1 Immune Regulation Tolerance and Autoimmunity Mark S
- Slides: 38
1 Immune Regulation, Tolerance, and Autoimmunity Mark S. Anderson, MD, Ph. D UCSF
2 Disclosures • Research support from Juno Therapeutics • Consultant for Sanofi
3 Lecture outline • Principles of immune regulation • Self-tolerance; mechanisms of central and peripheral tolerance • Inhibitory receptors of T cells • Treg’s and IL-2
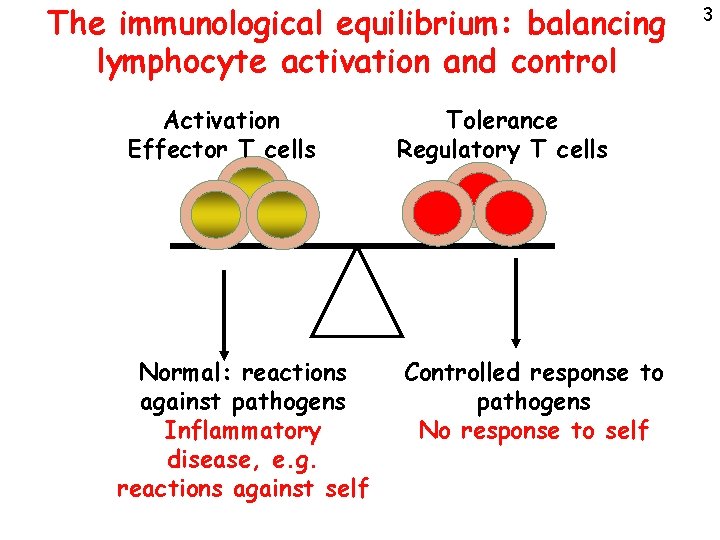
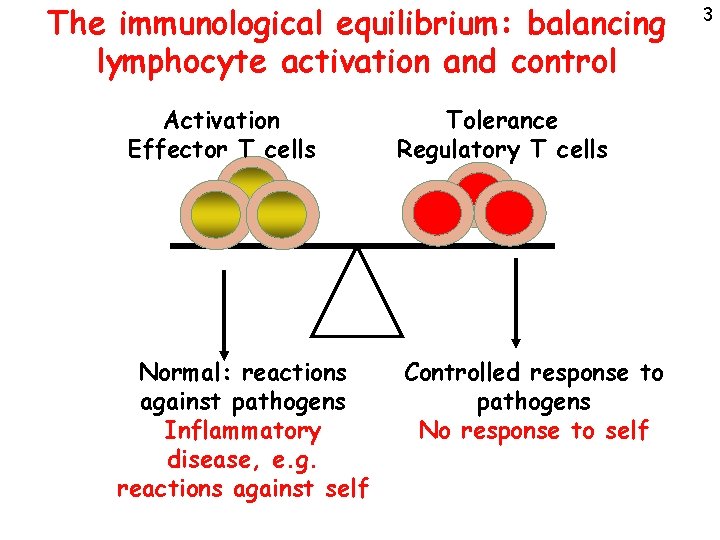
The immunological equilibrium: balancing lymphocyte activation and control Activation Effector T cells Normal: reactions against pathogens Inflammatory disease, e. g. reactions against self Tolerance Regulatory T cells Controlled response to pathogens No response to self 3
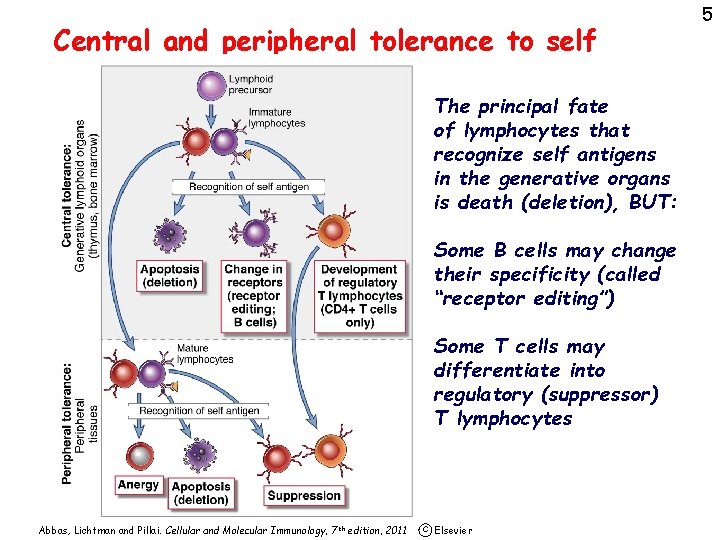
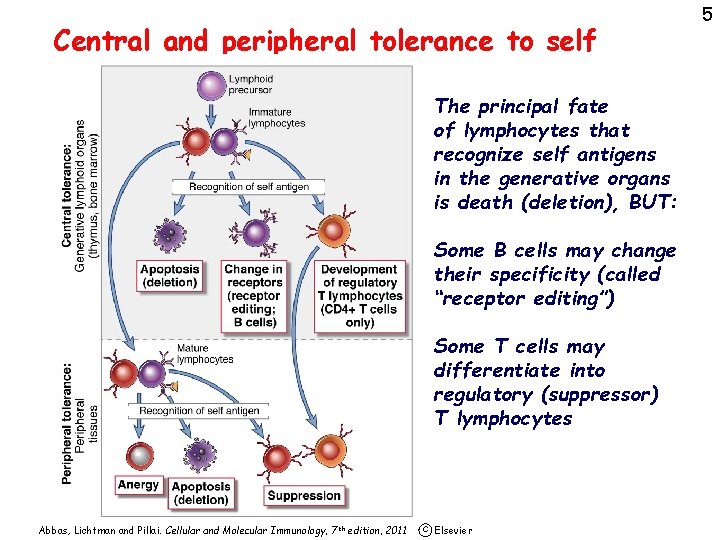
Central and peripheral tolerance to self The principal fate of lymphocytes that recognize self antigens in the generative organs is death (deletion), BUT: Some B cells may change their specificity (called “receptor editing”) Some T cells may differentiate into regulatory (suppressor) T lymphocytes Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 7 th edition, 2011 c Elsevier 5
