Management of Hypertension and Hypotension in the Emergency























- Slides: 79
Management of Hypertension and Hypotension in the Emergency Department
Hypertension How do we manage Hypertension in the ER? ?
Hypertension Management in the ED Annual Census = 78, 000 patients n Approximately 215 patients per day n 40 to 50% have elevated BP readings upon admission to the ED n That is roughly 39, 000 patients/yr with elevated blood pressure readings in the ER. n
First Step: Categorize Types of Hypertension
Four Categories of Hypertension - Hypertensive Emergency - Hypertensive Urgency - Acute Hypertensive Episode - Transient Hypertension
What is a Hypertensive Emergency?

Hypertensive Emergency - A relative increase in blood pressure from baseline combined with Target Organ Dysfunction (TOD) - No Defined Pressure Measurement - Target Organ Damage is evident - Also known as Hypertensive Crisis or Malignant Hypertension - The MOST Serious form of hypertension
How do we define Target Organ Dysfunction ? ? ?
Target Organ Dysfunction Evidence of Damage or Injury to “Target Organs” such as the Heart, Brain, Lungs, Kidneys, or Aorta.
Examples of Target Organ Dysfunction Acute MI/ Unstable Angina n CVA n ICH / Subarachnoid Hemorrhage n CHF n Aortic Dissection n Acute Renal Failure n Hypertensive Encephalopathy n
How do we determine if Target Organ Dysfunction is present?
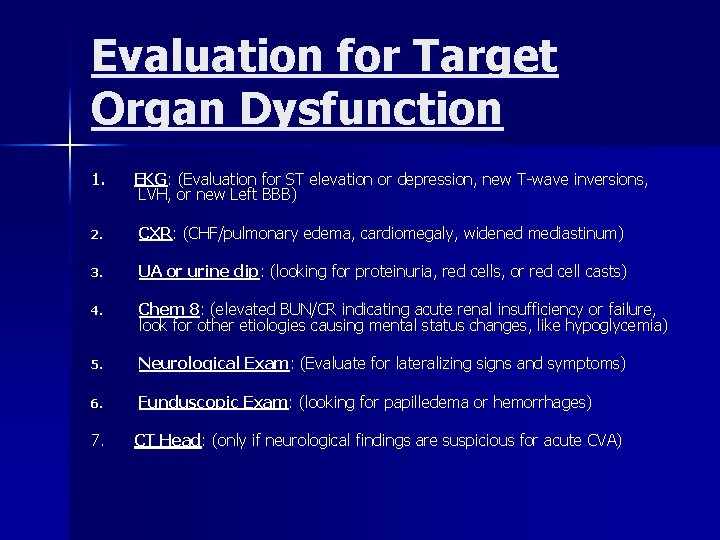
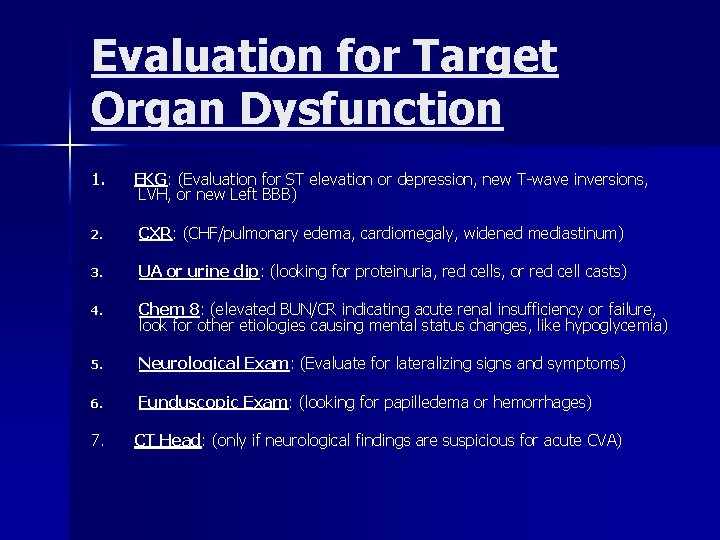
Evaluation for Target Organ Dysfunction 1. EKG: (Evaluation for ST elevation or depression, new T-wave inversions, LVH, or new Left BBB) 2. CXR: (CHF/pulmonary edema, cardiomegaly, widened mediastinum) 3. UA or urine dip: (looking for proteinuria, red cells, or red cell casts) 4. Chem 8: (elevated BUN/CR indicating acute renal insufficiency or failure, look for other etiologies causing mental status changes, like hypoglycemia) 5. Neurological Exam: (Evaluate for lateralizing signs and symptoms) 6. Funduscopic Exam: (looking for papilledema or hemorrhages) 7. CT Head: (only if neurological findings are suspicious for acute CVA)
Diagnosis and Management of Hypertensive Emergency
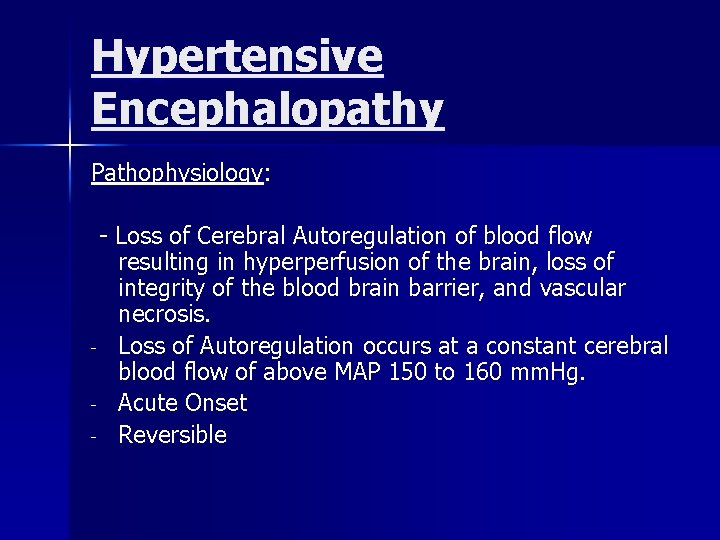
