ALLERGY AND IMMUNOLOGY FOR THE PEDIATRICS EXAM Luis






- Slides: 106
ALLERGY AND IMMUNOLOGY FOR THE PEDIATRICS EXAM Luis E. Murguía-Favela, MD FRCPC Immunology and Allergy January 30 th, 2020
Keep in mind n n n Despite the traumatic experience: the exam is quite reasonable and Gen. Peds-level CPS statements, CPS statements Old questions are helpful, but don’t fixate on the controversial ones: q q q Misremembered Very old Wrong
Outline: Need to know n n Cellular immunity: Di. George syndrome Humoral immunity: q q q n Combined (cellular/humoral) q q n XLA CVID Selective Ig. A deficiency SCID Specific diseases: WAS, CMCC, Ataxia Telangiectasia Innate immunity q q Complement: late components deficiency CGD
Need to know n Allergy q Types of hypersensitivity reactions n q q Drug allergy: antibiotics Food allergy n q q Very basics of immunotherapy Angioedema n q New recommendations on introduction of foods Environmental / stinging insects n q Anaphylaxis Hereditary Asthma Management of atopic dermatitis: OSCE
GENERAL QUESTIONS
SAQ n How many invasive infections would you be concerned about with respect to considering an immunodeficiency?

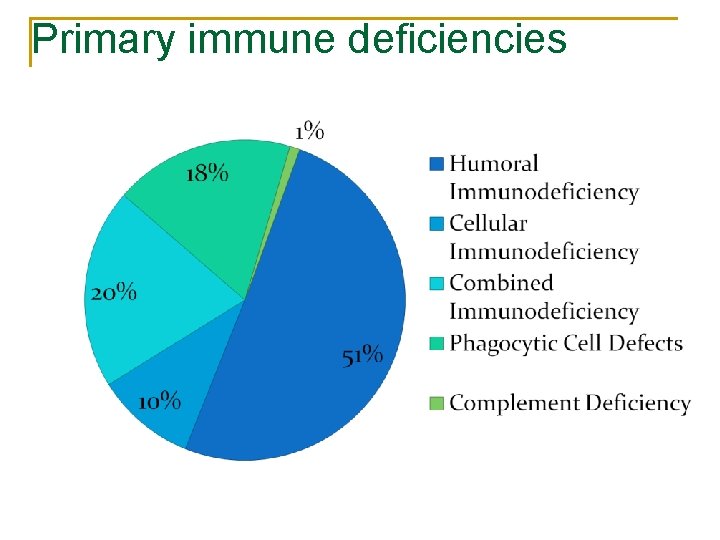
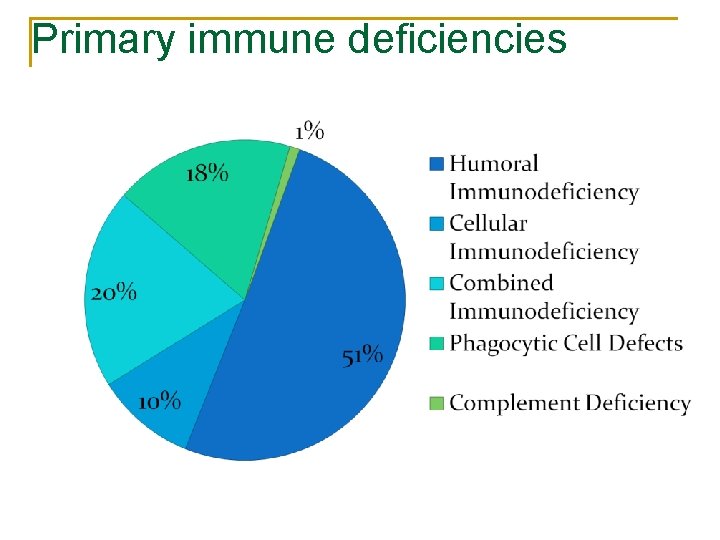
Primary immune deficiencies
SAQ n 1. 2. 3. 4. List 4 investigations for work-up of a patient with a suspected immunodeficiency. Immunoglobulins Specific antibodies T / B / NK cell markers: lymphocyte immunophenotyping T-cell function assays (proliferation)
CELLULAR IMMUNITY
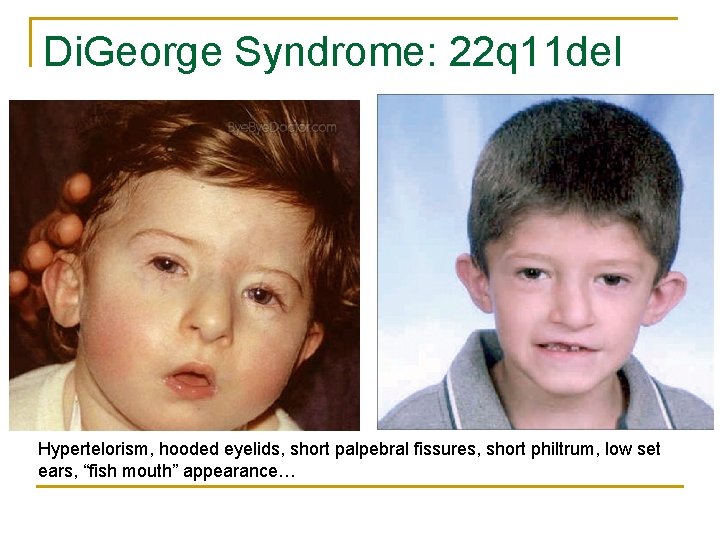
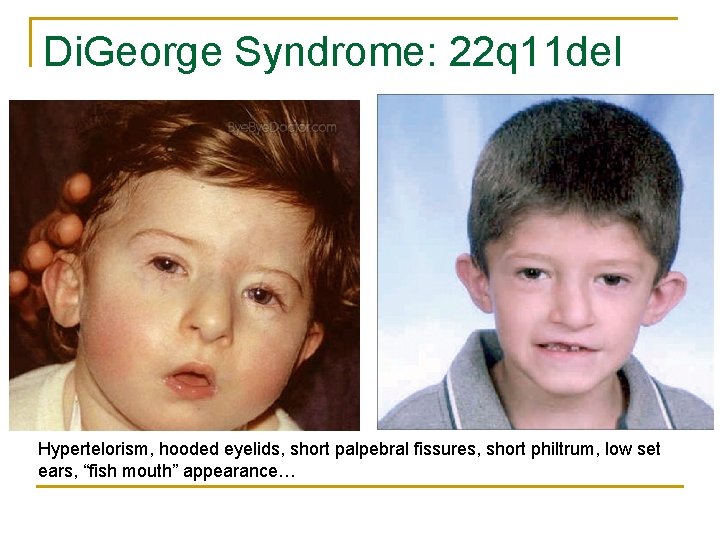
Di. George Syndrome: 22 q 11 del Hypertelorism, hooded eyelids, short palpebral fissures, short philtrum, low set ears, “fish mouth” appearance…
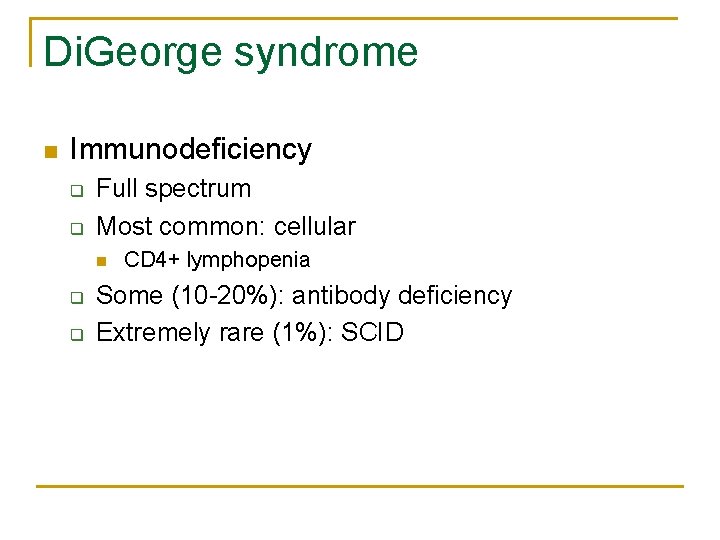
Di. George syndrome n Immunodeficiency q q Full spectrum Most common: cellular n q q CD 4+ lymphopenia Some (10 -20%): antibody deficiency Extremely rare (1%): SCID
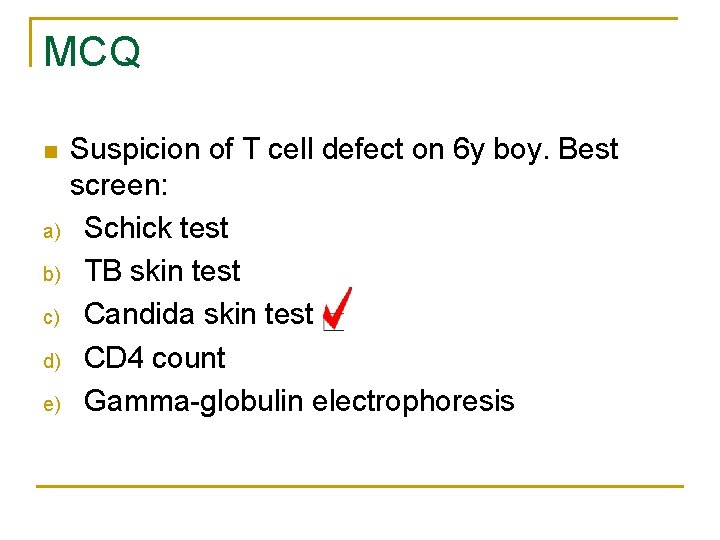
MCQ n a) b) c) d) e) Suspicion of T cell defect on 6 y boy. Best screen: Schick test TB skin test Candida skin test CD 4 count Gamma-globulin electrophoresis
HUMORAL IMMUNITY
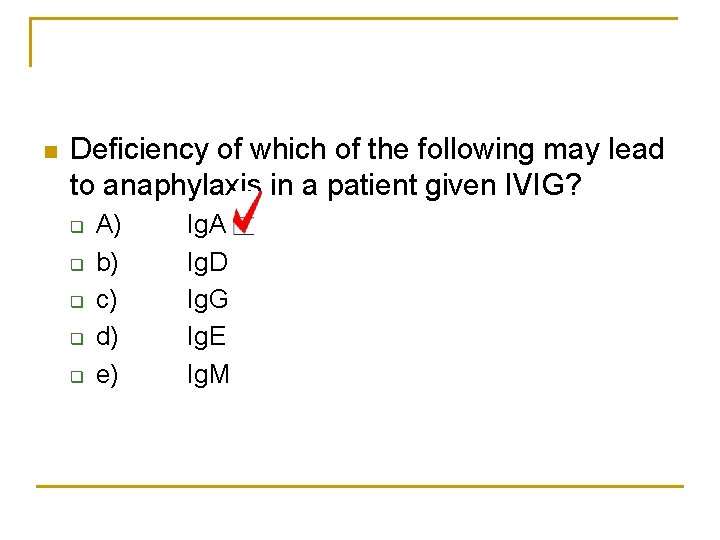
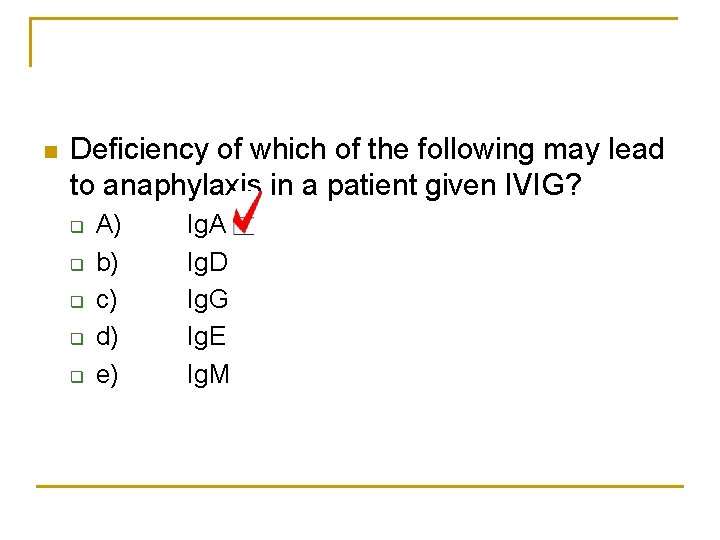
n Deficiency of which of the following may lead to anaphylaxis in a patient given IVIG? q q q A) b) c) d) e) Ig. A Ig. D Ig. G Ig. E Ig. M
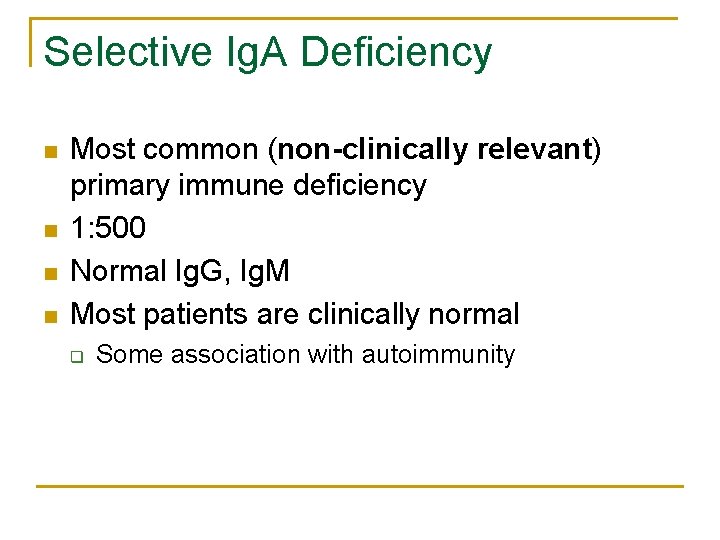
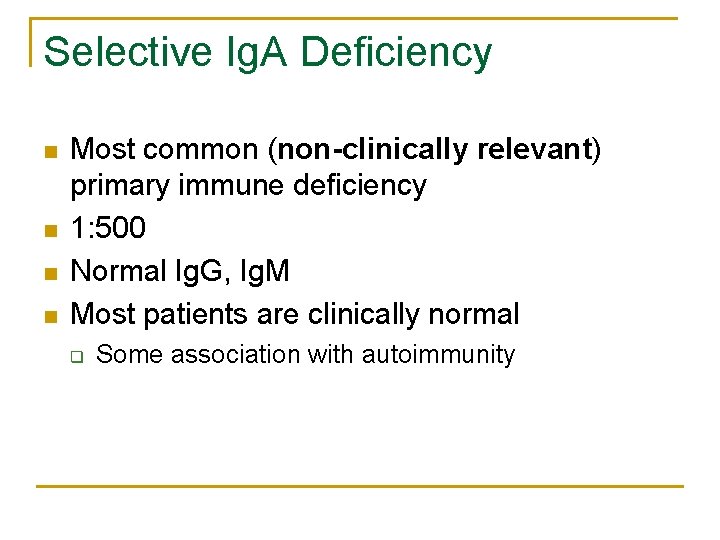
Selective Ig. A Deficiency n n Most common (non-clinically relevant) primary immune deficiency 1: 500 Normal Ig. G, Ig. M Most patients are clinically normal q Some association with autoimmunity
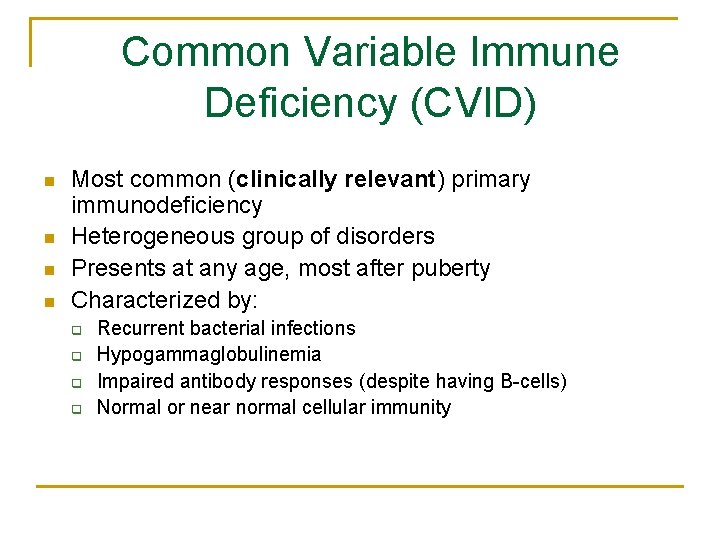
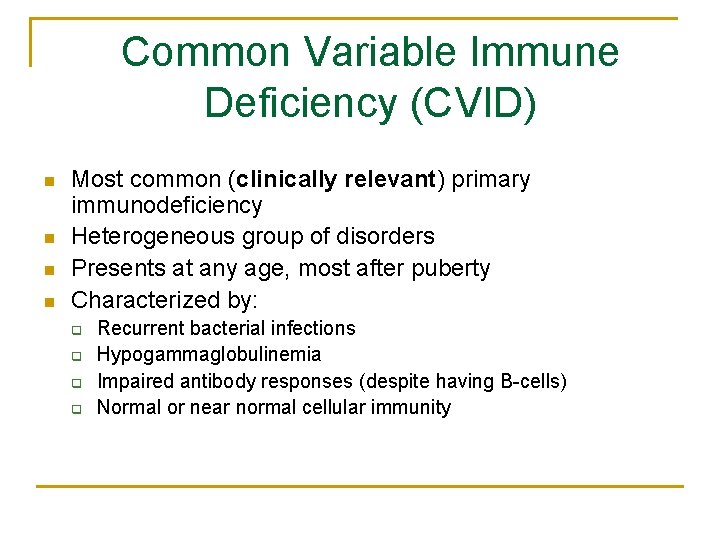
Common Variable Immune Deficiency (CVID) n n Most common (clinically relevant) primary immunodeficiency Heterogeneous group of disorders Presents at any age, most after puberty Characterized by: q q Recurrent bacterial infections Hypogammaglobulinemia Impaired antibody responses (despite having B-cells) Normal or near normal cellular immunity
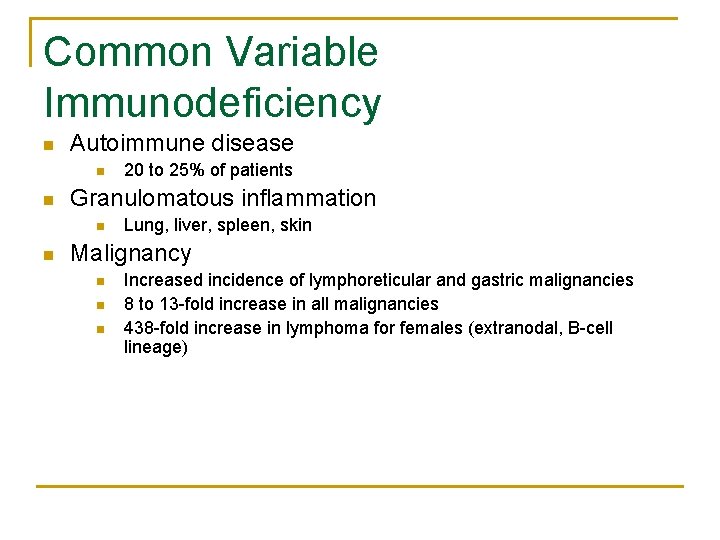