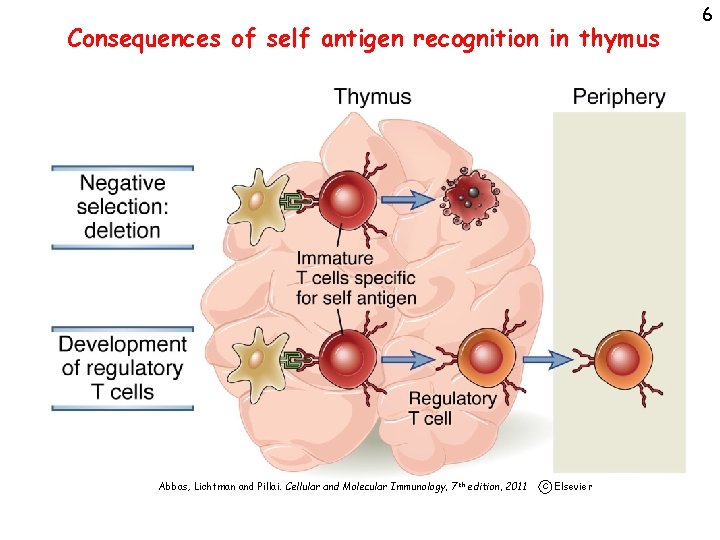
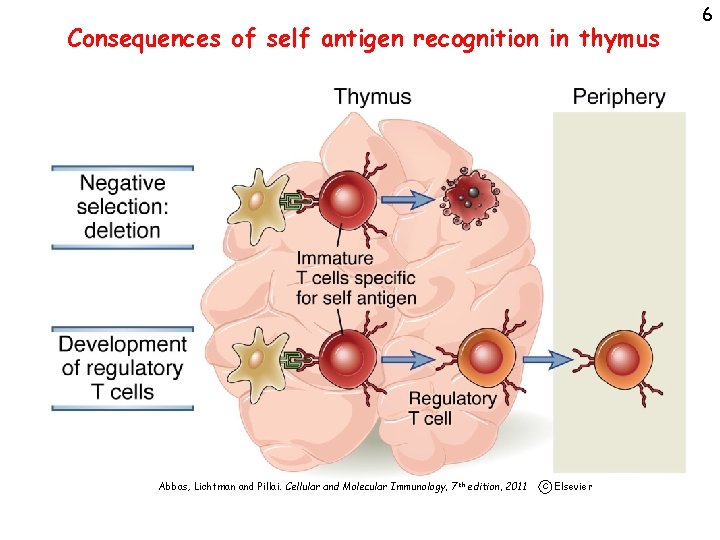
Consequences of self antigen recognition in thymus Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 7 th edition, 2011 c Elsevier 6
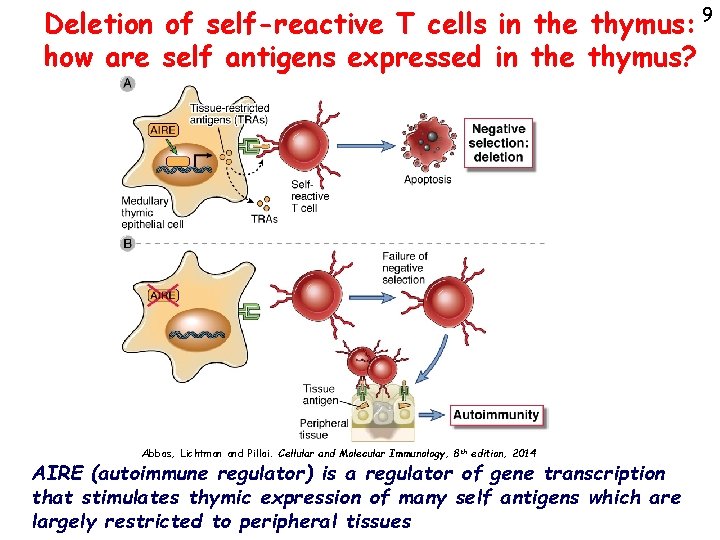
7 What self antigens are seen in the thymus? • Ubiquitous cell-associated and circulating proteins • The thymus has a special mechanism for displaying peripheral tissue antigens in thymic medullary epithelial cells, where they signal self-reactive thymocytes for death
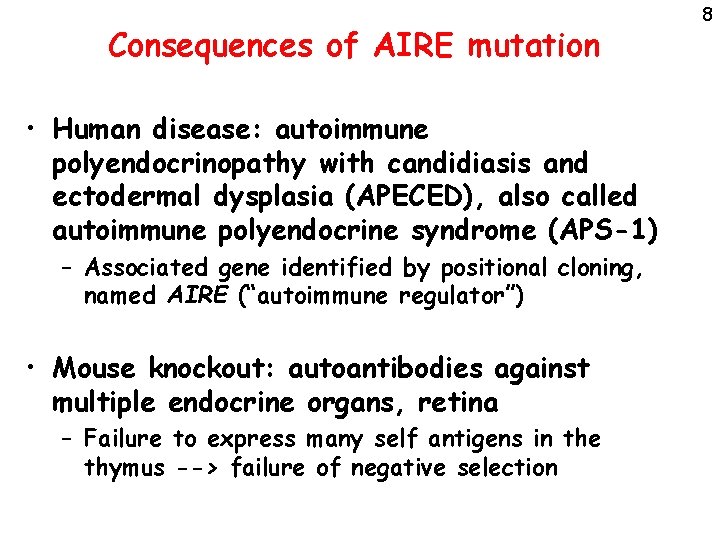
Consequences of AIRE mutation • Human disease: autoimmune polyendocrinopathy with candidiasis and ectodermal dysplasia (APECED), also called autoimmune polyendocrine syndrome (APS-1) – Associated gene identified by positional cloning, named AIRE (“autoimmune regulator”) • Mouse knockout: autoantibodies against multiple endocrine organs, retina – Failure to express many self antigens in the thymus --> failure of negative selection 8
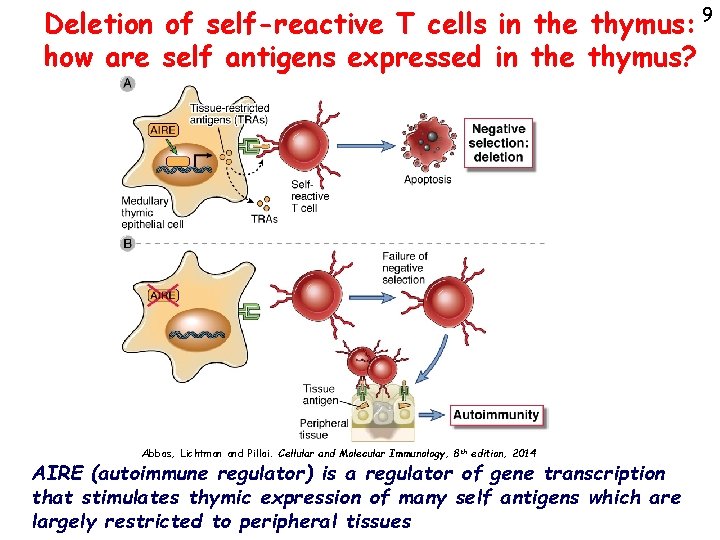
