Surgery in Chronic Pulmonary Aspergillosis Mr Rajesh Shah


- Slides: 20
Surgery in Chronic Pulmonary Aspergillosis Mr. Rajesh Shah
Intended Learning Outcomes 1. What Is Chronic Pulmonary Aspergillosis? 2. How Is CPA Managed ? 3. What’s The Prognosis Of CPA? 4. Is There Any Role For Surgery?
What is CPA? 1. A spectrum of disease entity characterised by slow and progressive destruction of the lung. 2. Patients are non-immunocompromised or slightly immunocompromised. 3. Patients usually have previous or current chronic lung disease (TB, NTM, COPD, etc. ) 4. Formation of new cavities or expansion of the existing ones +/- fungal ball or nodule
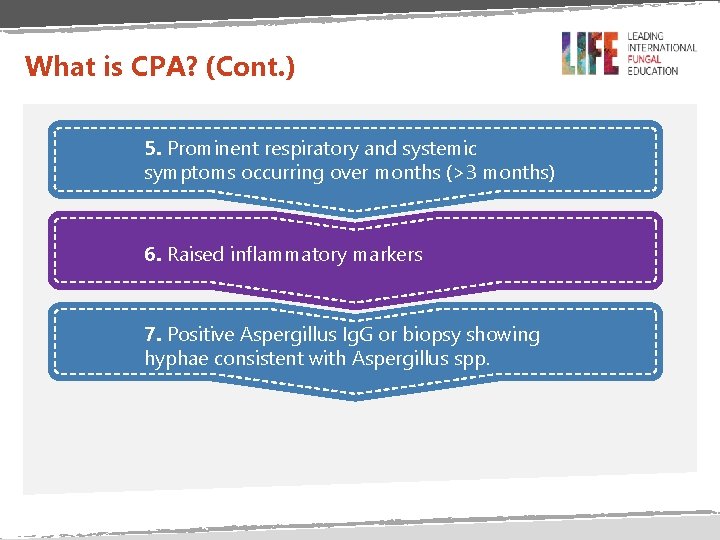
