Weaning from Mechanical Ventilation Mazen Kherallah MD FCCP


- Slides: 35

Weaning from Mechanical Ventilation Mazen Kherallah, MD, FCCP Consultant Intensivist King Faisal Specialist Hospital & Research Center Assistant Professor University of North Dakota, USA www. icumedicus. com mkherallah@msn. com
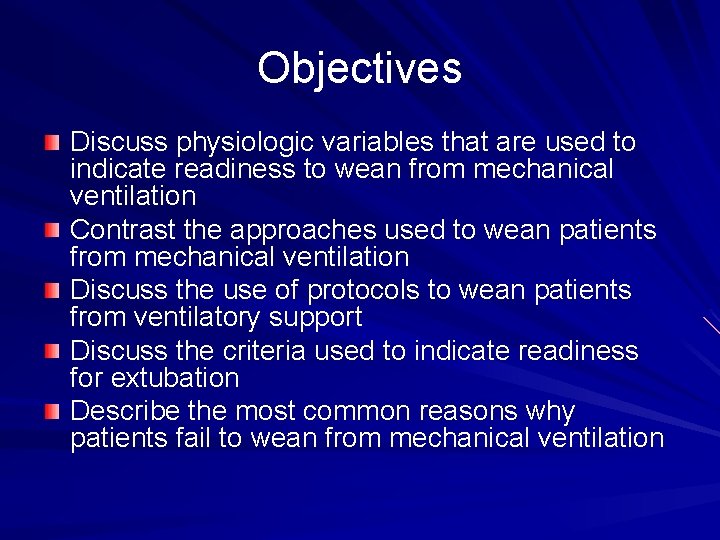
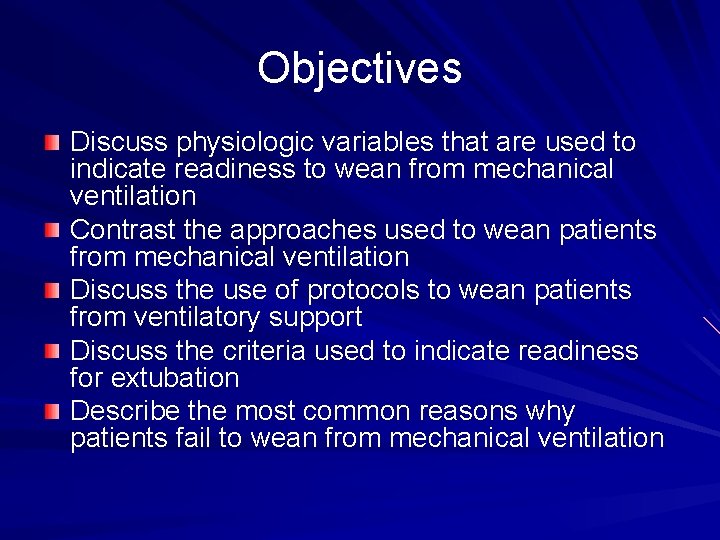
Objectives Discuss physiologic variables that are used to indicate readiness to wean from mechanical ventilation Contrast the approaches used to wean patients from mechanical ventilation Discuss the use of protocols to wean patients from ventilatory support Discuss the criteria used to indicate readiness for extubation Describe the most common reasons why patients fail to wean from mechanical ventilation

Introduction 75% of mechanically ventilated patients are easy to be weaned off the ventilator with simple process 10 -15% of patients require a use of a weaning protocol over a 24 -72 hours 5 -10% require a gradual weaning over longer time 1% of patients become chronically dependent on MV
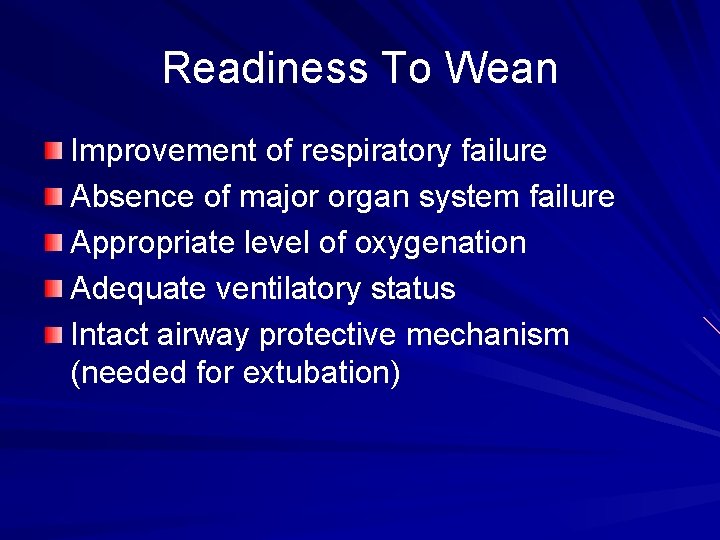
Readiness To Wean Improvement of respiratory failure Absence of major organ system failure Appropriate level of oxygenation Adequate ventilatory status Intact airway protective mechanism (needed for extubation)
