Chapter 4 The Integumentary System The Integumentary System



- Slides: 40
Chapter 4: The Integumentary System
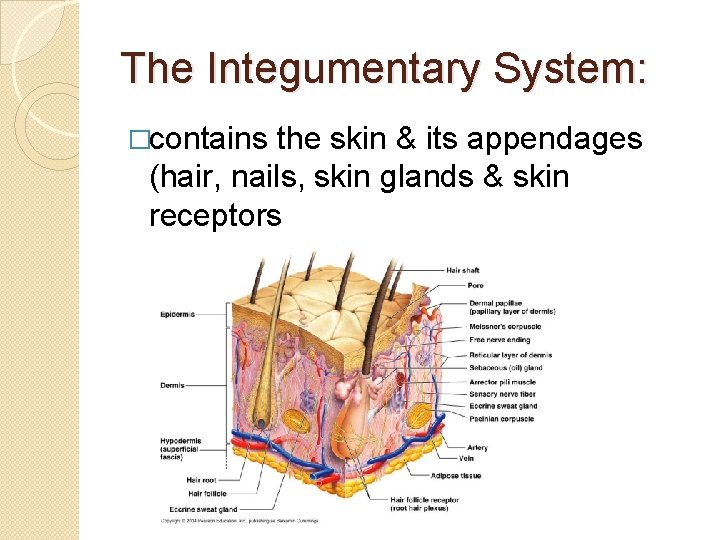
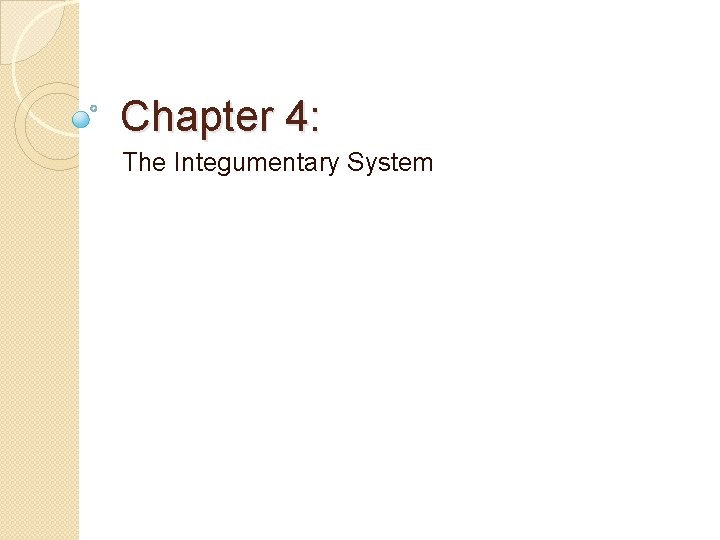
The Integumentary System: �contains the skin & its appendages (hair, nails, skin glands & skin receptors
Skin Facts!!!! - the largest (average size adults is about 1. 6 – 1. 9 m 2 (17 -20 square meters) - thinnest (slightly less than 0. 05 cm (1/50 inch) to 0. 3 cm (1/8 inch) - self-repairing - another name is integument
The skin is one of a group of simple sheetlike structures called membranes – thin, sheet-like structure that may have many important functions in the body – they are: 1. ) cover & protect the body surface 2. ) line body cavities 3. ) cover inner surfaces of hollow organs (dig, repro & resp passageways) 4. ) anchor organs to each other or to bone 5. ) secrete lubricating fluids that reduce friction (heartbeat, lung movement)
2 Major Types of Membranes: 1. ) Epithelial Membrane – composed of epithelial tissue & underlying layer of specialized connective tissue 3 types of epithelial membrane A. ) Cutaneous Membrane – covers body surfaces that are exposed to the external environment – the skin composes about 16% of body wt
B. ) Serous Membrane – lines cavities that are not open to external envir. & covers many of the organs inside these cavities - composed of 2 distinct layers of tissue – 1. ) an epithelial sheet (simple squamous) 2. ) a connective tissue layer - 2 types of serous membrane 1. ) parietal membrane – lines the wall of a cavity 2. )visceral membrane – covers the organ surface
