Chapter 5 Integumentary System With additions from Chapter
- Slides: 56
Chapter 5 Integumentary System With additions from Chapter 4
• Skin is cool
What is the integumentary system? • Skin = cutaneous membrane or cutaneous layer • derivatives of skin • • hair nails sweat glands other glands
What does the integumentary system do? • Protects inside of body from • trauma • microbes/viruses • Changes color in response to environment • suntan/burn, blushing • Helps to cool and warm body • Prevents water loss • Makes Vitamin D • Senses environment
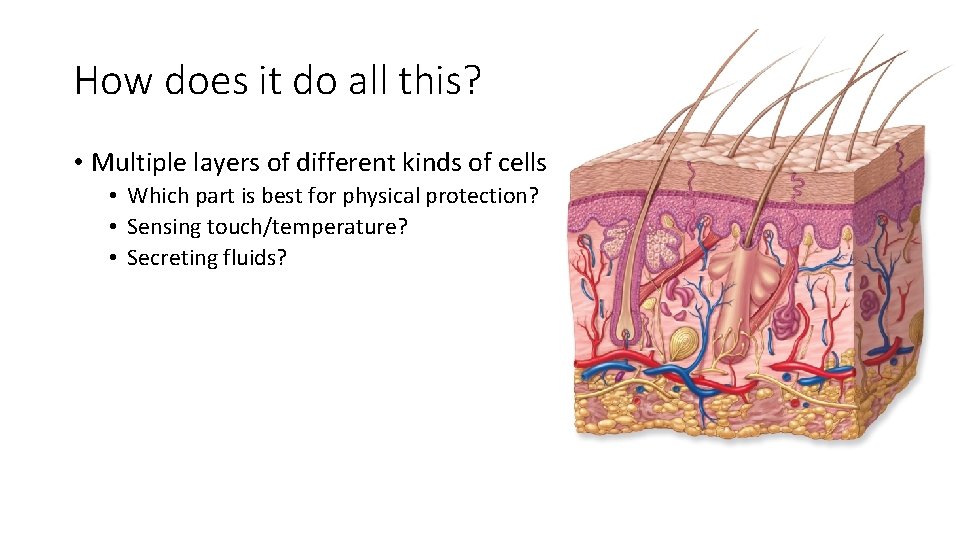
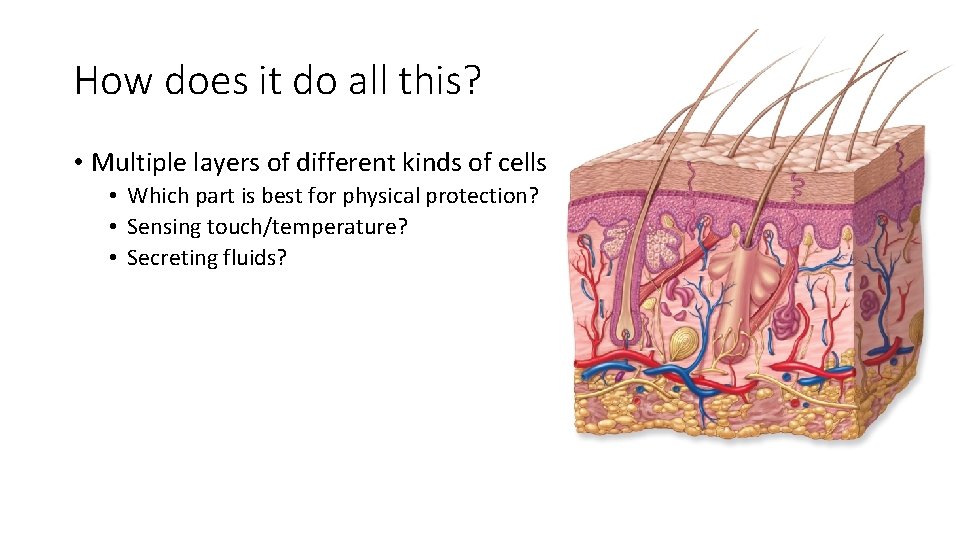
How does it do all this? • Multiple layers of different kinds of cells • Which part is best for physical protection? • Sensing touch/temperature? • Secreting fluids?
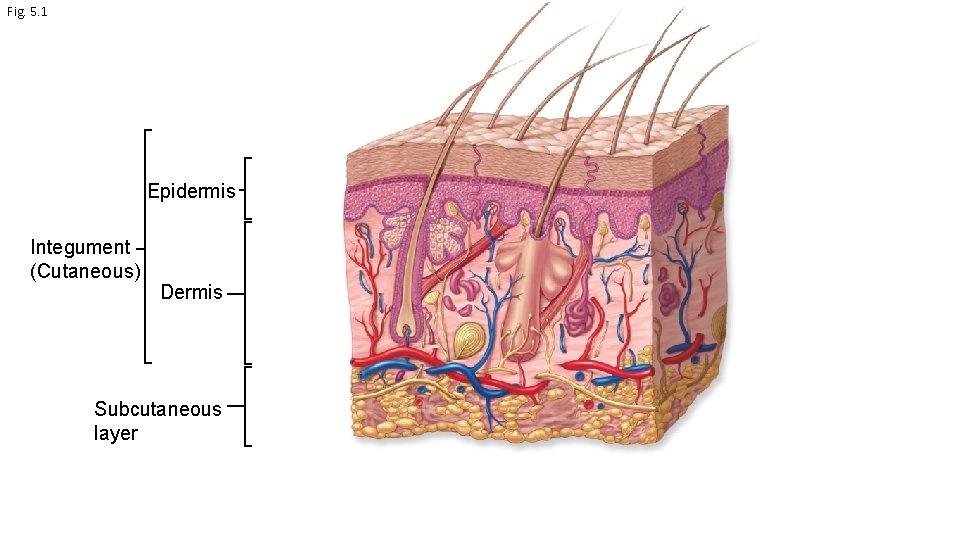
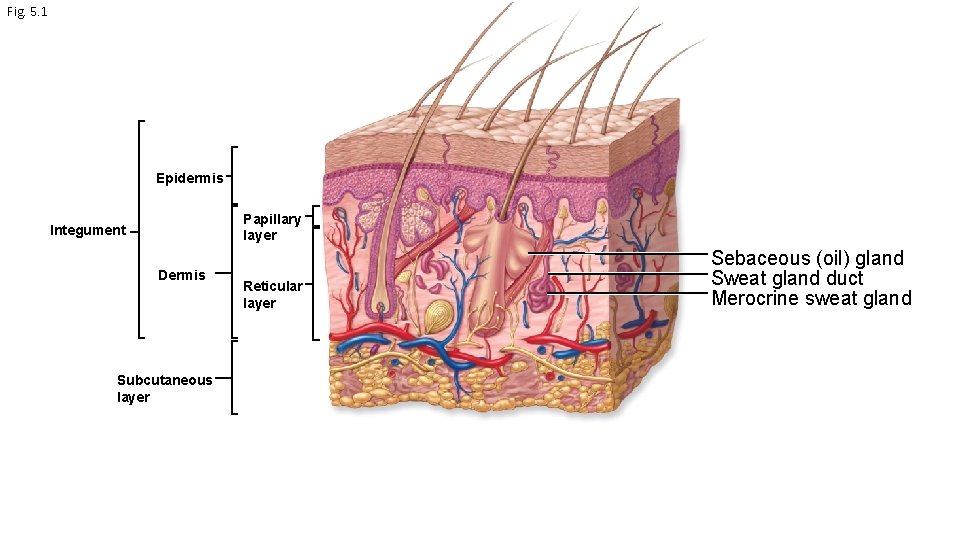
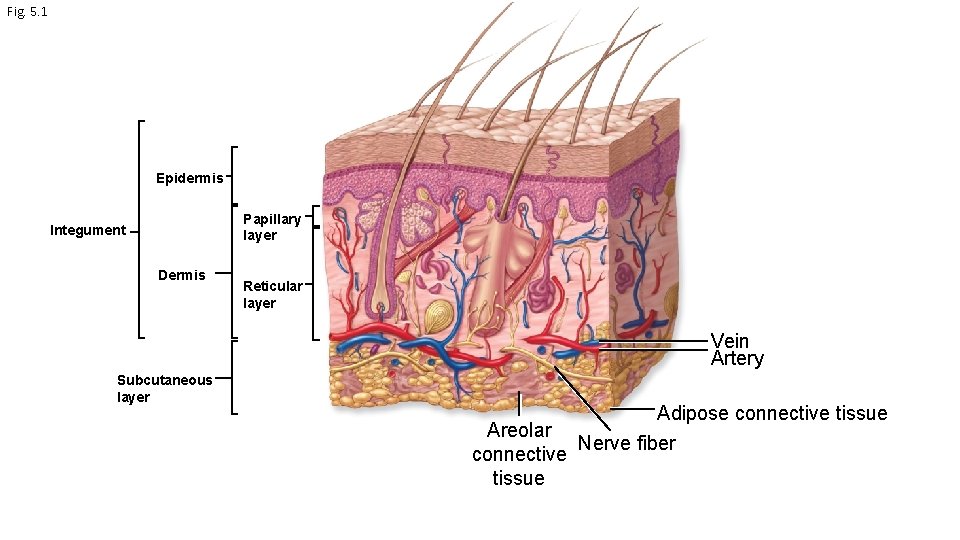
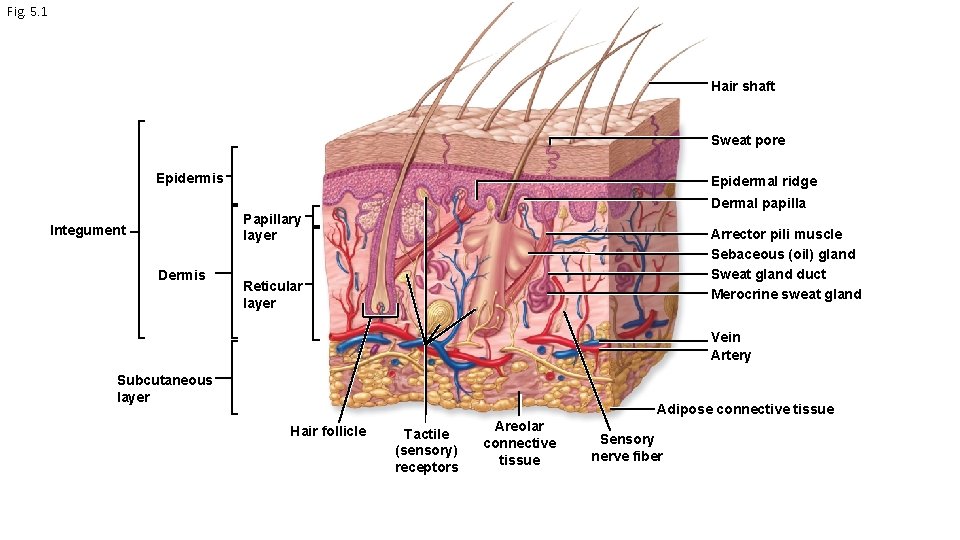
Fig. 5. 1 Epidermis Integument (Cutaneous) Dermis Subcutaneous layer
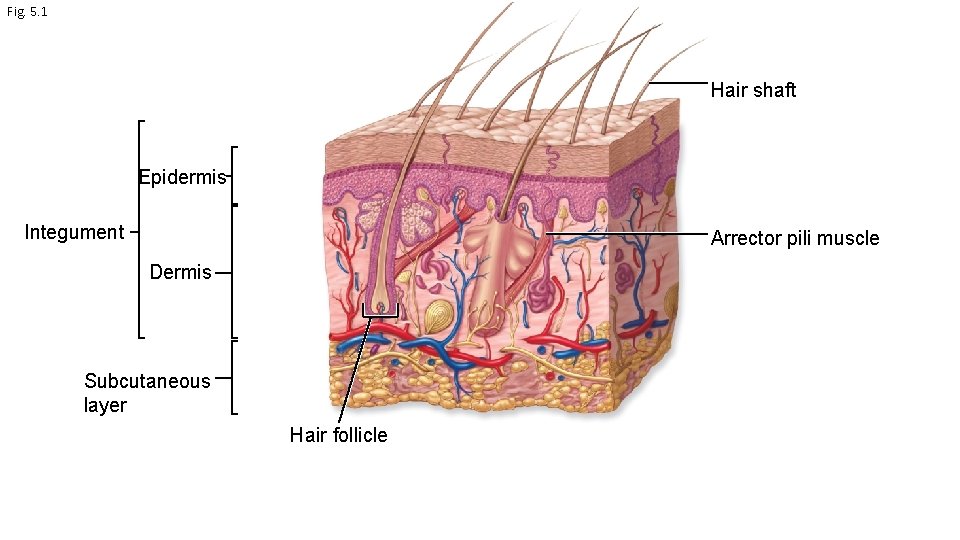
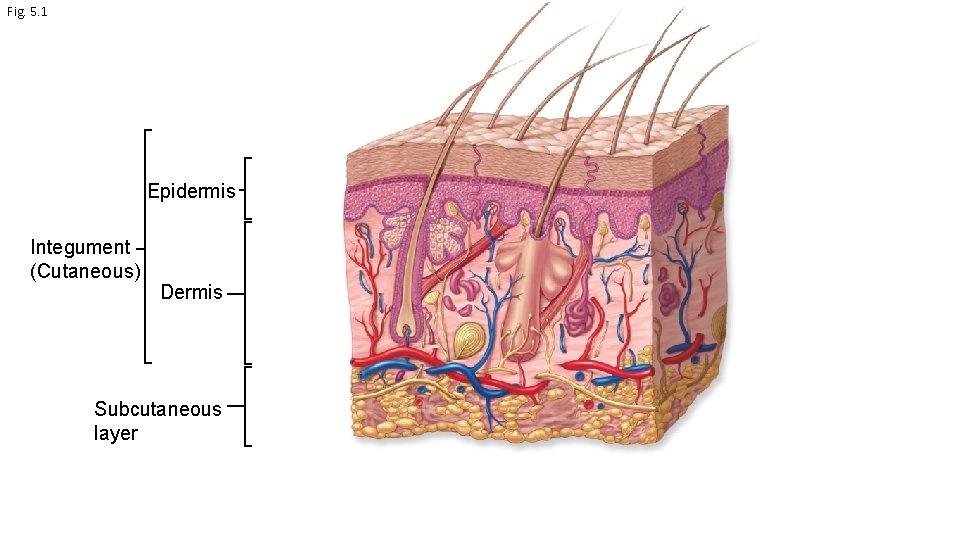
Fig. 5. 1 Hair shaft Epidermis Integument Arrector pili muscle Dermis Subcutaneous layer Hair follicle
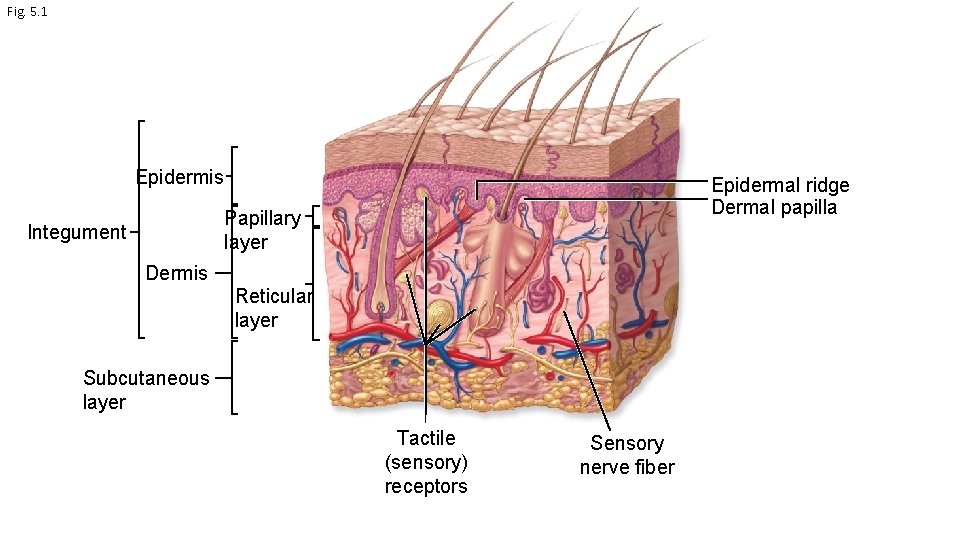
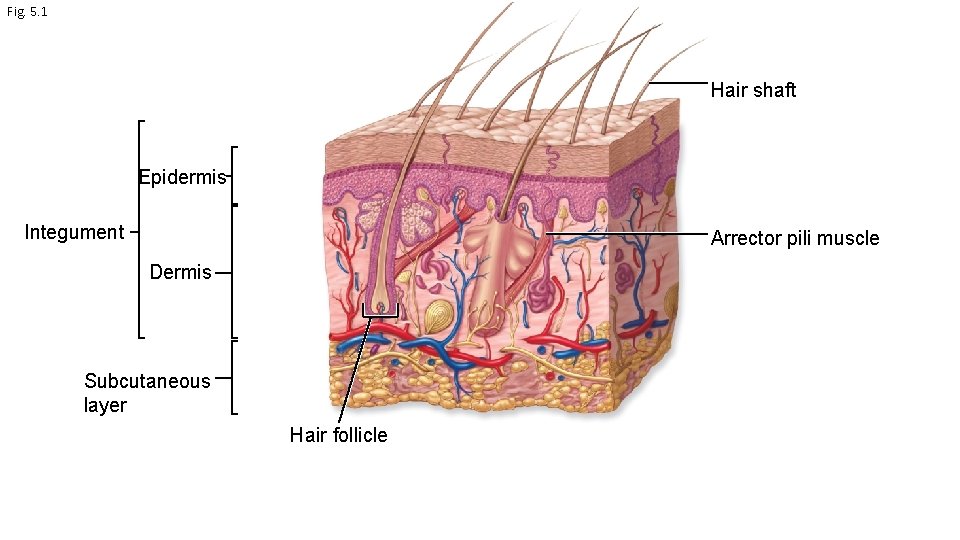
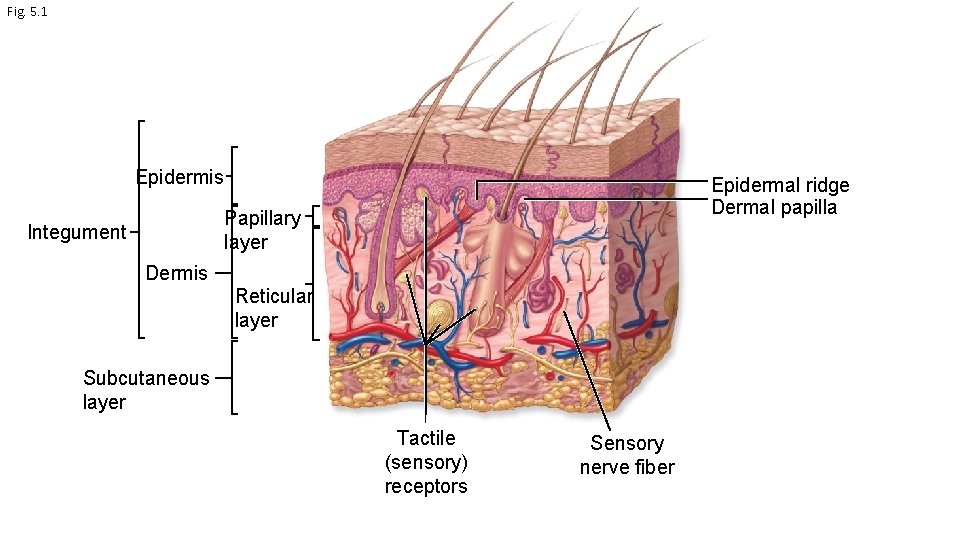
Fig. 5. 1 Epidermis Epidermal ridge Dermal papilla Papillary layer Integument Dermis Reticular layer Subcutaneous layer Tactile (sensory) receptors Sensory nerve fiber
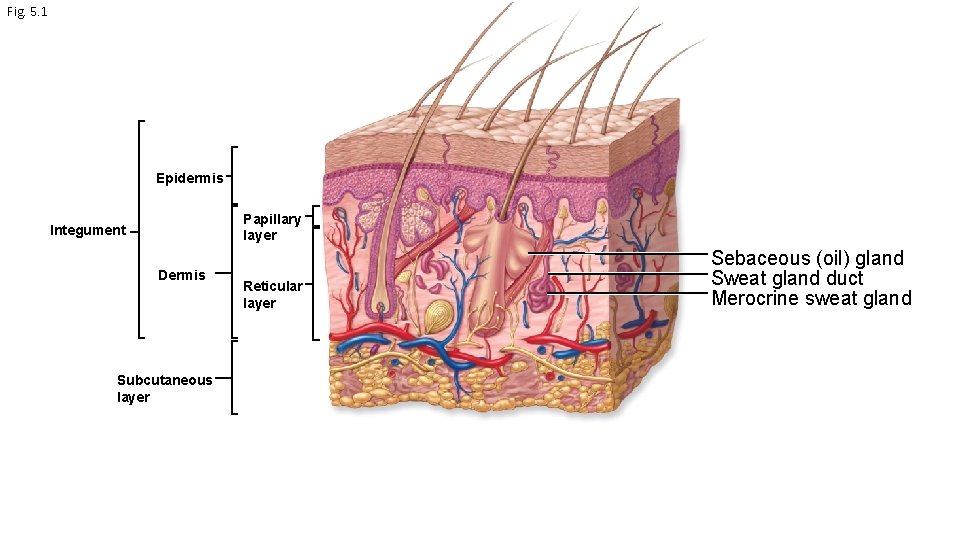
Fig. 5. 1 Epidermis Papillary layer Integument Dermis Subcutaneous layer Reticular layer Sebaceous (oil) gland Sweat gland duct Merocrine sweat gland
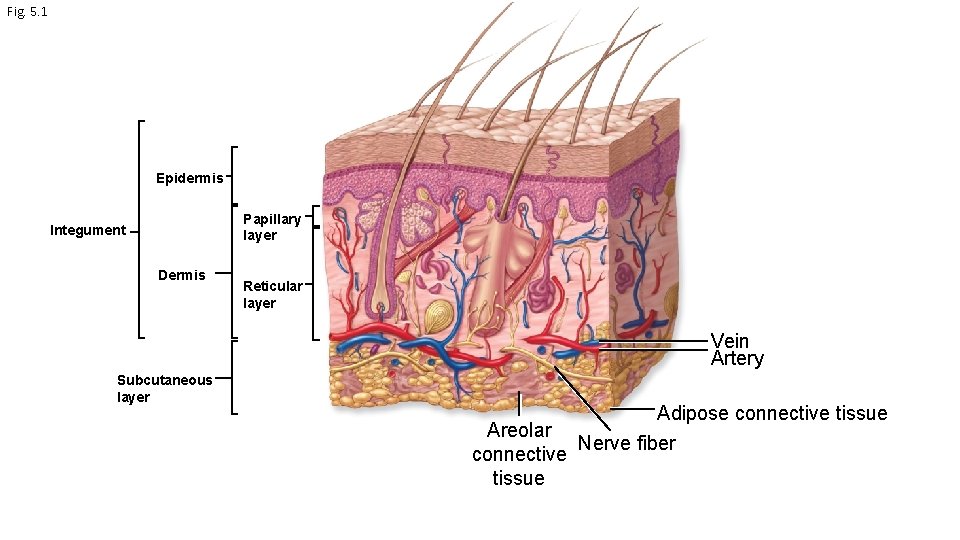
Fig. 5. 1 Epidermis Papillary layer Integument Dermis Reticular layer Vein Artery Subcutaneous layer Areolar connective tissue Adipose connective tissue Nerve fiber
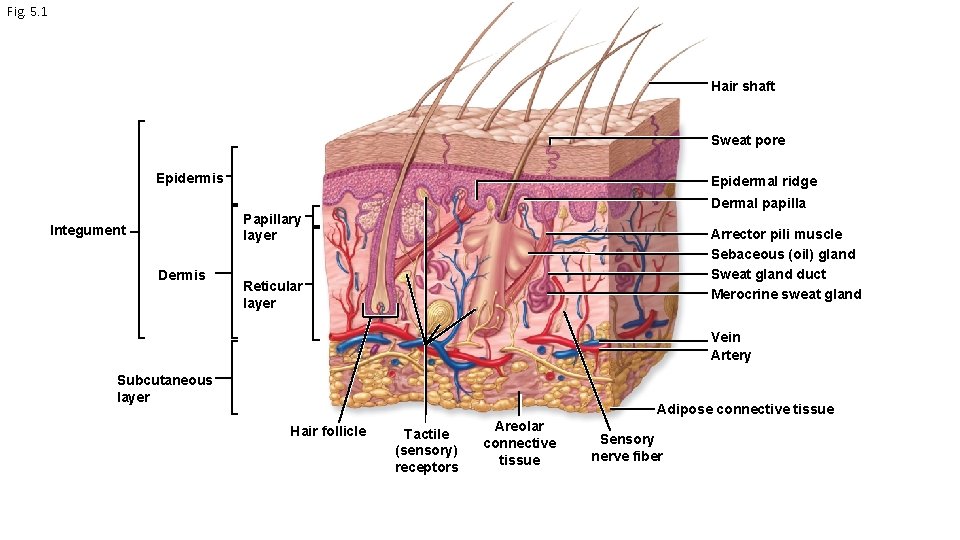