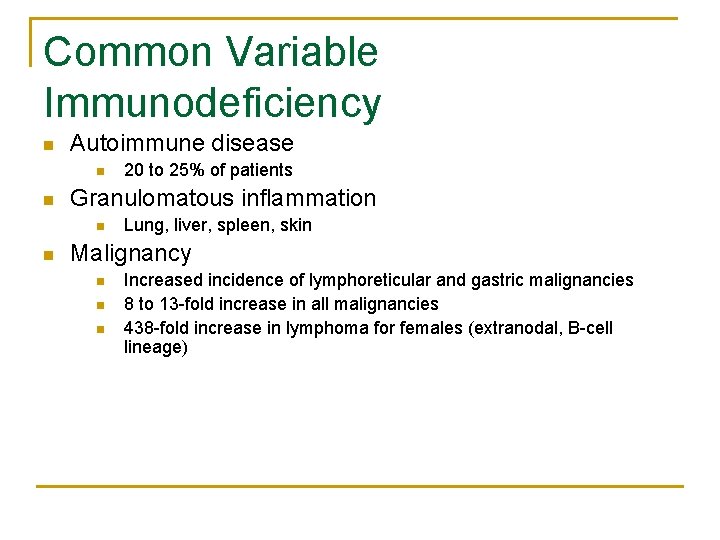
Common Variable Immunodeficiency n Autoimmune disease n n Granulomatous inflammation n n 20 to 25% of patients Lung, liver, spleen, skin Malignancy n n n Increased incidence of lymphoreticular and gastric malignancies 8 to 13 -fold increase in all malignancies 438 -fold increase in lymphoma for females (extranodal, B-cell lineage)
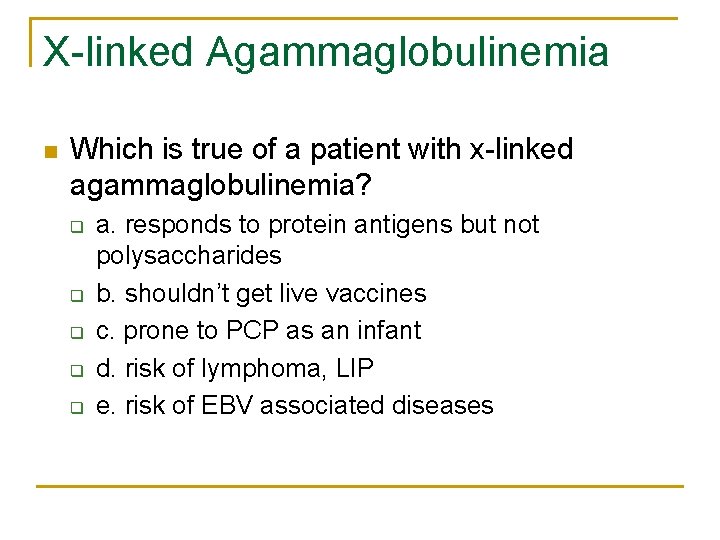
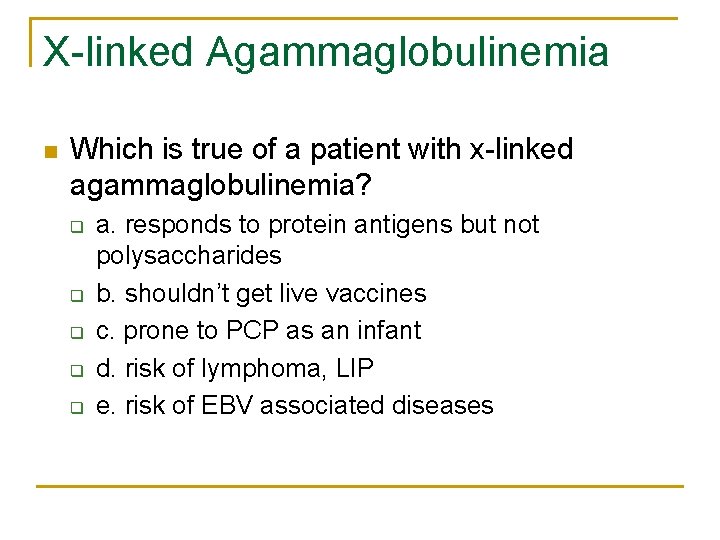
X-linked Agammaglobulinemia n Which is true of a patient with x-linked agammaglobulinemia? q q q a. responds to protein antigens but not polysaccharides b. shouldn’t get live vaccines c. prone to PCP as an infant d. risk of lymphoma, LIP e. risk of EBV associated diseases
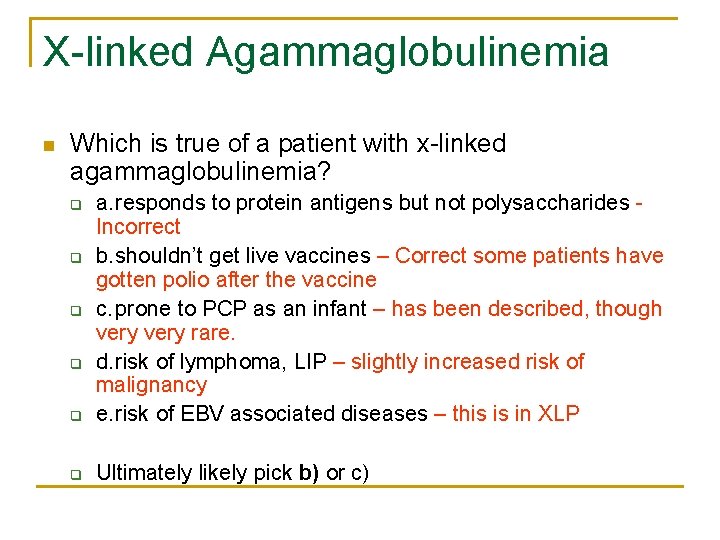
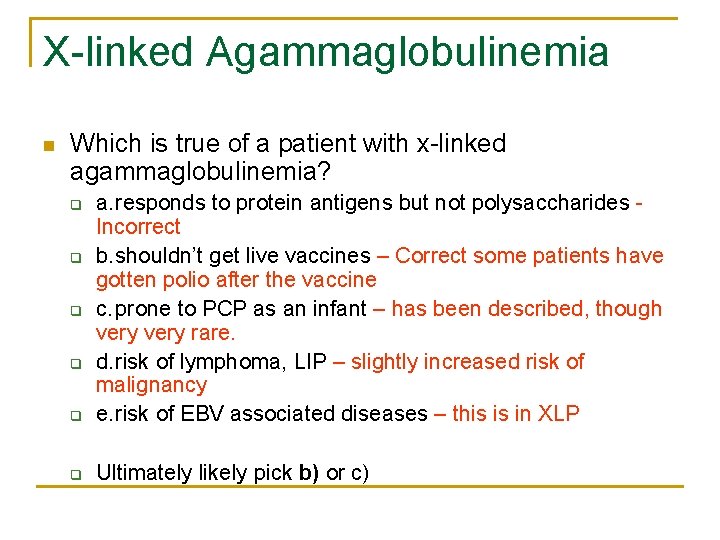
X-linked Agammaglobulinemia n Which is true of a patient with x-linked agammaglobulinemia? q a. responds to protein antigens but not polysaccharides Incorrect b. shouldn’t get live vaccines – Correct some patients have gotten polio after the vaccine c. prone to PCP as an infant – has been described, though very rare. d. risk of lymphoma, LIP – slightly increased risk of malignancy e. risk of EBV associated diseases – this is in XLP q Ultimately likely pick b) or c) q q
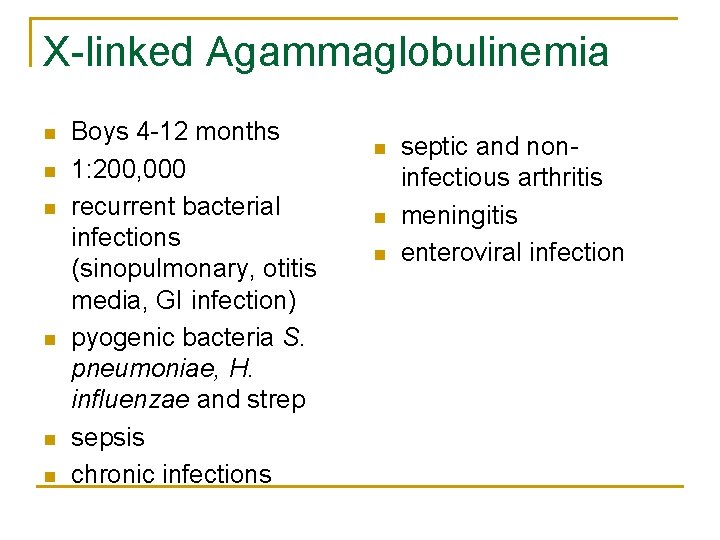
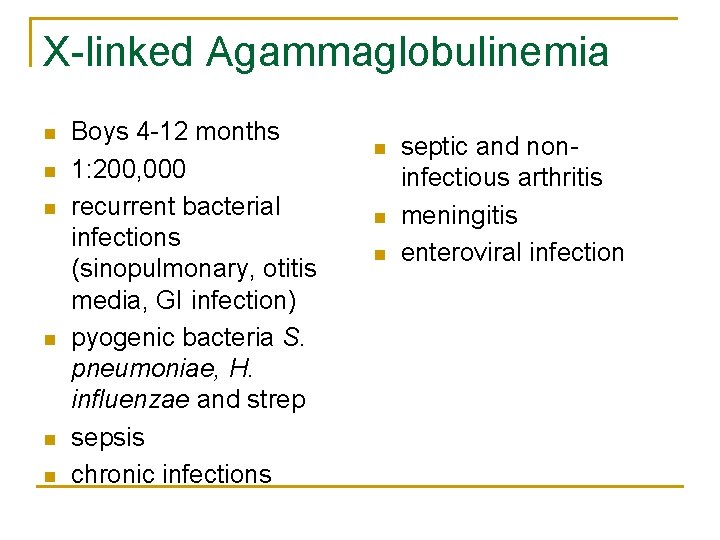
X-linked Agammaglobulinemia n n n Boys 4 -12 months 1: 200, 000 recurrent bacterial infections (sinopulmonary, otitis media, GI infection) pyogenic bacteria S. pneumoniae, H. influenzae and strep sepsis chronic infections n n n septic and noninfectious arthritis meningitis enteroviral infection
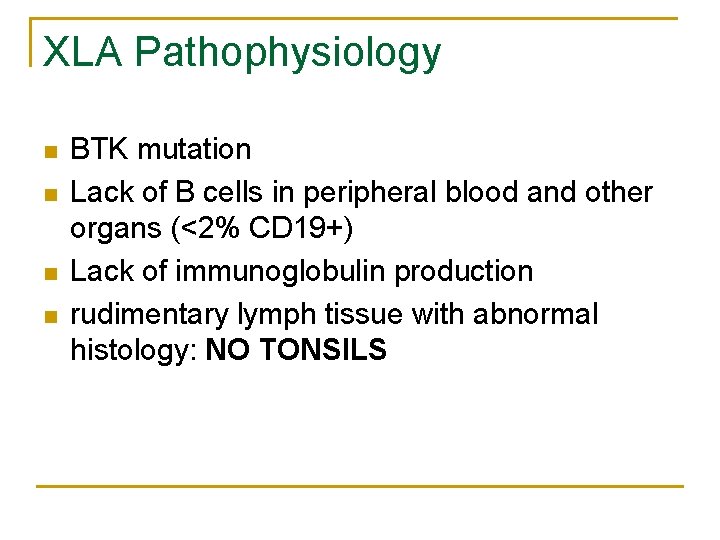
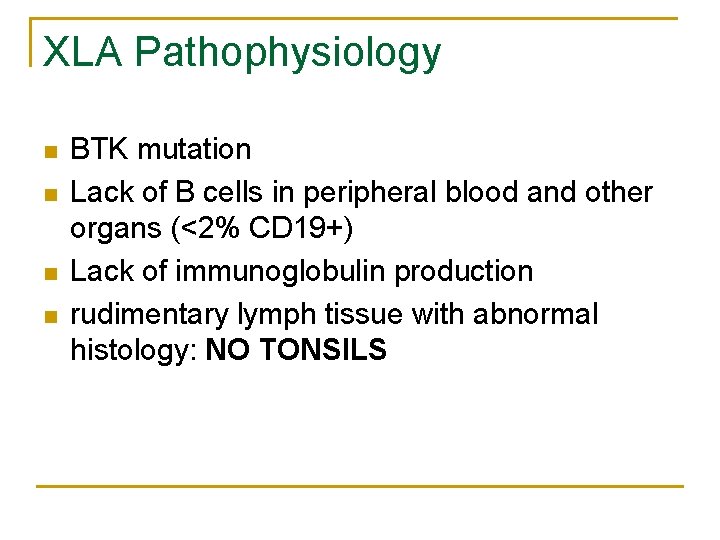
XLA Pathophysiology n n BTK mutation Lack of B cells in peripheral blood and other organs (<2% CD 19+) Lack of immunoglobulin production rudimentary lymph tissue with abnormal histology: NO TONSILS
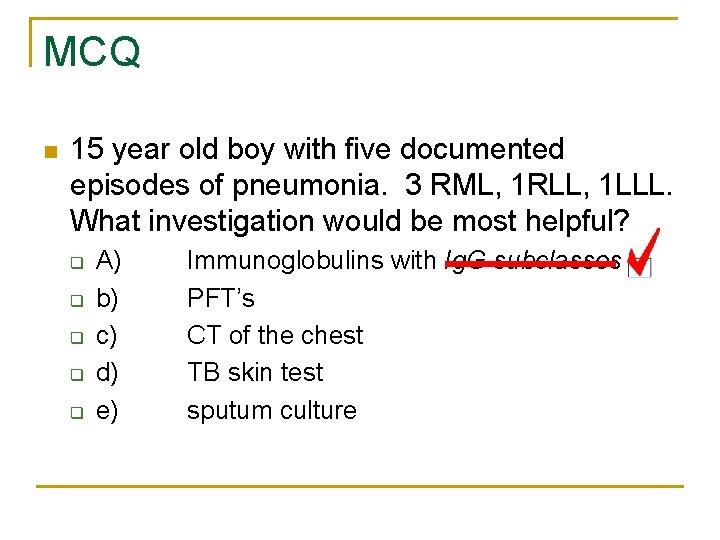
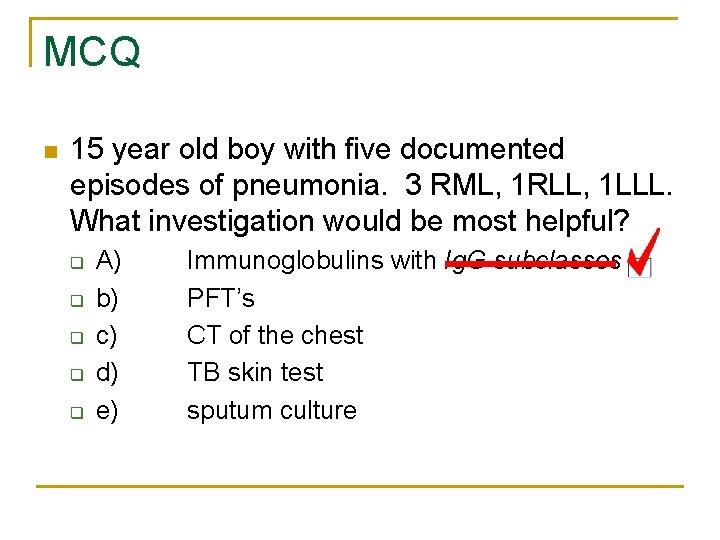
MCQ n 15 year old boy with five documented episodes of pneumonia. 3 RML, 1 RLL, 1 LLL. What investigation would be most helpful? q q q A) b) c) d) e) Immunoglobulins with Ig. G subclasses PFT’s CT of the chest TB skin test sputum culture
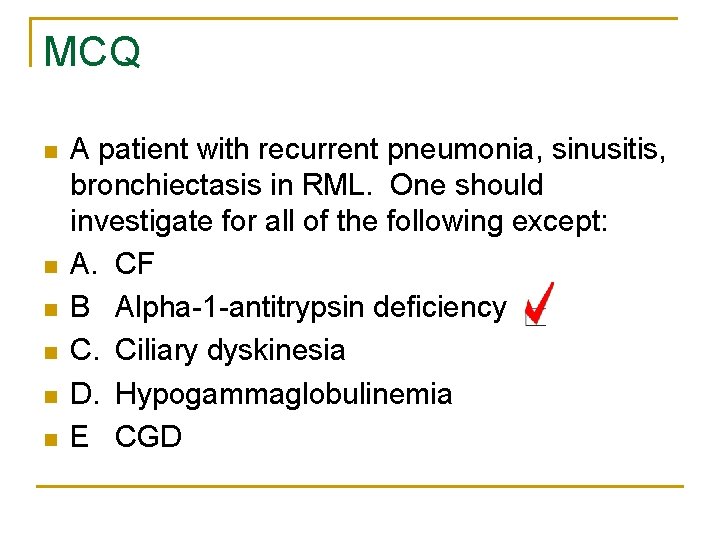
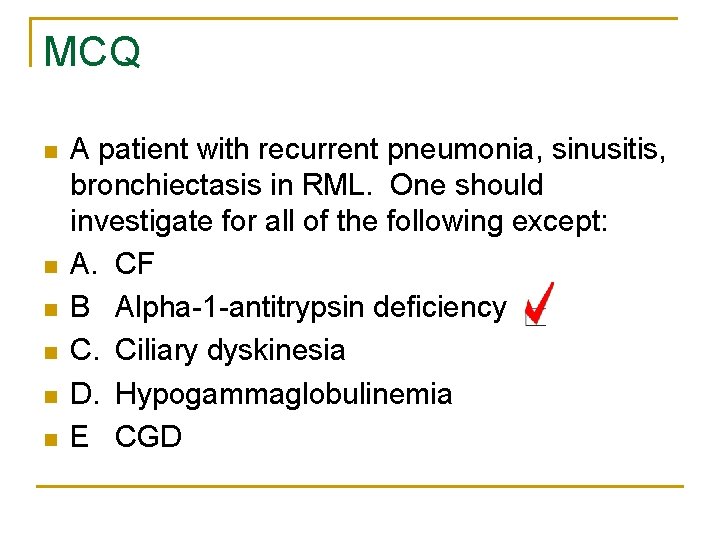
MCQ n n n A patient with recurrent pneumonia, sinusitis, bronchiectasis in RML. One should investigate for all of the following except: A. CF B Alpha-1 -antitrypsin deficiency C. Ciliary dyskinesia D. Hypogammaglobulinemia E CGD
COMBINED DEFECTS
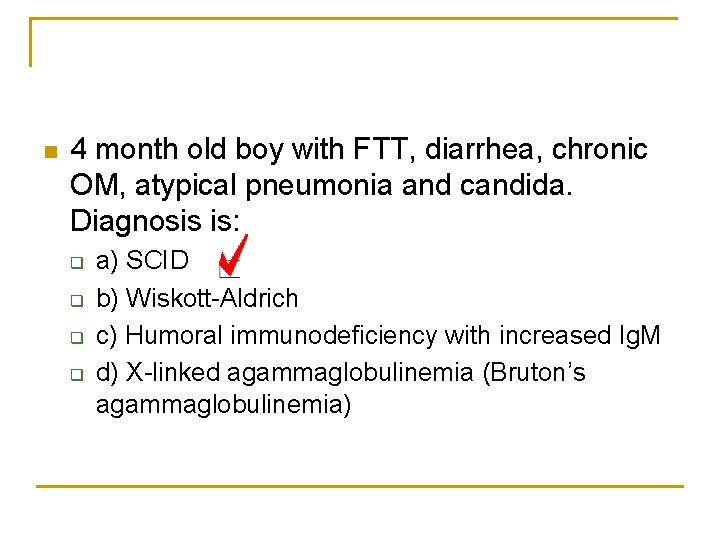
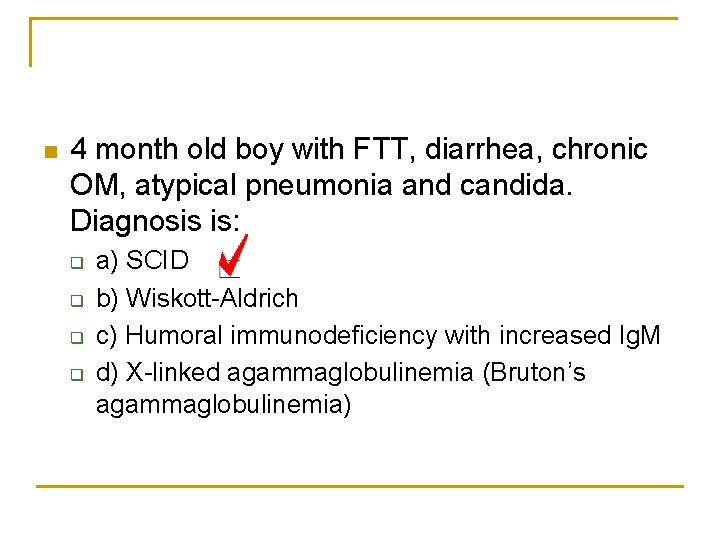
n 4 month old boy with FTT, diarrhea, chronic OM, atypical pneumonia and candida. Diagnosis is: q q a) SCID b) Wiskott-Aldrich c) Humoral immunodeficiency with increased Ig. M d) X-linked agammaglobulinemia (Bruton’s agammaglobulinemia)
SAQ n 4 month old boy presents with eczema, recurrent pneumonias and absent thymus shadow on CXR. What is the most likely diagnosis? SCID Omenn Syndrome
