Urology Hematuria Stones Tumours Outline Hematuria DDx General








- Slides: 111
Urology Hematuria Stones Tumours
Outline • Hematuria ▫ DDx ▫ General Work up • Renal Colic ▫ Stones • Malignancy ▫ Renal ▫ Bladder • Scrotal masses
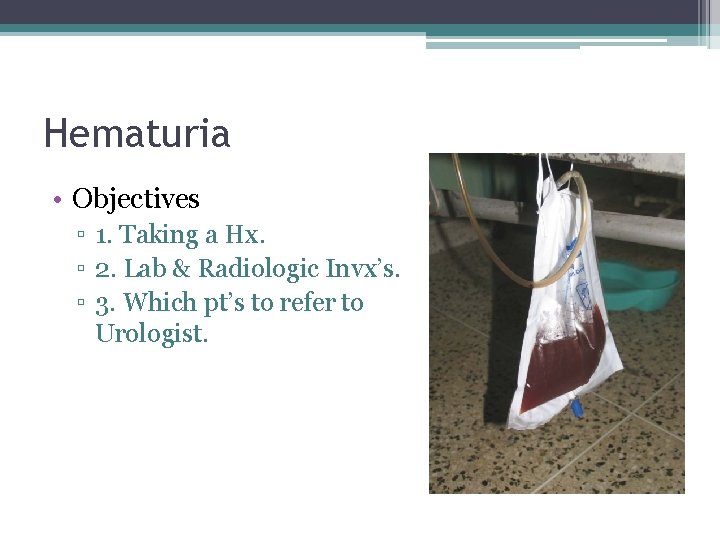
Hematuria • Objectives ▫ 1. Taking a Hx. ▫ 2. Lab & Radiologic Invx’s. ▫ 3. Which pt’s to refer to Urologist.
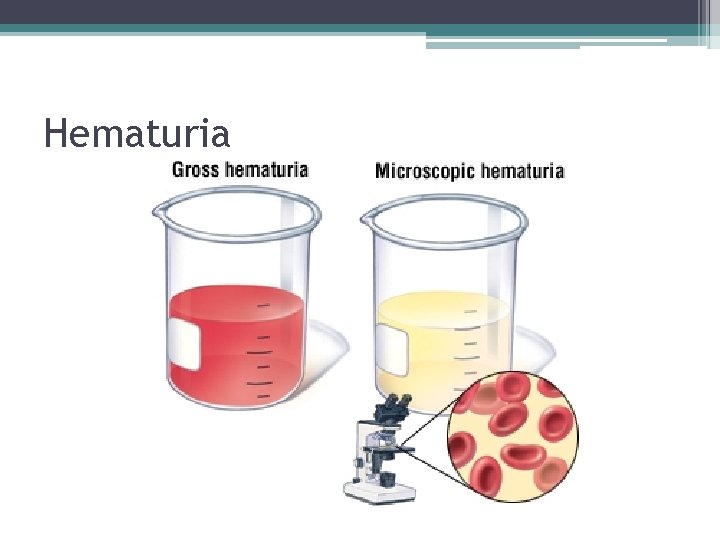
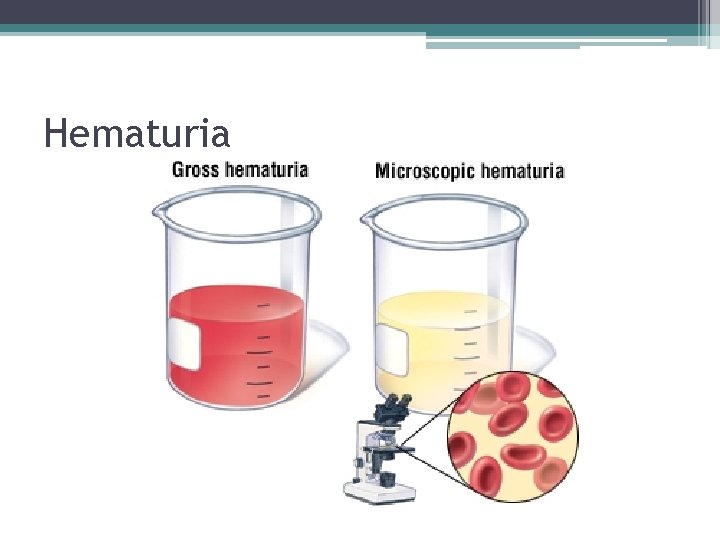
Hematuria
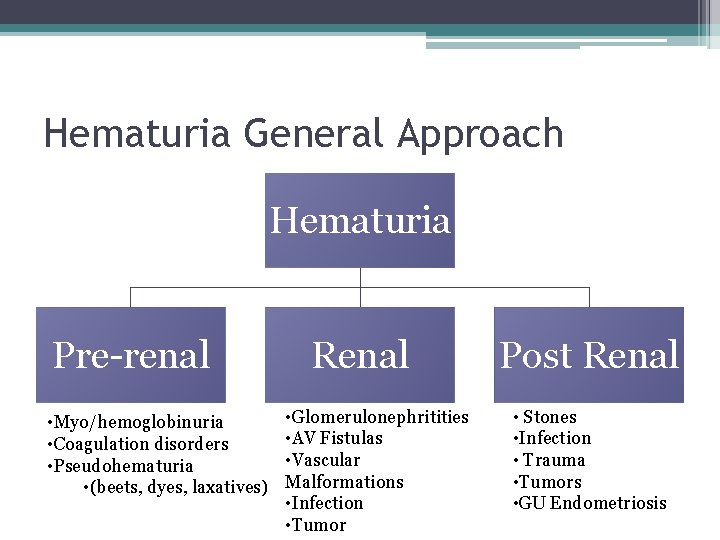
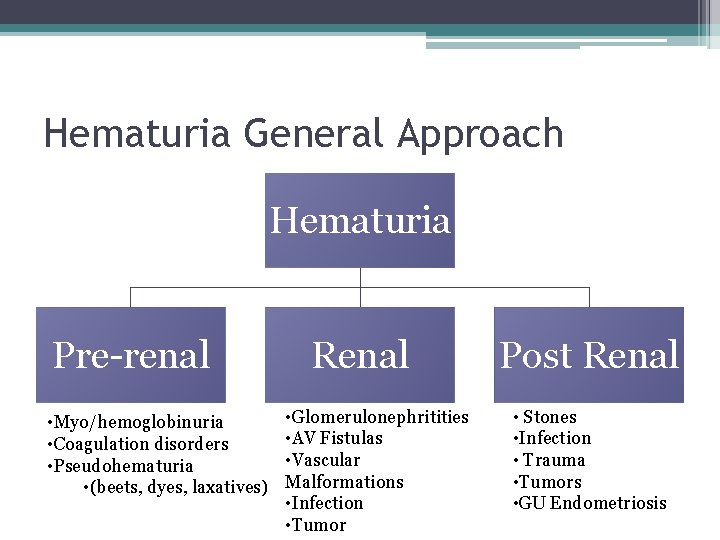
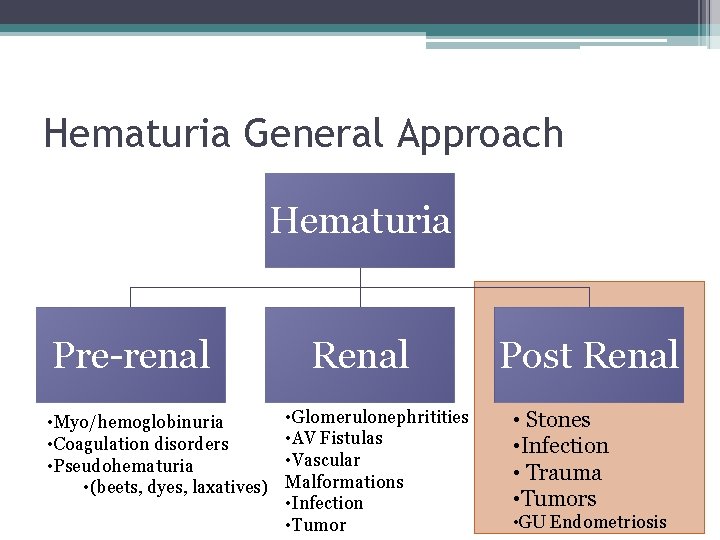
Hematuria General Approach Hematuria Pre-renal • Myo/hemoglobinuria • Coagulation disorders • Pseudohematuria • (beets, dyes, laxatives) Renal • Glomerulonephritities • AV Fistulas • Vascular Malformations • Infection • Tumor Post Renal • Stones • Infection • Trauma • Tumors • GU Endometriosis
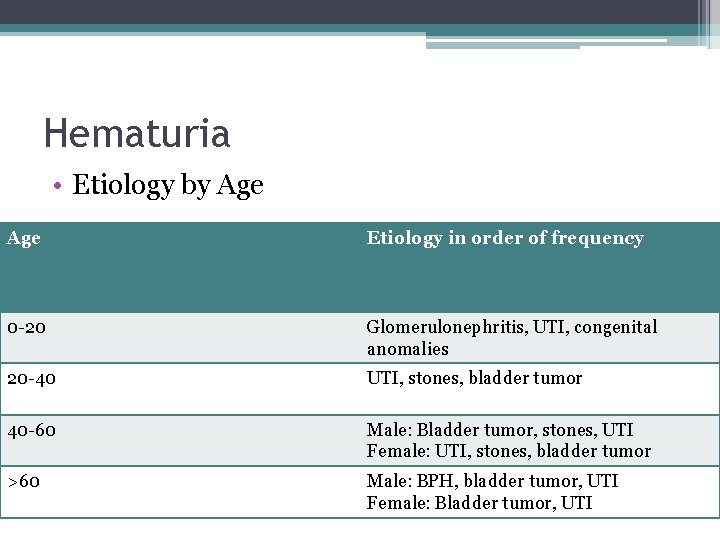
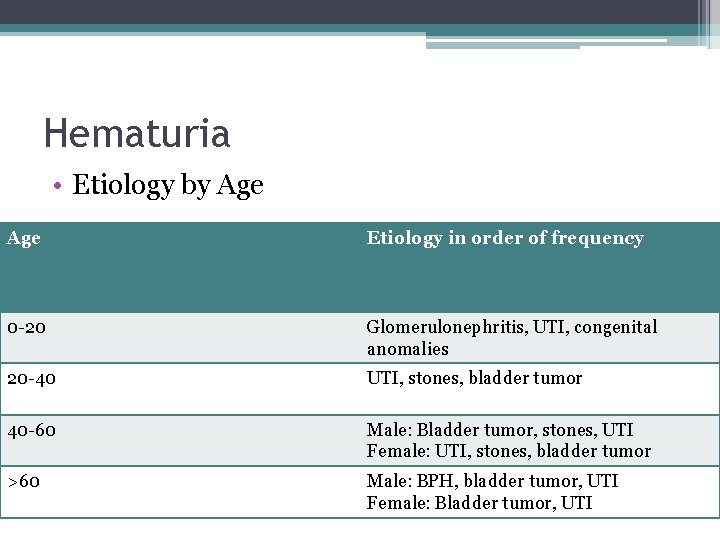
Hematuria • Etiology by Age Etiology in order of frequency 0 -20 Glomerulonephritis, UTI, congenital anomalies 20 -40 UTI, stones, bladder tumor 40 -60 Male: Bladder tumor, stones, UTI Female: UTI, stones, bladder tumor >60 Male: BPH, bladder tumor, UTI Female: Bladder tumor, UTI
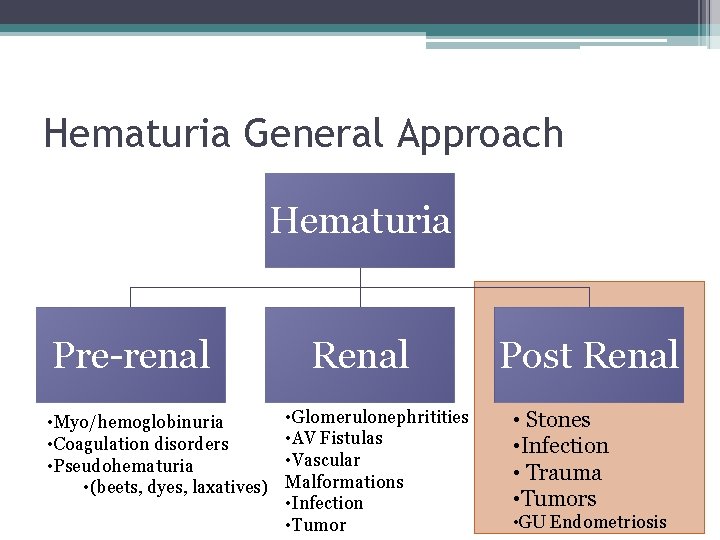
Hematuria General Approach Hematuria Pre-renal • Myo/hemoglobinuria • Coagulation disorders • Pseudohematuria • (beets, dyes, laxatives) Renal • Glomerulonephritities • AV Fistulas • Vascular Malformations • Infection • Tumor Post Renal • Stones • Infection • Trauma • Tumors • GU Endometriosis
Hematuria DDx ▫ ▫ Stones Infections Tumours Trauma
Hematuria HPI • Stones: ▫ Flank/Abdo pain, dysuria, PHx Stones. • Infection: ▫ Suprapubic pain, dysuria, frequency, fever/chills +/flank pain. • Malignancy ▫ Wt loss, night sweats, flank pain, voiding changes, Occupational Hx (petroleum exposure), smoking Hx, FMHx of Cancer • Trauma ▫ Recent encounters with Chuck Norris.
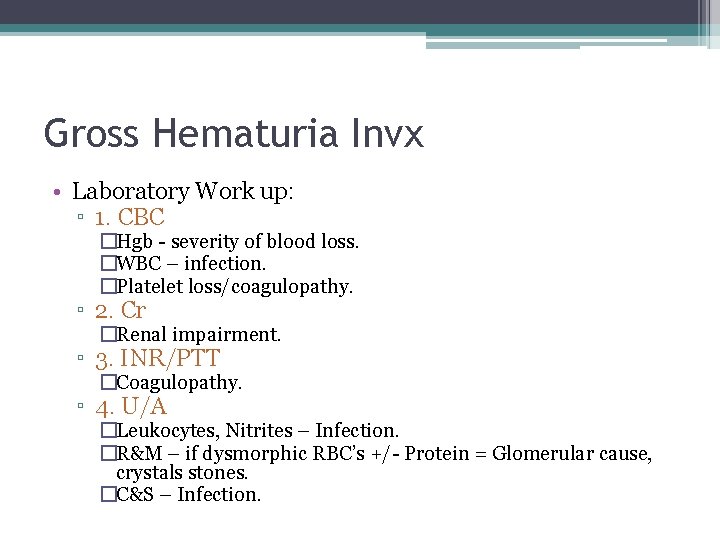
Gross Hematuria Invx • Laboratory Work up: ▫ 1. CBC �Hgb - severity of blood loss. �WBC – infection. �Platelet loss/coagulopathy. ▫ 2. Cr �Renal impairment. ▫ 3. INR/PTT �Coagulopathy. ▫ 4. U/A �Leukocytes, Nitrites – Infection. �R&M – if dysmorphic RBC’s +/- Protein = Glomerular cause, crystals stones. �C&S – Infection.
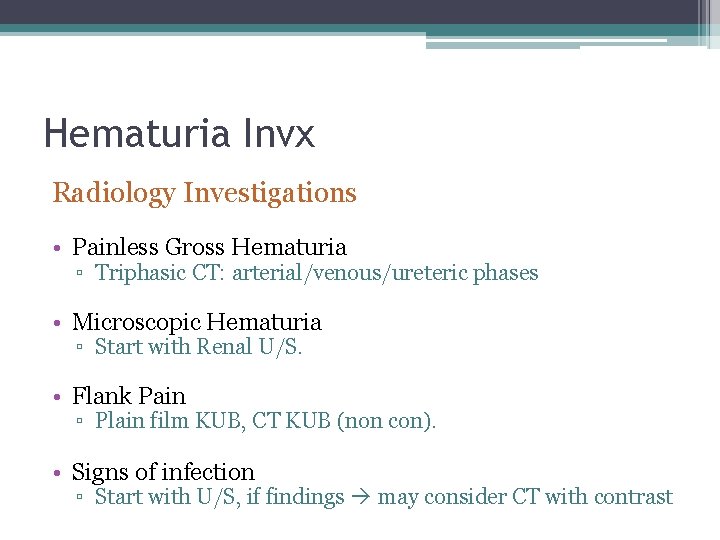
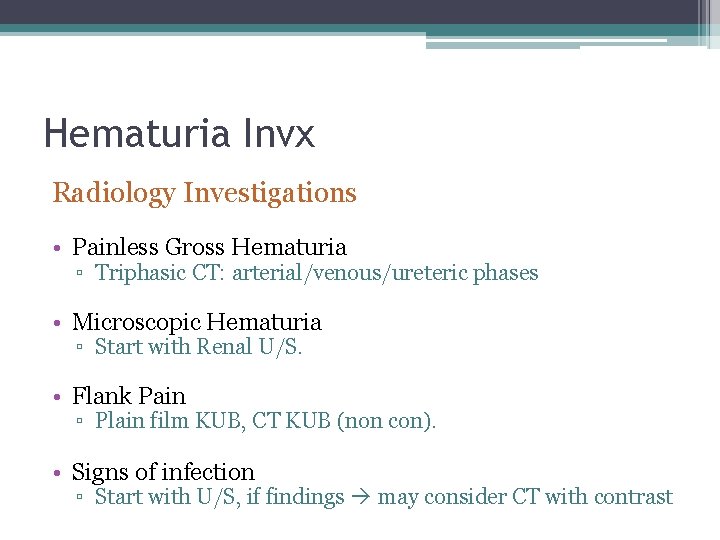
Hematuria Invx Radiology Investigations • Painless Gross Hematuria ▫ Triphasic CT: arterial/venous/ureteric phases • Microscopic Hematuria ▫ Start with Renal U/S. • Flank Pain ▫ Plain film KUB, CT KUB (non con). • Signs of infection ▫ Start with U/S, if findings may consider CT with contrast
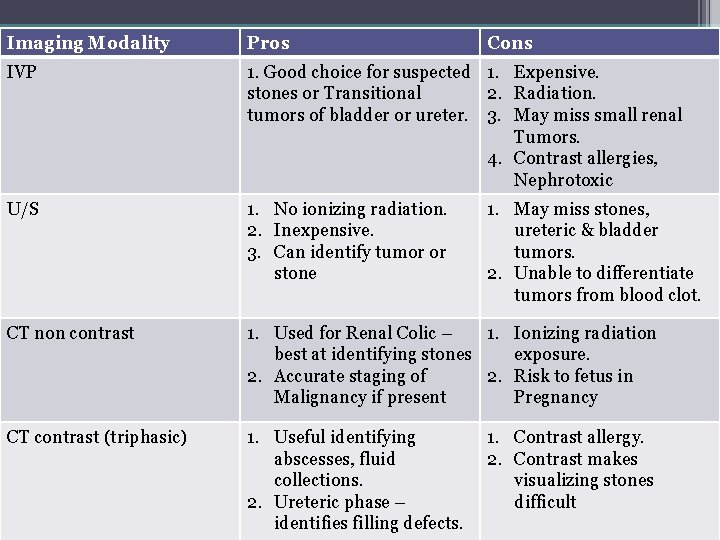
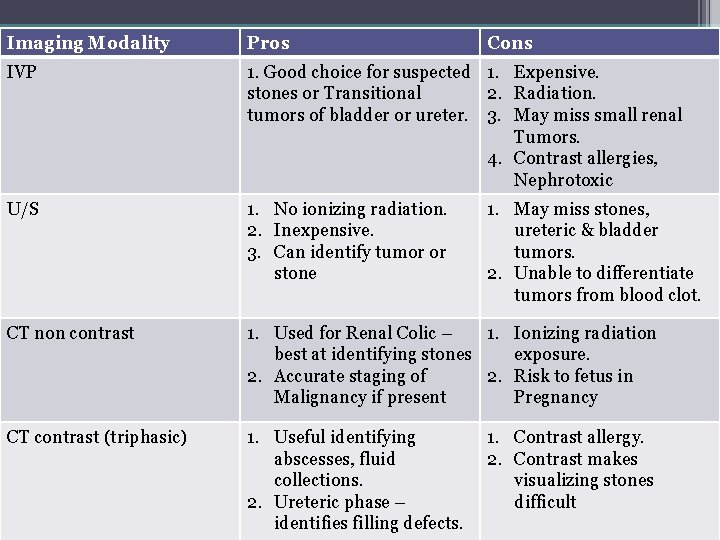
Imaging Modality Pros IVP 1. Good choice for suspected 1. Expensive. stones or Transitional 2. Radiation. tumors of bladder or ureter. 3. May miss small renal Tumors. 4. Contrast allergies, Nephrotoxic Hematuria Cons U/S 1. No ionizing radiation. 2. Inexpensive. 3. Can identify tumor or stone 1. May miss stones, ureteric & bladder tumors. 2. Unable to differentiate tumors from blood clot. CT non contrast 1. Used for Renal Colic – 1. Ionizing radiation best at identifying stones exposure. 2. Accurate staging of 2. Risk to fetus in Malignancy if present Pregnancy CT contrast (triphasic) 1. Useful identifying abscesses, fluid collections. 2. Ureteric phase – identifies filling defects. 1. Contrast allergy. 2. Contrast makes visualizing stones difficult
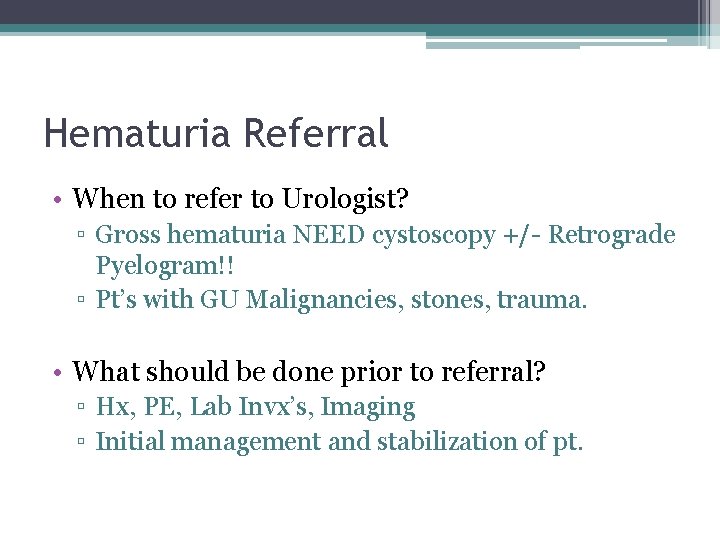
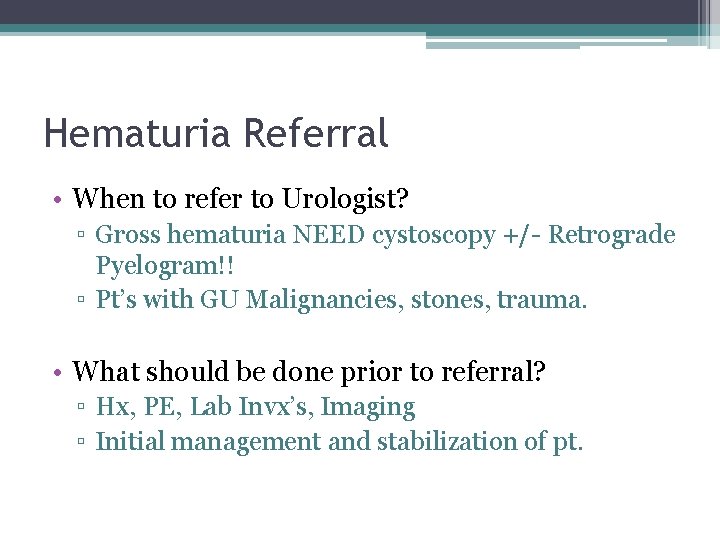
Hematuria Referral • When to refer to Urologist? ▫ Gross hematuria NEED cystoscopy +/- Retrograde Pyelogram!! ▫ Pt’s with GU Malignancies, stones, trauma. • What should be done prior to referral? ▫ Hx, PE, Lab Invx’s, Imaging ▫ Initial management and stabilization of pt.


