Weaning from Mechanical Ventilation Consensus Conference of the


- Slides: 49

Weaning from Mechanical Ventilation Consensus Conference of the ATS, ERS, ESCIM, SCCM and SRLF Budapest 2005 ERJ 2007; 29: 1033 -56 Tobias Welte Dept. of Respiratory Medicine Medizinische Hochschule Hannover Germany
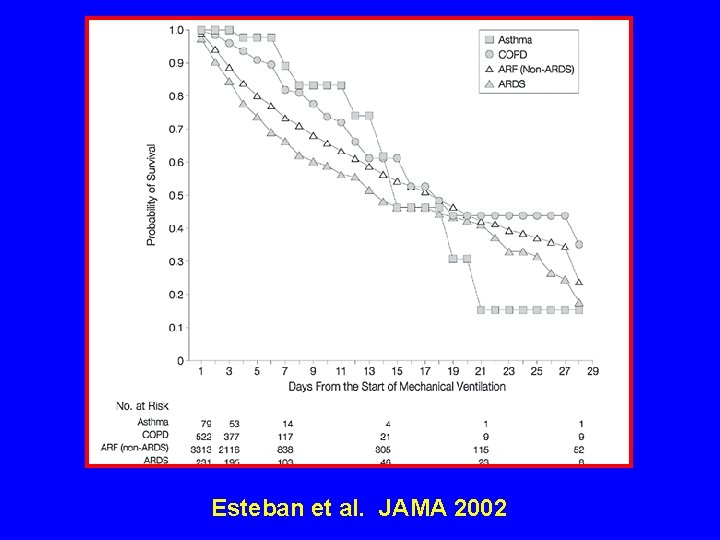
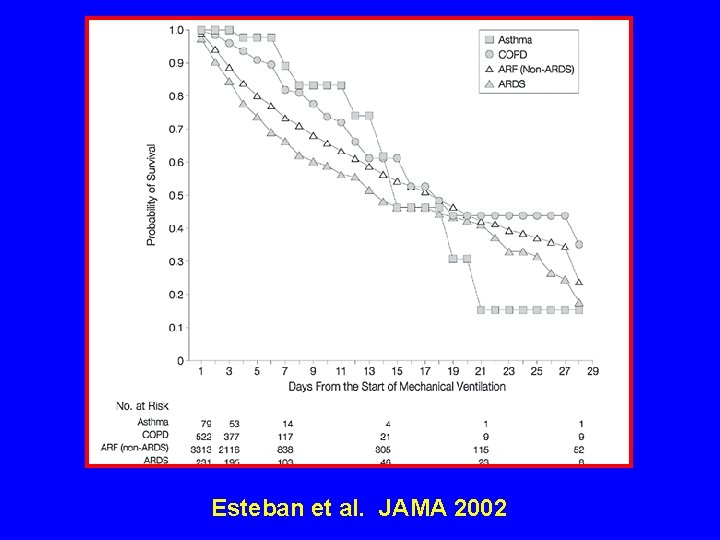
Esteban et al. JAMA 2002
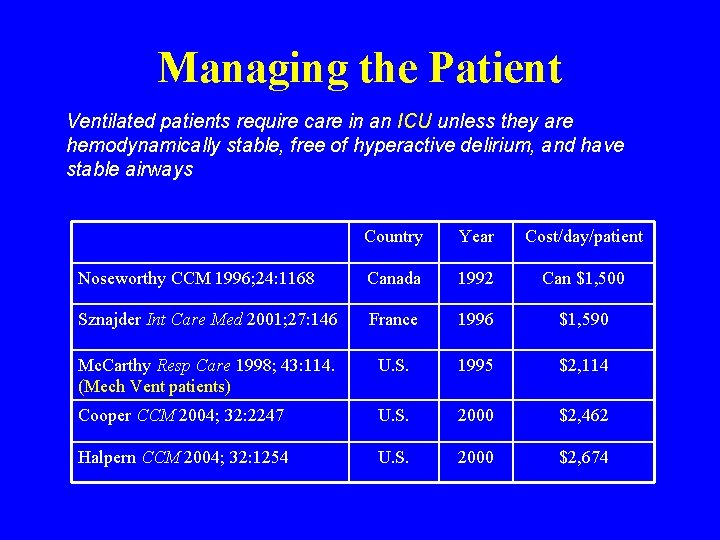
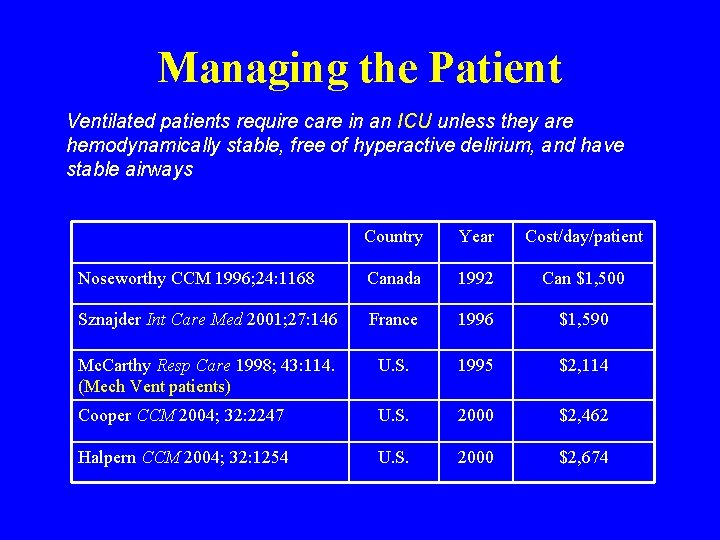
Managing the Patient Ventilated patients require care in an ICU unless they are hemodynamically stable, free of hyperactive delirium, and have stable airways Country Year Cost/day/patient Noseworthy CCM 1996; 24: 1168 Canada 1992 Can $1, 500 Sznajder Int Care Med 2001; 27: 146 France 1996 $1, 590 Mc. Carthy Resp Care 1998; 43: 114. (Mech Vent patients) U. S. 1995 $2, 114 Cooper CCM 2004; 32: 2247 U. S. 2000 $2, 462 Halpern CCM 2004; 32: 1254 U. S. 2000 $2, 674
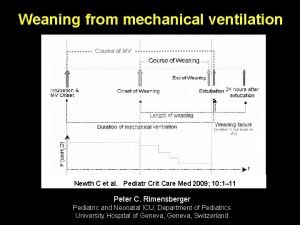
Weaning -“The process of liberating patients from the ventilator, … begins as soon as the patient is intubated by tailoring settings to the needs of the patient…” Hall JB, Wood L. JAMA 1987
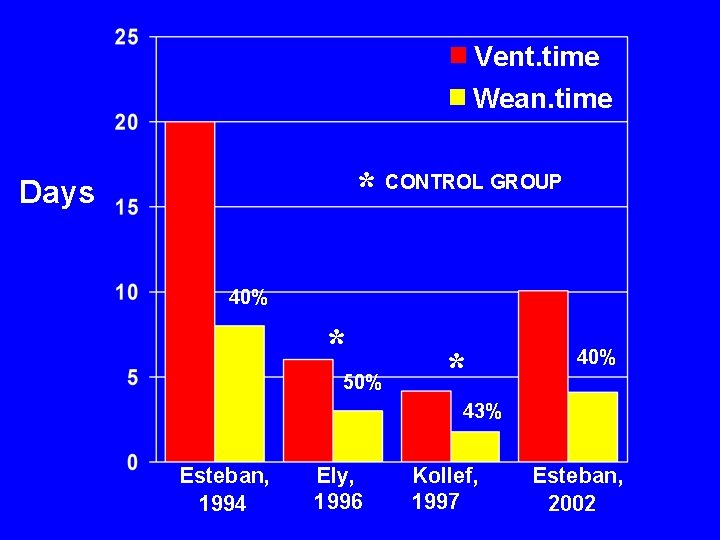
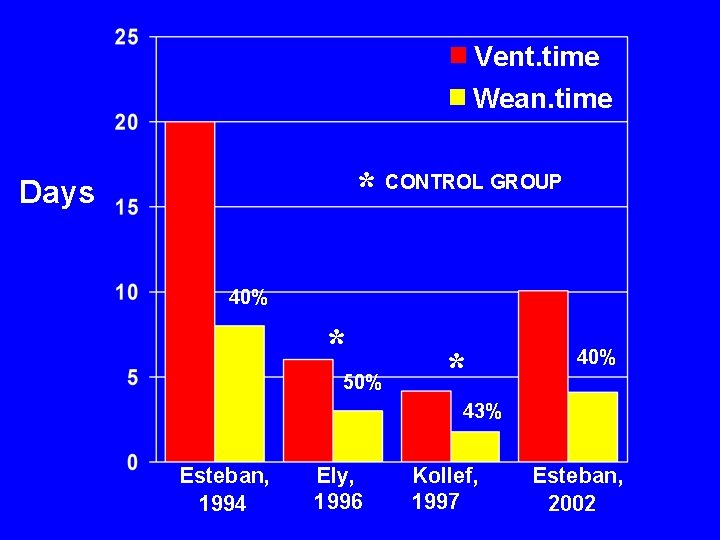
Vent. time Wean. time * CONTROL GROUP Days 40% * 50% * 40% 43% Esteban, 1994 Ely, 1996 Kollef, 1997 Esteban, 2002
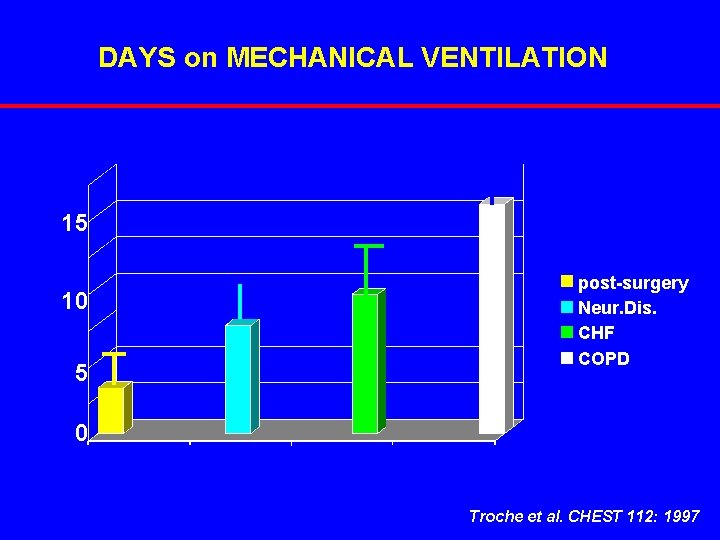
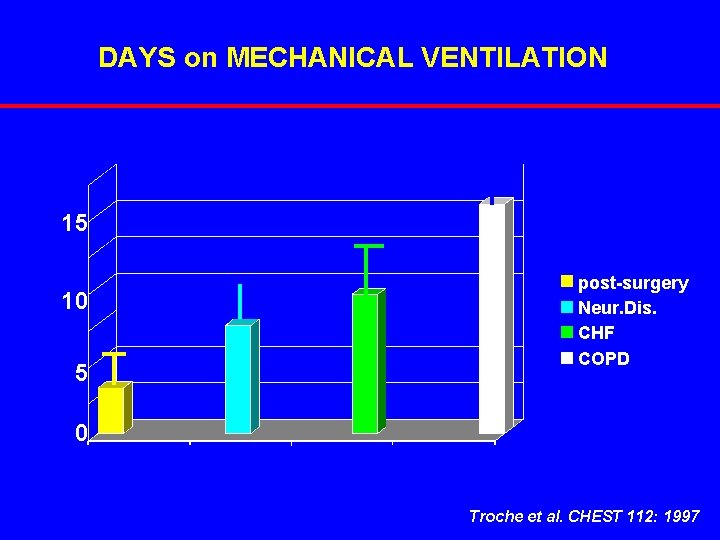
DAYS on MECHANICAL VENTILATION 15 10 5 post-surgery Neur. Dis. CHF COPD 0 Troche et al. CHEST 112: 1997
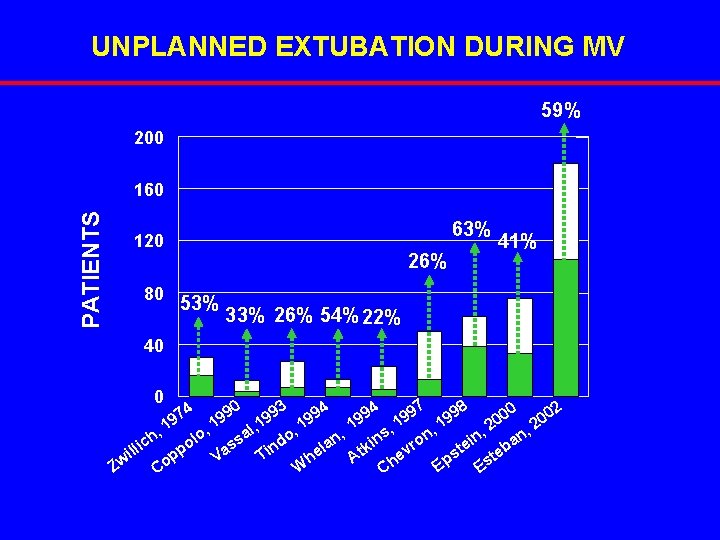
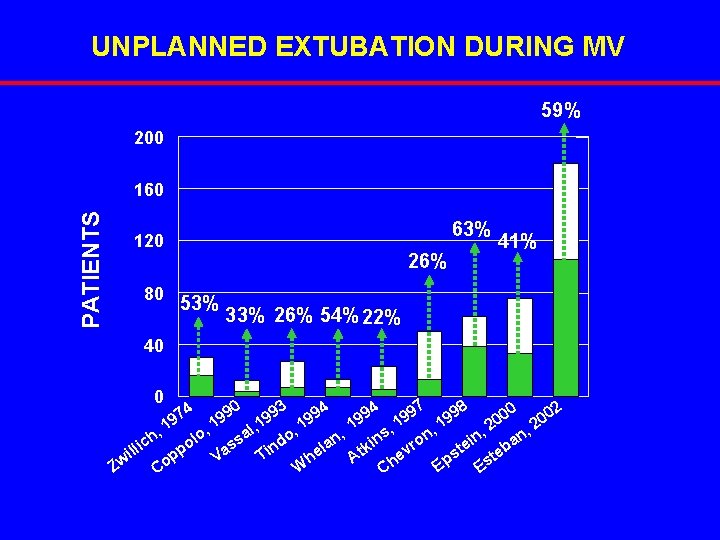
UNPLANNED EXTUBATION DURING MV 59% 200 PATIENTS 160 63% 120 80 26% 53% 41% 33% 26% 54% 22% 40 0 0 97 998 93 994 02 94 0 9 9 0 1 2 , 1 n, 1 l, 1 o, 1 , , 2 , , , s a o n h n l n in vro c o ss ind ei eba la k t p lli a t e i s p e t T V A h Ep Zw W Es Co Ch 7 19 4 0 9 19