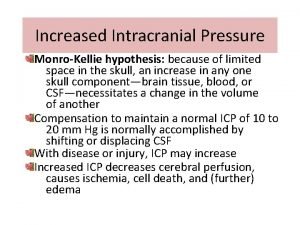
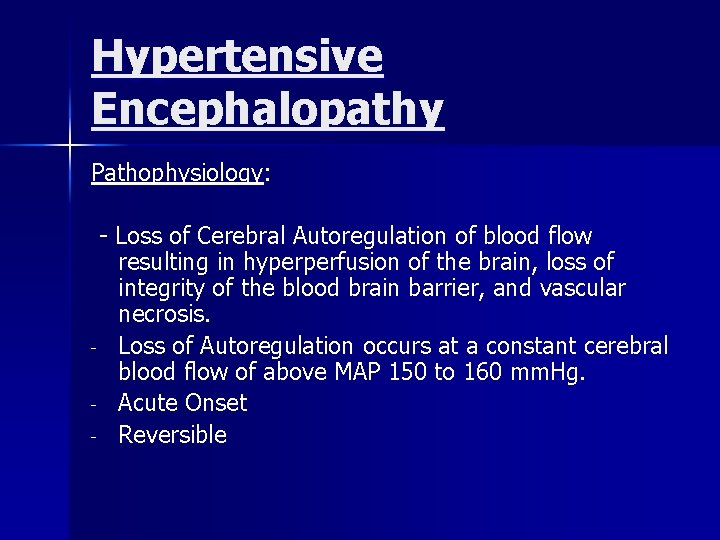
Hypertensive Encephalopathy Pathophysiology: - Loss of Cerebral Autoregulation of blood flow resulting in hyperperfusion of the brain, loss of integrity of the blood brain barrier, and vascular necrosis. - Loss of Autoregulation occurs at a constant cerebral blood flow of above MAP 150 to 160 mm. Hg. - Acute Onset - Reversible
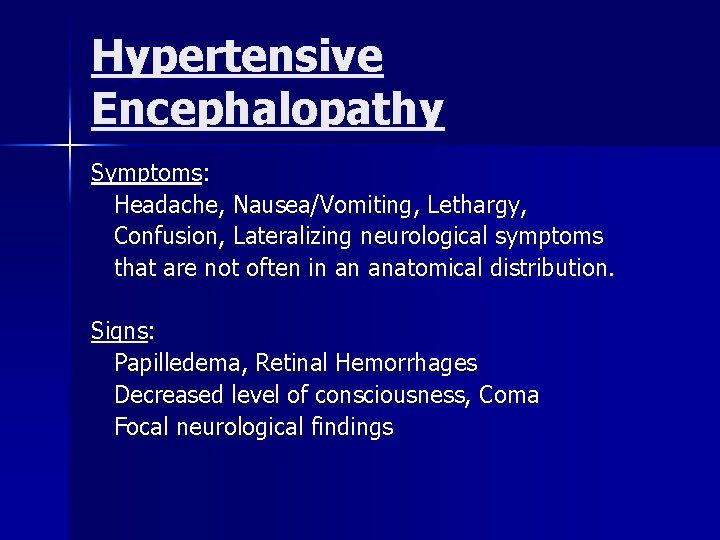
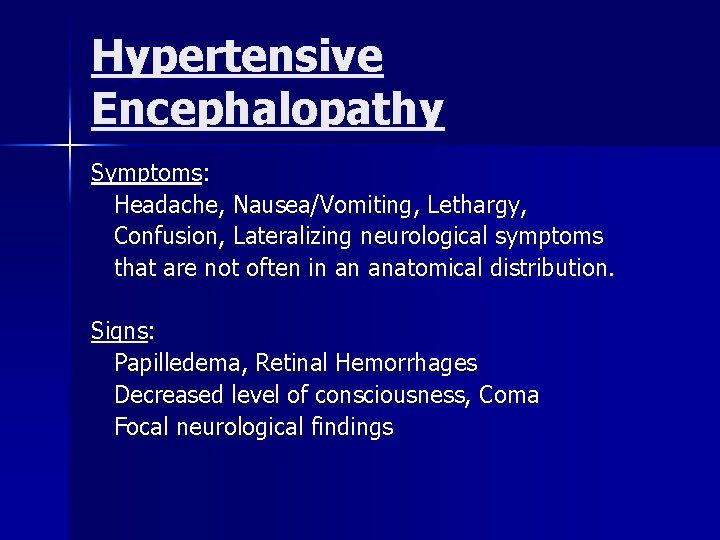
Hypertensive Encephalopathy Symptoms: Headache, Nausea/Vomiting, Lethargy, Confusion, Lateralizing neurological symptoms that are not often in an anatomical distribution. Signs: Papilledema, Retinal Hemorrhages Decreased level of consciousness, Coma Focal neurological findings
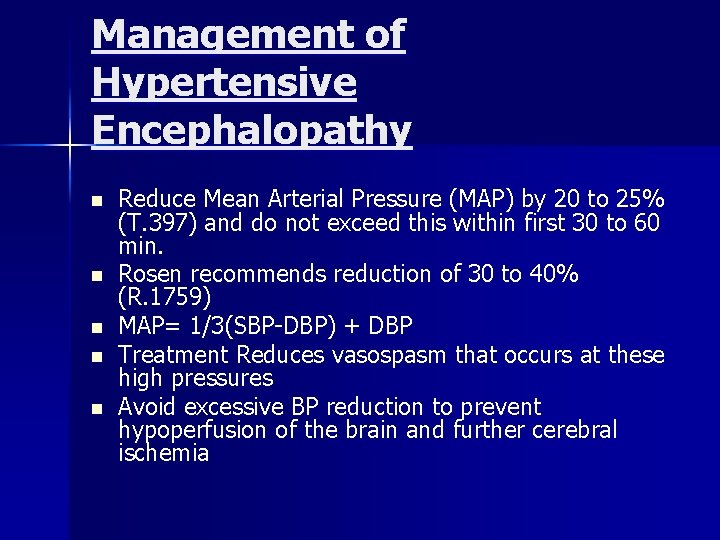
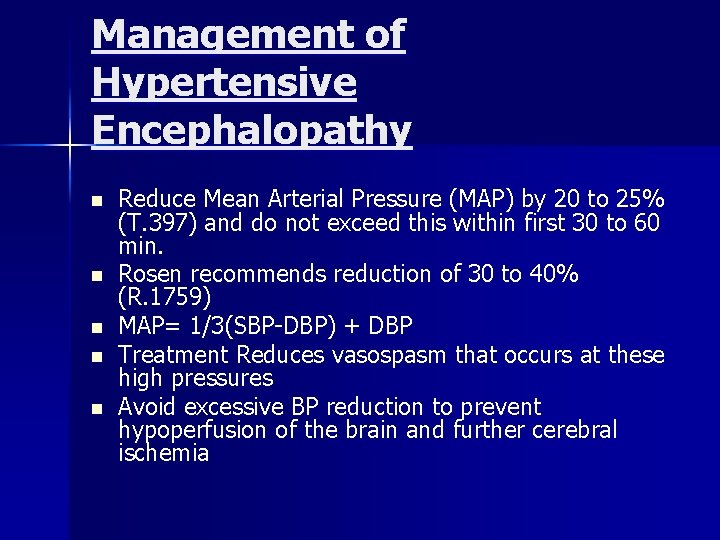
Management of Hypertensive Encephalopathy n n n Reduce Mean Arterial Pressure (MAP) by 20 to 25% (T. 397) and do not exceed this within first 30 to 60 min. Rosen recommends reduction of 30 to 40% (R. 1759) MAP= 1/3(SBP-DBP) + DBP Treatment Reduces vasospasm that occurs at these high pressures Avoid excessive BP reduction to prevent hypoperfusion of the brain and further cerebral ischemia

Management of Hypertensive Encephalopathy - Nitroprusside is the agent of choice (T. 397) and (R. 1759) - Nitroglycerin and Labetalol have been used successfully, but have not replaced Nitroprusside
Management of Ischemic CVA
Ischemic CVA Pathophysiology: Elevated Blood Pressure can be the cause of the central nervous system event, OR, it may be a normal physiologic response (Cushing’s Reflex)

Ischemic CVA Management n n n Elevated blood pressure is usually a physiologic response to the stroke itself and NOT the immediate cause This elevation of blood pressure maintains cerebral perfusion to viable but edematous tissue surrounding the ischemic area. Most embolic or thrombotic strokes do NOT have substantial BP elevations and do not need aggressive therapy

Ischemic CVA Management: VERY CONTROVERSIAL! Recent Trends leans towards NOT treating hypertension in the presence of a Cerebrovascular Accident (thrombotic or embolic) unless Diastolic Blood Pressure exceeds 140 mm. Hg.