What is CPA? (Cont. ) 5. Prominent respiratory and systemic symptoms occurring over months (>3 months) 6. Raised inflammatory markers 7. Positive Aspergillus Ig. G or biopsy showing hyphae consistent with Aspergillus spp.
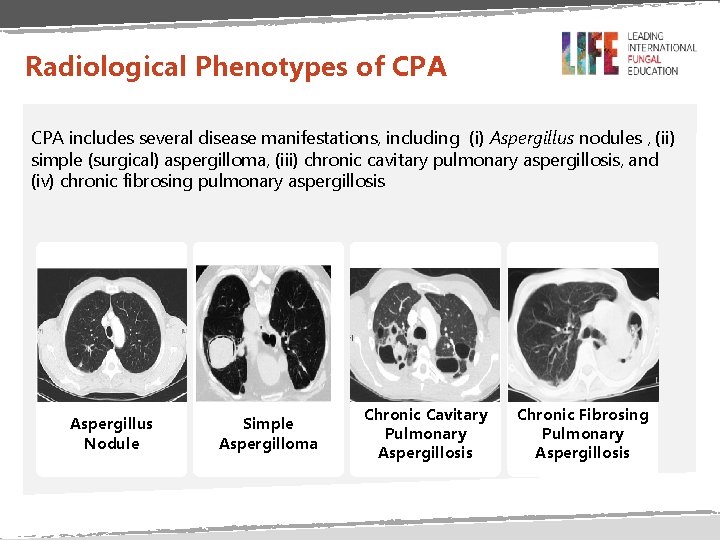
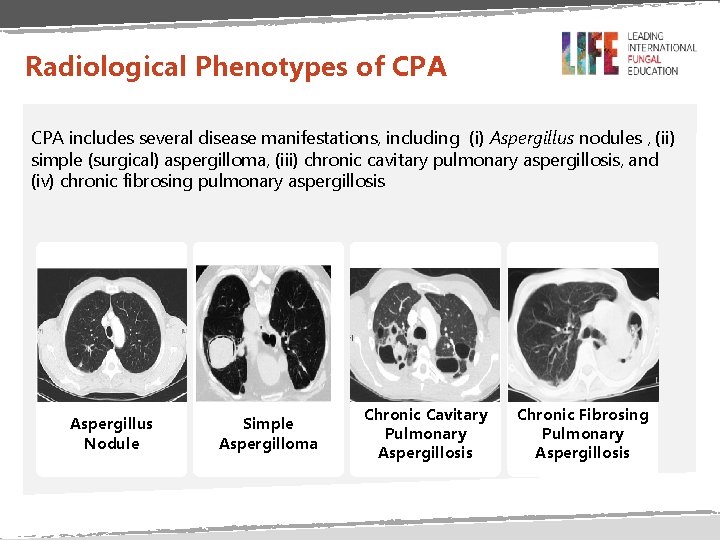
Radiological Phenotypes of CPA includes several disease manifestations, including (i) Aspergillus nodules , (ii) simple (surgical) aspergilloma, (iii) chronic cavitary pulmonary aspergillosis, and (iv) chronic fibrosing pulmonary aspergillosis Aspergillus Nodule Simple Aspergilloma Chronic Cavitary Pulmonary Aspergillosis Chronic Fibrosing Pulmonary Aspergillosis
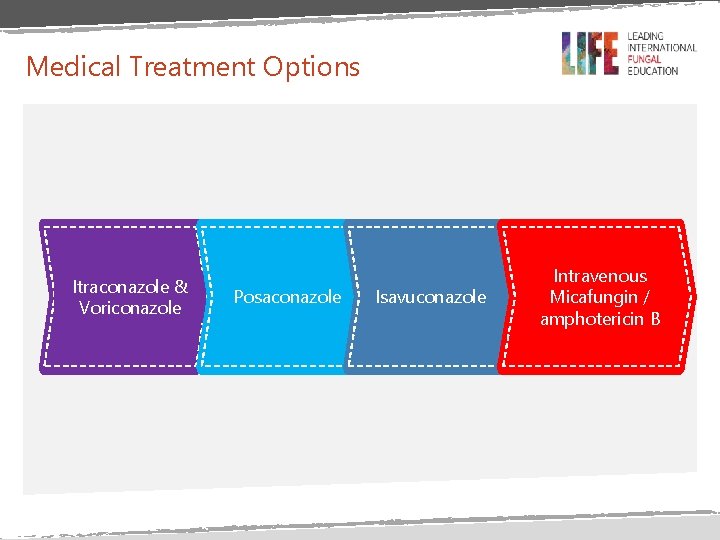
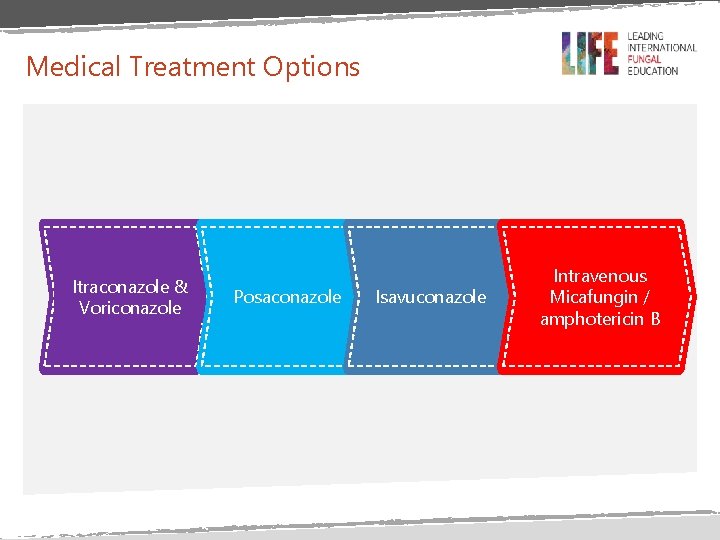
Medical Treatment Options Itraconazole & Voriconazole Posaconazole Isavuconazole Intravenous Micafungin / amphotericin B
