Kidney Stones in Children T Matthew Eison MD












- Slides: 64
Kidney Stones in Children T. Matthew Eison, MD LBCMC Pediatric Nephrology Fellow
Nephrolithiasis in Children • -relatively uncommon in the pediatric population • -significant long-term complications include possible progression of renal dysfunction • -may herald systemic metabolic disorder or underlying anatomical anomalies.
Pathophysiology of stone formation • The formation of renal calculi is a complex process; depends on the interaction of several factors: -Urinary concentration of stone forming ions -Urinary p. H -Urinary flow rate -The balance between promoter and inhibitory factors of crystallisation, (e. g. , citrate, magnesium, pyrophosphate) -Anatomic factors that encourage urinary stasis (e. g. , developmental anomalies, foreign bodies) Hulton SA. Evaluation of urinary tract calculi in children. Arch Dis Child 84: 320– 323, 2001
Mechanisms of Stone formation • -Steps required: • A) Crystallization • B) Crystal Growth • C) Aggregation (multiple crystals combining together; believed to take place in the tubules or collecting system) • D) Adherence of Crystals to Epithelium (must anchor in order not to be washed out of the urine long enough to aggregate)

Mechanisms of Stone formation (cont’d) -Supersaturation above saturation point of stone "promoters" (calcium, oxalate, uric acid) occurs in complex solution of urine due to other ions and molecules: • -"Inhibitors" of stone formation: citrate, pyrophosphate, magnesium, and glycosaminoglycans; (Tamm-Horsfall protein, uropontin, nephrocalcin, FKBP-12, bikunin, and lithostathine also described in literature) • -The point at which urine will no longer hold a substance in solution: "formation product" (influenced by urinary p. H): "nucleation" occurs to form new crystals • -Crystals may be A) homogeneous (similar ions join to form crystals) or B) heterogeneous (one crystal grows around another crystal, e. g. calcium oxalate crystallizing around a nidus: uric acid or cystine crystal, sloughed epithelial cell or other material provides nidus) • -Supersaturation affected by water intake and urine flow rate (true for all types of stones) • -Process of stone formation enhanced by anatomic abnormalities that impede urine flow •
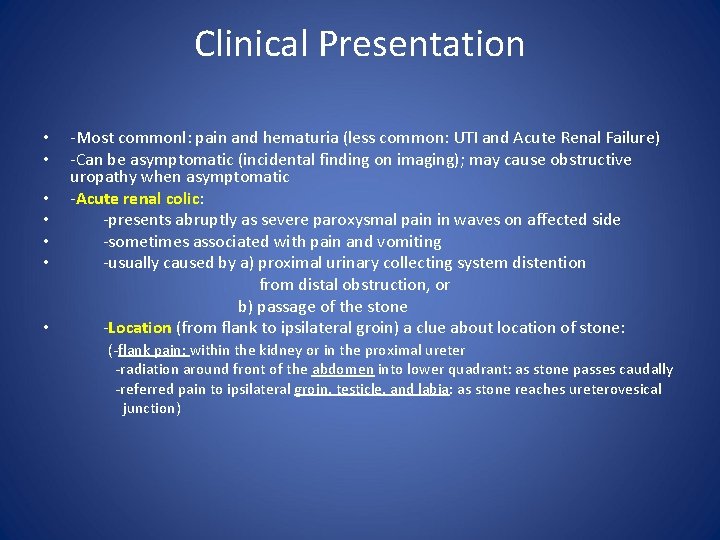
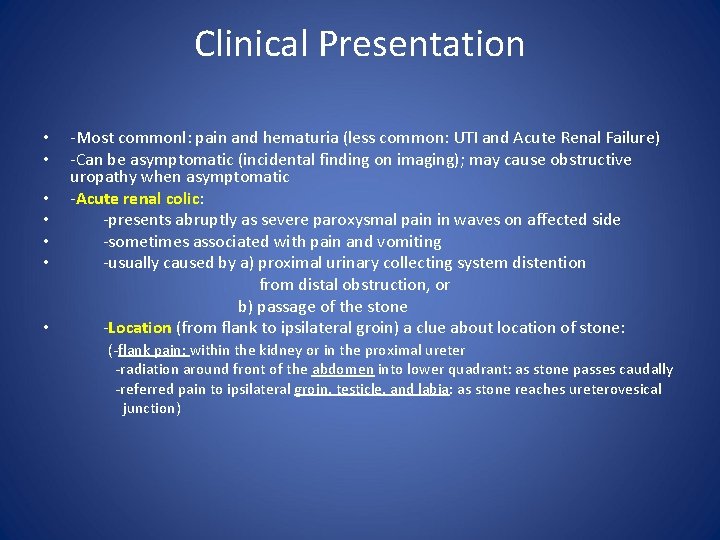
Clinical Presentation -Most commonl: pain and hematuria (less common: UTI and Acute Renal Failure) -Can be asymptomatic (incidental finding on imaging); may cause obstructive uropathy when asymptomatic • -Acute renal colic: • -presents abruptly as severe paroxysmal pain in waves on affected side • -sometimes associated with pain and vomiting • -usually caused by a) proximal urinary collecting system distention from distal obstruction, or b) passage of the stone • -Location (from flank to ipsilateral groin) a clue about location of stone: (-flank pain: within the kidney or in the proximal ureter • • -radiation around front of the abdomen into lower quadrant: as stone passes caudally -referred pain to ipsilateral groin, testicle, and labia: as stone reaches ureterovesical junction)
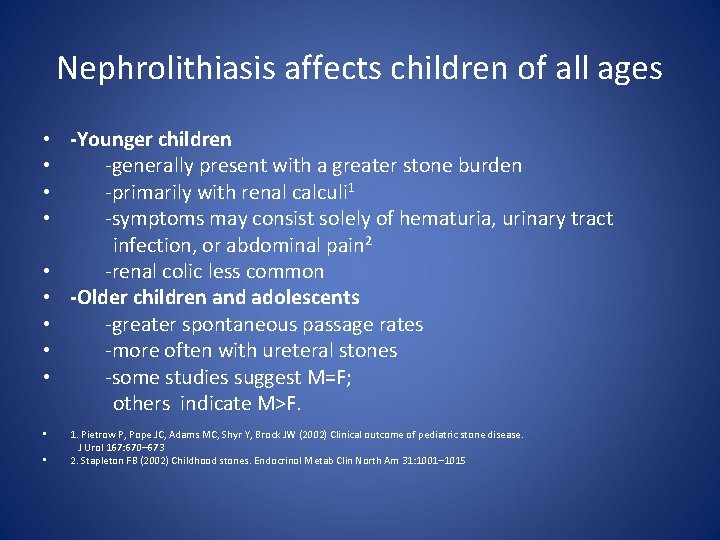
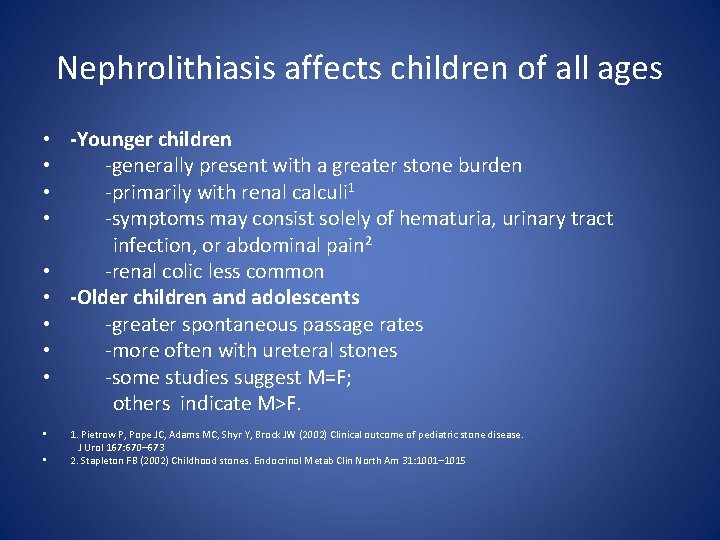
Nephrolithiasis affects children of all ages • -Younger children • -generally present with a greater stone burden • -primarily with renal calculi 1 • -symptoms may consist solely of hematuria, urinary tract infection, or abdominal pain 2 • -renal colic less common • -Older children and adolescents • -greater spontaneous passage rates • -more often with ureteral stones • -some studies suggest M=F; others indicate M>F. • 1. Pietrow P, Pope JC, Adams MC, Shyr Y, Brock JW (2002) Clinical outcome of pediatric stone disease. J Urol 167: 670– 673 • 2. Stapleton FB (2002) Childhood stones. Endocrinol Metab Clin North Am 31: 1001– 1015
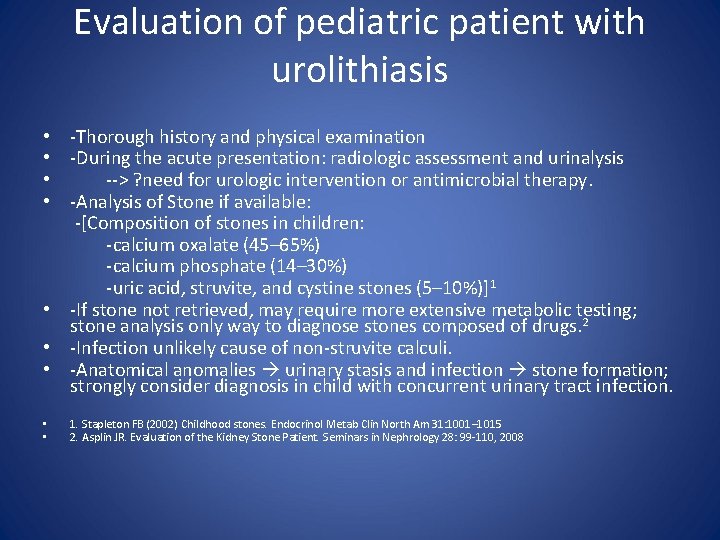
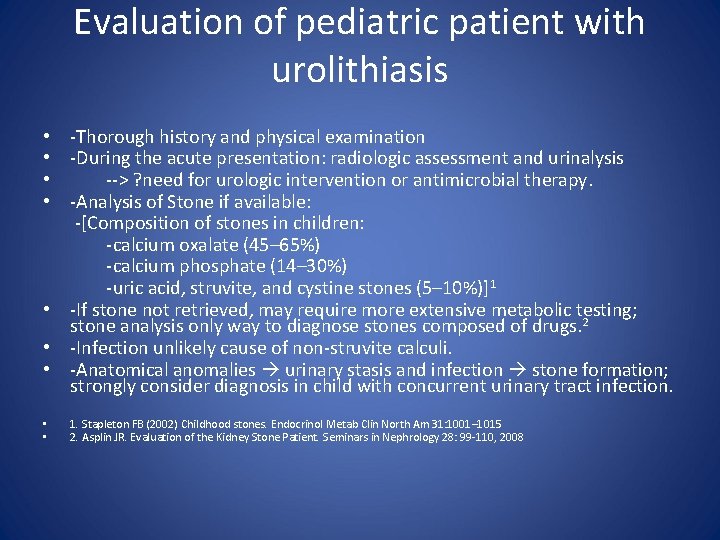
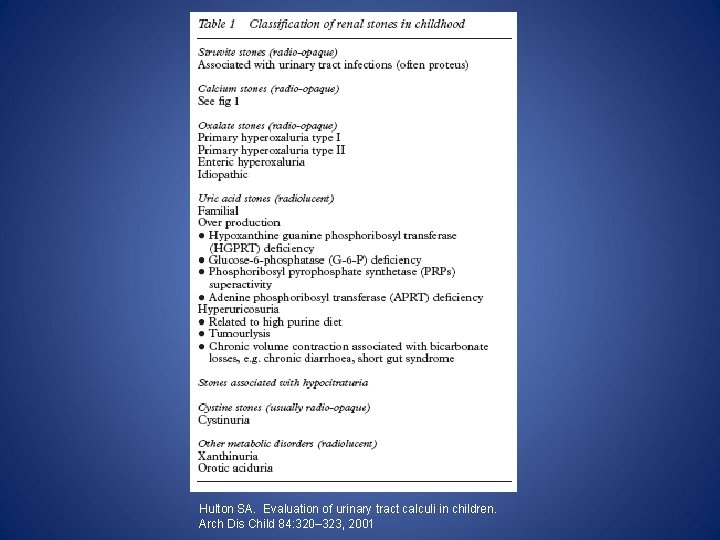
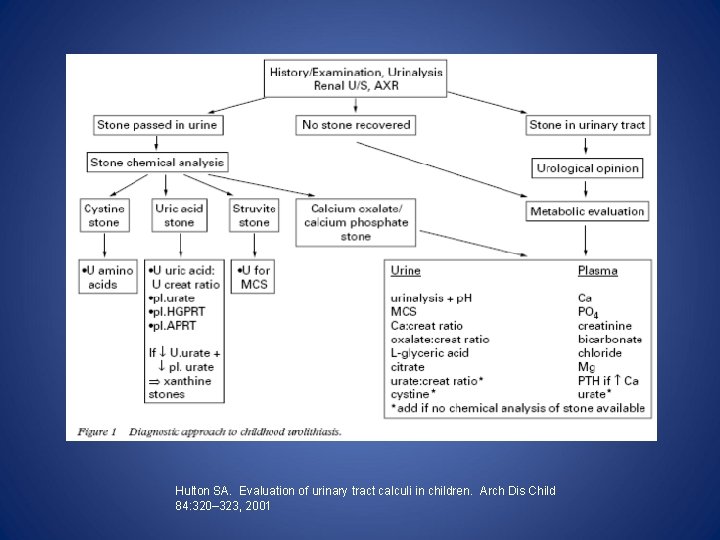
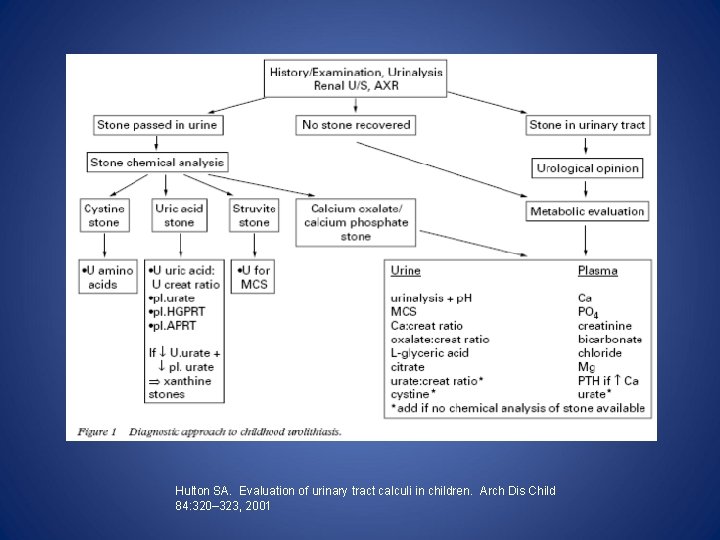
Evaluation of pediatric patient with urolithiasis • -Thorough history and physical examination • -During the acute presentation: radiologic assessment and urinalysis • --> ? need for urologic intervention or antimicrobial therapy. • -Analysis of Stone if available: -[Composition of stones in children: -calcium oxalate (45– 65%) -calcium phosphate (14– 30%) -uric acid, struvite, and cystine stones (5– 10%)]1 • -If stone not retrieved, may require more extensive metabolic testing; stone analysis only way to diagnose stones composed of drugs. 2 • -Infection unlikely cause of non-struvite calculi. • -Anatomical anomalies urinary stasis and infection stone formation; strongly consider diagnosis in child with concurrent urinary tract infection. • • 1. Stapleton FB (2002) Childhood stones. Endocrinol Metab Clin North Am 31: 1001– 1015 2. Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