- in the thoracic cavity, serous membrane is called pleura – surrounds a lung & lines the cavity - pleurisy – inflammation of the pleura - there is also pericardium – surrounds the heart - in the abdominal cavity, the serous membrane is called peritoneum – covers the abdominal viscera & lines the cavity - Peritonitis - inflammation of the peritoneum
C. ) Mucous Membrane – lines body surfaces opening directly to the exterior - secretes a thick, slimy material called mucus to keep the membrane moist & soft - mucocutaneous junction – junction where skin & mucous membrane meet
2 Major Membranes cont… 2. ) Connective Membrane – composed exclusively of various types of connective tissue – no epithelial cells are present – only 1 type: - Synovial Membranes – line the spaces between bones & joints - lubricated by synovial fluid
The Skin: - cutaneous membrane composed of: 1. ) Epidermis – outermost & thinnest layer of the skin - thick vs thin skin – only pertain to epidermis Ø most of the body’s skin is thin – 1 or more strata are absent – has hair Ø soles of feet, palms & other areas subject to friction are thick – all 5 strata are present – has fingerprints & footprints
Epidermis is composed of several types of epithelial cells a. ) keratinocytes – 90% of the epidermal cells – are filled w/ keratin – form outer skin b. ) melanocytes – 5% of the epidermal cells – give the skin color c. ) Langerhans cells – work with leukocytes to trigger immune rxns