Fig. 5. 1 Hair shaft Sweat pore Epidermis Epidermal ridge Dermal papilla Papillary layer Integument Dermis Arrector pili muscle Sebaceous (oil) gland Sweat gland duct Merocrine sweat gland Reticular layer Vein Artery Subcutaneous layer Adipose connective tissue Hair follicle Tactile (sensory) receptors Areolar connective tissue Sensory nerve fiber
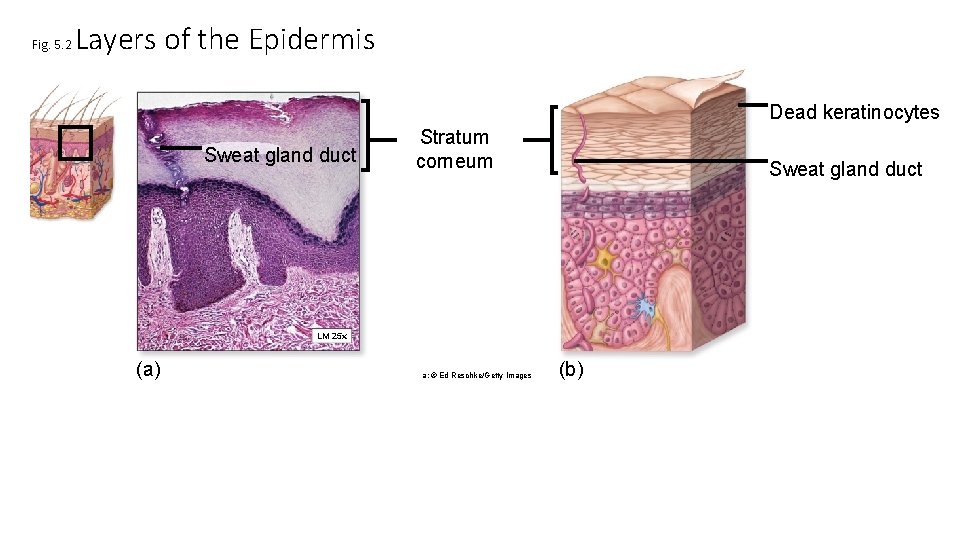
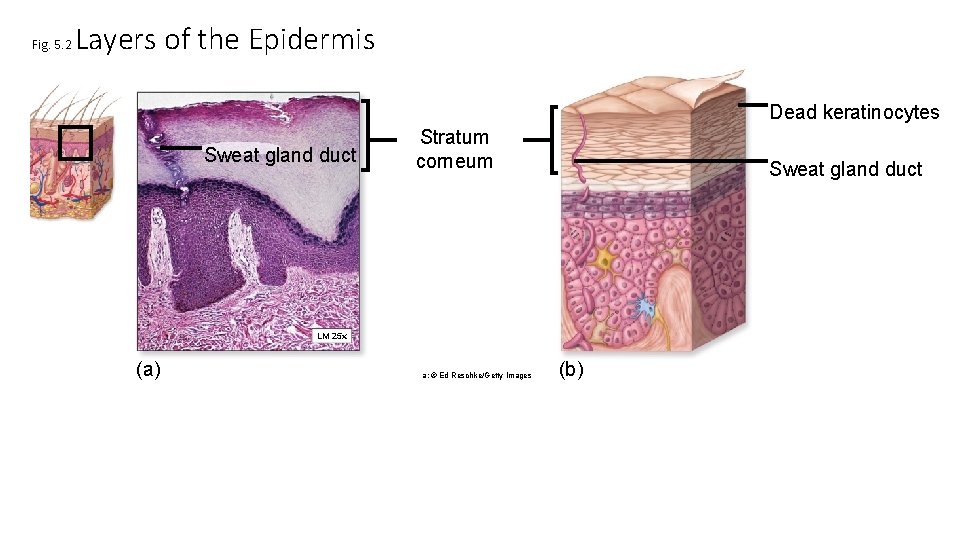
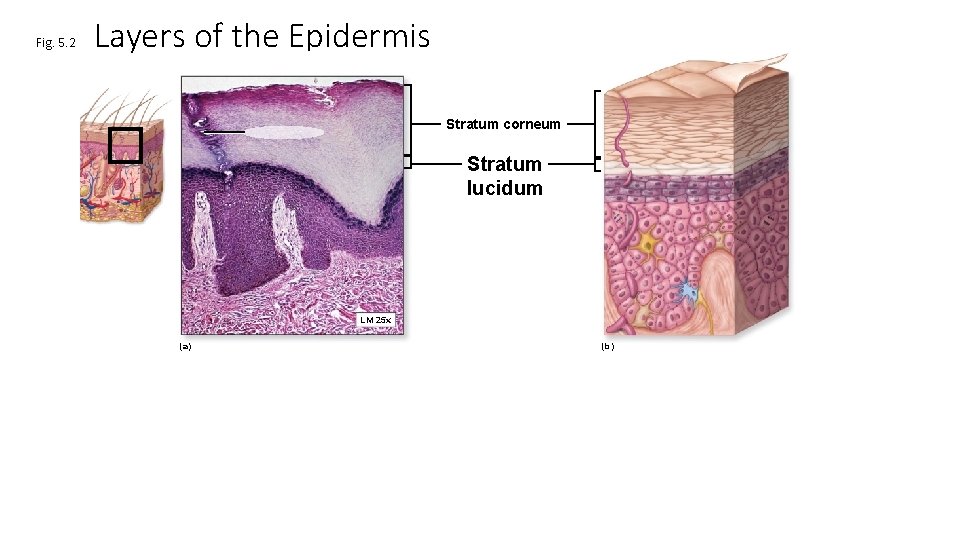
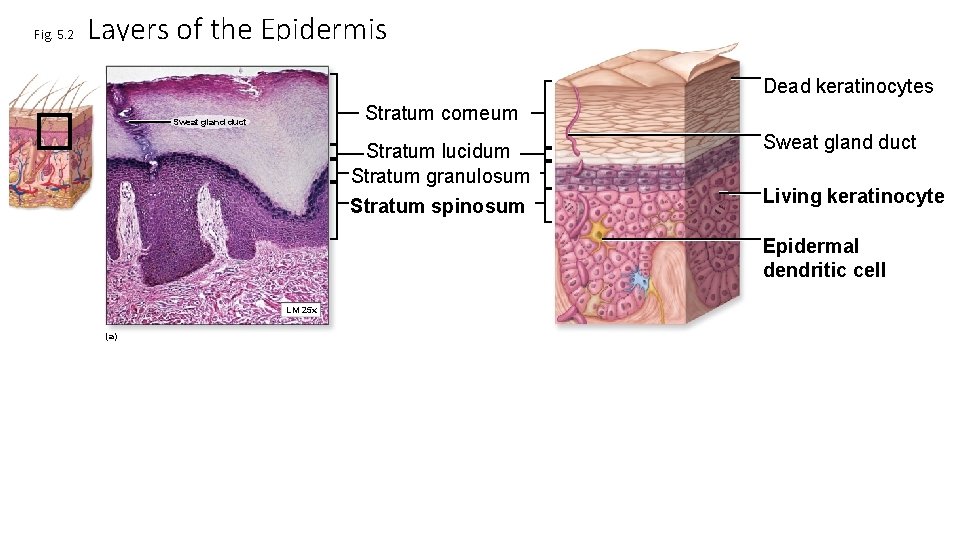
Fig. 5. 2 Layers of the Epidermis Dead keratinocytes Sweat gland duct Stratum corneum Sweat gland duct LM 25 x (a) a: © Ed Reschke/Getty Images (b)
Stratum corneum • 20 -30 layers of dead keratinocytes called corneocytes • Barrier protects live cells in lower layers • Keratinocytes make keratin • fibrous structural protein • tough and insoluble • Stratified squamous epithelium
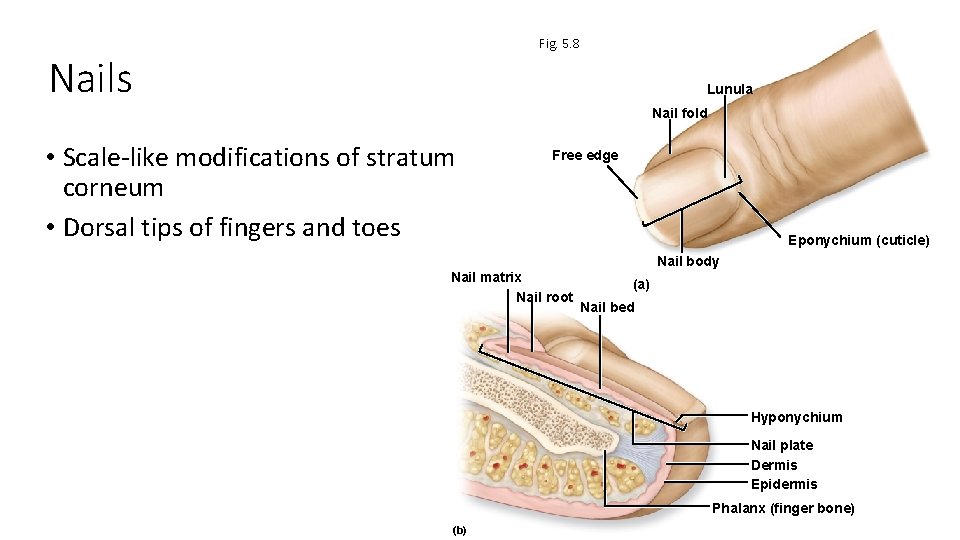
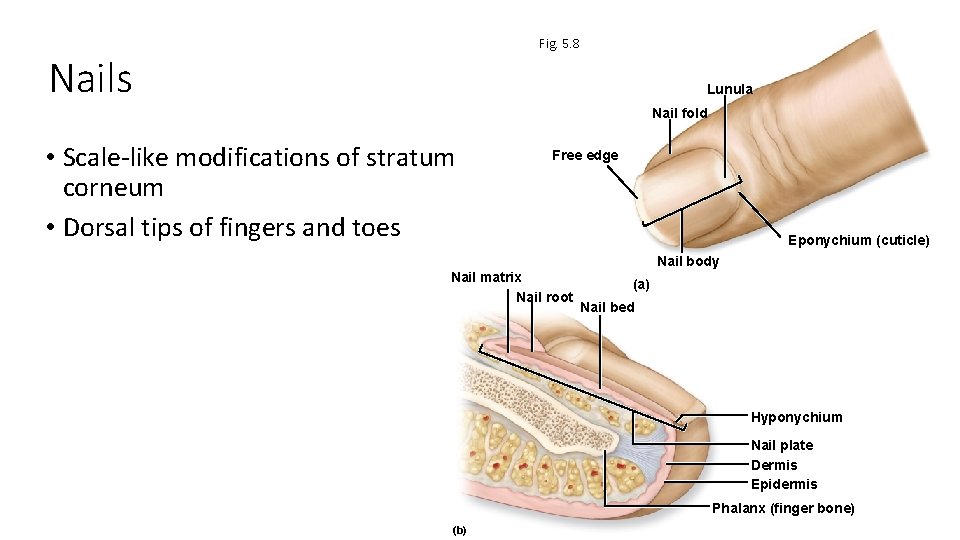
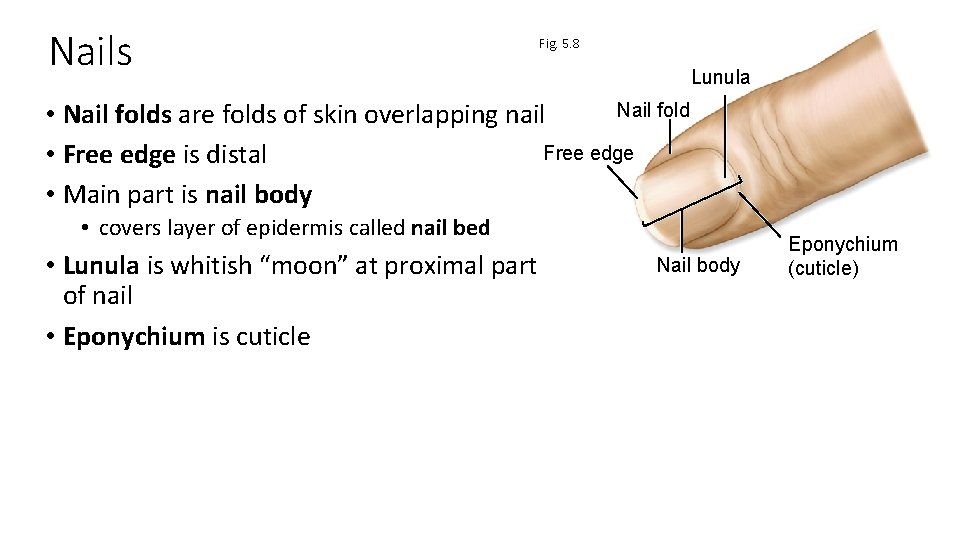
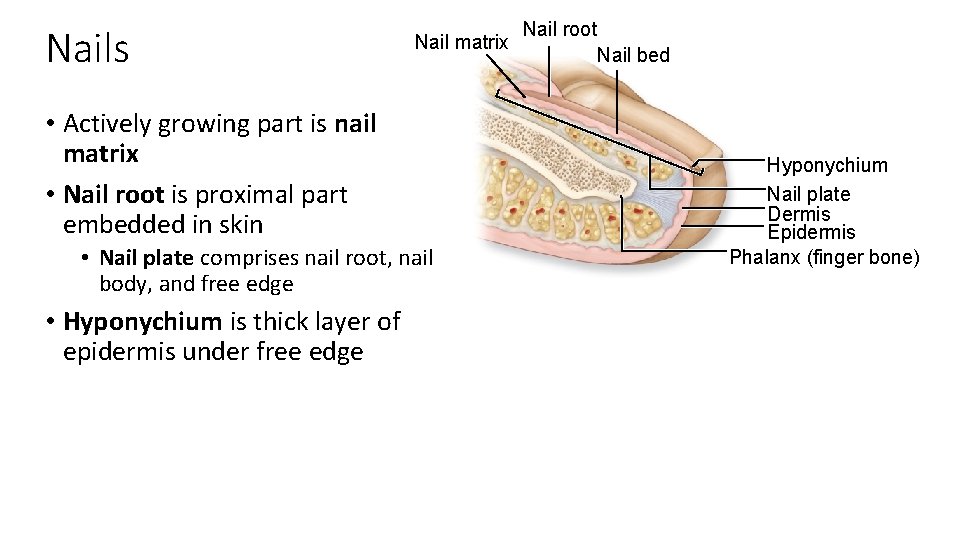
Fig. 5. 8 Nails Lunula Nail fold • Scale-like modifications of stratum corneum • Dorsal tips of fingers and toes Free edge Eponychium (cuticle) Nail body Nail matrix Nail root (a) Nail bed Hyponychium Nail plate Dermis Epidermis Phalanx (finger bone) (b)
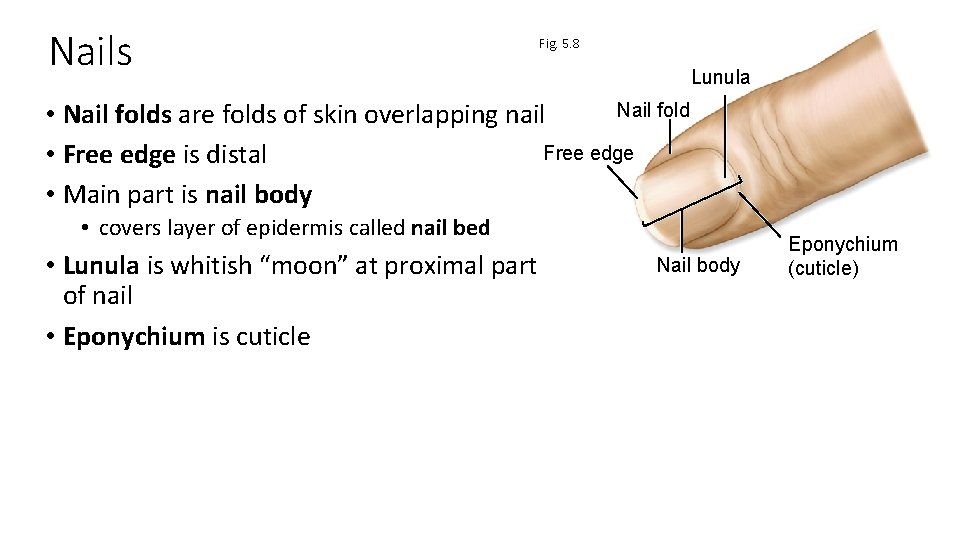
Nails Fig. 5. 8 Lunula Nail fold • Nail folds are folds of skin overlapping nail Free edge • Free edge is distal • Main part is nail body • covers layer of epidermis called nail bed • Lunula is whitish “moon” at proximal part of nail • Eponychium is cuticle Nail body Eponychium (cuticle)
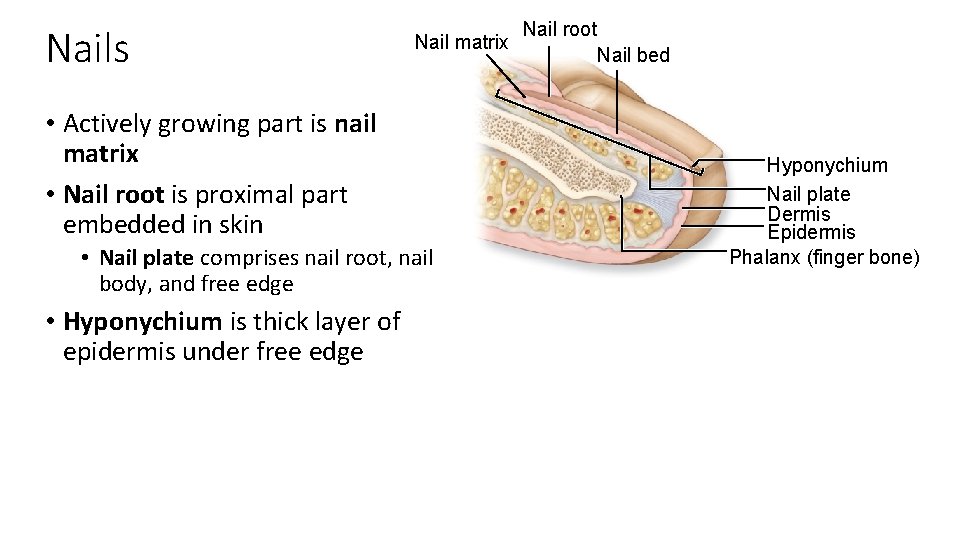
Nails Nail matrix • Actively growing part is nail matrix • Nail root is proximal part embedded in skin • Nail plate comprises nail root, nail body, and free edge • Hyponychium is thick layer of epidermis under free edge Nail root Nail bed Hyponychium Nail plate Dermis Epidermis Phalanx (finger bone)
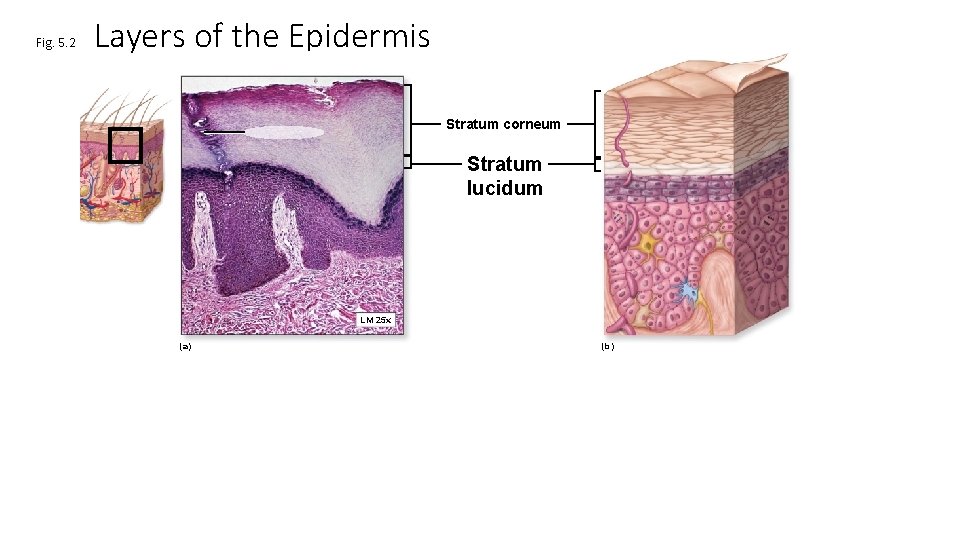
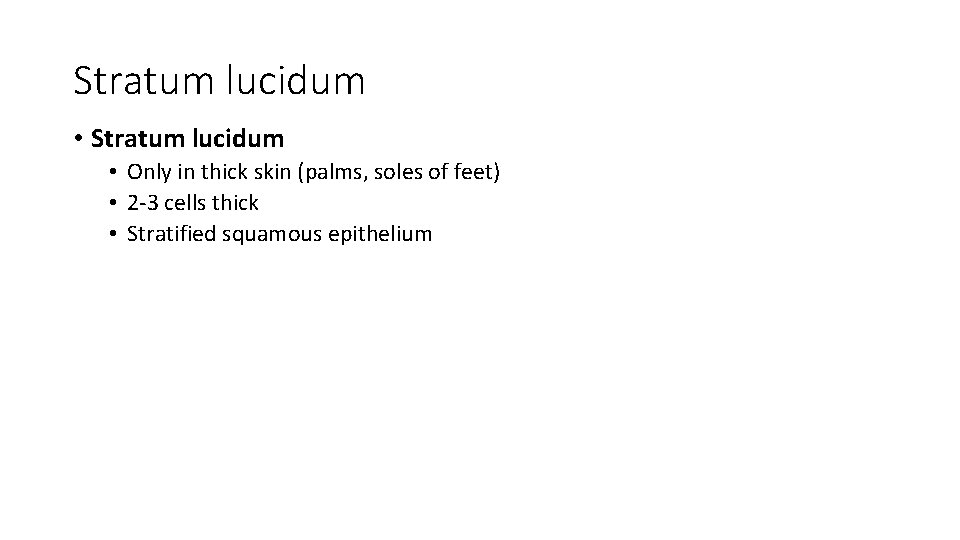
