RESTRICTIVE THORACIC DISEASE Thoracic Restriction due to causes
- Slides: 18
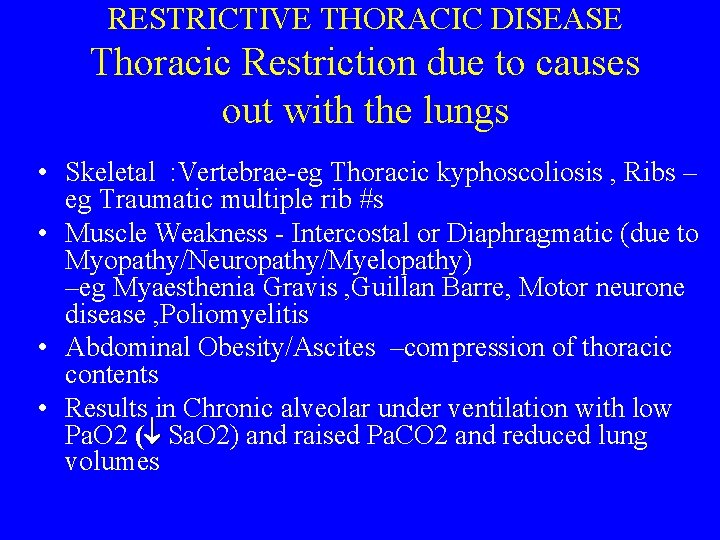
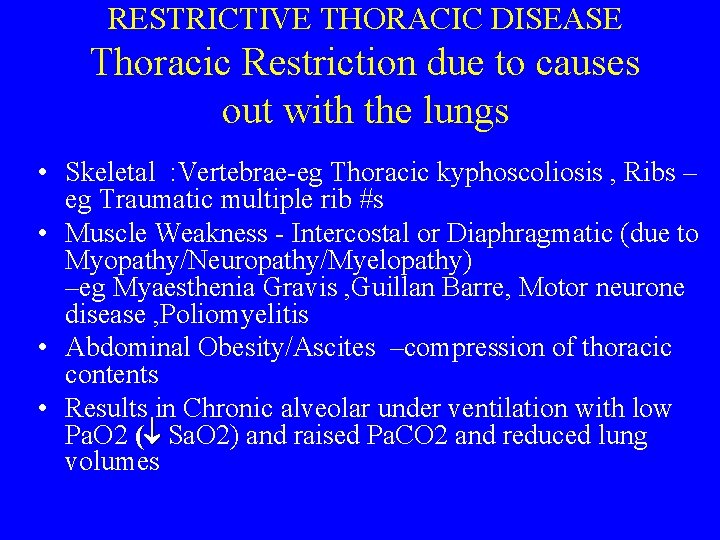
RESTRICTIVE THORACIC DISEASE Thoracic Restriction due to causes out with the lungs • Skeletal : Vertebrae-eg Thoracic kyphoscoliosis , Ribs – eg Traumatic multiple rib #s • Muscle Weakness - Intercostal or Diaphragmatic (due to Myopathy/Neuropathy/Myelopathy) –eg Myaesthenia Gravis , Guillan Barre, Motor neurone disease , Poliomyelitis • Abdominal Obesity/Ascites –compression of thoracic contents • Results in Chronic alveolar under ventilation with low Pa. O 2 ( Sa. O 2) and raised Pa. CO 2 and reduced lung volumes