Ischemic CVA Management Tintinelli: Favors lowering MAP (mean arterial pressure) by 20%. Recommends IV Labetalol in small doses of 5 mg increments IF Diastolic Blood Pressure is higher than 140 mm. Hg. (T. 398)

Ischemic CVA Managment Rosen: In most cases, recommends no treatment of Hypertension in CVA patients. (p. 1760). - However, the author does recommend treating HTN if diastolic blood pressure is greater than 140 mm. Hg.
Management of Hemorrhagic CVA
Causes of Hemorrhagic CVA n Hypertensive Vascular Disease n Arteriovenous Anomalies (AVM) n Arterial Aneurysms n Tumors n Trauma
Hemorrhagic CVA Management n Hypertension associated with hemorrhagic stroke is usually transitory and the result of increased intracranial pressure and irritation of the Autonomic Nervous System
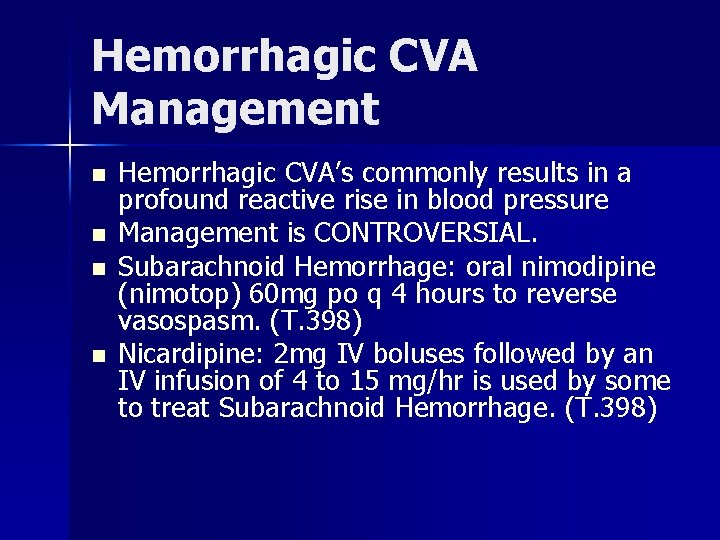
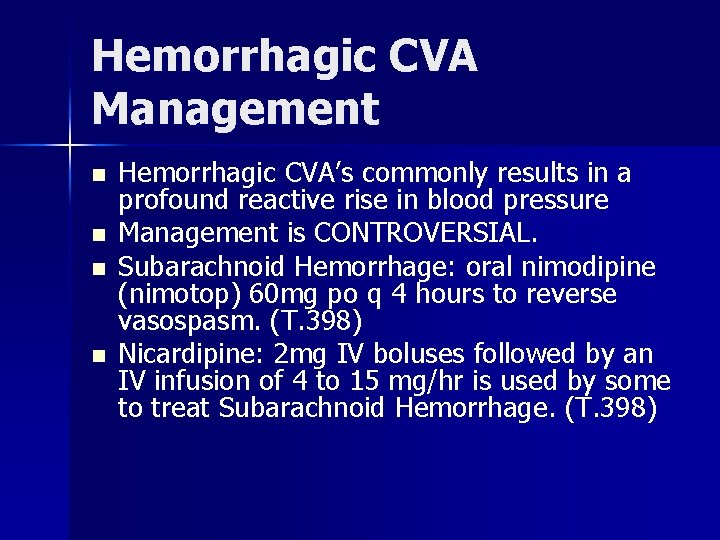
Hemorrhagic CVA Management n n Hemorrhagic CVA’s commonly results in a profound reactive rise in blood pressure Management is CONTROVERSIAL. Subarachnoid Hemorrhage: oral nimodipine (nimotop) 60 mg po q 4 hours to reverse vasospasm. (T. 398) Nicardipine: 2 mg IV boluses followed by an IV infusion of 4 to 15 mg/hr is used by some to treat Subarachnoid Hemorrhage. (T. 398)

Management of CHF/ Pulmonary Edema
Congestive Heart Failure / Pulmonary Edema Pathophysiology: Increased Afterload with decreased Cardiac Output

CHF / Pulmonary Edema Symptoms: Shortness of Breath, Cough, Chest Pain Lower Extremity Swelling Signs: Jugular Venous Distension, Rales, S 3 Gallop Hepatomegaly, Pedal Edema
CHF / Pulmonary Edema Management in the ED - - Nitroprusside or IV Nitroglycerin (T. 398) Rosen: May start with Nitroglycerin, but Nitroprusside is agent of choice if Pulmonary Edema is present. (R. 1760) Attempt treatment of CHF initially with standard agents (Lasix, sublingual NTG, morphine), as these often lower blood pressure, but resort to Nitroprusside if necessary (R. 1761)
Management of Acute Coronary Syndrome/ Acute MI

