Thoracic Ultrasound for Pulmonologists Interventional Pulmonology Course The



































- Slides: 85
Thoracic Ultrasound for Pulmonologists Interventional Pulmonology Course - The 24 th Year Lahey Clinic, Burlington, Boston, USA Mar 27 – 31, 2007 Highlights by Dr Arthur CW Lau








Introduction • Didactic lectures (AM) • Hands-on lab sessions (PM)
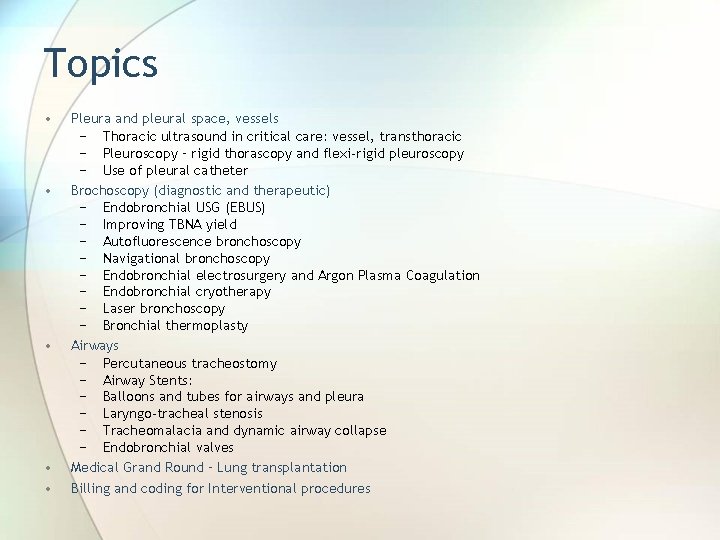
Topics • • • Pleura and pleural space, vessels − Thoracic ultrasound in critical care: vessel, transthoracic − Pleuroscopy – rigid thorascopy and flexi-rigid pleuroscopy − Use of pleural catheter Brochoscopy (diagnostic and therapeutic) − Endobronchial USG (EBUS) − Improving TBNA yield − Autofluorescence bronchoscopy − Navigational bronchoscopy − Endobronchial electrosurgery and Argon Plasma Coagulation − Endobronchial cryotherapy − Laser bronchoscopy − Bronchial thermoplasty Airways − Percutaneous tracheostomy − Airway Stents: − Balloons and tubes for airways and pleura − Laryngo-tracheal stenosis − Tracheomalacia and dynamic airway collapse − Endobronchial valves Medical Grand Round – Lung transplantation Billing and coding for Interventional procedures

