ARTERIAL STIFFNESS Dr R V S N Sarma
![Aortic pulse wave Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure Aortic pulse wave Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-23.jpg)
![Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-24.jpg)
![Variation of Einc with stretch Einc [Nm-2 x 105] 15 10 5 0 1. Variation of Einc with stretch Einc [Nm-2 x 105] 15 10 5 0 1.](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-30.jpg)

- Slides: 85
ARTERIAL STIFFNESS Dr. R. V. S. N. Sarma. , M. D. , M. Sc. , (Canada) Consultant Physician and Chest Specialist
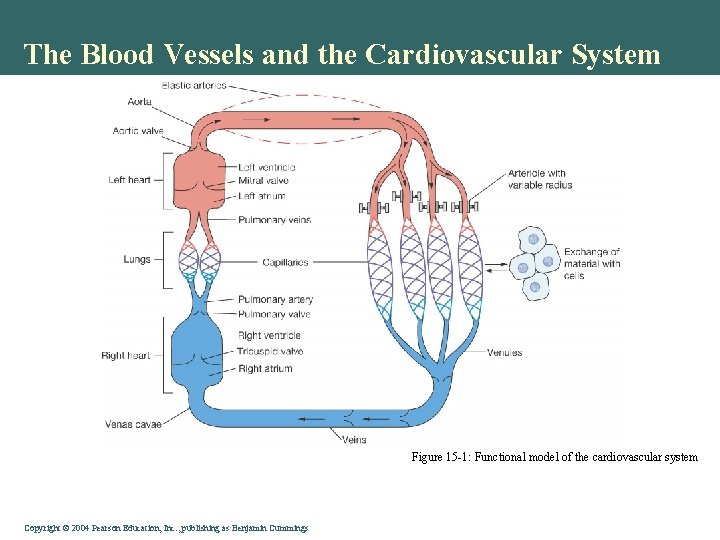
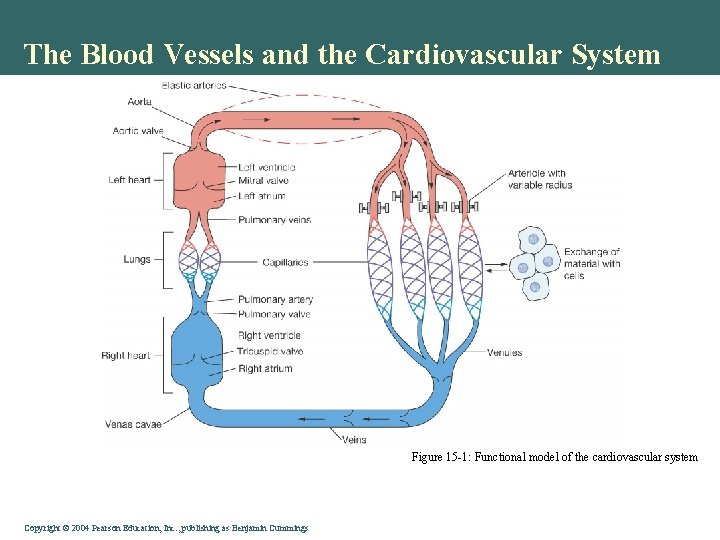
The Blood Vessels and the Cardiovascular System Figure 15 -1: Functional model of the cardiovascular system Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
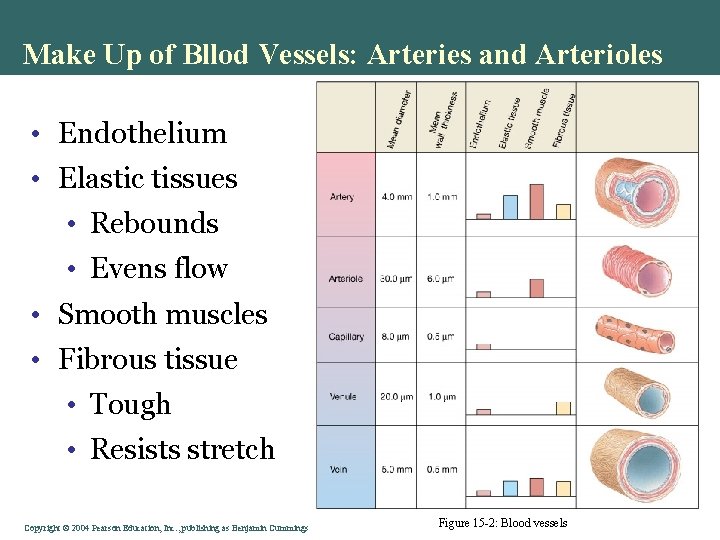
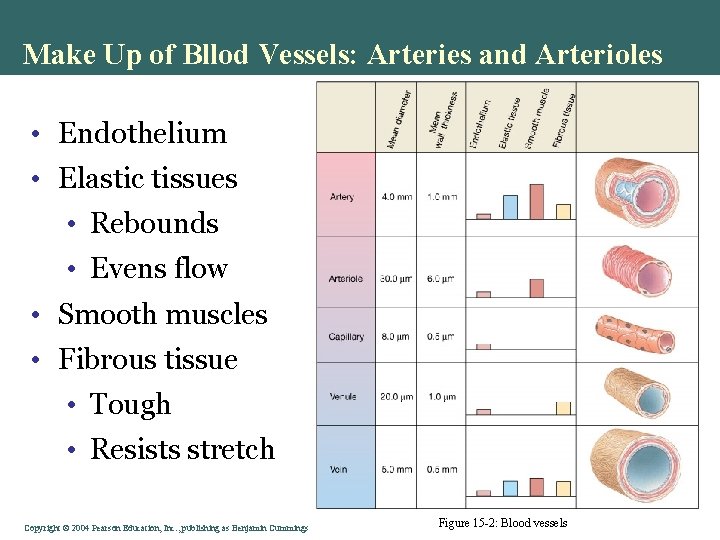
Make Up of Bllod Vessels: Arteries and Arterioles • Endothelium • Elastic tissues • Rebounds • Evens flow • Smooth muscles • Fibrous tissue • Tough • Resists stretch Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 15 -2: Blood vessels
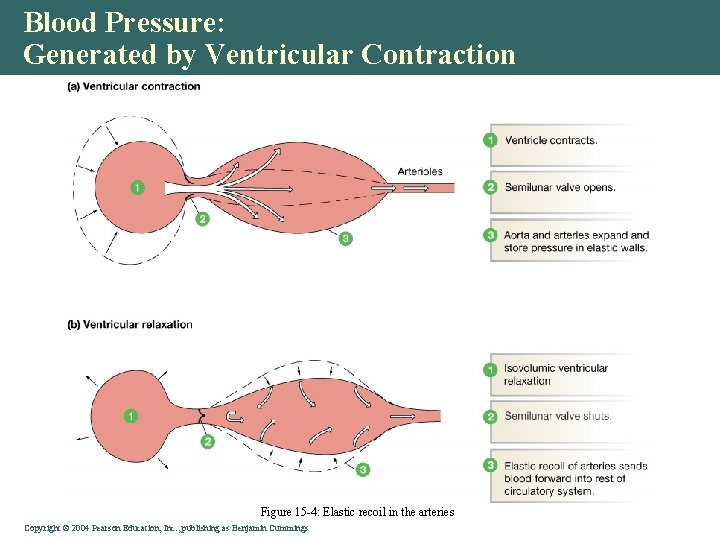
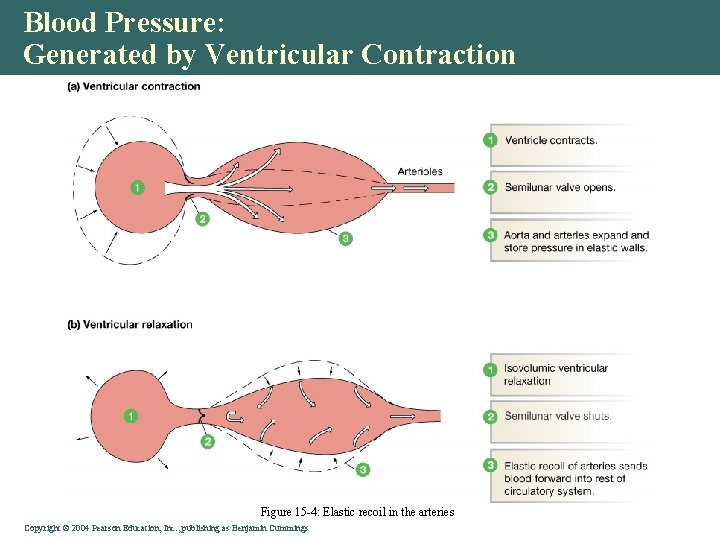
Blood Pressure: Generated by Ventricular Contraction Figure 15 -4: Elastic recoil in the arteries Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
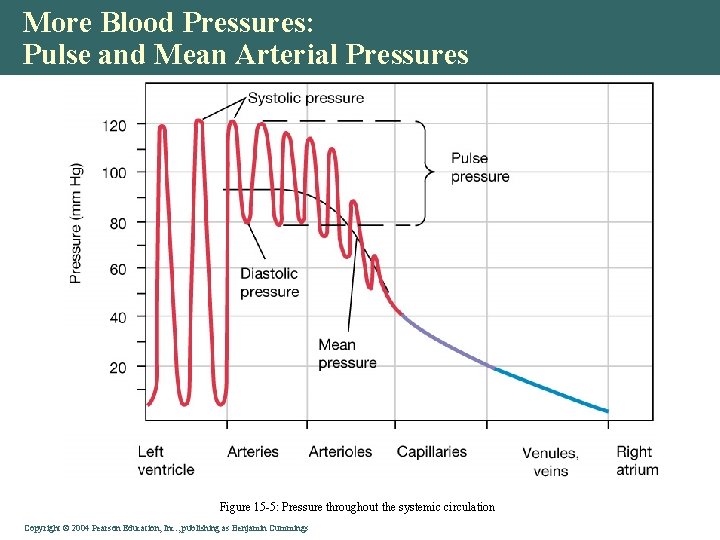
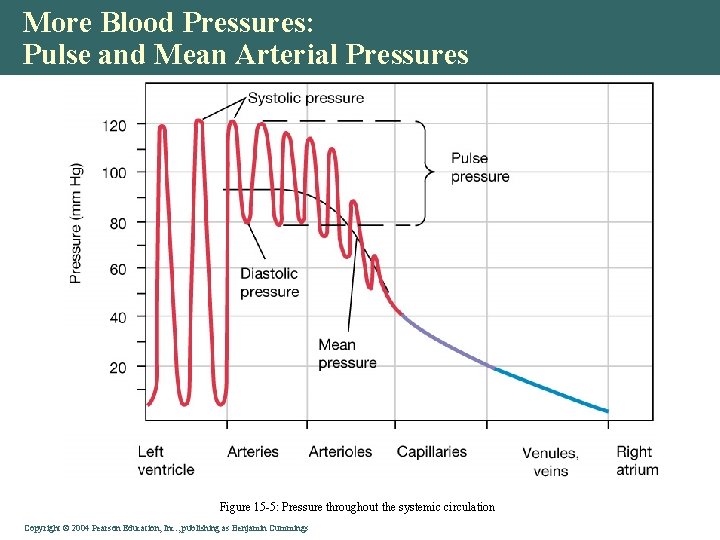
More Blood Pressures: Pulse and Mean Arterial Pressures Figure 15 -5: Pressure throughout the systemic circulation Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
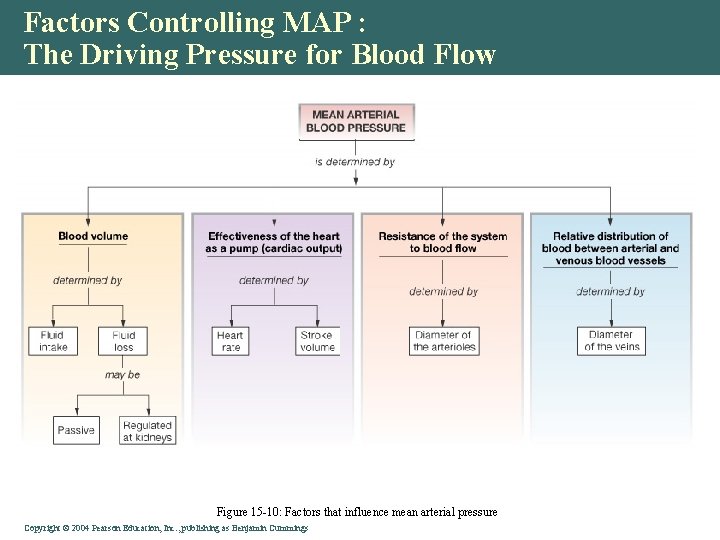
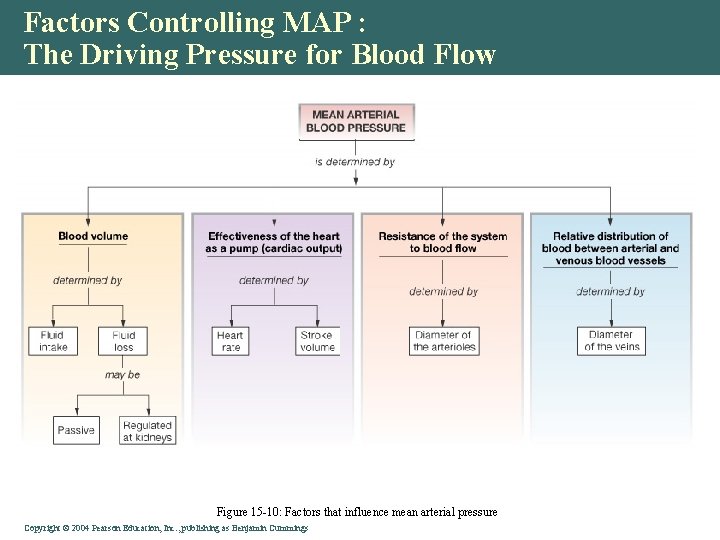
Factors Controlling MAP : The Driving Pressure for Blood Flow Figure 15 -10: Factors that influence mean arterial pressure Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
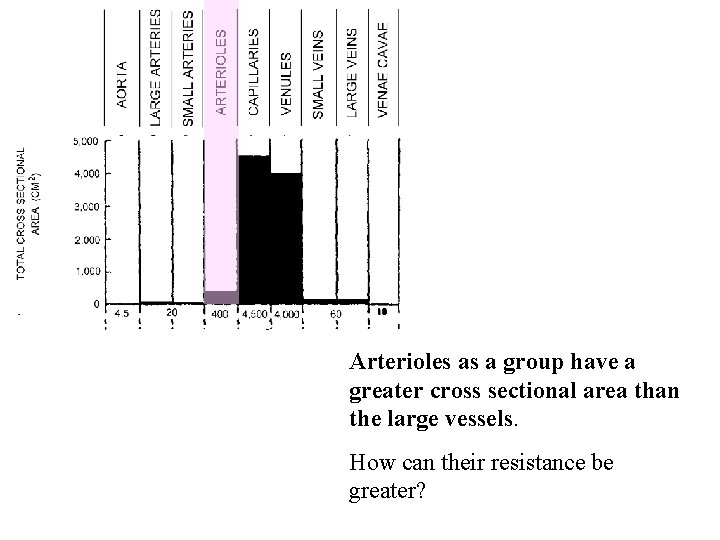
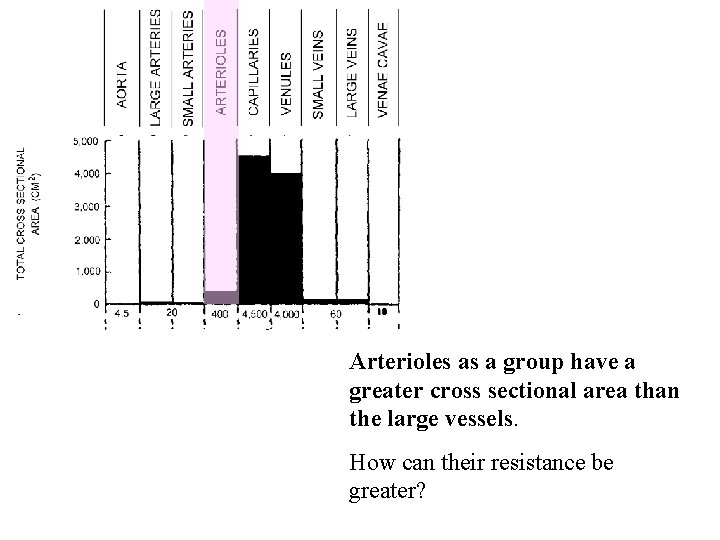
Arterioles as a group have a greater cross sectional area than the large vessels. How can their resistance be greater?
Branching to smaller radius vessels increases resistance r=1 A= 3. 14 Res=1 A r =. 707 A= 1. 57 Res=4 B C B and C in parallel have a combined resistance of 2 and a cross sectional area of 3. 14 Resistance ~ ( r 4) Area ~ (r 2 )
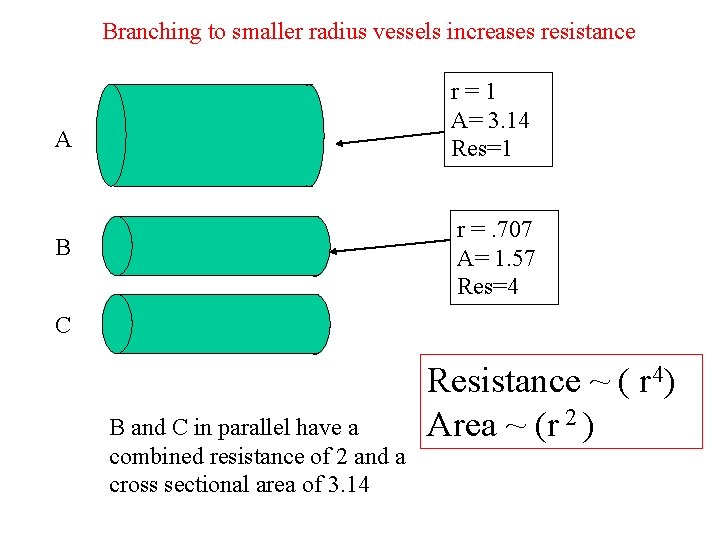
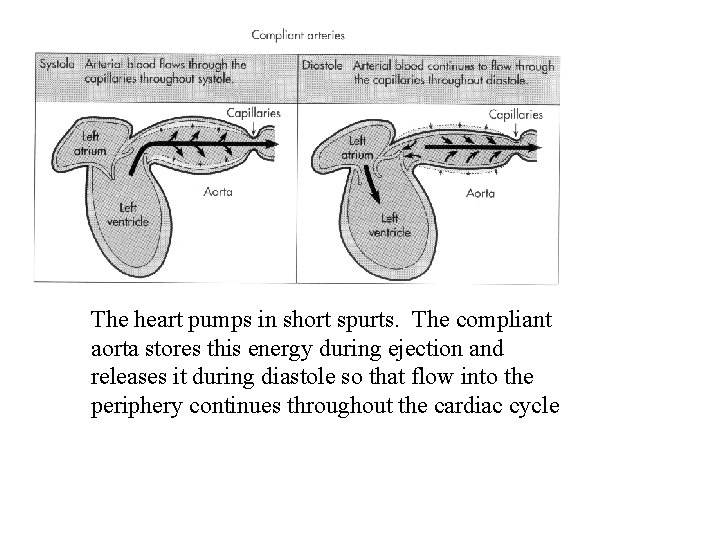
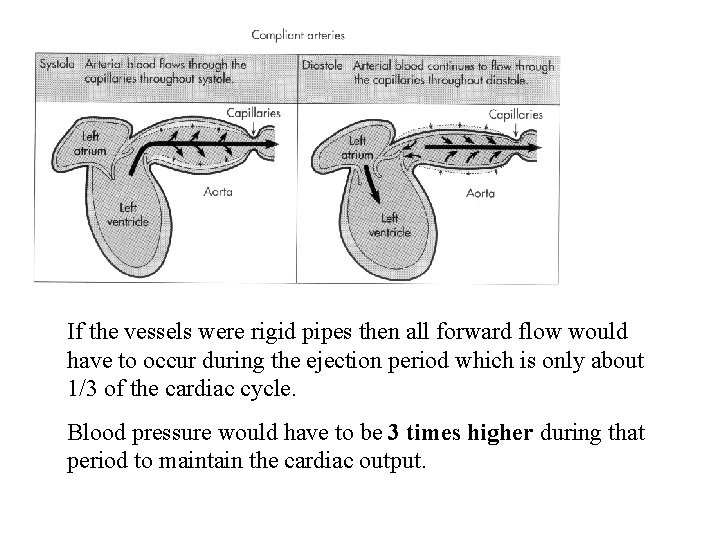
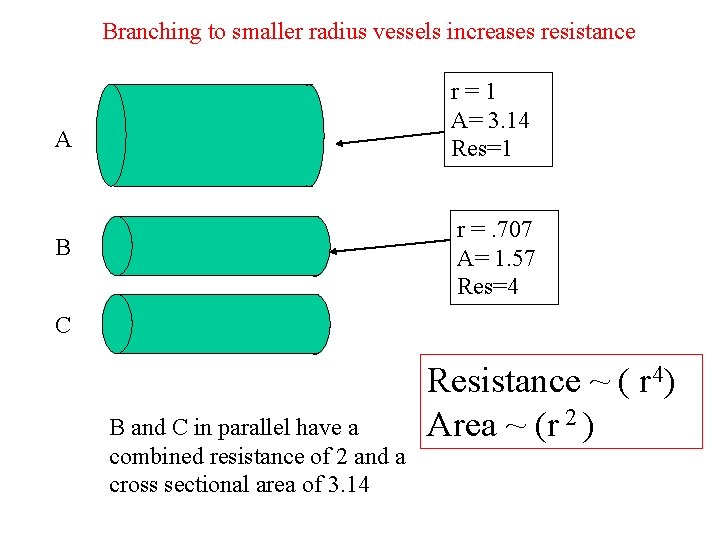
The heart pumps in short spurts. The compliant aorta stores this energy during ejection and releases it during diastole so that flow into the periphery continues throughout the cardiac cycle
The bagpipe player blows into the bag in short spurts. That energy is stored in the bag and the air escapes through the pipes in a continuous stream thanks to the bag's compliance.
