Chapter 6 The Integumentary System Integumentary System The

- Slides: 86
Chapter 6 The Integumentary System
Integumentary System • The integumentary system consists of the skin and its derivatives. – Nails, hair, sweat glands, sebaceous glands • The integument is the skin covering the body. – Also known as the cutaneous membrane – Barrier to the outside world – Visual indicator of our physiology and health – Its scientific study and treatment termed dermatology*
Composition of the Integument • The integument – Body’s largest organ – Protects internal body structures – Accounts for 7 -8% of body weight – Area ranges between 1. 5 -2. 0 m 2 – Thickness ranges between 1. 5 mm and 4. 0 mm
Composition of the Integument • Integument composed of all tissue types – Surface covered by an epithelium – Underlying connective tissue: • provides strength and resilience • contains smooth muscle associated with hair follicles – Nervous tissue: • provides information about touch, pressure, temperature, and pain
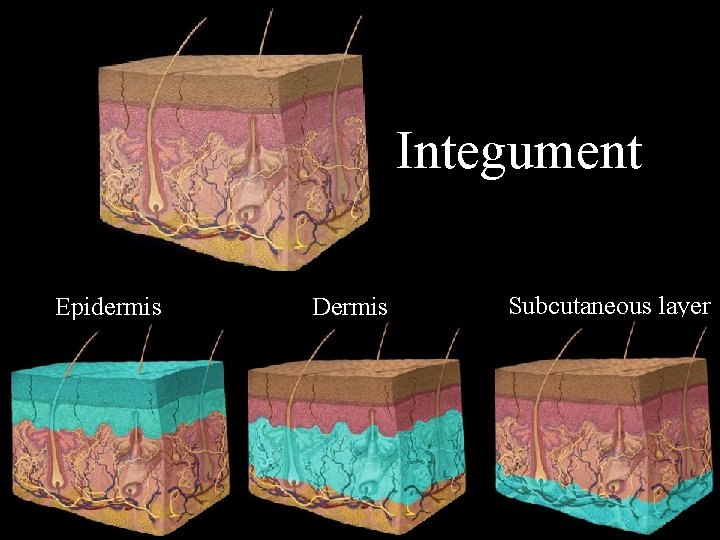
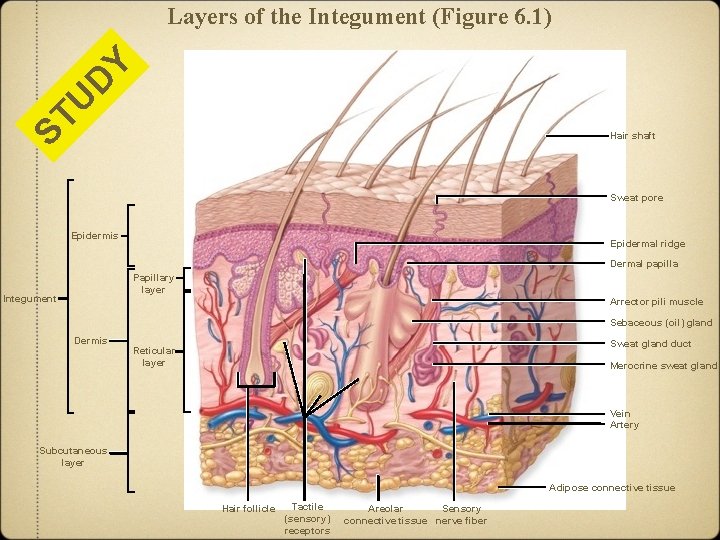
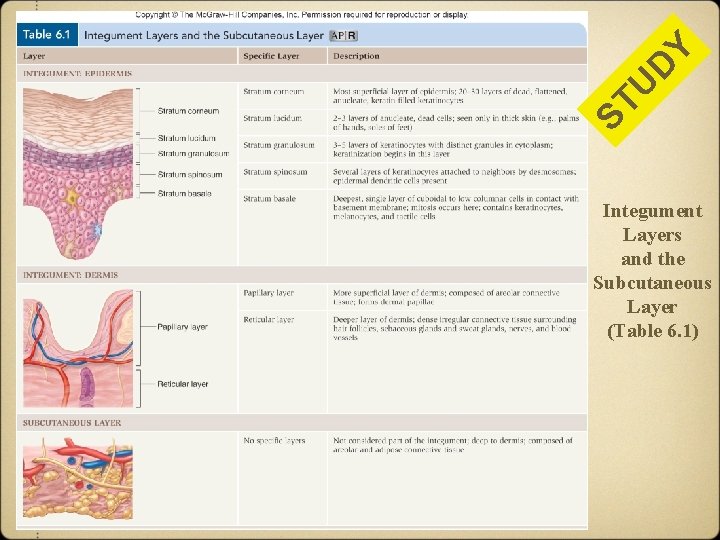
Composition of the Integument • Layers of the integument – Epidermis - stratified squamous epithelium – Dermis • deeper layer • primarily dense irregular connective tissue - Subcutaneous layer • Deep to dermis • Layer of alveolar and connective tissue • Termed subcutaneous layer or hypodermis • Not part of the integumentary system • Closely involved with structure and function of skin
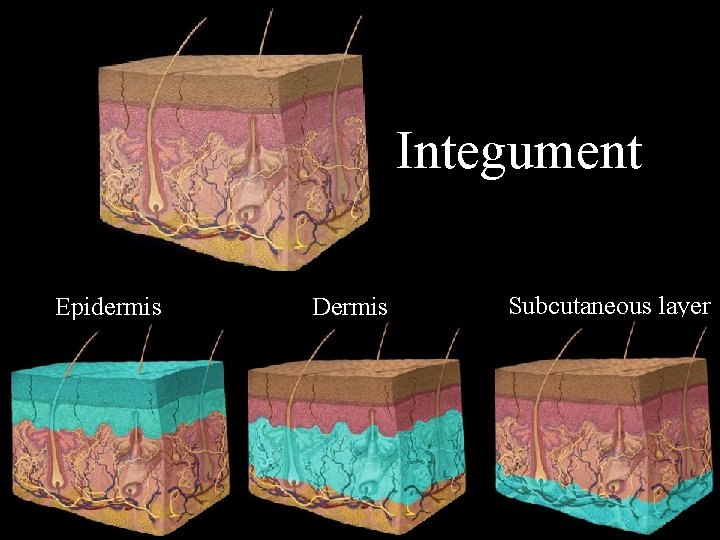
Integument Epidermis Dermis Subcutaneous layer
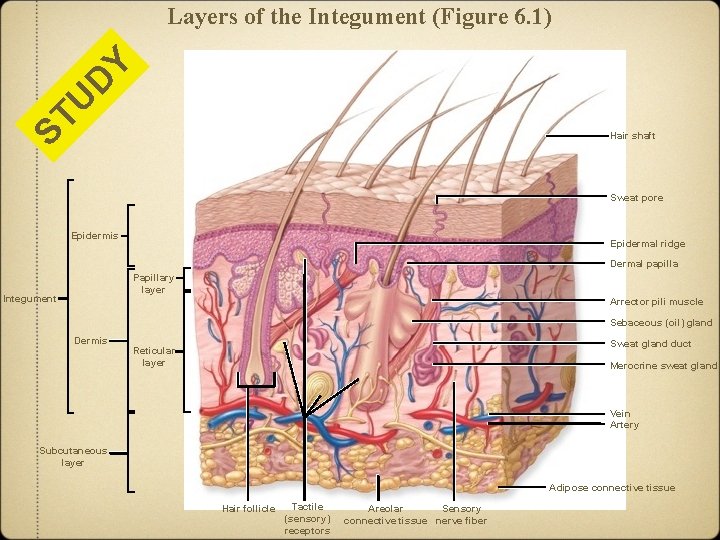
ST U D Y Layers of the Integument (Figure 6. 1) Hair shaft Sweat pore Epidermis Epidermal ridge Dermal papilla Papillary layer Integument Arrector pili muscle Sebaceous (oil) gland Dermis Sweat gland duct Reticular layer Merocrine sweat gland Vein Artery Subcutaneous layer Adipose connective tissue Hair follicle Tactile (sensory) receptors Areolar Sensory connective tissue nerve fiber
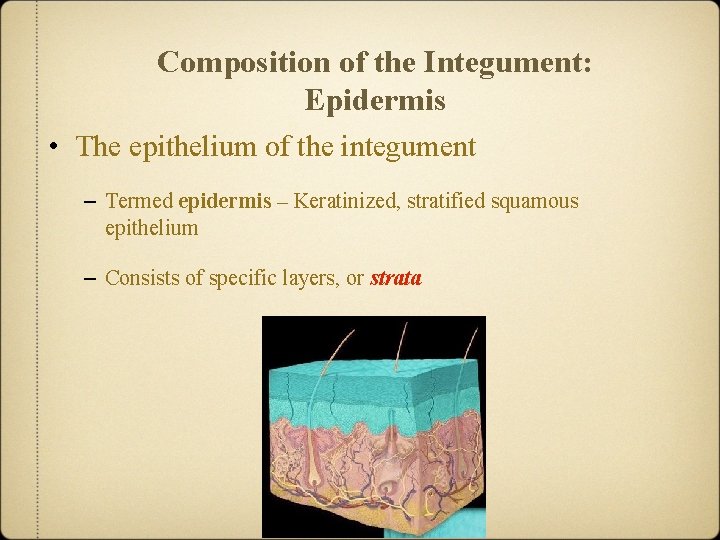
Composition of the Integument: Epidermis • The epithelium of the integument – Termed epidermis – Keratinized, stratified squamous epithelium – Consists of specific layers, or strata
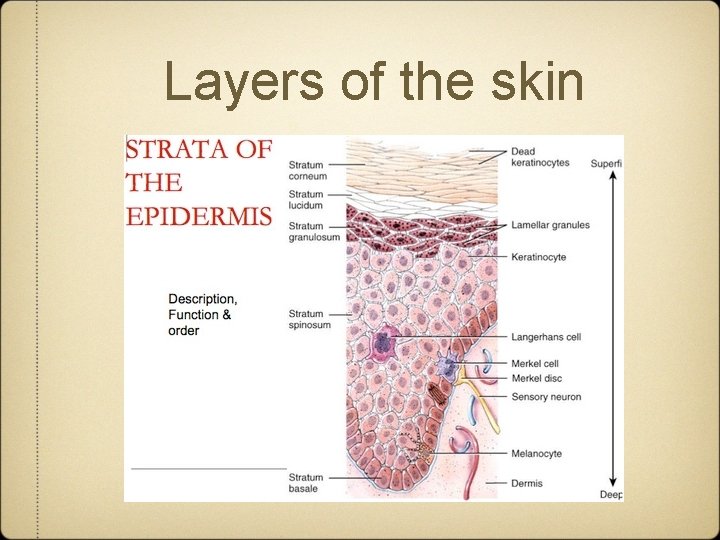
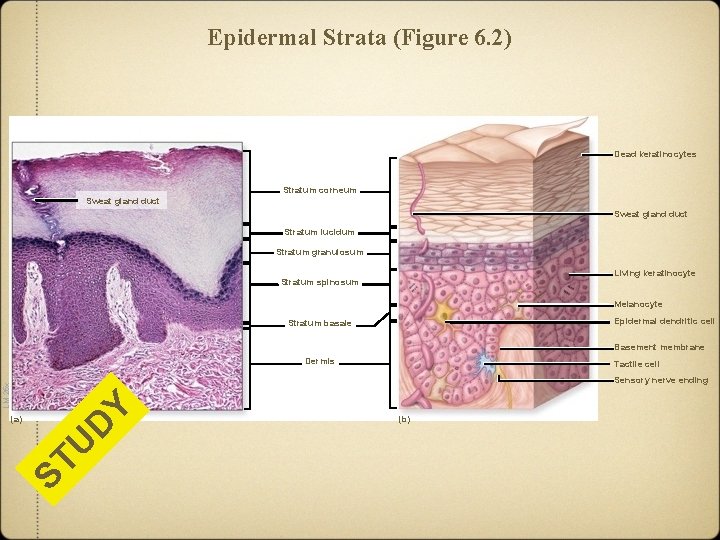
Composition of the Integument: Epidermis • The epithelium of the integument – Layers from deep to superficial: • stratum basale - living • stratum spinosum - living • stratum granulosum - living, but dying • stratum lucidum -- dead • stratum corneum - dead – first three layers with living keratinocytes – most superficial two layers with dead keratinocytes
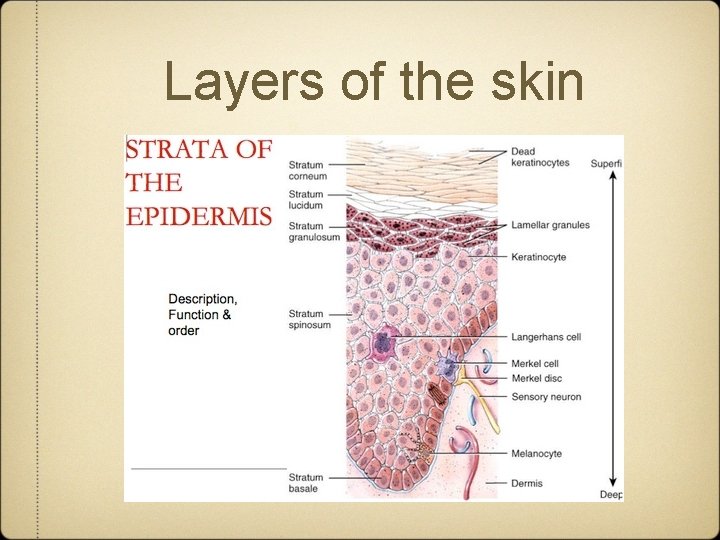
Layers of the skin
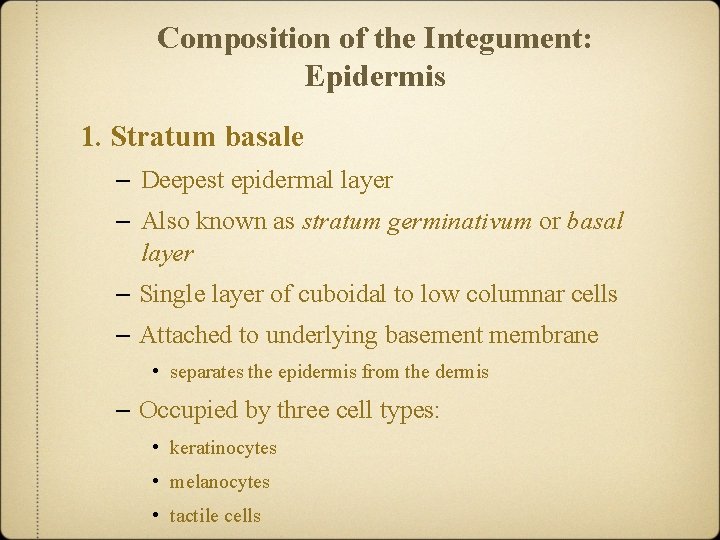
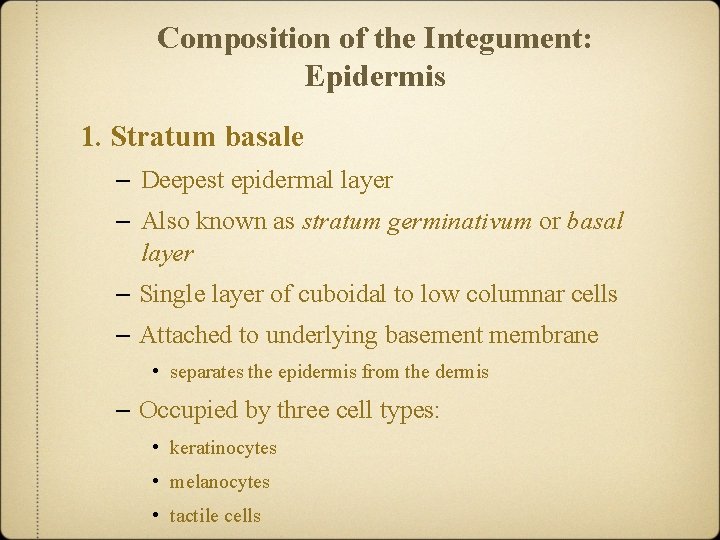
Composition of the Integument: Epidermis 1. Stratum basale – Deepest epidermal layer – Also known as stratum germinativum or basal layer – Single layer of cuboidal to low columnar cells – Attached to underlying basement membrane • separates the epidermis from the dermis – Occupied by three cell types: • keratinocytes • melanocytes • tactile cells
Composition of the Integument: Epidermis Stratum basale • Keratinocytes – Most abundant cells in epidermis – Found in all layers – Many keratinocytes stem cells present in this layer – Divide to regenerate new cells – Replace old cells shed at the surface – Name derived from the synthesis of keratin • protein that strengthens the epidermis