- Cell layers – Strata – the 5 strata are named for structural or functional characteristics A. ) Stratum Corneum – “horny layer” - most superficial • composed of squamous cells that are dead when they reach the surface • their cytoplasm has been replaced by keratin (keratinization) & their cell membrane is thick & chemically resistant • Desmosomes are present to hold these cells together & strengthen it for wear & tear • Called the barrier area because it prevents H 2 O loss & envir. threats • Certain diseases can cause this strata to thicken beyond normal limits hyperkeratosis – produces thick, dry, scaly skin that is inelastic & causes painful fissures

B. ) Stratum Lucidum – “clear layer” • Keratinocytes are packed together & clear – nuclei are absent & indistinct cell outlines • Cells are filled w/ eleidin (substance that blocks H 2 O loss or penetration) which will become keratin C. ) Stratum Granulosum – “granular layer” • Where keratinization begins • Cells are arranged in a sheet 2 -4 layers deep & filled w/ keratohyalin (staining granules) • Cell degeneration has begun, so lysosomal enzymes are present in cytoplasm & nuclei are absent
D. ) Stratum Spinosum – “spiny layer” • Formed from 8 -10 layers of irregularly shaped cells w/ prominent desmosomes • Cells are rich in RNA so they initiate protein synthesis to make keratin E. ) Stratum Basale – “base layer” • Single layer of columnar cells • Only cells to undergo mitosis – about 10 -12% of all cells in this layer enter mitosis each day these last 2 layers are called Stratum Germinativum (growth layer)
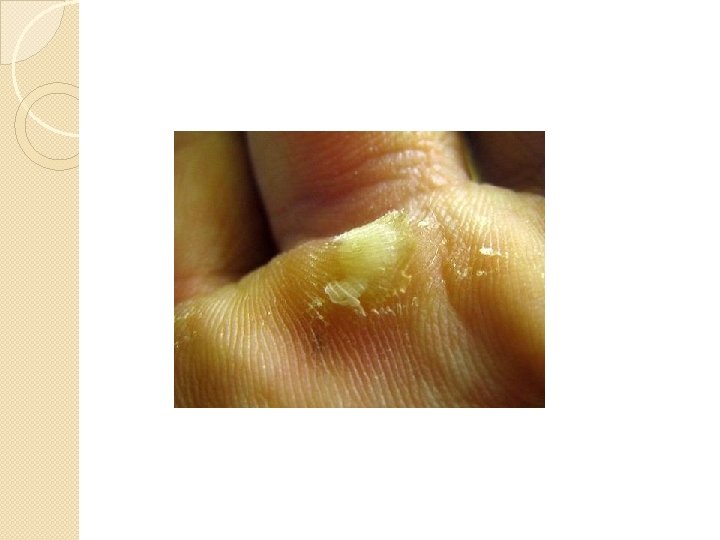
