Guidelines for Prevention and Treatment of Opportunistic Infections













- Slides: 65
Guidelines for Prevention and Treatment of Opportunistic Infections among HIV-Infected Children Fungal Infections Recommendations from Centers for Disease Control and Prevention, the National Institutes of Health, the HIV Medicine Association of the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the American Academy of Pediatrics July 2009 www. aidsetc. org
About This Presentation These slides were developed using the April 2008 Guidelines. The intended audience is clinicians involved in the care of patients with HIV. Users are cautioned that, because of the rapidly changing field of HIV care, this information could become out of date quickly. Finally, it is intended that these slides be used as prepared, without changes in either content or attribution. Users are asked to honor this intent. Expert opinion should be sought for complex treatment regimens. – AETC NRC 2 July 2009 www. aidsetc. org
Aspergillosis: Epidemiology § Aspergillus species are ubiquitous molds found in soil, on plants, and in decomposing organic materials § The most common species causing aspergillosis are A fumigatus and A flavus § Rare but frequently lethal infection § Risk factors include low CD 4 count, neutropenia, corticosteroids, concurrent malignancy with chemotherapy, HIV-related phagocytic impairment, previous respiratory infections, broad -spectrum antibiotic exposure 3 July 2009 www. aidsetc. org
Aspergillosis: Clinical Manifestations § Pulmonary aspergillosis is the most common presentation § Invasive pulmonary aspergillosis associated with fever, cough, dyspnea, pleuritic pain § Additional manifestations include necrotizing tracheobronchitis, pseudomembranous tracheobronchitis, CNS involvement, cutaneous, sinus, middle ear and mastoid infection 4 July 2009 www. aidsetc. org
Aspergillosis: Diagnosis § Usually isolated from the blood but also readily isolated from lung, sinus, brain, and skin biopsy § Definitive diagnosis includes histopathologic demonstration of organisms in biopsy specimens § Presumptive diagnosis of respiratory tract infection can be made if Aspergillus species is recovered from respiratory sample 5 July 2009 www. aidsetc. org
Aspergillosis: Diagnosis (2) § Chest radiograph demonstrates either diffuse interstitial pneumonitis or localized wedge-shaped infiltrates § CT of chest may be used to identify a “halo” sign § Cavitation and air crescent formation in chest CDT more frequent in older children and adults 6 July 2009 www. aidsetc. org
Aspergillosis: Prevention § Consider excluding plants and flowers from rooms and avoiding food items such as nuts and spices § Erect suitable barriers between patient care and construction sites, clean shower heads routinely as well as hotwater faucets and air-handling systems 7 July 2009 www. aidsetc. org
Aspergillosis: Treatment § Voriconazole is recommended for treatment of invasive aspergillosis § Adult data indicate that voriconazole is superior to amphotericin B but data in children are limited § Recommended dosage for children is 6 -8 mg/kg IV (or 8 mg/kg orally) Q 12 H, followed by 7 mg/kg IV or orally twice daily § Treatment is continued for 12 weeks 8 July 2009 www. aidsetc. org
Aspergillosis: Adverse Effects and Treatment Failure § Voriconazole side effects include reversible dose-dependent visual disturbances, elevated liver enzymes, and occasional skin rash § Amphotericin toxicity is associated primarily with fever, chills, and nephrotoxicity § Efficacy of antifungal therapy for aspergillosis is poor § Experimental approaches include evaluation of caspofungin 9 July 2009 www. aidsetc. org
