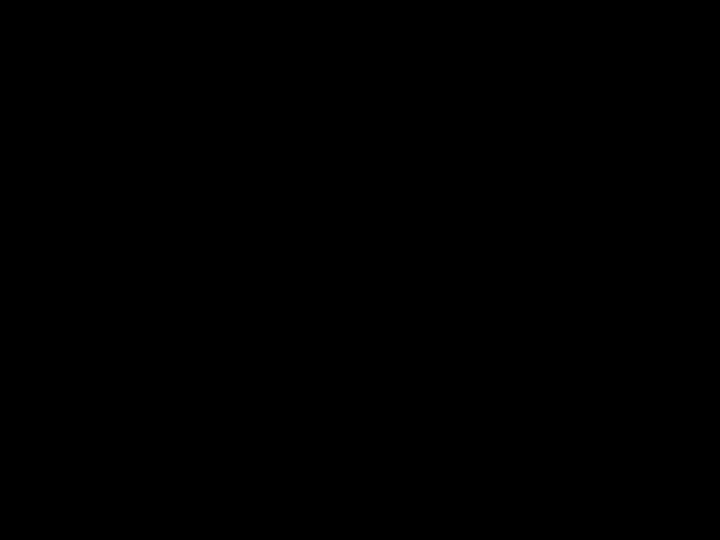
Weaning from mechanical ventilation Newth C et al
- Slides: 46
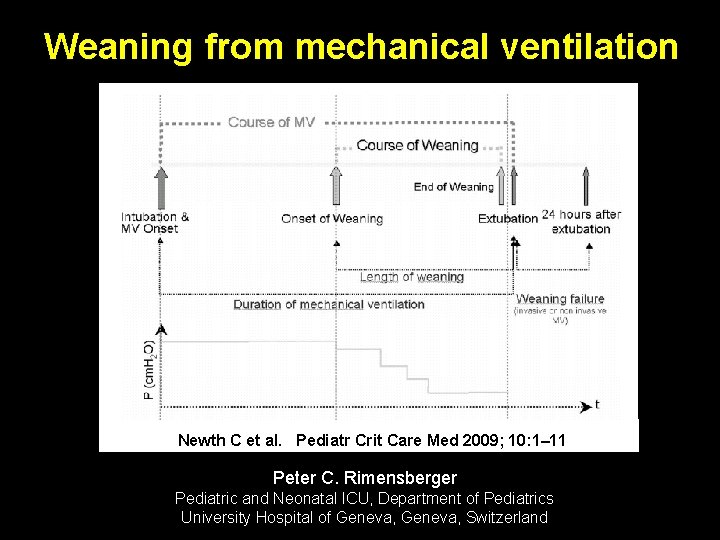
Weaning from mechanical ventilation Newth C et al. Pediatr Crit Care Med 2009; 10: 1– 11 Peter C. Rimensberger Pediatric and Neonatal ICU, Department of Pediatrics University Hospital of Geneva, Switzerland
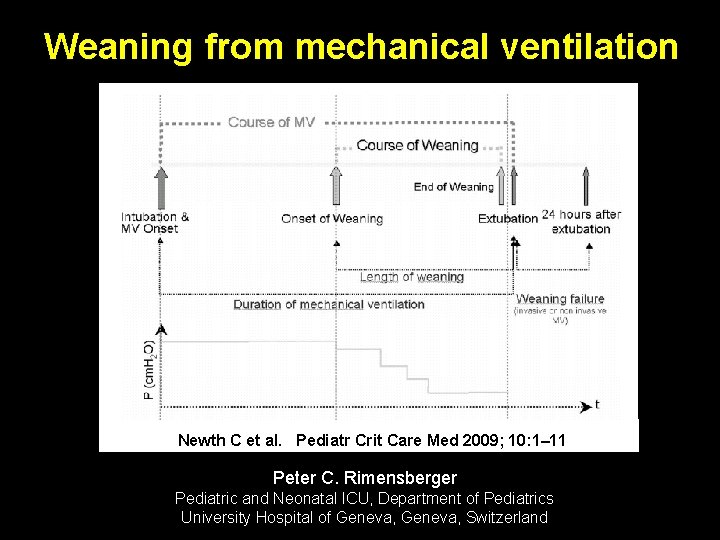
Weaning / Extubation failure: Is it a real problem in the PICU ? Reported extubation failure rates in PICUs range from 4. 1% to 19% Baisch SD, Wheeler WB, Kurachek SC, Cornfield DN. Extubation failure in pediatric intensive care incidence and outcomes. Pediatr Crit Care Med 2005; 6: 312– 318. Edmunds S, Weiss I, Harrison R. Extubation failure in a large pediatric ICU population. Chest 2001; 119: 897– 900. Fontela PS, Piva JP, Garcia PC, et al. Risk factors for extubation failure inmechanically ventilated pediatric patients. Pediatr Crit Care Med 2005; 6166– 170.
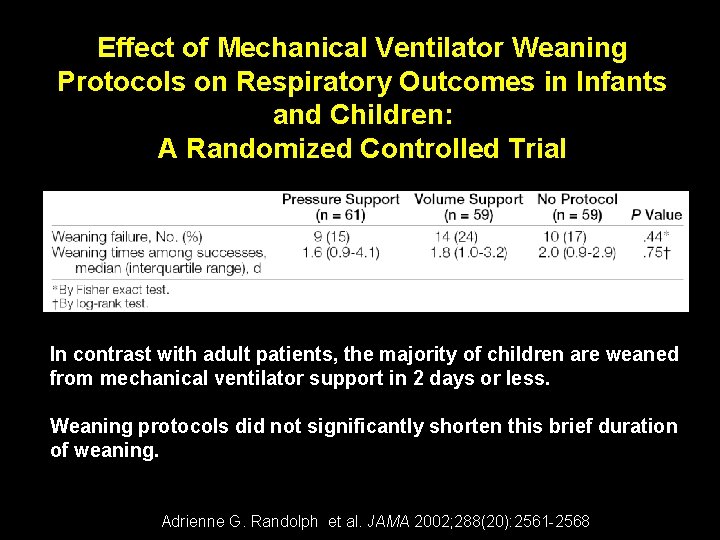
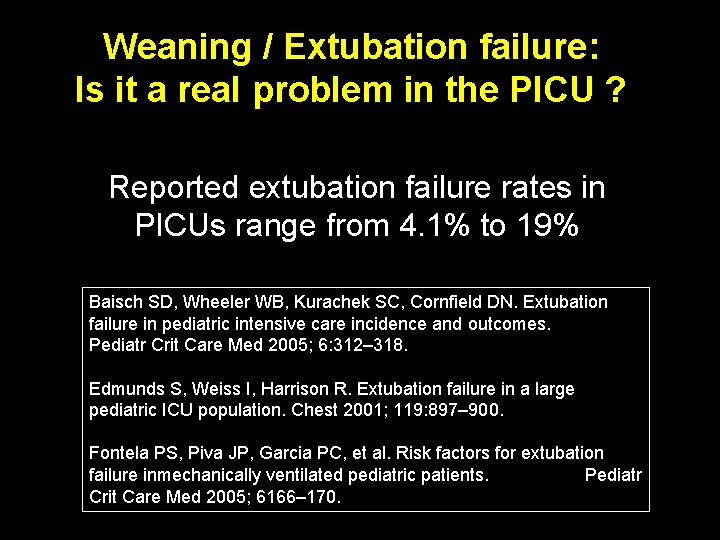
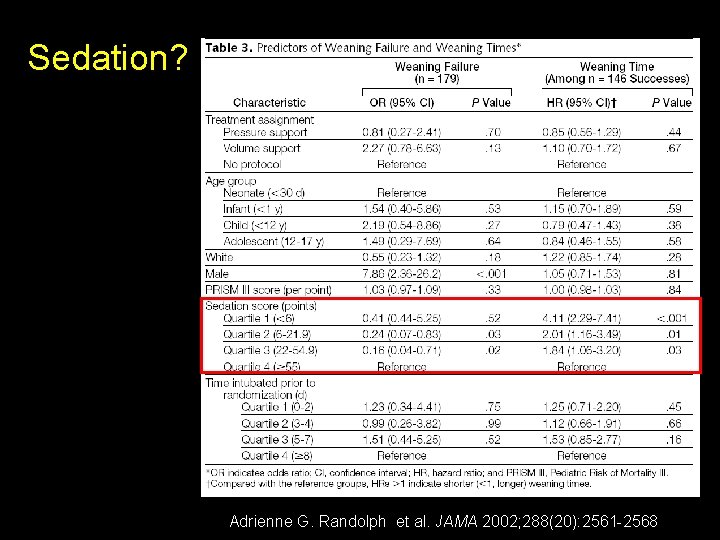
Effect of Mechanical Ventilator Weaning Protocols on Respiratory Outcomes in Infants and Children: A Randomized Controlled Trial In contrast with adult patients, the majority of children are weaned from mechanical ventilator support in 2 days or less. Weaning protocols did not significantly shorten this brief duration of weaning. Adrienne G. Randolph et al. JAMA 2002; 288(20): 2561 -2568
Weaning: The key questions 1. Is the cause of respiratory failure gone or getting better ? 2. Is the patient well oxygenated and ventilated ? 3. Can the heart tolerate the increased work of breathing ?
Discontinuation of Mechanical Ventilation To discontinue mechanical ventilation requires: – Patient preparation – Assessment of readiness Ø For independent breathing Ø For extubation – A brief trial of minimally assisted breathing Ø An assessment of probable upper airway patency after extubation – Either abrupt or gradual withdrawal of positive pressure, depending on the patient’s readiness
Factors that may contribute to extubation failure in pediatric patients • young age • duration of mechanical ventilation • prolonged treatment with sedatives and analgesics Fontela PS, Piva JP, Garcia PC, et al. Risk factors for extubation failure in mechanically ventilated pediatric patients. Pediatr Crit Care Med 2005; 6166– 170.