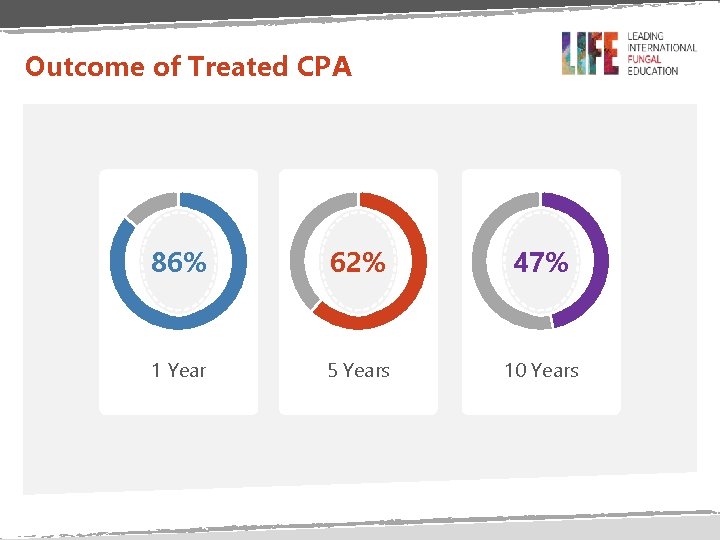
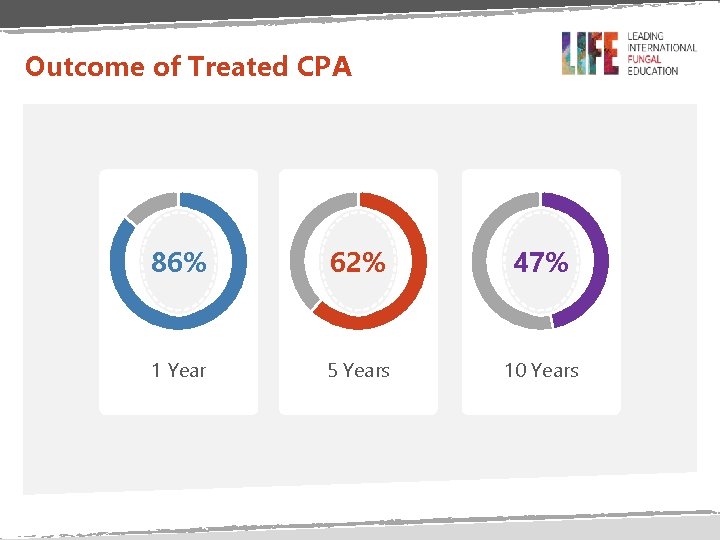
Outcome of Treated CPA 86% 62% 47% 1 Year 5 Years 10 Years
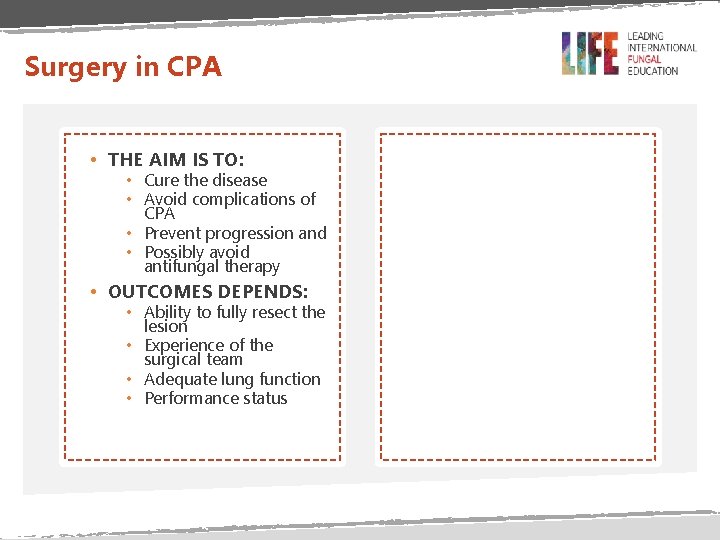
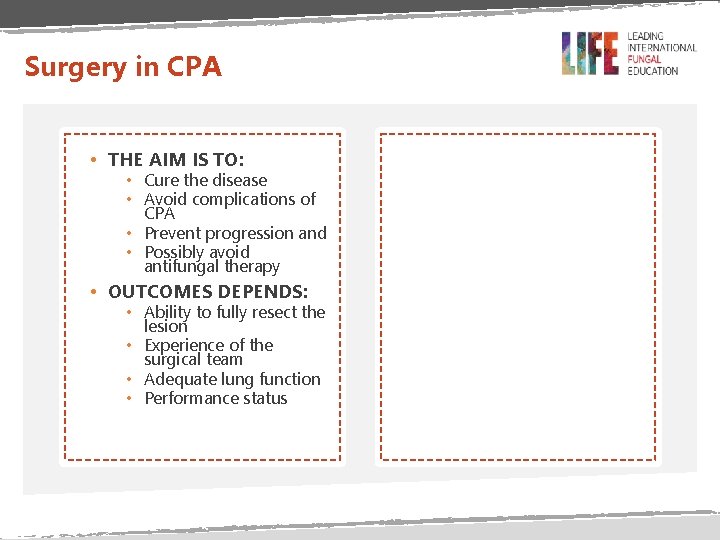
Surgery in CPA • THE AIM IS TO: • Cure the disease • Avoid complications of CPA • Prevent progression and • Possibly avoid antifungal therapy • OUTCOMES DEPENDS: • Ability to fully resect the lesion • Experience of the surgical team • Adequate lung function • Performance status
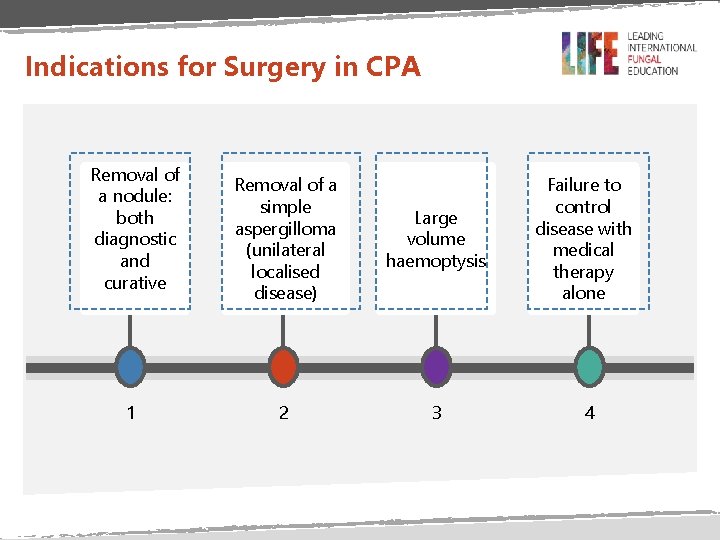
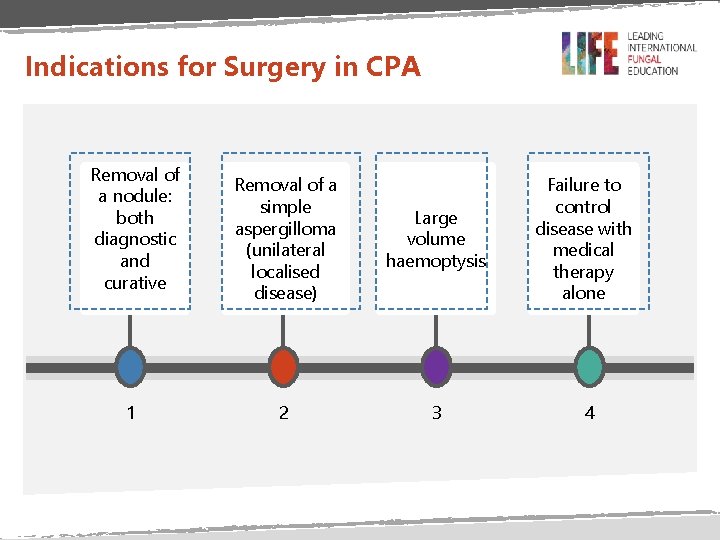
Indications for Surgery in CPA Removal of a nodule: both diagnostic and curative 1 Removal of a simple aspergilloma (unilateral localised disease) Large volume haemoptysis 2 3 Failure to control disease with medical therapy alone 4
