HEMATURIA AND MICROHEMATURIA IN CHILDREN Macroscopic gross hematuria
- Slides: 14
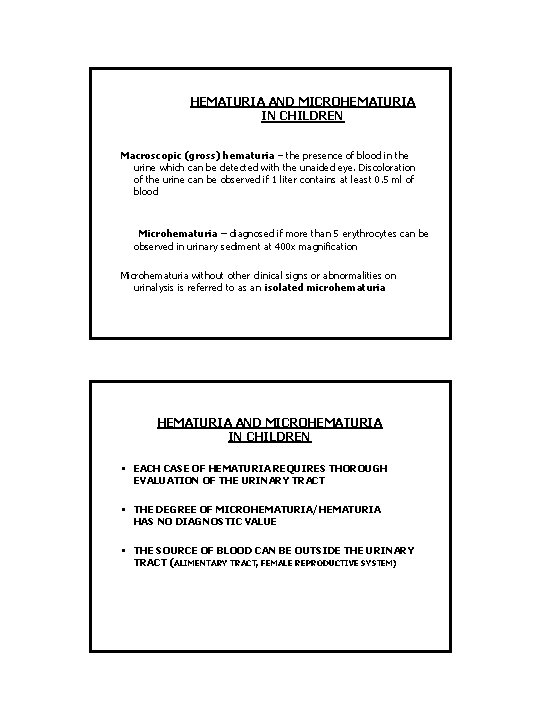
HEMATURIA AND MICROHEMATURIA IN CHILDREN Macroscopic (gross) hematuria – the presence of blood in the urine which can be detected with the unaided eye. Discoloration of the urine can be observed if 1 liter contains at least 0. 5 ml of blood Microhematuria – diagnosed if more than 5 erythrocytes can be observed in urinary sediment at 400 x magnification Microhematuria without other clinical signs or abnormalities on urinalysis is referred to as an isolated microhematuria HEMATURIA AND MICROHEMATURIA IN CHILDREN • EACH CASE OF HEMATURIA REQUIRES THOROUGH EVALUATION OF THE URINARY TRACT • THE DEGREE OF MICROHEMATURIA/HEMATURIA HAS NO DIAGNOSTIC VALUE • THE SOURCE OF BLOOD CAN BE OUTSIDE THE URINARY TRACT (ALIMENTARY TRACT, FEMALE REPRODUCTIVE SYSTEM)
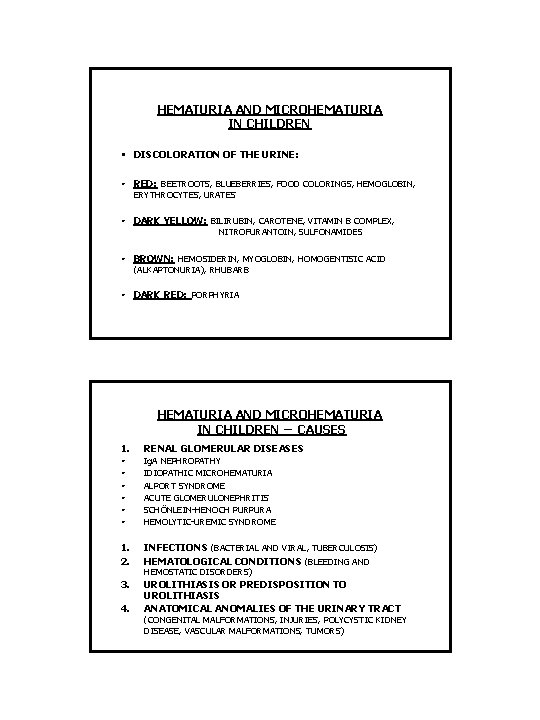
HEMATURIA AND MICROHEMATURIA IN CHILDREN • DISCOLORATION OF THE URINE: • RED: BEETROOTS, BLUEBERRIES, FOOD COLORINGS, HEMOGLOBIN, • DARK YELLOW: BILIRUBIN, CAROTENE, VITAMIN B COMPLEX, ERYTHROCYTES, URATES NITROFURANTOIN, SULFONAMIDES • BROWN: HEMOSIDERIN, MYOGLOBIN, HOMOGENTISIC ACID • DARK RED: PORPHYRIA (ALKAPTONURIA), RHUBARB HEMATURIA AND MICROHEMATURIA IN CHILDREN – CAUSES 1. RENAL GLOMERULAR DISEASES • • • Ig. A NEPHROPATHY IDIOPATHIC MICROHEMATURIA ALPORT SYNDROME ACUTE GLOMERULONEPHRITIS SCHÖNLEIN-HENOCH PURPURA HEMOLYTIC-UREMIC SYNDROME 1. 2. INFECTIONS (BACTERIAL AND VIRAL, TUBERCULOSIS) HEMATOLOGICAL CONDITIONS (BLEEDING AND 3. UROLITHIASIS OR PREDISPOSITION TO UROLITHIASIS ANATOMICAL ANOMALIES OF THE URINARY TRACT 4. HEMOSTATIC DISORDERS) (CONGENITAL MALFORMATIONS, INJURIES, POLYCYSTIC KIDNEY DISEASE, VASCULAR MALFORMATIONS, TUMORS)