Composition of the Integument: Epidermis Stratum basale • Melanocytes – Scattered among the keratinocytes – Produce and store pigment (melanin) in response to UV (ultraviolet) light. – Transfer pigment granules (melanosomes) into keratinocytes • accumulate around nucleus of keratinocytes • shield nuclear DNA from UV radiation • responsible for the darker tones of skin
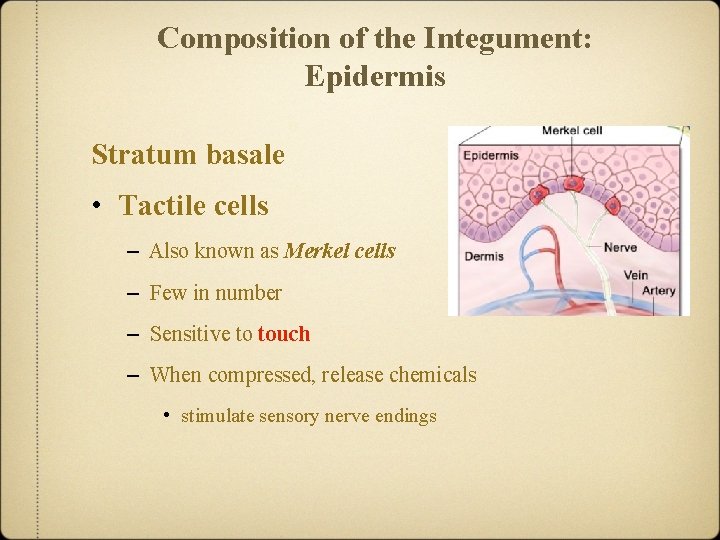
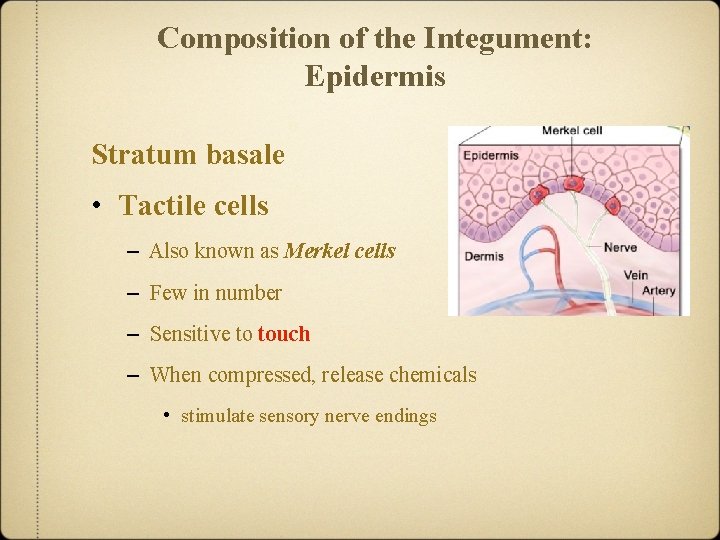
Composition of the Integument: Epidermis Stratum basale • Tactile cells – Also known as Merkel cells – Few in number – Sensitive to touch – When compressed, release chemicals • stimulate sensory nerve endings
Composition of the Integument: Epidermis Stratum spinosum – Several layers of polygonal keratinocytes – Also known as spiny layer • named for spiny appearance on microscopy – Daughter cells from stratum basale pushed into this layer – Begin to develop into specialized, non-dividing keratinocytes • some in deepest level still dividing cells – Non-dividing keratinocytes attached by intercellular junctions • called desmosomes
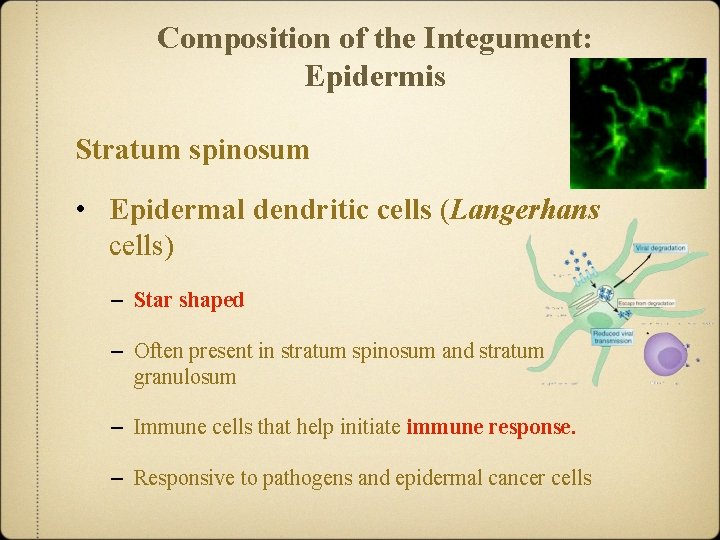
Composition of the Integument: Epidermis Stratum spinosum • Epidermal dendritic cells (Langerhans cells) – Star shaped – Often present in stratum spinosum and stratum granulosum – Immune cells that help initiate immune response. – Responsive to pathogens and epidermal cancer cells
Composition of the Integument: Epidermis Stratum granulosum – Three to five layers of keratinocytes – Also known as granular layer – Superficial to the stratum spinosum – First layer of keratinization • process where keratinocytes fill with keratin • causes nucleus and organelles to disintegrate • fully keratinized cell dead but structurally sound • process not complete until more superficial layers
Composition of the Integument: Epidermis Stratum lucidum – Two to three layers of keratinocytes – Translucent layer also known as clear layer – Superficial to the stratum granulosum – Found only on thick skin within the palms and soles – Filled with a translucent protein, eleidin • intermediate product in keratin maturation
Composition of the Integument: Epidermis Stratum corneum – 20 to 30 layers of dead, interlocking keratinized cells • cells anucleate (without a nucleus) and tightly packed • plasma membrane enclosing keratin protein – Also known as the hornlike layer – Most superficial layer of epidermis – Surface unsuitable for the growth of many microorganisms • secretions of exocrine glands also helping prevent growth
Composition of the Integument: Epidermis Stratum corneum • Migration of keratinocytes – Originate from stem cells in stratum basale – Migrate through strata to stratum corneum over two weeks • undergoing structural changes – Remain in stratum corneum another two weeks WHERE does 80% of all the dust in your – Are shed home originate? Your skin !!
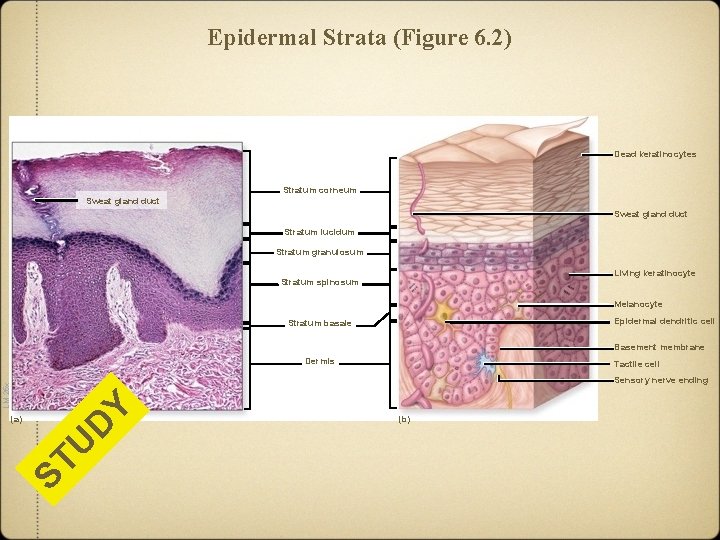
Epidermal Strata (Figure 6. 2) Dead keratinocytes Stratum corneum Sweat gland duct Stratum lucidum Stratum granulosum Living keratinocyte Stratum spinosum Melanocyte Epidermal dendritic cell Stratum basale Basement membrane Dermis Tactile cell D ST U (a) Y LM 25 x Sensory nerve ending (b)
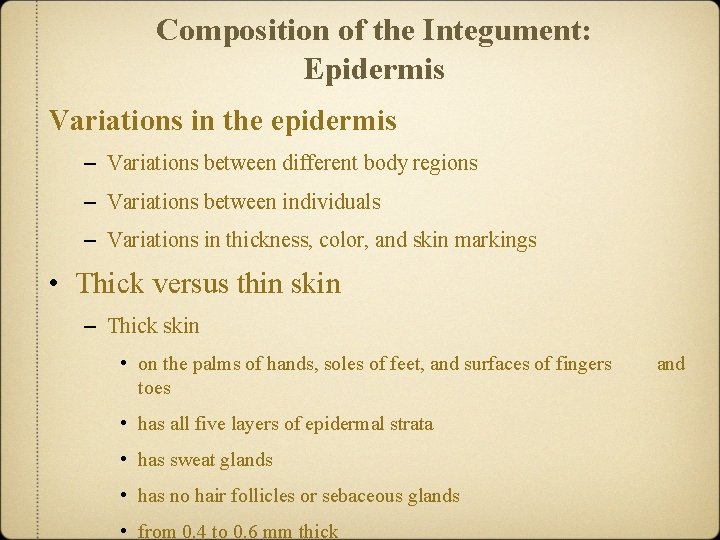
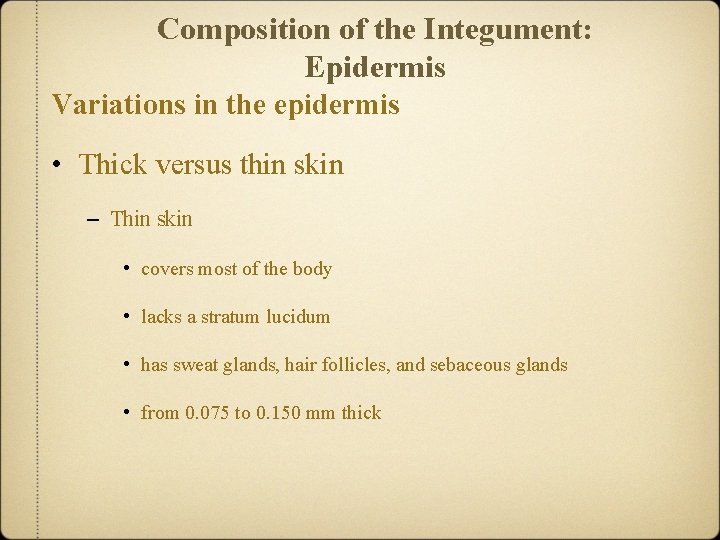
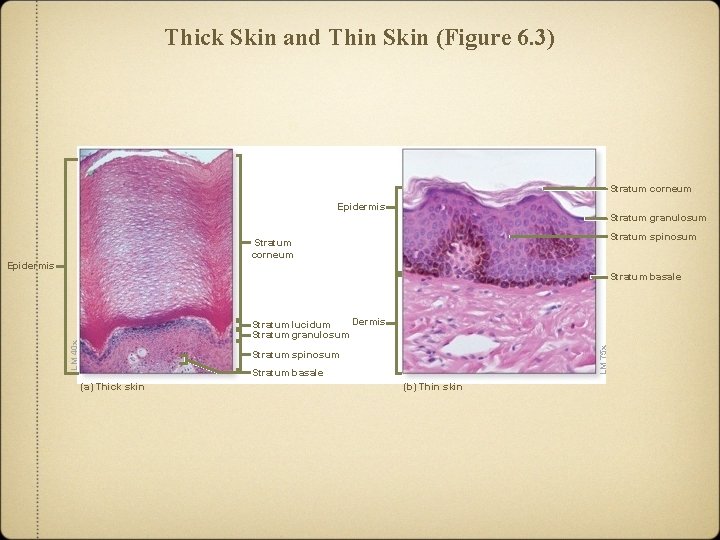