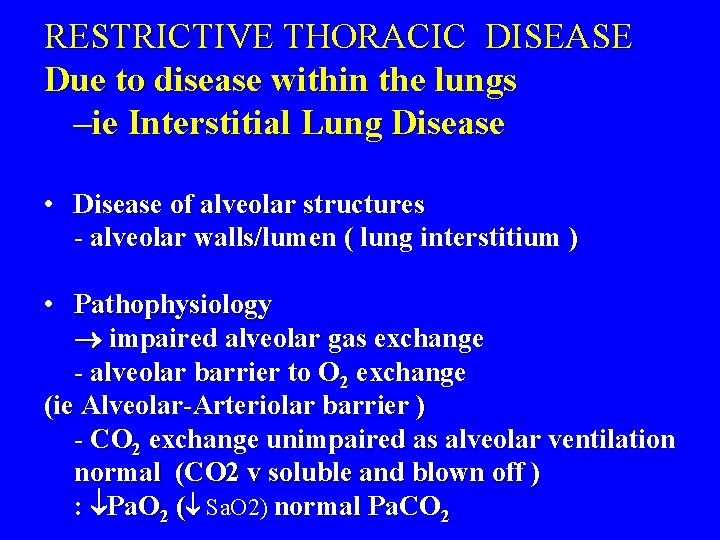
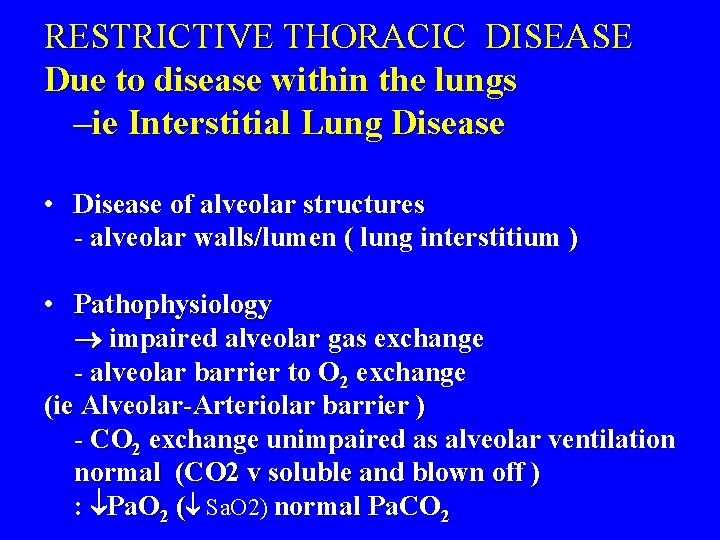
RESTRICTIVE THORACIC DISEASE Due to disease within the lungs –ie Interstitial Lung Disease • Disease of alveolar structures - alveolar walls/lumen ( lung interstitium ) • Pathophysiology impaired alveolar gas exchange - alveolar barrier to O 2 exchange (ie Alveolar-Arteriolar barrier ) - CO 2 exchange unimpaired as alveolar ventilation normal (CO 2 v soluble and blown off ) : Pa. O 2 ( Sa. O 2) normal Pa. CO 2