Acute Coronary Syndrome / Acute MI Pathophysiology: - Increased afterload, cardiac workload, and myocardial oxygen demand - Decreased coronary artery blood flow
Acute Coronary Syndrome / Acute MI Symptoms: Chest Pain, Nausea / Vomiting, Diaphoresis, Shortness of Breath Signs: Congestive Heart Failure Signs, S 4 Gallop (due to decreased ventricular compliance) Few physical findings in many patients Clinical History is very Important
Acute Coronary Syndrome/ Acute MI - - Immediate Blood Pressure reduction is indicated to prevent Myocardial Damage No specific Defined BP target Tailor treatment to symptom relief (T. 398)
Acute Coronary Syndrome / Acute MI Management: Nitroglycerin IV or Sublingual (T. 398) Nitroprusside (T. 398) Beta Blockers (Esmolol, Lopressor) (T. 356357) Nitroglycerin is Drug of Choice (R. 1761)
Dissection of Thoracic Aorta
Dissection of Thoracic Aorta Pathophysiology: - Atherosclerotic Vascular Disease, Chronic Hypertension, increased shearing force on the thoracic aorta, leading to intimal tear. - 50% begin in ascending aorta - 30% at aortic arch - 20% in descending aorta (R. 1762 -3)
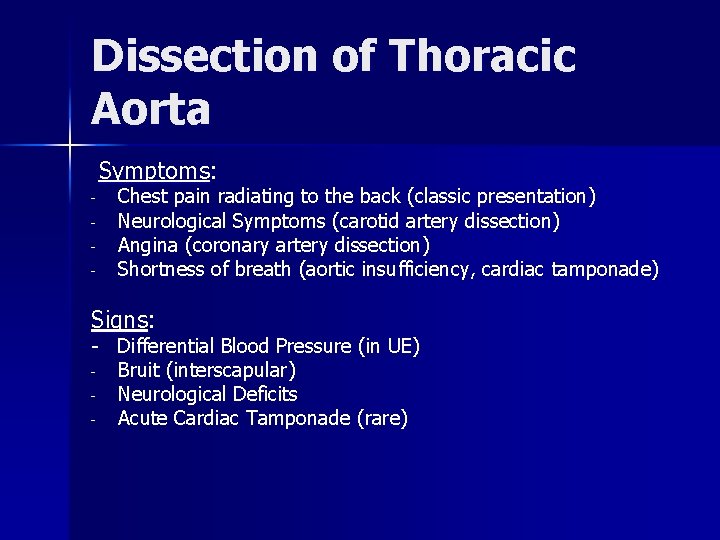
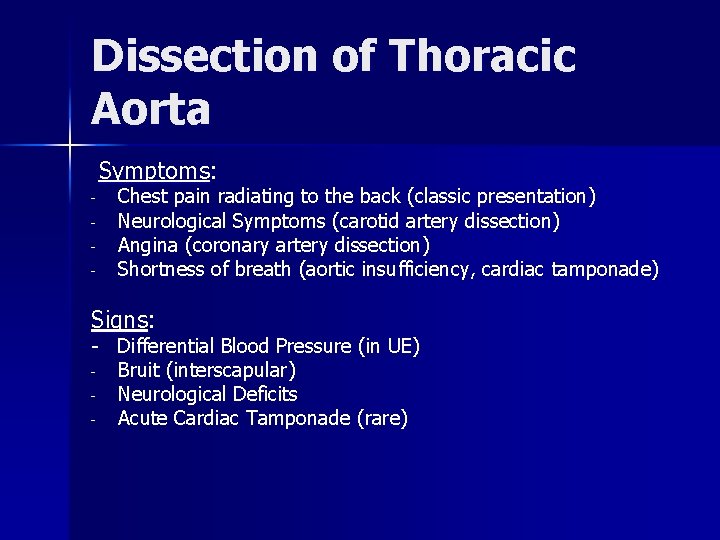
Dissection of Thoracic Aorta Symptoms: - Chest pain radiating to the back (classic presentation) Neurological Symptoms (carotid artery dissection) Angina (coronary artery dissection) Shortness of breath (aortic insufficiency, cardiac tamponade) Signs: - Differential Blood Pressure (in UE) - Bruit (interscapular) - Neurological Deficits - Acute Cardiac Tamponade (rare)
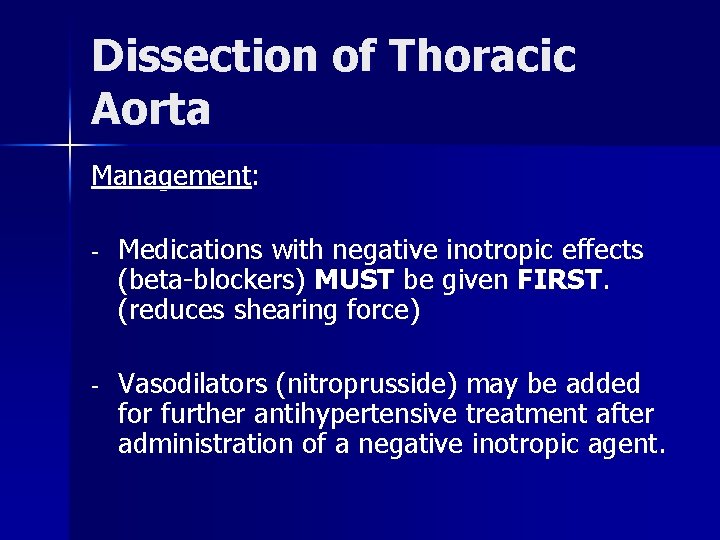
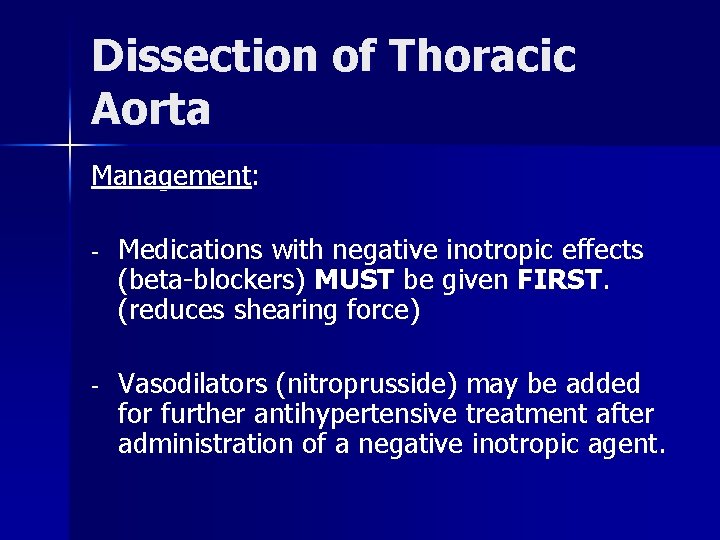
Dissection of Thoracic Aorta Management: - Medications with negative inotropic effects (beta-blockers) MUST be given FIRST. (reduces shearing force) - Vasodilators (nitroprusside) may be added for further antihypertensive treatment after administration of a negative inotropic agent.

Dissection of Thoracic Aorta Optimal Blood Pressure in these patients is undefined and must be tailored for each patient, however, SBP of 120 -130 mm. Hg may be a intial starting point. (T. 408)
Acute Renal Failure