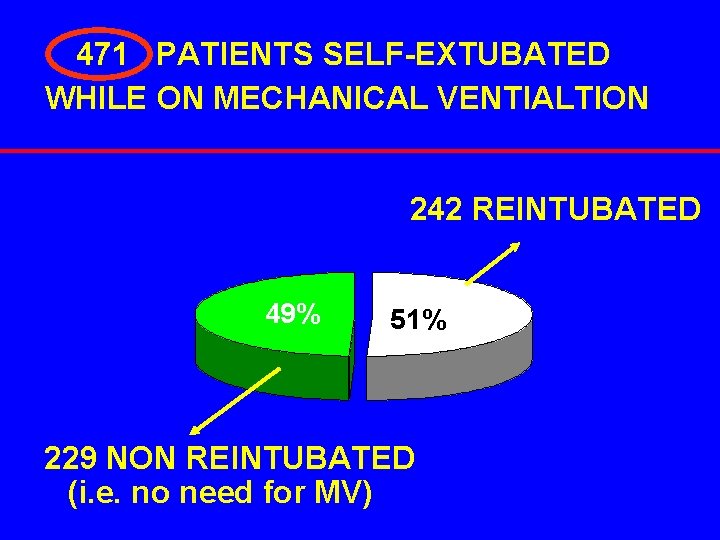
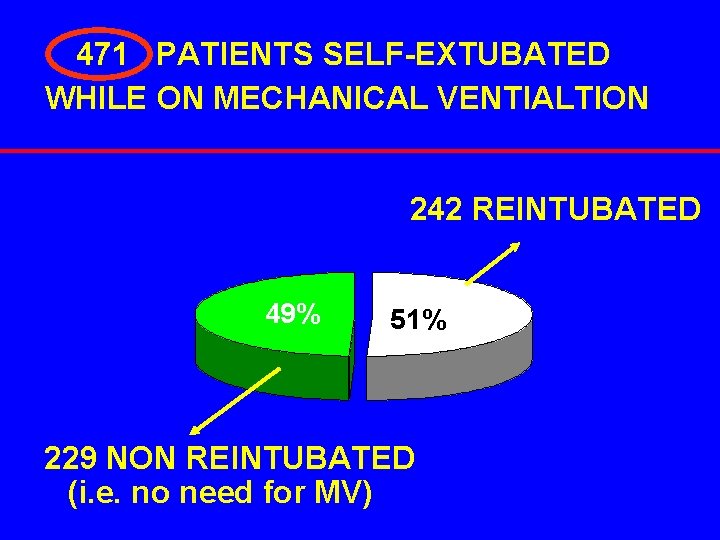
471 PATIENTS SELF-EXTUBATED WHILE ON MECHANICAL VENTIALTION 242 REINTUBATED 49% 51% 229 NON REINTUBATED (i. e. no need for MV)
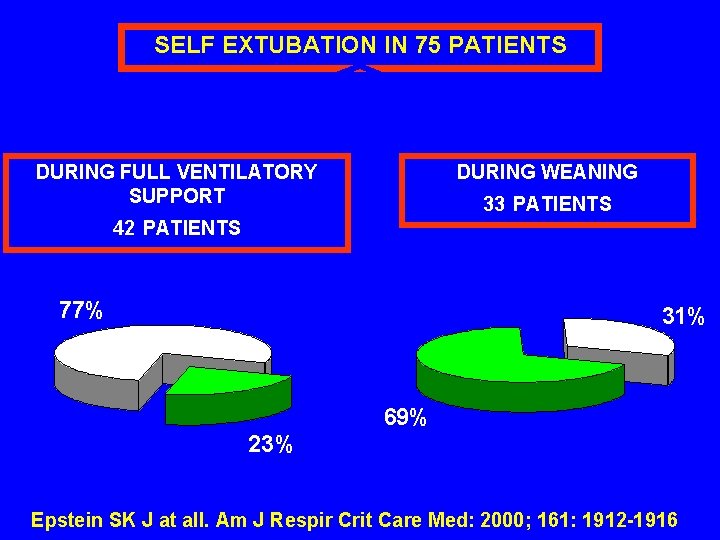
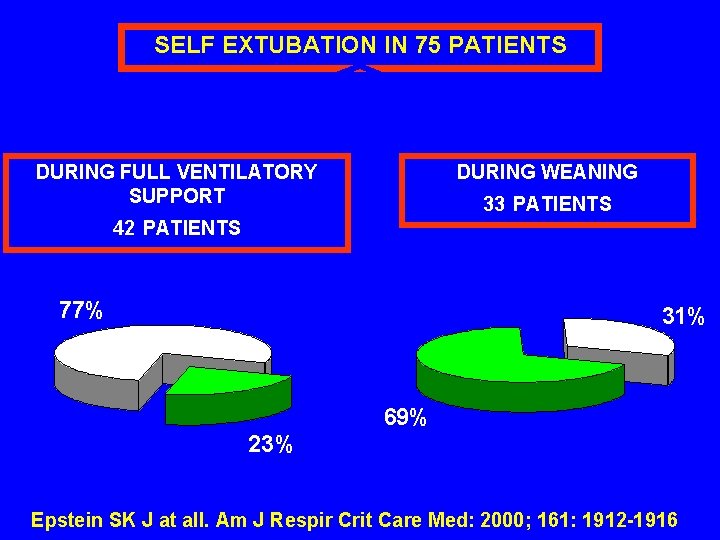
SELF EXTUBATION IN 75 PATIENTS DURING WEANING DURING FULL VENTILATORY SUPPORT 33 PATIENTS 42 PATIENTS 77% 31% 69% 23% Epstein SK J at all. Am J Respir Crit Care Med: 2000; 161: 1912 -1916
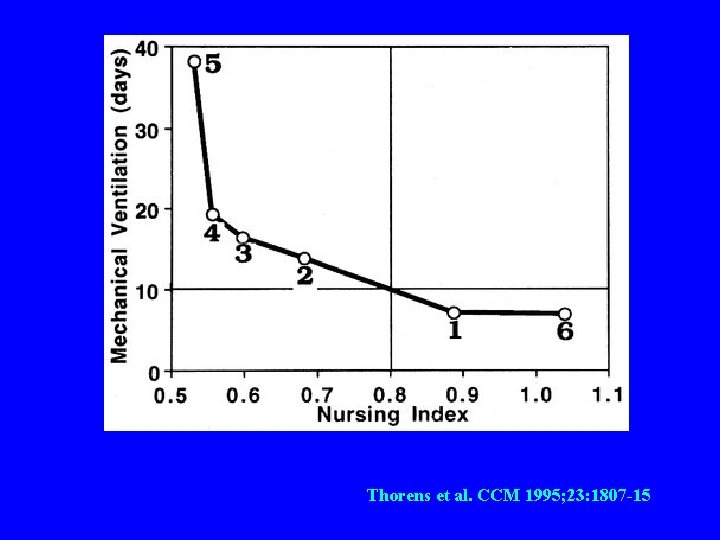
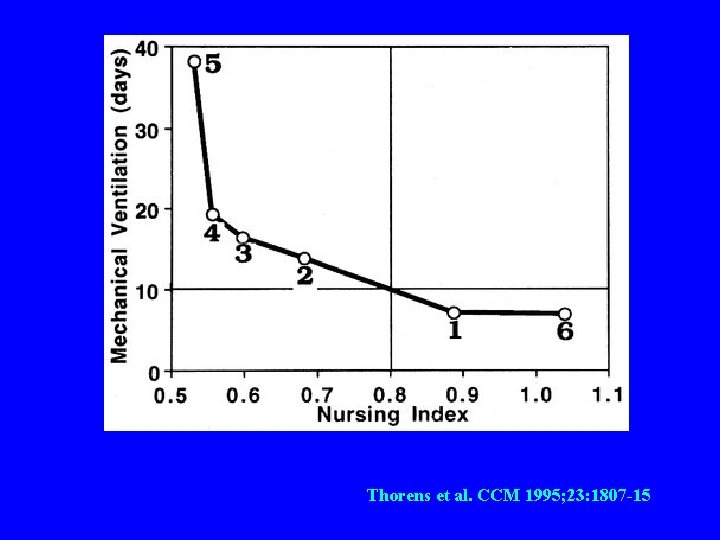
Thorens et al. CCM 1995; 23: 1807 -15
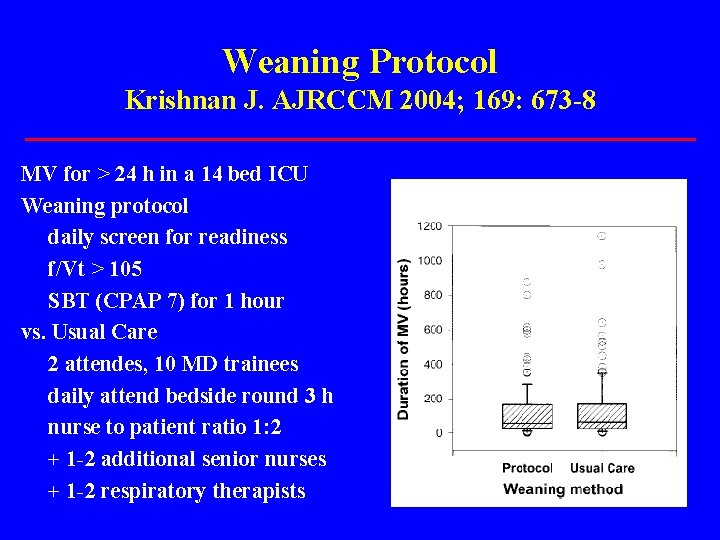
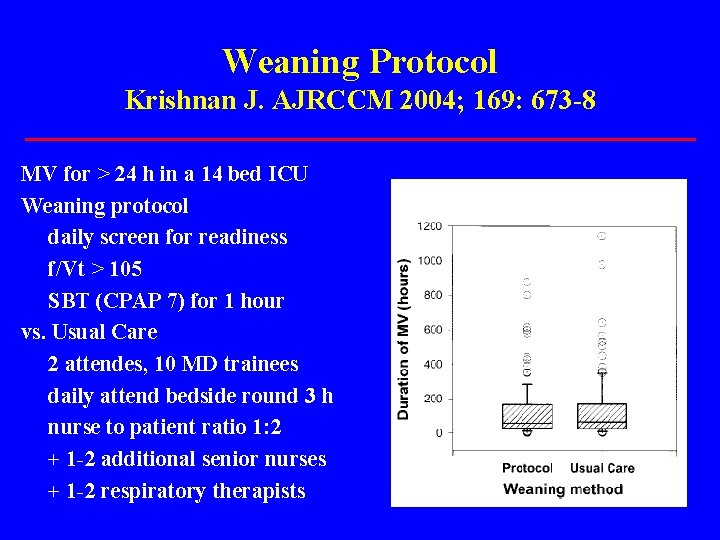
Weaning Protocol Krishnan J. AJRCCM 2004; 169: 673 -8 MV for > 24 h in a 14 bed ICU Weaning protocol daily screen for readiness f/Vt > 105 SBT (CPAP 7) for 1 hour vs. Usual Care 2 attendes, 10 MD trainees daily attend bedside round 3 h nurse to patient ratio 1: 2 + 1 -2 additional senior nurses + 1 -2 respiratory therapists
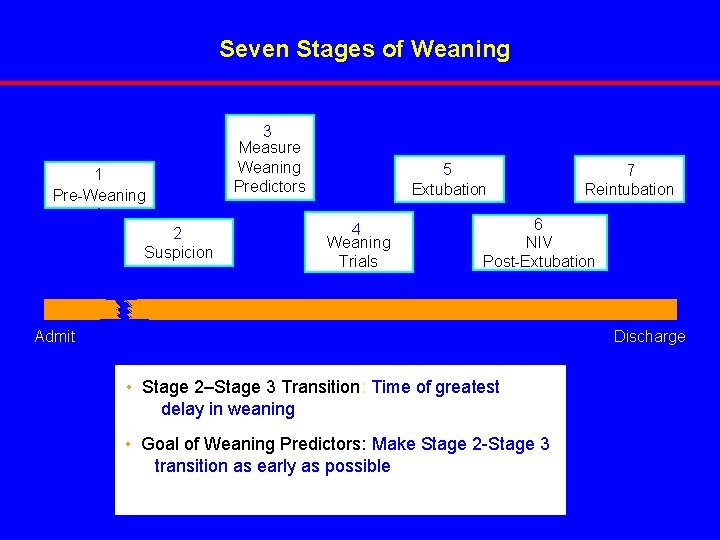
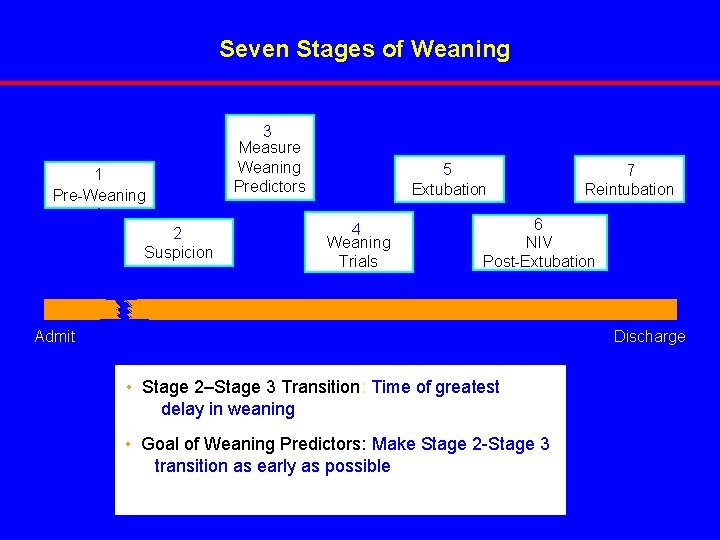
Seven Stages of Weaning 1 Pre-Weaning 2 Suspicion 3 Measure Weaning Predictors 5 Extubation 4 Weaning Trials 7 Reintubation 6 NIV Post-Extubation Discharge Admit • Stage 2–Stage 3 Transition: Time of greatest delay in weaning • Goal of Weaning Predictors: Make Stage 2 -Stage 3 transition as early as possible
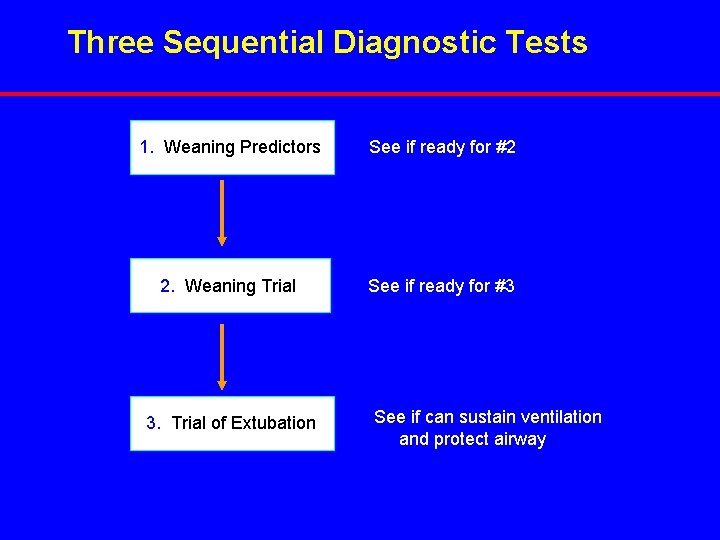
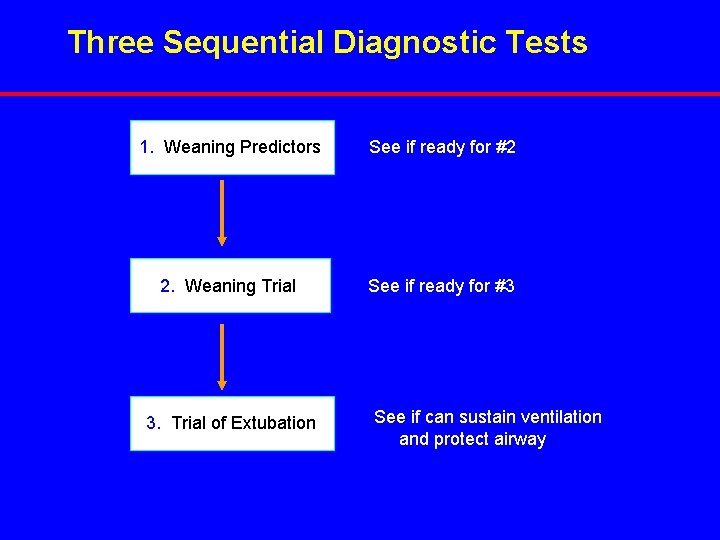
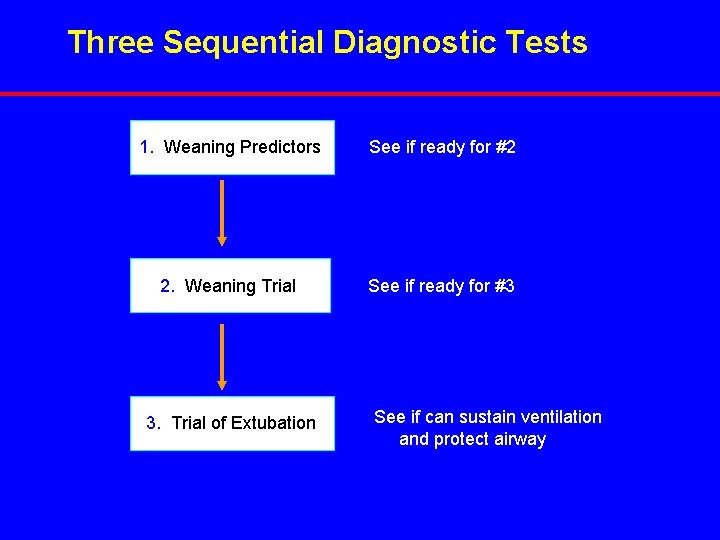
Three Sequential Diagnostic Tests 1. Weaning Predictors See if ready for #2 2. Weaning Trial See if ready for #3 3. Trial of Extubation See if can sustain ventilation and protect airway
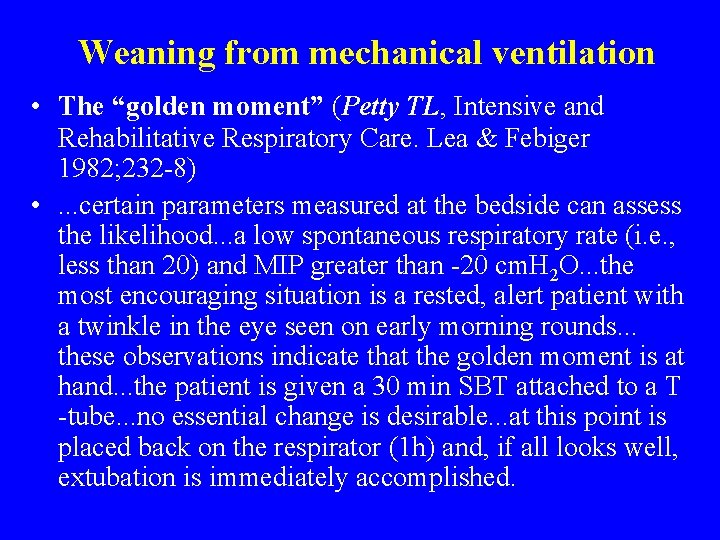
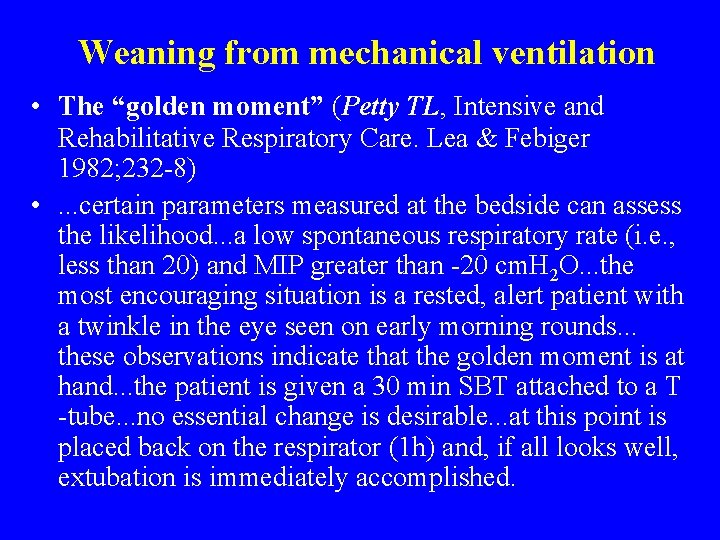