Harvard University
Pleura and pleural space Ultrasound

Thoracic ultrasound in critical care • Transthoracic −curvilinear • Vessel −linear
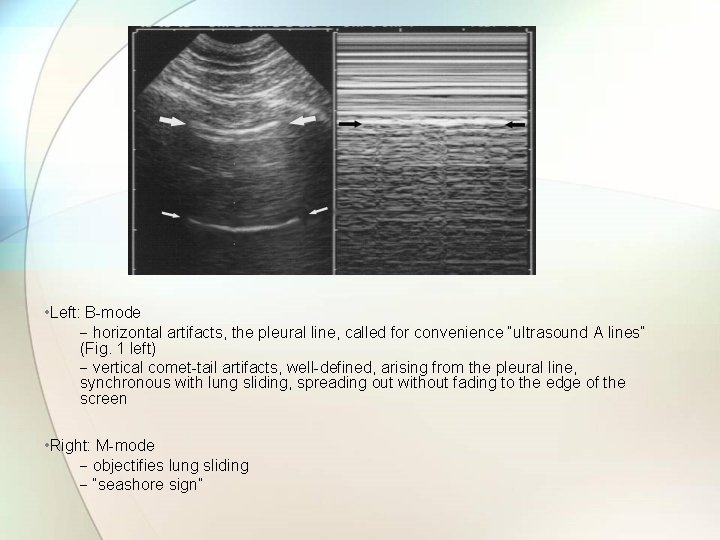
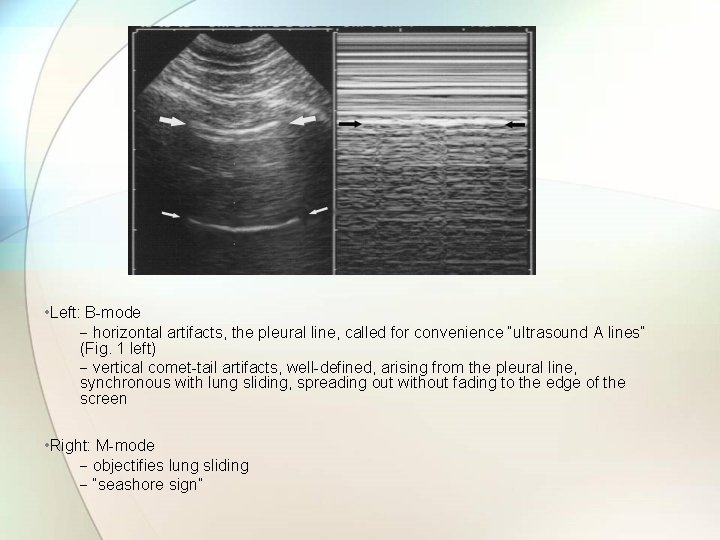
• Left: B-mode − horizontal artifacts, the pleural line, called for convenience “ultrasound A lines” (Fig. 1 left) − vertical comet-tail artifacts, well-defined, arising from the pleural line, synchronous with lung sliding, spreading out without fading to the edge of the screen • Right: M-mode − objectifies lung sliding − “seashore sign”
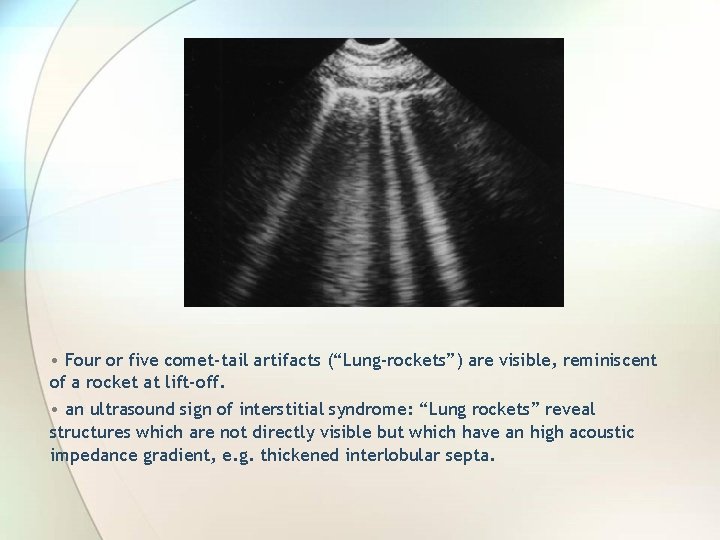
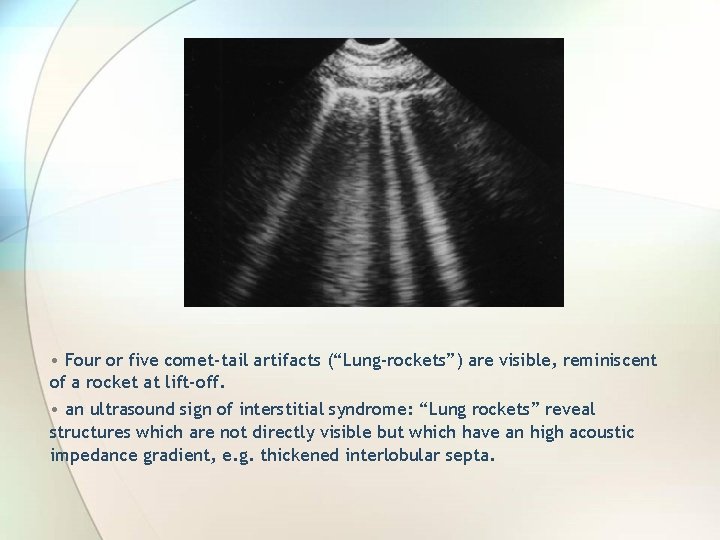
• Four or five comet-tail artifacts (“Lung-rockets”) are visible, reminiscent of a rocket at lift-off. • an ultrasound sign of interstitial syndrome: “Lung rockets” reveal structures which are not directly visible but which have an high acoustic impedance gradient, e. g. thickened interlobular septa.
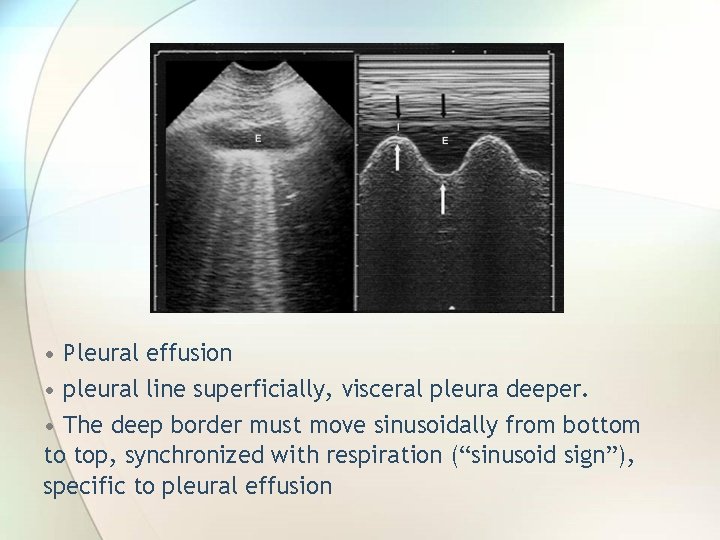
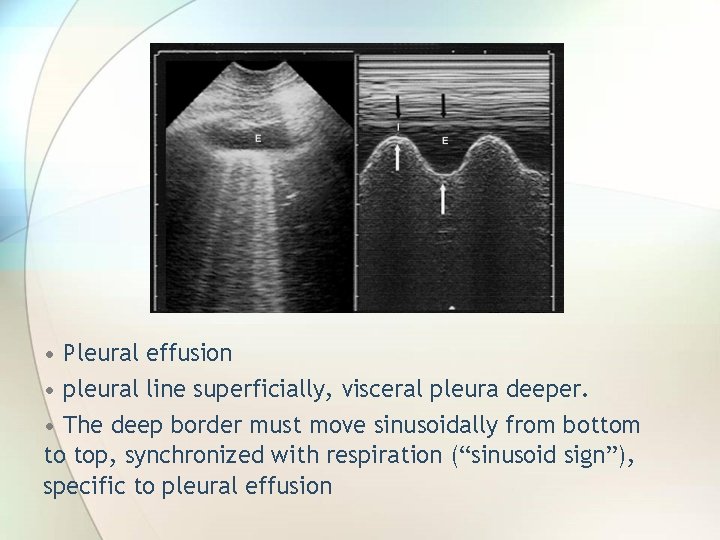
• Pleural effusion • pleural line superficially, visceral pleura deeper. • The deep border must move sinusoidally from bottom to top, synchronized with respiration (“sinusoid sign”), specific to pleural effusion
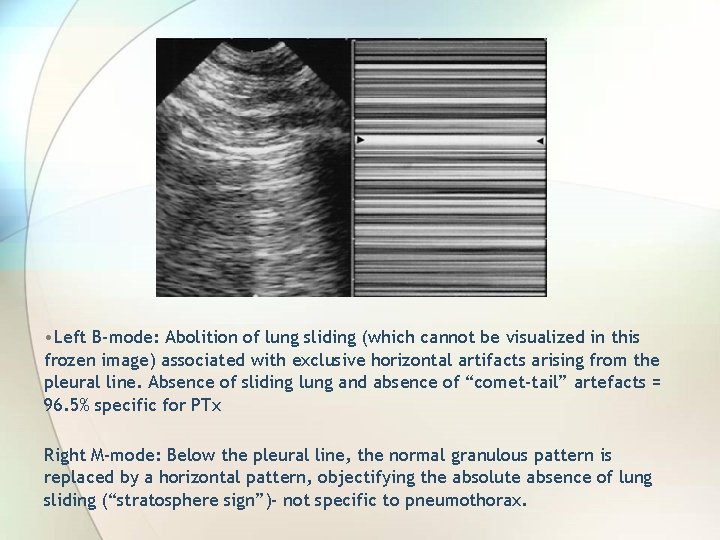
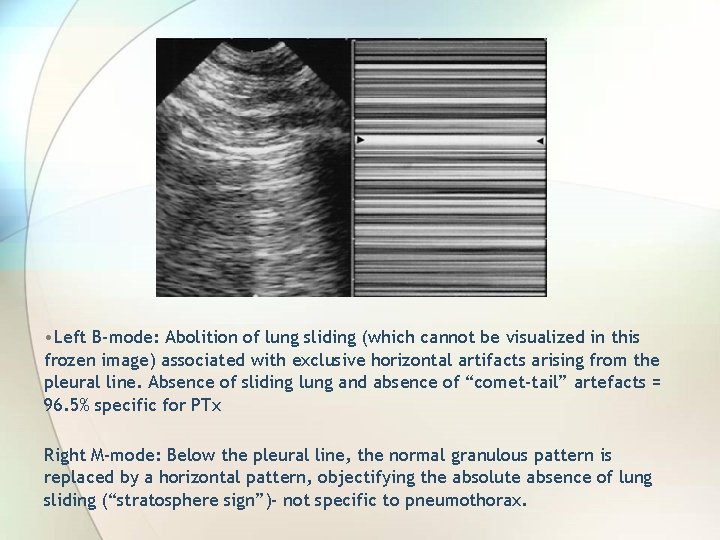
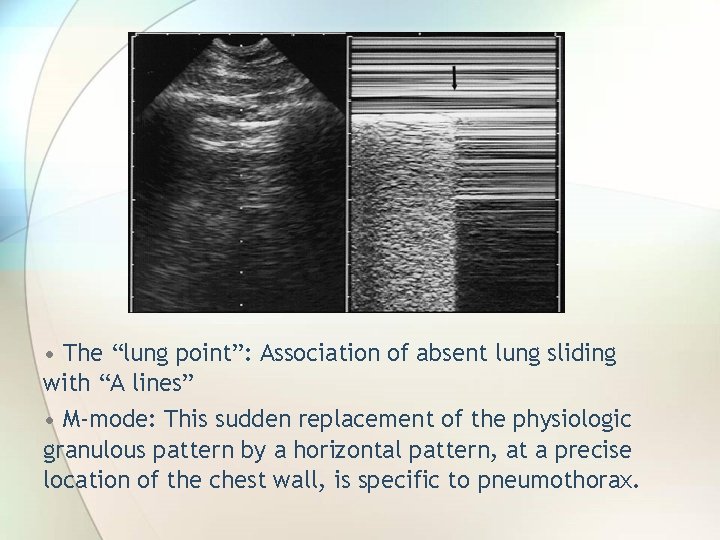
• Left B-mode: Abolition of lung sliding (which cannot be visualized in this frozen image) associated with exclusive horizontal artifacts arising from the pleural line. Absence of sliding lung and absence of “comet-tail” artefacts = 96. 5% specific for PTx Right M-mode: Below the pleural line, the normal granulous pattern is replaced by a horizontal pattern, objectifying the absolute absence of lung sliding (“stratosphere sign”)- not specific to pneumothorax.
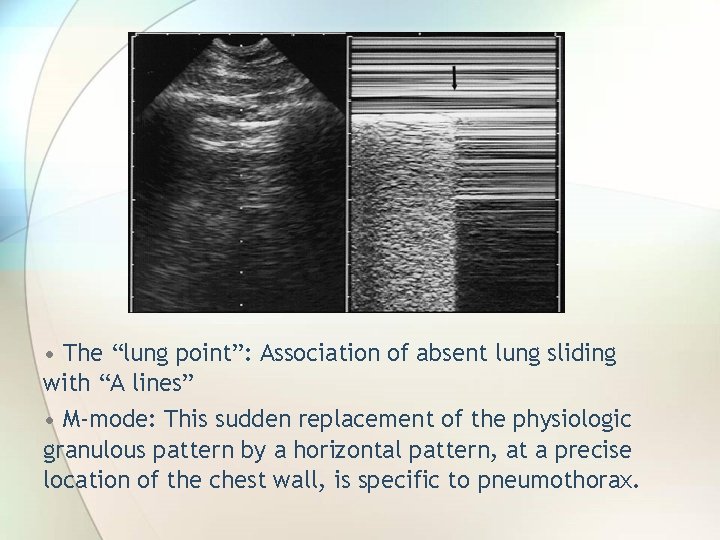
• The “lung point”: Association of absent lung sliding with “A lines” • M-mode: This sudden replacement of the physiologic granulous pattern by a horizontal pattern, at a precise location of the chest wall, is specific to pneumothorax.
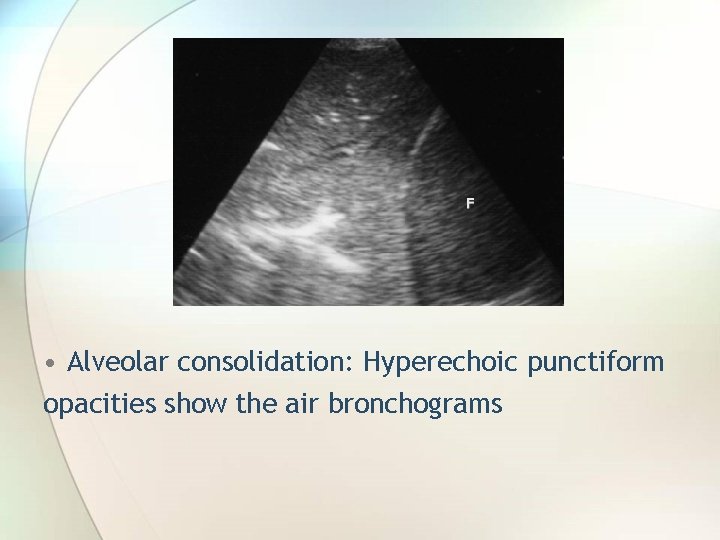
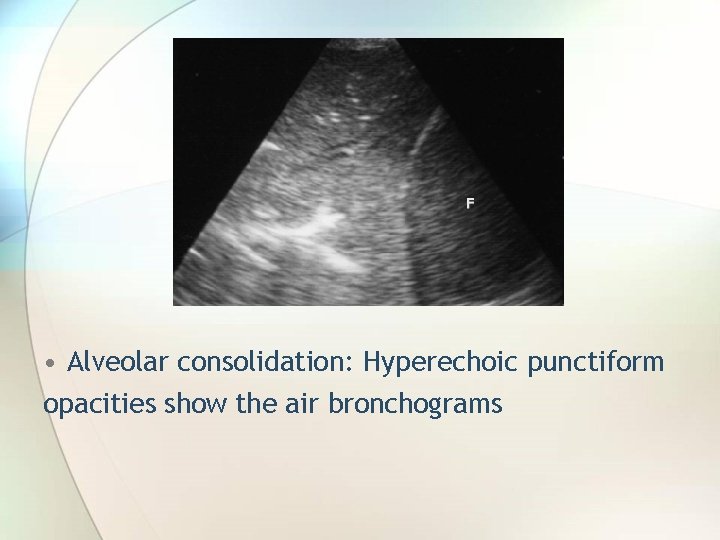
• Alveolar consolidation: Hyperechoic punctiform opacities show the air bronchograms
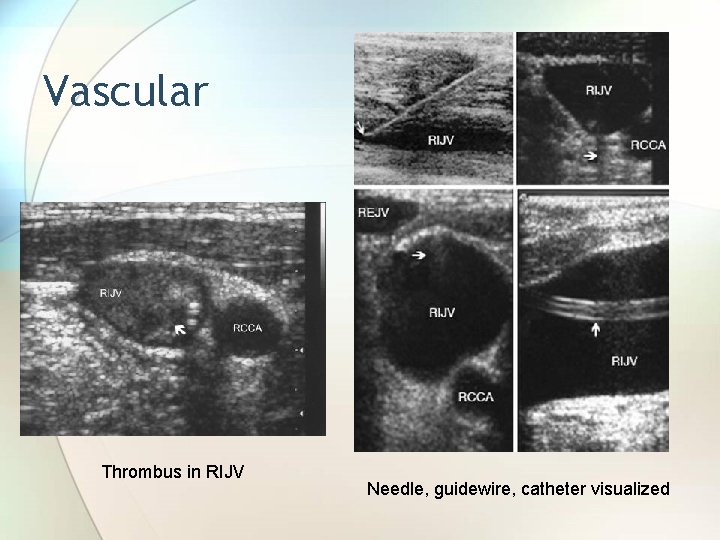
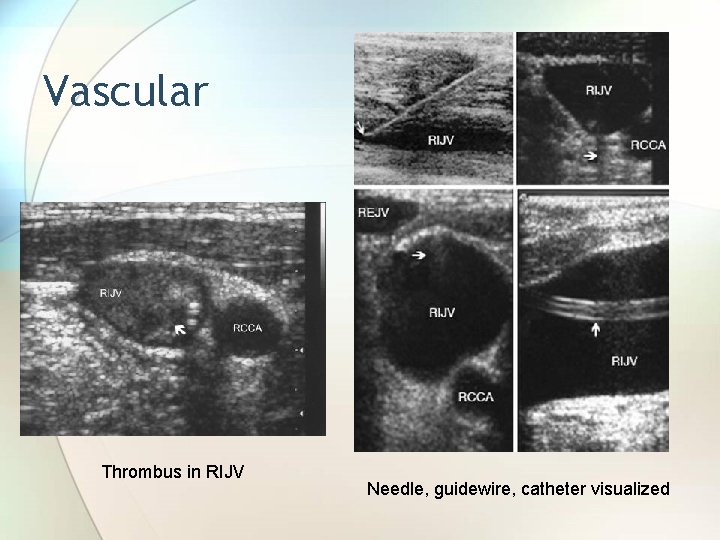
Vascular Thrombus in RIJV Needle, guidewire, catheter visualized
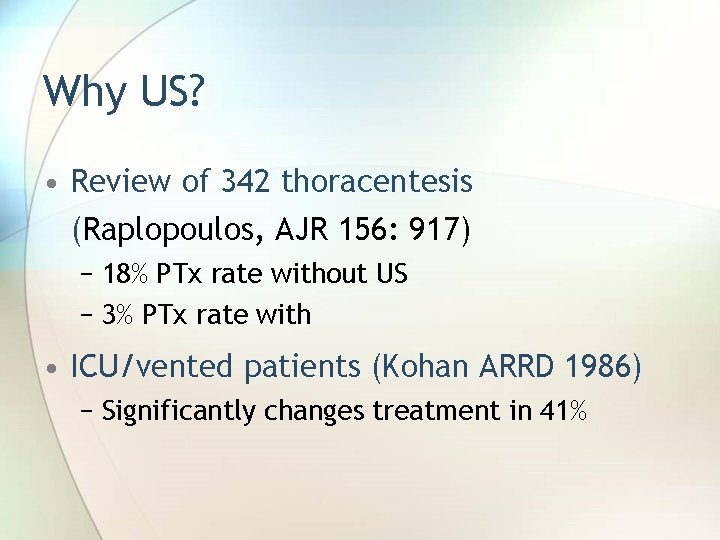
Why US? • Review of 342 thoracentesis (Raplopoulos, AJR 156: 917) − 18% PTx rate without US − 3% PTx rate with • ICU/vented patients (Kohan ARRD 1986) − Significantly changes treatment in 41%
Vessels • IVC (distensibility index >12% predicted fluid responsiveness) – Feissel ICM 2004 • Echocardiography − Changes Mx in 34 – 64% • USG-guided central line placement − Position, thrombus
Endoscopic ultrasound (EUS) • To image and access beyond the mucosa of the GI tract for dx and staging • First described in Japan in 1988 • Use radial or linear probes • EUS with FNA for lung cancer staging: − Left lobe of liver − Left adrenal − Stations (2, 4), 5, 7, 8, 9
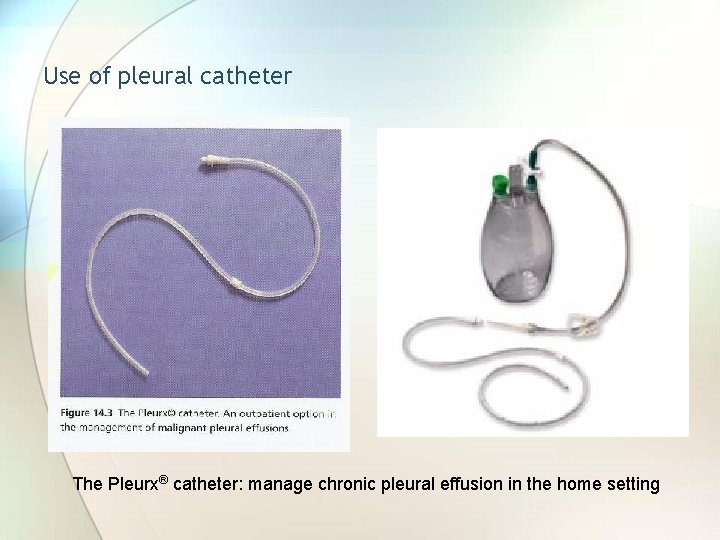
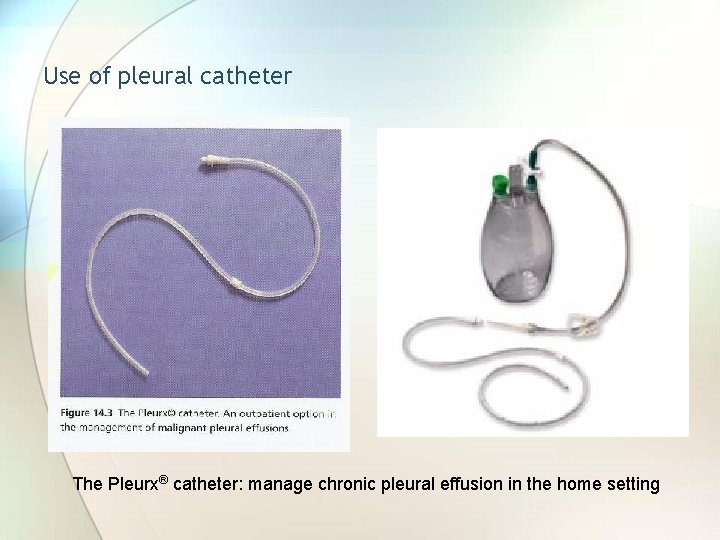
Use of pleural catheter The Pleurx® catheter: manage chronic pleural effusion in the home setting