Acute Renal Failure Pathophysiology: - Hypertensive Glomerulonephropathy, Acute Tubular Necrosis (ATN) - Worsening renal function in the setting of severe hypertension with elevation of BUN/CR, proteinuria, or the presence of red cells and red cell casts in the urine.
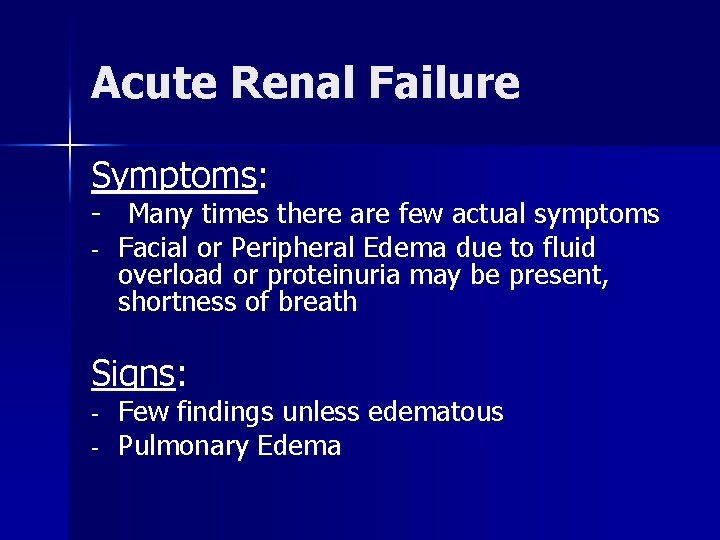
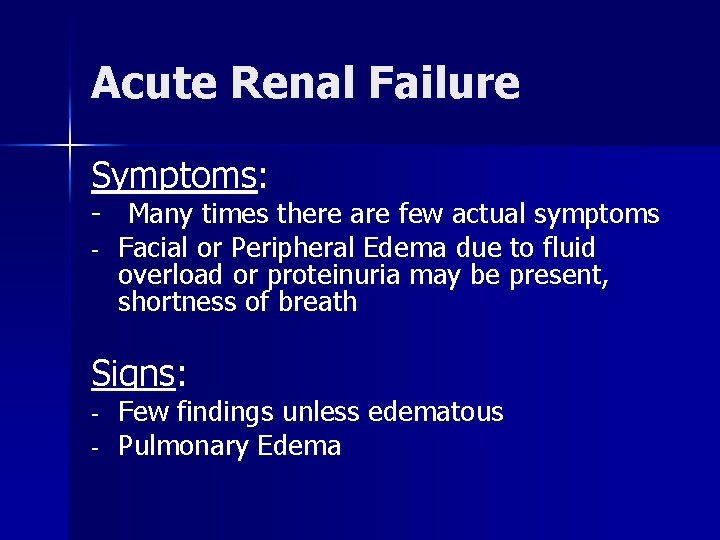
Acute Renal Failure Symptoms: - Many times there are few actual symptoms - Facial or Peripheral Edema due to fluid overload or proteinuria may be present, shortness of breath Signs: - Few findings unless edematous Pulmonary Edema

Acute Renal Failure Management: - - Nitroprusside is agent of choice (T. 398) Dialysis (as needed) Rosen: Lasix to enhance Sodium excretion; Also recommends Nitroprusside or Nifedipine (R. 1761) Nitroglycerin is also a good agent in this setting since it is hepatically metabolized and gastrointestinally excreted.

Pheochromocytoma
Pheochromocytoma Pathophysiology: - Alpha and Beta stimulation of the cardiovascular system due to adrenergic excess states
Pheochromocytoma Symptoms: Episodic Headaches, flushing, tremor, diaphoresis, diarrhea, hyperactivity, and palpitations Signs: Tachycardia, tachypnea, tremor, hyperdynamic state (high output CHF)
Pheochromocytoma Management: - Alpha Blocker FIRST, followed by a Beta Blocker Phentolamine (alpha) + Esmolol (beta) Labetalol IV (combined alpha and beta blockade)
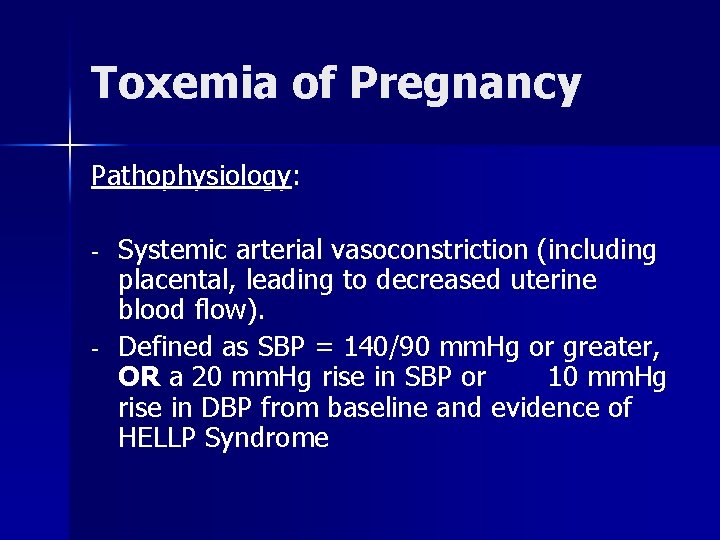
Toxemia of Pregnancy Eclampsia/Pre-Eclampsia
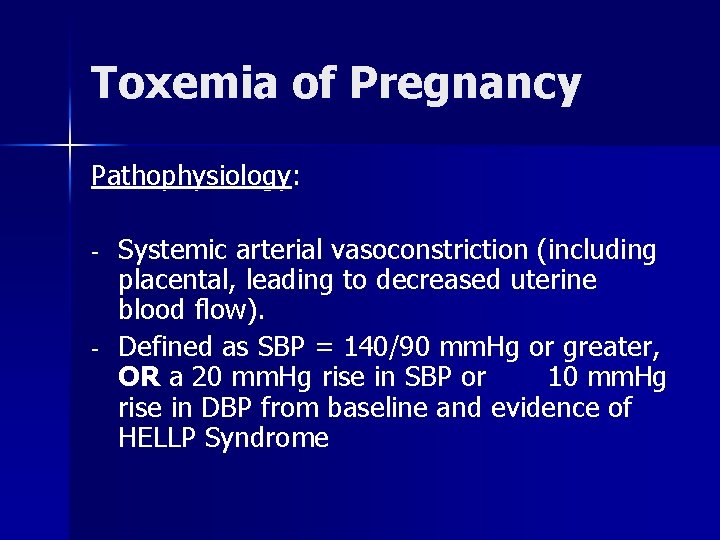
Toxemia of Pregnancy Pathophysiology: - - Systemic arterial vasoconstriction (including placental, leading to decreased uterine blood flow). Defined as SBP = 140/90 mm. Hg or greater, OR a 20 mm. Hg rise in SBP or 10 mm. Hg rise in DBP from baseline and evidence of HELLP Syndrome

Toxemia of Pregnancy Symptoms: Lower extremity swelling, headache, confusion, seizures, coma Signs: Edema, hyperreflexia, elevation of blood pressure related to baseline BP prior to pregnancy (elevation may be mild 125/75)

Toxemia of Pregnancy Management: - IV Magnesium Sulfate, Hydralazine. May also use nifedipine or labetalol (R. 1762) Delivery of Fetus is definitive treatment of pre-eclampsia