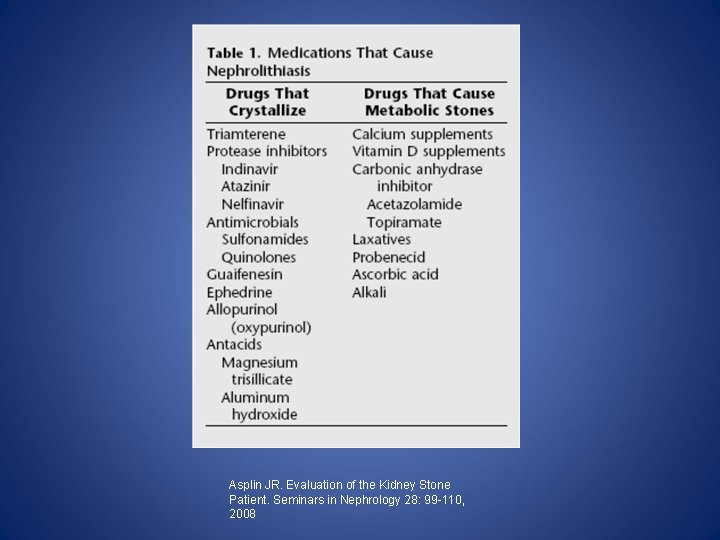
Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
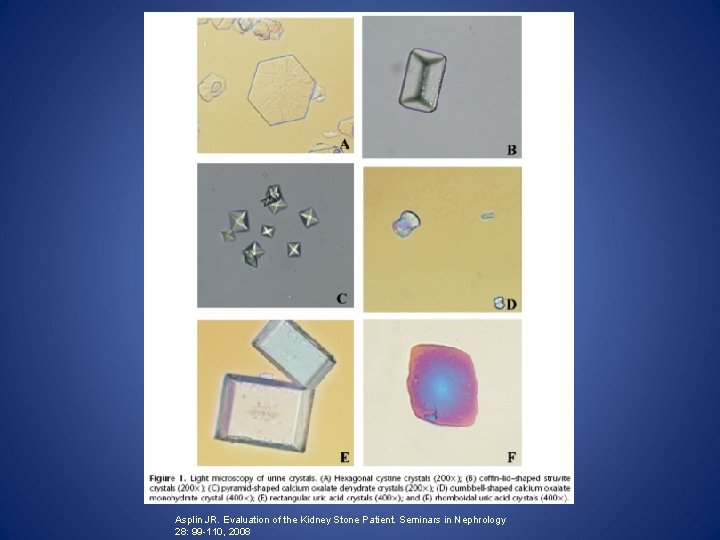
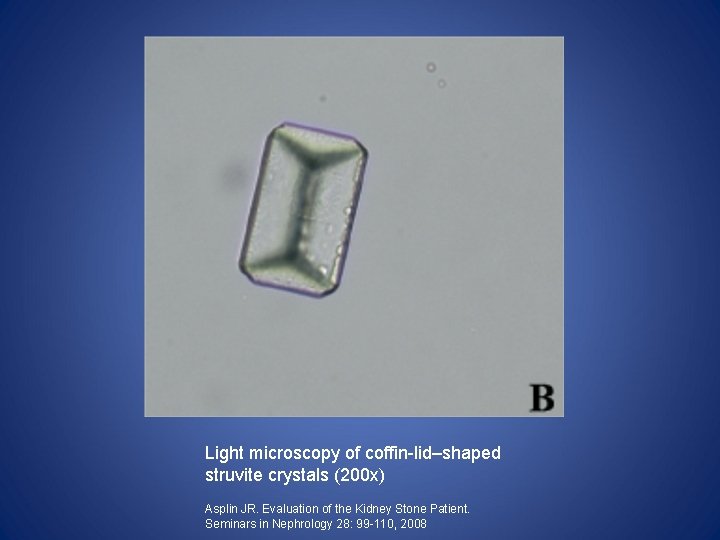
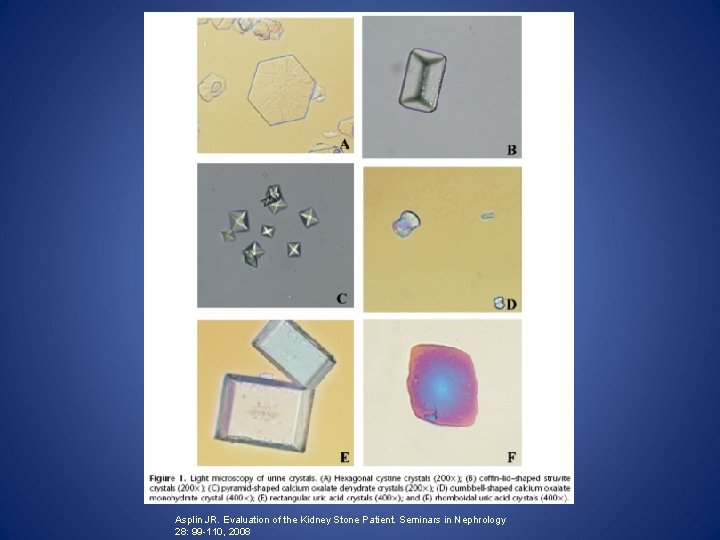
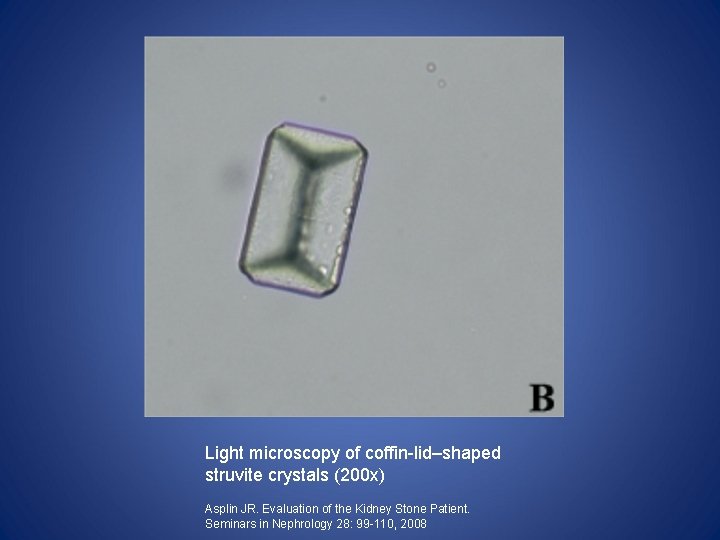
Evaluation (cont'd): Urinalysis • -Calcium crystals more numerous and larger in stone formers than in normal subjects; (however, Ca. Ox and calcium phosphate crystals by themselves have no diagnostic significance) • -Uric acid crystals also seen in both normal subjects & stone formers; usually form in acidic urine. • -However, cystine or struvite crystals always abnormal ; provides a diagnosis even in the absence of a stone analysis.
Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
Evaluation (cont’d): History taking • • • • -should focus on risk factors for and complications of stone formation (e. g. UTI, voiding dysfunction, surgical procedures on urinary tract) -positive family history for stone disease can be obtained in 75% of children with urolithiasis in USA* -Medical conditions associated with urolithiasis in children: -malabsorption -Cystic fibrosis -myelodysplasia -immobilization -Recurrent skeletal fractures may indicate presence of hyperparathyroidism or other bone diseases -Additional important history questions: prematurity (especially with the use of furosemide), use of supplemental Vitatmin D, enteral or parenteral nutrition formulas high in calcium and/or phosphorus *Stapleton FB. Idiopathic hypercalciuria: association with isolated hematuria and risk for urolithiasis in children. The Southwest Pediatric Nephrology Study Group. Kidney Int 37: 807, 1990.

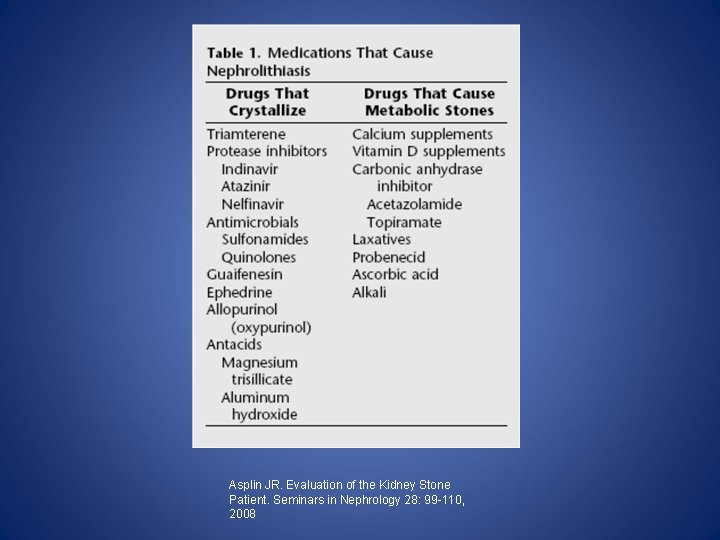
Evaluation: History taking (cont’d) • -Medications such as steroids, chemotherapy drugs, anticonvulsants, loop diuretics, acetazolamide, other carbonic anhydrase inhibitors, uricosuric drugs, and antacids • -Ketogenic diets used to treat intractable seizures in children associated with uric acid stones 1 • -Excess salt and insufficient potassium intake may contribute to stone formation 2 • -Urogenital tract abnormalities predispose to the formation of infected stones (children on clean intermittent catheterization with a Mitrofanoff conduit, exstrophy-epispadias complex, and bladder augmentation frequently develop urolithiasis)3 -5 • • • 1. Kielb S, Koo HP, Bloom DA, Faerber GJ. Nephrolithiasis associated with the ketogenic diet. J Urol 164: 464, 2000. 2. Osorio AV, Alon US. The relationship between urinary calcium, sodium, and potassium excretion and the role of potassium in treating idiopathic hypercalciuria. Pediatrics 100: 675, 1997. 3. Barroso U, Jednak R, Felming P et al. Bladder caculi in children who perform clean intermittent catheterization. BJU Int 85: 879, 2000. 4. Mathoera RB, Kok DJ, Nijman RJ. Bladder calculi in augmentation cystoplasty in children. Urology 56: 482, 2000. 5. Miller LA, Stapleton, FB. Urinary volume in children with urolithiasis. J Urol 158: 1322, 1997

Evaluation: Physical Exam • -Failure to thrive (Distal Renal Tubular Acidosis) • -Hypertension (Renal Disease) • -Skeletal findings of rickets, soft tissue calcification (hypercalcemia)
Evaluation: Radiological Imaging • -Plain abdominal radiographs detect only radiopaque stones; low sensitivity (62%) and specificity (67%) for diagnosis of urolithiasis 1 • -Plain radiographs and intravenous pyelography replaced in recent years by ultrasonography and CT 2 -4 • -Non-contrast spiral computerized axial tomography (spiral CT) now replacing other imaging techniques during acute episodes • -In patients requiring repeat studies, maximal use of ultrasound to is recommended (minimize exposure to CT-related radiation) • -IVP still important for complex urologic anatomy prior to surgery • • 1. Roth CS, Bowyer BA, Berquist TH. Utility of the plain abdominal radiograph for diagnosisng ureteral calculi. Ann Emerg Med 14: 311, 1985. 2. Monk RD, Bushinsky DA. Nephrolithiasis and nephrocalcinosis. In: Johnson RJ, Reehally J, eds. Comprehensive Clinical Nephrology, 2 nd edn. New York: Mosby; 2003: 731. 3. Fielding JR, Steele G, Fox LA et al. Spiral computerized tomography in the evaluation of acute flank pain: a replacement for excretory urography. J Urol 157: 2071, 1997. 4. Sinclair D, Wilson S, Toi A, Greenspan L. The evaluation of suspected renal colic: ultrasound scan versus excretory urography. Ann Emerg Med 18: 556, 1989.