Deletion of self-reactive T cells in the thymus: 9 how are self antigens expressed in the thymus? Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 8 th edition, 2014 AIRE (autoimmune regulator) is a regulator of gene transcription that stimulates thymic expression of many self antigens which are largely restricted to peripheral tissues
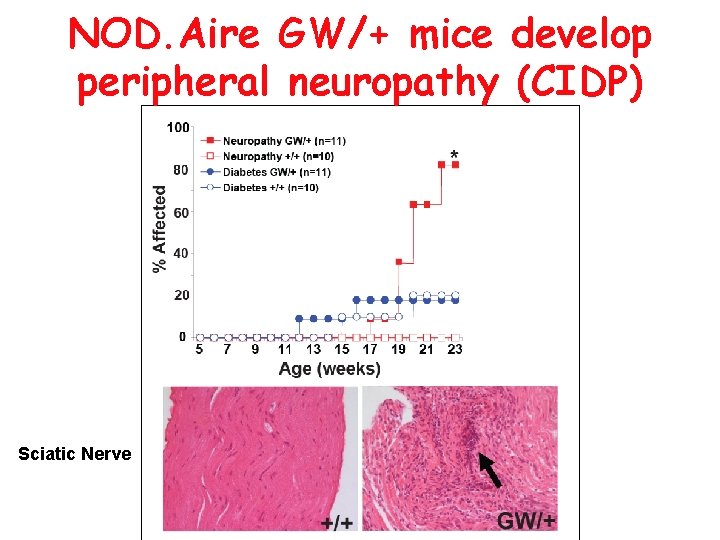
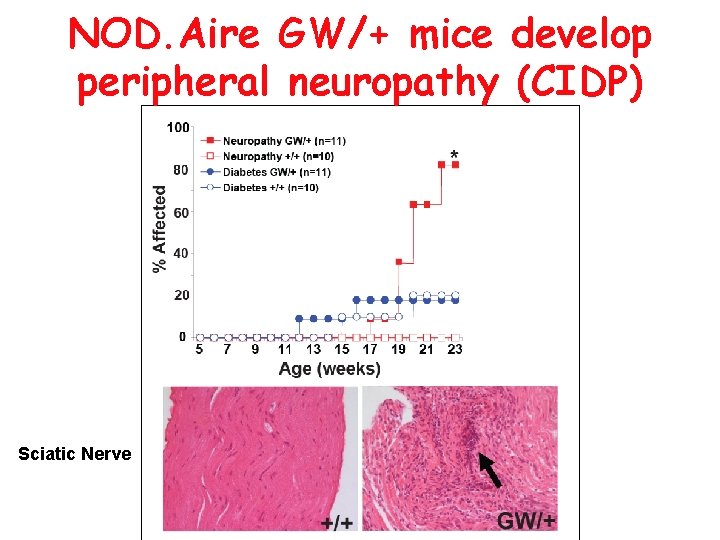
NOD. Aire GW/+ mice develop peripheral neuropathy (CIDP) Sciatic Nerve
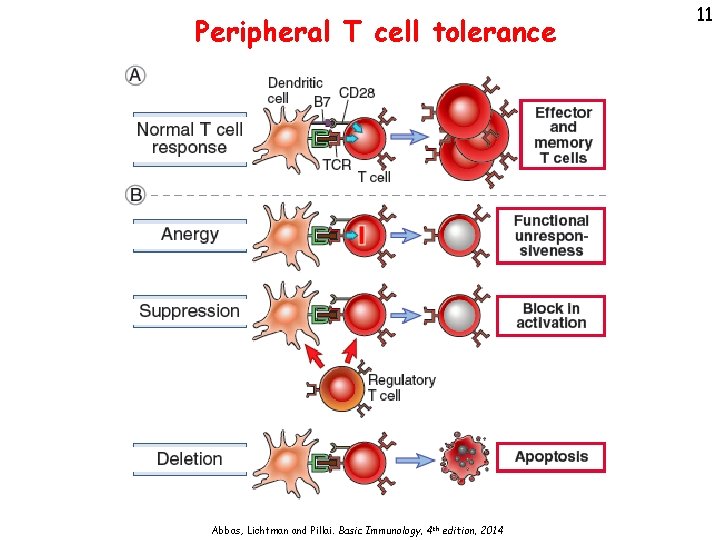
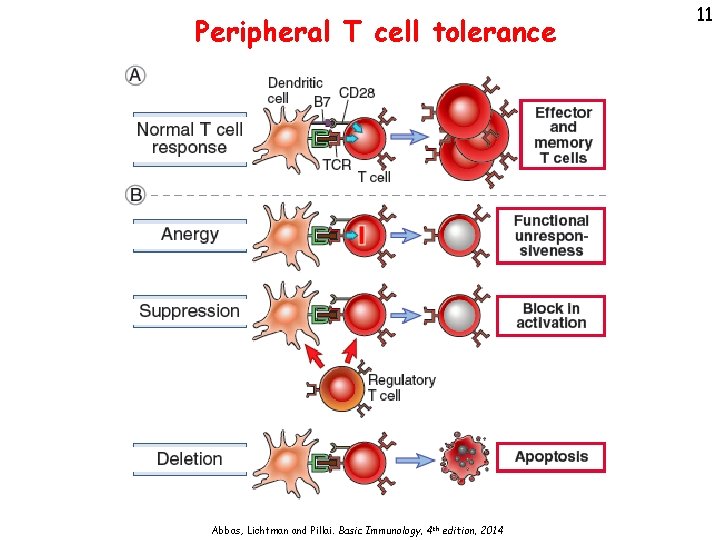
Peripheral T cell tolerance Abbas, Lichtman and Pillai. Basic Immunology, 4 th edition, 2014 11
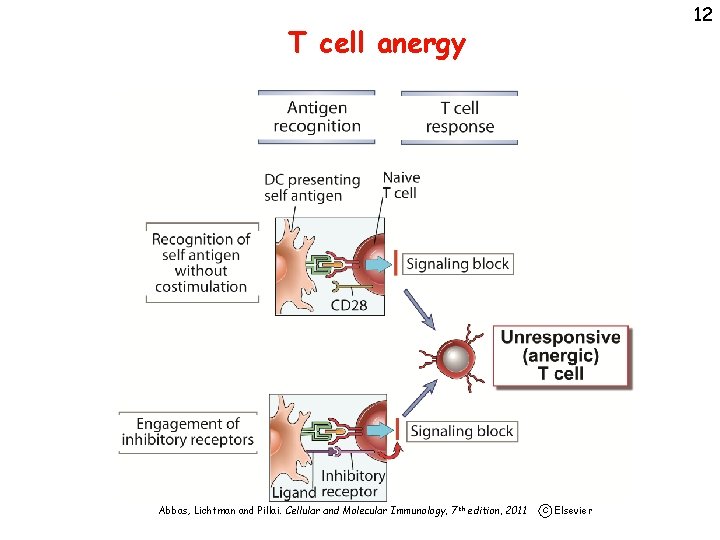
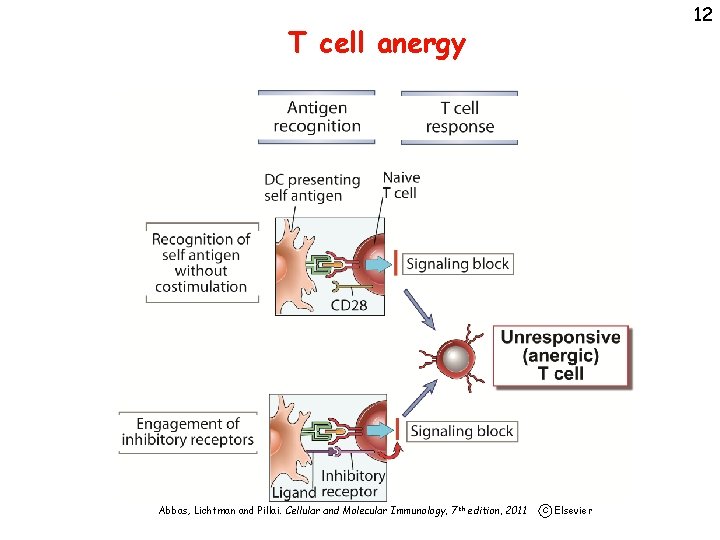
12 T cell anergy Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 7 th edition, 2011 c Elsevier
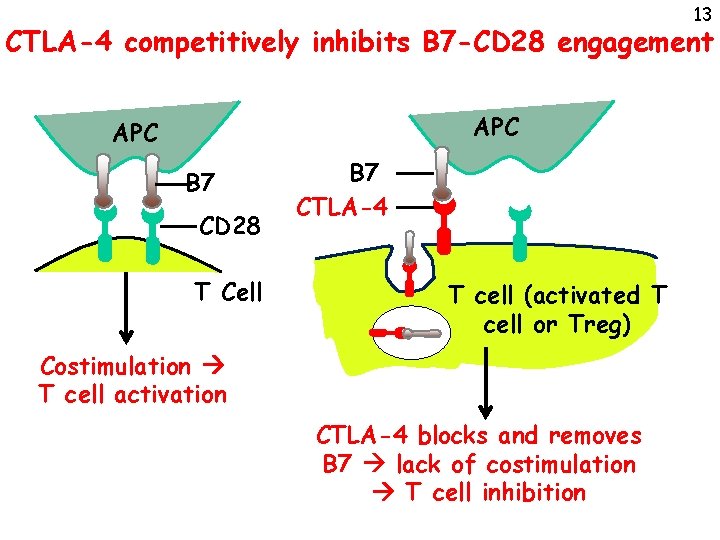
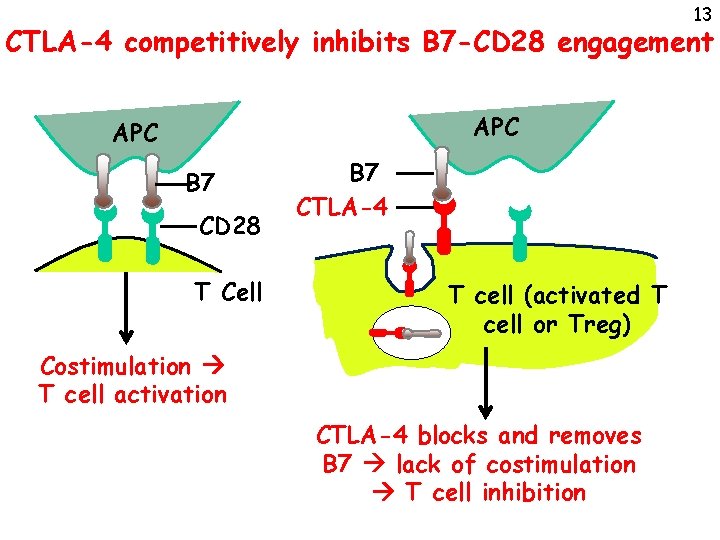
13 CTLA-4 competitively inhibits B 7 -CD 28 engagement APC B 7 CD 28 T Cell B 7 CTLA-4 T cell (activated T cell or Treg) Costimulation T cell activation CTLA-4 blocks and removes B 7 lack of costimulation T cell inhibition