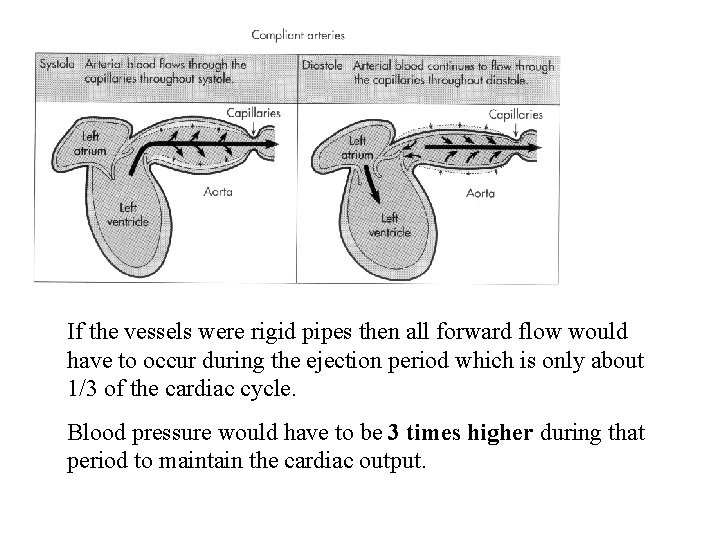
If the vessels were rigid pipes then all forward flow would have to occur during the ejection period which is only about 1/3 of the cardiac cycle. Blood pressure would have to be 3 times higher during that period to maintain the cardiac output.
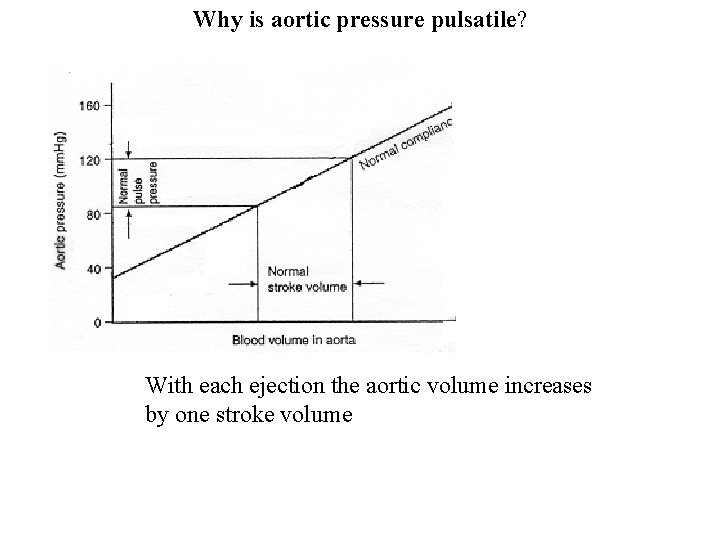
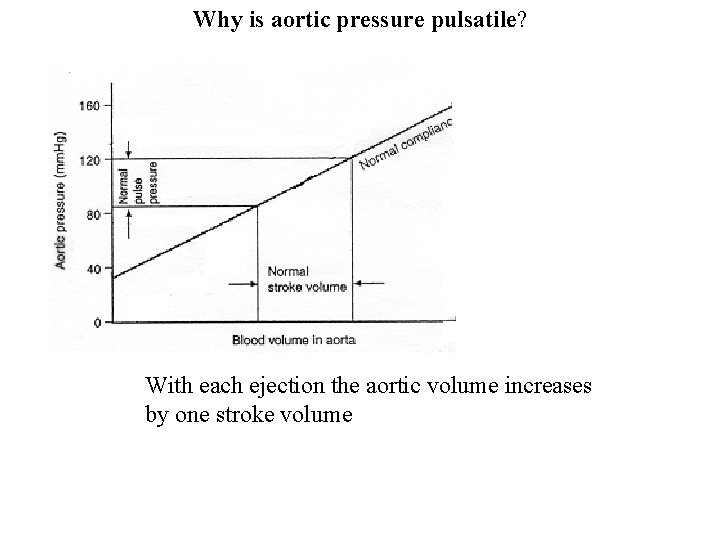
Why is aortic pressure pulsatile? With each ejection the aortic volume increases by one stroke volume
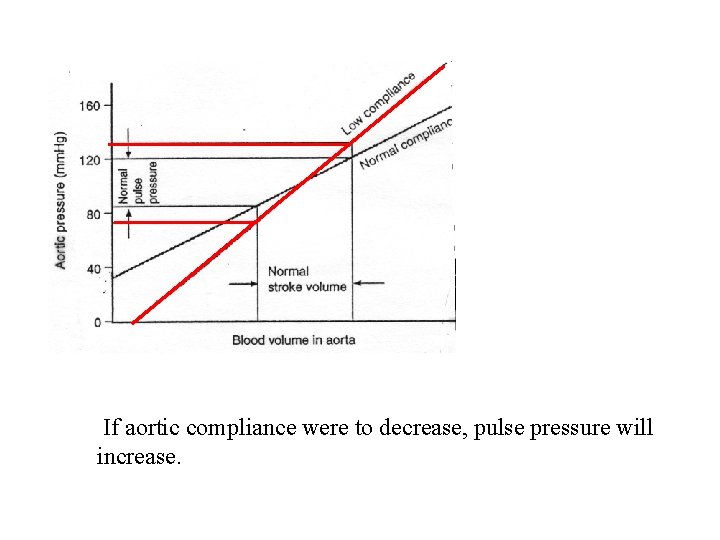
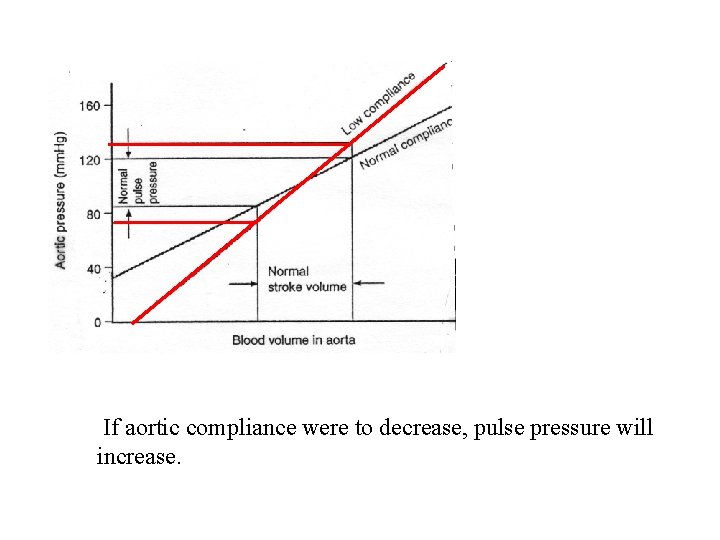
If aortic compliance were to decrease, pulse pressure will increase.
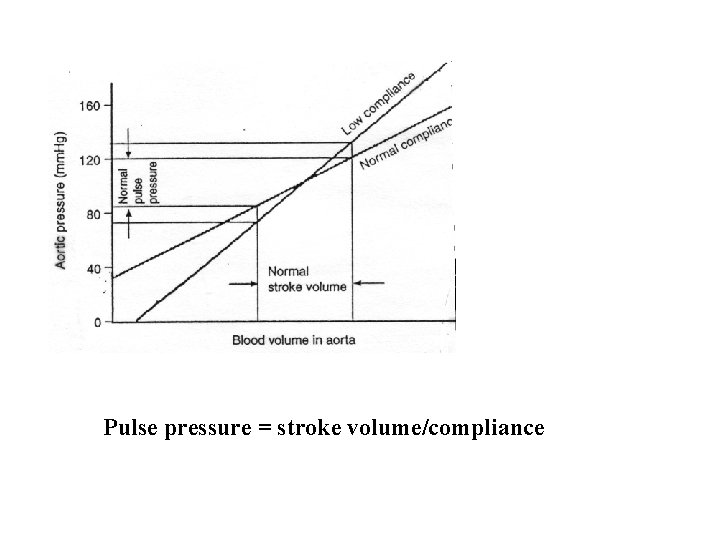
Pulse pressure = stroke volume/compliance
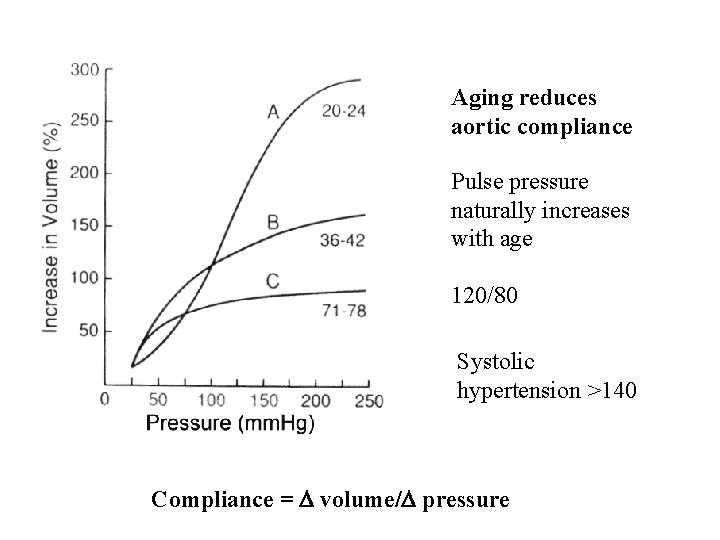
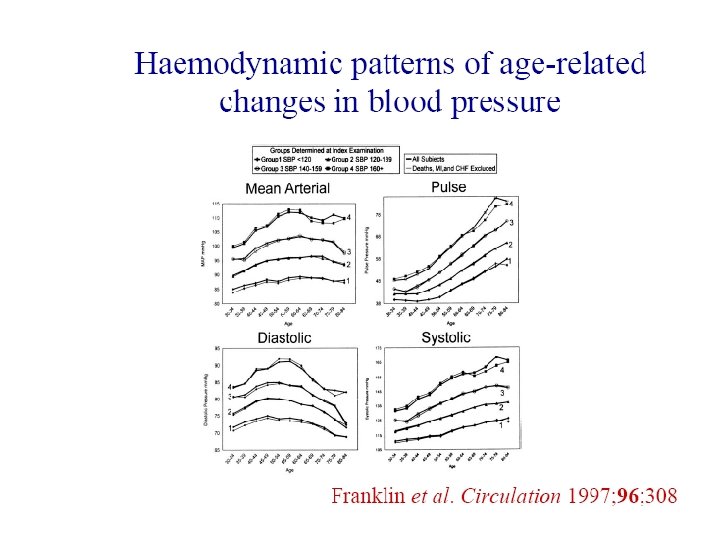
Aging reduces aortic compliance Pulse pressure naturally increases with age 120/80 Systolic hypertension >140 Compliance = volume/ pressure
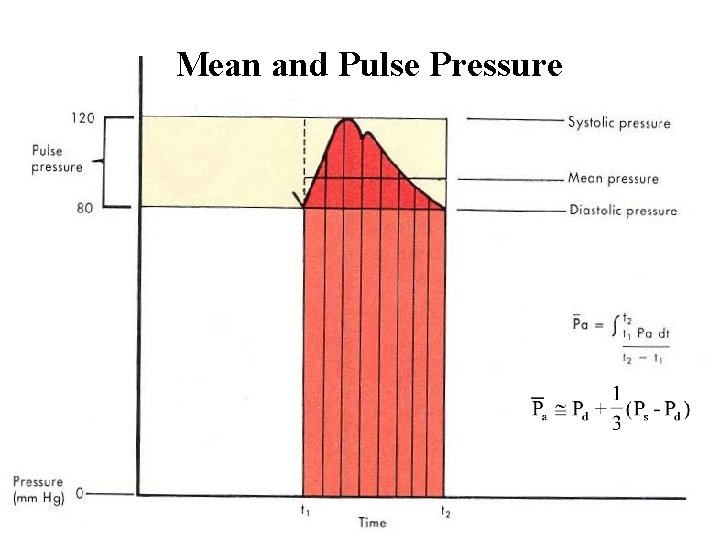
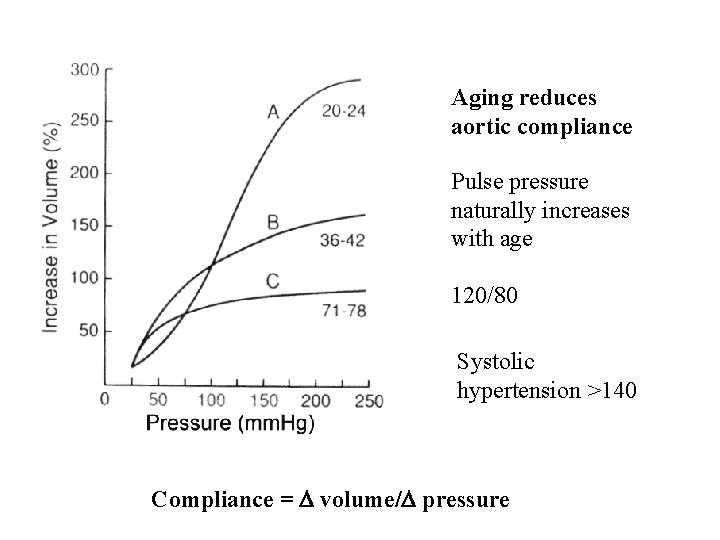
Mean and Pulse Pressure
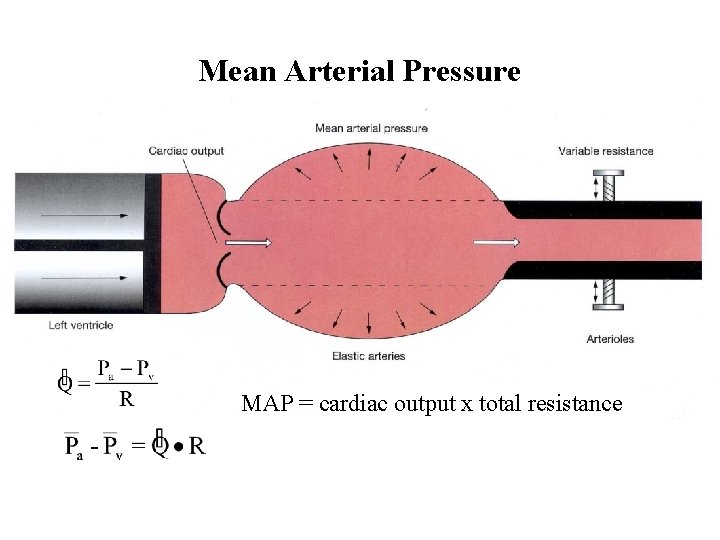
Mean Arterial Pressure MAP = cardiac output x total resistance
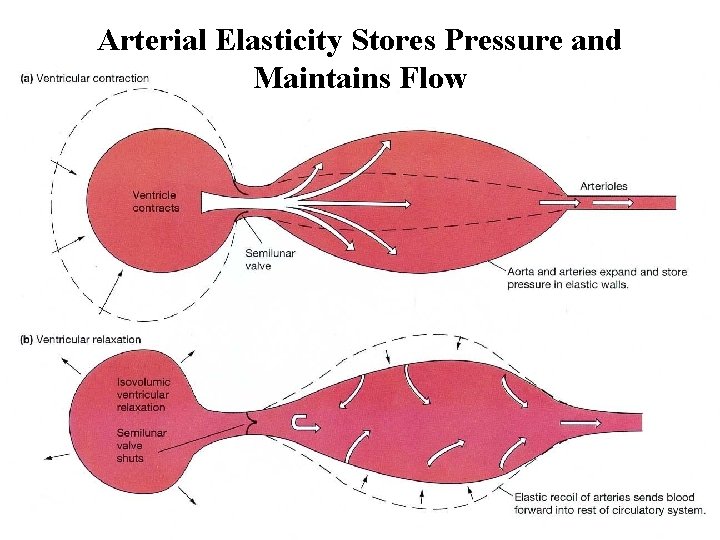
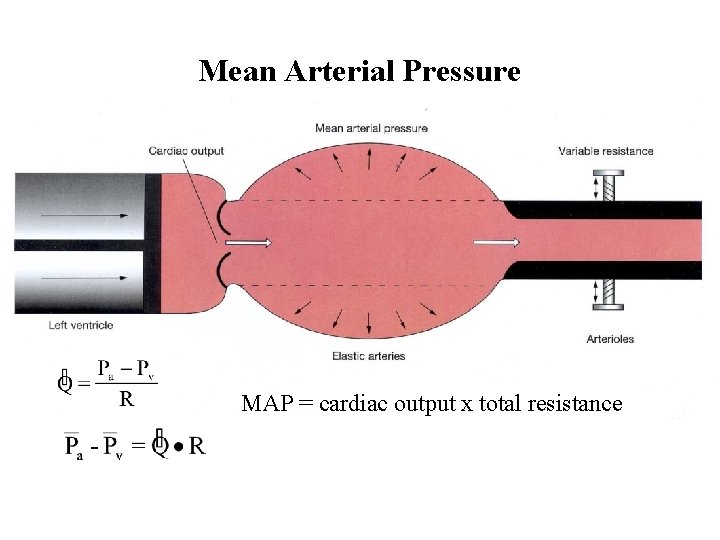
Arterial Elasticity Stores Pressure and Maintains Flow
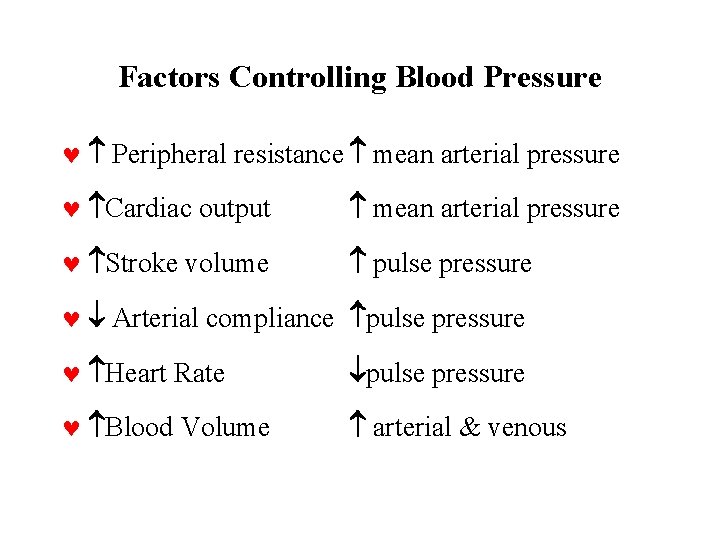
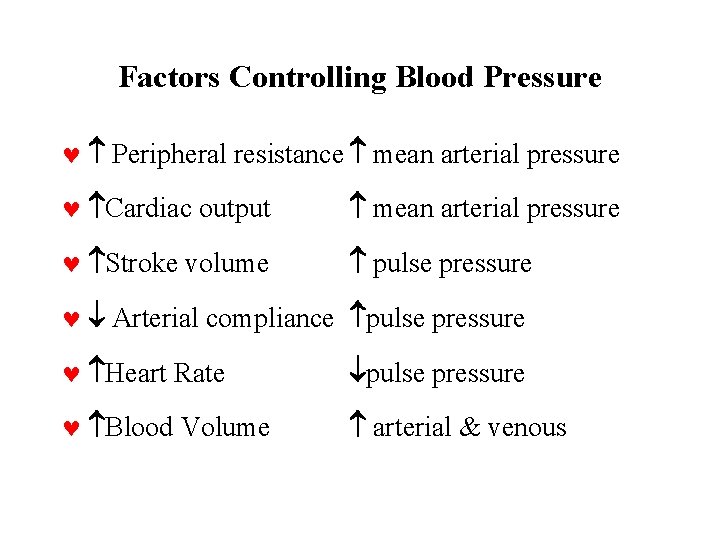
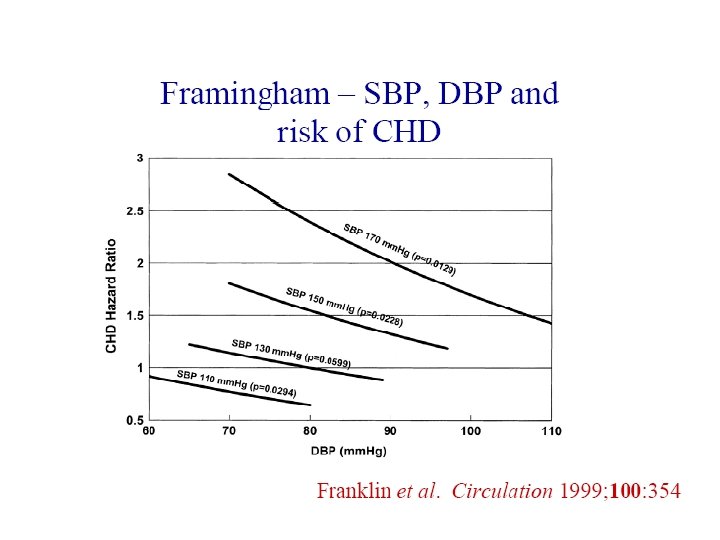
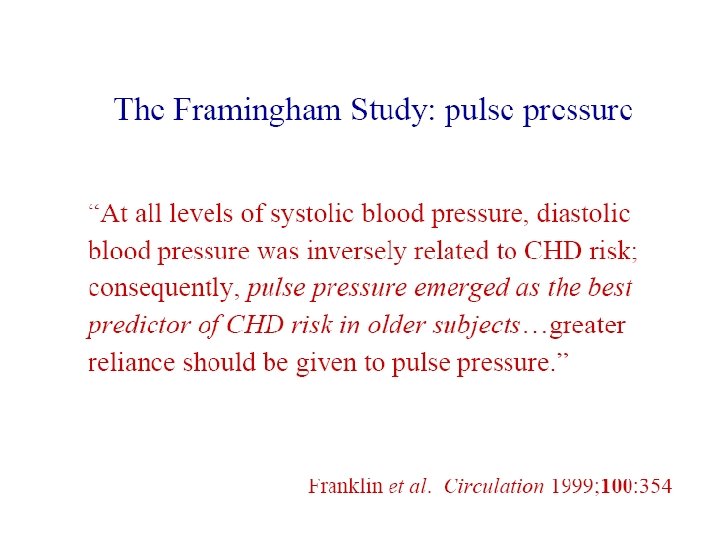
Factors Controlling Blood Pressure © Peripheral resistance mean arterial pressure © Cardiac output mean arterial pressure © Stroke volume pulse pressure © Arterial compliance pulse pressure © Heart Rate pulse pressure © Blood Volume arterial & venous
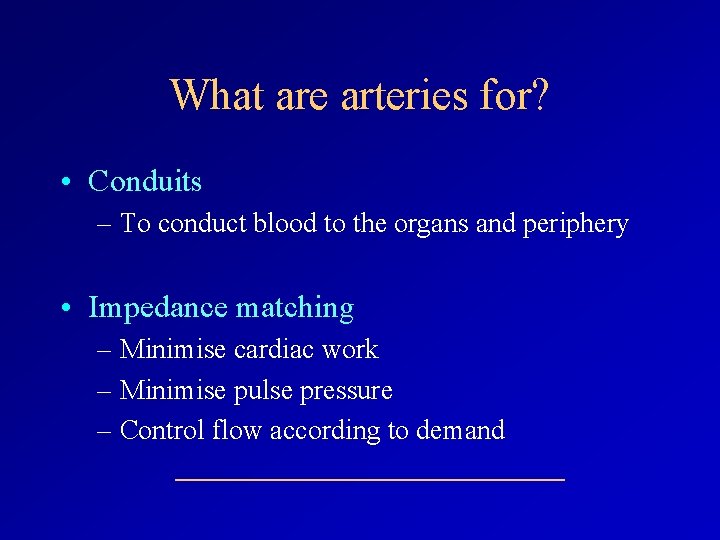
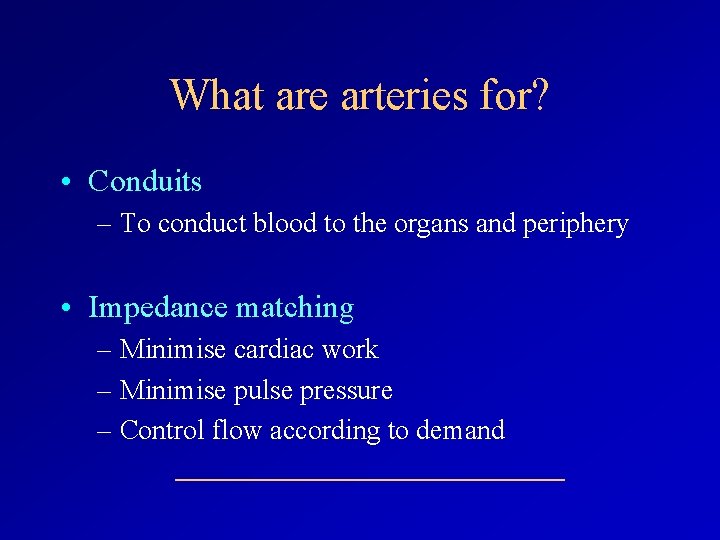
What are arteries for? • Conduits – To conduct blood to the organs and periphery • Impedance matching – Minimise cardiac work – Minimise pulse pressure – Control flow according to demand
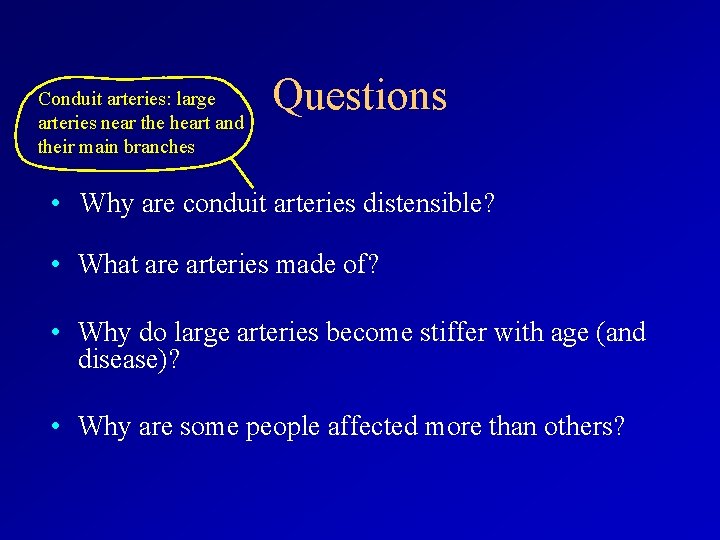
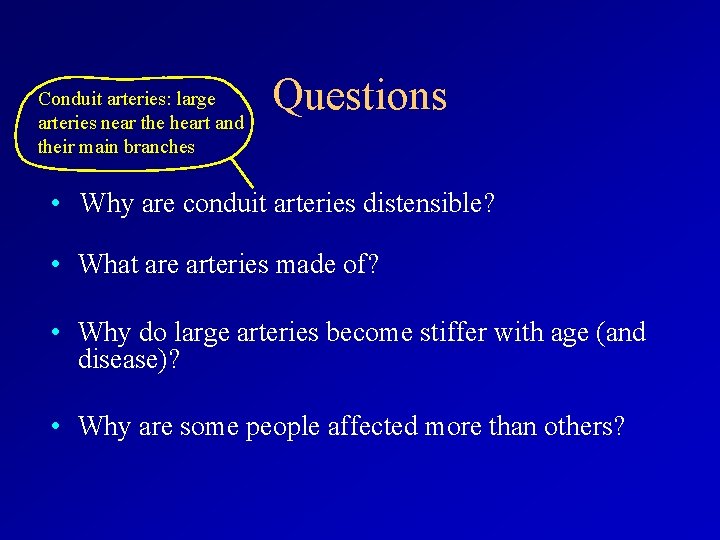
Conduit arteries: large arteries near the heart and their main branches Questions • Why are conduit arteries distensible? • What are arteries made of? • Why do large arteries become stiffer with age (and disease)? • Why are some people affected more than others?