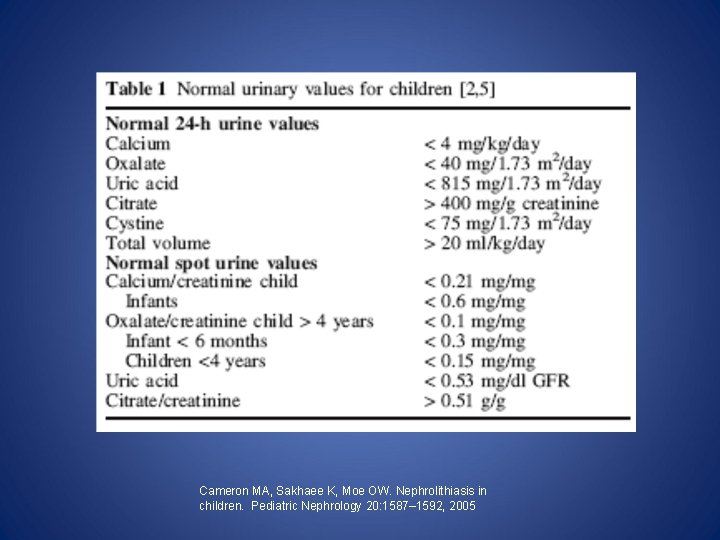
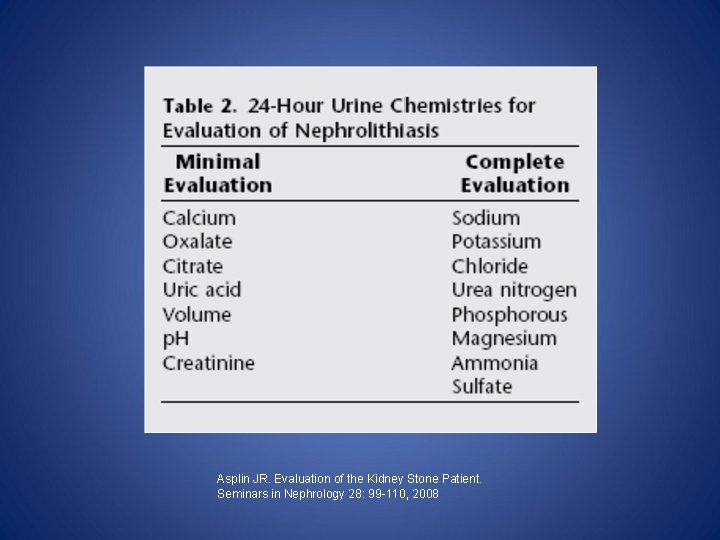
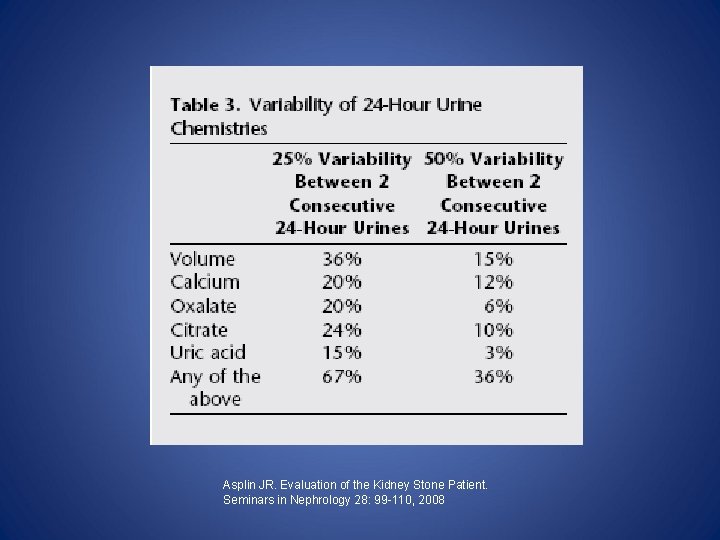
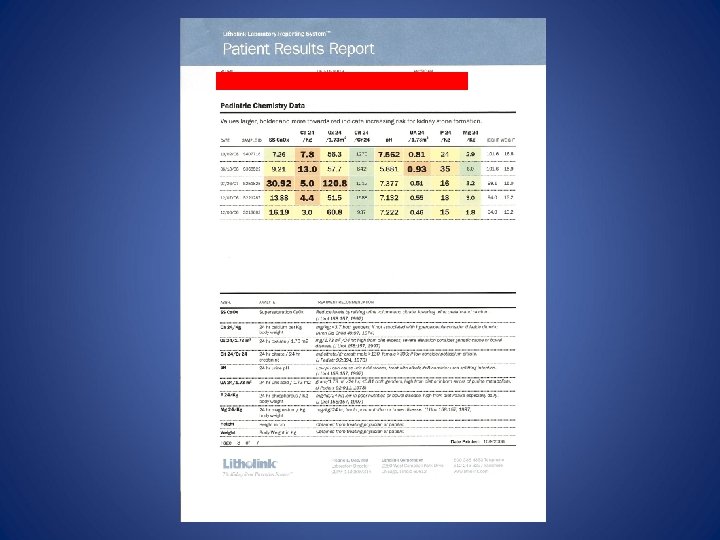
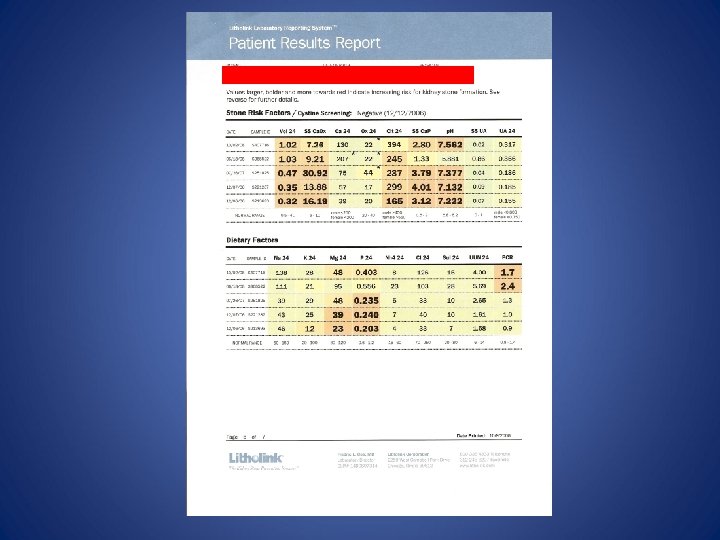
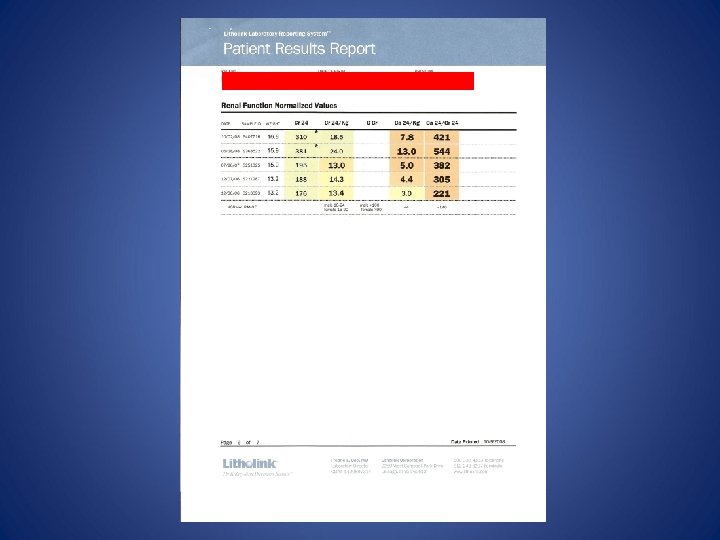
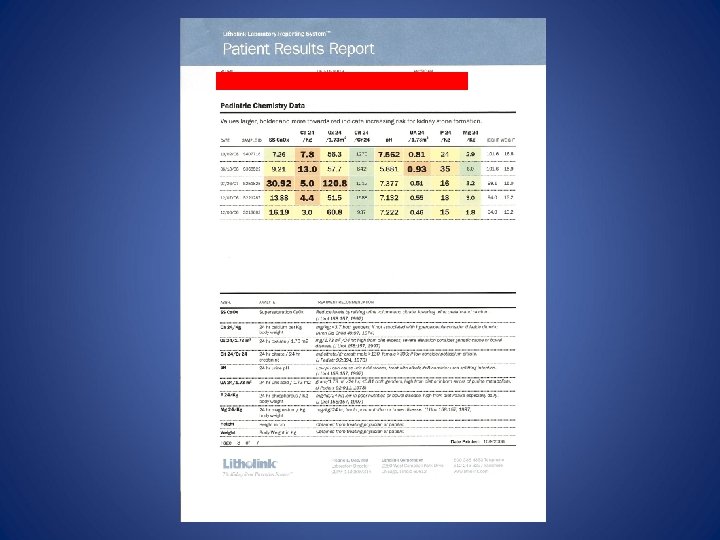
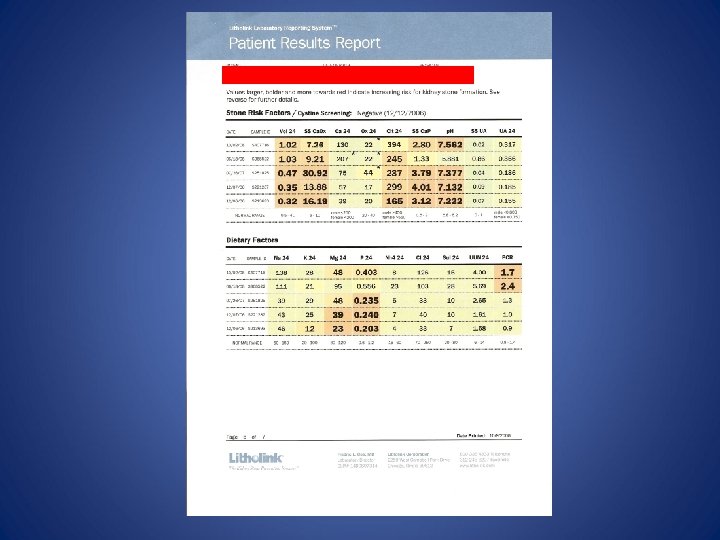
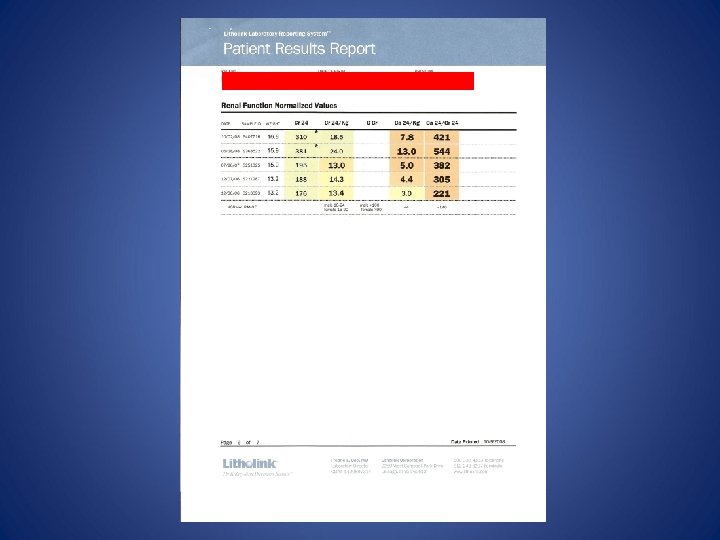
Evaluation: Metabolic Assessment • -All metabolic evaluation should be postponed until acute event resolves & antimicrobial treatment complete. • - >40% of affected children have identifiable metabolic predisposition • -Initial metabolic assessment should consist of: -Repeated urinalysis (to ensure the absence of infection) -Serum for electrolytes, renal function, calcium, phosphorus, magnesium, and uric acid; also consider PTH, Vitamin D levels -24 -hour urine total urinary volume, calcium, sodium, potassium, magnesium, phosphorus, creatinine, p. H, citrate, oxalate, uric acid, cystine and protein (In certain circumstances, measurements of glycerate, hypoxanthine, ornithine, lysine, and arginine may need to be done)
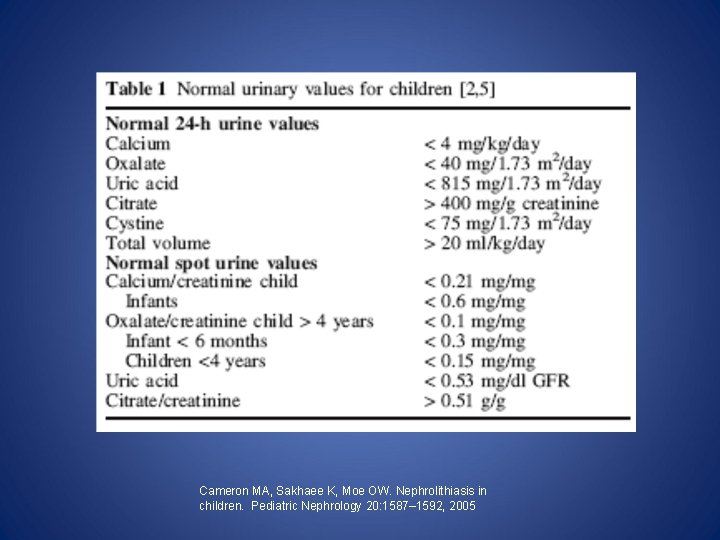
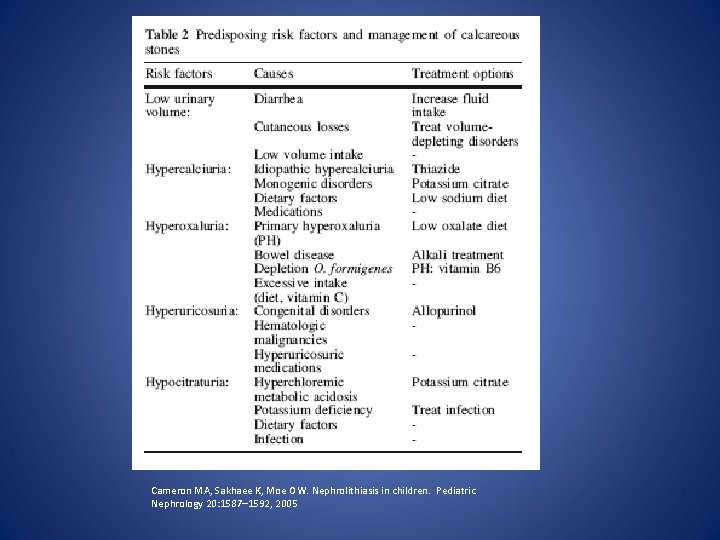
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005
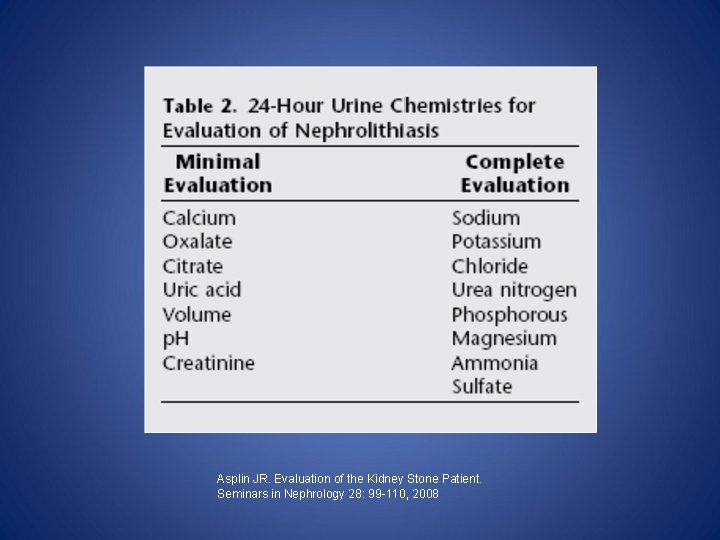
Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
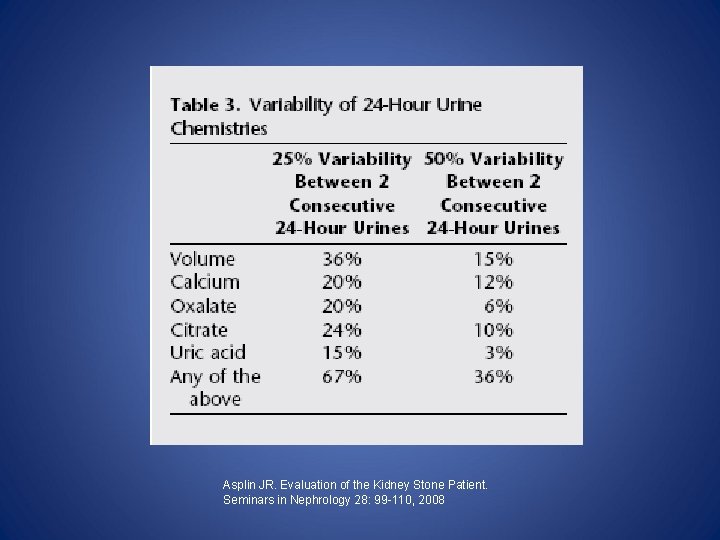
Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
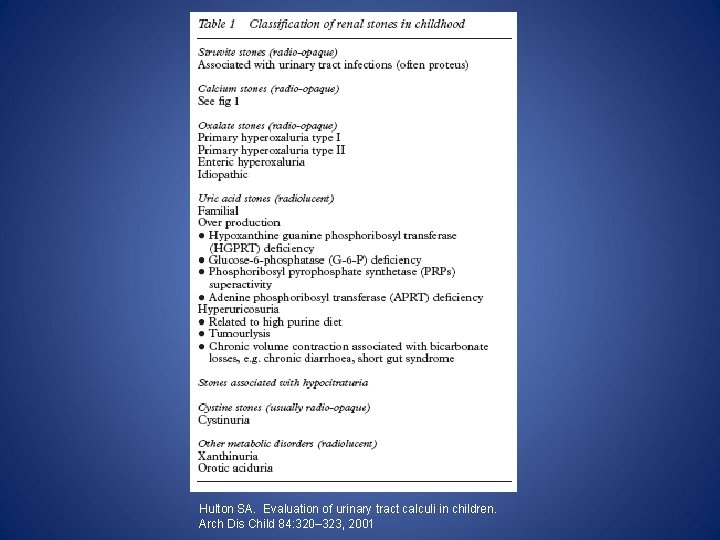
Hulton SA. Evaluation of urinary tract calculi in children. Arch Dis Child 84: 320– 323, 2001

Calcium stones • -Majority of calculi in children either • • • -calcium oxalate or -calcium phosphate. -Supersaturation of urine with calcium oxalate may result from -a) elevated excretion of calcium, oxalate, or uric acid -b) hypocitraturia
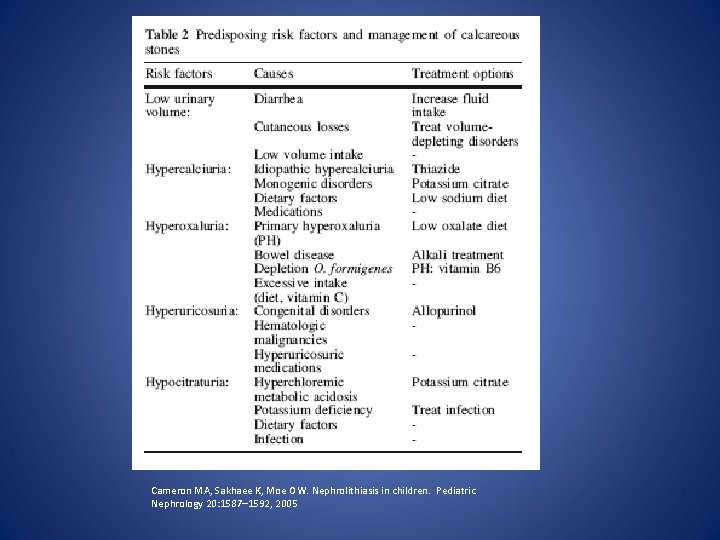
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005
Calcium Stones (cont'd): Hypercalciuria • • • • -Hypercalciuria accounts for 50– 97% of stones with an identifiable metabolic etiology 1, 2 -Definition: urinary calcium excretion > 4 mg/kg/day, or a urinary calcium/creatinine (U Ca/Cr) ratio > 0. 213 -Calcium excretion: lessens with increasing age lower in African American than in Caucasian children 3 -Risk of stone formation with hypercalciuria dependent on other factors, such as urine volume and citrate content -Hypercalciuria should be considered in children with hematuria, even in the absence of nephrolithiasis 4 -Review of the medical history, diet, and serum laboratory tests etiology intervention and stone prevention. -If no underlying cause identified, thiazide treatment has been found to be of benefit 5 1. Coward RJ, Peters CJ, Duffy PG, Corry D, Kellett MJ, Choong S, van’t Hoff WG (2003) Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child 88: 962– 965 2. Alon US, Zimmerman H, Alon M (2004) Evaluation and treatment of pediatric idiopathic urolithiasis-revisited. Pediatr Nephrol 19: 516 – 520 3. Butani L, Kalia A (2004) Idiopathic hypercalciuria in children— how valid are the existing diagnostic criteria? Pediatr Nephrol 19: 577– 582 4. Stapleton FB, Roy S 3 rd, Noe HN, Jerkins G (1984) Hypercalciuria in children with hematuria. N Engl J Med 310: 1345 -1348 5. Hymes LC, Warshaw BL (1987) Thiazide diuretics for the treatment of children with idiopathic hypercalciuria and hematuria. J Urol 138: 1217– 1219
Medications Associated with Calcium Stone Formation • • • Acetazolamide Amphotericin B Antacids (calcium and non-calcium antacids) Glucocorticoids Loop diuretics Theophylline Topiramate Vitamin D Zonisamide