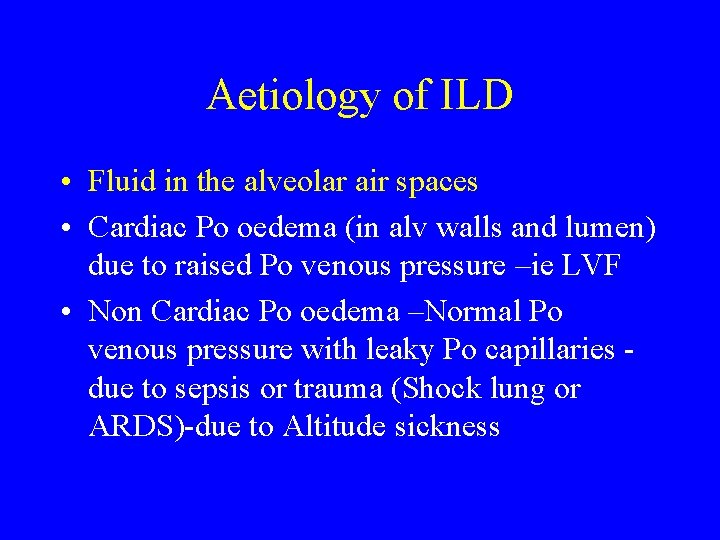
Aetiology of ILD • Fluid in the alveolar air spaces • Cardiac Po oedema (in alv walls and lumen) due to raised Po venous pressure –ie LVF • Non Cardiac Po oedema –Normal Po venous pressure with leaky Po capillaries due to sepsis or trauma (Shock lung or ARDS)-due to Altitude sickness
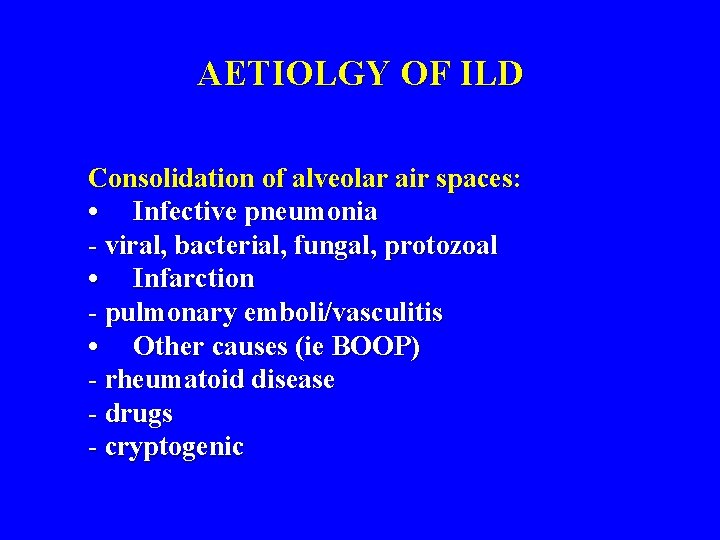
AETIOLGY OF ILD Consolidation of alveolar air spaces: • Infective pneumonia - viral, bacterial, fungal, protozoal • Infarction - pulmonary emboli/vasculitis • Other causes (ie BOOP) - rheumatoid disease - drugs - cryptogenic