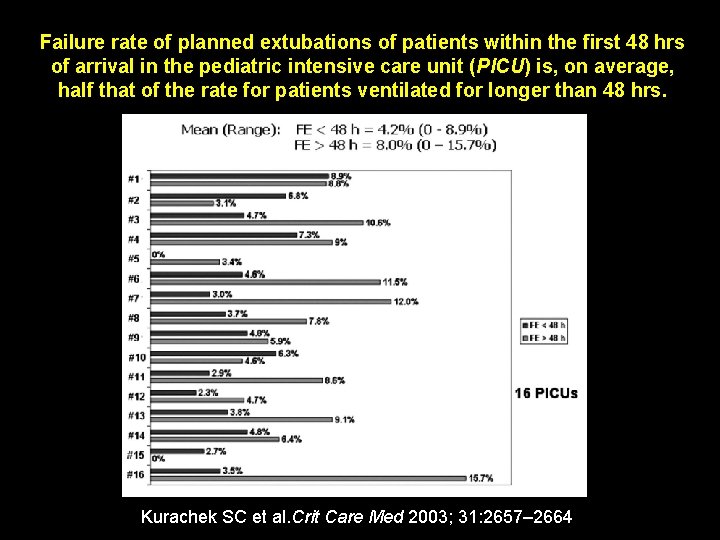
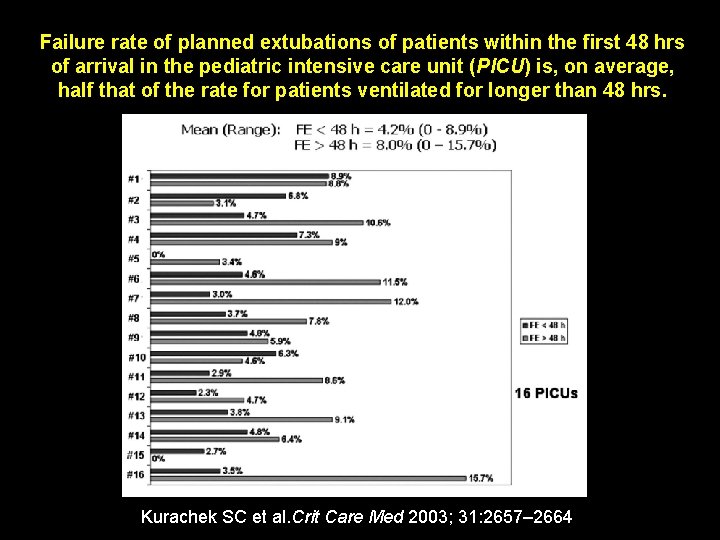
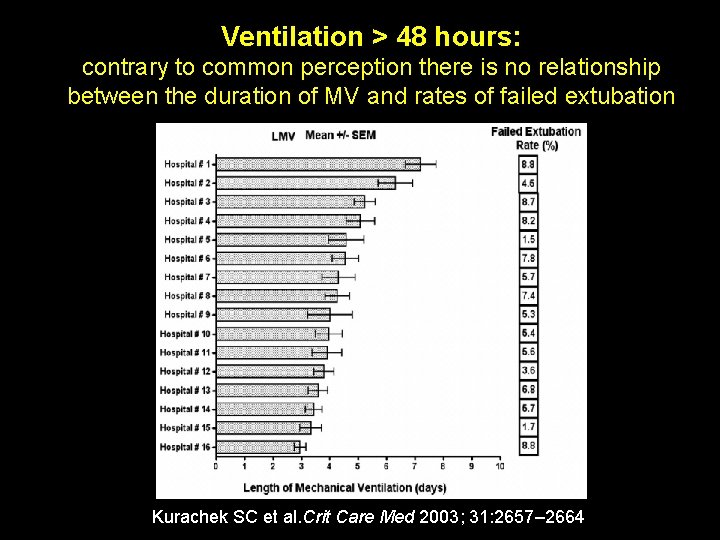
Failure rate of planned extubations of patients within the first 48 hrs of arrival in the pediatric intensive care unit (PICU) is, on average, half that of the rate for patients ventilated for longer than 48 hrs. Kurachek SC et al. Crit Care Med 2003; 31: 2657– 2664
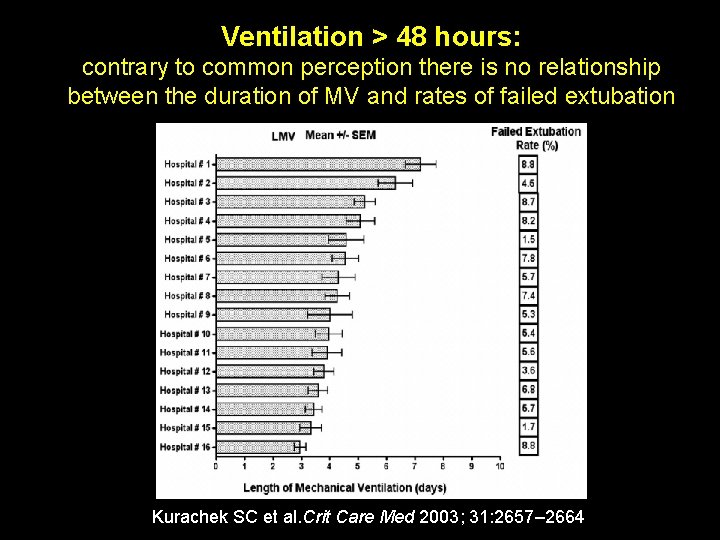
Ventilation > 48 hours: contrary to common perception there is no relationship between the duration of MV and rates of failed extubation Kurachek SC et al. Crit Care Med 2003; 31: 2657– 2664
Concepts of Weaning
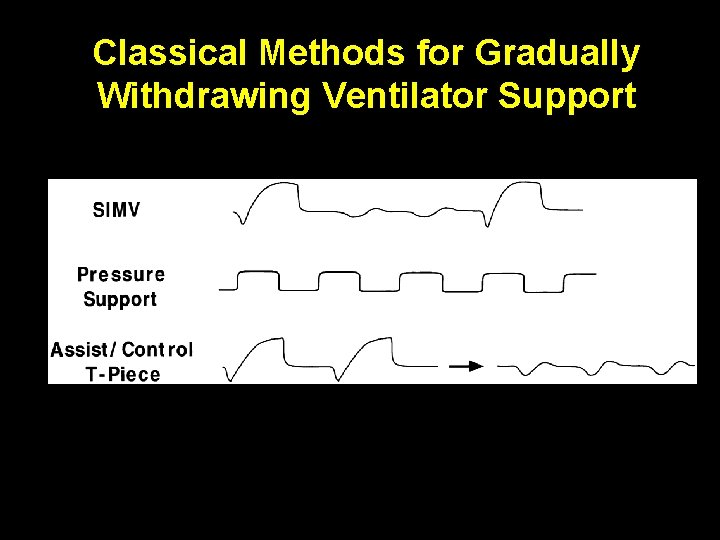
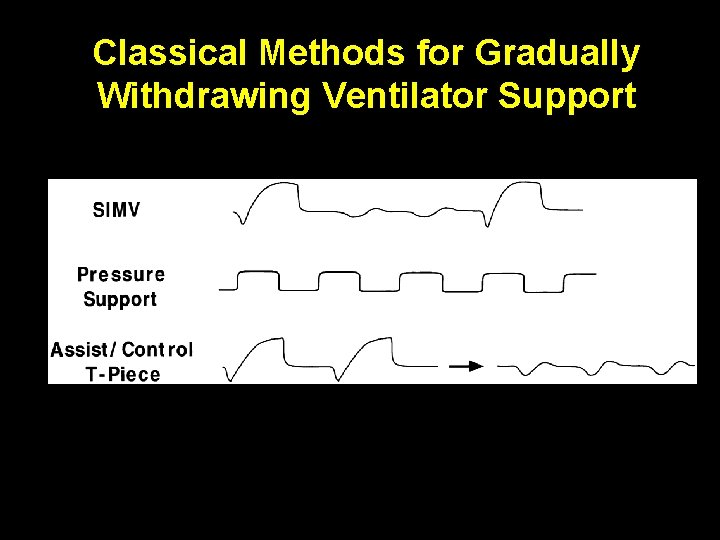
Classical Methods for Gradually Withdrawing Ventilator Support
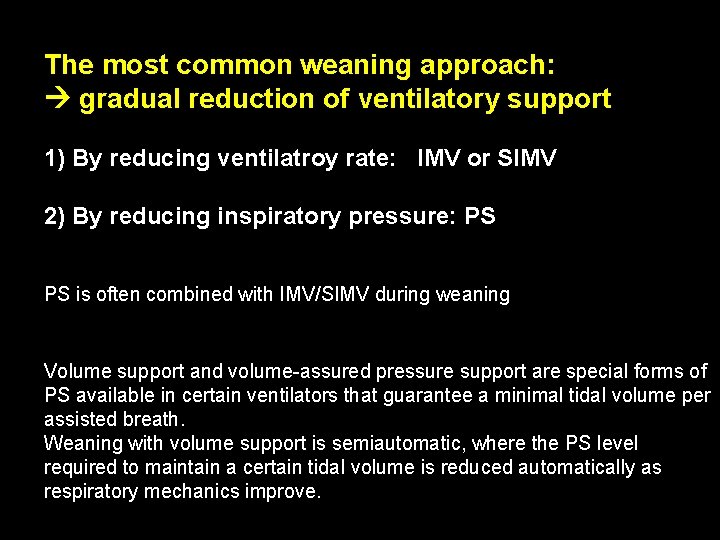
The most common weaning approach: gradual reduction of ventilatory support 1) By reducing ventilatroy rate: IMV or SIMV 2) By reducing inspiratory pressure: PS PS is often combined with IMV/SIMV during weaning Volume support and volume-assured pressure support are special forms of PS available in certain ventilators that guarantee a minimal tidal volume per assisted breath. Weaning with volume support is semiautomatic, where the PS level required to maintain a certain tidal volume is reduced automatically as respiratory mechanics improve.
