molecule cell Mouth function in digestive system
Mouth function in digestive system Base of prostate gland
Base of prostate gland Plant organ
Plant organ Level of organization organ system
Level of organization organ system Accessory organs
Accessory organs Organ system examples
Organ system examples Organ system
Organ system Is a heart an organ system
Is a heart an organ system A pathogen passing from a mother to her fetus could cause *
A pathogen passing from a mother to her fetus could cause * Organ system definition
Organ system definition Organ system
Organ system Organ system
Organ system Identify the structure
Identify the structure Renal vein
Renal vein Cell tissue organ system body
Cell tissue organ system body Which is an accessory organ of the digestive system
Which is an accessory organ of the digestive system Which is an accessory organ of the digestive system
Which is an accessory organ of the digestive system Decision support systems and intelligent systems
Decision support systems and intelligent systems Principles of complex systems for systems engineering
Principles of complex systems for systems engineering Embedded systems vs cyber physical systems
Embedded systems vs cyber physical systems Elegant systems
Elegant systems Is the earth an open or closed system?
Is the earth an open or closed system? Digestive system respiratory system and circulatory system
Digestive system respiratory system and circulatory system Cause of splenomegaly in malaria
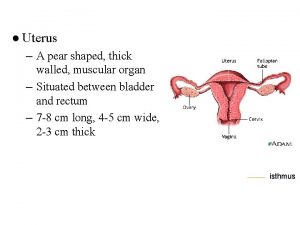
Cause of splenomegaly in malaria Uterus pear shaped
Uterus pear shaped Organ niezespolonej administracji rządowej w województwie
Organ niezespolonej administracji rządowej w województwie Hepar anatomy
Hepar anatomy Largest lymphoid organ
Largest lymphoid organ Peta konsep tumbuhan
Peta konsep tumbuhan Skin is the largest organ
Skin is the largest organ Spermatogonii
Spermatogonii Organ limfatik primer dan sekunder
Organ limfatik primer dan sekunder Penis od kornjace
Penis od kornjace Subincrengatura
Subincrengatura Paratiroid
Paratiroid Polypoid zooids
Polypoid zooids Fetomaternal organ
Fetomaternal organ Pielea este organ
Pielea este organ Organ penyerap air
Organ penyerap air Plant organ
Plant organ