Composition of the Integument: Epidermis Variations in the epidermis – Variations between different body regions – Variations between individuals – Variations in thickness, color, and skin markings • Thick versus thin skin – Thick skin • on the palms of hands, soles of feet, and surfaces of fingers toes • has all five layers of epidermal strata • has sweat glands • has no hair follicles or sebaceous glands • from 0. 4 to 0. 6 mm thick and

Thin Skin Bl G ue ro M up a ? ? n Thick Skin
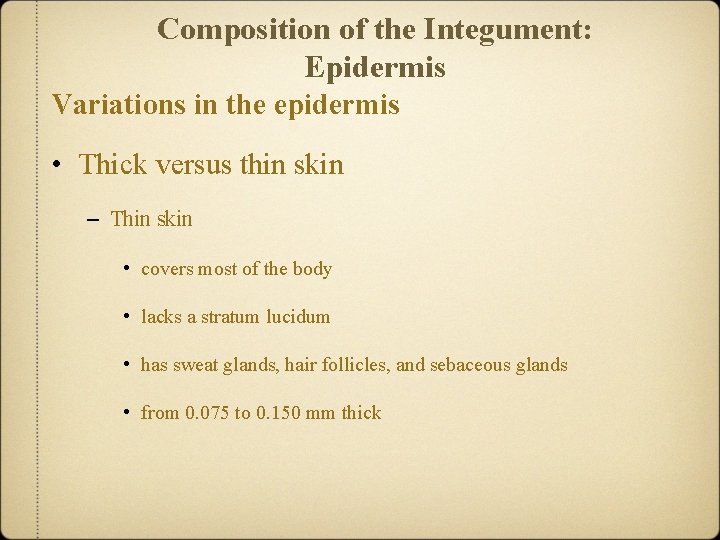
Composition of the Integument: Epidermis Variations in the epidermis • Thick versus thin skin – Thin skin • covers most of the body • lacks a stratum lucidum • has sweat glands, hair follicles, and sebaceous glands • from 0. 075 to 0. 150 mm thick
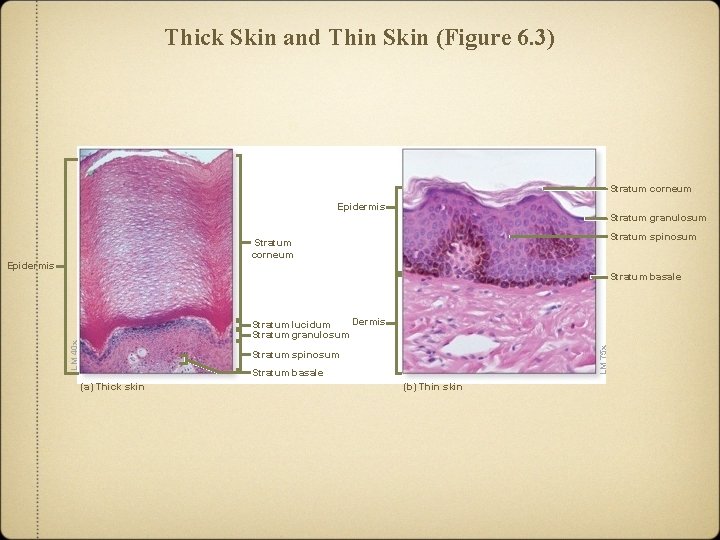
Thick Skin and Thin Skin (Figure 6. 3) Stratum corneum Epidermis Stratum granulosum Stratum spinosum Stratum corneum Epidermis Stratum basale LM 75 x LM 40 x Dermis Stratum lucidum Stratum granulosum Stratum spinosum Stratum basale (a) Thick skin (b) Thin skin
Composition of the Integument: Epidermis Variations in the epidermis • Coloring from hemoglobin – Hemoglobin: an oxygen binding compound • present in red blood cells – Bright red color upon binding oxygen – Gives blood vessels in dermis a reddish tint – Seen most easily in fair skinned individuals – More visible if blood vessels dilate
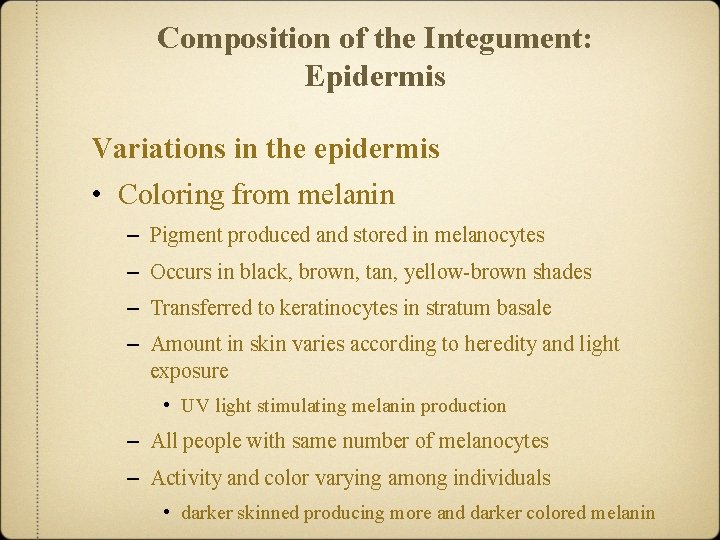
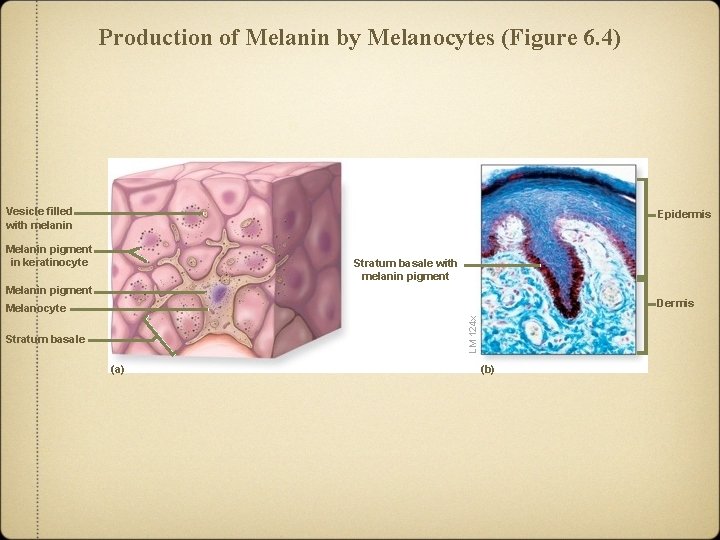
Composition of the Integument: Epidermis Variations in the epidermis • Coloring from melanin – Pigment produced and stored in melanocytes – Occurs in black, brown, tan, yellow-brown shades – Transferred to keratinocytes in stratum basale – Amount in skin varies according to heredity and light exposure • UV light stimulating melanin production – All people with same number of melanocytes – Activity and color varying among individuals • darker skinned producing more and darker colored melanin
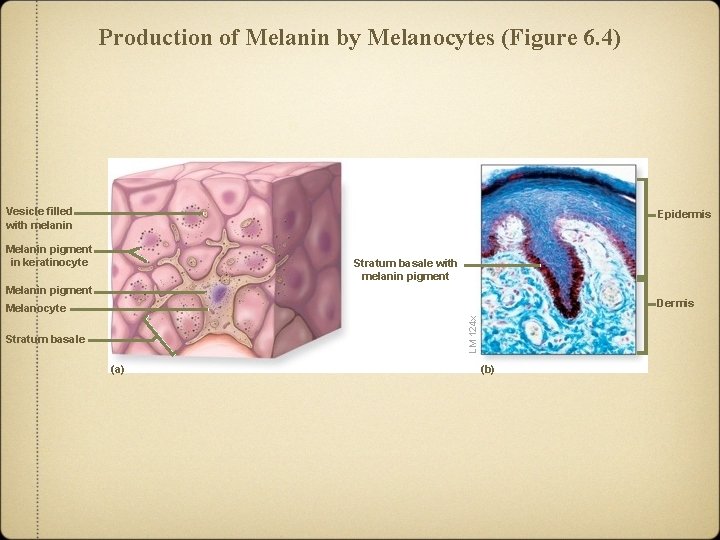
Production of Melanin by Melanocytes (Figure 6. 4) Vesicle filled with melanin Epidermis Melanin pigment in keratinocyte Stratum basale with melanin pigment Melanin pigment Dermis LM 124 x Melanocyte Stratum basale (a) (b)
Composition of the Integument: Epidermis Variations in the epidermis • Coloring from carotene – Yellow-orange pigment – Acquired from yellow-orange vegetables – Accumulates inside subcutaneous fat and keratinocytes of stratum corneum – Converted to vitamin A within the body – Plays important roles: • in vision • in reducing free radicals • in immune function
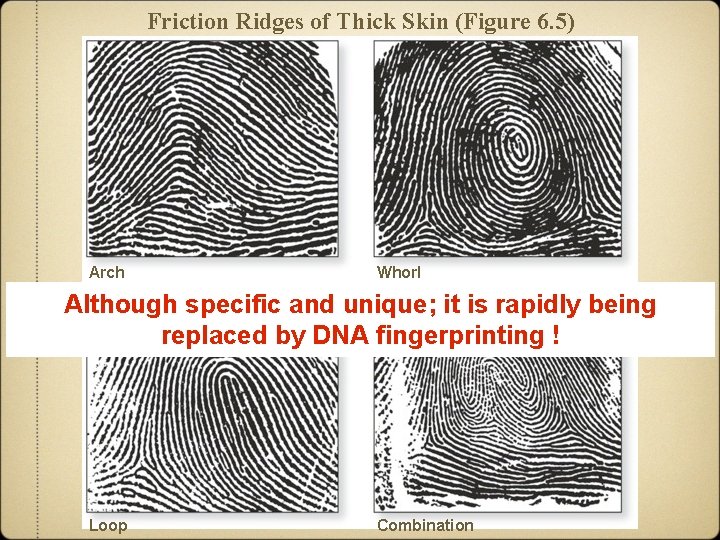
Composition of the Integument: Epidermis Variations in the epidermis • Ridge patterns of the skin – Small conical pegs in thin skin – Complex arches and whorls on finger, palms, soles, and toes • called friction ridges • formed from large folds and valleys of dermis and epidermis • help increase friction on contact • each individual with a unique pattern of friction ridges • allows for personal identification
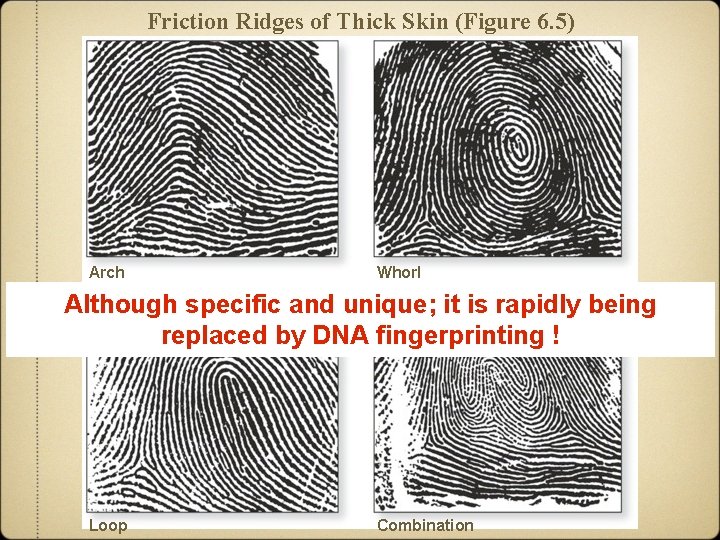
Friction Ridges of Thick Skin (Figure 6. 5) Arch Whorl Although specific and unique; it is rapidly being replaced by DNA fingerprinting ! Loop Combination