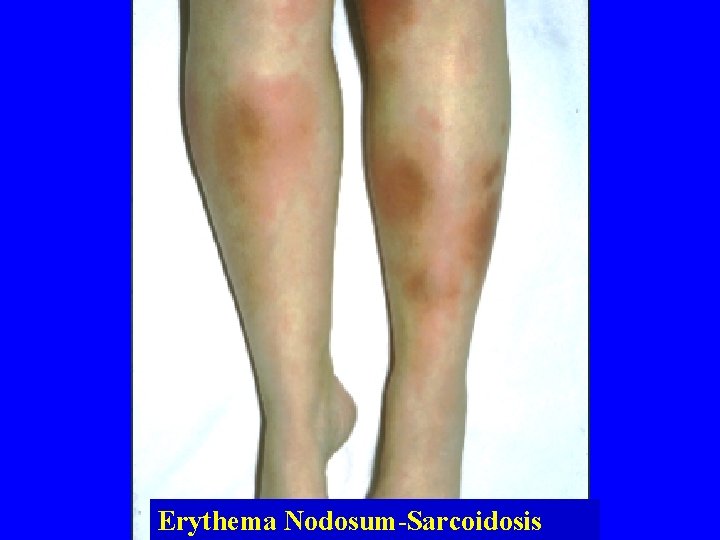
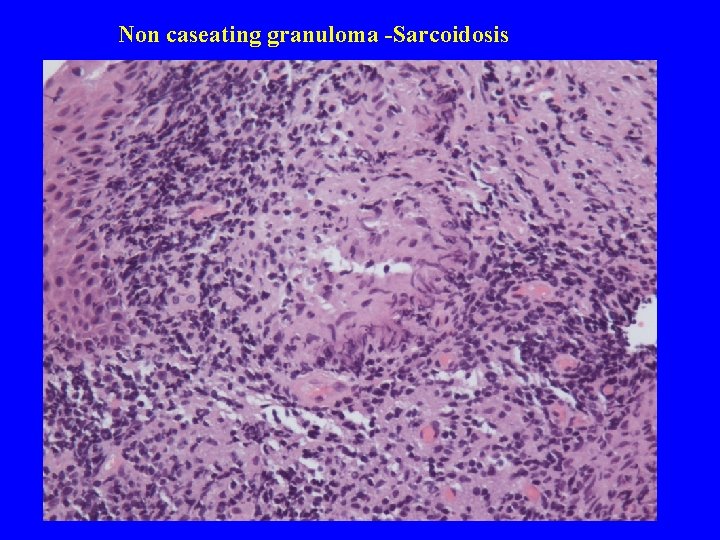
AETIOLGY OF ILD Inflam Infiltrate of alveolar walls (ie Alveolitis): • Granulomatous-alveolitis • Extrinsic-Allergic-Alveolitis (Hypersensitivity Pneumonitis-Type 3 reaction) - Farmers lung - Avian (pigeon, budgie) • Sarcoidosis Multisystem disease Lymphadenopathy/Erythema nodosum Uveitis/Myocarditis/Neuropathy
Aetiology of ILD Alveolitis continued • Drug induced alveolitis - Amiodarone - Bleomycin, Methotrexate - Gold • Fibrosing alveolitis - Rheumatoid , Cryptogenic • Autoimmune(multisystem) -SLE, Polyarteritis, Wegeners, Churg-Strauss