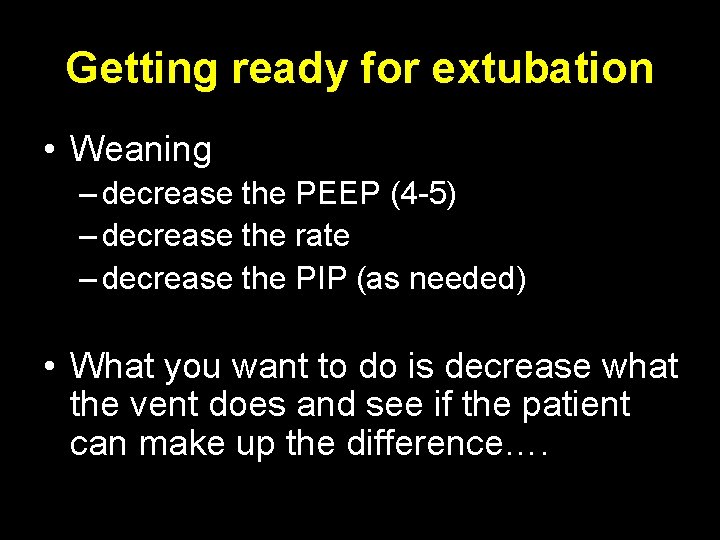
Getting ready for extubation • Weaning – decrease the PEEP (4 -5) – decrease the rate – decrease the PIP (as needed) • What you want to do is decrease what the vent does and see if the patient can make up the difference….
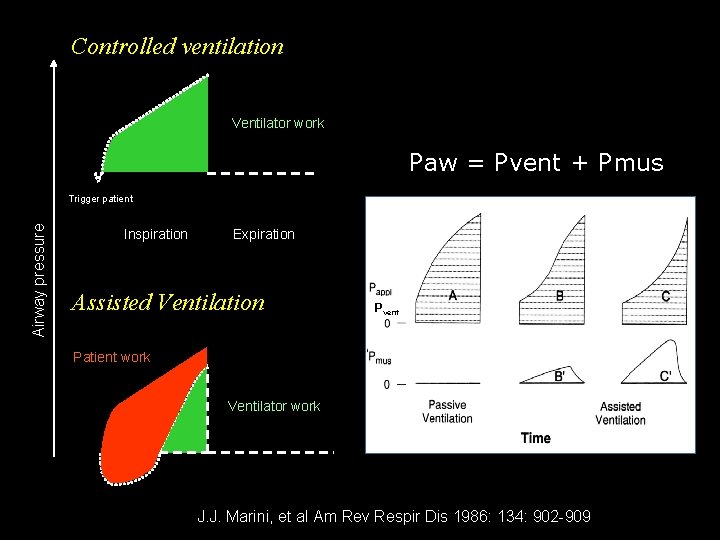
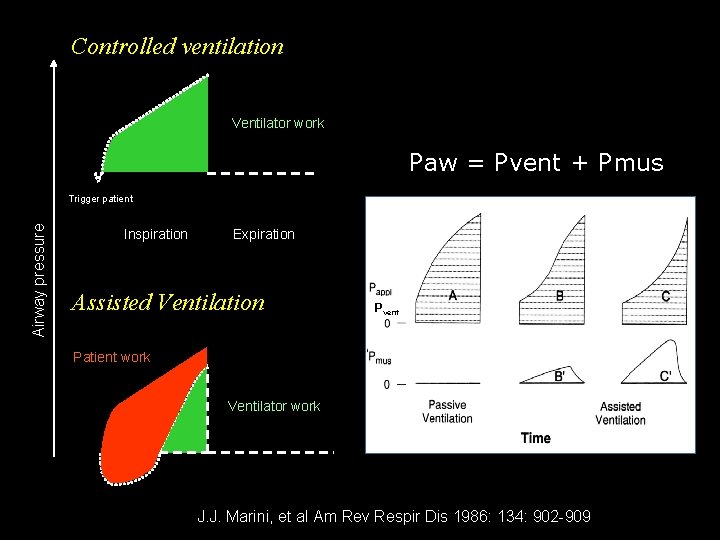
Controlled ventilation Ventilator work Paw = Pvent + Pmus Airway pressure Trigger patient Inspiration Expiration Assisted Ventilation Pvent Patient work Ventilator work J. J. Marini, et al Am Rev Respir Dis 1986: 134: 902 -909
Spontaneous Breathing Trials and Extubation Readiness Tests
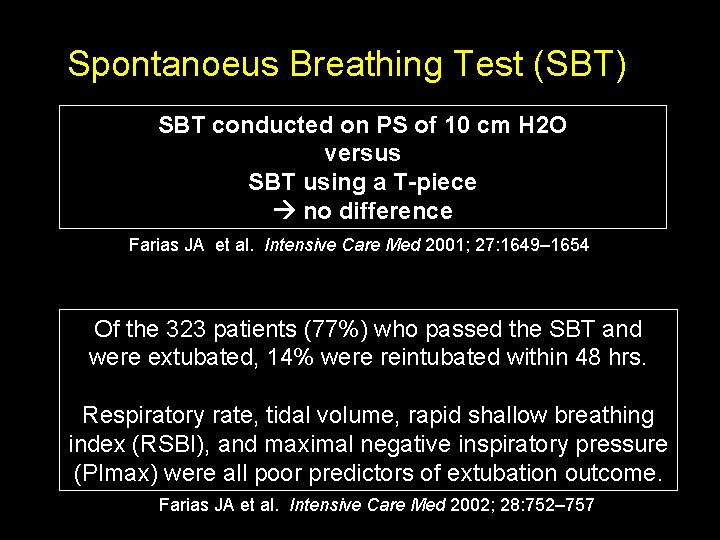
Spontanoeus Breathing Test (SBT) SBT conducted on PS of 10 cm H 2 O versus SBT using a T-piece no difference Farias JA et al. Intensive Care Med 2001; 27: 1649– 1654 Of the 323 patients (77%) who passed the SBT and were extubated, 14% were reintubated within 48 hrs. Respiratory rate, tidal volume, rapid shallow breathing index (RSBI), and maximal negative inspiratory pressure (PImax) were all poor predictors of extubation outcome. Farias JA et al. Intensive Care Med 2002; 28: 752– 757
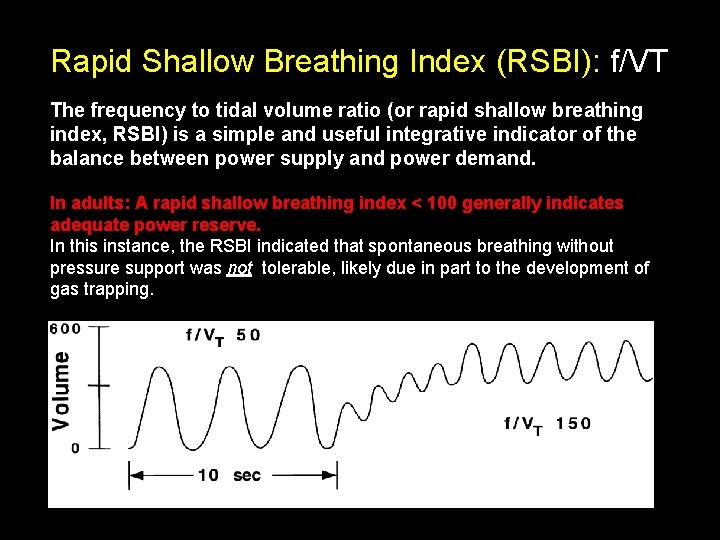
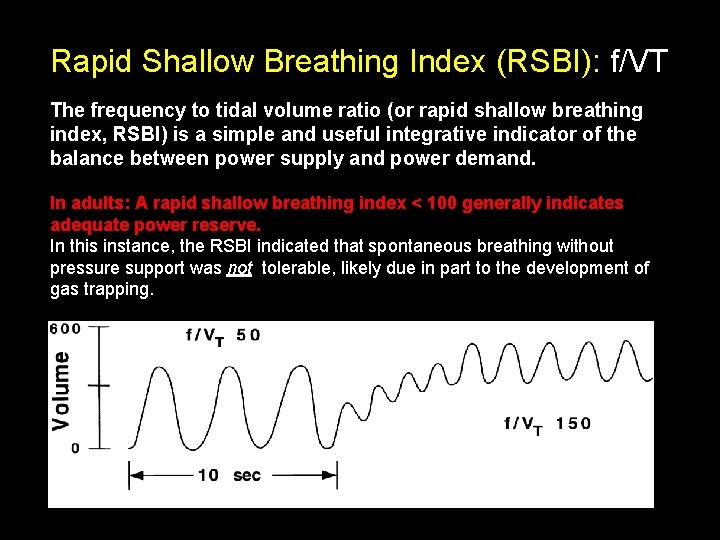
Rapid Shallow Breathing Index (RSBI): f/VT The frequency to tidal volume ratio (or rapid shallow breathing index, RSBI) is a simple and useful integrative indicator of the balance between power supply and power demand. In adults: A rapid shallow breathing index < 100 generally indicates adequate power reserve. In this instance, the RSBI indicated that spontaneous breathing without pressure support was not tolerable, likely due in part to the development of gas trapping.