Composition of the Integument: Epidermis Clinical View: UV Radiation, Sunscreens, and Sunless Tanners • Ultraviolet radiation is believed to cause skin cancer. – UVA between 320 and 400 nm – UVB between 290 and 320 nm • Sunscreens block UVA and UVB rays. – Protect the skin if used correctly – Need high enough SPF (sun protection factor) - 40 to 50 minimum ! • Sunless tanners create tanned skin without UV light exposure. – Offer no protection against UV rays
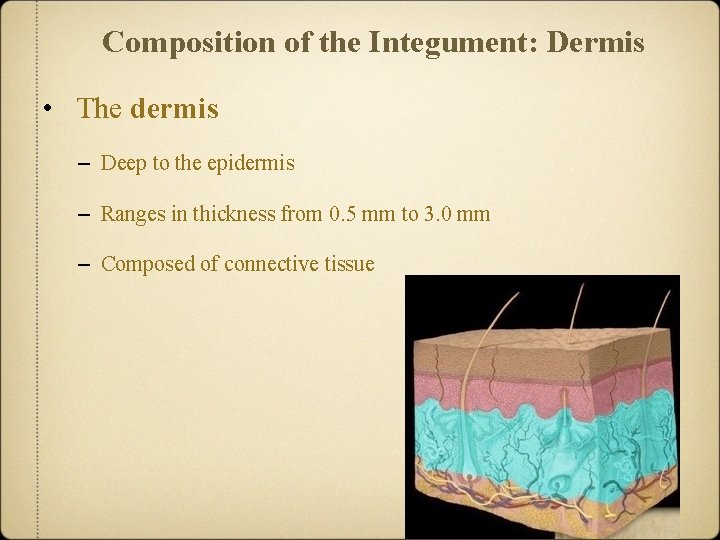
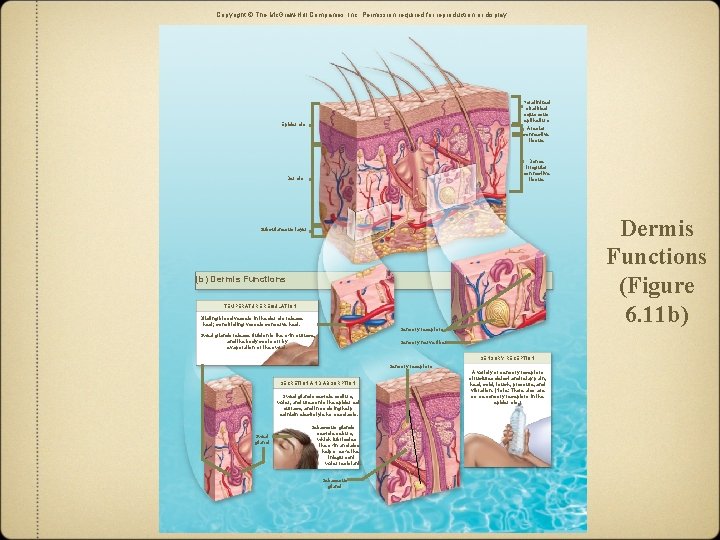
Composition of the Integument: Dermis • The dermis – Deep to the epidermis – Ranges in thickness from 0. 5 mm to 3. 0 mm – Composed of connective tissue
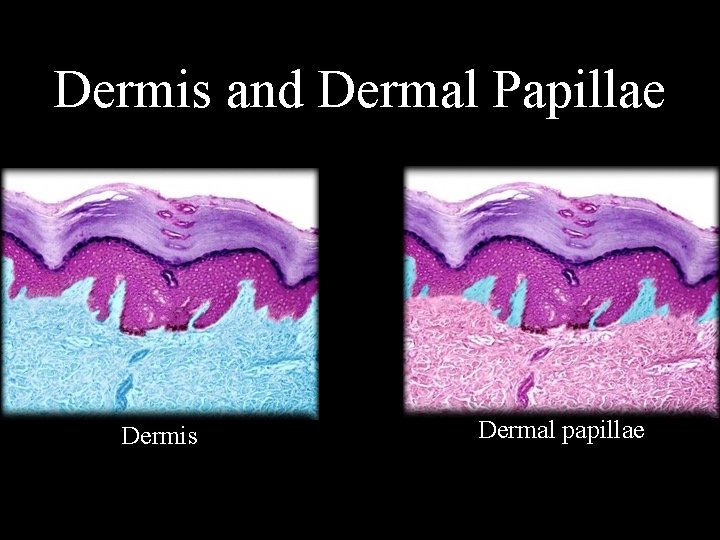
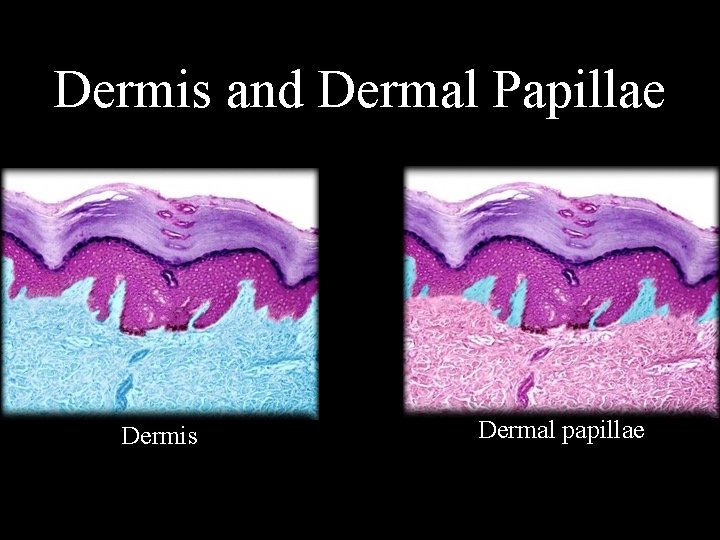
Dermis and Dermal Papillae Dermis Dermal papillae
Composition of the Integument: Dermis • Components of the dermis – Primarily collage with elastic and reticular fibers – Motile dendritic cells serving an immune function – Blood vessels, sweat glands, sebaceous glands – Hair follicles, nail roots, sensory nerve endings, arrector pili – Divided between the papillary layer and deeper reticular layer
Composition of the Integument: Dermis • Papillary layer of the dermis – Superficial region of the dermis – Directly adjacent to epidermis – Composed of areolar connective tissue – Derives name from projections of the dermis • termed dermal papillae • contain capillaries and sensory nerve endings – Projections of epidermis interdigitating with papillae • termed epidermal ridges – Interlock and increase the area of contact between layers
Composition of the Integument: Dermis • Reticular layer of the dermis – Deeper, major portion of the dermis – Extends from papillary layer to subcutaneous layer – Consists primarily of dense irregular connective tissue – Contains large bundles of collage fibers • fibers interwoven into a meshwork surrounding structures in dermis
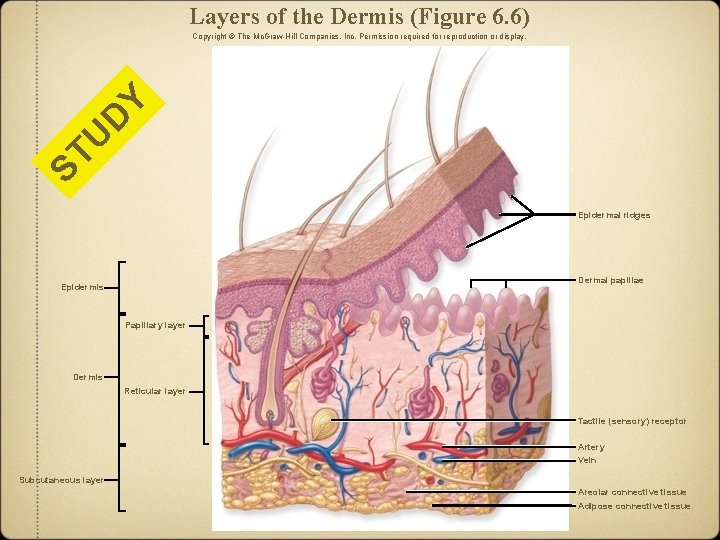
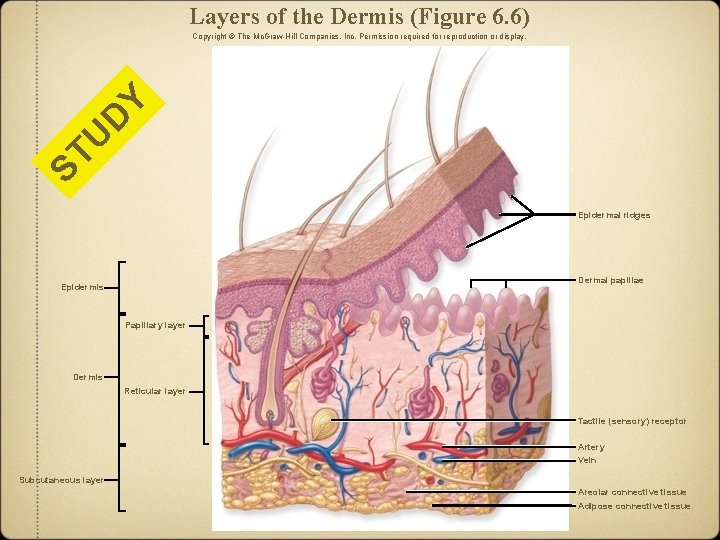
Layers of the Dermis (Figure 6. 6) ST U D Y Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Epidermal ridges Dermal papillae Epidermis Papillary layer Dermis Reticular layer Tactile (sensory) receptor Artery Vein Subcutaneous layer Areolar connective tissue Adipose connective tissue
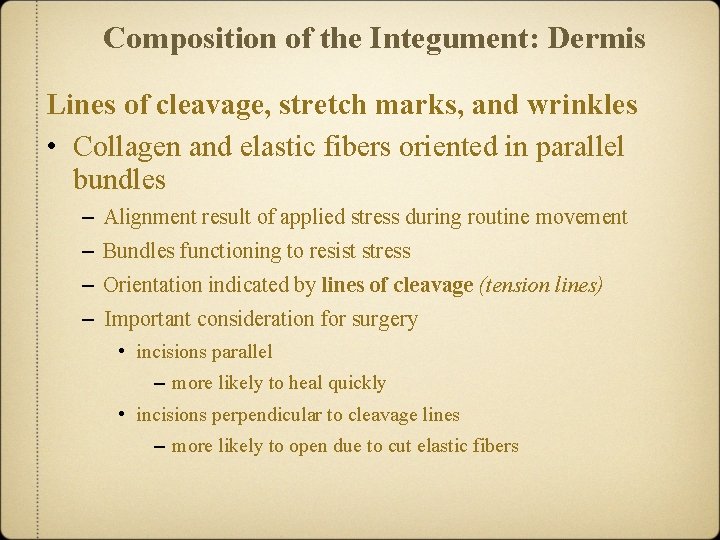
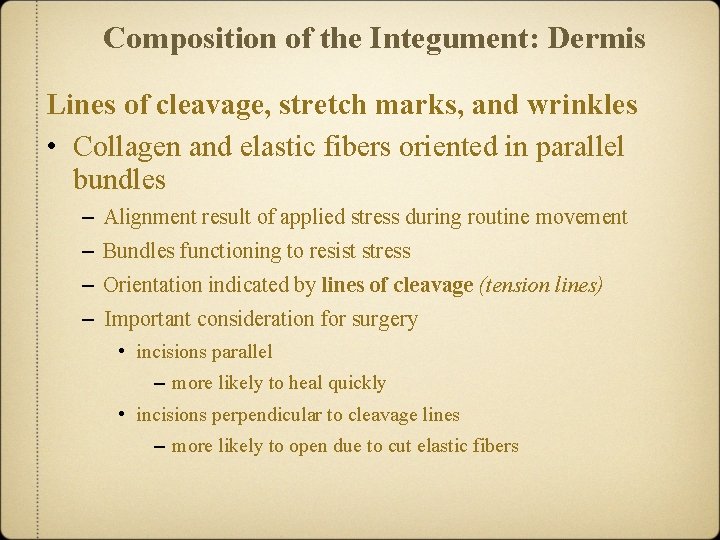
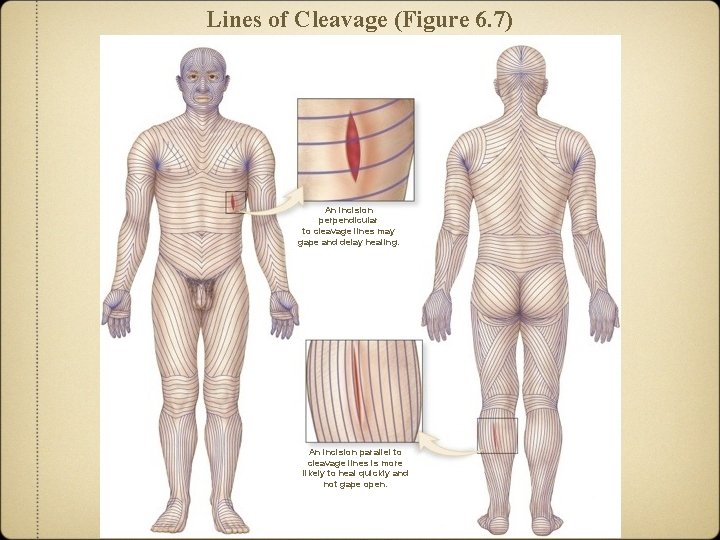
Composition of the Integument: Dermis Lines of cleavage, stretch marks, and wrinkles • Collagen and elastic fibers oriented in parallel bundles – Alignment result of applied stress during routine movement – Bundles functioning to resist stress – Orientation indicated by lines of cleavage (tension lines) – Important consideration for surgery • incisions parallel – more likely to heal quickly • incisions perpendicular to cleavage lines – more likely to open due to cut elastic fibers
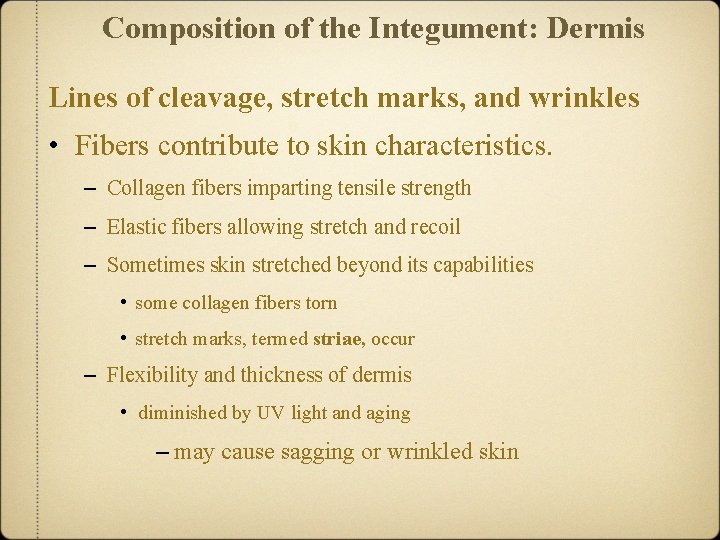
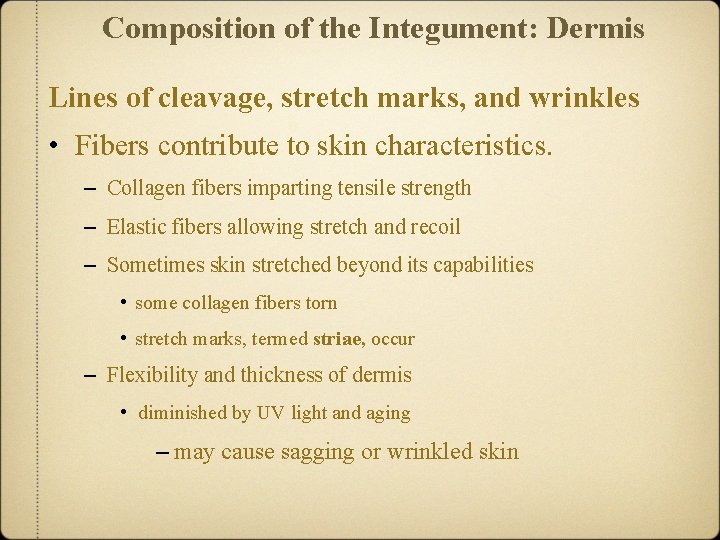
Composition of the Integument: Dermis Lines of cleavage, stretch marks, and wrinkles • Fibers contribute to skin characteristics. – Collagen fibers imparting tensile strength – Elastic fibers allowing stretch and recoil – Sometimes skin stretched beyond its capabilities • some collagen fibers torn • stretch marks, termed striae, occur – Flexibility and thickness of dermis • diminished by UV light and aging – may cause sagging or wrinkled skin
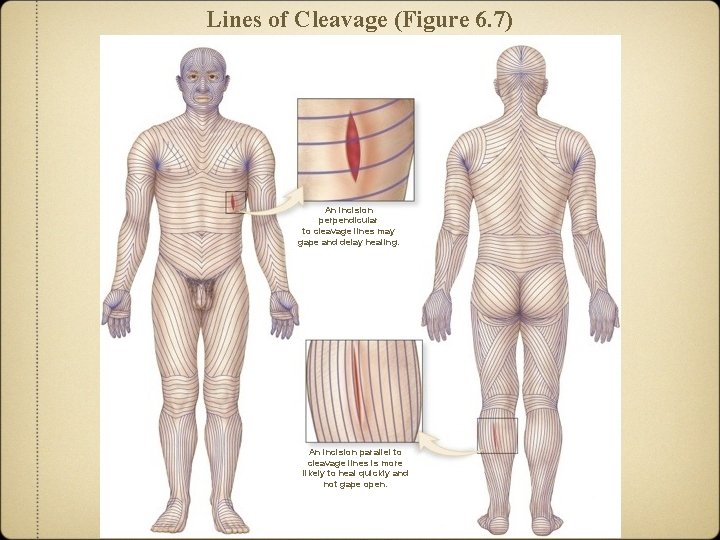
Lines of Cleavage (Figure 6. 7) An incision perpendicular to cleavage lines may gape and delay healing. An incision parallel to cleavage lines is more likely to heal quickly and not gape open.
