Guidelines for Prevention and Treatment of Opportunistic Infections

- Slides: 31
Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents Bacterial Enteric Infections Prepared by the AETC National Coordinating Resource Center based on recommendations from the CDC, Slide Set National Institutes of Health, and HIV Medicine Association/Infectious Diseases Society of America
About This Presentation These slides were developed using recommendations published in May 2013 and updated in May 2016. The intended audience is clinicians involved in the care of patients with HIV. Users are cautioned that, because of the rapidly changing field of HIV care, this information could become out of date quickly. Finally, it is intended that these slides be used as prepared, without changes in either content or attribution. Users are asked to honor this intent. – AETC National Resource Center http: //www. aidsetc. org May 2016 2

Bacterial Enteric Infections § § § Epidemiology Clinical Manifestations Diagnosis Prevention Treatment Considerations in Pregnancy www. aidsetc. org May 2016 3
Bacterial Enteric Disease: Epidemiology § Higher incidence of gram-negative enteric infections among HIV-infected patients § Risk greatest if CD 4 <200 cells/µL or AIDS § Risk decreased with ART § Most commonly cultured bacteria: § § § Salmonella Shigella Campylobacter E coli Clostridium difficile www. aidsetc. org May 2016 4
Bacterial Enteric Disease: Epidemiology (2) § Source usually ingestion of contaminated food or water § Other risks: § Oral-fecal exposure through sexual activity (especially Shigella and Campylobacter) § HIV-related alterations in mucosal immunity or intestinal integrity, gastric acid-blocking medications www. aidsetc. org May 2016 5
Bacterial Enteric Disease: Clinical Manifestations § Three major clinical syndromes § Self-limited gastroenteritis § Diarrheal disease +/- fever, bloody diarrhea, weight loss, possible bacteremia § Bacteremia associated with extraintestinal involvement, with or without GI illness www. aidsetc. org May 2016 6
Bacterial Enteric Disease: Clinical Manifestations (2) § Severe diarrhea: ≥ 6 loose stools per day, with our without other signs/symptoms § In HIV infection: § Greater risk of more serious illness with greater immunosuppression § Relapses may occur after treatment § Recurrent Salmonella bacteremia is an AIDSdefining illness www. aidsetc. org May 2016 7
Bacterial Enteric Disease: Diagnosis § History: exposures; medication review; diarrhea frequency, volume, presence of blood; associated signs/symptoms (eg, fever) § Physical exam including temperature, assessment of hydration and nutritional status www. aidsetc. org May 2016 8
Bacterial Enteric Disease: Diagnosis (2) § Stool and blood cultures § Obtain blood cultures in patients with diarrhea and fever § Routine stool culture may not identify non-jejuni noncoli Campylobacter species; request special testing for these if initial evaluation is unrevealing § Antibiotic susceptibility should be performed on all stool samples § Increased rates of resistant and multidrug-resistant Enterobacteriaceae, especially outside the U. S. § Consider possible resistance when prescribing empiric treatment for persons who develop diarrhea or systemic infection while traveling or returning to the U. S. www. aidsetc. org May 2016 9