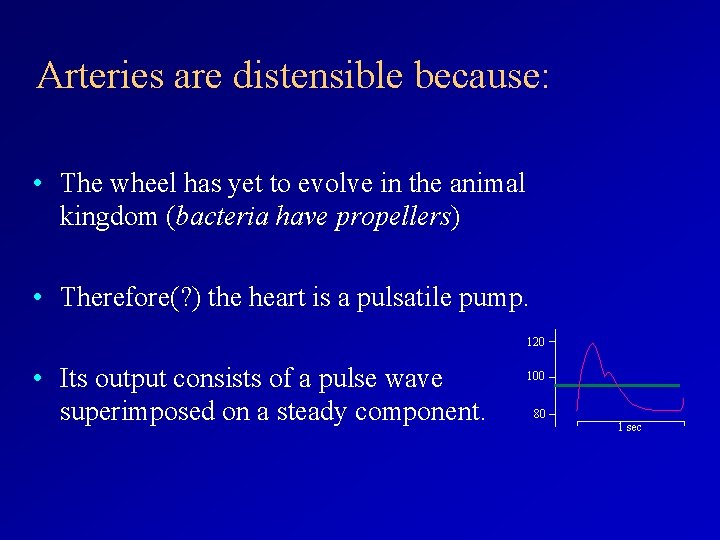
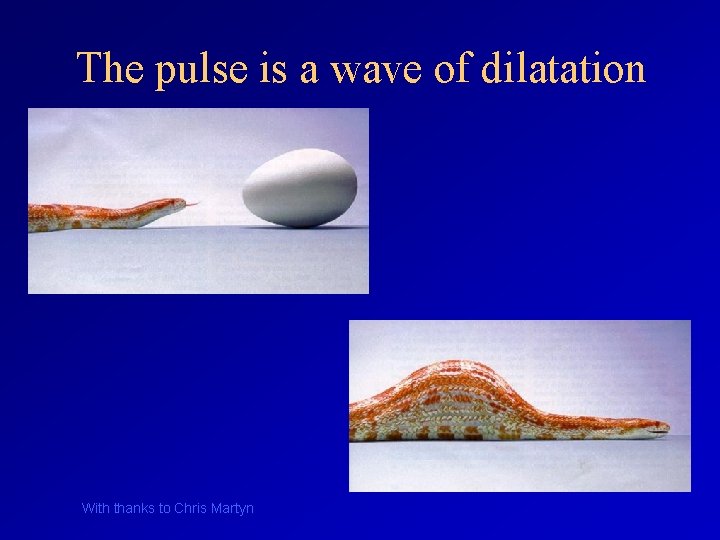
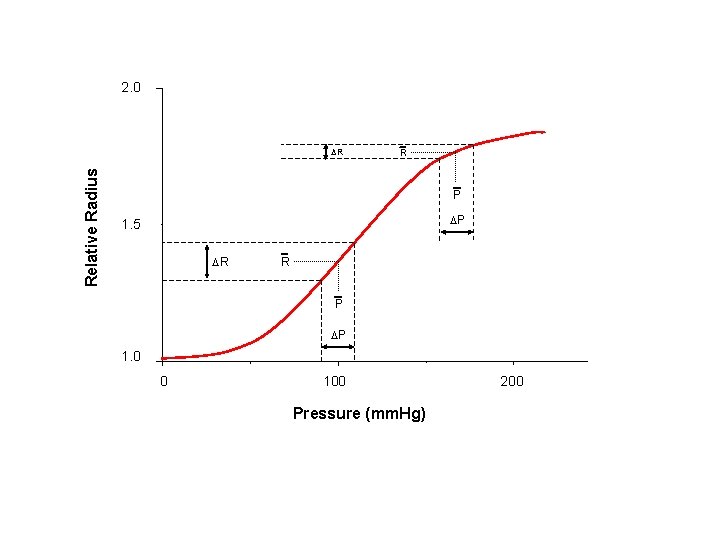
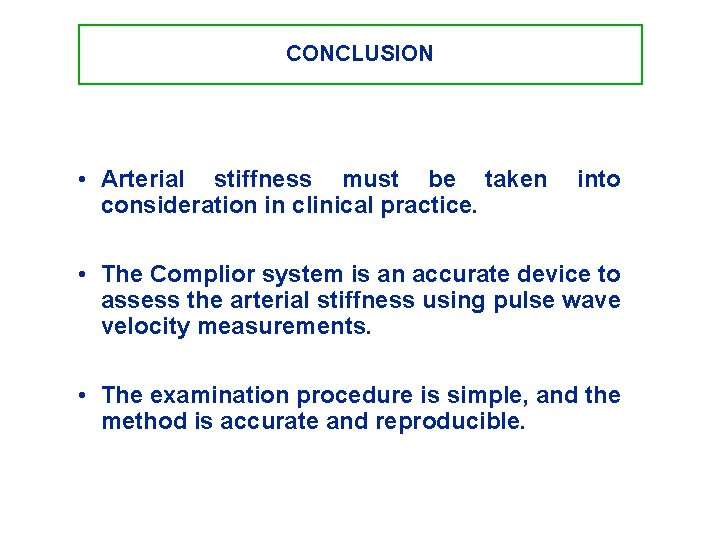
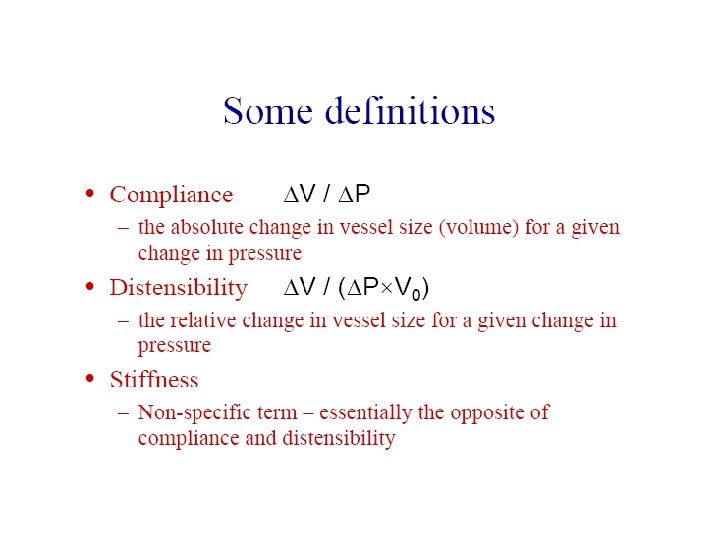
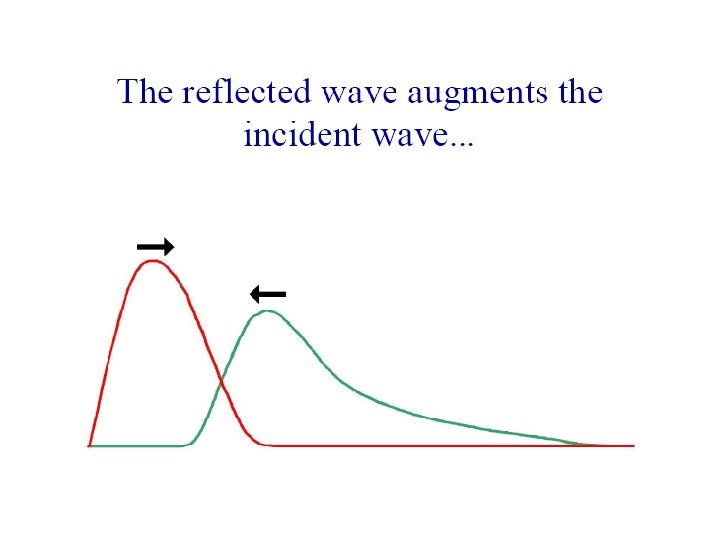
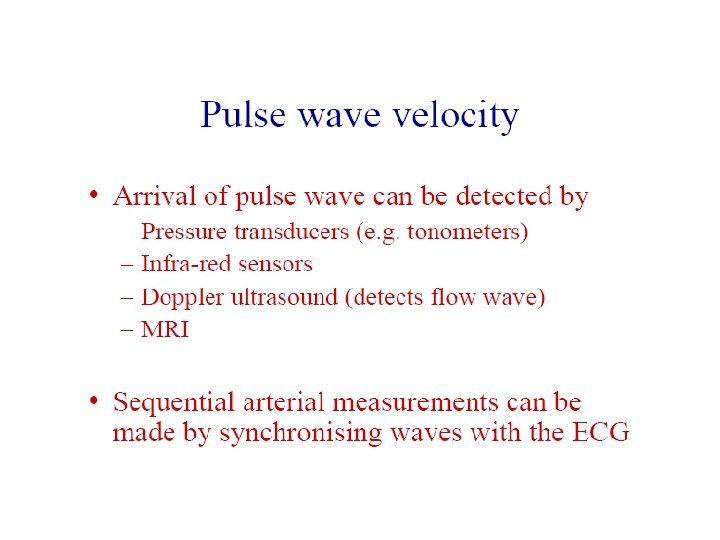
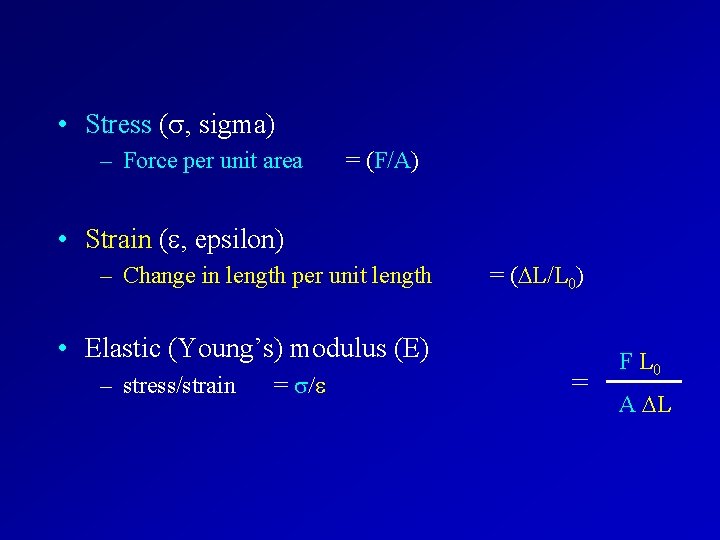
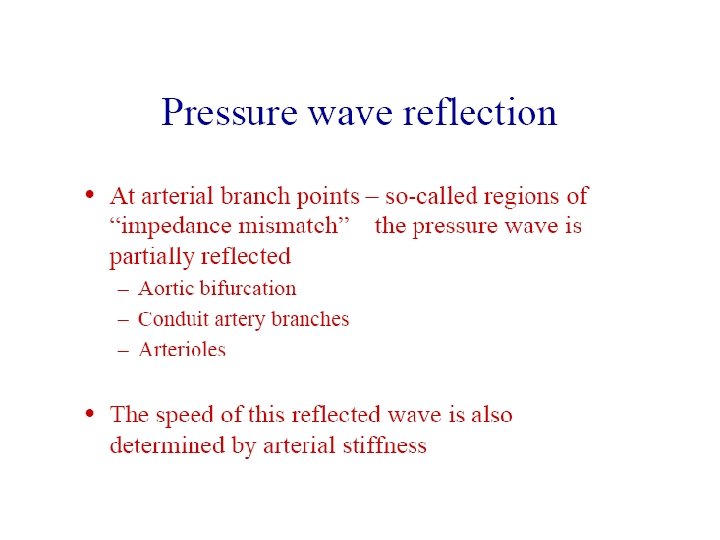
Arteries are distensible because: • The wheel has yet to evolve in the animal kingdom (bacteria have propellers) • Therefore(? ) the heart is a pulsatile pump. 120 • Its output consists of a pulse wave superimposed on a steady component. 100 80 1 sec
![Aortic pulse wave Pressure mm Hg Systolic pressure 120 100 80 Mean Arterial Pressure Aortic pulse wave Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-23.jpg)
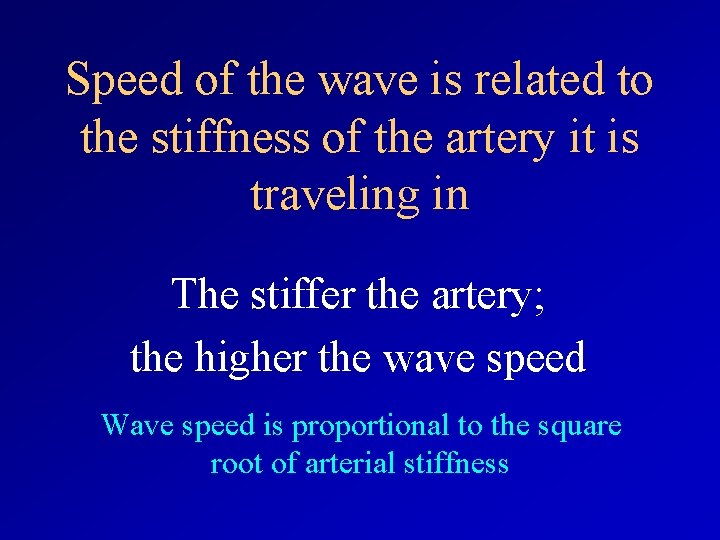
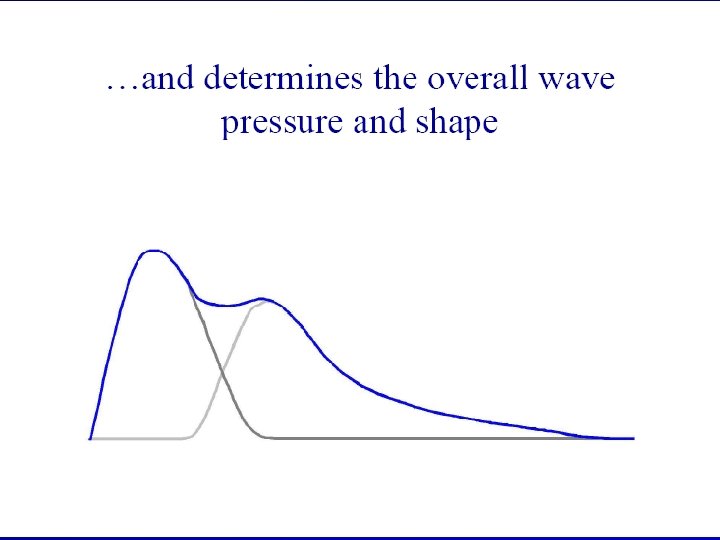
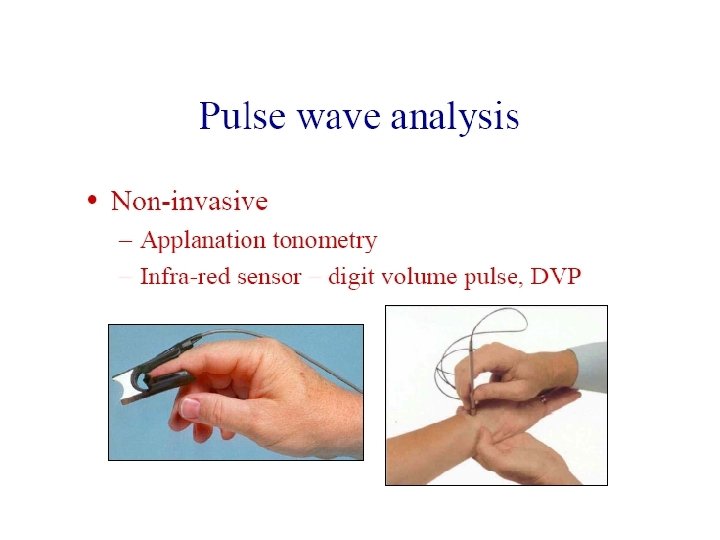
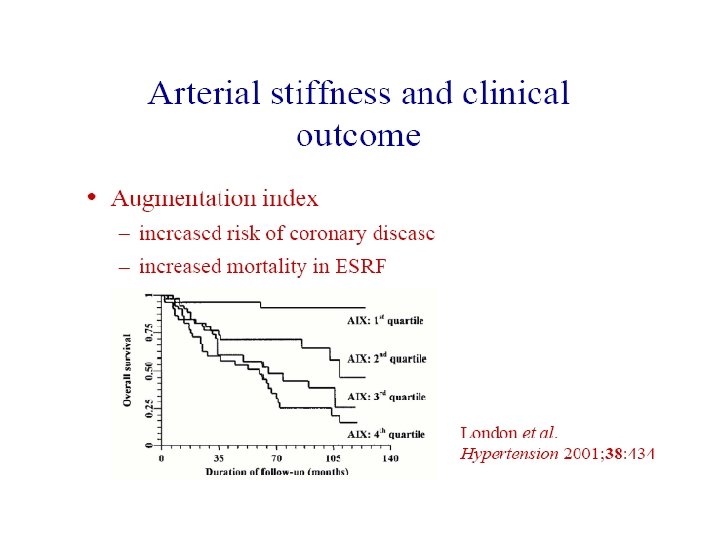
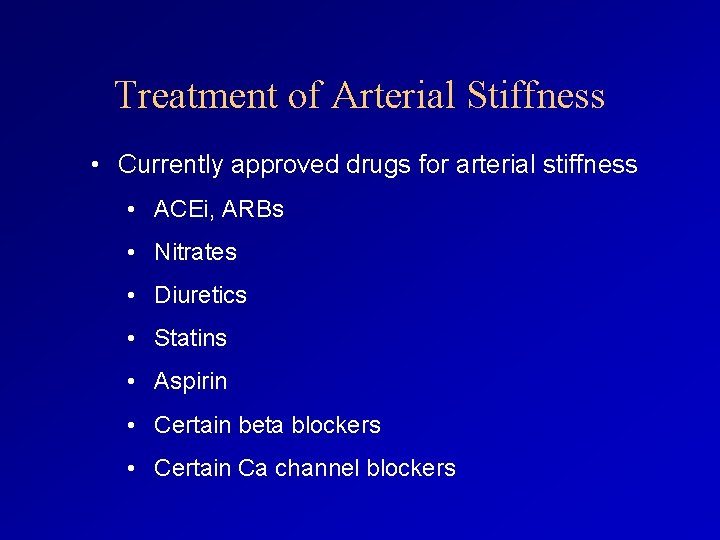
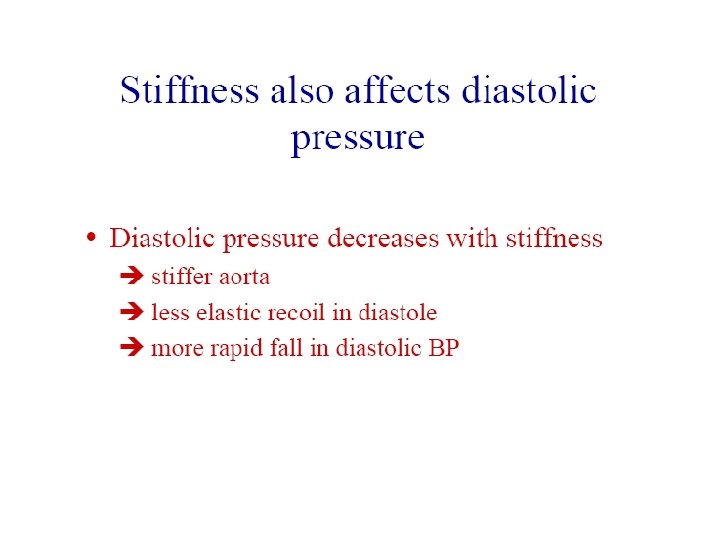
Aortic pulse wave Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic pressure Pulse pressure = systolic pressure - diastolic pressure
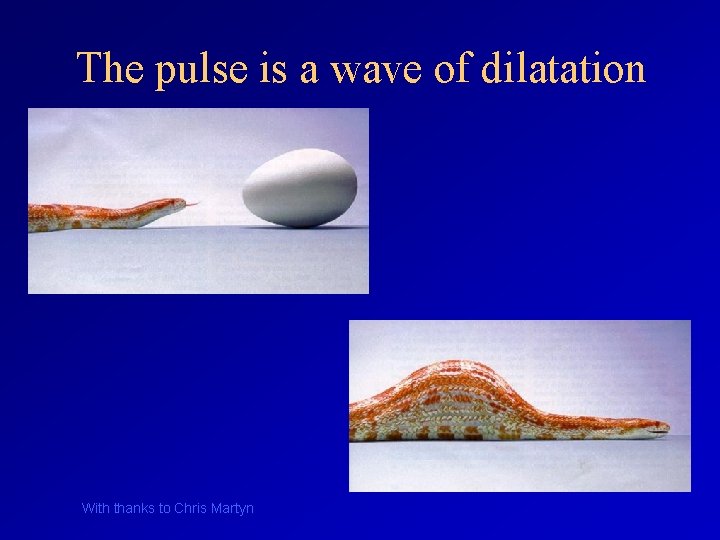
![Pressure mm Hg Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-24.jpg)
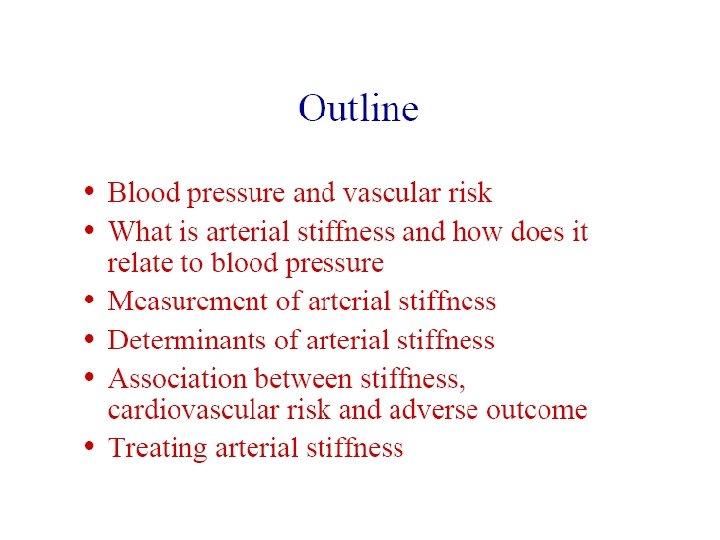
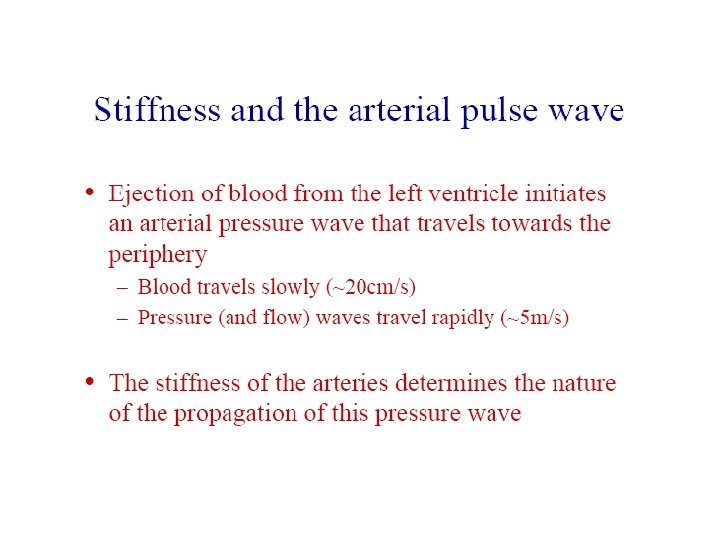
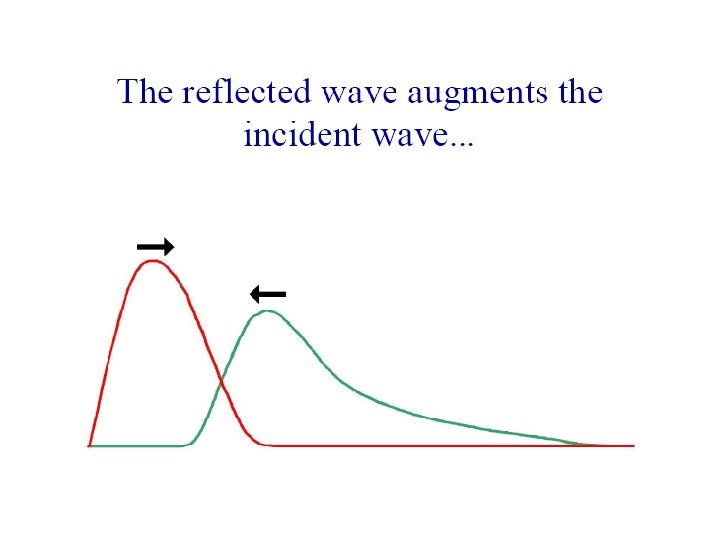
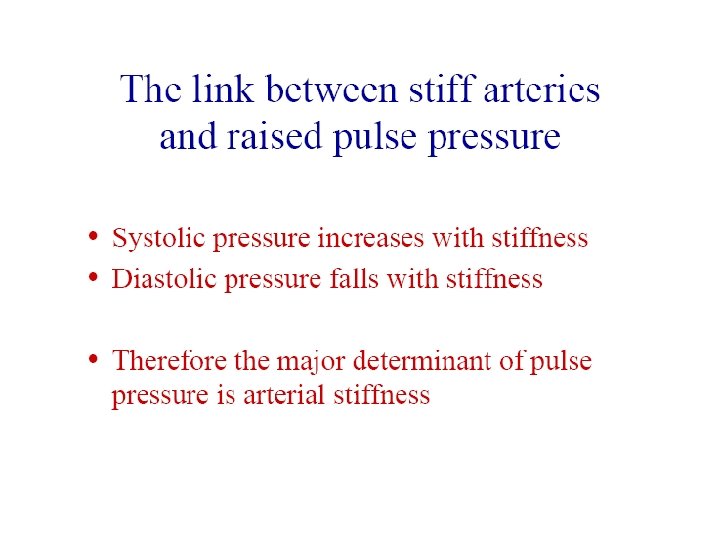
Pressure [mm. Hg] Systolic pressure 120 100 80 Mean Arterial Pressure 1 second Diastolic pressure Pulse pressure = systolic pressure - diastolic pressure • MAP determined by resistance of peripheral arteries = Pd +1/3 PP • Pulse pressure determined by elasticity of large arteries