Weaning from mechanical ventilation • The “golden moment” (Petty TL, Intensive and Rehabilitative Respiratory Care. Lea & Febiger 1982; 232 -8) • . . . certain parameters measured at the bedside can assess the likelihood. . . a low spontaneous respiratory rate (i. e. , less than 20) and MIP greater than -20 cm. H 2 O. . . the most encouraging situation is a rested, alert patient with a twinkle in the eye seen on early morning rounds. . . these observations indicate that the golden moment is at hand. . . the patient is given a 30 min SBT attached to a T -tube. . . no essential change is desirable. . . at this point is placed back on the respirator (1 h) and, if all looks well, extubation is immediately accomplished.
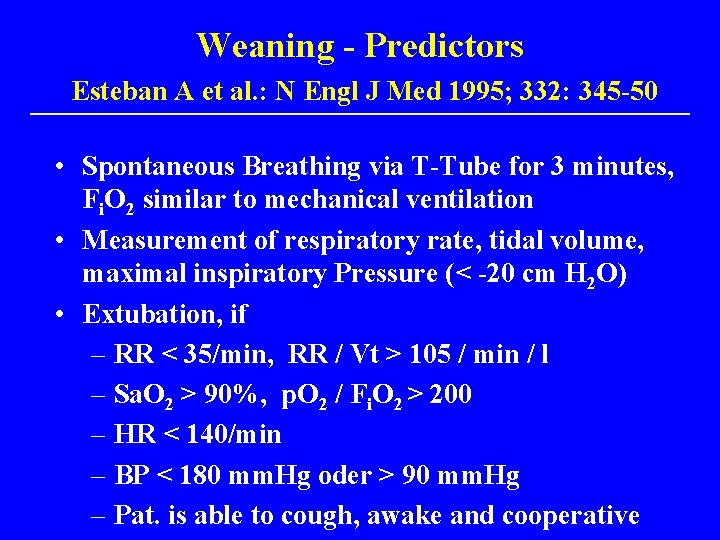
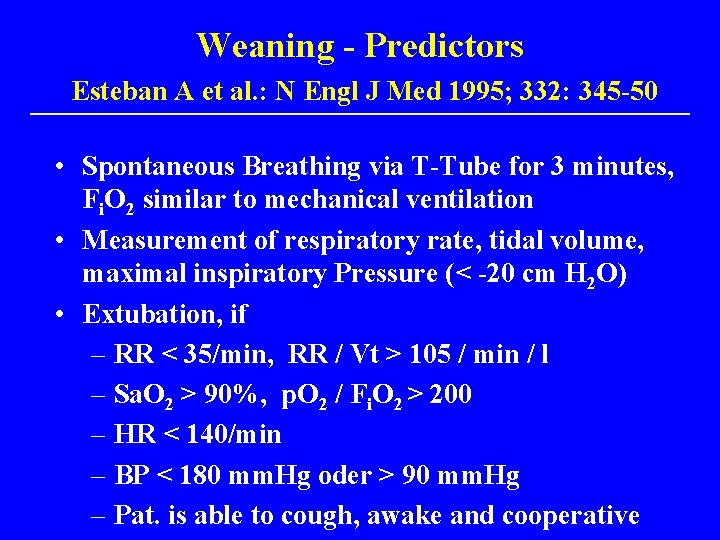
Weaning - Predictors Esteban A et al. : N Engl J Med 1995; 332: 345 -50 • Spontaneous Breathing via T-Tube for 3 minutes, Fi. O 2 similar to mechanical ventilation • Measurement of respiratory rate, tidal volume, maximal inspiratory Pressure (< -20 cm H 2 O) • Extubation, if – RR < 35/min, RR / Vt > 105 / min / l – Sa. O 2 > 90%, p. O 2 / Fi. O 2 > 200 – HR < 140/min – BP < 180 mm. Hg oder > 90 mm. Hg – Pat. is able to cough, awake and cooperative
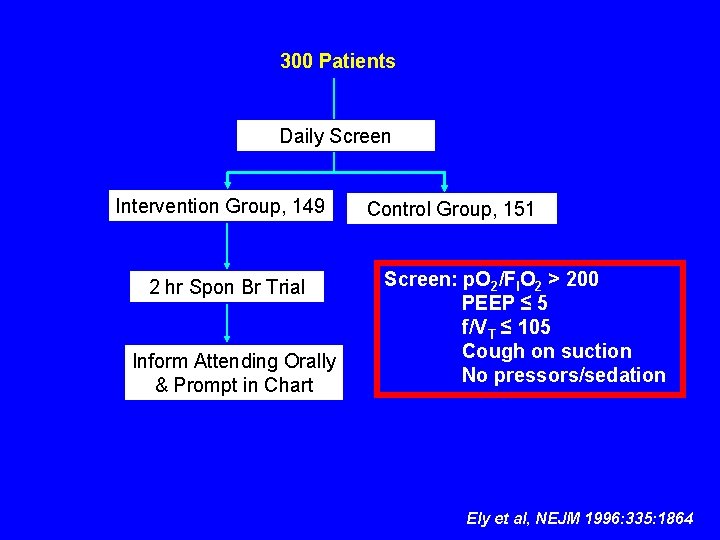
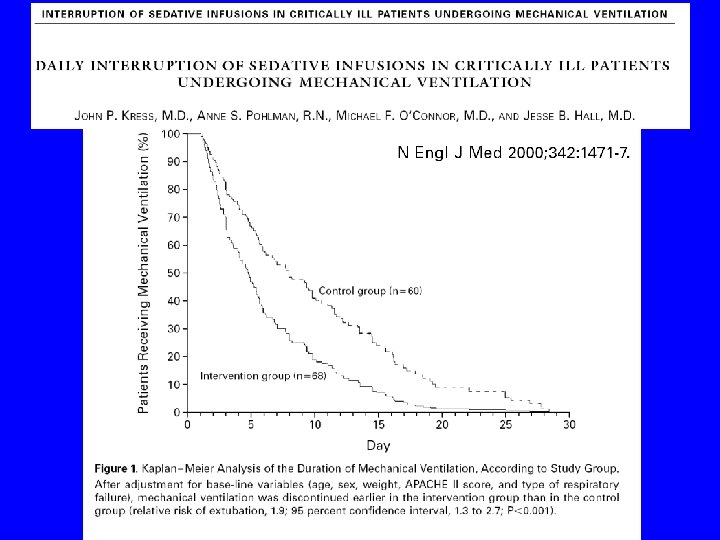
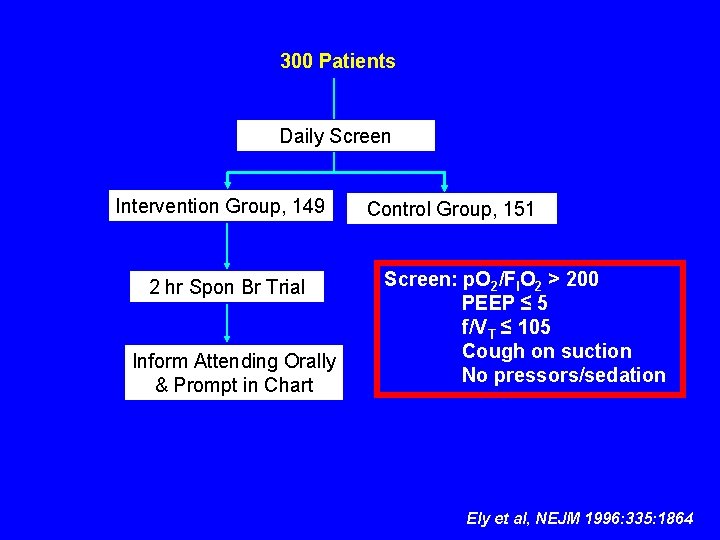
300 Patients Daily Screen Intervention Group, 149 2 hr Spon Br Trial Inform Attending Orally & Prompt in Chart Control Group, 151 Screen: p. O 2/FIO 2 > 200 PEEP ≤ 5 f/VT ≤ 105 Cough on suction No pressors/sedation Ely et al, NEJM 1996: 335: 1864
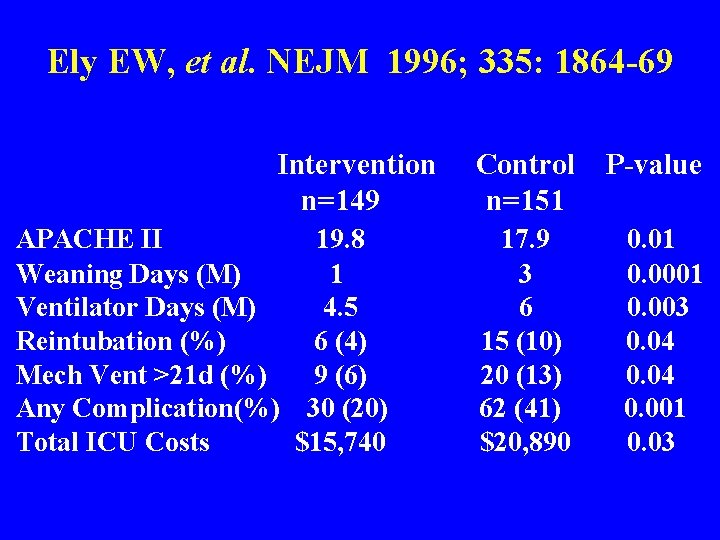
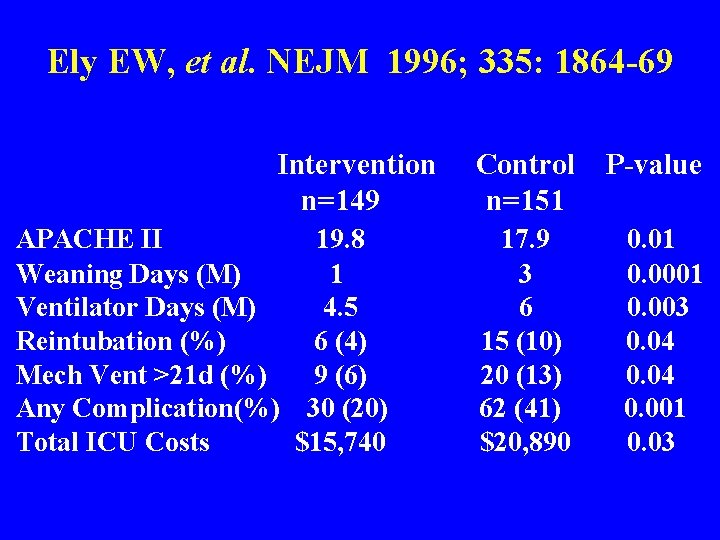
Ely EW, et al. NEJM 1996; 335: 1864 -69 Intervention n=149 APACHE II 19. 8 Weaning Days (M) 1 Ventilator Days (M) 4. 5 Reintubation (%) 6 (4) Mech Vent >21 d (%) 9 (6) Any Complication(%) 30 (20) Total ICU Costs $15, 740 Control n=151 P-value 17. 9 3 6 15 (10) 20 (13) 62 (41) $20, 890 0. 01 0. 003 0. 04 0. 001 0. 03