Candida Infections: Epidemiology § Most common fungal infections in HIV-infected children § Thrush and diaper dermatitis occur in 50 -85% of HIV-infected children § In pre-ART era, oropharyngeal candidiasis found in 94% of children with Candida esophagitis § Disseminated candidiasis rare in children except those with CMV or HSV coinfection, and those with central venous catheter 10 July 2009 www. aidsetc. org
Candida Infections: Epidemiology (2) § A substantial percentage of children with fungemia receive oral, systemically absorbable azole antifungals (eg, ketoconazole) § Complications include disseminated infection of bone, liver, and kidney; endophthalmitis § Mortality from disseminated candidiasis >90% in children with fever and symptoms >14 days 11 July 2009 www. aidsetc. org
Candida Infections: Clinical Manifestations § Thrush and erythematous, hyperplastic, and angular cheilitis § Esophageal candidiasis may present with odynophagia, dysphagia, or retrosternal pain § Children may develop nausea, vomiting, or weight loss and dehydration § New onset of fever in individuals with central venous catheters § Systemic fungemia may lead to endophthalmitis 12 July 2009 www. aidsetc. org

Candida Infections: Diagnosis § Culture and KOH preparation with microscopic demonstration of budding yeast cells in wet mounts or biopsy § Blood culture using lysis centrifugation § “Cobblestone” appearance on barium swallow § Perform endoscopy in refractory cases to look for CMV, HSV, MAC coinfections § Research studies or evaluating detection of candidate antigens for early diagnosis 13 July 2009 www. aidsetc. org
Candida Infections: Prevention § Routine primary prophylaxis of candidiasis in HIV-infected children is not indicated § Candida organisms are common commensals on mucosal surfaces in healthy individuals and no measures are available to reduce exposure 14 July 2009 www. aidsetc. org

Candida Infections: Treatment Treat early uncomplicated oropharyngeal candidiasis (OPC) with topical therapy § Cotrimoxazole: 10 mg troches 4 -5 times/day for 2 weeks (B II) § Nystatin suspension: 4 -6 m. L (400, 000 -600, 000 units/m. L) 4 times/day § Amphotericin B suspension: (100 mg/m. L) 1 m. L 4 times/day 15 July 2009 www. aidsetc. org
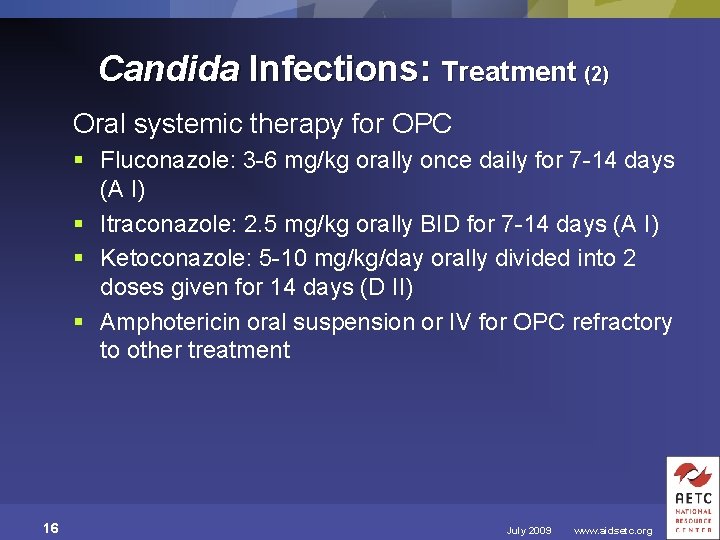
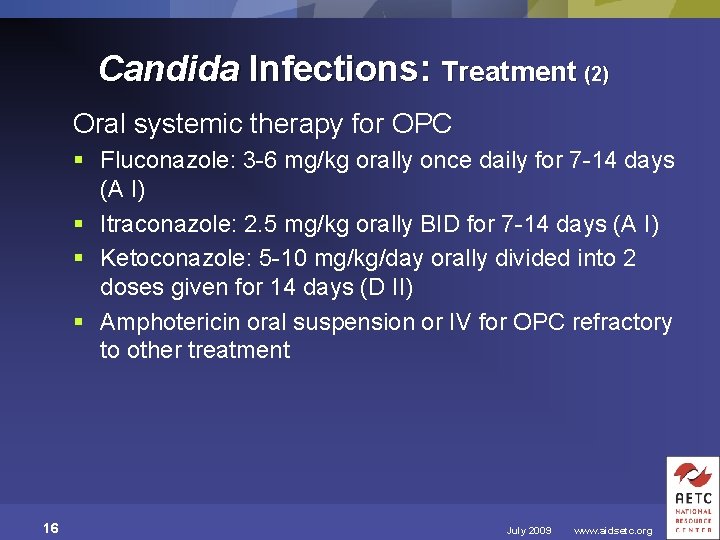
Candida Infections: Treatment (2) Oral systemic therapy for OPC § Fluconazole: 3 -6 mg/kg orally once daily for 7 -14 days (A I) § Itraconazole: 2. 5 mg/kg orally BID for 7 -14 days (A I) § Ketoconazole: 5 -10 mg/kg/day orally divided into 2 doses given for 14 days (D II) § Amphotericin oral suspension or IV for OPC refractory to other treatment 16 July 2009 www. aidsetc. org
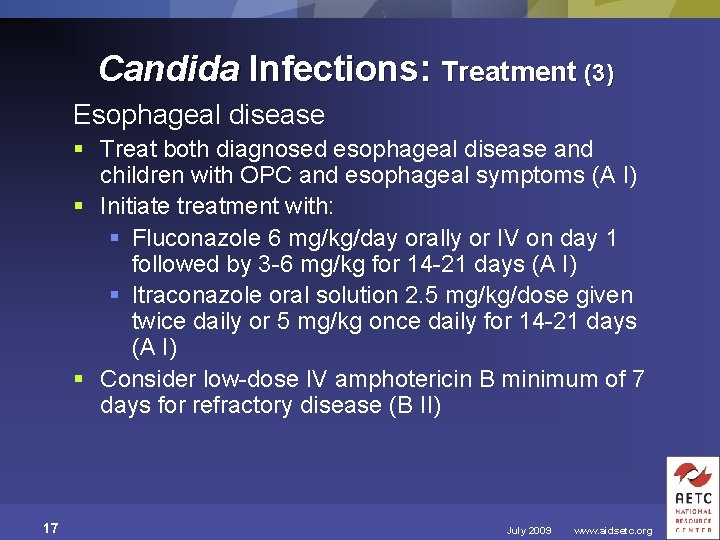
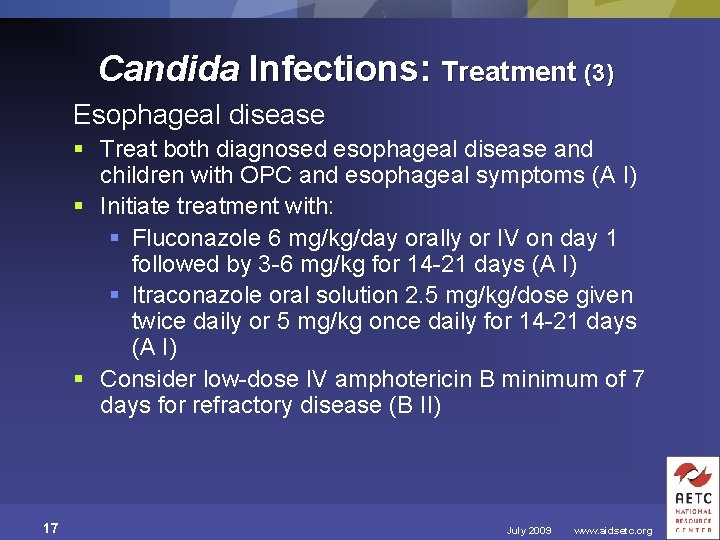
Candida Infections: Treatment (3) Esophageal disease § Treat both diagnosed esophageal disease and children with OPC and esophageal symptoms (A I) § Initiate treatment with: § Fluconazole 6 mg/kg/day orally or IV on day 1 followed by 3 -6 mg/kg for 14 -21 days (A I) § Itraconazole oral solution 2. 5 mg/kg/dose given twice daily or 5 mg/kg once daily for 14 -21 days (A I) § Consider low-dose IV amphotericin B minimum of 7 days for refractory disease (B II) 17 July 2009 www. aidsetc. org
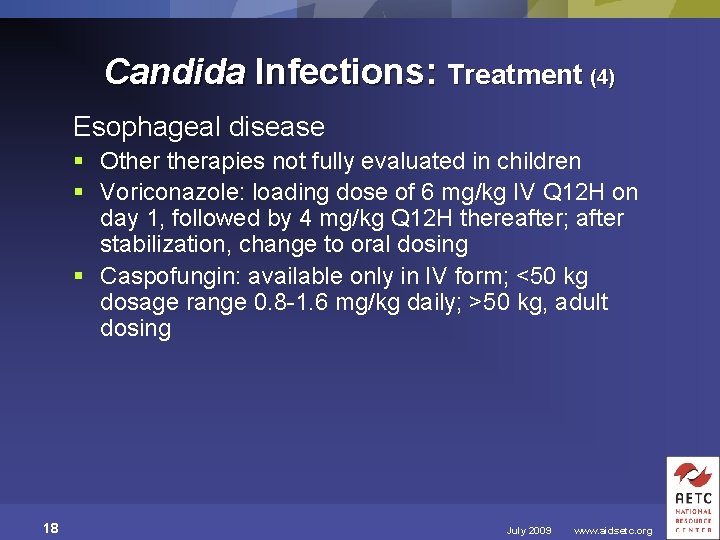