n 2 year old male. Which of the following is associated with a serious immunodeficiency? q q q A) b) c) d) e) Recurrent otitis media pneumonia at 6 months of age T&A at 18 months >6 colds per year oral candida at > than 6 months
OSCE n n Take a history from the mother of a 2 year old child with recurrent chest infections. Hx: DDx: Investigations:
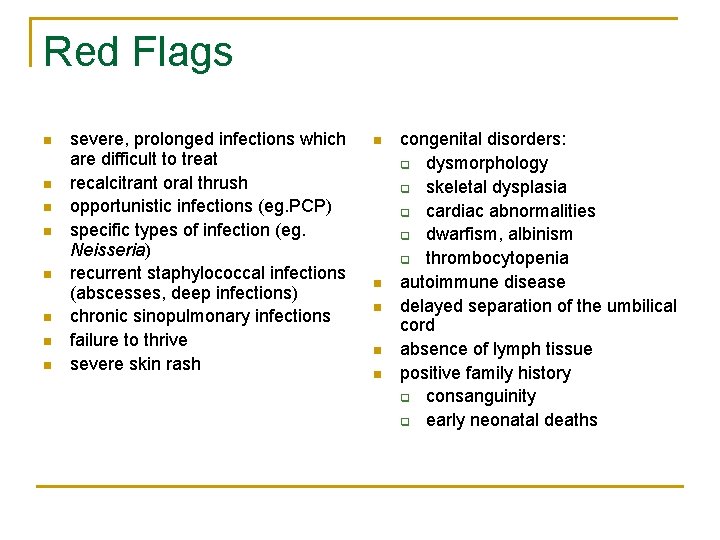
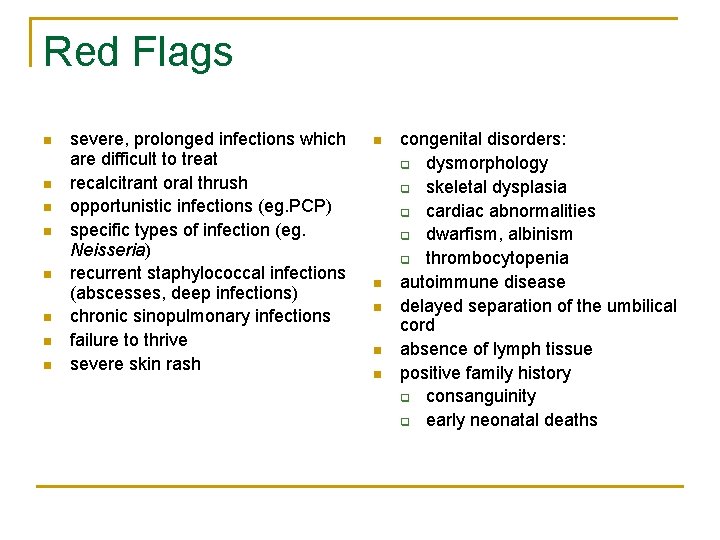
Red Flags n n n n severe, prolonged infections which are difficult to treat recalcitrant oral thrush opportunistic infections (eg. PCP) specific types of infection (eg. Neisseria) recurrent staphylococcal infections (abscesses, deep infections) chronic sinopulmonary infections failure to thrive severe skin rash n n n congenital disorders: q dysmorphology q skeletal dysplasia q cardiac abnormalities q dwarfism, albinism q thrombocytopenia autoimmune disease delayed separation of the umbilical cord absence of lymph tissue positive family history q consanguinity q early neonatal deaths
Severe Combined Immunodeficiency (SCID) q q q Severe deficiency of both B-cell and T-cell function T lymphocytes severely reduced B cells and NK cells vary
Severe Combined Immunodeficiency (SCID) Ø 4 -12 months ØPersistent/recurrent bacterial, fungal & viral infections ØChronic diarrhea ØPneumonitis ØFTT ØPJP infection ØOral thrush ØDisseminated CMV SCID = PEDIATRIC EMERGENCY Bubble Boy
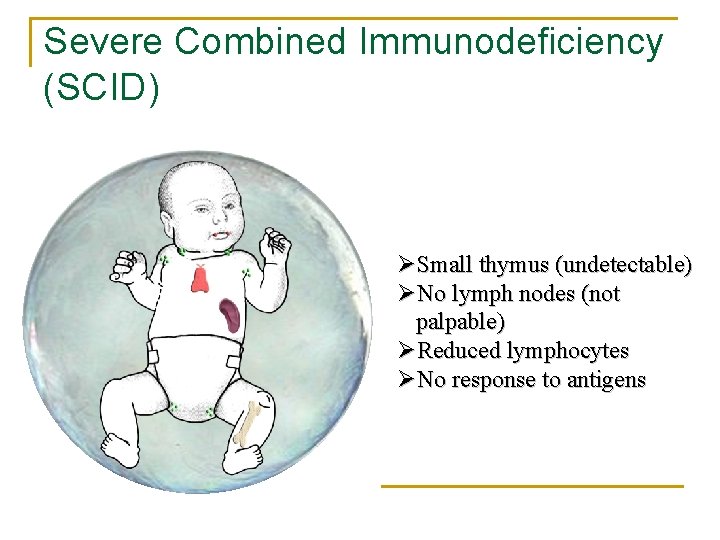
Severe Combined Immunodeficiency (SCID) ØSmall thymus (undetectable) ØNo lymph nodes (not palpable) ØReduced lymphocytes ØNo response to antigens
Severe Combined Immunodeficiency
Graft vs. Host Disease n Chronic GVHD affects all except: q q q a) b) c) d) e) skin eyes liver GI tract oral mucosa q. It does in fact affect all these areas…
Graft vs. Host Disease n Up to 60% of bone marrow transplant recipients n Severity depends on donor type, marrow treatment, and immunosuppressive prophylactic regimen
Graft vs. Host Disease n Acute GVHD q q clinical manifestations occur from 14 (engraftment) to 100 days after transplantation SKIN-LIVER-GUT n n n q skin rash hepatocellular injury GI inflammation causing diarrhea treated with steroids, CSA, MTX
Graft vs. Host Disease n Chronic GVHD q q q 3 to 15 months after transplantation and may last for years progressive systemic sclerosis, mucous membranes may become dry, anemia thrombocytopenia, eosinophilia, restrictive pulmonary defects involvement of esophagus, small intestine and liver may result in loss of weight and cholestatic liver disease
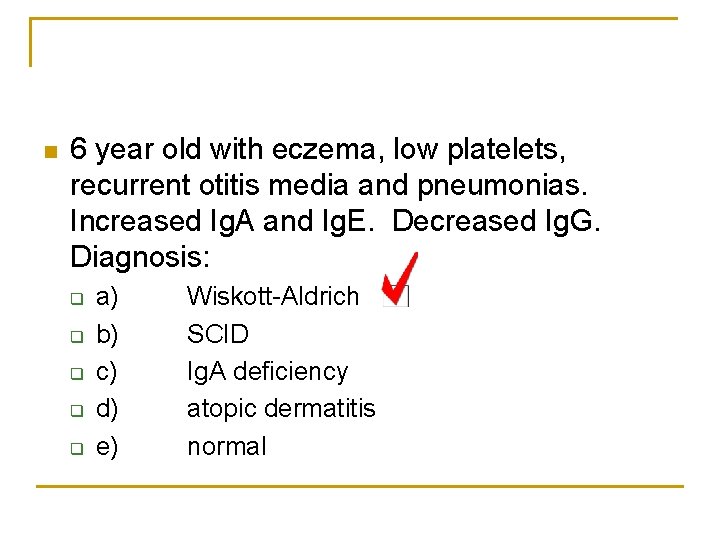
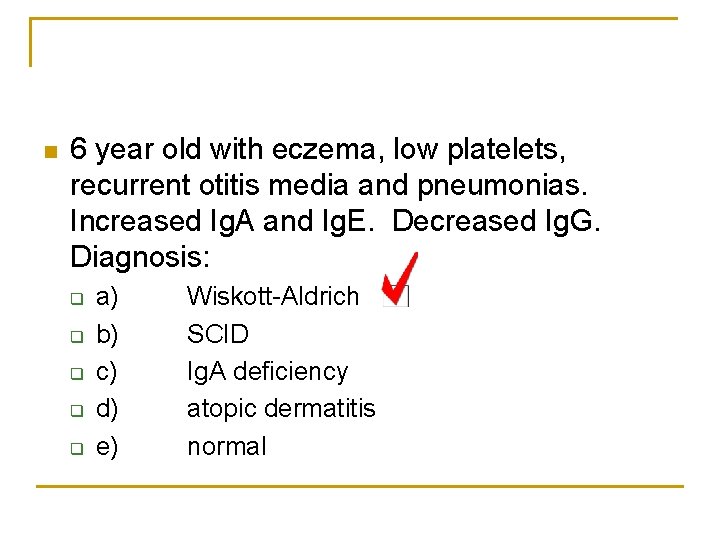
n 6 year old with eczema, low platelets, recurrent otitis media and pneumonias. Increased Ig. A and Ig. E. Decreased Ig. G. Diagnosis: q q q a) b) c) d) e) Wiskott-Aldrich SCID Ig. A deficiency atopic dermatitis normal
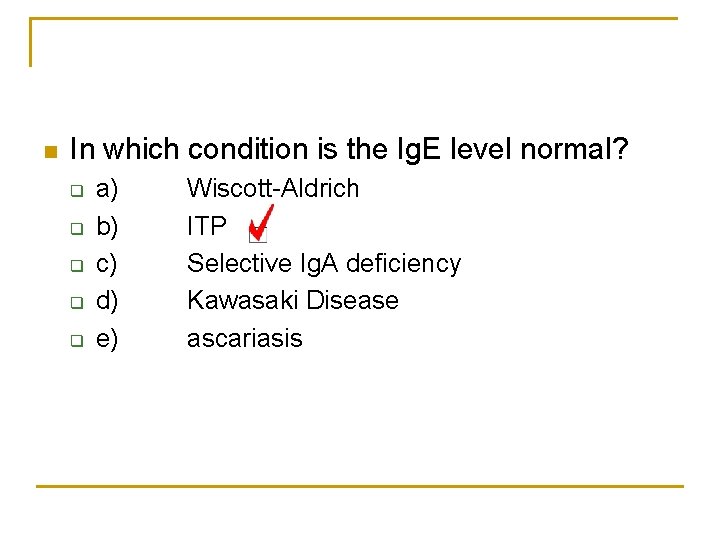
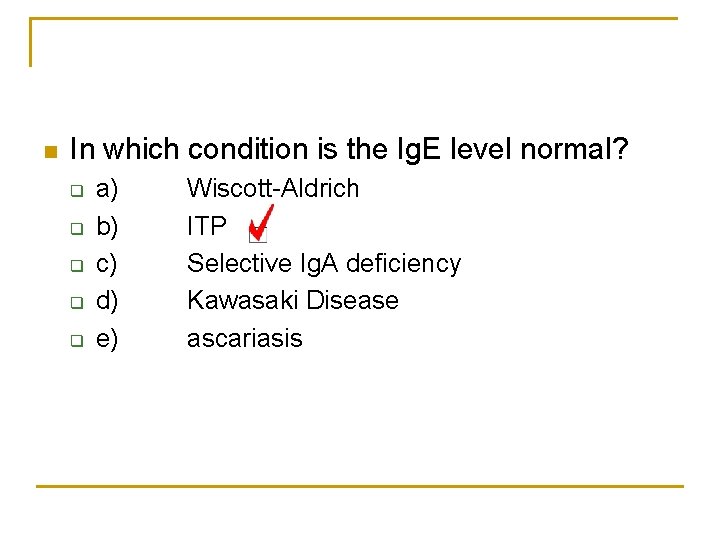
n In which condition is the Ig. E level normal? q q q a) b) c) d) e) Wiscott-Aldrich ITP Selective Ig. A deficiency Kawasaki Disease ascariasis
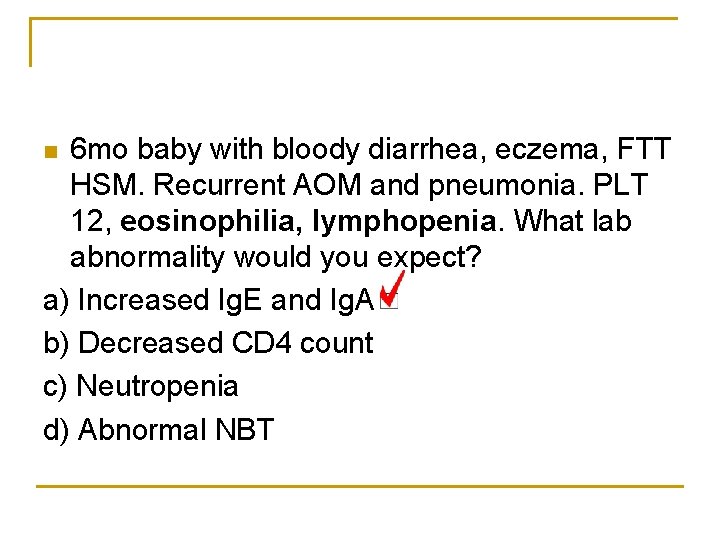
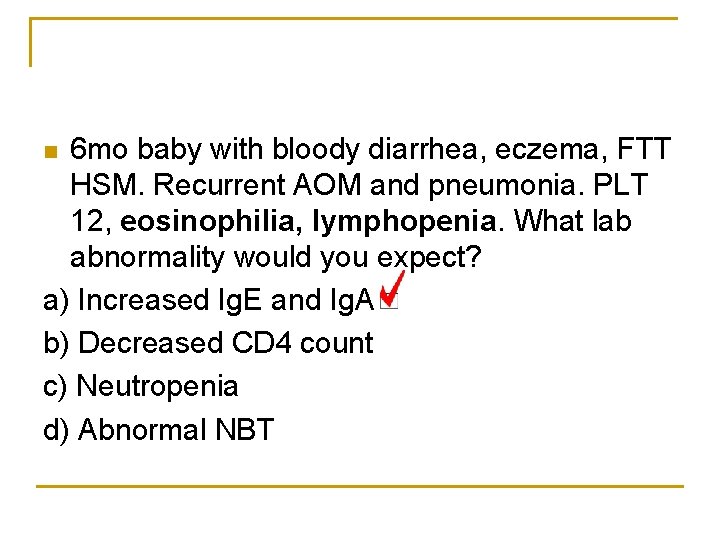