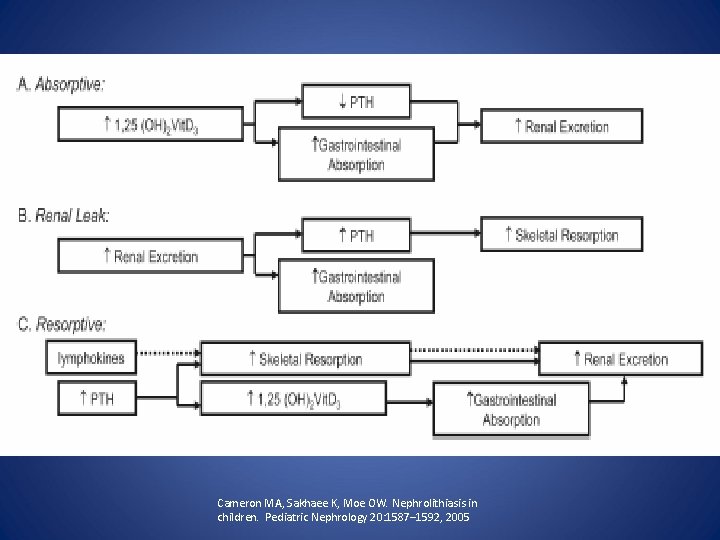
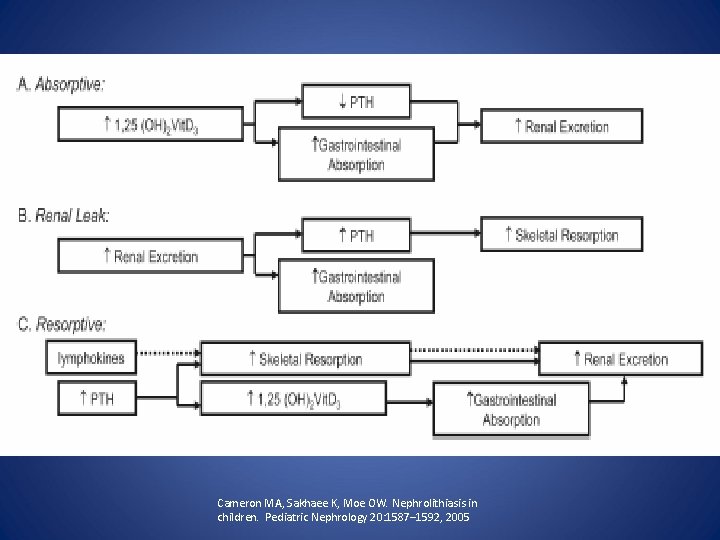
How does Hypercalciuria occur? • A) increased gastrointestinal calcium absorption • B) imbalance of bone formation and resorption, or • C) renal loss of calcium* (Typically all three systems affected because of secondary changes) *Pak CYC, Ohata M, Lawrence EC, Snyder W (1974) The hypercalciurias: causes, parathyroid functions, and diagnostic criteria. J Clin Invest 54: 387– 400
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005

Absorptive hypercalciuria (AH) • -Definition: a normal fasting U Ca/Cr (<0. 20 mg Ca/mg Cr) that significantly increases following a calcium load (>0. 20 mg Ca/mg Cr). • -Up to 40% of children with AH have family history of nephrolithiasis, suggesting a genetic predisposition. • -Likely results from polygenic anomalies, impeding determination of the molecular cause. A whole genome search in three kindreds has identified a candidate gene, but the pathophysiological mechanisms remain unknown 1 • -An additional mediator of AH may be 1, 25 -dihydroxyvitamin D, as elevated concentrations have been reported in hypercalciuric children 2 • • • 1. Reed BY, Gitomer WL, Heller HJ, Hsu MC, Lemke M, Padalino P, Pak CY (2002) Identification and characterization of a gene with base substitutions associated with the absorptive hypercalciuria phenotype and low spinal bone density. J Clin Endocrinol Metab 87: 1476– 1485 2. Stapleton FB, Langman CB, Bittle J, Miller LA (1987) Increased serum concentrations of 1, 25(OH)2 vitamin D in children with fasting hypercalciuria. J Pediatr 110: 234– 237
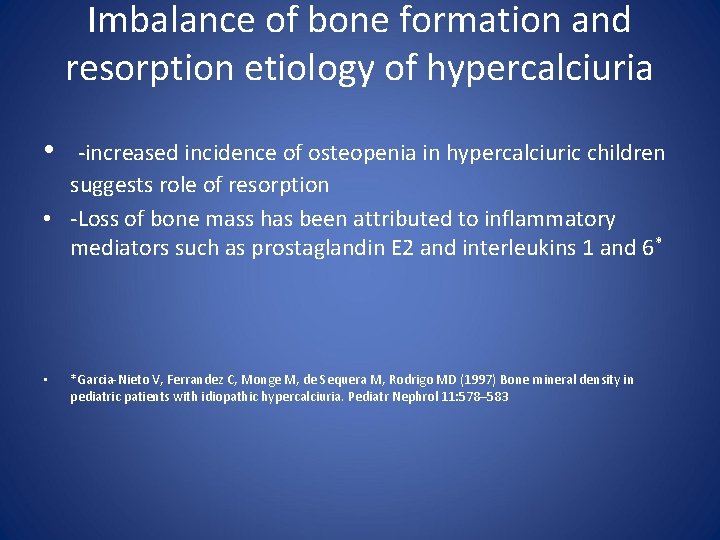
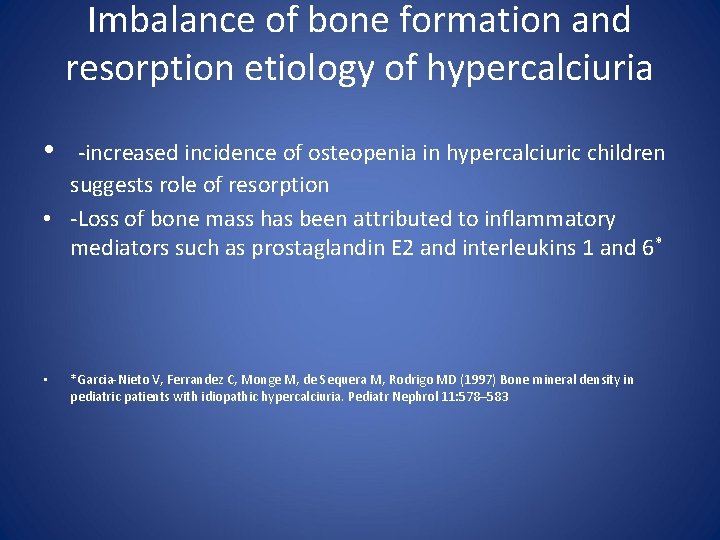
Imbalance of bone formation and resorption etiology of hypercalciuria • -increased incidence of osteopenia in hypercalciuric children suggests role of resorption • -Loss of bone mass has been attributed to inflammatory mediators such as prostaglandin E 2 and interleukins 1 and 6* • *Garcia-Nieto V, Ferrandez C, Monge M, de Sequera M, Rodrigo MD (1997) Bone mineral density in pediatric patients with idiopathic hypercalciuria. Pediatr Nephrol 11: 578– 583

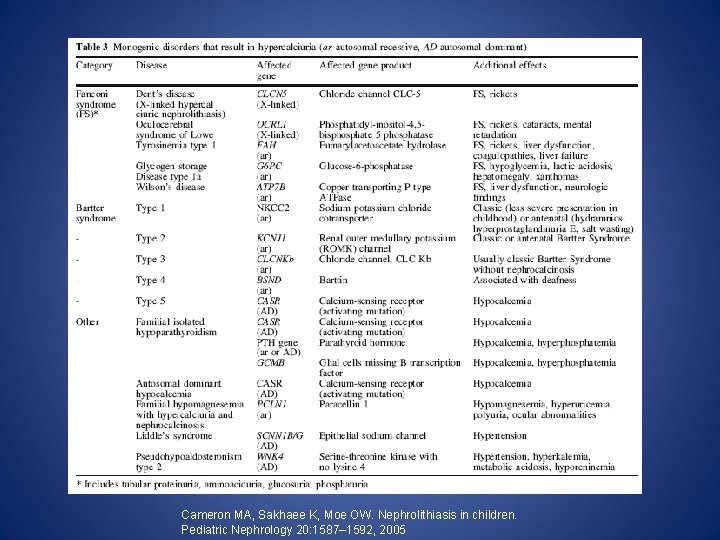
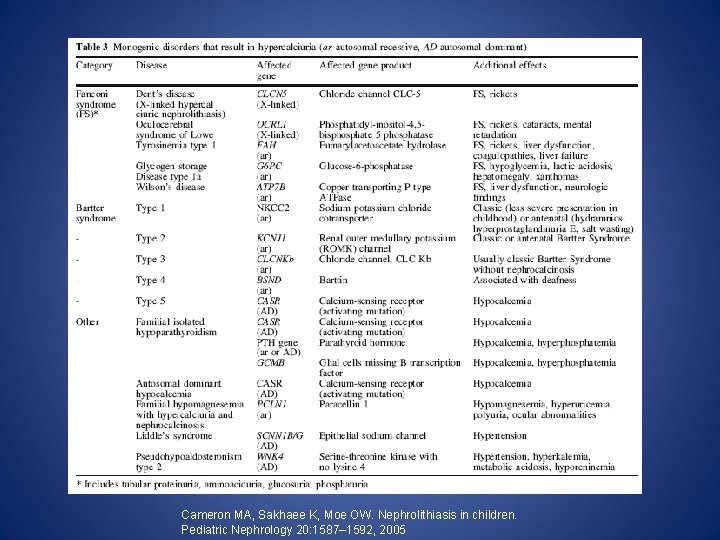
Renal calcium wasting as etiology of hypercalciuria • -occurs in several hereditary conditions, including monogenic disorders that should be considered in children 1 • -Environmental factors (e. g. high sodium or ketogenic diets) promote calcium excretion 2, 3 • -Hypercalcemic conditions may cause hypercalciuria by • a) increasing the calcium filtered load • b) directly inhibiting renal calcium absorption 4 • • 1. Langman CB (2004) The molecular basis of kidney stones. Curr Opin Pediatr 16: 188– 193 2. Reddy ST, Wang CY, Sakhaee K, Brinkley L, Pak CYC (2002) Effect of low-carbohydrate high-protein diets on acid-base balance, stoneforming propensity, and calcium metabolism. Am J Kidney Dis 40: 265 274 3. Furth SL, Casey JC, Pyzik PL, Neu AM, Docimo SG, Vining EPG, Freeman JM, Fivush BA (2000) Risk factors for urolithiasis in children on the ketogenic diet. Pediatr Nephrol 15: 125– 128 4. Bergstrom WH (1978) Hypercalciuria and hypercalcemia complicating immobilization. Am J Dis Child 132: 553– 554
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005