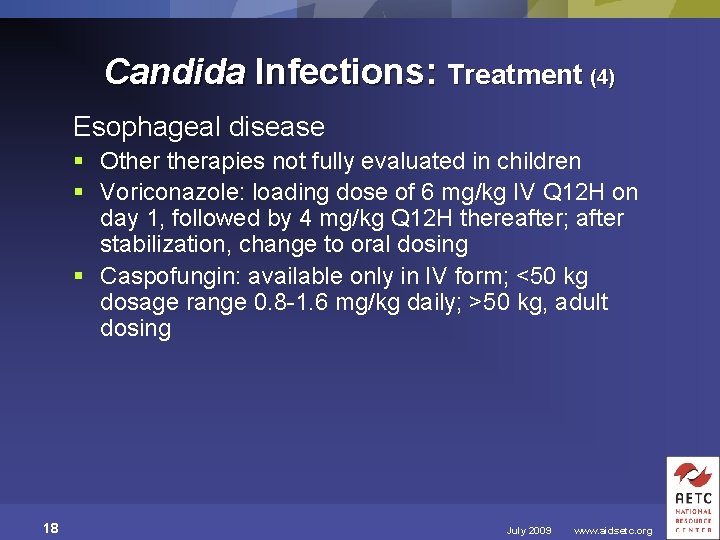
Candida Infections: Treatment (4) Esophageal disease § Otherapies not fully evaluated in children § Voriconazole: loading dose of 6 mg/kg IV Q 12 H on day 1, followed by 4 mg/kg Q 12 H thereafter; after stabilization, change to oral dosing § Caspofungin: available only in IV form; <50 kg dosage range 0. 8 -1. 6 mg/kg daily; >50 kg, adult dosing 18 July 2009 www. aidsetc. org
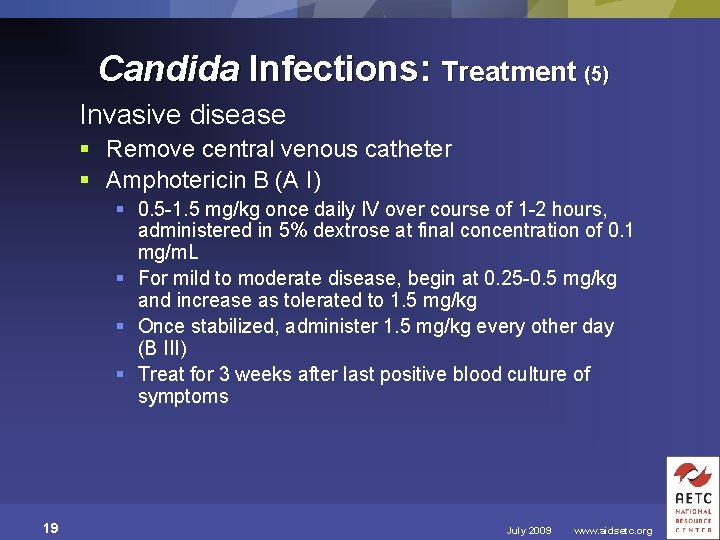
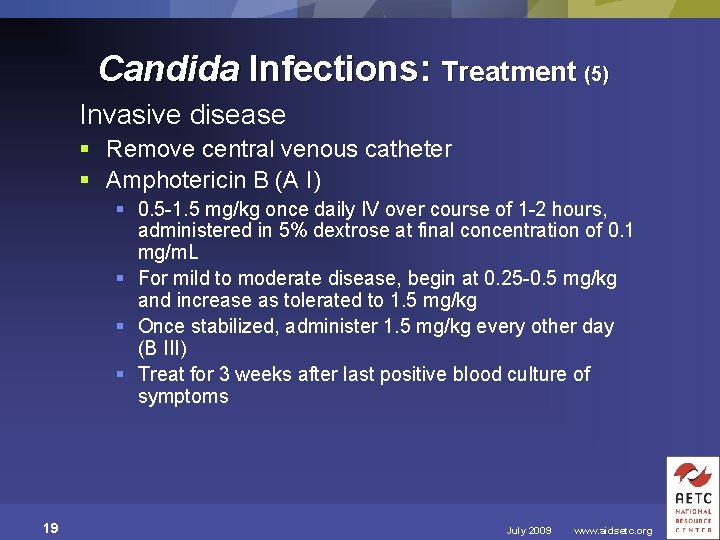
Candida Infections: Treatment (5) Invasive disease § Remove central venous catheter § Amphotericin B (A I) § 0. 5 -1. 5 mg/kg once daily IV over course of 1 -2 hours, administered in 5% dextrose at final concentration of 0. 1 mg/m. L § For mild to moderate disease, begin at 0. 25 -0. 5 mg/kg and increase as tolerated to 1. 5 mg/kg § Once stabilized, administer 1. 5 mg/kg every other day (B III) § Treat for 3 weeks after last positive blood culture of symptoms 19 July 2009 www. aidsetc. org
Candida Infections: Treatment (6) Invasive disease: alternative therapy § Fluconazole in stable patients with uncomplicated candidemia without previous azole treatment (identification of Candida species essential; C krusei and C glabrata are resistant) (E III) § Amphotericin lipid formulations (limited pediatric experience) § Amphotericin lipid complex (ABLC, Abelcet) § Liposomal amphotericin lipid complex (Am. Bisome) § Amphotericin B cholesteryl sulfate complex (ABCD) 20 July 2009 www. aidsetc. org

Candida Infections: Treatment (7) Treatment under development § Caspofungin, micafungin, and anidulafungin have been studied in battles with HIV infection, neutropenic children at risk of fungal infection in children with documented candidiasis § Data on HIV-infected children are limited 21 July 2009 www. aidsetc. org
Candida Infections: Treatment (8) Amphotericin toxicity § Nephrotoxicity: azotemia, hypokalemia § Nephrotoxicity can be minimized by hydration with 0. 9% saline intravenously 30 minutes before amphotericin B infusion § Infusion-related chills, fever, and vomiting; pretreat with acetaminophen or diphenhydramine § Rarely: hypotension, arrhythmias, neurotoxicity, hepatic toxicity 22 July 2009 www. aidsetc. org
Candida Infections: Treatment (9) Fluconazole, itraconazole, ketoconazole toxicity § Inhibition of CYP 450 -dependent hepatic enzymes can result in either decreased levels of azole when administered with other drugs with hepatic metabolism or increased levels of other drugs with hepatic metabolism § Nausea, vomiting, rash, pruritus, Stevens-Johnson syndrome (rare), increased liver enzymes, hepatitis, leukopenia, anemia, hemolytic anemia, alopecia (fluconazole) 23 July 2009 www. aidsetc. org
Candida Infections: Treatment Failure Oral pharyngeal and esophageal candidiasis § Initial failure should be treated with oral fluconazole, itraconazole, oral amphotericin B, or low-dose IV amphotericin B Invasive disease § Amphotericin B lipid formulations can be used for children who cannot tolerate amphotericin B, have disseminated Candida infection that is resistance to amphotericin B, or are at risk of nephrotoxicity 24 July 2009 www. aidsetc. org
Coccidioidomycosis: Epidemiology § Increased risk of infection with Coccidioides immitis and Coccidioides posadasii among HIV -infected children in endemic areas (eg, southwestern United States, northern Mexico, Central and South America) § Primary infection of newborn rare § In utero and perinatal transmission of C immitis reported § Reports of infection in nonendemic areas usually due to reactivation 25 July 2009 www. aidsetc. org