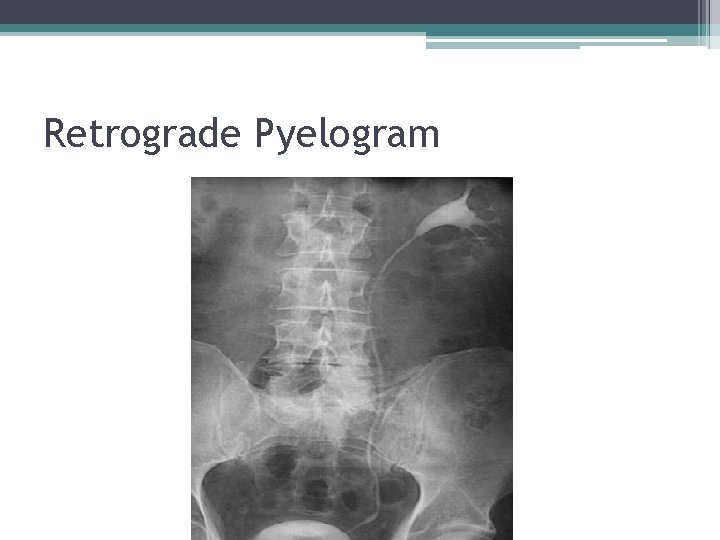
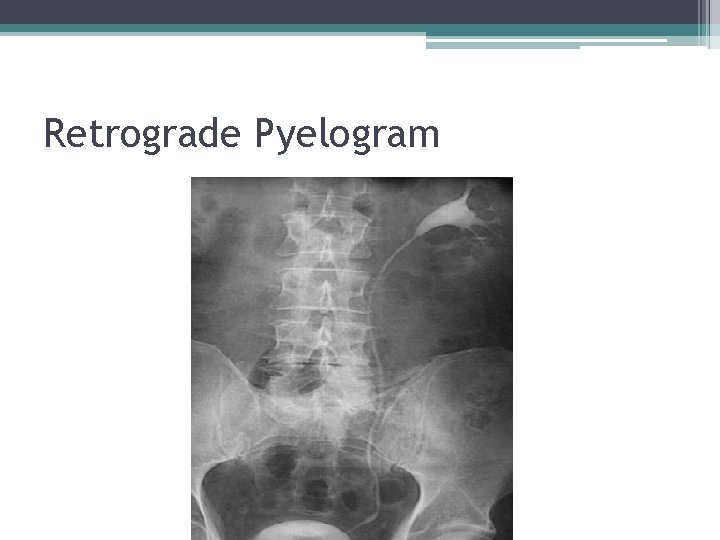
Retrograde Pyelogram
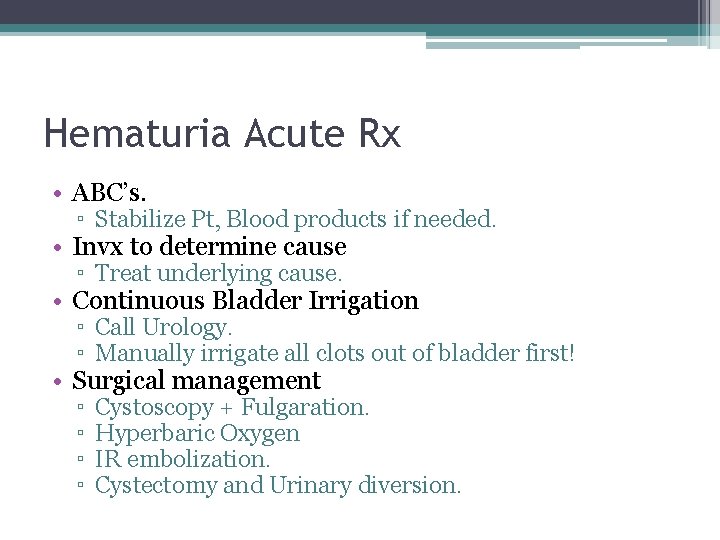
Hematuria Acute Rx • ABC’s. ▫ Stabilize Pt, Blood products if needed. • Invx to determine cause ▫ Treat underlying cause. • Continuous Bladder Irrigation ▫ Call Urology. ▫ Manually irrigate all clots out of bladder first! • Surgical management ▫ ▫ Cystoscopy + Fulgaration. Hyperbaric Oxygen IR embolization. Cystectomy and Urinary diversion.
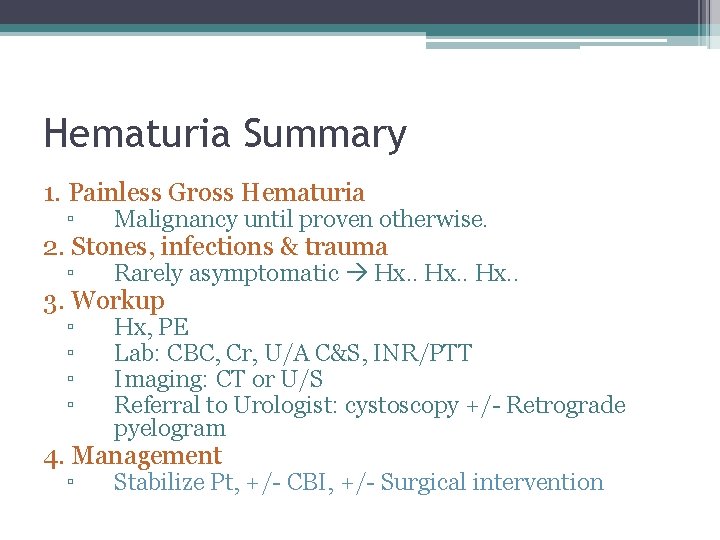
Hematuria Summary 1. Painless Gross Hematuria ▫ Malignancy until proven otherwise. ▫ Rarely asymptomatic Hx. . ▫ ▫ Hx, PE Lab: CBC, Cr, U/A C&S, INR/PTT Imaging: CT or U/S Referral to Urologist: cystoscopy +/- Retrograde pyelogram 2. Stones, infections & trauma 3. Workup 4. Management ▫ Stabilize Pt, +/- CBI, +/- Surgical intervention
Hematuria Cases • Geeyu Malignansey, a 67 yo female with 114 pk/yr smoking hx presents with Gross Hematuria. • Wazun Mi, 23 yo male minding his own business gets stabbed to the flank, while voiding and notices he urine becomes red… • 24 yo Engineering student comes in with dysuria after holding her urine for 14 hours playing ‘Call of duty’, she has leuks, nitrites and RBC’s on U/A…
Outline • Hematuria ▫ DDx ▫ General Work up • Renal Colic ▫ Stones • Malignancy ▫ Renal ▫ Bladder • Scrotal masses
Stones
Renal Colic Objectives; 1. Give a differential diagnosis for acute flank pain including two life-threatening conditions 2. Describe the laboratory and radiologic evaluation of a patient with renal colic 3. Know 4 different kinds of kidney stones and the risk factors for stone formation 4. Know 3 indications for emergency drainage of an obstructed kidney
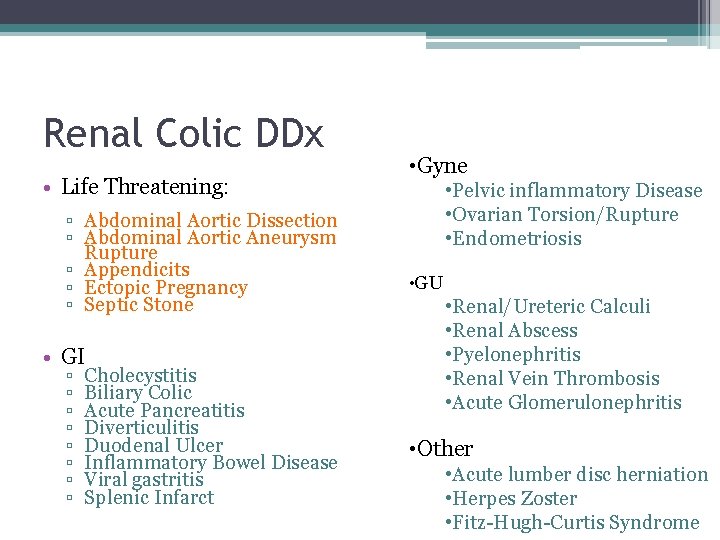
Renal Colic DDx • Life Threatening: ▫ Abdominal Aortic Dissection ▫ Abdominal Aortic Aneurysm Rupture ▫ Appendicits ▫ Ectopic Pregnancy ▫ Septic Stone • GI ▫ ▫ ▫ ▫ Cholecystitis Biliary Colic Acute Pancreatitis Diverticulitis Duodenal Ulcer Inflammatory Bowel Disease Viral gastritis Splenic Infarct • Gyne • Pelvic inflammatory Disease • Ovarian Torsion/Rupture • Endometriosis • GU • Renal/Ureteric Calculi • Renal Abscess • Pyelonephritis • Renal Vein Thrombosis • Acute Glomerulonephritis • Other • Acute lumber disc herniation • Herpes Zoster • Fitz-Hugh-Curtis Syndrome
Renal Colic Invx • Rocky, a 32 yo Male comes to ED with microscopic hematuria and is writhing with Lt Flank pain. • What Laboratory Invx’s do you order? • What initial imaging do you order?
Stones – Acute Lab Invx’s • CBC ▫ WBC – increased indicates inflammation or infection. • Creatinine ▫ Assess for impaired renal function (obstruction). • Urine Microscopy ▫ Bacteriuria, pyuria, p. H
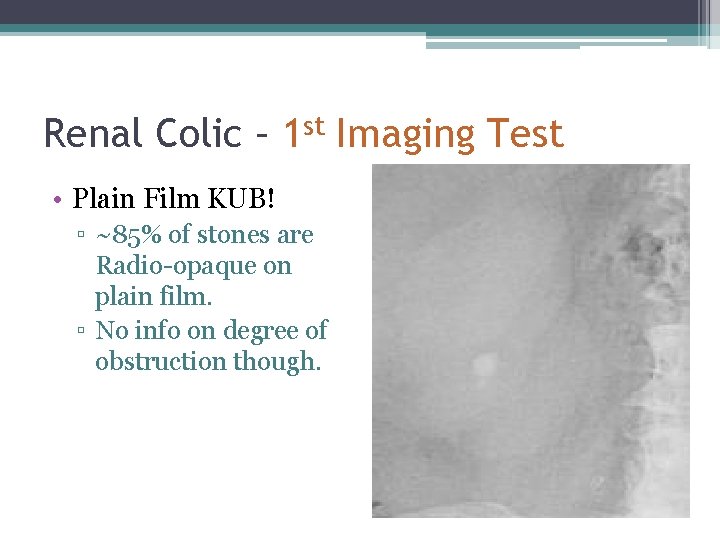
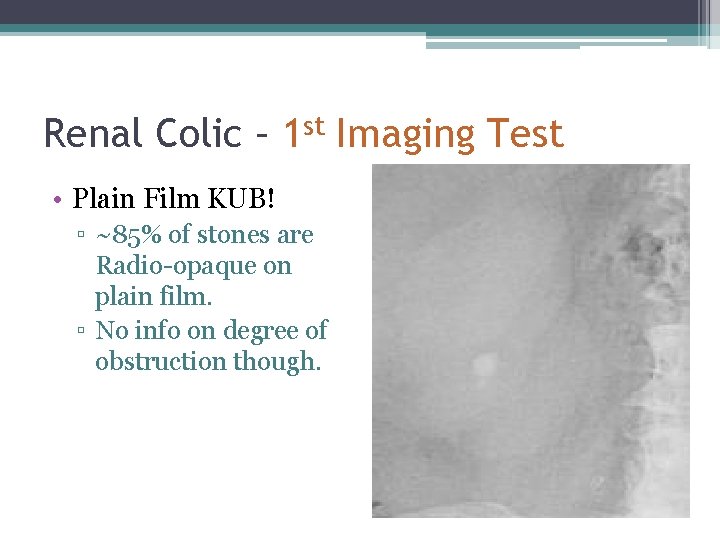
Renal Colic – 1 st Imaging Test • Plain Film KUB! ▫ ~85% of stones are Radio-opaque on plain film. ▫ No info on degree of obstruction though.
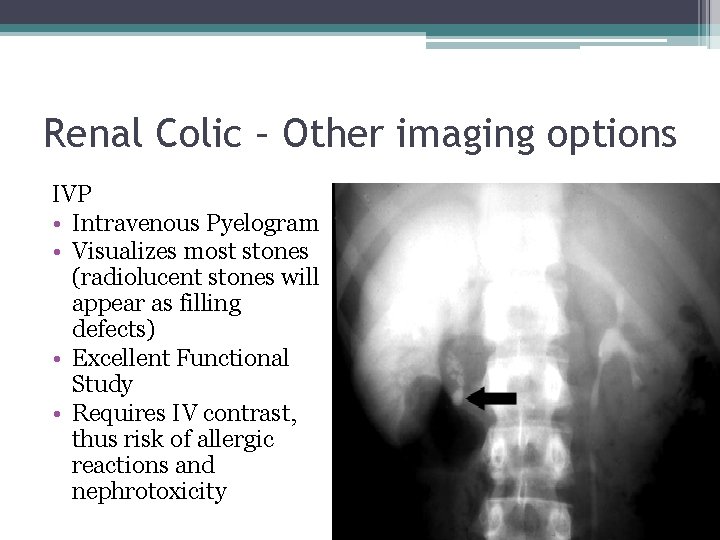
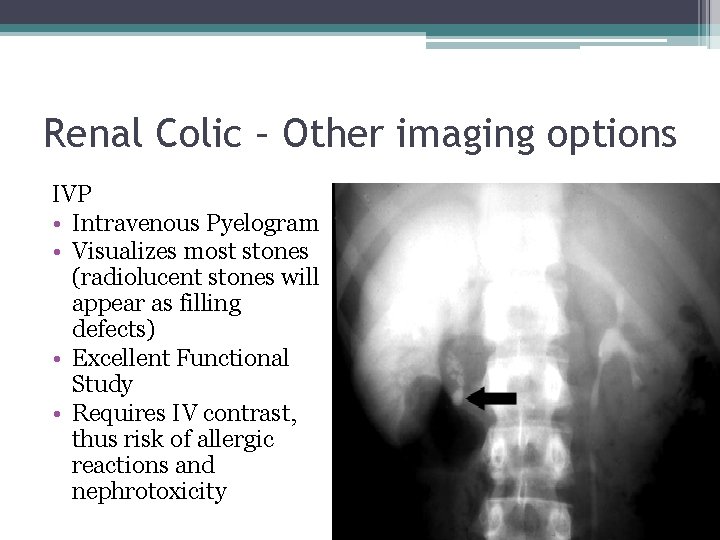
Renal Colic – Other imaging options IVP • Intravenous Pyelogram • Visualizes most stones (radiolucent stones will appear as filling defects) • Excellent Functional Study • Requires IV contrast, thus risk of allergic reactions and nephrotoxicity
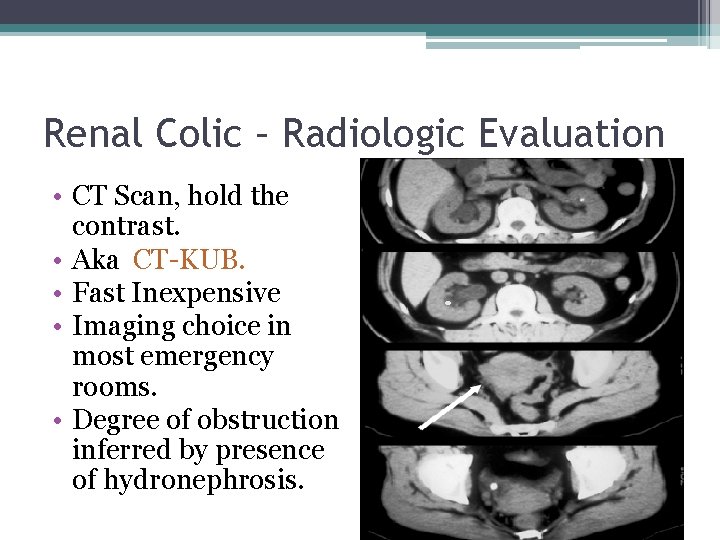
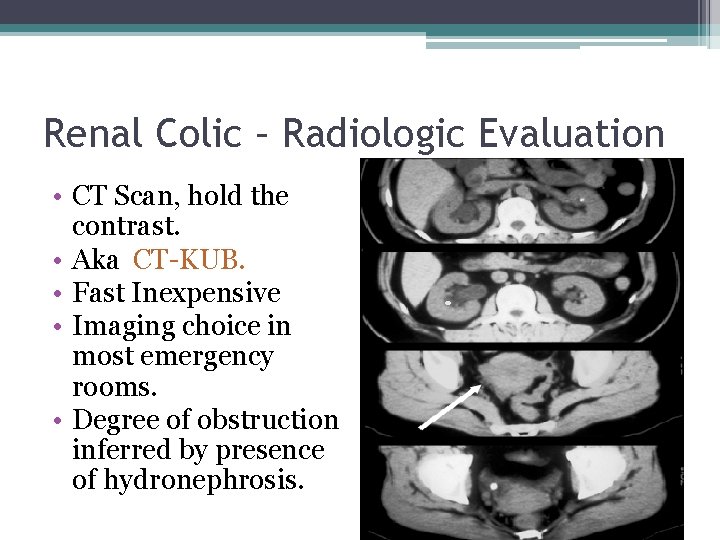
Renal Colic – Radiologic Evaluation • CT Scan, hold the contrast. • Aka CT-KUB. • Fast Inexpensive • Imaging choice in most emergency rooms. • Degree of obstruction inferred by presence of hydronephrosis.