Oxygenation Status Pa. O 2 ≥ 60 mm Hg Fi. O 2 ≤ 0. 40 PEEP ≤ 5 cm H 2 O
Ventilation Status Intact ventilatory drive: ability to control their own level of ventilation Respiratory rate < 30 Minute ventilation of < 12 L to maintain Pa. CO 2 in normal range VD/VT < 60% Functional respiratory muscles
Intact Airway Protective Mechanism Appropriate level of consciousness Cooperation Intact cough reflex Intact gag reflex Functional respiratory muscles with ability to support a strong and effective cough
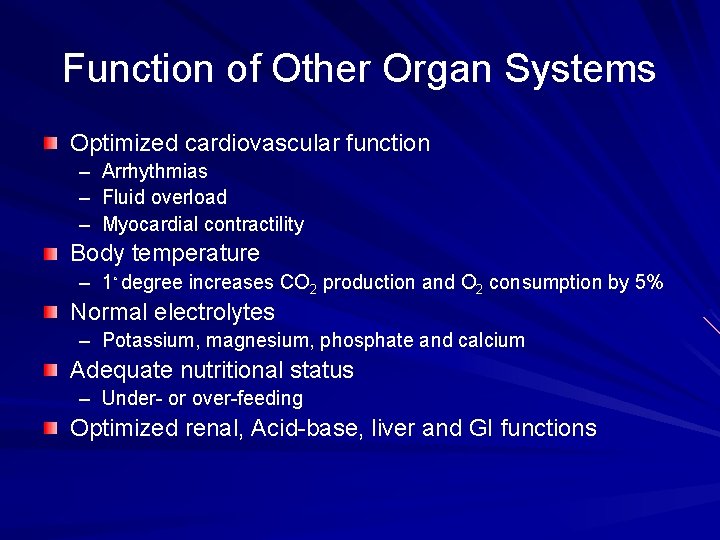
Function of Other Organ Systems Optimized cardiovascular function – Arrhythmias – Fluid overload – Myocardial contractility Body temperature – 1◦ degree increases CO 2 production and O 2 consumption by 5% Normal electrolytes – Potassium, magnesium, phosphate and calcium Adequate nutritional status – Under- or over-feeding Optimized renal, Acid-base, liver and GI functions
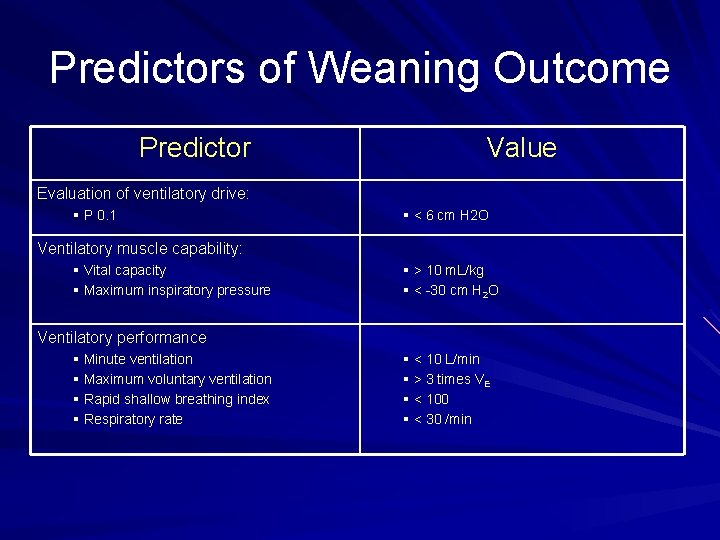
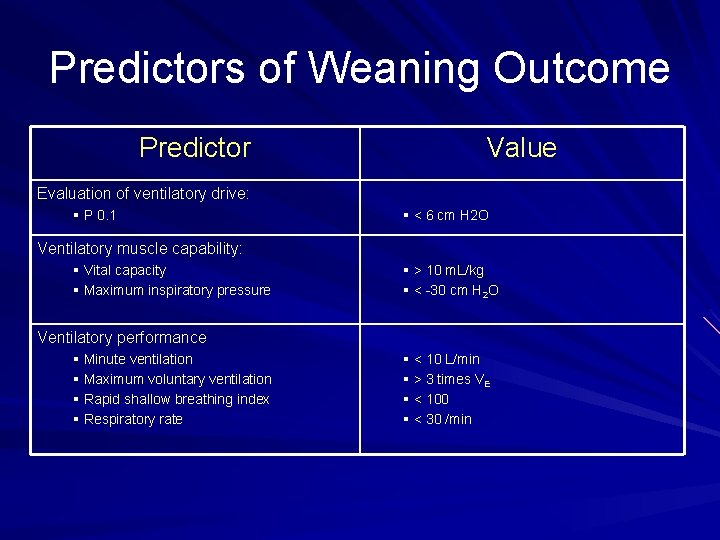
Predictors of Weaning Outcome Predictor Value Evaluation of ventilatory drive: § P 0. 1 § < 6 cm H 2 O Ventilatory muscle capability: § Vital capacity § Maximum inspiratory pressure § > 10 m. L/kg § < -30 cm H 2 O Ventilatory performance § Minute ventilation § Maximum voluntary ventilation § Rapid shallow breathing index § Respiratory rate § < 10 L/min § > 3 times VE § < 100 § < 30 /min