Limitations of RSBI in children wide range of age groups with different respiratory rates
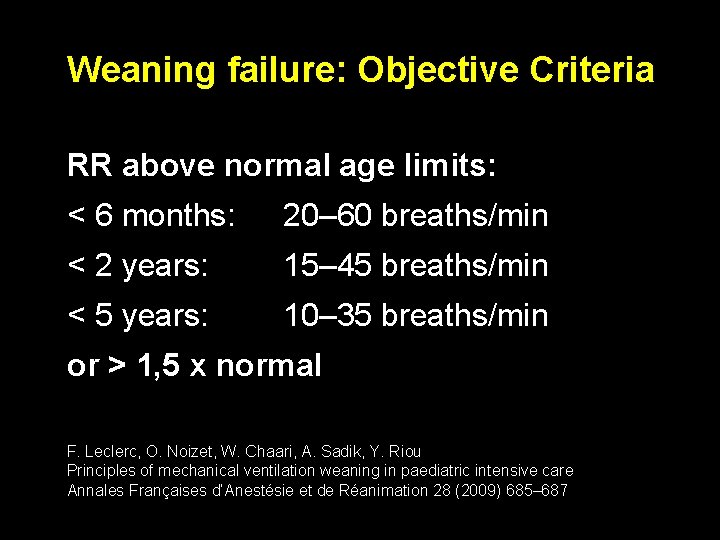
Weaning failure: Objective Criteria RR above normal age limits: < 6 months: 20– 60 breaths/min < 2 years: 15– 45 breaths/min < 5 years: 10– 35 breaths/min or > 1, 5 x normal F. Leclerc, O. Noizet, W. Chaari, A. Sadik, Y. Riou Principles of mechanical ventilation weaning in paediatric intensive care Annales Françaises d’Anestésie et de Réanimation 28 (2009) 685– 687
Rapid Shallow Breathing Index (RSBI): f/VT Compliance, Resistance, Oxygenation, Pressure Index (CROP Index): (Dynamic Compliance x Maximal Negative Inspiratory Pressure x (Pa. O 2/PAO 2)/ Respiratory Rate)
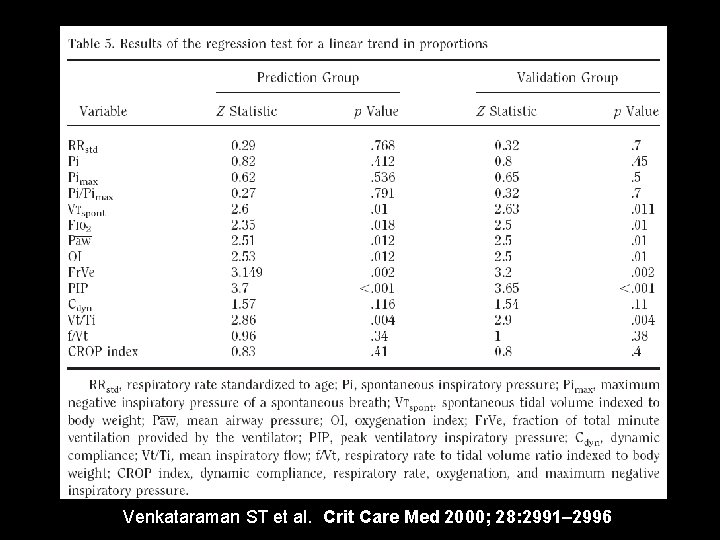
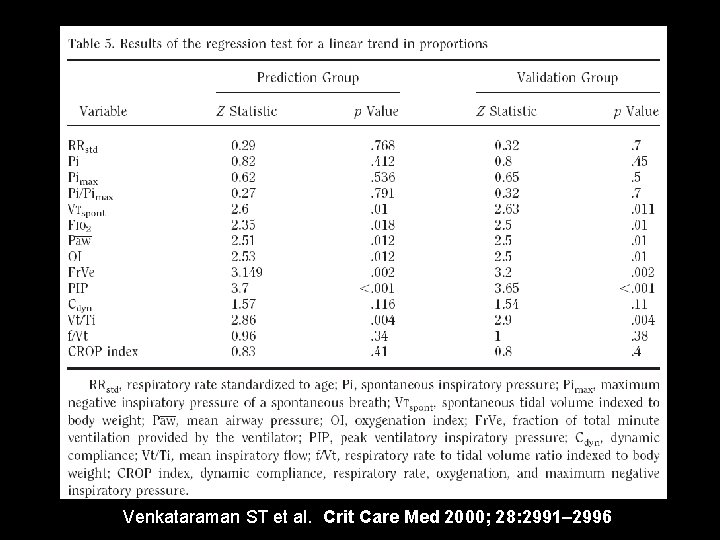
Venkataraman ST et al. Crit Care Med 2000; 28: 2991– 2996
Rapid Shallow Breathing Index (RSBI): f/VT Compliance, Resistance, Oxygenation, Pressure Index (CROP Index): (Dynamic Compliance x Maximal Negative Inspiratory Pressure x (Pa. O 2/PAO 2)/ Respiratory Rate) Volumetric Capnography: physiologic dead space (VD/VT)
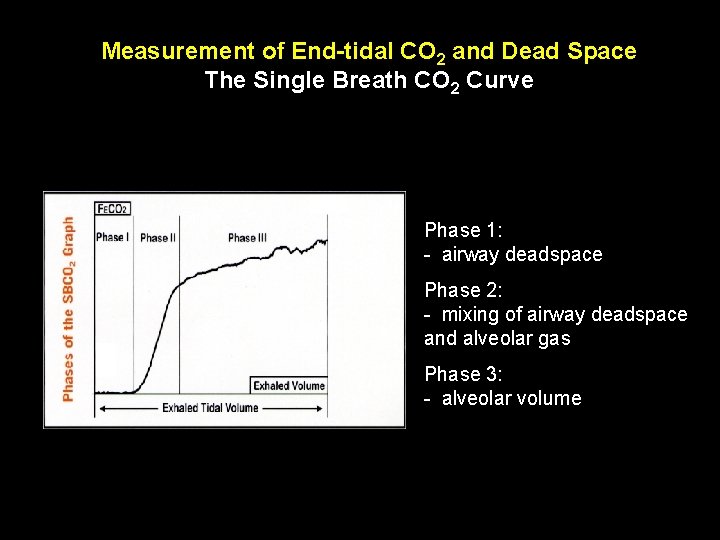
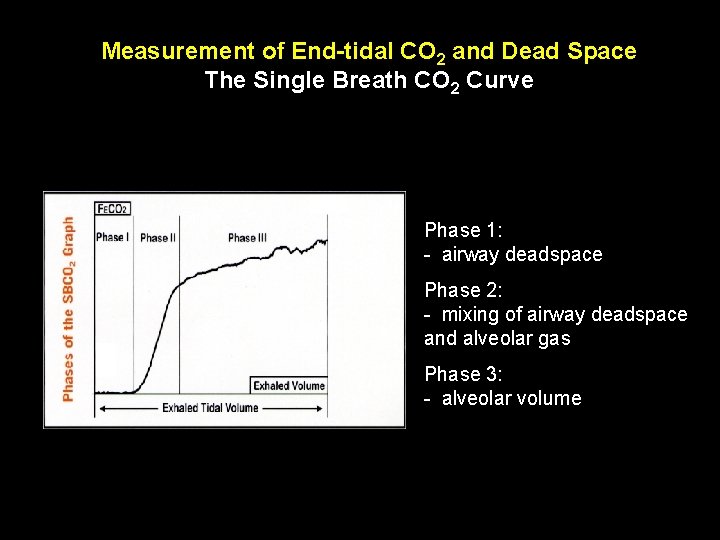
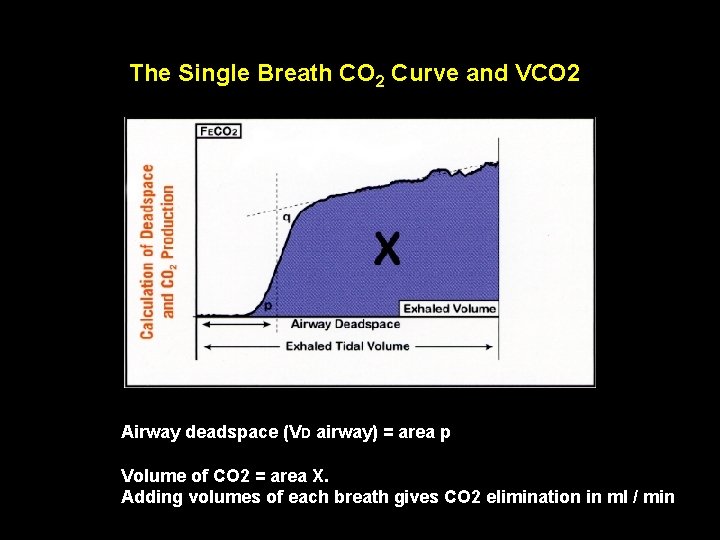
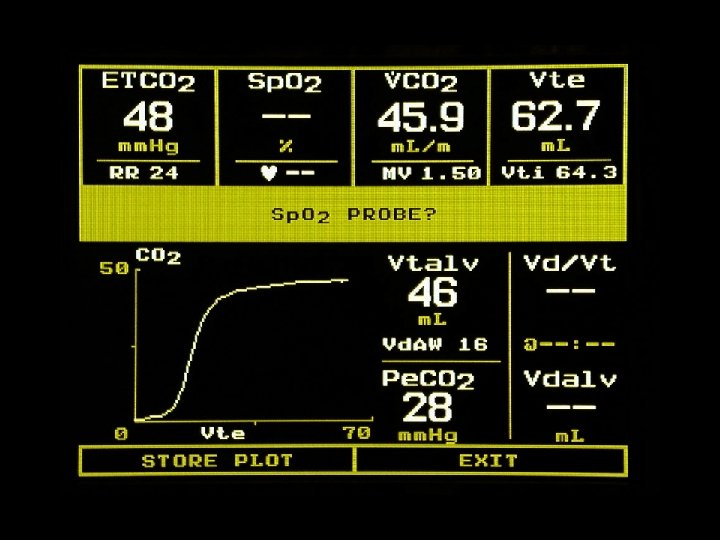
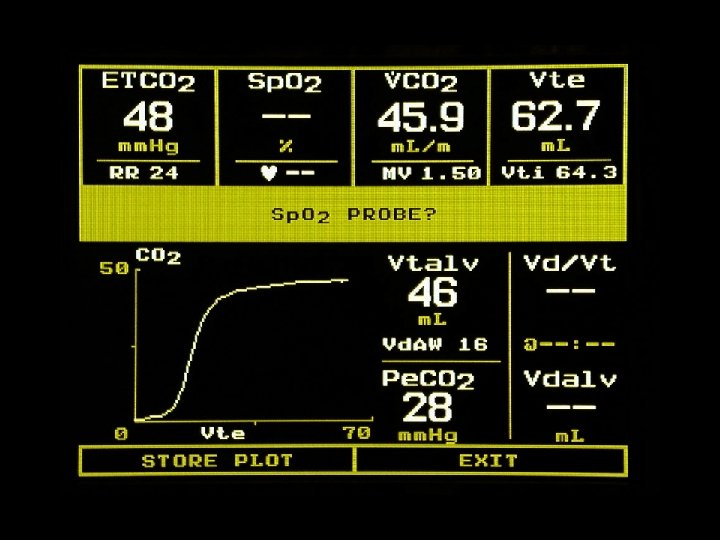
Measurement of End-tidal CO 2 and Dead Space The Single Breath CO 2 Curve Phase 1: - airway deadspace Phase 2: - mixing of airway deadspace and alveolar gas Phase 3: - alveolar volume
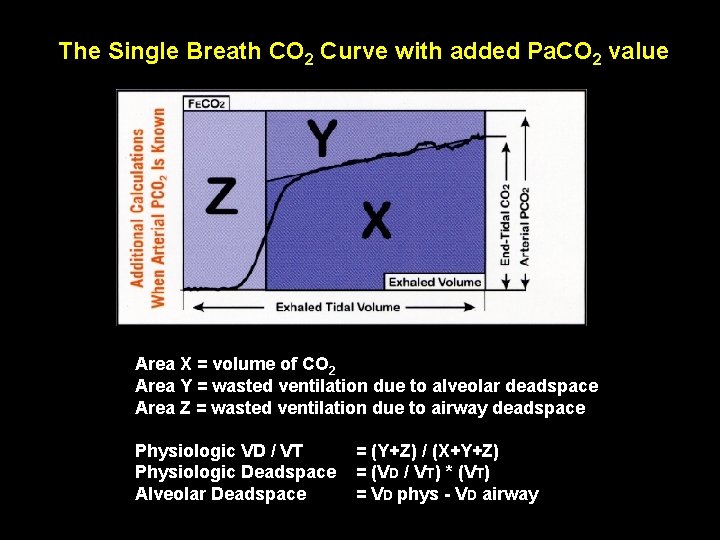