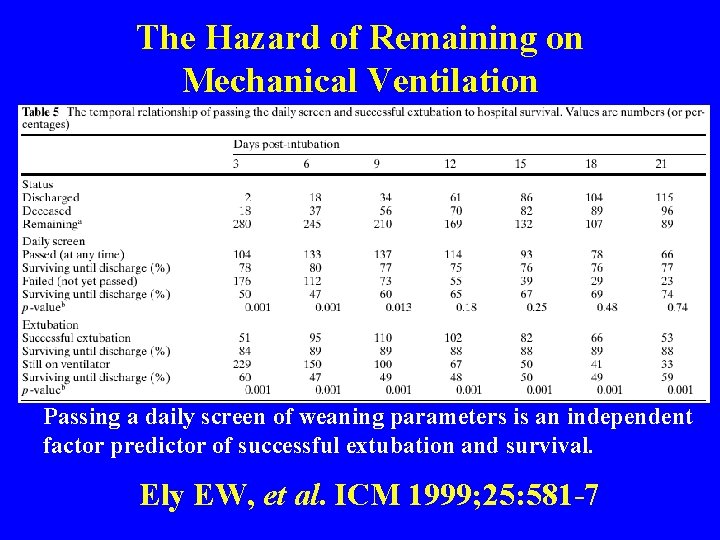
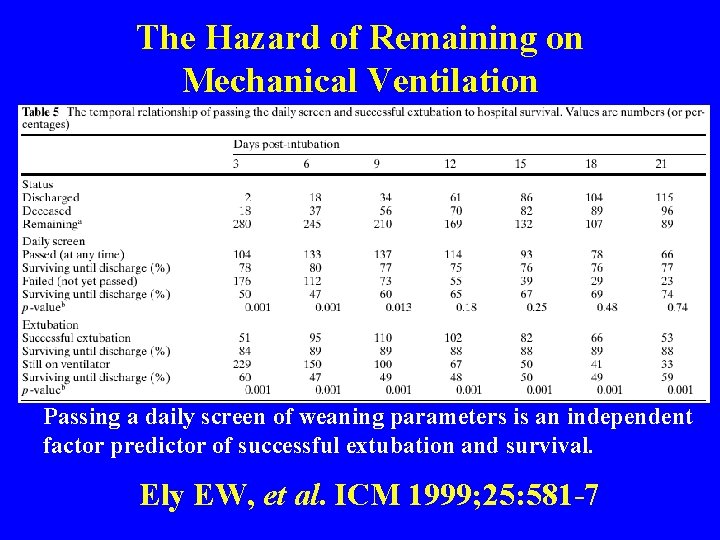
The Hazard of Remaining on Mechanical Ventilation Passing a daily screen of weaning parameters is an independent factor predictor of successful extubation and survival. Ely EW, et al. ICM 1999; 25: 581 -7
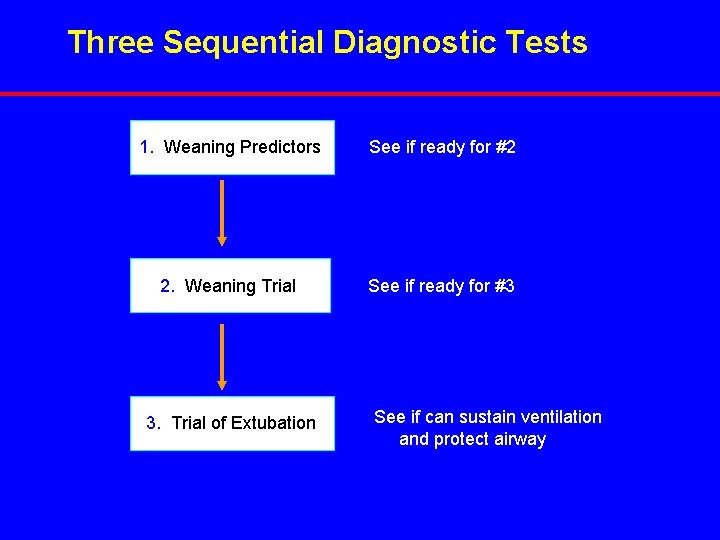
Three Sequential Diagnostic Tests 1. Weaning Predictors See if ready for #2 2. Weaning Trial See if ready for #3 3. Trial of Extubation See if can sustain ventilation and protect airway
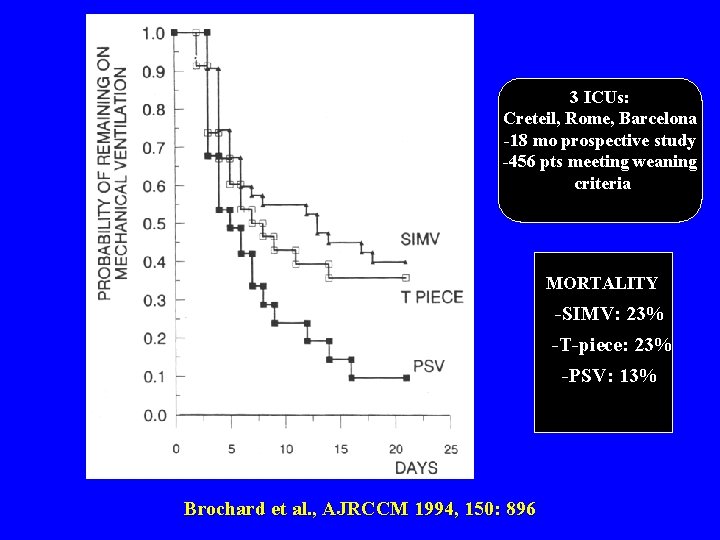
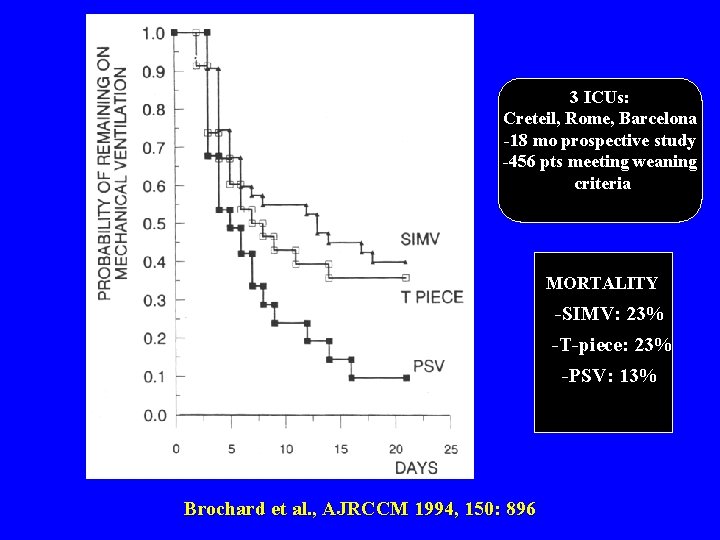
3 ICUs: Creteil, Rome, Barcelona -18 mo prospective study -456 pts meeting weaning criteria MORTALITY -SIMV: 23% -T-piece: 23% -PSV: 13% Brochard et al. , AJRCCM 1994, 150: 896
Multicenter trial • PS was decreased twice a day • RR < 35 breaths/min • Minimal level of PS has to be tolerated 24 hours before extubation
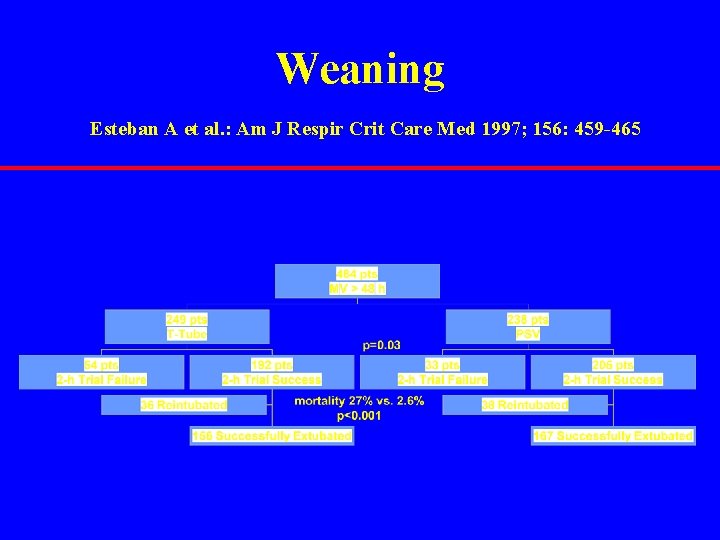
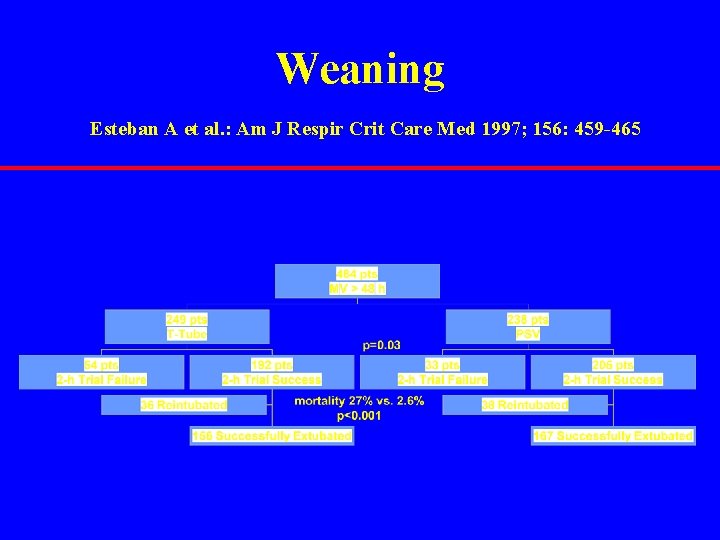
Weaning Esteban A et al. : Am J Respir Crit Care Med 1997; 156: 459 -465
Mechanical Ventilation in COPD additional problems • • Size of the endotracheal tube Secretions Nutritional Status Medication – Sedatives – Steroides – Theophyllin and ß 2 -mimetics
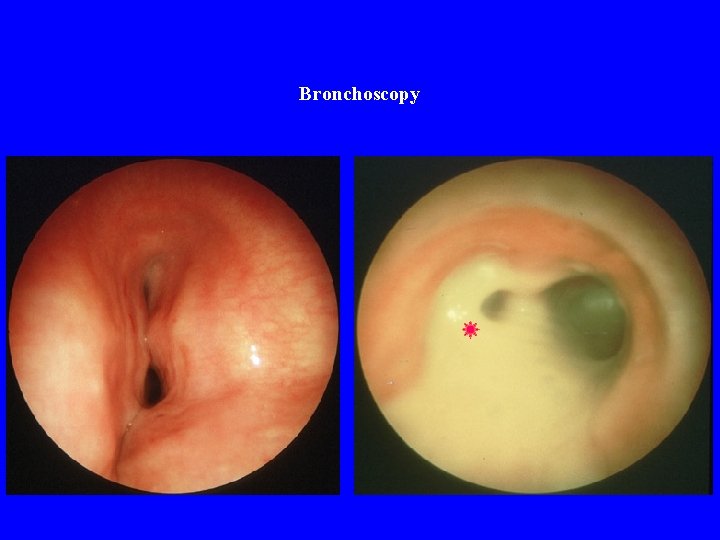
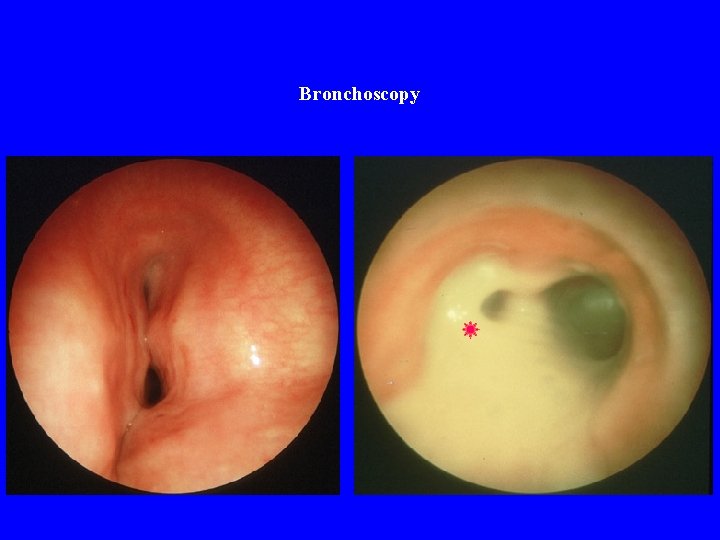
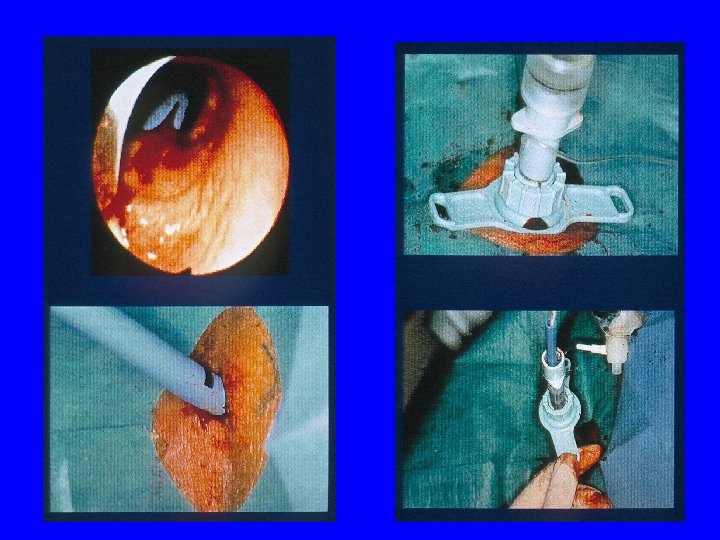
Bronchoscopy
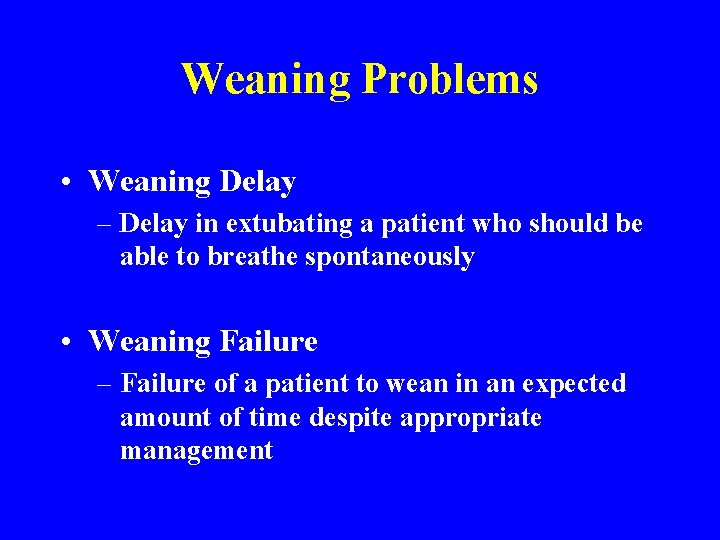
Weaning Problems • Weaning Delay – Delay in extubating a patient who should be able to breathe spontaneously • Weaning Failure – Failure of a patient to wean in an expected amount of time despite appropriate management
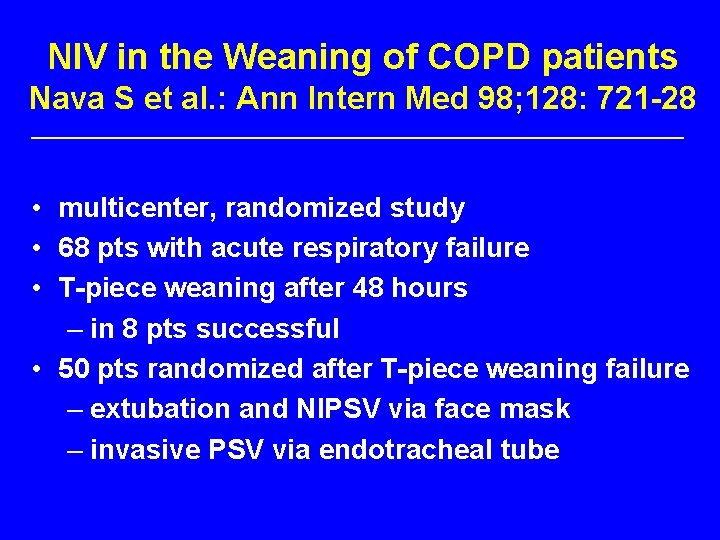
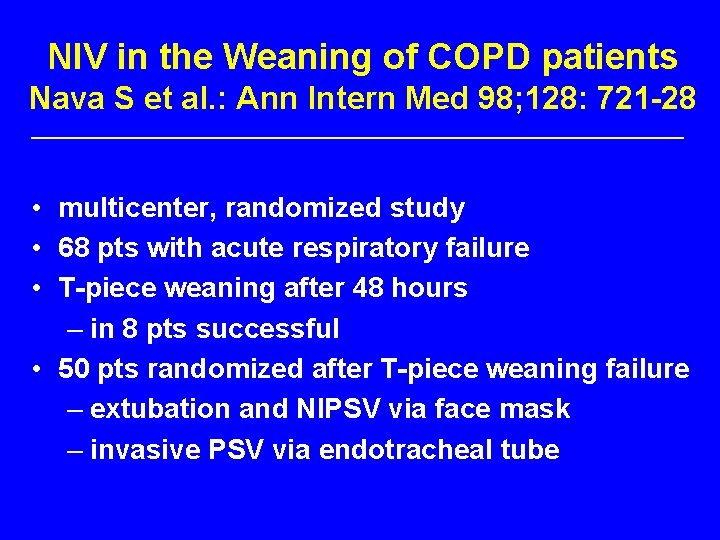
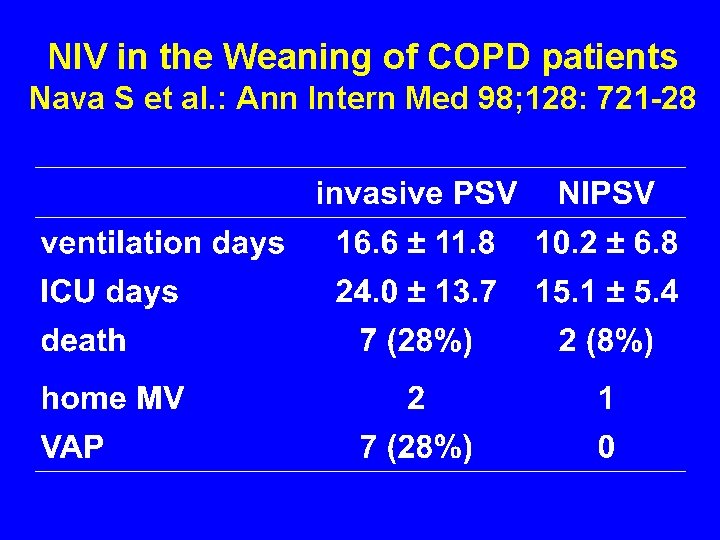