Coccidioidomycosis: Clinical Manifestations § Fever and dyspnea most common presentation § Chills, weight loss, lymphadenopathy, chest pain, diffuse reticulonodular pulmonary infiltrates, meningitis § Disseminated disease associated with erythema multiforme; erythema nodosum; erythematous maculopapular rash; arthralgia; bone, joint, and CNS infection 26 July 2009 www. aidsetc. org
Coccidioidomycosis: Diagnosis § Direct examination and culture of respiratory secretions and CSF or biopsy of lesions § Blood cultures positive in 15% of cases § Complement fixation assay detects Ig. G antibody, positive Ig. M assays suggest active or recent infection, complement fixation titers > 1: 16 correlate with presence and severity of extrapulmonary infection 27 July 2009 www. aidsetc. org
Coccidioidomycosis: Prevention § Difficult to avoid exposure in endemic areas § Exposure can be reduced by avoiding activities that predispose to inhalation of spores such as disturbing contaminated soil, being outdoors during dust storms 28 July 2009 www. aidsetc. org
Coccidioidomycosis: Treatment § Limited data in children; recommendations based on adult data § Treat diffuse pulmonary disease or disseminated disease with amphotericin B dosage of 0. 5 -1. 5 mg/kg/day until clinical improvement occurs (A II) § Follow with chronic suppressive fluconazole or itraconazole therapy (A II) § Alterative therapy: fluconazole 5 -6 mg/kg BID or itraconazole 4 -10 mg/kg BID for 3 days followed by 2 -5 mg/kg BID (B III) 29 July 2009 www. aidsetc. org

Coccidioidomycosis: Treatment (2) CNS infection, including meningitis § High-dose fluconazole 5 -6 mg/kg BID § If unresponsive to fluconazole, use IV amphotericin B augmented by intrathecal amphotericin B (C I) 30 July 2009 www. aidsetc. org

Coccidioidomycosis: § § 31 Monitoring, Adverse Events and Toxicity Monitoring of complement fixing Ig. G antibody is useful Toxicity of antifungal drugs includes fevers, chills, nausea and vomiting, nephrotoxicity Interaction of all antifungal agents with ARVs should be investigated; fluconazole and itraconazole appear to be safe in combination with ARVs Voriconazole should be avoided in patients on PIs or NNRTIs July 2009 www. aidsetc. org
Cryptococcosis: Epidemiology § Most infections caused by Cryptococcosis neoformans and Cryptococcosis gattii § Infection occurs primarily in tropical and subtropical areas § Low incidence of infection in children, especially with use of ART § Children usually infected during 6 -12 year age range § Usually severely immunosuppressed 32 July 2009 www. aidsetc. org
Cryptococcosis: Clinical Manifestations § Meningoencephalitis most common manifestation § Fever, headache, altered mental status evolving over days to weeks § Acute illness with nuchal rigidity, seizures, focal neurologic signs observed in developing countries § Translucent, umbilicated, papules, nodules, ulcers, infiltrated plaques seen in disseminated disease § Pulmonary cryptococcosis unusual in children 33 July 2009 www. aidsetc. org

Cryptococcosis: Diagnosis § Microscopic examination of CSF on India ink-stained wet mounts § Detection of cryptococcal antigen in CSF, serum, bronchoalveolar lavage fluid (can be negative in culture-positive meningitis) § Fungal cultures from CSF, sputum, and blood cultures can identify the organism § Antigen levels useful in evaluating response to treatment and relapse § Pulmonary disease diagnosed by bronchoalveolar lavage and direct examination of India ink-stained specimens 34 July 2009 www. aidsetc. org