Pleuroscopy – rigid thorascopy and flexi-rigid pleuroscopy • Rigid thoracoscope: in OR • Flexi-rigid pleuroscopy: can be done in the bronchoscopy suite under conscious sedation





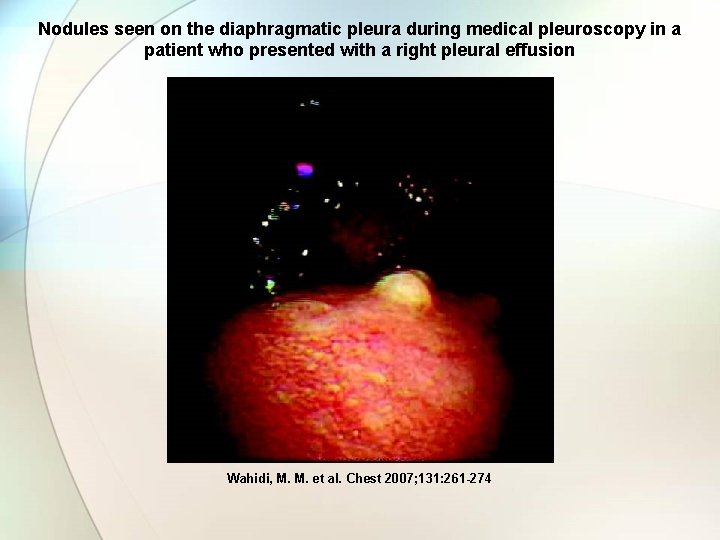
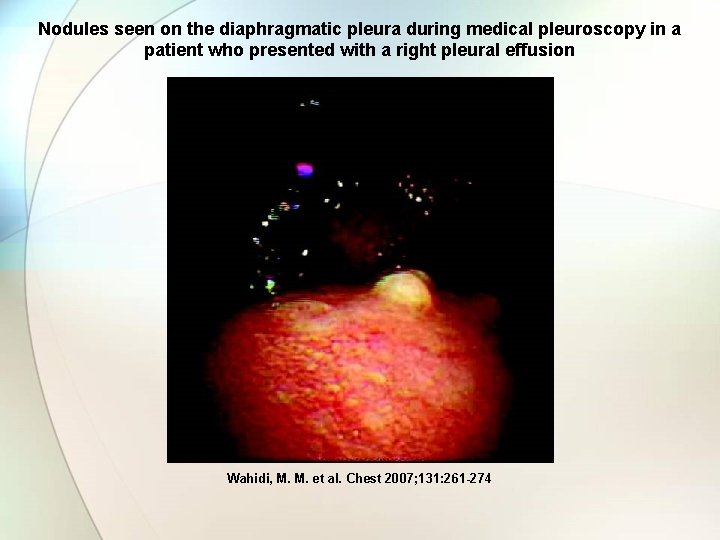
Nodules seen on the diaphragmatic pleura during medical pleuroscopy in a patient who presented with a right pleural effusion Wahidi, M. M. et al. Chest 2007; 131: 261 -274



Bronchoscopy Diagnostic and therapeutic
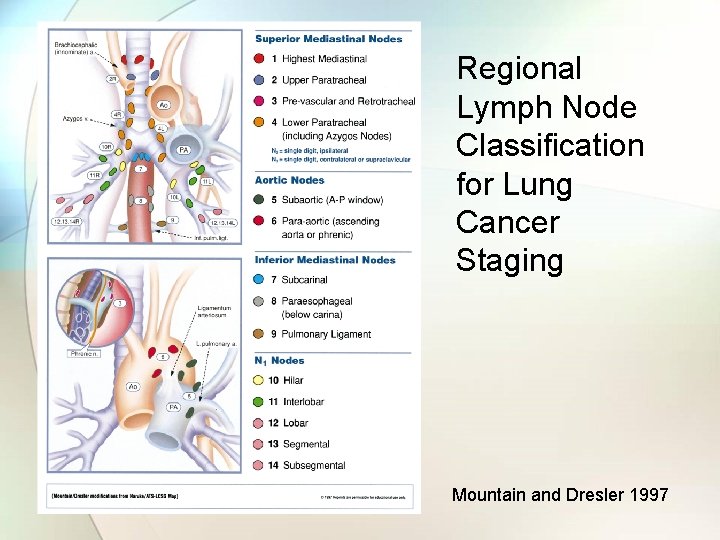
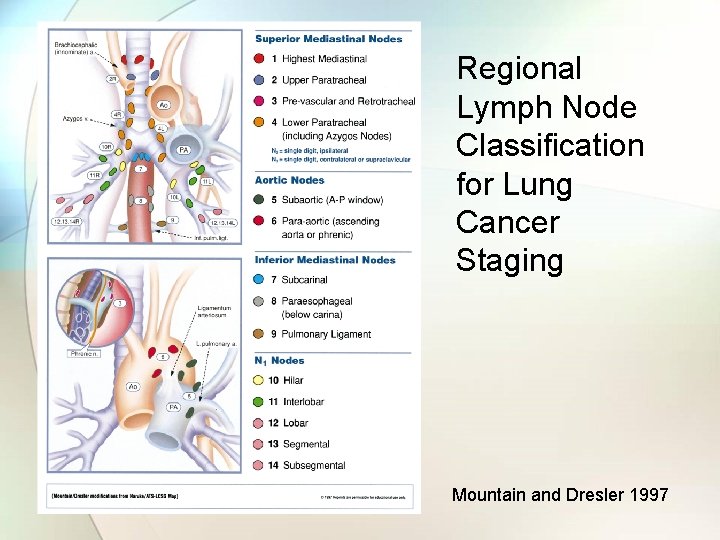
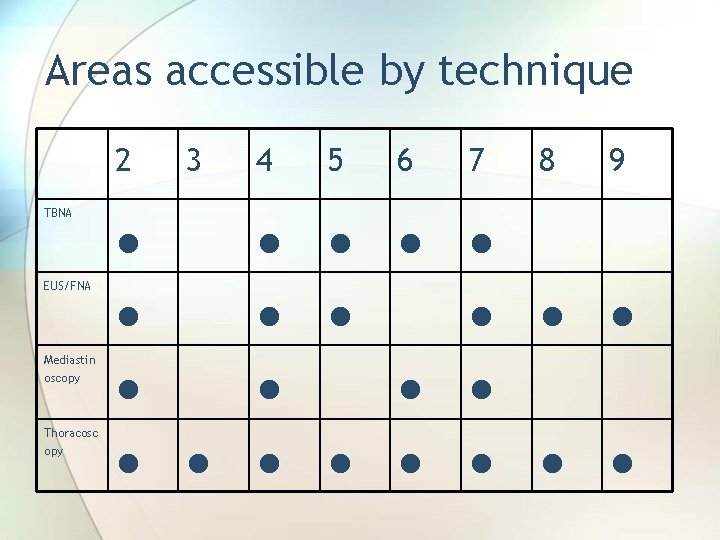
Regional Lymph Node Classification for Lung Cancer Staging Mountain and Dresler 1997
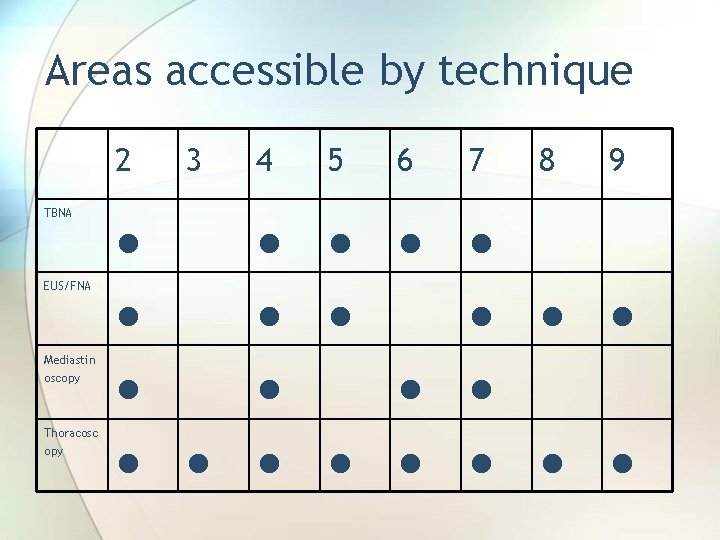
Areas accessible by technique 2 TBNA EUS/FNA Mediastin oscopy Thoracosc opy 4 5 6 7 ● ● ● 3 ● ● ● ● 8 9 ● ●
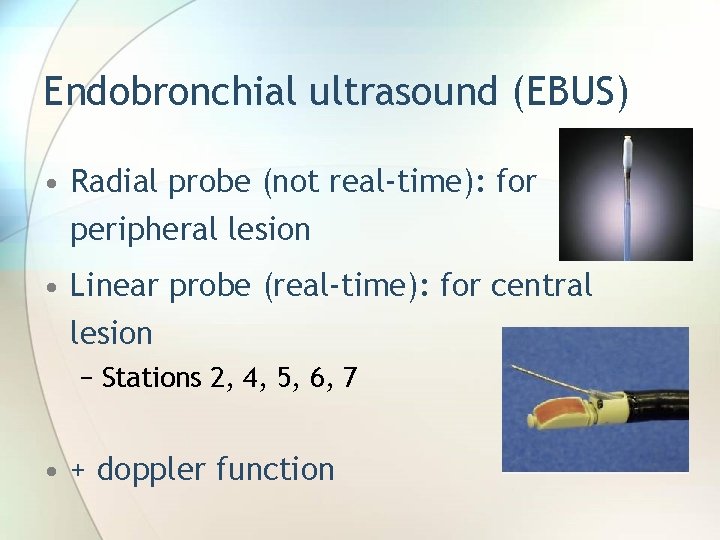
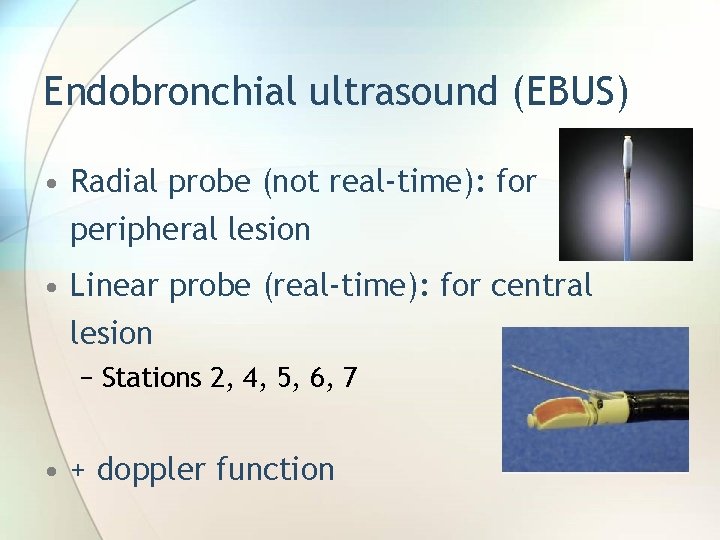
Endobronchial ultrasound (EBUS) • Radial probe (not real-time): for peripheral lesion • Linear probe (real-time): for central lesion − Stations 2, 4, 5, 6, 7 • + doppler function