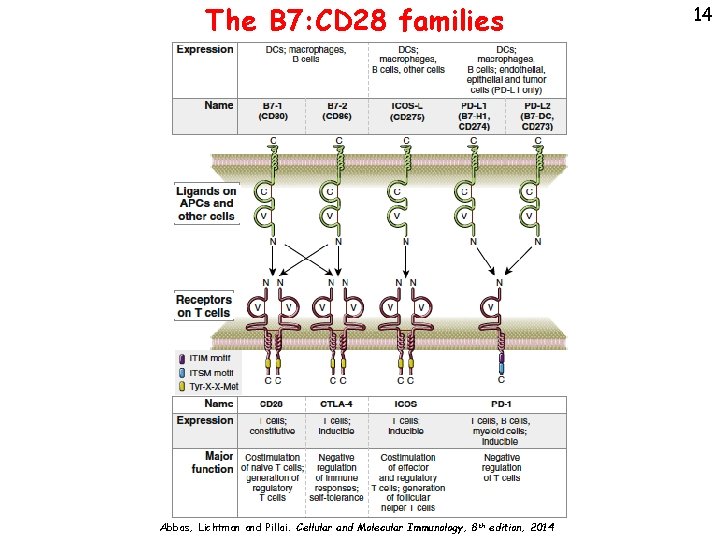
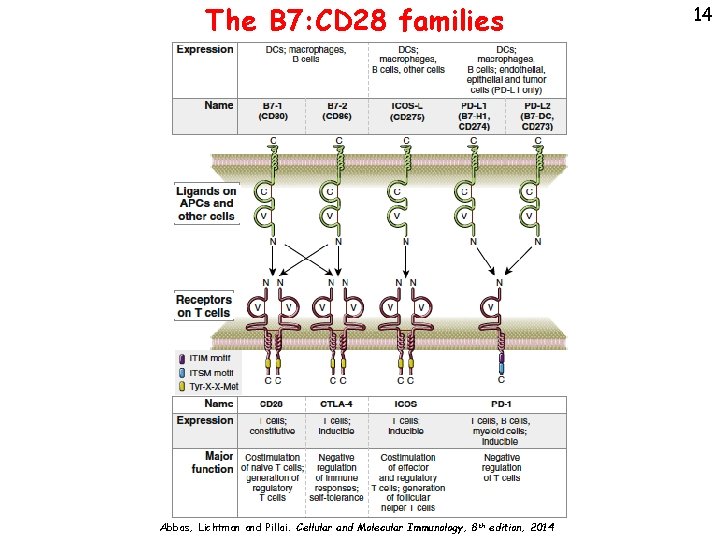
The B 7: CD 28 families Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 8 th edition, 2014 14
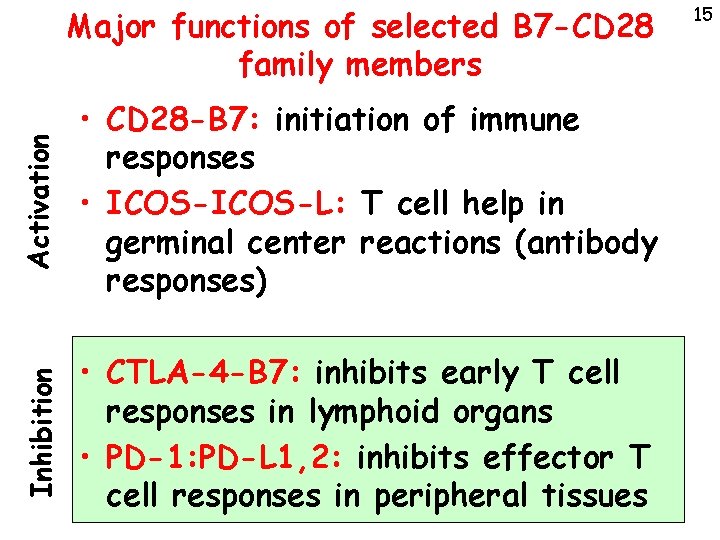
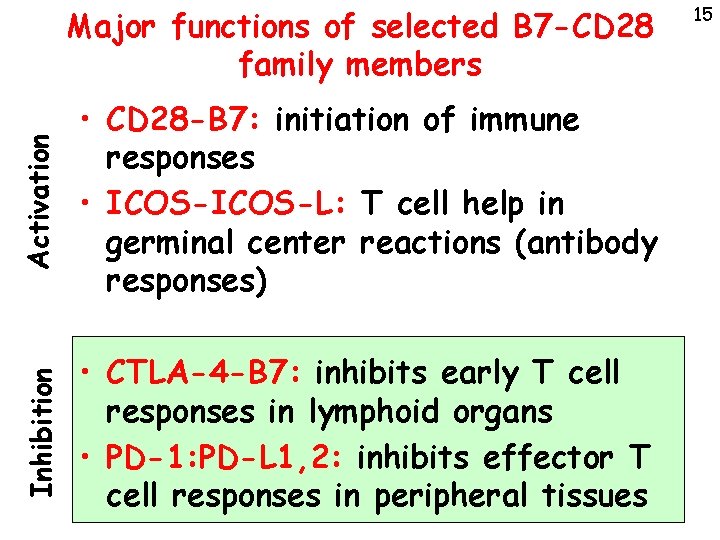
Activation • CD 28 -B 7: initiation of immune responses • ICOS-L: T cell help in germinal center reactions (antibody responses) Inhibition Major functions of selected B 7 -CD 28 family members • CTLA-4 -B 7: inhibits early T cell responses in lymphoid organs • PD-1: PD-L 1, 2: inhibits effector T cell responses in peripheral tissues 15
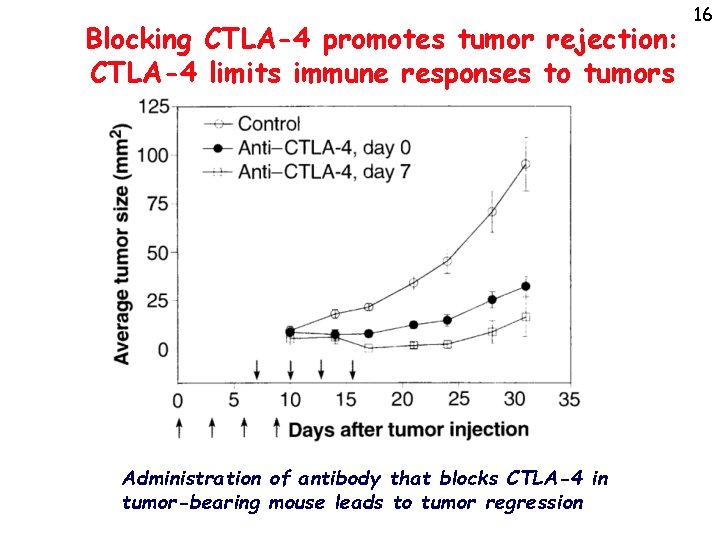
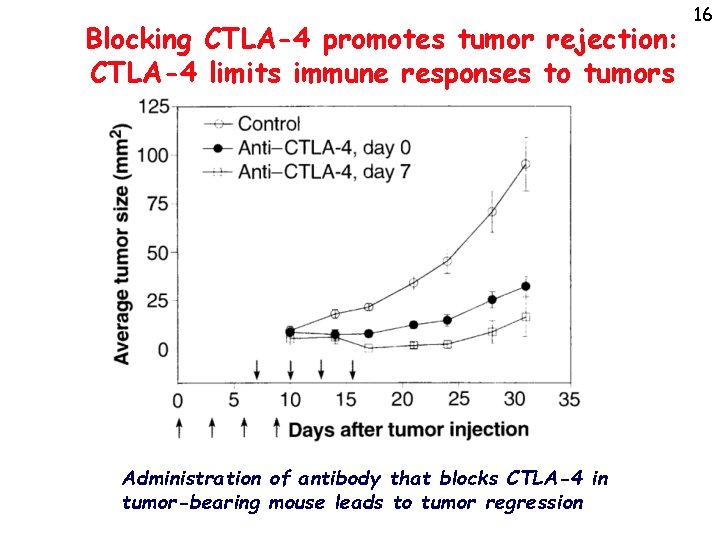
Blocking CTLA-4 promotes tumor rejection: CTLA-4 limits immune responses to tumors Administration of antibody that blocks CTLA-4 in tumor-bearing mouse leads to tumor regression 16
17 The PD-1 inhibitory pathway • PD-1 recognizes two widely expressed ligands (PD-L 1, PD-L 2) • Knockout of PD-1 leads to autoimmune disease (less severe than CTLA-4 -KO) • Role of PD-1 in T cell suppression in chronic infections, tumors?