Cryptococcosis: Prevention § No proven strategies to prevent exposure § Believed to be acquired by inhalation of aerosolized particles from the environment 35 July 2009 www. aidsetc. org
Cryptococcosis: Treatment Not well studied in children; infection is often fatal in the absence of treatment CNS Disease § Amphotericin B induction (0. 7 -1. 5 mg/kg/day IV) combined with 2 weeks of flucytosine (25 mg/kg/dose given 4 times daily) followed by fluconazole for a minimum of 8 weeks § After symptoms are controlled, treat with fluconazole or itraconazole maintenance § Use amphotericin B alone if flucytosine is not tolerated § Fluconazole plus flucytosine is an alternative to amphotericin B (limited data in children) 36 July 2009 www. aidsetc. org
Cryptococcosis: Treatment (2) Pulmonary and extrapulmonary cryptococcosis § No clinical trials on the outcome of non-CNS cryptococcosis in HIV-infected patients § Treat with amphotericin B with or without the addition of fluconazole (A III) § Fluconazole or itraconazole should be continued long-term 37 July 2009 www. aidsetc. org
Cryptococcosis: Monitoring and Drug Toxicity Amphotericin toxicity § Nephrotoxicity: azotemia, hypokalemia § Nephrotoxicity can be minimized by hydration with 0. 9% saline intravenously 30 minutes before amphotericin B infusion § Infusion-related chills, fever, and vomiting; pretreat with acetaminophen or diphenhydramine § Rarely: hypotension, arrhythmias, neurotoxicity, hepatic toxicity 38 July 2009 www. aidsetc. org

Cryptococcosis: Monitoring and Drug Toxicity (2) Flucytosine toxicity § Bone marrow: anemia, leukopenia, thrombocytopenia § Liver, GI, and renal toxicity Fluconazole toxicity § Potential interaction with ARV should be evaluated before initiating treatment (A III) 39 July 2009 www. aidsetc. org
Cryptococcosis: § § § 40 IRIS and Treatment Failure IRIS related to cryptococcosis can present within weeks Optimal treatment of patients experiencing treatment failure has not been defined Patients failing initial azole treatment should be switched to amphotericin B in combination with flucytosine Consider use of liposomal amphotericin B Experience with posaconazole or voriconazole is limited July 2009 www. aidsetc. org
Histoplasmosis: § § 41 Epidemiology Pathogen is Histoplasma capsulatum Incidence of disseminated histoplasmosis in HIV-infected children in the United States is <0. 4% Incidence is higher in countries such as Brazil, Argentina, and Mexico (2. 7% to 3. 8%) No evidence of dissemination of maternal infection to the fetus or greater severity of infection during pregnancy July 2009 www. aidsetc. org

Histoplasmosis: Clinical Manifestations § Prolonged fever is the most common presentation § Malaise, weight loss, and nonproductive cough § Primary pulmonary focus leads to widespread dissemination in children § Pulmonary manifestations common § Physical findings include hepatosplenomegaly, erythematous nodular coetaneous lesions, CNS involvement with meningitis § Anemia, thrombocytopenia, elevated liver transaminases § Progressive disseminated histoplasmosis (PDH) is fatal if untreated 42 July 2009 www. aidsetc. org
Histoplasmosis: Diagnosis § Serologic testing using CF and immunodiffusion is insensitive in the presence of HIV infection. § Positive in most patients but not useful for diagnosis of acute infection § For diagnosis of CNS disease, a combination of CSF antibody, antigen, and culture is most sensitive § Skin testing not recommended for diagnosis 43 July 2009 www. aidsetc. org