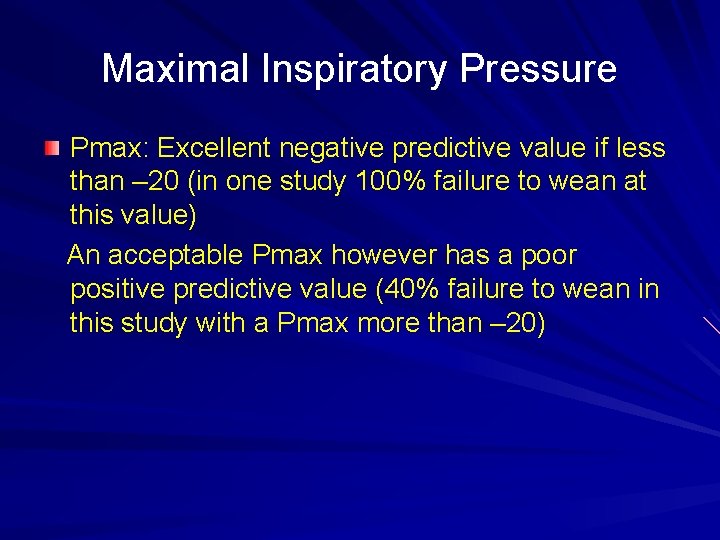
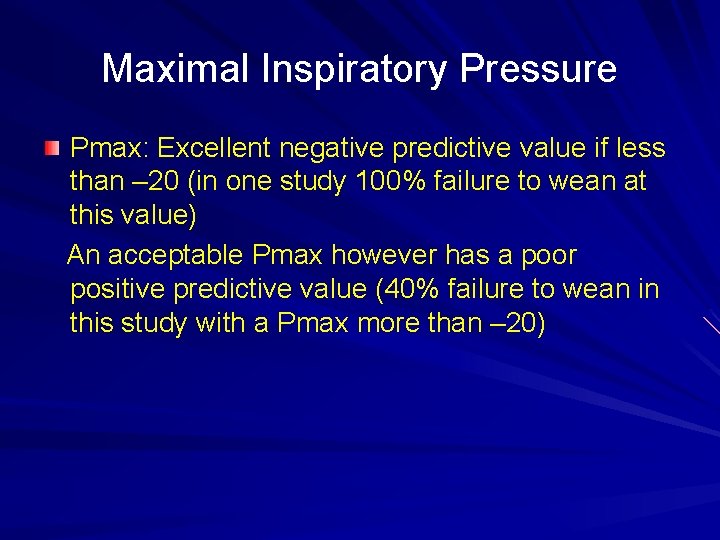
Maximal Inspiratory Pressure Pmax: Excellent negative predictive value if less than – 20 (in one study 100% failure to wean at this value) An acceptable Pmax however has a poor positive predictive value (40% failure to wean in this study with a Pmax more than – 20)
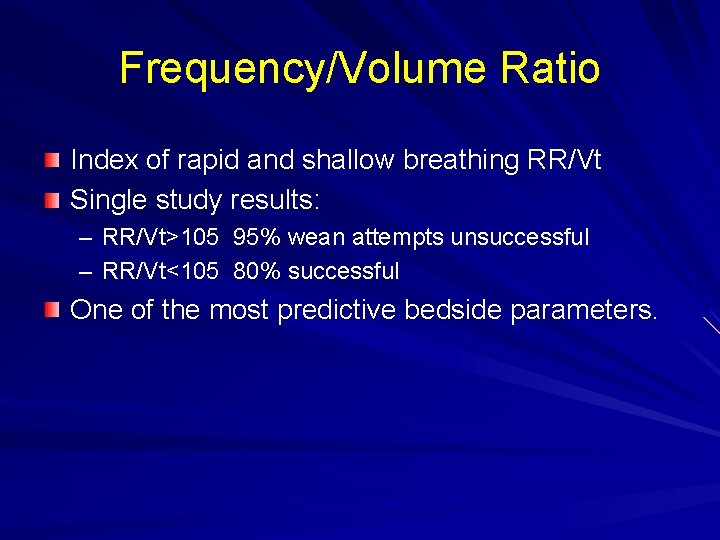
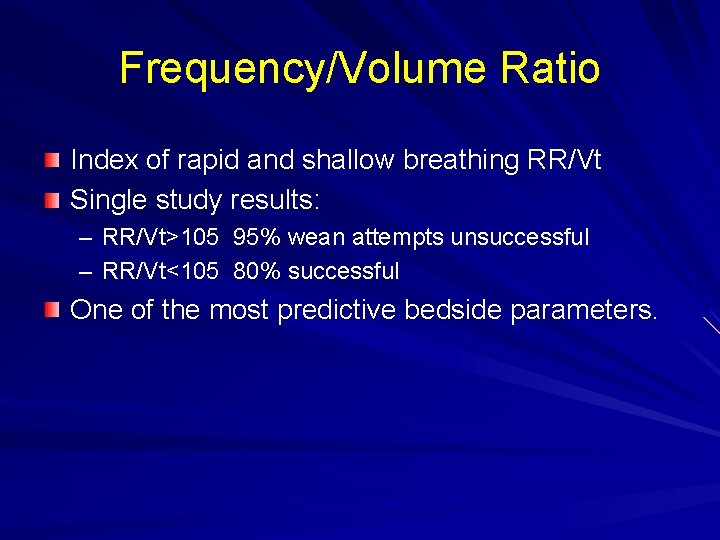
Frequency/Volume Ratio Index of rapid and shallow breathing RR/Vt Single study results: – RR/Vt>105 95% wean attempts unsuccessful – RR/Vt<105 80% successful One of the most predictive bedside parameters.
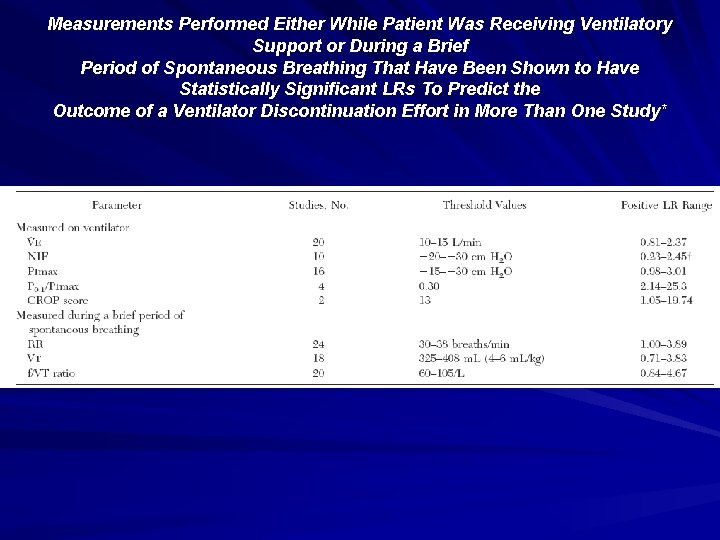
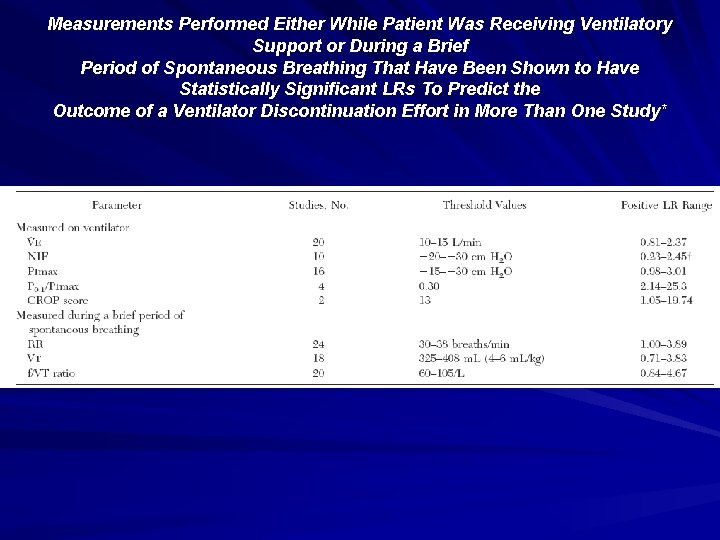
Measurements Performed Either While Patient Was Receiving Ventilatory Support or During a Brief Period of Spontaneous Breathing That Have Been Shown to Have Statistically Significant LRs To Predict the Outcome of a Ventilator Discontinuation Effort in More Than One Study*
Refertences 2 Tobin MJ, Alex CG. Discontinuation of mechanical ventilation. In: Tobin MJ, ed. Principles and practice of mechanical ventilation. New York, NY: Mc. Graw-Hill, 1994; 1177– 1206 4 Cook D, Meade M, Guyatt G, et al. Evidence report on criteria for weaning from mechanical ventilation. Rockville, MD: Agency for Health Care Policy and Research, 