HEMATURIA AND MICROHEMATURIA IN CHILDREN – EVALUATION 1. History: • • Diseases of the skeletal system, endocrinopathies, hematological diseases and clotting disorders, alimentary tract disorders, heart defects, diseases of the urinary tract, arterial hypertension, tuberculosis, hearing disorders and visual impairment, infectious diseases, used medications Family history – abovementioned conditions + urolithiasis, microhematuria, mortality due to kidney diseases, mortality due to arterial hypertension 2. Physical examination: • Skin • • • Abdomen and parenchymal organs Vision and hearing Arterial blood pressure HEMATURIA AND MICROHEMATURIA IN CHILDREN – EVALUATION 3. Basic laboratory tests: • Complete blood count + peripheral smear + platelet count • • • Coagulation profile Creatinine Uric acid Complete ionogram Gasometry Bilirubin and transaminases, HBV and HCV profile ASO Urinalysis + urine sediment; creatinine Tuberculin sensitivity test Abdominal ultrasound with thorough evaluation of the urinary bladder wall
HEMOGLOBINURIA AND MYOGLOBINURIA • HEMOGLOBINURIA CAN BE ASSOCIATED WITH INTRAVASCULAR HEMOLYSIS OR HEMATURIA, IF URINALYSIS WAS NOT CONDUCTED SHORTLY AFTER URINE SAMPLING • MYOGLOBINURIA CAN BE ASSOCIATED WITH CRUSH INJURIES, INTENSIVE PHYSICAL EXERCISE, SEIZURES, FEVER, DISEASES OF MUSCLES, AND METABOLIC DISORDERS • LABORATORY TESTS 1. 