Composition of the Integument: Dermis Innervation and blood supply • Dermis with extensive nerve fibers – Sensory nerve fibers • detect pressure, vibration, and cold – Motor nerve fibers • control blood flow and gland secretions • Dermal blood vessels – Supply nutrients to epidermis and dermis – Large vessels along reticular and subcutaneous border – Smaller vessels branching into dermis and dermal papillae – Play an important role in body temperature and blood pressure regulation
Composition of the Integument: Dermis Innervation and blood supply • Dermal blood vessels (continued) – Vasoconstriction • blood vessel diameters narrowed • blood shunted from periphery toward deeper structures • occurring when trying to conserve heat • look pale when exposed to cold – Vasodilation • blood vessel diameter increased • more blood close to body surface • occurs when needing to loose heat • why people may become flushed during exercise
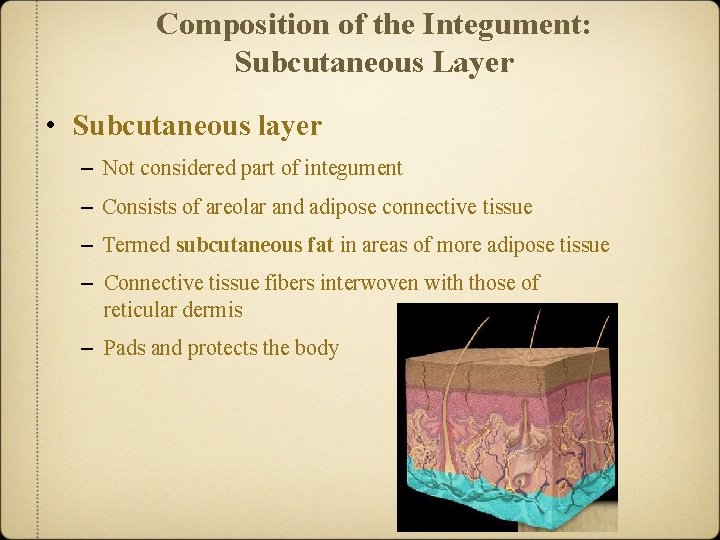
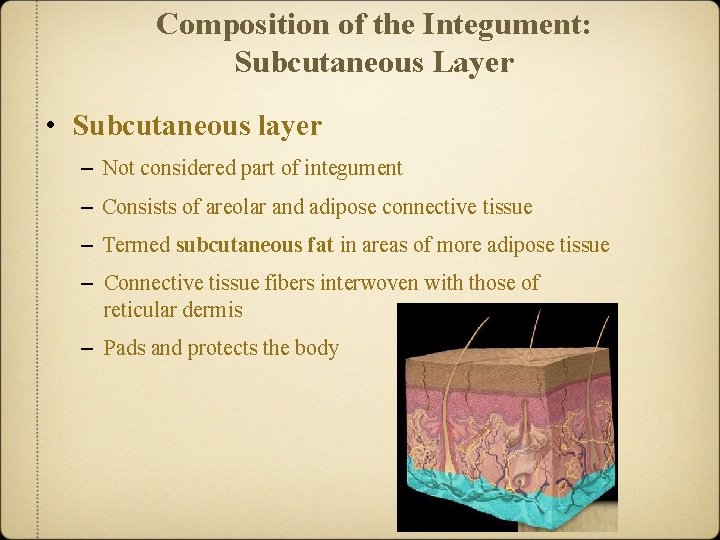
Composition of the Integument: Subcutaneous Layer • Subcutaneous layer – Not considered part of integument – Consists of areolar and adipose connective tissue – Termed subcutaneous fat in areas of more adipose tissue – Connective tissue fibers interwoven with those of reticular dermis – Pads and protects the body
Composition of the Integument: Subcutaneous Layer • Subcutaneous layer – Acts as energy reservoir – Provides thermal insulation – Drugs often injected here – Sexes with different layer thickness and distribution • women, generally thicker – primarily in breasts, buttocks, hips, and thighs • men, generally thinner – primarily in neck, upper arms, abdomen, lower back, buttocks
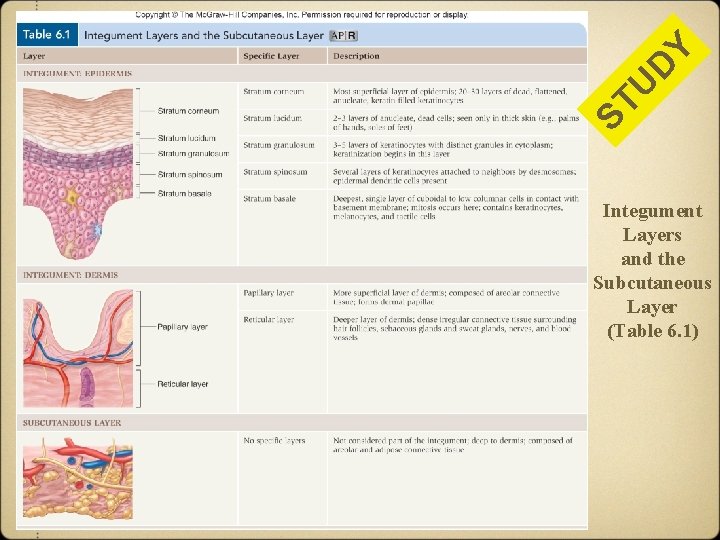
Y D ST U Integument Layers and the Subcutaneous Layer (Table 6. 1)
Integumentary Structures Derived from Epidermis • Nails, hair, exocrine glands derived from epidermal epithelium – Known as epidermal derivatives – Formed from portions of epidermis invaginated into the dermis
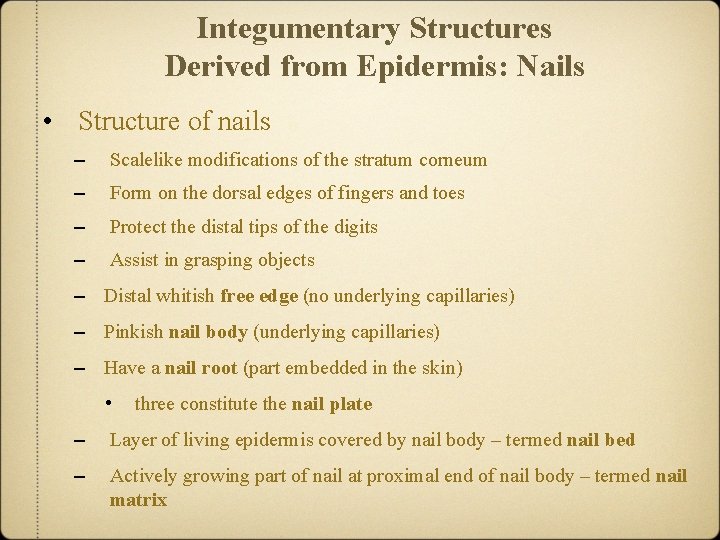
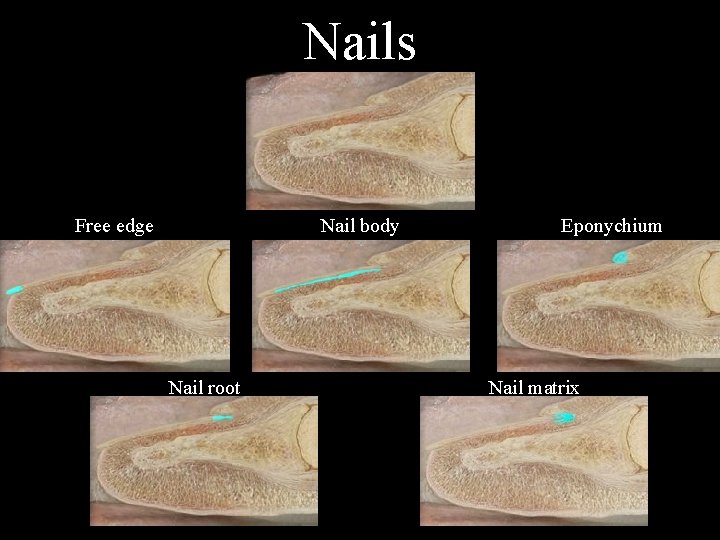
Integumentary Structures Derived from Epidermis: Nails • Structure of nails – Scalelike modifications of the stratum corneum – Form on the dorsal edges of fingers and toes – Protect the distal tips of the digits – Assist in grasping objects – Distal whitish free edge (no underlying capillaries) – Pinkish nail body (underlying capillaries) – Have a nail root (part embedded in the skin) • three constitute the nail plate – Layer of living epidermis covered by nail body – termed nail bed – Actively growing part of nail at proximal end of nail body – termed nail matrix
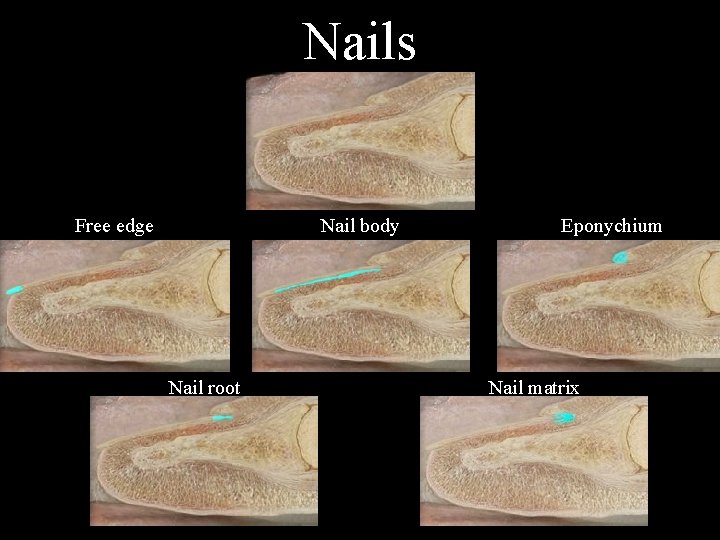
Nails Free edge Nail body Nail root Eponychium Nail matrix
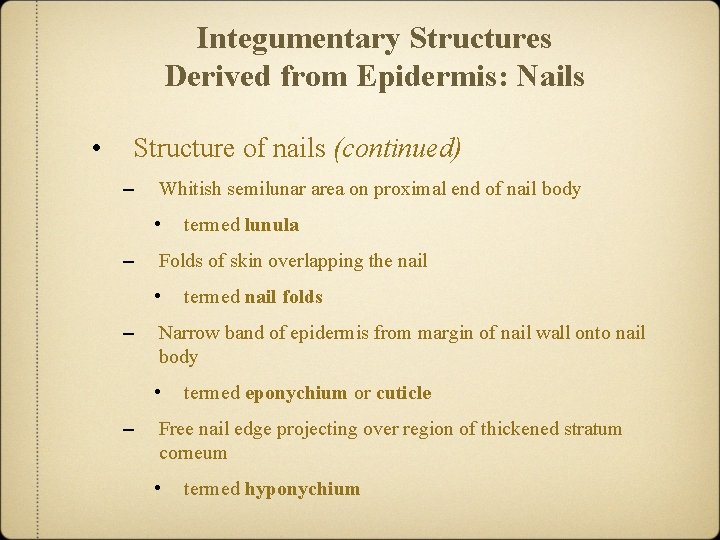
Integumentary Structures Derived from Epidermis: Nails • Structure of nails (continued) – Whitish semilunar area on proximal end of nail body • – Folds of skin overlapping the nail • – termed nail folds Narrow band of epidermis from margin of nail wall onto nail body • – termed lunula termed eponychium or cuticle Free nail edge projecting over region of thickened stratum corneum • termed hyponychium
Integumentary Structures Derived from Epidermis: Hair • Hair found almost everywhere on the body except: – the hands and palmar surface of the fingers – the sides and soles of the feet and toes – the lips – portions of the external genitalia • Hair composition – Single hair, termed pilus, with shape of a slender filament – Composed of keratinized cells growing from hair follicles
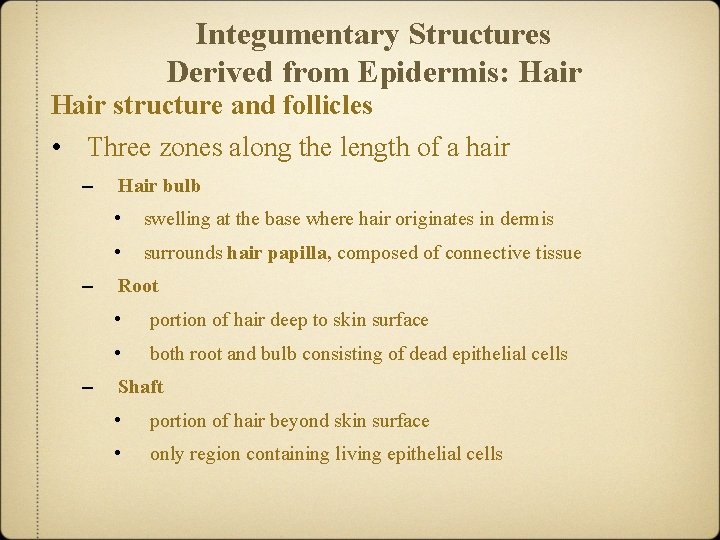
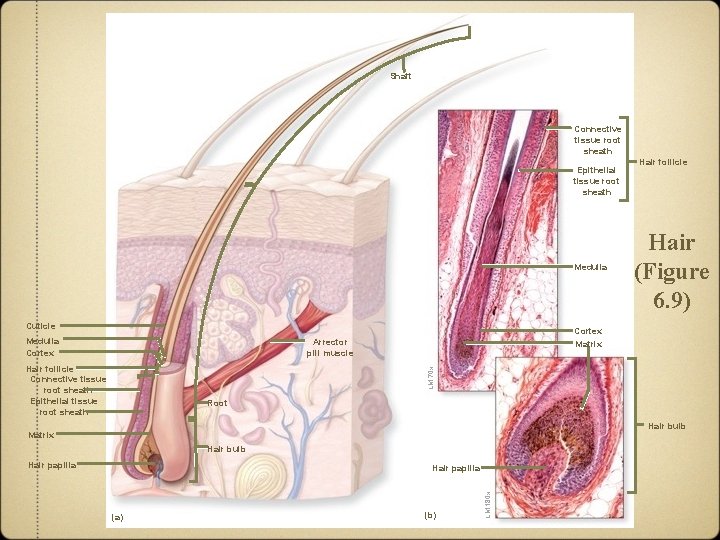
Integumentary Structures Derived from Epidermis: Hair structure and follicles • Three zones along the length of a hair – – – Hair bulb • swelling at the base where hair originates in dermis • surrounds hair papilla, composed of connective tissue Root • portion of hair deep to skin surface • both root and bulb consisting of dead epithelial cells Shaft • portion of hair beyond skin surface • only region containing living epithelial cells
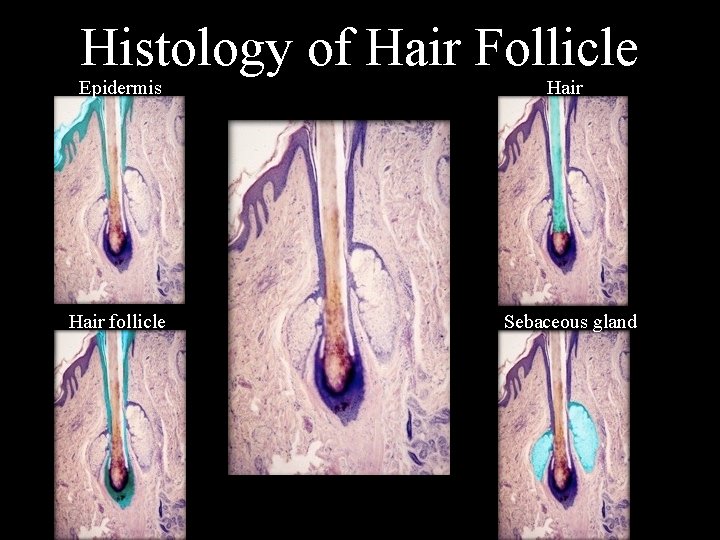
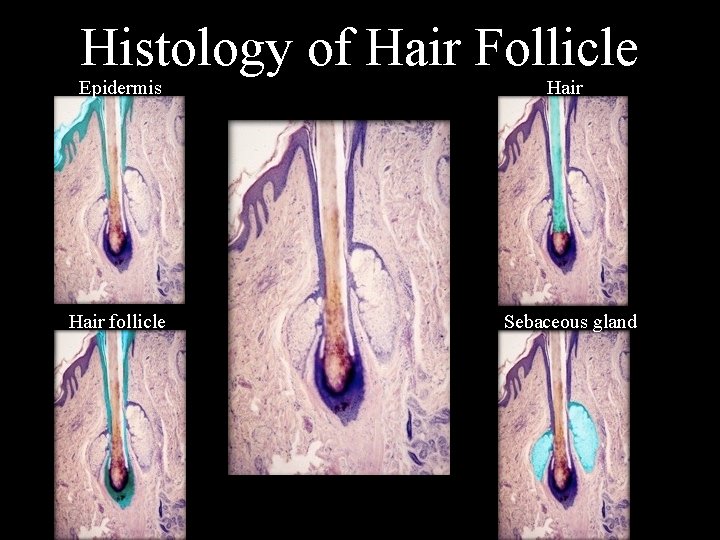
Histology of Hair Follicle Epidermis Hair follicle Sebaceous gland
Integumentary Structures Derived from Epidermis: Hair structure and follicles • Hair components – – Hair follicle • oblique tube surrounding hair root • extends into dermis and sometimes subcutaneous layer • has an outer connective tissue root sheath originating in dermis • has inner epithelial tissue root sheath originating from epidermis Arrector pili • thin ribbons of smooth muscle • extend from hair follicle to the dermal papillae • elevates hair with contraction, producing “goosebumps”