Epidermal Growth & Repair: Takes about 35 days for a new keratinocyte to complete mitosis, differentiation & movement to the surface of the epidermis Can be accelerated by abrasions – continuous abrasions can result in an increase in mitotic activity & shortened turnover time to produce an abnormally thick stratum corneum at the point of friction (a callus)
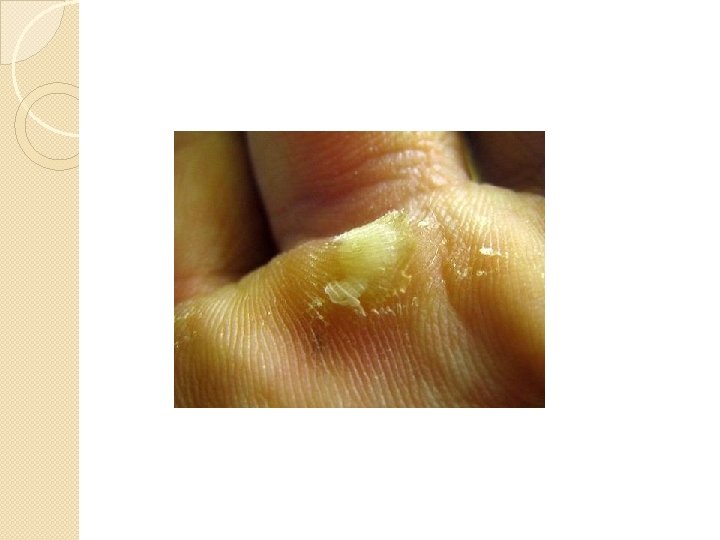
Dermal-Epidermal Junction – composed of basement membrane, fibrous elements & polysaccharide gel that cements the 2 layers together – functions as a mechanical support & partial barrier - detachment of the 2 layers in large amts could lead to infection & death!!!
2. ) Dermis – or corium – “true skin” – deeper & thicker of the 2 - may exceed 4 mm on soles & palms, thinnest on eyelids & penis - generally thinner on the ventral side & thicker on the dorsal - mechanical strength lies in the dermis, also provides storage for H 2 O & electrolytes contains somatic sensory receptors that detect pain, pressure, touch & temp. also has muscle fibers, hair follicles, sweat & sebaceous glands & blood vessels
Dermal Cell Layers: A. ) Papillary Layer – contains papillae (bumps) made of loose connective tissue & thin collagenous & elastic fibers • Creates the fingerprint & footprint that allows us to grip things B. ) to up Reticular Layer – thicker, w/ more network of fibers • Contains collagenous & elastic fibers – able rebound • Point of attachment for skeletal & smooth muscles - arrector pili muscles – causes hair to stand in goose pimples
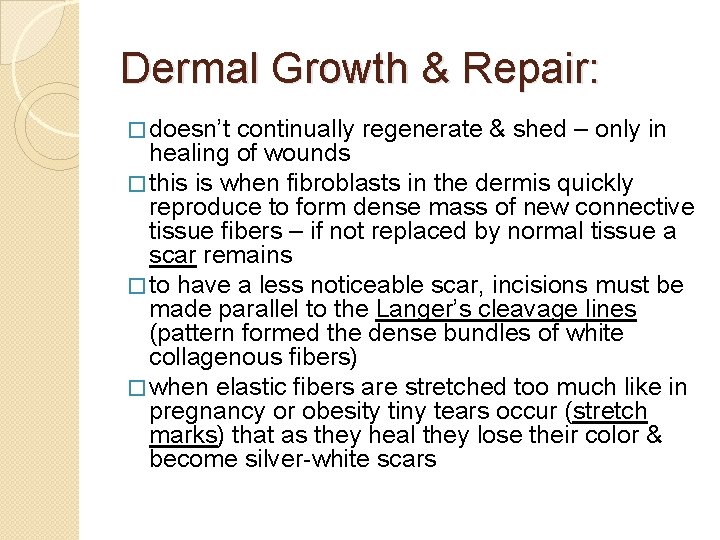
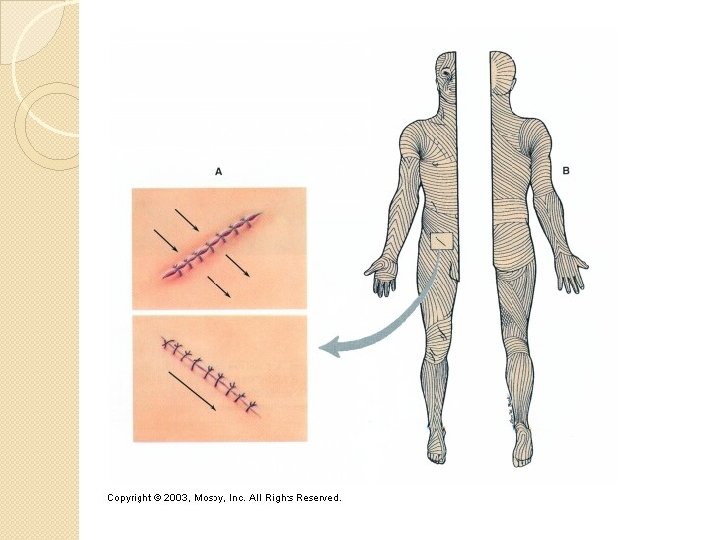
