THORACIC AND NECK TRAUMA Epidemiology Thoracic and neck



- Slides: 94
THORACIC AND NECK TRAUMA
Epidemiology • Thoracic and neck injuries are the 2 nd leading cause of death due to trauma • The mortality rate of neck injuries has declined • Increase in violence has had an impact on the pattern of injuries to the chest and neck
Mechanisms of Injury and Biomechanics • • Motor vehicle crashes Falls Crush Injuries Assaults Firearms Stabbings Motor vehicle versus pedestrian
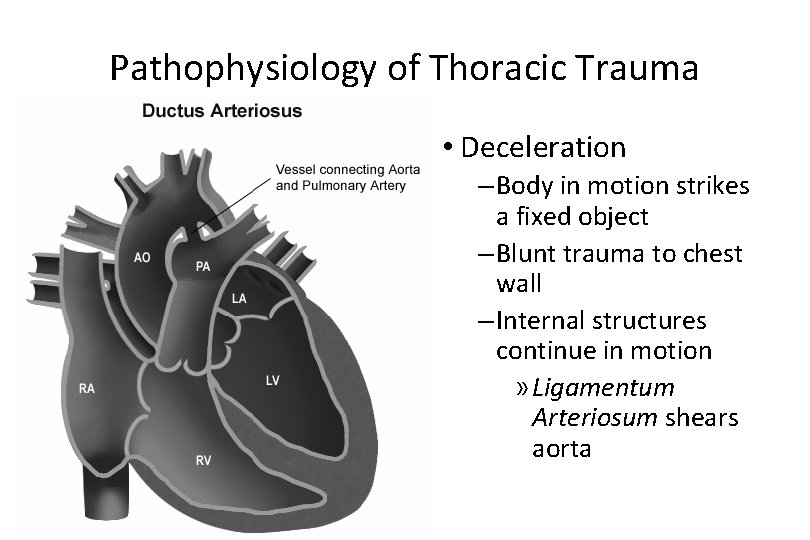
Mechanisms of Injury and Biomechanics • Acceleration forces • Deceleration forces – Thoracic aorta – Relative fixed attachment – Ligamentum arteriosum • Motor vehicle crashes account for two-thirds of all chest traumarelated deaths

Concurrent Injuries • Head • Extremity • Abdomen 5
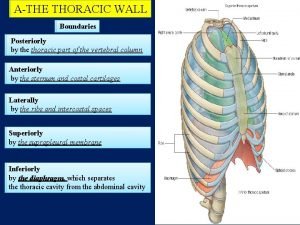
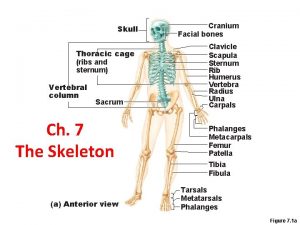
Introduction to Thoracic Injury • Vital Structures – Heart, Great Vessels, Esophagus, Tracheobronchial Tree, & Lungs • Abdominal injuries are common with chest trauma.
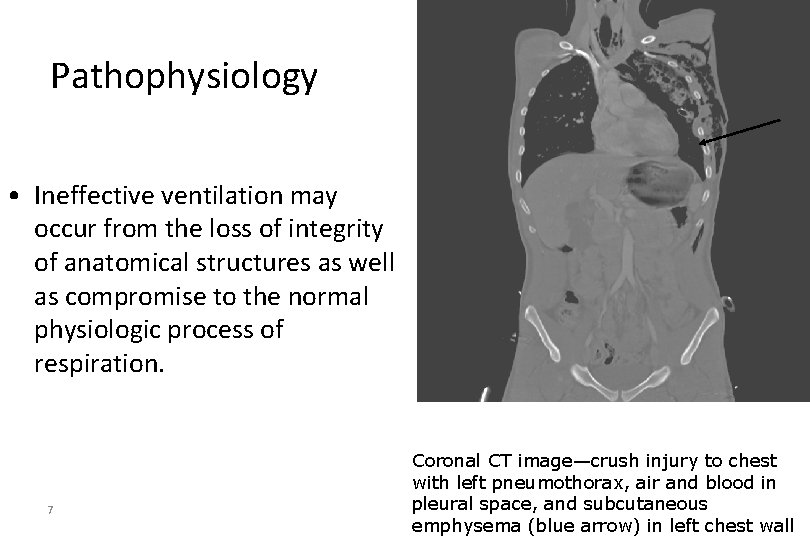
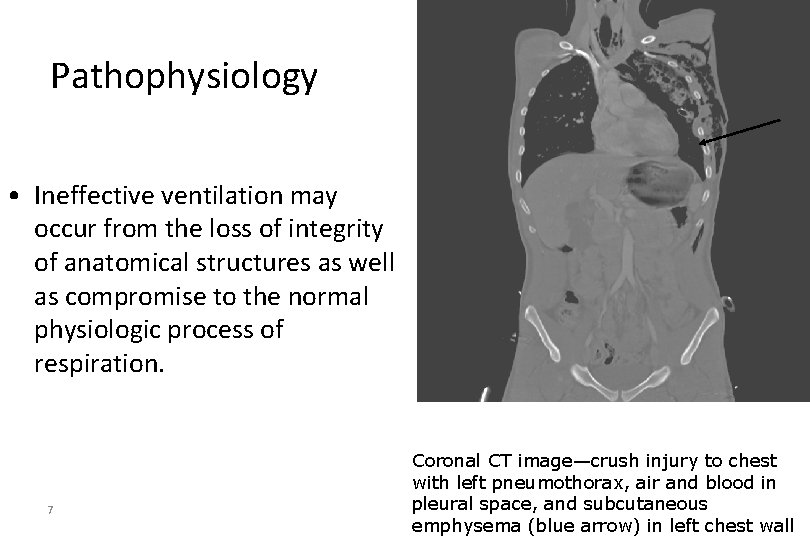
Pathophysiology • Ineffective ventilation may occur from the loss of integrity of anatomical structures as well as compromise to the normal physiologic process of respiration. 7 Coronal CT image—crush injury to chest with left pneumothorax, air and blood in pleural space, and subcutaneous emphysema (blue arrow) in left chest wall
Pathophysiology • Some causes of ineffective ventilation include: • Tears or lacerations to tracheobronchial tree • Rib or sternal fractures • Pain • Lung contusion or puncture • Penetrating injury of the chest wall
Pathophysiology • Ineffective circulation can occur from injury to the heart or thoracic great vessels causing internal and external hemorrhage which can lead to hypovolemia and shock. • Direct trauma to the heart may result in a reduced cardiac output from decreased myocardial contractility. 9
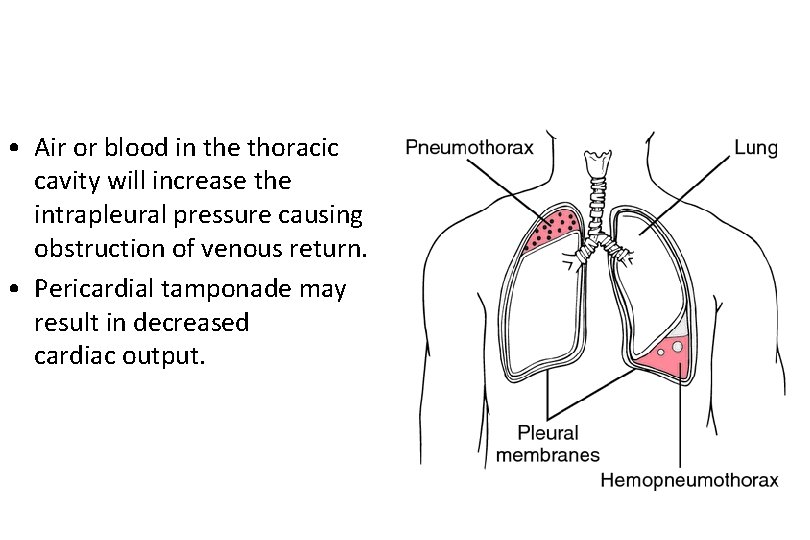
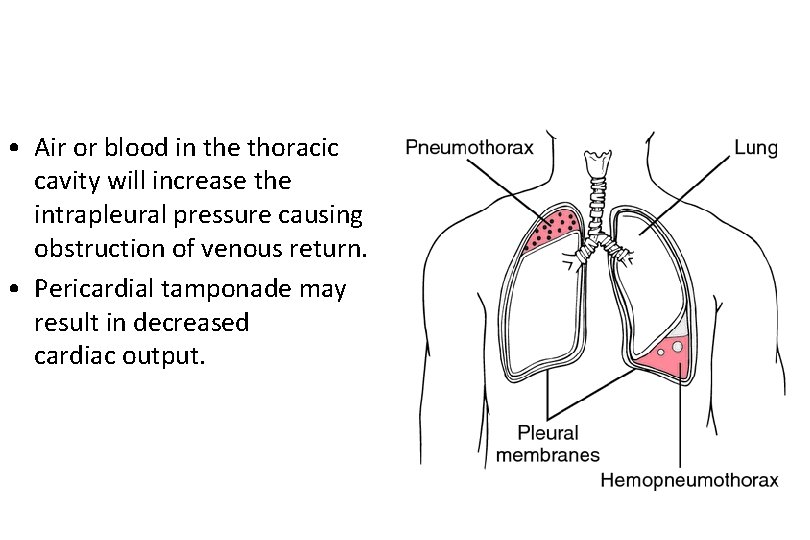
• Air or blood in the thoracic cavity will increase the intrapleural pressure causing obstruction of venous return. • Pericardial tamponade may result in decreased cardiac output.
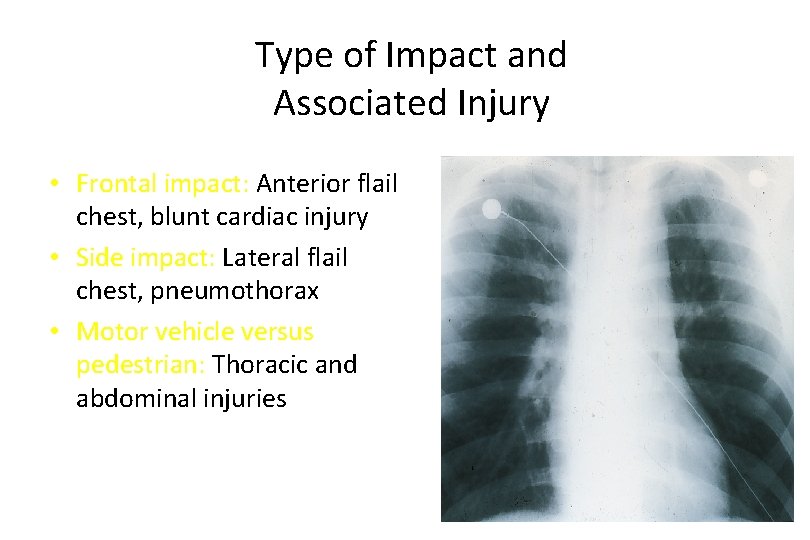
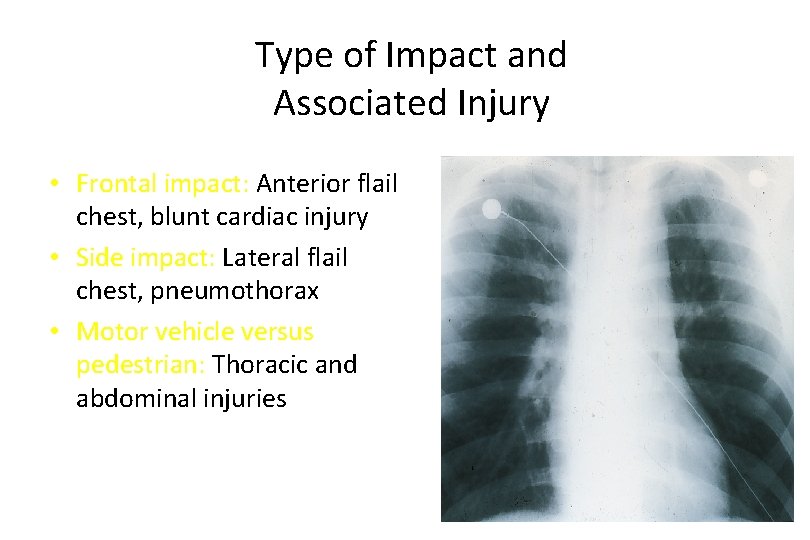
Type of Impact and Associated Injury • Frontal impact: Anterior flail chest, blunt cardiac injury • Side impact: Lateral flail chest, pneumothorax • Motor vehicle versus pedestrian: Thoracic and abdominal injuries
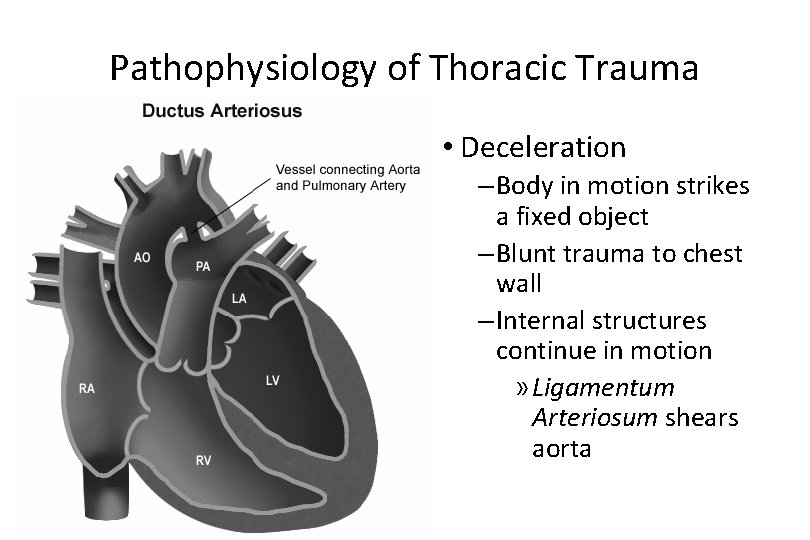