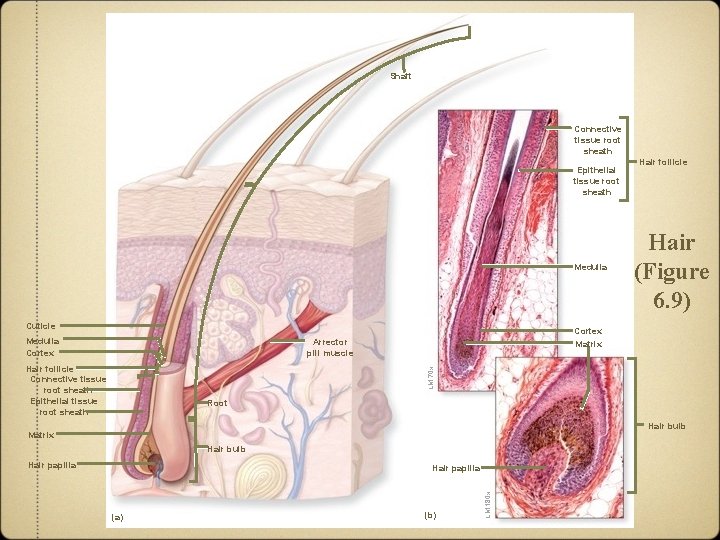
Shaft Connective tissue root sheath Epithelial tissue root sheath Medulla Cuticle Medulla Cortex Hair (Figure 6. 9) Cortex Matrix Arrector pili muscle LM 70 x Hair follicle Connective tissue root sheath Epithelial tissue root sheath Hair follicle Root Hair bulb Matrix Hair bulb Hair papilla (a) (b) LM 180 x Hair papilla
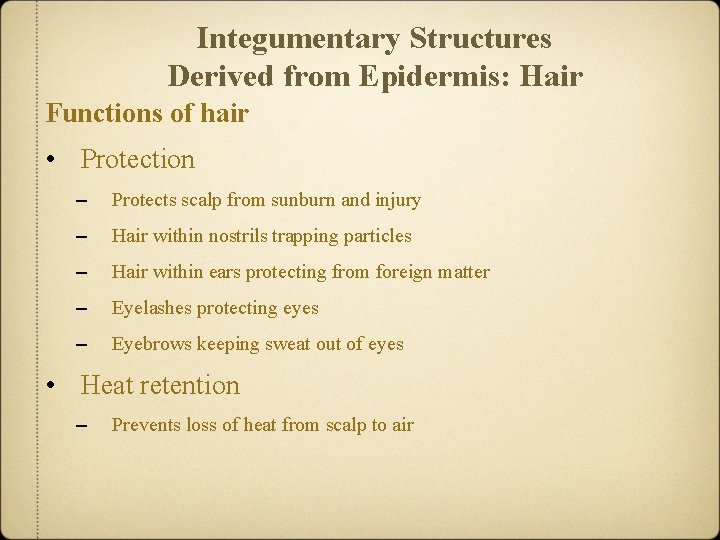
Integumentary Structures Derived from Epidermis: Hair Functions of hair • Protection – Protects scalp from sunburn and injury – Hair within nostrils trapping particles – Hair within ears protecting from foreign matter – Eyelashes protecting eyes – Eyebrows keeping sweat out of eyes • Heat retention – Prevents loss of heat from scalp to air
Integumentary Structures Derived from Epidermis: Hair Functions of hair • Sensory reception – Has associated tactile receptors • Visual identification – Important in determining age, sex, specific individuals • Chemical signal dispersal – Disperse pheromones • chemical signals involved in attracting sexual partners • secreted by specific sweat glands onto hairs in axillary and pubic regions
Integumentary Structures Derived from Epidermis: Hair color – Results from synthesis of melanin in the matrix adjacent to hair papillae – Reflects genetic, environmental, and hormonal factors – Becomes lighter with age as pigment production decreases • Growth rate – One-third mm per day in the scalp for 2 to 5 years – Eventually pushed out and replaced by new hair • Hair loss – Normal scalp loss of 10 to 100 hairs per day • may be result of drugs, dietary factors, radiation, high fever, stress – Thinning of hair termed alopecia • usually a result of aging
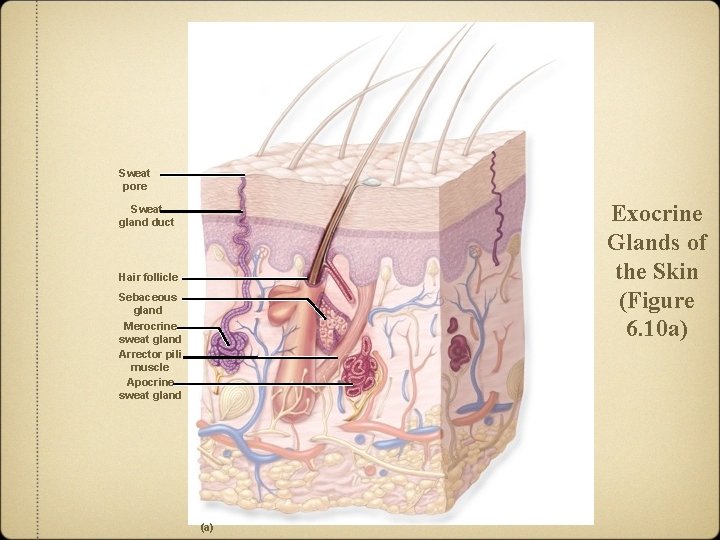
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin • Skin houses many types of exocrine glands • Two most common: – A. sweat glands – B. sebaceous glands
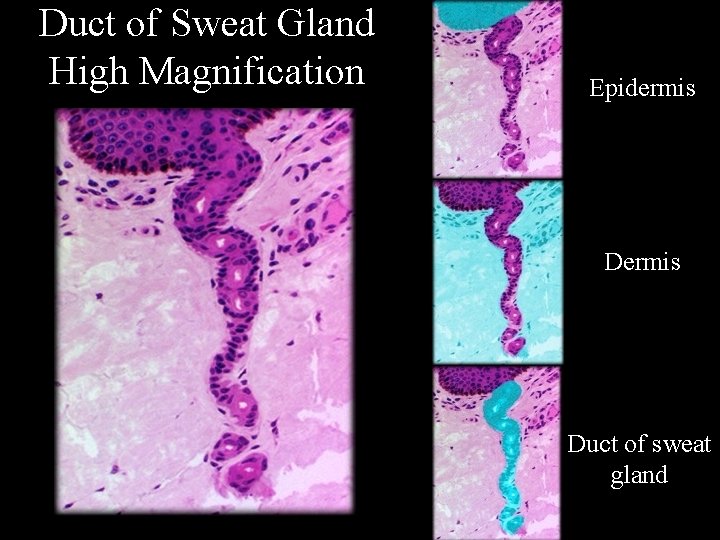
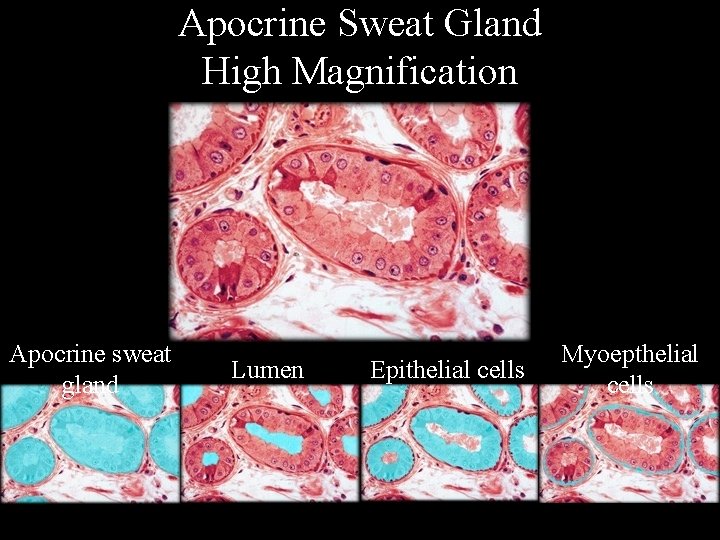
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin A. Sweat glands • Two groups: merocrine and apocrine • General structure – Coiled, tubular secretory portion in reticular dermis – Sweat gland duct carrying secretions – Opening of the gland duct on epidermal surface termed sweat pore – Contain myoepithelial cells • contract to squeeze the gland • discharge secretions in response to sympathetic stimulation
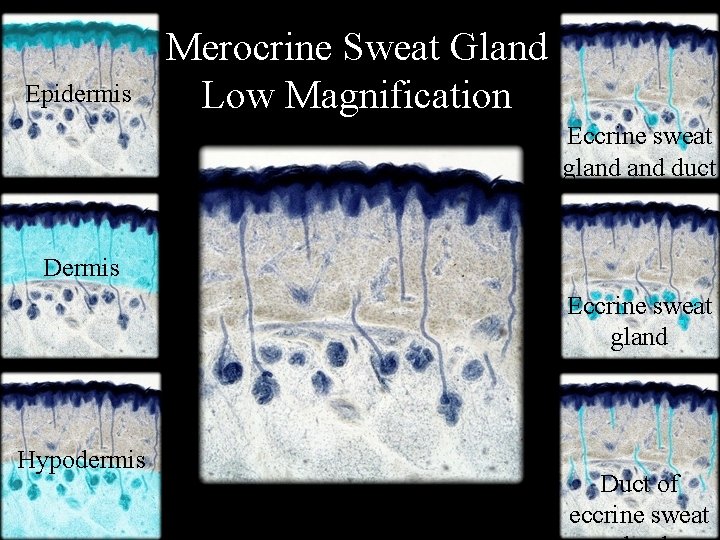
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin Sweat glands • Merocrine sweat glands – Most numerous and widely distributed sweat glands – Simple, coiled tubular glands – Discharge their secretions onto skin surface – Secrete sweat • composed of 99% water and 1% other chemicals; include electrolytes, metabolites, and waste products – Major function of thermoregulation • regulation of body temperature by fluid evaporation – Provide a means for loss of water and electrolytes – Secretions diluting harmful chemicals; has antibacterial activity – Produce secretions by exocytosis
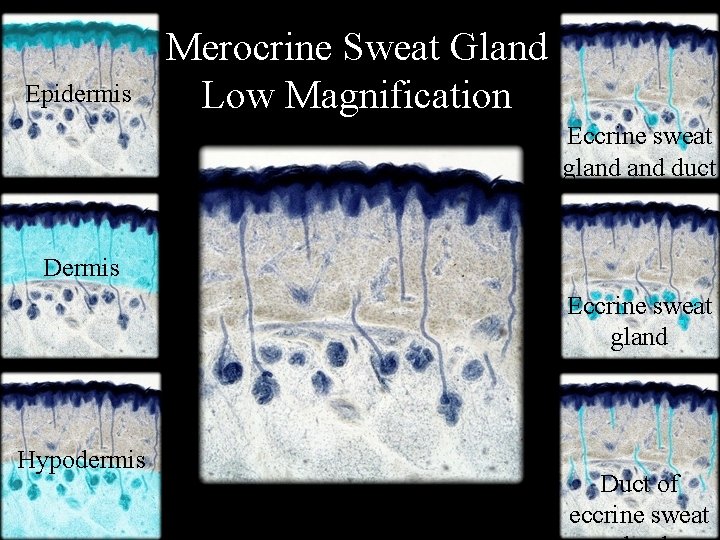
Epidermis Merocrine Sweat Gland Low Magnification Eccrine sweat gland duct Dermis Eccrine sweat gland Hypodermis Duct of eccrine sweat
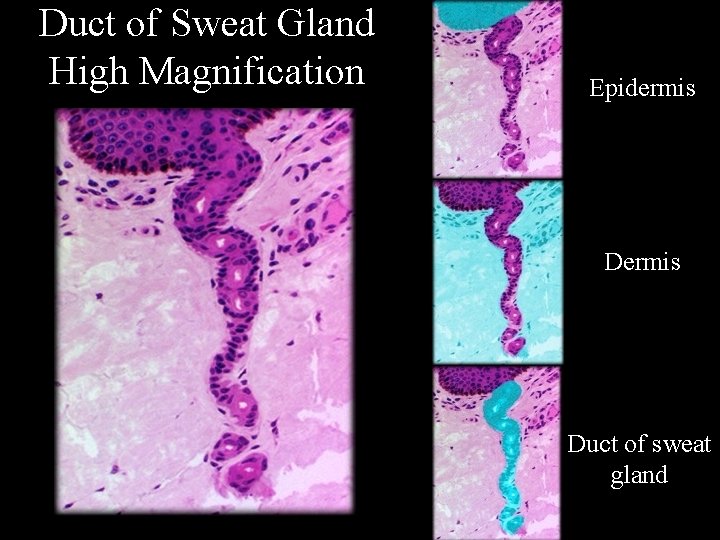
Duct of Sweat Gland High Magnification Epidermis Duct of sweat gland
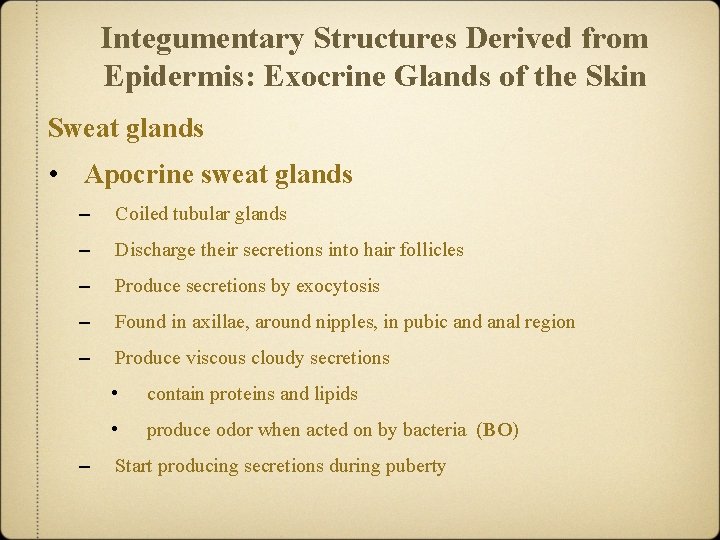
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin Sweat glands • Apocrine sweat glands – Coiled tubular glands – Discharge their secretions into hair follicles – Produce secretions by exocytosis – Found in axillae, around nipples, in pubic and anal region – Produce viscous cloudy secretions – • contain proteins and lipids • produce odor when acted on by bacteria (BO) Start producing secretions during puberty
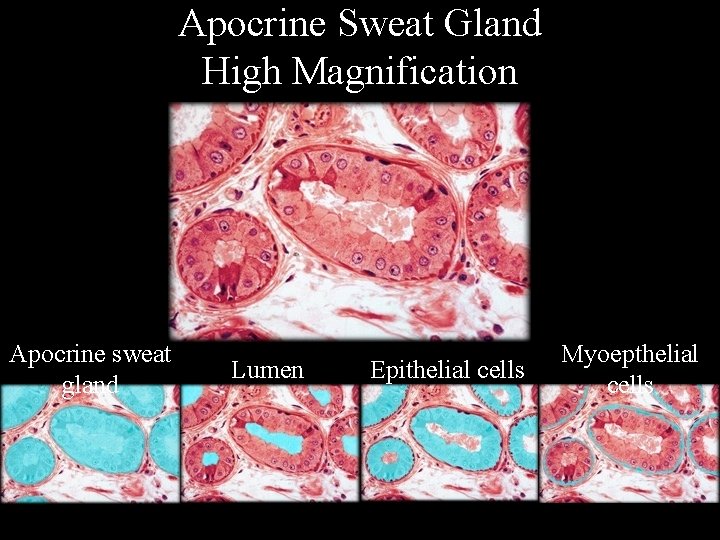
Apocrine Sweat Gland High Magnification Apocrine sweat gland Lumen Epithelial cells Myoepthelial cells
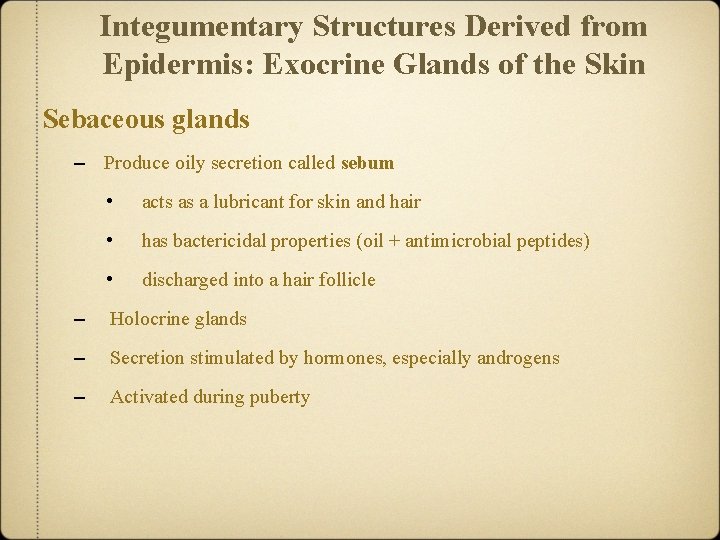
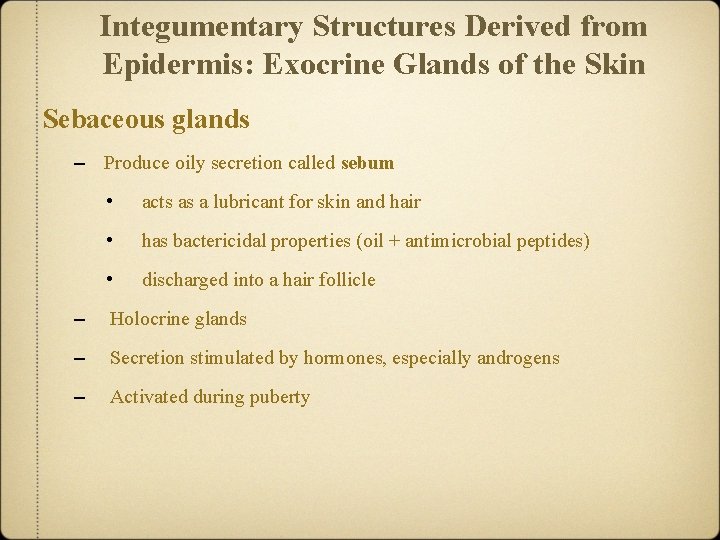
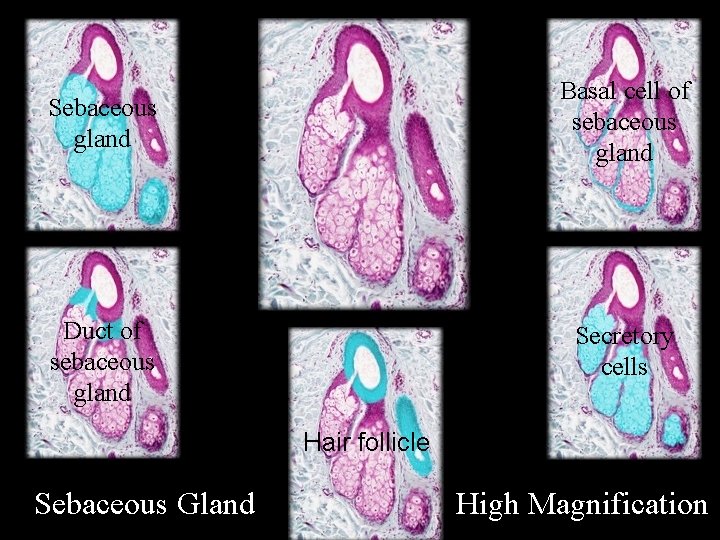
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin Sebaceous glands – Produce oily secretion called sebum • acts as a lubricant for skin and hair • has bactericidal properties (oil + antimicrobial peptides) • discharged into a hair follicle – Holocrine glands – Secretion stimulated by hormones, especially androgens – Activated during puberty
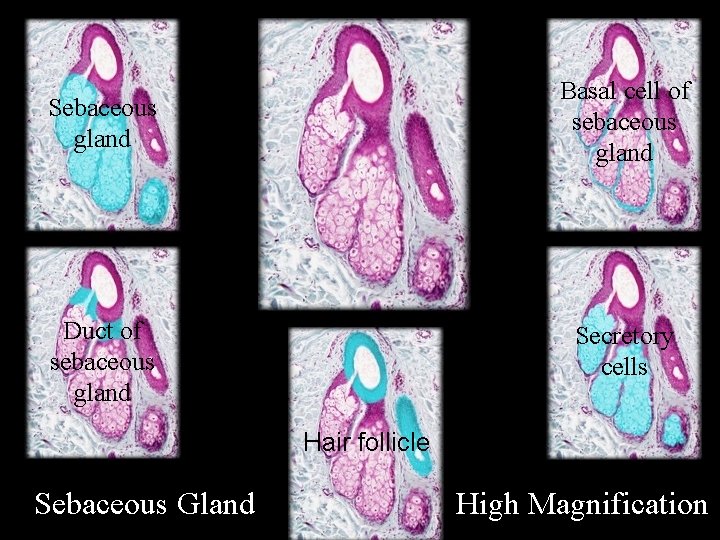