Fig. 5. 2 Layers of the Epidermis Stratum corneum Stratum lucidum LM 25 x (a) (b)
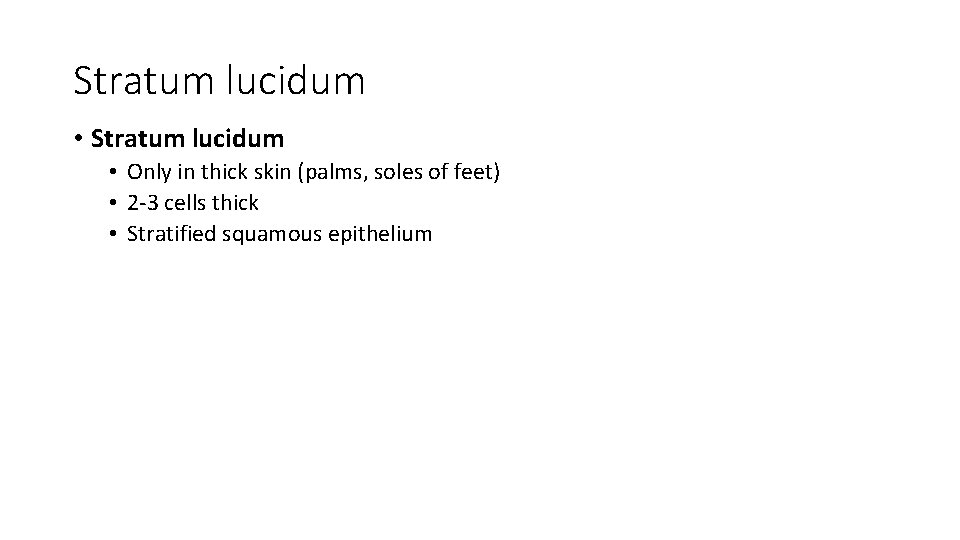
Stratum lucidum • Only in thick skin (palms, soles of feet) • 2 -3 cells thick • Stratified squamous epithelium
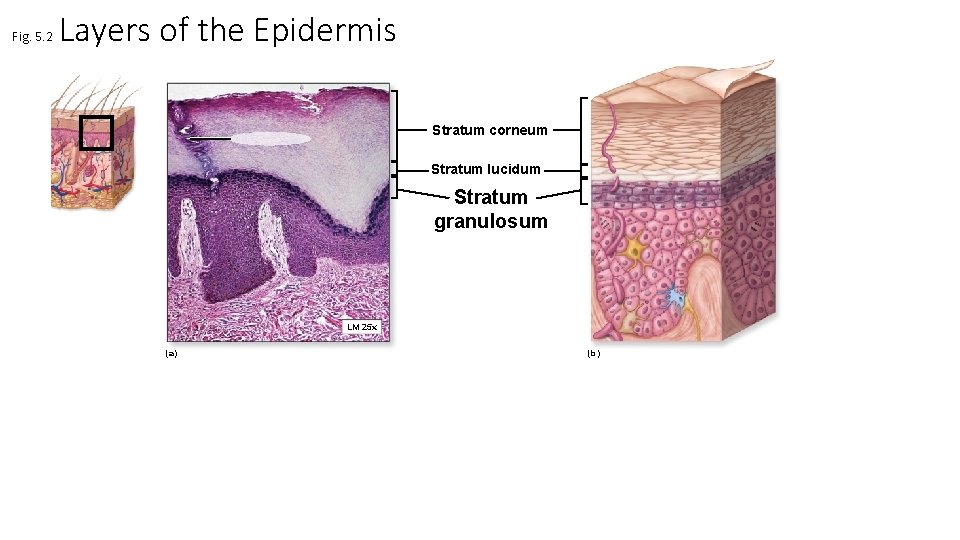
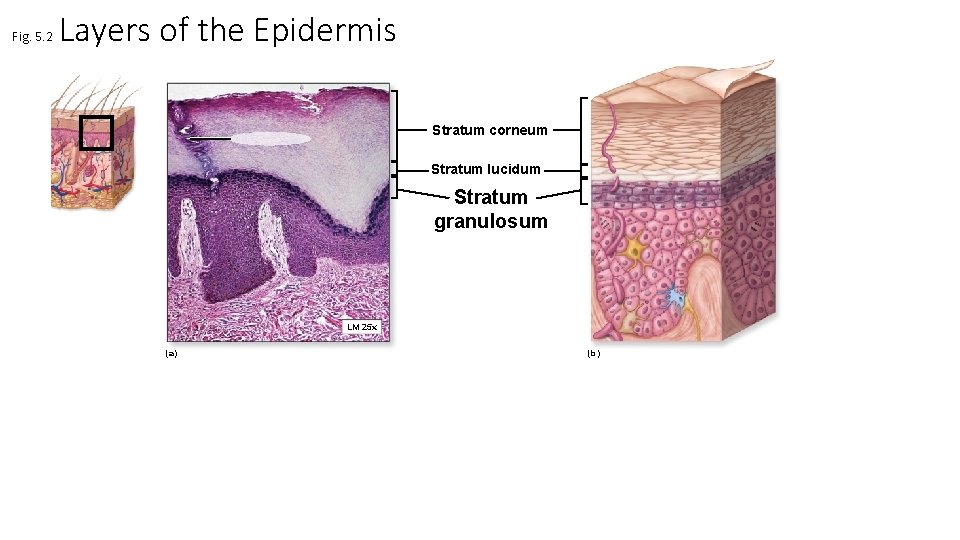
Fig. 5. 2 Layers of the Epidermis Stratum corneum Stratum lucidum Stratum granulosum LM 25 x (a) (b)
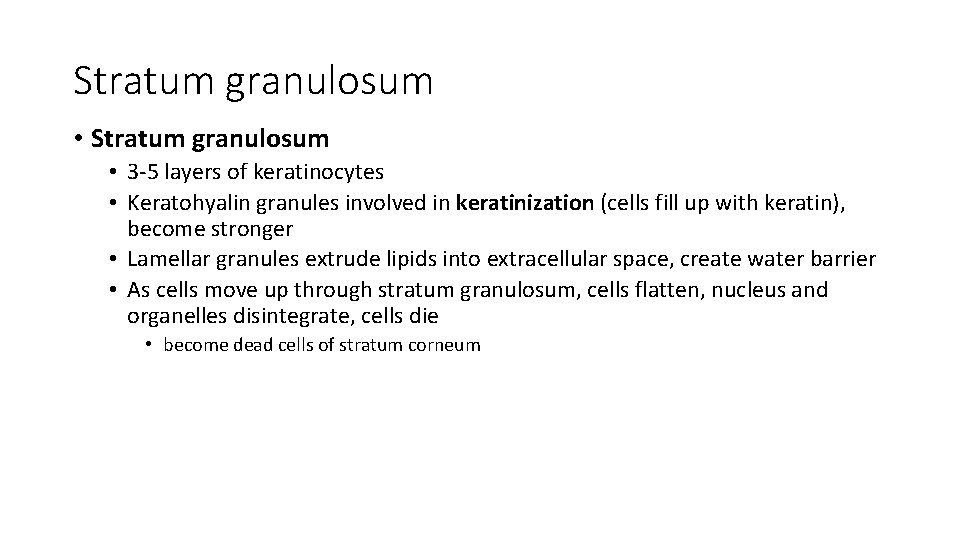
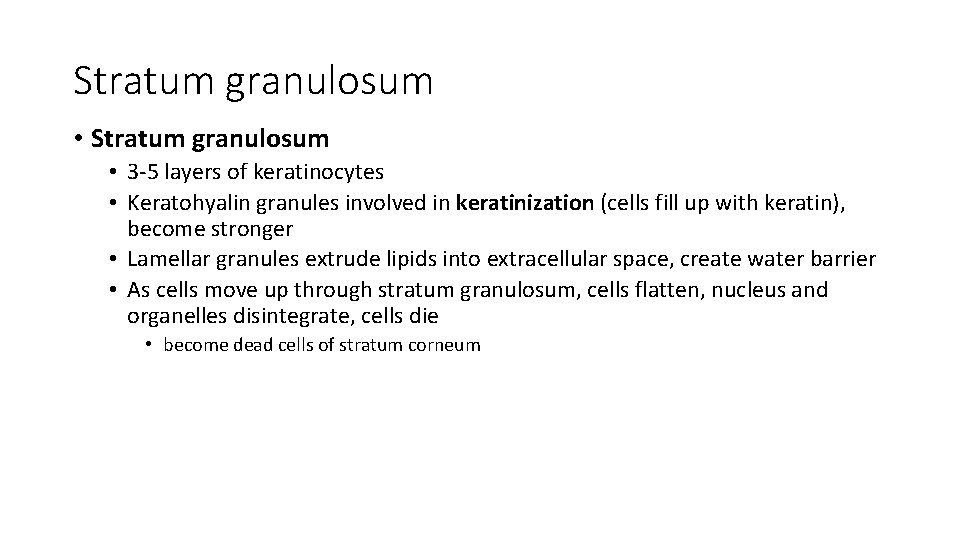
Stratum granulosum • 3 -5 layers of keratinocytes • Keratohyalin granules involved in keratinization (cells fill up with keratin), become stronger • Lamellar granules extrude lipids into extracellular space, create water barrier • As cells move up through stratum granulosum, cells flatten, nucleus and organelles disintegrate, cells die • become dead cells of stratum corneum
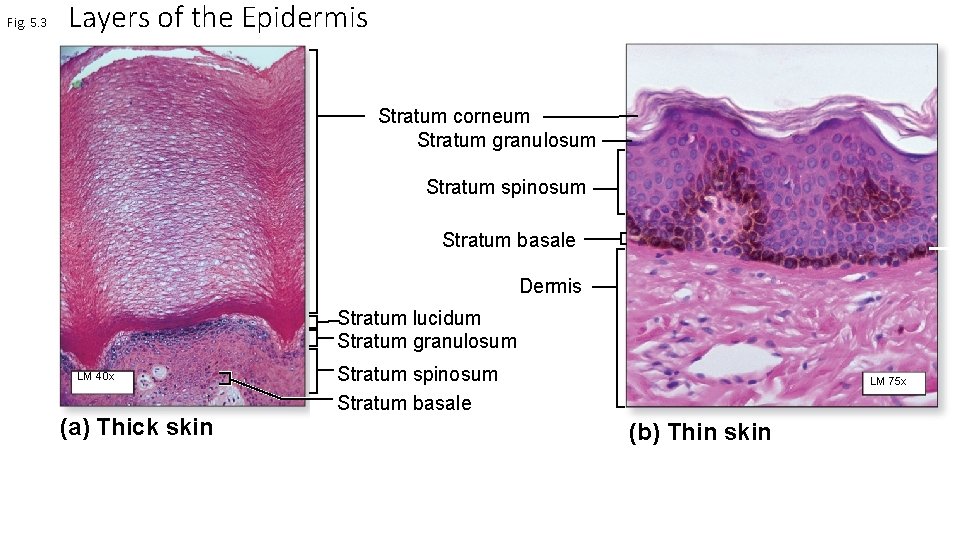
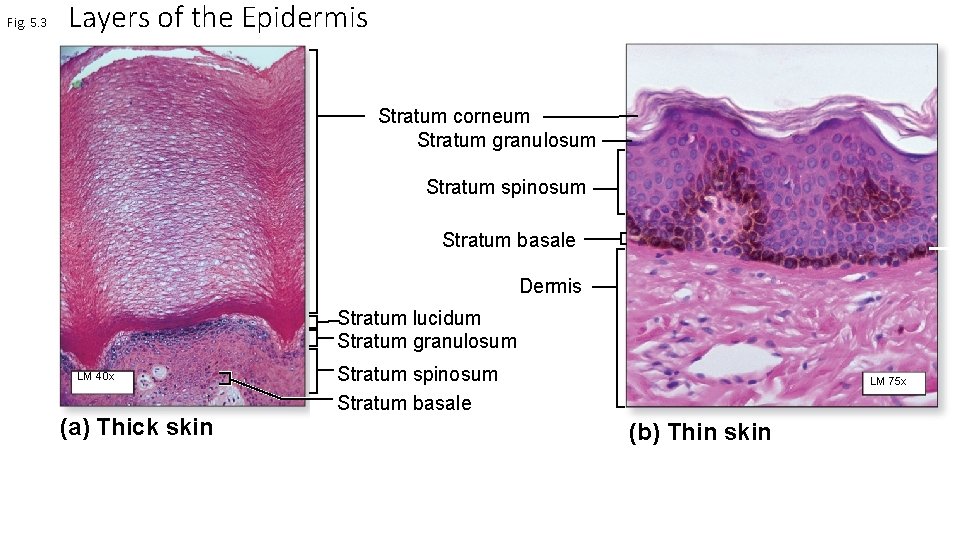
Fig. 5. 3 Layers of the Epidermis Stratum corneum Stratum granulosum Stratum spinosum Stratum basale Dermis Stratum lucidum Stratum granulosum LM 40 x (a) Thick skin Stratum spinosum Stratum basale LM 75 x (b) Thin skin
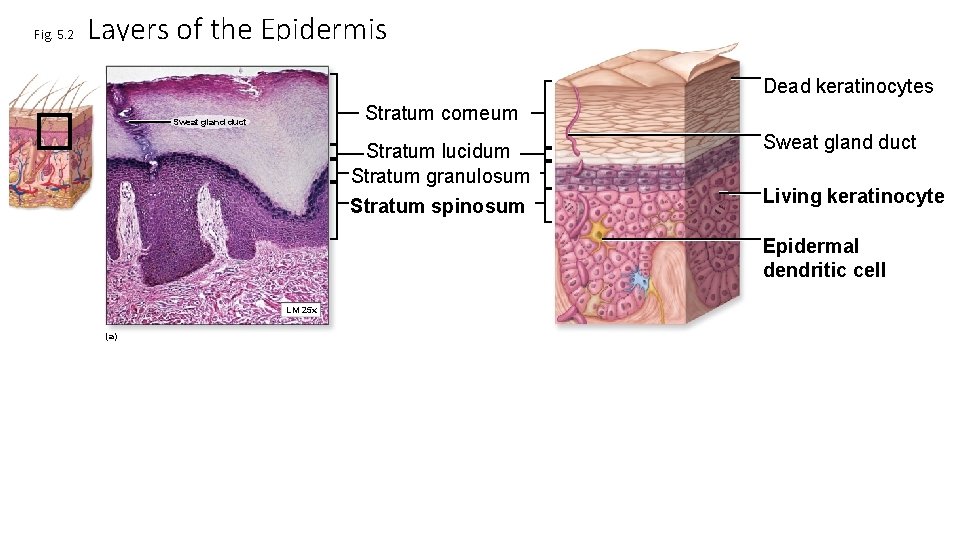
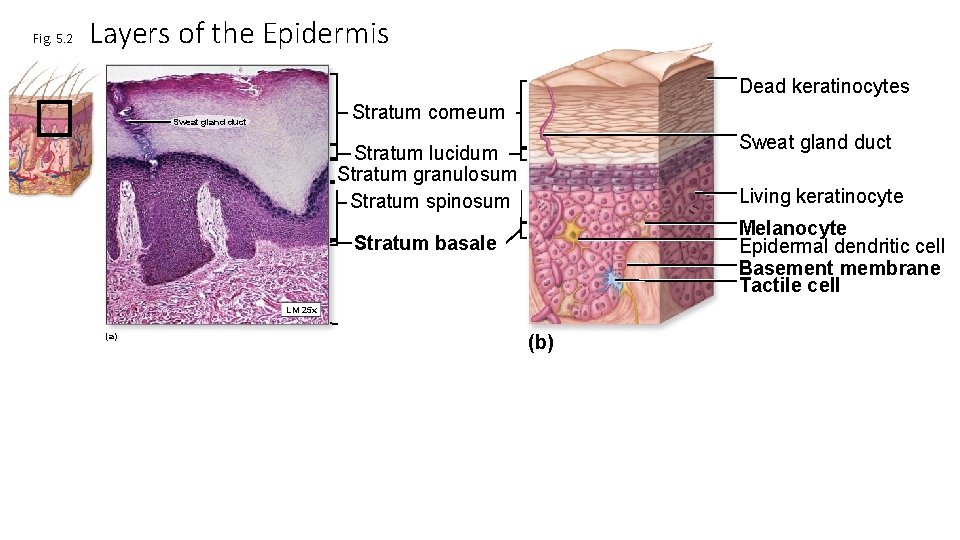
Fig. 5. 2 Layers of the Epidermis Dead keratinocytes Stratum corneum Sweat gland duct Stratum lucidum Stratum granulosum Stratum spinosum Sweat gland duct Living keratinocyte Epidermal dendritic cell LM 25 x (a)
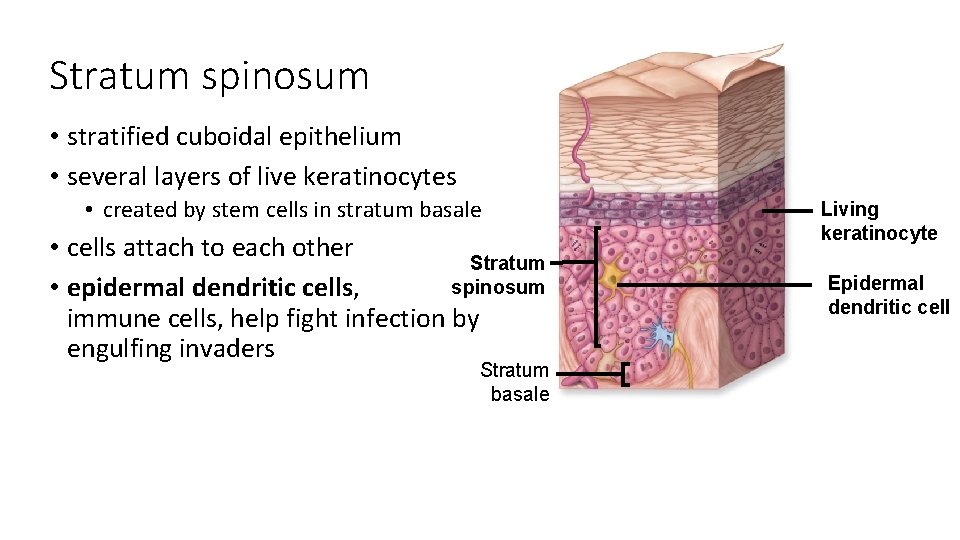
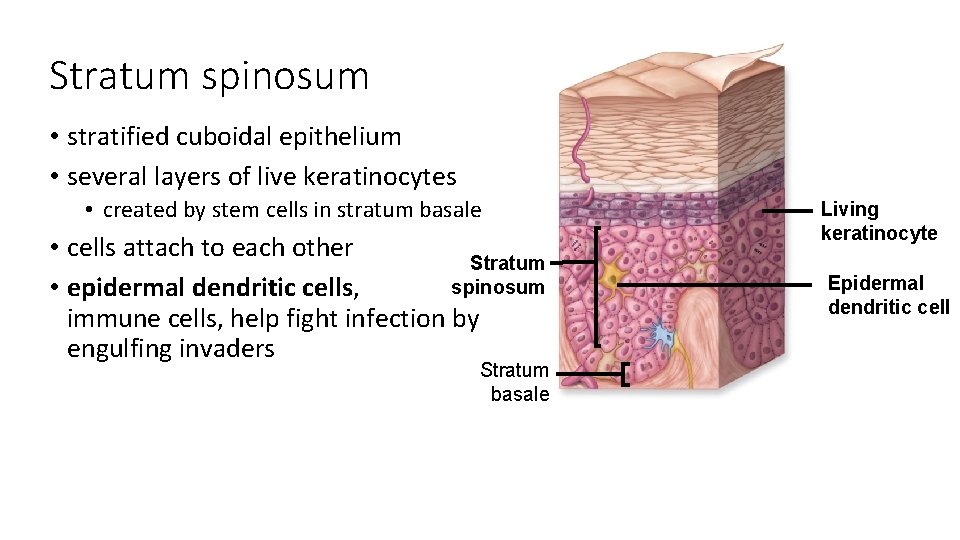
Stratum spinosum • stratified cuboidal epithelium • several layers of live keratinocytes • created by stem cells in stratum basale • cells attach to each other Stratum spinosum • epidermal dendritic cells, immune cells, help fight infection by engulfing invaders Stratum basale Living keratinocyte Epidermal dendritic cell
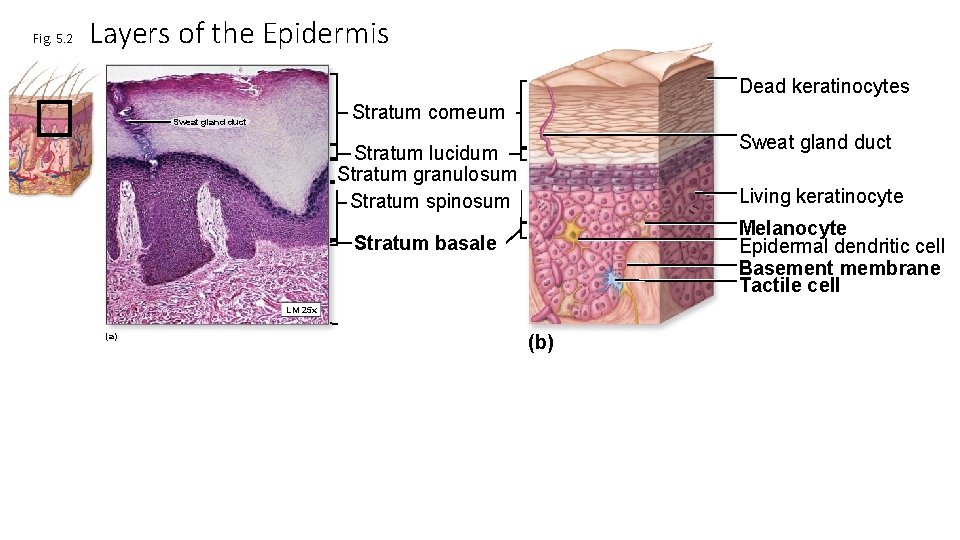
Fig. 5. 2 Layers of the Epidermis Dead keratinocytes Stratum corneum Sweat gland duct Stratum lucidum Stratum granulosum Stratum spinosum Living keratinocyte Melanocyte Epidermal dendritic cell Basement membrane Tactile cell Stratum basale LM 25 x (a) (b)