2. DIRECT METHODS INDIRECT METHODS: DETERMINATION OF PIGMENT’S ORIGIN, e. g. low value of blood urea nitrogen/creatinine ratio (creatinine is released from destroyed muscle cells) and high concentration of creatine phosphokinase in the case of nephropathy associated with myoglobinuria PROTEINURIA • • Proteinuria, especially albuminuria, is frequently an initial sign of progressive nephropathy. Microalbuminuria can be a manifestation of systemic endothelial dysfunction predisposing to the development of nephropathy. DEFINITION: • Proteinuria is diagnosed whenever the amount of protein in 4 urine samples exceeds 4 mg/m 2/hour, i. e. 100 -200 mg/day depending on age, or the protein to creatinine ratio (mg/mg) in the first morning urine sample is higher than 0. 25
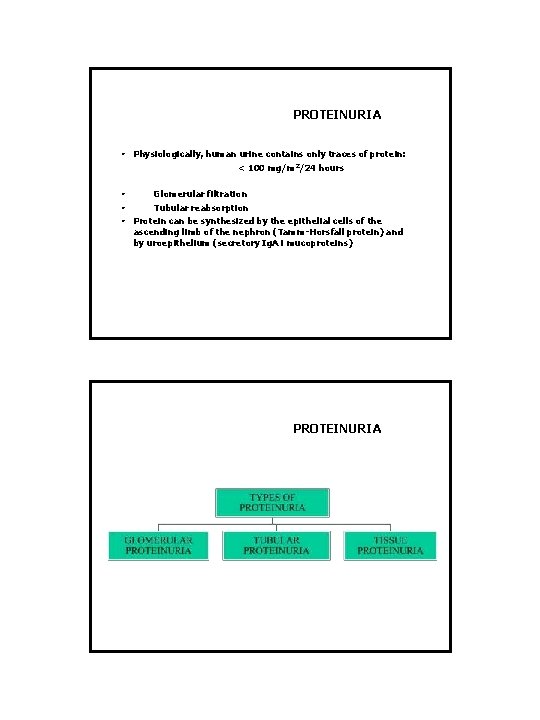
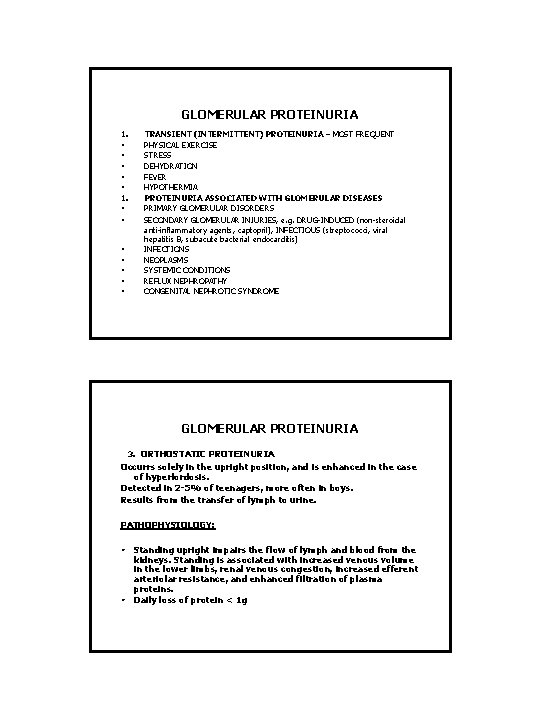
PROTEINURIA • Physiologically, human urine contains only traces of protein: < 100 mg/m 2/24 hours • • • Glomerular filtration Tubular reabsorption Protein can be synthesized by the epithelial cells of the ascending limb of the nephron (Tamm-Horsfall protein) and by uroepithelium (secretory Ig. A i mucoproteins) PROTEINURIA
GLOMERULAR PROTEINURIA 1. • • • • TRANSIENT (INTERMITTENT) PROTEINURIA – MOST FREQUENT PHYSICAL EXERCISE STRESS DEHYDRATION FEVER HYPOTHERMIA PROTEINURIA ASSOCIATED WITH GLOMERULAR DISEASES PRIMARY GLOMERULAR DISORDERS SECONDARY GLOMERULAR INJURIES, e. g. DRUG-INDUCED (non-steroidal anti-inflammatory agents, captopril), INFECTIOUS (streptococci, viral hepatitis B, subacute bacterial endocarditis) INFECTIONS NEOPLASMS SYSTEMIC CONDITIONS REFLUX NEPHROPATHY CONGENITAL NEPHROTIC