199910 Lopata M, Onal E. Mass loading, sleep apnea, and the pathogenesis of obesity hypoventilation. Am Rev Respir Dis 1982; 126: 640– 645 16 Hansen-Flaschen JH, Cowen J, Raps EC, et al. Neuromuscular blockade in the intensive care unit: more than we bargained for. Am Rev Respir Dis 1993; 147: 234– 236 18 Bellemare F, Grassino A. Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol 1982; 53: 1190– 1195 20 Roussos C, Macklem PT. The respiratory muscles. N Engl J Med 1982; 307: 786– 797 24 Le Bourdelles G, Viires N, Boezkowski J, et al. Effects of mechanical ventilation on diaphragmatic contractile properties in rats. Am J Respir Crit Care Med 1994; 149: 1539– 1544
Approaches To Weaning Spontaneous breathing trials Pressure support ventilation (PSV) SIMV New weaning modes
Do Not Wean To Exhaustion
Spontaneous Breathing Trials SBT to assess extubation readiness – T-piece or CPAP 5 cm H 2 O – 30 -120 minutes trials – If tolerated, patient can be extubated SBT as a weaning method – Increasing length of SBT trials – Periods of rest between trials and at night
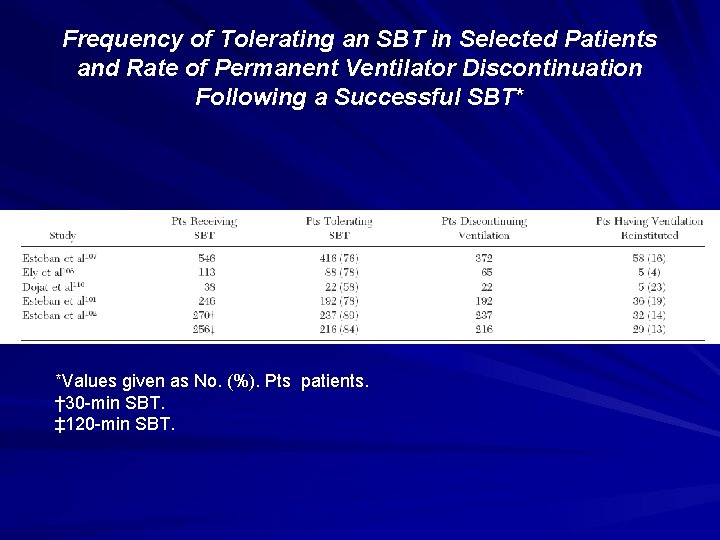
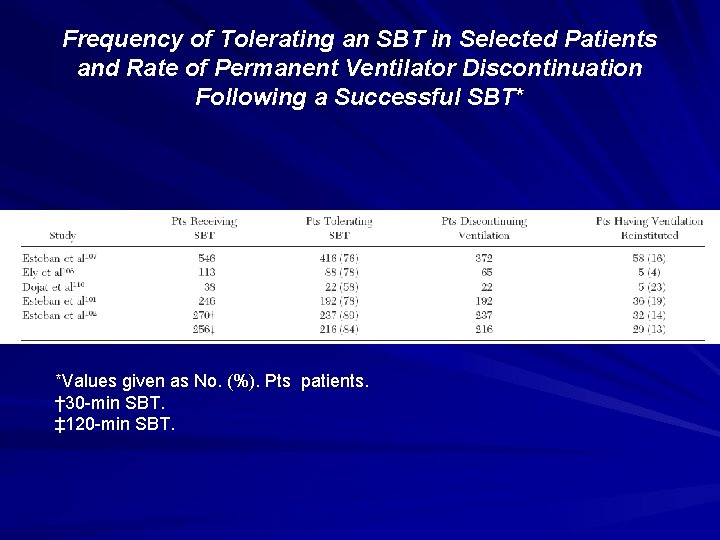
Frequency of Tolerating an SBT in Selected Patients and Rate of Permanent Ventilator Discontinuation Following a Successful SBT* *Values given as No. (%). Pts patients. † 30 -min SBT. ‡ 120 -min SBT.