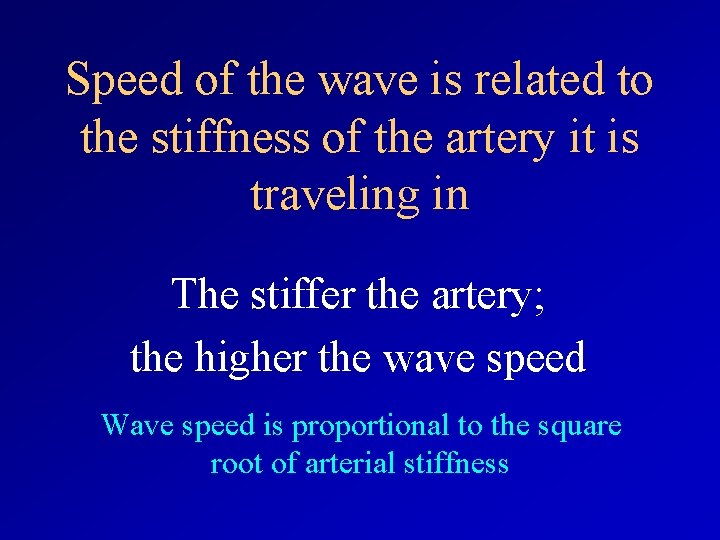
The pulse is a wave of dilatation With thanks to Chris Martyn
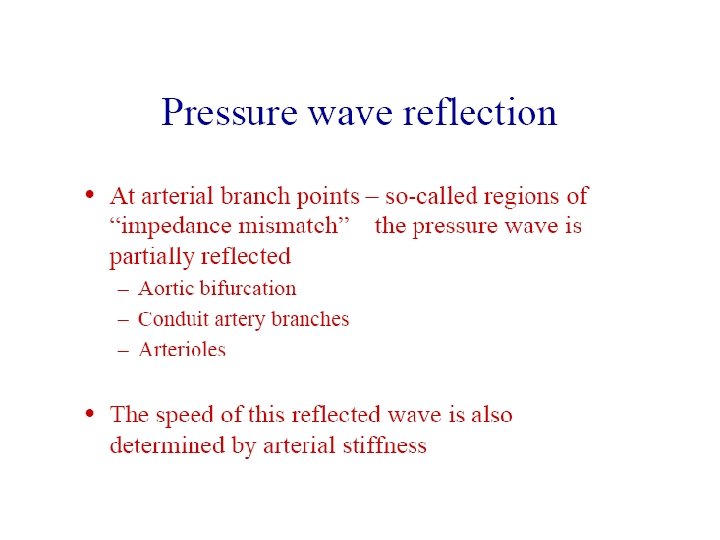
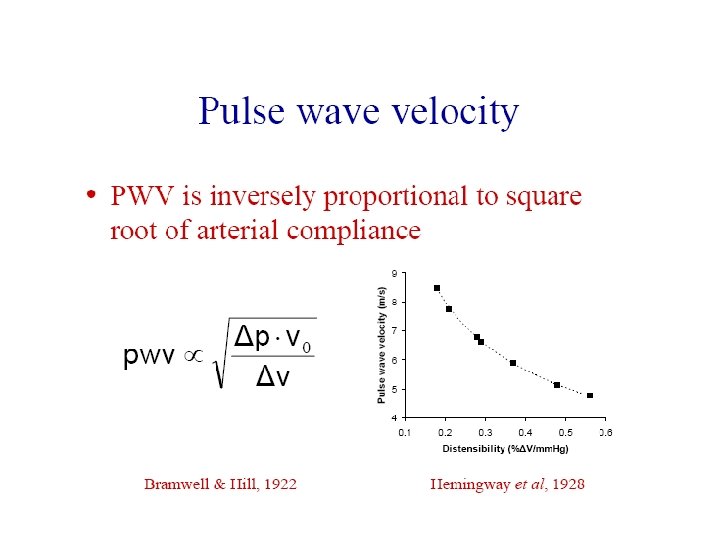
Speed of the wave is related to the stiffness of the artery it is traveling in The stiffer the artery; the higher the wave speed Wave speed is proportional to the square root of arterial stiffness
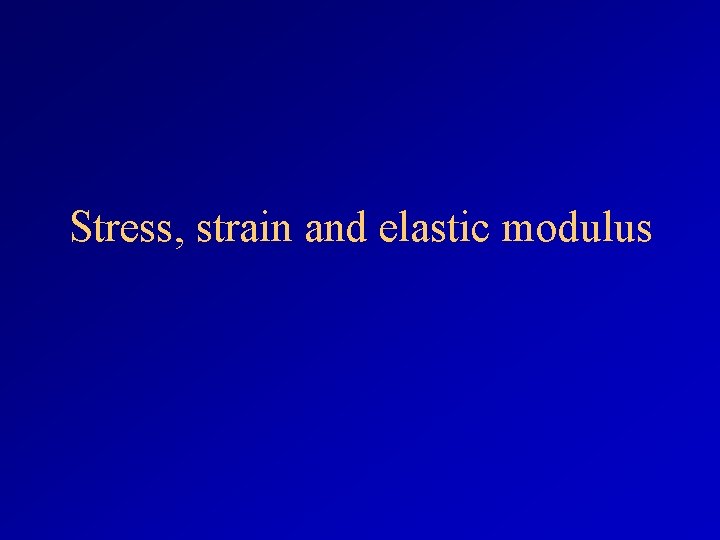
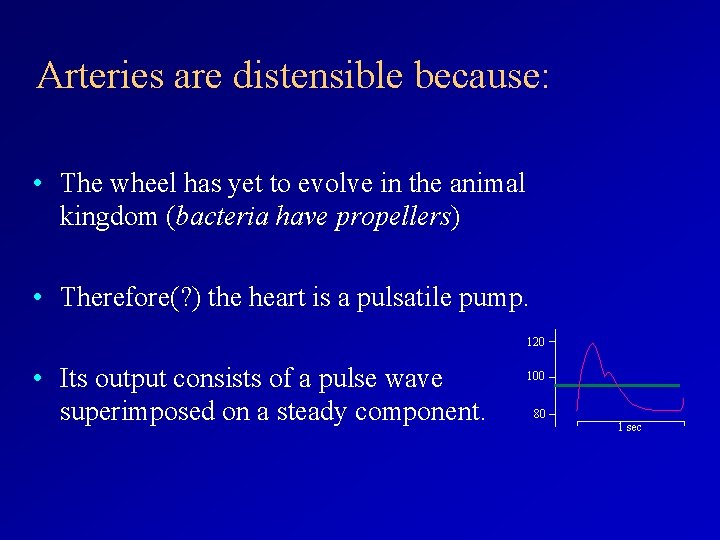
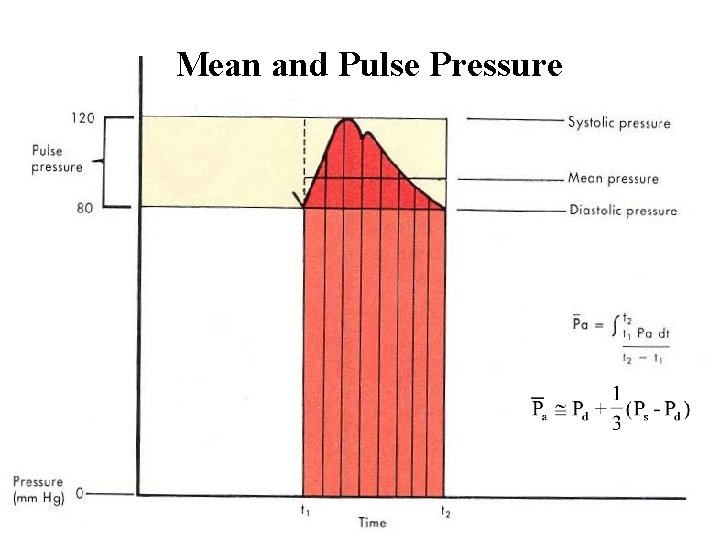
Stress, strain and elastic modulus
• Stress ( , sigma) – Force per unit area = (F/A) • Strain ( , epsilon) – Change in length per unit length = ( L/L 0) • Elastic (Young’s) modulus (E) – stress/strain = / = F L 0 A L
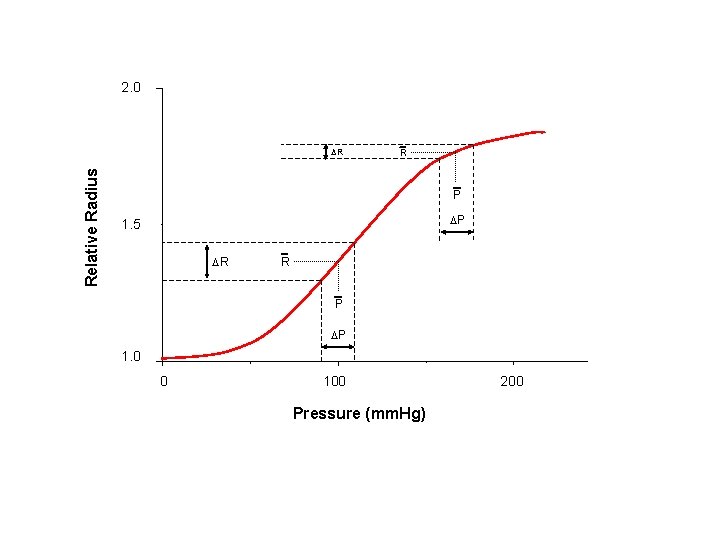
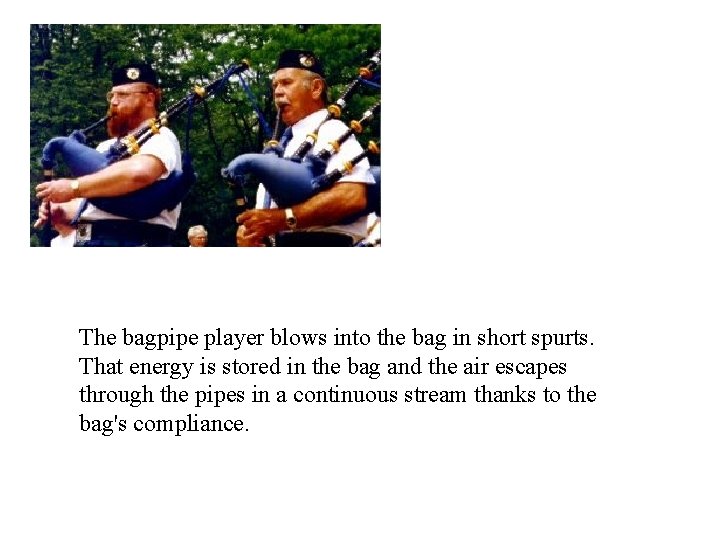
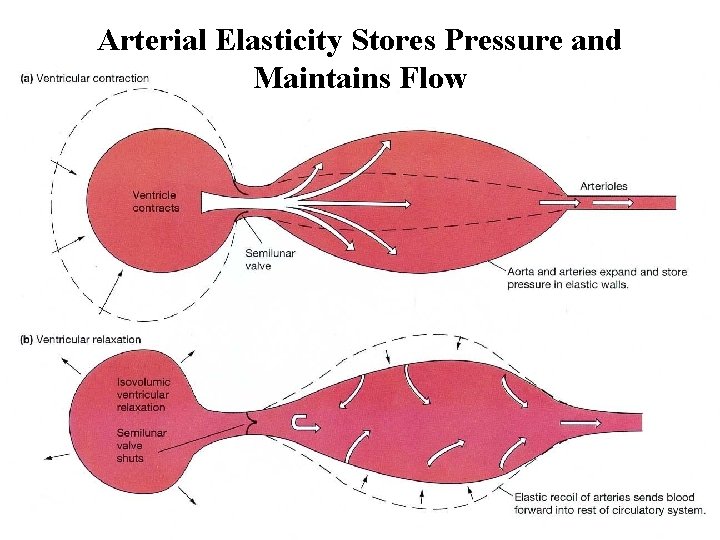
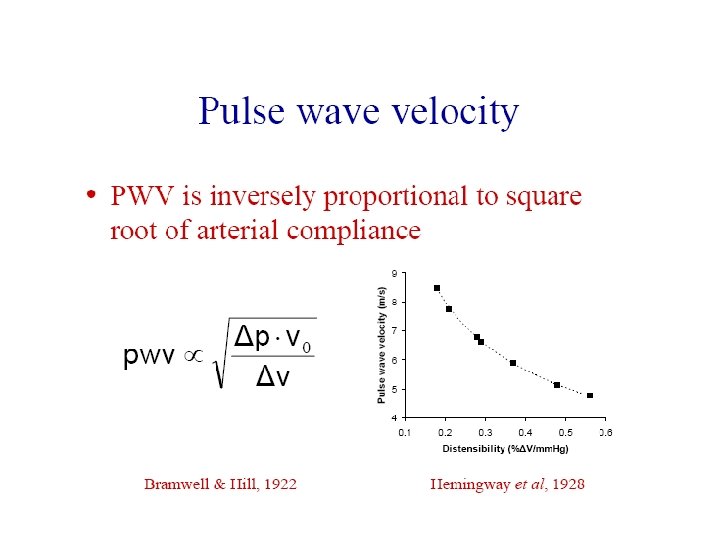
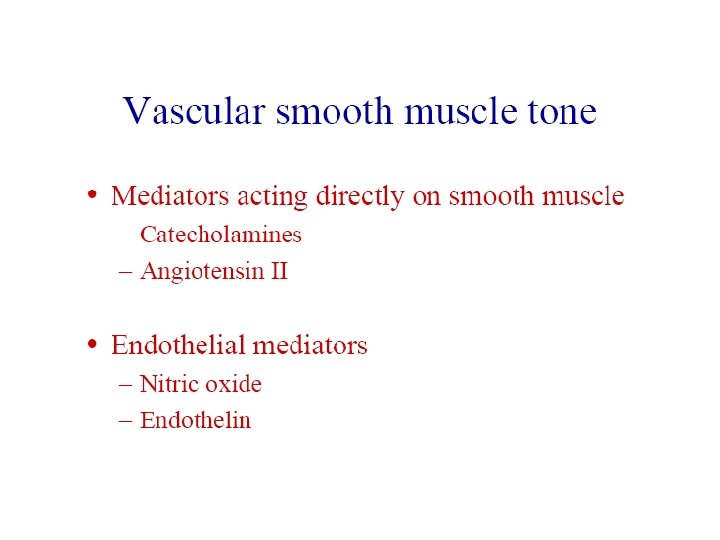
2. 0 Relative Radius R R P P 1. 5 R R P P 1. 0 0 100 Pressure (mm. Hg) 200
![Variation of Einc with stretch Einc Nm2 x 105 15 10 5 0 1 Variation of Einc with stretch Einc [Nm-2 x 105] 15 10 5 0 1.](https://slidetodoc.com/presentation_image_h2/f0c235299cc305a71cc38ccb470e2d40/image-30.jpg)
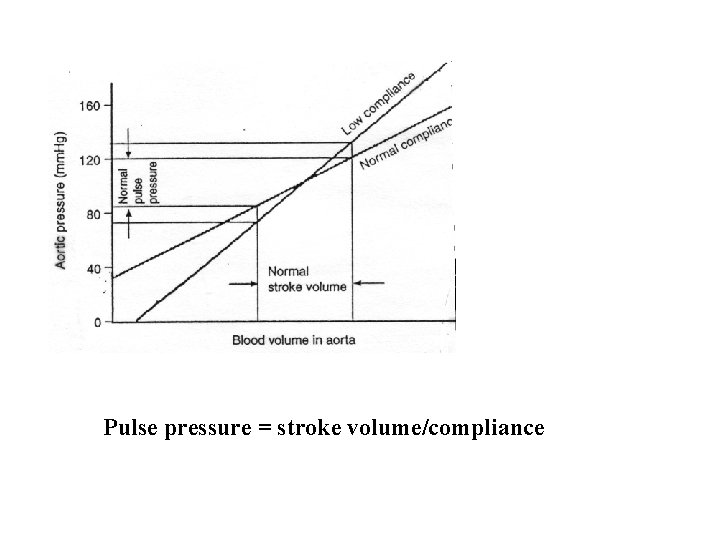
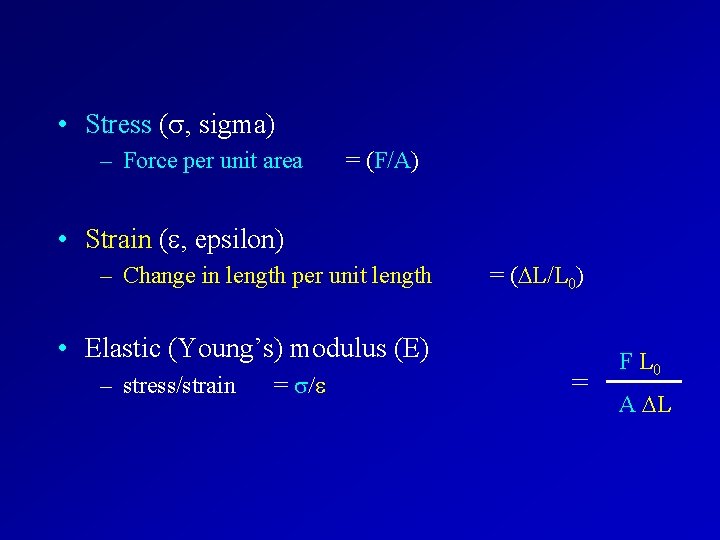
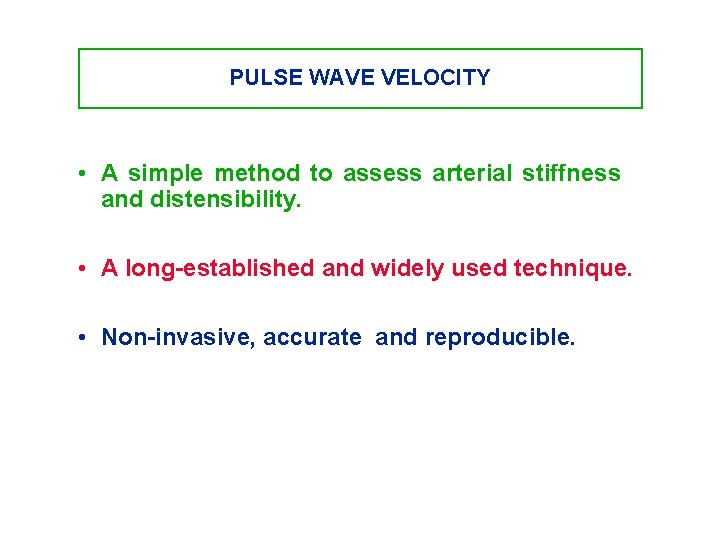
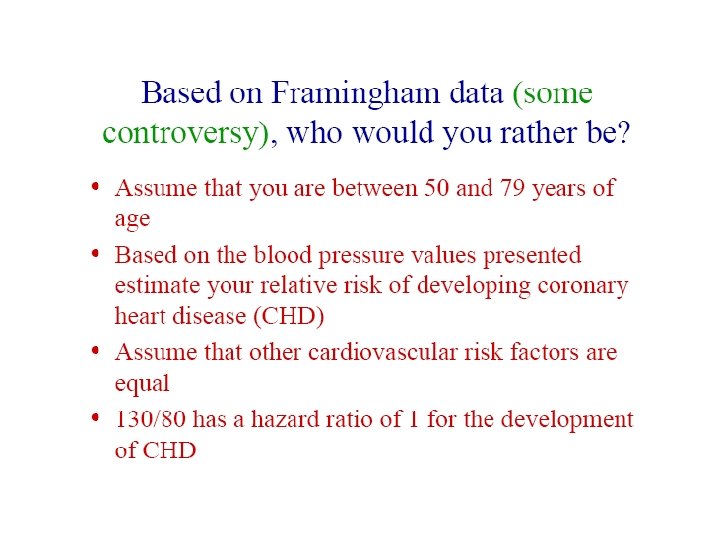
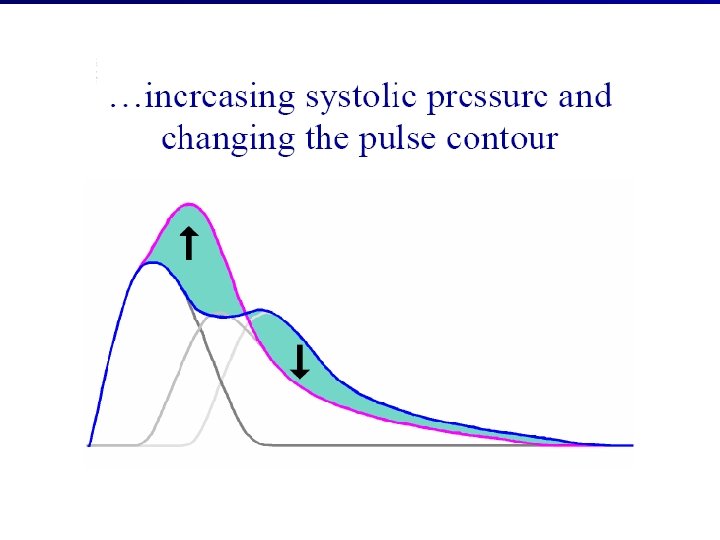
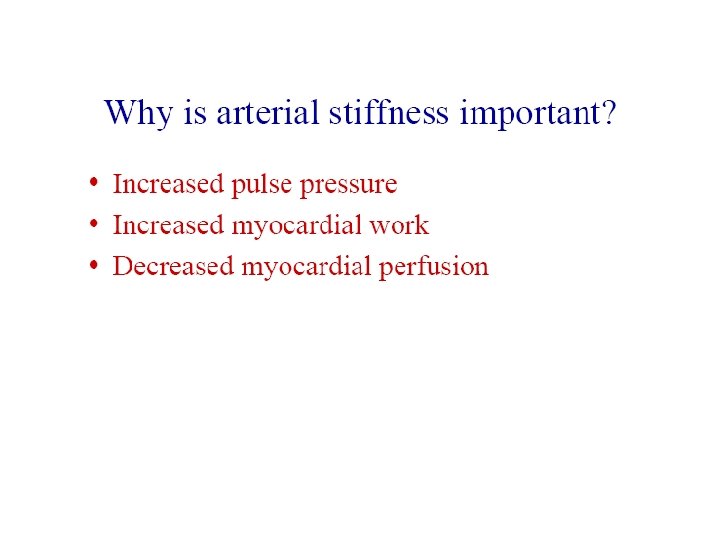
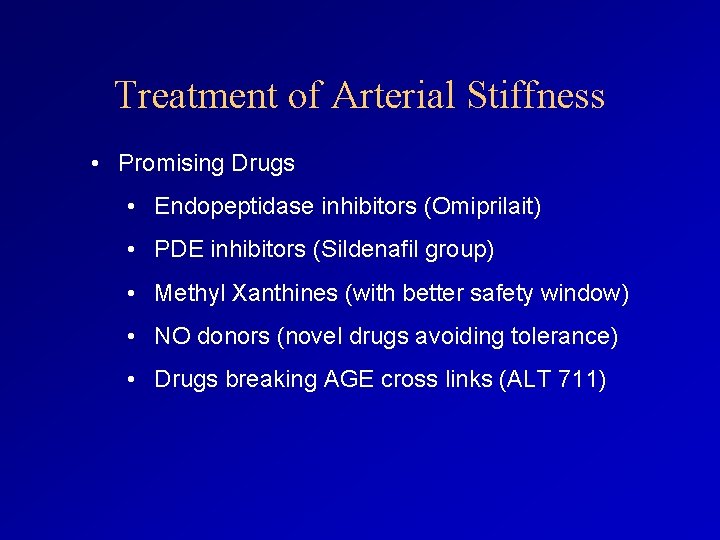
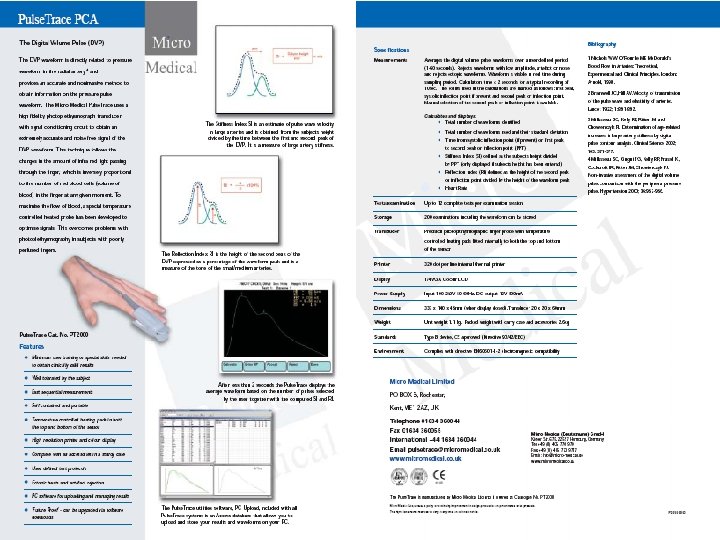
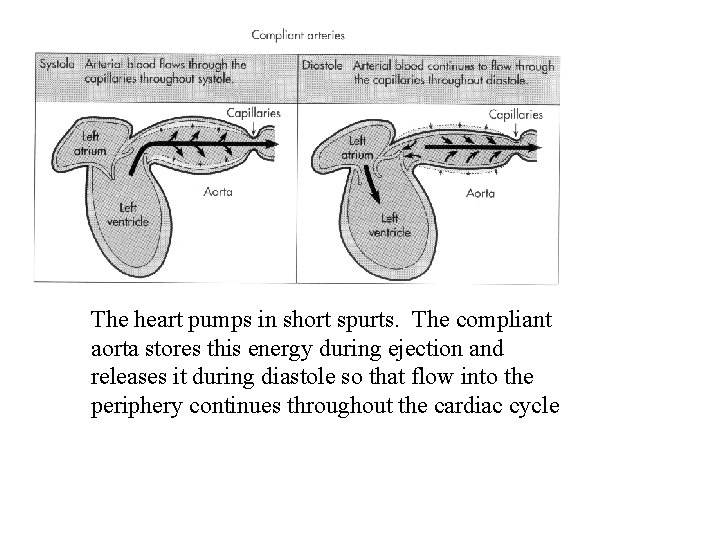
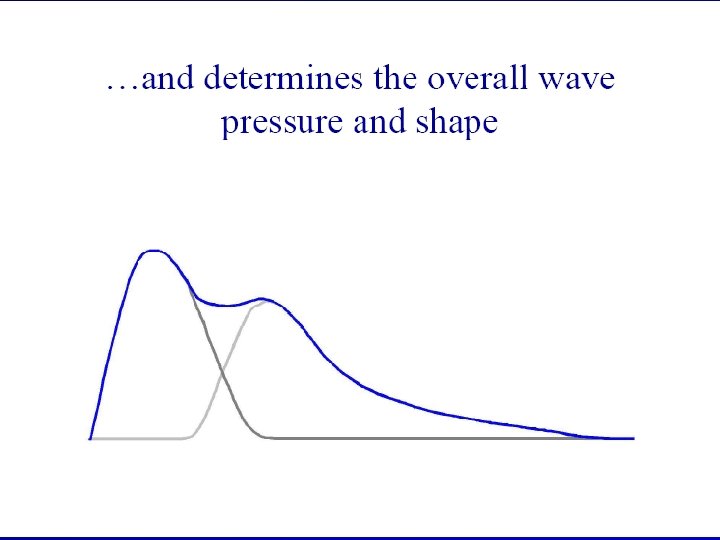
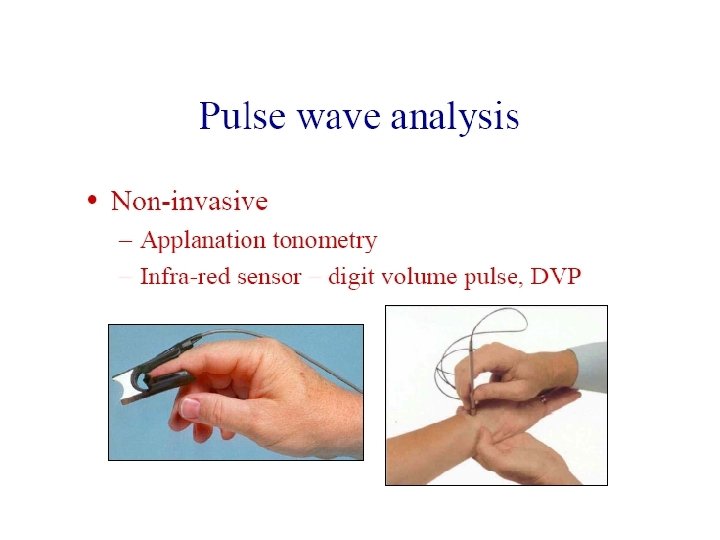