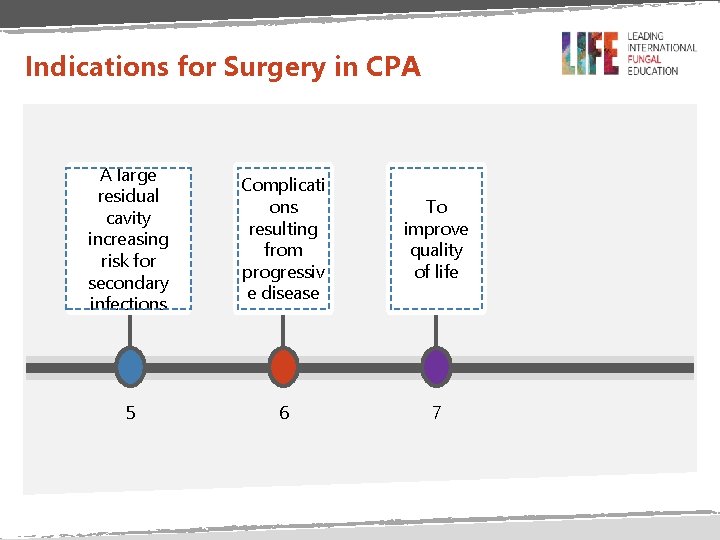
Indications for Surgery in CPA A large residual cavity increasing risk for secondary infections Complicati ons resulting from progressiv e disease To improve quality of life 5 6 7

When is Surgery Indicated? Risks ü Pleural space spillage (empyema) ü Bronchopleural fistula ü Haemoptysis ü Relapse ü CCPA>>Simple aspergilloma Benefits ü Life-saving ü Potentially curative
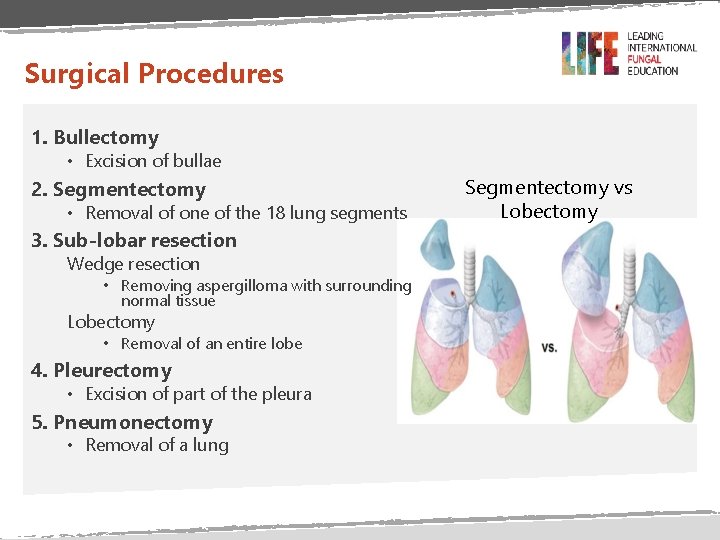
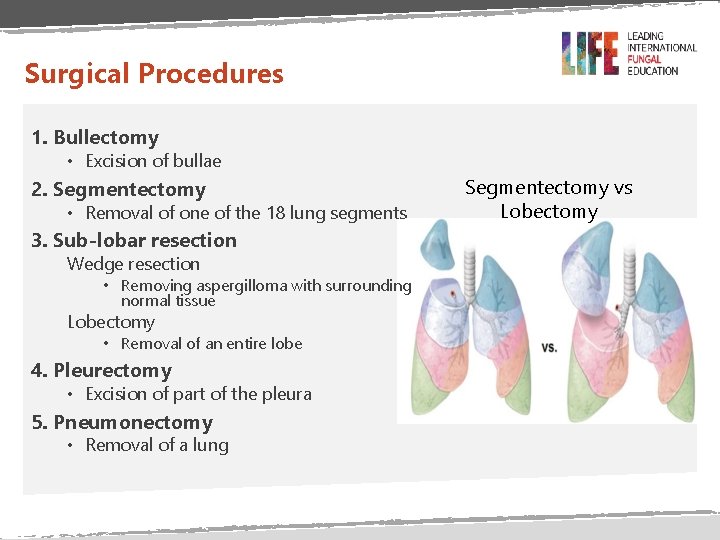
Surgical Procedures 1. Bullectomy • Excision of bullae 2. Segmentectomy • Removal of one of the 18 lung segments 3. Sub-lobar resection Wedge resection • Removing aspergilloma with surrounding normal tissue Lobectomy • Removal