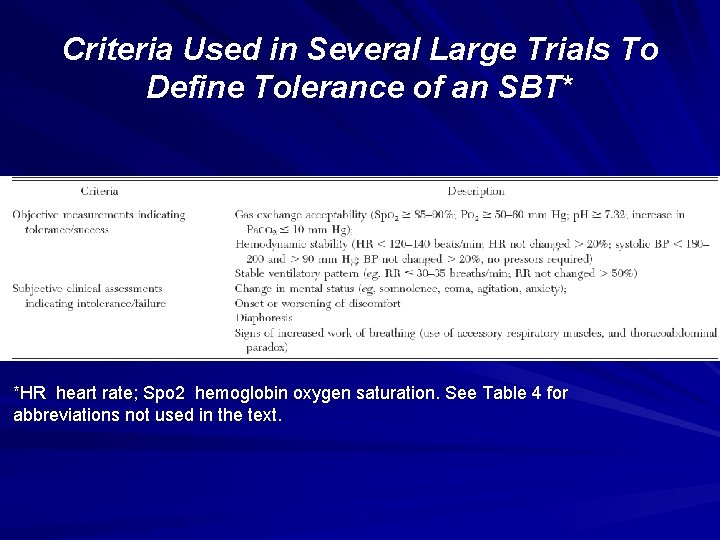
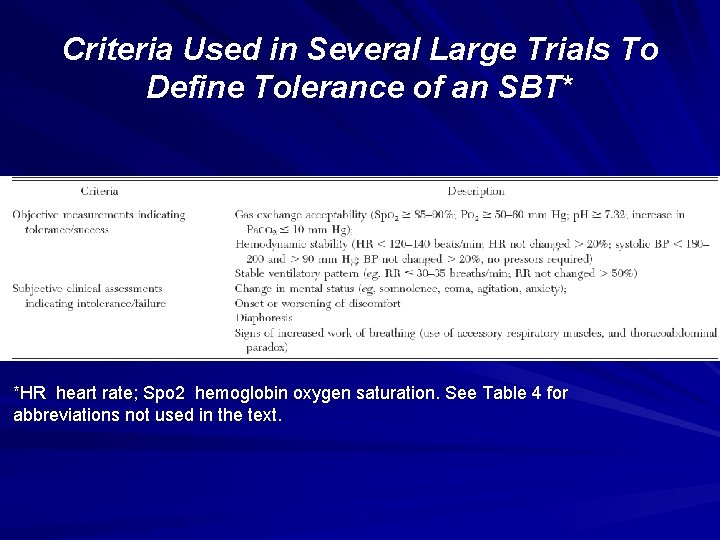
Criteria Used in Several Large Trials To Define Tolerance of an SBT* *HR heart rate; Spo 2 hemoglobin oxygen saturation. See Table 4 for abbreviations not used in the text.
Pressure Support Gradual reduction in the level of PSV that prevents activation of accessory muscles Gradula decrease on regular basis (hours or days) to minimum level of 5 -8 cm H 2 O Once the patient is capable of maintaining the target ventilatory pattern and gas exchange at this level, MV is discontinued
SIMV Gradual decrease in mandatory breaths It may be applied with PSV Has the worst weaning outcomes in clinical trials Its use is not recommended
New Modes Volume support Automode MMV ATC
Protocols Developed by multidisciplinary team Implemented by respiratory therapists and nurses to make clinical decisions Results in shorter weaning times and shorter length of mechanical ventilation than physician-directed weaning
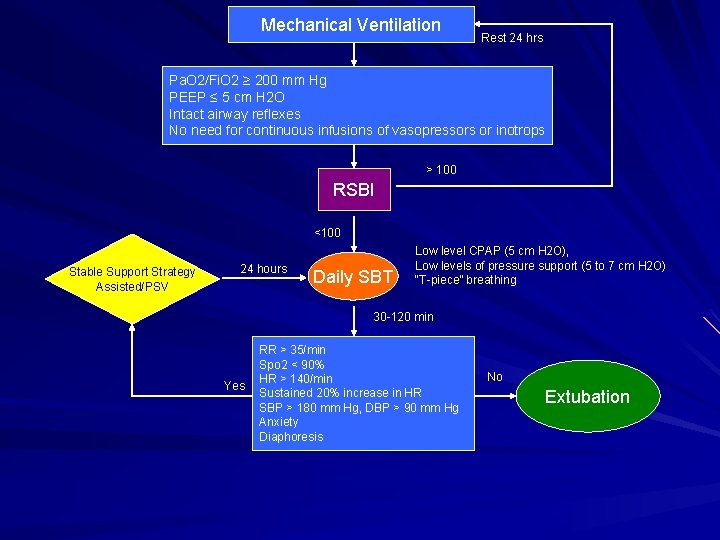
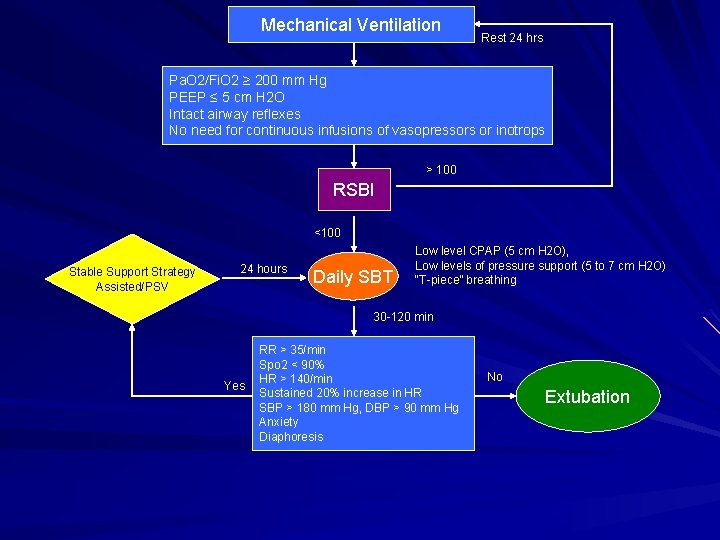
Mechanical Ventilation Rest 24 hrs Pa. O 2/Fi. O 2 ≥ 200 mm Hg PEEP ≤ 5 cm H 2 O Intact airway reflexes No need for continuous infusions of vasopressors or inotrops > 100 RSBI <100 Stable Support Strategy Assisted/PSV 24 hours Daily SBT Low level CPAP (5 cm H 2 O), Low levels of pressure support (5 to 7 cm H 2 O) “T-piece” breathing 30 -120 min Yes RR > 35/min Spo 2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis No Extubation
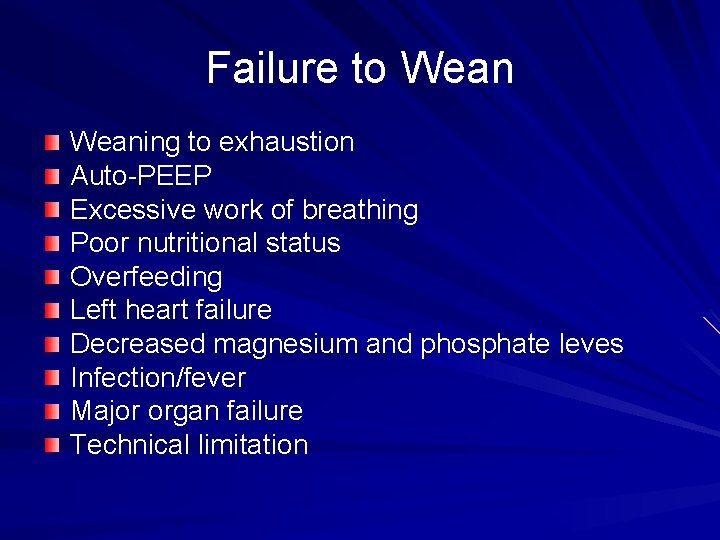