Variation of Einc with stretch Einc [Nm-2 x 105] 15 10 5 0 1. 2 1. 4 1. 6 1. 8 R/Ro 2. 0 2. 2 2. 4 2. 6
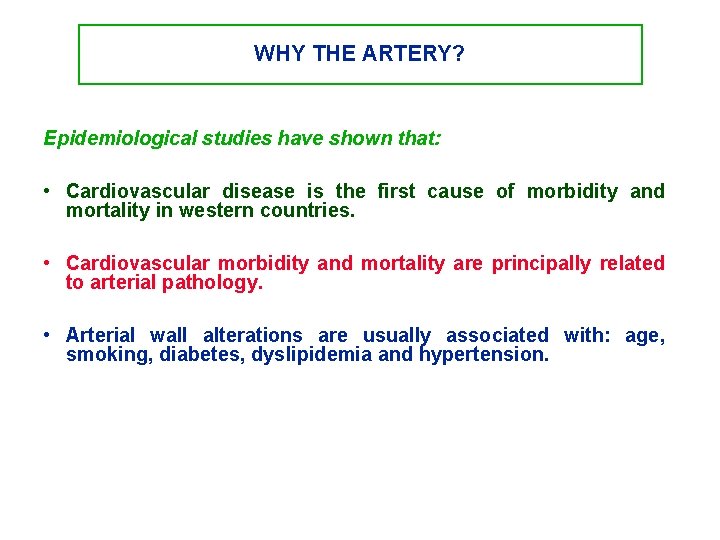
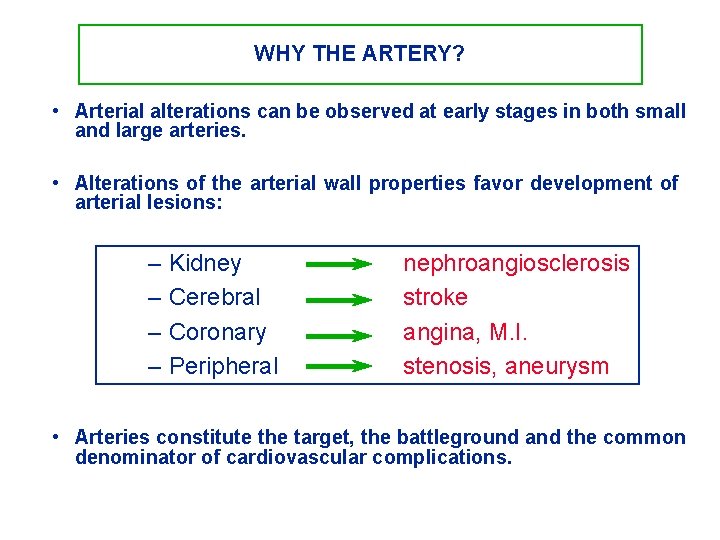
WHY THE ARTERY? Epidemiological studies have shown that: • Cardiovascular disease is the first cause of morbidity and mortality in western countries. • Cardiovascular morbidity and mortality are principally related to arterial pathology. • Arterial wall alterations are usually associated with: age, smoking, diabetes, dyslipidemia and hypertension.
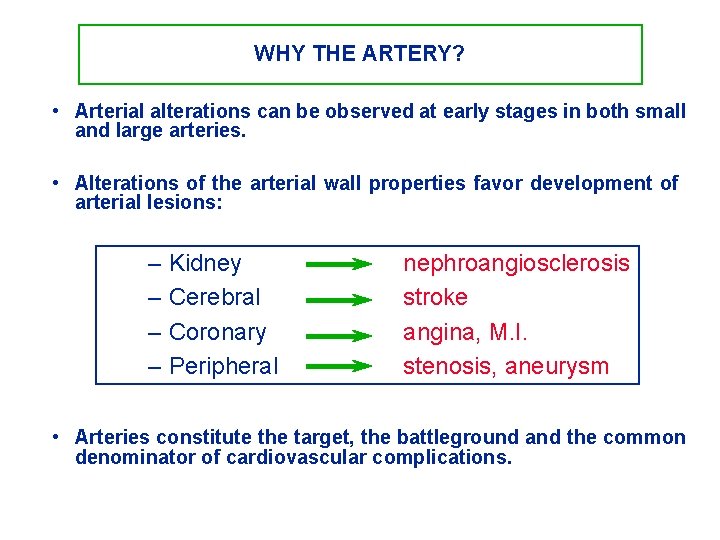
WHY THE ARTERY? • Arterial alterations can be observed at early stages in both small and large arteries. • Alterations of the arterial wall properties favor development of arterial lesions: – Kidney – Cerebral – Coronary – Peripheral nephroangiosclerosis stroke angina, M. I. stenosis, aneurysm • Arteries constitute the target, the battleground and the common denominator of cardiovascular complications.
WHY THE ARTERY? • Cardiovascular morbidity and mortality are principally due to arterial lesions. • Treatments differ by their effect on the arterial wall. • The evaluation of cardiovascular prevention and its impact on the arterial wall is important as an intermediate marker • Large therapeutic trials including arterial evaluation are required.
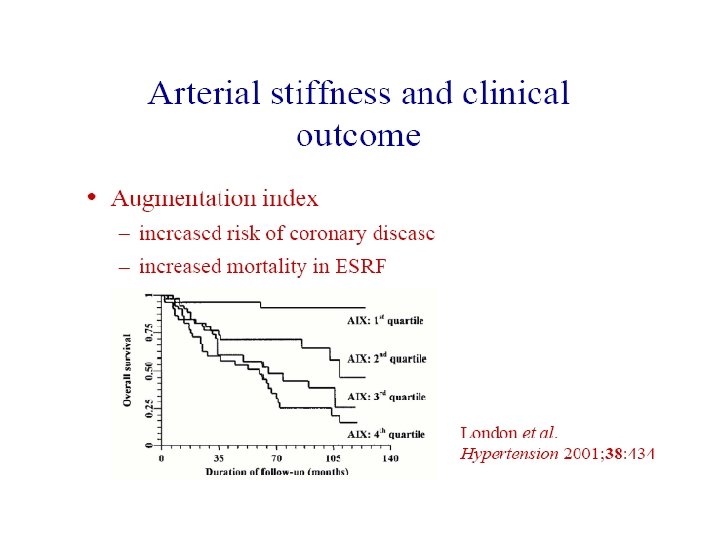
WHY PULSE WAVE VELOCITY? • Arterial pathology is a major contributor to cardiovascular disease, morbidity and mortality. • Most non-invasive methods to assess large arteries are ultrasound based: – Doppler velocity measurement – Echography – High resolution Echo-tracking Sophisticated, costly and reserved for a few clinical research labs.