of an entire lobe 4. Pleurectomy • Excision of part of the pleura 5. Pneumonectomy • Removal of a lung Segmentectomy vs Lobectomy
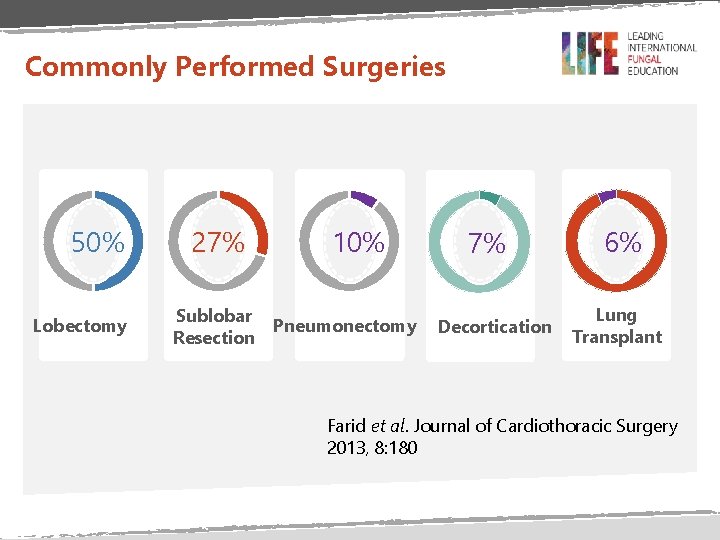
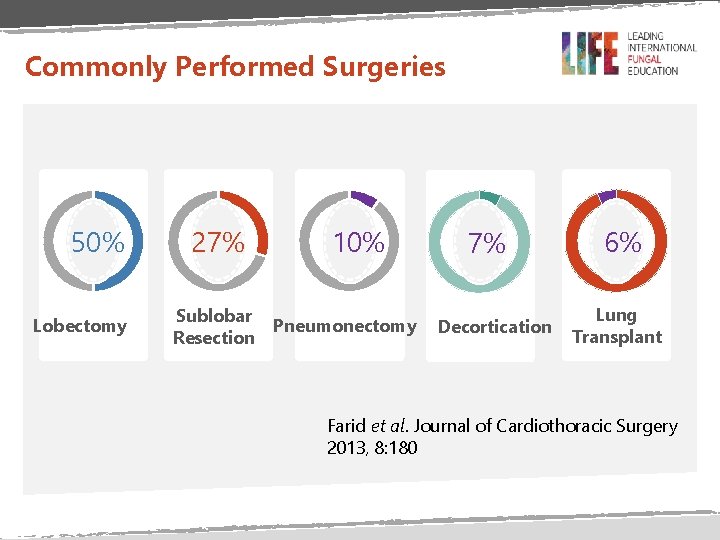
Commonly Performed Surgeries 50% Lobectomy 27% Sublobar Resection 10% Pneumonectomy 7% Decortication 6% Lung Transplant Farid et al. Journal of Cardiothoracic Surgery 2013, 8: 180
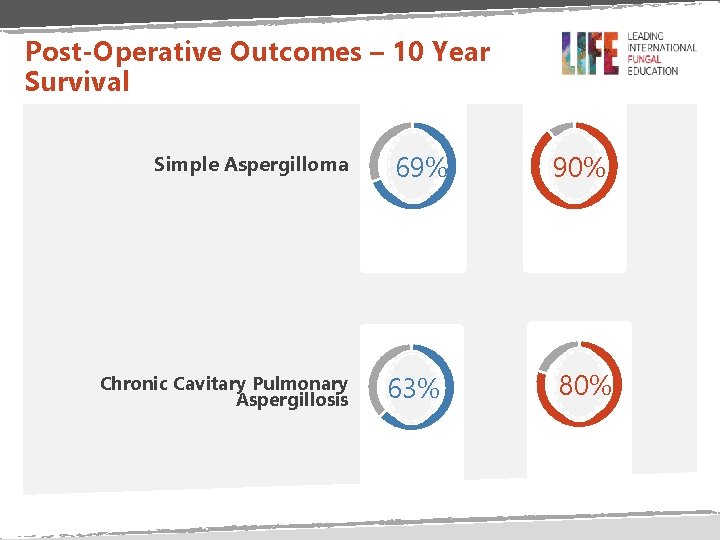
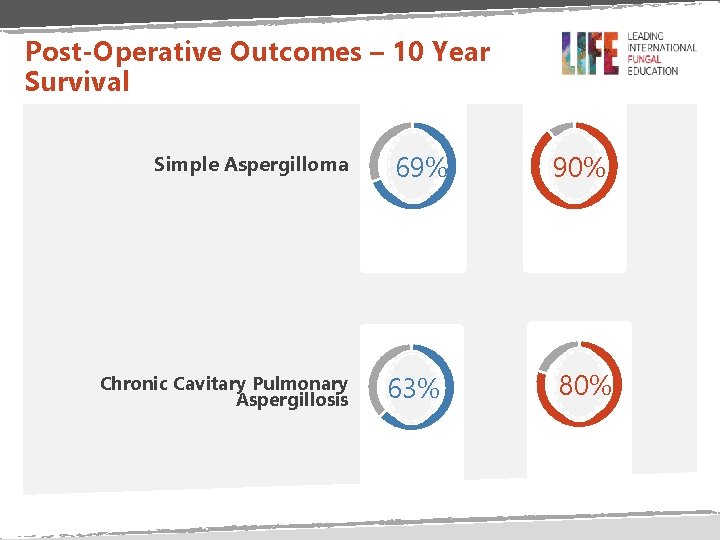
Post-Operative Outcomes – 10 Year Survival Simple Aspergilloma Chronic Cavitary Pulmonary Aspergillosis 69% 90% 63% 80%
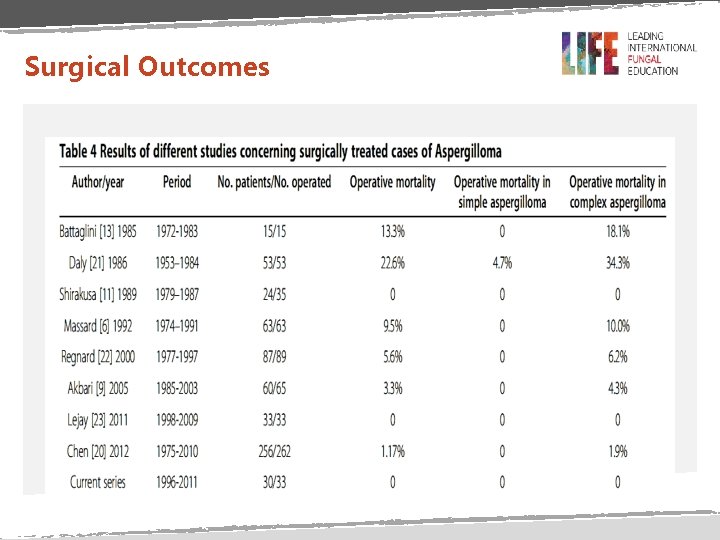
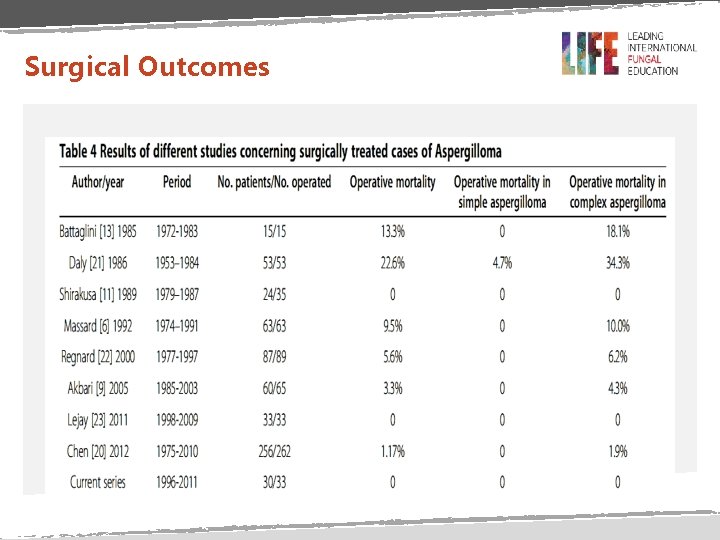
Surgical Outcomes
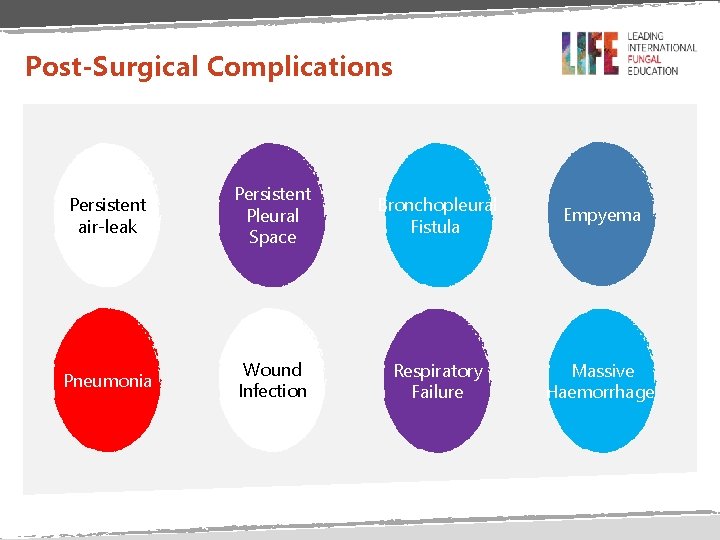
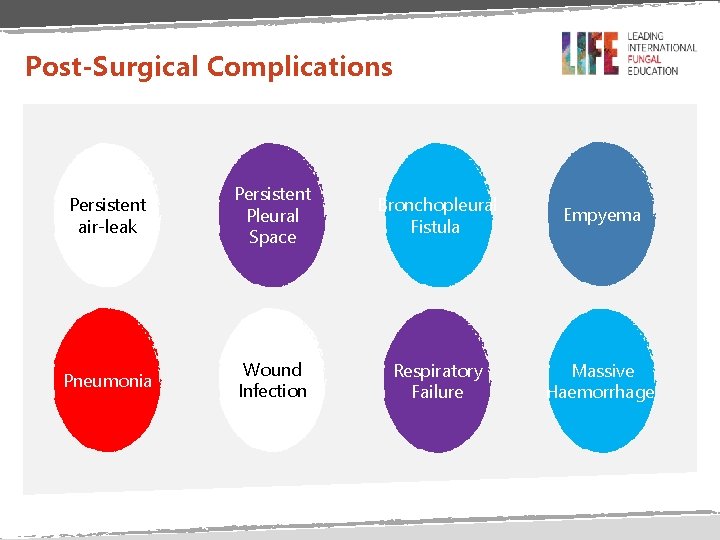