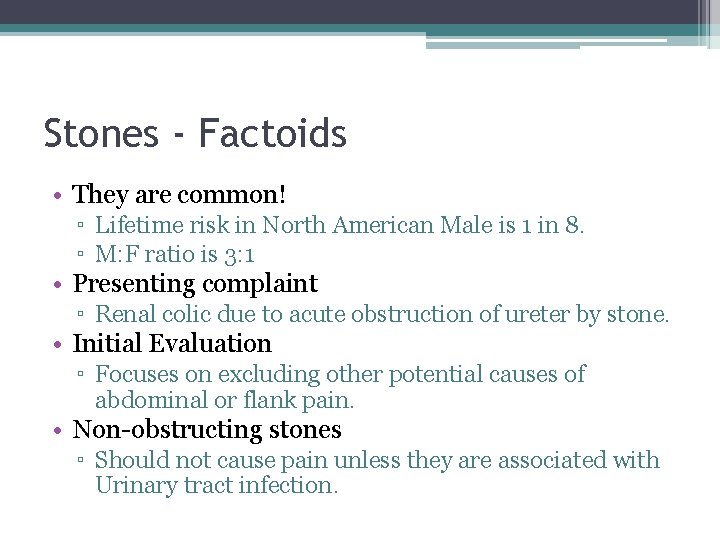
Stones - Factoids • They are common! ▫ Lifetime risk in North American Male is 1 in 8. ▫ M: F ratio is 3: 1 • Presenting complaint ▫ Renal colic due to acute obstruction of ureter by stone. • Initial Evaluation ▫ Focuses on excluding other potential causes of abdominal or flank pain. • Non-obstructing stones ▫ Should not cause pain unless they are associated with Urinary tract infection.
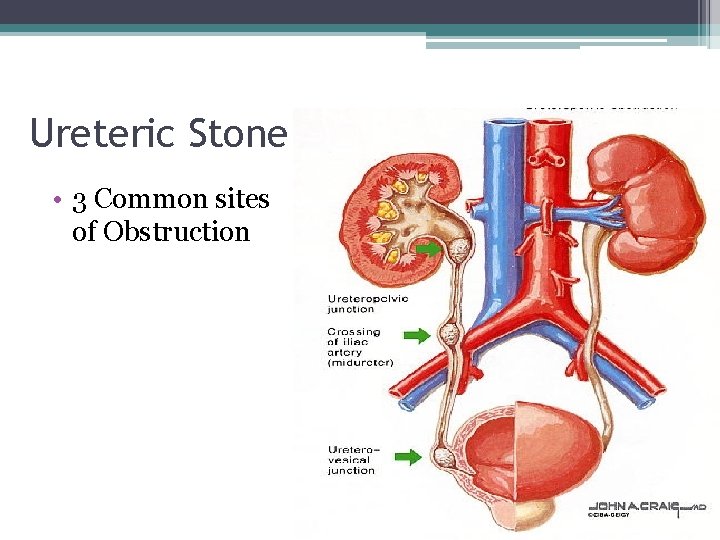
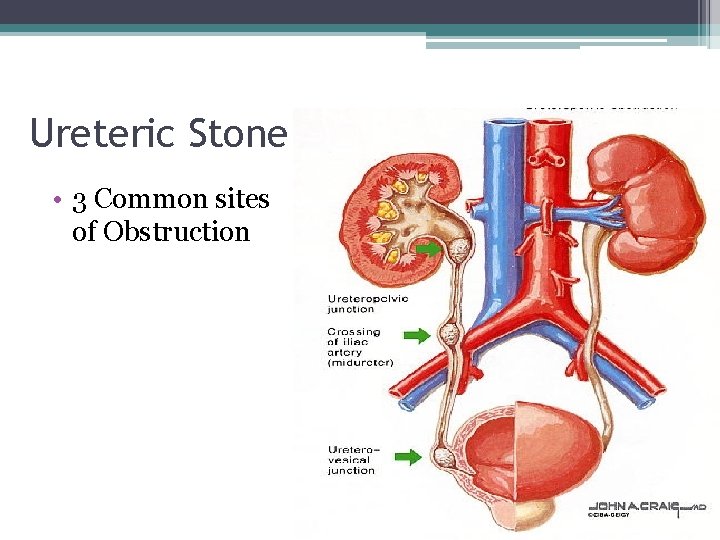
Ureteric Stone • 3 Common sites of Obstruction
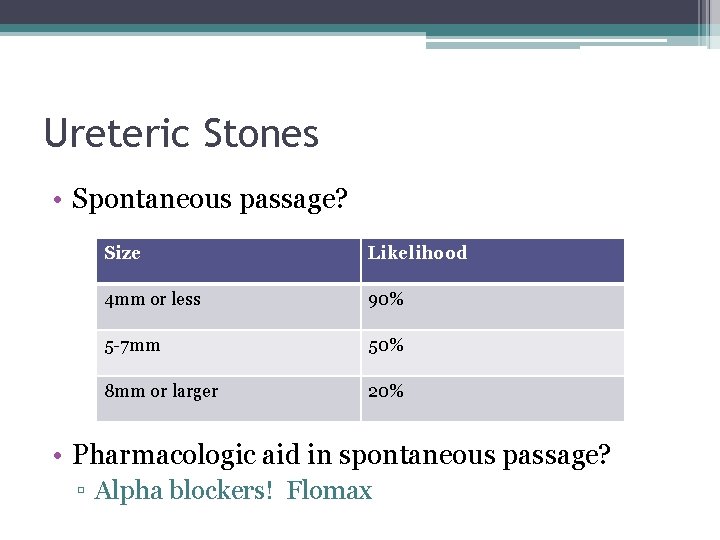
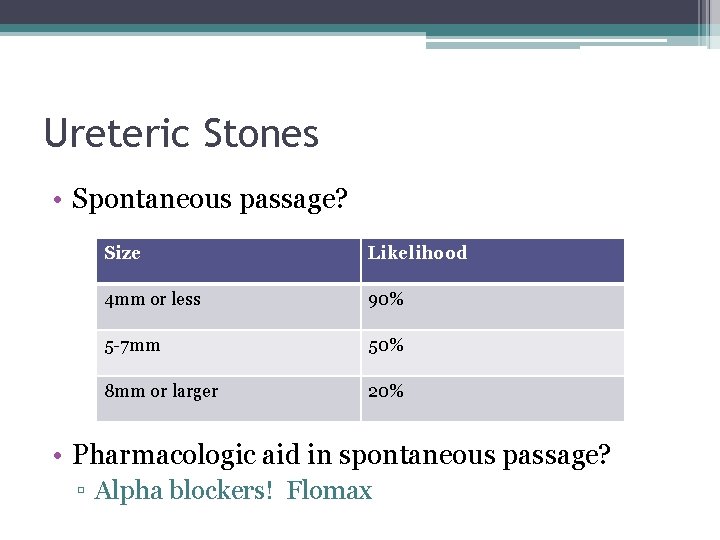
Ureteric Stones • Spontaneous passage? Size Likelihood 4 mm or less 90% 5 -7 mm 50% 8 mm or larger 20% • Pharmacologic aid in spontaneous passage? ▫ Alpha blockers! Flomax
Renal and Ureteric Stones • So you have established that there is a stone. ▫ When is ‘immediate’ referral to a Urologist Necessary?
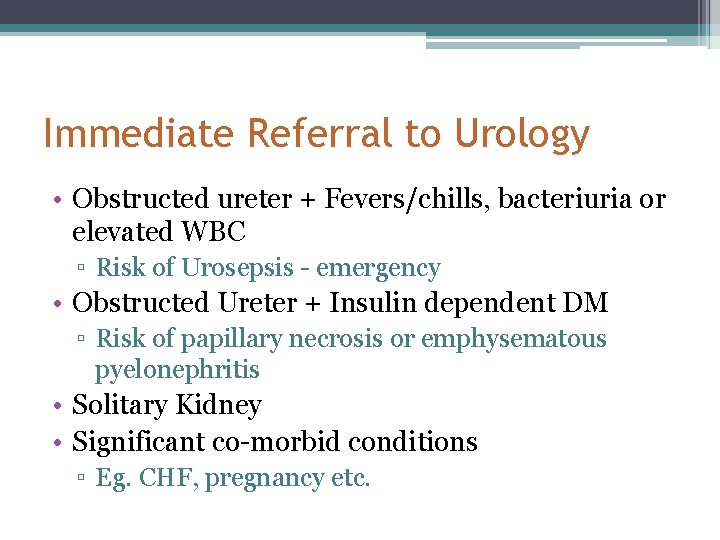
Immediate Referral to Urology • Obstructed ureter + Fevers/chills, bacteriuria or elevated WBC ▫ Risk of Urosepsis - emergency • Obstructed Ureter + Insulin dependent DM ▫ Risk of papillary necrosis or emphysematous pyelonephritis • Solitary Kidney • Significant co-morbid conditions ▫ Eg. CHF, pregnancy etc.
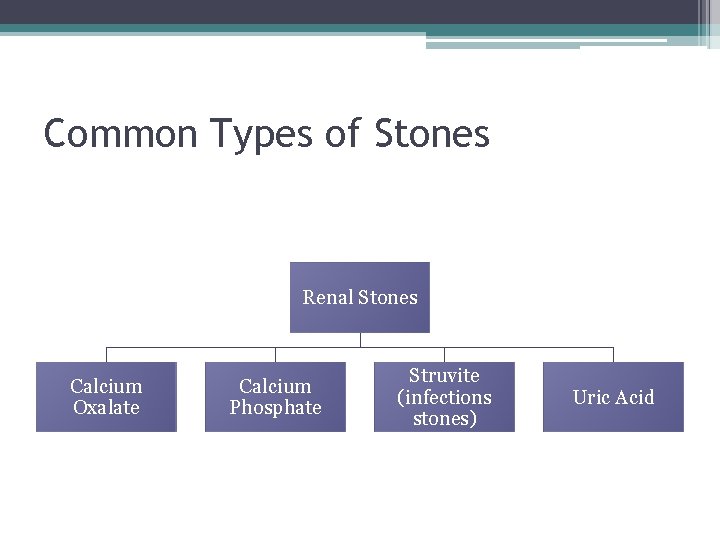
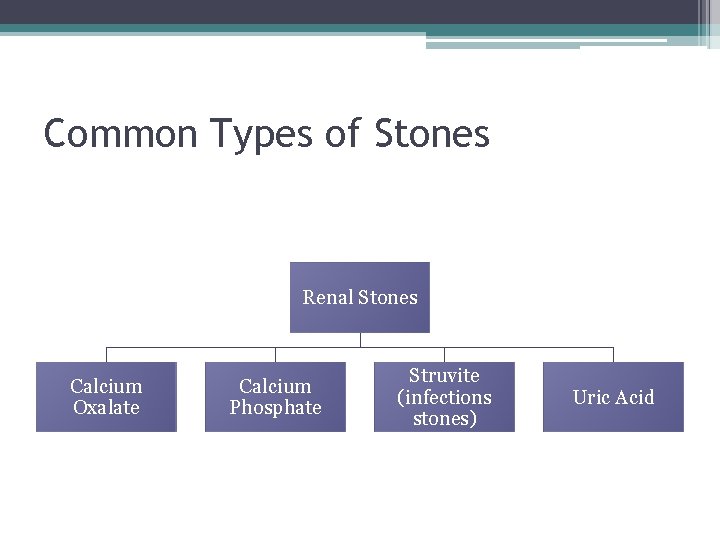
Common Types of Stones Renal Stones Calcium Oxalate Calcium Phosphate Struvite (infections stones) Uric Acid
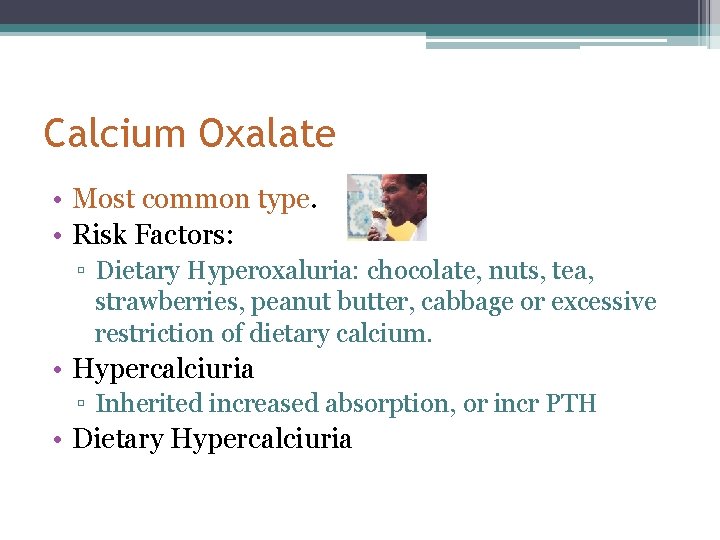
Calcium Oxalate • Most common type. • Risk Factors: ▫ Dietary Hyperoxaluria: chocolate, nuts, tea, strawberries, peanut butter, cabbage or excessive restriction of dietary calcium. • Hypercalciuria ▫ Inherited increased absorption, or incr PTH • Dietary Hypercalciuria
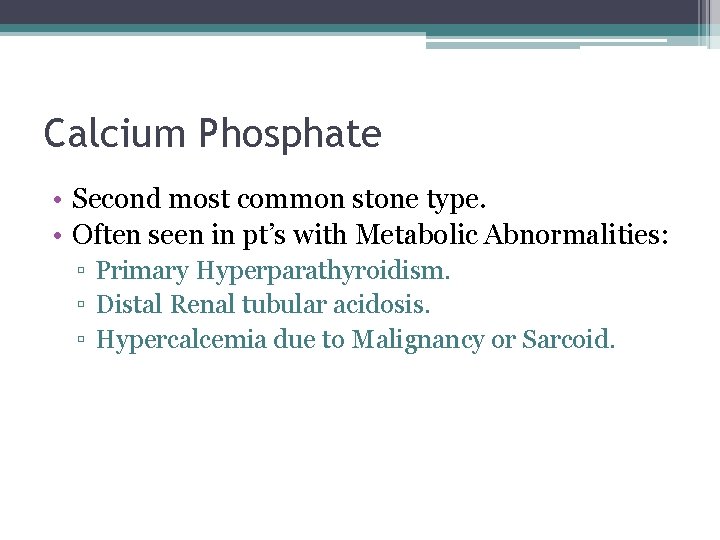
Calcium Phosphate • Second most common stone type. • Often seen in pt’s with Metabolic Abnormalities: ▫ Primary Hyperparathyroidism. ▫ Distal Renal tubular acidosis. ▫ Hypercalcemia due to Malignancy or Sarcoid.
Uric Acid • Radiolucent on Plain X-Rays, but is visualized on CT scan • Risk Factors: ▫ Persistent Acidic urine: ie l �Low urine volumes �Chronic diarrhea �Excessive sweating �Inadequate fluid intake ▫ Gout (Hyperuricemia) ▫ Excess dietary purine (Meataholics) ▫ Chemotherapy for lymphoma, leukemia
Struvite (Infection Stones) • Composed of MAP ▫ Magnesium + Ammonium Phosphate & Calcium • Can only form if urine p. H >8. 0! ▫ Thus: usually only in presence of urease +ve bacteria �Proteus, Klebsiella, Providentia, Pseudomonas, Staph Aureus �Note: E Coli does NOT produce urease • Tend to form Staghorn stones

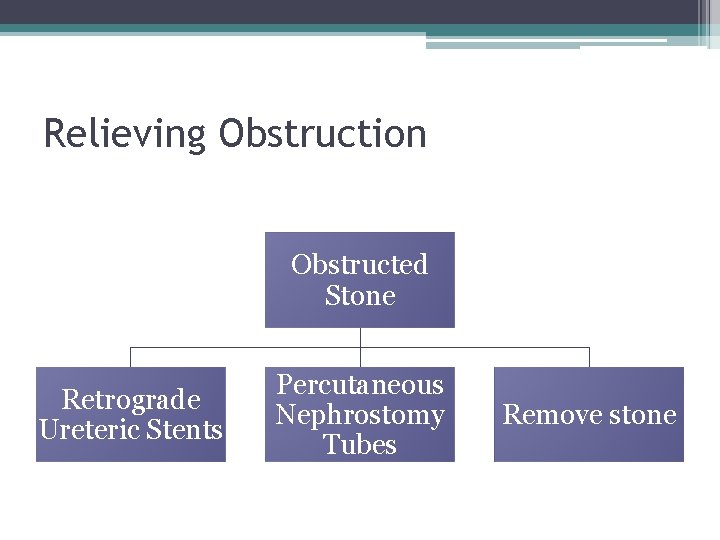
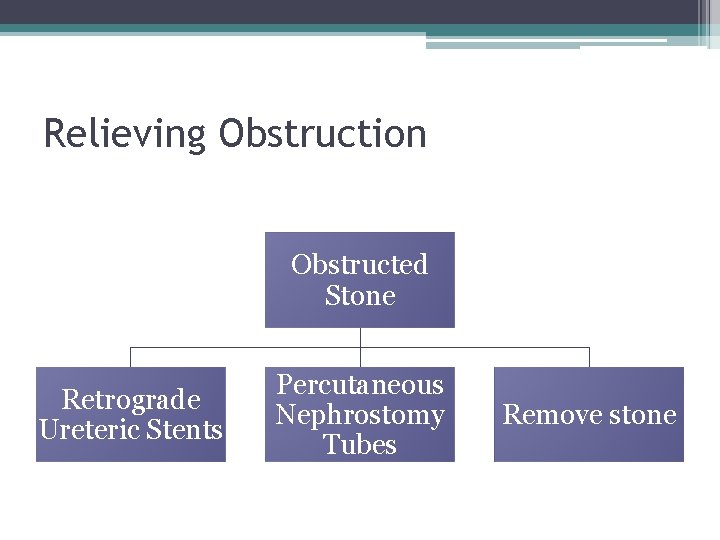
Relieving Obstruction Obstructed Stone Retrograde Ureteric Stents Percutaneous Nephrostomy Tubes Remove stone
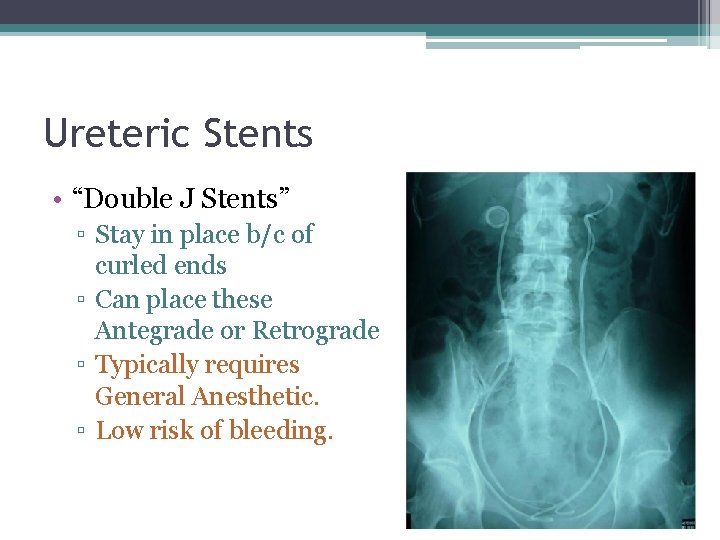
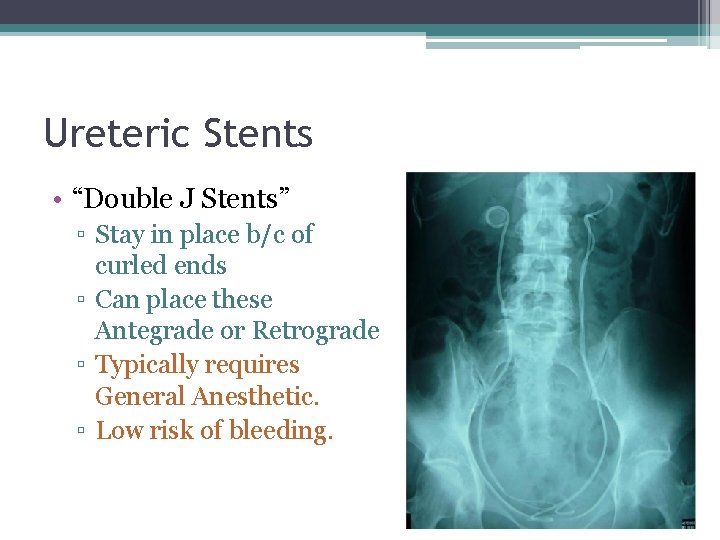
Ureteric Stents • “Double J Stents” ▫ Stay in place b/c of curled ends ▫ Can place these Antegrade or Retrograde ▫ Typically requires General Anesthetic. ▫ Low risk of bleeding.