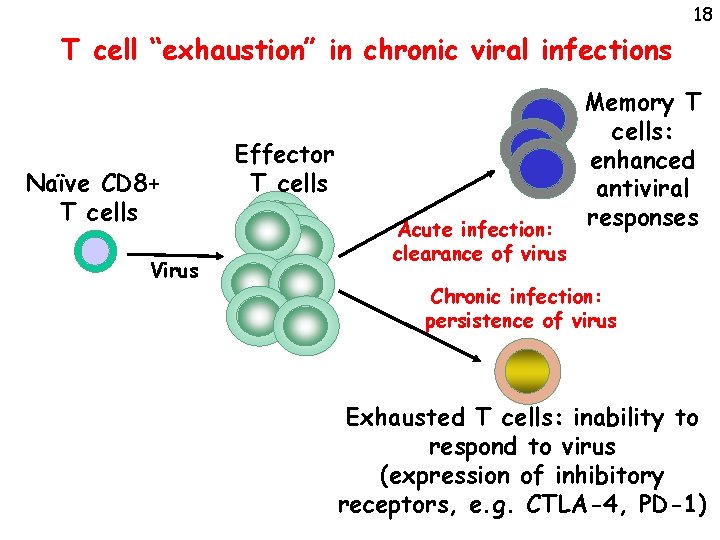
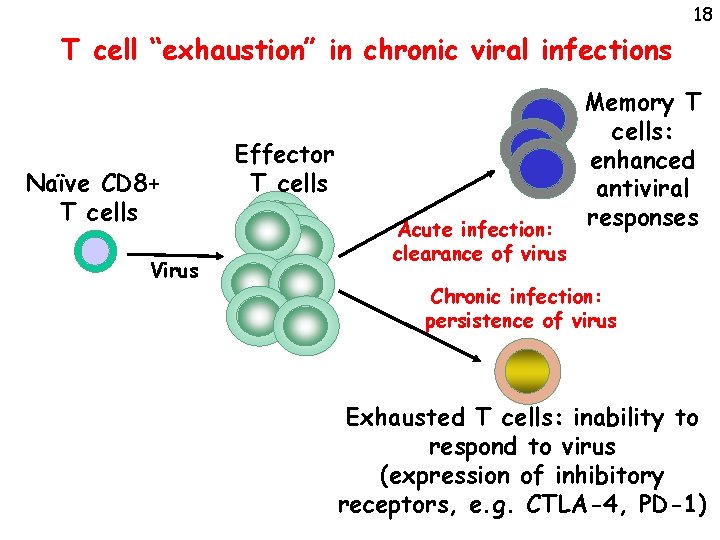
18 T cell “exhaustion” in chronic viral infections Naïve CD 8+ T cells Virus Effector T cells Acute infection: clearance of virus Memory T cells: enhanced antiviral responses Chronic infection: persistence of virus Exhausted T cells: inability to respond to virus (expression of inhibitory receptors, e. g. CTLA-4, PD-1)
19 Actions of PD-1 • PD-1 attenuates TCR signaling in responding T cells • Limits harmful consequences of chronic stimulation with persistent antigen (self, tumors, chronic viral infections) • Greater role in CD 8 than in CD 4 T cells • Also expressed on follicular helper T cells; function?
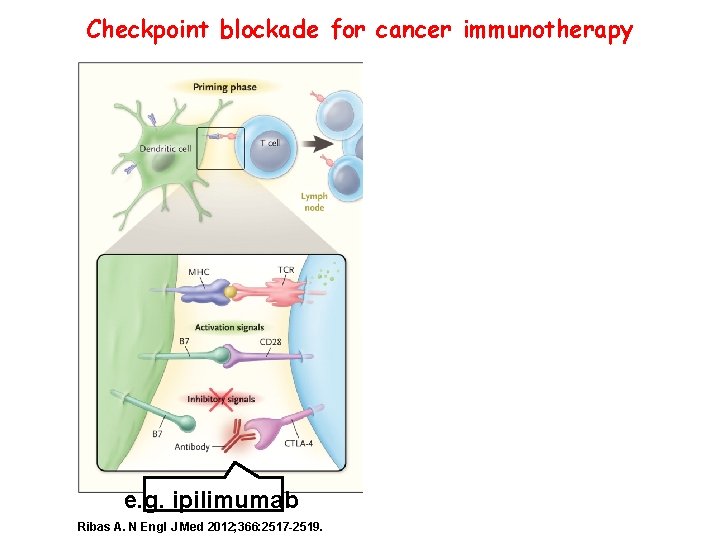
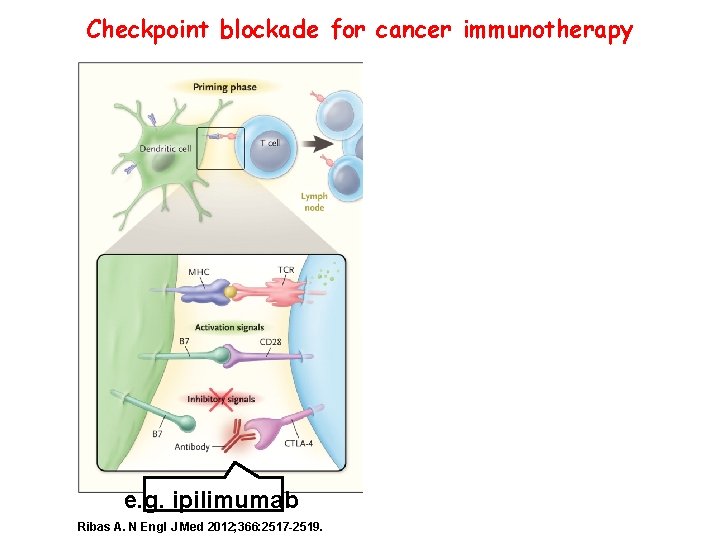
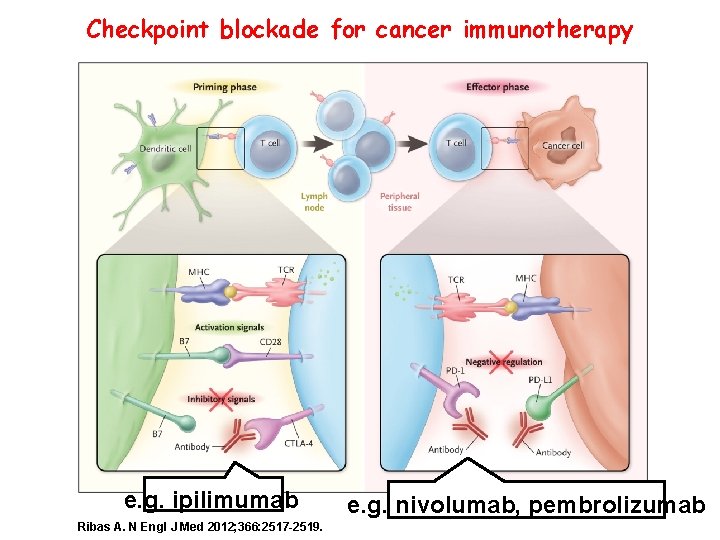
Checkpoint blockade for cancer immunotherapy e. g. ipilimumab Ribas A. N Engl J Med 2012; 366: 2517 -2519.