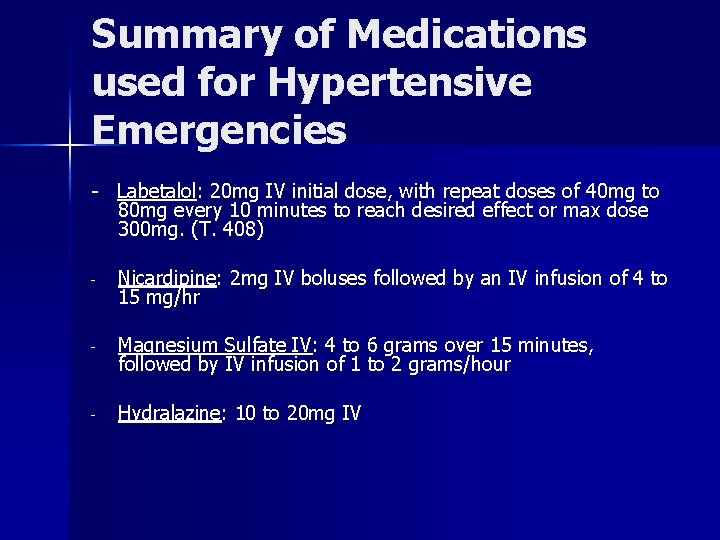
Summary of Medications used for Hypertensive Emergencies - Intravenous Nitroglycerin: Start at 0. 2 to 0. 4 mcg/kg/min (10 to 30 mcg/min) and rapidly increase in 5 to 10 mcg/min increments. Titrate to BP and symptomatic improvement. (T. 369) - Nitroprusside: Start 0. 3 mcg/kg/min and titrate up every 5 to 10 minutes based on BP and clinical response. (T. 369) - Esmolol: 500 mcg/kg initial bolus over 1 minute, then start infusion at 50 to 150 mcg/kg/min (T. 408) - Metoprolol (Lopressor): 5 mg IV every 2 minutes for a total of 3 doses, then start infusion at 2 to 5 mg/hr. (T. 408)
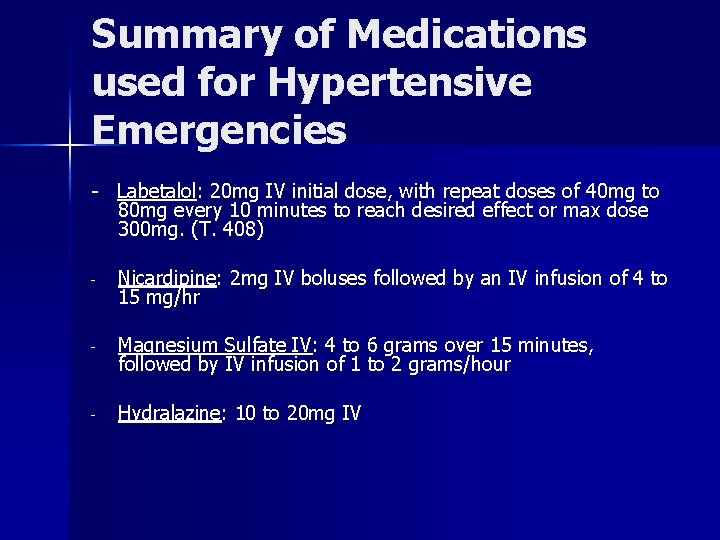
Summary of Medications used for Hypertensive Emergencies - Labetalol: 20 mg IV initial dose, with repeat doses of 40 mg to 80 mg every 10 minutes to reach desired effect or max dose 300 mg. (T. 408) - Nicardipine: 2 mg IV boluses followed by an IV infusion of 4 to 15 mg/hr - Magnesium Sulfate IV: 4 to 6 grams over 15 minutes, followed by IV infusion of 1 to 2 grams/hour - Hydralazine: 10 to 20 mg IV
What is a Hypertensive Urgency? ?
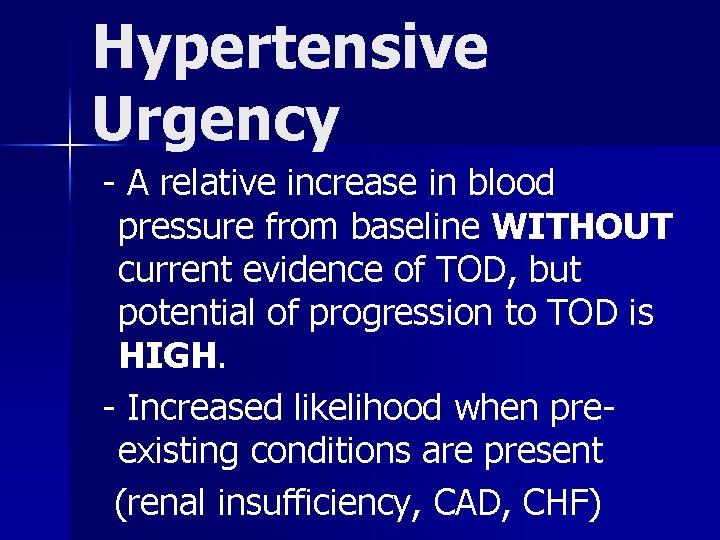
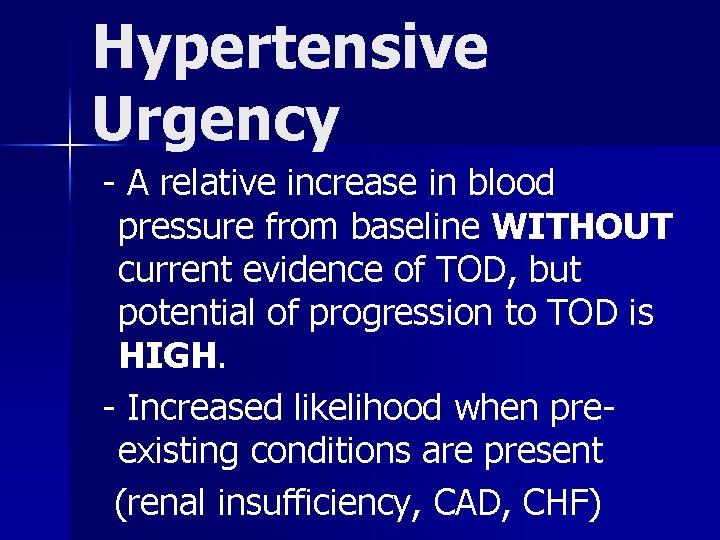