Calcium Stones (cont'd): Hypocitraturia • -Urinary citrate: mult. effects on stone formation and growth: * • a) binds ionized calcium (decreasing urinary calcium saturation) • b) impairs agglomeration of calcium oxalate (impeding growth of calcium phosphate crystals) • c) minimizes salting out of calcium oxalate by sodium urate. • * Cameron MA, Pak CYC (2004) Approach to the patient with the first episode of nephrolithiasis. Clin Rev Bone Miner Metab 2: 265– 278
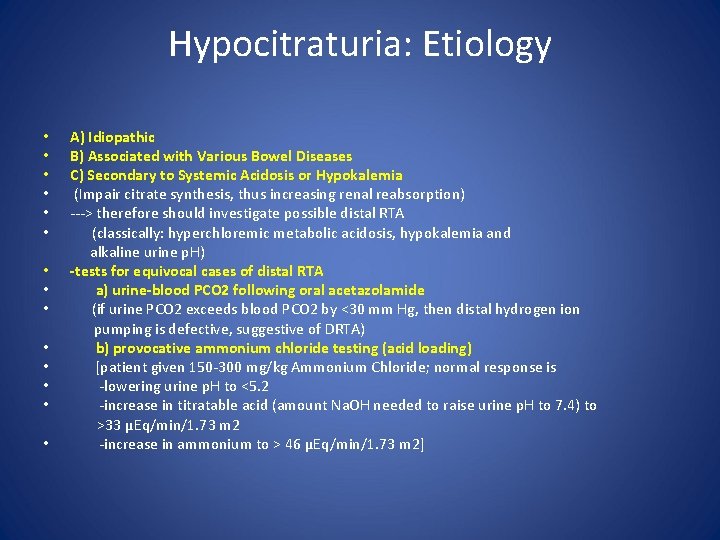
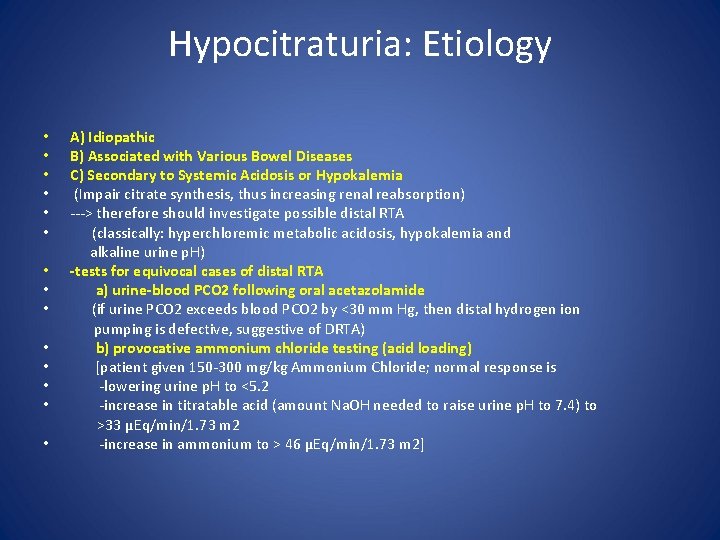
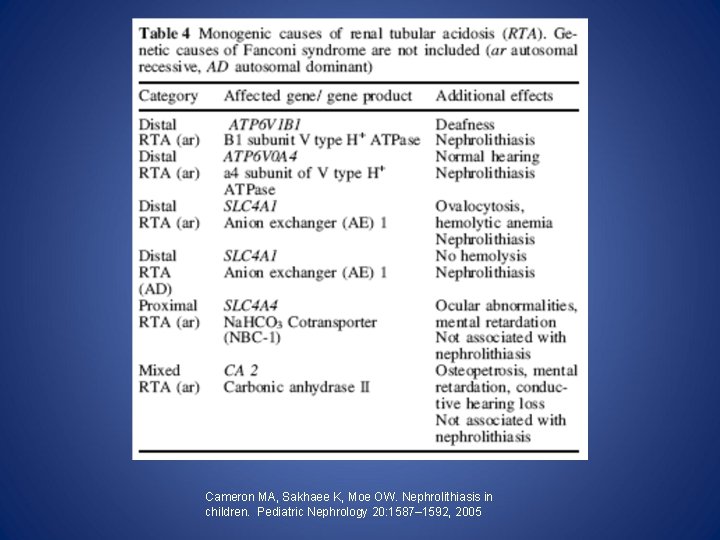
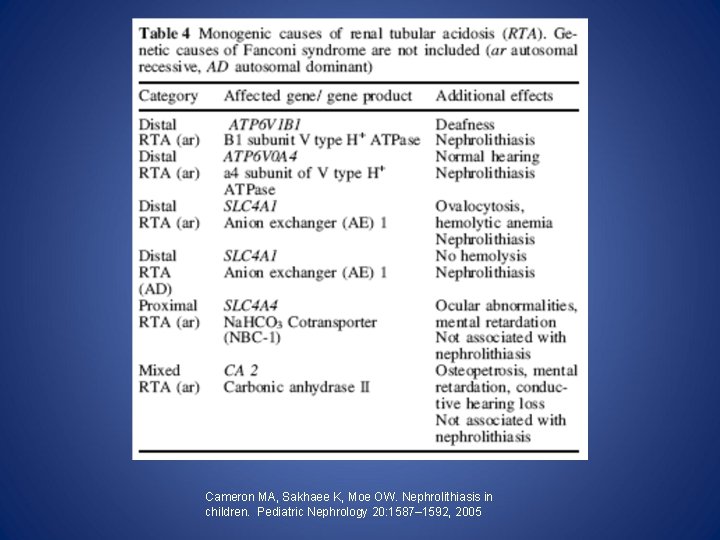
Hypocitraturia: Etiology • A) Idiopathic • B) Associated with Various Bowel Diseases • C) Secondary to Systemic Acidosis or Hypokalemia • (Impair citrate synthesis, thus increasing renal reabsorption) • ---> therefore should investigate possible distal RTA • (classically: hyperchloremic metabolic acidosis, hypokalemia and alkaline urine p. H) • -tests for equivocal cases of distal RTA • a) urine-blood PCO 2 following oral acetazolamide • (if urine PCO 2 exceeds blood PCO 2 by <30 mm Hg, then distal hydrogen ion pumping is defective, suggestive of DRTA) • b) provocative ammonium chloride testing (acid loading) • [patient given 150 -300 mg/kg Ammonium Chloride; normal response is • -lowering urine p. H to <5. 2 • -increase in titratable acid (amount Na. OH needed to raise urine p. H to 7. 4) to >33 µEq/min/1. 73 m 2 • -increase in ammonium to > 46 µEq/min/1. 73 m 2]
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005
Hypocitraturia: Treatment • -Administration of Potassium Citrate • -Close monitoring of Urine p. H • -Diet rich in fruit and vegetables (enhances urine potassium and consequently citrate excretion)* • *Meschi T, Maggiore U, Fiaccadori E et al. The effect of fruits and vegetables on urinary stone risk factors. Kidney Int 66: 2402, 2004
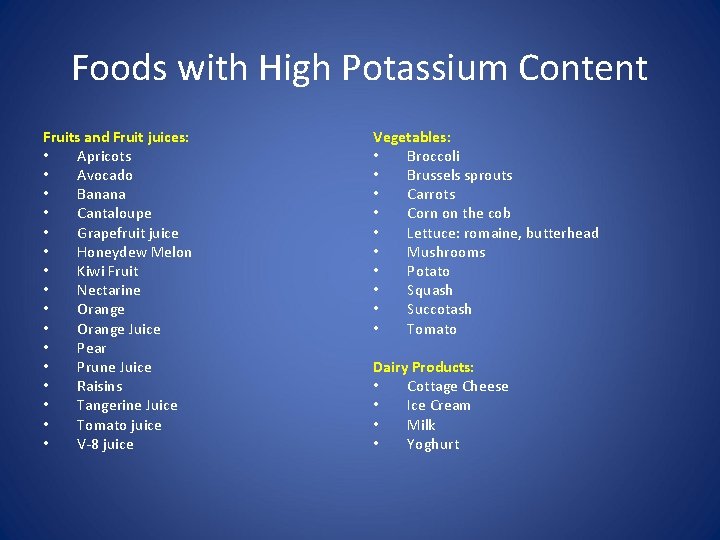
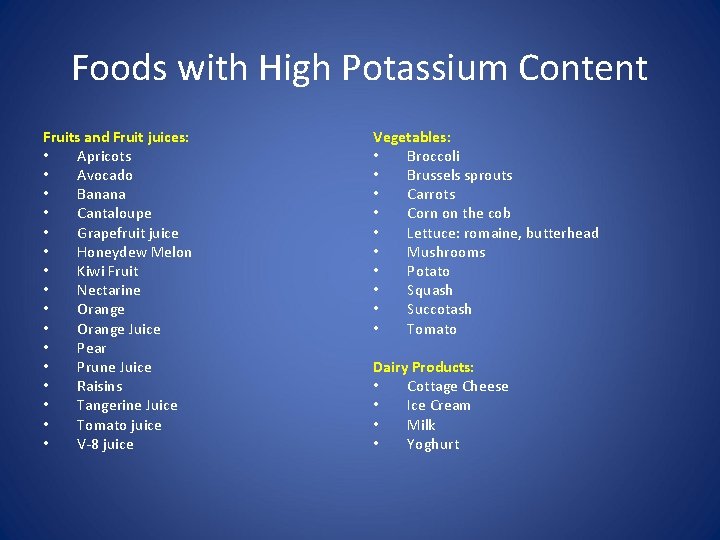
Foods with High Potassium Content Fruits and Fruit juices: • Apricots • Avocado • Banana • Cantaloupe • Grapefruit juice • Honeydew Melon • Kiwi Fruit • Nectarine • Orange Juice • Pear • Prune Juice • Raisins • Tangerine Juice • Tomato juice • V-8 juice Vegetables: • Broccoli • Brussels sprouts • Carrots • Corn on the cob • Lettuce: romaine, butterhead • Mushrooms • Potato • Squash • Succotash • Tomato Dairy Products: • Cottage Cheese • Ice Cream • Milk • Yoghurt
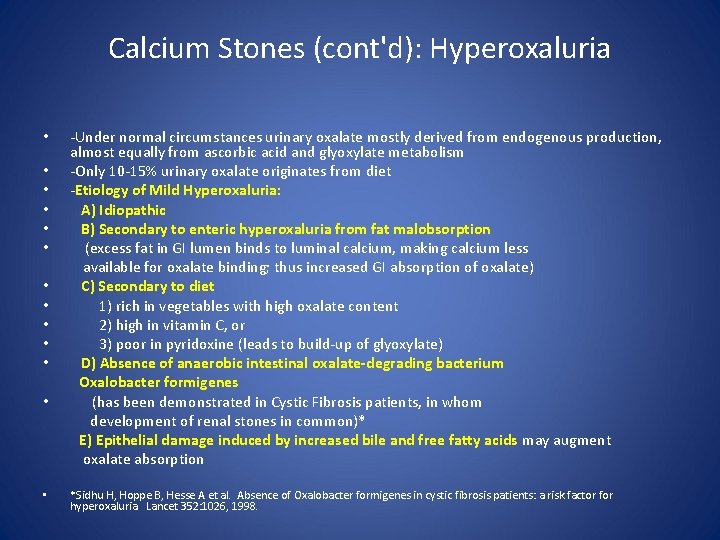
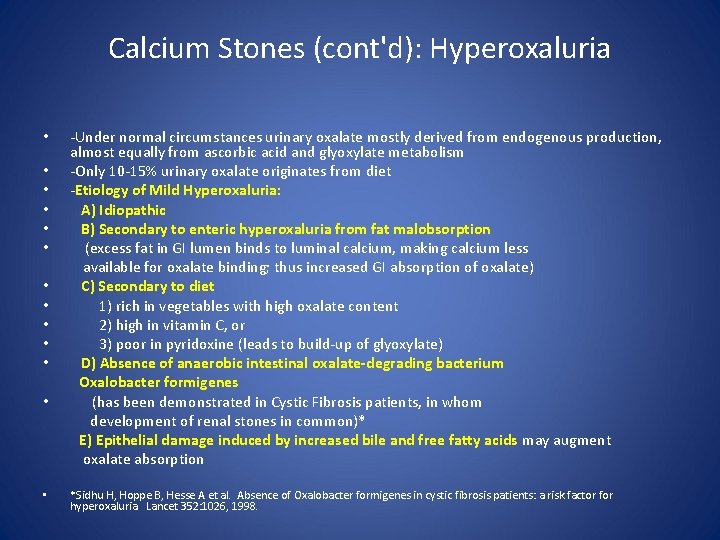
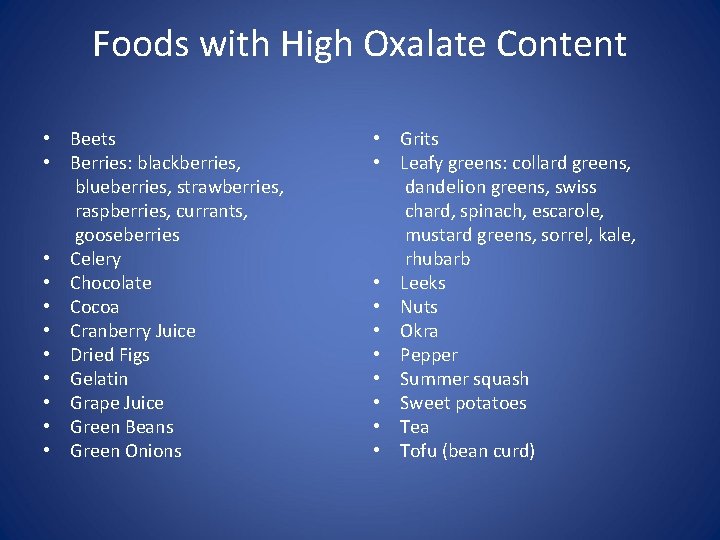
Calcium Stones (cont'd): Hyperoxaluria -Under normal circumstances urinary oxalate mostly derived from endogenous production, almost equally from ascorbic acid and glyoxylate metabolism • -Only 10 -15% urinary oxalate originates from diet • -Etiology of Mild Hyperoxaluria: • A) Idiopathic • B) Secondary to enteric hyperoxaluria from fat malobsorption • (excess fat in GI lumen binds to luminal calcium, making calcium less available for oxalate binding; thus increased GI absorption of oxalate) • C) Secondary to diet • 1) rich in vegetables with high oxalate content • 2) high in vitamin C, or • 3) poor in pyridoxine (leads to build-up of glyoxylate) • D) Absence of anaerobic intestinal oxalate-degrading bacterium Oxalobacter formigenes • (has been demonstrated in Cystic Fibrosis patients, in whom development of renal stones in common)* E) Epithelial damage induced by increased bile and free fatty acids may augment oxalate absorption • • *Sidhu H, Hoppe B, Hesse A et al. Absence of Oxalobacter formigenes in cystic fibrosis patients: a risk factor for hyperoxaluria. Lancet 352: 1026, 1998.