Pathophysiology of Thoracic Trauma • Deceleration – Body in motion strikes a fixed object – Blunt trauma to chest wall – Internal structures continue in motion » Ligamentum Arteriosum shears aorta
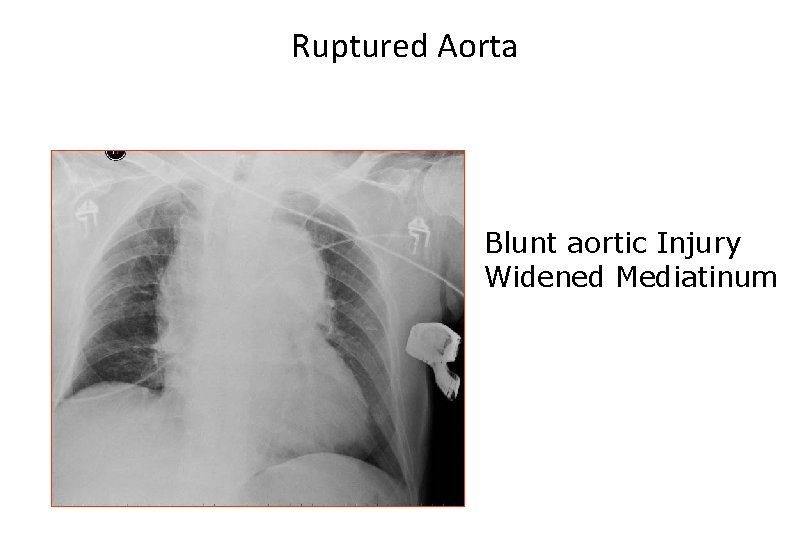
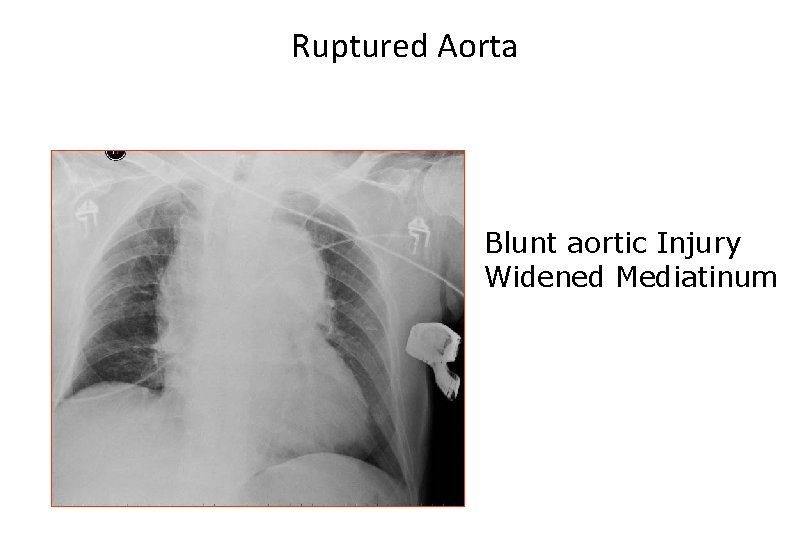
Ruptured Aorta Blunt aortic Injury Widened Mediatinum
Types of Injuries • Blunt trauma: 70% – Most common cause is motor vehicle crashes • Penetrating trauma: 30% – Firearms – Stabbings
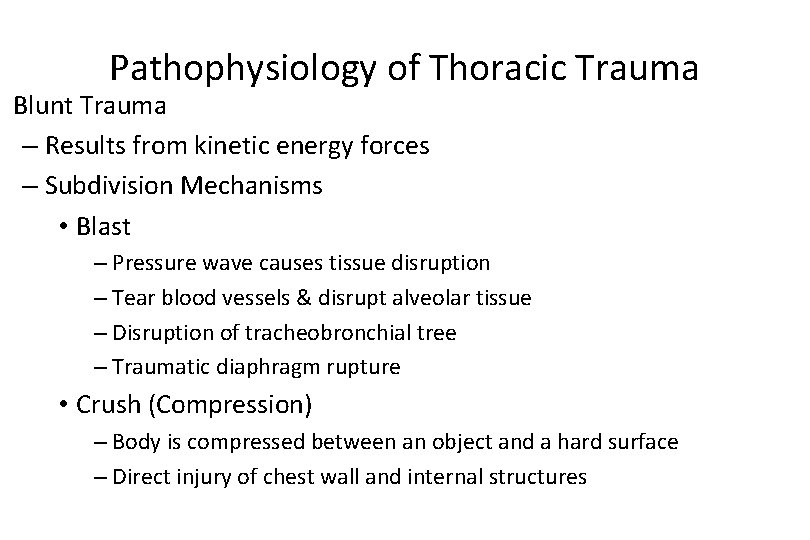
Pathophysiology of Thoracic Trauma Blunt Trauma – Results from kinetic energy forces – Subdivision Mechanisms • Blast – Pressure wave causes tissue disruption – Tear blood vessels & disrupt alveolar tissue – Disruption of tracheobronchial tree – Traumatic diaphragm rupture • Crush (Compression) – Body is compressed between an object and a hard surface – Direct injury of chest wall and internal structures
Blunt Cardiac Injury • Formerly called cardiac contusion or cardiac concussion • Suspect following an associated mechanism of injury (motor vehicle crash) or in those patients with poor cardiovascular response to injury 16
Blunt Cardiac Injury Signs and Symptoms • ECG abnormalities • Chest pain • Chest wall ecchymosis 17
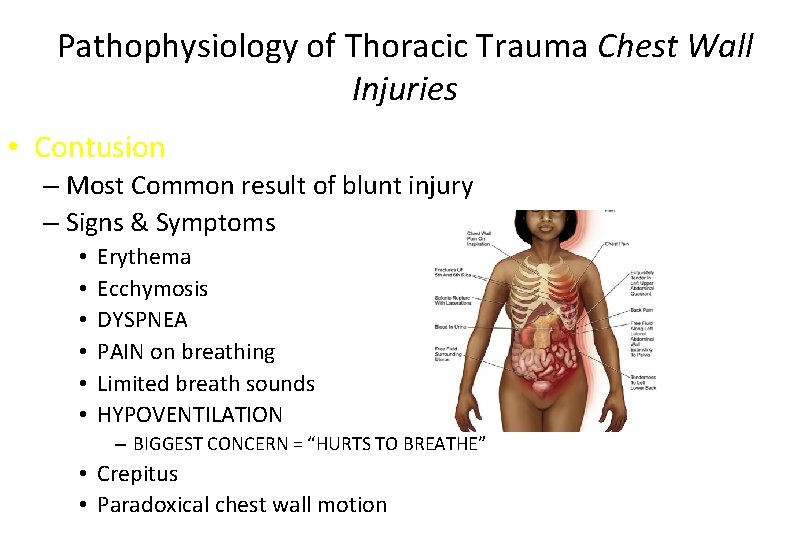
Pathophysiology of Thoracic Trauma Chest Wall Injuries • Contusion – Most Common result of blunt injury – Signs & Symptoms • • • Erythema Ecchymosis DYSPNEA PAIN on breathing Limited breath sounds HYPOVENTILATION – BIGGEST CONCERN = “HURTS TO BREATHE” • Crepitus • Paradoxical chest wall motion
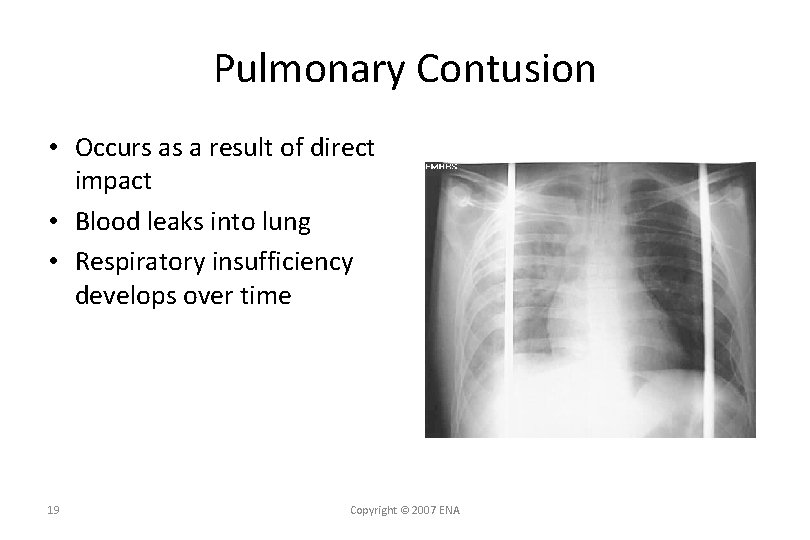
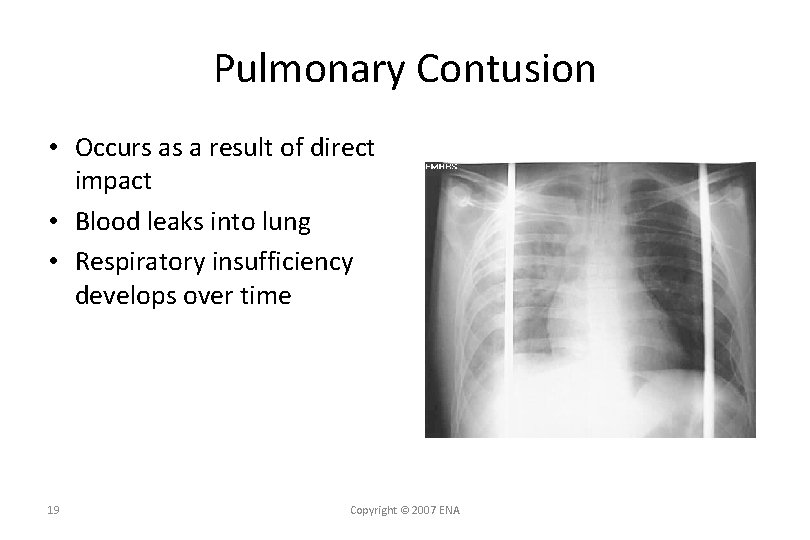
Pulmonary Contusion • Occurs as a result of direct impact • Blood leaks into lung • Respiratory insufficiency develops over time 19 Copyright © 2007 ENA
Pulmonary Contusion Signs and Symptoms • Dyspnea • Ineffective cough • Hemoptysis • Hypoxia • Chest pain • Chest wall contusion or abrasions 20 Copyright © 2007 ENA
Pathophysiology of Thoracic Trauma • Penetrating Trauma – Low Energy • Arrows, knives, handguns • Injury caused by direct contact and cavitation – High Energy • Military, hunting rifles & high powered hand guns • Extensive injury due to high pressure cavitation
Pathophysiology of Thoracic Trauma • Penetrating Injuries (cont. ) – Shotgun • Injury severity based upon the distance between the victim and shotgun & caliber of shot • Type I: >7 meters from the weapon – Soft tissue injury • Type II: 3 -7 meters from weapon – Penetration into deep fascia and some internal organs • Type III: <3 meters from weapon – Massive tissue destruction