SYNDROME GLOMERULAR PROTEINURIA 3. ORTHOSTATIC PROTEINURIA Occurrs solely in the upright position, and is enhanced in the case of hyperlordosis. Detected in 2 -5% of teenagers, more often in boys. Results from the transfer of lymph to urine. PATHOPHYSIOLOGY: • • Standing upright impairs the flow of lymph and blood from the kidneys. Standing is associated with increased venous volume in the lower limbs, renal venous congestion, increased efferent arteriolar resistance, and enhanced filtration of plasma proteins. Daily loss of protein < 1 g
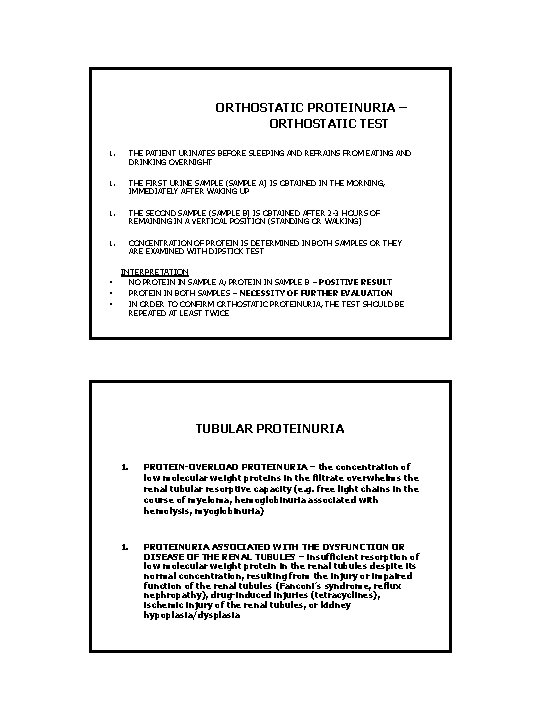
ORTHOSTATIC PROTEINURIA – ORTHOSTATIC TEST 1. THE PATIENT URINATES BEFORE SLEEPING AND REFRAINS FROM EATING AND DRINKING OVERNIGHT 1. THE FIRST URINE SAMPLE (SAMPLE A) IS OBTAINED IN THE MORNING, IMMEDIATELY AFTER WAKING UP 1. THE SECOND SAMPLE (SAMPLE B) IS OBTAINED AFTER 2 -3 HOURS OF REMAINING IN A VERTICAL POSITION (STANDING OR WALKING) 1. CONCENTRATION OF PROTEIN IS DETERMINED IN BOTH SAMPLES OR THEY ARE EXAMINED WITH DIPSTICK TEST INTERPRETATION • • • NO PROTEIN IN SAMPLE A; PROTEIN IN SAMPLE B – POSITIVE RESULT PROTEIN IN BOTH SAMPLES – NECESSITY OF FURTHER EVALUATION IN ORDER TO CONFIRM ORTHOSTATIC PROTEINURIA, THE TEST SHOULD BE REPEATED AT LEAST TWICE TUBULAR PROTEINURIA 1. PROTEIN-OVERLOAD PROTEINURIA – the concentration of low molecular weight proteins in the filtrate overwhelms the renal tubular resorptive capacity (e. g. free light chains in the course of myeloma, hemoglobinuria associated with hemolysis, myoglobinuria) 1. PROTEINURIA ASSOCIATED WITH THE DYSFUNCTION OR DISEASE OF THE RENAL