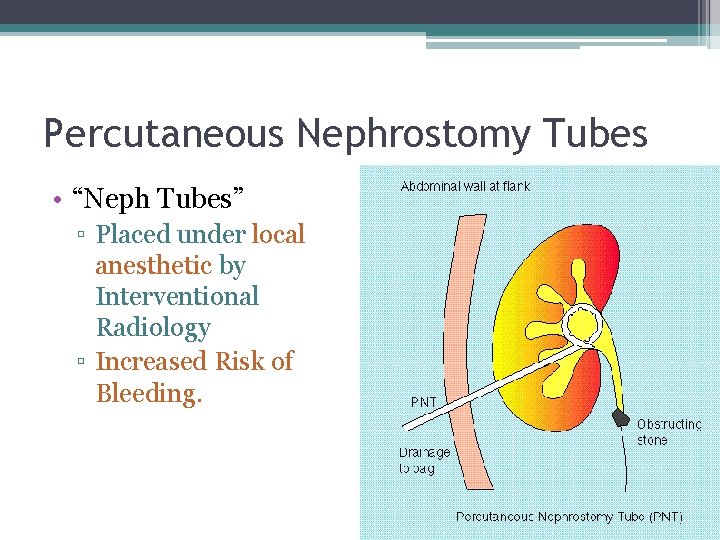
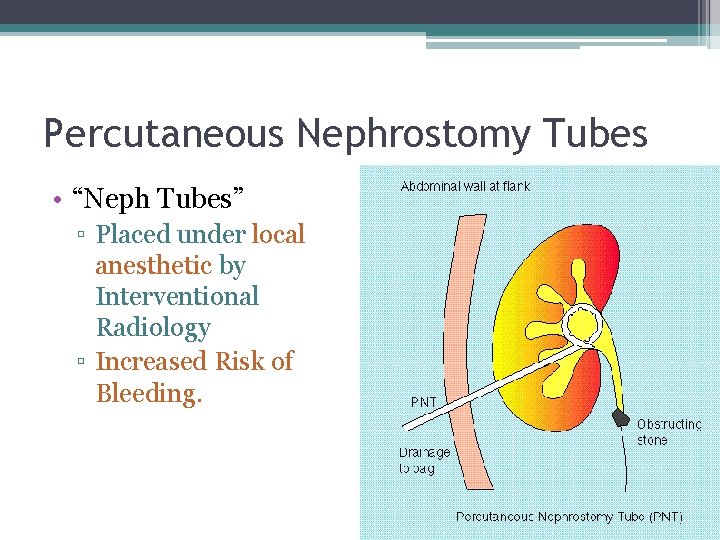
Percutaneous Nephrostomy Tubes • “Neph Tubes” ▫ Placed under local anesthetic by Interventional Radiology ▫ Increased Risk of Bleeding.
Treating/Removing Stones • Ways to Treat stones. ▫ Conservative passage + Alpha Blocker (Flomax) + Hydration + NSAID (if Normal GFR) ▫ Extracorporeal Shockwave Lithotripsy (ESWL) ▫ Ureteroscopy + Basket or Laser ▫ Percutaneous Nephrolithotomy
Treating Stones • Conservative passage + Alpha Blocker (Flomax) + Hydration + NSAID (if Normal GFR) ▫ Indications �Pain can be controlled with Ketorolac + Narcotic �No renal impairment �No Intractable Vomiting (aka pt not hypovolemic) �No sign of infection. �No previous failed trials of conservative passage.
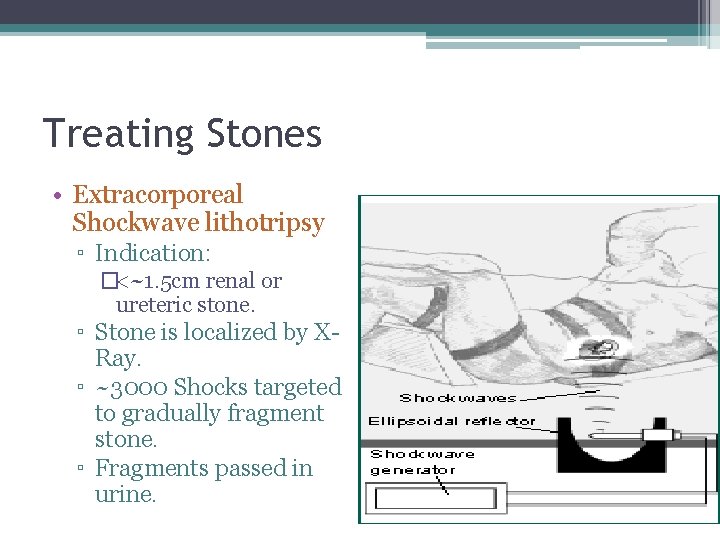
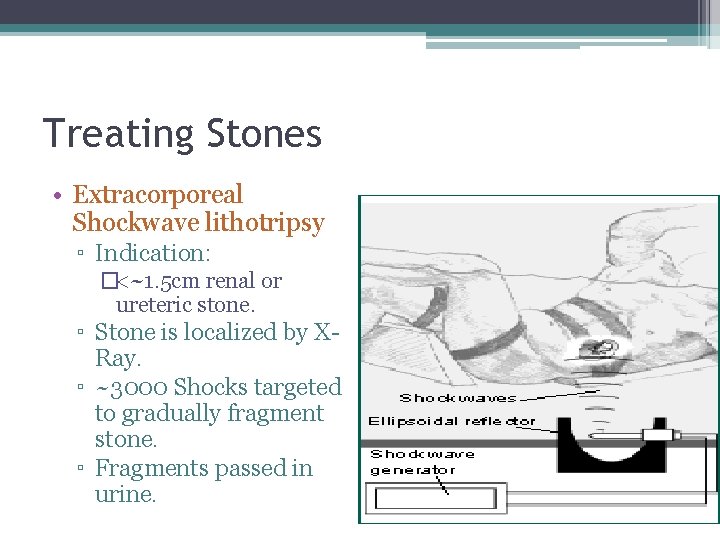
Treating Stones • Extracorporeal Shockwave lithotripsy ▫ Indication: �<~1. 5 cm renal or ureteric stone. ▫ Stone is localized by XRay. ▫ ~3000 Shocks targeted to gradually fragment stone. ▫ Fragments passed in urine.
Treating Stones • Ureteroscopy ▫ + Basket �If stone is small enough to adequately remove by basket. ▫ + Holmium Laser �If stone is ‘impacted’ or cannot simply be basketed out.


Treating Stones • Percutaneous Nephrolithotomy ▫ Indications �Large Proximal ureteric or Renal Calculi >~1 -1. 5 cm �Treatment of Staghorn Calculi ▫ Risks: �Bleeding �Renal Perforation or Avulsion

• http: //www. youtube. com/watch? v=ir. KCg. Fr. AO RA
Outline • Hematuria ▫ DDx ▫ General Work up • Renal Colic ▫ Stones • Malignancy ▫ Renal ▫ Bladder • Scrotal masses
Renal Mass Objectives: 1. Give a differential diagnosis for a solid mass in the kidney. 2. Describe the evaluation of a patient with a suspected renal cell carcinoma 3. Give three indications for a partial nephrectomy rather than a radical nephrectomy for renal cell carcinoma.
Renal Tumors • Presentation: ▫ Incidental finding! ▫ Triad: Flank pain, hematuria, palpable mass (not common) • How do you ‘work-up’ a Renal mass?
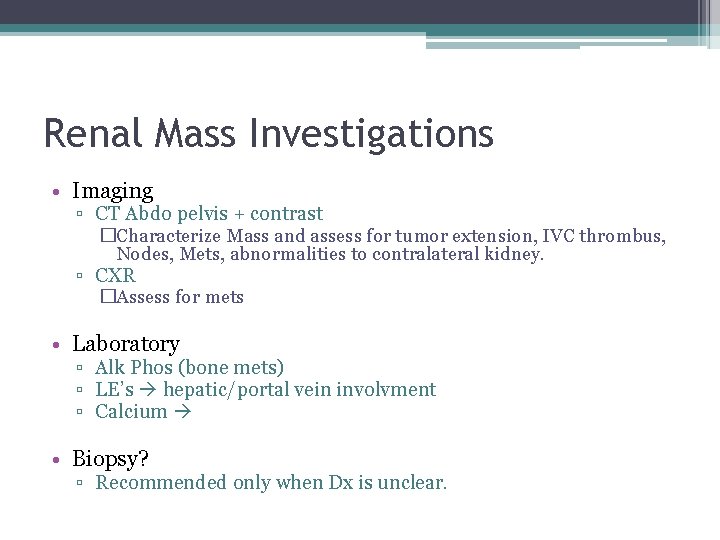
Renal Mass Investigations • Imaging ▫ CT Abdo pelvis + contrast �Characterize Mass and assess for tumor extension, IVC thrombus, Nodes, Mets, abnormalities to contralateral kidney. ▫ CXR �Assess for mets • Laboratory ▫ Alk Phos (bone mets) ▫ LE’s hepatic/portal vein involvment ▫ Calcium • Biopsy? ▫ Recommended only when Dx is unclear.
Why Investigate Calcium? • Bone Mets or Paraneoplastic syndrome! ▫ 20 -30% of RCC have Paraneoplastic Syndrome �Increased ESR �Wt loss, cachexia �Fever �Anemia �Hypertension (incr Renin) �Hypercalcemia (PTH-like Substance) �Incr ALP �Polycythemia (incr EPO production) �Stauffer’s syndrome – reversible hepatitis
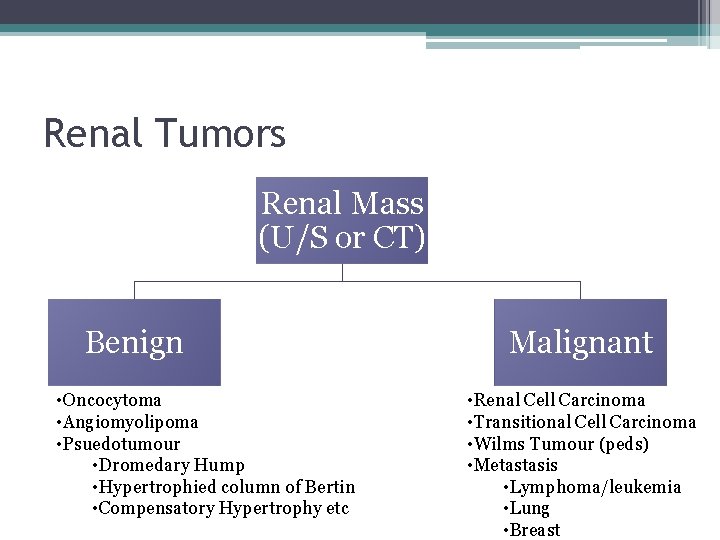
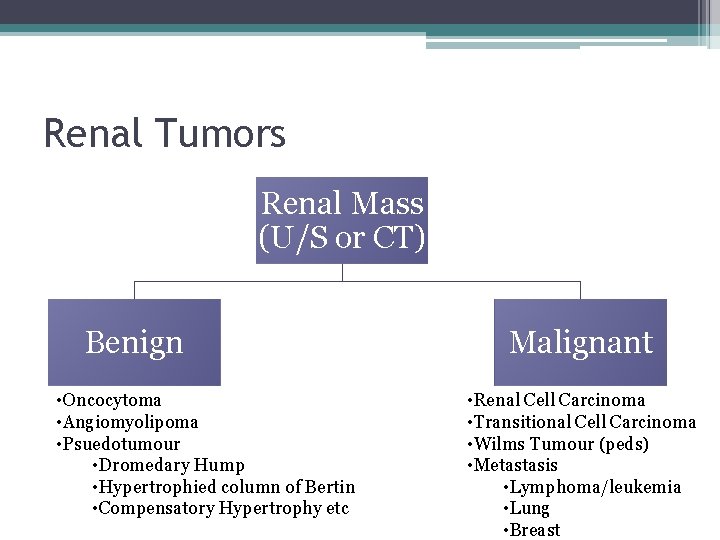
Renal Tumors Renal Mass (U/S or CT) Benign • Oncocytoma • Angiomyolipoma • Psuedotumour • Dromedary Hump • Hypertrophied column of Bertin • Compensatory Hypertrophy etc Malignant • Renal Cell Carcinoma • Transitional Cell Carcinoma • Wilms Tumour (peds) • Metastasis • Lymphoma/leukemia • Lung • Breast
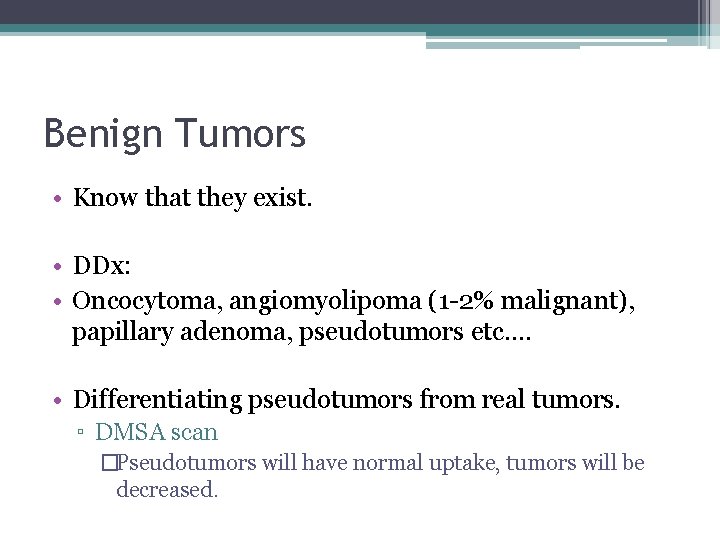
Benign Tumors • Know that they exist. • DDx: • Oncocytoma, angiomyolipoma (1 -2% malignant), papillary adenoma, pseudotumors etc…. • Differentiating pseudotumors from real tumors. ▫ DMSA scan �Pseudotumors will have normal uptake, tumors will be decreased.
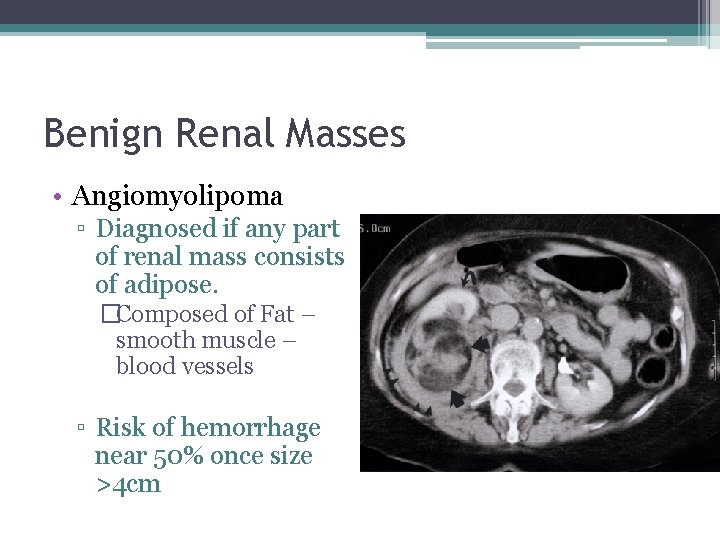
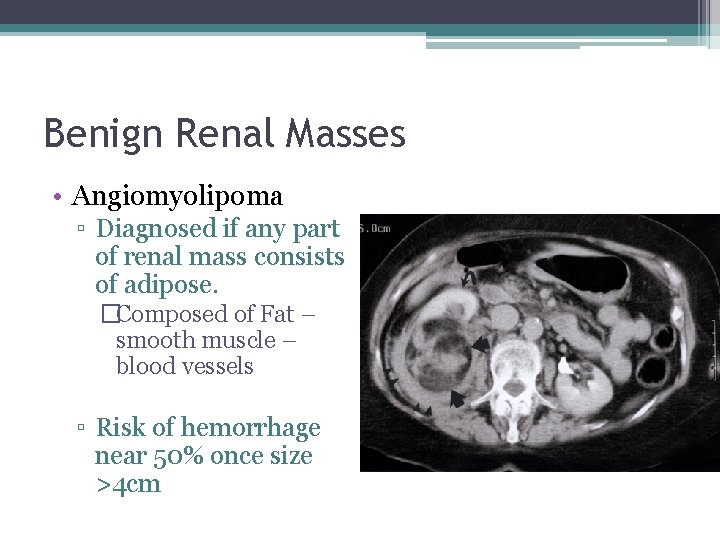
Benign Renal Masses • Angiomyolipoma ▫ Diagnosed if any part of renal mass consists of adipose. �Composed of Fat – smooth muscle – blood vessels ▫ Risk of hemorrhage near 50% once size >4 cm