WHY PULSE WAVE VELOCITY? • Clinical assessment of large arteries requires a simple, practical method. Pulse wave velocity = Index of arterial stiffness • Arterial stiffness will – – Play a potential etiologic role in cardiovascular disease. Help to recognize arterial changes. Constitute an "early risk marker". Be useful in assessing the arterial effects of drugs.
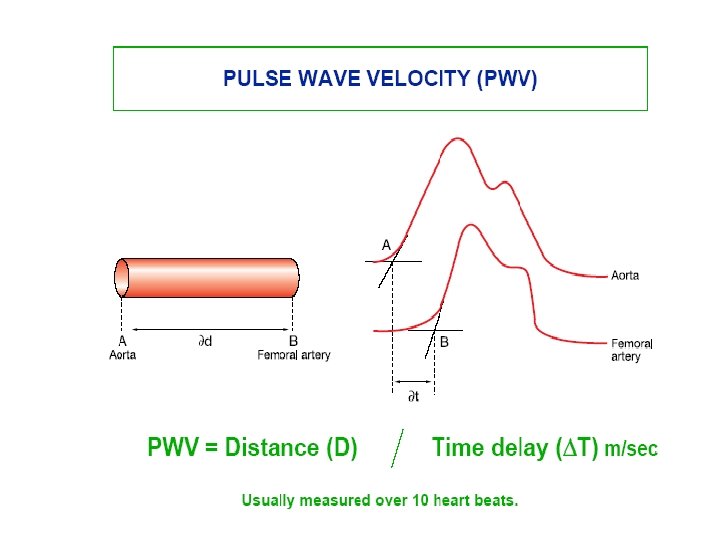
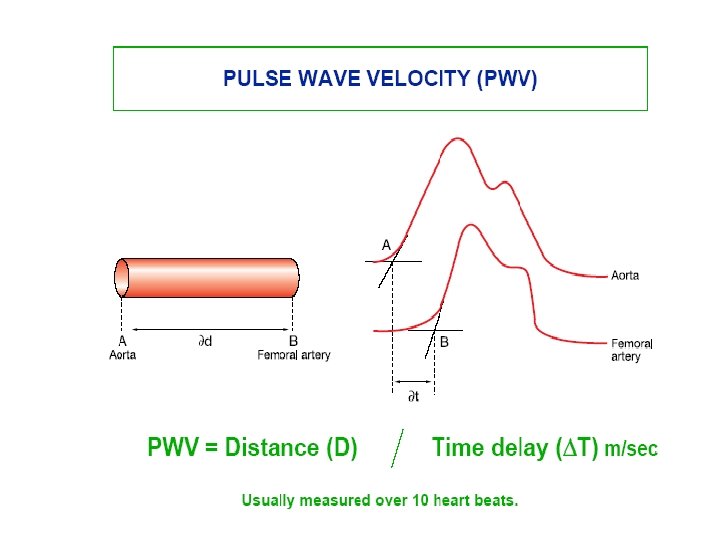
PULSE WAVE VELOCITY • A simple method to assess arterial stiffness and distensibility. • A long-established and widely used technique. • Non-invasive, accurate and reproducible.
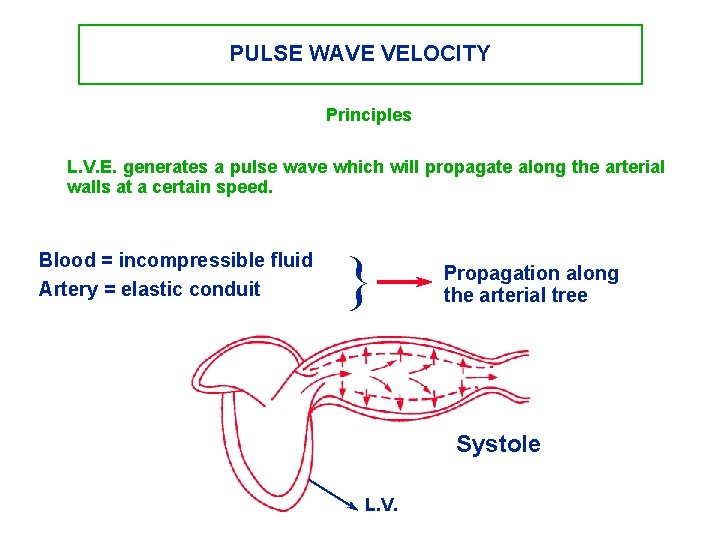
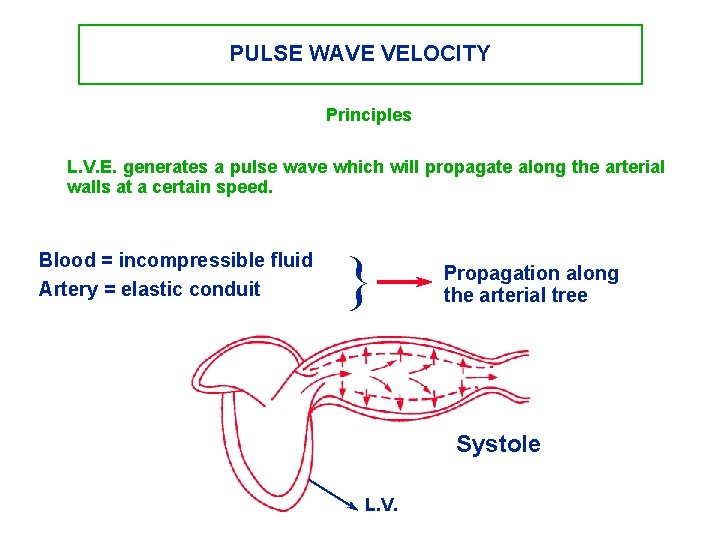
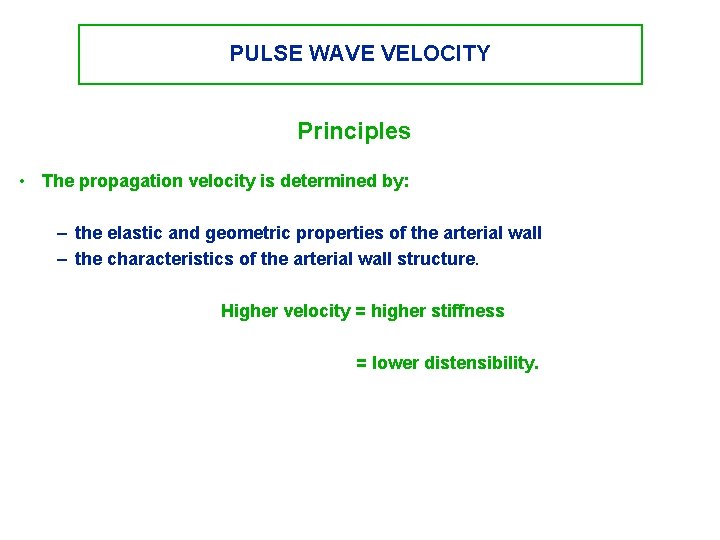
PULSE WAVE VELOCITY Principles L. V. E. generates a pulse wave which will propagate along the arterial walls at a certain speed. Blood = incompressible fluid Artery = elastic conduit } Propagation along the arterial tree Systole L. V.
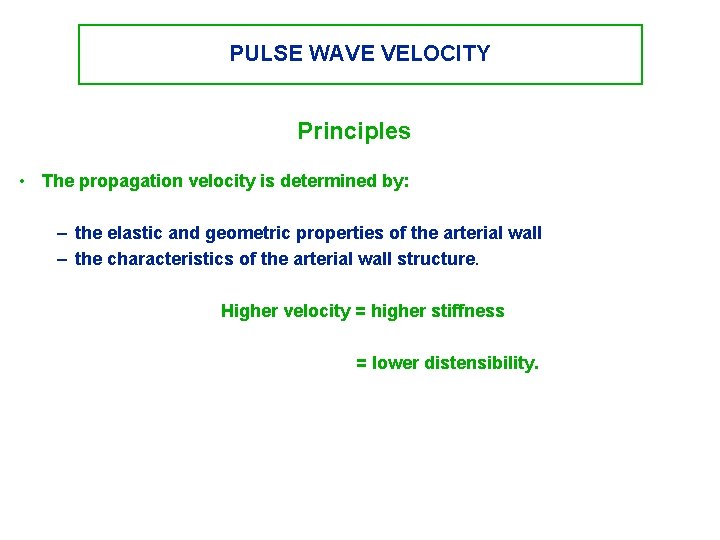
PULSE WAVE VELOCITY Principles • The propagation velocity is determined by: – the elastic and geometric properties of the arterial wall – the characteristics of the arterial wall structure. Higher velocity = higher stiffness = lower distensibility.
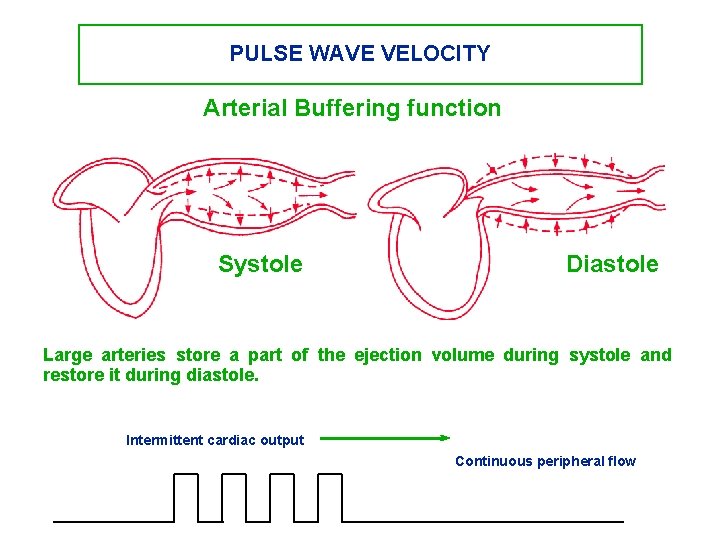
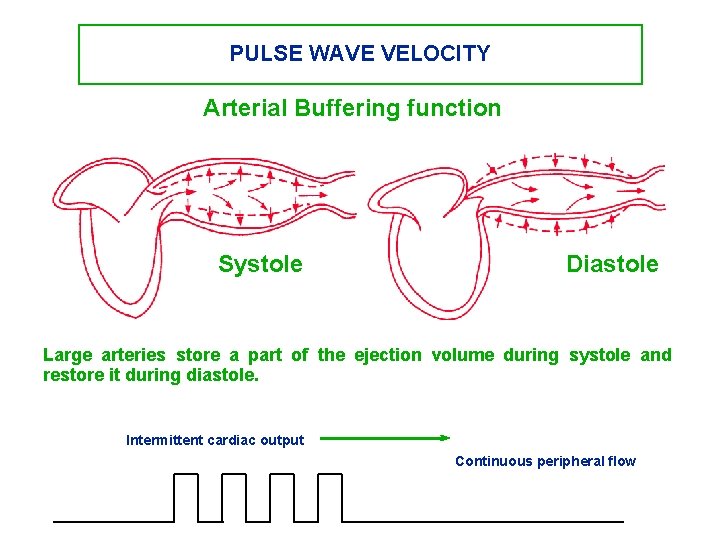
PULSE WAVE VELOCITY Arterial Buffering function Systole Diastole Large arteries store a part of the ejection volume during systole and restore it during diastole. Intermittent cardiac output Continuous peripheral flow
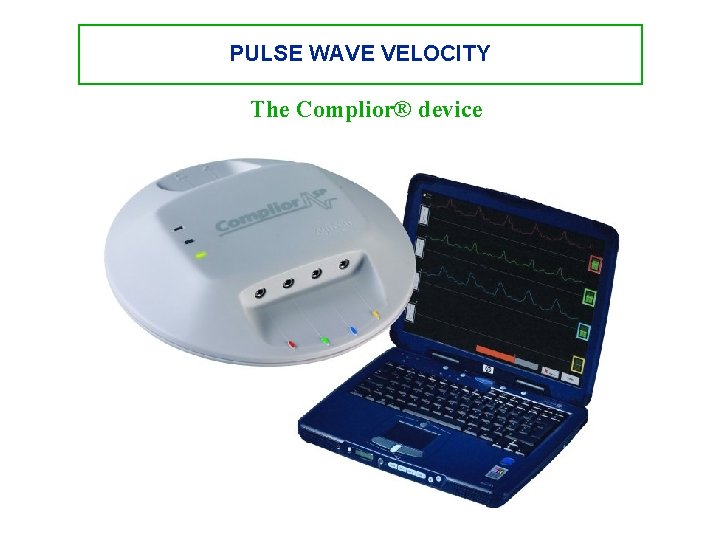
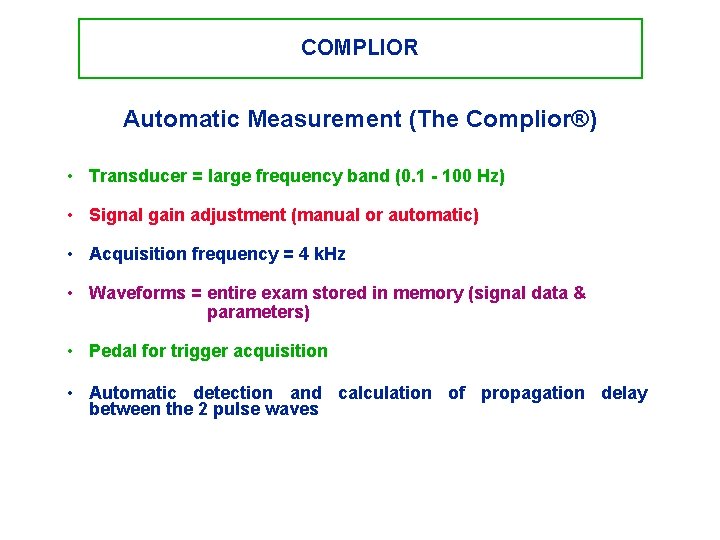
PULSE WAVE VELOCITY The Complior® device
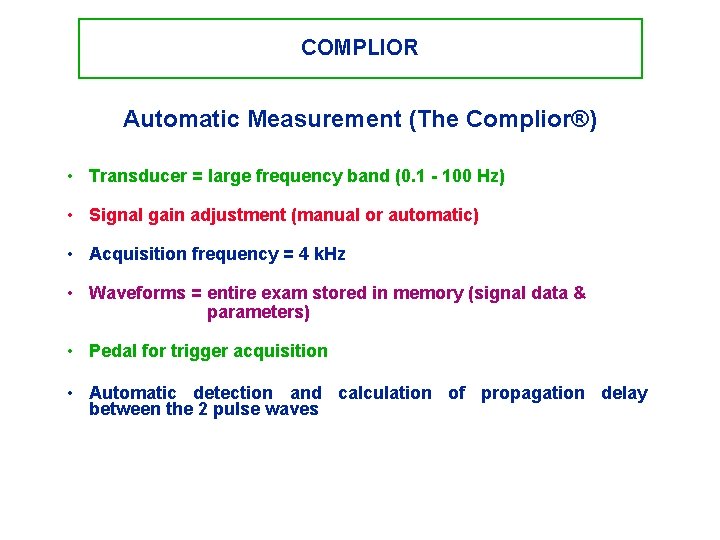
COMPLIOR Automatic Measurement (The Complior®) • Transducer = large frequency band (0. 1 - 100 Hz) • Signal gain adjustment (manual or automatic) • Acquisition frequency = 4 k. Hz • Waveforms = entire exam stored in memory (signal data & parameters) • Pedal for trigger acquisition • Automatic detection and calculation of propagation delay between the 2 pulse waves
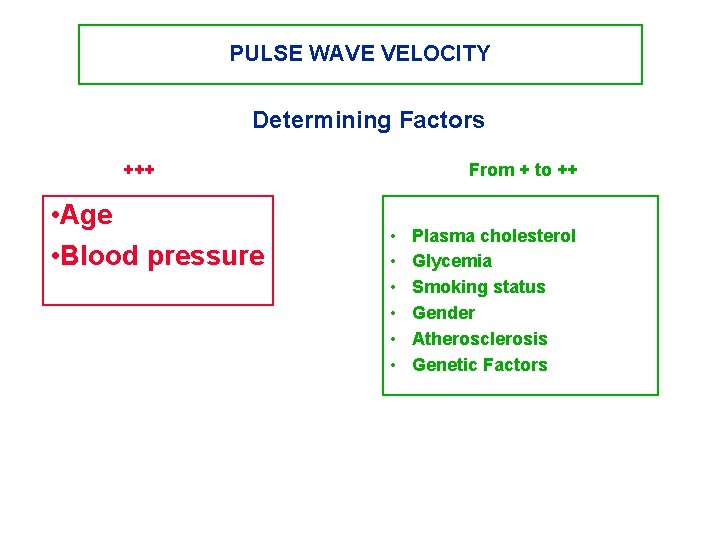
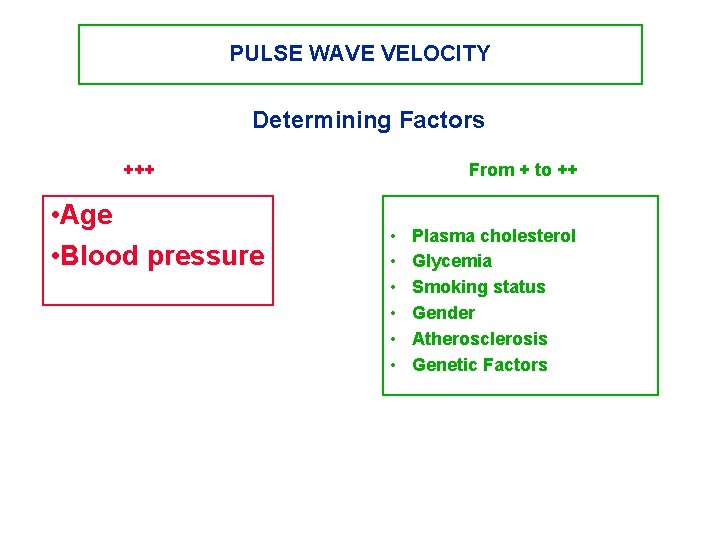
PULSE WAVE VELOCITY Determining Factors +++ • Age • Blood pressure From + to ++ • • • Plasma cholesterol Glycemia Smoking status Gender Atherosclerosis Genetic Factors
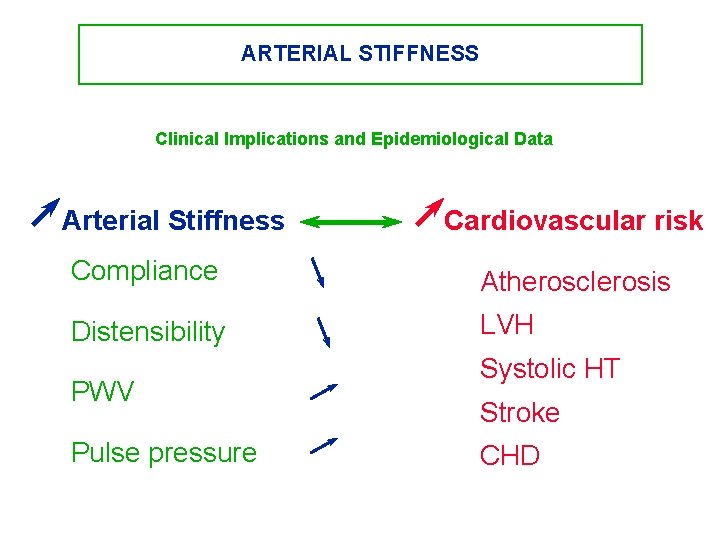
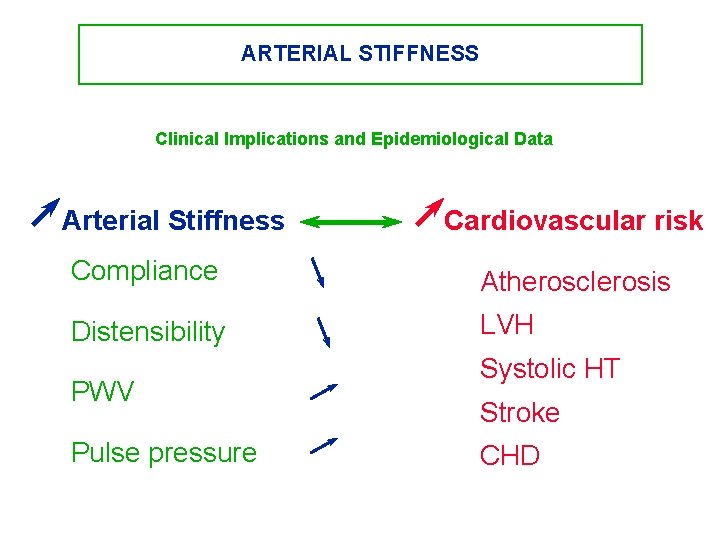
ARTERIAL STIFFNESS Clinical Implications and Epidemiological Data Arterial Stiffness Cardiovascular risk Compliance Atherosclerosis Distensibility LVH PWV Pulse pressure Systolic HT Stroke CHD
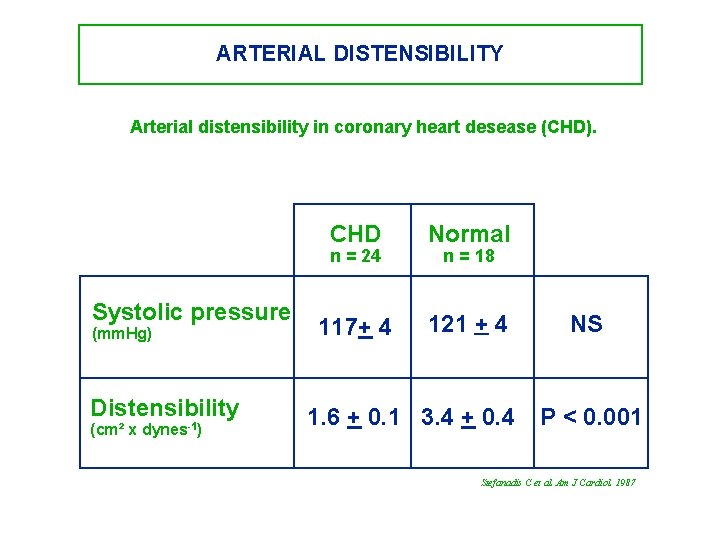
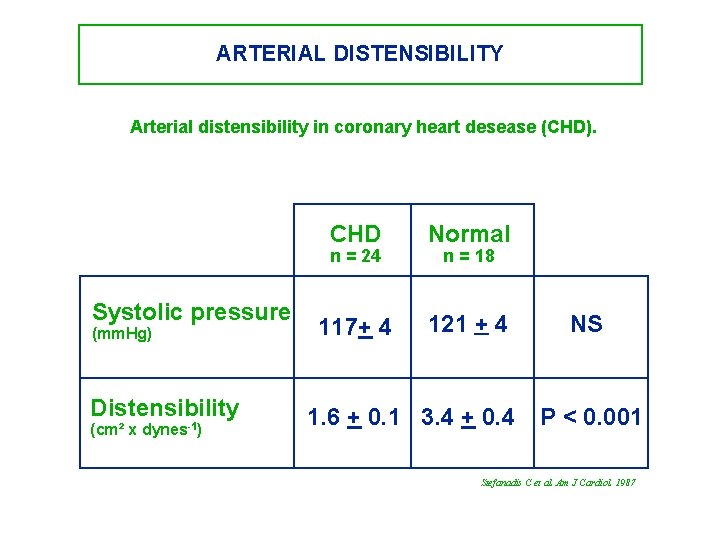
ARTERIAL DISTENSIBILITY Arterial distensibility in coronary heart desease (CHD). CHD Normal 117+ 4 121 + 4 n = 24 Systolic pressure (mm. Hg) Distensibility (cm² x dynes-1) n = 18 1. 6 + 0. 1 3. 4 + 0. 4 NS P < 0. 001 Stefanadis C et al. Am J Cardiol. 1987