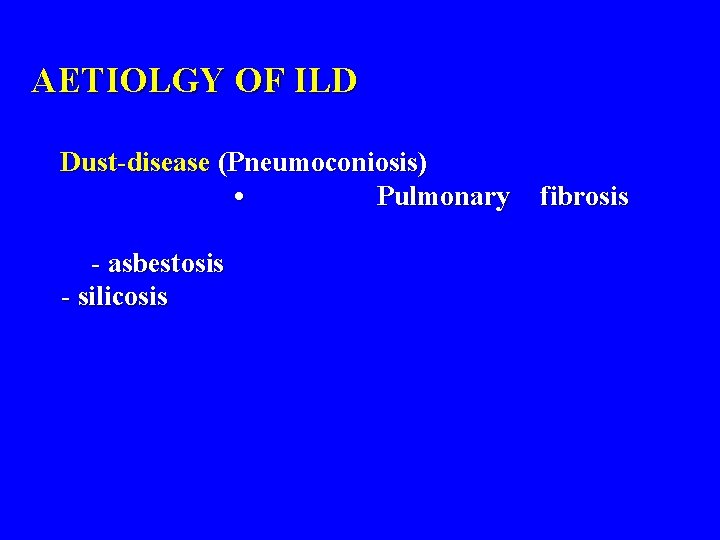
AETIOLGY OF ILD Dust-disease (Pneumoconiosis) • Pulmonary - asbestosis - silicosis fibrosis
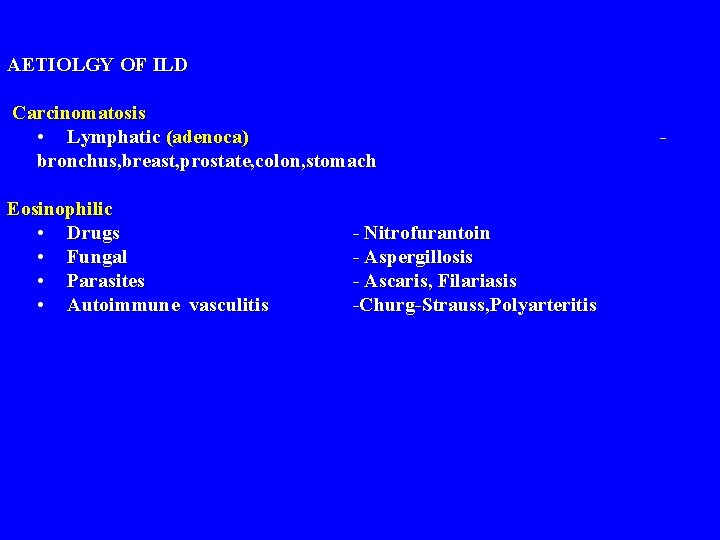
AETIOLGY OF ILD Carcinomatosis • Lymphatic (adenoca) bronchus, breast, prostate, colon, stomach Eosinophilic • Drugs • Fungal • Parasites • Autoimmune vasculitis - Nitrofurantoin - Aspergillosis - Ascaris, Filariasis -Churg-Strauss, Polyarteritis -
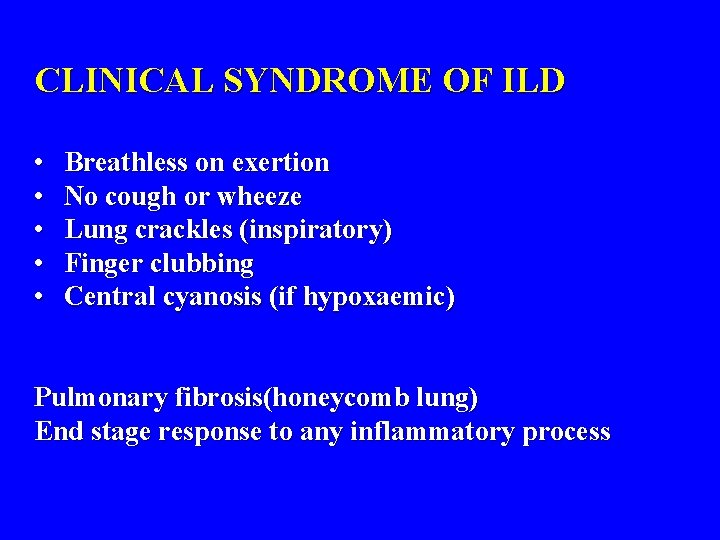
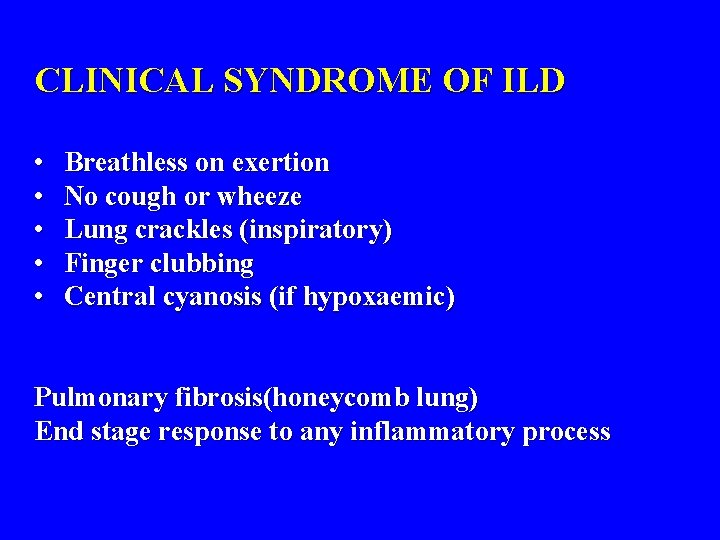