Post-Surgical Complications Persistent air-leak Persistent Pleural Space Bronchopleural Fistula Empyema Pneumonia Wound Infection Respiratory Failure Massive Haemorrhage
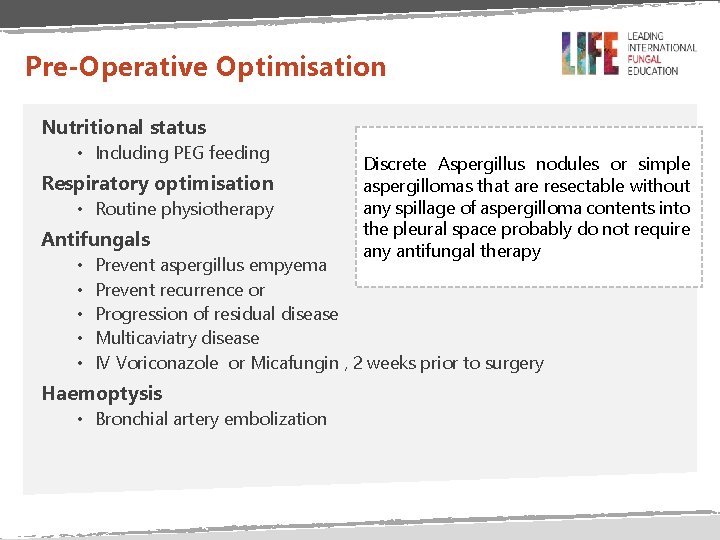
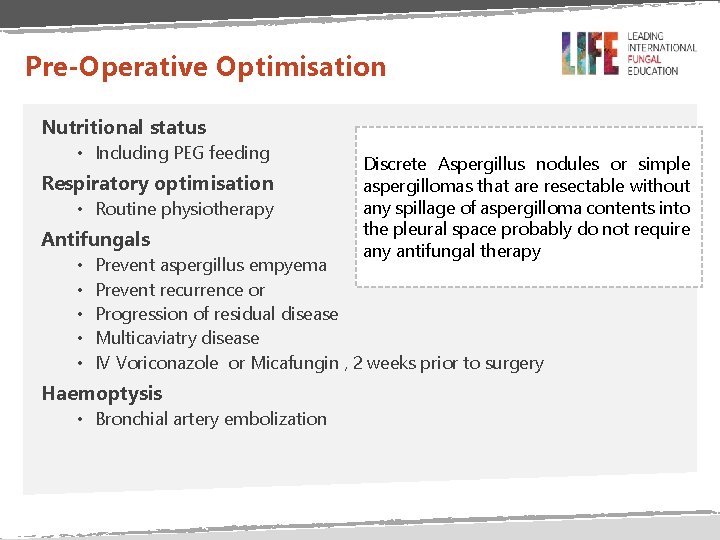
Pre-Operative Optimisation Nutritional status • Including PEG feeding Respiratory optimisation • Routine physiotherapy Antifungals • • • Discrete Aspergillus nodules or simple aspergillomas that are resectable without any spillage of aspergilloma contents into the pleural space probably do not require any antifungal therapy Prevent aspergillus empyema Prevent recurrence or Progression of residual disease Multicaviatry disease IV Voriconazole or Micafungin , 2 weeks prior to surgery Haemoptysis • Bronchial artery embolization