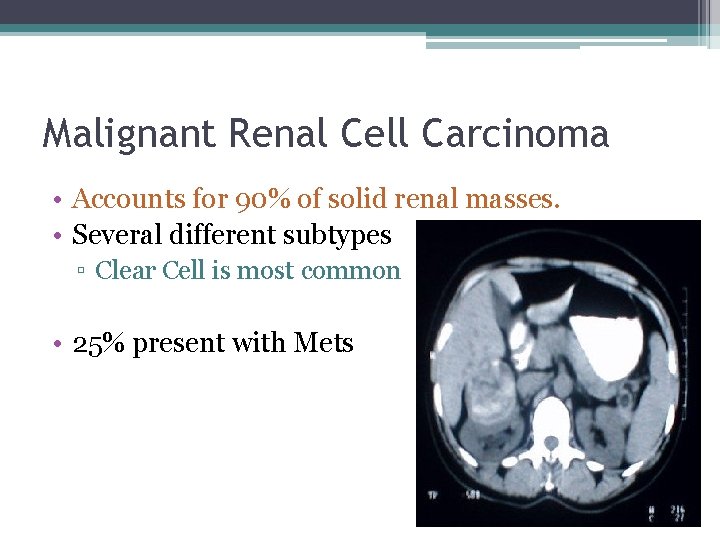
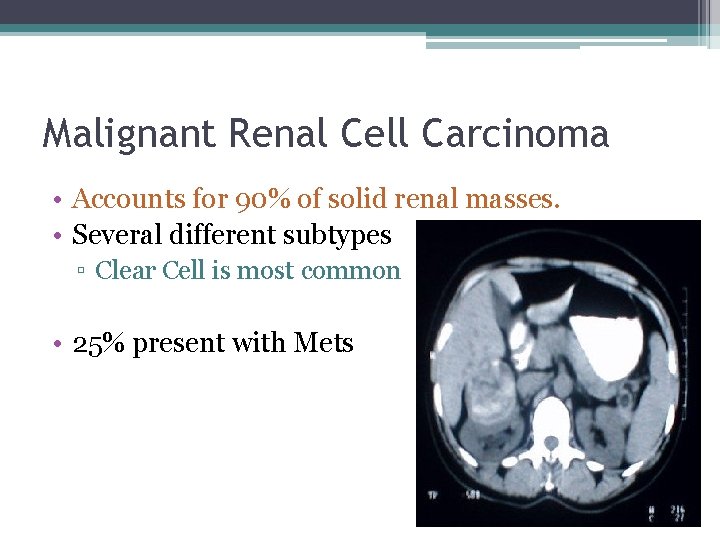
Malignant Renal Cell Carcinoma • Accounts for 90% of solid renal masses. • Several different subtypes ▫ Clear Cell is most common • 25% present with Mets
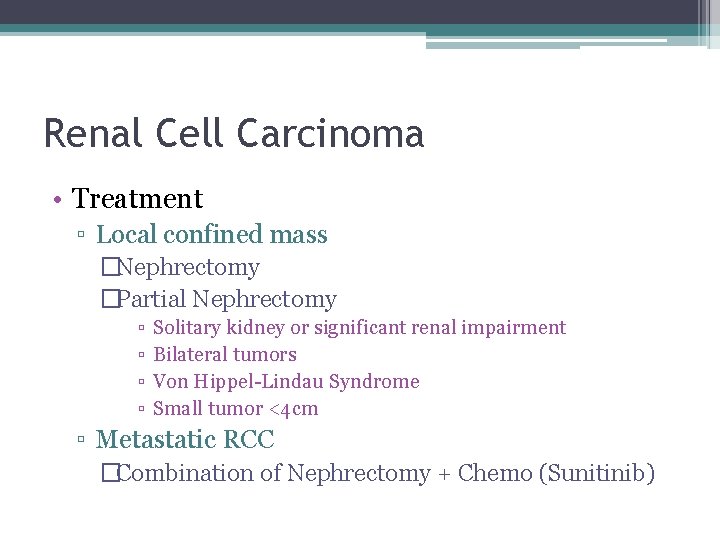
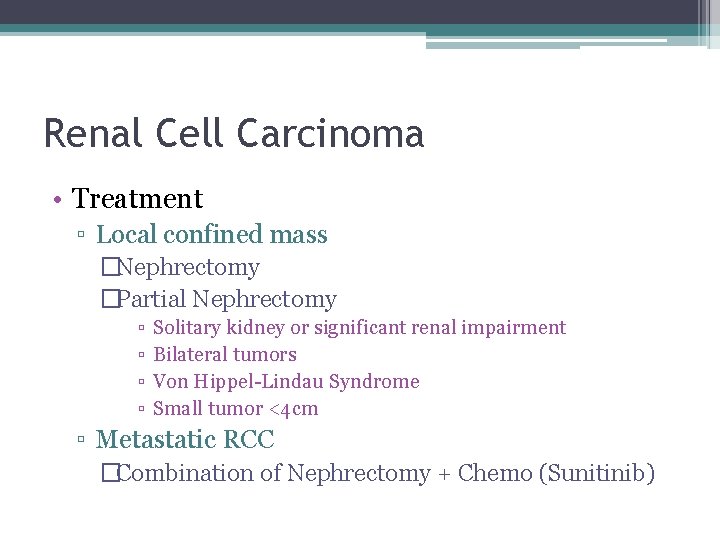
Renal Cell Carcinoma • Treatment ▫ Local confined mass �Nephrectomy �Partial Nephrectomy ▫ ▫ Solitary kidney or significant renal impairment Bilateral tumors Von Hippel-Lindau Syndrome Small tumor <4 cm ▫ Metastatic RCC �Combination of Nephrectomy + Chemo (Sunitinib)
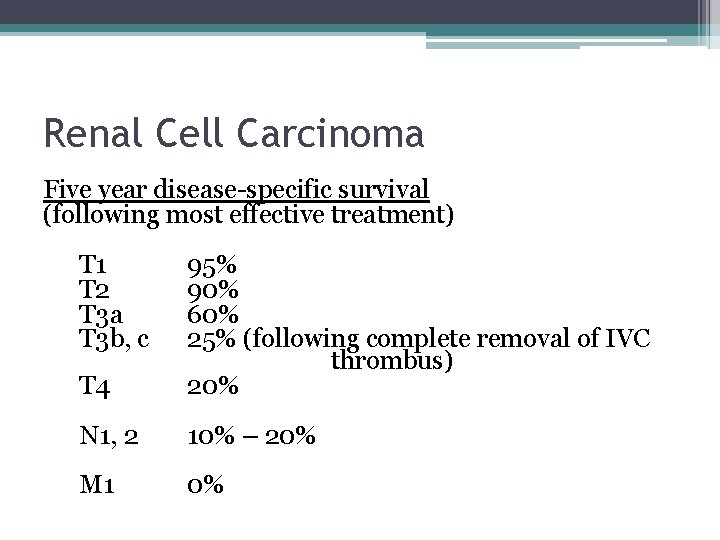
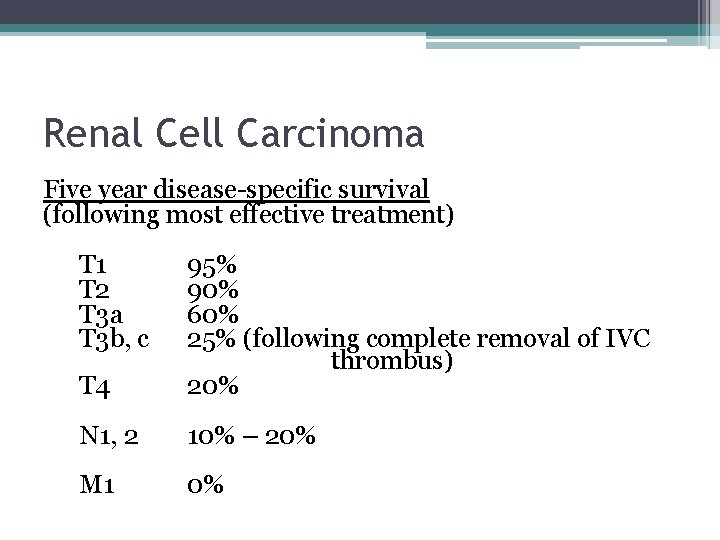
Renal Cell Carcinoma Five year disease-specific survival (following most effective treatment) T 1 T 2 T 3 a T 3 b, c T 4 95% 90% 60% 25% (following complete removal of IVC thrombus) 20% N 1, 2 10% – 20% M 1 0%
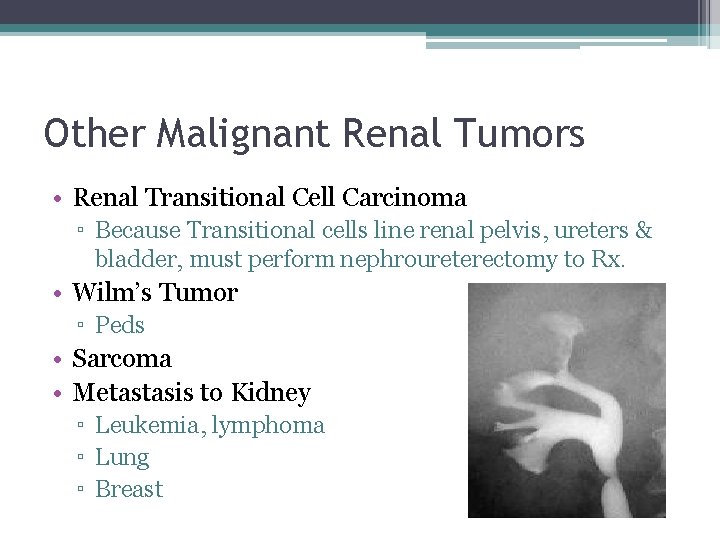
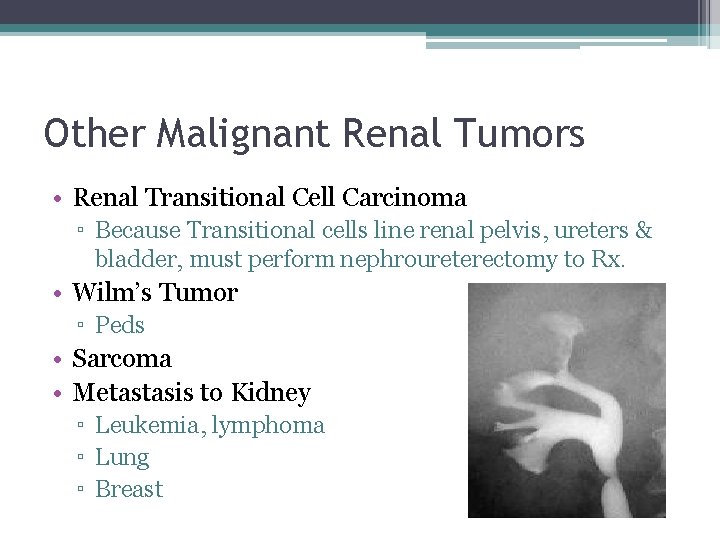
Other Malignant Renal Tumors • Renal Transitional Cell Carcinoma ▫ Because Transitional cells line renal pelvis, ureters & bladder, must perform nephroureterectomy to Rx. • Wilm’s Tumor ▫ Peds • Sarcoma • Metastasis to Kidney ▫ Leukemia, lymphoma ▫ Lung ▫ Breast

Bladder Cancer Objectives: 1. State 3 risk factors for transitional cell carcinoma of the bladder 2. State the treatment options for superficial and invasive TCC of the bladder
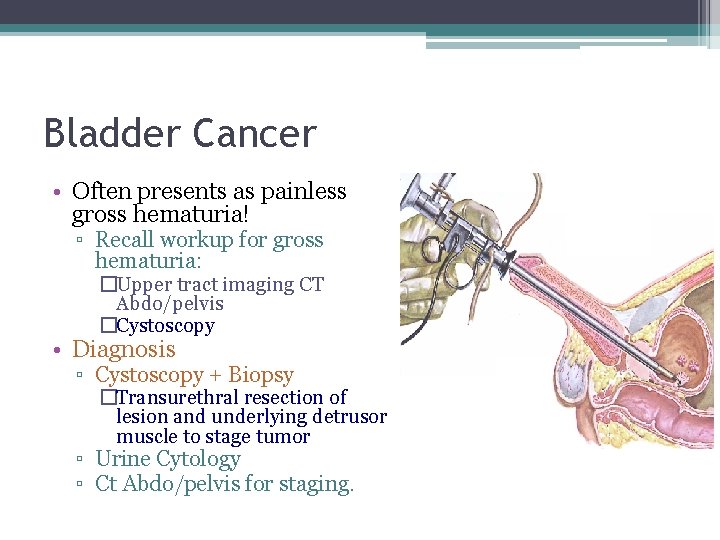
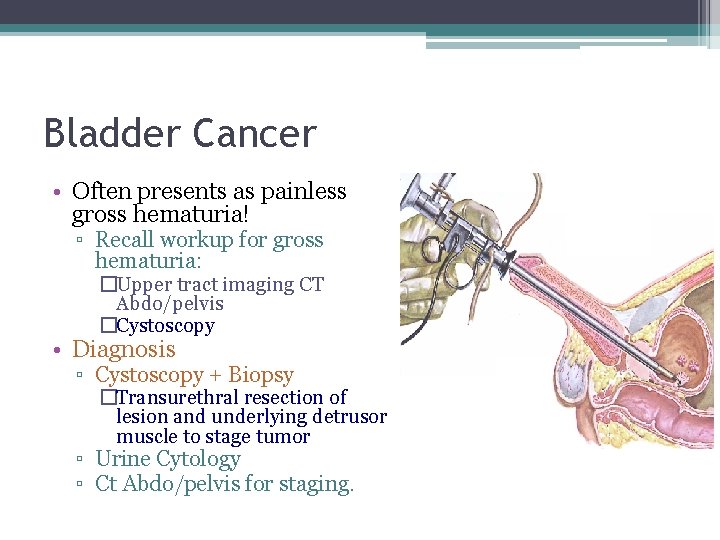
Bladder Cancer • Often presents as painless gross hematuria! ▫ Recall workup for gross hematuria: �Upper tract imaging CT Abdo/pelvis �Cystoscopy • Diagnosis ▫ Cystoscopy + Biopsy �Transurethral resection of lesion and underlying detrusor muscle to stage tumor ▫ Urine Cytology ▫ Ct Abdo/pelvis for staging.
Bladder Cancer • Risk Factors ▫ SMOKING (RR 4 vs non smokers) ▫ Occupational Exposure �Aniline dyes, aromatic amines �Ie. Textile manufacturing, dry cleaning, painting) ▫ Previous Cyclophosphamide �(ie chemo for lymphoma) ▫ Previous Radiaiton Rx in pelvis
Bladder Cancer • DDx • Transitional Cell carcinoma ▫ Most common! • Adenocarcinoma ▫ Dome of bladder, associated with Urachus. • Squamous Cell Carcinoma ▫ Associated with chronic inflammation �Indwelling foley’s, bladder stones.
Transitional Cell Carcinoma • Staging ▫ Non-invasive �Tis, Ta, T 1 disease ▫ Invasive �>T 1 disease (muscle invasive

Treatment of Non-invasive TCC • 1. Transurethral resection of lesion • 2. PLUS intravesical chemotherapy IF: ▫ ▫ ▫ Carcinoma in-situ Multi focal tumors Unable to completely resect transurethrally Rapid recurrence after initial resection Superficial, high grade tumor Lamina propria invasion (Stage T 1)
Treatment of Non-invasive TCC • Intravesical Chemotherapeutic Agents: ▫ ▫ Bacille Calmette-Guerin (BCG) Mitomycin Doxorubicin Thiotepa
Treatment of Non-Invasive TCC • But…. IF: ▫ Persistent CIS after intravesical chemotherapy ▫ Extensive superficial tumors that cannot be resected. • Then Pt will require Radical Cystectomy and Urinary diversion for curative intent.
Treatment of Invasive TCC • Radical Cystectomy • +/- Chemotherapy for metastatic disease • If palliative, may still require cystectomy if uncontrollable hematuria (requiring transfusions etc)
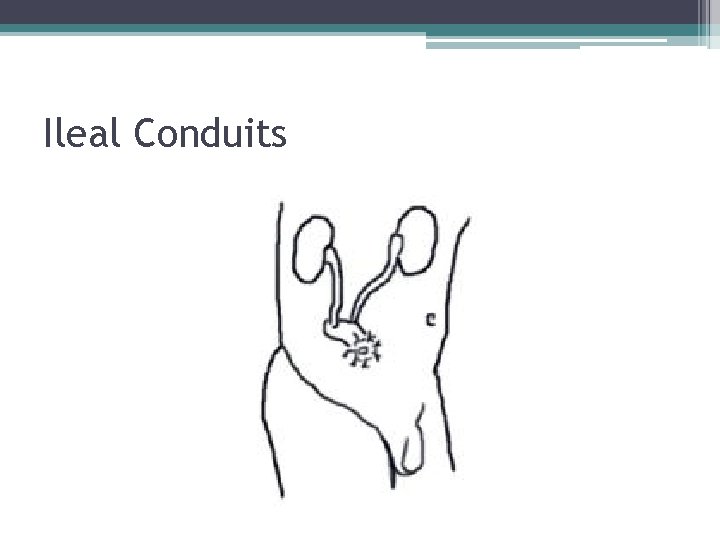
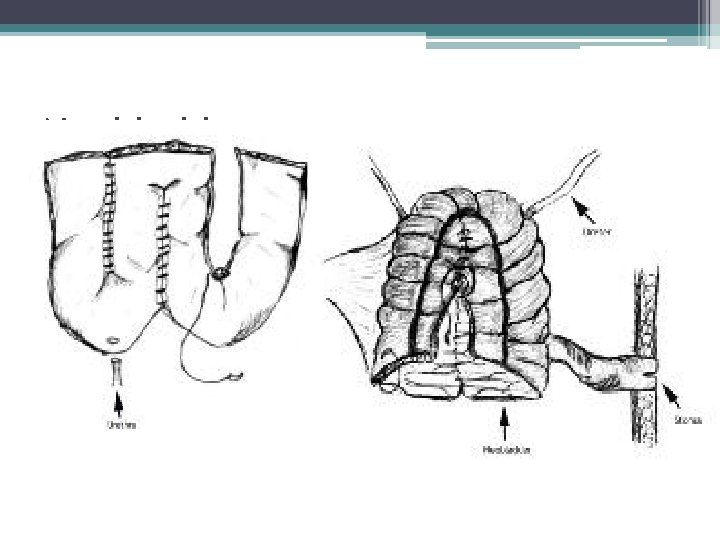
Radical Cystectomy + Urinary Diversion • Once Bladder is removed… • Urinary diversion is needed ▫ Ileal Conduit �Pros – simple, least complications �Cons – abdominal stoma, no continence. ▫ Neobladder �Pros – continent with use of catheters �Cons – Increased surgical complications, increased risk of metabolic derrangements.