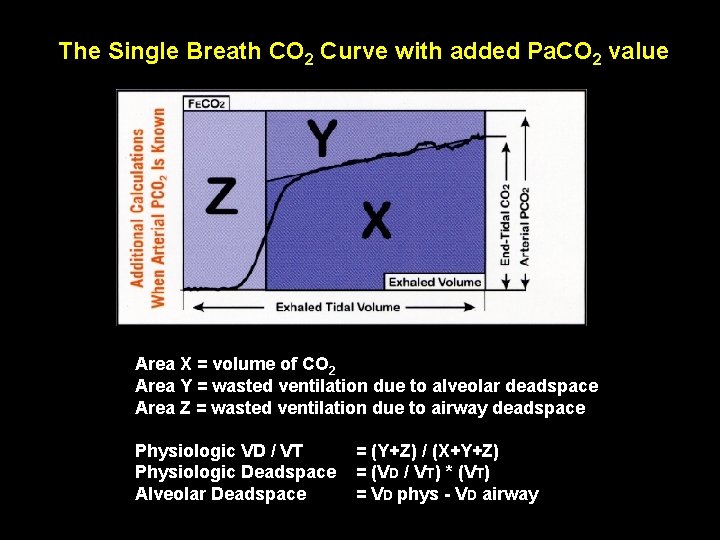
The Single Breath CO 2 Curve with added Pa. CO 2 value Area X = volume of CO 2 Area Y = wasted ventilation due to alveolar deadspace Area Z = wasted ventilation due to airway deadspace Physiologic VD / VT Physiologic Deadspace Alveolar Deadspace = (Y+Z) / (X+Y+Z) = (VD / VT) * (VT) = VD phys - VD airway
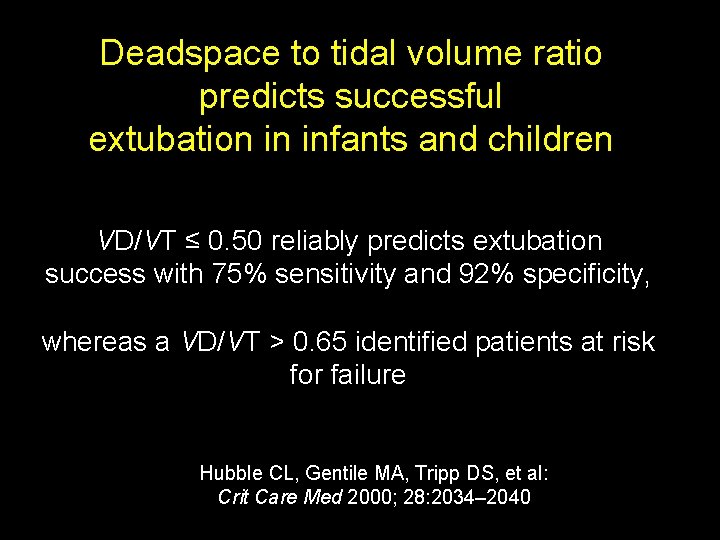
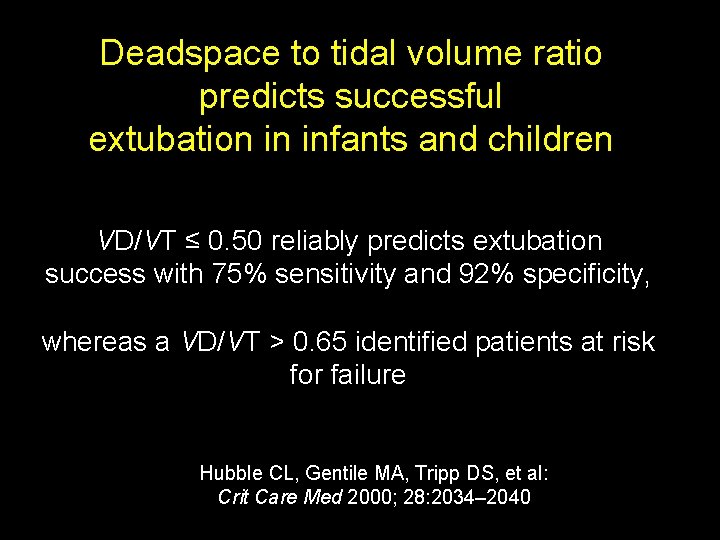
Deadspace to tidal volume ratio predicts successful extubation in infants and children VD/VT ≤ 0. 50 reliably predicts extubation success with 75% sensitivity and 92% specificity, whereas a VD/VT > 0. 65 identified patients at risk for failure Hubble CL, Gentile MA, Tripp DS, et al: Crit Care Med 2000; 28: 2034– 2040
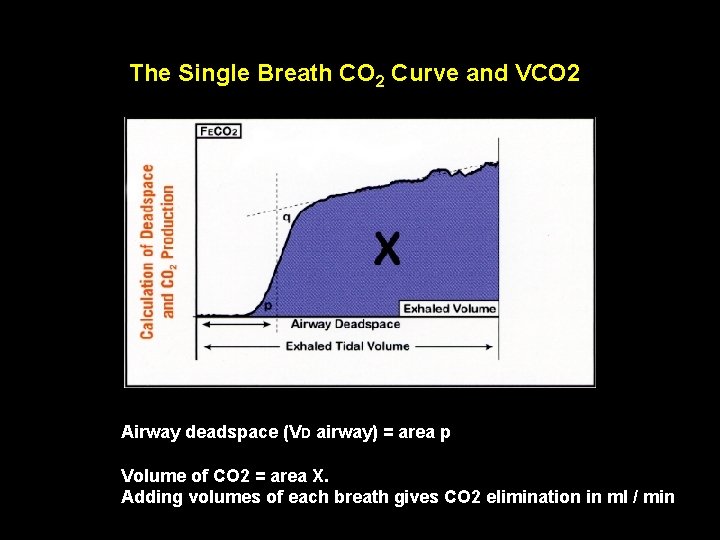
The Single Breath CO 2 Curve and VCO 2 Airway deadspace (VD airway) = area p Volume of CO 2 = area X. Adding volumes of each breath gives CO 2 elimination in ml / min
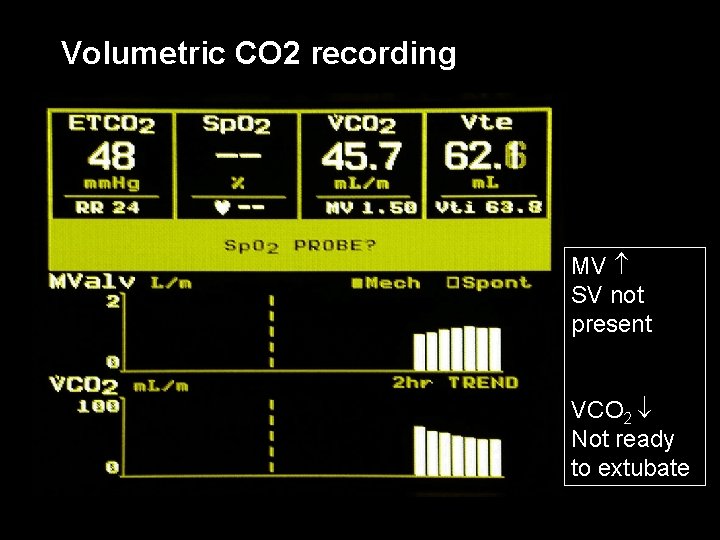
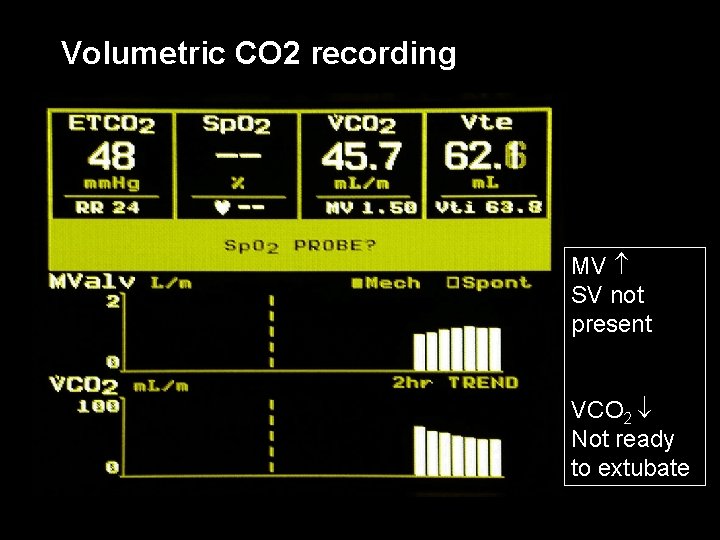
Volumetric CO 2 recording MV SV not present VCO 2 Not ready to extubate
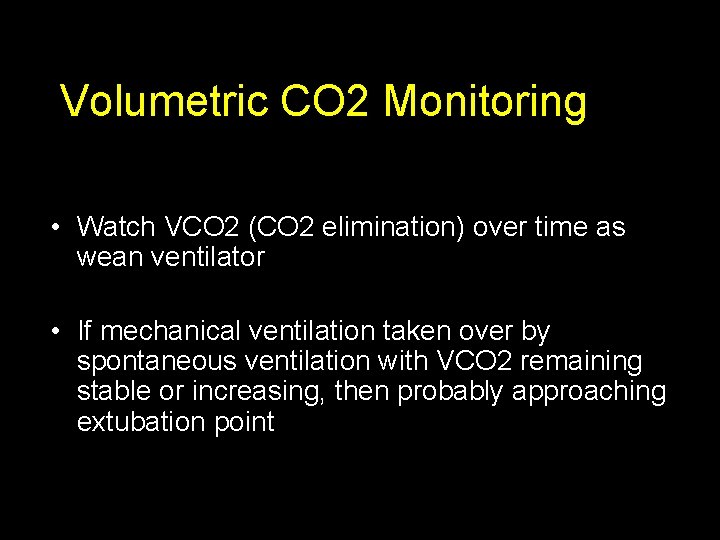
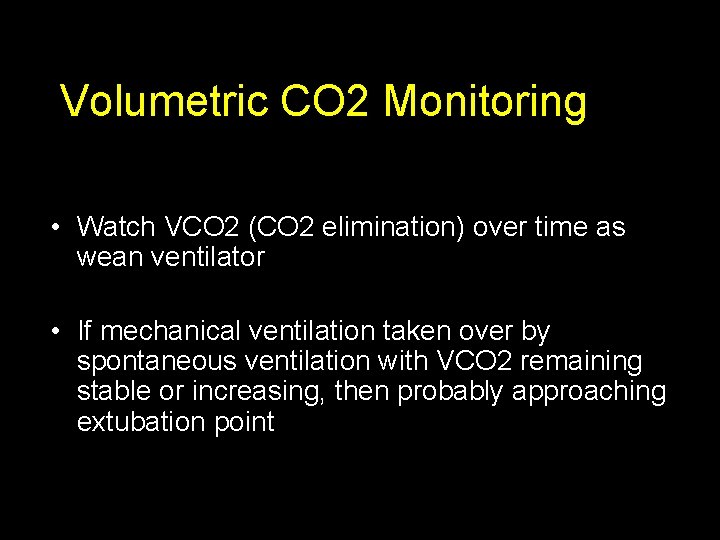
Volumetric CO 2 Monitoring • Watch VCO 2 (CO 2 elimination) over time as wean ventilator • If mechanical ventilation taken over by spontaneous ventilation with VCO 2 remaining stable or increasing, then probably approaching extubation point
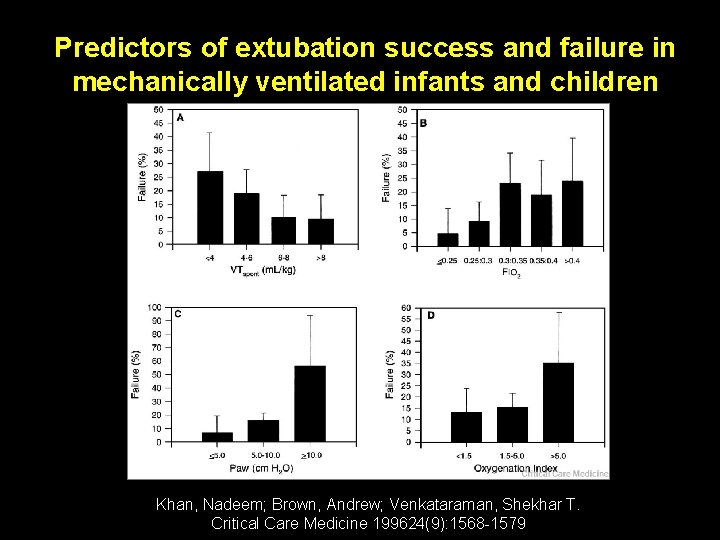
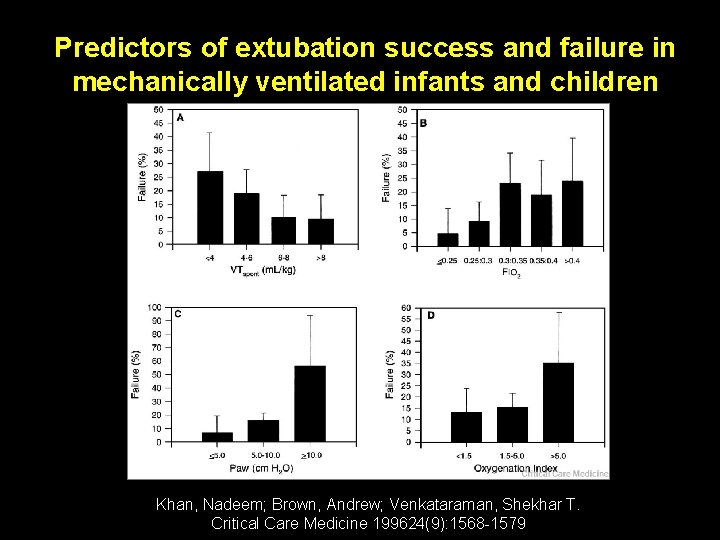