TUBULES – insufficient resorption of low molecular weight protein in the renal tubules despite its normal concentration, resulting from the injury or impaired function of the renal tubules (Fanconi’s syndrome, reflux nephropathy), drug-induced injuries (tetracyclines), ischemic injury of the renal tubules, or kidney hypoplasia/dysplasia
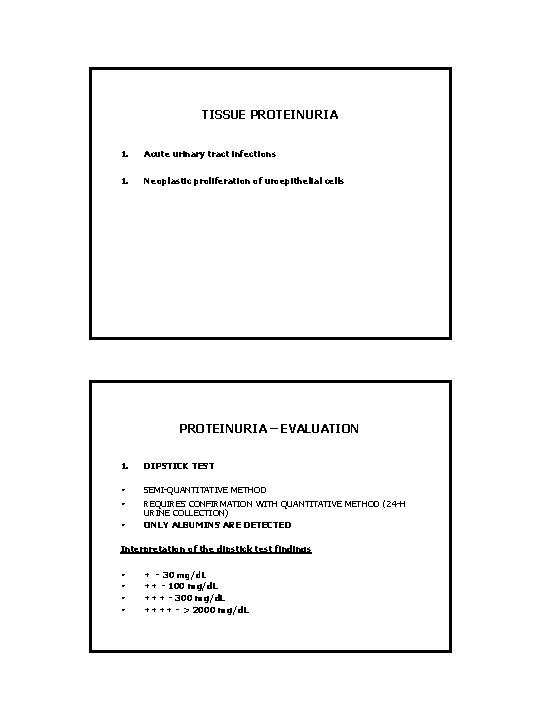
TISSUE PROTEINURIA 1. Acute urinary tract infections 1. Neoplastic proliferation of uroepithelial cells PROTEINURIA – EVALUATION 1. DIPSTICK TEST • • SEMI-QUANTITATIVE METHOD REQUIRES CONFIRMATION WITH QUANTITATIVE METHOD (24 -H URINE COLLECTION) ONLY ALBUMINS ARE DETECTED • Interpretation of the dipstick test findings • • + - 30 mg/d. L ++ - 100 mg/d. L +++ - 300 mg/d. L ++++ - > 2000 mg/d. L
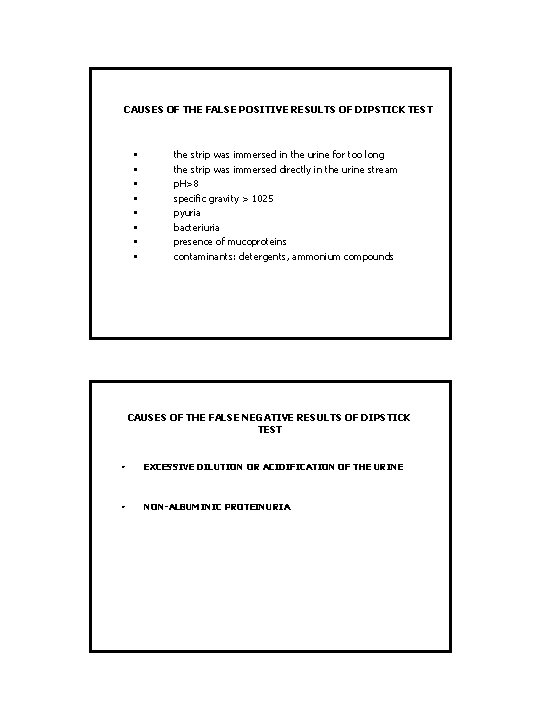
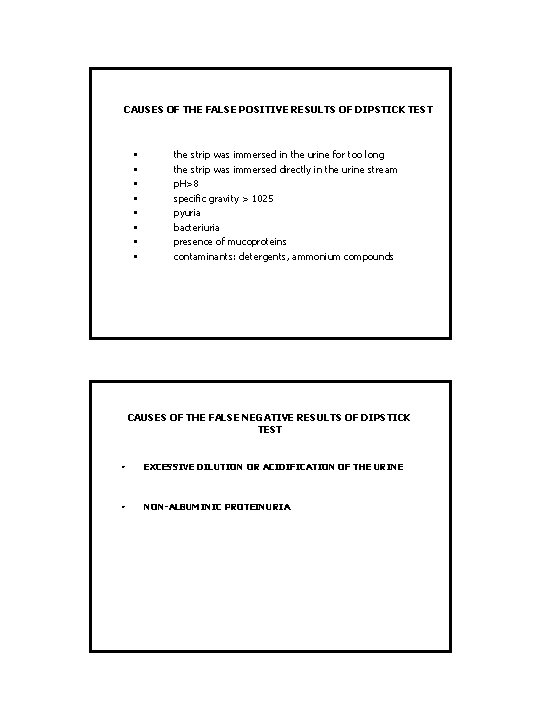
CAUSES OF THE FALSE POSITIVE RESULTS OF DIPSTICK TEST • • the strip was immersed in the urine for too long the strip was immersed directly in the urine stream p. H>8 specific gravity > 1025 pyuria bacteriuria presence of mucoproteins contaminants: detergents, ammonium compounds CAUSES OF THE FALSE NEGATIVE RESULTS OF DIPSTICK TEST • EXCESSIVE DILUTION OR ACIDIFICATION OF THE URINE • NON-ALBUMINIC PROTEINURIA
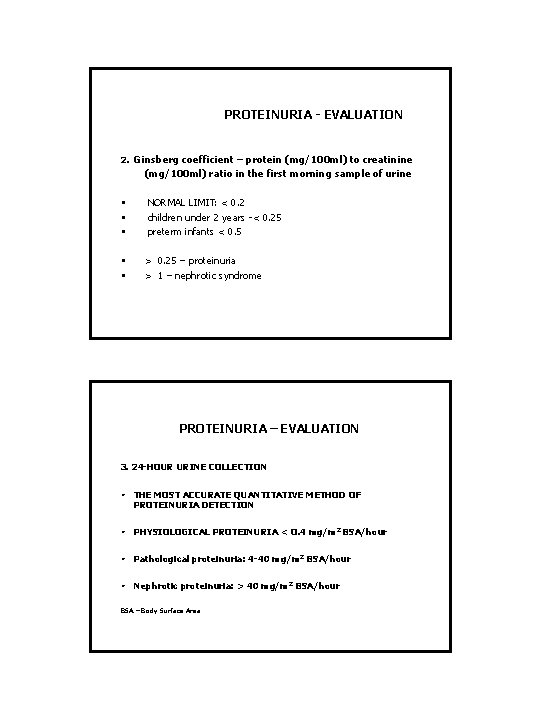
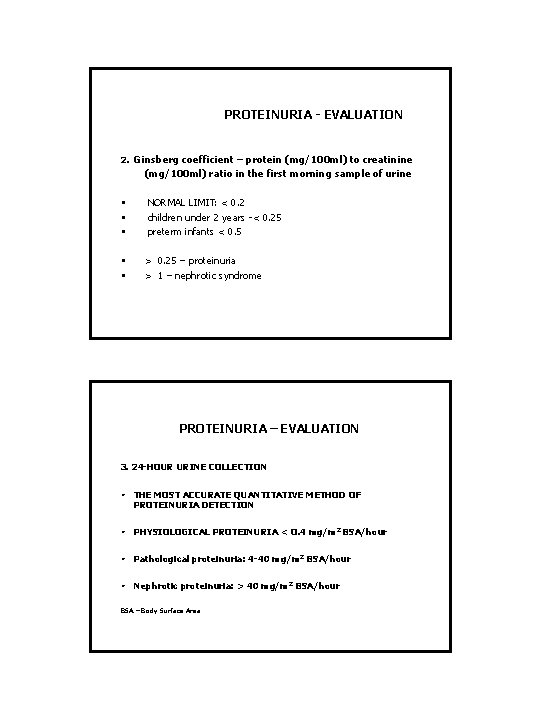
PROTEINURIA - EVALUATION . 2 Ginsberg coefficient – protein (mg/100 ml) to creatinine (mg/100 ml) ratio in the first morning sample of urine • • • NORMAL LIMIT: < 0. 2 children under 2 years -< 0. 25 preterm infants < 0. 5 > 0. 