NIV in the Weaning of COPD patients Nava S et al. : Ann Intern Med 98; 128: 721 -28 • multicenter, randomized study • 68 pts with acute respiratory failure • T-piece weaning after 48 hours – in 8 pts successful • 50 pts randomized after T-piece weaning failure – extubation and NIPSV via face mask – invasive PSV via endotracheal tube
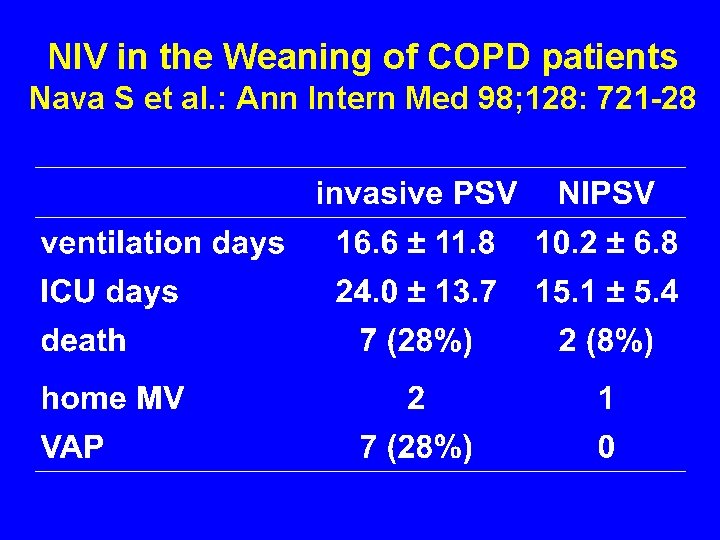
NIV in the Weaning of COPD patients Nava S et al. : Ann Intern Med 98; 128: 721 -28
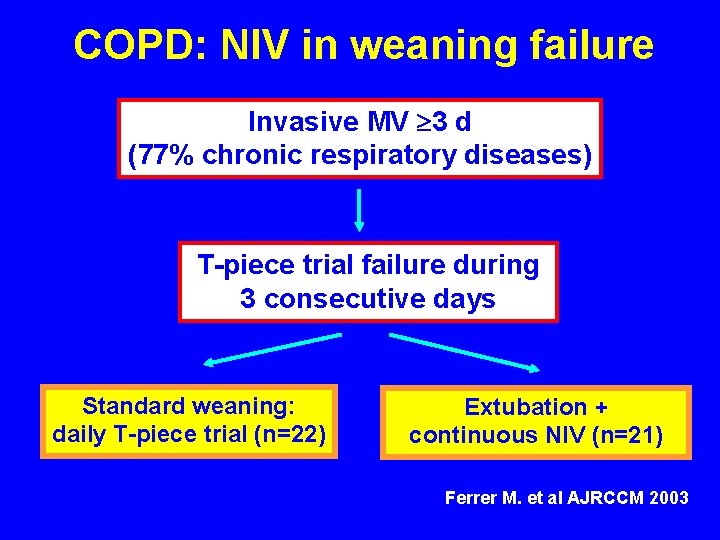
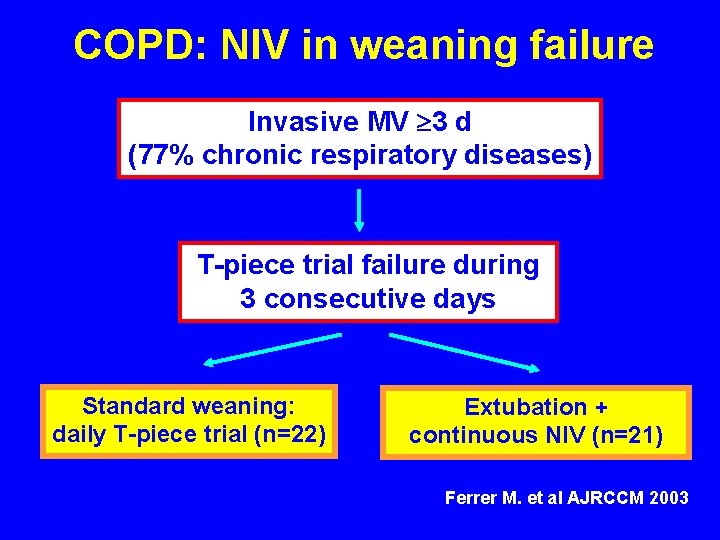
COPD: NIV in weaning failure Invasive MV 3 d (77% chronic respiratory diseases) T-piece trial failure during 3 consecutive days Standard weaning: daily T-piece trial (n=22) Extubation + continuous NIV (n=21) Ferrer M. et al AJRCCM 2003
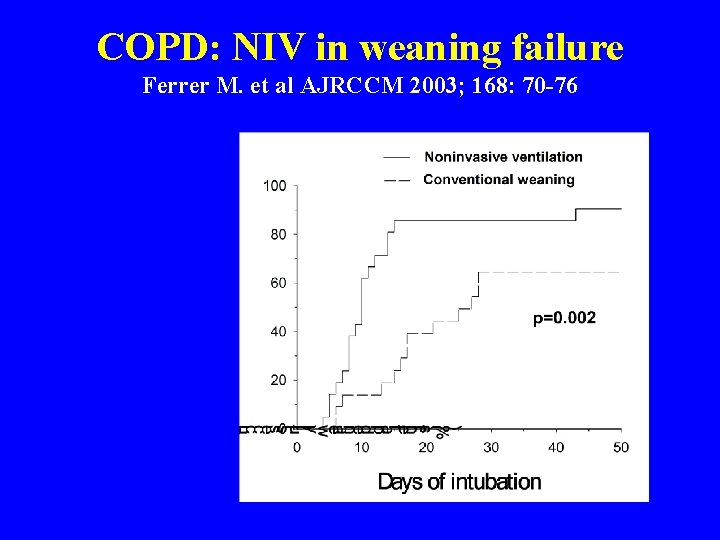
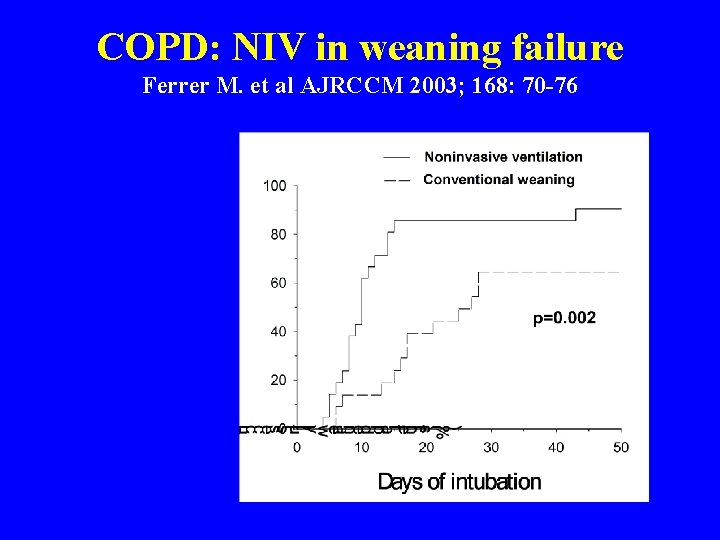
COPD: NIV in weaning failure Ferrer M. et al AJRCCM 2003; 168: 70 -76
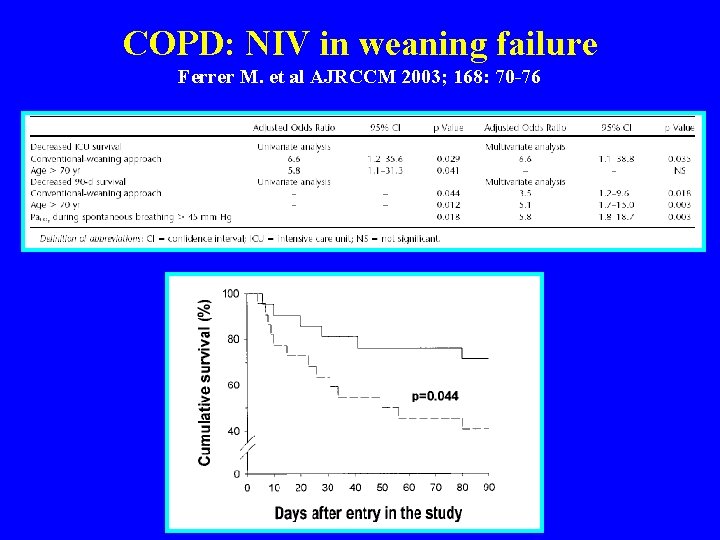
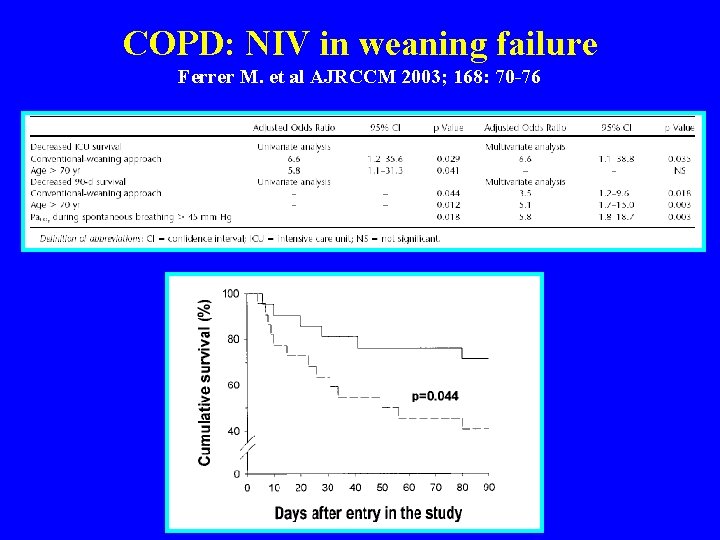
COPD: NIV in weaning failure Ferrer M. et al AJRCCM 2003; 168: 70 -76
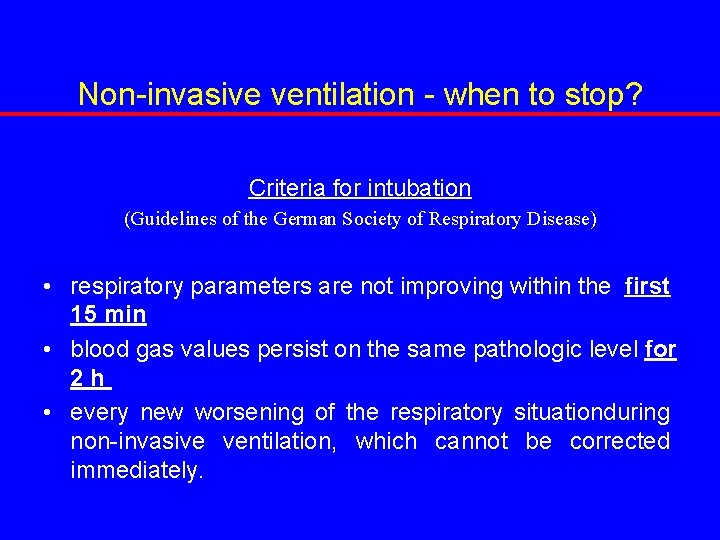
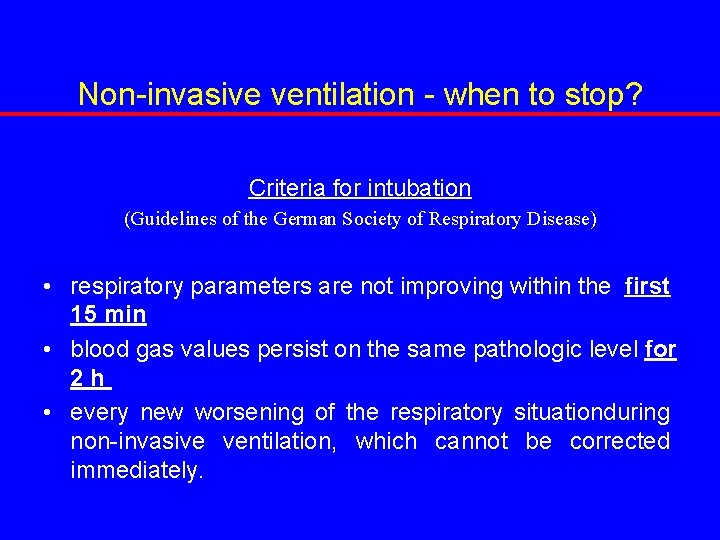
Non-invasive ventilation - when to stop? Criteria for intubation (Guidelines of the German Society of Respiratory Disease) • respiratory parameters are not improving within the first 15 min • blood gas values persist on the same pathologic level for 2 h • every new worsening of the respiratory situationduring non-invasive ventilation, which cannot be corrected immediately.
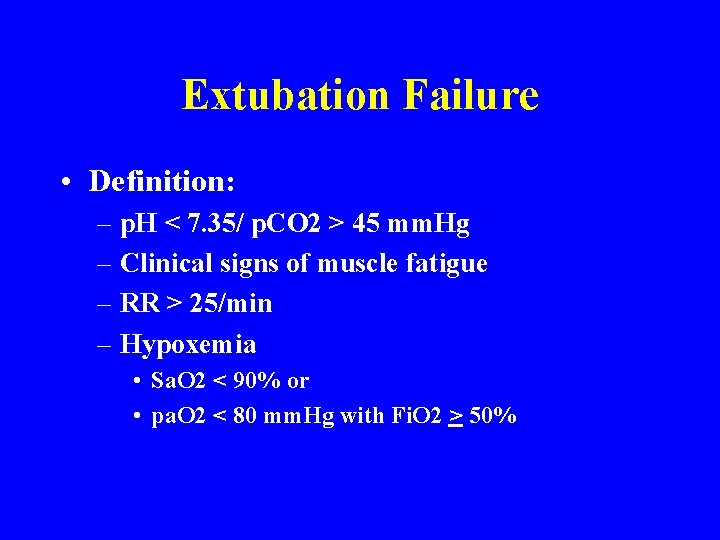
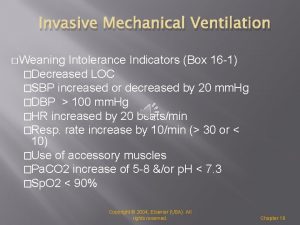
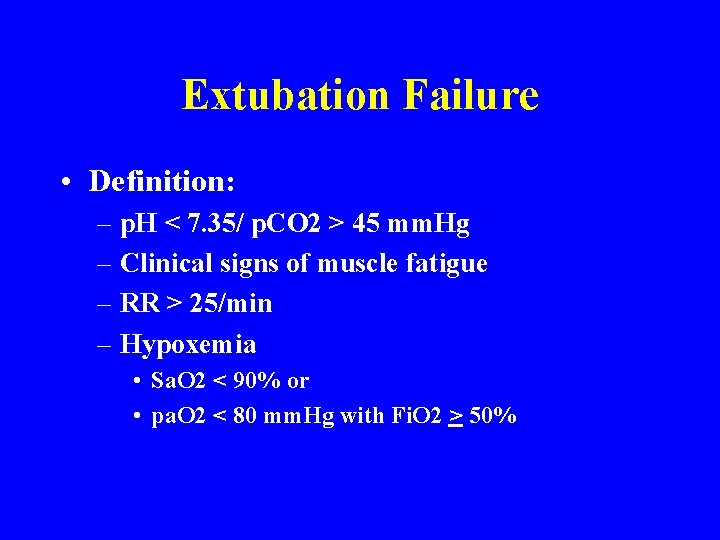
Extubation Failure • Definition: – p. H < 7. 35/ p. CO 2 > 45 mm. Hg – Clinical signs of muscle fatigue – RR > 25/min – Hypoxemia • Sa. O 2 < 90% or • pa. O 2 < 80 mm. Hg with Fi. O 2 > 50%
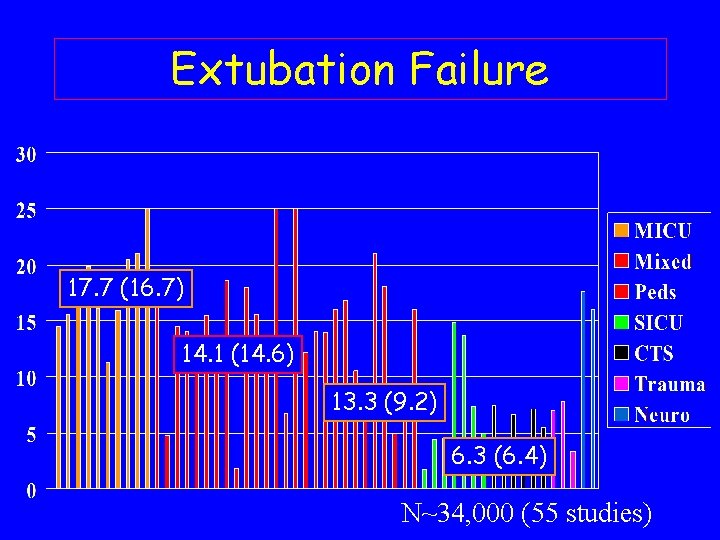
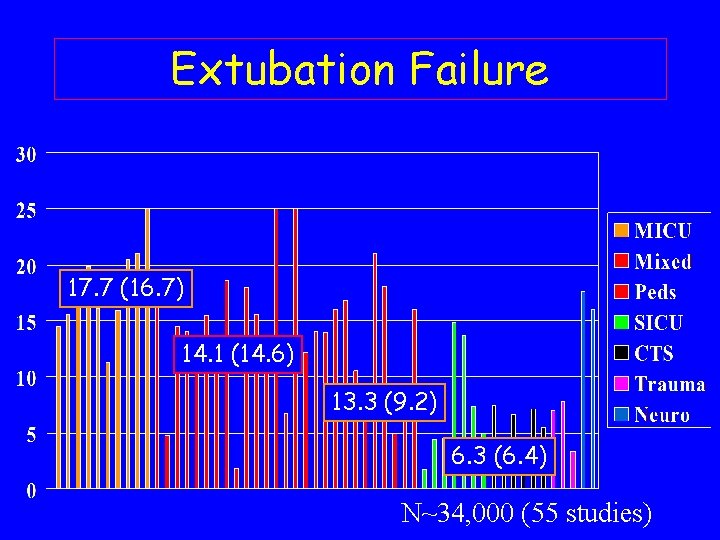
Extubation Failure 17. 7 (16. 7) 14. 1 (14. 6) 13. 3 (9. 2) 6. 3 (6. 4) N~34, 000 (55 studies)
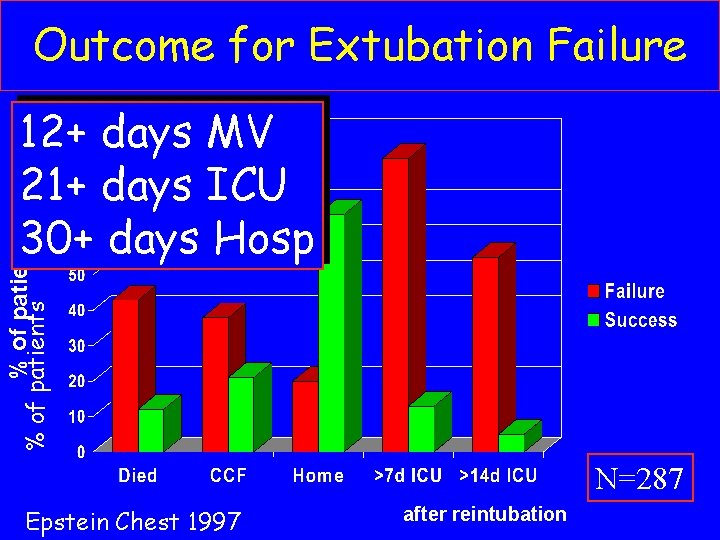