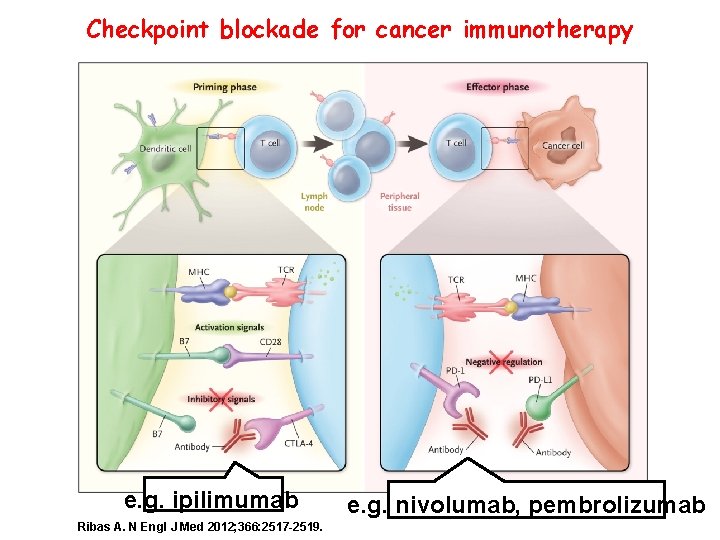
Checkpoint blockade for cancer immunotherapy e. g. ipilimumab Ribas A. N Engl J Med 2012; 366: 2517 -2519. 21 e. g. nivolumab, pembrolizumab
22 Risks of blocking CTLA-4 or PD-1 • Blocking a mechanism of self-tolerance leads to:
23 Risks of blocking CTLA-4 or PD-1 • Blocking a mechanism of self-tolerance leads to: • Autoimmune reactions (a new cottage industry for clinicians? ) – Colitis and dermatitis are common – Vitiligo, Endocrinopathies, hepatitis less common but described – Severity of adverse effects has to be balanced against potential for treating serious cancers – Less severe with anti-PD 1 antibody
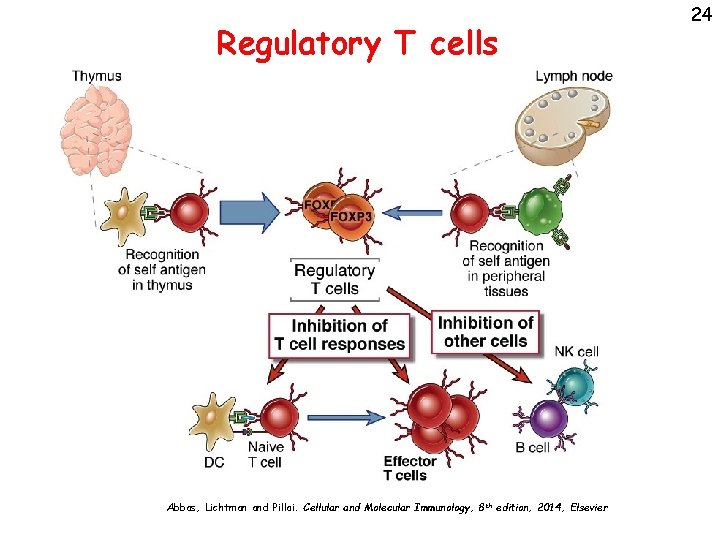
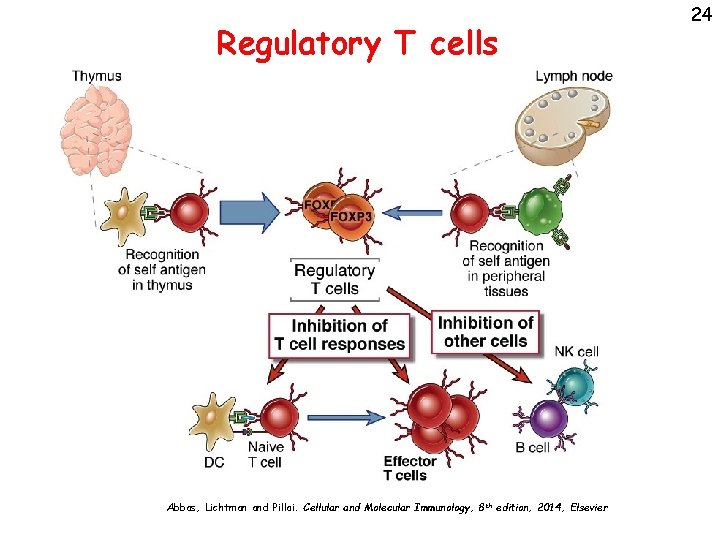
Regulatory T cells Abbas, Lichtman and Pillai. Cellular and Molecular Immunology, 8 th edition, 2014, Elsevier 24
25 Properties of regulatory T cells • Phenotype: CD 4+, high IL-2 receptor (CD 25), low IL-7 receptor, Foxp 3 transcription factor; other markers • Essential features of stable Tregs: – Foxp 3 expression: requires demethylated noncoding CNS 2 sequence in promoter – CD 25 (IL-2 Ra) expression: IL-2 is a necessary survival factor – CTLA-4 expression: required for suppressive function of most Tregs – (Inability to produce IL-2) Take home messages
26 The significance of Foxp 3+ Tregs • Genetic evidence: Foxp 3 mutations --> autoimmune disease (IPEX); in mice, disease can be corrected by providing normal Foxp 3+ cells • Do defects in Foxp 3+ Tregs or resistance to Treg-mediated suppression contribute to common autoimmune diseases? – Inconsistent and variable data