Predictors of extubation success and failure in mechanically ventilated infants and children Khan, Nadeem; Brown, Andrew; Venkataraman, Shekhar T. Critical Care Medicine 199624(9): 1568 -1579
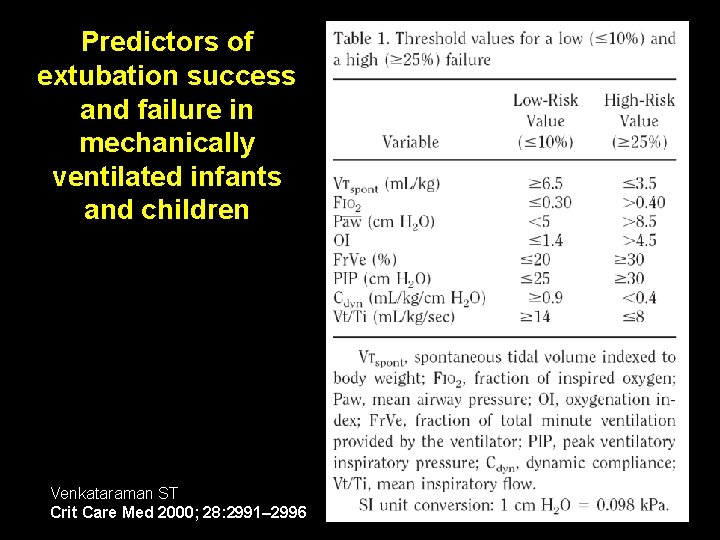
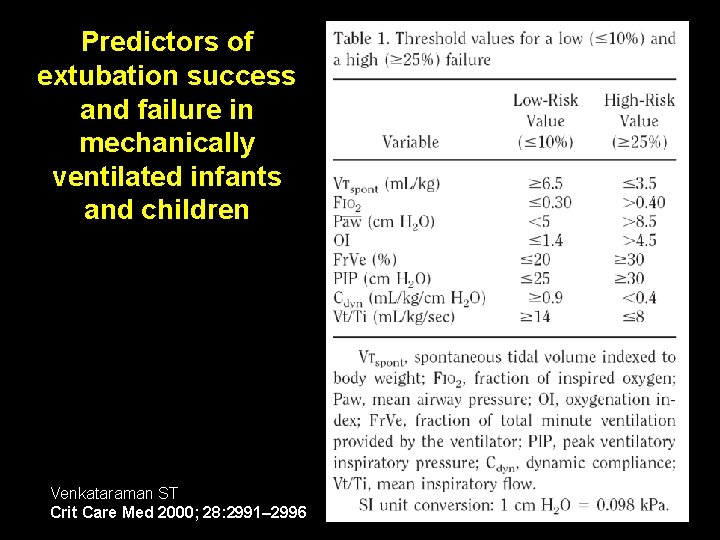
Predictors of extubation success and failure in mechanically ventilated infants and children Venkataraman ST Crit Care Med 2000; 28: 2991– 2996
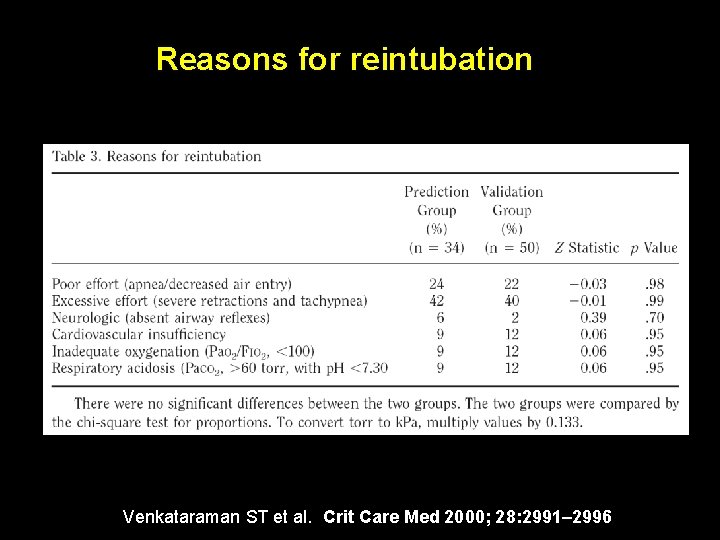
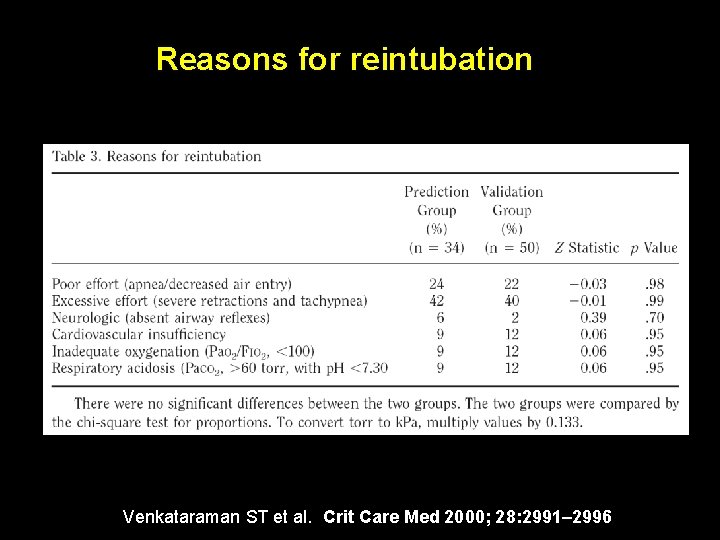
Reasons for reintubation Venkataraman ST et al. Crit Care Med 2000; 28: 2991– 2996
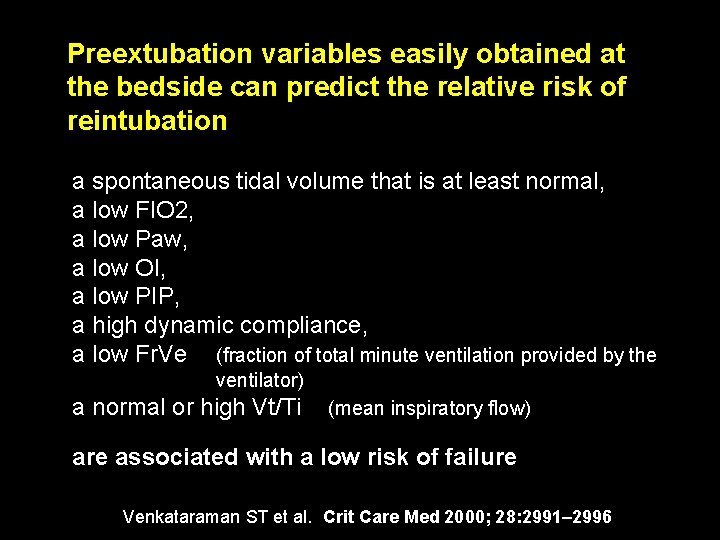
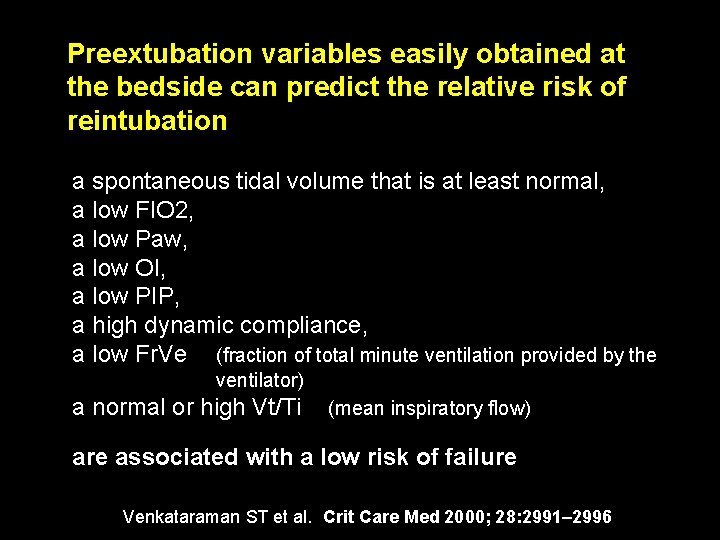
Preextubation variables easily obtained at the bedside can predict the relative risk of reintubation a spontaneous tidal volume that is at least normal, a low FIO 2, a low Paw, a low OI, a low PIP, a high dynamic compliance, a low Fr. Ve (fraction of total minute ventilation provided by the ventilator) a normal or high Vt/Ti (mean inspiratory flow) are associated with a low risk of failure Venkataraman ST et al. Crit Care Med 2000; 28: 2991– 2996
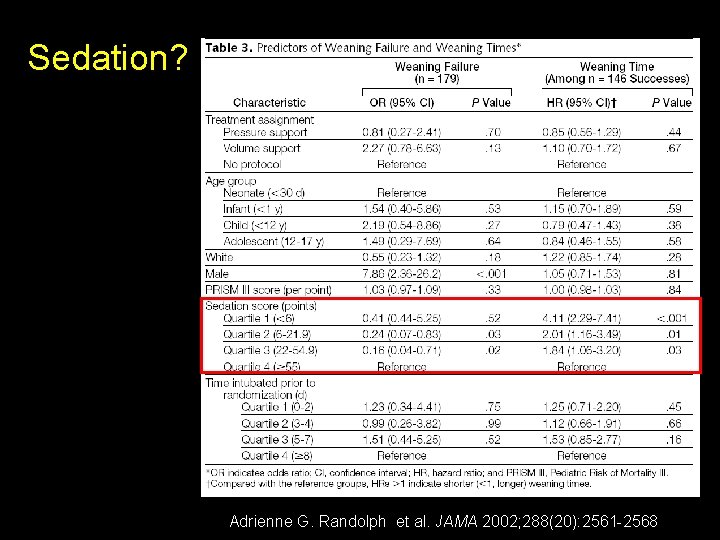
Sedation? Adrienne G. Randolph et al. JAMA 2002; 288(20): 2561 -2568
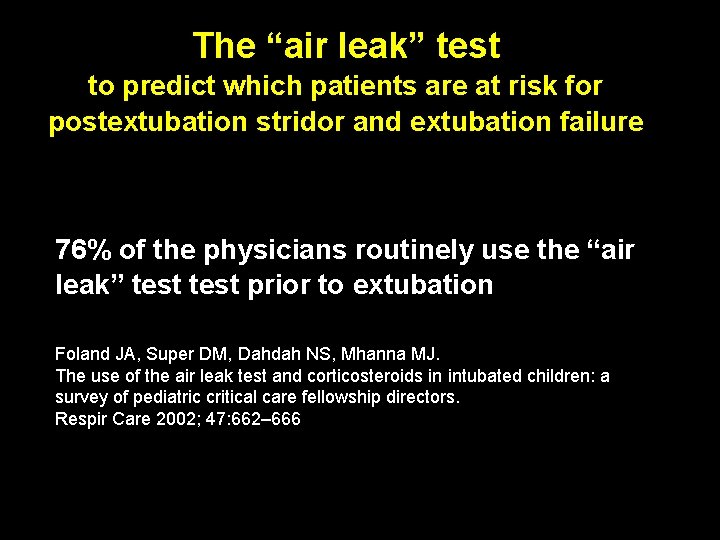
The “air leak” test to predict which patients are at risk for postextubation stridor and extubation failure 76% of the physicians routinely use the “air leak” test prior to extubation Foland JA, Super DM, Dahdah NS, Mhanna MJ. The use of the air leak test and corticosteroids in intubated children: a survey of pediatric critical care fellowship directors. Respir Care 2002; 47: 662– 666