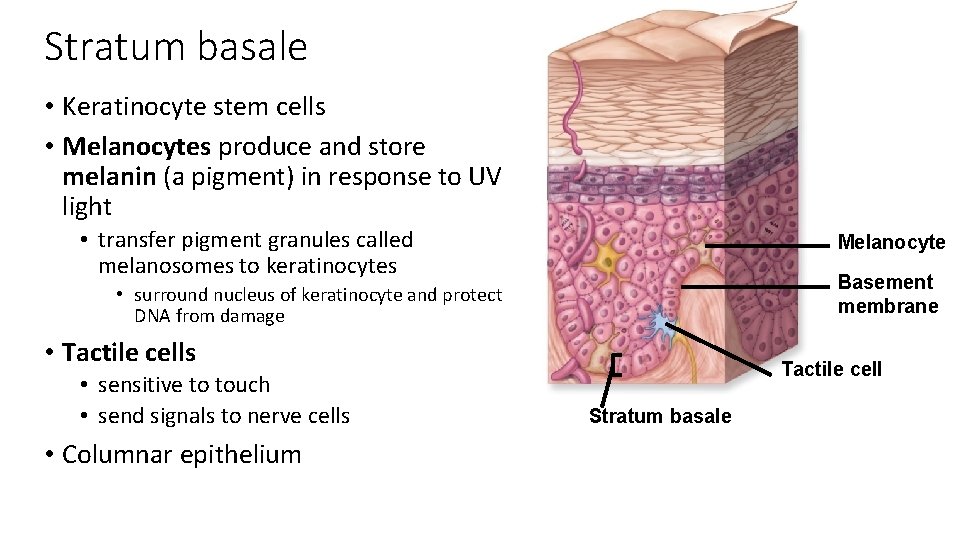
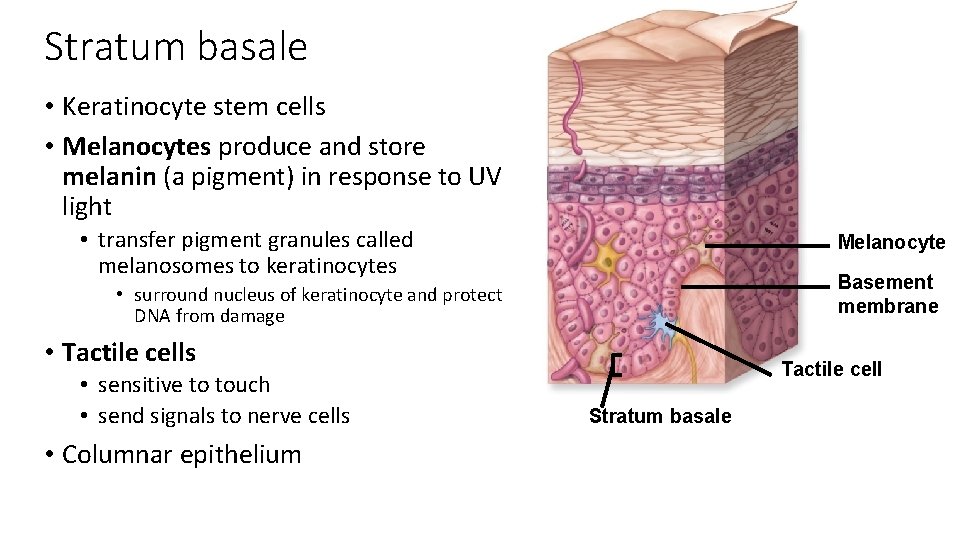
Stratum basale • Keratinocyte stem cells • Melanocytes produce and store melanin (a pigment) in response to UV light • transfer pigment granules called melanosomes to keratinocytes Melanocyte Basement membrane • surround nucleus of keratinocyte and protect DNA from damage • Tactile cells • sensitive to touch • send signals to nerve cells • Columnar epithelium Tactile cell Stratum basale
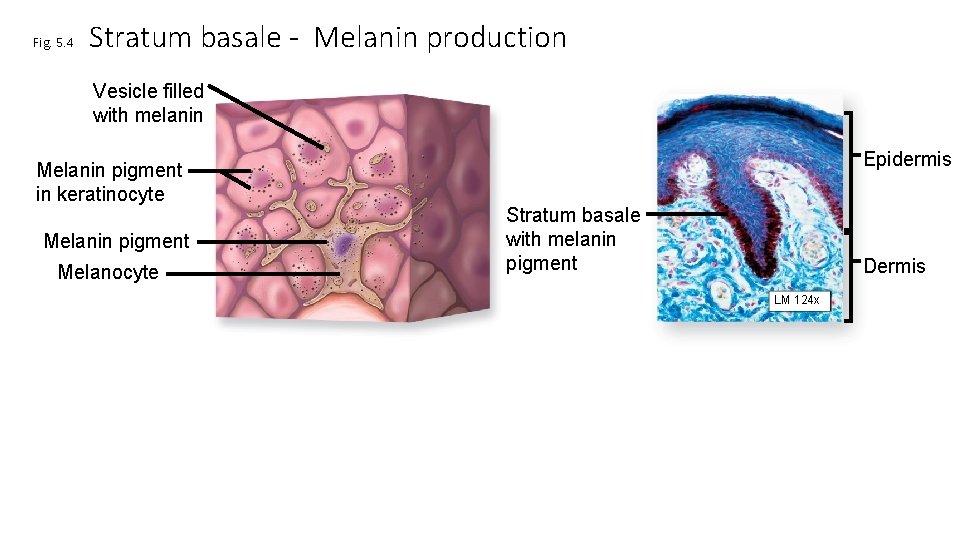
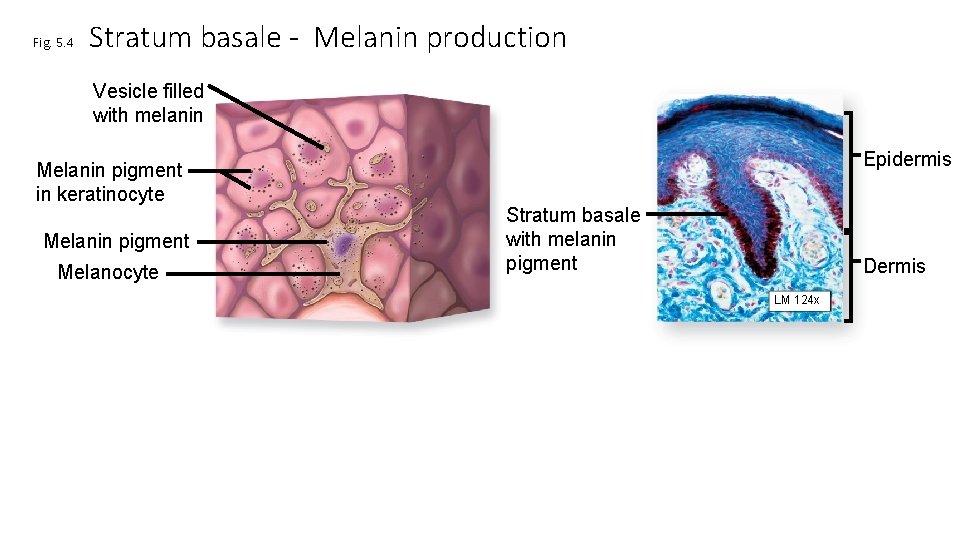
Fig. 5. 4 Stratum basale - Melanin production Vesicle filled with melanin Melanin pigment in keratinocyte Melanin pigment Melanocyte Epidermis Stratum basale with melanin pigment Dermis LM 124 x
Skin color • Combination of • hemoglobin in blood vessels • melanin in stratum basale • everyone has same number of melanocytes • darker-skinned people’s melanocytes make more melanin • carotene (from yellow-orange vegetables) • stored in keratinocytes in stratum corneum • stored in subcutaneous fat
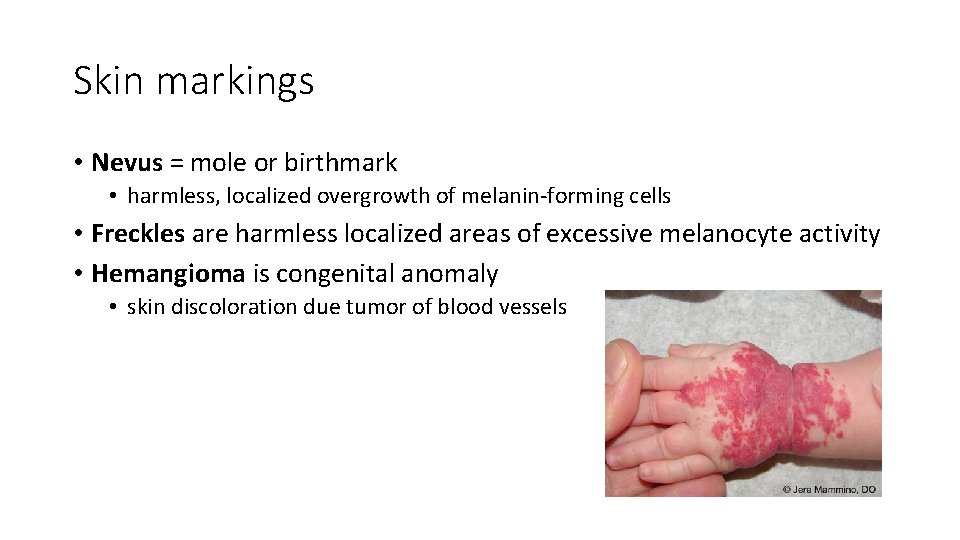
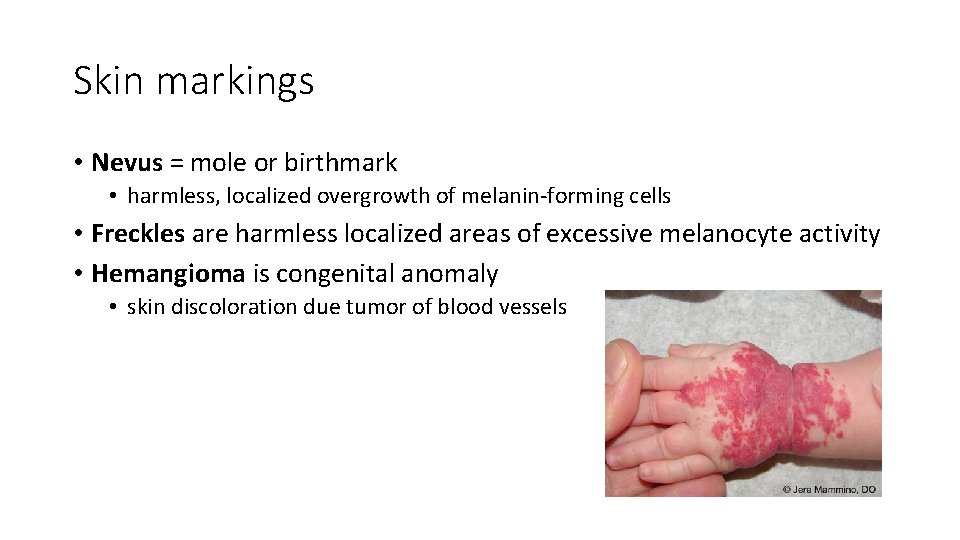
Skin markings • Nevus = mole or birthmark • harmless, localized overgrowth of melanin-forming cells • Freckles are harmless localized areas of excessive melanocyte activity • Hemangioma is congenital anomaly • skin discoloration due tumor of blood vessels
Fingerprints • AKA friction ridges • increase friction to help us hold onto things • Unique to each individual • Study of friction ridges called dermatoglyphics
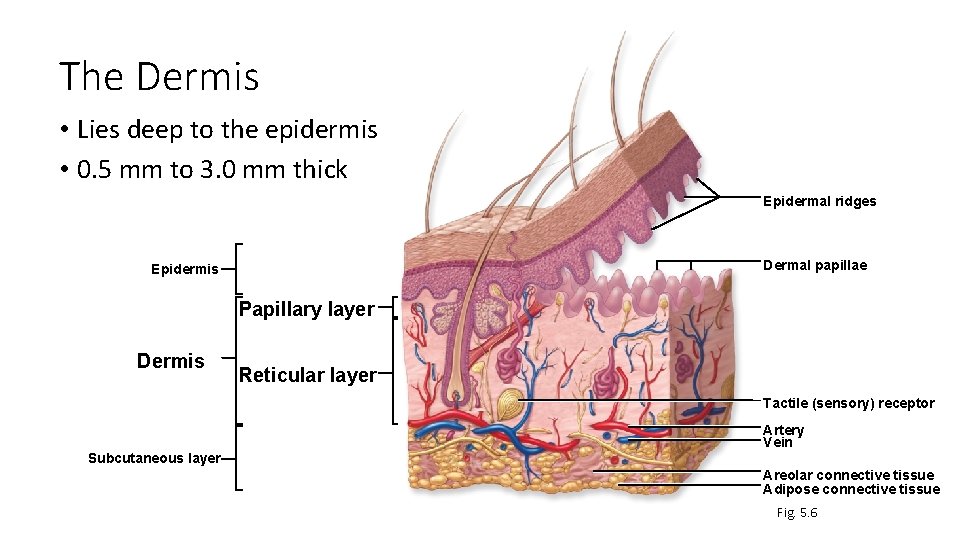
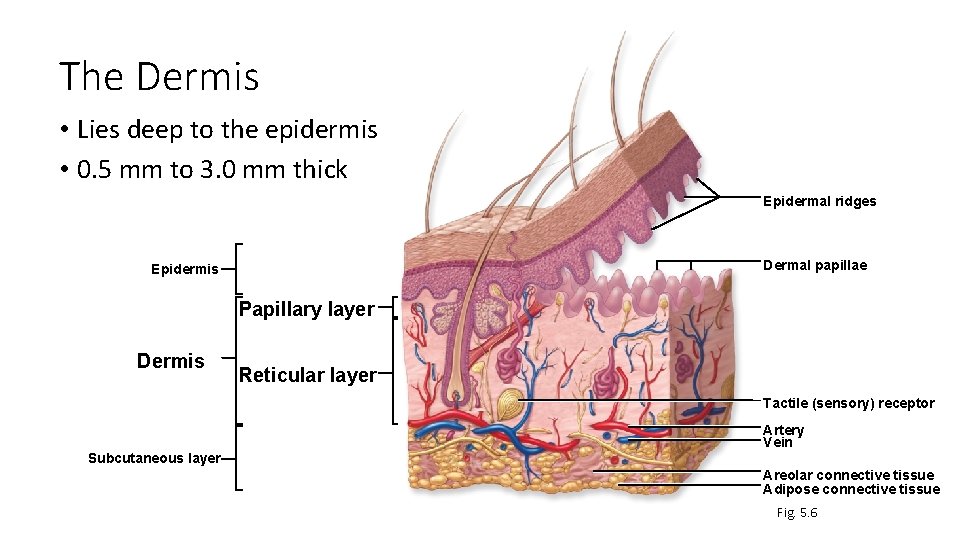
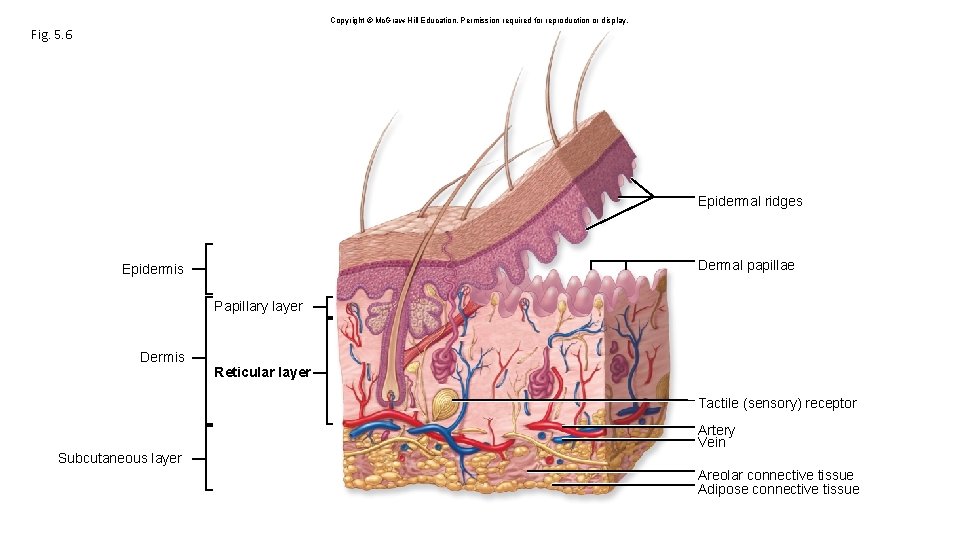
The Dermis • Lies deep to the epidermis • 0. 5 mm to 3. 0 mm thick Epidermal ridges Dermal papillae Epidermis Papillary layer Dermis Reticular layer Tactile (sensory) receptor Artery Vein Subcutaneous layer Areolar connective tissue Adipose connective tissue Fig. 5. 6