25 – proteinuria > 1 – nephrotic syndrome PROTEINURIA – EVALUATION 3. 24 -HOUR URINE COLLECTION • THE MOST ACCURATE QUANTITATIVE METHOD OF PROTEINURIA DETECTION • PHYSIOLOGICAL PROTEINURIA < O. 4 mg/m 2 BSA/hour • Pathological proteinuria: 4 -40 mg/m 2 BSA/hour • Nephrotic proteinuria: > 40 mg/m 2 BSA/hour BSA – Body Surface Area
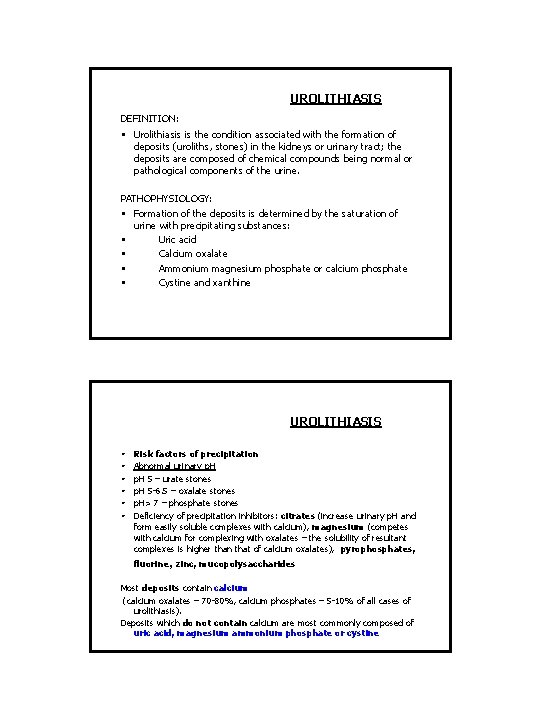
UROLITHIASIS DEFINITION: • Urolithiasis is the condition associated with the formation of deposits (uroliths, stones) in the kidneys or urinary tract; the deposits are composed of chemical compounds being normal or pathological components of the urine. PATHOPHYSIOLOGY: • Formation of the deposits is determined by the saturation of urine with precipitating substances: • Uric acid • Calcium oxalate • Ammonium magnesium phosphate or calcium phosphate • Cystine and xanthine UROLITHIASIS • • • Risk factors of precipitation Abnormal urinary p. H 5 – urate stones p. H 5 -6. 5 – oxalate stones p. H> 7 – phosphate stones Deficiency of precipitation inhibitors: citrates (increase urinary p. H and form easily soluble complexes with calcium), magnesium (competes with calcium for complexing with oxalates – the solubility of resultant complexes is higher than that of calcium oxalates), pyrophosphates, fluorine, zinc, mucopolysaccharides Most deposits contain calcium (calcium oxalates – 70 -80%, calcium phosphates – 5 -10% of all cases of urolithiasis). Deposits which do not contain calcium are most commonly composed of uric acid, magnesium ammonium phosphate or cystine
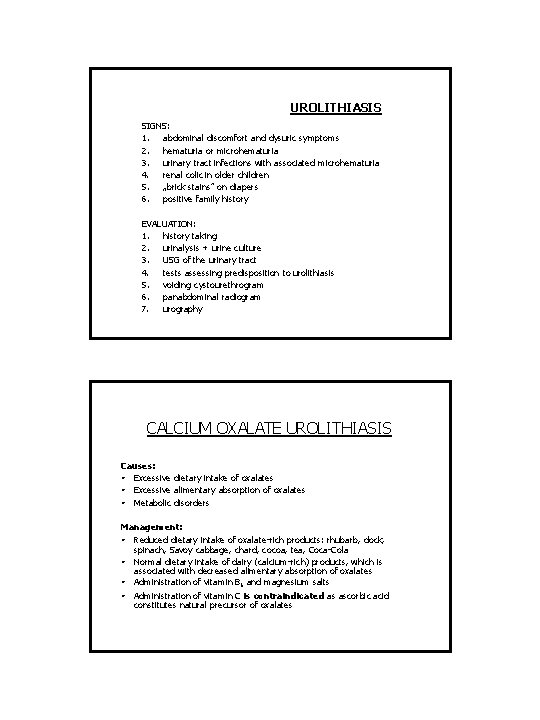