CLINICAL SYNDROME OF ILD • • • Breathless on exertion No cough or wheeze Lung crackles (inspiratory) Finger clubbing Central cyanosis (if hypoxaemic) Pulmonary fibrosis(honeycomb lung) End stage response to any inflammatory process
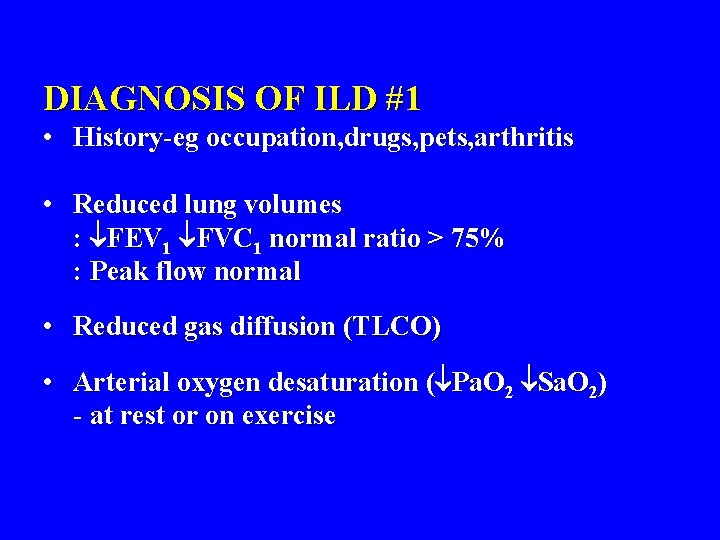
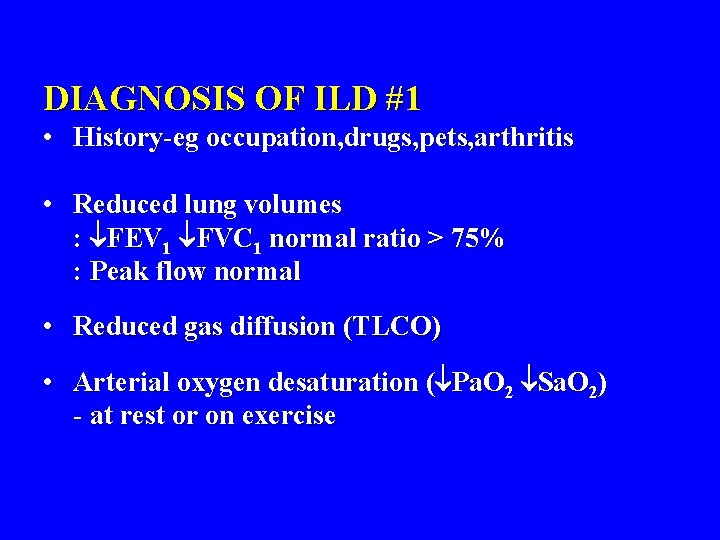
DIAGNOSIS OF ILD #1 • History-eg occupation, drugs, pets, arthritis • Reduced lung volumes : FEV 1 FVC 1 normal ratio > 75% : Peak flow normal • Reduced gas diffusion (TLCO) • Arterial oxygen desaturation ( Pa. O 2 Sa. O 2) - at rest or on exercise
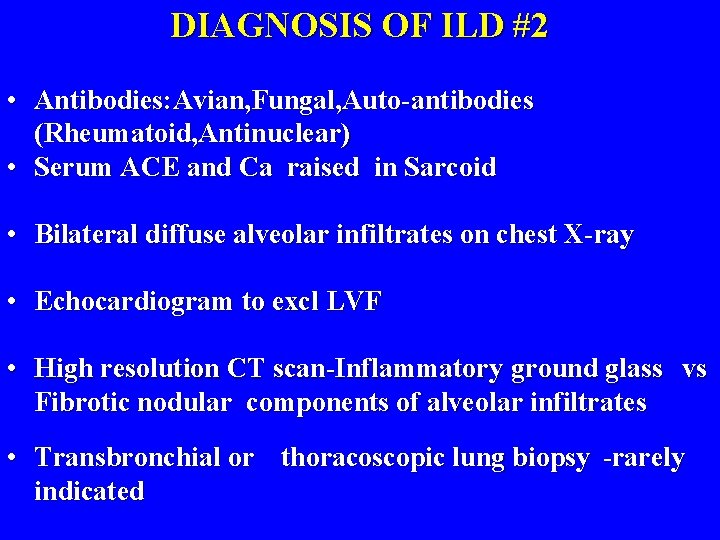
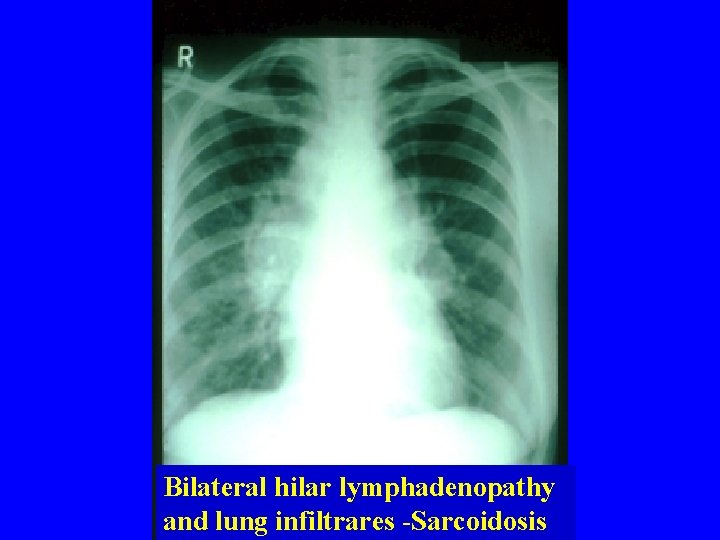