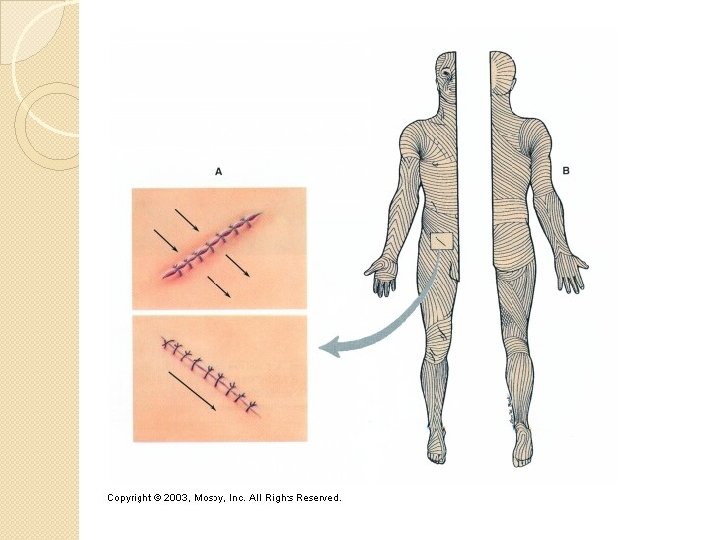
Dermal Growth & Repair: � doesn’t continually regenerate & shed – only in healing of wounds � this is when fibroblasts in the dermis quickly reproduce to form dense mass of new connective tissue fibers – if not replaced by normal tissue a scar remains � to have a less noticeable scar, incisions must be made parallel to the Langer’s cleavage lines (pattern formed the dense bundles of white collagenous fibers) � when elastic fibers are stretched too much like in pregnancy or obesity tiny tears occur (stretch marks) that as they heal they lose their color & become silver-white scars

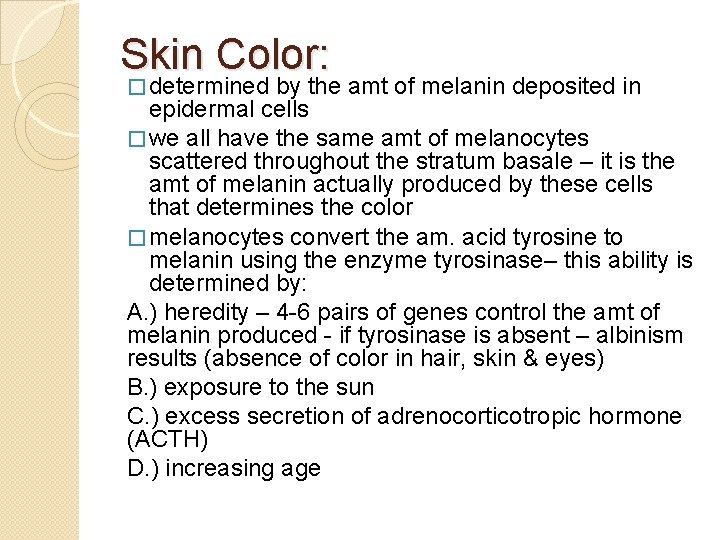
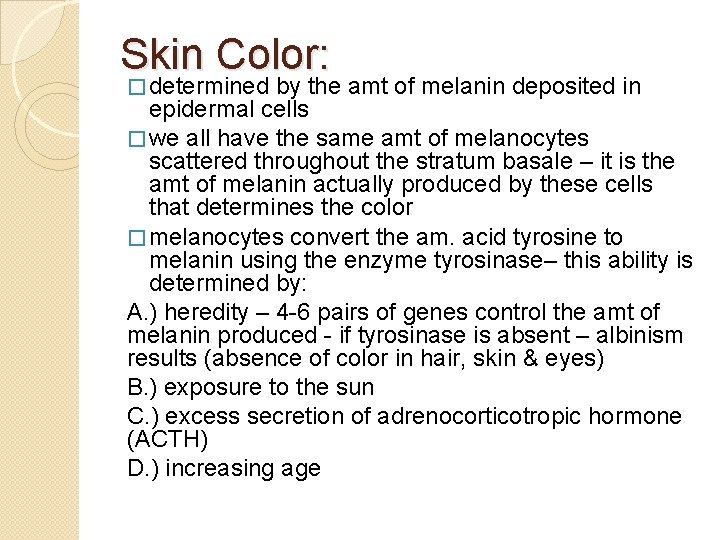
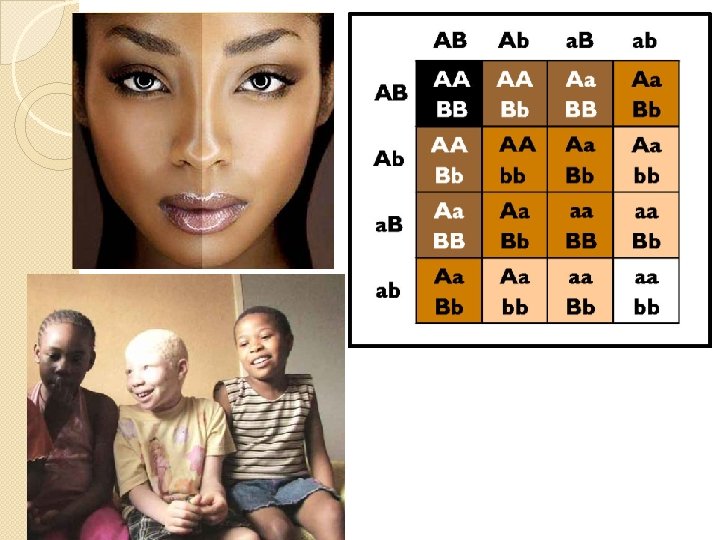
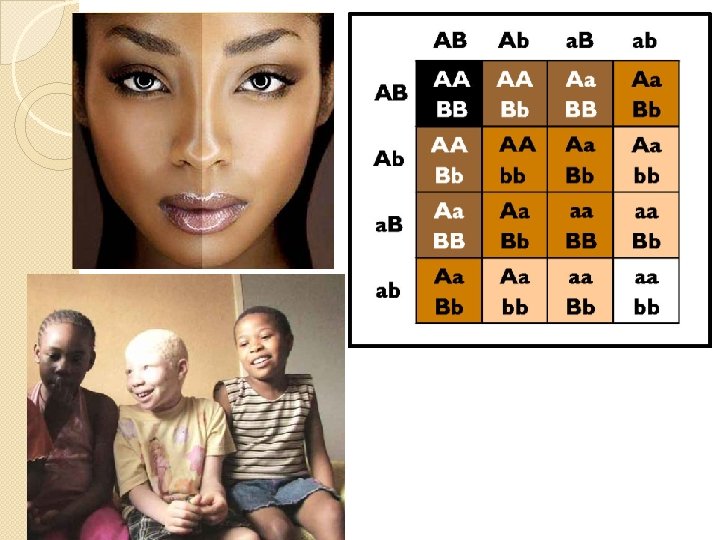
Skin Color: � determined by the amt of melanin deposited in epidermal cells � we all have the same amt of melanocytes scattered throughout the stratum basale – it is the amt of melanin actually produced by these cells that determines the color � melanocytes convert the am. acid tyrosine to melanin using the enzyme tyrosinase– this ability is determined by: A. ) heredity – 4 -6 pairs of genes control the amt of melanin produced - if tyrosinase is absent – albinism results (absence of color in hair, skin & eyes) B. ) exposure to the sun C. ) excess secretion of adrenocorticotropic hormone (ACTH) D. ) increasing age