Failure to Weaning to exhaustion Auto-PEEP Excessive work of breathing Poor nutritional status Overfeeding Left heart failure Decreased magnesium and phosphate leves Infection/fever Major organ failure Technical limitation
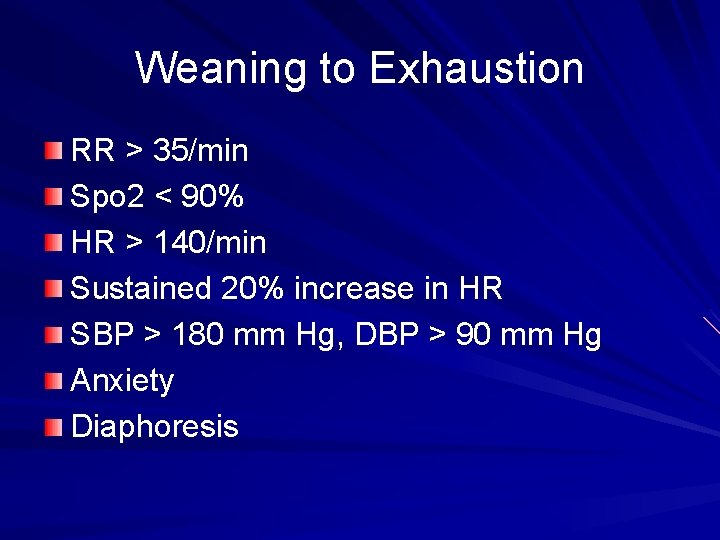
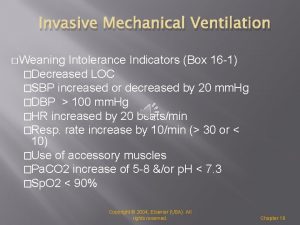
Weaning to Exhaustion RR > 35/min Spo 2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis
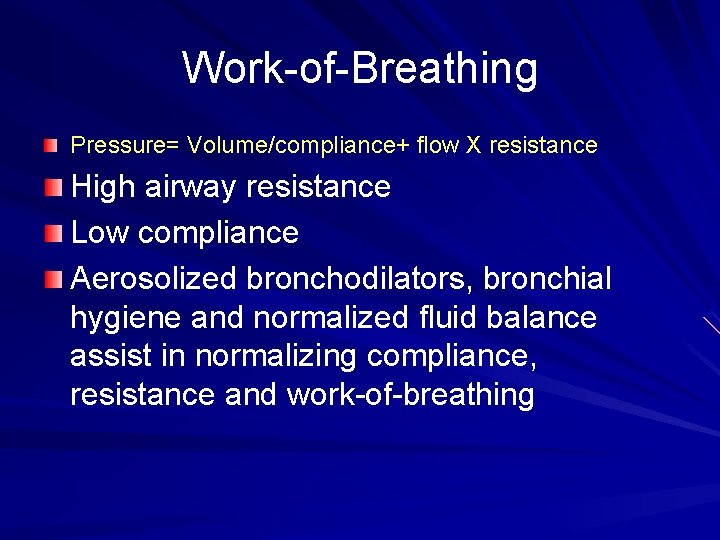
Work-of-Breathing Pressure= Volume/compliance+ flow X resistance High airway resistance Low compliance Aerosolized bronchodilators, bronchial hygiene and normalized fluid balance assist in normalizing compliance, resistance and work-of-breathing
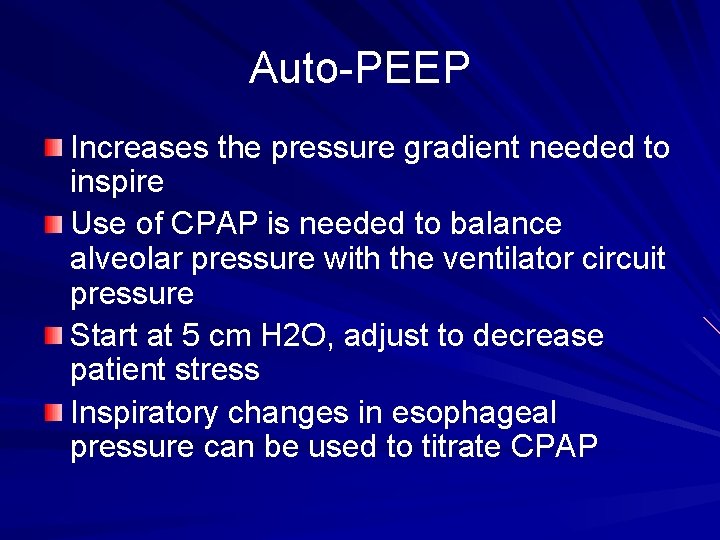
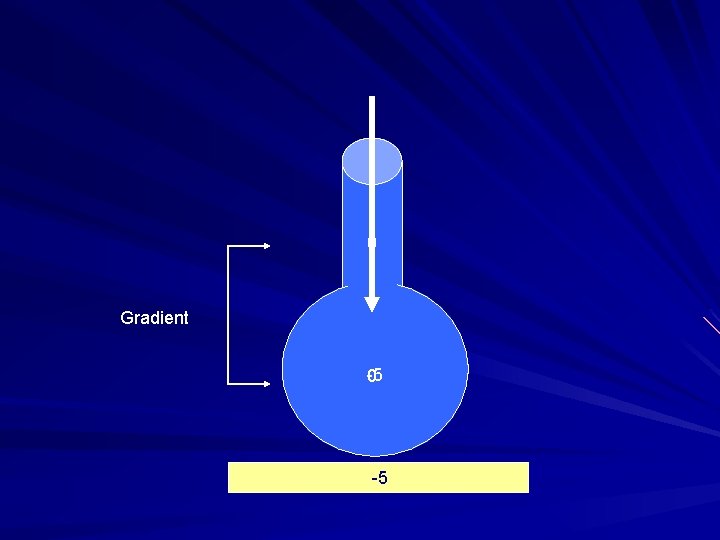
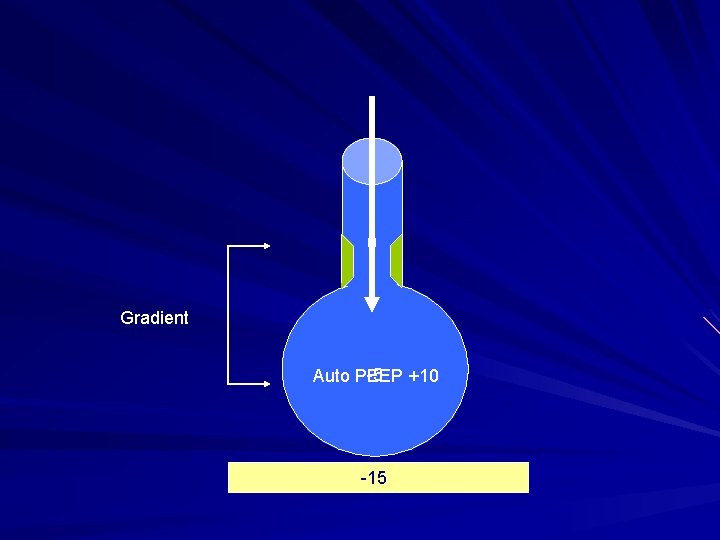
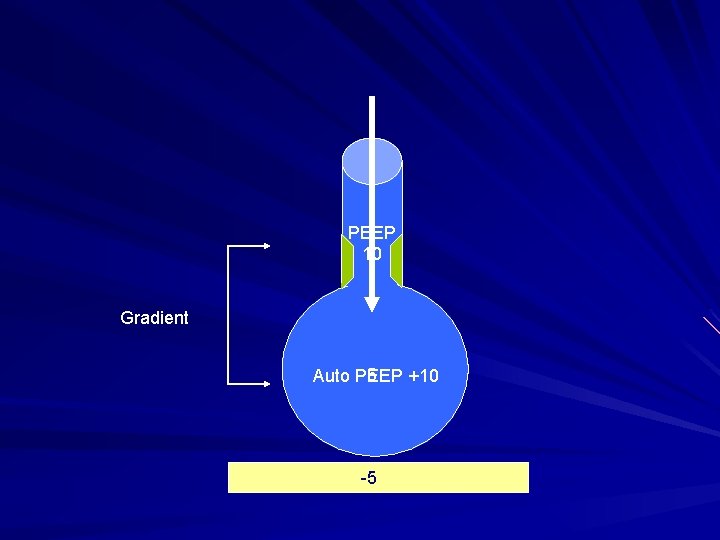
Auto-PEEP Increases the pressure gradient needed to inspire Use of CPAP is needed to balance alveolar pressure with the ventilator circuit pressure Start at 5 cm H 2 O, adjust to decrease patient stress Inspiratory changes in esophageal pressure can be used to titrate CPAP
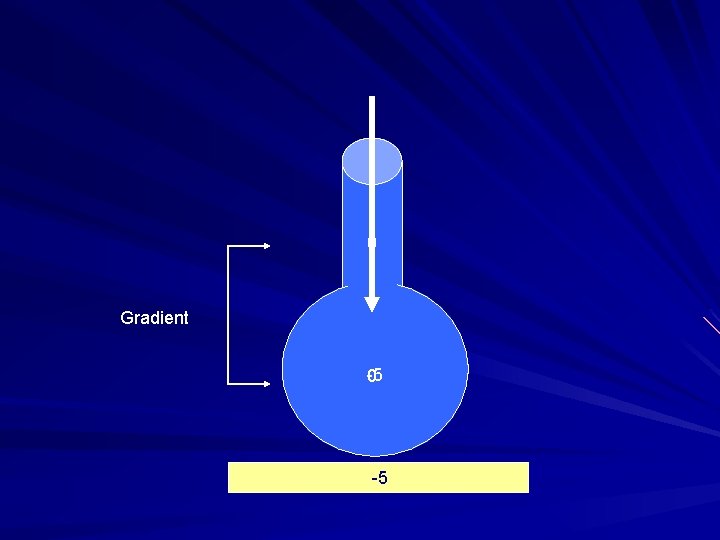
0 Gradient -5 0 -5
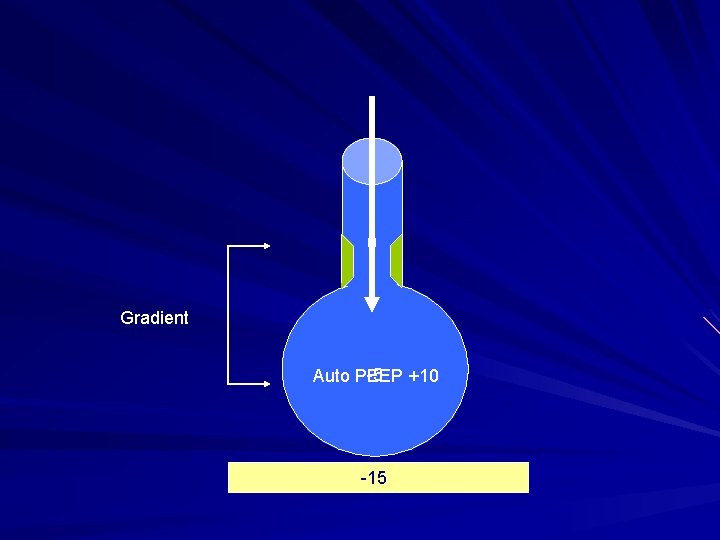
0 Gradient -5 +10 Auto PEEP -15
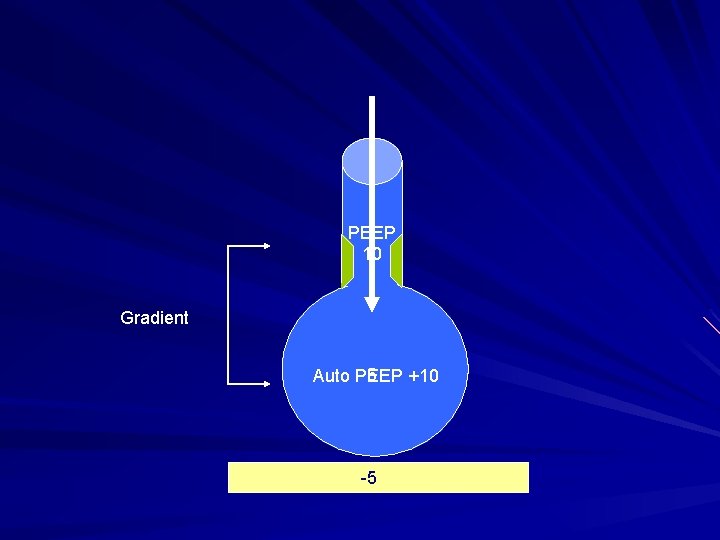
PEEP 10 Gradient 5 Auto PEEP +10 -5
Left Heart Failure Increased metabolic demands that are associated with the transition from mechanical ventilation to spontaneous breathing Increases in venous return as that is associated with the negative pressure ventilation and the contracting diaphragm which results into an increase in PCWP and pulmonary edema Appropriate management of cardiovascular status is necessary before weaning will be successful