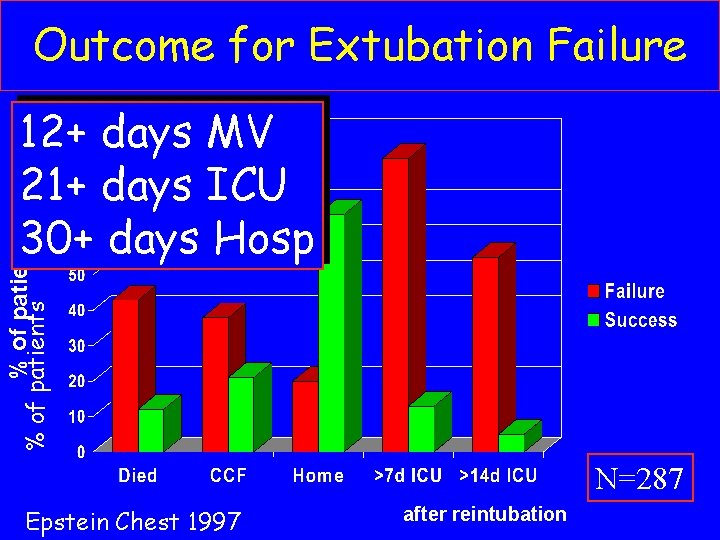
Outcome for Extubation Failure % of patients 12+ days MV 21+ days ICU 30+ days Hosp N=287 Epstein Chest 1997 after reintubation
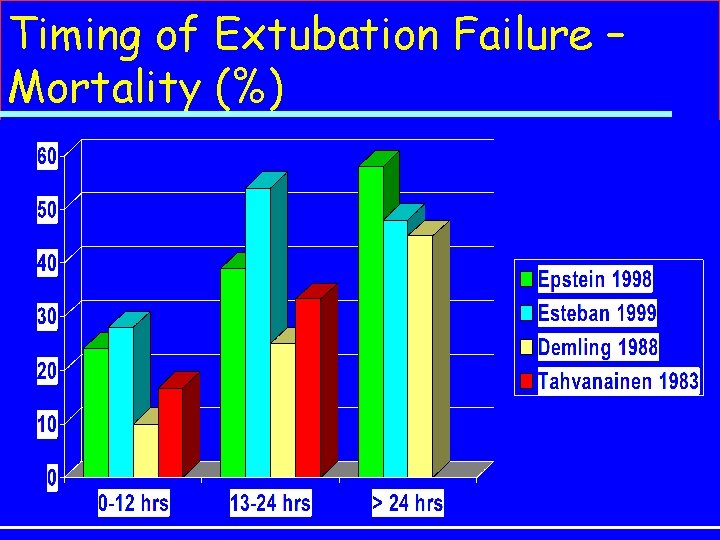
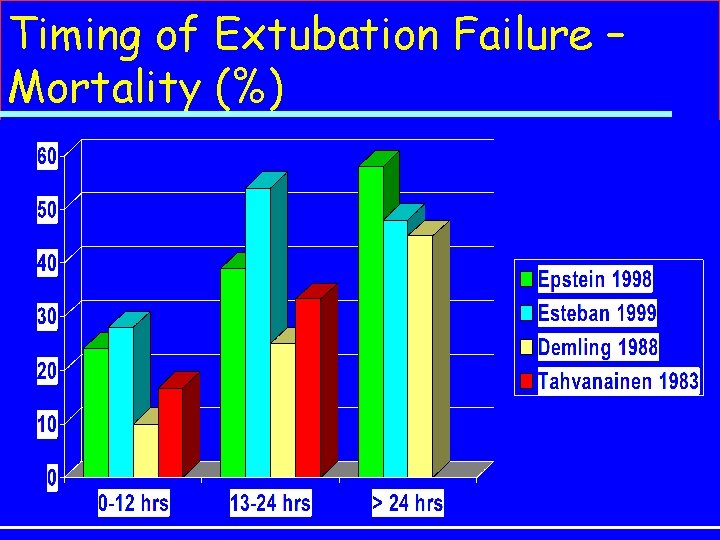
Timing of Extubation Failure – Mortality (%)
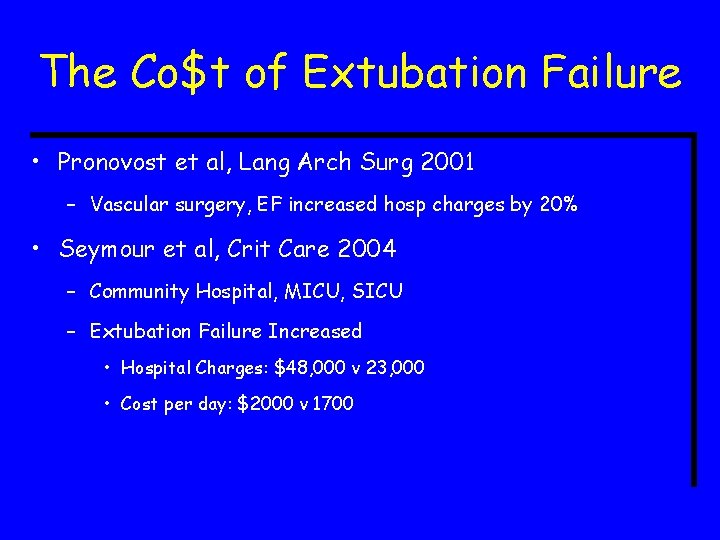
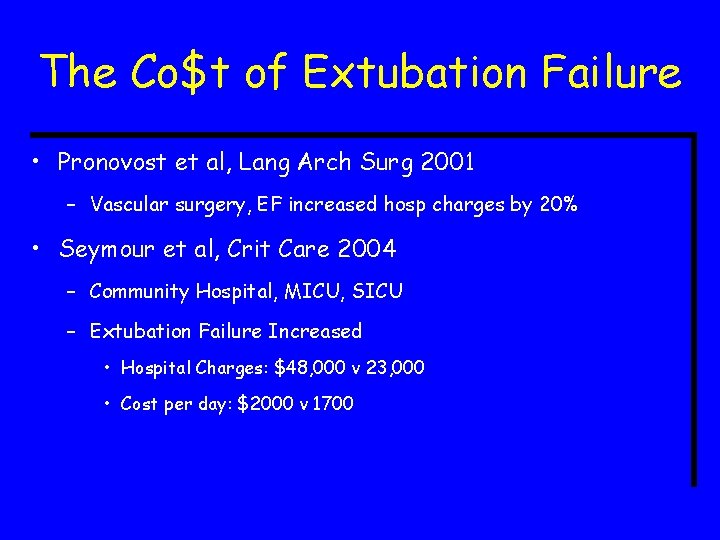
The Co$t of Extubation Failure • Pronovost et al, Lang Arch Surg 2001 – Vascular surgery, EF increased hosp charges by 20% • Seymour et al, Crit Care 2004 – Community Hospital, MICU, SICU – Extubation Failure Increased • Hospital Charges: $48, 000 v 23, 000 • Cost per day: $2000 v 1700
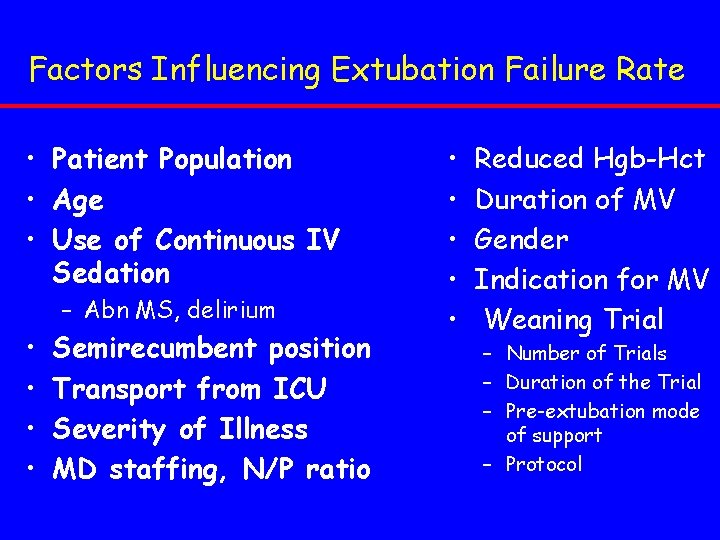
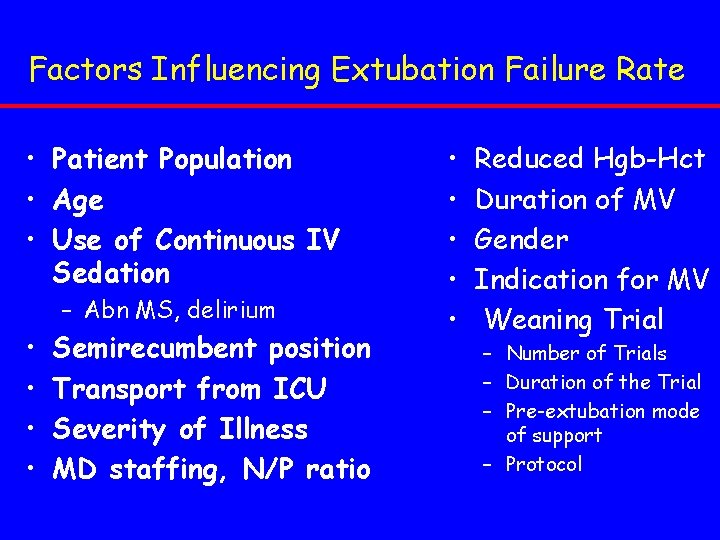
Factors Influencing Extubation Failure Rate • Patient Population • Age • Use of Continuous IV Sedation – Abn MS, delirium • • Semirecumbent position Transport from ICU Severity of Illness MD staffing, N/P ratio • • • Reduced Hgb-Hct Duration of MV Gender Indication for MV Weaning Trial – Number of Trials – Duration of the Trial – Pre-extubation mode of support – Protocol
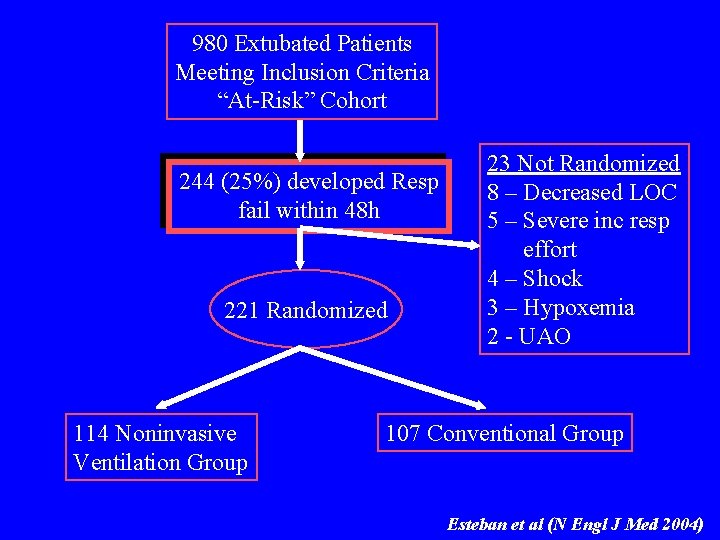
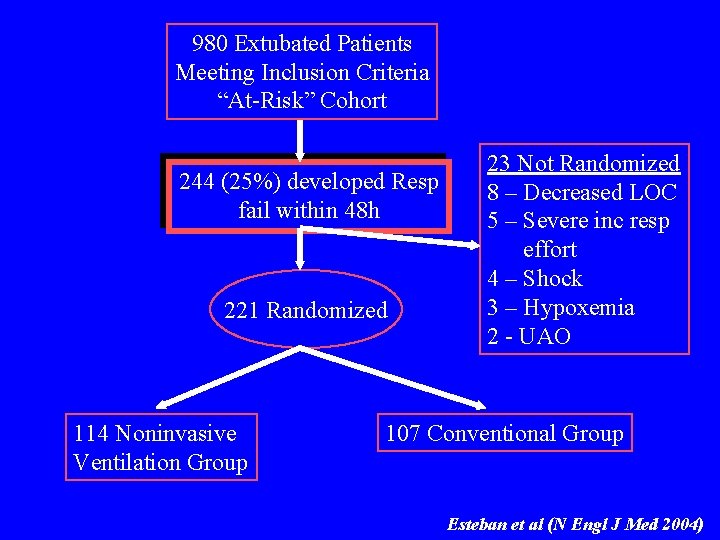
980 Extubated Patients Meeting Inclusion Criteria “At-Risk” Cohort 244 (25%) developed Resp fail within 48 h 221 Randomized 114 Noninvasive Ventilation Group 23 Not Randomized 8 – Decreased LOC 5 – Severe inc resp effort 4 – Shock 3 – Hypoxemia 2 - UAO 107 Conventional Group Esteban et al (N Engl J Med 2004)
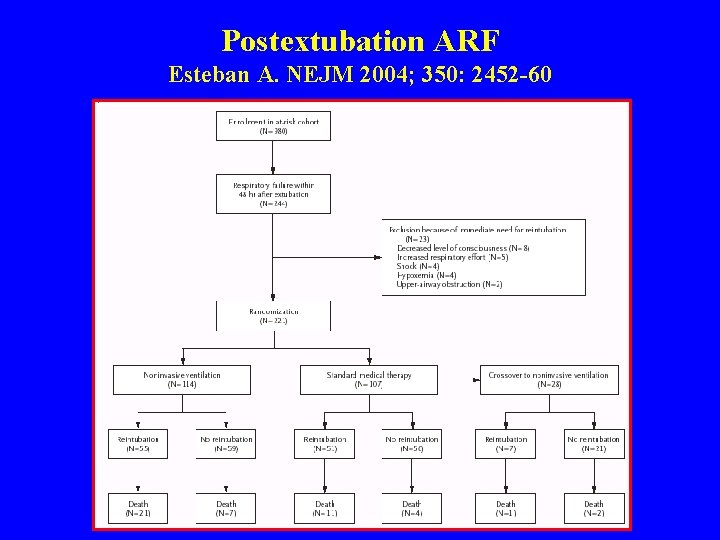
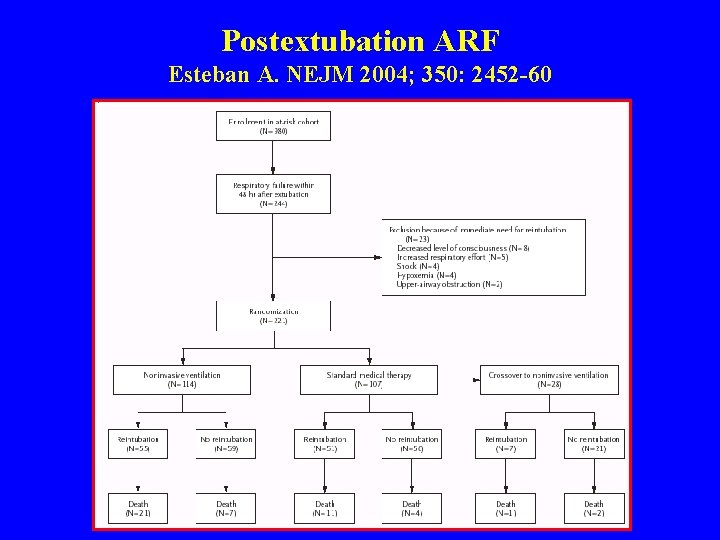
Postextubation ARF Esteban A. NEJM 2004; 350: 2452 -60
Postextubation ARF Esteban A. NEJM 2004; 350: 2452 -60 • Problems of the Esteban Study – Unexperienced centers – Inspiratory Pressure too low – NIV started too late
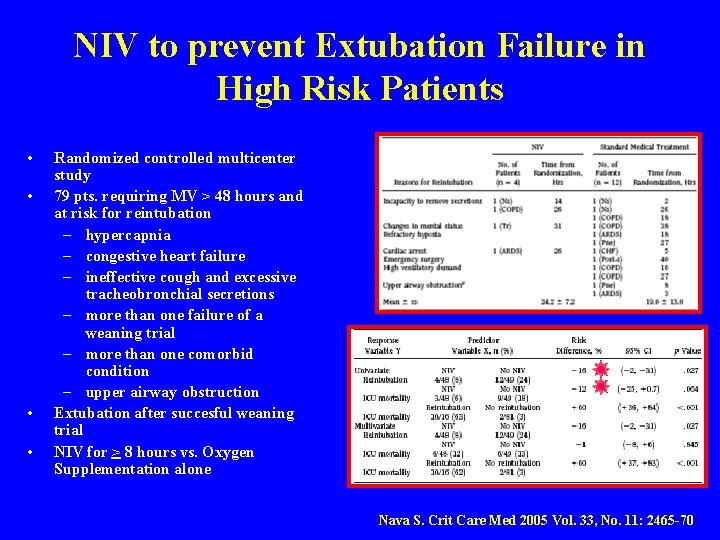
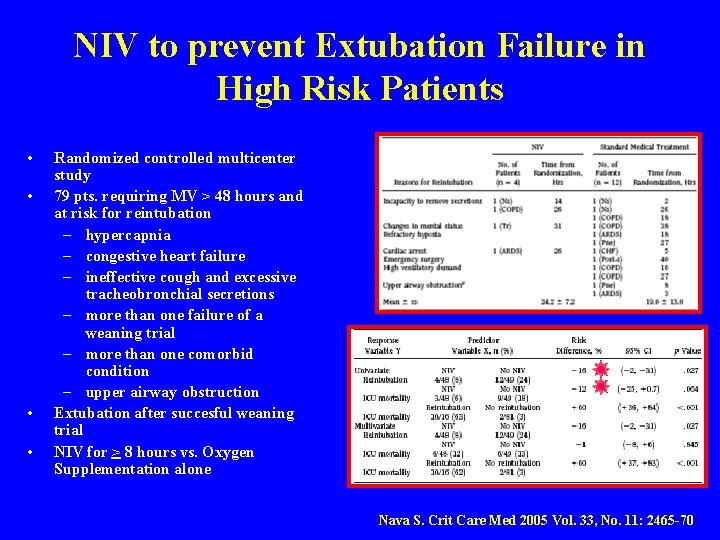