6 mo baby with bloody diarrhea, eczema, FTT HSM. Recurrent AOM and pneumonia. PLT 12, eosinophilia, lymphopenia. What lab abnormality would you expect? a) Increased Ig. E and Ig. A b) Decreased CD 4 count c) Neutropenia d) Abnormal NBT n
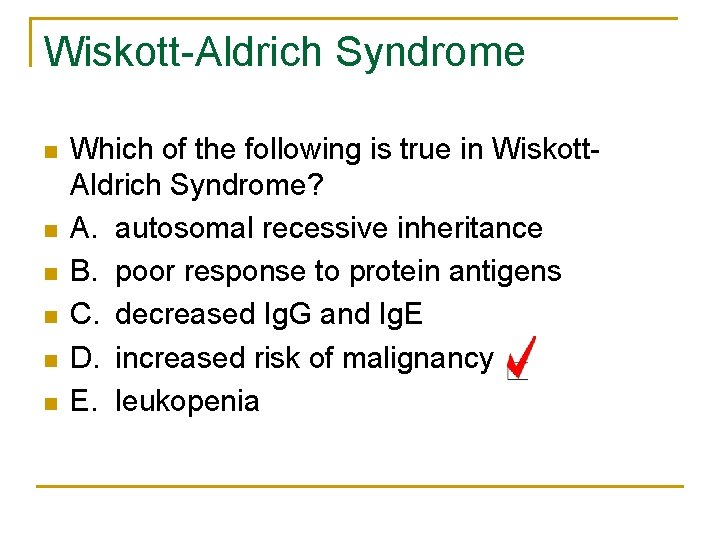
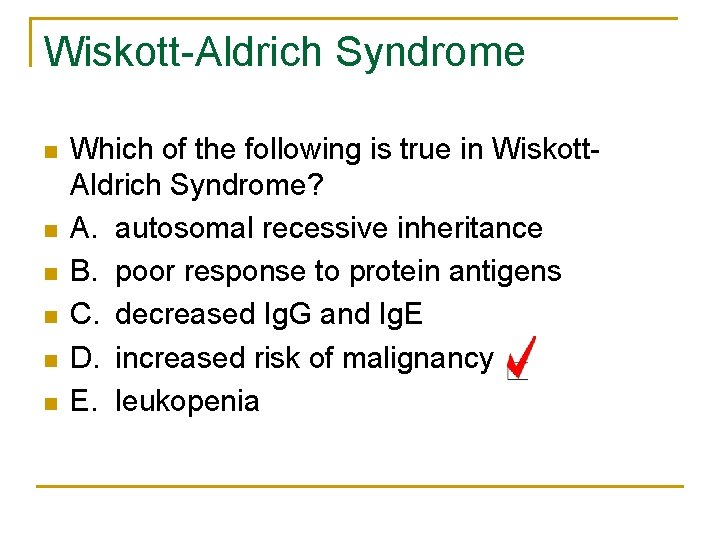
Wiskott-Aldrich Syndrome n n n Which of the following is true in Wiskott. Aldrich Syndrome? A. autosomal recessive inheritance B. poor response to protein antigens C. decreased Ig. G and Ig. E D. increased risk of malignancy E. leukopenia
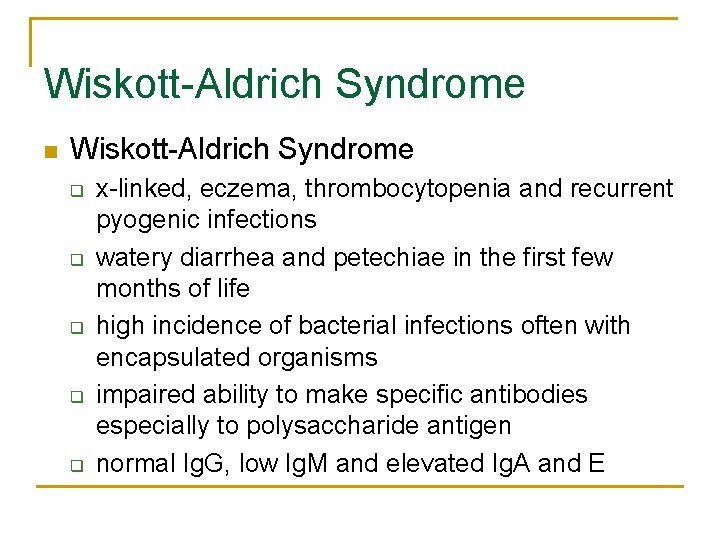
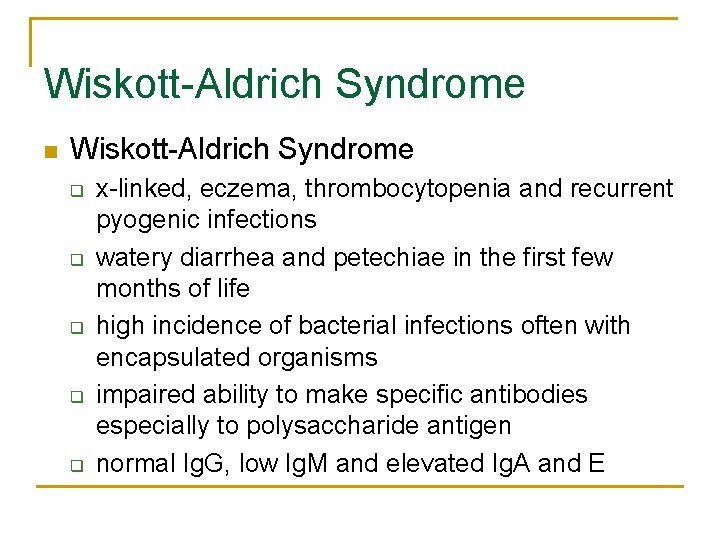
Wiskott-Aldrich Syndrome n Wiskott-Aldrich Syndrome q q q x-linked, eczema, thrombocytopenia and recurrent pyogenic infections watery diarrhea and petechiae in the first few months of life high incidence of bacterial infections often with encapsulated organisms impaired ability to make specific antibodies especially to polysaccharide antigen normal Ig. G, low Ig. M and elevated Ig. A and E

Wiskott-Aldrich Syndrome
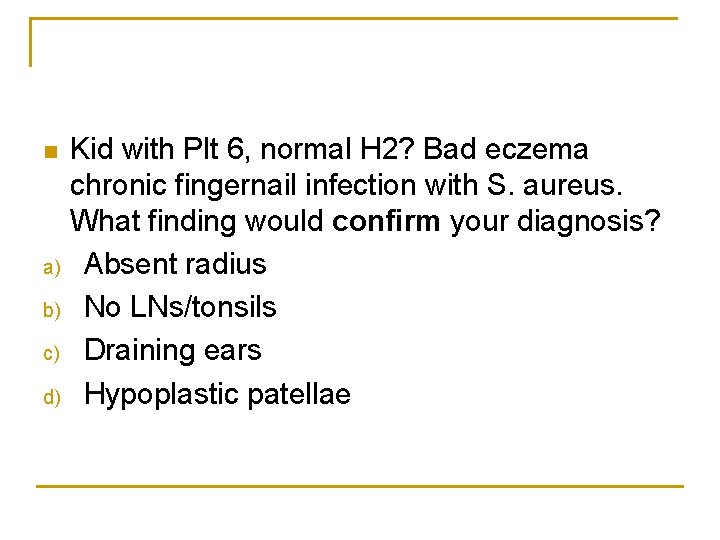
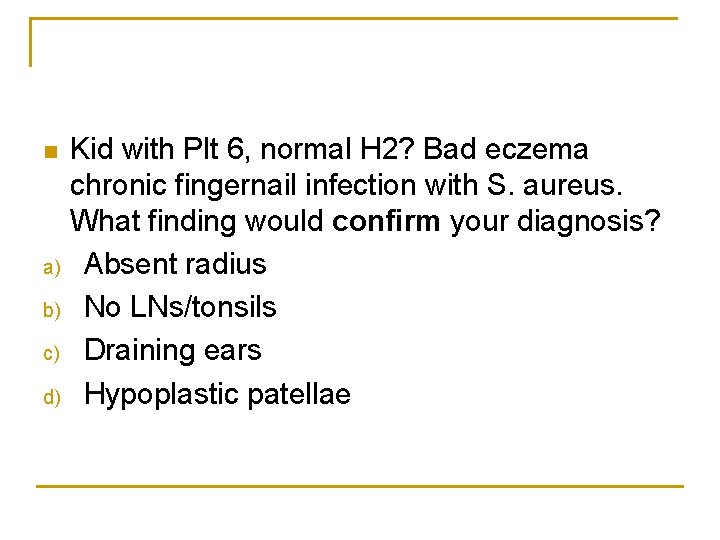
n a) b) c) d) Kid with Plt 6, normal H 2? Bad eczema chronic fingernail infection with S. aureus. What finding would confirm your diagnosis? Absent radius No LNs/tonsils Draining ears Hypoplastic patellae
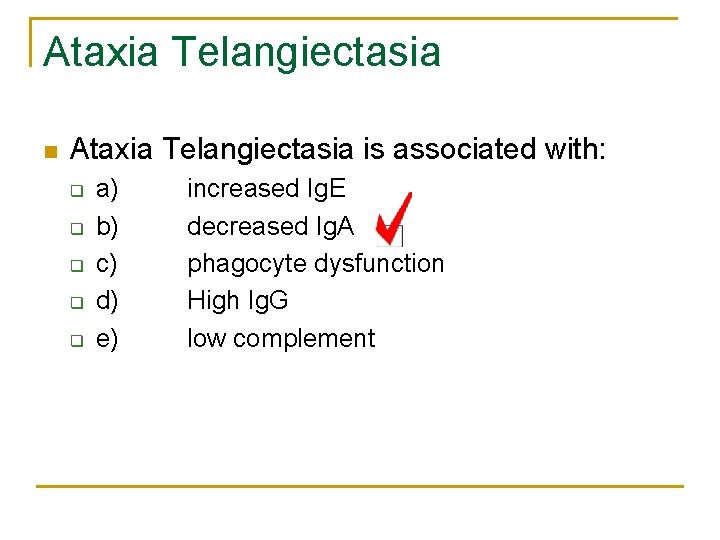
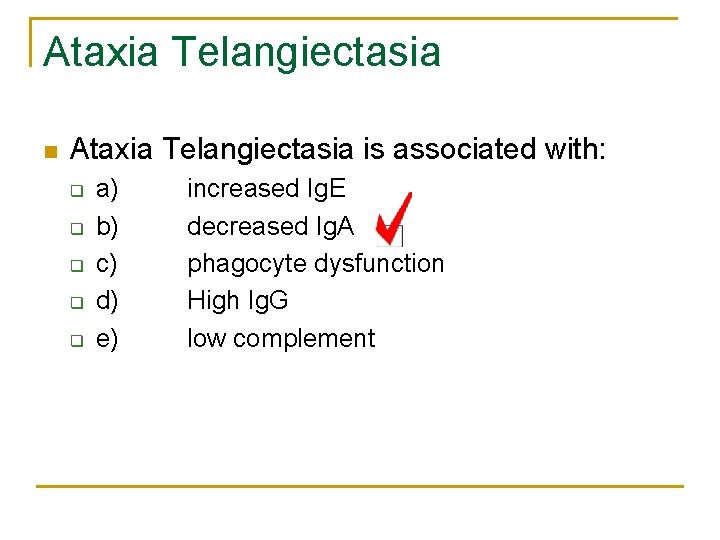
Ataxia Telangiectasia n Ataxia Telangiectasia is associated with: q q q a) b) c) d) e) increased Ig. E decreased Ig. A phagocyte dysfunction High Ig. G low complement
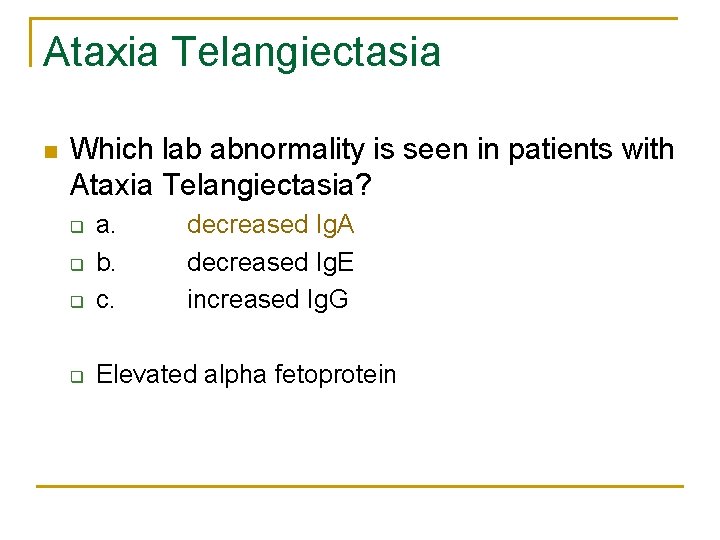
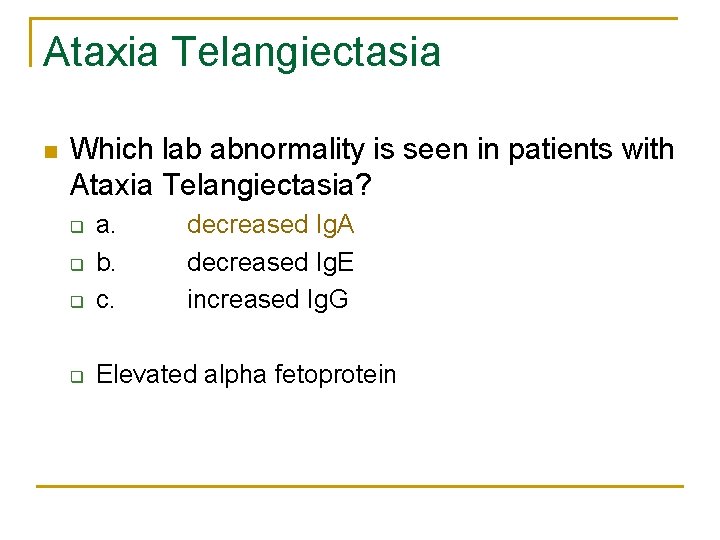
Ataxia Telangiectasia n Which lab abnormality is seen in patients with Ataxia Telangiectasia? q a. b. c. q Elevated alpha fetoprotein q q decreased Ig. A decreased Ig. E increased Ig. G
Ataxia Telangiectasia n Ataxia-Telangiectasia q q q complex multisystem disease with variable immune system involvement progressive cerebellar ataxia child usually confined to a wheelchair by 10 to 12 years occulomotor abnormalities are prominent recurrent sinopulmonary infections, pneumonia and bronchiectasis
Ataxia Telangiectasia q q q q 15% of patients develop malignancy abnormal DNA repair 50% - 80% have absent Ig. A reduced ability to make antibodies slightly decreased T-cell numbers decreased proliferations treatment is supportive

Ataxia Telangiectasia
Recurrent Candida n Which of the following is not associated with recurrent candida infection: q q a) b) c) d) complement deficiency prolonged antibiotics hypoparathyroidism addison’s disease
Chronic Mucocutaneous Candidiasis n Chronic Mucocutaneous Candidiasis q q group of syndromes characterized by persistent infections of the skin, nails and mucous membranes with Candida species disseminated infection is almost unheard of (mechanism is not understood)
Chronic Mucocutaneous Candidiasis q q q endocrine abnormalities include, hypothyroidism, hyperthyroidism, hypoadrenalism and gonadal dysfunction pernicious anemia may be associated also supportive therapy - antifungals etc.