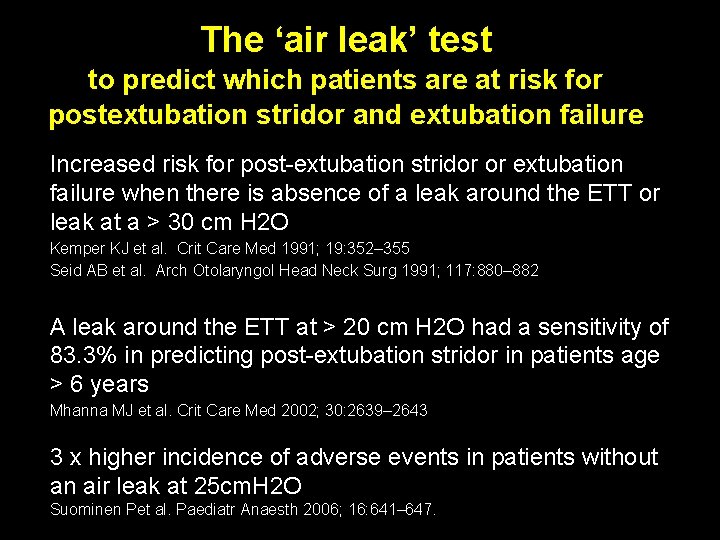
The ‘air leak’ test to predict which patients are at risk for postextubation stridor and extubation failure Increased risk for post-extubation stridor or extubation failure when there is absence of a leak around the ETT or leak at a > 30 cm H 2 O Kemper KJ et al. Crit Care Med 1991; 19: 352– 355 Seid AB et al. Arch Otolaryngol Head Neck Surg 1991; 117: 880– 882 A leak around the ETT at > 20 cm H 2 O had a sensitivity of 83. 3% in predicting post-extubation stridor in patients age > 6 years Mhanna MJ et al. Crit Care Med 2002; 30: 2639– 2643 3 x higher incidence of adverse events in patients without an air leak at 25 cm. H 2 O Suominen Pet al. Paediatr Anaesth 2006; 16: 641– 647.
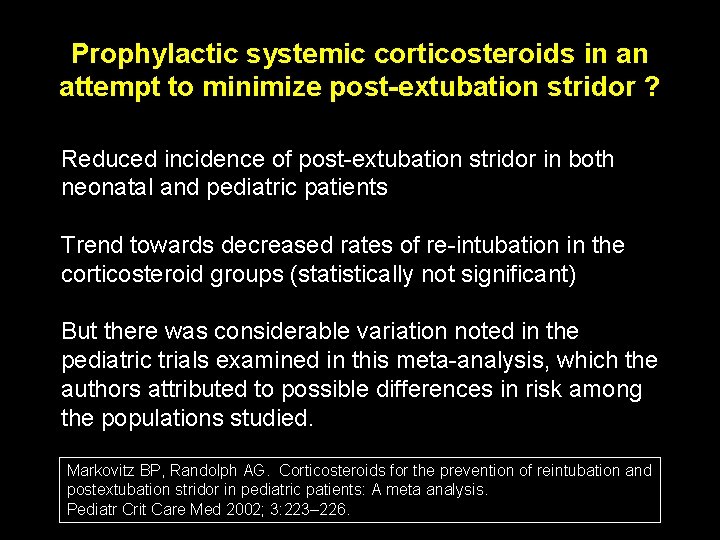
Prophylactic systemic corticosteroids in an attempt to minimize post-extubation stridor ? Reduced incidence of post-extubation stridor in both neonatal and pediatric patients Trend towards decreased rates of re-intubation in the corticosteroid groups (statistically not significant) But there was considerable variation noted in the pediatric trials examined in this meta-analysis, which the authors attributed to possible differences in risk among the populations studied. Markovitz BP, Randolph AG. Corticosteroids for the prevention of reintubation and postextubation stridor in pediatric patients: A meta analysis. Pediatr Crit Care Med 2002; 3: 223– 226.