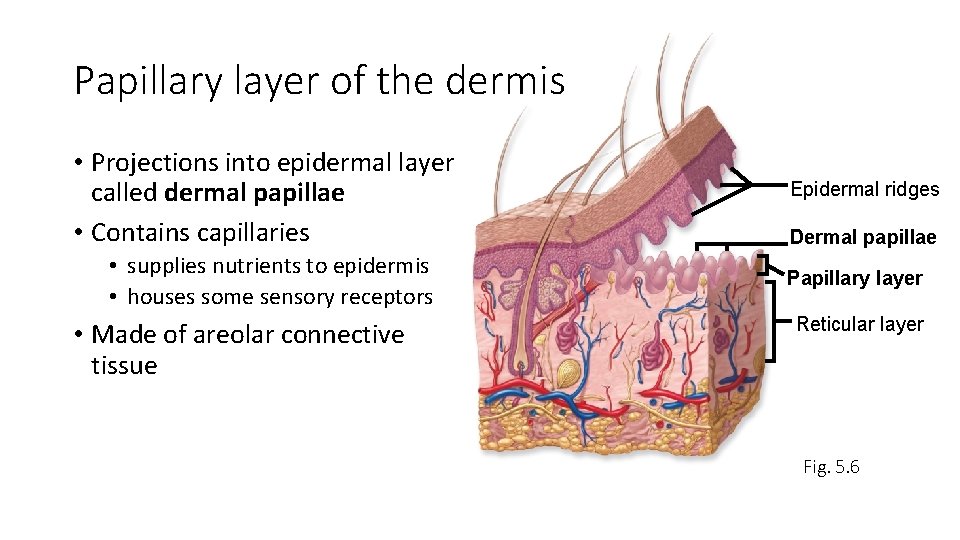
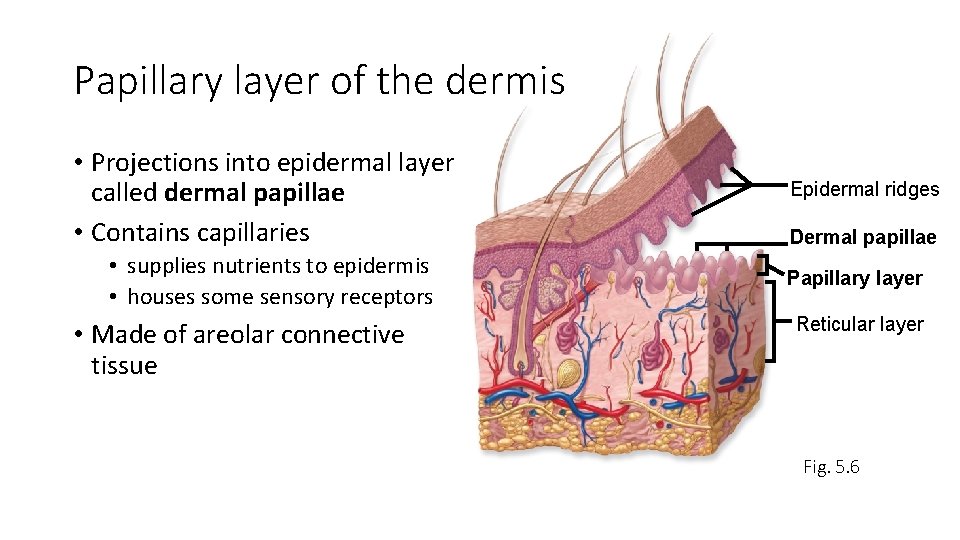
Papillary layer of the dermis • Projections into epidermal layer called dermal papillae • Contains capillaries • supplies nutrients to epidermis • houses some sensory receptors • Made of areolar connective tissue Epidermal ridges Dermal papillae Papillary layer Reticular layer Fig. 5. 6
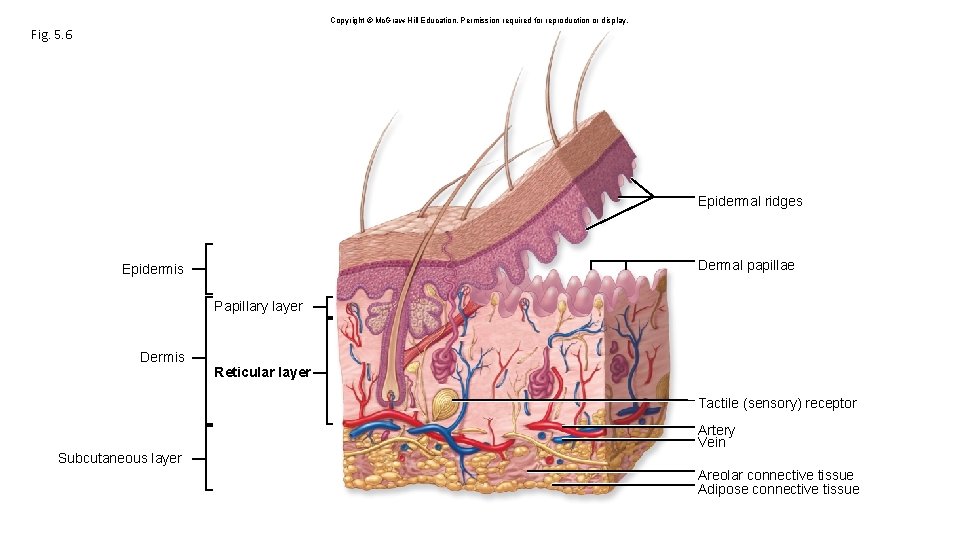
Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. Fig. 5. 6 Epidermal ridges Dermal papillae Epidermis Papillary layer Dermis Reticular layer Tactile (sensory) receptor Artery Vein Subcutaneous layer Areolar connective tissue Adipose connective tissue
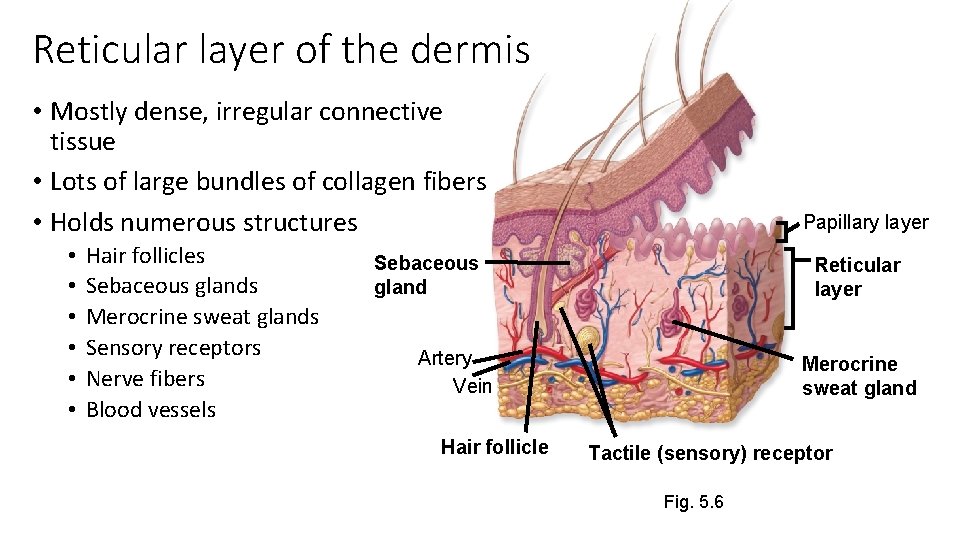
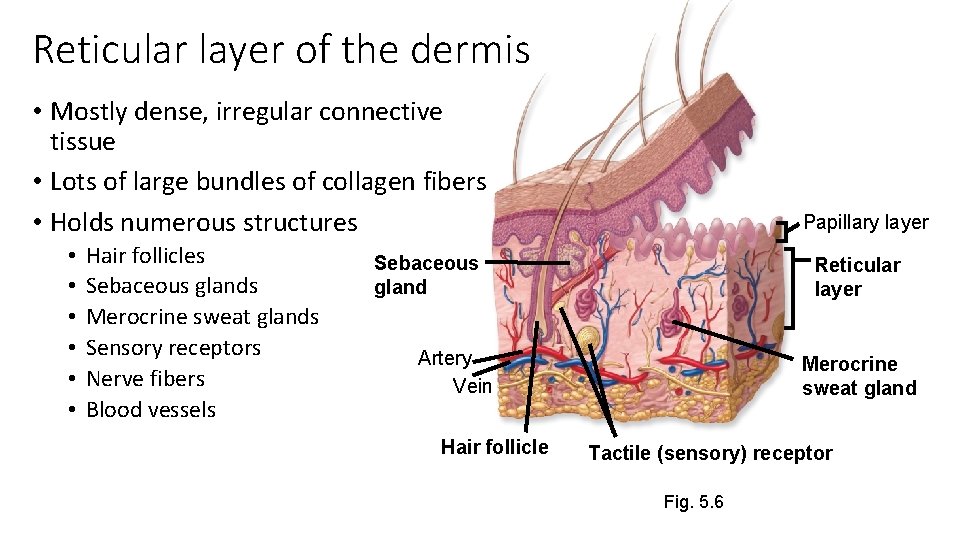
Reticular layer of the dermis • Mostly dense, irregular connective tissue • Lots of large bundles of collagen fibers • Holds numerous structures • • • Hair follicles Sebaceous glands Merocrine sweat glands Sensory receptors Nerve fibers Blood vessels Papillary layer Sebaceous gland Reticular layer Artery Vein Hair follicle Merocrine sweat gland Tactile (sensory) receptor Fig. 5. 6
Why are tattoos permanent? • Dye injected into dermis • Scar tissue surrounds dye granules • granules too large for dendritic cells to digest
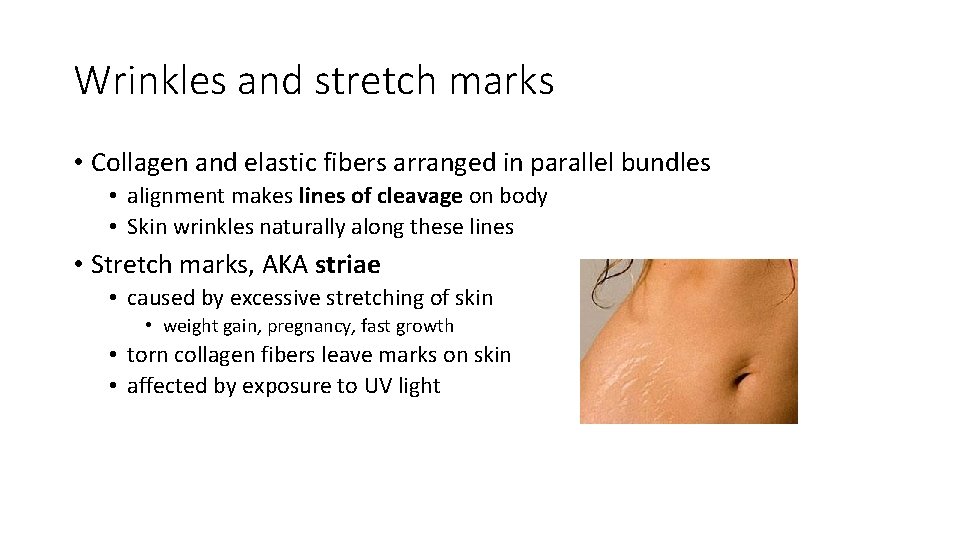
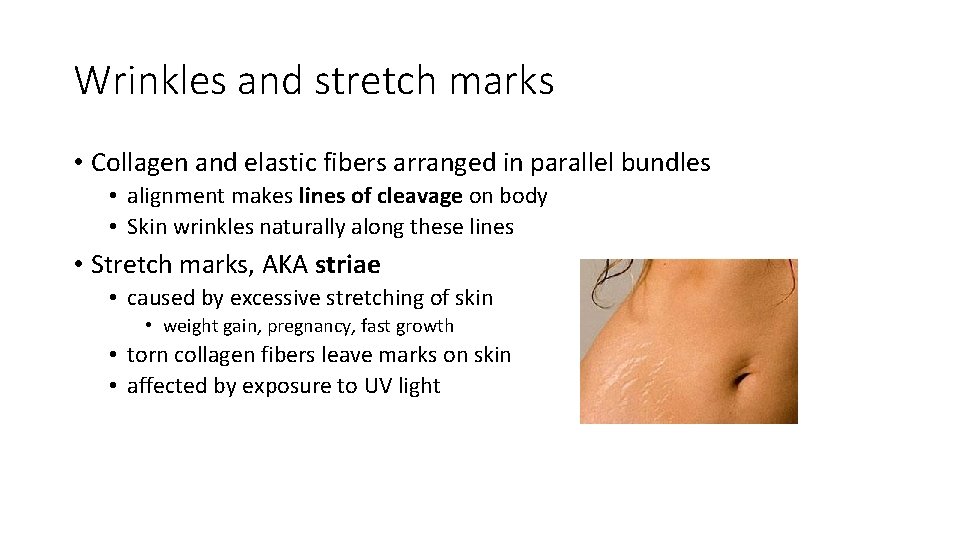
Wrinkles and stretch marks • Collagen and elastic fibers arranged in parallel bundles • alignment makes lines of cleavage on body • Skin wrinkles naturally along these lines • Stretch marks, AKA striae • caused by excessive stretching of skin • weight gain, pregnancy, fast growth • torn collagen fibers leave marks on skin • affected by exposure to UV light
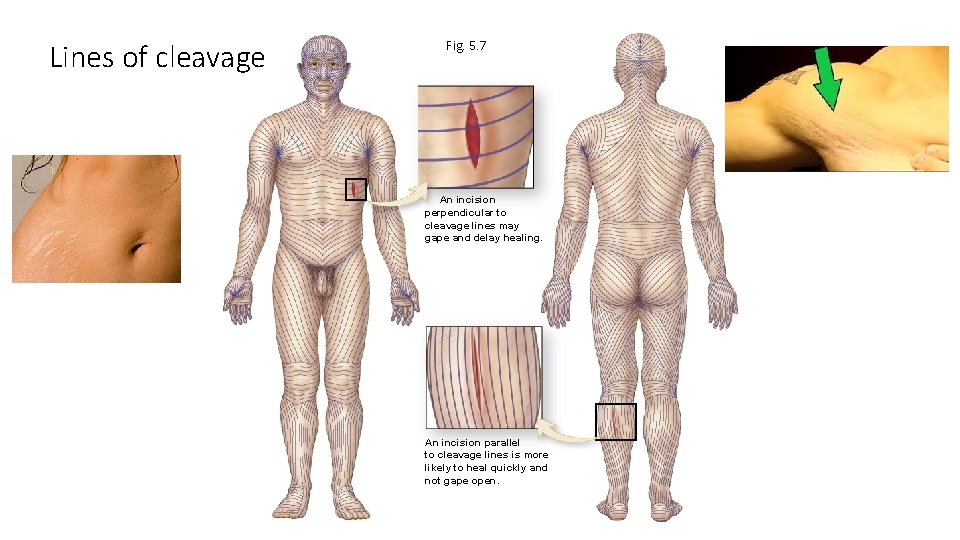
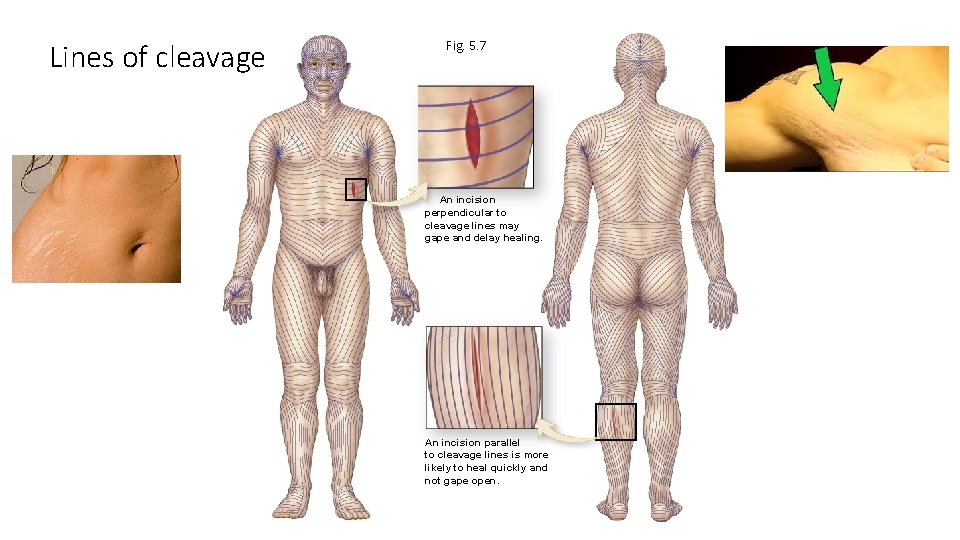
Lines of cleavage Fig. 5. 7 An incision perpendicular to cleavage lines may gape and delay healing. An incision parallel to cleavage lines is more likely to heal quickly and not gape open.