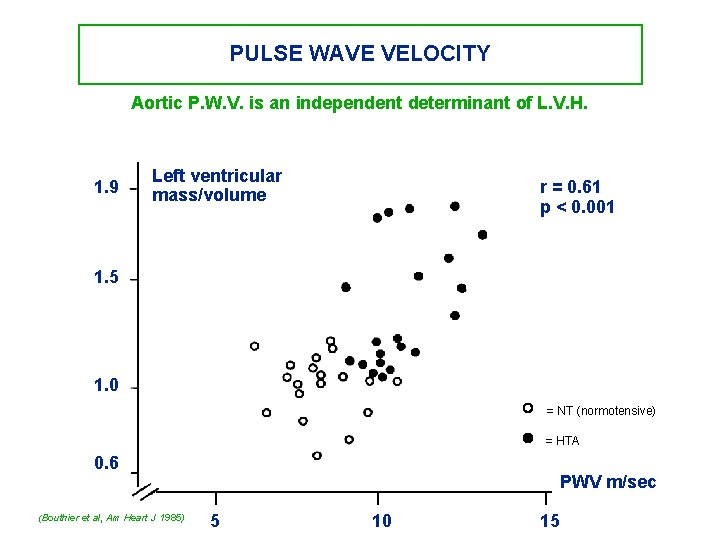
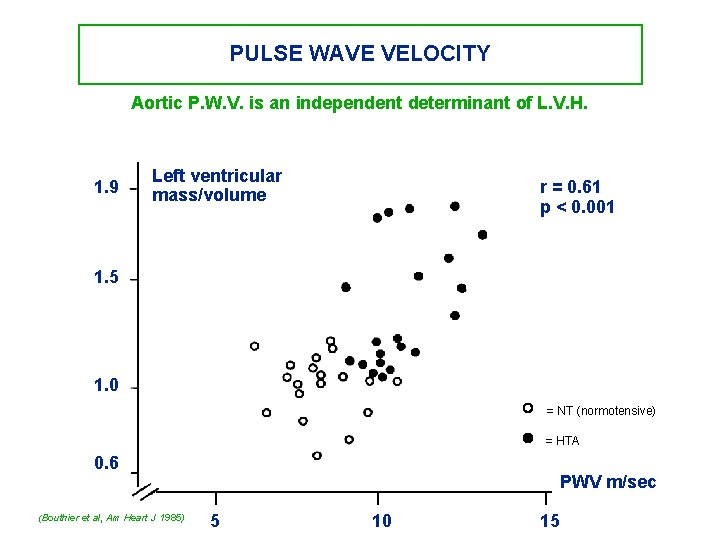
PULSE WAVE VELOCITY Aortic P. W. V. is an independent determinant of L. V. H. 1. 9 Left ventricular mass/volume r = 0. 61 p < 0. 001 1. 5 1. 0 = NT (normotensive) = HTA 0. 6 (Bouthier et al, Am Heart J 1985) PWV m/sec 5 10 15
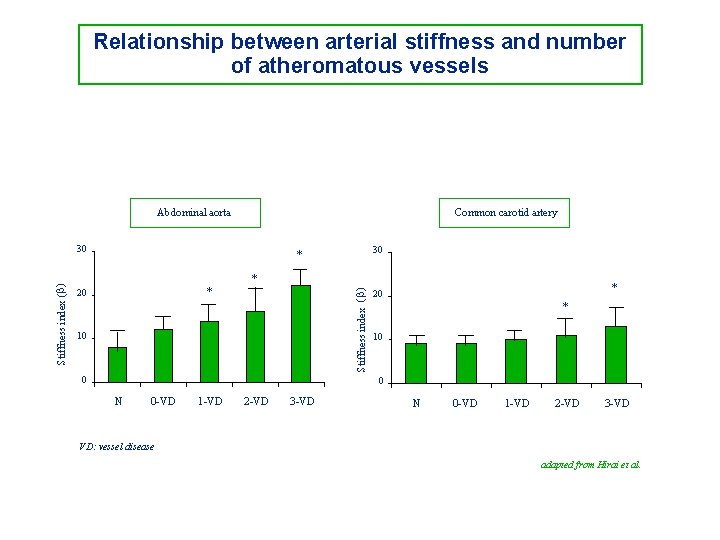
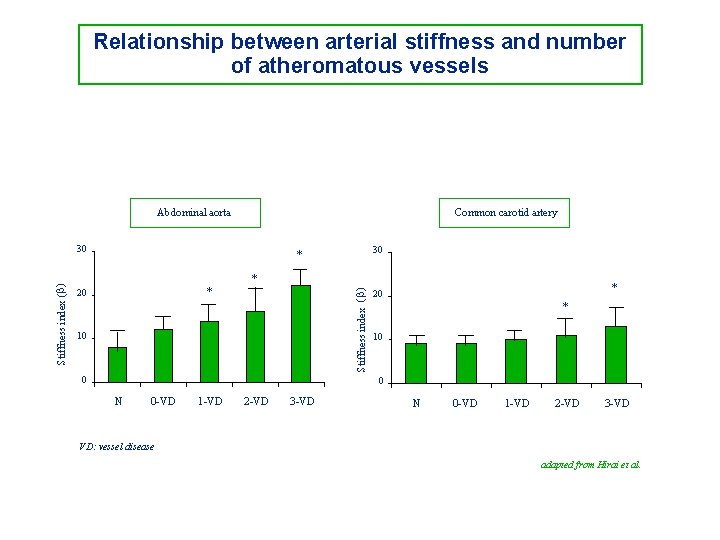
Relationship between arterial stiffness and number of atheromatous vessels Common carotid artery Abdominal aorta 30 * * 20 * Stiffness index (b) 30 10 0 * 20 * 10 0 N 0 -VD 1 -VD 2 -VD 3 -VD VD: vessel disease adapted from Hirai et al.
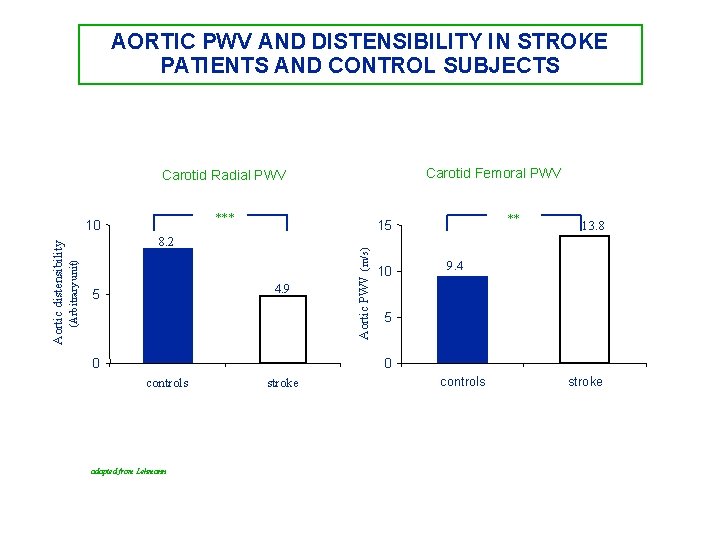
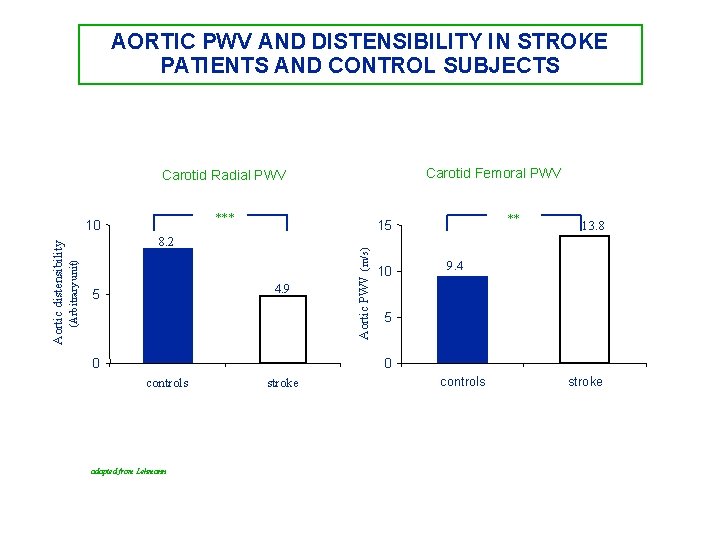
AORTIC PWV AND DISTENSIBILITY IN STROKE PATIENTS AND CONTROL SUBJECTS Carotid Femoral PWV Carotid Radial PWV *** 0 Aortic PWV (m/s) 4. 9 5 ** 15 8. 2 (Arbitrary unit) Aortic distensibility 10 10 13. 8 9. 4 5 0 controls adapted from Lehmann stroke controls stroke
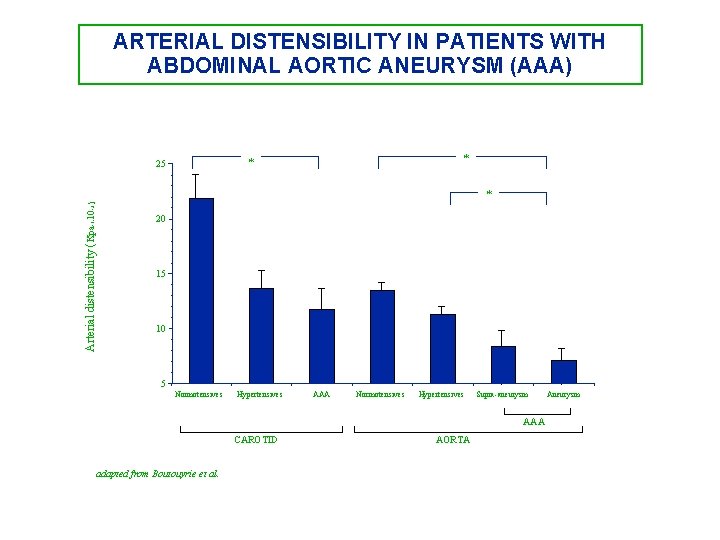
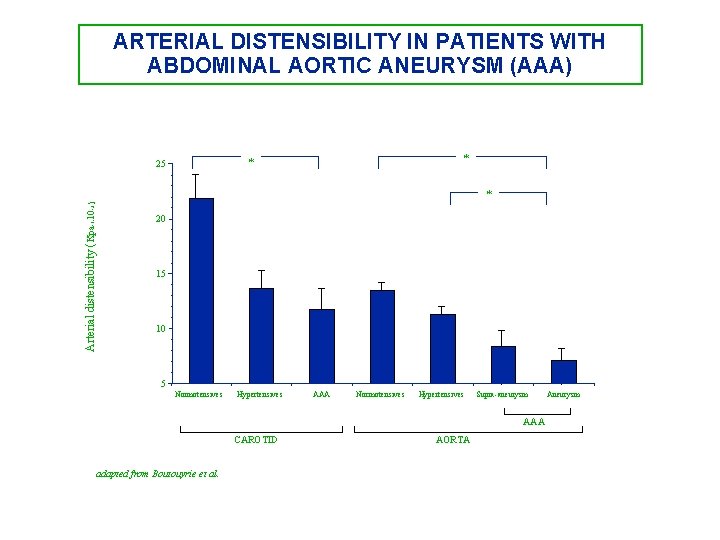
ARTERIAL DISTENSIBILITY IN PATIENTS WITH ABDOMINAL AORTIC ANEURYSM (AAA) * * 25 Arterial distensibility ( Kpa-1. 10 -3 ) * 20 15 10 5 Normotensives Hypertensives AAA Normotensives Hypertensives Supra-aneurysm AAA CAROTID adapted from Boutouyrie et al. AORTA Aneurysm
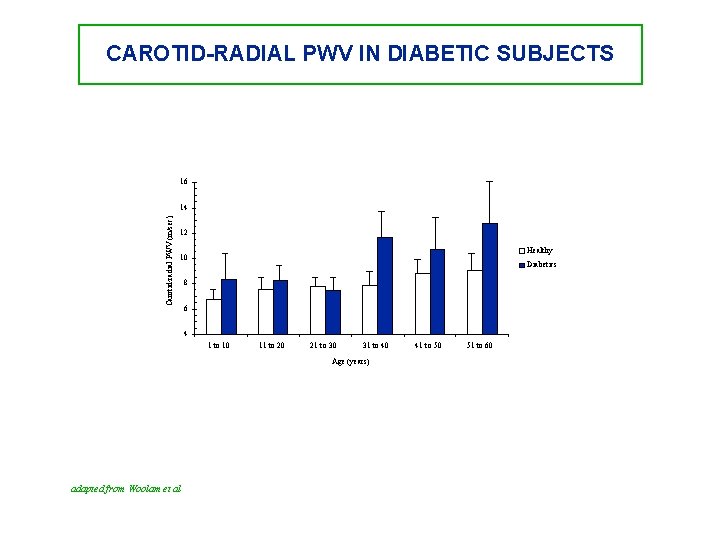
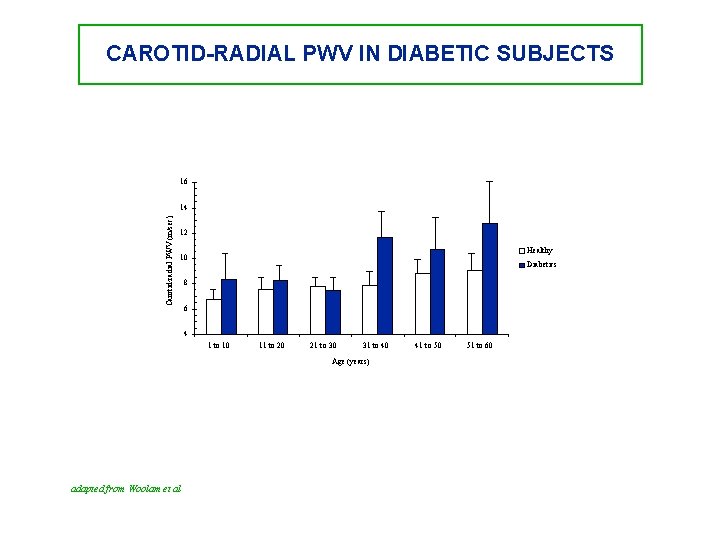
CAROTID-RADIAL PWV IN DIABETIC SUBJECTS 16 Carotid-radial PWV (m/sec) 14 12 Healthy 10 Diabetics 8 6 4 1 to 10 11 to 20 21 to 30 31 to 40 Age (years) adapted from Woolam et al 41 to 50 51 to 60
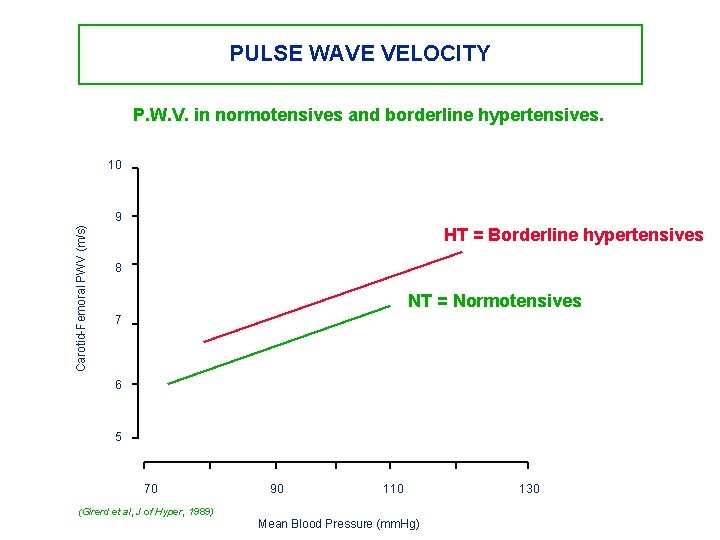
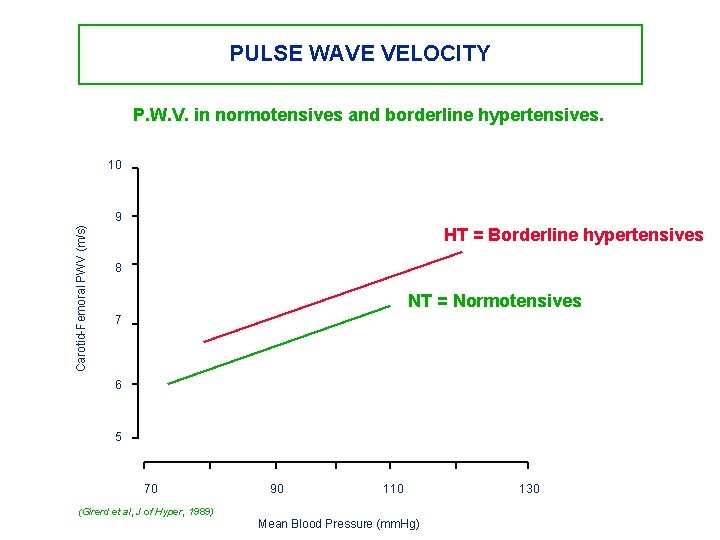
PULSE WAVE VELOCITY P. W. V. in normotensives and borderline hypertensives. 10 Carotid-Femoral PWV (m/s) 9 HT = Borderline hypertensives 8 NT = Normotensives 7 6 5 70 90 110 (Girerd et al, J of Hyper, 1989) Mean Blood Pressure (mm. Hg) 130
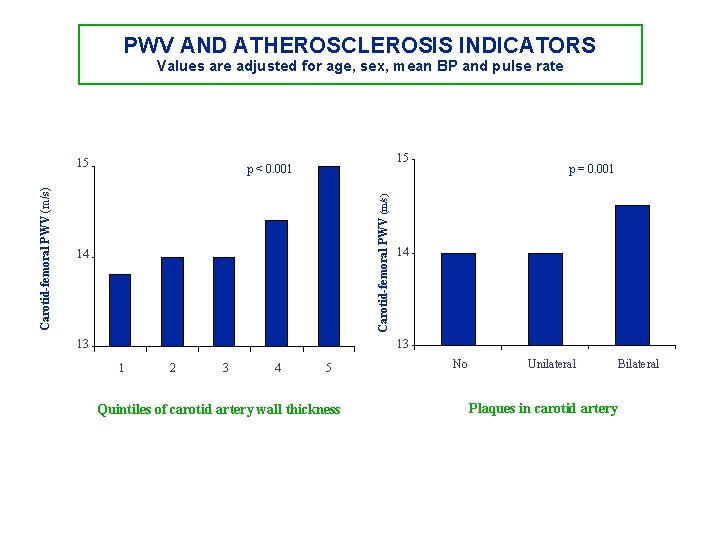
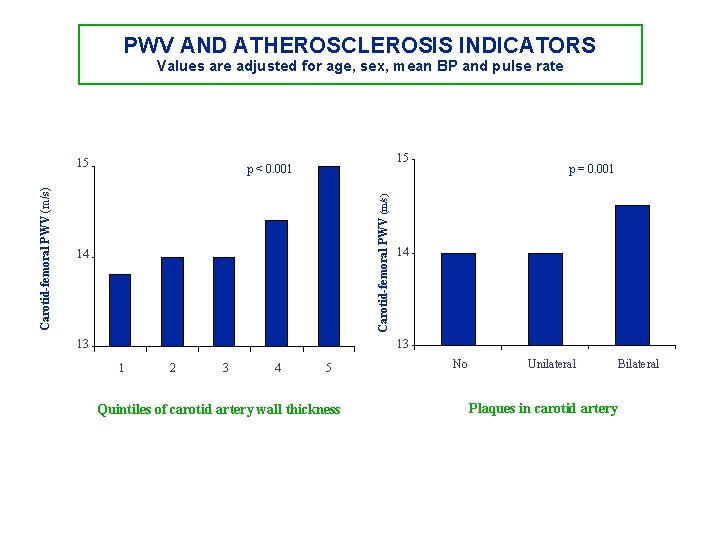
PWV AND ATHEROSCLEROSIS INDICATORS Values are adjusted for age, sex, mean BP and pulse rate 15 p < 0. 001 Carotid-femoral PWV (m/s) 15 14 13 p = 0. 001 14 13 1 2 3 4 5 Quintiles of carotid artery wall thickness No Unilateral Plaques in carotid artery Bilateral
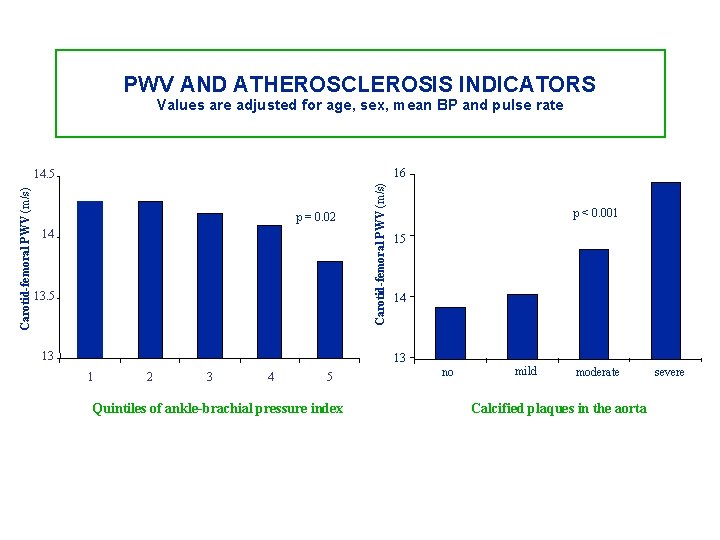
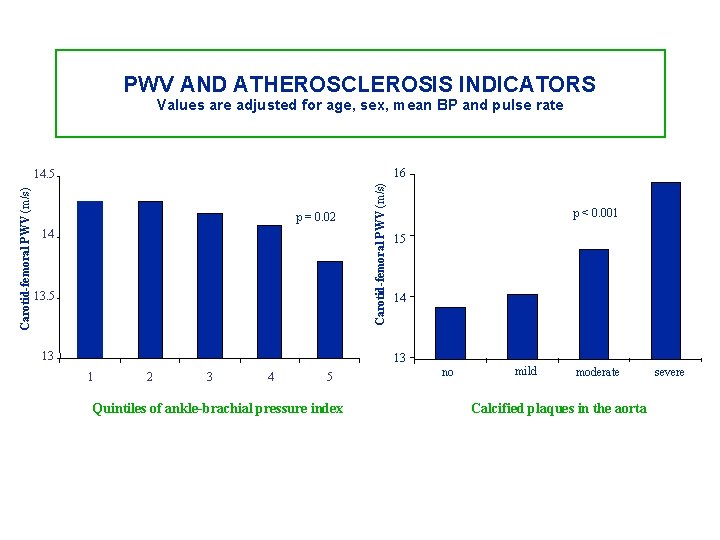
PWV AND ATHEROSCLEROSIS INDICATORS Values are adjusted for age, sex, mean BP and pulse rate 16 p = 0. 02 14 13. 5 13 Carotid-femoral PWV (m/s) 14. 5 p < 0. 001 15 14 13 1 2 3 4 5 Quintiles of ankle-brachial pressure index no mild moderate Calcified plaques in the aorta severe
CONCLUSION • Arterial stiffness must be taken consideration in clinical practice. into • The Complior system is an accurate device to assess the arterial stiffness using pulse wave velocity measurements. • The examination procedure is simple, and the method is accurate and reproducible.