Nutritional/Electrolytes Imbalance of electrolytes causes muscular weakness Nutritional support improves outcome Overfeeding elevates CO 2 production due to excessive carbohydrate ingestion
Infection/Fever/Organ Failure Organ failure precipitate weaning failure Infection and fever increase O 2 consumption and CO 2 production resulting in an increase ventilatory drive
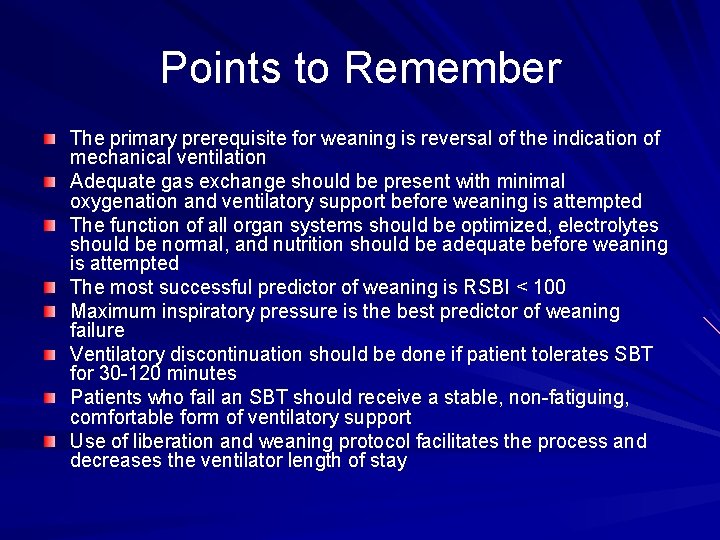
Points to Remember The primary prerequisite for weaning is reversal of the indication of mechanical ventilation Adequate gas exchange should be present with minimal oxygenation and ventilatory support before weaning is attempted The function of all organ systems should be optimized, electrolytes should be normal, and nutrition should be adequate before weaning is attempted The most successful predictor of weaning is RSBI < 100 Maximum inspiratory pressure is the best predictor of weaning failure Ventilatory discontinuation should be done if patient tolerates SBT for 30 -120 minutes Patients who fail an SBT should receive a stable, non-fatiguing, comfortable form of ventilatory support Use of liberation and weaning protocol facilitates the process and decreases the ventilator length of stay
 Minute ventilation
Minute ventilation Weaning ventilation
Weaning ventilation Mode of ventilation
Mode of ventilation Weaning prolongado
Weaning prolongado Simplified weaning index
Simplified weaning index Mazen zenati
Mazen zenati Weight loss after stopping amitriptyline