Mechanisms of action of Foxp 3+ Tregs • CTLA-4 on Tregs removes B 7 on APCs, reduces CD 28 engagement and T cell activation – Genetic deletion of CTLA-4 in Foxp 3+ cells results in severe systemic autoimmunity and lymphoproliferation • Inhibitory cytokines produced by Tregs (TGF-b, IL-10, others? ) suppress immune responses (DCs, Macs, T cells) – IL-10 deletion in Foxp 3+ cells results in colitis – IL-10 is also produced by Foxp 3 - cells • Consumption of IL-2 27
28 Regulatory T cells • Explosion of information about the generation, properties, functions and significance of these cells • Will cellular therapy with ex vivo expanded Treg become a reality? • Therapeutic goal: induction or activation of Treg in immune diseases Take home messages
The therapeutic potential of regulatory T lymphocytes • Cell transfer of autologous Tregs to suppress immune responses – Grow up patient’s Tregs ex vivo – Ongoing clinical trials in graft rejection, T 1 D show it is safe – In one study of liver Tx, single infusion of Tregs resulted in tolerance (withdrawal of immunosuppression) in 7/10 patients (vs ~10% historically) 29
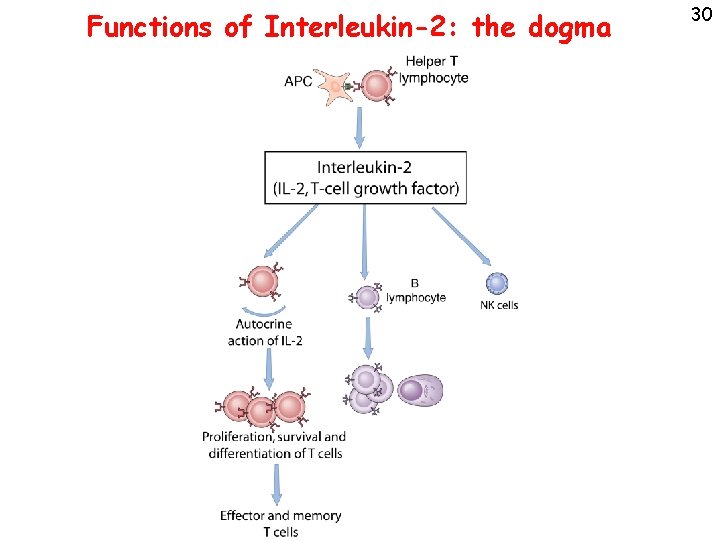
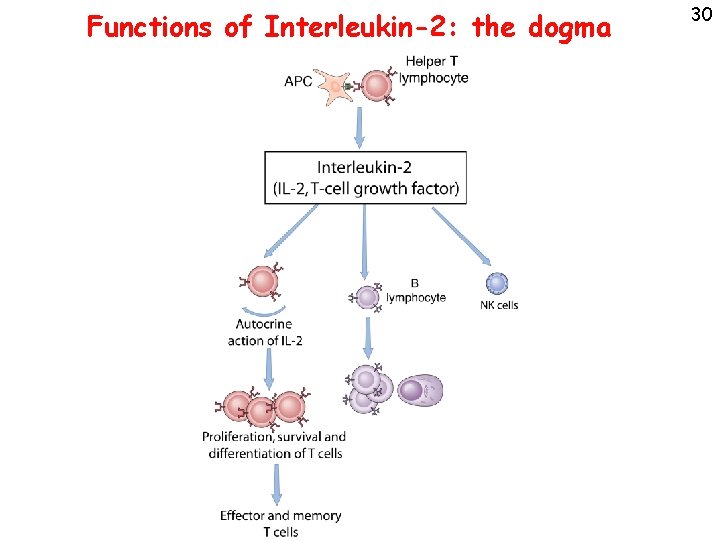
Functions of Interleukin-2: the dogma 30
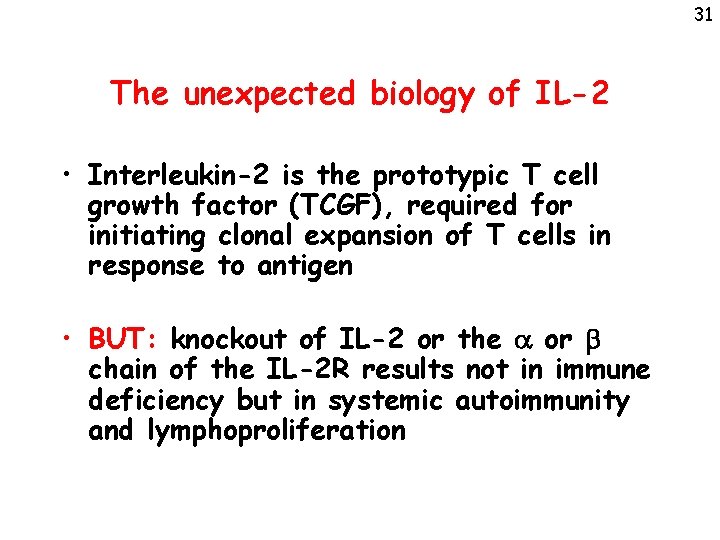