Injuries Associated with Penetrating Thoracic Trauma • Closed pneumothorax • Open pneumothorax (including sucking chest wound) • Tension pneumothorax • Pneumomediastinum • Hemothorax • Hemopneumothorax • Laceration of vascular structures • • Tracheobronchial tree lacerations Esophageal lacerations Penetrating cardiac injuries Pericardial tamponade Spinal cord injuries Diaphragm trauma Intra-abdominal penetration with associated organ injury
Pathophysiology of Thoracic Trauma – Age Factors • Pediatric Thorax: More cartilage = Absorbs forces • Geriatric Thorax: Calcification & osteoporosis = More fractures
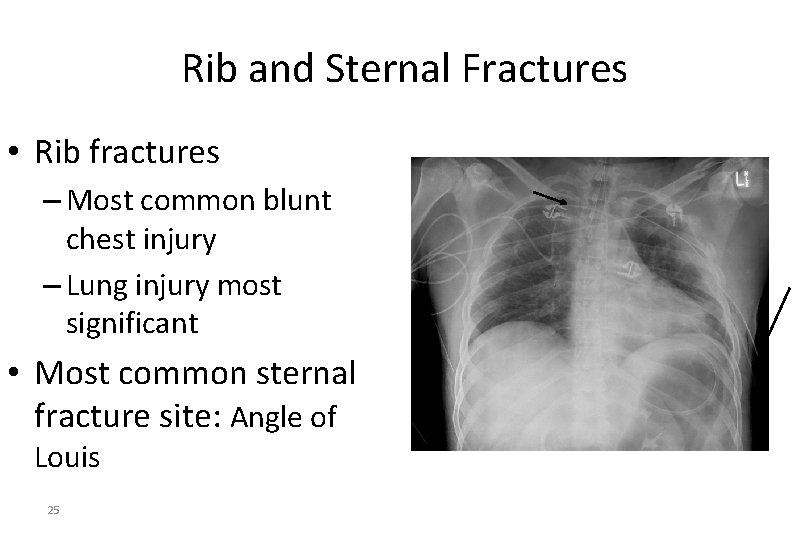
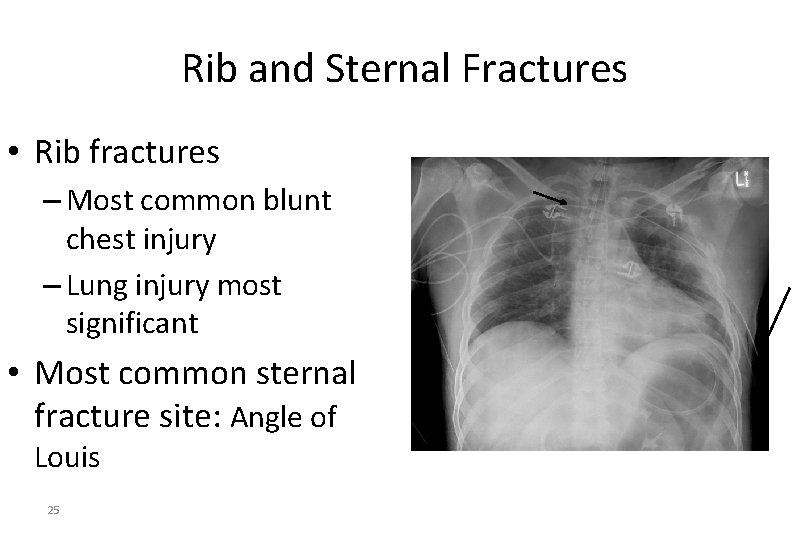
Rib and Sternal Fractures • Rib fractures – Most common blunt chest injury – Lung injury most significant • Most common sternal fracture site: Angle of Louis 25
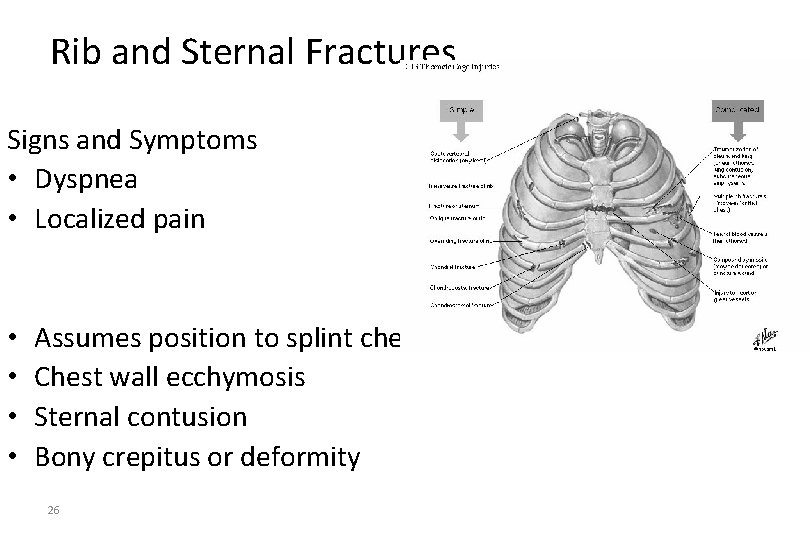
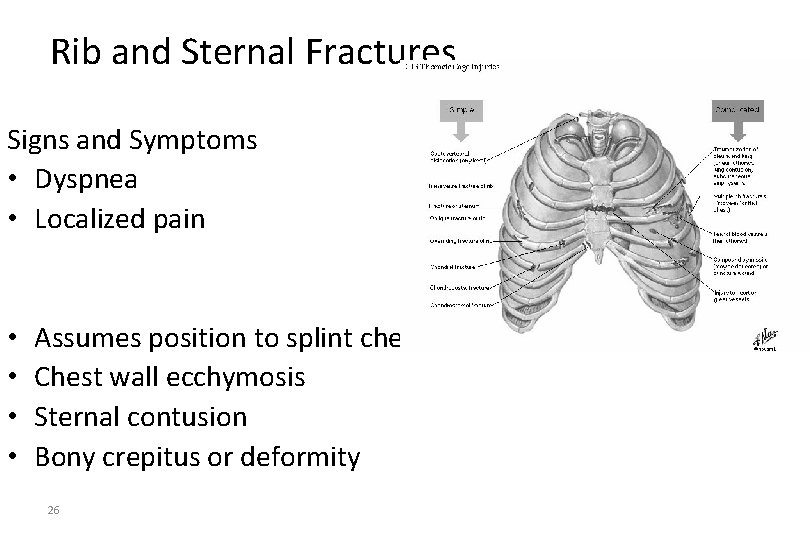
Rib and Sternal Fractures Signs and Symptoms • Dyspnea • Localized pain • • Assumes position to splint chest wall Chest wall ecchymosis Sternal contusion Bony crepitus or deformity 26

Management of the Chest Injury Patient • Rib Fractures – Consider analgesics for pain and to improve chest excursion • Versed • Morphine Sulfate – CONTRAINDICATION • Nitrous Oxide – May migrate into pleural or mediastinal space and worsen condition
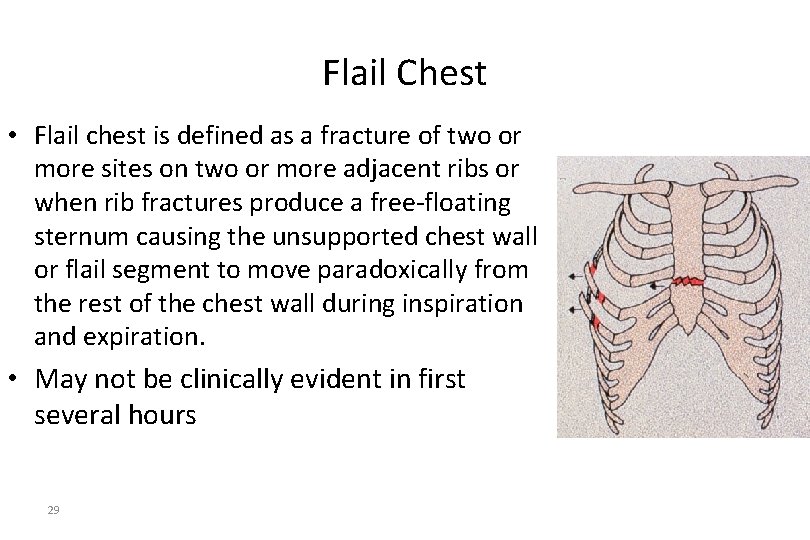
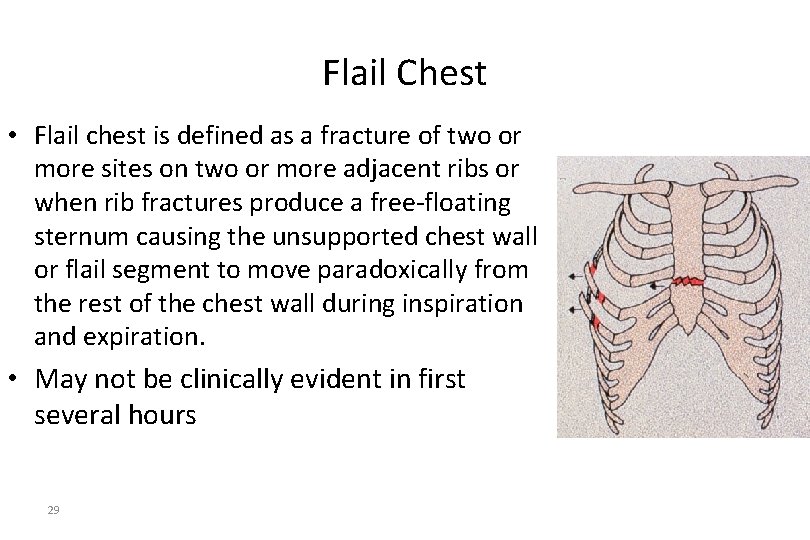
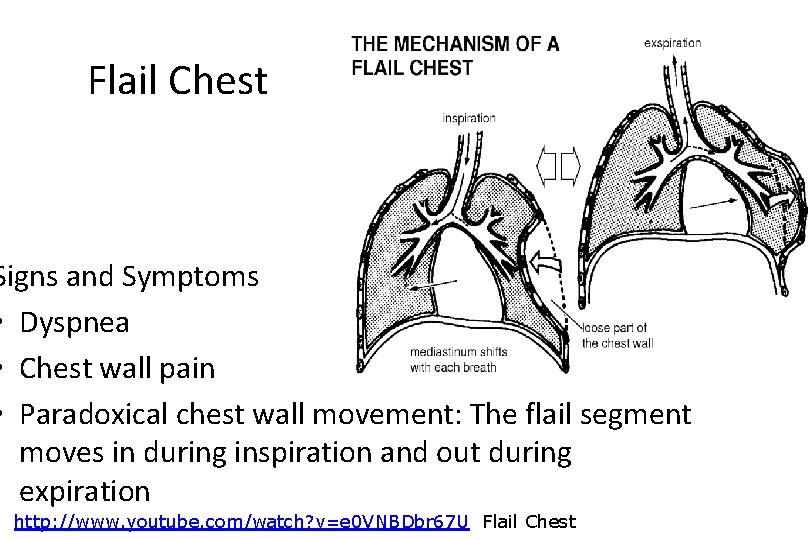
Flail Chest • Flail chest is defined as a fracture of two or more sites on two or more adjacent ribs or when rib fractures produce a free-floating sternum causing the unsupported chest wall or flail segment to move paradoxically from the rest of the chest wall during inspiration and expiration. • May not be clinically evident in first several hours 29
Pathophysiology of Thoracic Trauma Chest Wall Injuries • Flail Chest – Segment of the chest that becomes free to move with the pressure changes of respiration – Three or more adjacent rib fracture in two or more places – Serious chest wall injury with underlying pulmonary injury • Reduces volume of respiration • Adds to increased mortality – Paradoxical flail segment movement – Positive pressure ventilation can restore tidal volume
• A flail chest may be associated with the following: • Ineffective ventilation • Pulmonary contusion • Lacerated parenchyma • Flail chest may not be clinically evident in the first several hours because of muscle spasms that cause splinting.