Skin Functions: 1. ) Protection – 1 st line of defense for the body – protects the body from: A. ) Daily Invasion D. ) Water Loss B. ) Entry of harmful chemicals E. ) Sun’s rays C. ) Tears & Cuts F. ) Pain How does this function work? - Surface Film – produced by mixing residue & secretions from sweat & sebaceous glands with epithelial cells that are being cast off from the epidermis Functions: a. ) antibacterial & antifungal activity d. ) lubrication b. ) hydration of skin surface e. ) toxic agent blockade c. ) Caustic irritant buffering
2. ) Sensation – millions of somatic sensory receptors serve as receivers for the body, keeping it informed of changes in the envir. 3. ) Movement & Growth w/out Injury – skin is supple & elastic 4. ) Excretion – gets rid of H 2 O, urea, ammonia, uric acid to regulate sweat vol. & content 5. ) Vitamin D Production – UV light triggers molecules in the skin to convert to precursors that will produce Vitamin D to be used in biological rxns
6. ) Immunity – Langerhans cells function w/ helper T cells to trigger immune rxns in certain diseases 7. ) Temperature Regulation – done by: a. ) sweat secretion – cools the body by evaporation b. ) blood flows close to the body surface - temperature is detected by the hypothalamus - which will use negative feedback until the homeostatic set point for normal body temp. is reached – usually 37°C
Appendages of the Skin: 1. ) Hair • Areas w/ no hair: lips, soles of the feet, palms of the hands, nipples, & certain regions of the genitalia • Hair follicles dvlp before birth – will be called lanugo (“down”) – is extremely fine & most will be lost before birth • Will be replaced by vellus hair – stronger, fine & less pigmented
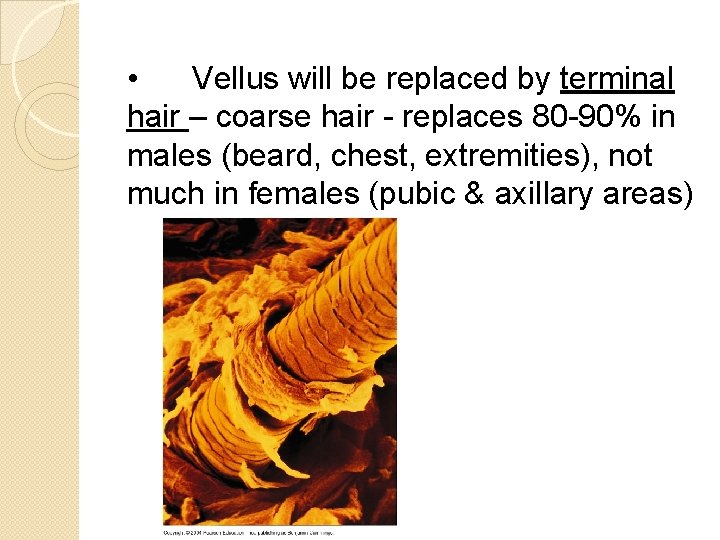