INNATE IMMUNITY
Complement Deficiencies n The causes of infection in C 2 deficiency include: q q a) b) c) d) candida staph strep pneumo mycoplasma
Complement Deficiencies n n 18 month old with knee arthritis, aspirate grew N. meningitidis. This is the same organism that grew in his CSF when he had meningitis at 10 months. Which of the following tests is most likely to be abnormal in this child? A. Immunoglobulins B. C 3, C 4, total hemolytic complement C. lymphocyte differentiation
Complement deficiencies n 18 mo boy with meningococcal meningitis and sepsis. Which is most likely to be abnormal? a) b) C 3, C 4, CH 50 Immunoglobulins
Complement Deficiencies n Recurrent meningococcal meningitis. The most common immunodeficiency would be: q C 5, C 6, C 7, C 8 CH 50 will be low (0) in early and late components dificiencies
Complement Deficiencies n n n 2 - 5% of all immunodeficiency disorders presents with recurrent infections, rheumatic disorders, or angioedema C 5 -9 = systemic Neisserial infections C 1 -4 = rheumatologic may present with Lupus-like syndrome
Complement Deficiencies n C 2 deficiency is the most commonly reported complement deficiency q q 1: 10, 000 to 1: 28, 000 associated with a variety of collagen vascular diseases as well as in normal subjects SLE, discoid lupus, MPGN, HSP, RA, dermatomyositis, Crohn’s disease, ITP there is a clear association with certain infections: n Pneumococcus is the most common but also with meningococcus, H. flu, enteric bacteria and Staph
Chronic Granulomatous Disease n n n In chronic granulomatous disease, all of the following features are present EXCEPT: A. usually present in males B. leukocytosis C. lymphadenopathy D. Hepatomegaly E. Hypogammablobulinemia
Chronic Granulomatous Disease n n n What is true about chronic granulomatous disease: A. all girls with the disease must be 45 XO karyotype B. suppurative lymhadenopathy is a characteristic feature C. there are decreased lymphocytes in 90% of cases D. there a decreased number of absolute neutrophils E. rarely present before 5 years of age
Chronic Granulomatous Disease n n n Majority are x-linked, AR has been described NBT (nitroblue of tetrazolium) was test of choice, now using flow cytometry (NOBI or neutrophil oxidative burst index) disorder of bactericidal activity due to defective oxidative metabolism aggressive antibiotic therapy has improved outcome without bone marrow transplantation Only cure: BMT
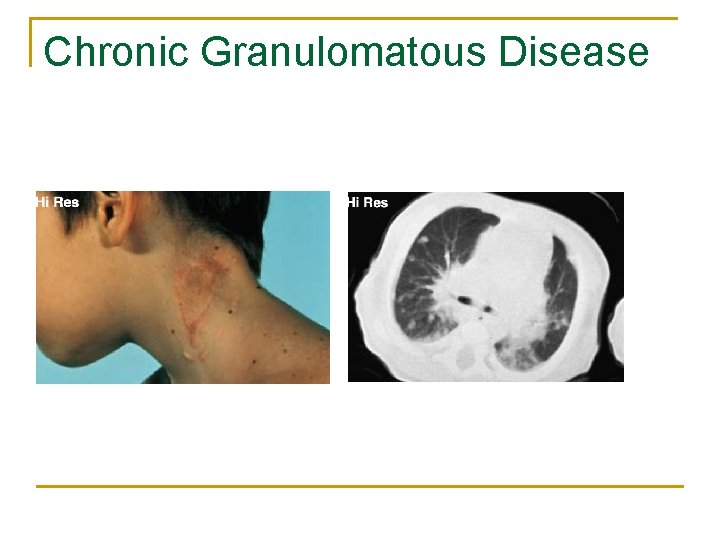
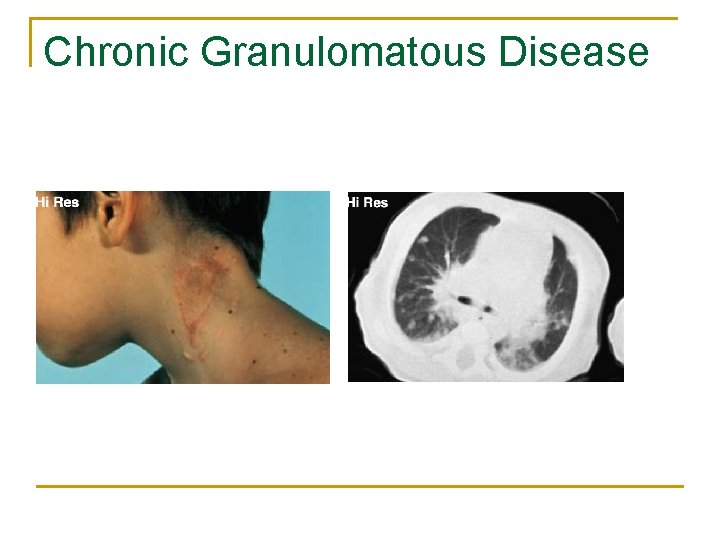
Chronic Granulomatous Disease
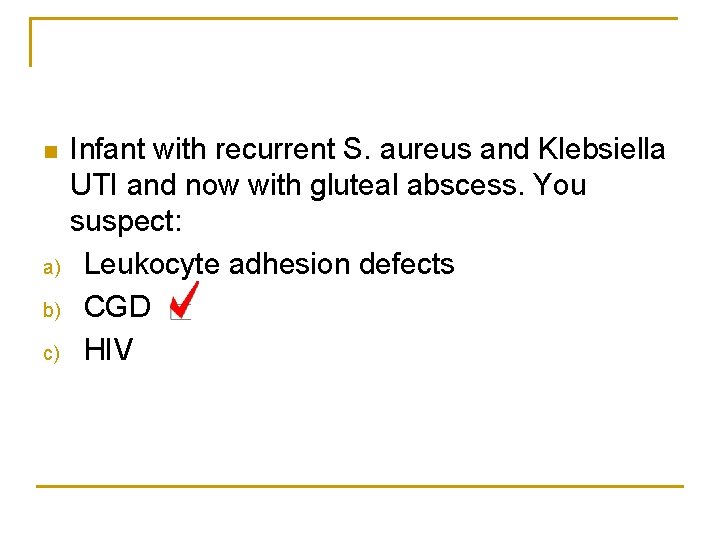
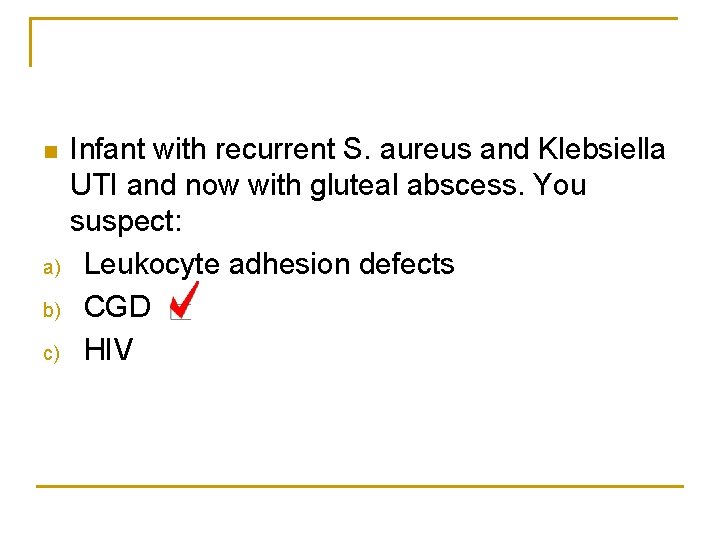
n a) b) c) Infant with recurrent S. aureus and Klebsiella UTI and now with gluteal abscess. You suspect: Leukocyte adhesion defects CGD HIV
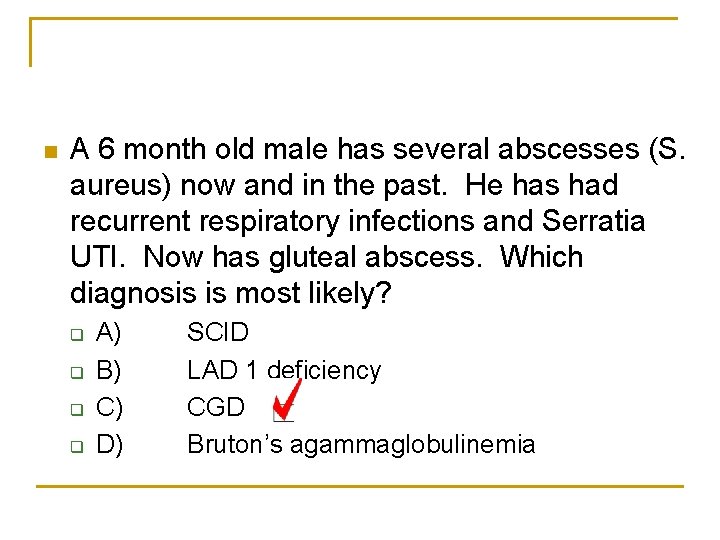
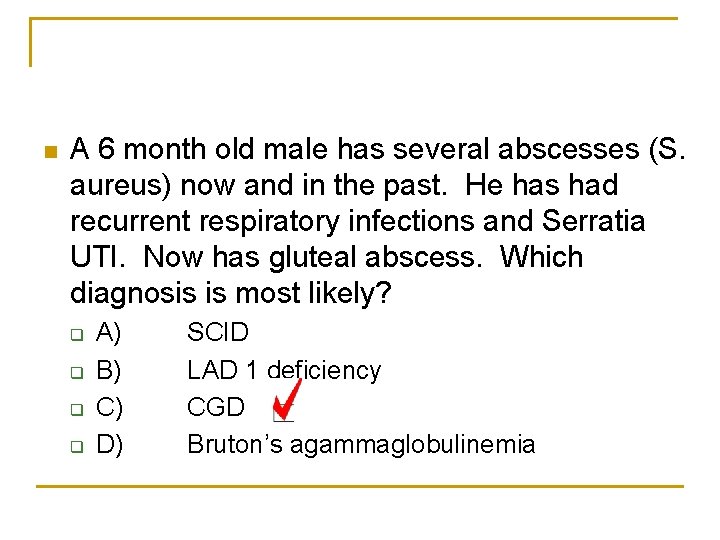
n A 6 month old male has several abscesses (S. aureus) now and in the past. He has had recurrent respiratory infections and Serratia UTI. Now has gluteal abscess. Which diagnosis is most likely? q q A) B) C) D) SCID LAD 1 deficiency CGD Bruton’s agammaglobulinemia