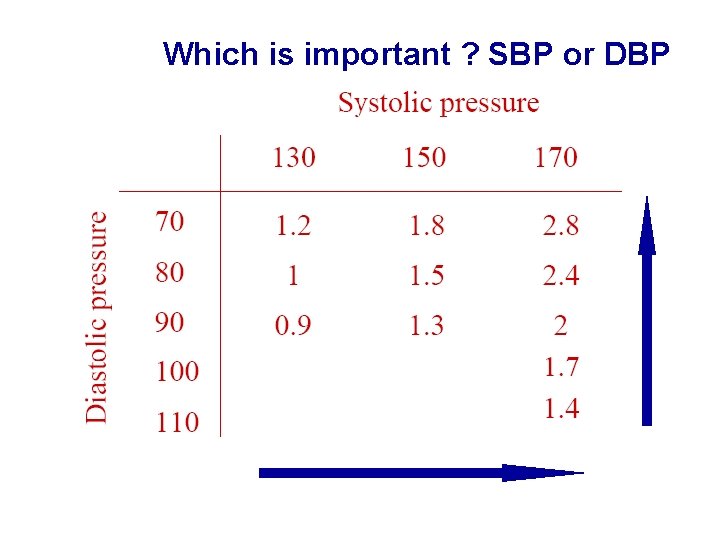
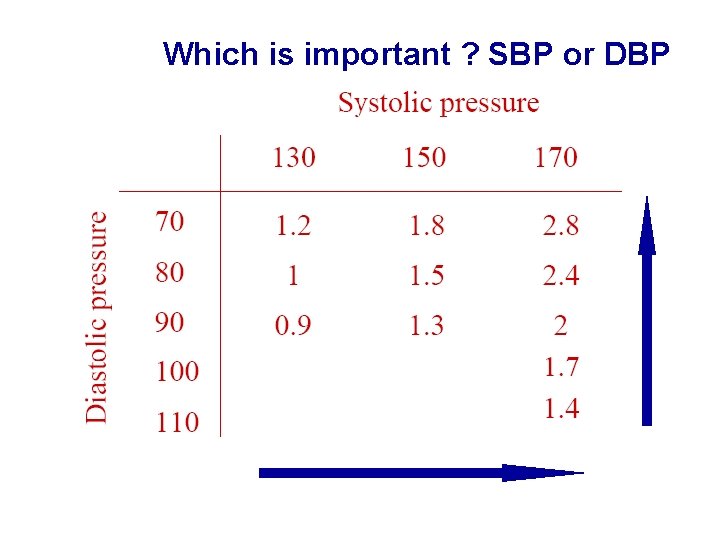
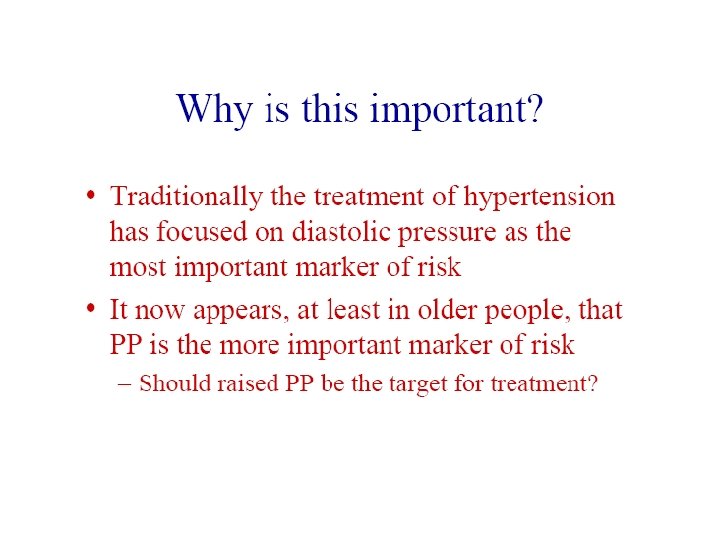
Which is important ? SBP or DBP
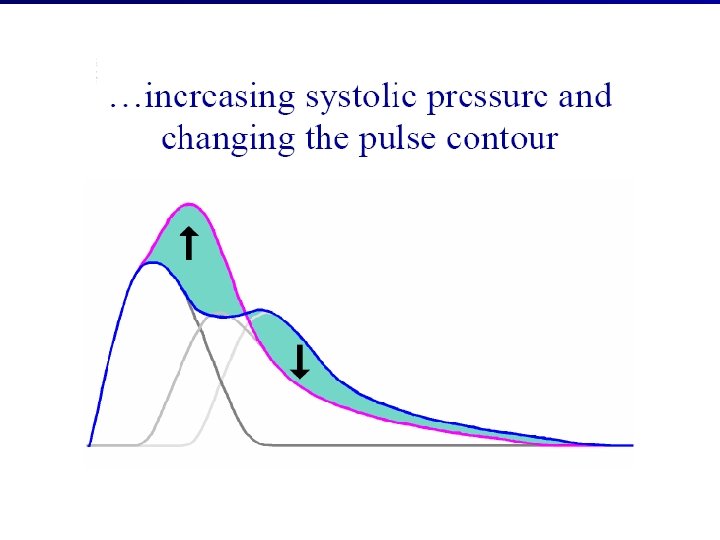
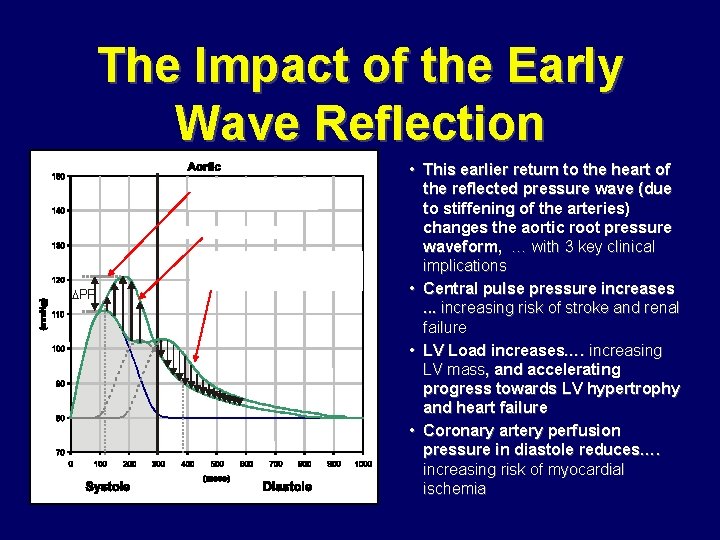
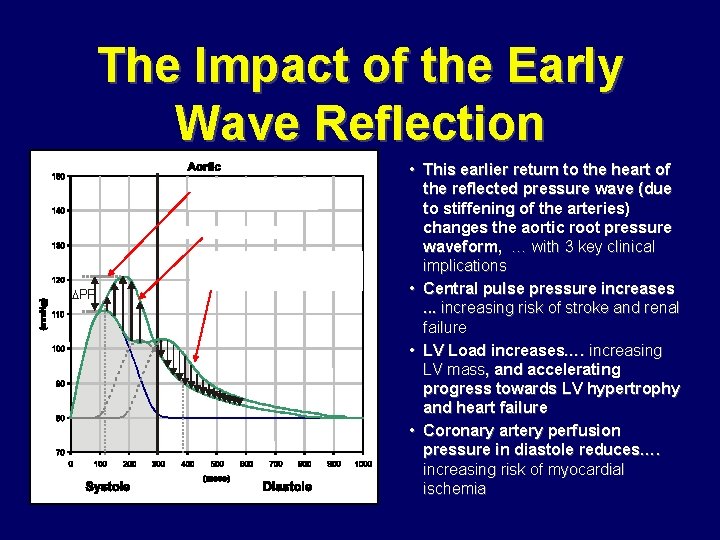
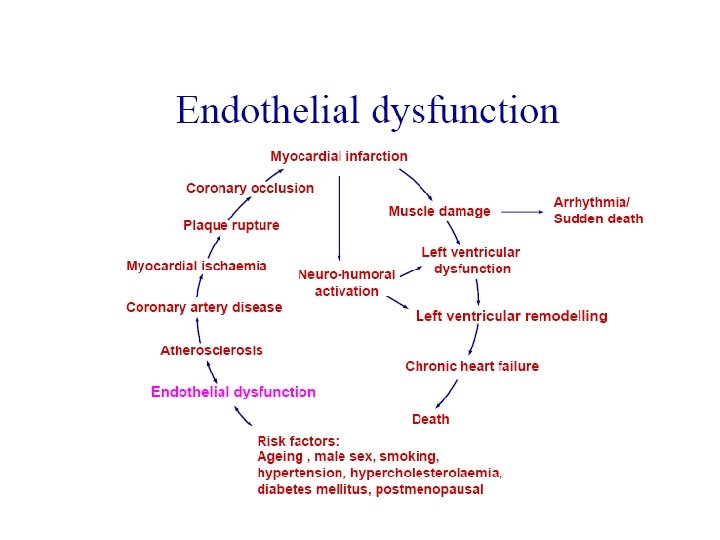
The Impact of the Early Wave Reflection Increased Central Pulse Pressure Increased LV Load PP Decreased Coronary Artery Perfusion Pressure in Diastole • This earlier return to the heart of the reflected pressure wave (due to stiffening of the arteries) changes the aortic root pressure waveform, … with 3 key clinical implications • Central pulse pressure increases. . . increasing risk of stroke and renal failure • LV Load increases…. increasing LV mass, and accelerating progress towards LV hypertrophy and heart failure • Coronary artery perfusion pressure in diastole reduces…. increasing risk of myocardial ischemia

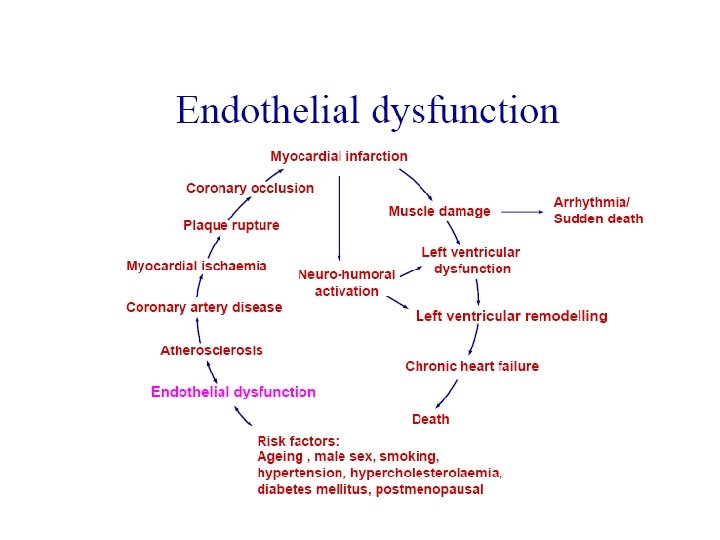
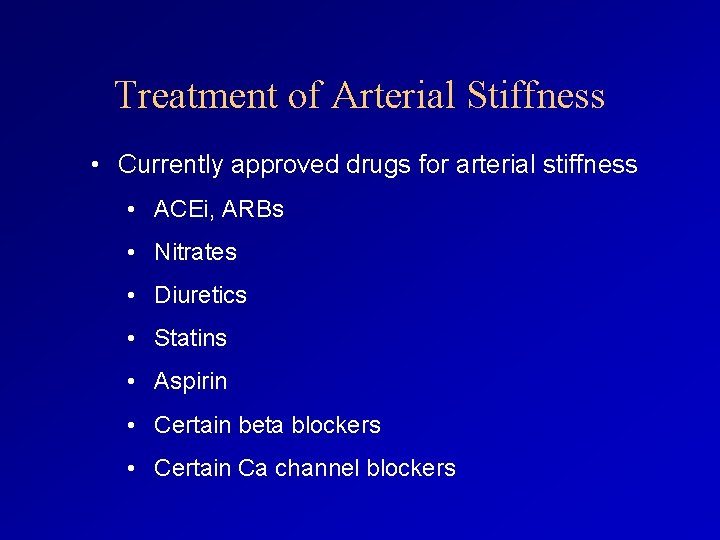
Treatment of Arterial Stiffness • Currently approved drugs for arterial stiffness • ACEi, ARBs • Nitrates • Diuretics • Statins • Aspirin • Certain beta blockers • Certain Ca channel blockers
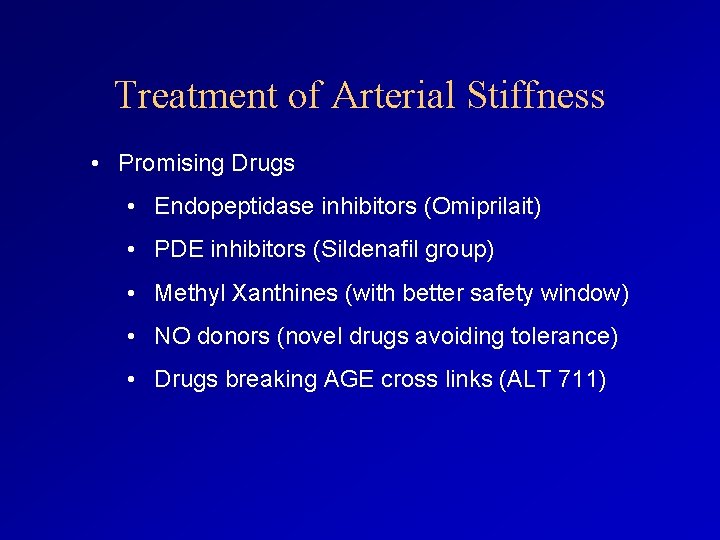
Treatment of Arterial Stiffness • Promising Drugs • Endopeptidase inhibitors (Omiprilait) • PDE inhibitors (Sildenafil group) • Methyl Xanthines (with better safety window) • NO donors (novel drugs avoiding tolerance) • Drugs breaking AGE cross links (ALT 711)
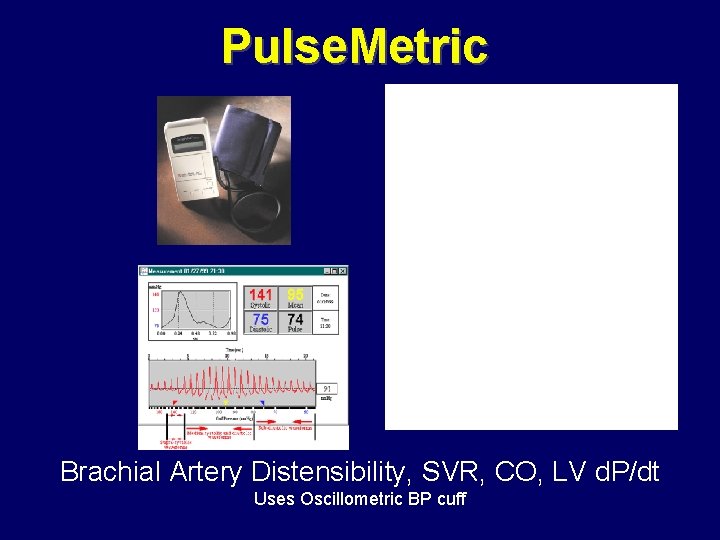
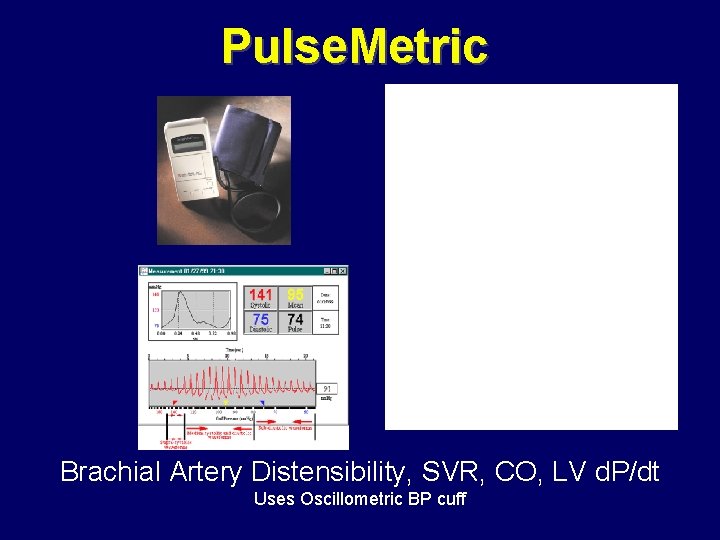
Pulse. Metric Brachial Artery Distensibility, SVR, CO, LV d. P/dt Uses Oscillometric BP cuff
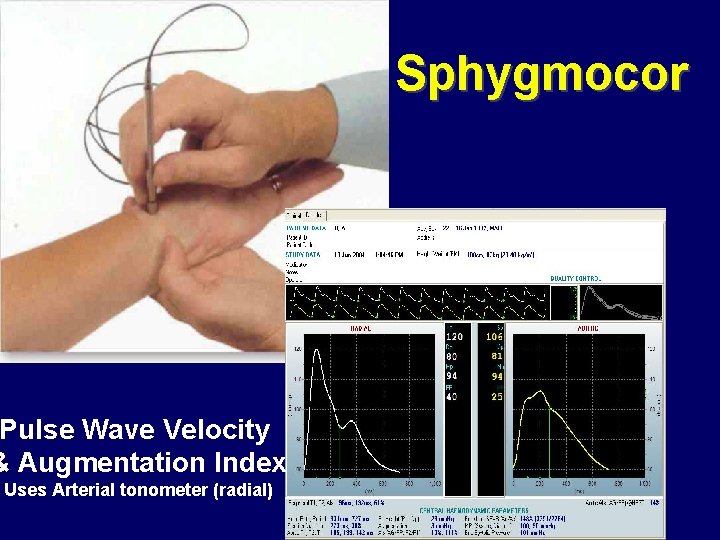
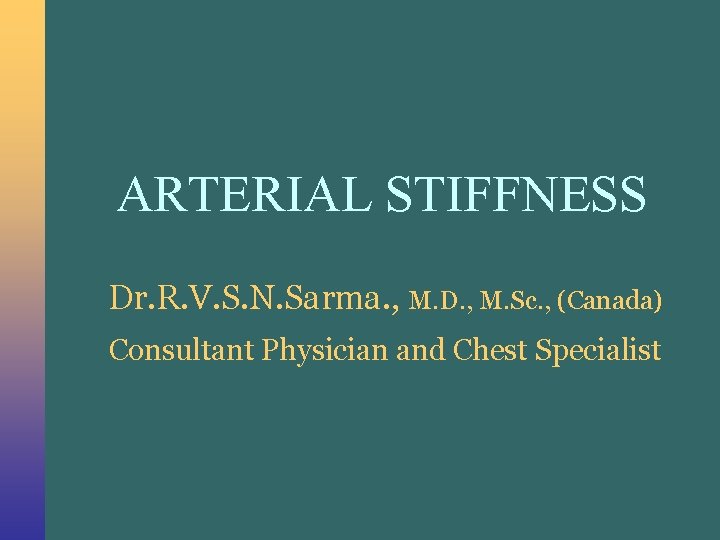
Sphygmocor Pulse Wave Velocity & Augmentation Index Uses Arterial tonometer (radial)