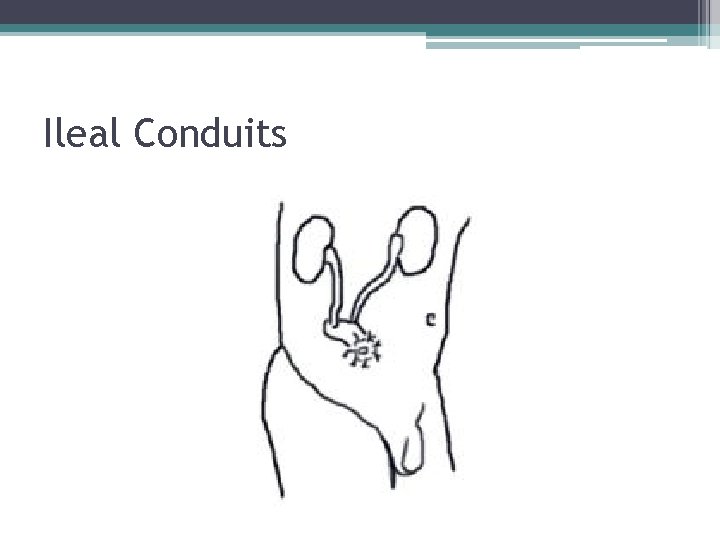
Ileal Conduits
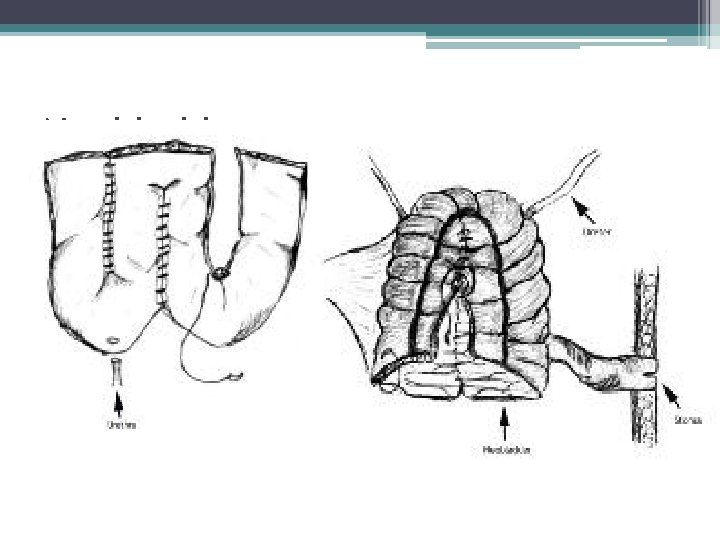
Neobladders
Scrotal Mass Objectives • Differential diagnosis of a scrotal mass • Know how to diagnose and treat testicular torsion • Classify testicular tumors • Treatment of testicular malignancies
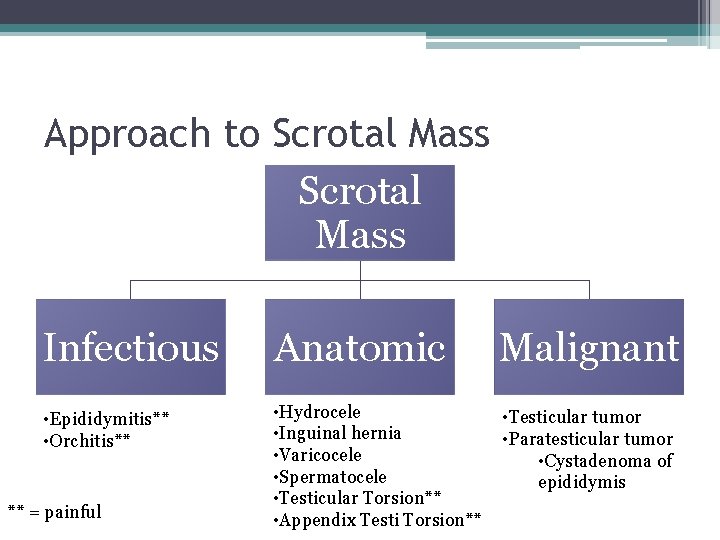
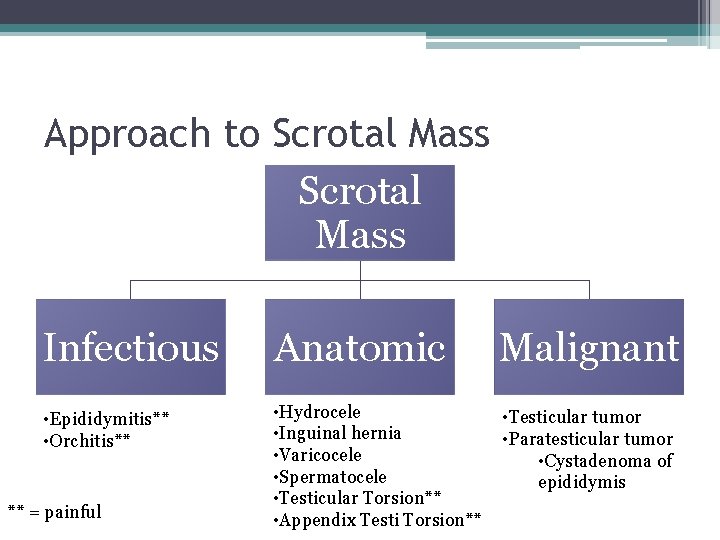
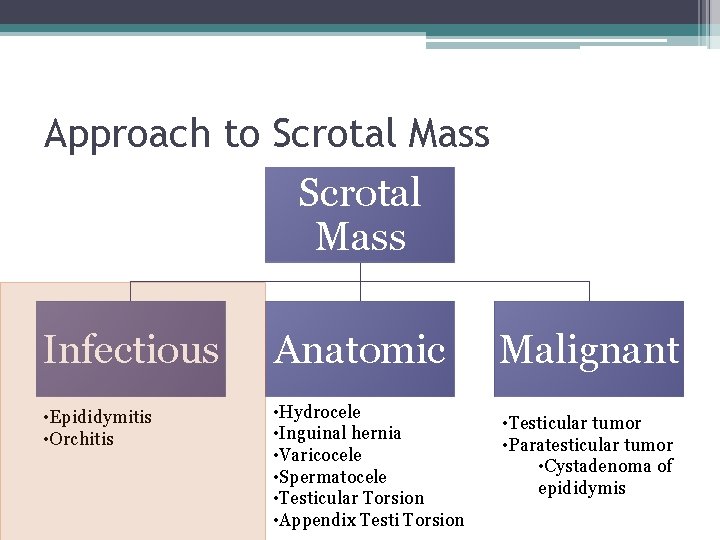
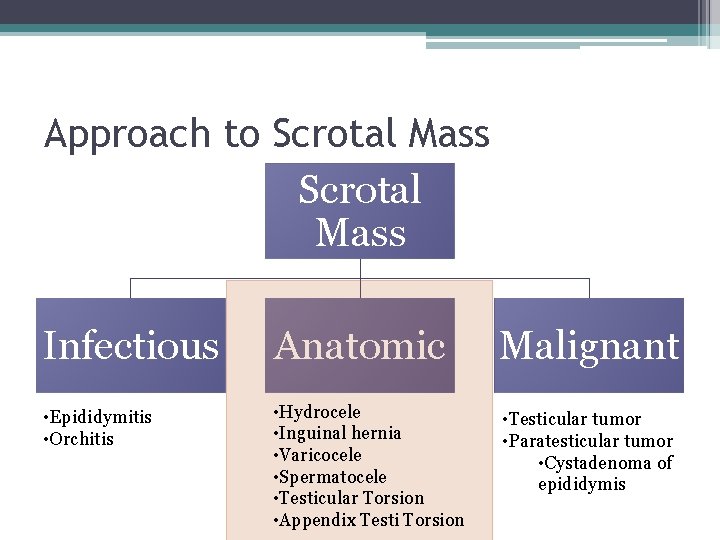
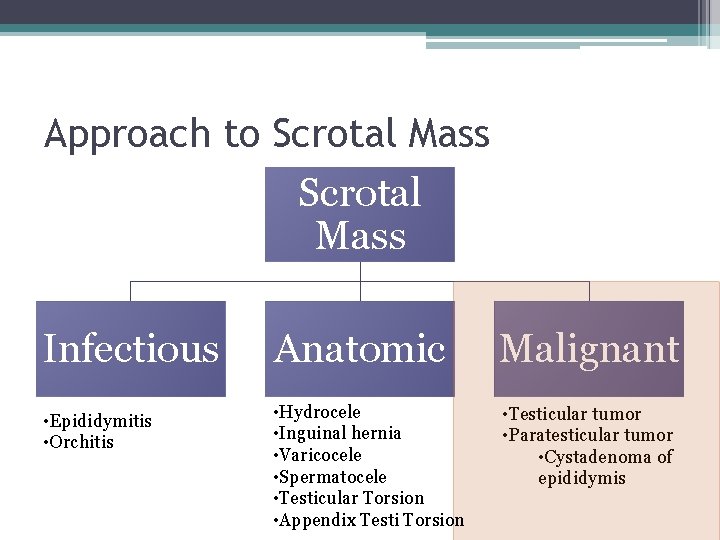
Approach to Scrotal Mass Infectious Anatomic Malignant • Epididymitis** • Orchitis** • Hydrocele • Inguinal hernia • Varicocele • Spermatocele • Testicular Torsion** • Appendix Testi Torsion** • Testicular tumor • Paratesticular tumor • Cystadenoma of epididymis ** = painful
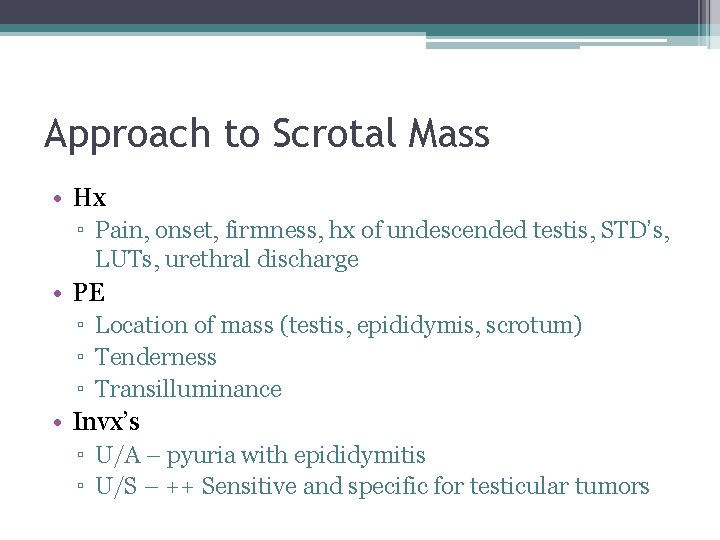
Approach to Scrotal Mass • Hx ▫ Pain, onset, firmness, hx of undescended testis, STD’s, LUTs, urethral discharge • PE ▫ Location of mass (testis, epididymis, scrotum) ▫ Tenderness ▫ Transilluminance • Invx’s ▫ U/A – pyuria with epididymitis ▫ U/S – ++ Sensitive and specific for testicular tumors
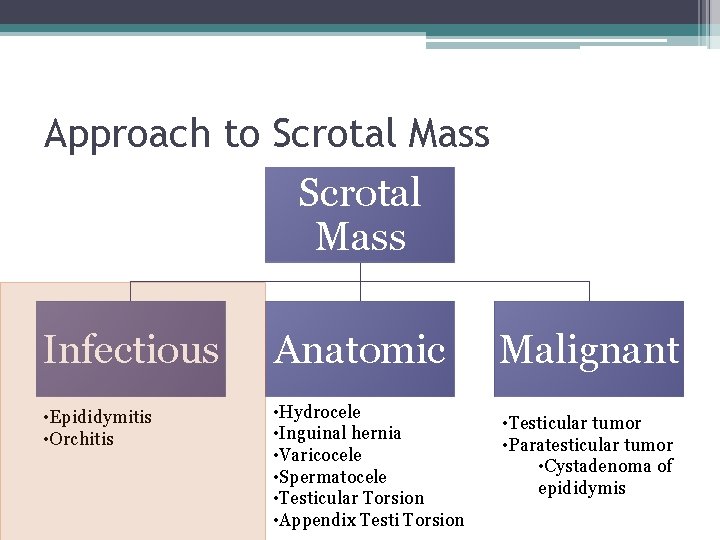
Approach to Scrotal Mass Infectious Anatomic • Epididymitis • Orchitis • Hydrocele • Inguinal hernia • Varicocele • Spermatocele • Testicular Torsion • Appendix Testi Torsion Malignant • Testicular tumor • Paratesticular tumor • Cystadenoma of epididymis
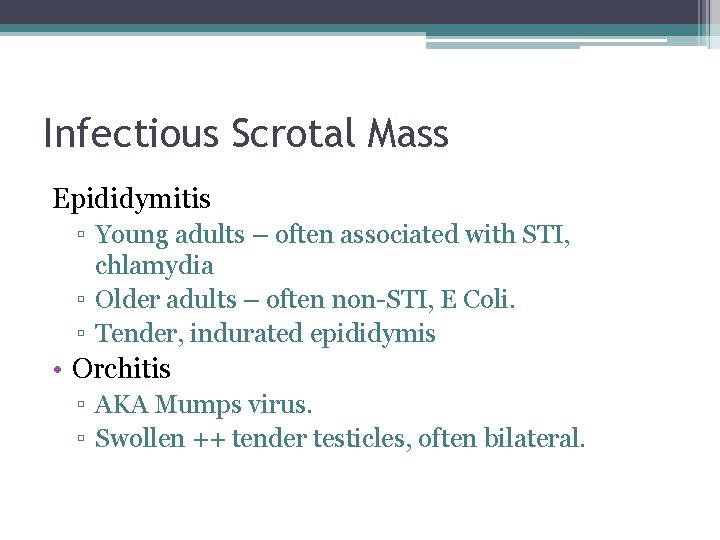
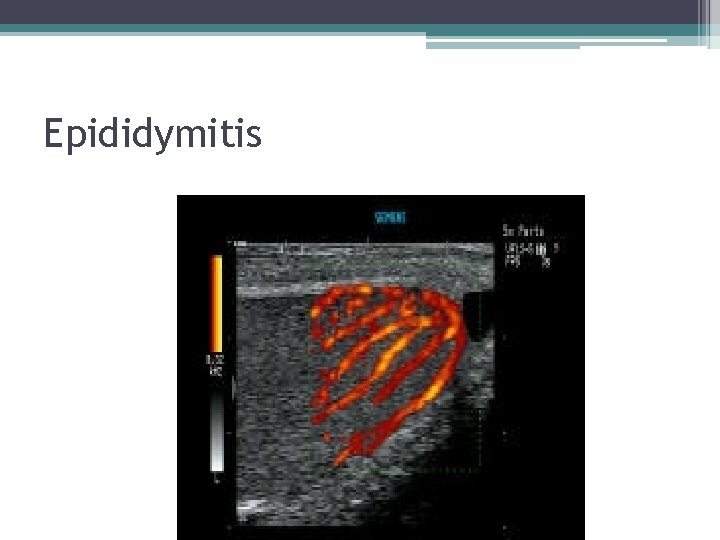
Infectious Scrotal Mass Epididymitis ▫ Young adults – often associated with STI, chlamydia ▫ Older adults – often non-STI, E Coli. ▫ Tender, indurated epididymis • Orchitis ▫ AKA Mumps virus. ▫ Swollen ++ tender testicles, often bilateral.
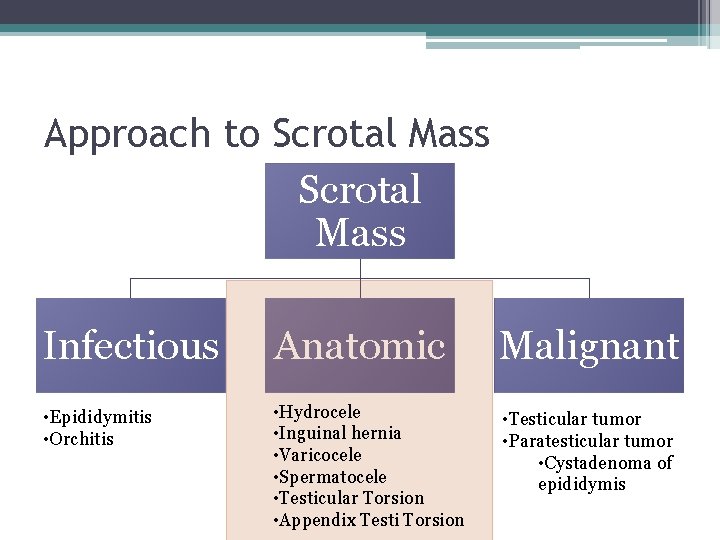
Approach to Scrotal Mass Infectious Anatomic Malignant • Epididymitis • Orchitis • Hydrocele • Inguinal hernia • Varicocele • Spermatocele • Testicular Torsion • Appendix Testi Torsion • Testicular tumor • Paratesticular tumor • Cystadenoma of epididymis
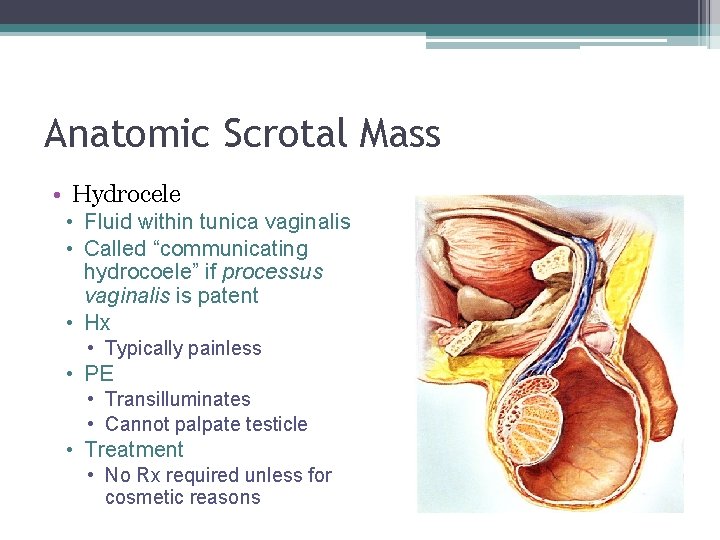
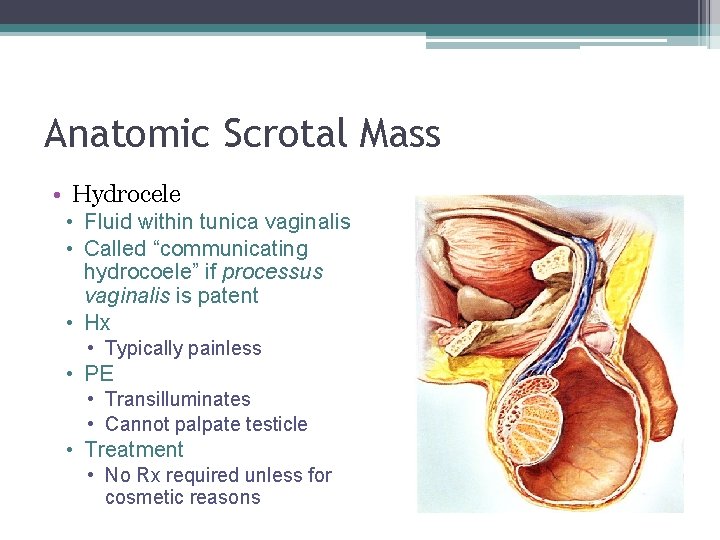
Anatomic Scrotal Mass • Hydrocele • Fluid within tunica vaginalis • Called “communicating hydrocoele” if processus vaginalis is patent • Hx • Typically painless • PE • Transilluminates • Cannot palpate testicle • Treatment • No Rx required unless for cosmetic reasons
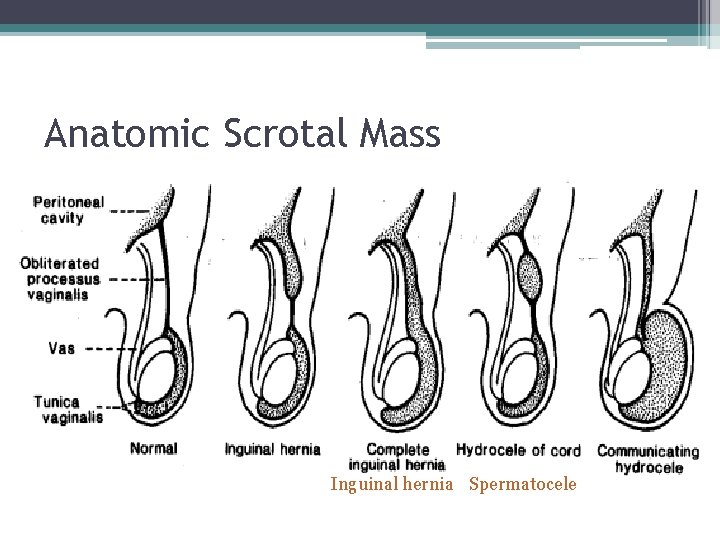
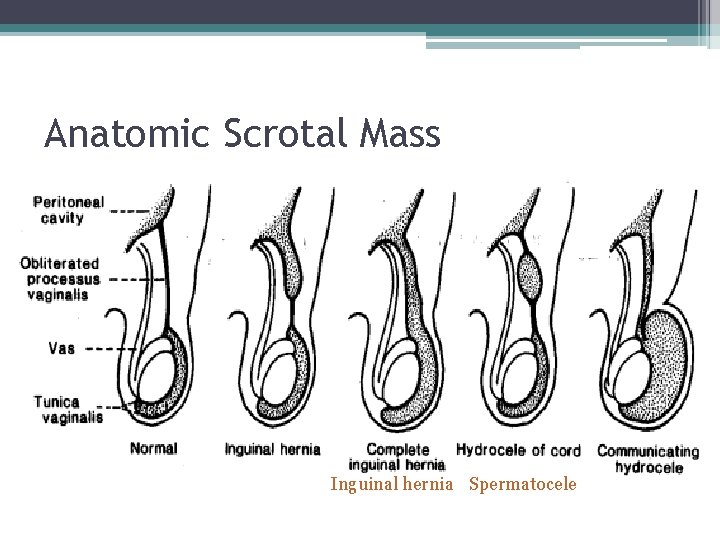
Anatomic Scrotal Mass Inguinal hernia Spermatocele
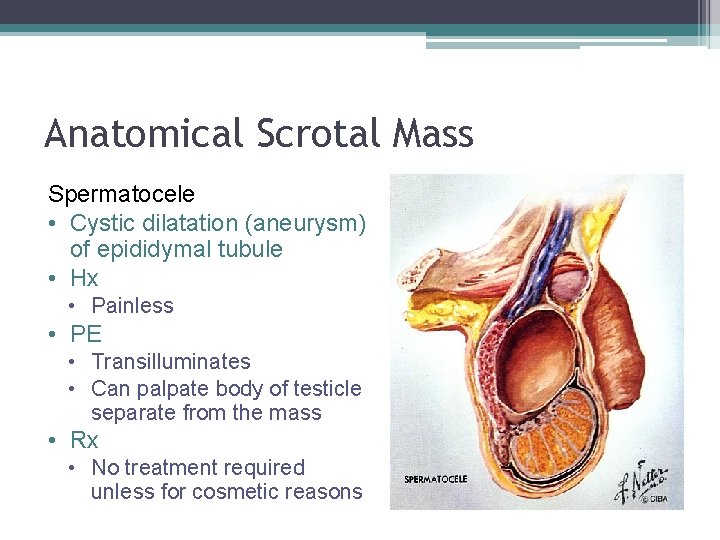
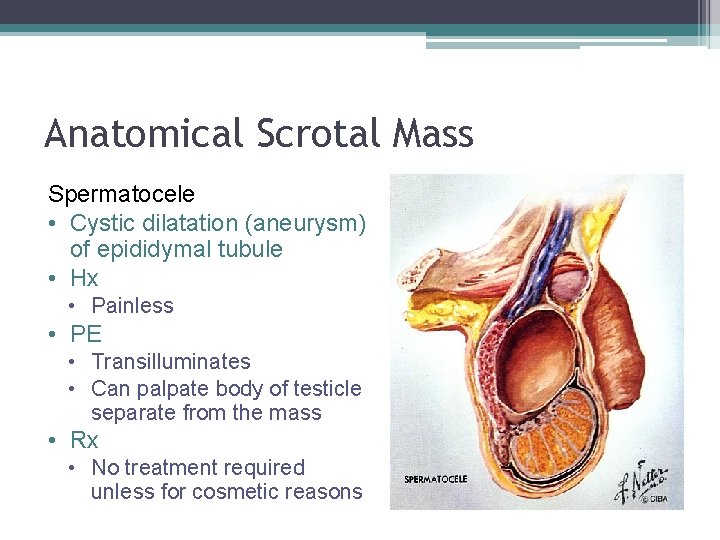
Anatomical Scrotal Mass Spermatocele • Cystic dilatation (aneurysm) of epididymal tubule • Hx • Painless • PE • Transilluminates • Can palpate body of testicle separate from the mass • Rx • No treatment required unless for cosmetic reasons
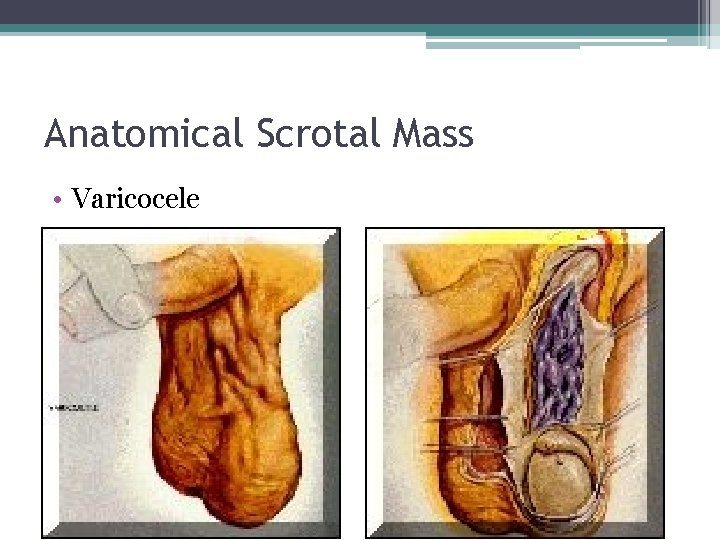
Anatomical Scrotal Mass • Varicocele
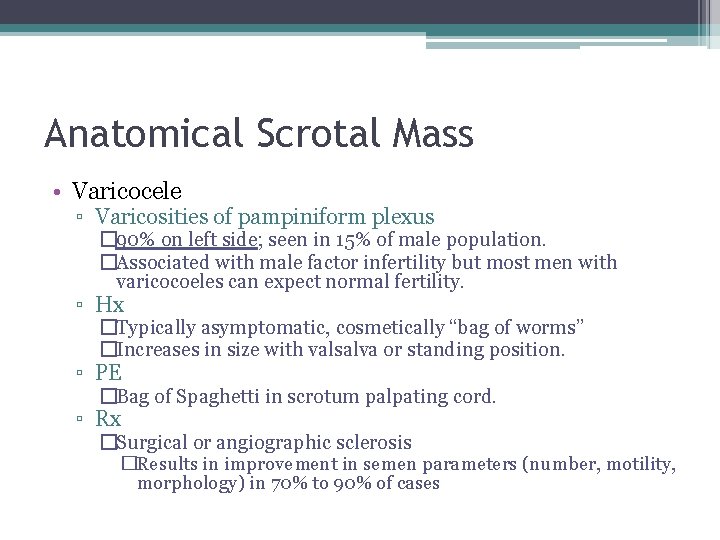
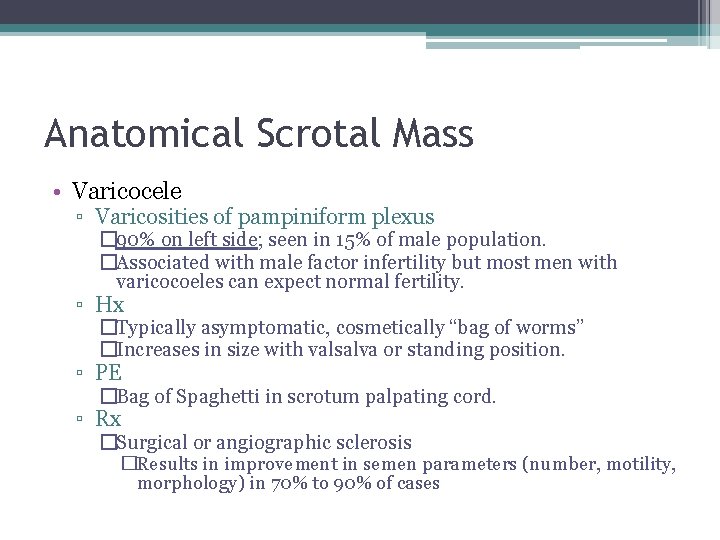
Anatomical Scrotal Mass • Varicocele ▫ Varicosities of pampiniform plexus � 90% on left side; seen in 15% of male population. �Associated with male factor infertility but most men with varicocoeles can expect normal fertility. ▫ Hx �Typically asymptomatic, cosmetically “bag of worms” �Increases in size with valsalva or standing position. ▫ PE �Bag of Spaghetti in scrotum palpating cord. ▫ Rx �Surgical or angiographic sclerosis �Results in improvement in semen parameters (number, motility, morphology) in 70% to 90% of cases
Torsion – it hurts!