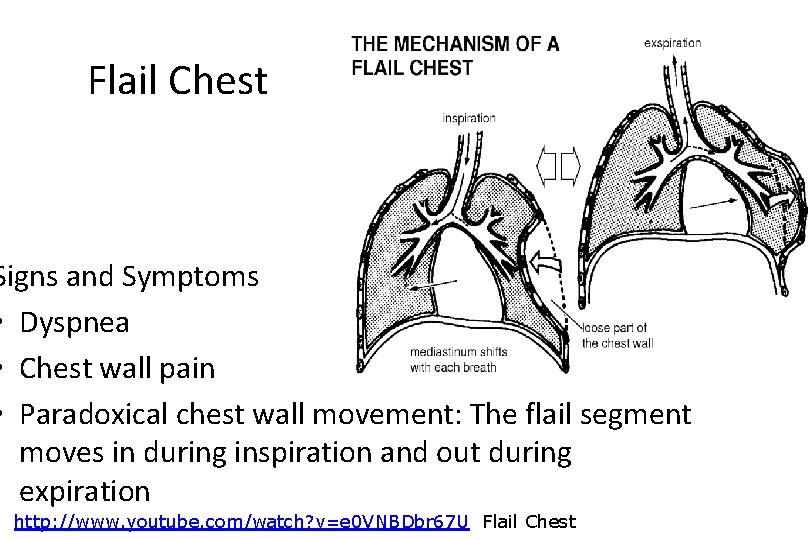
Flail Chest Signs and Symptoms • Dyspnea • Chest wall pain • Paradoxical chest wall movement: The flail segment moves in during inspiration and out during expiration http: //www. youtube. com/watch? v=e 0 VNBDbr 67 U Flail Chest
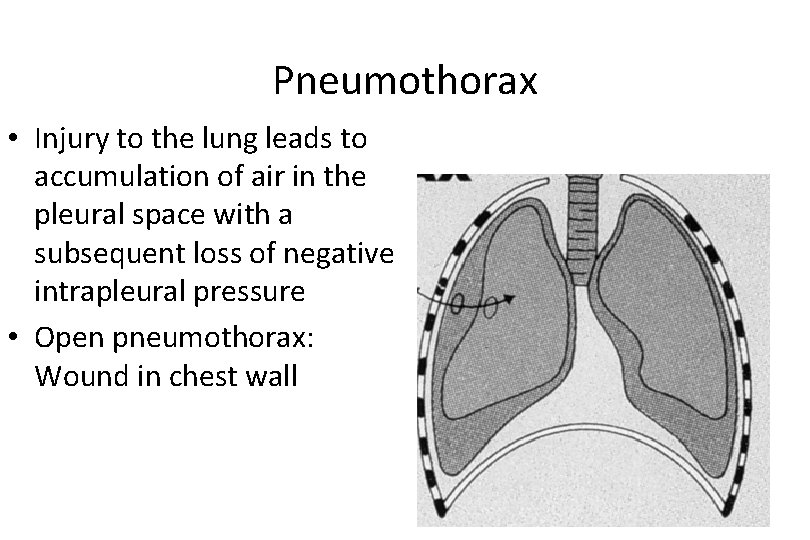
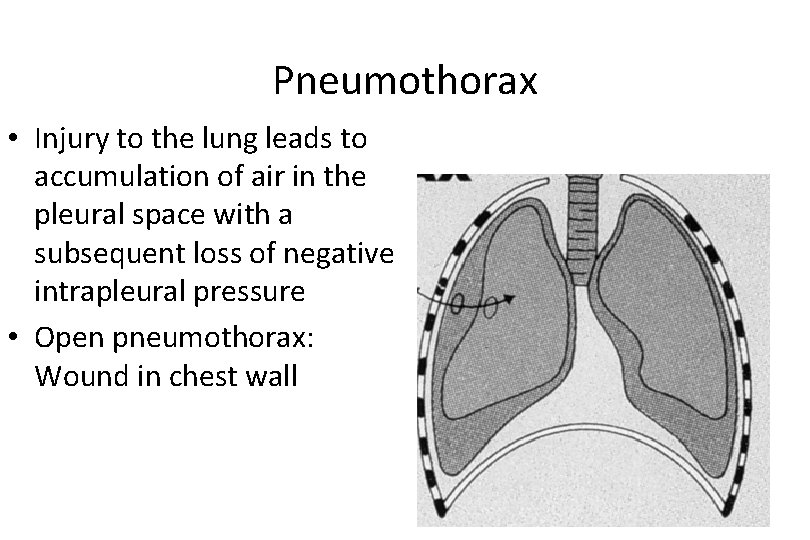
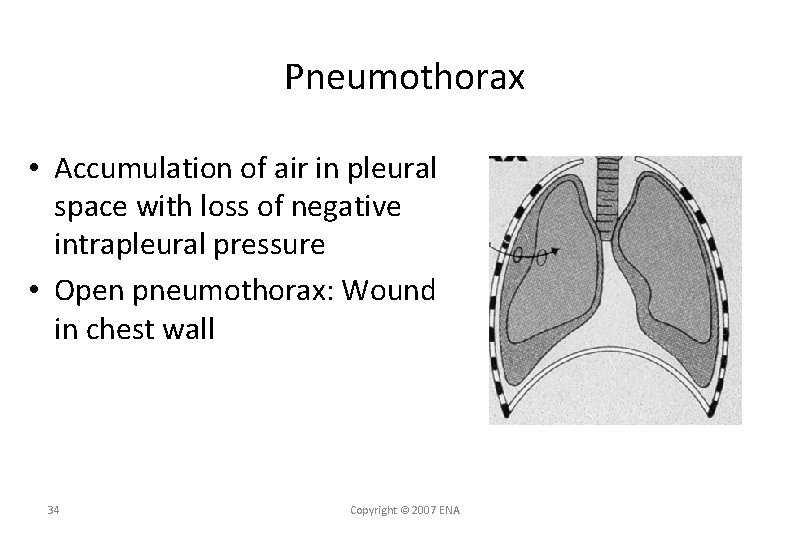
Pneumothorax • Injury to the lung leads to accumulation of air in the pleural space with a subsequent loss of negative intrapleural pressure • Open pneumothorax: Wound in chest wall
Pneumothorax • Accumulation of air in pleural space with loss of negative intrapleural pressure • Open pneumothorax: Wound in chest wall 34 Copyright © 2007 ENA
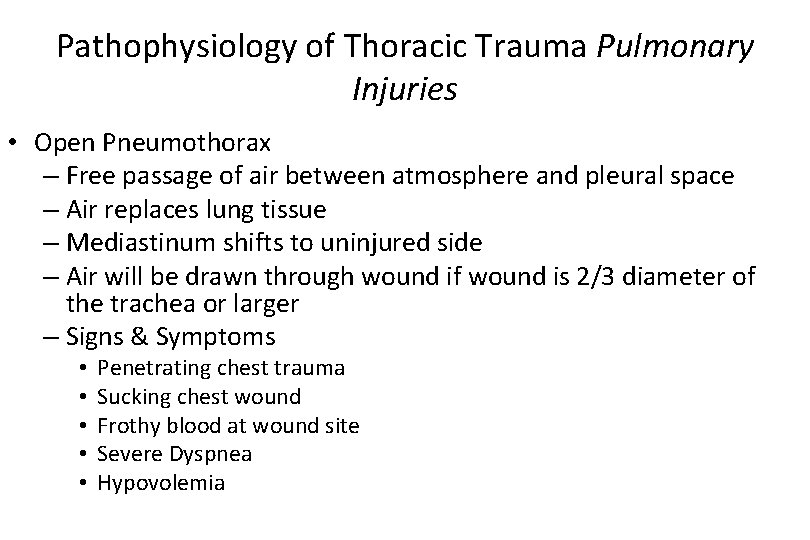
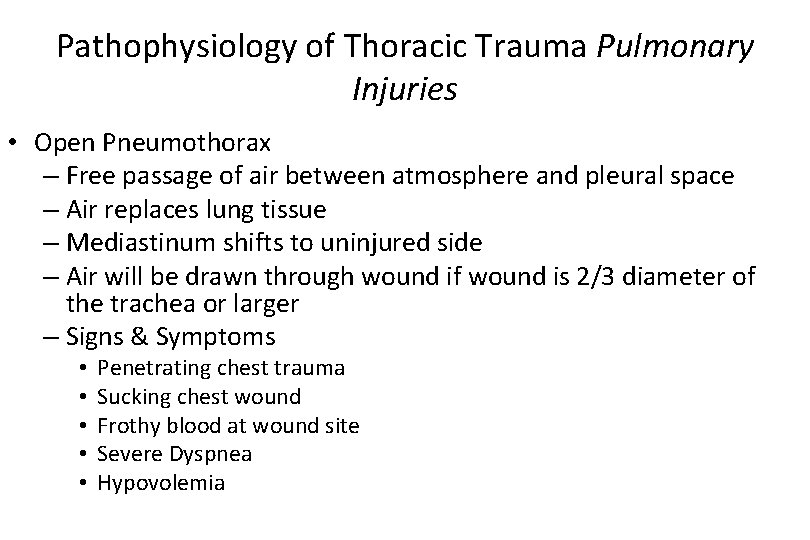
Pathophysiology of Thoracic Trauma Pulmonary Injuries • Open Pneumothorax – Free passage of air between atmosphere and pleural space – Air replaces lung tissue – Mediastinum shifts to uninjured side – Air will be drawn through wound if wound is 2/3 diameter of the trachea or larger – Signs & Symptoms • • • Penetrating chest trauma Sucking chest wound Frothy blood at wound site Severe Dyspnea Hypovolemia
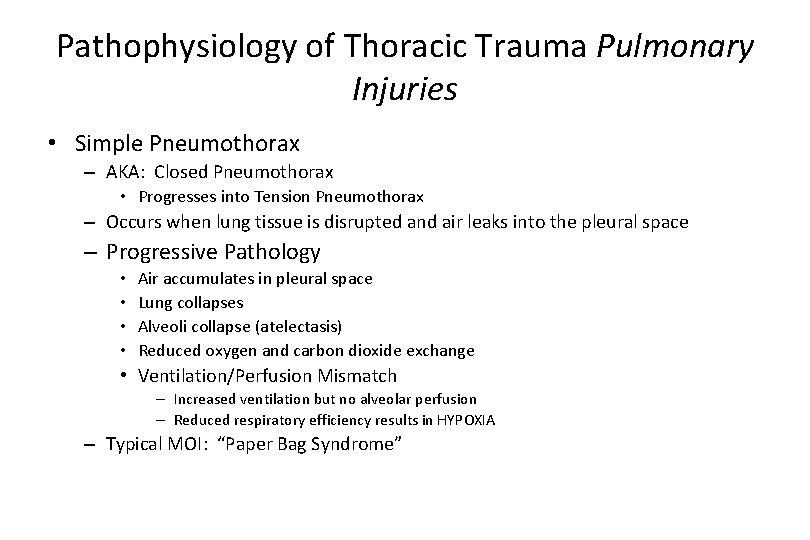
Pathophysiology of Thoracic Trauma Pulmonary Injuries • Simple Pneumothorax – AKA: Closed Pneumothorax • Progresses into Tension Pneumothorax – Occurs when lung tissue is disrupted and air leaks into the pleural space – Progressive Pathology • • Air accumulates in pleural space Lung collapses Alveoli collapse (atelectasis) Reduced oxygen and carbon dioxide exchange • Ventilation/Perfusion Mismatch – Increased ventilation but no alveolar perfusion – Reduced respiratory efficiency results in HYPOXIA – Typical MOI: “Paper Bag Syndrome”
Pneumothorax Signs and Symptoms • Dyspnea, tachypnea • Tachycardia • Hyperresonance on injured side • Decreased or absent breath sounds on the injured side • Chest pain • Open, sucking wound on inspiration (open pneumothorax)
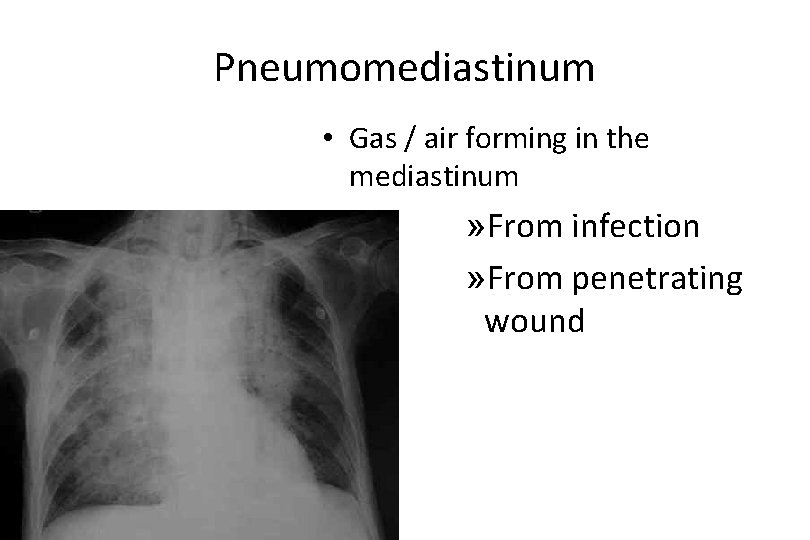
Pneumomediastinum • Gas / air forming in the mediastinum » From infection » From penetrating wound
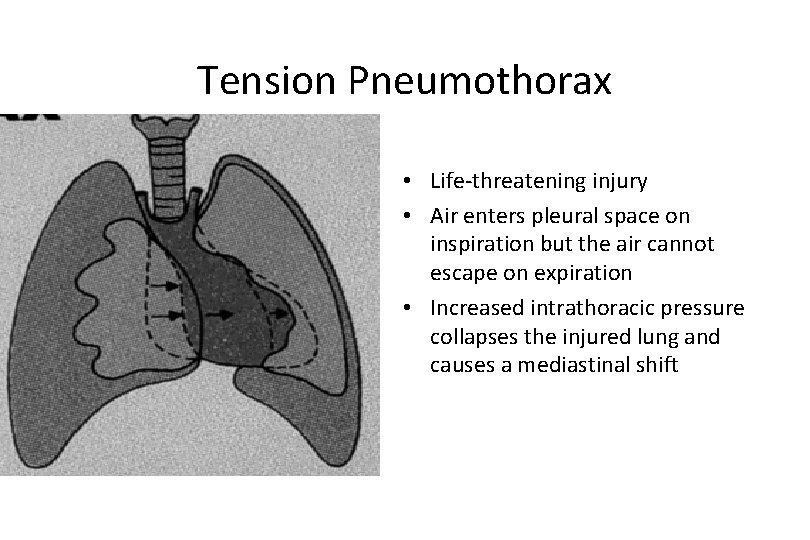
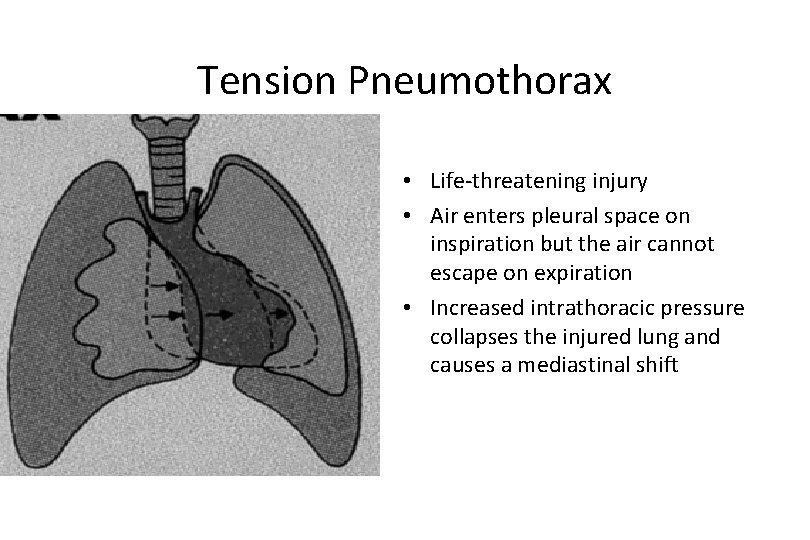
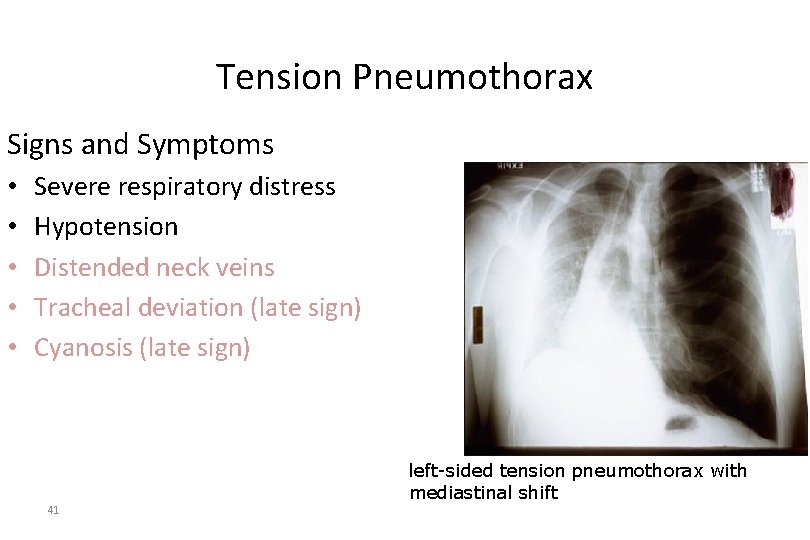
Tension Pneumothorax • Life-threatening injury • Air enters pleural space on inspiration but the air cannot escape on expiration • Increased intrathoracic pressure collapses the injured lung and causes a mediastinal shift
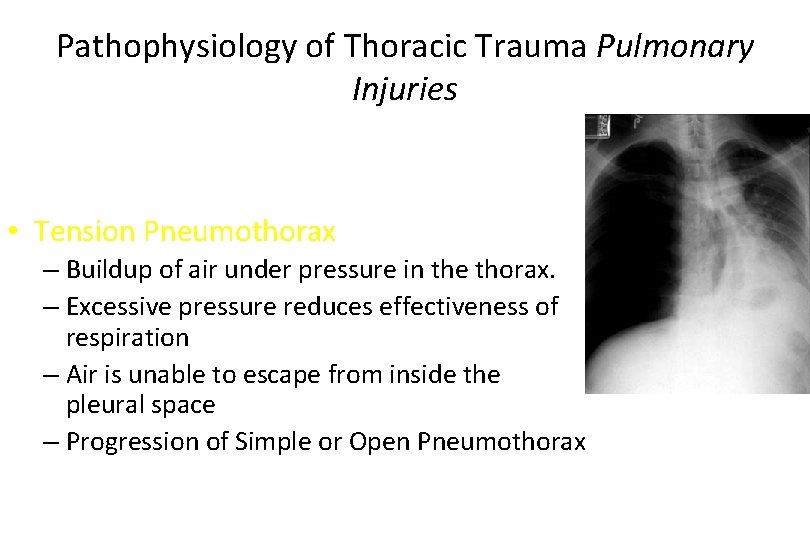