Weight loss after stopping amitriptyline Terminal weaning vs immediate extubation
Terminal weaning vs immediate extubation Dr mazen al hakim
Dr mazen al hakim China weaning fence
China weaning fence Tidal volume normal range
Tidal volume normal range Principles of weaning slideshare
Principles of weaning slideshare Mazen arakji
Mazen arakji Va ecmo indications
Va ecmo indications Mazen zenati
Mazen zenati Mazen salloum
Mazen salloum Weaning oksigen
Weaning oksigen Dr mazen abou chaaban
Dr mazen abou chaaban Furoseride
Furoseride China weaning fence
China weaning fence Iron lung
Iron lung Indication for mechanical ventilation
Indication for mechanical ventilation Mechanical ventilation learning package
Mechanical ventilation learning package Tidal volume normal range
Tidal volume normal range ütube
ütube Types of ventilation fire fighting
Types of ventilation fire fighting Purpose of mechanical ventilation
Purpose of mechanical ventilation Basic terms and concepts of mechanical ventilation
Basic terms and concepts of mechanical ventilation Positive end expiratory pressure
Positive end expiratory pressure Mechanical ventilation indications
Mechanical ventilation indications Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Difference between right and left bronchus
Difference between right and left bronchus Non invasive ventilation
Non invasive ventilation Dyspnea index calculation formula
Dyspnea index calculation formula Refrigeration and air conditioning ppt
Refrigeration and air conditioning ppt Fläktförstärkt självdrag
Fläktförstärkt självdrag