Radial probe


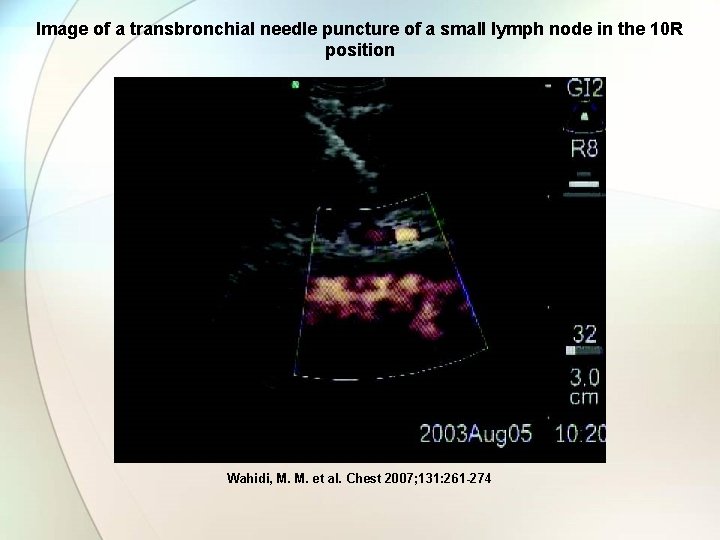
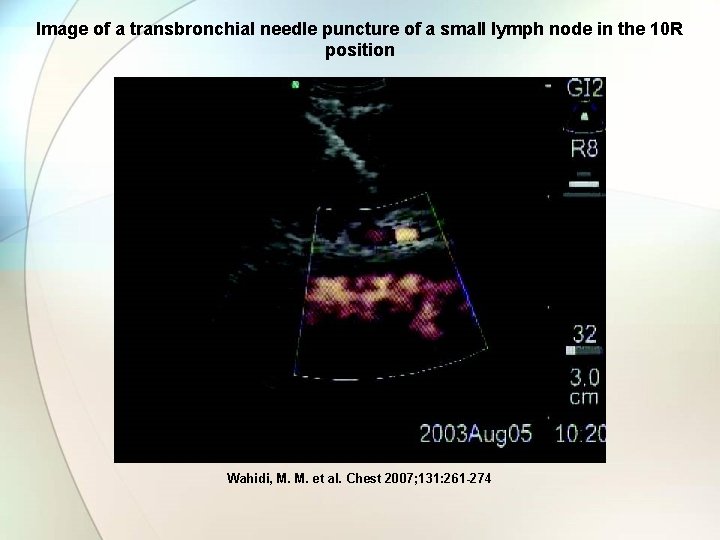
Image of a transbronchial needle puncture of a small lymph node in the 10 R position Wahidi, M. M. et al. Chest 2007; 131: 261 -274

Autofluorescence systems
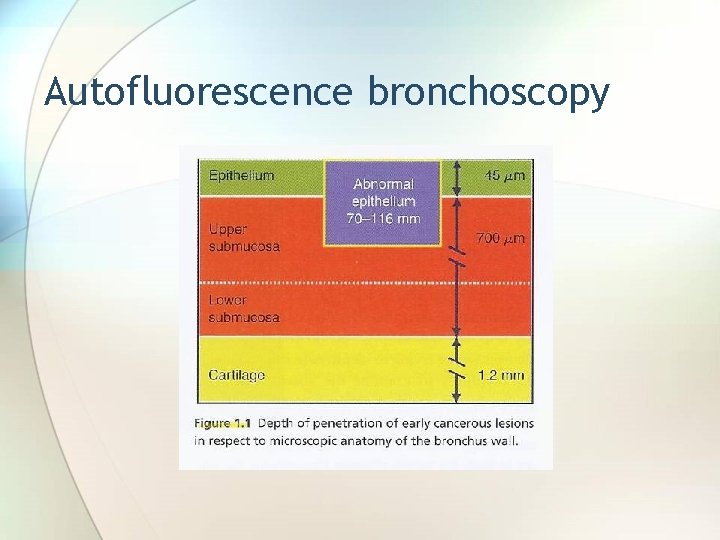
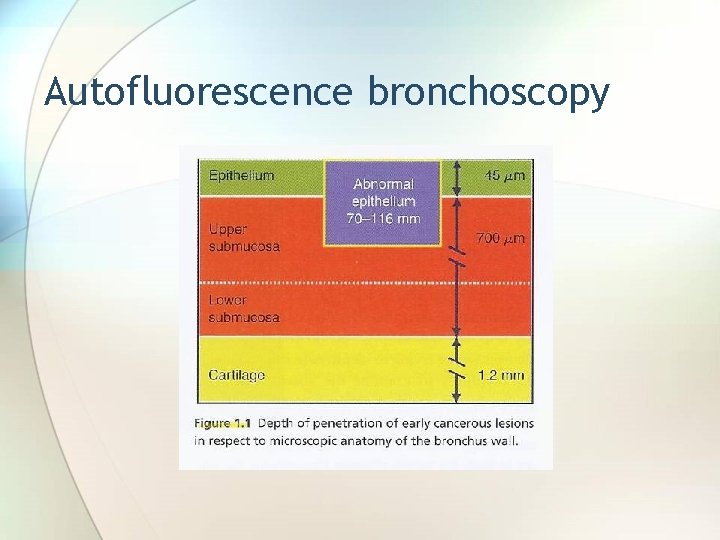
Autofluorescence bronchoscopy



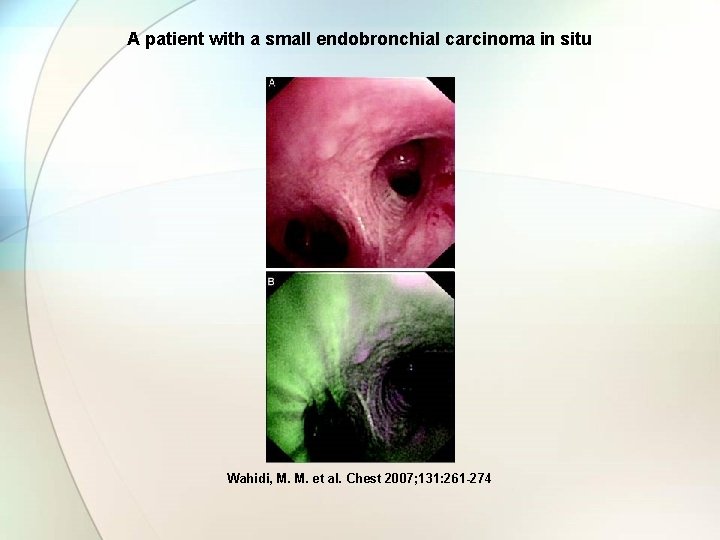
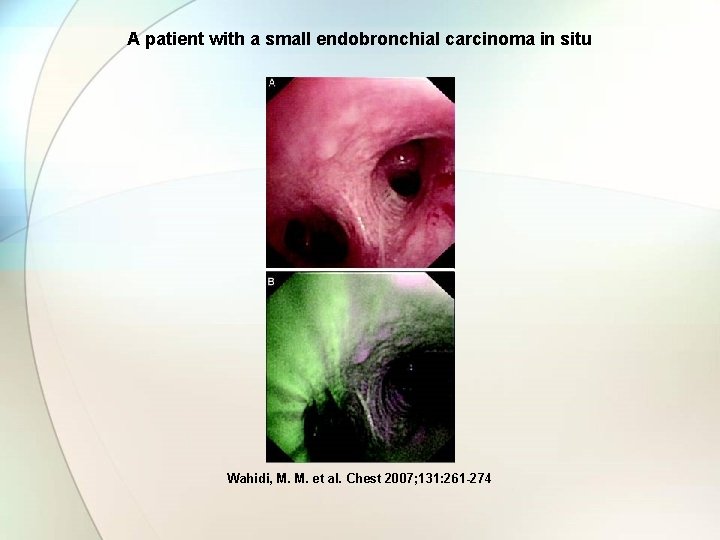
A patient with a small endobronchial carcinoma in situ Wahidi, M. M. et al. Chest 2007; 131: 261 -274
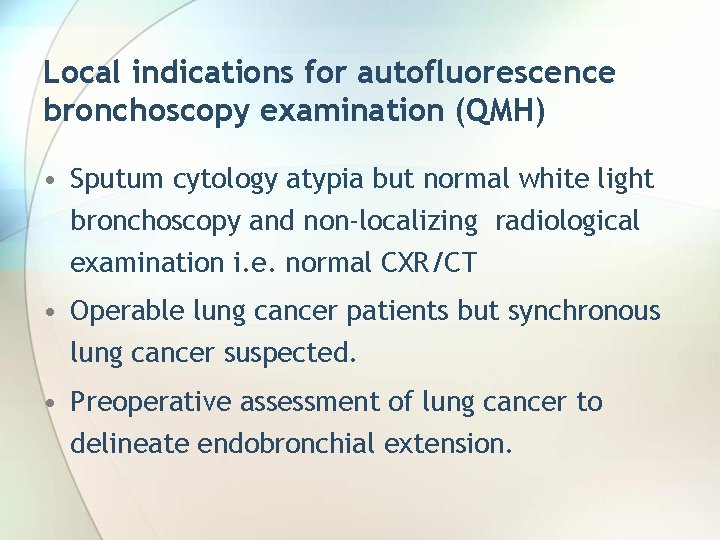
Local indications for autofluorescence bronchoscopy examination (QMH) • Sputum cytology atypia but normal white light bronchoscopy and non-localizing radiological examination i. e. normal CXR/CT • Operable lung cancer patients but synchronous lung cancer suspected. • Preoperative assessment of lung cancer to delineate endobronchial extension.
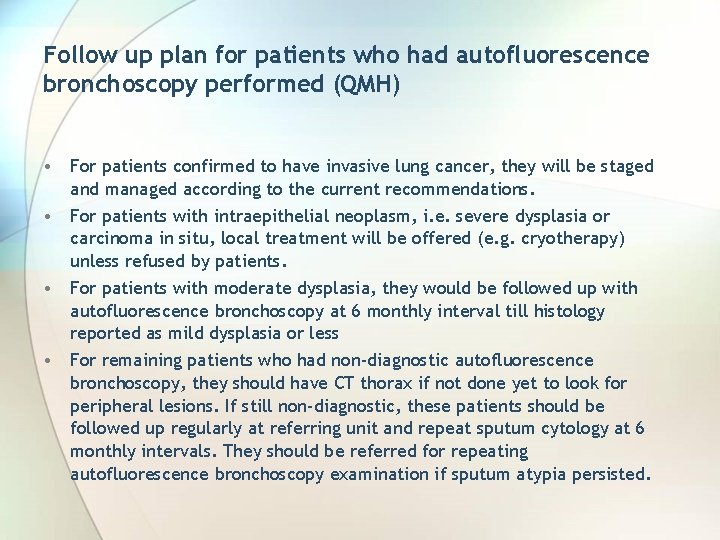
Follow up plan for patients who had autofluorescence bronchoscopy performed (QMH) • For patients confirmed to have invasive lung cancer, they will be staged and managed according to the current recommendations. • For patients with intraepithelial neoplasm, i. e. severe dysplasia or carcinoma in situ, local treatment will be offered (e. g. cryotherapy) unless refused by patients. • For patients with moderate dysplasia, they would be followed up with autofluorescence bronchoscopy at 6 monthly interval till histology reported as mild dysplasia or less • For remaining patients who had non-diagnostic autofluorescence bronchoscopy, they should have CT thorax if not done yet to look for peripheral lesions. If still non-diagnostic, these patients should be followed up regularly at referring unit and repeat sputum cytology at 6 monthly intervals. They should be referred for repeating autofluorescence bronchoscopy examination if sputum atypia persisted.