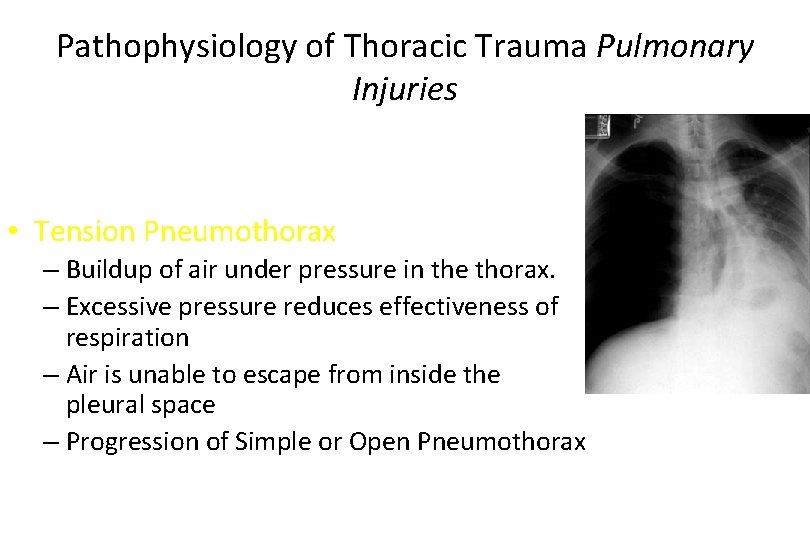
Pathophysiology of Thoracic Trauma Pulmonary Injuries • Tension Pneumothorax – Buildup of air under pressure in the thorax. – Excessive pressure reduces effectiveness of respiration – Air is unable to escape from inside the pleural space – Progression of Simple or Open Pneumothorax
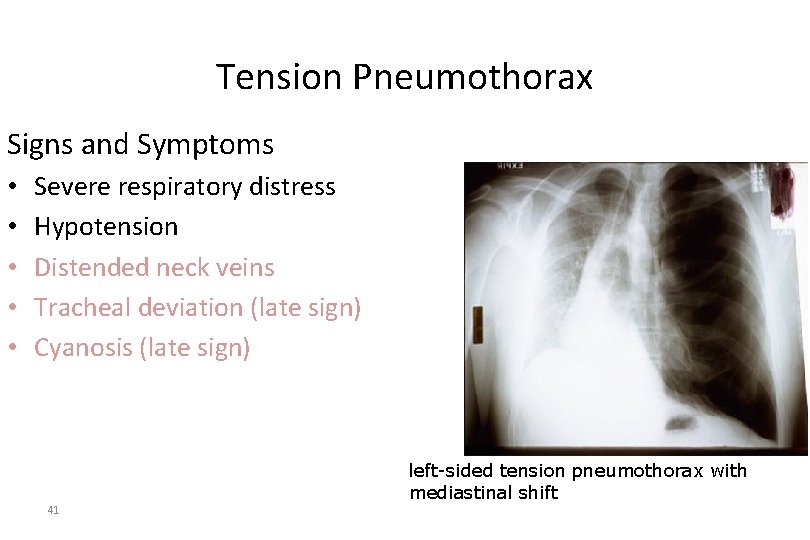
Tension Pneumothorax Signs and Symptoms • • • Severe respiratory distress Hypotension Distended neck veins Tracheal deviation (late sign) Cyanosis (late sign) 41 left-sided tension pneumothorax with mediastinal shift
Planning and Implementation • Ensure patent airway • Administer oxygen • Cover open chest wounds with a sterile, nonporous dressing and tape on three sides • IMMEDIATELY prepare for needle thoracentesis 42
Planning and Implementation Prepare for: • Chest tube insertion • Autotransfusion • Aggressive ventilatory support • Surgical intervention • Emergency thoracotomy 43
Management of the Chest Injury Patient • Tension Pneumothorax – Confirmation • Auscultaton & Percussion – Pleural Decompression • 2 nd intercostal space in mid-clavicular line – TOP OF RIB • Consider multiple decompression sites if patient remains symptomatic • Large over the needle catheter: 14 ga • Create a one-way-valve: Glove tip or Heimlich valve
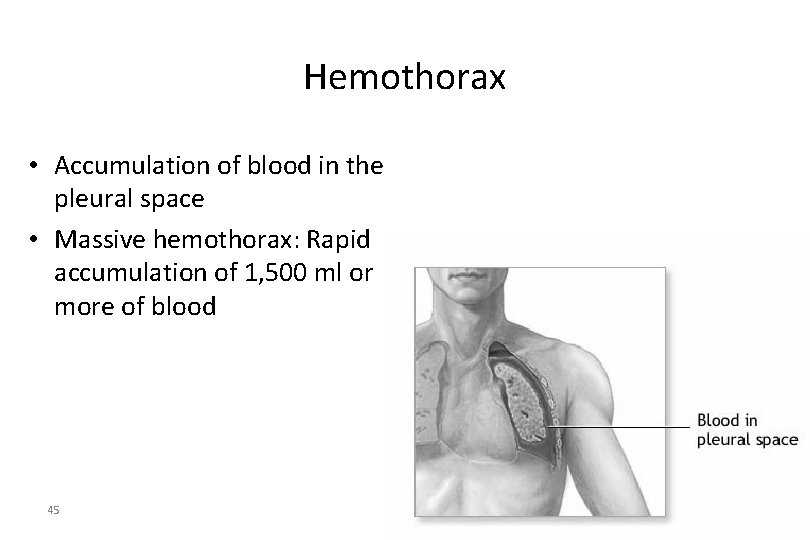
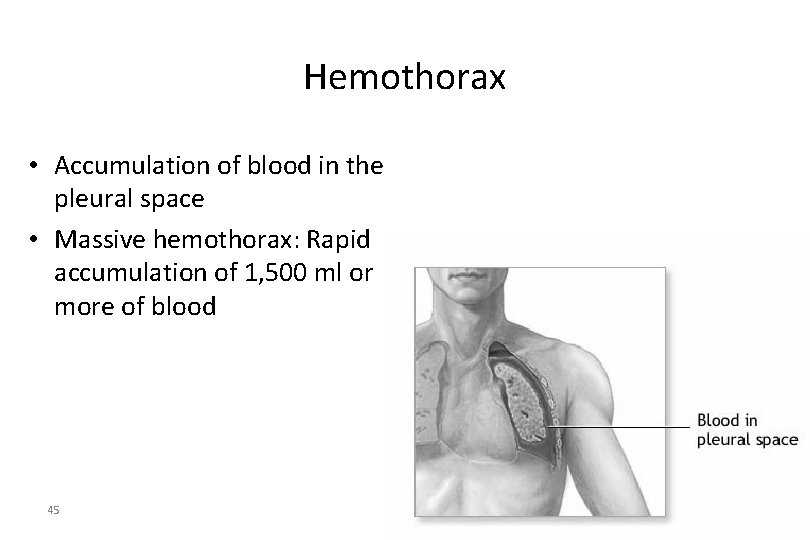
Hemothorax • Accumulation of blood in the pleural space • Massive hemothorax: Rapid accumulation of 1, 500 ml or more of blood 45
Pathophysiology of Thoracic Trauma Pulmonary Injuries • Hemothorax – Accumulation of blood in the pleural space – Serious hemorrhage may accumulate 1, 500 m. L of blood • Mortality rate of 75% • Each side of thorax may hold up to 3, 000 m. L – Blood loss in thorax causes a decrease in tidal volume • Ventilation/Perfusion Mismatch & Shock – Typically accompanies pneumothorax • Hemopneumothorax
Hemothorax Signs and Symptoms • Dyspnea, tachypnea • Tachycardia • Diaphoresis • Chest pain • Hypotension & Signs of shock • Decreased breath sounds on the injured side • Dullness to percussion on the injured side 47
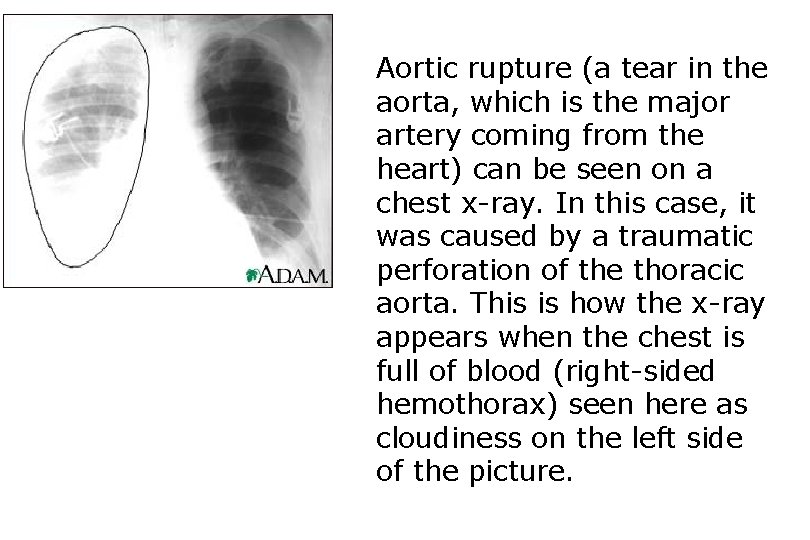
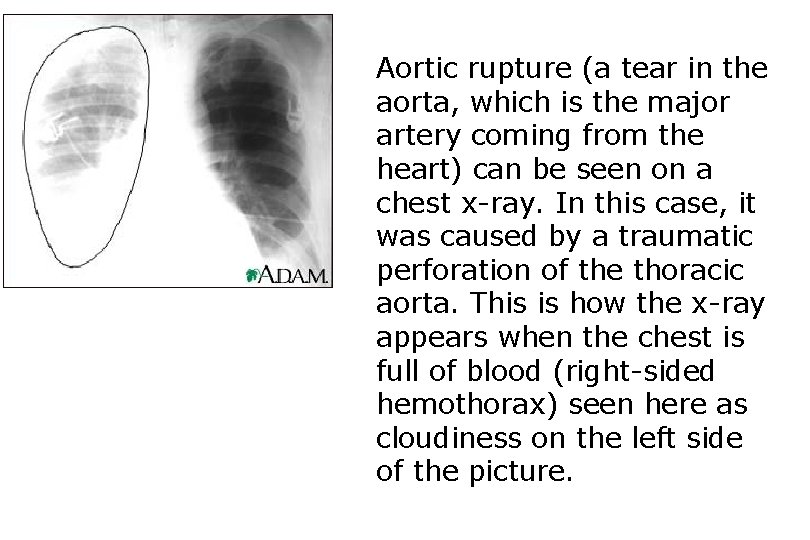
Aortic rupture (a tear in the aorta, which is the major artery coming from the heart) can be seen on a chest x-ray. In this case, it was caused by a traumatic perforation of the thoracic aorta. This is how the x-ray appears when the chest is full of blood (right-sided hemothorax) seen here as cloudiness on the left side of the picture.