Hair • Single hair = pilus; plural = pili • Lanugo = fine, unpigmented, downy hair on fetus and baby (sometimes) • Vellus = hair found on most of body • Terminal hair = hair on head, eyebrows, eyelashes, beard, pubic regions after puberty • coarser, longer
Hair Functions • Protection • protects scalp from sunburn and injury • protects ear, eyes, and nose from particles • Heat retention • Sensory perception • Visual identification • Chemical signal dispersal • pheromones secreted onto hairs
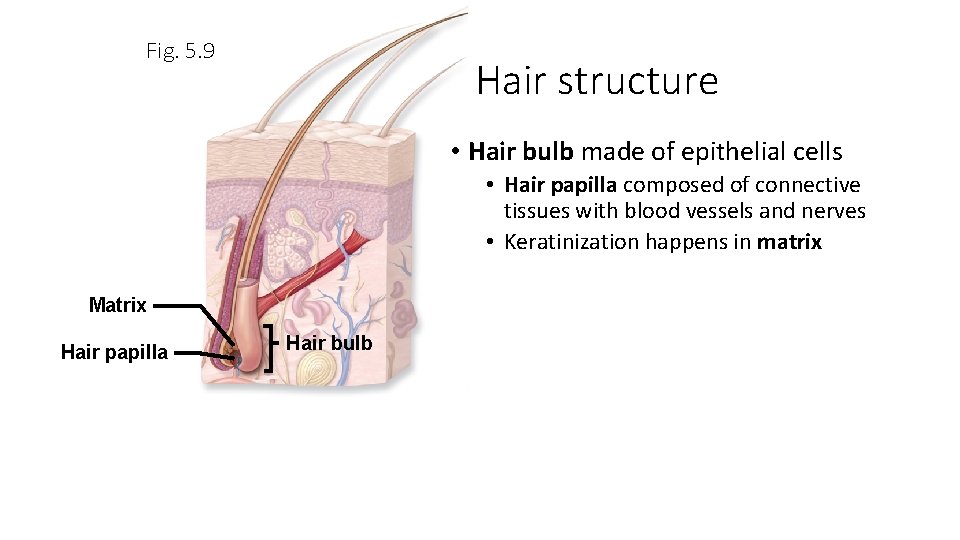
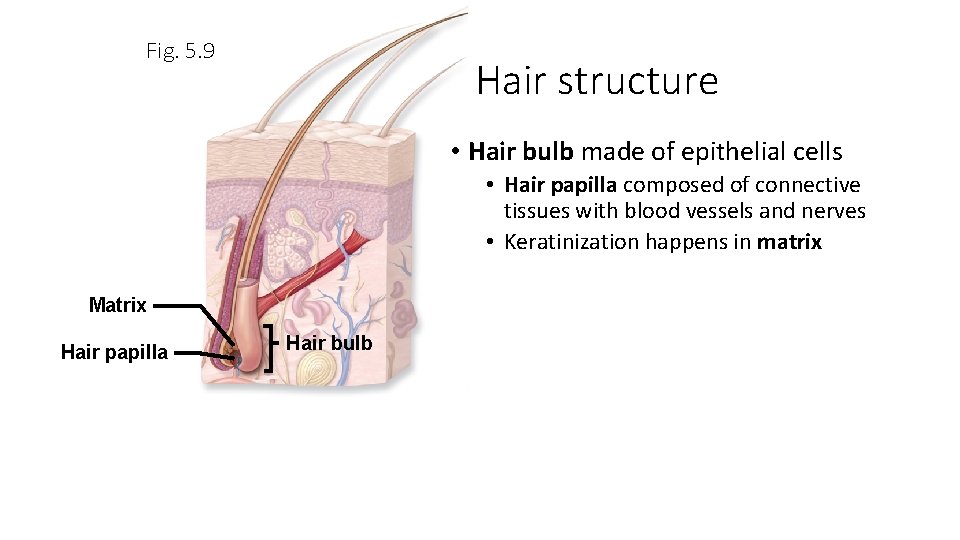
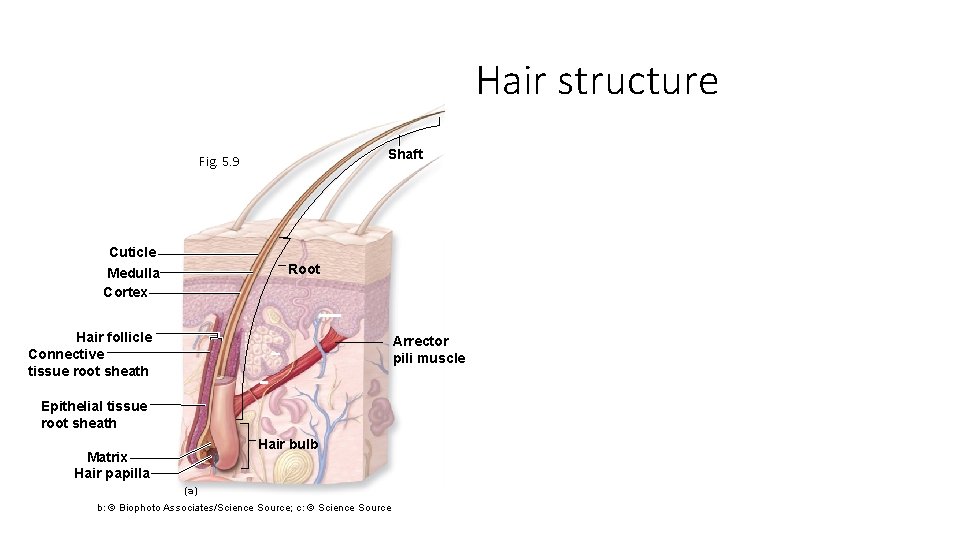
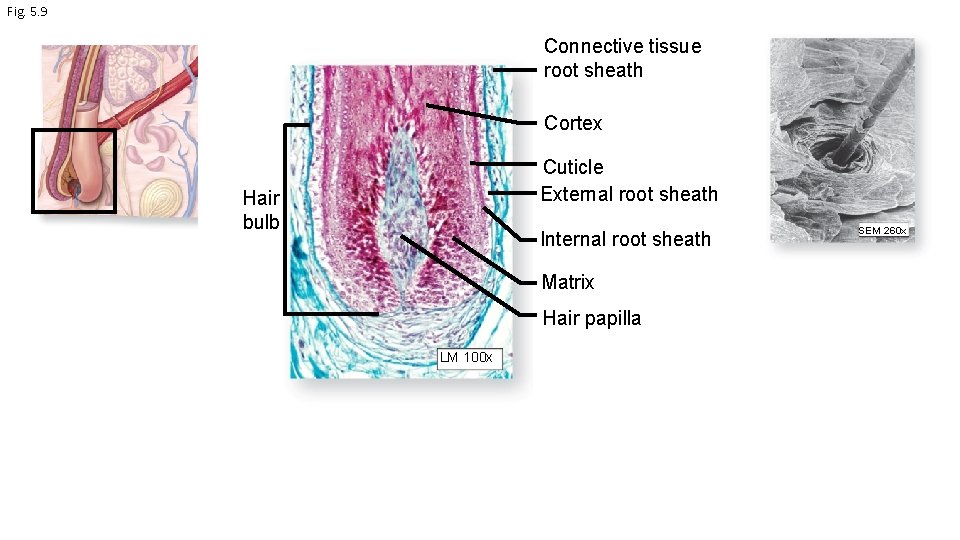
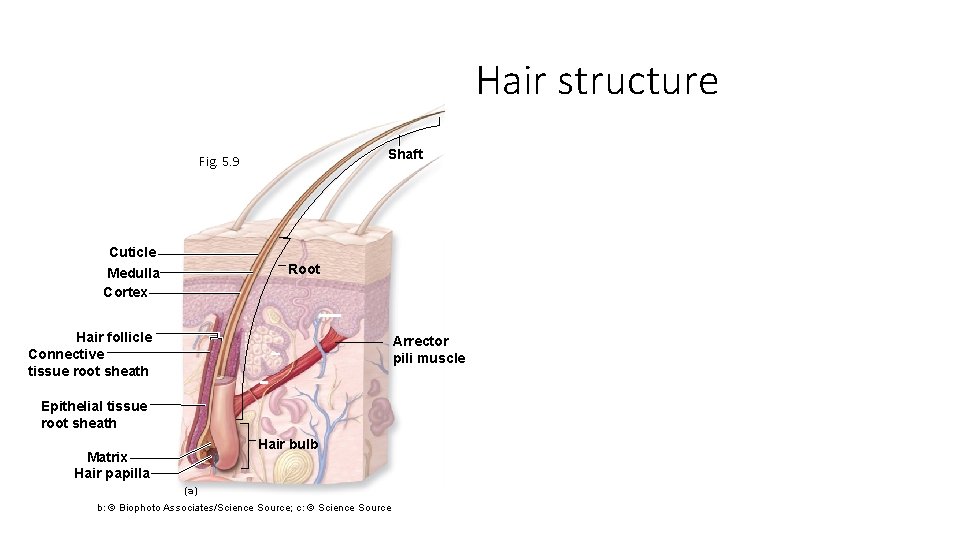
Fig. 5. 9 Hair structure • Hair bulb made of epithelial cells • Hair papilla composed of connective tissues with blood vessels and nerves • Keratinization happens in matrix Matrix Hair papilla Hair bulb
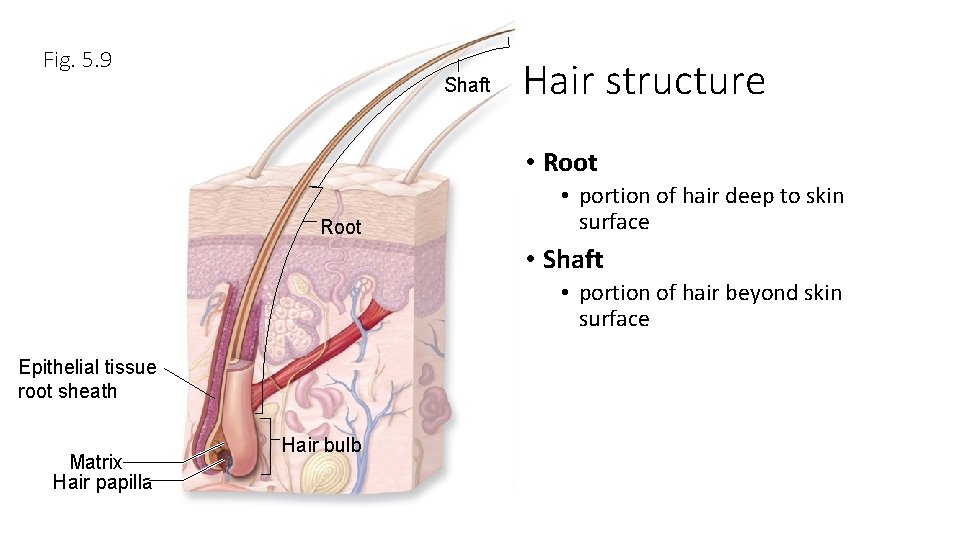
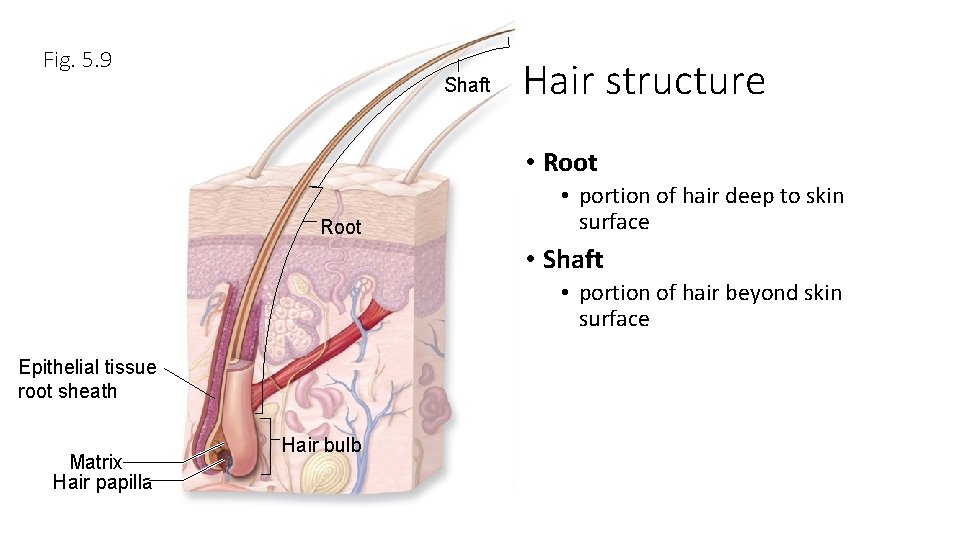
Fig. 5. 9 Shaft Hair structure • Root • portion of hair deep to skin surface • Shaft • portion of hair beyond skin surface Epithelial tissue root sheath Matrix Hair papilla Hair bulb
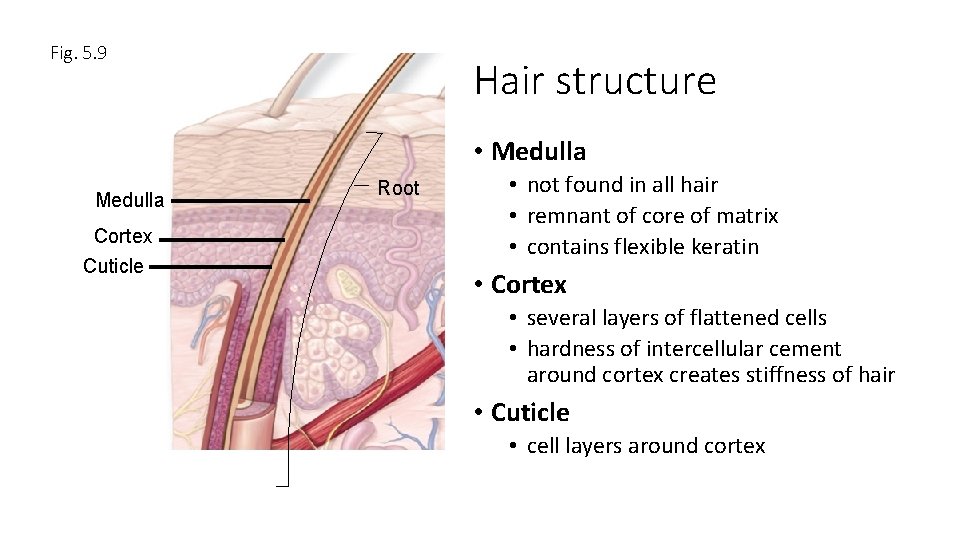
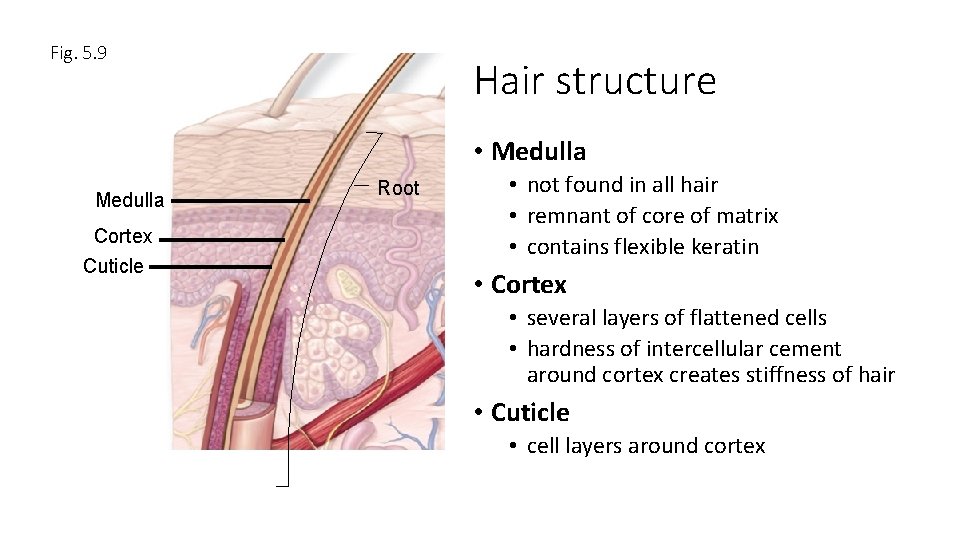
Fig. 5. 9 Hair structure • Medulla Cortex Cuticle Root • not found in all hair • remnant of core of matrix • contains flexible keratin • Cortex • several layers of flattened cells • hardness of intercellular cement around cortex creates stiffness of hair • Cuticle • cell layers around cortex
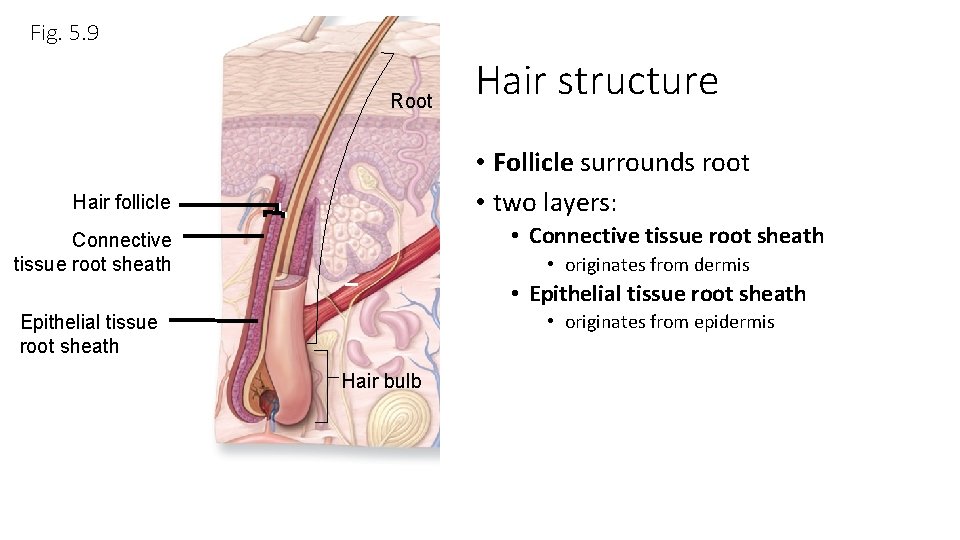
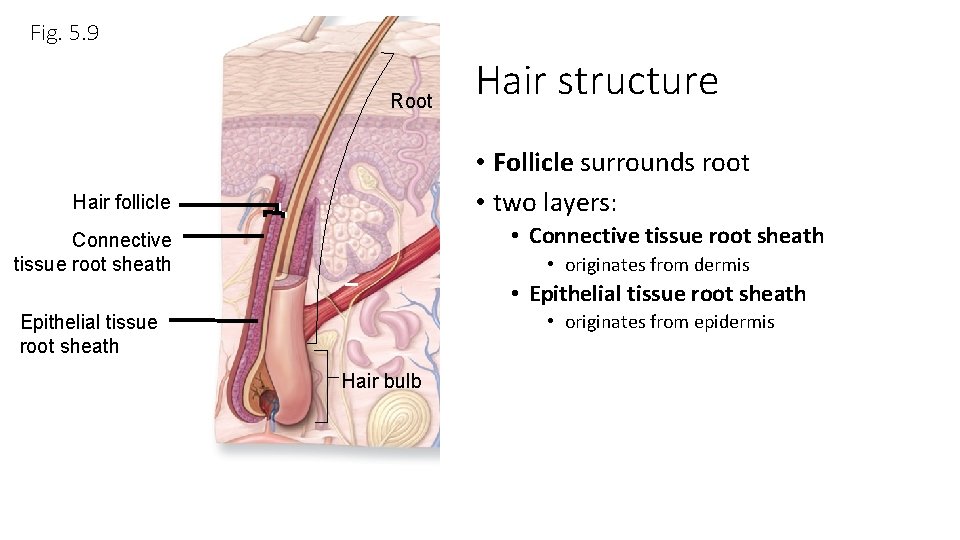
Fig. 5. 9 Root Hair structure • Follicle surrounds root • two layers: Hair follicle • Connective tissue root sheath • originates from dermis • Epithelial tissue root sheath • originates from epidermis Epithelial tissue root sheath Hair bulb
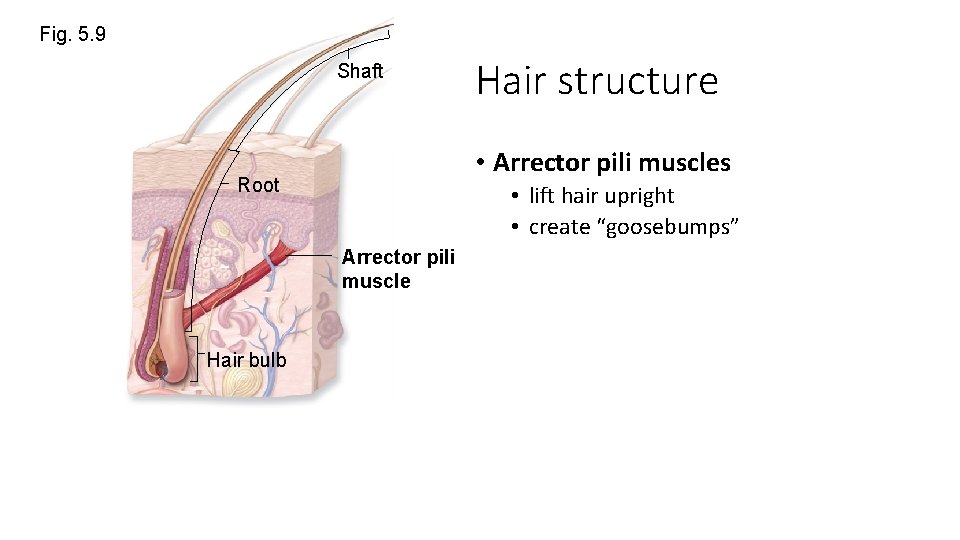
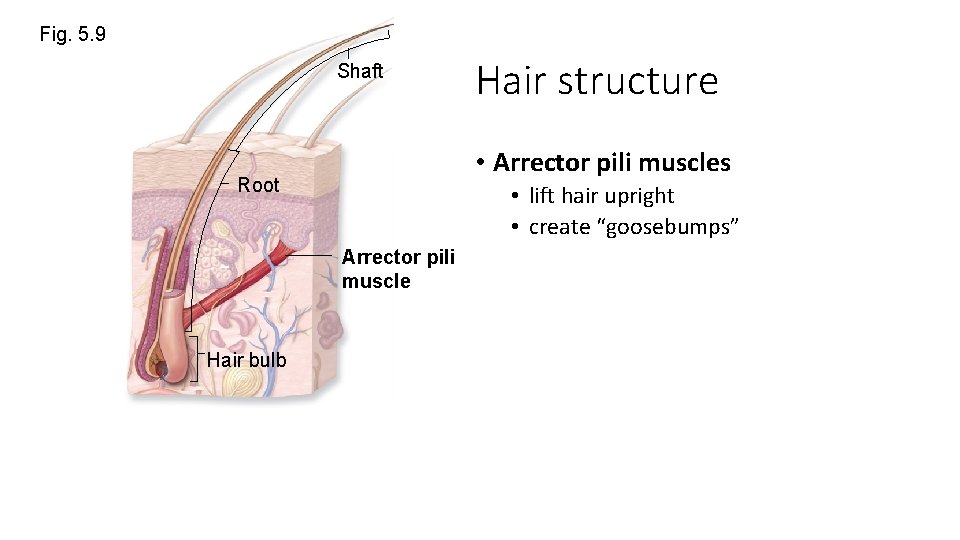