Histoplasmosis: § § 44 Diagnosis (2) Culture of Histoplasma from blood or other sources Detection of H capsulatum polysaccharide antigen in urine, blood, CSF, or bronchoalveolar lavage using EIA sensitivity greater in disseminated disease or acute pulmonary disease; greater in urine than in serum Antigen levels decline with treatment and correlate with both response to treatment and relapse July 2009 www. aidsetc. org

Histoplasmosis: Prevention § Most infections occur without a recognized history of exposure § Sites and conditions commonly implicated include outbreaks of soil contamination with bird or bat droppings, older urban and rural structures, and decaying vegetation 45 July 2009 www. aidsetc. org
Histoplasmosis: Treatment § Limited data for children; recommendations based on adult data § PDH is fatal without treatment and should be treated with either amphotericin B or itraconazole § Fluconazole has been used successfully as an alternative for patients with mild disease and for those who cannot tolerate itraconazole 46 July 2009 www. aidsetc. org

Histoplasmosis: Treatment (2) § Amphotericin B for patients with severe disseminated disease requiring hospitalization and for those who are immunocompromised § Amphotericin B induction dosage: 1 mg/kg for 4 -6 weeks followed by itraconazole chronic suppressive therapy for 12 months (A I) § After successful treatment of acute disease, use chronic lifelong suppressive therapy with itraconazole § Liposomal amphotericin B alternative in event of amphotericin B intolerance 47 July 2009 www. aidsetc. org
Histoplasmosis: Monitoring and Adverse Effects § Antigen levels should be monitored during treatment and for 1 year thereafter § Adverse effects of amphotericin B include nephrotoxicity, infusion related fever, chills, nausea, and vomiting § Azole drugs inhibit CYP 450 -dependent hepatic enzymes, warranting careful review of drug interactions when using ARVs 48 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Epidemiology § Organisms are found worldwide in the lungs of humans and lower animals § Antibody in 80% of normal children by 4 years § Most common AIDS indicator disease in children § Incidence highest in first year of life, peaking at 3 -6 months § Accounted for 57% of AIDS-defining illnesses in infants age <1 year pre-ART § CD 4 T-cell count not a good indicator of risk in infants <1 year old § Infection now unusual owing to routine prophylaxis with TMP-SMX 49 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Clinical Manifestations § Fever, tachypnea, cough, dyspnea, poor feeding, weight loss § Abrupt or insidious onset § Bibasilar rales with evidence of hypoxia and respiratory distress § Extrapulmonary locations: spleen, liver, colon, pancreas, ear, eye, GI tract, bone marrow, heart, kidney, lymph nodes, CNS 50 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Diagnosis § Hypoxia with low arterial oxygen pressure (alveolar-arterial oxygen gradient >30 mm. Hg) § Definitive diagnosis requires demonstrating organism § Induced sputum (difficult <2 years) § Bronchoscopy with bronchoalveolar lavage § Fiberoptic bronchoscopy with biopsy – generally not recommended 51 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Diagnosis (2) § Open lung biopsy most sensitive § Requires thoracotomy, chest tube drainage § Organisms seen on