DIAGNOSIS OF ILD #2 • Antibodies: Avian, Fungal, Auto-antibodies (Rheumatoid, Antinuclear) • Serum ACE and Ca raised in Sarcoid • Bilateral diffuse alveolar infiltrates on chest X-ray • Echocardiogram to excl LVF • High resolution CT scan-Inflammatory ground glass vs Fibrotic nodular components of alveolar infiltrates • Transbronchial or thoracoscopic lung biopsy -rarely indicated
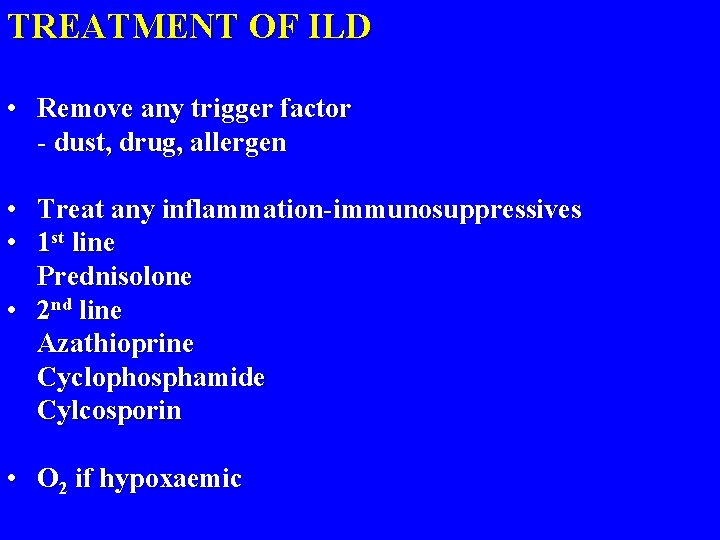
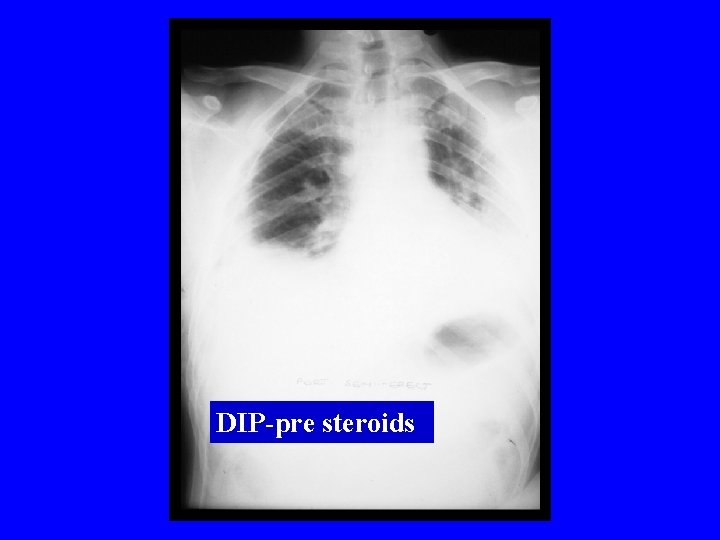
TREATMENT OF ILD • Remove any trigger factor - dust, drug, allergen • Treat any inflammation-immunosuppressives • 1 st line Prednisolone • 2 nd line Azathioprine Cyclophosphamide Cylcosporin • O 2 if hypoxaemic