• Vellus will be replaced by terminal hair – coarse hair - replaces 80 -90% in males (beard, chest, extremities), not much in females (pubic & axillary areas)
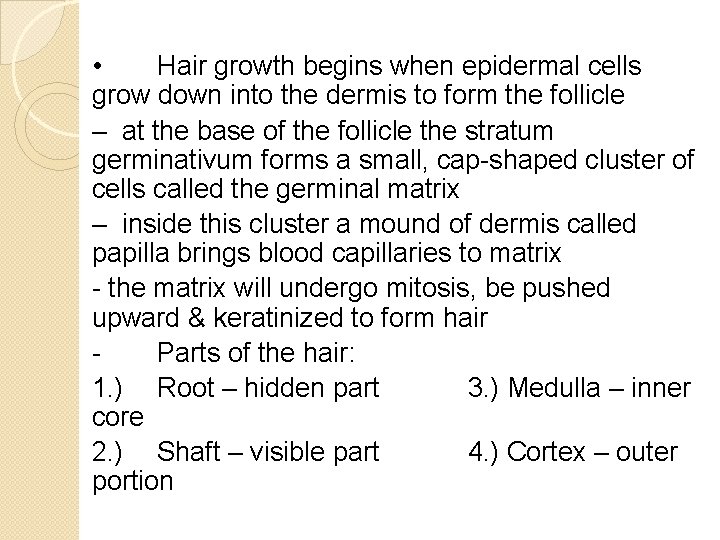
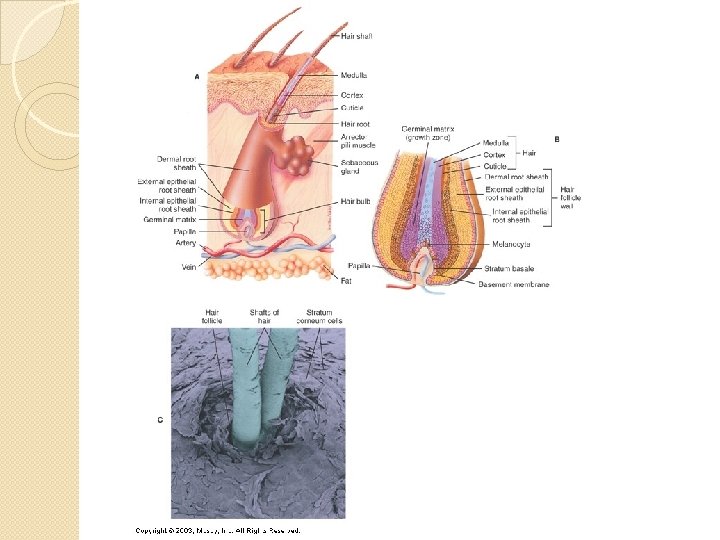
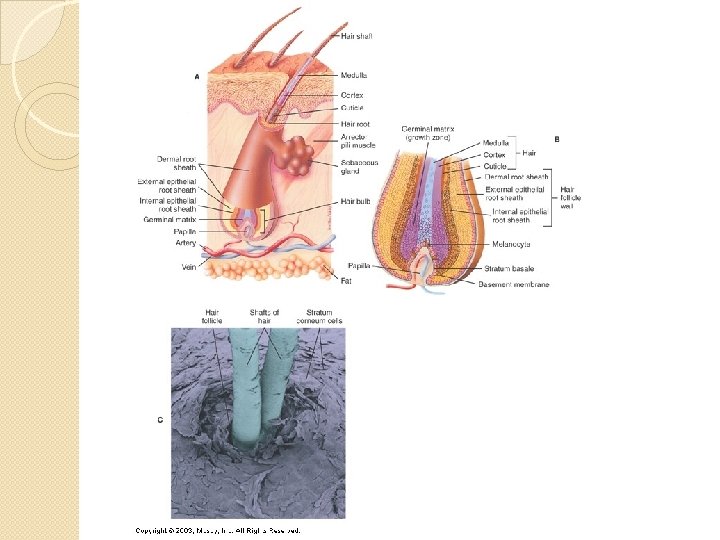
• Hair growth begins when epidermal cells grow down into the dermis to form the follicle – at the base of the follicle the stratum germinativum forms a small, cap-shaped cluster of cells called the germinal matrix – inside this cluster a mound of dermis called papilla brings blood capillaries to matrix - the matrix will undergo mitosis, be pushed upward & keratinized to form hair Parts of the hair: 1. ) Root – hidden part 3. ) Medulla – inner core 2. ) Shaft – visible part 4. ) Cortex – outer portion
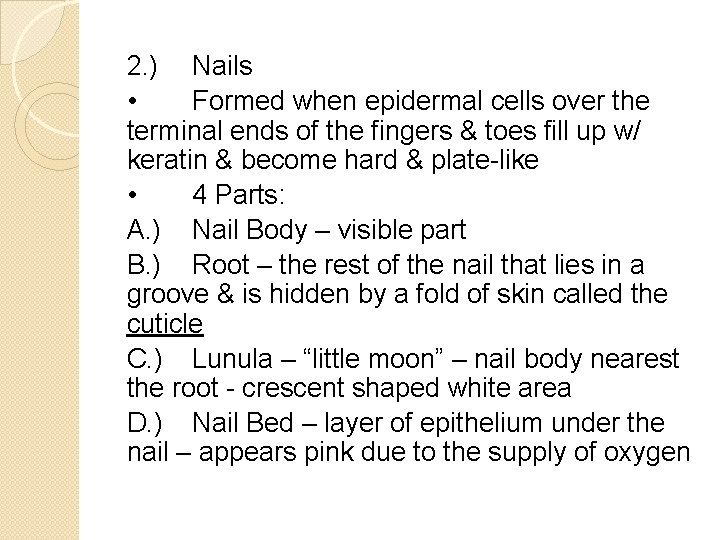
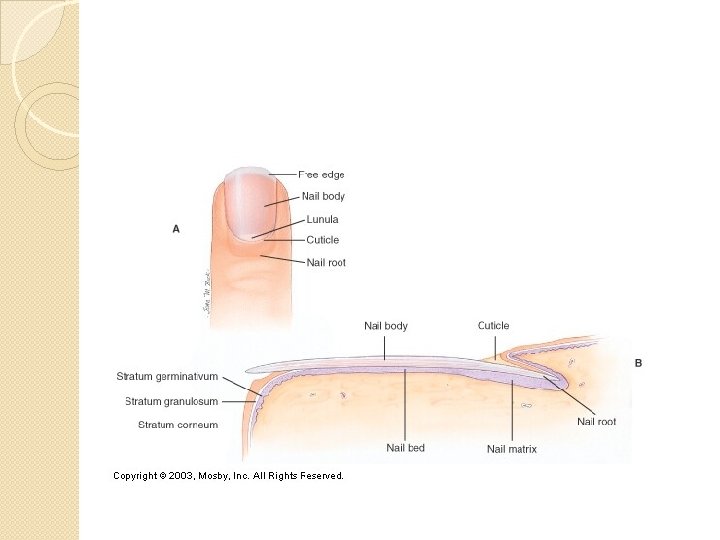
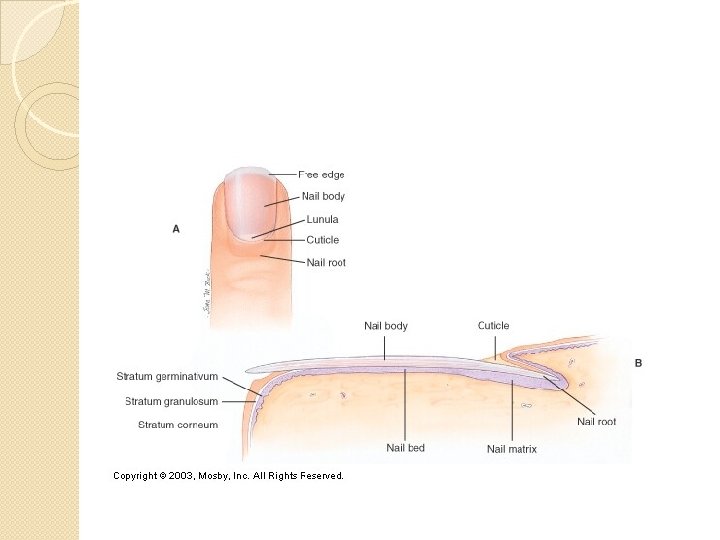
2. ) Nails • Formed when epidermal cells over the terminal ends of the fingers & toes fill up w/ keratin & become hard & plate-like • 4 Parts: A. ) Nail Body – visible part B. ) Root – the rest of the nail that lies in a groove & is hidden by a fold of skin called the cuticle C. ) Lunula – “little moon” – nail body nearest the root - crescent shaped white area D. ) Nail Bed – layer of epithelium under the nail – appears pink due to the supply of oxygen
3. ) Skin Glands • Includes 3 kinds: A. ) Sudoriferous Glands – sweat glands – most numerous – classified 2 groups: 1. ) Eccrine Sweat Glands • Most numerous, imp & widespread • Small & distributed over total body surface except for the lips, ear canal, glans penis & nail bed • Produce perspiration (sweat) • Sweat secreted through pores eliminates waste • Maintains constant body temp • Numerous on palms, soles, forehead & upper torso