Harvard Museum of Natural History
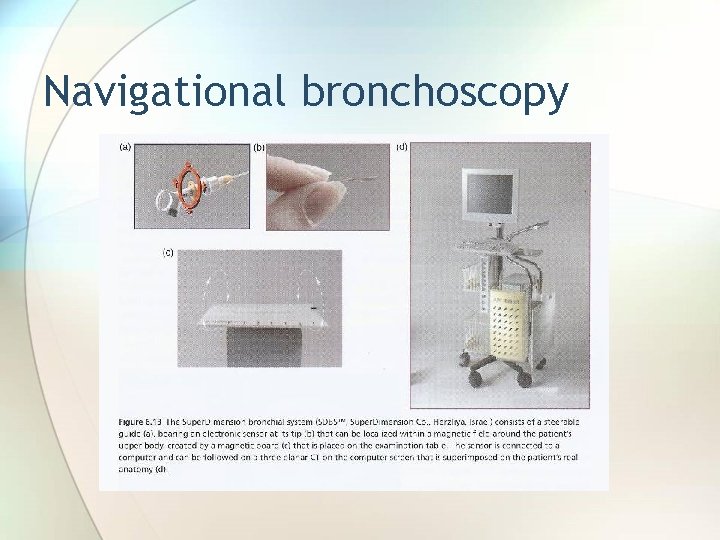
Navigational bronchoscopy
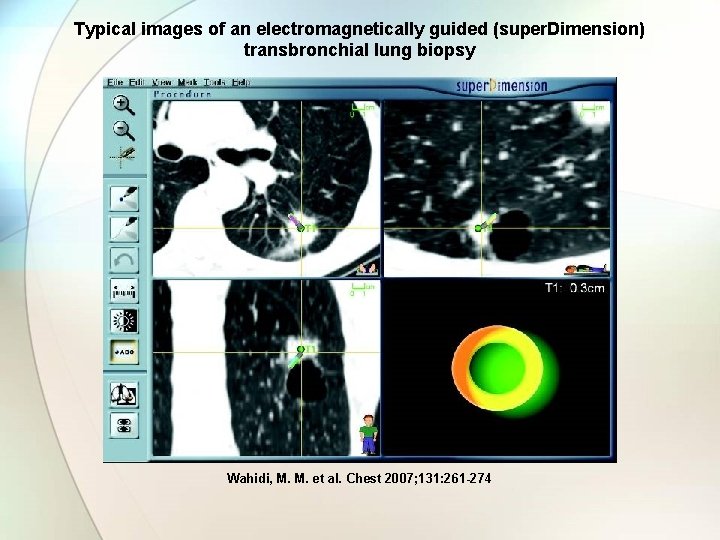
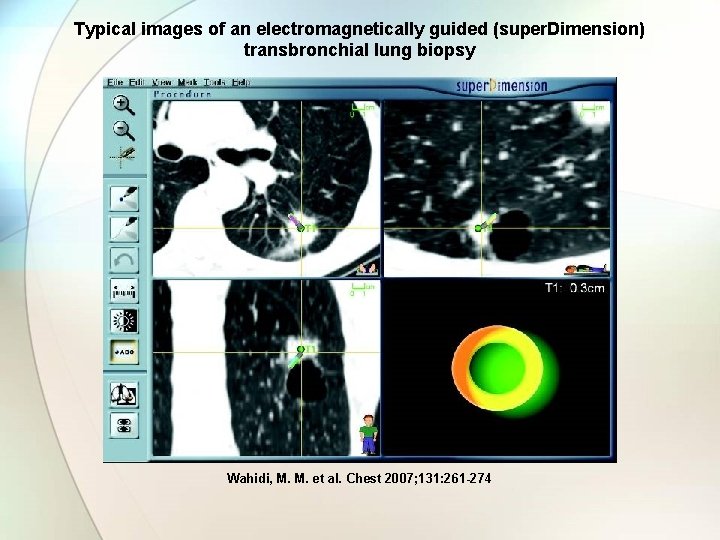
Typical images of an electromagnetically guided (super. Dimension) transbronchial lung biopsy Wahidi, M. M. et al. Chest 2007; 131: 261 -274

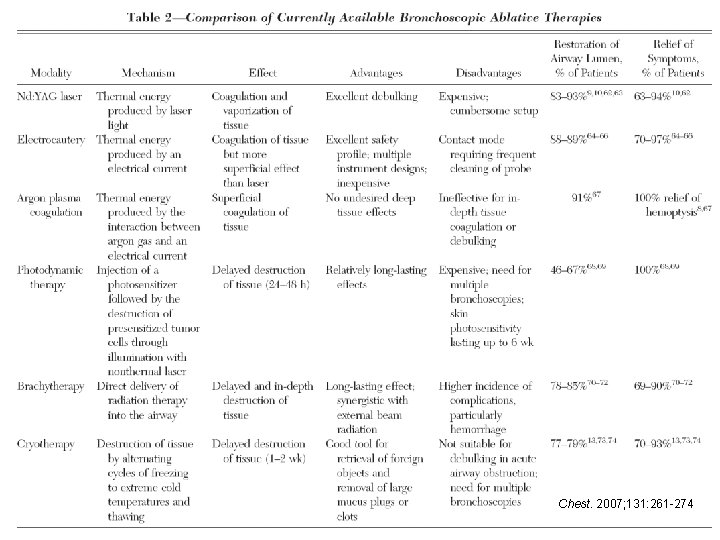
Electrosurgery • Electrocautery with • Argon Plasma Coagulation • Nd: YAG Laser • Cryotherapy
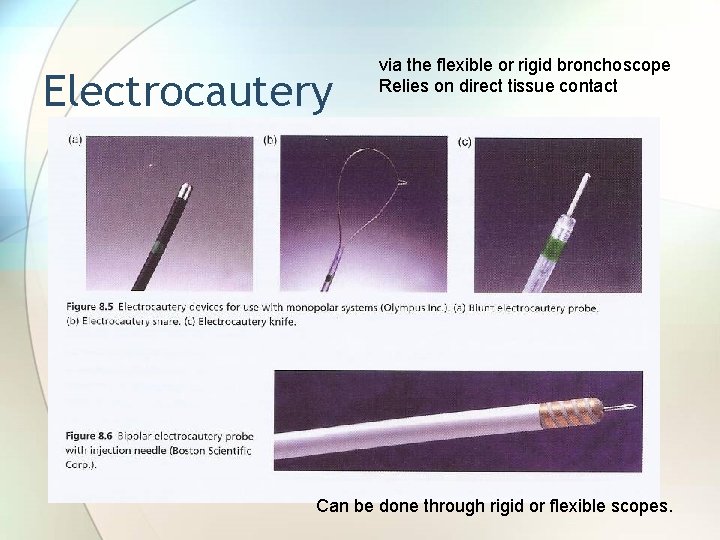
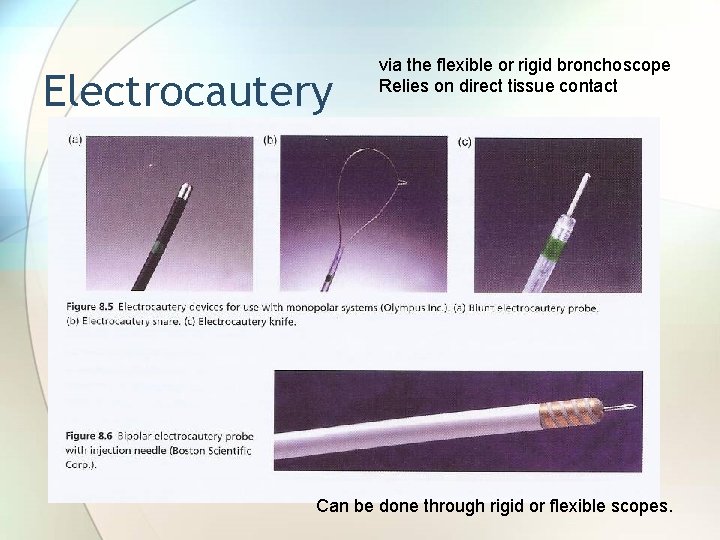
Electrocautery via the flexible or rigid bronchoscope Relies on direct tissue contact Can be done through rigid or flexible scopes.