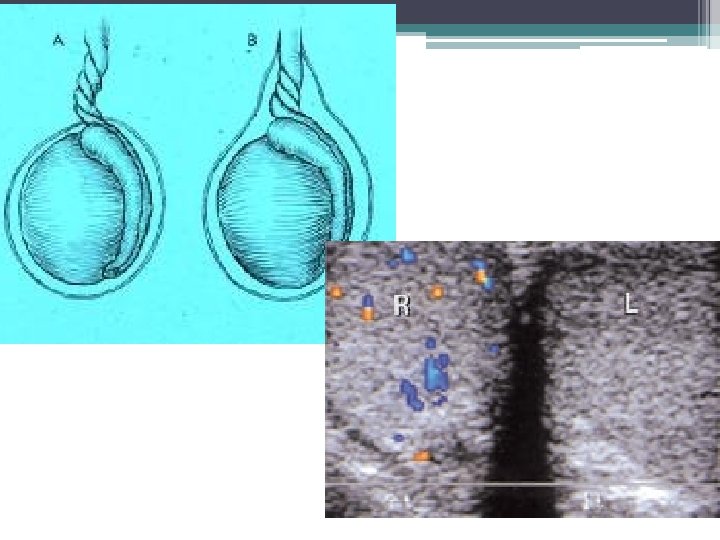
Anatomical – Acute Scrotum • Testicular torsion ▫ Surgical Emergency!! ▫ Only definitive Diagnosis is Surgical Scrotal Exploration. ▫ Typically in 12 -18 yr olds ▫ 6 hr window prior to irreversible testicular ischemia ▫ Associated with ‘Bell Clapper Deformity” ▫ Detort – “like opening a book”
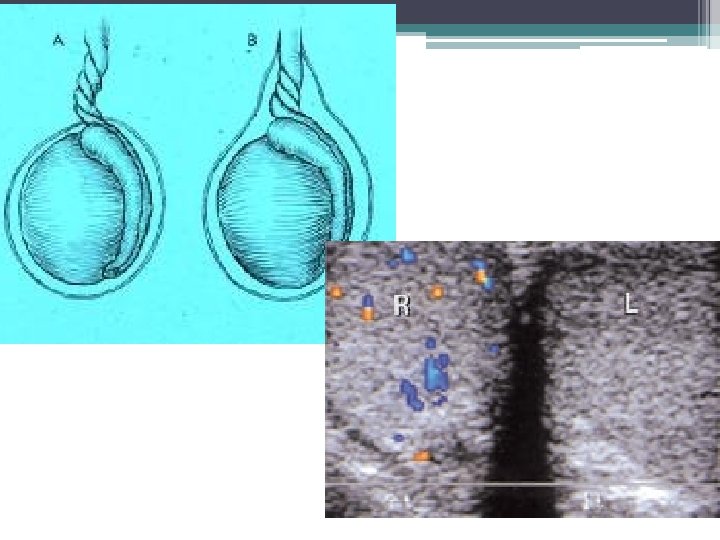
Testicular Torsion
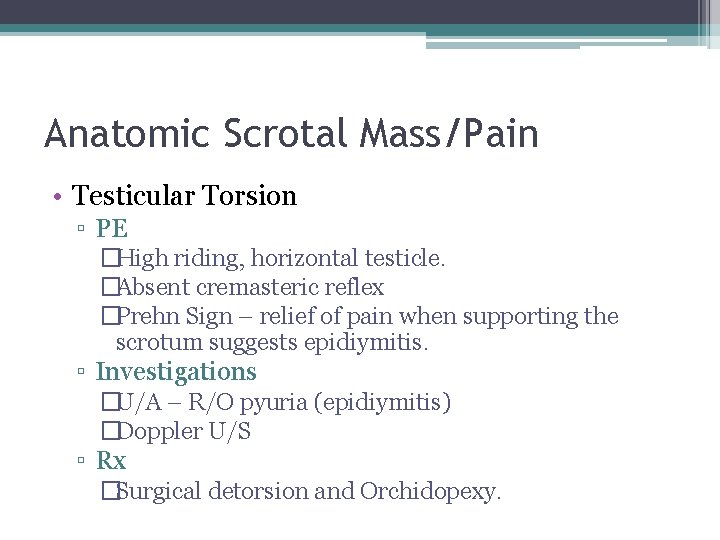
Anatomic Scrotal Mass/Pain • Testicular Torsion ▫ PE �High riding, horizontal testicle. �Absent cremasteric reflex �Prehn Sign – relief of pain when supporting the scrotum suggests epidiymitis. ▫ Investigations �U/A – R/O pyuria (epidiymitis) �Doppler U/S ▫ Rx �Surgical detorsion and Orchidopexy.
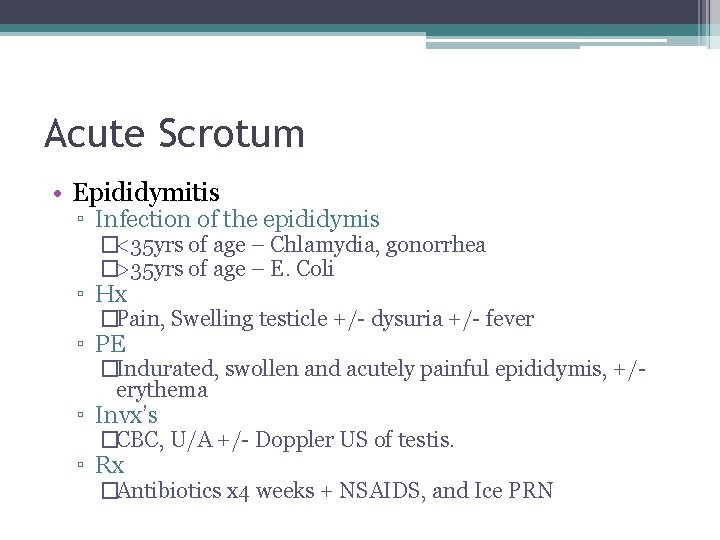
Acute Scrotum • Epididymitis ▫ Infection of the epididymis �<35 yrs of age – Chlamydia, gonorrhea �>35 yrs of age – E. Coli ▫ Hx �Pain, Swelling testicle +/- dysuria +/- fever ▫ PE �Indurated, swollen and acutely painful epididymis, +/erythema ▫ Invx’s �CBC, U/A +/- Doppler US of testis. ▫ Rx �Antibiotics x 4 weeks + NSAIDS, and Ice PRN
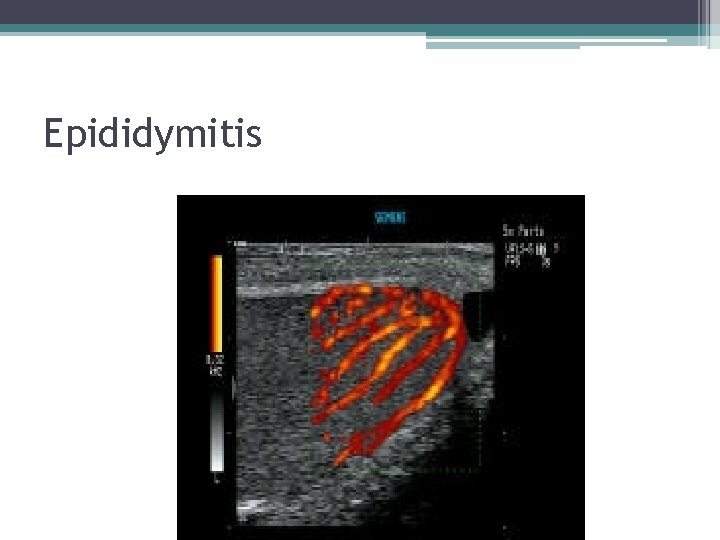
Epididymitis
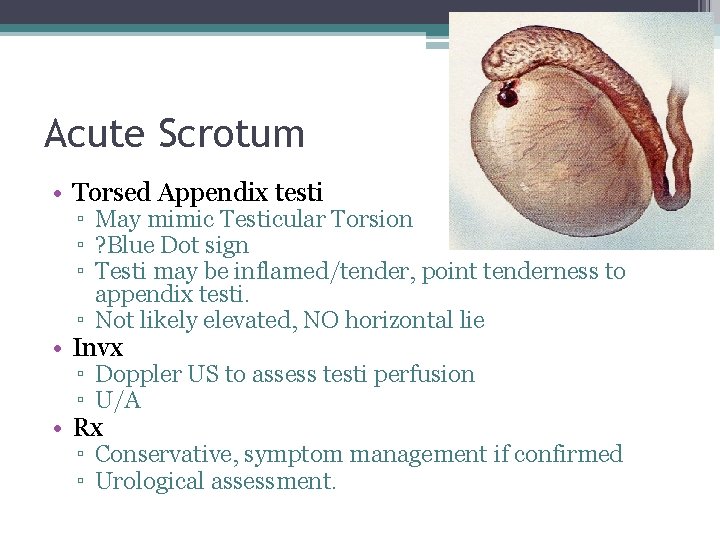
Acute Scrotum • Torsed Appendix testi ▫ May mimic Testicular Torsion ▫ ? Blue Dot sign ▫ Testi may be inflamed/tender, point tenderness to appendix testi. ▫ Not likely elevated, NO horizontal lie • Invx ▫ Doppler US to assess testi perfusion ▫ U/A • Rx ▫ Conservative, symptom management if confirmed ▫ Urological assessment.
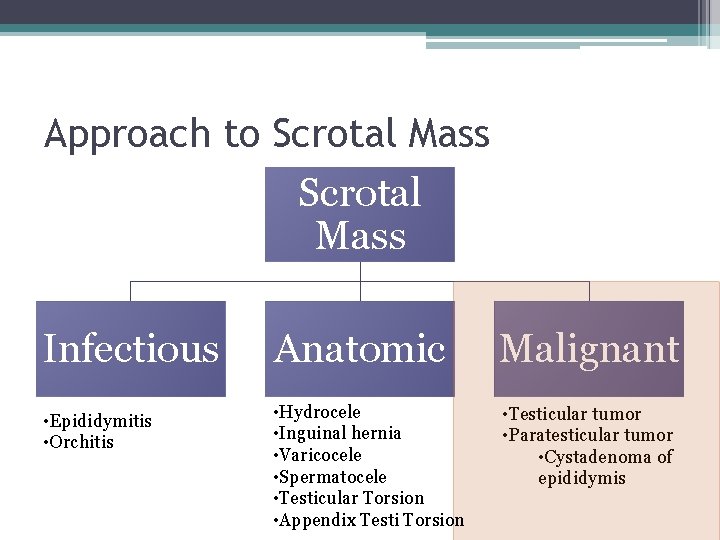
Approach to Scrotal Mass Infectious Anatomic Malignant • Epididymitis • Orchitis • Hydrocele • Inguinal hernia • Varicocele • Spermatocele • Testicular Torsion • Appendix Testi Torsion • Testicular tumor • Paratesticular tumor • Cystadenoma of epididymis
Testicular Cancer • Typically occurs in young healthy Men. • Very good cure rates Even for Metastatic Disease!
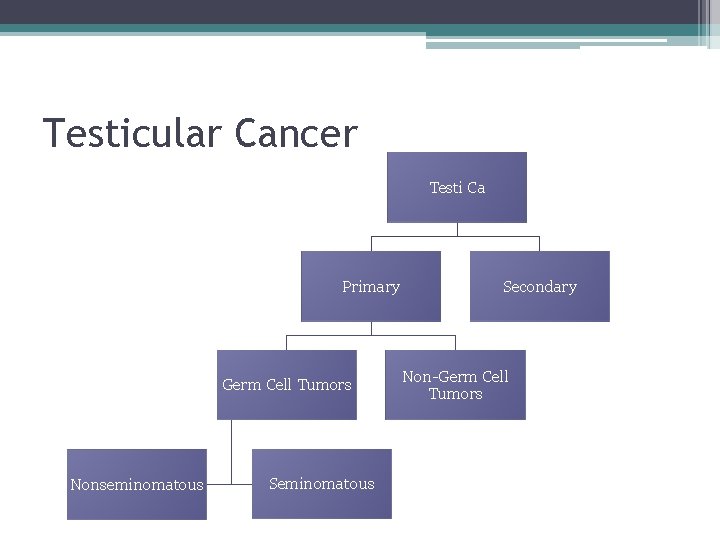
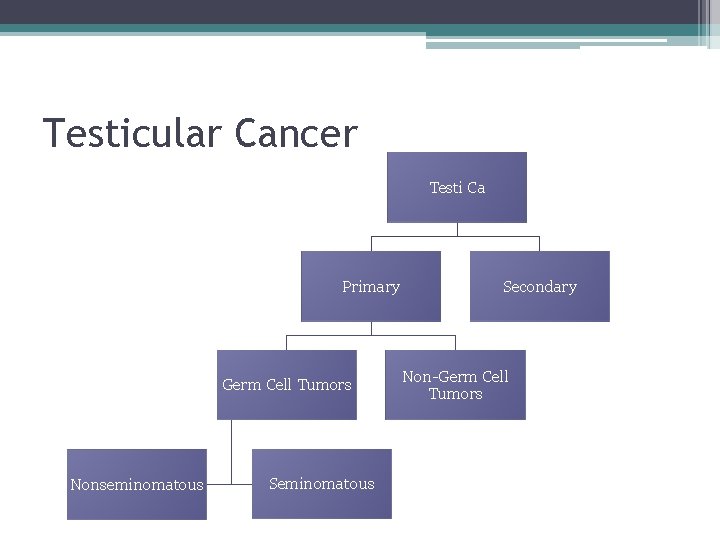
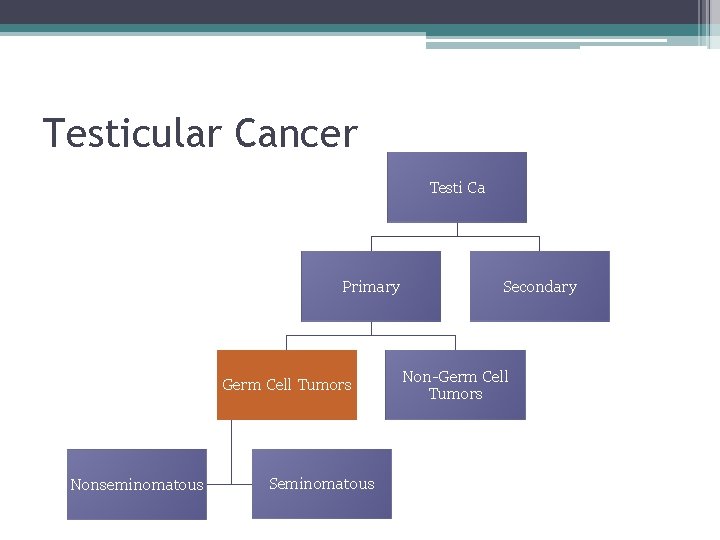
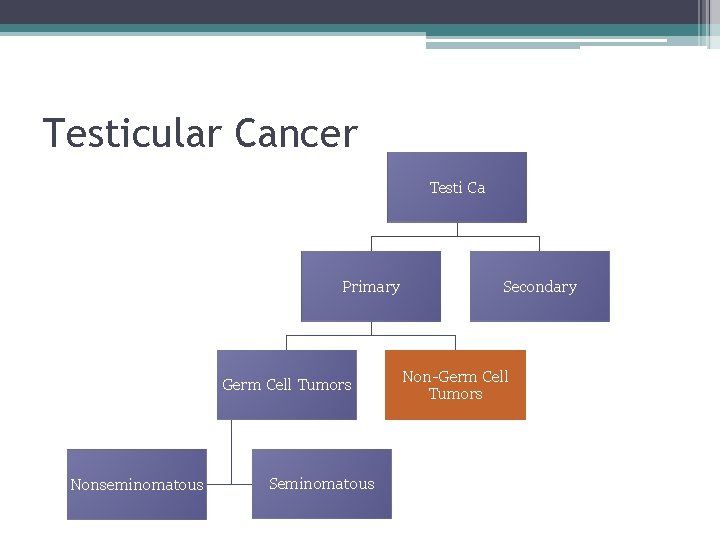
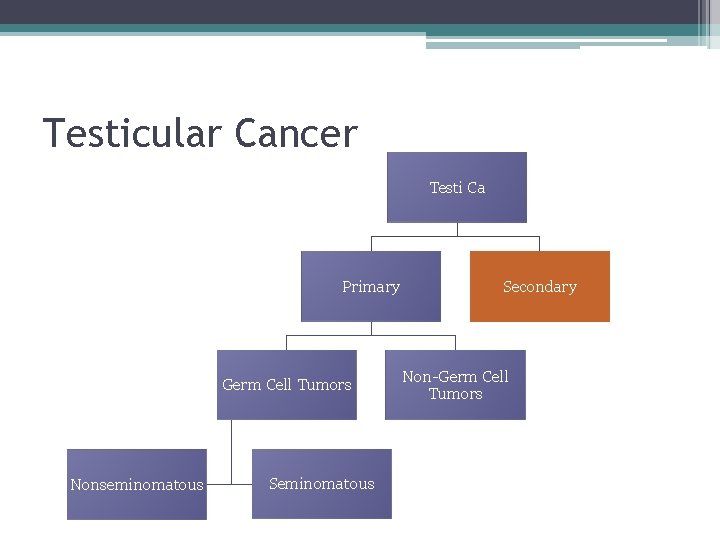
Testicular Cancer Testi Ca Primary Germ Cell Tumors Nonseminomatous Secondary Non-Germ Cell Tumors
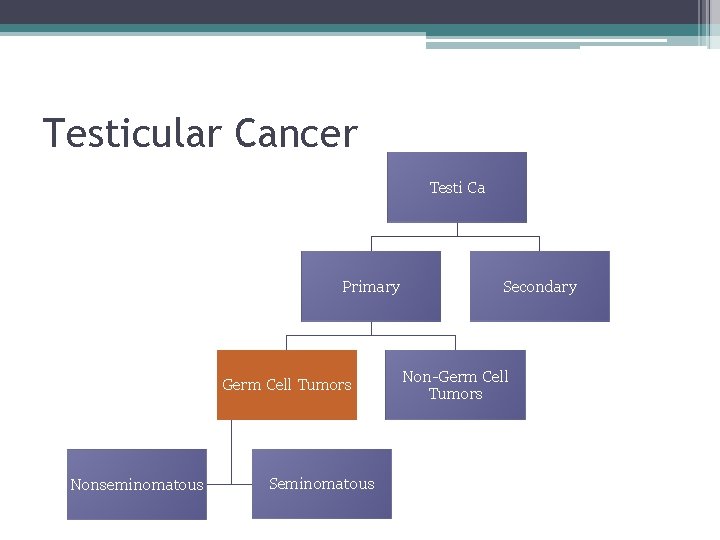
Testicular Cancer Testi Ca Primary Germ Cell Tumors Nonseminomatous Secondary Non-Germ Cell Tumors
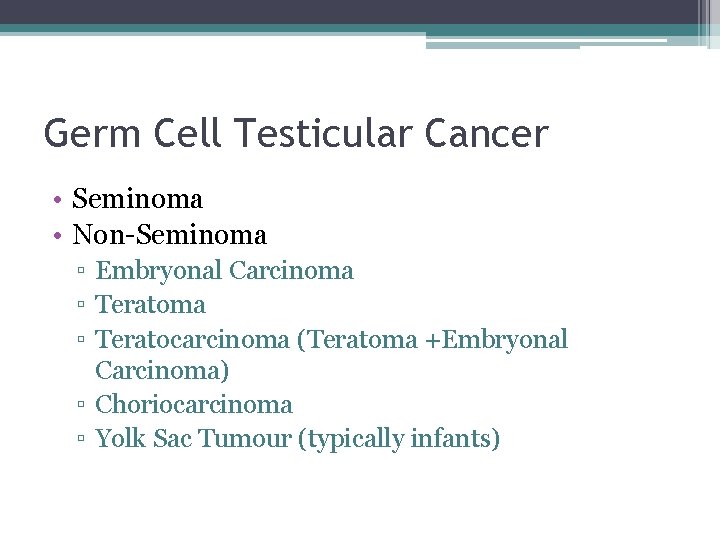
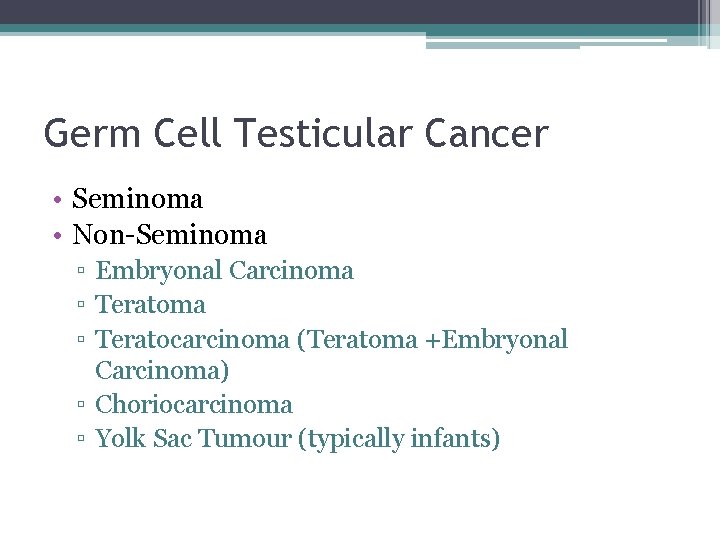
Germ Cell Testicular Cancer • Seminoma • Non-Seminoma ▫ Embryonal Carcinoma ▫ Teratocarcinoma (Teratoma +Embryonal Carcinoma) ▫ Choriocarcinoma ▫ Yolk Sac Tumour (typically infants)
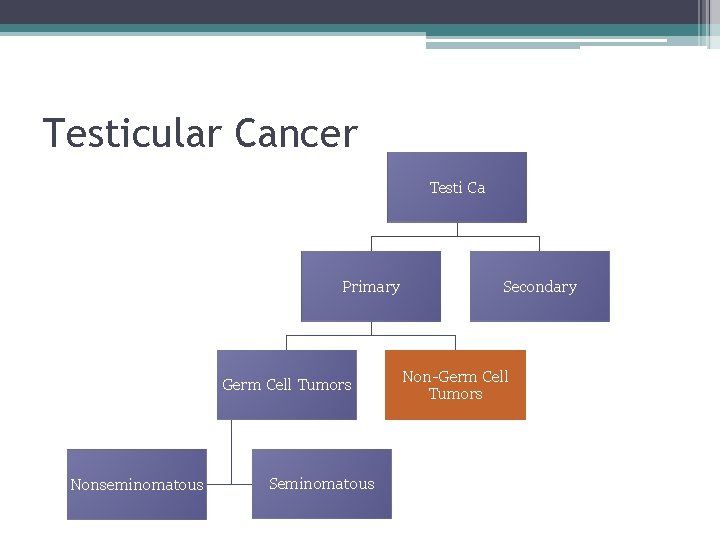
Testicular Cancer Testi Ca Primary Germ Cell Tumors Nonseminomatous Secondary Non-Germ Cell Tumors
Non-Germ Cell Testicular Cancer • Leydig Cell Tumor • Sertoli Cell Tumor
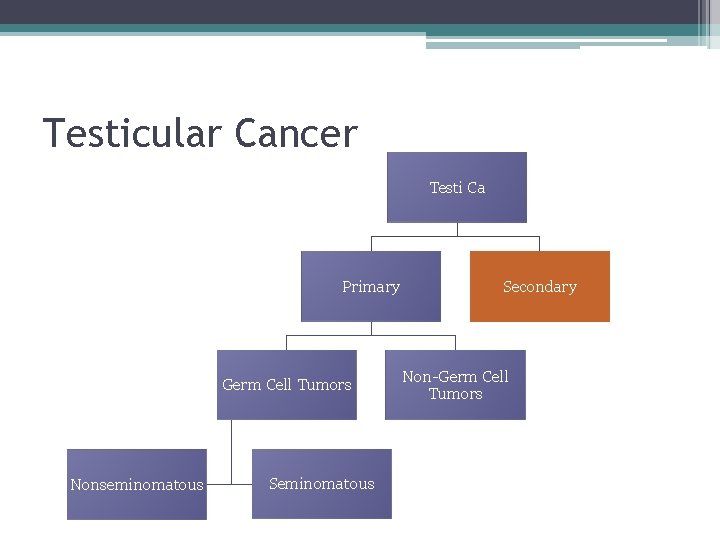
Testicular Cancer Testi Ca Primary Germ Cell Tumors Nonseminomatous Secondary Non-Germ Cell Tumors
Secondary Testicular Cancer • Lymphoma • Leukemia
Testicular Cancer • Presentation ▫ Typically painless intratesticular mass discovered on self examination ▫ Age 15 -35 �Albeit some tumor subytpes cluster in infancy and 60’s
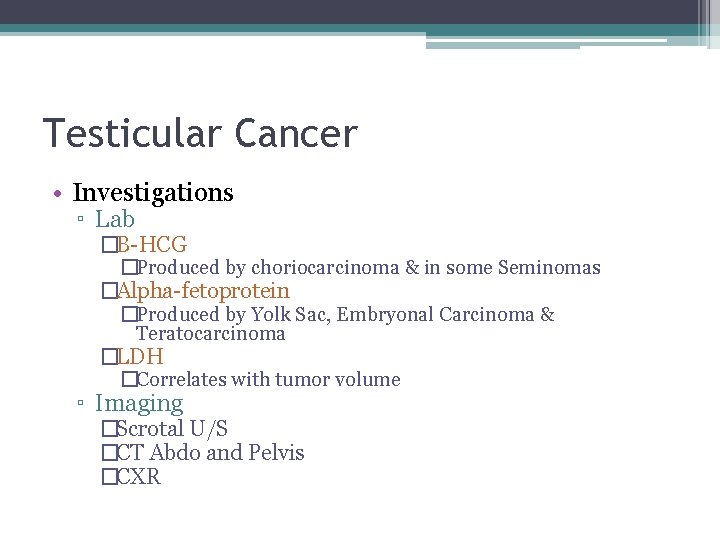
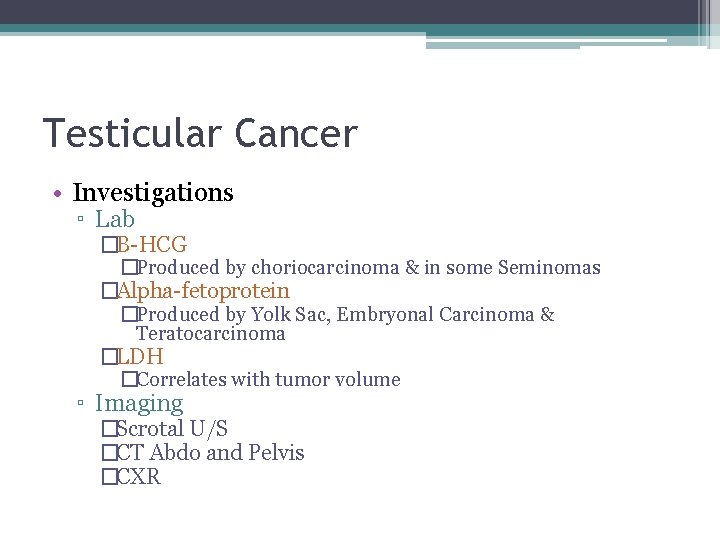
Testicular Cancer • Investigations ▫ Lab �B-HCG �Produced by choriocarcinoma & in some Seminomas �Alpha-fetoprotein �Produced by Yolk Sac, Embryonal Carcinoma & Teratocarcinoma �LDH �Correlates with tumor volume ▫ Imaging �Scrotal U/S �CT Abdo and Pelvis �CXR
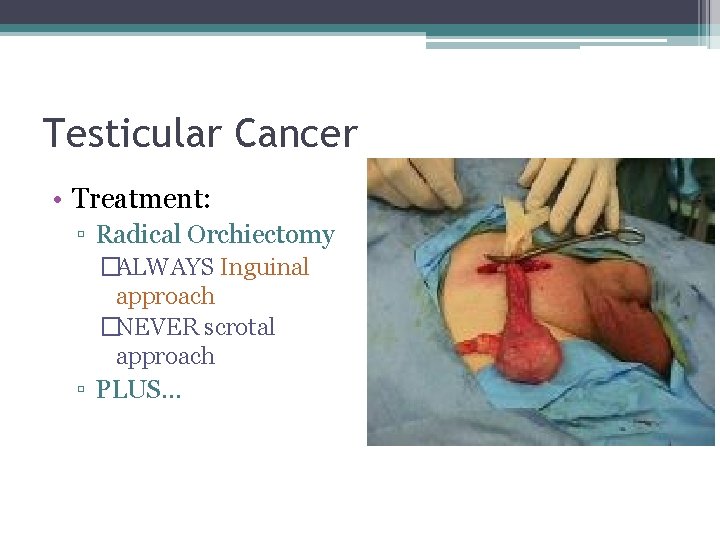
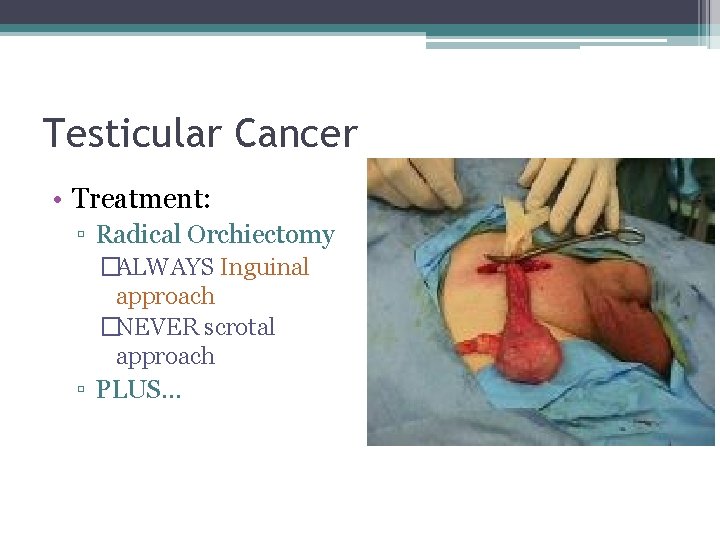
Testicular Cancer • Treatment: ▫ Radical Orchiectomy �ALWAYS Inguinal approach �NEVER scrotal approach ▫ PLUS…
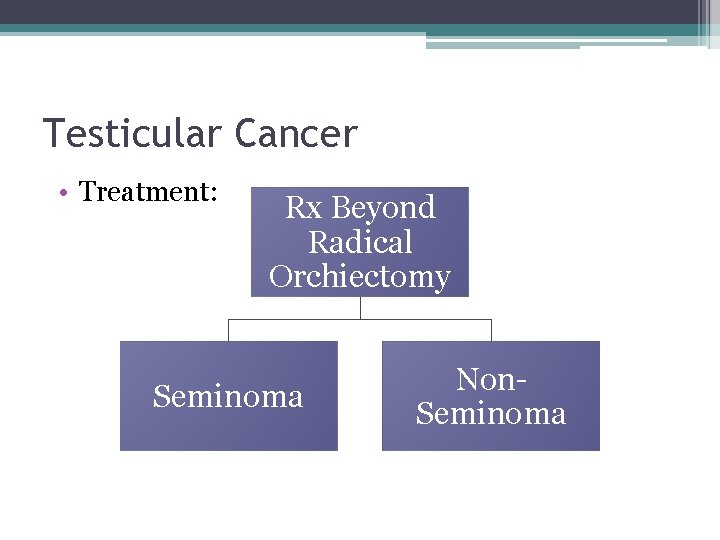
Testicular Cancer • Treatment: Rx Beyond Radical Orchiectomy Seminoma Non. Seminoma
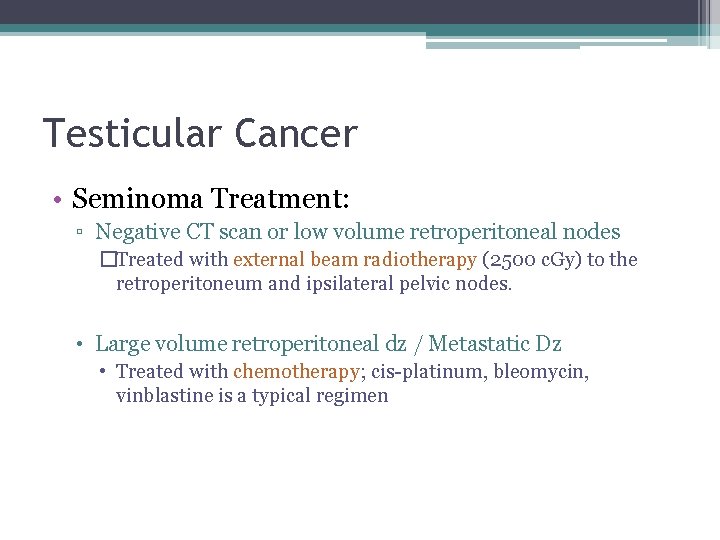
Testicular Cancer • Seminoma Treatment: ▫ Negative CT scan or low volume retroperitoneal nodes �Treated with external beam radiotherapy (2500 c. Gy) to the retroperitoneum and ipsilateral pelvic nodes. • Large volume retroperitoneal dz / Metastatic Dz • Treated with chemotherapy; cis-platinum, bleomycin, vinblastine is a typical regimen
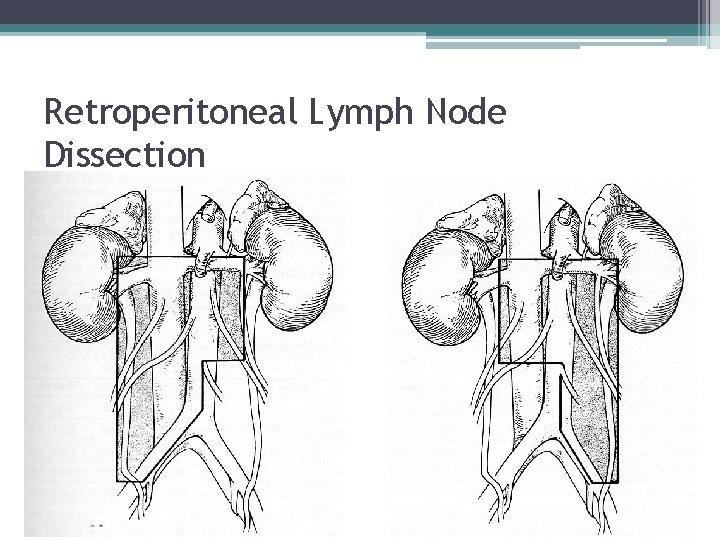
Testicular Cancer • Non-Seminoma Treatment: ▫ Negative CT scan & N tumour markers post orchiectomy �Surveillance. �OR, Retroperitoneal lymph node dissection may be done to determine the actual stage and potentially cure patients with low volume nodal mets. ▫ Large volume retroperitoneal disease or mets �Chemotherapy �cisplatinum, VP-16, bleomycin. �Residual teratoma may be seen after successful chemotherapy and should be excised (RPLND).
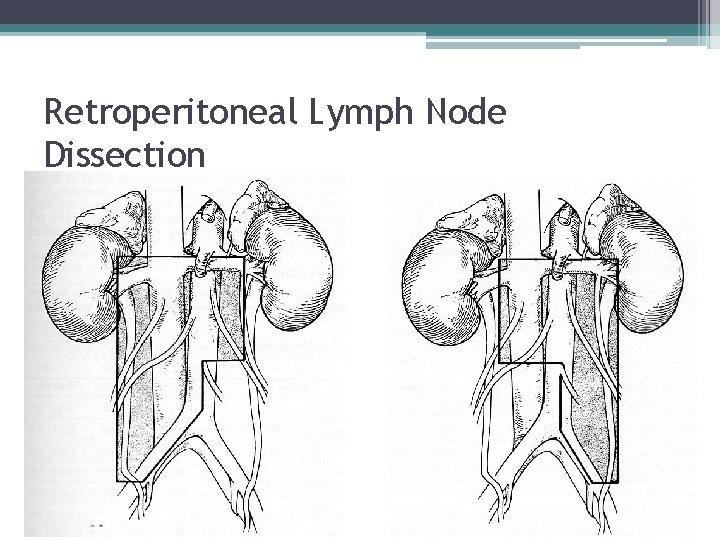
Retroperitoneal Lymph Node Dissection
 Tongue rough edges
Tongue rough edges Trasodone
Trasodone Ddx of cough
Ddx of cough What is it
What is it Ddx of hemoptysis
Ddx of hemoptysis Dislocation of patella
Dislocation of patella Differentials for hydrocephalus
Differentials for hydrocephalus Shock ddx
Shock ddx Hematuria
Hematuria Hematuria ex vacuo
Hematuria ex vacuo Macroscopic hematuria causes
Macroscopic hematuria causes Hematuria