Sebaceous gland Basal cell of sebaceous gland Duct of sebaceous gland Secretory cells Hair follicle Sebaceous Gland High Magnification
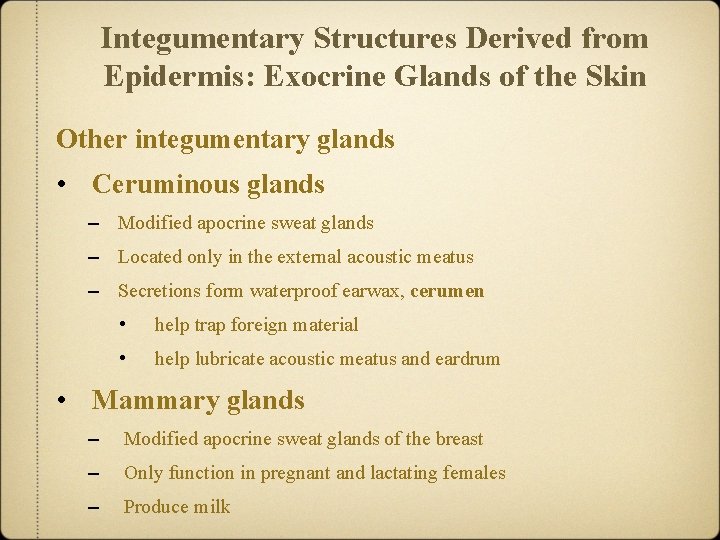
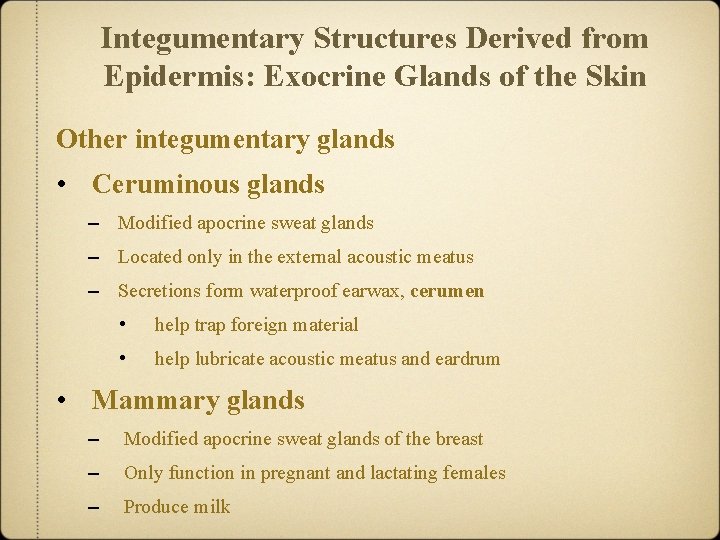
Integumentary Structures Derived from Epidermis: Exocrine Glands of the Skin Other integumentary glands • Ceruminous glands – Modified apocrine sweat glands – Located only in the external acoustic meatus – Secretions form waterproof earwax, cerumen • help trap foreign material • help lubricate acoustic meatus and eardrum • Mammary glands – Modified apocrine sweat glands of the breast – Only function in pregnant and lactating females – Produce milk
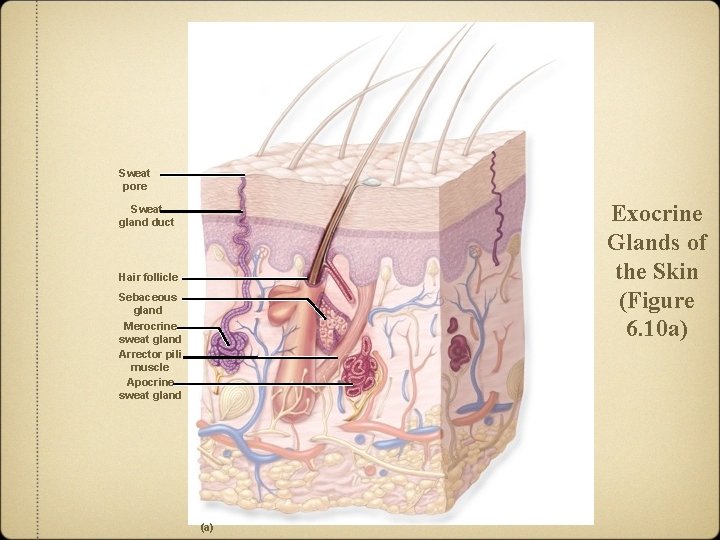
Sweat pore Exocrine Glands of the Skin (Figure 6. 10 a) Sweat gland duct Hair follicle Sebaceous gland Merocrine sweat gland Arrector pili muscle Apocrine sweat gland (a)
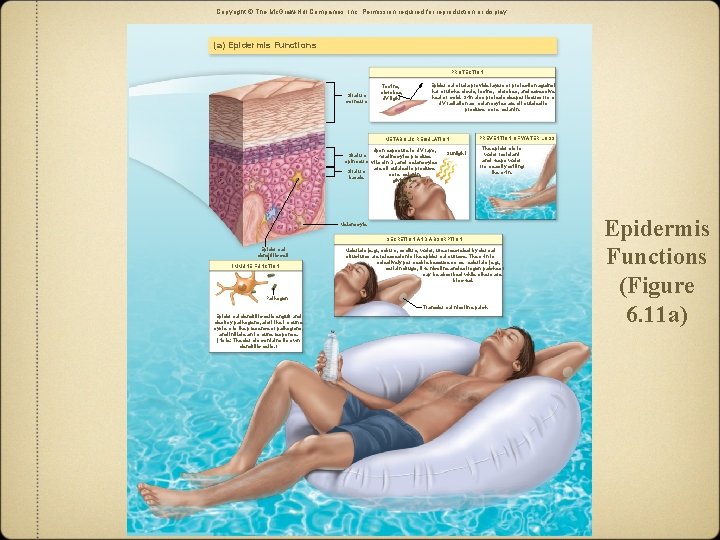
Functions of the Integument—Protection and More: Epidermis Functions Protection – Acts as a physical barrier – Protects body from physical injury and trauma – Protects from chemicals, toxins, microbes, temperature extremes – Protects deeper tissue from solar radiation Prevention of water loss – Helps prevent unnecessary water loss – Water unable to exit skin unless secreted by sweat glands – Dehydration a danger with severe burns – Water resistant, not waterproof • some interstitial fluid penetrating through epidermis to air • release of water vapor from sweat glands when not sweating • termed transpiration
Functions of the Integument—Protection and More: Epidermis Functions Metabolic regulation • Vitamin D (“sunshine vitamin”) – Vitamin D 3 also termed cholecalciferol – Synthesized from a steroid precursor by keratinocytes – Occurs upon UV exposure – Released into the blood and transported to the liver – Converted to another intermediate molecule – Transported to kidney and converted to calcitriol • the active form of vitamin D
Functions of the Integument—Protection and More: Epidermis Functions Metabolic regulation • • Vitamin D (continued) – Considered a hormone – Increases absorption of calcium and phosphate – Important in regulating blood levels of calcium and phosphate Other forms of metabolic regulation – Skin able to convert some compounds to slightly different forms – UV rays stimulating melanocytes to produce melanin
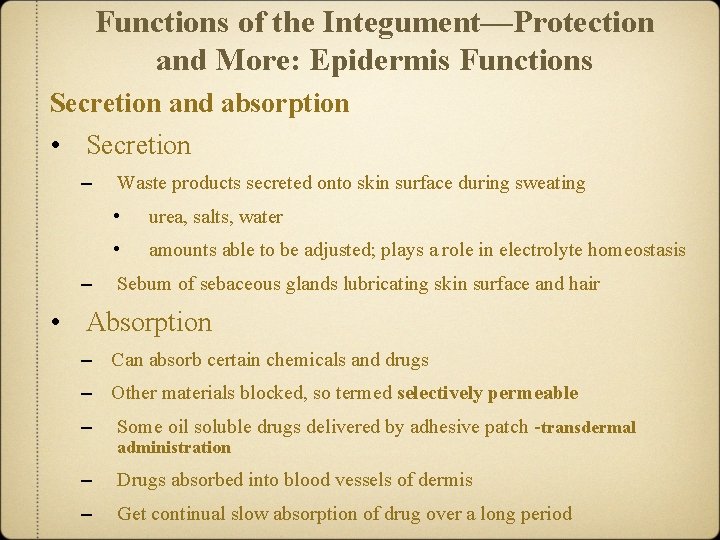
Functions of the Integument—Protection and More: Epidermis Functions Secretion and absorption • Secretion – – Waste products secreted onto skin surface during sweating • urea, salts, water • amounts able to be adjusted; plays a role in electrolyte homeostasis Sebum of sebaceous glands lubricating skin surface and hair • Absorption – Can absorb certain chemicals and drugs – Other materials blocked, so termed selectively permeable – Some oil soluble drugs delivered by adhesive patch -transdermal – Drugs absorbed into blood vessels of dermis – Get continual slow absorption of drug over a long period administration
Functions of the Integument—Protection and More: Epidermis Functions Immune function • Dendritic cells – Within stratum spinosum in epidermis – Initiate immune response against pathogens – Attack cancer cells – Also present in the dermis
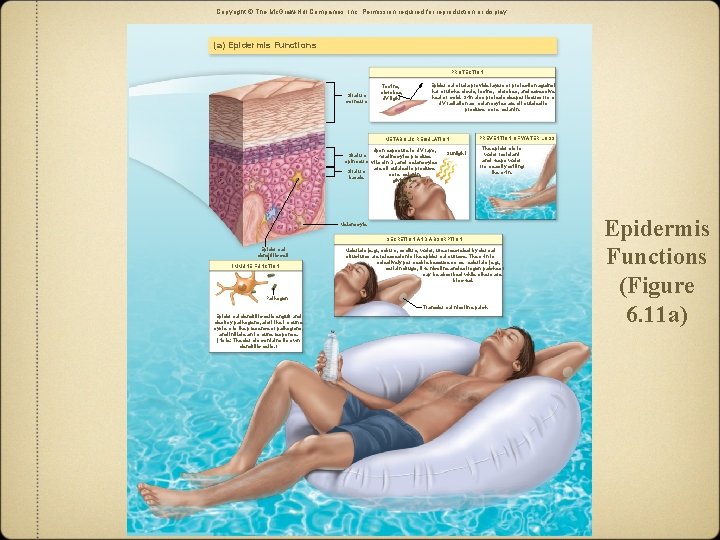
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. (a) Epidermis Functions PROTECTION Stratum corneum Toxins, microbes, UV light Epidermal strata provide layers of protection against harmful chemicals, toxins, microbes, and excessive heat or cold. Skin also protects deeper tissues from UV radiation as melanocytes are stimulated to produce more melanin. METABOLIC REGULATION Upon exposure to UV rays, Stratum keratinocytes produce spinosum vitamin D 3 and melanocytes are stimulated to produce Stratum more melanin, basale giving the skin a more tanned look. Sunlight PREVENTION OF WATER LOSS The epidermis is water resistant and keeps water from easily exiting the skin. Melanocyte SECRETION AND ABSORPTION Epidermal dendritic cell IMMUNE FUNCTION Materials (e. g. , sebum, sodium, water, urea) secreted by dermal structures are released onto the epidermal surface. The skin is selectively permeable because some materials (e. g. , certain drugs, like nicotine and estrogen patches) may be absorbed while others are blocked. Pathogen Transdermal nicotine patch Epidermal dendritic cells engulf and destroy pathogens, alert the immune system to the presence of pathogens, and initiate an immune response. (Note: The dermis contains its own dendritic cells. ) Epidermis Functions (Figure 6. 11 a)