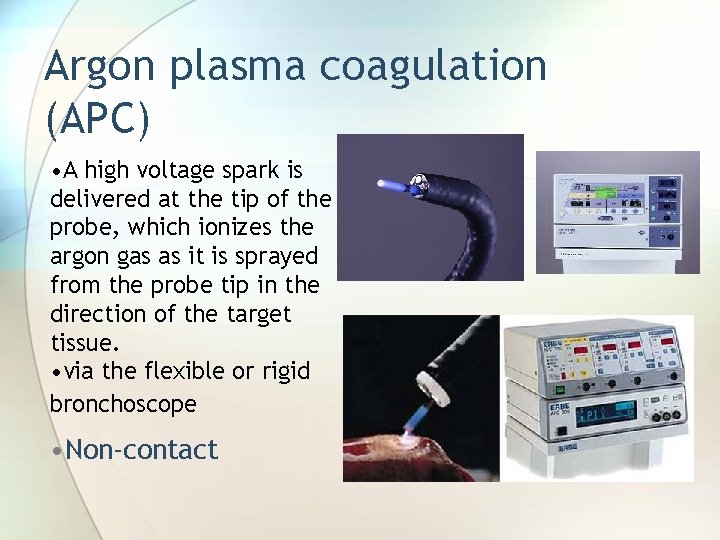
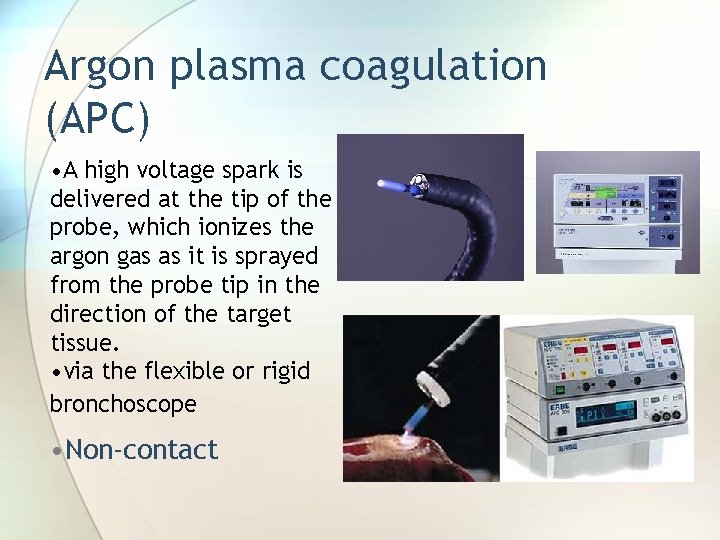
Argon plasma coagulation (APC) • A high voltage spark is delivered at the tip of the probe, which ionizes the argon gas as it is sprayed from the probe tip in the direction of the target tissue. • via the flexible or rigid bronchoscope • Non-contact
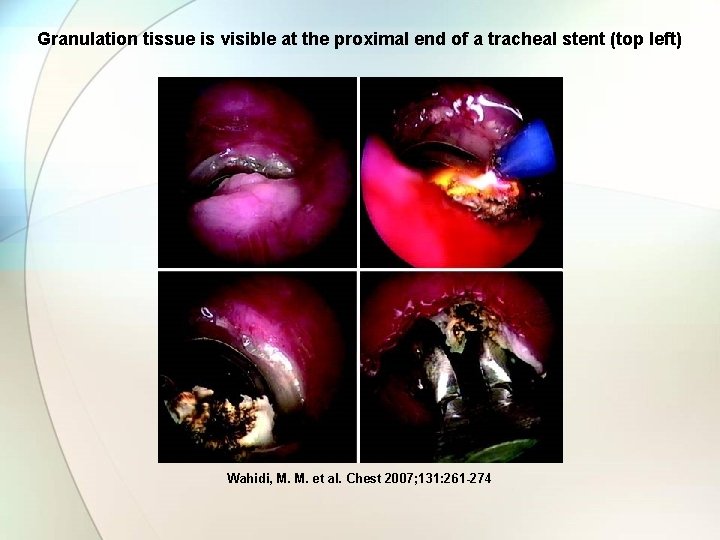
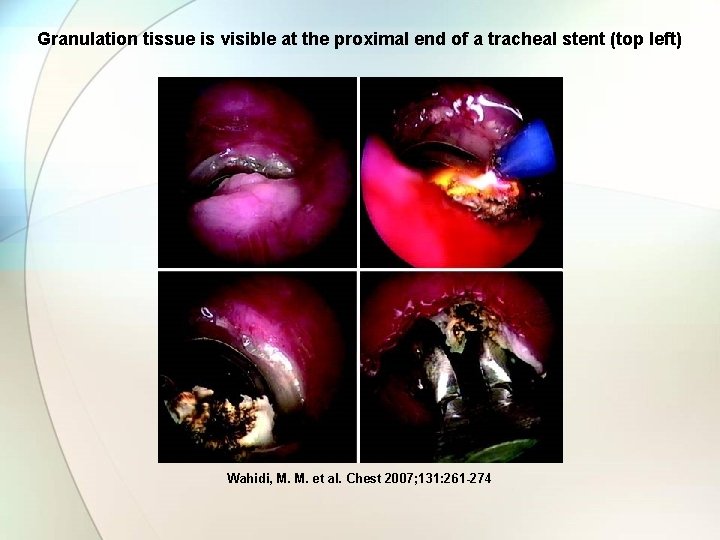
Granulation tissue is visible at the proximal end of a tracheal stent (top left) Wahidi, M. M. et al. Chest 2007; 131: 261 -274
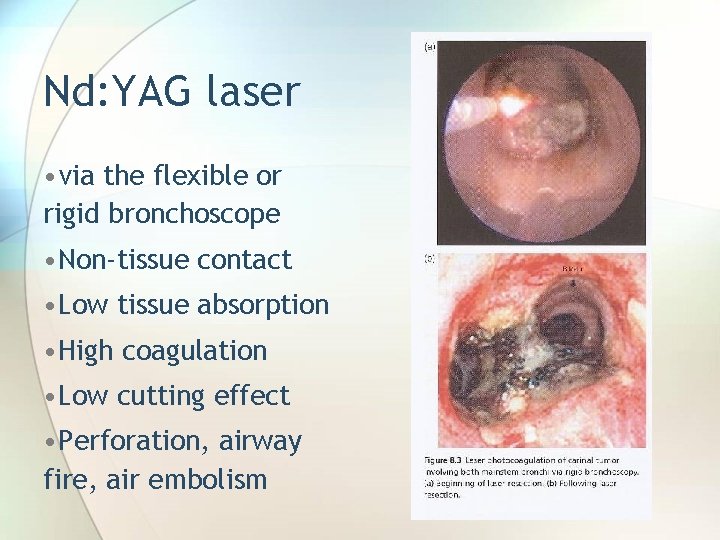
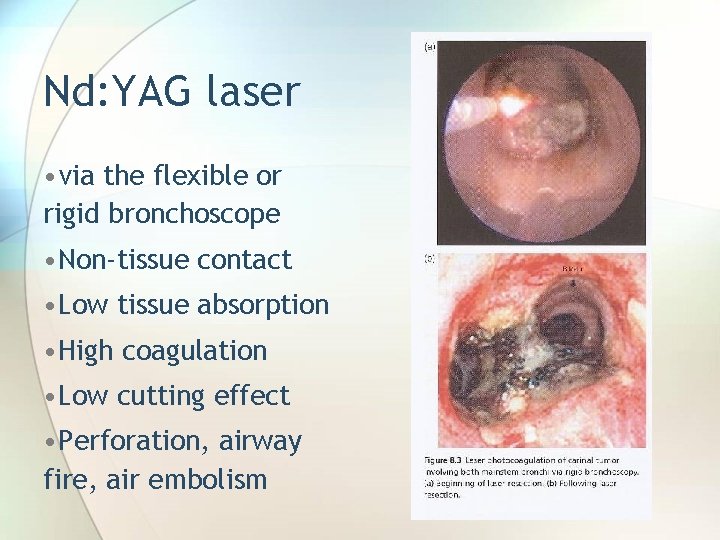
Nd: YAG laser • via the flexible or rigid bronchoscope • Non-tissue contact • Low tissue absorption • High coagulation • Low cutting effect • Perforation, airway fire, air embolism
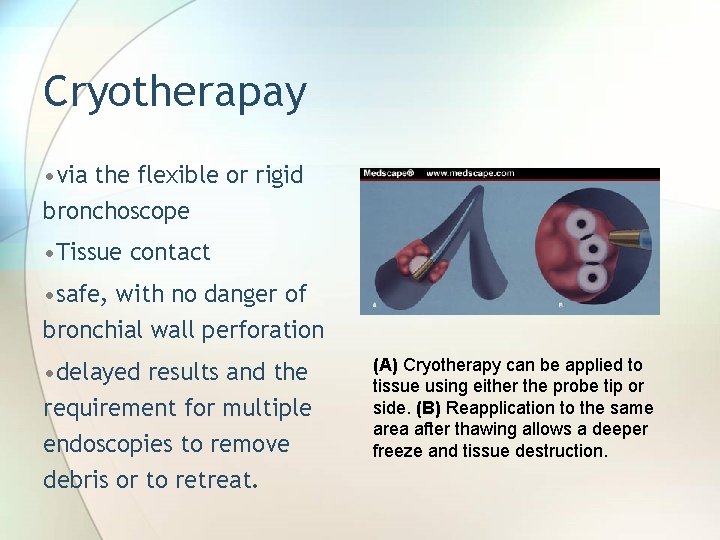
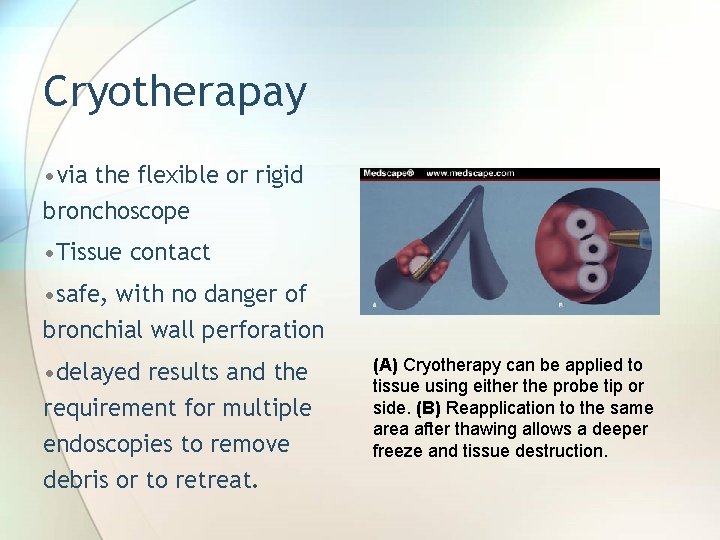
Cryotherapay • via the flexible or rigid bronchoscope • Tissue contact • safe, with no danger of bronchial wall perforation • delayed results and the requirement for multiple endoscopies to remove debris or to retreat. (A) Cryotherapy can be applied to tissue using either the probe tip or side. (B) Reapplication to the same area after thawing allows a deeper freeze and tissue destruction.
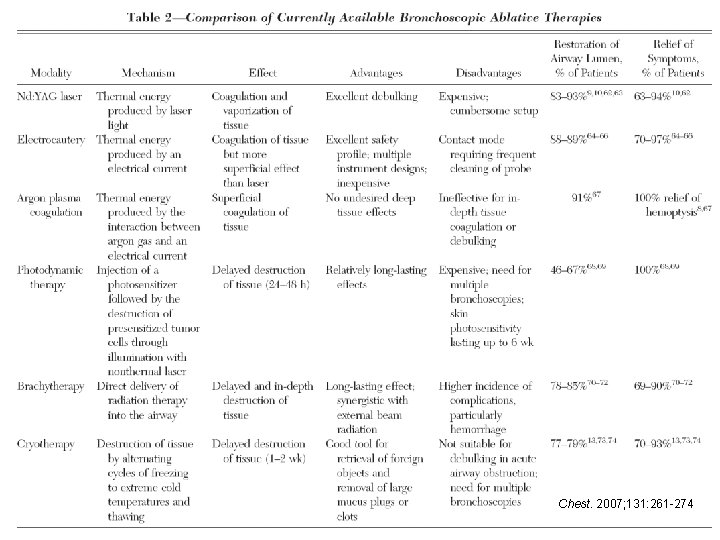
Chest. 2007; 131: 261 -274
Bronchial thermoplasty The Alair® System - which is manufactured by Asthmatx, Inc. - consists of a single-use device and a controller that delivers thermal energy to the bronchial wall during an outpatient bronchoscopic procedure known as Bronchial Thermoplasty™.

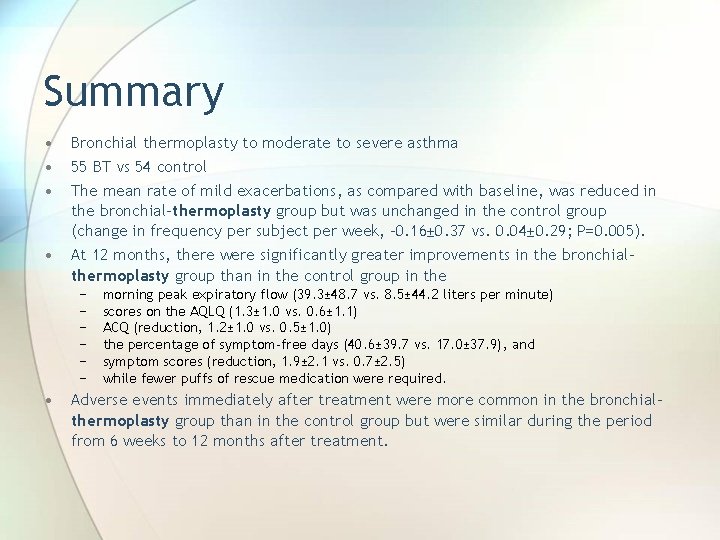
The Asthma Intervention Research (AIR) Trial Cox G et al. NEJM 2007; 356: 33 - 43
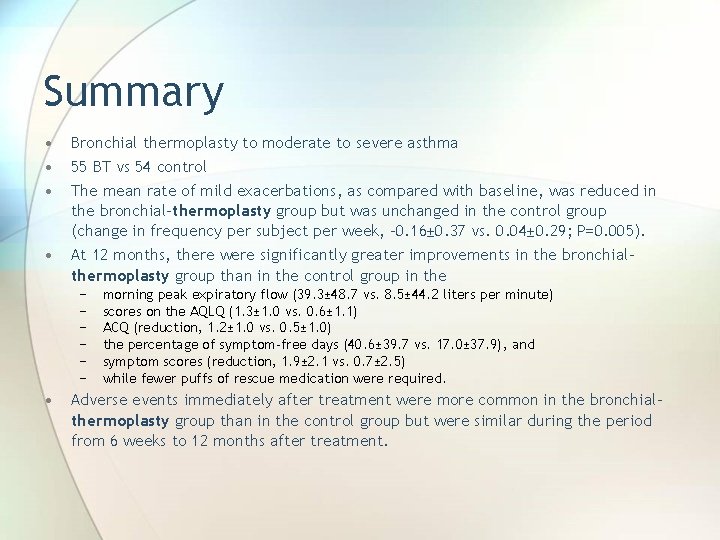
Summary • • Bronchial thermoplasty to moderate to severe asthma 55 BT vs 54 control The mean rate of mild exacerbations, as compared with baseline, was reduced in the bronchial-thermoplasty group but was unchanged in the control group (change in frequency per subject per week, – 0. 16± 0. 37 vs. 0. 04± 0. 29; P=0. 005). At 12 months, there were significantly greater improvements in the bronchialthermoplasty group than in the control group in the − − − • morning peak expiratory flow (39. 3± 48. 7 vs. 8. 5± 44. 2 liters per minute) scores on the AQLQ (1. 3± 1. 0 vs. 0. 6± 1. 1) ACQ (reduction, 1. 2± 1. 0 vs. 0. 5± 1. 0) the percentage of symptom-free days (40. 6± 39. 7 vs. 17. 0± 37. 9), and symptom scores (reduction, 1. 9± 2. 1 vs. 0. 7± 2. 5) while fewer puffs of rescue medication were required. Adverse events immediately after treatment were more common in the bronchialthermoplasty group than in the control group but were similar during the period from 6 weeks to 12 months after treatment.
AIR 2 Trial • Subjects: severe asthma • Aims to recruit 280 patients by March 31 2007