Hypertensive Urgency - A relative increase in blood pressure from baseline WITHOUT current evidence of TOD, but potential of progression to TOD is HIGH. - Increased likelihood when preexisting conditions are present (renal insufficiency, CAD, CHF)
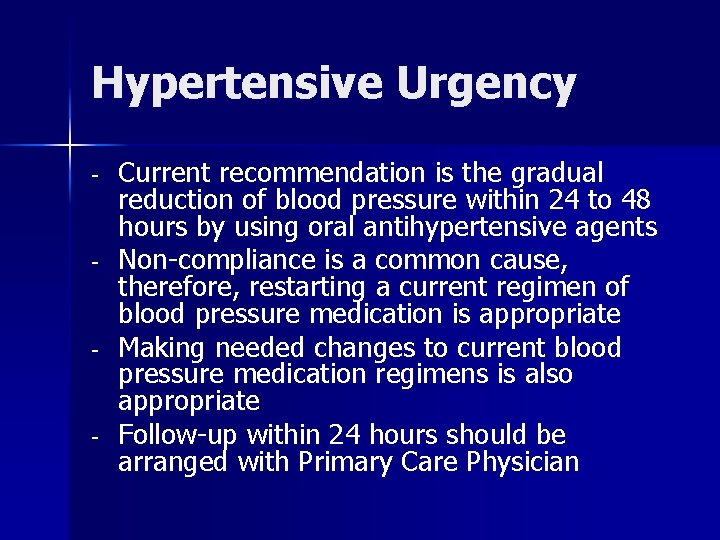
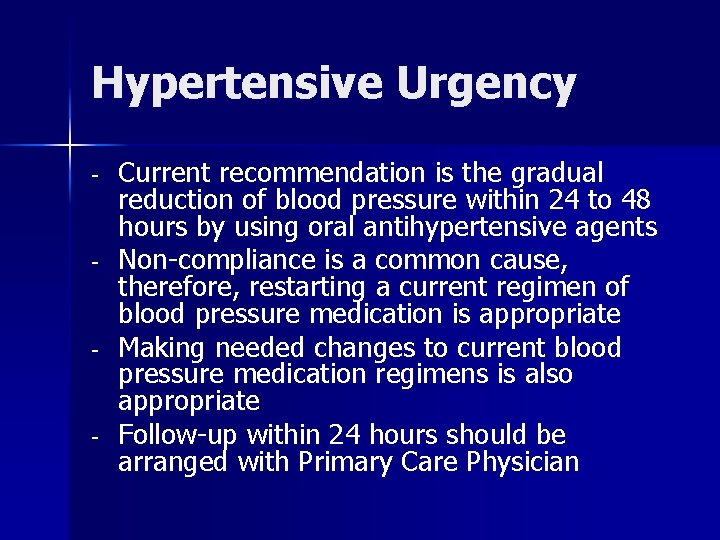
Hypertensive Urgency - - Current recommendation is the gradual reduction of blood pressure within 24 to 48 hours by using oral antihypertensive agents Non-compliance is a common cause, therefore, restarting a current regimen of blood pressure medication is appropriate Making needed changes to current blood pressure medication regimens is also appropriate Follow-up within 24 hours should be arranged with Primary Care Physician
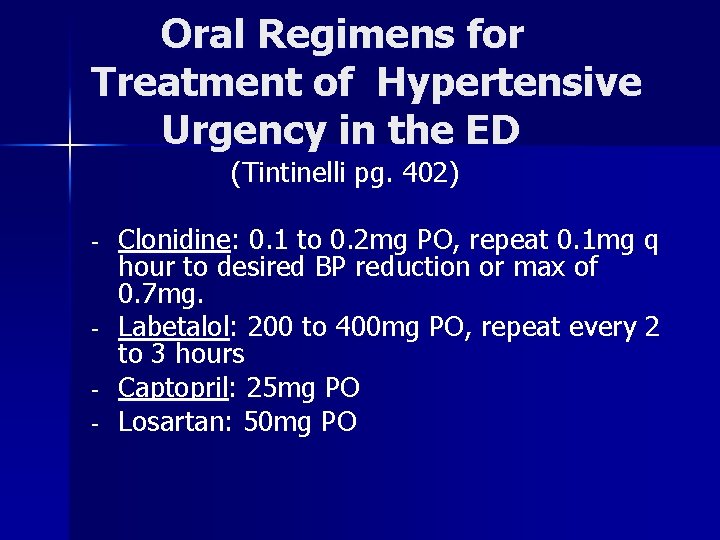
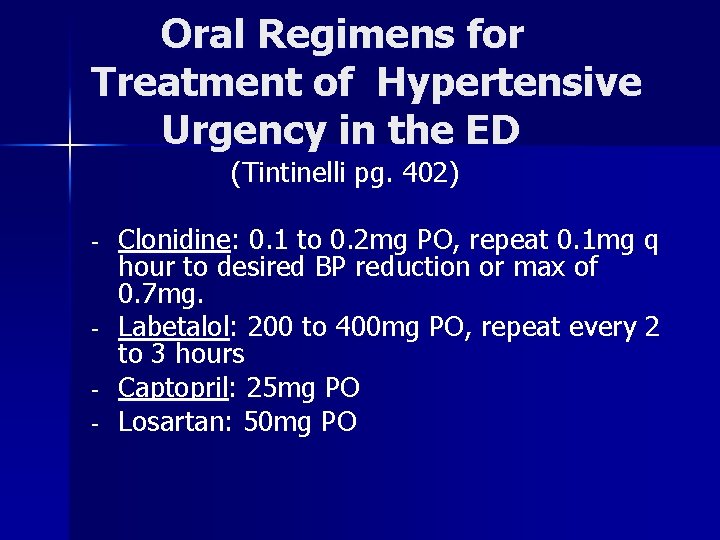
Oral Regimens for Treatment of Hypertensive Urgency in the ED (Tintinelli pg. 402) - - Clonidine: 0. 1 to 0. 2 mg PO, repeat 0. 1 mg q hour to desired BP reduction or max of 0. 7 mg. Labetalol: 200 to 400 mg PO, repeat every 2 to 3 hours Captopril: 25 mg PO Losartan: 50 mg PO
What is an Acute Hypertensive Episode?
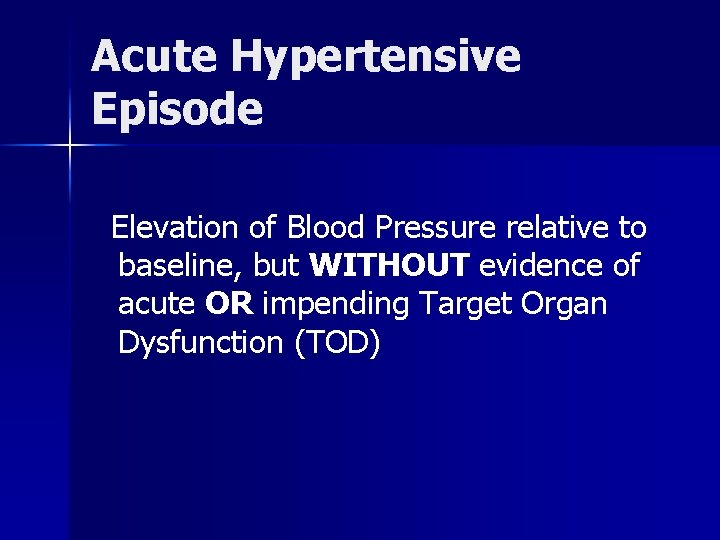
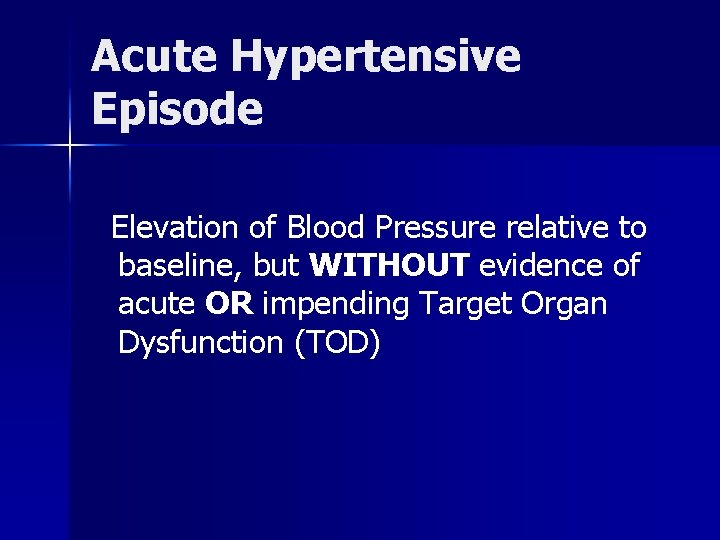
Acute Hypertensive Episode Elevation of Blood Pressure relative to baseline, but WITHOUT evidence of acute OR impending Target Organ Dysfunction (TOD)