Fig. 5. 9 Shaft • Arrector pili muscles Root • lift hair upright • create “goosebumps” Arrector pili muscle Hair bulb Hair structure
Hair structure Shaft Fig. 5. 9 Cuticle Medulla Cortex Root Hair follicle Connective tissue root sheath Arrector pili muscle Epithelial tissue root sheath Hair bulb Matrix Hair papilla (a) b: © Biophoto Associates/Science Source; c: © Science Source
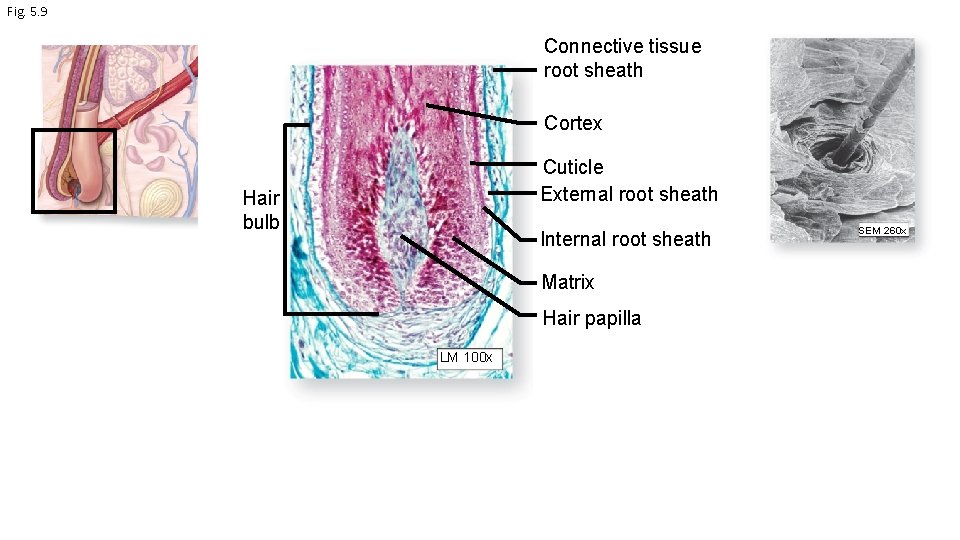
Fig. 5. 9 Connective tissue root sheath Cortex Cuticle External root sheath Hair bulb Internal root sheath Matrix Hair papilla LM 100 x SEM 260 x
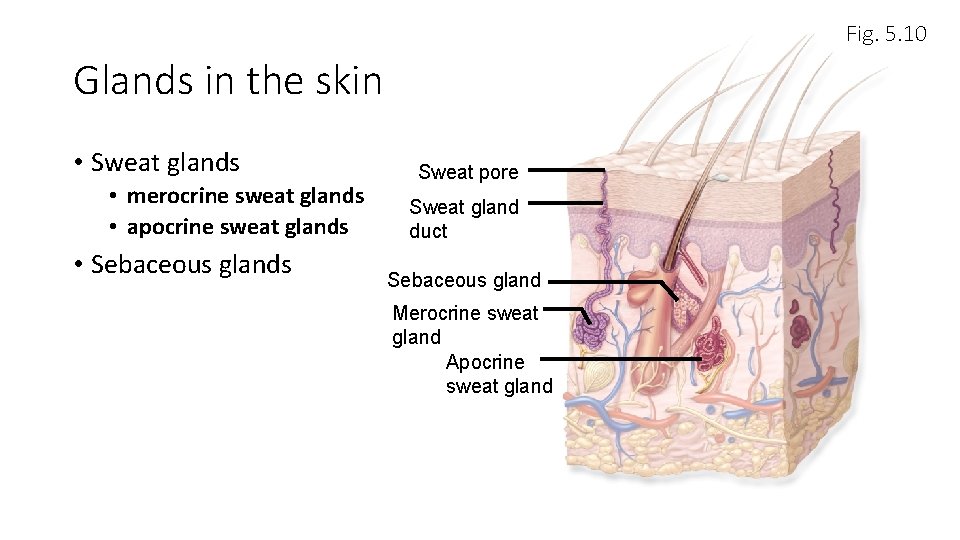
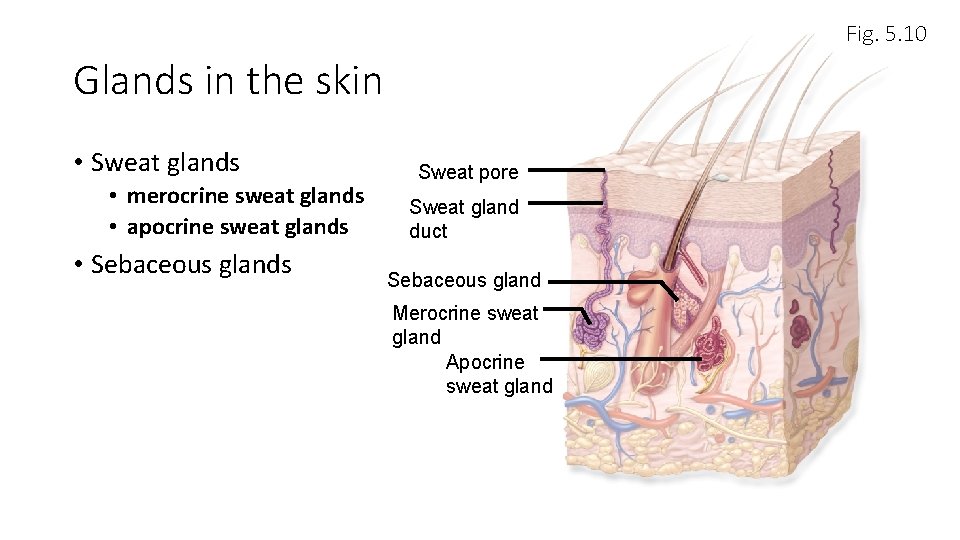
Fig. 5. 10 Glands in the skin • Sweat glands • merocrine sweat glands • apocrine sweat glands • Sebaceous glands Sweat pore Sweat gland duct Sebaceous gland Merocrine sweat gland Apocrine sweat gland
What are glands? (Chapter 4, pp. 88 -95) • individual cells or multicellular organs of epithelial tissue • secrete substances for use elsewhere in body • secrete substances for elimination from body • endocrine glands secrete into bloodstream • exocrine glands secrete to surface of skin or lining of internal passageway • usually connected to outside by a duct
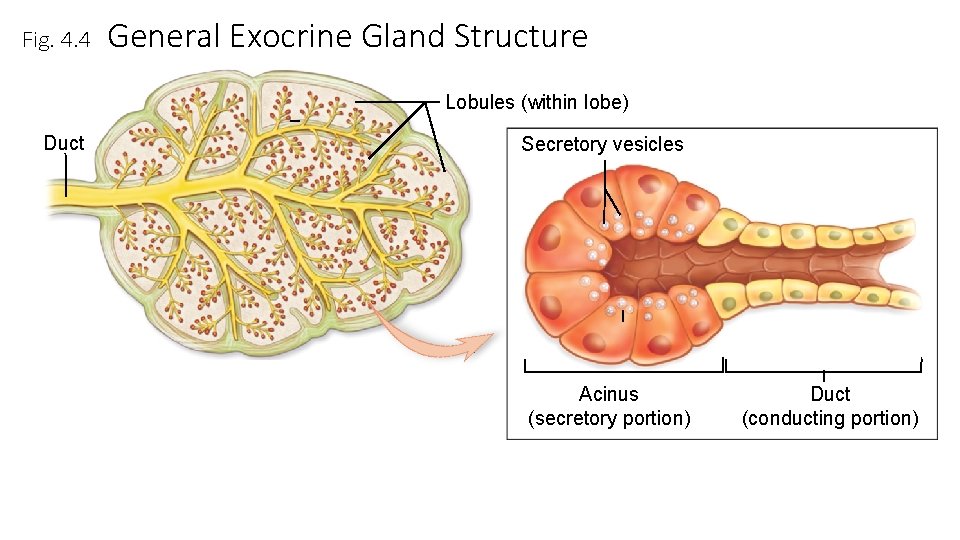
Gland structure • Enclosed in fibrous capsule • Extensions of capsule, called septa, may separate gland into lobes • Simple glands have single, unbranched duct • sweat glands are simple • Compound glands have branched ducts
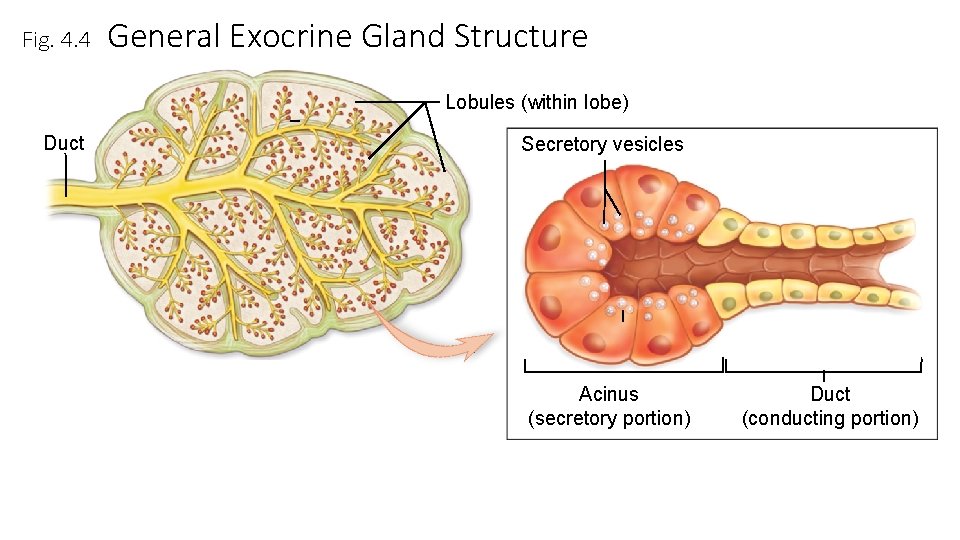
Fig. 4. 4 General Exocrine Gland Structure Lobules (within lobe) Duct Secretory vesicles Acinus (secretory portion) Duct (conducting portion)
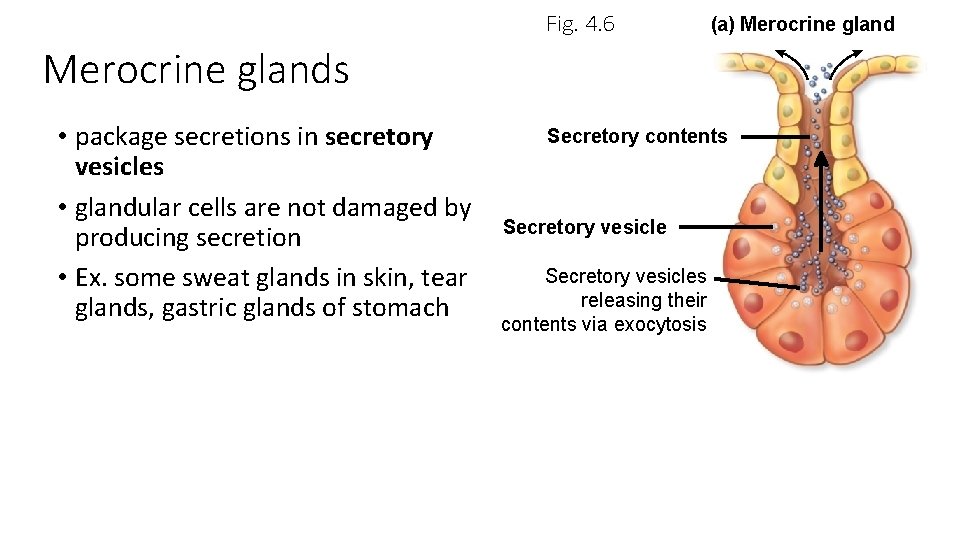
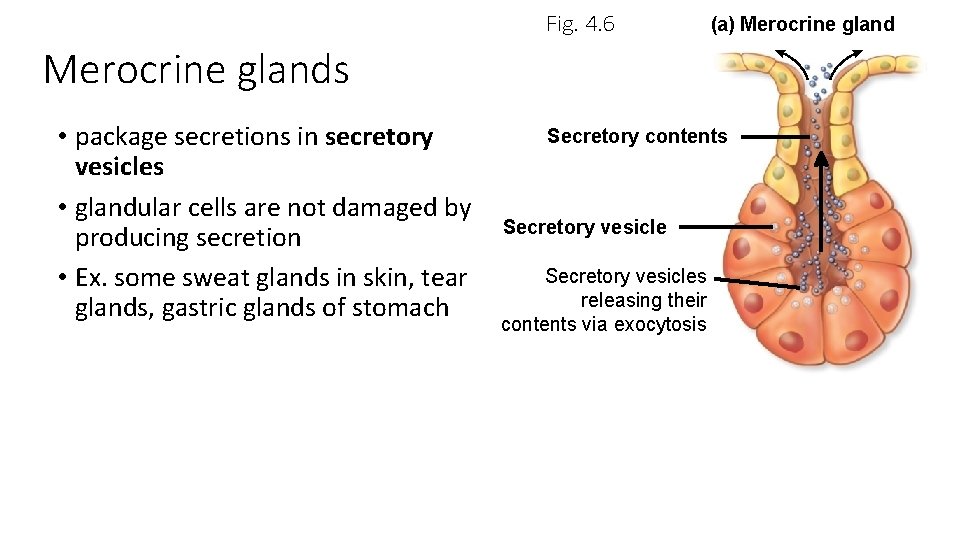
Fig. 4. 6 (a) Merocrine glands • package secretions in secretory vesicles • glandular cells are not damaged by producing secretion • Ex. some sweat glands in skin, tear glands, gastric glands of stomach Secretory contents Secretory vesicles releasing their contents via exocytosis