NIV to prevent Extubation Failure in High Risk Patients • • Randomized controlled multicenter study 79 pts. requiring MV > 48 hours and at risk for reintubation – hypercapnia – congestive heart failure – ineffective cough and excessive tracheobronchial secretions – more than one failure of a weaning trial – more than one comorbid condition – upper airway obstruction Extubation after succesful weaning trial NIV for > 8 hours vs. Oxygen Supplementation alone Nava S. Crit Care Med 2005 Vol. 33, No. 11: 2465 -70
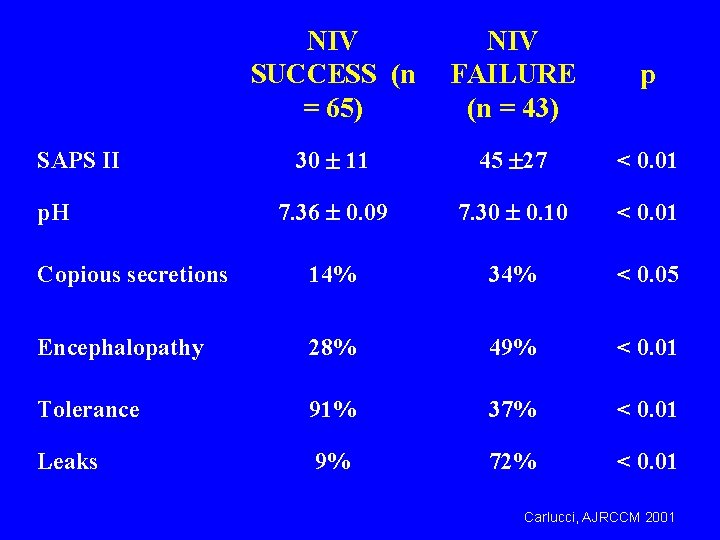
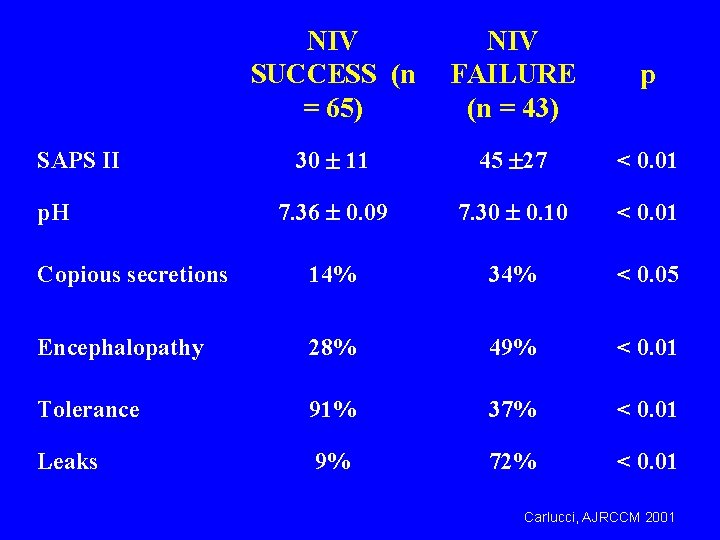
NIV SUCCESS (n = 65) NIV FAILURE (n = 43) p 30 11 45 27 < 0. 01 7. 36 0. 09 7. 30 0. 10 < 0. 01 Copious secretions 14% 34% < 0. 05 Encephalopathy 28% 49% < 0. 01 Tolerance 91% 37% < 0. 01 Leaks 9% 72% < 0. 01 SAPS II p. H Carlucci, AJRCCM 2001
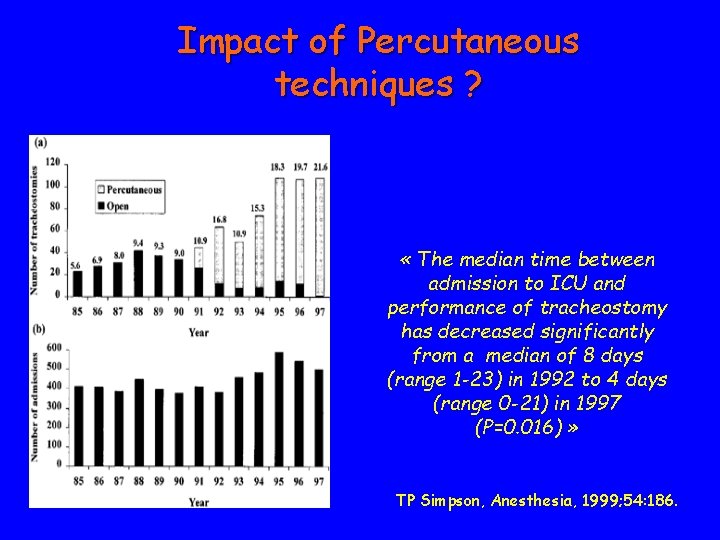
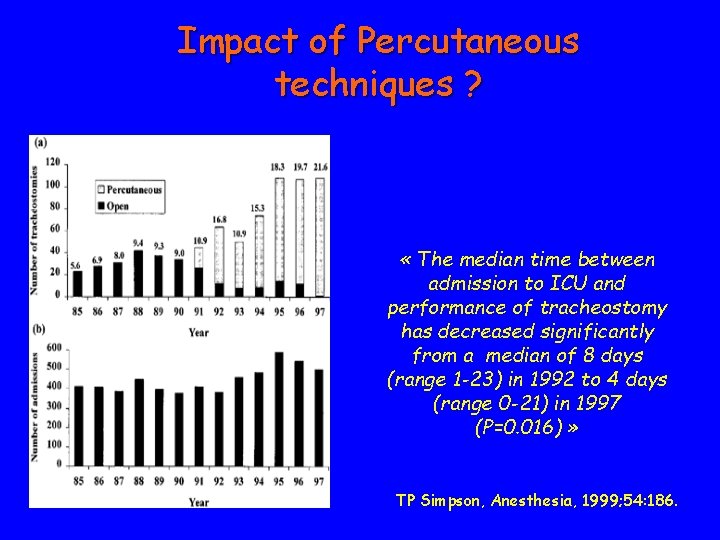
Impact of Percutaneous techniques ? « The median time between admission to ICU and performance of tracheostomy has decreased significantly from a median of 8 days (range 1 -23) in 1992 to 4 days (range 0 -21) in 1997 (P=0. 016) » TP Simpson, Anesthesia, 1999; 54: 186.
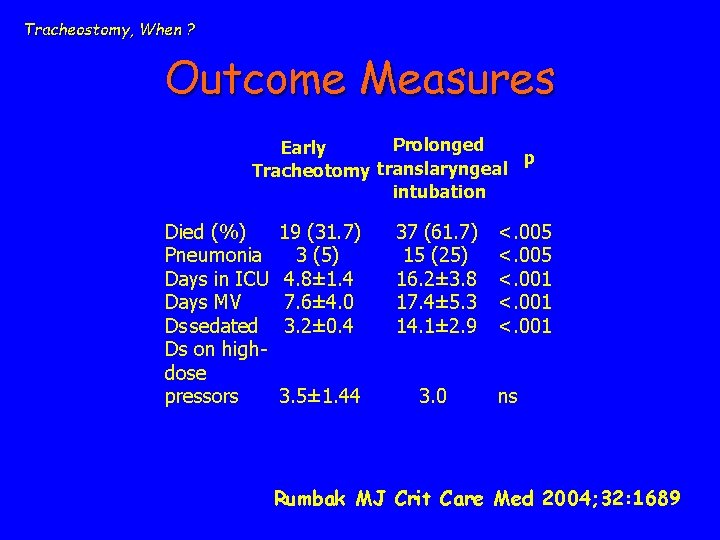
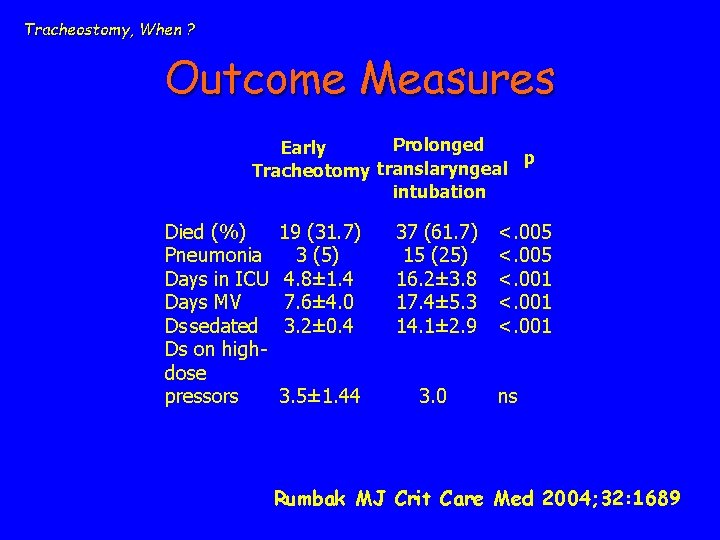
Tracheostomy, When ? Outcome Measures Prolonged Early p translaryngeal Tracheotomy intubation Died (%) Pneumonia Days in ICU Days MV Ds sedated Ds on highdose pressors 19 (31. 7) 3 (5) 4. 8± 1. 4 7. 6± 4. 0 3. 2± 0. 4 37 (61. 7) 15 (25) 16. 2± 3. 8 17. 4± 5. 3 14. 1± 2. 9 3. 5± 1. 44 3. 0 <. 005 <. 001 ns Rumbak MJ Crit Care Med 2004; 32: 1689
Weaning with Pressure Support Ventilation: Three situations • 1) Easy weaning (first attempt): detect as early as possible with daily screening + T-piece or low PSV trials, or use of CDS. • 2) difficult weaning (more than one attempt): reduce assistance (PSV) and daily tests with low PSV trials, or