UROLITHIASIS SIGNS: 1. abdominal discomfort and dysuric symptoms 2. hematuria or microhematuria 3. urinary tract infections with associated microhematuria 4. renal colic in older children 5. „brick stains” on diapers 6. positive family history EVALUATION: 1. history taking 2. urinalysis + urine culture 3. USG of the urinary tract 4. tests assessing predisposition to urolithiasis 5. voiding cystourethrogram 6. panabdominal radiogram 7. urography CALCIUM OXALATE UROLITHIASIS Causes: • Excessive dietary intake of oxalates • Excessive alimentary absorption of oxalates • Metabolic disorders Management: • Reduced dietary intake of oxalate-rich products: rhubarb, dock, spinach, Savoy cabbage, chard, cocoa, tea, Coca-Cola • Normal dietary intake of dairy (calcium-rich) products, which is associated with decreased alimentary absorption of oxalates • Administration of vitamin B 6 and magnesium salts • Administration of vitamin C is contraindicated as ascorbic acid constitutes natural precursor of oxalates
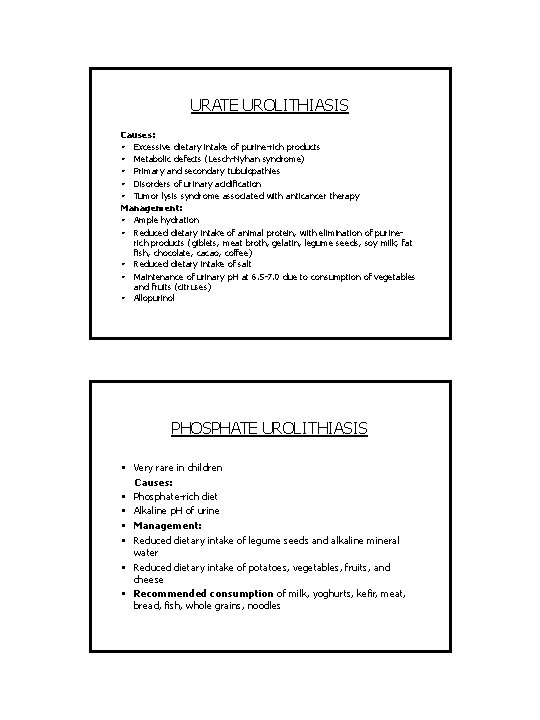
URATE UROLITHIASIS Causes: • Excessive dietary intake of purine-rich products • Metabolic defects (Lesch-Nyhan syndrome) • Primary and secondary tubulopathies • Disorders of urinary acidification • Tumor lysis syndrome associated with anticancer therapy Management: • Ample hydration • Reduced dietary intake of animal protein, with elimination of purinerich products (giblets, meat broth, gelatin, legume seeds, soy milk, fat fish, chocolate, cacao, coffee) • Reduced dietary intake of salt • Maintenance of urinary p. H at 6. 5 -7. 