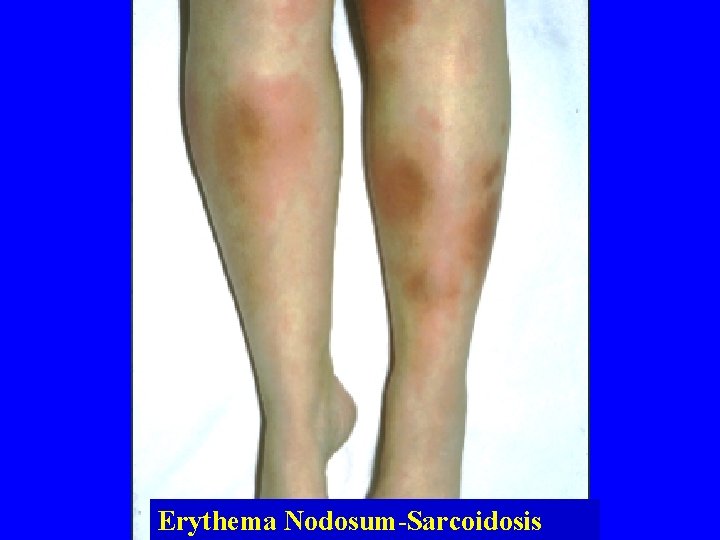
Erythema Nodosum-Sarcoidosis
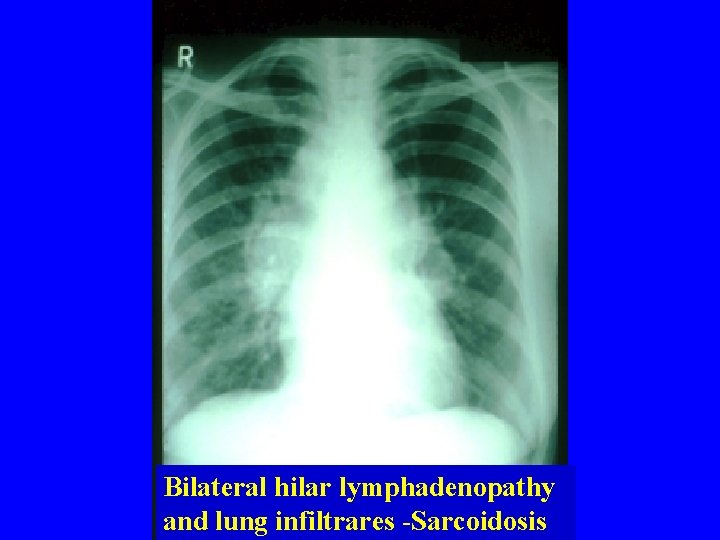
Bilateral hilar lymphadenopathy and lung infiltrares -Sarcoidosis
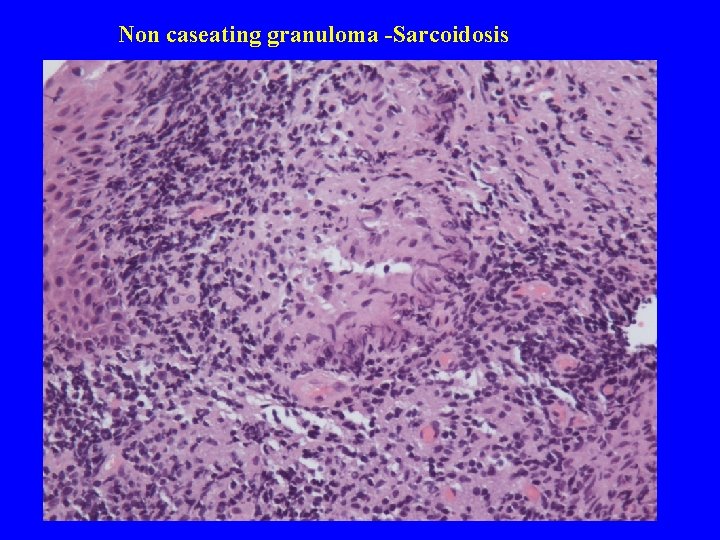
Non caseating granuloma -Sarcoidosis
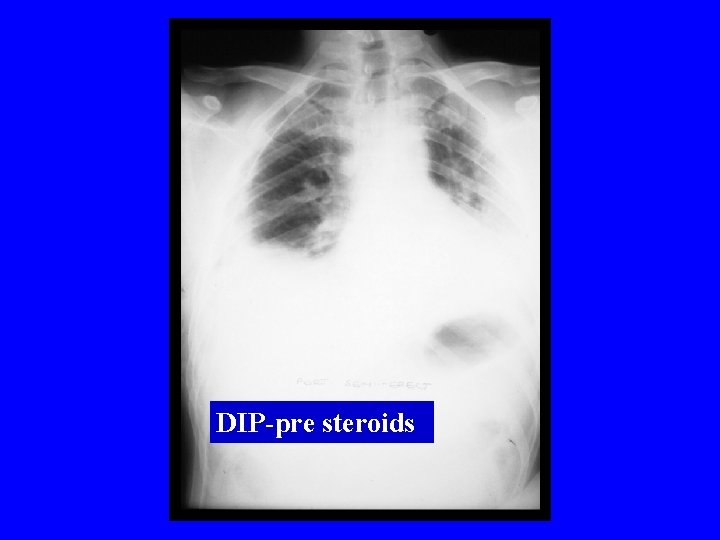
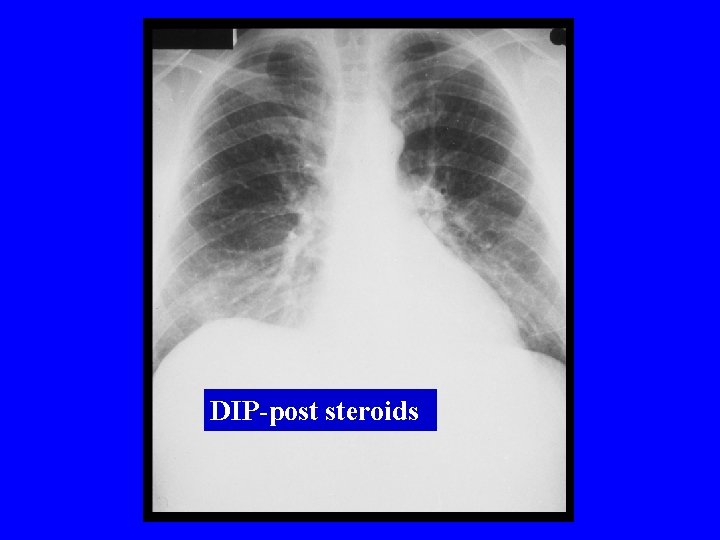
DIP-pre steroids
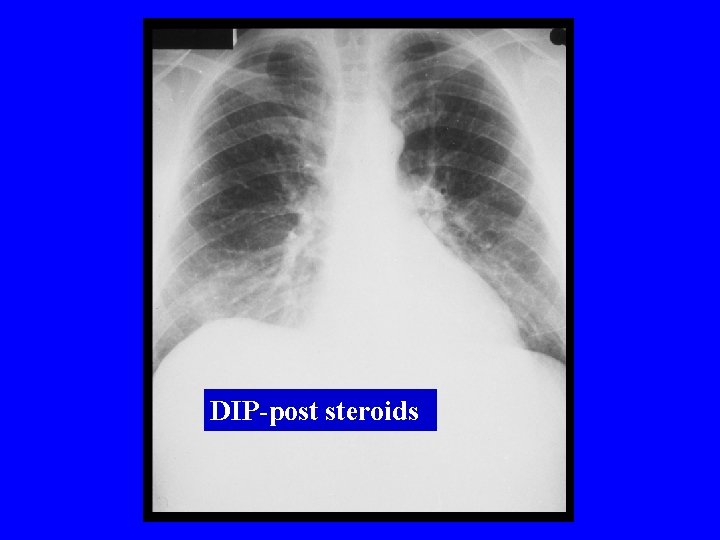
DIP-post steroids
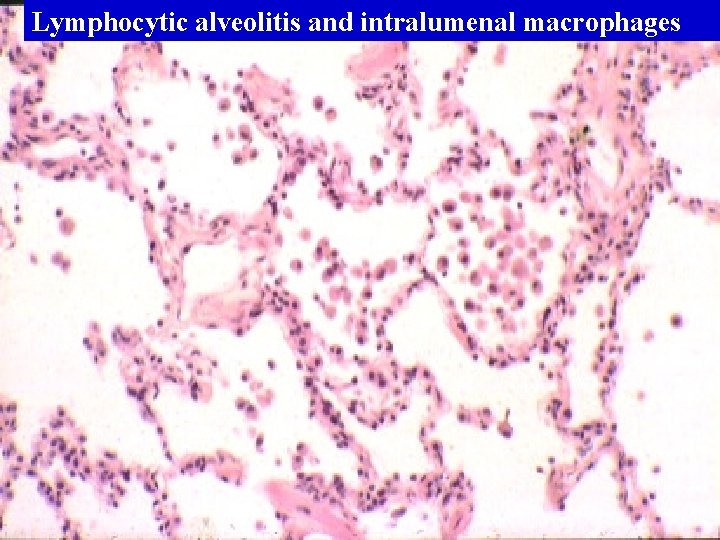
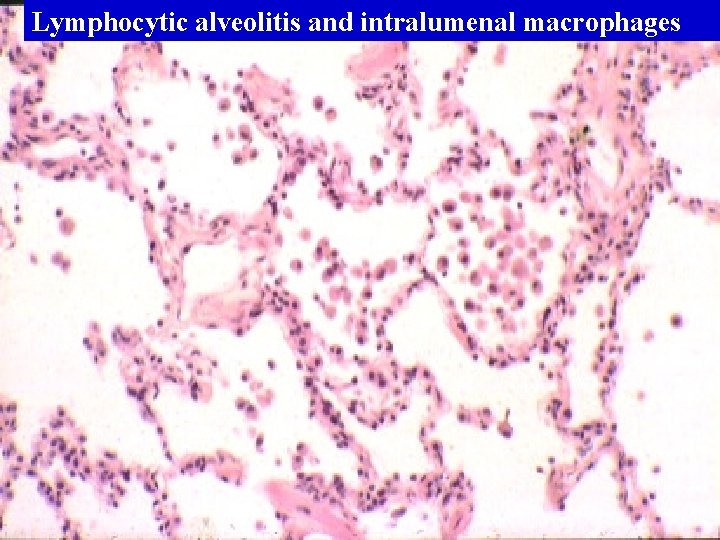
Lymphocytic alveolitis and intralumenal macrophages