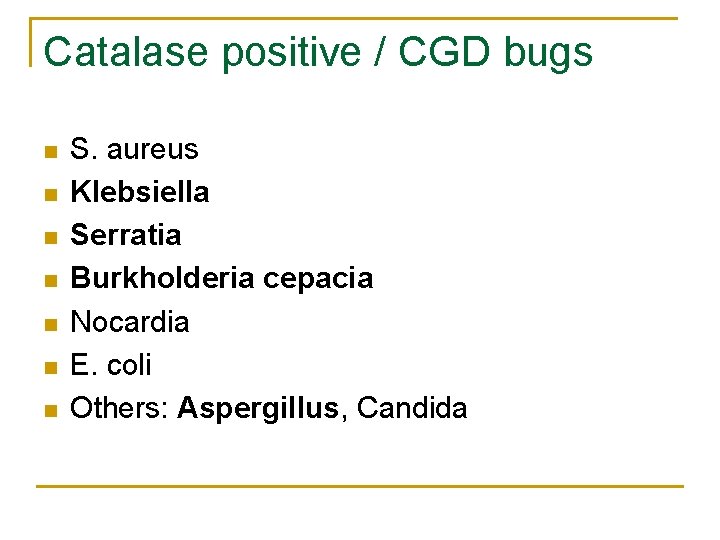
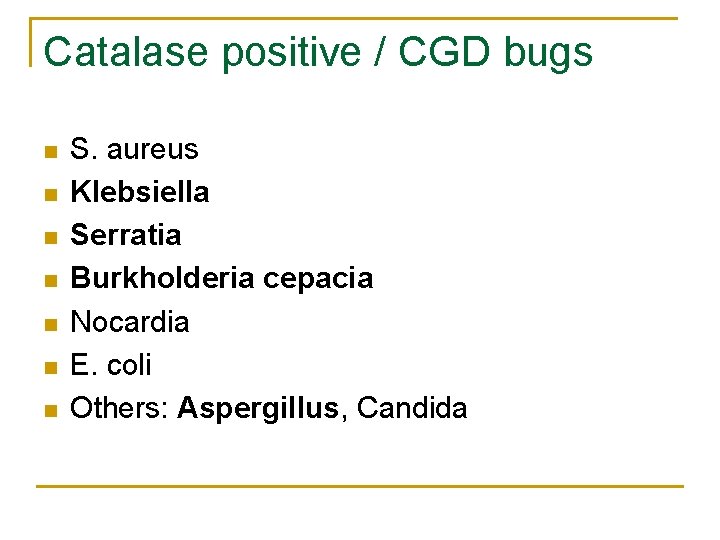
Catalase positive / CGD bugs n n n n S. aureus Klebsiella Serratia Burkholderia cepacia Nocardia E. coli Others: Aspergillus, Candida
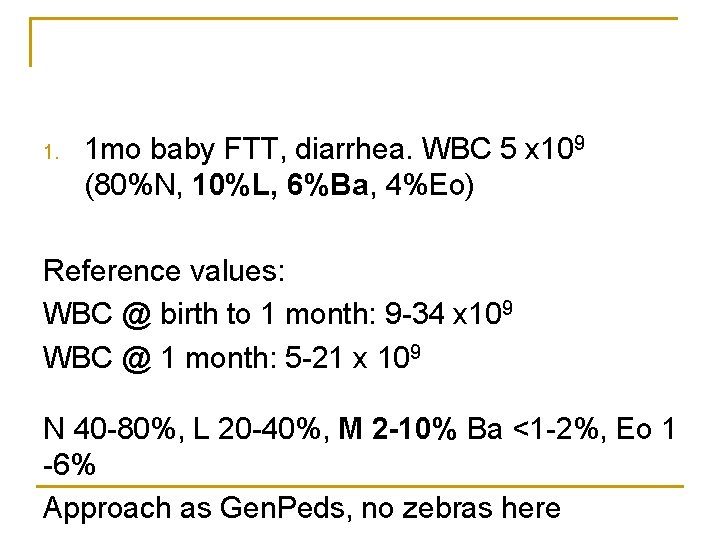
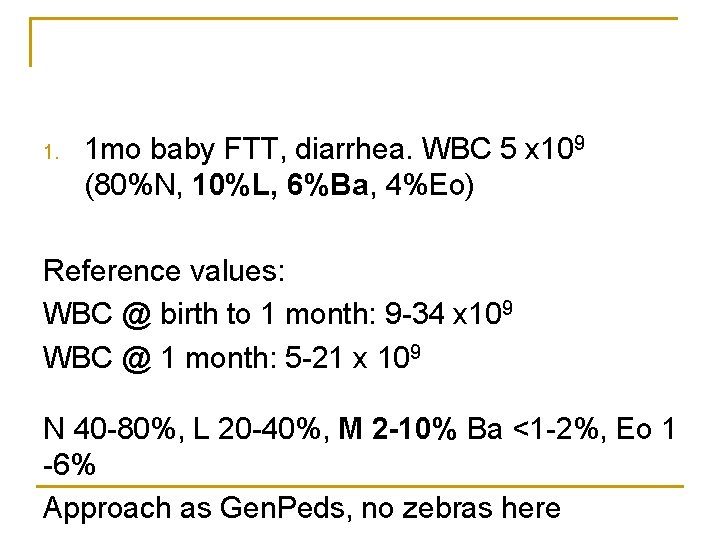
1. 1 mo baby FTT, diarrhea. WBC 5 x 109 (80%N, 10%L, 6%Ba, 4%Eo) Reference values: WBC @ birth to 1 month: 9 -34 x 109 WBC @ 1 month: 5 -21 x 109 N 40 -80%, L 20 -40%, M 2 -10% Ba <1 -2%, Eo 1 -6% Approach as Gen. Peds, no zebras here
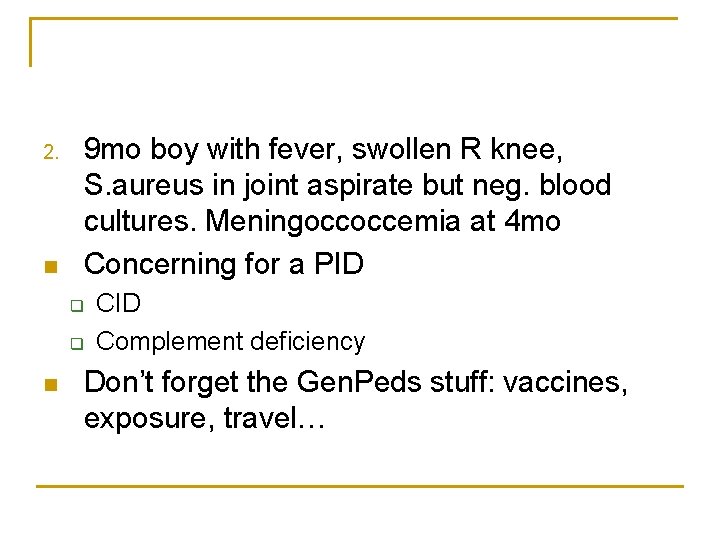
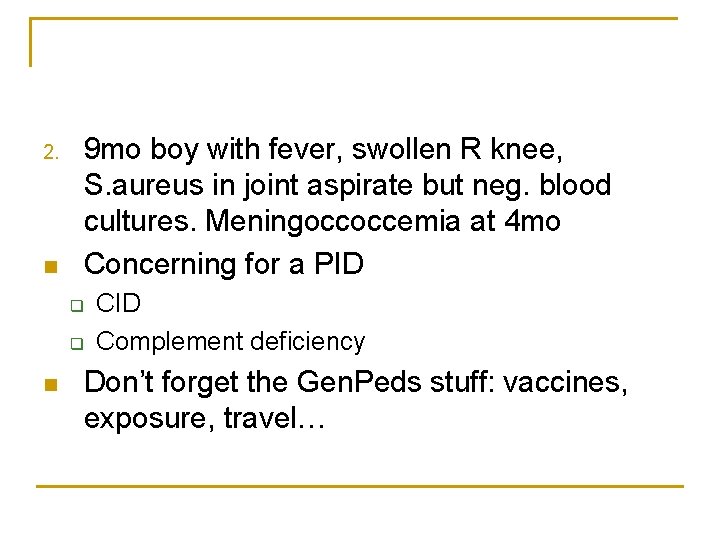
2. n 9 mo boy with fever, swollen R knee, S. aureus in joint aspirate but neg. blood cultures. Meningoccoccemia at 4 mo Concerning for a PID q q n CID Complement deficiency Don’t forget the Gen. Peds stuff: vaccines, exposure, travel…
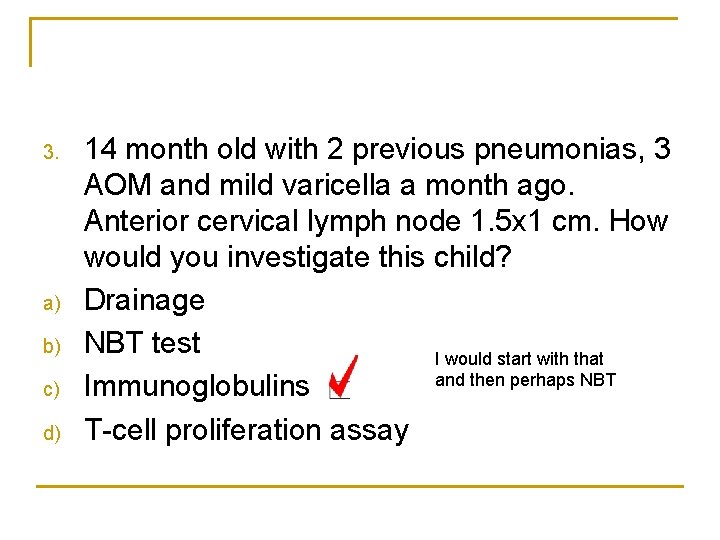
3. a) b) c) d) 14 month old with 2 previous pneumonias, 3 AOM and mild varicella a month ago. Anterior cervical lymph node 1. 5 x 1 cm. How would you investigate this child? Drainage NBT test I would start with that and then perhaps NBT Immunoglobulins T-cell proliferation assay
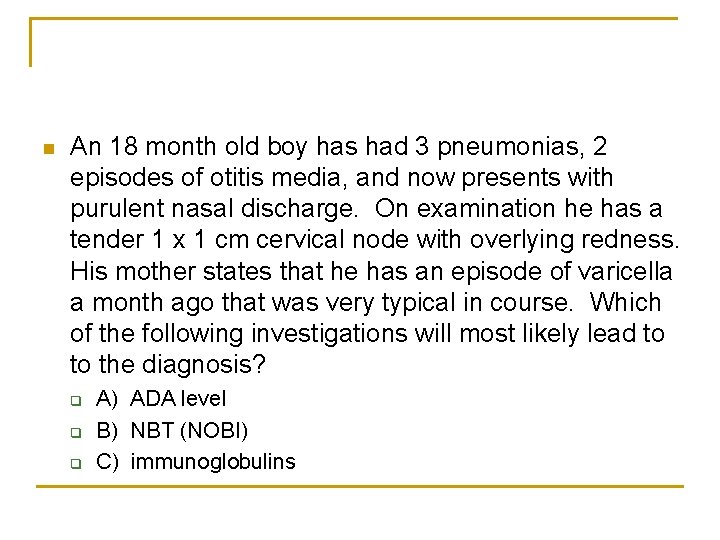
n An 18 month old boy has had 3 pneumonias, 2 episodes of otitis media, and now presents with purulent nasal discharge. On examination he has a tender 1 x 1 cm cervical node with overlying redness. His mother states that he has an episode of varicella a month ago that was very typical in course. Which of the following investigations will most likely lead to to the diagnosis? q q q A) ADA level B) NBT (NOBI) C) immunoglobulins

ALLERGY
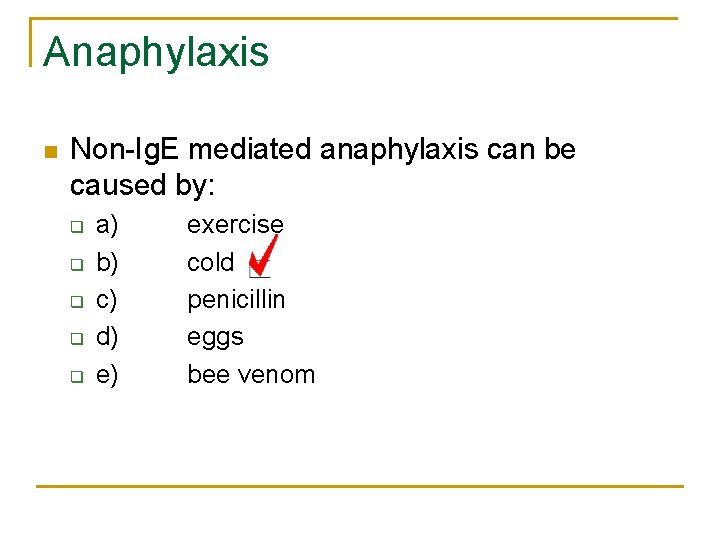
Anaphylaxis n Non-Ig. E mediated anaphylaxis can be caused by: q q q a) b) c) d) e) exercise cold penicillin eggs bee venom
Anaphylaxis n Child with anaphylaxis reaction. How should epinephrine be adminstered? q q A) B) C) D) SQ in arm IM in thigh SQ in the abdomen IV
Anaphylaxis n A child is brought to the emergency room after being stung by a bee. He is wheezing and moderately tachypneic and tachycardic. BP 100/70. First step in management: q q q A) B) C) D) E) 0. 01 mg/kg SC epi 0. 01 mg/kg IV epi oxygen methylprednisolone Benadryl ABC’s
n 6 year old child. Allergy to peanuts. Had peanuts 30 minutes ago. No respiratory distress, VSS, rash and itchy. Management: q q q a) IV epinephrine would be the preferred medication b) benadryl IV/ PO/IM*** c) Ventolin and pulmicort should be administered d) steroids would not affect secondary reaction d) desensitization therapy should be undertaken
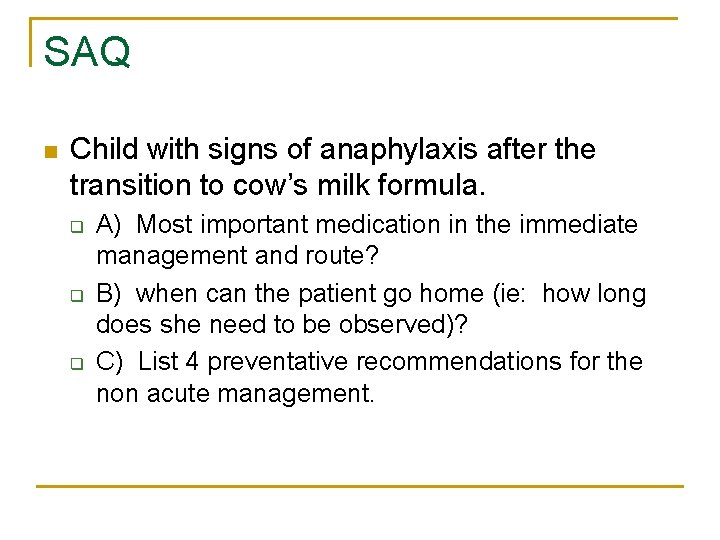
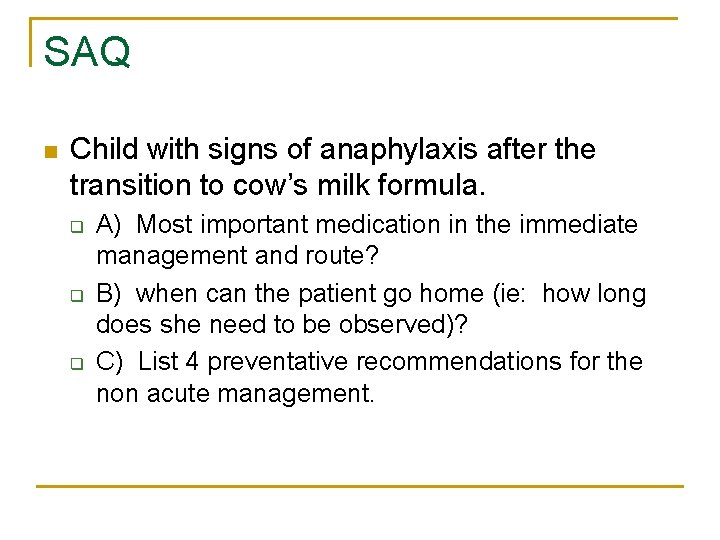
SAQ n Child with signs of anaphylaxis after the transition to cow’s milk formula. q q q A) Most important medication in the immediate management and route? B) when can the patient go home (ie: how long does she need to be observed)? C) List 4 preventative recommendations for the non acute management.