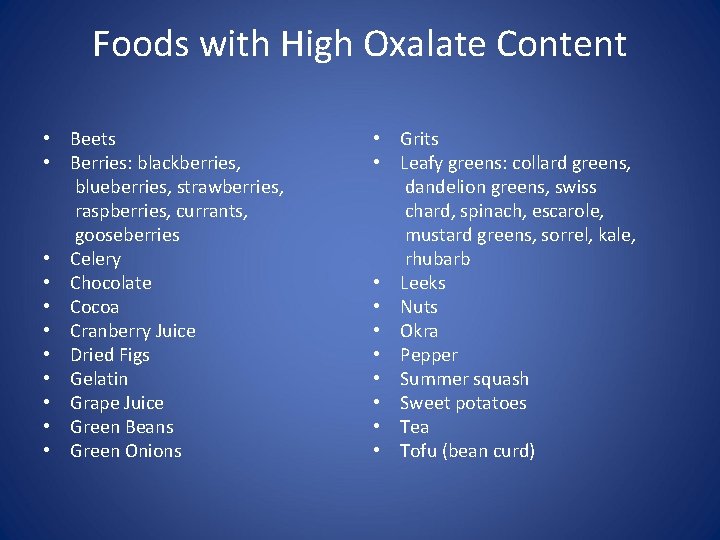
Foods with High Oxalate Content • Beets • Berries: blackberries, blueberries, strawberries, raspberries, currants, gooseberries • Celery • Chocolate • Cocoa • Cranberry Juice • Dried Figs • Gelatin • Grape Juice • Green Beans • Green Onions • Grits • Leafy greens: collard greens, dandelion greens, swiss chard, spinach, escarole, mustard greens, sorrel, kale, rhubarb • Leeks • Nuts • Okra • Pepper • Summer squash • Sweet potatoes • Tea • Tofu (bean curd)
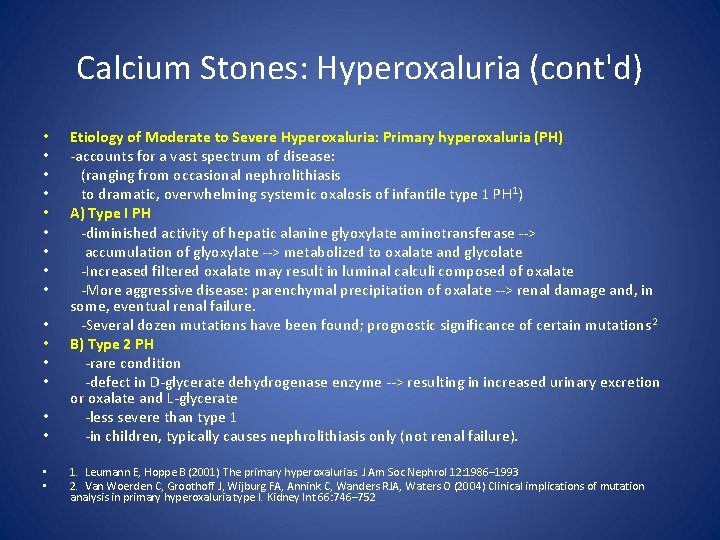
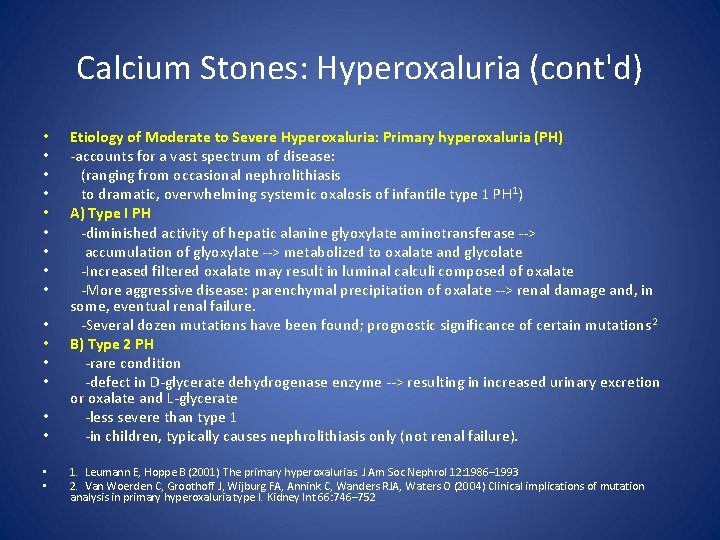
Calcium Stones: Hyperoxaluria (cont'd) • • • • • Etiology of Moderate to Severe Hyperoxaluria: Primary hyperoxaluria (PH) -accounts for a vast spectrum of disease: (ranging from occasional nephrolithiasis to dramatic, overwhelming systemic oxalosis of infantile type 1 PH 1) A) Type I PH -diminished activity of hepatic alanine glyoxylate aminotransferase --> accumulation of glyoxylate --> metabolized to oxalate and glycolate -Increased filtered oxalate may result in luminal calculi composed of oxalate -More aggressive disease: parenchymal precipitation of oxalate --> renal damage and, in some, eventual renal failure. -Several dozen mutations have been found; prognostic significance of certain mutations 2 B) Type 2 PH -rare condition -defect in D-glycerate dehydrogenase enzyme --> resulting in increased urinary excretion or oxalate and L-glycerate -less severe than type 1 -in children, typically causes nephrolithiasis only (not renal failure). 1. Leumann E, Hoppe B (2001) The primary hyperoxalurias. J Am Soc Nephrol 12: 1986– 1993 2. Van Woerden C, Groothoff J, Wijburg FA, Annink C, Wanders RJA, Waters O (2004) Clinical implications of mutation analysis in primary hyperoxaluria type I. Kidney Int 66: 746– 752
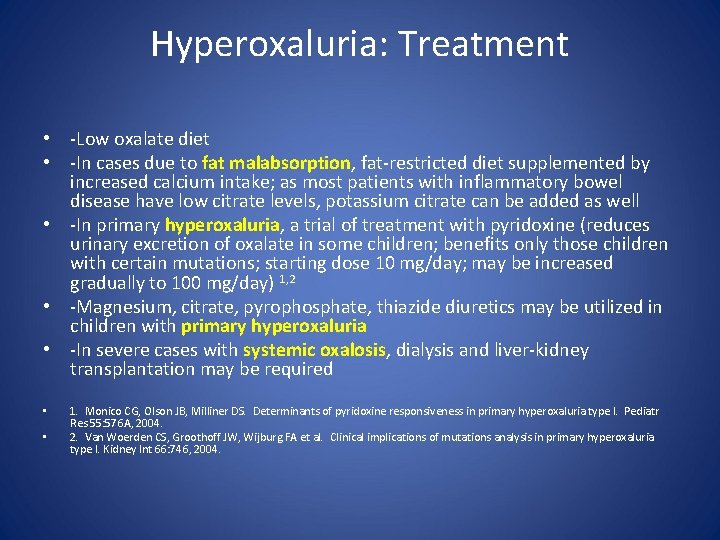
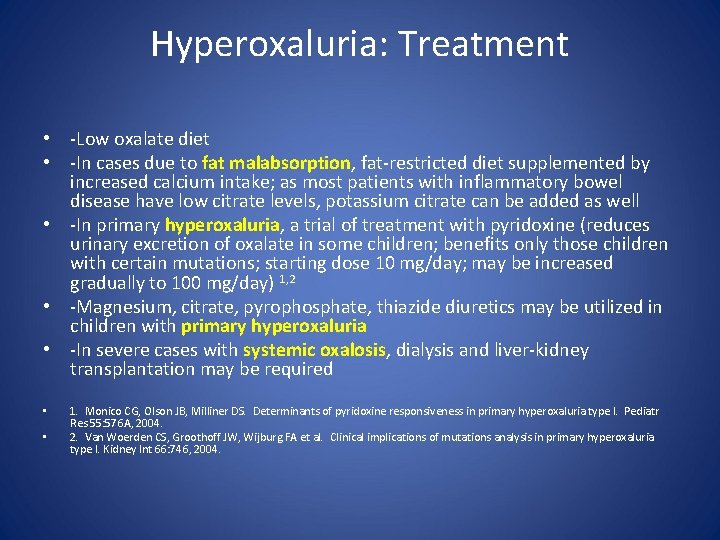
Hyperoxaluria: Treatment • -Low oxalate diet • -In cases due to fat malabsorption, fat-restricted diet supplemented by increased calcium intake; as most patients with inflammatory bowel disease have low citrate levels, potassium citrate can be added as well • -In primary hyperoxaluria, a trial of treatment with pyridoxine (reduces urinary excretion of oxalate in some children; benefits only those children with certain mutations; starting dose 10 mg/day; may be increased gradually to 100 mg/day) 1, 2 • -Magnesium, citrate, pyrophosphate, thiazide diuretics may be utilized in children with primary hyperoxaluria • -In severe cases with systemic oxalosis, dialysis and liver-kidney transplantation may be required • • 1. Monico CG, Olson JB, Milliner DS. Determinants of pyridoxine responsiveness in primary hyperoxaluria type I. Pediatr Res 55: 576 A, 2004. 2. Van Woerden CS, Groothoff JW, Wijburg FA et al. Clinical implications of mutations analysis in primary hyperoxaluria type I. Kidney Int 66: 746, 2004.
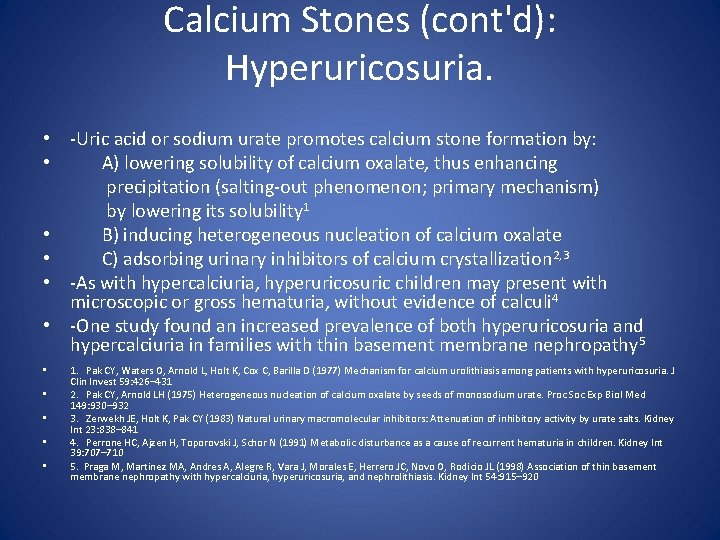
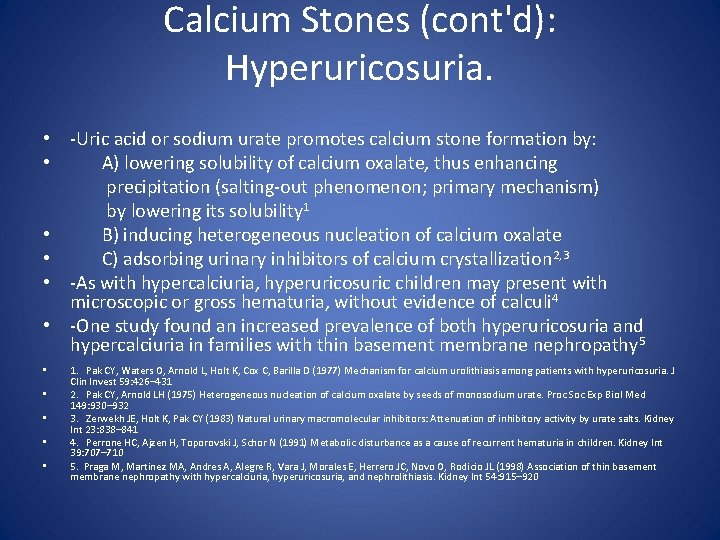
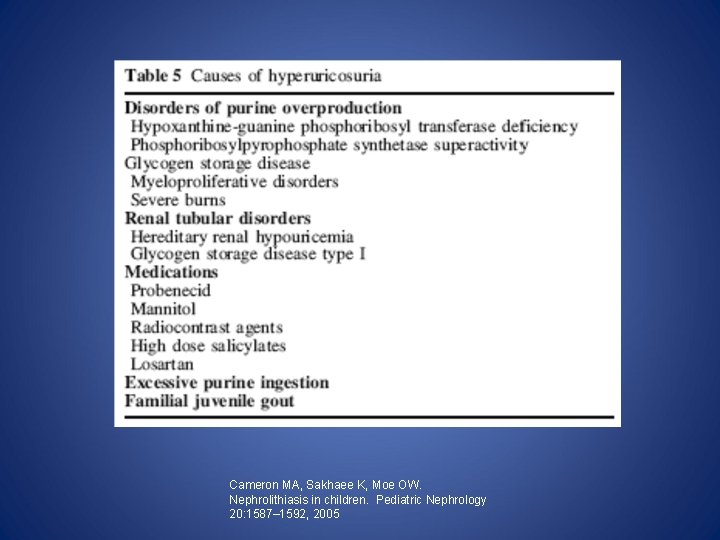
Calcium Stones (cont'd): Hyperuricosuria. • -Uric acid or sodium urate promotes calcium stone formation by: • A) lowering solubility of calcium oxalate, thus enhancing precipitation (salting-out phenomenon; primary mechanism) by lowering its solubility 1 • B) inducing heterogeneous nucleation of calcium oxalate • C) adsorbing urinary inhibitors of calcium crystallization 2, 3 • -As with hypercalciuria, hyperuricosuric children may present with microscopic or gross hematuria, without evidence of calculi 4 • -One study found an increased prevalence of both hyperuricosuria and hypercalciuria in families with thin basement membrane nephropathy 5 • • • 1. Pak CY, Waters O, Arnold L, Holt K, Cox C, Barilla D (1977) Mechanism for calcium urolithiasis among patients with hyperuricosuria. J Clin Invest 59: 426– 431 2. Pak CY, Arnold LH (1975) Heterogeneous nucleation of calcium oxalate by seeds of monosodium urate. Proc Soc Exp Biol Med 149: 930– 932 3. Zerwekh JE, Holt K, Pak CY (1983) Natural urinary macromolecular inhibitors: Attenuation of inhibitory activity by urate salts. Kidney Int 23: 838– 841 4. Perrone HC, Ajzen H, Toporovski J, Schor N (1991) Metabolic disturbance as a cause of recurrent hematuria in children. Kidney Int 39: 707– 710 5. Praga M, Martinez MA, Andres A, Alegre R, Vara J, Morales E, Herrero JC, Novo O, Rodicio JL (1998) Association of thin basement membrane nephropathy with hypercalciuria, hyperuricosuria, and nephrolithiasis. Kidney Int 54: 915– 920
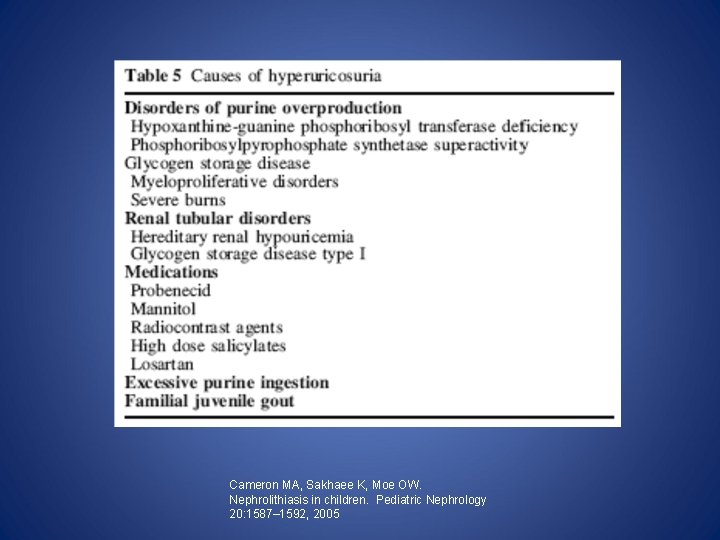
Uric Acid Stones • -account for 2 -4% of urolithiasis in children • -in contrast with calcium stones, are radiolucent • -In children >2 yrs old, normal uric acid excreted per GFR value is <0. 56 mg/dl by formula* (age related nomograms published; higher in infancy and decrease with age): Uric Acid/GFR = U uric acid x S creatinine/U creatinine • -Increased urinary uric acid excretion may result from A) increased glomerular load of uric acid B) isolated or generalized tubular defects C) Iatrogenic administration of uricosuric drugs D) persistently low urinary p. H • * Matos V, Van Melle G, Werner D et al. Urinary oxalate and urate to creatinine ratios in a healthy pediatric population. Am J Kidney Dis 34: e 6, 1999.
Uric Acid Stones (cont’d): Etiology • A) Increased glomerular load of uric acid • 1) excessive dietary purine intake • 2) hematologic/myeloproliferative disorders • 3) metabolic errors such as Lesch-Nyhan syndrome, glycogen storage disease type 1, etc • -therefore, work up for uric acid stones + hyperuricemia: evaluation for purine salvage enzymes * • a) hypoxanthine-guanine phosphoribosyl transferase (HPRT) (complete deficiency: Lesch-Nyhan syndrome; afflicted males with severe neurologic abnormalities in addition to recurrent uric acid calculi) • b) phosphoribosyl pyrophosphate synthetase (PRPS) • * Cameron JS, Moro F, Simmonds HA. Gout, uric acid, and purine metabolism in paediatric nephrology. Pediatr Nephrol 7: 105, 1993.