Management of Acute Hypertensive Episode - - Paucity of evidence that acute intervention in ED is warranted for Hypertensive Episode Complications can occur in acute treatment of patients with chronically elevated blood pressure If HTN is newly diagnosed in the ER, patients should be referred to Primary Care physician for evaluation and initiation of therapy within 24 to 48 hours Again, restarting prior blood pressure medication regimens or adjusting doses is appropriate for patients with previously diagnosed hypertension.
What is Transient Hypertension? ?
Treatment of Transient Hypertension - - Transient HTN occurs in association with other conditions like anxiety, alcohol withdrawal syndromes, toxicological substances, and sudden cessation of medications) Treatment is aimed at underlying cause “White-Coat Hypertension” Single encounter in ED does not warrant diagnosis of HTN or treatment of HTN Follow-up with Primary Care Physician

SWITCHING GEARS
Hypotension/Shock Management in the ED
Hypotension/Shock Types of Shock: - Hypovolemic (inadequate circulating volume) - Cardiogenic (inadequate pump function) - Distributive (peripheral vasodilitation) - Obstructive (extra-cardiac obstruction of blood flow)
Hypotension/Shock Goals of Management 1. Determine Cause: - Usually very apparent - Can be subtle - No single Vital Sign that is diagnostic of Shock - Initial Therapy guided by clinical findings
Management of Hypotension/Shock 2. Evaluate Signs and Symptoms: - Tachycardia - Decreased Urine Output - Cool, Mottled Skin - Cyanosis - Confusion
Hypotension/Shock Goals of Resuscitation ABC’s: A- Secure Airway (intubate if needed) B- Insure oxygenation and ventillation C- Provide Hemodynamic Stabilization (correction of hypotension based on etiology)
Resuscitation Initiate Fluid Therapy: 0. 25 to 0. 5 Liters of Normal Saline (NS) or similar isotonic crystalloid should be administered every 5 to 10 minutes as needed for correction of hypotension

Rapid Fluid Administration It is not unusual for a patient to require 4 to 6 Liters of fluid in the initial phase of resuscitation.

Goal of Fluid Resusciation - Stabilization of pt’s mentation Improvement in Blood Pressure Reduction of Pulse Rate Improved Skin Perfusion Urine Output > 30 ml per hour

Inotropic Support If NO response to initial fluid infusion of 3 to 4 L is noted, OR if there are signs of fluid overload (pulmonary edema), Inotropic agents should be started.

Inotropic Agents - - Dopamine: Start infusion at 5 mcg/kg/min and titrate up to 20 mcg/kg/min in order to achieve desired BP Indicated for reversing hypotension related to AMI, trauma, sepsis, heart failure, and renal failure when fluid resuscitation is unsuccessful or not appropriate (T. 212)
Inotropic Agents - - - Dobutamine: Dosage range is 2 to 20 mcg/kg/min, however, most patients can be maintained at a rate of 10 mcg/kg/min Indicated for cardiovascular decompensation due to ventricular dysfunction or low-output heart failure Agent of choice for management of Cardiogenic Shock Less effect on Heart Rate than Dopamine (T. 212)
Inotropic Agents - - - Norepinephrine (Levophed): start infusion at 2 mcg/min and titrate to achieve desired blood pressure. Used when there is inadequate response to other pressors. Lowest dosage that maintains BP should be used in order to minimize the complications of vasoconstriction Increased survival rates of up to 40% in septic shock have been reported in the literature (T. 246)
End Point of Resuscitation - Normalization of blood pressure, heart rate, and urine output - Goal is to maximize survival and minimize morbidity using objective hemodynamic and physiologic values to guide therapy

Questions ? ? ?
 Hypertension vs hypotension
Hypertension vs hypotension Hypertension vs hypotension
Hypertension vs hypotension Htn emergency vs urgency
Htn emergency vs urgency Gagandeep singh bedi
Gagandeep singh bedi Orthostatic vitals definition
Orthostatic vitals definition Isoloitu systolinen verenpaine
Isoloitu systolinen verenpaine Hypersiallorhée
Hypersiallorhée L'hypotension orthostatique que faire
L'hypotension orthostatique que faire Poul humeral
Poul humeral Orthostatic hypotension
Orthostatic hypotension Hypotension
Hypotension Permissive hypotension
Permissive hypotension Intracranial hypotension radiopedia
Intracranial hypotension radiopedia Non pharmacological management of hypertension
Non pharmacological management of hypertension Stage 1 hypertension
Stage 1 hypertension Cataractectomy
Cataractectomy Nursing management of portal hypertension
Nursing management of portal hypertension Coma sign
Coma sign Diueritique
Diueritique Hypertension
Hypertension Disease state awareness
Disease state awareness Syndrome méningé
Syndrome méningé Medslide
Medslide Hypertension
Hypertension Equivalence hbpm
Equivalence hbpm Endorine
Endorine Demadex
Demadex Varices cardio tubérositaires
Varices cardio tubérositaires Rules of halves in hypertension
Rules of halves in hypertension Systemic vascular resistance
Systemic vascular resistance Definition of hypertension
Definition of hypertension Masked hypertension
Masked hypertension Definition of pulmonary hypertension
Definition of pulmonary hypertension Causes of secondary hypertension
Causes of secondary hypertension Dcld vs cld
Dcld vs cld Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Esterman efficiency score driving
Esterman efficiency score driving Definition of hypertension
Definition of hypertension Conclusion of hypertension
Conclusion of hypertension Aobp vs obpm
Aobp vs obpm Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Pah groups
Pah groups Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Hypokalemia
Hypokalemia Pico question examples labor and delivery
Pico question examples labor and delivery Conclusion of hypertension
Conclusion of hypertension Sohil rangwala
Sohil rangwala Hypertensive urgency
Hypertensive urgency Presenting complaints of hypertension
Presenting complaints of hypertension Conclusion of hypertension
Conclusion of hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Case scenario for hypertension
Case scenario for hypertension Ambulatory venous hypertension meaning
Ambulatory venous hypertension meaning Intracranial hypertension
Intracranial hypertension Intracranial hypertension
Intracranial hypertension Complications of cirrhosis
Complications of cirrhosis Health coaches for hypertension control
Health coaches for hypertension control Rules of halves in hypertension
Rules of halves in hypertension Dianne zwicke
Dianne zwicke Chd pulmonary hypertension
Chd pulmonary hypertension Hypertension
Hypertension Pulmonary hypertension
Pulmonary hypertension Isolated systolic hypertension
Isolated systolic hypertension Traitement hypertension
Traitement hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Presinusoidal portal hypertension
Presinusoidal portal hypertension Bp
Bp Classification of hypertension
Classification of hypertension Hypertension
Hypertension Hematocrit
Hematocrit American heart association 2020
American heart association 2020 Antihypertensive drugs
Antihypertensive drugs Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Heart hypertrophy
Heart hypertrophy Hypertension investigation chart
Hypertension investigation chart Portal hypertension definition
Portal hypertension definition Pulmonary hypertension
Pulmonary hypertension Gestational hypertension symptoms
Gestational hypertension symptoms Conclusion of hypertension
Conclusion of hypertension