biopsy with: § § Gomori methenamine silver stain Toluidine blue stain Giemsa or Wright stain Monoclonal antibody § DNA PCR for Pneumocystis MSG gene in fluids, lavage – sensitive but less specific than histology 52 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Prevention § Need for isolation of hospitalized patients has not been demonstrated, but when prophylaxis cannot be given, may need to isolate patient or susceptible contacts § Infants born to HIV-infected mothers should be considered for prophylaxis at 4 -6 weeks of age and continued until 1 year of age (A II) 53 July 2009 www. aidsetc. org
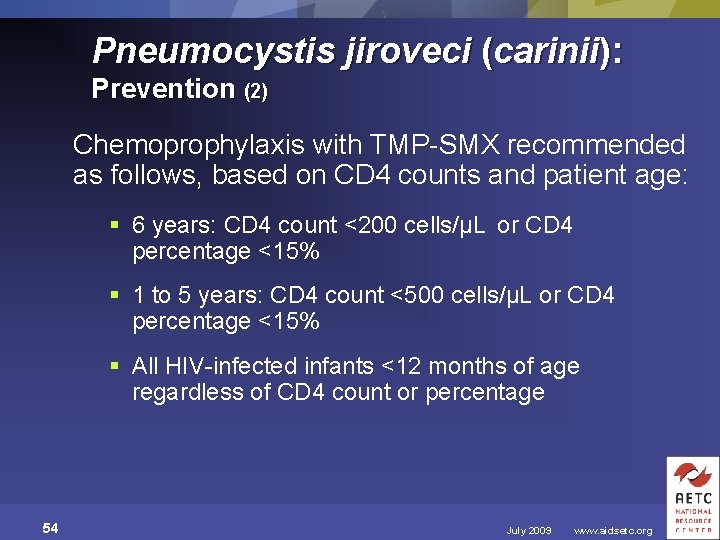
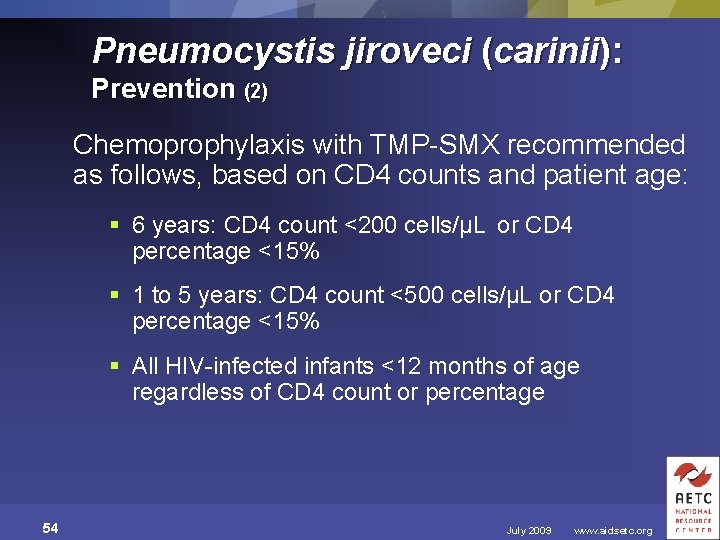
Pneumocystis jiroveci (carinii): Prevention (2) Chemoprophylaxis with TMP-SMX recommended as follows, based on CD 4 counts and patient age: § 6 years: CD 4 count <200 cells/µL or CD 4 percentage <15% § 1 to 5 years: CD 4 count <500 cells/µL or CD 4 percentage <15% § All HIV-infected infants <12 months of age regardless of CD 4 count or percentage 54 July 2009 www. aidsetc. org

Pneumocystis jiroveci (carinii): Treatment TMP-SMX (A I) § >2 months 15 -20 mg/kg/day of TMP component IV in 3 -4 divided doses § Infuse over course of 1 hour § Administer for 21 days § Can be given orally in children with mild to moderate disease § Lifelong prophylaxis indicated 55 July 2009 www. aidsetc. org

Pneumocystis jiroveci (carinii): Treatment (2) § Adverse reactions: § Rash § Stevens-Johnson syndrome (rare) § Neutropenia, thrombocytopenia, megaloblastic or aplastic anemia 56 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Treatment (3) Pentamidine isethionate § Recommended for patients with intolerance to TMP-SMX or clinical failure with TMP-SMX (A I); do not combine use § 4 mg/kg/day IV once daily over period of 6090 minutes § Consider oral atovaquone after 7 -10 days (B III) 57 July 2009 www. aidsetc. org

Pneumocystis jiroveci (carinii): Treatment Alternatives Atovaquone (B I) § Limited data in children § 30 -40 mg/kg/day divided into 2 doses, given with fatty foods § Infants 3 -24 months may require 45 mg/kg/day divided into 2 doses, given with fatty foods (A II) § Adverse reactions include rash, nausea, diarrhea, increased liver enzymes 58 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Treatment Alternatives (2) Clindamycin/primaquine § Used for mild to moderate PCP in adults; no data in children (C III) § Primaquine contraindicated in G 6 PD deficiency 59 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Treatment Alternatives (3) Clindamycin/primaquine § Pediatric clindamycin dosing based on other uses: 20 -40 mg/kg/day IV divided into 3 or 4 doses, administered for 21 days § Primaquine dosing based on malaria: 0. 3 mg/kg daily of the base, administered orally for 21 days § Adverse reactions include rash, nausea, diarrhea, pseudomembranous colitis 60 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Treatment Alternatives (4) Dapsone/TMP § Use for mild to moderate PCP in adults; no data in children (C III) § Dapsone dosage <13 years 2 mg/kg/day orally once daily (A II) for 21 days § TMP 15/mg/kg/day orally divided into 3 daily doses for 21 days § Adverse reactions include rash, anemia, thrombocytopenia, increased liver enzymes 61 July 2009 www. aidsetc. org
Pneumocystis jiroveci (carinii): Treatment Adjunct Corticosteroids § Consider use in moderate to severe PCP § Use within 72 hours of diagnosis § Results in reduced respiratory failure, decreased ventilation requirements, and decreased mortality 62 July 2009 www. aidsetc. org