Foods with High Purine Content Alcohol Asparagus Cauliflower Chickoo Custard apple Dry beans (lentils, lima, and kidney beans) • Fish: anchovies, sardines (canned), herring, mackerel, cod, halibut, tuna, carp • Gravies • Meat extracts: boillion, broth, consomme, stock • • Meat: beef, pork, lamb, poultry • Mushrooms • Organ meats: kidney, liver, pancreas, brain, heart • Peas • Pulses • Shellfish • Spinach • Sweet breads • Tea and coffee
Uric Acid Stones: Etiology (cont’d) • B) Urolithiasis associated with hyperuricosuria and low to normal serum uric acid • -1) Renal tubular defects (Renal processing or uric acid is complex; involves glomerular filtration, proximal tubular reabsorption and secretion)1 • a) primary tubular defect in uric acid handling • -results from defect in renal urate exchanger URAT 1 (responsible for proximal uric acid absorption)2 b) secondary generalized proximal tubular disorders • -2) Iatrogenic administration of various uricosuric drugs • • 1. Maalouf N, Sakhaee K, Parks JH, Coe FL, Adams-Huet B, Pak CYC (2004) Association of urinary p. H with body weight in nephrolithiasis. Kidney Int 65: 386– 392 2. Enomoto A, Kimura H, Chairoungdua A, Shigeta Y, Jutabha P, Cha SH, Hosoyamada M, Takeda M, Sekine T, Igarashi T, Matsuo H, Kikuchi Y, Oda T, Ichida K, Hosoya T, Shimokata K, Niwa T, Kanai Y, Endou H (2002) Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 417: 447– 452

Medications Associated with Uric Acid Stone Formation • • • • Acetohexamide Allopurinol (xanthine stones) Ascorbic Acid Benzbromarone Calcium ipodate Chorprothixene Cinchphen Dicumarol Estrogen Glycerol guaiacolate Halofenate Iodopyracet Iopanoic acid Ketogenic Diet • • • Meglumine iodipamide Orotic Acid Outdated tetracyclines Phenylbutazone Phenylsulfonphthalein Phenylbutazone Probenecid Salicylates Sodium diatrizoate Ticrynafen Zoxazolamine
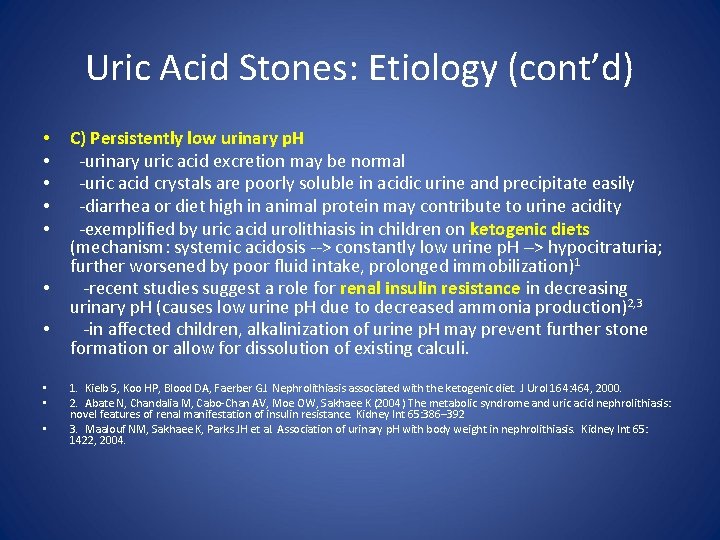
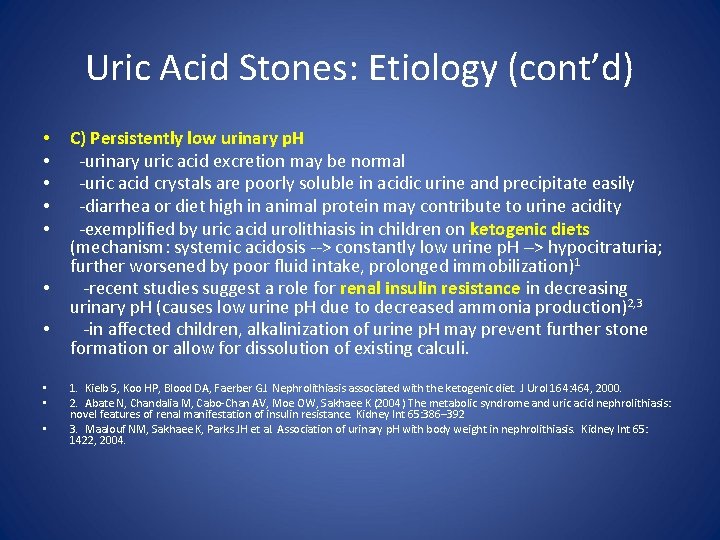
Uric Acid Stones: Etiology (cont’d) • • • C) Persistently low urinary p. H -urinary uric acid excretion may be normal -uric acid crystals are poorly soluble in acidic urine and precipitate easily -diarrhea or diet high in animal protein may contribute to urine acidity -exemplified by uric acid urolithiasis in children on ketogenic diets (mechanism: systemic acidosis --> constantly low urine p. H --> hypocitraturia; further worsened by poor fluid intake, prolonged immobilization)1 -recent studies suggest a role for renal insulin resistance in decreasing urinary p. H (causes low urine p. H due to decreased ammonia production)2, 3 -in affected children, alkalinization of urine p. H may prevent further stone formation or allow for dissolution of existing calculi. 1. Kielb S, Koo HP, Blood DA, Faerber GJ. Nephrolithiasis associated with the ketogenic diet. J Urol 164: 464, 2000. 2. Abate N, Chandalia M, Cabo-Chan AV, Moe OW, Sakhaee K (2004) The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int 65: 386– 392 3. Maalouf NM, Sakhaee K, Parks JH et al. Association of urinary p. H with body weight in nephrolithiasis. Kidney Int 65: 1422, 2004.
Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005
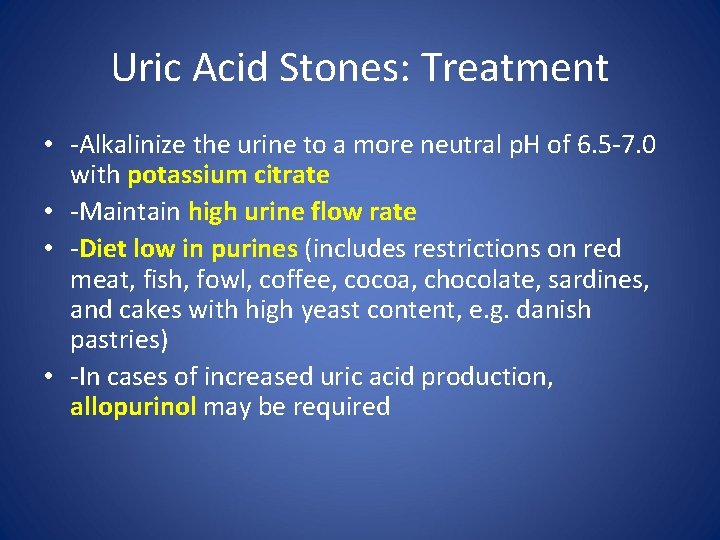
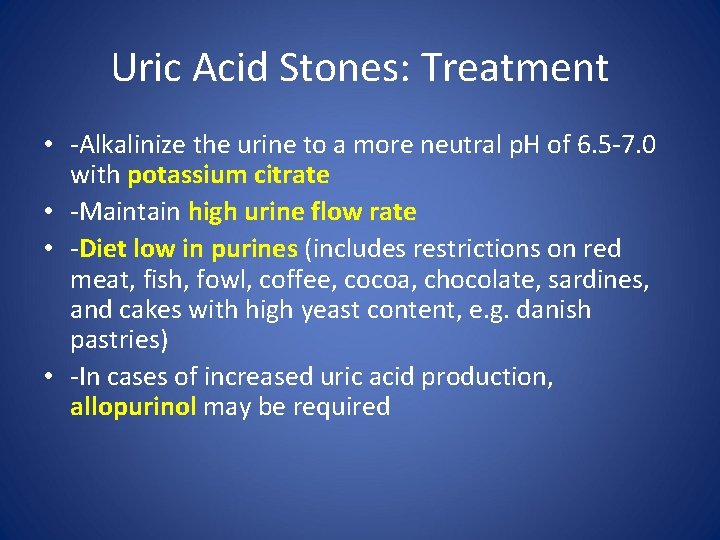
Uric Acid Stones: Treatment • -Alkalinize the urine to a more neutral p. H of 6. 5 -7. 0 with potassium citrate • -Maintain high urine flow rate • -Diet low in purines (includes restrictions on red meat, fish, fowl, coffee, cocoa, chocolate, sardines, and cakes with high yeast content, e. g. danish pastries) • -In cases of increased uric acid production, allopurinol may be required

2, 8 Dihydroxyadenine calculi • -results from autosomal recessive disorder • -deficiency of adenine phosphoribosyl transferase (APRT) • -calculi difficult to distinguish from uric acid stones (requires specialized chemical analysis) • -normal levels of uric acid in the serum and urine • -clue to diagnosis can be brownish crystals in baby's diaper • -probably underdiagnosed (misdiagnosed as urid acid stone; both disorders respond to allopurinol; both respond to low purine diet) • -Importance of correct diagnosis: alkalinization of urine (indicated for uric acid stones) decreases solubility of 2, 8 dihyroxyadenine, thus increasing urolithiasis risk
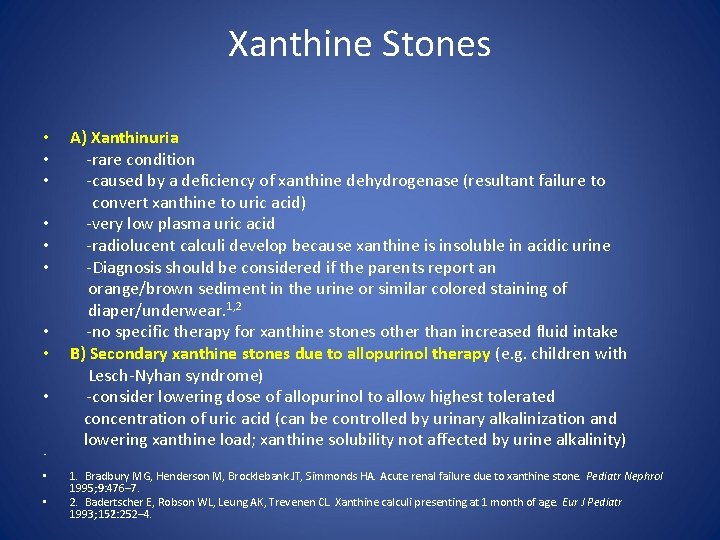
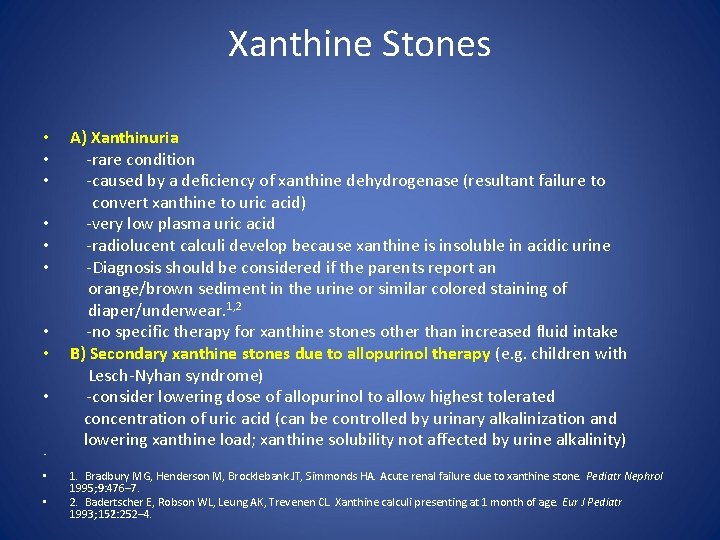
Xanthine Stones • A) Xanthinuria • -rare condition • -caused by a deficiency of xanthine dehydrogenase (resultant failure to convert xanthine to uric acid) • -very low plasma uric acid • -radiolucent calculi develop because xanthine is insoluble in acidic urine • -Diagnosis should be considered if the parents report an orange/brown sediment in the urine or similar colored staining of diaper/underwear. 1, 2 • -no specific therapy for xanthine stones other than increased fluid intake • B) Secondary xanthine stones due to allopurinol therapy (e. g. children with Lesch-Nyhan syndrome) • -consider lowering dose of allopurinol to allow highest tolerated concentration of uric acid (can be controlled by urinary alkalinization and lowering xanthine load; xanthine solubility not affected by urine alkalinity) • 1. Bradbury MG, Henderson M, Brocklebank JT, Simmonds HA. Acute renal failure due to xanthine stone. Pediatr Nephrol 1995; 9: 476– 7. 2. Badertscher E, Robson WL, Leung AK, Trevenen CL. Xanthine calculi presenting at 1 month of age. Eur J Pediatr 1993; 152: 252– 4. •
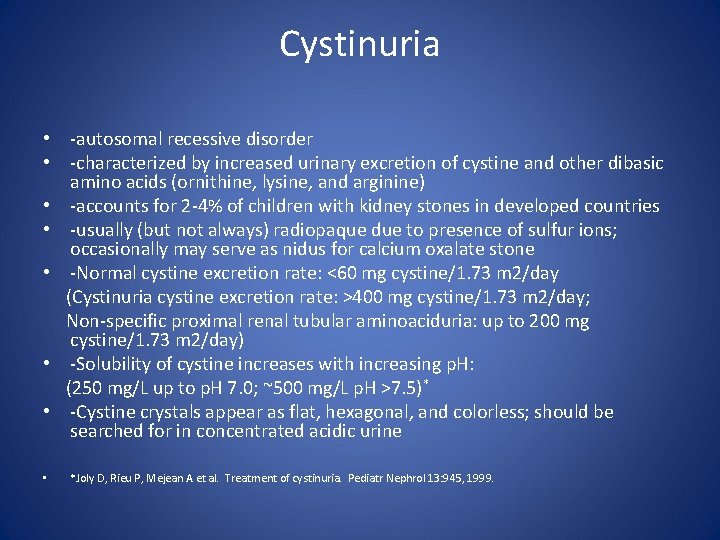
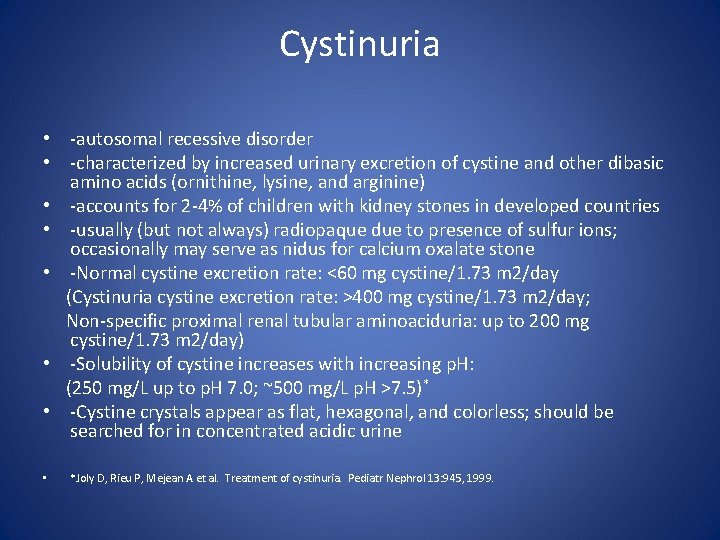
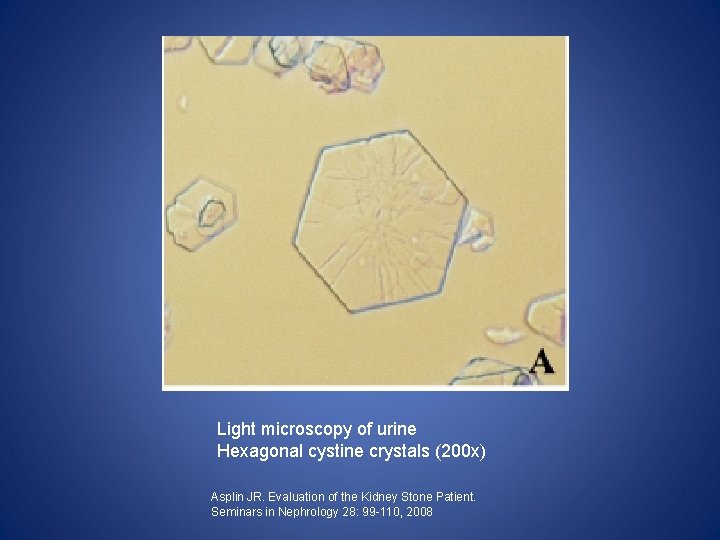
Cystinuria • -autosomal recessive disorder • -characterized by increased urinary excretion of cystine and other dibasic amino acids (ornithine, lysine, and arginine) • -accounts for 2 -4% of children with kidney stones in developed countries • -usually (but not always) radiopaque due to presence of sulfur ions; occasionally may serve as nidus for calcium oxalate stone • -Normal cystine excretion rate: <60 mg cystine/1. 73 m 2/day (Cystinuria cystine excretion rate: >400 mg cystine/1. 73 m 2/day; Non-specific proximal renal tubular aminoaciduria: up to 200 mg cystine/1. 73 m 2/day) • -Solubility of cystine increases with increasing p. H: (250 mg/L up to p. H 7. 0; ~500 mg/L p. H >7. 5)* • -Cystine crystals appear as flat, hexagonal, and colorless; should be searched for in concentrated acidic urine • *Joly D, Rieu P, Mejean A et al. Treatment of cystinuria. Pediatr Nephrol 13: 945, 1999.