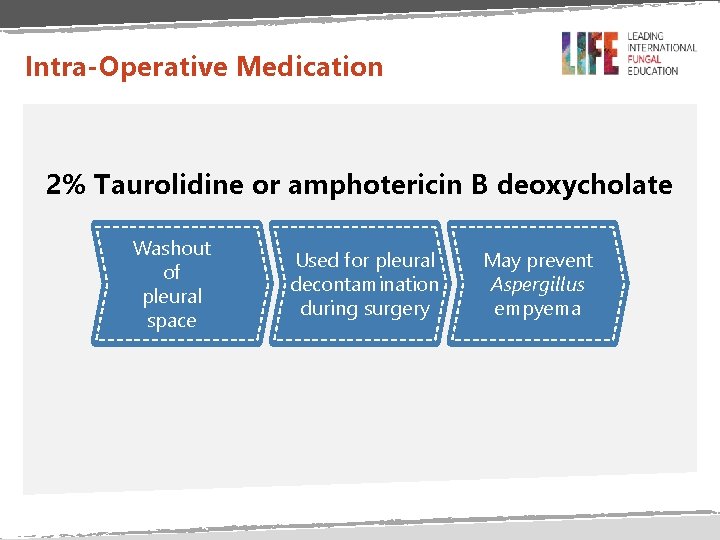
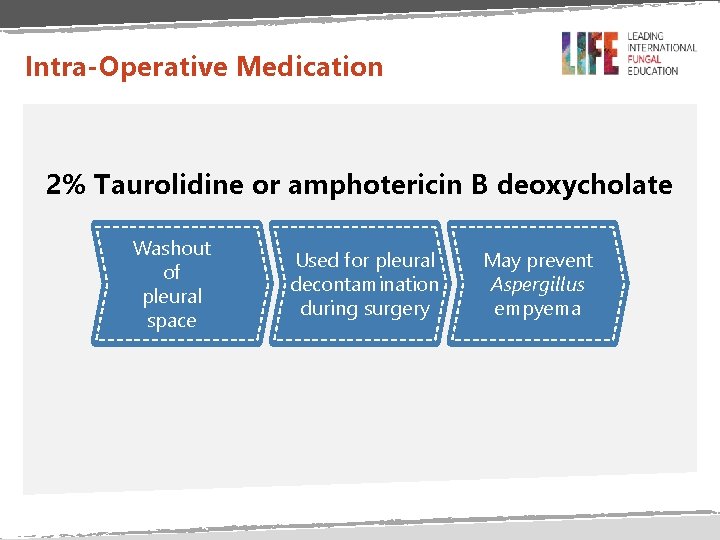
Intra-Operative Medication 2% Taurolidine or amphotericin B deoxycholate Washout of pleural space Used for pleural decontamination during surgery May prevent Aspergillus empyema
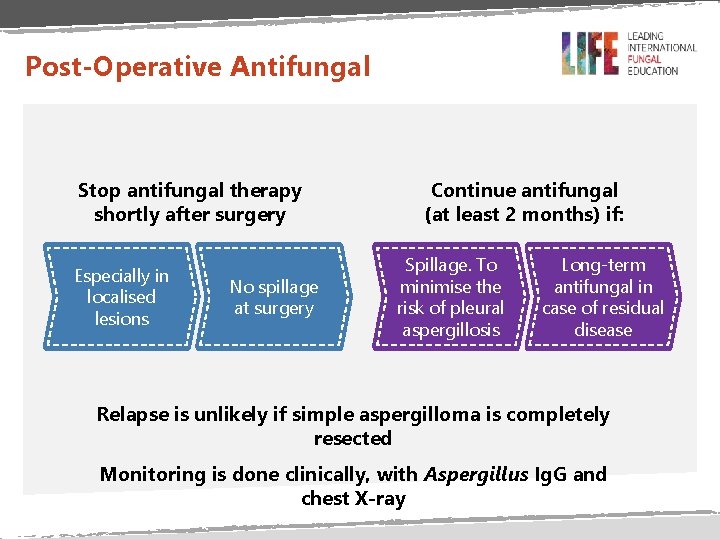
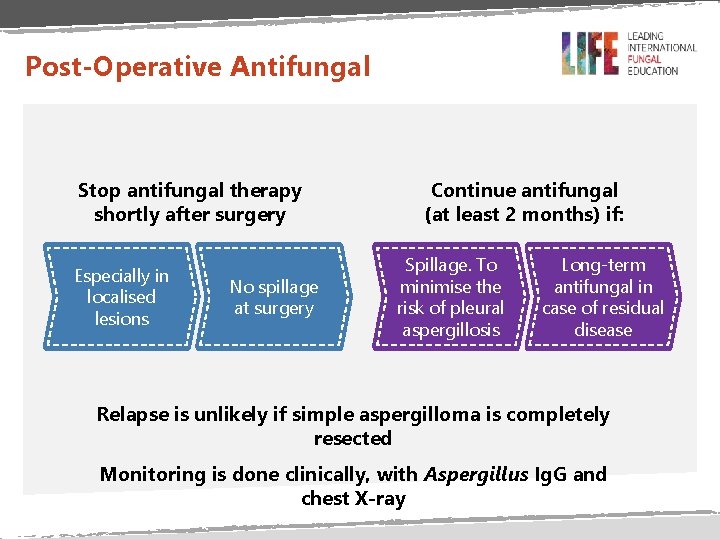
Post-Operative Antifungal Stop antifungal therapy shortly after surgery Especially in localised lesions No spillage at surgery Continue antifungal (at least 2 months) if: Spillage. To minimise the risk of pleural aspergillosis Long-term antifungal in case of residual disease Relapse is unlikely if simple aspergilloma is completely resected Monitoring is done clinically, with Aspergillus Ig. G and chest X-ray

Thank You
 Rajesh shah thoracic surgeon
Rajesh shah thoracic surgeon Copd medical abbreviation
Copd medical abbreviation Aspergillosis symptoms
Aspergillosis symptoms Aspergillosis
Aspergillosis Aspergillosis
Aspergillosis What is aspergillosis
What is aspergillosis Doc for invasive aspergillosis
Doc for invasive aspergillosis Tcs
Tcs Scaling memcache at facebook
Scaling memcache at facebook Dr rajesh bharani
Dr rajesh bharani Codcs
Codcs Rajesh kumar bhagat
Rajesh kumar bhagat Silverlight ppt
Silverlight ppt Rajesh bhaskaran cornell
Rajesh bhaskaran cornell Rajesh kadakia
Rajesh kadakia Dr rajesh batajoo
Dr rajesh batajoo Transportation engineering
Transportation engineering Dr rajesh garg
Dr rajesh garg Creatrine
Creatrine Rajesh das
Rajesh das Rajesh shewani
Rajesh shewani