Management of the Chest Injury Patient • Hemothorax – High flow O 2 – 2 large bore IV’s • Maintain SBP of 90 -100 • EVALUATE BREATH SOUNDS for fluid overload • Myocardial Contusion – Monitor ECG • Alert for dysrhythmias – IV if antidysrhythmics are needed
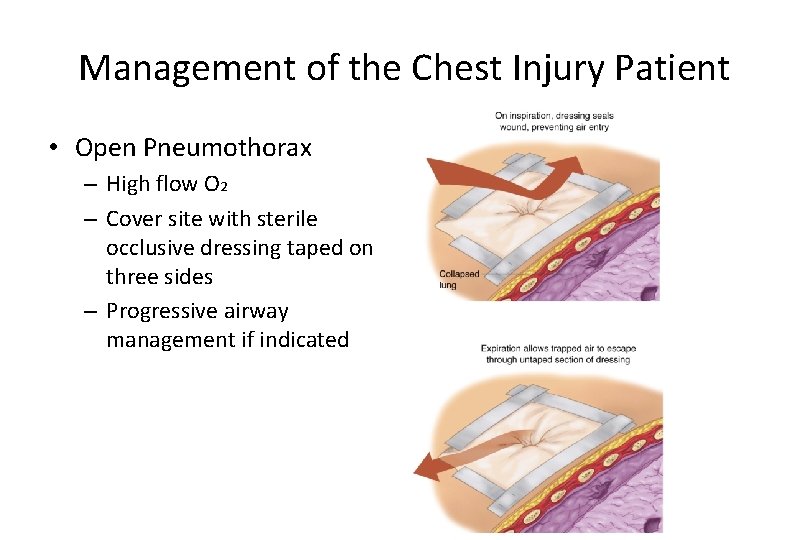
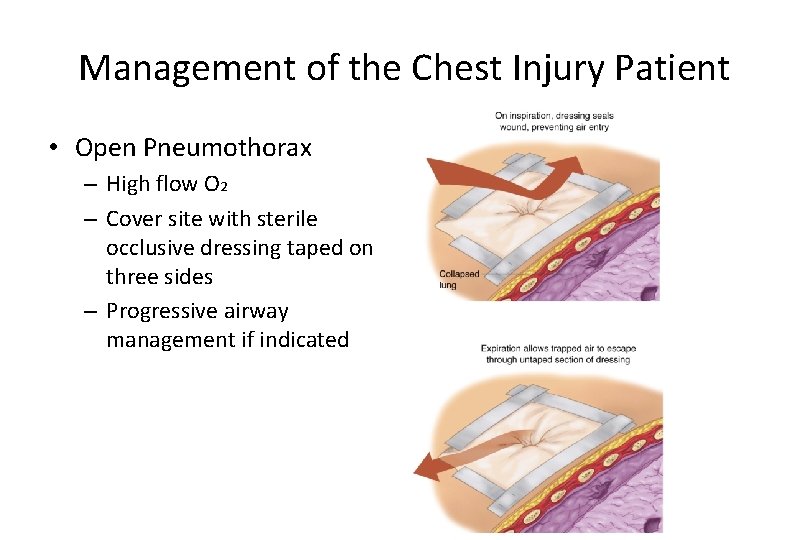
Management of the Chest Injury Patient • Open Pneumothorax – High flow O 2 – Cover site with sterile occlusive dressing taped on three sides – Progressive airway management if indicated
Pulmonary Contusion • Occurs as a result of direct impact, deceleration, high velocity bullet wounds • Respiratory insufficiency develops over time
Pathophysiology of Thoracic Trauma Pulmonary Injuries • Pulmonary Contusion – Soft tissue contusion of the lung – 30 -75% of patients with significant blunt chest trauma – Frequently associated with rib fracture – Typical MOI • Deceleration – Chest impact on steering wheel • Bullet Cavitation – High velocity ammunition – Micro hemorrhage may account for 1 - 1 ½ L of blood loss in alveolar tissue • Progressive deterioration of ventilatory status – Hemoptysis typically present
Pulmonary Contusion Signs and Symptoms • Dyspnea • Ineffective cough • Hemoptysis • Hypoxia • Chest pain • Chest wall contusion or abrasions
Ruptured Diaphragm • Potentially life-threatening • Left side more prone to injury • Results in respiratory compromise 54
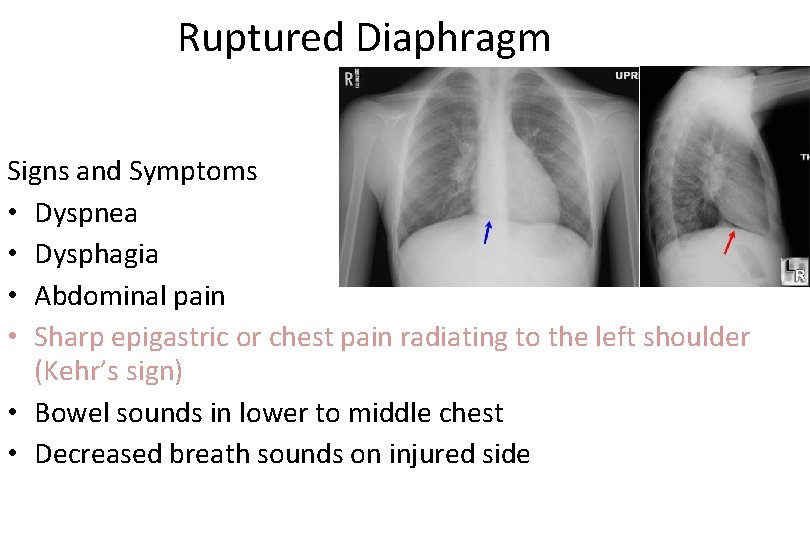
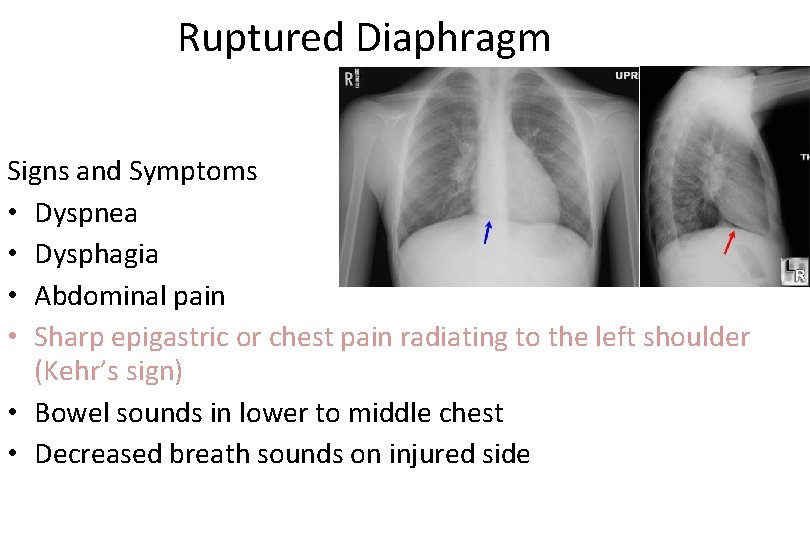
Ruptured Diaphragm Signs and Symptoms • Dyspnea • Dysphagia • Abdominal pain • Sharp epigastric or chest pain radiating to the left shoulder (Kehr’s sign) • Bowel sounds in lower to middle chest • Decreased breath sounds on injured side

Blunt Cardiac Injury • Formerly called cardiac contusion or cardiac concussion • Suspect following an associated mechanism of injury (motor vehicle crash) or in those patients with poor cardiovascular response to injury
Blunt Cardiac Injury Signs and Symptoms • ECG abnormalities from dysrhythmias – Premature ventricular contractions and AV blocks are the most common • Chest pain • Chest wall ecchymosis
Pathophysiology of Thoracic Trauma Cardiovascular Injuries • Myocardial Contusion – Occurs in 76% of patients with severe blunt chest trauma – Right Atrium and Ventricle is commonly injured – Injury may reduce strength of cardiac contractions • Reduced cardiac output – Electrical Disturbances due to irritability of damaged myocardial cells – Progressive Problems • Hematoma • Hemoperitoneum • Myocardial necrosis • Dysrhythmias • CHF & or Cardiogenic shock
Pathophysiology of Thoracic Trauma Cardiovascular Injuries Myocardial Contusion Signs & Symptoms • • Bruising of chest wall Tachycardia and/or irregular rhythm Retrosternal pain similar to MI Associated injuries – Rib/Sternal fractures • Chest pain unrelieved by oxygen – May be relieved with rest – THIS IS TRAUMA-RELATED PAIN • Similar signs and symptoms of medical chest pain
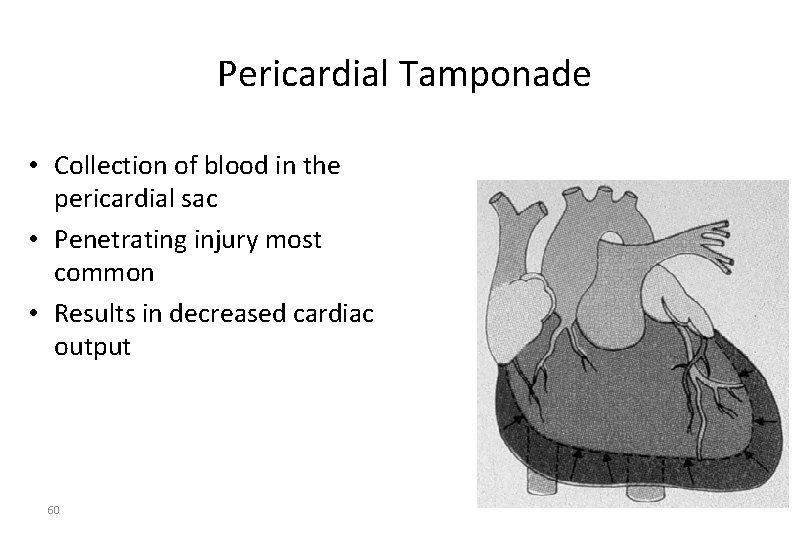
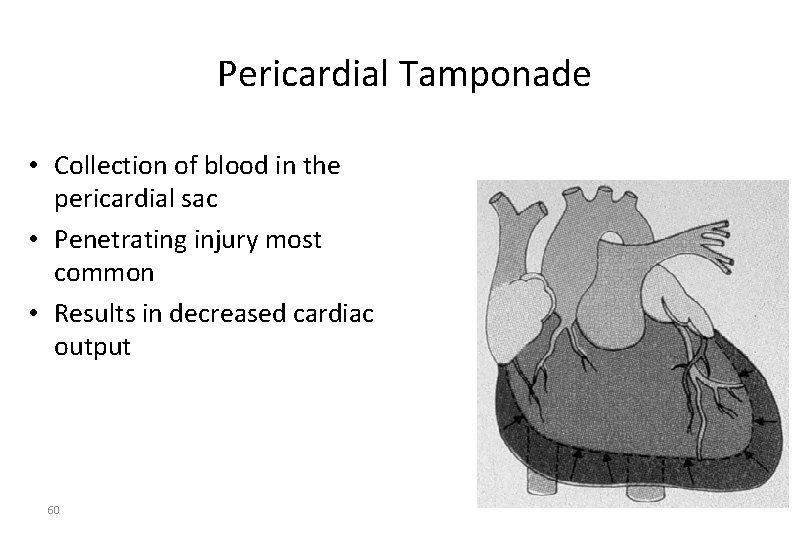
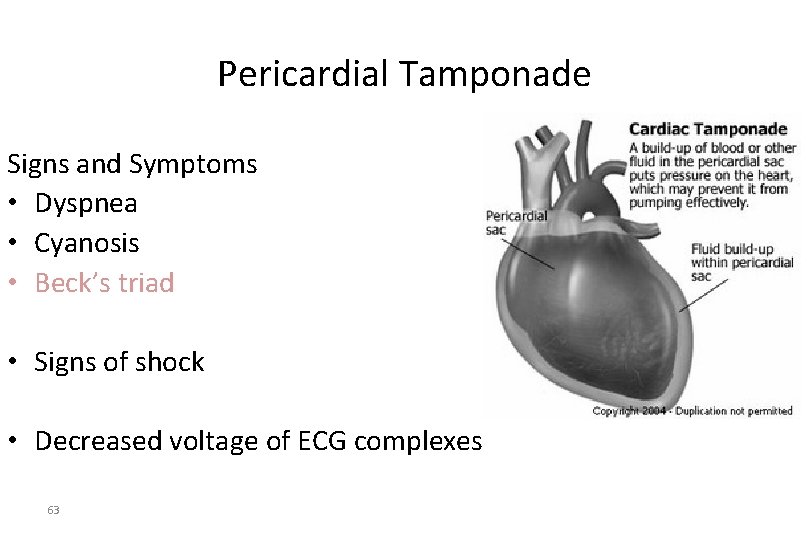
Pericardial Tamponade • Collection of blood in the pericardial sac • Penetrating injury most common • Results in decreased cardiac output 60
Pathophysiology of Thoracic Trauma Cardiovascular Injuries • Pericardial Tamponade – Restriction to cardiac filling caused by blood or other fluid within the pericardium – Occurs in <2% of all serious chest trauma • However, very high mortality – Results from tear in the coronary artery or penetration of myocardium • Blood seeps into pericardium and is unable to escape • 200 -300 ml of blood can restrict effectiveness of cardiac contractions – Removing as little as 20 ml can provide relief
Pathophysiology of Thoracic Trauma Cardiovascular Injuries Pericardial Tamponade Signs & Symptoms • Dyspnea • Possible cyanosis • Beck’s Triad – JVD – Distant heart tones – Hypotension or narrowing pulse pressure • Weak, thready pulse • Shock • Kussmaul’s sign – Decrease or absence of JVD during inspiration • Pulsus Paradoxus – Drop in SBP >10 during inspiration – Due to increase in CO 2 during inspiration • Electrical Alterans – P, QRS, & T amplitude changes in every other cardiac cycle • PEA
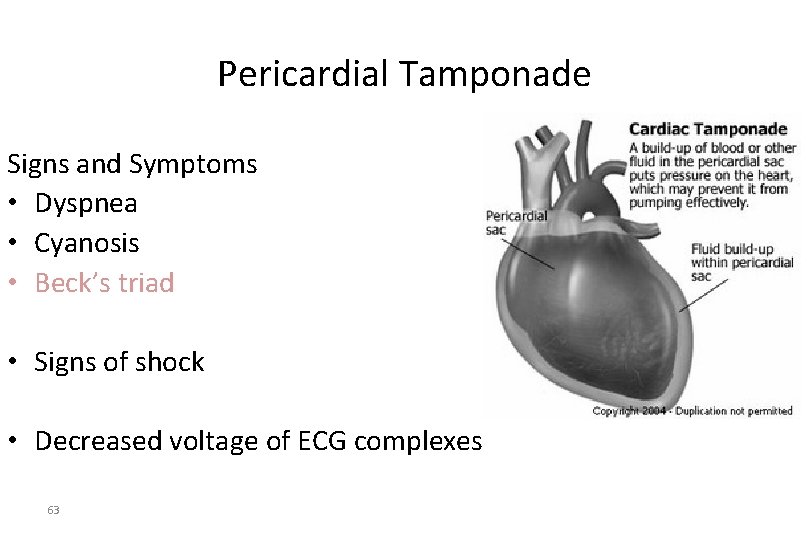
Pericardial Tamponade Signs and Symptoms • Dyspnea • Cyanosis • Beck’s triad • Signs of shock • Decreased voltage of ECG complexes 63
Management of the Chest Injury Patient • Pericardial Tamponade –High flow O 2 –IV therapy –Consider pericardiocentesis; rapidly deteriorating patient
Pericardiocentesis • <iframe width="420" height="315" src="http: //www. youtube. com/embed/n. S_VUNZTk. Y" frameborder="0" allowfullscreen></iframe>
Pathophysiology of Thoracic Trauma Cardiovascular Injuries • Myocardial Aneurysm or Rupture – Occurs almost exclusively with extreme blunt thoracic trauma – Secondary due to necrosis resulting from MI – Signs & Symptoms • Severe rib or sternal fracture • Possible signs and symptoms of cardiac tamponade • If affects valves only – Signs & symptoms of right or left heart failure • Absence of vital signs
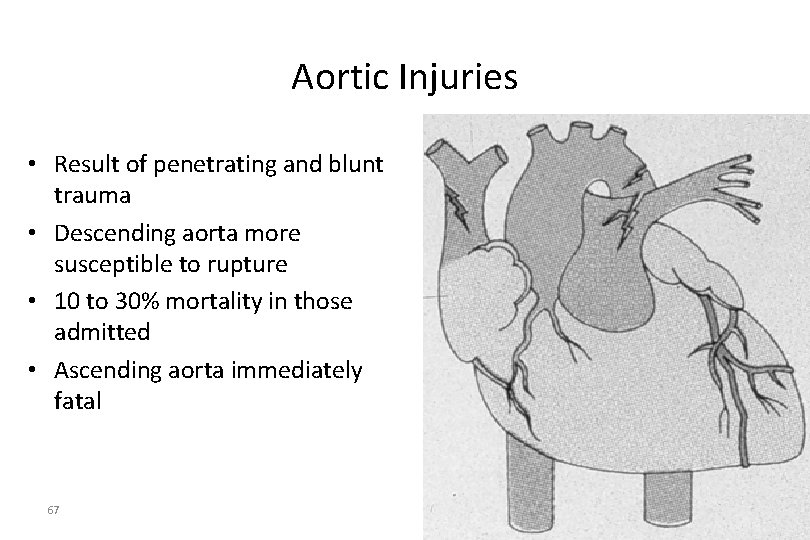
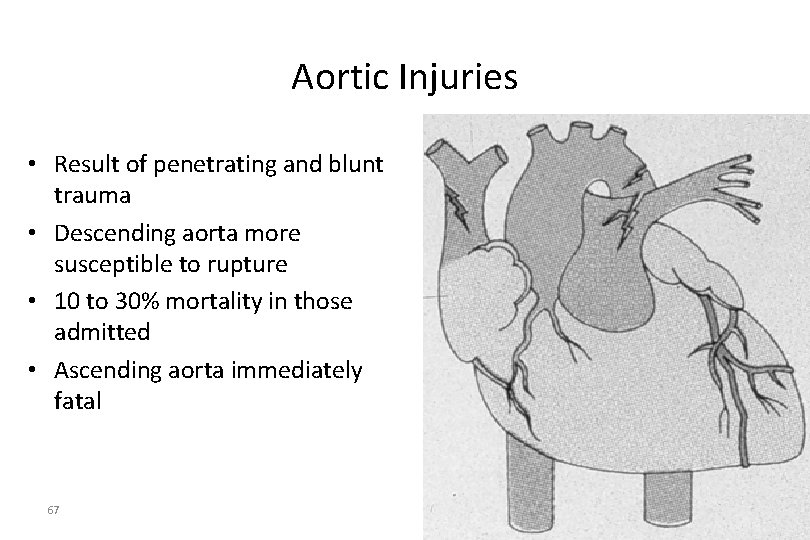
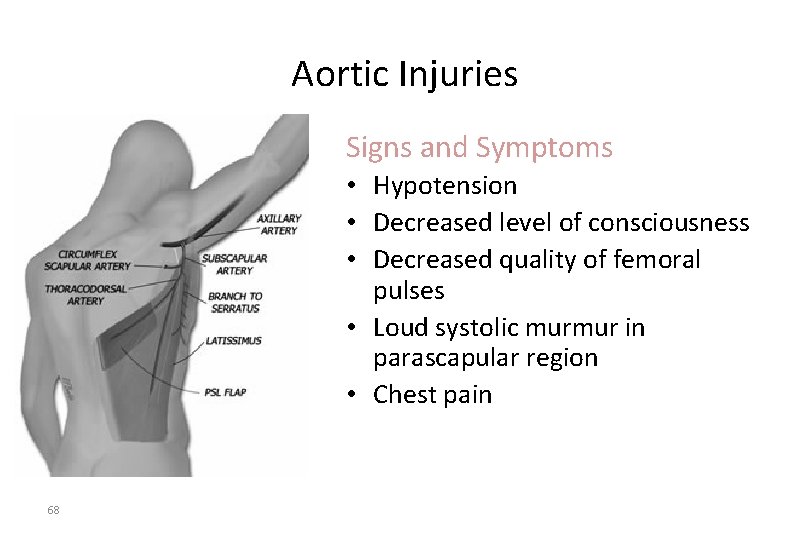
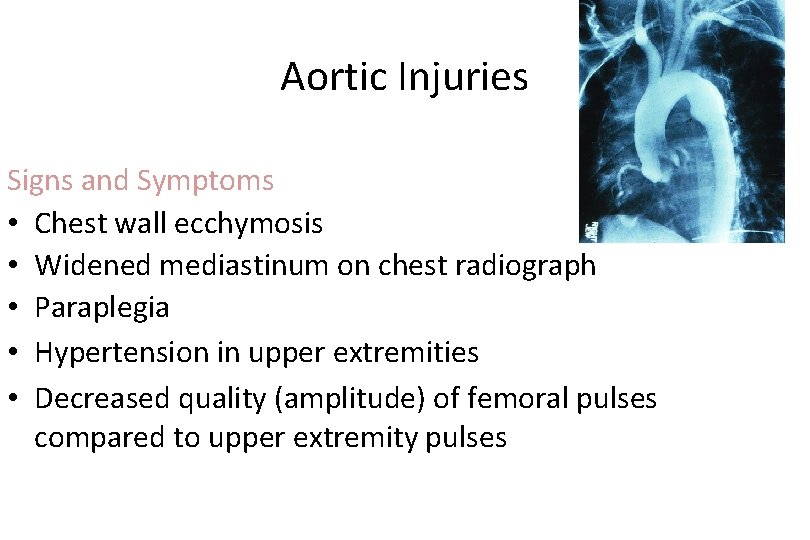
Aortic Injuries • Result of penetrating and blunt trauma • Descending aorta more susceptible to rupture • 10 to 30% mortality in those admitted • Ascending aorta immediately fatal 67