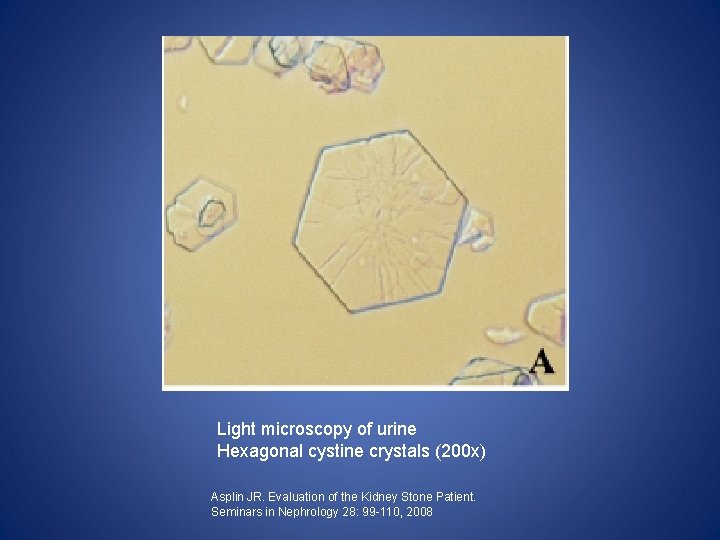
Light microscopy of urine Hexagonal cystine crystals (200 x) Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
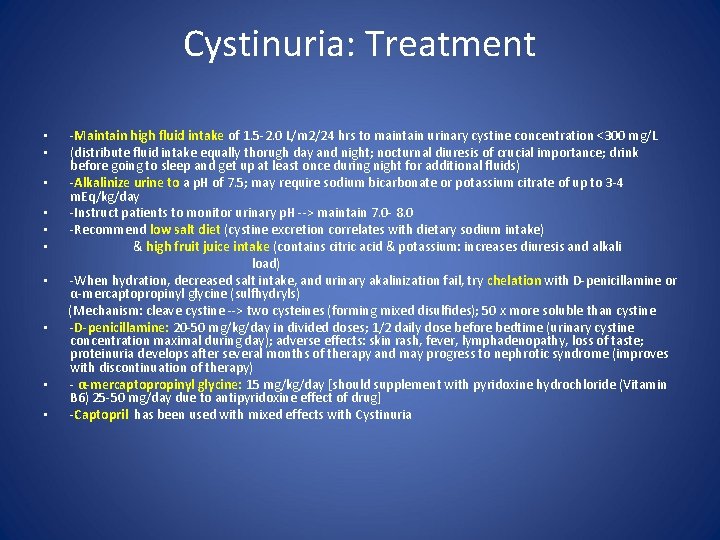
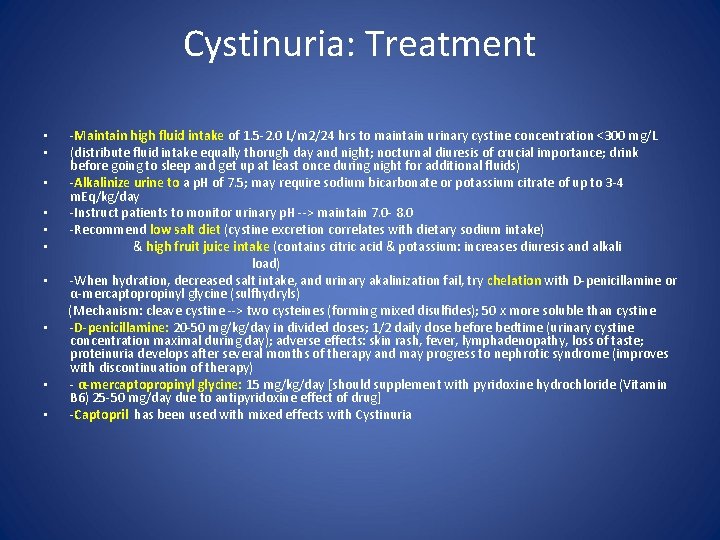
Cystinuria: Treatment -Maintain high fluid intake of 1. 5 -2. 0 L/m 2/24 hrs to maintain urinary cystine concentration <300 mg/L (distribute fluid intake equally thorugh day and night; nocturnal diuresis of crucial importance; drink before going to sleep and get up at least once during night for additional fluids) • -Alkalinize urine to a p. H of 7. 5; may require sodium bicarbonate or potassium citrate of up to 3 -4 m. Eq/kg/day • -Instruct patients to monitor urinary p. H --> maintain 7. 0 - 8. 0 • -Recommend low salt diet (cystine excretion correlates with dietary sodium intake) • & high fruit juice intake (contains citric acid & potassium: increases diuresis and alkali load) • -When hydration, decreased salt intake, and urinary akalinization fail, try chelation with D-penicillamine or α-mercaptopropinyl glycine (sulfhydryls) (Mechanism: cleave cystine --> two cysteines (forming mixed disulfides); 50 x more soluble than cystine • -D-penicillamine: 20 -50 mg/kg/day in divided doses; 1/2 daily dose before bedtime (urinary cystine concentration maximal during day); adverse effects: skin rash, fever, lymphadenopathy, loss of taste; proteinuria develops after several months of therapy and may progress to nephrotic syndrome (improves with discontinuation of therapy) • - α-mercaptopropinyl glycine: 15 mg/kg/day [should supplement with pyridoxine hydrochloride (Vitamin B 6) 25 -50 mg/day due to antipyridoxine effect of drug] • -Captopril has been used with mixed effects with Cystinuria • •
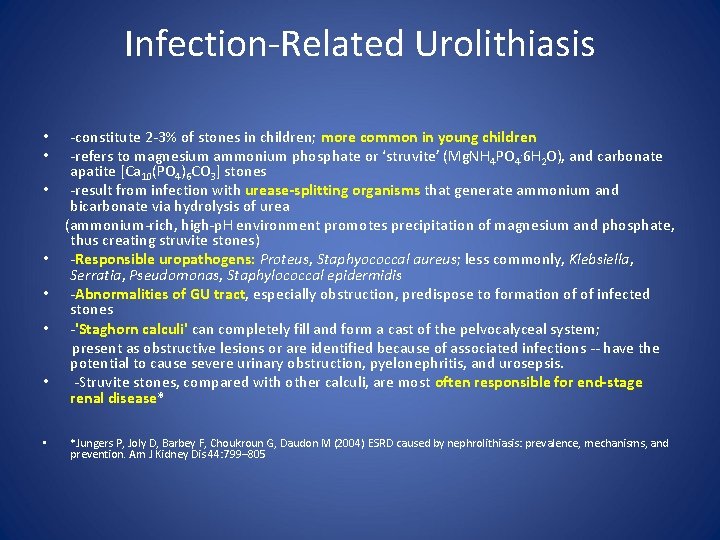
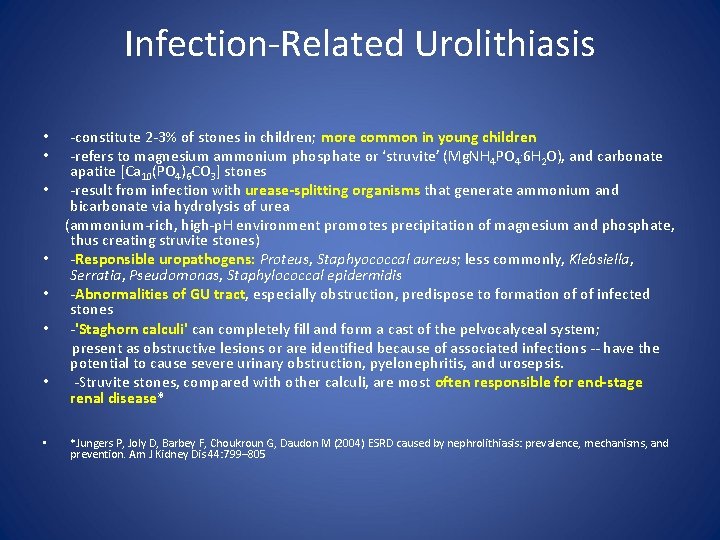
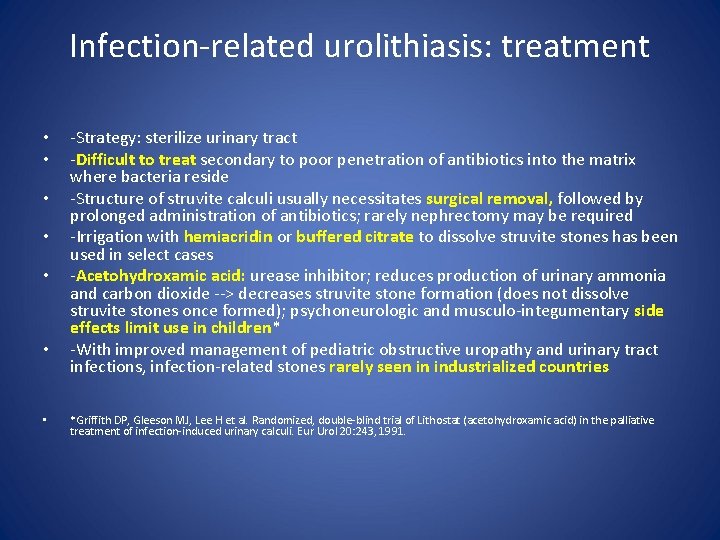
Infection-Related Urolithiasis -constitute 2 -3% of stones in children; more common in young children -refers to magnesium ammonium phosphate or ‘struvite’ (Mg. NH 4 PO 4. 6 H 2 O), and carbonate apatite [Ca 10(PO 4)6 CO 3] stones • -result from infection with urease-splitting organisms that generate ammonium and bicarbonate via hydrolysis of urea (ammonium-rich, high-p. H environment promotes precipitation of magnesium and phosphate, thus creating struvite stones) • -Responsible uropathogens: Proteus, Staphyococcal aureus; less commonly, Klebsiella, Serratia, Pseudomonas, Staphylococcal epidermidis • -Abnormalities of GU tract, especially obstruction, predispose to formation of of infected stones • -'Staghorn calculi' can completely fill and form a cast of the pelvocalyceal system; present as obstructive lesions or are identified because of associated infections -- have the potential to cause severe urinary obstruction, pyelonephritis, and urosepsis. • -Struvite stones, compared with other calculi, are most often responsible for end-stage renal disease* • • • *Jungers P, Joly D, Barbey F, Choukroun G, Daudon M (2004) ESRD caused by nephrolithiasis: prevalence, mechanisms, and prevention. Am J Kidney Dis 44: 799– 805
Light microscopy of coffin-lid–shaped struvite crystals (200 x) Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99 -110, 2008
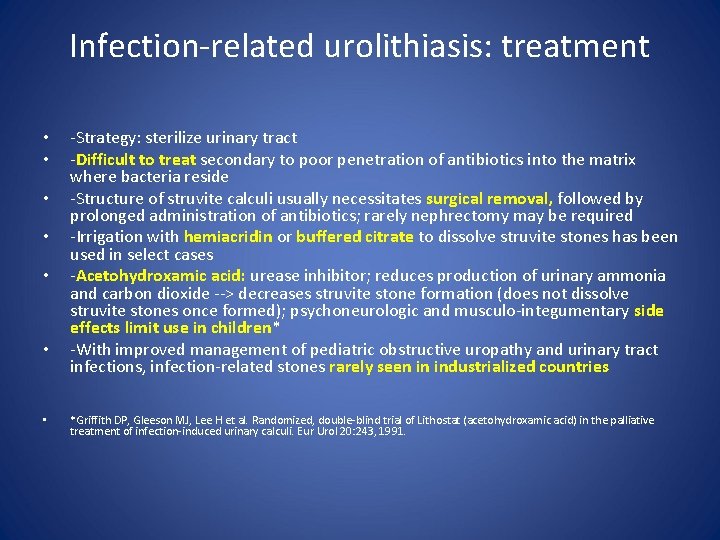
Infection-related urolithiasis: treatment • • -Strategy: sterilize urinary tract -Difficult to treat secondary to poor penetration of antibiotics into the matrix where bacteria reside -Structure of struvite calculi usually necessitates surgical removal, followed by prolonged administration of antibiotics; rarely nephrectomy may be required -Irrigation with hemiacridin or buffered citrate to dissolve struvite stones has been used in select cases -Acetohydroxamic acid: urease inhibitor; reduces production of urinary ammonia and carbon dioxide --> decreases struvite stone formation (does not dissolve struvite stones once formed); psychoneurologic and musculo-integumentary side effects limit use in children* -With improved management of pediatric obstructive uropathy and urinary tract infections, infection-related stones rarely seen in industrialized countries *Griffith DP, Gleeson MJ, Lee H et al. Randomized, double-blind trial of Lithostat (acetohydroxamic acid) in the palliative treatment of infection-induced urinary calculi. Eur Urol 20: 243, 1991.
Hulton SA. Evaluation of urinary tract calculi in children. Arch Dis Child 84: 320– 323, 2001


Resources • Cameron MA, Sakhaee K, Moe OW. Nephrolithiasis in children. Pediatric Nephrology 20: 1587– 1592, 2005 • Asplin JR. Evaluation of the Kidney Stone Patient. Seminars in Nephrology 28: 99110, 2008 • Hulton SA. Evaluation of urinary tract calculi in children. Arch Dis Child 84: 320– 323, 2001 • Alon US, Srivastava T. Urolithiasis. In: Kher KK, Schnaper HW, Makker SP, eds. Clinical Pediatric Nephrology, 2 nd ed. Abingdon: Informa Health Care; 2007: 539.