Anaphylaxis n n n Food, drugs and insect stings are all Ig. E mediated reactions which may lead to anaphylaxis exercise-induced anaphylaxis has been associated with an Ig. E mechanism cold induced urticaria/anaphylaxis is usually listed as anaphylactoid (non-Ig. E)
Anaphylaxis n Etiology q q q q food - peanuts and shellfish insect stings - Hymenoptera including yellow jackets, yellow hornet, white-faced hornet, wasp and honeybee medications - antibiotics, ASA, NSAID’s exercise vaccines latex immunotherapy
Anaphylaxis n Clinical Course q q usually uniphasic but can be biphasic or protracted biphasic reaction occurs in approximately 15 to 30% of cases within 4 to 8 hours
Anaphylaxis n Management q acute n n n A B C’s large bore IV epinephrine 0. 01 mg/kg/dose (0. 01 ml/kg/dose of 1: 1000 concentration solution) up to a maximum of 0. 5 given IM IV epinephrine may be used in the critically ill patient as long as the patient is highly monitored diphenhydramine 1 - 2 mg/kg steroids
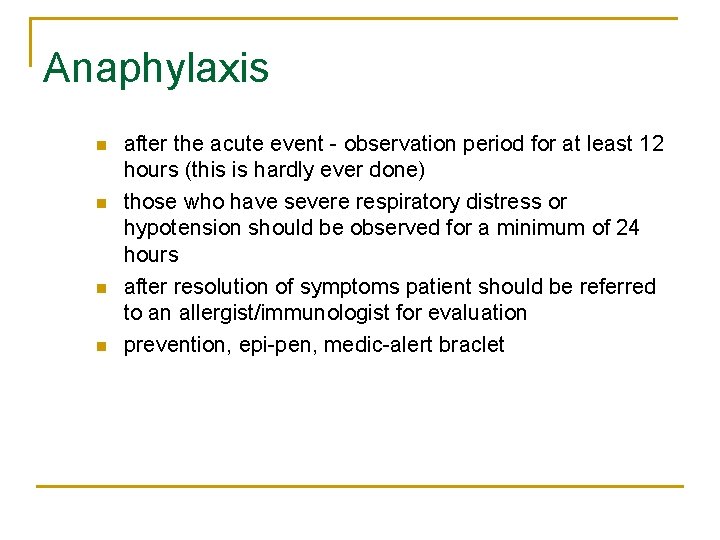
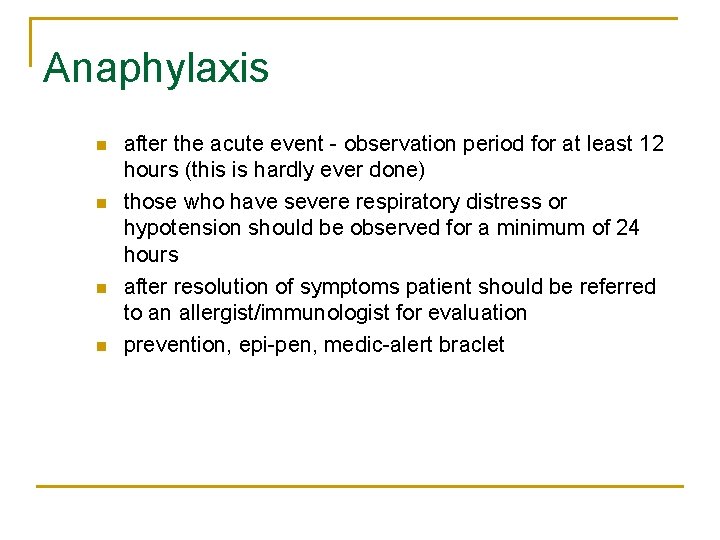
Anaphylaxis n n after the acute event - observation period for at least 12 hours (this is hardly ever done) those who have severe respiratory distress or hypotension should be observed for a minimum of 24 hours after resolution of symptoms patient should be referred to an allergist/immunologist for evaluation prevention, epi-pen, medic-alert braclet
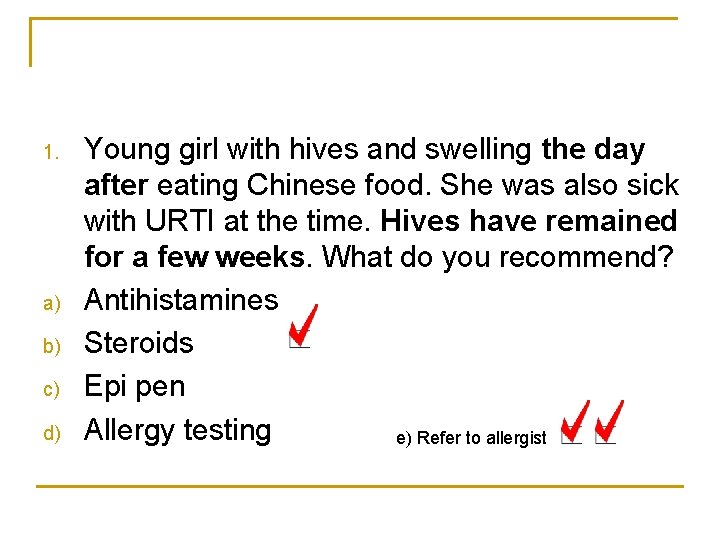
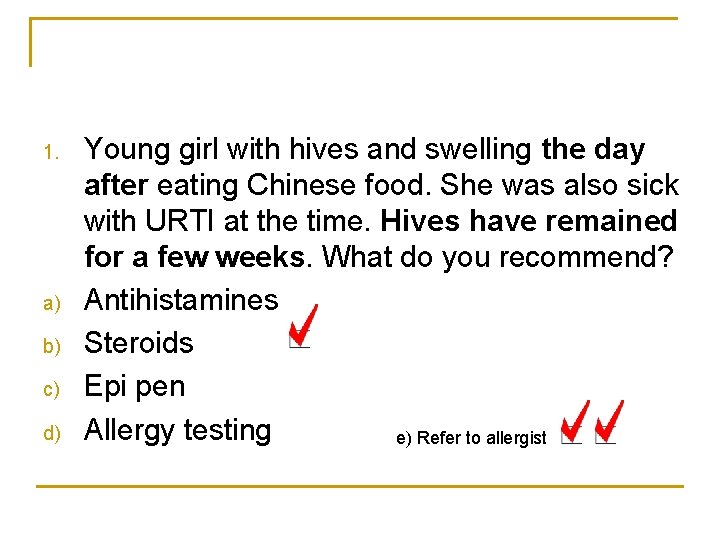
1. a) b) c) d) Young girl with hives and swelling the day after eating Chinese food. She was also sick with URTI at the time. Hives have remained for a few weeks. What do you recommend? Antihistamines Steroids Epi pen Allergy testing e) Refer to allergist
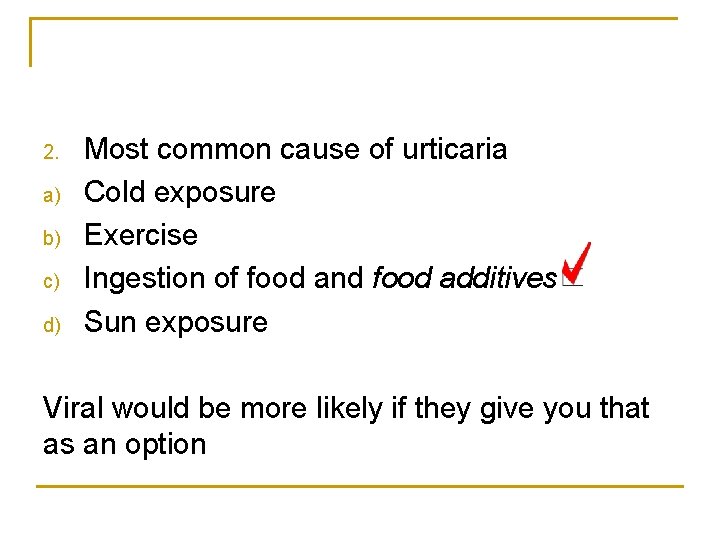
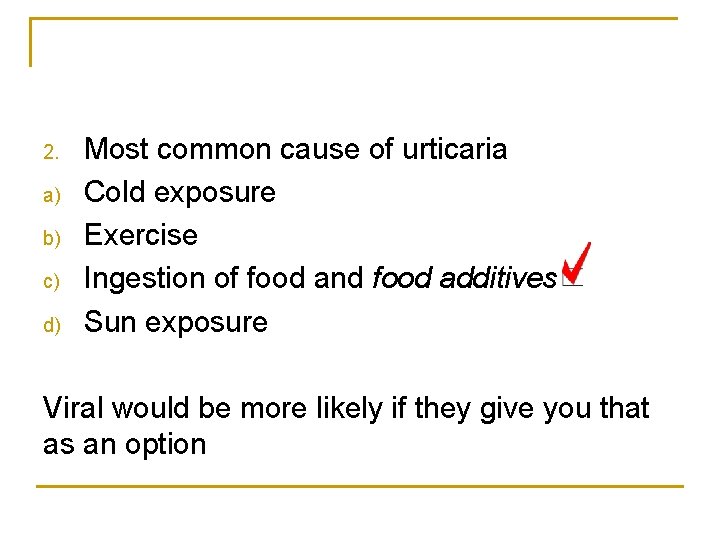
2. a) b) c) d) Most common cause of urticaria Cold exposure Exercise Ingestion of food and food additives Sun exposure Viral would be more likely if they give you that as an option
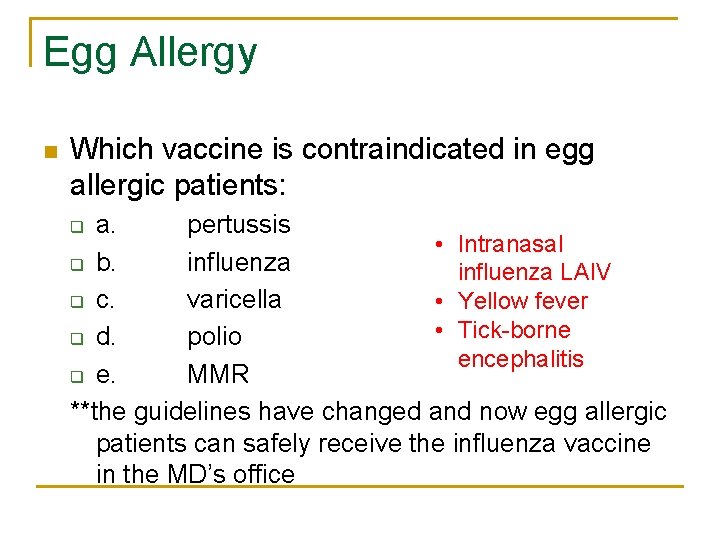
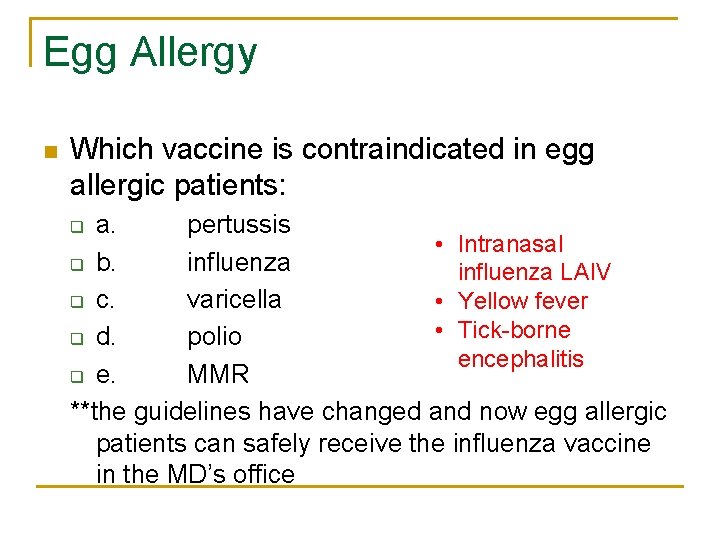
Egg Allergy n Which vaccine is contraindicated in egg allergic patients: a. pertussis • Intranasal q b. influenza LAIV q c. varicella • Yellow fever • Tick-borne q d. polio encephalitis q e. MMR **the guidelines have changed and now egg allergic patients can safely receive the influenza vaccine in the MD’s office q
Milk Allergy n Confirmation of milk intolerance: q q q A) B) C) D) E) D-xylose Jejunal biopsy milk rast test serum Ig. E Milk challenge
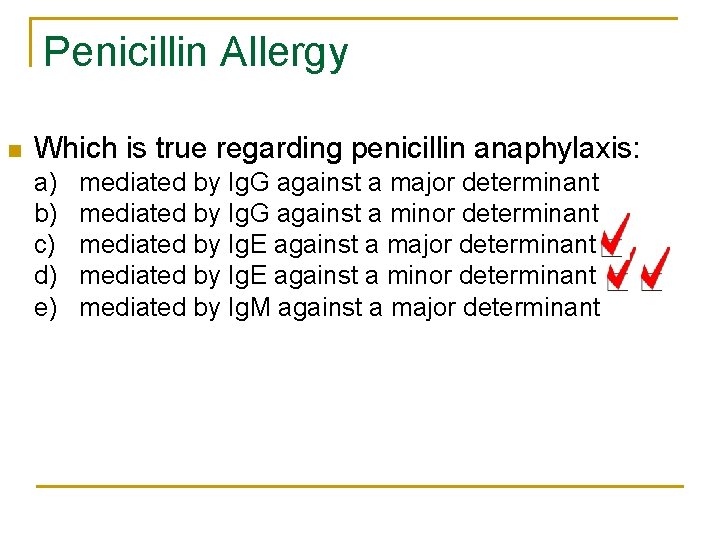
Penicillin Allergy n Which is true regarding penicillin anaphylaxis: a) b) c) d) e) mediated by Ig. G against a major determinant mediated by Ig. G against a minor determinant mediated by Ig. E against a major determinant mediated by Ig. E against a minor determinant mediated by Ig. M against a major determinant
Penicillin Allergy n Penicillin anaphylaxis: q q a) Ig. M mediated b) followed by serum sickness c) commonly cross-reacts with cephalosporins d) associated with a morbilliform rash
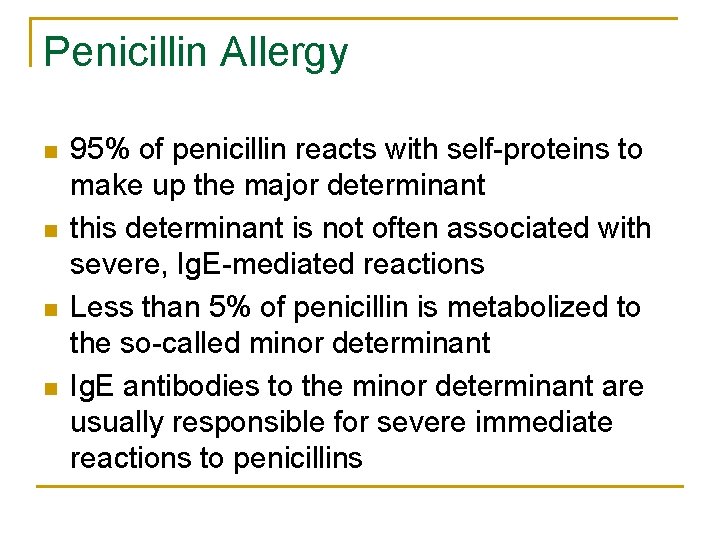
Penicillin Allergy n n 95% of penicillin reacts with self-proteins to make up the major determinant this determinant is not often associated with severe, Ig. E-mediated reactions Less than 5% of penicillin is metabolized to the so-called minor determinant Ig. E antibodies to the minor determinant are usually responsible for severe immediate reactions to penicillins
Allergic Rhinitis – SAQ n 8 year old boy with a runny nose and itchy eyes in the summertime. q q a. what are three signs on exam which help determine DDx b. what initial treatment would you implement c. Name two advantages of second generation anti-histamines d. What 4 things might you obtain on history
Allergic Rhinitis n Allergic rhinitis in childhood: q q q A) most children present before 2 years of age B) Most children will also develop asthma C) Perennial rhinitis is due to ingested rather than inhaled allergens D) Mold is not an etiologic agent E) In most cases, symptoms persist
Allergic Rhinitis n Which is true regarding allergic rhinitis: q q q A) Indoor mould is not a trigger B) long term follow-up shows that symptoms persist into adulthood C) these children go on to develop asthma D) ingested substances are more significant than inhaled substances in perennial rhinitis E) it always starts less than 5 years of age
Allergic Rhinitis n n n Boys > girls 80% develop symptoms prior to age 20 years 20% of children develop symptoms prior to age 2 Risk increases with age and positive skin tests Perennial rhinitis - molds, dust mite, animal dander, cockroach
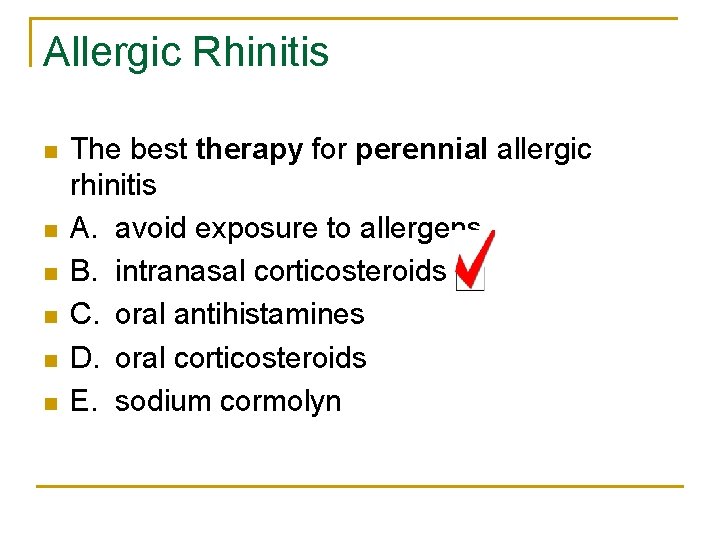
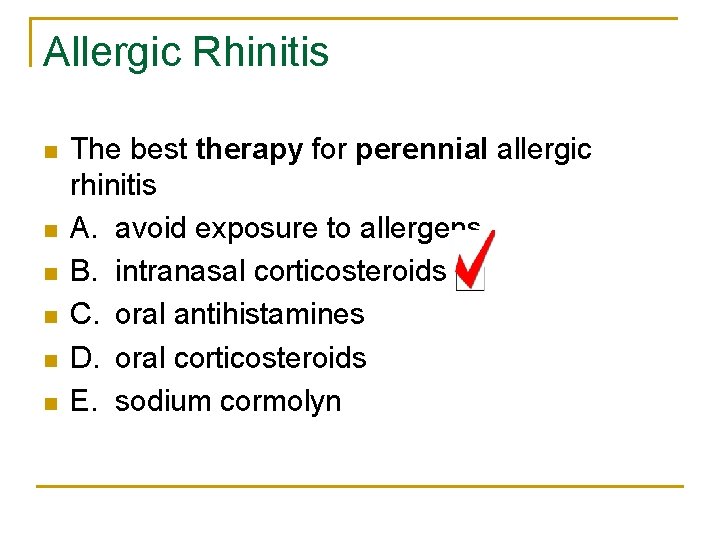
Allergic Rhinitis n n n The best therapy for perennial allergic rhinitis A. avoid exposure to allergens B. intranasal corticosteroids C. oral antihistamines D. oral corticosteroids E. sodium cormolyn
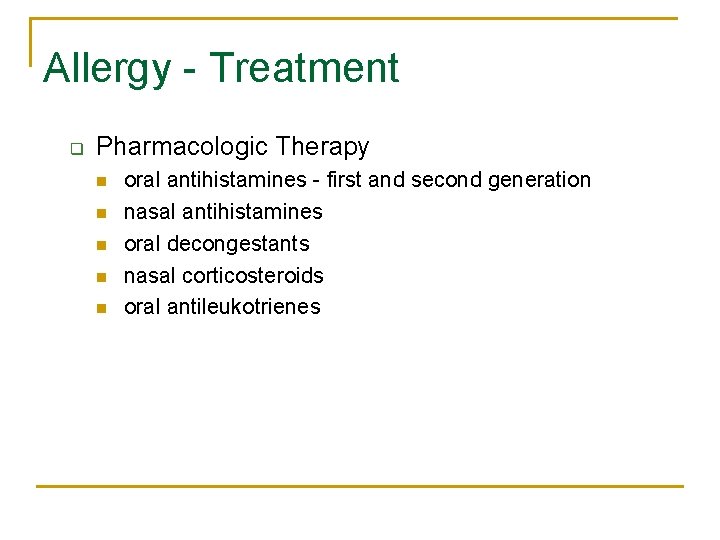
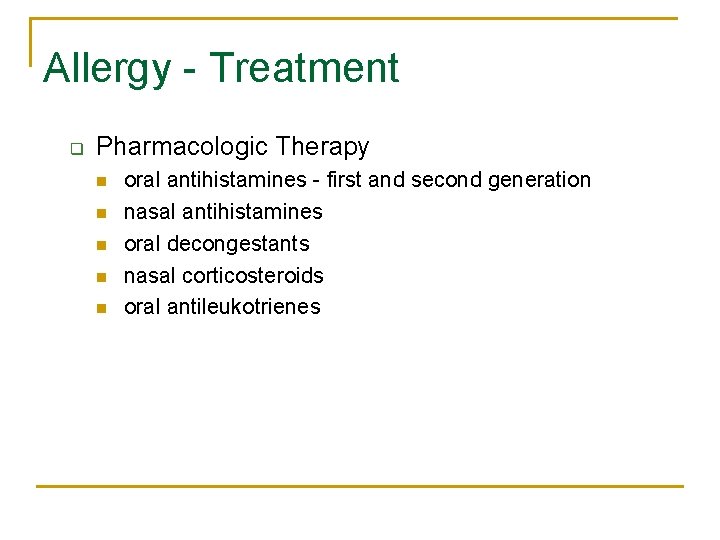
Allergy - Treatment q Pharmacologic Therapy n n n oral antihistamines - first and second generation nasal antihistamines oral decongestants nasal corticosteroids oral antileukotrienes
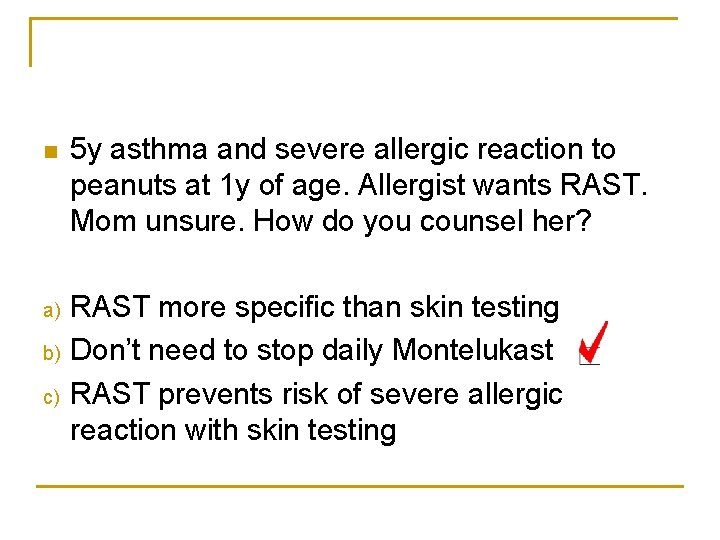
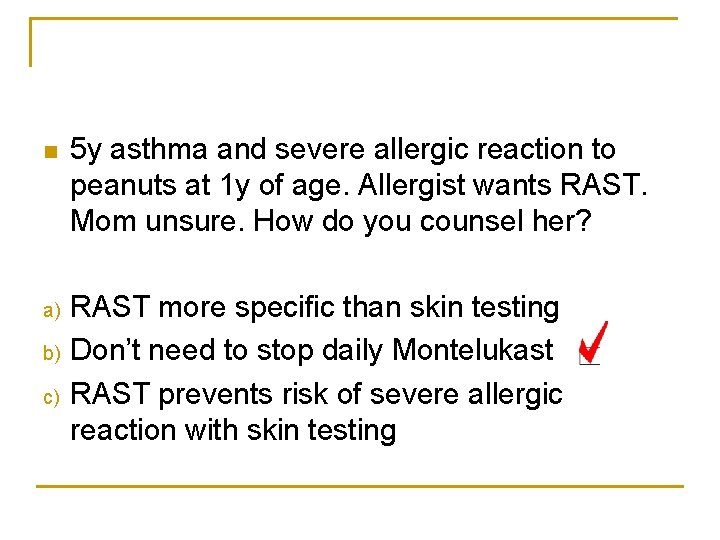
n 5 y asthma and severe allergic reaction to peanuts at 1 y of age. Allergist wants RAST. Mom unsure. How do you counsel her? a) RAST more specific than skin testing Don’t need to stop daily Montelukast RAST prevents risk of severe allergic reaction with skin testing b) c)
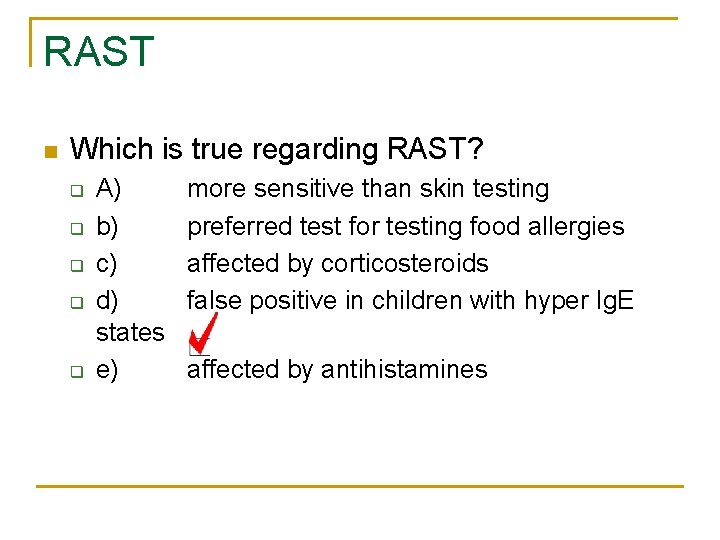
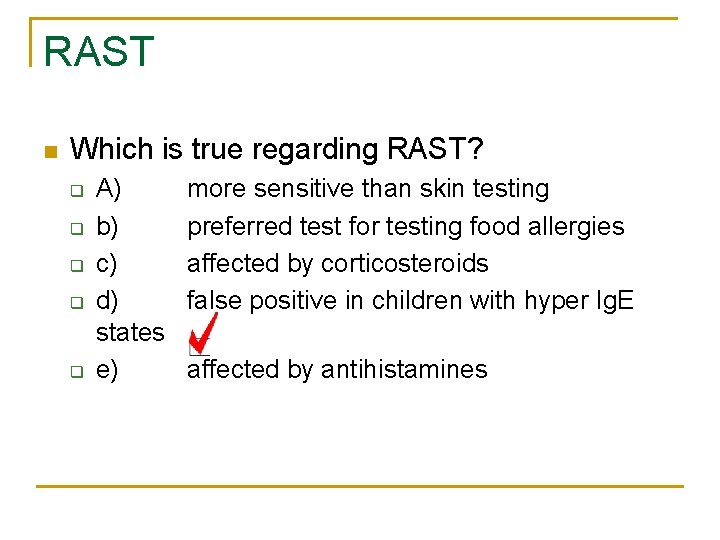
RAST n Which is true regarding RAST? q q q A) b) c) d) states e) more sensitive than skin testing preferred test for testing food allergies affected by corticosteroids false positive in children with hyper Ig. E affected by antihistamines
RAST n Radioallergosorbent Test q q q in vitro test looking at specific Ig. E to specific allergens high negative predictive value positive predictive value low SPT more sensitive may be some efficacy when SPT not practical Not affected by medications, (except maybe Omalizumab)
Immunotherapy n Which can be treated with immunotherapy? q q q A) b) c) d) e) Food allergy bee sting allergy penicillin allergy atopic dermatitis cholinergic urticaria