Aortic Injuries Signs and Symptoms • Hypotension • Decreased level of consciousness • Decreased quality of femoral pulses • Loud systolic murmur in parascapular region • Chest pain 68
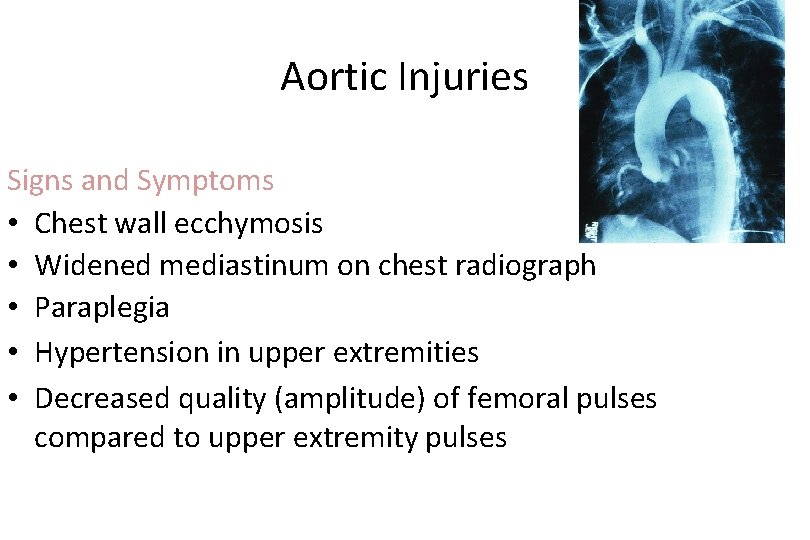
Aortic Injuries Signs and Symptoms • Chest wall ecchymosis • Widened mediastinum on chest radiograph • Paraplegia • Hypertension in upper extremities • Decreased quality (amplitude) of femoral pulses compared to upper extremity pulses
Aortic Aneurysm • AVOID jarring or rough handling • Initiate IV therapy enroute – Mild hypotension may be protective – Rapid fluid bolus if aneurysm ruptures • Keep patient calm
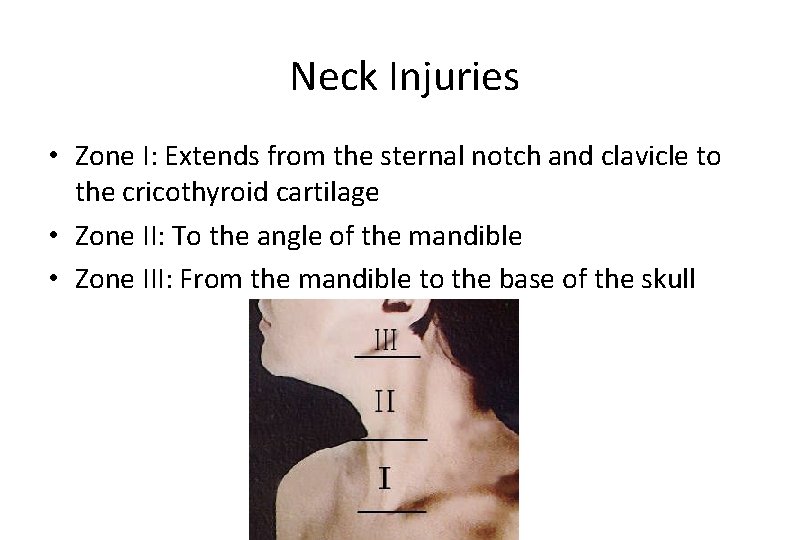
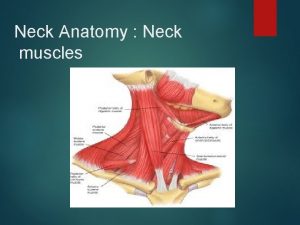
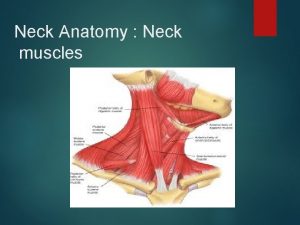
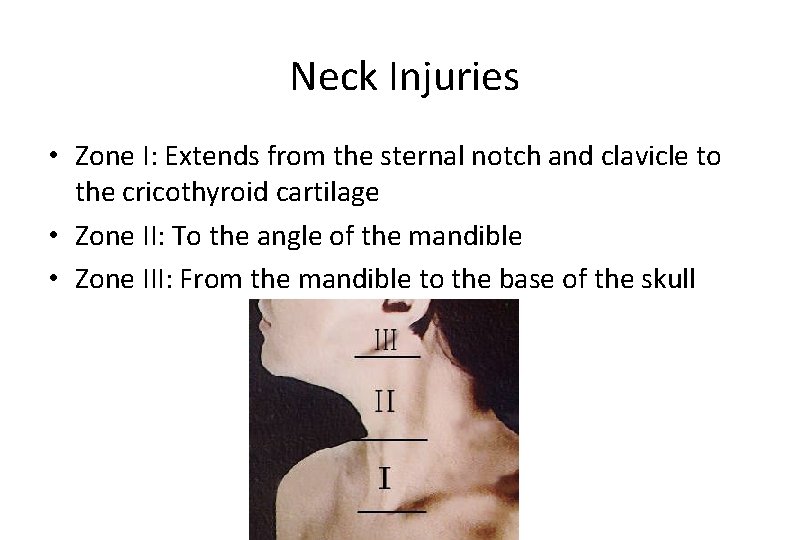
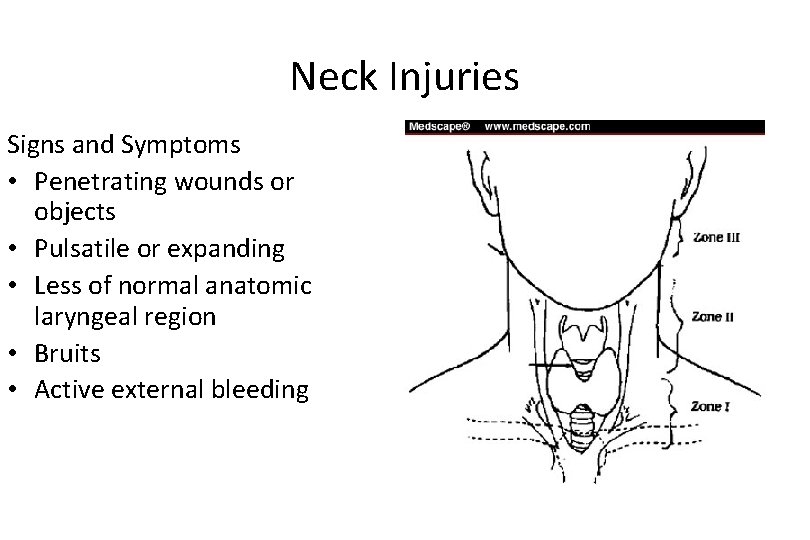
Neck Injuries • Zone I: Extends from the sternal notch and clavicle to the cricothyroid cartilage • Zone II: To the angle of the mandible • Zone III: From the mandible to the base of the skull
Neck Injuries • Zones Clinical Significance – Identification of structures potentially injured – Potential for surgery or observation – Potential to control bleeding
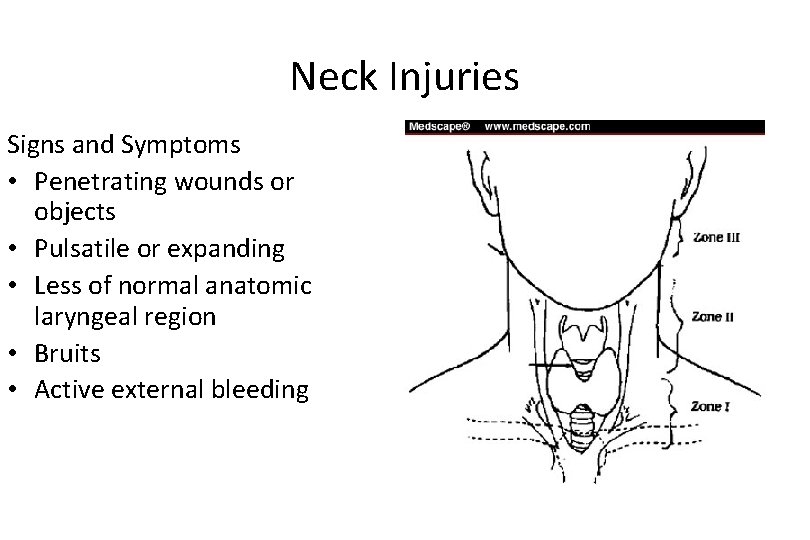
Neck Injuries Signs and Symptoms • Penetrating wounds or objects • Pulsatile or expanding • Less of normal anatomic laryngeal region • Bruits • Active external bleeding impaled hematomas prominence of the
Neck Injuries Signs and Symptoms (continued) • Neurologic deficit • Cranial nerve deficits • Facial sensory or motor nerve deficits • Subcutaneous emphysema • Dysphonia • Dysphagia
Nursing Interventions for a Neck Injury • Monitor for progressive airway edema • Control external bleeding with direct pressure • Monitor for continued bleeding and expanding hematomas
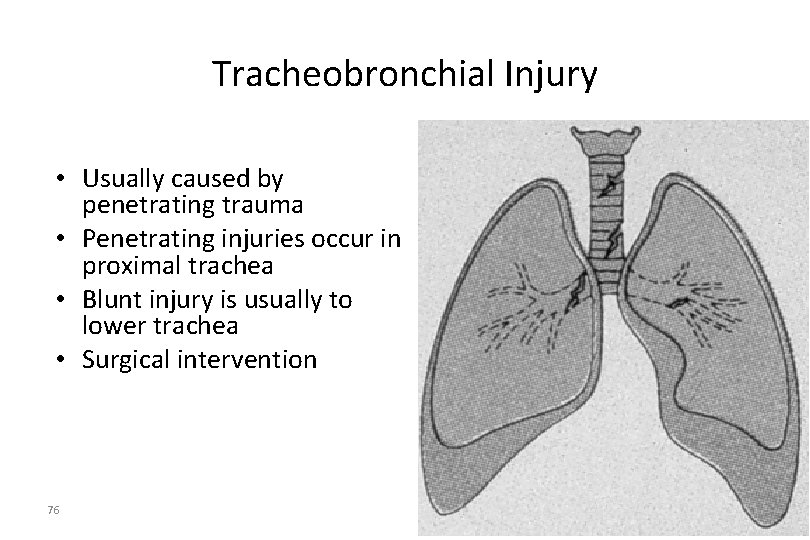
Tracheobronchial Injury • Usually caused by penetrating trauma • Penetrating injuries occur in proximal trachea • Blunt injury is usually to lower trachea • Surgical intervention 76
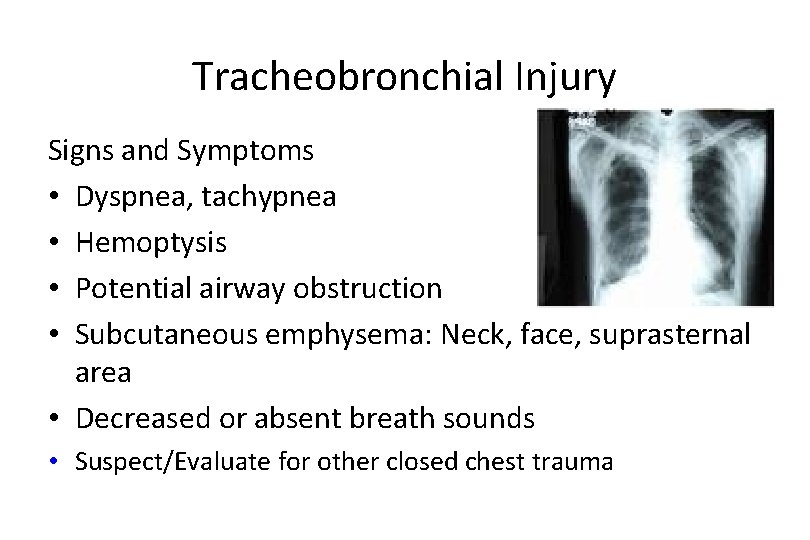
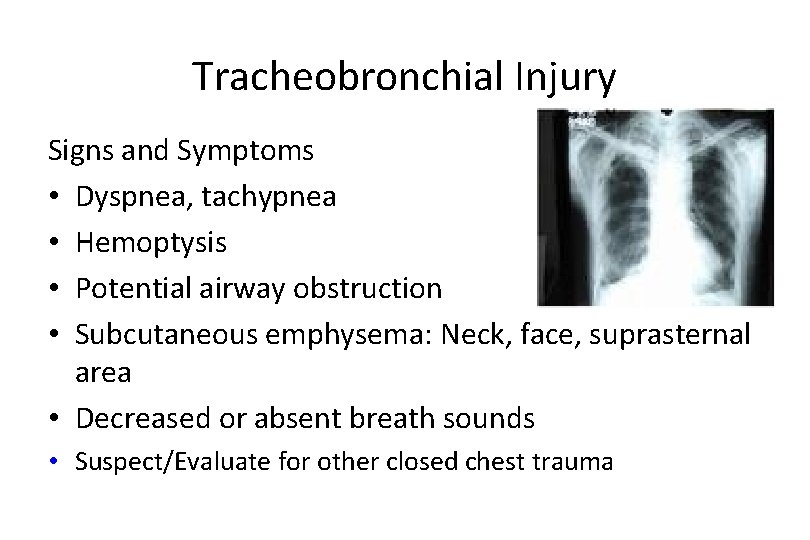
Tracheobronchial Injury Signs and Symptoms • Dyspnea, tachypnea • Hemoptysis • Potential airway obstruction • Subcutaneous emphysema: Neck, face, suprasternal area • Decreased or absent breath sounds • Suspect/Evaluate for other closed chest trauma
Tracheobronchial Injury • Support therapy – Keep airway clear – Administer high flow O 2 • Consider intubation if unable to maintain patient airway – Observe for development of tension pneumothorax and SQ emphysema
Nursing Care - Assessment History • What was the mechanism of injury? • What are the patient’s complaints? • What were the patient’s vital signs prior to admission?
Nursing Care Physical Assessment Inspection • Observe chest wall for injuries • Assess breathing effectiveness and rate • Observe chest wall for symmetrical movement • Inspect the neck for signs of trauma
Nursing Care Physical Assessment Inspection (continued) • Jugular veins • Zone of injury • Upper abdominal region for evidence of blunt or penetrating injury
Nursing Care Physical Assessment • Percuss the chest • Palpate – Chest wall, clavicles, neck for presence of bony crepitus – Central and peripheral pulses and compare quality – The trachea – Extremities for motor and sensory function
Nursing Care Physical Assessment Auscultation • Compare blood pressure in both upper and lower extremities • Breath sounds • Chest for bowel sounds • Heart sounds • Neck vessels for bruits
Diagnostic Procedures Radiographic Studies • • • Chest radiograph Arteriography Esophagoscopy Bronchoscopy and laryngoscopy Computerized tomography (CT) scan Focused assessment sonography for trauma (FAST) 84
Nursing Diagnoses • • Ineffective airway clearance Ineffective breathing pattern Impaired gas exchange Fluid volume deficit Decreased cardiac output Altered tissue perfusion Pain
Planning and Implementation • Ensure patent airway • Administer oxygen via a nonrebreather mask at a flow rate sufficient to keep the reservoir bag inflated, 12 to 15 L/min • Prepare for ventilatory support • Cover open chest wounds with a sterile, nonporous dressing and tape on three sides • IMMEDIATELY prepare for needle thoracentesis
Planning and Implementation • Prepare for: – Chest tube insertion – Aggressive ventilatory support – Surgical intervention – Emergency thoracotomy – Autotransfusion
Evaluation and Ongoing Assessment Monitor • Airway patency, respiratory effort, and arterial blood gases • Respiratory effort after covering wounds • Vital signs • Chest tube drainage
Management of the Chest Injury Patient • Sternoclavicular Dislocation – Supportive O 2 therapy – Evaluate for concomitant injury • Flail Chest – Place patient on side of injury • ONLY if spinal injury is NOT suspected – Expose injury site – Dress with bulky bandage against flail segment • Stabilizes fracture site – High flow O 2 • Consider PPV or ET if decreasing respiratory status – DO NOT USE SANDBAGS TO STABILIZE FX
Management of the Chest Injury Patient • Traumatic Asphyxia – Support airway • Provide O 2 • PPV with BVM to assure adequate ventilation – 2 large bore IV’s – Evaluate and treat for concomitant injuries – If entrapment > 20 min with chest compression • Consider 1 m. Eq/kg of Sodium Bicarbonate
Planning and Implementation • Stabilize impaled objects • Cannulate 2 veins with large bore 14 - or 16 -gauge catheters and infuse lactated Ringer’s solution • Pericardiocentesis, as indicated • Assist with emergency department thoracotomy • Monitor and treat cardiac dysrhythmias • Administer analgesic medications