31 The unexpected biology of IL-2 • Interleukin-2 is the prototypic T cell growth factor (TCGF), required for initiating clonal expansion of T cells in response to antigen • BUT: knockout of IL-2 or the a or b chain of the IL-2 R results not in immune deficiency but in systemic autoimmunity and lymphoproliferation
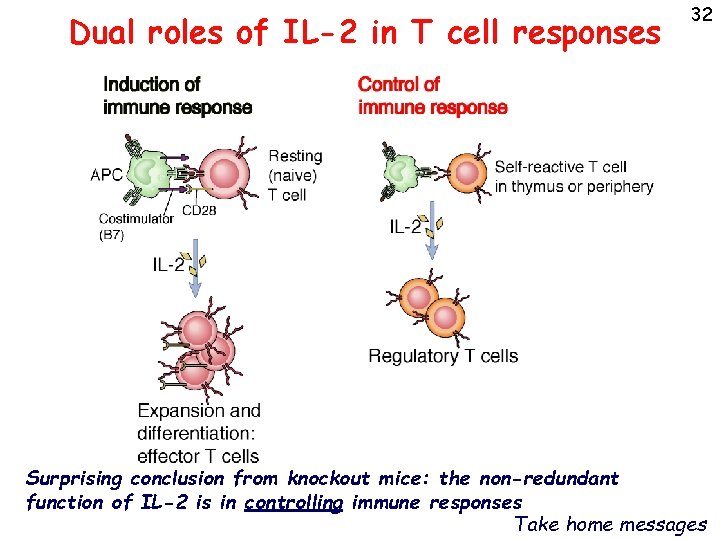
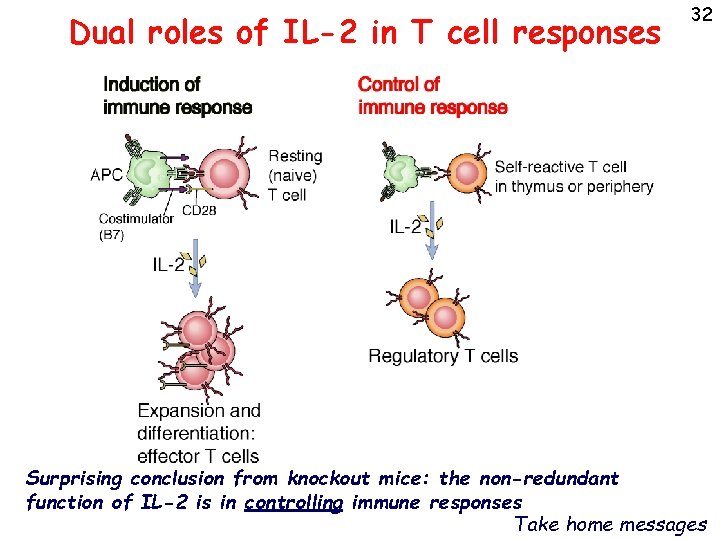
Dual roles of IL-2 in T cell responses 32 Surprising conclusion from knockout mice: the non-redundant function of IL-2 is in controlling immune responses Take home messages
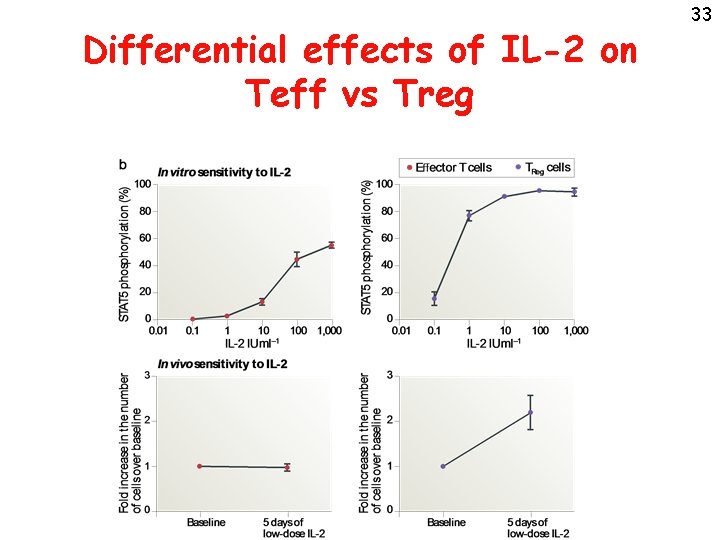
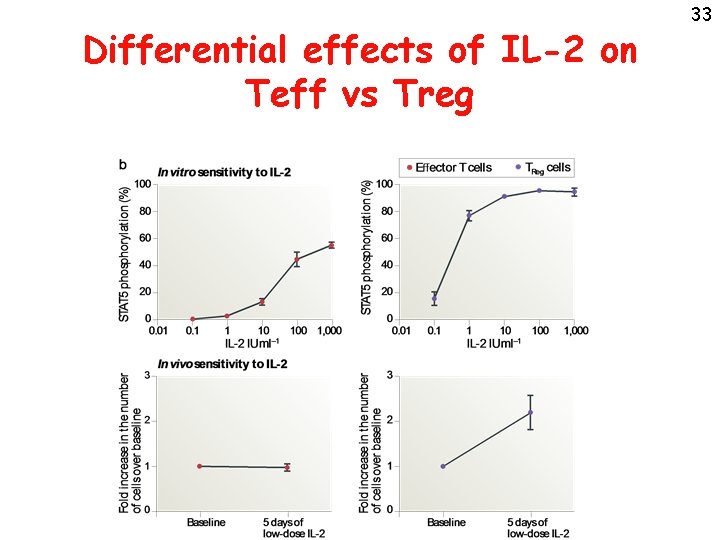
Differential effects of IL-2 on Teff vs Treg 33
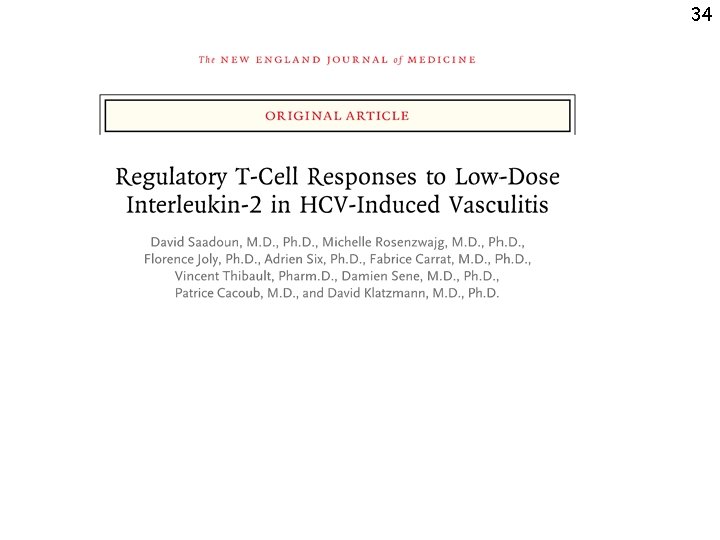
34
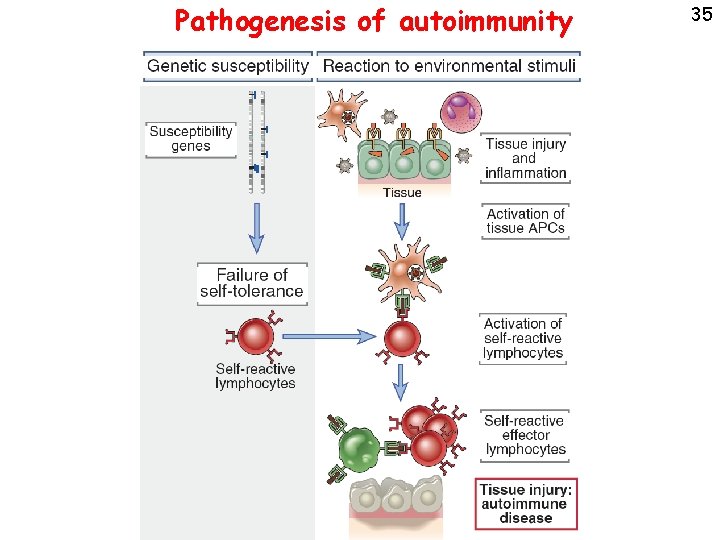
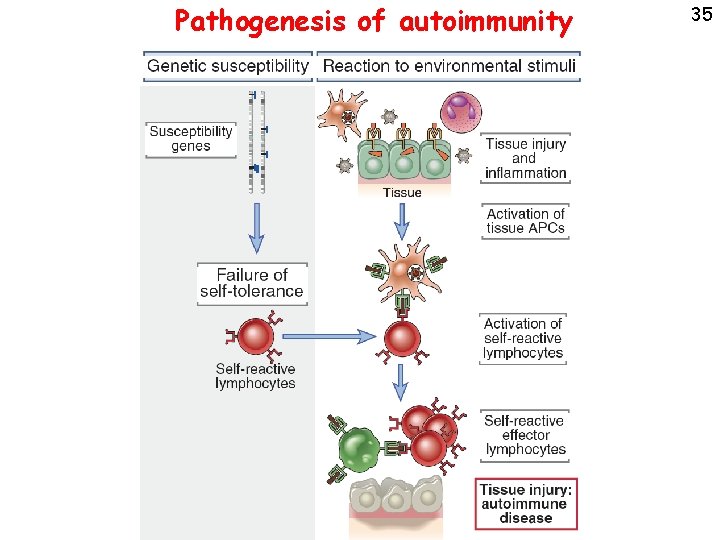
Pathogenesis of autoimmunity 35
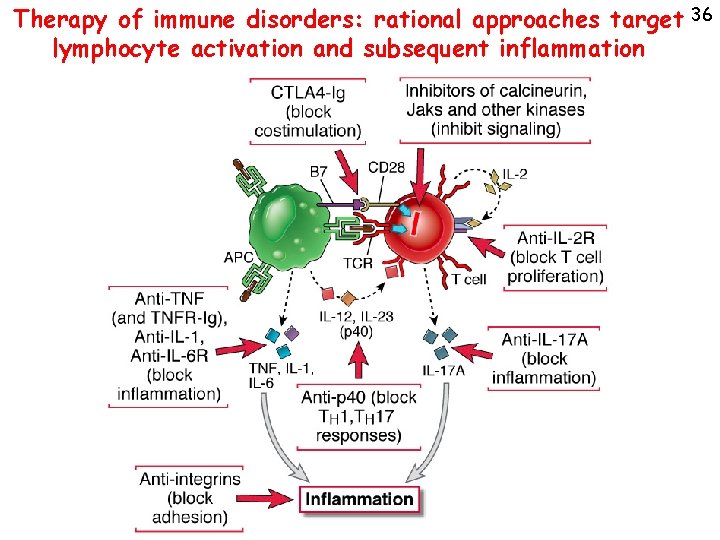
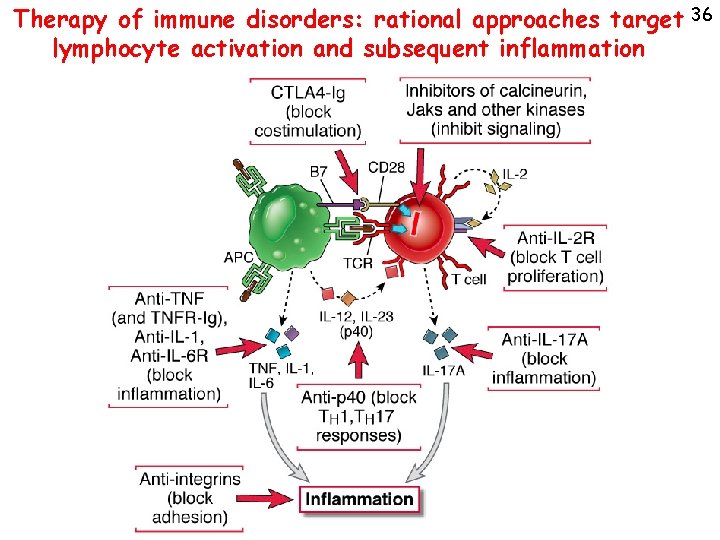
Therapy of immune disorders: rational approaches target 36 lymphocyte activation and subsequent inflammation
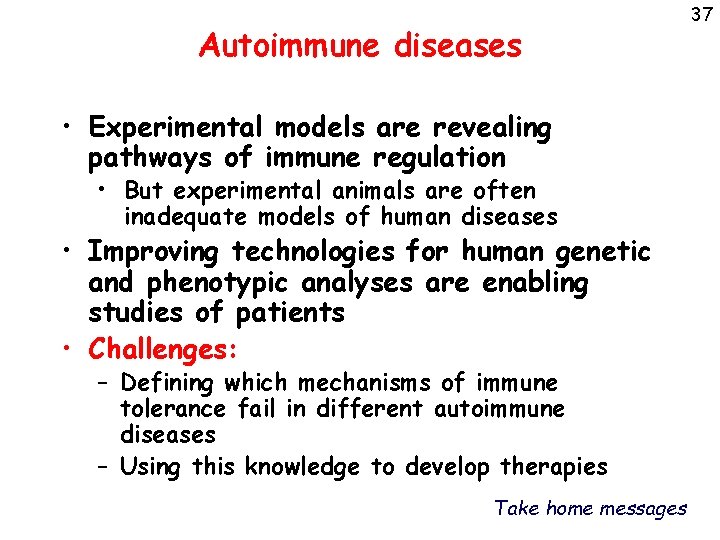
Autoimmune diseases • Experimental models are revealing pathways of immune regulation • But experimental animals are often inadequate models of human diseases • Improving technologies for human genetic and phenotypic analyses are enabling studies of patients • Challenges: – Defining which mechanisms of immune tolerance fail in different autoimmune diseases – Using this knowledge to develop therapies Take home messages 37
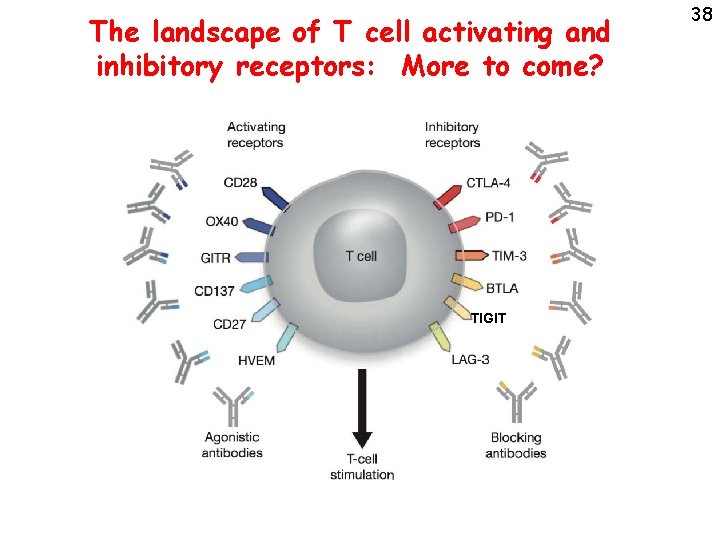
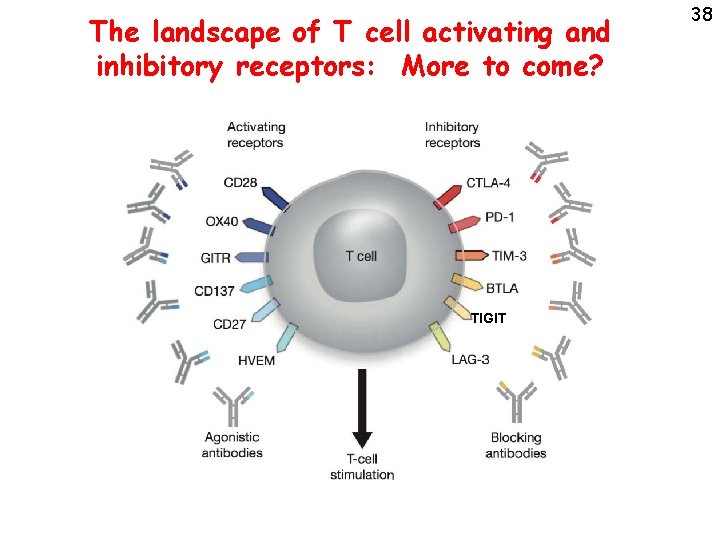
The landscape of T cell activating and inhibitory receptors: More to come? TIGIT 38