Allergen immunotherapy n Indications for SCIT: 1. 2. 3. 4. Allergic rhinitis, with or w/o allergic conjunctivitis Allergic asthma Atopic dermatitis if sensitized to inhalant allergens Anaphylaxis to venom (stinging insects) Indications for SLIT: n 1. Allergic rhinitis: grass, ragweed, dust mites
Allergen immunotherapy n OIT: q q n Not yet approved for food allergy. Not safe yet. Being tried for milk, egg, fish, peanut Epicutaneous: q q Research at this point Peanut
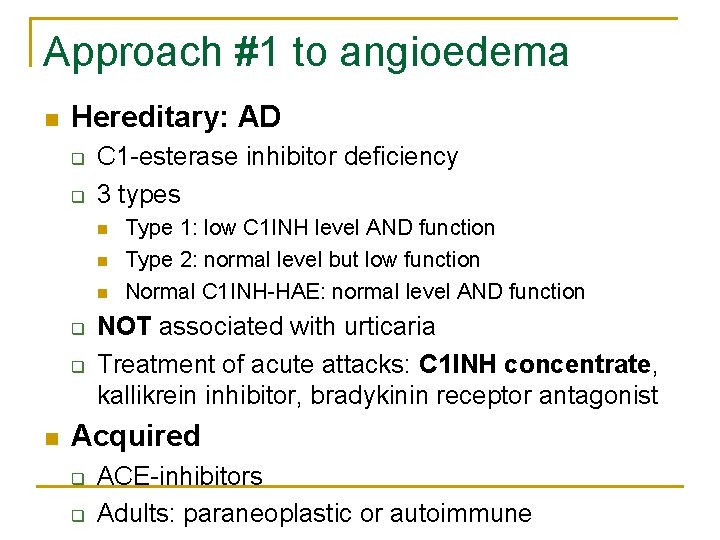
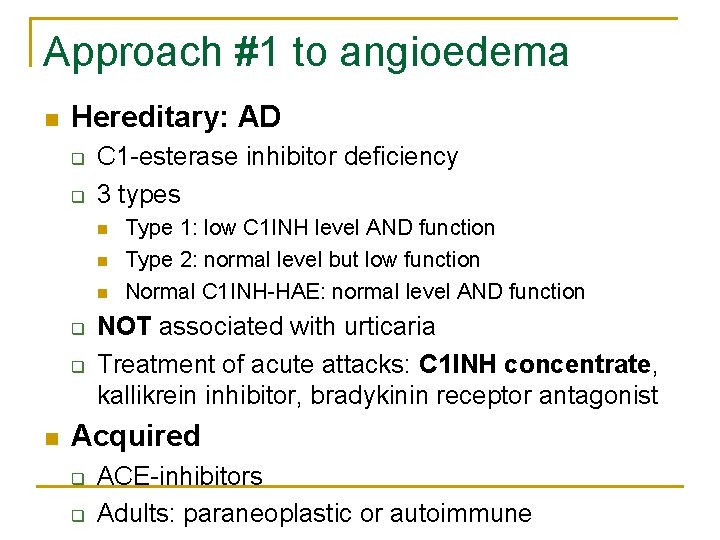
Approach #1 to angioedema n Hereditary: AD q q C 1 -esterase inhibitor deficiency 3 types n n n q q n Type 1: low C 1 INH level AND function Type 2: normal level but low function Normal C 1 INH-HAE: normal level AND function NOT associated with urticaria Treatment of acute attacks: C 1 INH concentrate, kallikrein inhibitor, bradykinin receptor antagonist Acquired q q ACE-inhibitors Adults: paraneoplastic or autoimmune


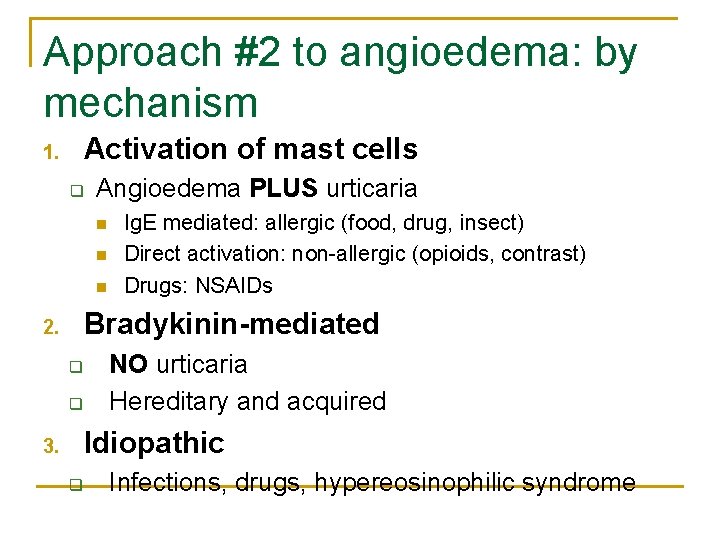
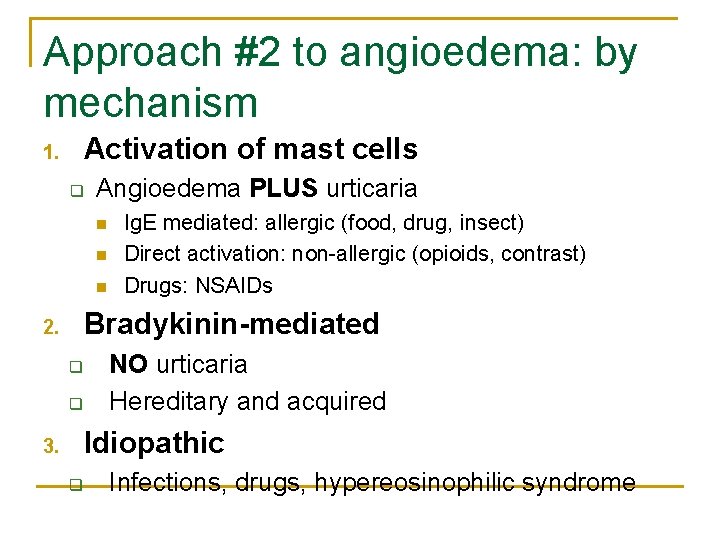
Approach #2 to angioedema: by mechanism Activation of mast cells 1. q Angioedema PLUS urticaria n n n Ig. E mediated: allergic (food, drug, insect) Direct activation: non-allergic (opioids, contrast) Drugs: NSAIDs Bradykinin-mediated 2. q q NO urticaria Hereditary and acquired Idiopathic 3. q Infections, drugs, hypereosinophilic syndrome
THE END n ANY MORE QUESTIONS? n Feel free to contact me: luis. murguiafavela@ahs. ca n YOU WILL PASS!
 American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Family medicine shelf percentiles
Family medicine shelf percentiles Central tolerance and peripheral tolerance
Central tolerance and peripheral tolerance Assisting in microbiology and immunology
Assisting in microbiology and immunology Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology History of immunology
History of immunology Antigen antibody
Antigen antibody Elsever
Elsever 17 tc
17 tc Abbas basic immunology
Abbas basic immunology Abbas basic immunology
Abbas basic immunology Diploma in immunology
Diploma in immunology Pcams immunology
Pcams immunology Nature reviews immunology
Nature reviews immunology Ras
Ras Esol unina
Esol unina Molecular immunology ppt
Molecular immunology ppt Trends in education
Trends in education Nature reviews immunology
Nature reviews immunology Pals immunology
Pals immunology Kuby immunology
Kuby immunology Tumor immunology
Tumor immunology Nature reviews immunology
Nature reviews immunology Avidity in immunology
Avidity in immunology Hematopoiesis wikipedia
Hematopoiesis wikipedia Ucsd immunology course
Ucsd immunology course Bmc immunology impact factor
Bmc immunology impact factor Servier medical art immunology
Servier medical art immunology Shellfish allergy and chloraprep
Shellfish allergy and chloraprep Pediatric medication administration guidelines
Pediatric medication administration guidelines Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics The allergy guy
The allergy guy Latex in outlook
Latex in outlook Latex fruit allergy
Latex fruit allergy Allergy wise
Allergy wise Weights of the backpacks of first graders on a school bus
Weights of the backpacks of first graders on a school bus Latex fruit syndrome
Latex fruit syndrome Macaulay allergy
Macaulay allergy Loratadine pregnancy category
Loratadine pregnancy category Blue boggy nasal turbinates
Blue boggy nasal turbinates Allergy shiners
Allergy shiners Allergy
Allergy Allergy
Allergy Allergy
Allergy Allergic reaction icd 9 code
Allergic reaction icd 9 code Allergy rates
Allergy rates Rhinitis allergy
Rhinitis allergy Allergy board review course
Allergy board review course Rhinitis allergy
Rhinitis allergy Allergy
Allergy Acr contrast reaction
Acr contrast reaction Anaphylaxis vs anaphylactoid
Anaphylaxis vs anaphylactoid Penicillin allergy cme
Penicillin allergy cme World allergy organ j
World allergy organ j Keva allergy care
Keva allergy care Food allergy testing auckland
Food allergy testing auckland Food information for consumers regulation
Food information for consumers regulation Capers allergy
Capers allergy Allergy asthma immunol res impact factor
Allergy asthma immunol res impact factor Pulse grading 2+
Pulse grading 2+ Normal level of vital signs
Normal level of vital signs Types of jaundice
Types of jaundice Elbow restraints for pediatrics
Elbow restraints for pediatrics Costochondritis
Costochondritis Normal vitals
Normal vitals The flacc pain scale
The flacc pain scale General appearance physical exam
General appearance physical exam Modern concept of pediatrics
Modern concept of pediatrics Current concept of pediatric nursing
Current concept of pediatric nursing Chest pain in pediatrics
Chest pain in pediatrics New river valley pediatrics
New river valley pediatrics Trends of pediatric nursing
Trends of pediatric nursing Necrotizing enterocolitis symptoms
Necrotizing enterocolitis symptoms Duke pediatrics durham nc
Duke pediatrics durham nc 11yo
11yo Vancouver clinic pediatrics
Vancouver clinic pediatrics Equipment used in pediatrics
Equipment used in pediatrics Lsu pediatrics residency
Lsu pediatrics residency Himalaya vigorcare benefits
Himalaya vigorcare benefits Nelson pediatrics
Nelson pediatrics Practical approach pediatrics
Practical approach pediatrics Randall neustaedter
Randall neustaedter Fv pediatrics
Fv pediatrics Warm chain in pediatrics
Warm chain in pediatrics Disease xxx
Disease xxx Nelson pediatria bibliografia
Nelson pediatria bibliografia Nelson pediatrics
Nelson pediatrics Albuterol dosis para nebulizar
Albuterol dosis para nebulizar Normal vital signs
Normal vital signs Introduction of pediatrics
Introduction of pediatrics Tlc pediatrics flint
Tlc pediatrics flint Nn pediatrics
Nn pediatrics Mummy restraint in pediatrics
Mummy restraint in pediatrics Carrie tingley pediatrics
Carrie tingley pediatrics Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Returpilarna
Returpilarna Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Personlig tidbok för yrkesförare
Personlig tidbok för yrkesförare Sura för anatom
Sura för anatom Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Debattartikel struktur
Debattartikel struktur