Airways
Percutaneous tracheostomy • Human cadaver available for practice
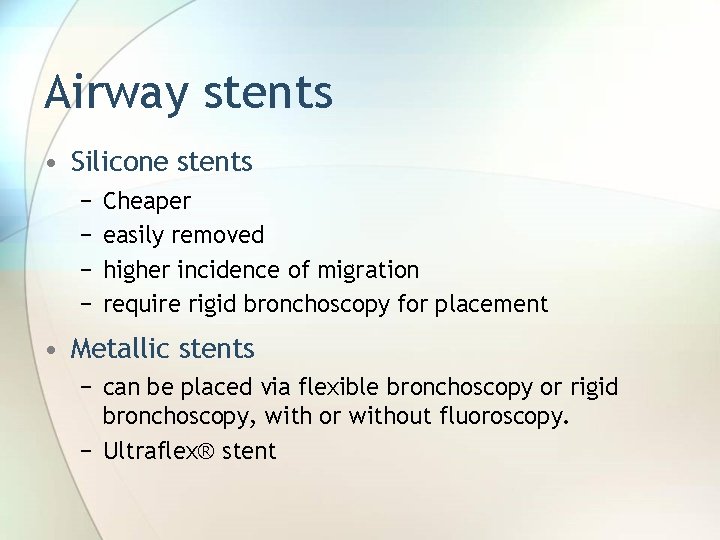
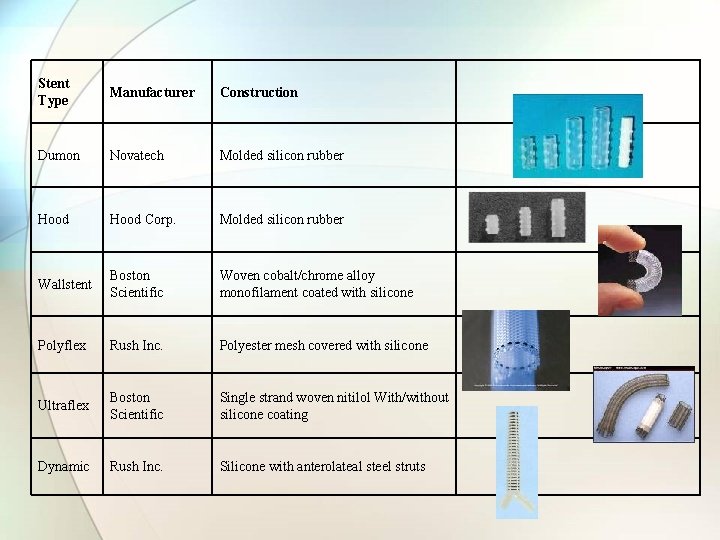
Airway stents • Silicone stents − − Cheaper easily removed higher incidence of migration require rigid bronchoscopy for placement • Metallic stents − can be placed via flexible bronchoscopy or rigid bronchoscopy, with or without fluoroscopy. − Ultraflex® stent
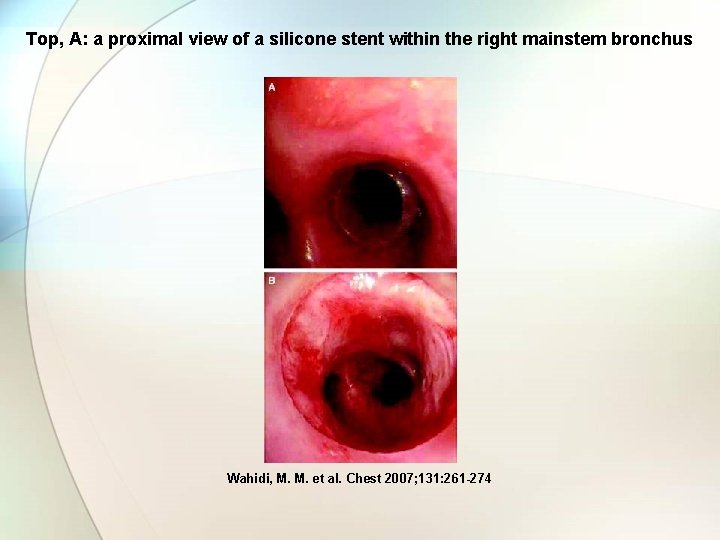
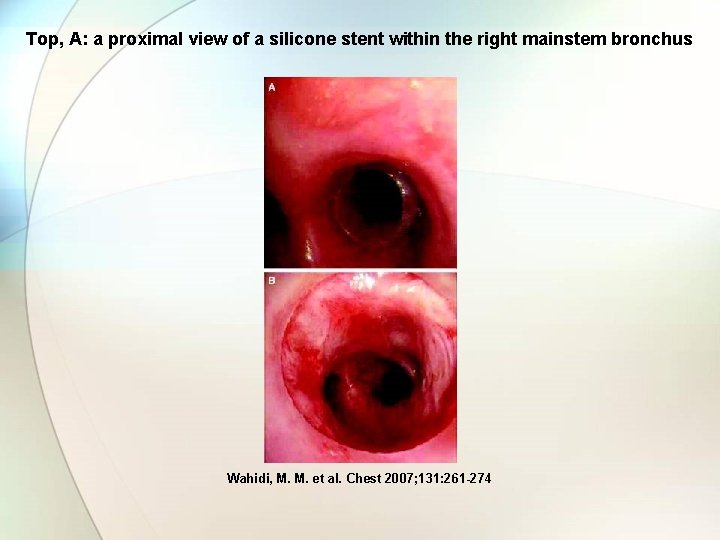
Top, A: a proximal view of a silicone stent within the right mainstem bronchus Wahidi, M. M. et al. Chest 2007; 131: 261 -274
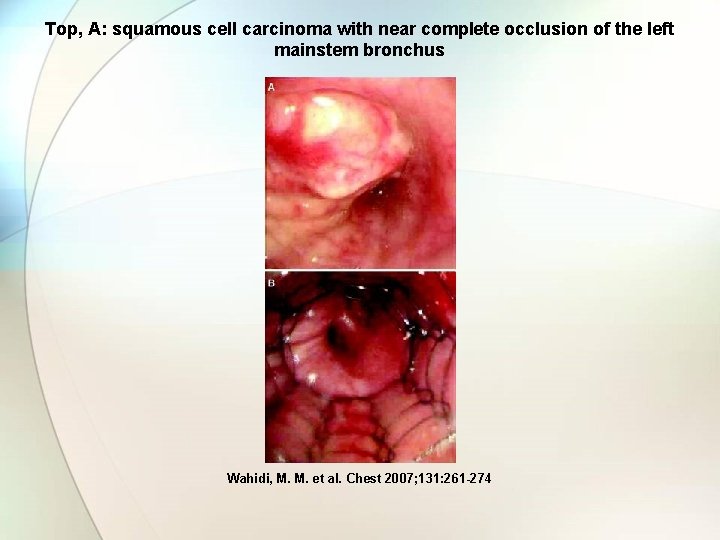
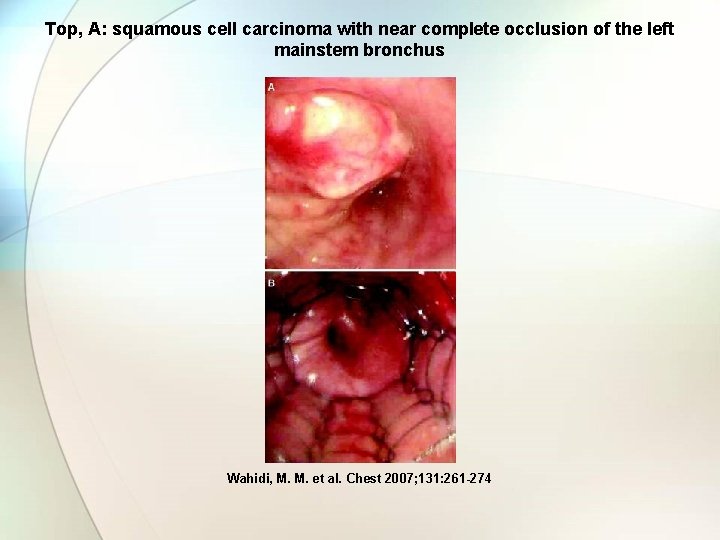
Top, A: squamous cell carcinoma with near complete occlusion of the left mainstem bronchus Wahidi, M. M. et al. Chest 2007; 131: 261 -274
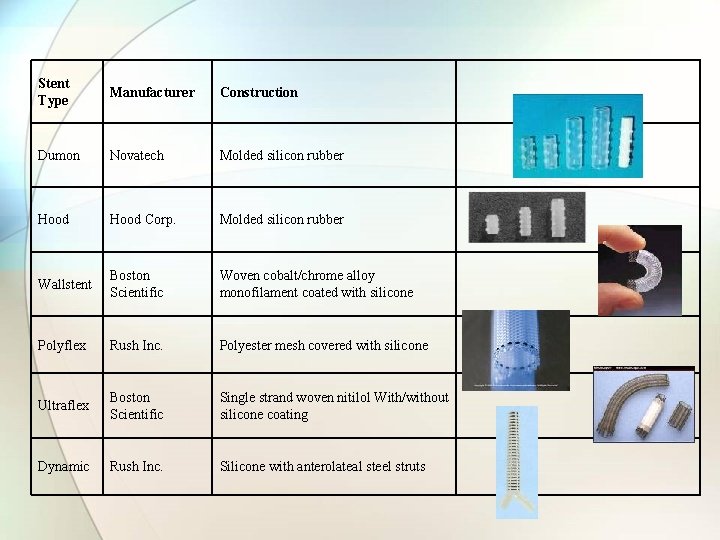
Stent Type Manufacturer Construction Dumon Novatech Molded silicon rubber Hood Corp. Molded silicon rubber Wallstent Boston Scientific Woven cobalt/chrome alloy monofilament coated with silicone Polyflex Rush Inc. Ultraflex Boston Scientific Dynamic Rush Inc. Polyester mesh covered with silicone Single strand woven nitilol With/without silicone coating Silicone with anterolateal steel struts