2. ) Apocrine Sweat Glands • Located in armpits, areola of breast, & pigmented skin around anus • Larger • Enlarge & begin function at puberty • Secretes a thicker, milky secretion – in females it can show cyclic changes linked to menstrual cycle • Odor comes from the contamination of this secretion by skin bacteria
B. ) Sebaceous Glands – oil glands • Secrete oil for hair & skin • Located where hair grows & other small places where it doesn’t (lip, eyelid, etc) • Secrete sebum – contains triglycerides, waxes, fatty acids & cholesterol to produce an antifungal effect • Vary in size – not located on palms or soles • Sebum secretion increases during adolescence when stimulated by increased blood levels of sex hormones • Frequent sebum accumulation enlarges some of the ducts forming white pimples sebum will darken when oxidized to form a blackhead
C. ) Ceruminous Glands – modification of apocrine glands • Ducts open onto free surface of skin in external ear canal, or w/ sebaceous glands into the necks of hair follicles in this area • Secretions mixed with sebaceous glands produces cerumen (earwax) • Protects ear canal skin from dehydration • Can harden & cause blockage which leads to loss of hearing
4. Skin Receptors - 5 types: - Meissner Corpuscles – light touch Pacinian Corpuscles – pressure Free nerve endings – pain Krauses’s end bulbs – cold Others