0 due to consumption of vegetables and fruits (citruses) • Allopurinol PHOSPHATE UROLITHIASIS • Very rare in children Causes: • Phosphate-rich diet • Alkaline p. H of urine • Management: • Reduced dietary intake of legume seeds and alkaline mineral water • Reduced dietary intake of potatoes, vegetables, fruits, and cheese • Recommended consumption of milk, yoghurts, kefir, meat, bread, fish, whole grains, noodles
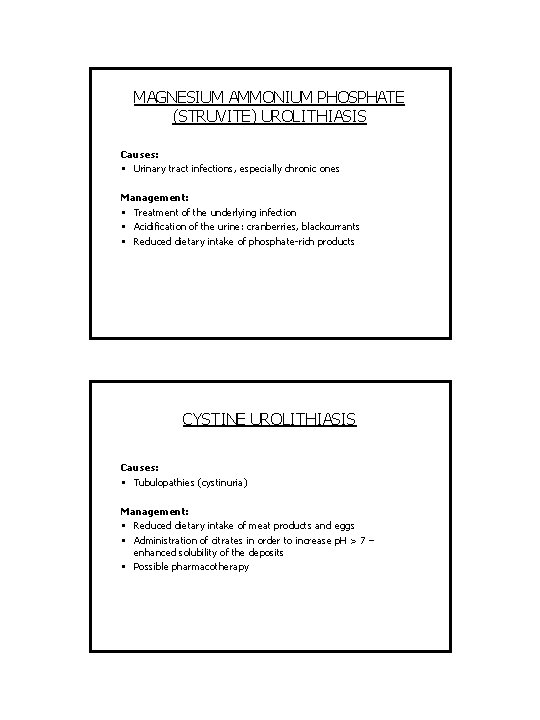
MAGNESIUM AMMONIUM PHOSPHATE (STRUVITE) UROLITHIASIS Causes: • Urinary tract infections, especially chronic ones Management: • Treatment of the underlying infection • Acidification of the urine: cranberries, blackcurrants • Reduced dietary intake of phosphate-rich products CYSTINE UROLITHIASIS Causes: • Tubulopathies (cystinuria) Management: • Reduced dietary intake of meat products and eggs • Administration of citrates in order to increase p. H > 7 – enhanced solubility of the deposits • Possible pharmacotherapy
 Macroscopic hematuria causes
Macroscopic hematuria causes Icd 10 code for microhematuria
Icd 10 code for microhematuria Kriteria npv
Kriteria npv Hemoglobinuria vs hematuria
Hemoglobinuria vs hematuria Fountain valley hematuria
Fountain valley hematuria Eritrocitos isomorficos
Eritrocitos isomorficos Hematuria
Hematuria Hematuria
Hematuria Hematuria causes
Hematuria causes Anuria disuria poliuria oliguria hematuria
Anuria disuria poliuria oliguria hematuria Hemoglucosa
Hemoglucosa Hematuria ex vacuo
Hematuria ex vacuo Dr donald lamm
Dr donald lamm Macroscopic momentum balance
Macroscopic momentum balance Overall mechanical energy balance
Overall mechanical energy balance