Functions of the Integument: Protection and More Clinical View: Acne and Acne Treatments • Acne – Plugged sebaceous ducts (Proprionibacteria acne) – Prevalent during the teenage years - sebum increases – Treatments • include benzyol peroxide, salicyclic acid, antibiotics, A-like compounds ($3 billion industry in US) • may lead to scarring if untreated vitamin
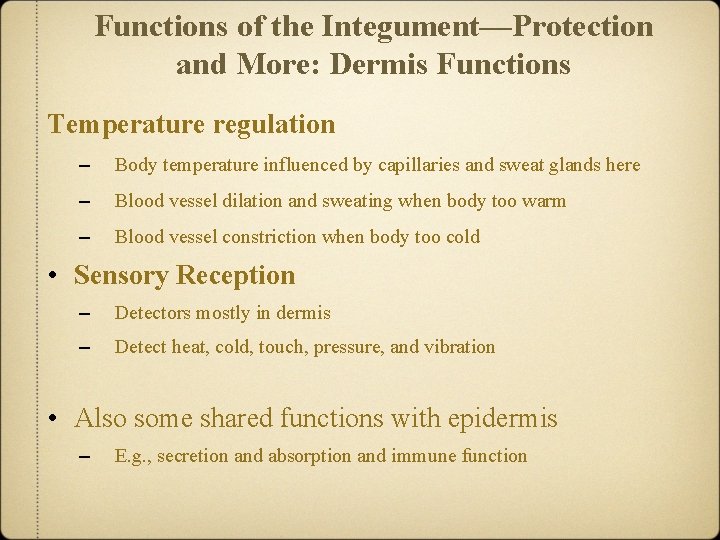
Functions of the Integument—Protection and More: Dermis Functions Temperature regulation – Body temperature influenced by capillaries and sweat glands here – Blood vessel dilation and sweating when body too warm – Blood vessel constriction when body too cold • Sensory Reception – Detectors mostly in dermis – Detect heat, cold, touch, pressure, and vibration • Also some shared functions with epidermis – E. g. , secretion and absorption and immune function
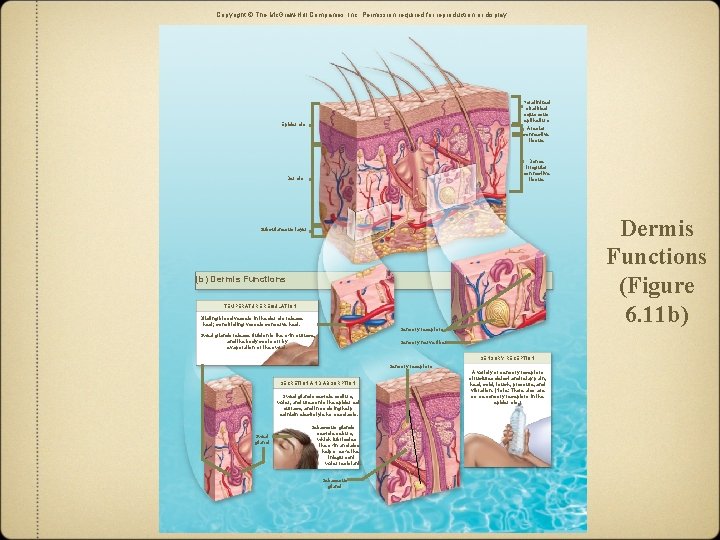
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Keratinized stratified squamous epithelium Epidermis Areolar connective tissue Dense irregular connective tissue Dermis Functions (Figure 6. 11 b) Subcutaneous layer (b) Dermis Functions TEMPERATURE REGULATION Dilating blood vessels in the dermis release heat; constricting vessels conserve heat. Sensory receptors Sweat glands release fluid onto the skin surface, and the body cools off by evaporation of the sweat. Sensory nerve fiber SENSORY RECEPTION Sensory receptors SECRETION AND ABSORPTION Sweat glands secrete sodium, water, and urea onto the epidermal surface, and in so doing help maintain electrolyte homeostasis. Sweat gland Sebaceous glands secrete sebum, which lubricates the skin and also helps make the integument water resistant. Sebaceous gland A variety of sensory receptors structures detect and relay pain, heat, cold, touch, pressure, and vibration. (Note: There also are some sensory receptors in the epidermis. )
Repair and Regeneration of the Integumentary System • Response to repetitive mechanical stress – Mitosis stimulated in stratum basale – Thickening of the epidermis – Provides more protection • e. g. , thickened soles after walking barefoot
Repair and Regeneration of the Integumentary System • Response to damaged tissues – – Regeneration • replacement of damaged cells with same cell type • restores organ function Fibrosis • gap filled with scar tissue • composed primarily of collagen produced by fibroblasts • functional activities not restored • if organ too damaged or cells lack ability to divide
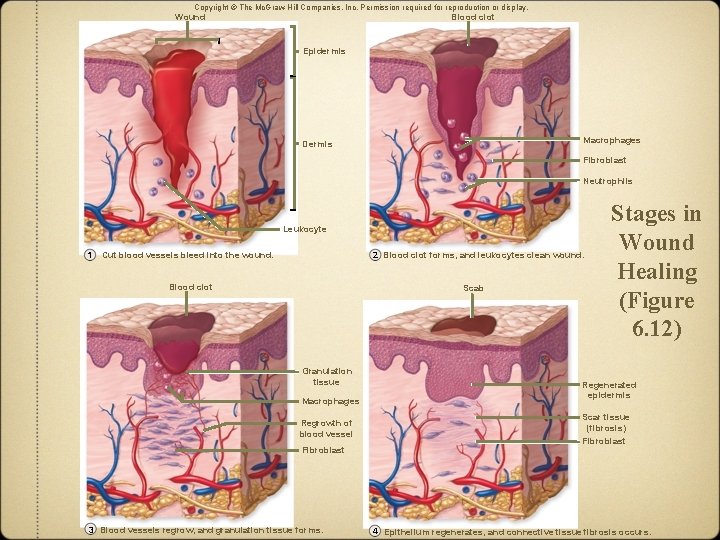
Repair and Regeneration of the Integumentary System • Stages of wound healing 1) Cut blood vessels bleed into wound. 2) Blood clot forms and leukocytes clean wound. – clot a temporary barrier for pathogens 3) Blood vessels regrow and granulation tissue forms. – vascular connective tissue that initially forms in wound 4) Epithelium regenerates and connective tissue fibrosis occurs.
Repair and Regeneration of the Integumentary System • Wound healing – Not rapid – Longer for wider and deeper surfaces – With severe damage • less likely to return to original condition • hair follicles, exocrine glands, nerves, and arrector pili muscle cells not repaired
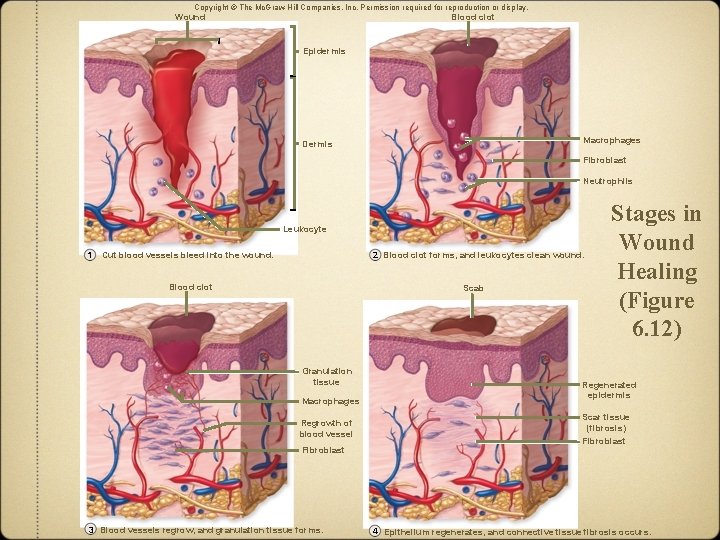
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Wound Blood clot Epidermis Macrophages Dermis Fibroblast Neutrophils Leukocyte 1 2 Blood clot forms, and leukocytes clean wound. Cut blood vessels bleed into the wound. Blood clot Scab Granulation tissue Macrophages Regrowth of blood vessel Fibroblast 3 Blood vessels regrow, and granulation tissue forms. Stages in Wound Healing (Figure 6. 12) Regenerated epidermis Scar tissue (fibrosis) Fibroblast 4 Epithelium regenerates, and connective tissue fibrosis occurs.
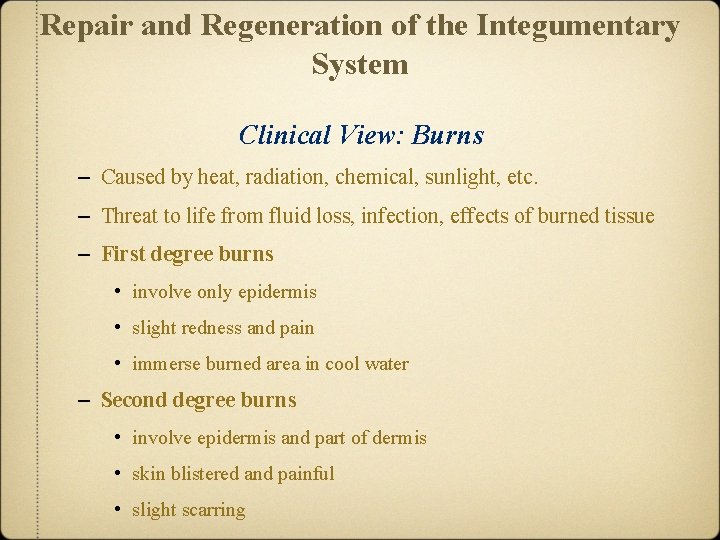
Repair and Regeneration of the Integumentary System Clinical View: Burns – Caused by heat, radiation, chemical, sunlight, etc. – Threat to life from fluid loss, infection, effects of burned tissue – First degree burns • involve only epidermis • slight redness and pain • immerse burned area in cool water – Second degree burns • involve epidermis and part of dermis • skin blistered and painful • slight scarring
Repair and Regeneration of the Integumentary System Clinical View: Burns – Third-degree burns • involve epidermis, and subcutaneous layer • require hospitalization • treatment for dehydration and infection • require additional caloric intake • severe scarring • may need debridement and skin graft from one part of body to another – Burn area can be estimated by the rule of nines • tool for estimating severity – Secondary Bacterial Infection - Pseudomonas aeruginosa
THE END