Hematuria Dr donald lamm
Dr donald lamm Dr shezad tejani
Dr shezad tejani Anuria disuria poliuria oliguria hematuria
Anuria disuria poliuria oliguria hematuria Hematuria causes
Hematuria causes Eritrocitos isomorficos
Eritrocitos isomorficos Hemoglucosa
Hemoglucosa Hemoglobinuria vs hematuria
Hemoglobinuria vs hematuria Children urology
Children urology Ubc urology
Ubc urology Refhelp
Refhelp Urology match
Urology match Grading of varicocele
Grading of varicocele Srmc urology
Srmc urology Pediatric urology salary
Pediatric urology salary Urology match
Urology match Usc
Usc Dr donaldson urology
Dr donaldson urology Rpug in urology
Rpug in urology Vaginal agensis
Vaginal agensis Urology coding cheat sheet
Urology coding cheat sheet Urology near oakley
Urology near oakley Citation sandwich example
Citation sandwich example Design elements hair
Design elements hair Which type of lines are used in the one-length hairstyle
Which type of lines are used in the one-length hairstyle The rolling stones origin
The rolling stones origin Gilgal meaning
Gilgal meaning The lottery sacrifice
The lottery sacrifice Magnesium ammonium phosphate stones
Magnesium ammonium phosphate stones Cart before the horse
Cart before the horse Stepping stones to glory cartoon analysis
Stepping stones to glory cartoon analysis Stepping stones triple p
Stepping stones triple p Hypercalauria
Hypercalauria Lamp with ibex design
Lamp with ibex design Collective nouns for stamps
Collective nouns for stamps Nursery rhyme sticks and stones
Nursery rhyme sticks and stones Sufi proverb in the desert there is no sign
Sufi proverb in the desert there is no sign Pleased to meet you rolling stones
Pleased to meet you rolling stones Sum in sigma notation
Sum in sigma notation Stepping stones to glory cartoon analysis
Stepping stones to glory cartoon analysis Parable of stones by gemino h. abad
Parable of stones by gemino h. abad Weihnachtskugel rolling stones
Weihnachtskugel rolling stones Stones bones and petroglyphs
Stones bones and petroglyphs Odowa stones
Odowa stones Perinephric abscess symptoms
Perinephric abscess symptoms Sticks and stones origin
Sticks and stones origin Magnesium ammonium phosphate stones
Magnesium ammonium phosphate stones Chris drury medicine wheel
Chris drury medicine wheel Emily wants to buy turquoise stones
Emily wants to buy turquoise stones Large monuments created by huge stones
Large monuments created by huge stones What does kidney stones look like
What does kidney stones look like Stepping stones portsmouth ohio
Stepping stones portsmouth ohio Built of living stones
Built of living stones Whats the difference between rocks and minerals
Whats the difference between rocks and minerals The rolling stones history
The rolling stones history Chronic hyperplastic pulpitis
Chronic hyperplastic pulpitis Calcium phosphate calculi
Calcium phosphate calculi Where did general lee surrender to general grant?
Where did general lee surrender to general grant? Diferencia entre gran plano general y plano general
Diferencia entre gran plano general y plano general Classification outline example
Classification outline example Linear recursion example
Linear recursion example Toulmin model example paragraph
Toulmin model example paragraph Prewriting outline
Prewriting outline Technical paper outline
Technical paper outline Anar outline
Anar outline Impression about work immersion
Impression about work immersion Outline 213
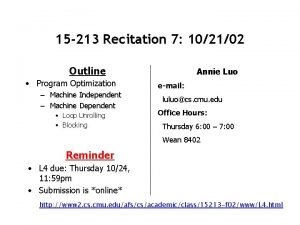
Outline 213 Imaginary feelings i am poem
Imaginary feelings i am poem Mandt system crisis cycle
Mandt system crisis cycle Lecture outline example
Lecture outline example Lesson outline physical properties lesson 2
Lesson outline physical properties lesson 2 Lesson outline classifying organisms
Lesson outline classifying organisms Knowledge based agent
Knowledge based agent Land biomes lesson outline answers
Land biomes lesson outline answers Outline form.
Outline form. Cookie monster real name
Cookie monster real name American literature course outline
American literature course outline Outline spectra
Outline spectra Outline laporan penelitian
Outline laporan penelitian Making a difference outline
Making a difference outline An outline of british history
An outline of british history Research paper outline example
Research paper outline example Ivan pavlov classical conditioning
Ivan pavlov classical conditioning Army aar questions
Army aar questions Allah outline
Allah outline Smurf outline
Smurf outline Outline concept
Outline concept Legal research outline
Legal research outline Outline eksempel
Outline eksempel English essay outline
English essay outline Tools of development control
Tools of development control Chapter 38 a world without borders outline
Chapter 38 a world without borders outline Outline of leviticus
Outline of leviticus Jeffy outline
Jeffy outline Spine outline
Spine outline Csc problem solving
Csc problem solving Knowledge management course outline
Knowledge management course outline Mock interview workshop outline
Mock interview workshop outline Smurf outline
Smurf outline Language font style
Language font style What are protists lesson outline
What are protists lesson outline