Diagnostic Procedures • Laboratory Studies – Cardiac enzymes • Other – Electrocardiogram – Central venous pressure – Echocardiography 92
Evaluation and Ongoing Assessment • Airway patency and respiratory effort – Respiratory effort after covering wounds • Vital signs • Chest tube drainage –FOCA –DOPE 93
Planning and Implementation • • • 94 Stabilize impaled objects Initiate two large-caliber intravenous catheters Assist with pericardiocentesis Monitor and treat cardiac dysrhythmias Administer analgesic medications
 Thesourceagents
Thesourceagents Nutritional epidemiology definition
Nutritional epidemiology definition Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology How to calculate incidence rate example
How to calculate incidence rate example Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Person place and time model in epidemiology
Person place and time model in epidemiology Contoh relative risk
Contoh relative risk Logistic regression epidemiology
Logistic regression epidemiology Prevalence calculation
Prevalence calculation Classification of epidemiological studies
Classification of epidemiological studies Attack rate epidemiology formula
Attack rate epidemiology formula Pros and cons of cross sectional study
Pros and cons of cross sectional study Association vs causality
Association vs causality Formula for attack rate
Formula for attack rate Rambo critical appraisal tool
Rambo critical appraisal tool Wheel of causation example
Wheel of causation example Percentage defination
Percentage defination Defination of epidemiology
Defination of epidemiology Distribution in epidemiology
Distribution in epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association in epidemiology
Spurious association in epidemiology Field epidemiology ppt
Field epidemiology ppt Level of prevention
Level of prevention Gordon nichols
Gordon nichols Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Distribution in epidemiology
Distribution in epidemiology Confounding vs effect modification
Confounding vs effect modification Distribution in epidemiology
Distribution in epidemiology Ramboman
Ramboman Define epidemiology
Define epidemiology Prevalence
Prevalence How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Nutritional epidemiology
Nutritional epidemiology Mp test for malaria
Mp test for malaria Attack rate epidemiology
Attack rate epidemiology How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Epidemiology definition
Epidemiology definition Define epidemiology
Define epidemiology Epidemiological triad
Epidemiological triad Celiac beri beri
Celiac beri beri Epidemiology made easy
Epidemiology made easy Dorsal cavity
Dorsal cavity Abdominopelvic cavity regions
Abdominopelvic cavity regions Thoracic membranes and cavities
Thoracic membranes and cavities Difference between cervical thoracic and lumbar vertebrae
Difference between cervical thoracic and lumbar vertebrae Flat thoracic spine
Flat thoracic spine Blood supply to thoracic wall
Blood supply to thoracic wall Superficial fascia of thorax
Superficial fascia of thorax Arteries of thoracic wall
Arteries of thoracic wall Sibson's fascia
Sibson's fascia Superficial lymph nodes abdomen
Superficial lymph nodes abdomen Anterior lumbar counterstrain points
Anterior lumbar counterstrain points Portal and caval venous system
Portal and caval venous system Where is the sternal notch
Where is the sternal notch Facet joint anatomy
Facet joint anatomy Pig thoracic cavity diagram
Pig thoracic cavity diagram Intercostal artery
Intercostal artery Thoracic inlet x ray
Thoracic inlet x ray Cupola diaphragm
Cupola diaphragm Thoracic kyphosis
Thoracic kyphosis Gr chest 2 projections
Gr chest 2 projections Branches of aorta
Branches of aorta Thoracic membranes
Thoracic membranes British thoracic society oxygen guidelines
British thoracic society oxygen guidelines Angle of louis
Angle of louis Tactile fremitus
Tactile fremitus The purified lymph with lymphocytes and antibodies added
The purified lymph with lymphocytes and antibodies added Thorcic spine
Thorcic spine Pulmonary aortic window
Pulmonary aortic window Layers of chest wall
Layers of chest wall Posterior mediastinum contents
Posterior mediastinum contents Thoracic outlet wedge pillow
Thoracic outlet wedge pillow Neurogeen thoracic outlet syndroom
Neurogeen thoracic outlet syndroom Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Transverse costal facet
Transverse costal facet Rib tubercle
Rib tubercle Thoracodorsal nerve supplies
Thoracodorsal nerve supplies Muscles of thoracic spine
Muscles of thoracic spine Thoracic cavity labeled
Thoracic cavity labeled Thoracic duct
Thoracic duct Thoracic cage anterior view
Thoracic cage anterior view Volume of thoracic cavity
Volume of thoracic cavity Thoracic vertebrae superior view
Thoracic vertebrae superior view Thoracic duct
Thoracic duct Thoracic cavity
Thoracic cavity Thoracolumbar fascia
Thoracolumbar fascia Intercostal space
Intercostal space Cervical lateral flexion
Cervical lateral flexion Canal cervicoaxilar
Canal cervicoaxilar Jugular notch
Jugular notch Thoracic surgeon
Thoracic surgeon Soft spongy cone shaped organs in the thoracic cavity
Soft spongy cone shaped organs in the thoracic cavity Mitral stenosis chest x ray
Mitral stenosis chest x ray Thoracic mri images
Thoracic mri images