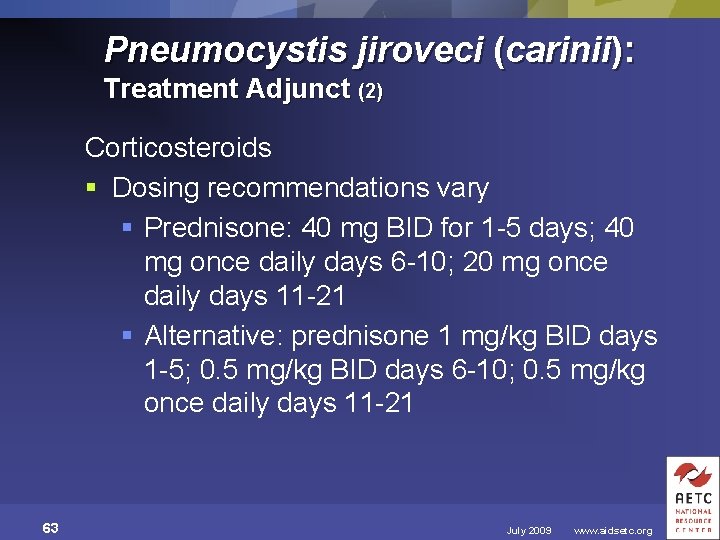
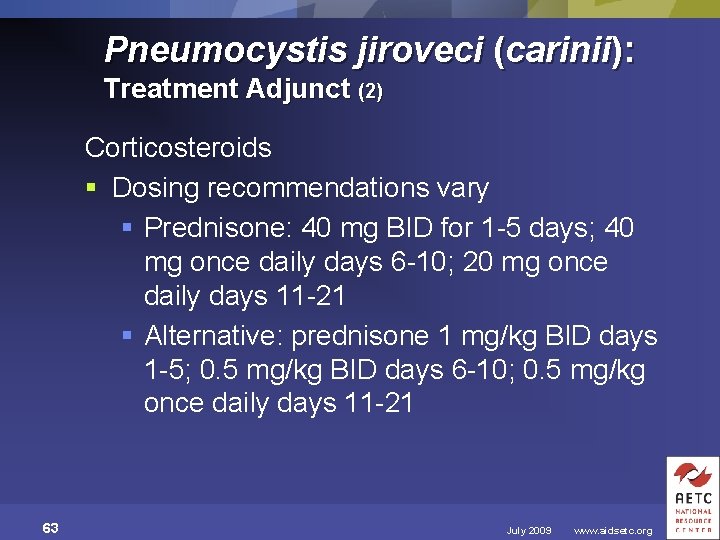
Pneumocystis jiroveci (carinii): Treatment Adjunct (2) Corticosteroids § Dosing recommendations vary § Prednisone: 40 mg BID for 1 -5 days; 40 mg once daily days 6 -10; 20 mg once daily days 11 -21 § Alternative: prednisone 1 mg/kg BID days 1 -5; 0. 5 mg/kg BID days 6 -10; 0. 5 mg/kg once daily days 11 -21 63 July 2009 www. aidsetc. org
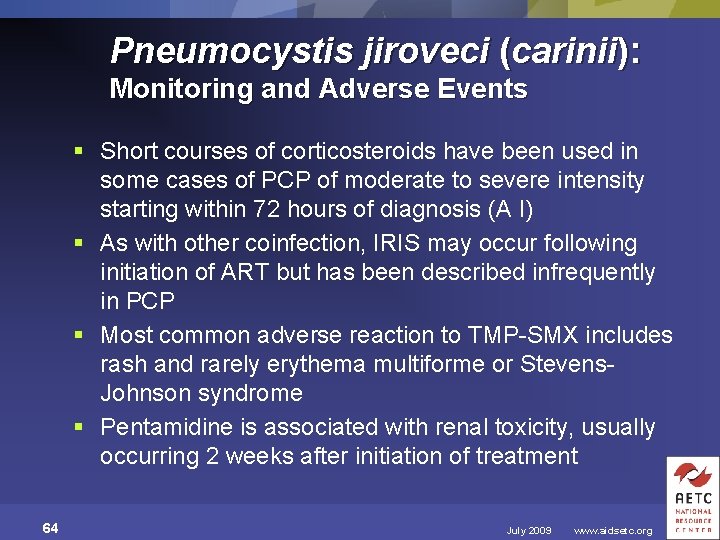
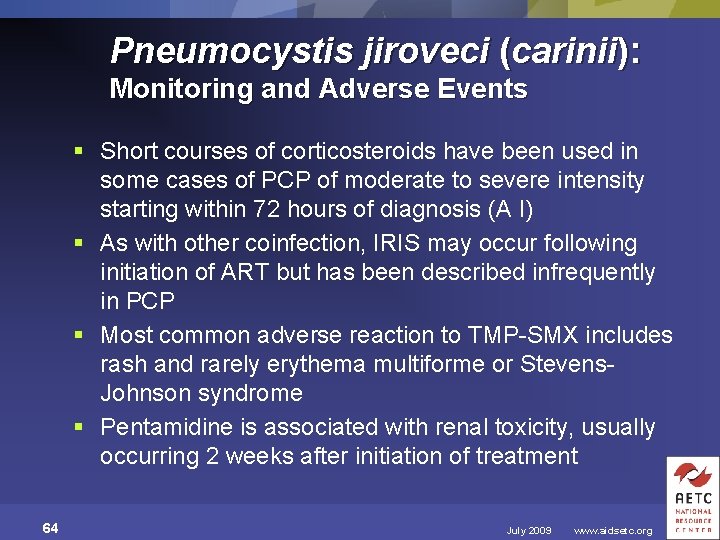
Pneumocystis jiroveci (carinii): Monitoring and Adverse Events § Short courses of corticosteroids have been used in some cases of PCP of moderate to severe intensity starting within 72 hours of diagnosis (A I) § As with other coinfection, IRIS may occur following initiation of ART but has been described infrequently in PCP § Most common adverse reaction to TMP-SMX includes rash and rarely erythema multiforme or Stevens. Johnson syndrome § Pentamidine is associated with renal toxicity, usually occurring 2 weeks after initiation of treatment 64 July 2009 www. aidsetc. org
About This Slide Set § This presentation was prepared by Arthur Ammann, MD, Clinical Professor of Pediatrics University of California and President of Global Strategies for HIV Prevention for the AETC National Resource Center, in July 2009 § See the AETC NRC website for the most current version of this presentation: http: //www. aidsetc. org 65 July 2009 www. aidsetc. org
 Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Opportunistic approach adalah model proses
Opportunistic approach adalah model proses Nation and macalister 2010
Nation and macalister 2010 A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Ttkg
Ttkg Odg guidelines by state
Odg guidelines by state Sbp prophylaxis guidelines
Sbp prophylaxis guidelines Allergic crease adalah
Allergic crease adalah Management of allergic rhinitis
Management of allergic rhinitis Ich treatment guidelines
Ich treatment guidelines Hepatic encephalopathy staging
Hepatic encephalopathy staging Storch infections
Storch infections Storch infections
Storch infections Cryptosporidiose
Cryptosporidiose Eye infections
Eye infections Postpartum infections
Postpartum infections Genital infections
Genital infections Genital infections
Genital infections Cell lysis complement system
Cell lysis complement system Acute gingival infections
Acute gingival infections Fspos
Fspos Typiska drag för en novell
Typiska drag för en novell Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Vilotidsbok
Vilotidsbok Sura för anatom
Sura för anatom Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Debattartikel mall
Debattartikel mall För och nackdelar med firo
För och nackdelar med firo Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Kraft per area
Kraft per area Publik sektor
Publik sektor Kyssande vind analys
Kyssande vind analys Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Kanaans land
Kanaans land Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Mjälthilus
Mjälthilus Bästa kameran för astrofoto
Bästa kameran för astrofoto Cks
Cks Byggprocessen steg för steg
Byggprocessen steg för steg Bra mat för unga idrottare
Bra mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Mall för referat
Mall för referat Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Atmosfr
Atmosfr Borra hål för knoppar
Borra hål för knoppar Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Fr formel
Fr formel