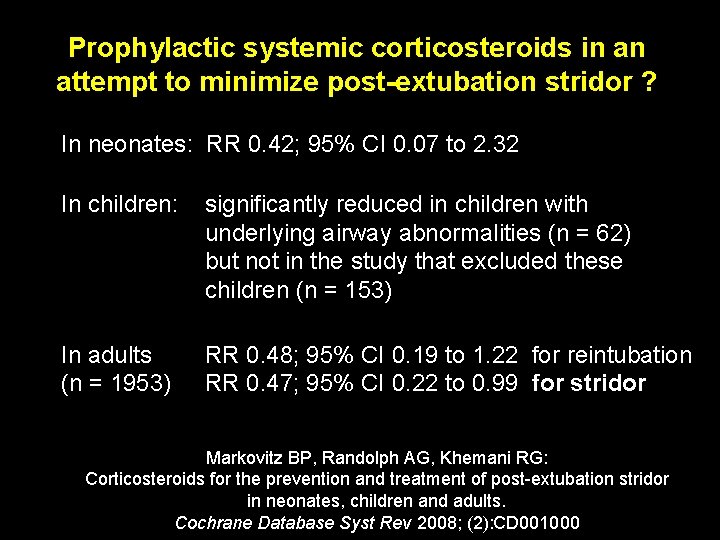
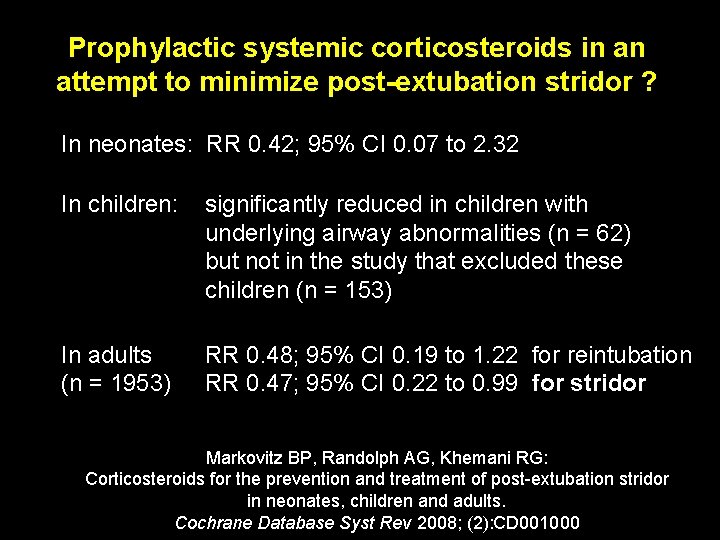
Prophylactic systemic corticosteroids in an attempt to minimize post-extubation stridor ? In neonates: RR 0. 42; 95% CI 0. 07 to 2. 32 In children: significantly reduced in children with underlying airway abnormalities (n = 62) but not in the study that excluded these children (n = 153) In adults (n = 1953) RR 0. 48; 95% CI 0. 19 to 1. 22 for reintubation RR 0. 47; 95% CI 0. 22 to 0. 99 for stridor Markovitz BP, Randolph AG, Khemani RG: Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev 2008; (2): CD 001000
Using corticosteroids to prevent (or treat) stridor after extubation has not proven effective for neonates, children or adults. However, given the consistent trend toward benefit, this intervention does merit further study Markovitz BP, Randolph AG, Khemani RG: Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev 2008; (2): CD 001000
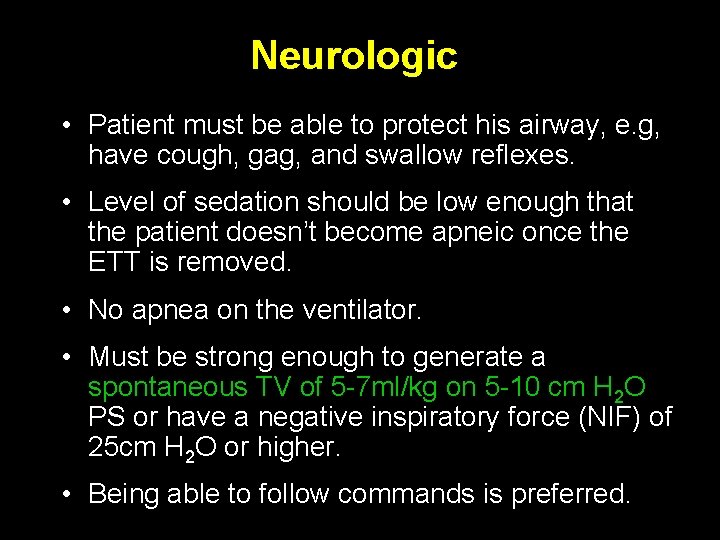
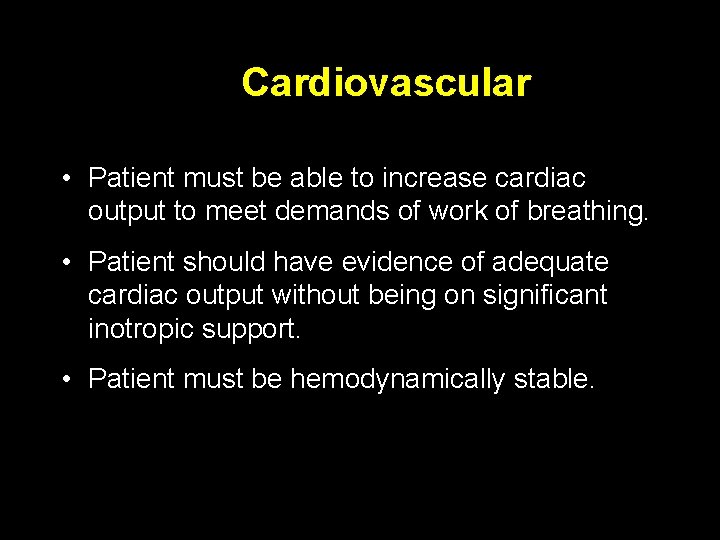
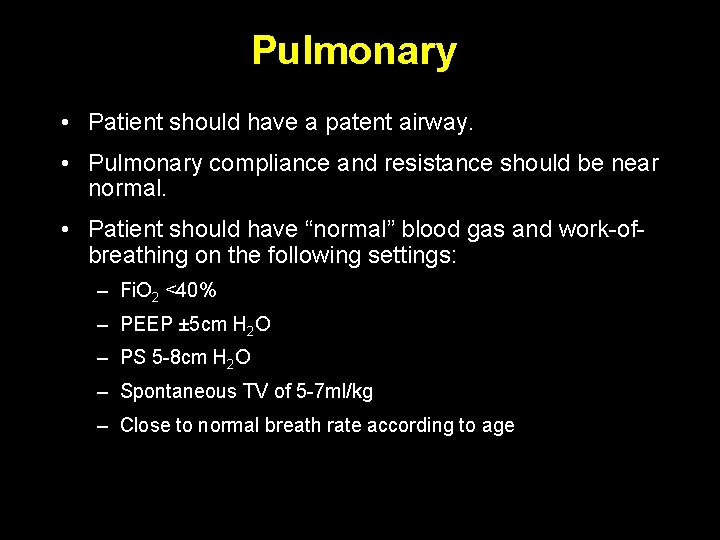
Extubation Criteria 1. Neurologic 2. Cardiovascular 3. Pulmonary
Neurologic • Patient must be able to protect his airway, e. g, have cough, gag, and swallow reflexes. • Level of sedation should be low enough that the patient doesn’t become apneic once the ETT is removed. • No apnea on the ventilator. • Must be strong enough to generate a spontaneous TV of 5 -7 ml/kg on 5 -10 cm H 2 O PS or have a negative inspiratory force (NIF) of 25 cm H 2 O or higher. • Being able to follow commands is preferred.
Cardiovascular • Patient must be able to increase cardiac output to meet demands of work of breathing. • Patient should have evidence of adequate cardiac output without being on significant inotropic support. • Patient must be hemodynamically stable.
Pulmonary • Patient should have a patent airway. • Pulmonary compliance and resistance should be near normal. • Patient should have “normal” blood gas and work-ofbreathing on the following settings: – Fi. O 2 <40% – PEEP ± 5 cm H 2 O – PS 5 -8 cm H 2 O – Spontaneous TV of 5 -7 ml/kg – Close to normal breath rate according to age
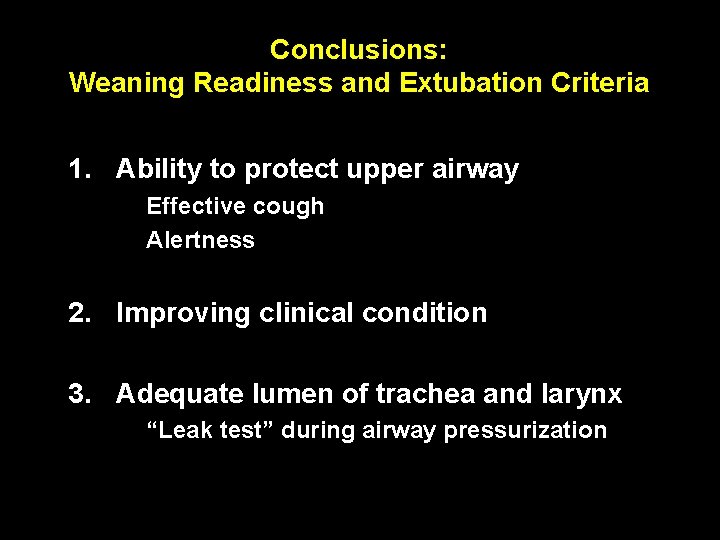
Conclusions: Weaning Readiness and Extubation Criteria 1. Ability to protect upper airway Effective cough Alertness 2. Improving clinical condition 3. Adequate lumen of trachea and larynx “Leak test” during airway pressurization
Conclusions: Weaning Readiness and Extubation Criteria Upper airway obstruction is the single most common cause of extubation failure. A reliable method of assessing readiness for weaning and predicting extubation success is not evident from the pediatric literature. Weaning is often not considered early enough in the course of ventilation.
Extubation – Control of airway reflexes – Patent upper airway (air leak around tube? ) – Minimal oxygen requirement – Minimize pressure support (0 - max 10) (Normal compliance = Vt 8 ml/kg with PS of 8) – Comfortable spontaneous breathing – “Awake ” patient