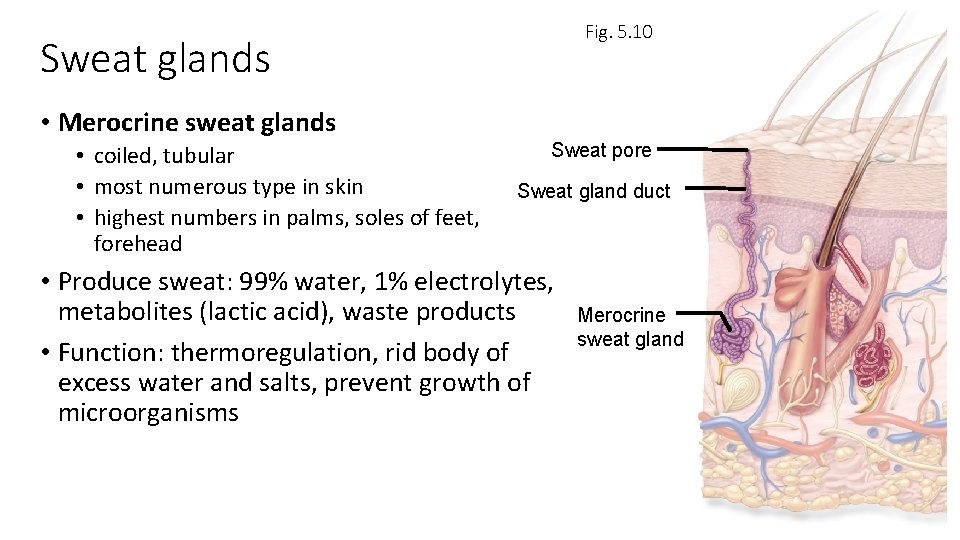
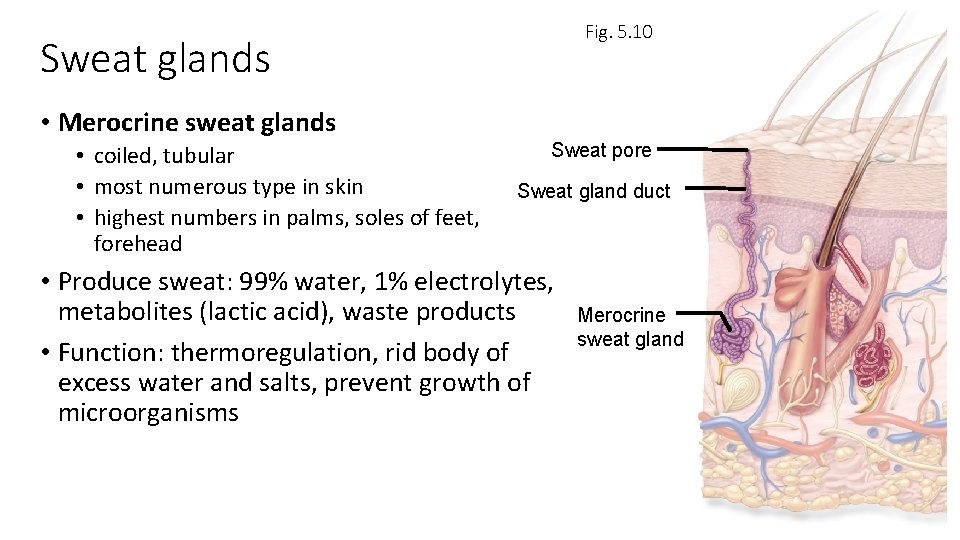
Fig. 5. 10 Sweat glands • Merocrine sweat glands • coiled, tubular • most numerous type in skin • highest numbers in palms, soles of feet, forehead Sweat pore Sweat gland duct • Produce sweat: 99% water, 1% electrolytes, metabolites (lactic acid), waste products • Function: thermoregulation, rid body of excess water and salts, prevent growth of microorganisms Merocrine sweat gland
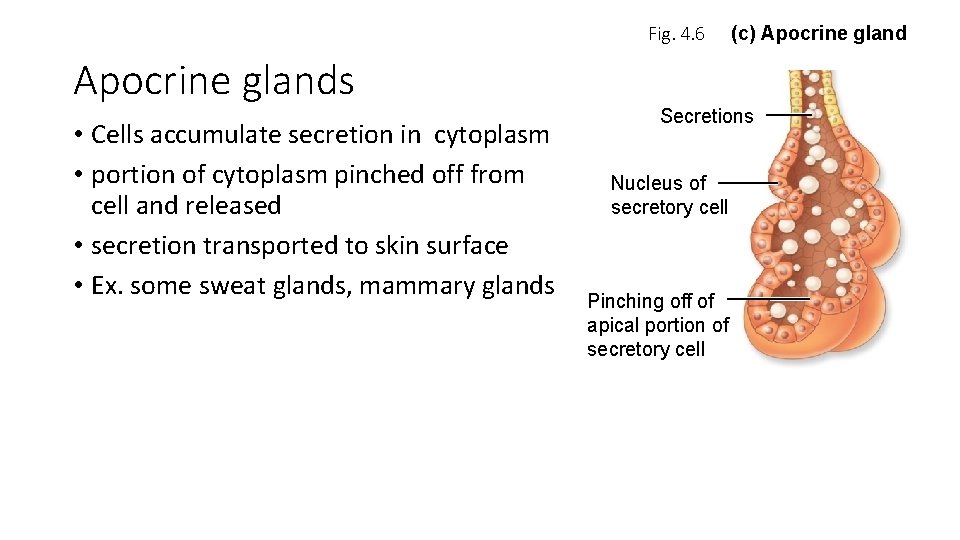
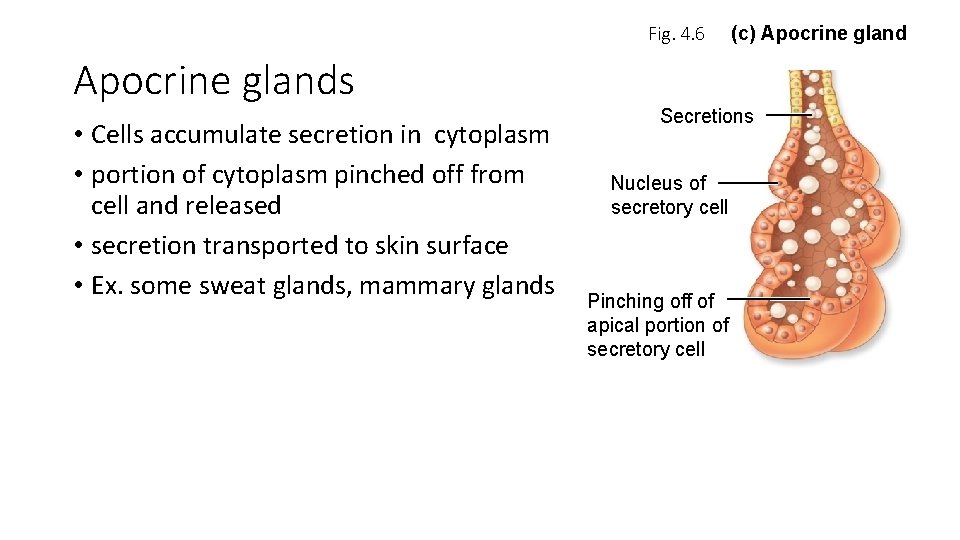
Fig. 4. 6 Apocrine glands • Cells accumulate secretion in cytoplasm • portion of cytoplasm pinched off from cell and released • secretion transported to skin surface • Ex. some sweat glands, mammary glands (c) Apocrine gland Secretions Nucleus of secretory cell Pinching off of apical portion of secretory cell
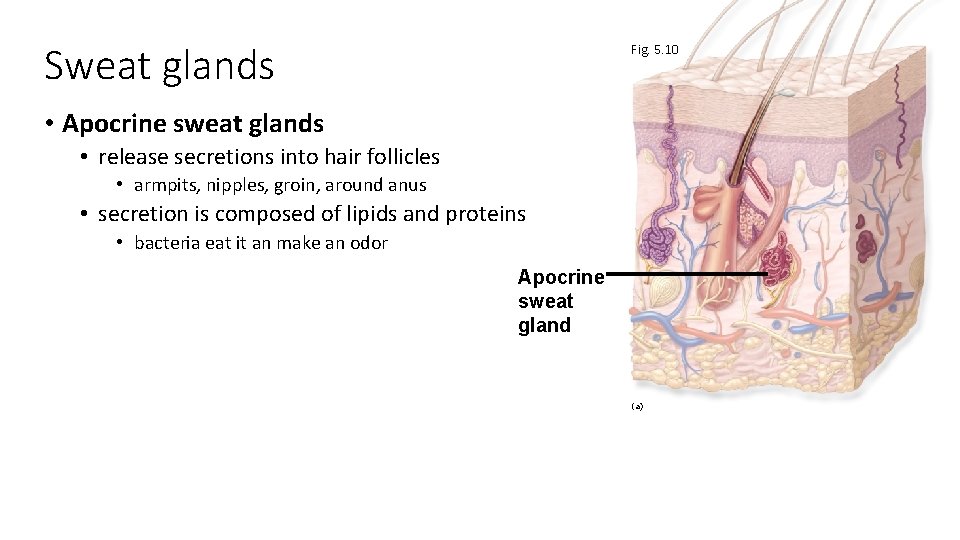
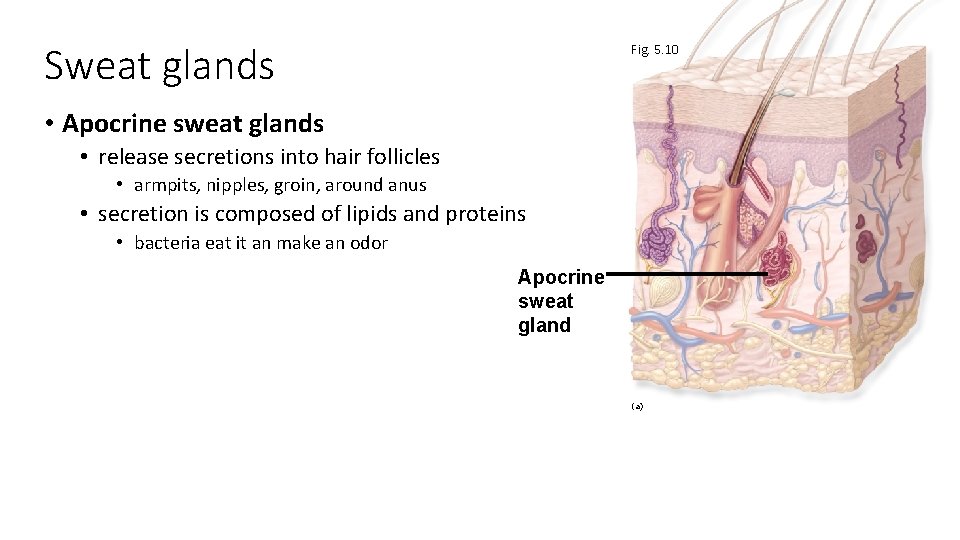
Sweat glands Fig. 5. 10 • Apocrine sweat glands • release secretions into hair follicles • armpits, nipples, groin, around anus • secretion is composed of lipids and proteins • bacteria eat it an make an odor Apocrine sweat gland (a)
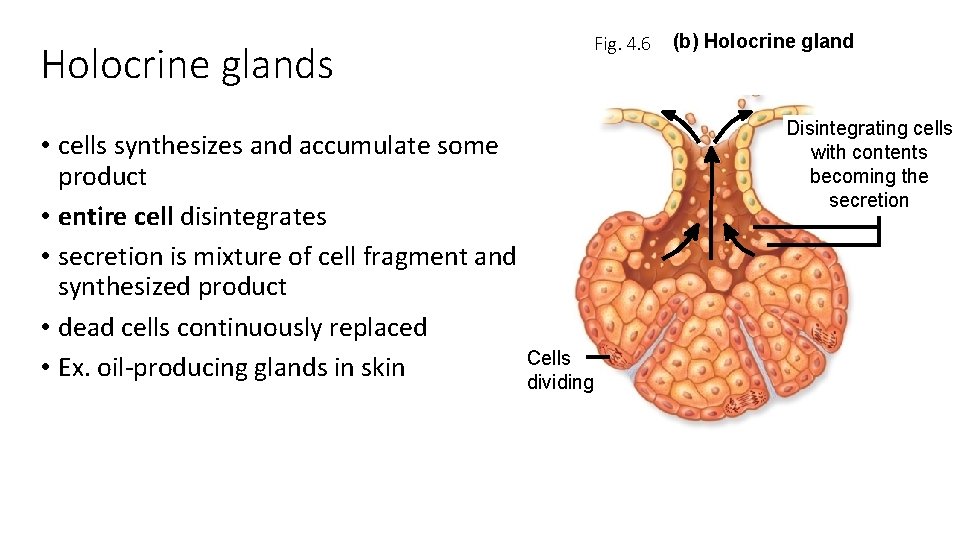
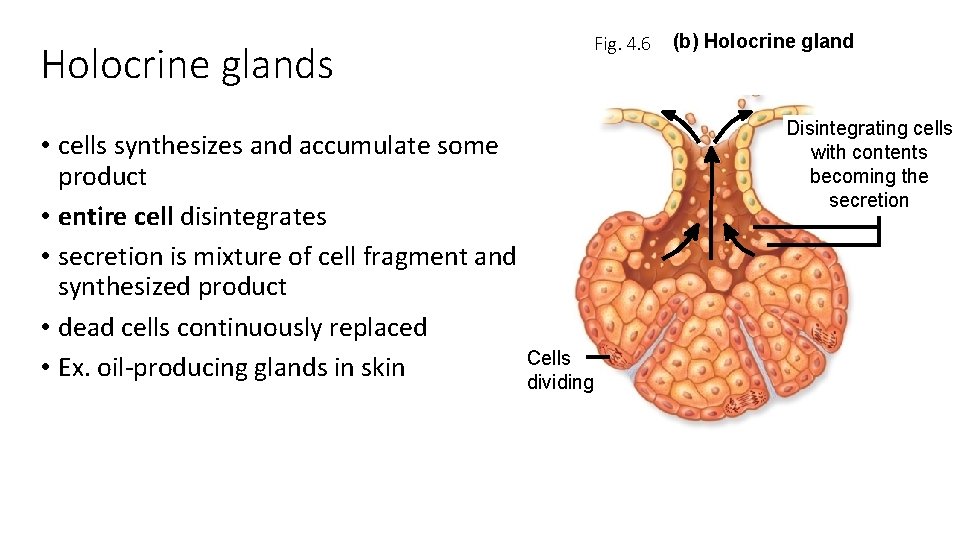
Holocrine glands • cells synthesizes and accumulate some product • entire cell disintegrates • secretion is mixture of cell fragment and synthesized product • dead cells continuously replaced • Ex. oil-producing glands in skin Fig. 4. 6 (b) Holocrine gland Disintegrating cells with contents becoming the secretion Cells dividing
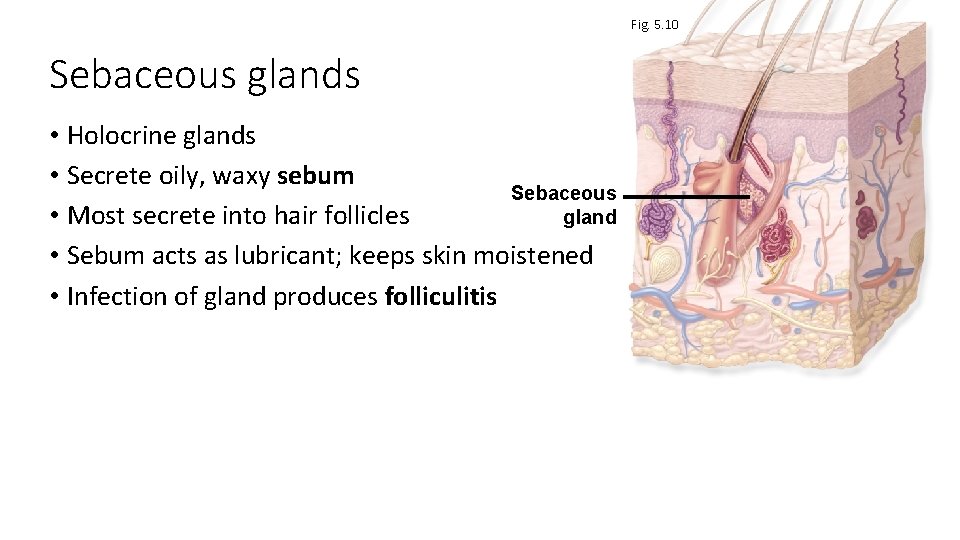
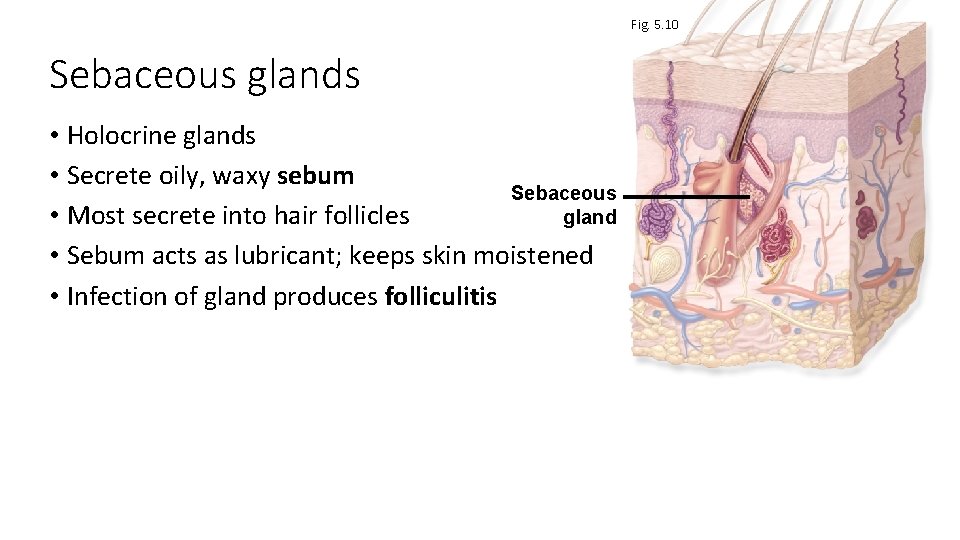
Fig. 5. 10 Sebaceous glands • Holocrine glands • Secrete oily, waxy sebum Sebaceous • Most secrete into hair follicles gland • Sebum acts as lubricant; keeps skin moistened • Infection of gland produces folliculitis
Subcutaneous layer • AKA hypodermis • not part of the integument • areolar connective tissue and adipose connective tissue