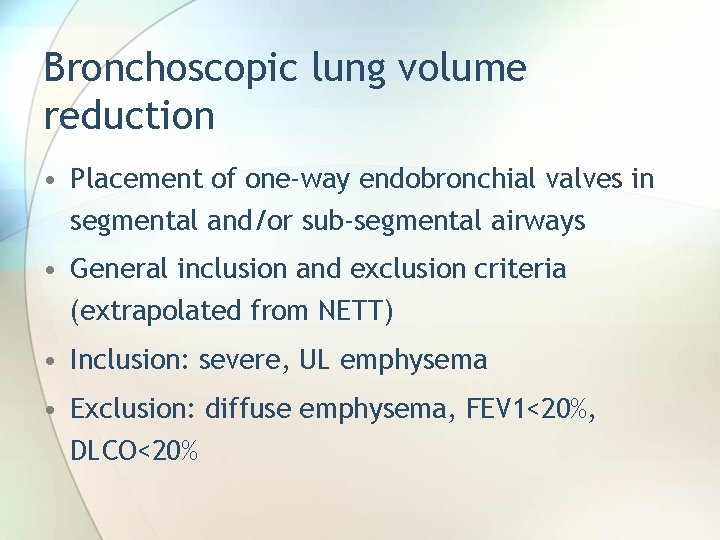
Bronchoscopic lung volume reduction • Placement of one-way endobronchial valves in segmental and/or sub-segmental airways • General inclusion and exclusion criteria (extrapolated from NETT) • Inclusion: severe, UL emphysema • Exclusion: diffuse emphysema, FEV 1<20%, DLCO<20%
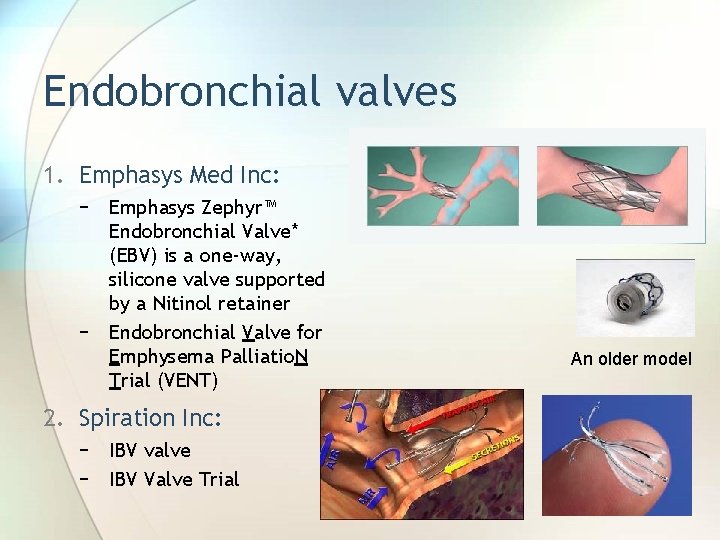
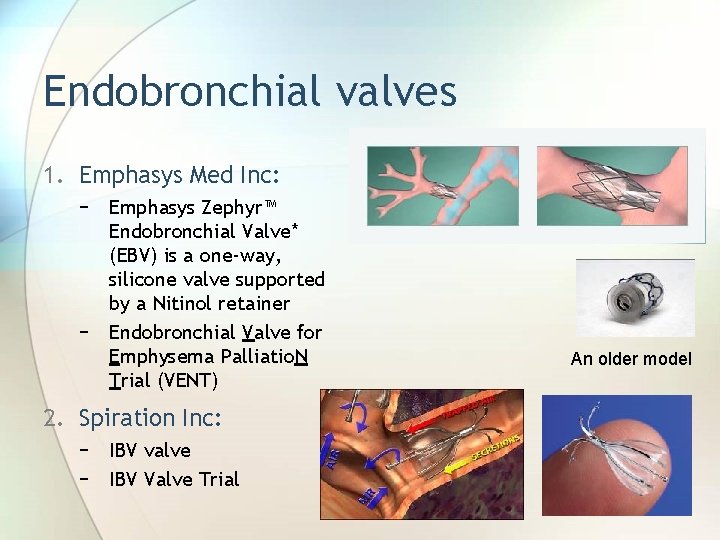
Endobronchial valves 1. Emphasys Med Inc: − Emphasys Zephyr™ Endobronchial Valve* (EBV) is a one-way, silicone valve supported by a Nitinol retainer − Endobronchial Valve for Emphysema Palliatio. N Trial (VENT) 2. Spiration Inc: − IBV valve − IBV Valve Trial An older model
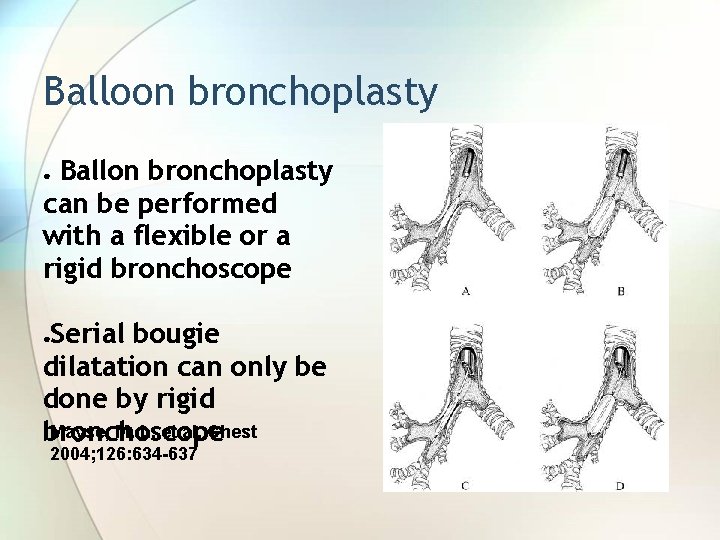
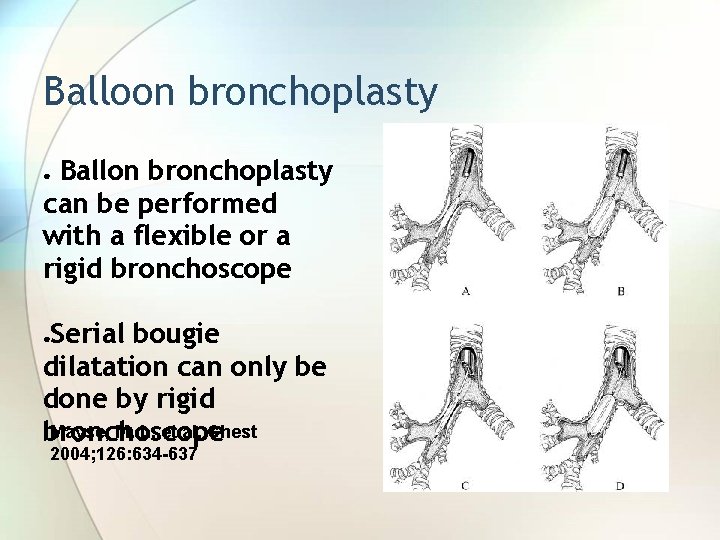
Balloon bronchoplasty Ballon bronchoplasty can be performed with a flexible or a rigid bronchoscope ● Serial bougie dilatation can only be done by rigid Mayse, M. L. et al. Chest bronchoscope ● 2004; 126: 634 -637
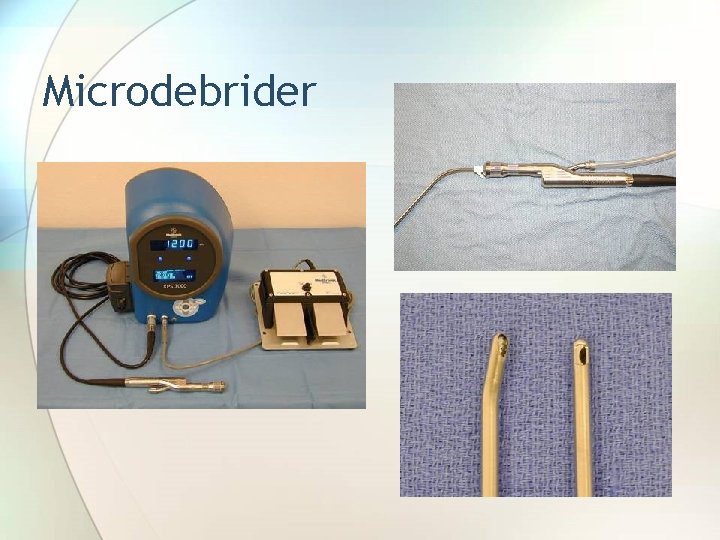
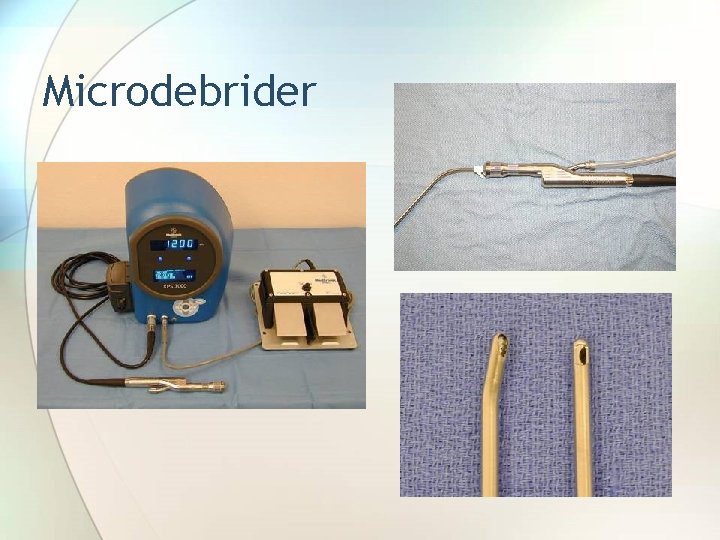
Microdebrider
Other topics • Medical Grand Round: Lung transplantation • Billing and coding for Interventional procedures • Improving yield of TBNA • Laryngotracheal stenosis • Tracheomalacia and excessive dynamic collapse • Chest tube insertion and management

Boston downtown

Thank you.
 Score de ferriman
Score de ferriman Jenis investigasi dalam penelitian
Jenis investigasi dalam penelitian Porofessor overlay
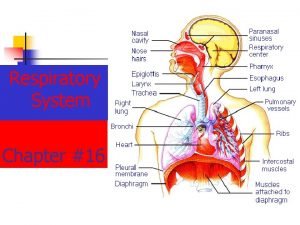
Porofessor overlay Uhs pulmonology
Uhs pulmonology Fcps pulmonology
Fcps pulmonology Fcps pulmonology
Fcps pulmonology Staxis medical term
Staxis medical term Sailor course brick
Sailor course brick Course title and course number
Course title and course number Course interne course externe
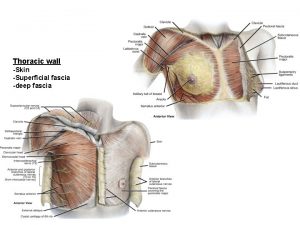
Course interne course externe Muscles of thoracic spine
Muscles of thoracic spine Sternum
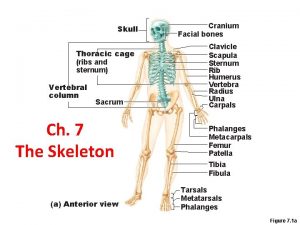
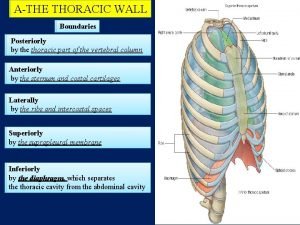
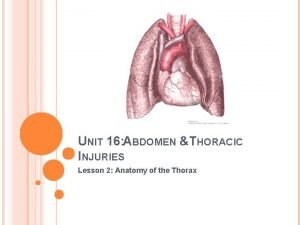
Sternum Thorax anatomy
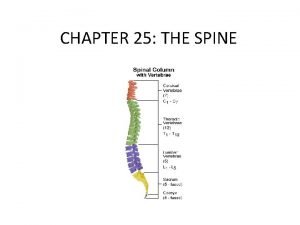
Thorax anatomy Thorcic spine
Thorcic spine Thoracic kyphosis
Thoracic kyphosis Thoracic nerves
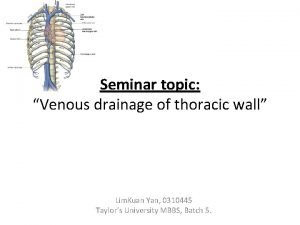
Thoracic nerves Venous drainage of thoracic wall
Venous drainage of thoracic wall Axilla posterior wall
Axilla posterior wall Volume of thoracic cavity
Volume of thoracic cavity Thoracic outlet wedge pillow
Thoracic outlet wedge pillow Plumb line posture
Plumb line posture Fascia of thorax
Fascia of thorax British thoracic society guidelines oxygen
British thoracic society guidelines oxygen Lumbar vertebrae characteristics
Lumbar vertebrae characteristics Internal vs external intercostal muscles
Internal vs external intercostal muscles Celiac ganglion
Celiac ganglion Abdominal wall lymph nodes
Abdominal wall lymph nodes Thoracic cavity labeled
Thoracic cavity labeled Rib tubercle
Rib tubercle Thorax cavity
Thorax cavity Thoracic aortic aneurysm
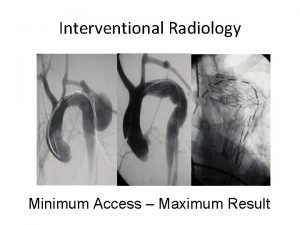
Thoracic aortic aneurysm Aortic knob
Aortic knob Mitral stenosis chest x ray
Mitral stenosis chest x ray Interior
Interior Lung surface anatomy
Lung surface anatomy Median sacral crest
Median sacral crest Neurogeen thoracic outlet syndroom
Neurogeen thoracic outlet syndroom Blood supply to thoracic wall
Blood supply to thoracic wall Thoracic configuration
Thoracic configuration Which ventral cavity subdivision has no bony protection:
Which ventral cavity subdivision has no bony protection: Thyroid isotope scan
Thyroid isotope scan Subcostal angle
Subcostal angle Orbital body cavity
Orbital body cavity Chyle leak
Chyle leak Muscles of thoracic spine
Muscles of thoracic spine Intercostal muscles
Intercostal muscles Thoracic aorta supplies blood to
Thoracic aorta supplies blood to Body planes directions and cavities
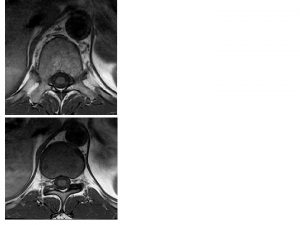
Body planes directions and cavities Thoracic mri images
Thoracic mri images Vertebrae
Vertebrae Thoracic surgeon
Thoracic surgeon Thoracic duct
Thoracic duct Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Fascia of thoracic wall
Fascia of thoracic wall The purified lymph with lymphocytes and antibodies added
The purified lymph with lymphocytes and antibodies added Ajith sominanda
Ajith sominanda Thoracic surgery
Thoracic surgery Anterior lumbar counterstrain points
Anterior lumbar counterstrain points Thoracic extension
Thoracic extension Thoracic cage anterior view
Thoracic cage anterior view Superior mediastinum contents
Superior mediastinum contents Which membrane encloses the abdominopelvic viscera?
Which membrane encloses the abdominopelvic viscera? Thoracic membranes
Thoracic membranes Arteries of upper limb
Arteries of upper limb Pig thoracic cavity diagram
Pig thoracic cavity diagram Soft, spongy, cone-shaped organs in the thoracic cavity.
Soft, spongy, cone-shaped organs in the thoracic cavity. Thoracic cavity
Thoracic cavity Arkimedes princip formel
Arkimedes princip formel Rbk-mätning
Rbk-mätning Vad är densitet
Vad är densitet Elektronik för barn
Elektronik för barn Kassaregister ideell förening
Kassaregister ideell förening Borra hål för knoppar
Borra hål för knoppar Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Fimbrietratt
Fimbrietratt Trög för kemist
Trög för kemist Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Humanitr
Humanitr Enheter för massa
Enheter för massa Delegerande ledarskap
Delegerande ledarskap Toppslätskivling dos
Toppslätskivling dos Ekologiskt fotavtryck
Ekologiskt fotavtryck Redogör för vad psykologi är
Redogör för vad psykologi är Geometriska former i förskolan
Geometriska former i förskolan Bris för vuxna
Bris för vuxna