use assisted ventilation (ACV or PSV) + once daily T-piece or low PSV trials, or use of CDS. • 3) prolonged weaning (multiple attempts, tracheostomy): assisted ventilation (PSV or ACV) and prolonged “unassisted” trials with T-piece or low PSV; NIV? • For 2 and 3: search for factors impeding weaning.

 Respiratory
Respiratory Vent modes
Vent modes Consensus conference definition
Consensus conference definition Weaning oksigen
Weaning oksigen Weaning off amitriptyline 20 mg
Weaning off amitriptyline 20 mg Simplified weaning index
Simplified weaning index Weaning prolongado
Weaning prolongado Principles of weaning slideshare
Principles of weaning slideshare Weaning parameter
Weaning parameter China weaning fence
China weaning fence China weaning fence
China weaning fence Terminal weaning vs immediate extubation
Terminal weaning vs immediate extubation Meconium aspiration syndrome cxr
Meconium aspiration syndrome cxr Minute ventilation
Minute ventilation Mechanical ventilation firefighting
Mechanical ventilation firefighting 332 rule intubation
332 rule intubation Iron lung
Iron lung Mechanical ventilation settings
Mechanical ventilation settings Mechanical ventilation learning package
Mechanical ventilation learning package Tidal volume per kg
Tidal volume per kg Pinsp ventilation definition
Pinsp ventilation definition Purpose of mechanical ventilation
Purpose of mechanical ventilation Transpulmonary pressure formula
Transpulmonary pressure formula Dope mechanical ventilation
Dope mechanical ventilation Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Frameset trong html5
Frameset trong html5 Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Tư thế worm breton
Tư thế worm breton Bổ thể
Bổ thể ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Thế nào là giọng cùng tên
Thế nào là giọng cùng tên 101012 bằng
101012 bằng Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em