Bacterial Enteric Disease: Diagnosis (3) § C difficile toxin or PCR § If recent or current antibiotic exposure, cancer chemotherapy, recent hospitalization, residence in long-term care facility, CD 4 <200 cells/µL, acid-suppressive medications, moderate-severe community-acquired diarrhea § Endoscopy § If stool studies and blood culture are nondiagnostic, or if treatment for an established diagnosis fails § May diagnose nonbacterial causes (eg, parasites, CMV, MAC, noninfectious causes) § Consider STDs (eg, rectal infections caused by lymphogranuloma venereum or N gonorrhoeae) www. aidsetc. org May 2016 10
Bacterial Enteric Disease: Preventing Exposure § Advice to patients: § Handwashing: § After potential contact with feces, pets or other animals, gardening or contact with soil; before preparing food, eating; before and after sex § For prevention of enteric infection, soap and water preferred over alcohol-based cleansers (these do not kill C difficile spores, are partly active against norovirus and Cryptosporidium) § Sex: § Avoid unprotected sexual practices that might result in oral exposure to feces www. aidsetc. org May 2016 11
Bacterial Enteric Disease: Preventing Disease § Antimicrobial prophylaxis usually not recommended, including for travellers § Risk of adverse reactions, resistant organisms, C difficile infection § Can be considered in rare cases, depending on level of immunosuppression and the region and duration of travel § Fluoroquinolone (FQ) or rifaximin § TMP-SMX may give limited protection (eg, if pregnant or already taking for PCP prophylaxis) www. aidsetc. org May 2016 12
Bacterial Enteric Disease: Treatment § Treatments usually the same as in HIVuninfected patients § Give oral or IV rehydration if indicated § Advise bland diet and avoidance of fat, dairy, and complex carbohydrates § Effectiveness and safety of probiotics or antimotility agents not adequately studied in HIVinfected patients § Avoid antimotility agents if concern about inflammatory diarrhea www. aidsetc. org May 2016 13
Bacterial Enteric Disease: Treatment (2) § Empiric Therapy § CD 4 count and clinical status guide initiation and duration of empiric antibiotics, eg: § CD 4 count >500 cells/µL with mild symptoms: only rehydration may be needed § CD 4 count 200 -500 cells/µL and symptoms that compromise quality of life: consider short course of antibiotics § CD 4 count <200 cells/µL with severe diarrhea, bloody stool, or fevers/chills: diagnostic evaluation and antibiotics; empiric treatment with ciprofloxacin is reasonable www. aidsetc. org May 2016 14
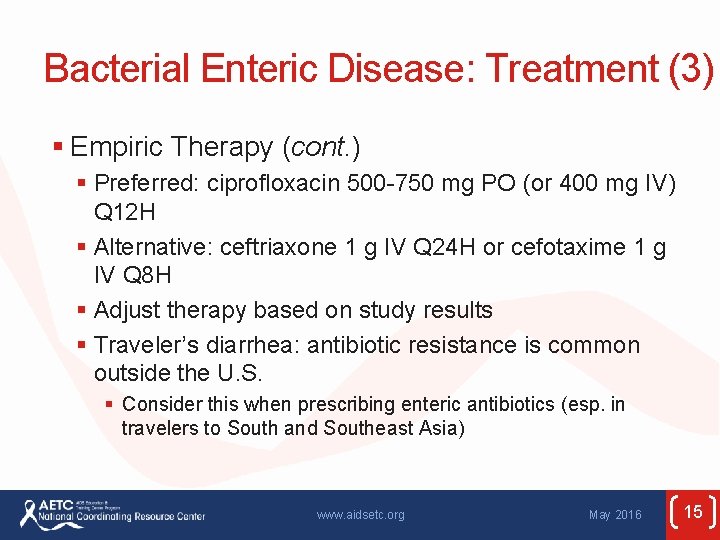
Bacterial Enteric Disease: Treatment (3) § Empiric Therapy (cont. ) § Preferred: ciprofloxacin 500 -750 mg PO (or 400 mg IV) Q 12 H § Alternative: ceftriaxone 1 g IV Q 24 H or cefotaxime 1 g IV Q 8 H § Adjust therapy based on study results § Traveler’s diarrhea: antibiotic resistance is common outside the U. S. § Consider this when prescribing enteric antibiotics (esp. in travelers to South and Southeast Asia) www. aidsetc. org May 2016 15
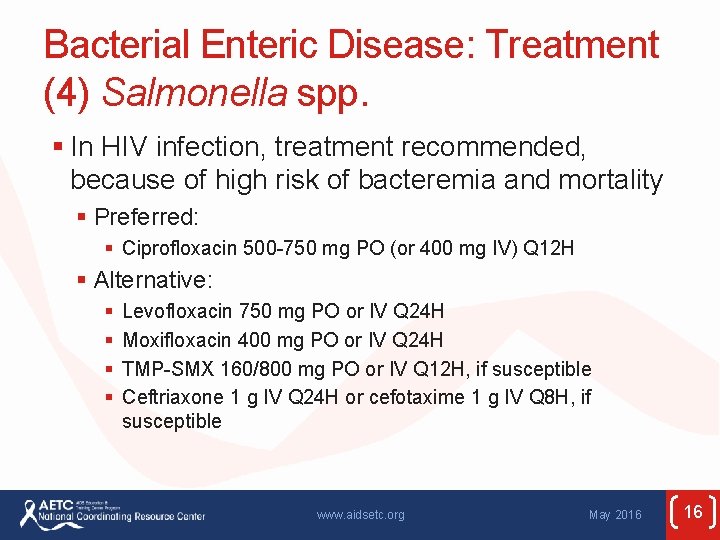
Bacterial Enteric Disease: Treatment (4) Salmonella spp. § In HIV infection, treatment recommended, because of high risk of bacteremia and mortality § Preferred: § Ciprofloxacin 500 -750 mg PO (or 400 mg IV) Q 12 H § Alternative: § § Levofloxacin 750 mg PO or IV Q 24 H Moxifloxacin 400 mg PO or IV Q 24 H TMP-SMX 160/800 mg PO or IV Q 12 H, if susceptible Ceftriaxone 1 g IV Q 24 H or cefotaxime 1 g IV Q 8 H, if susceptible www. aidsetc. org May 2016 16
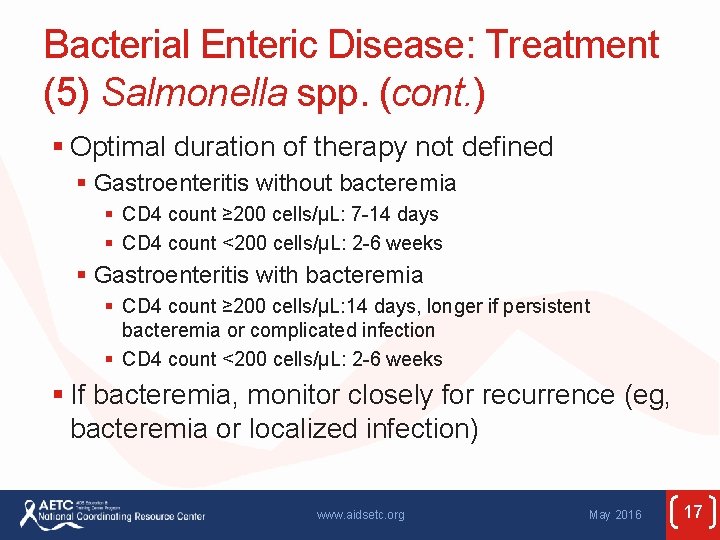
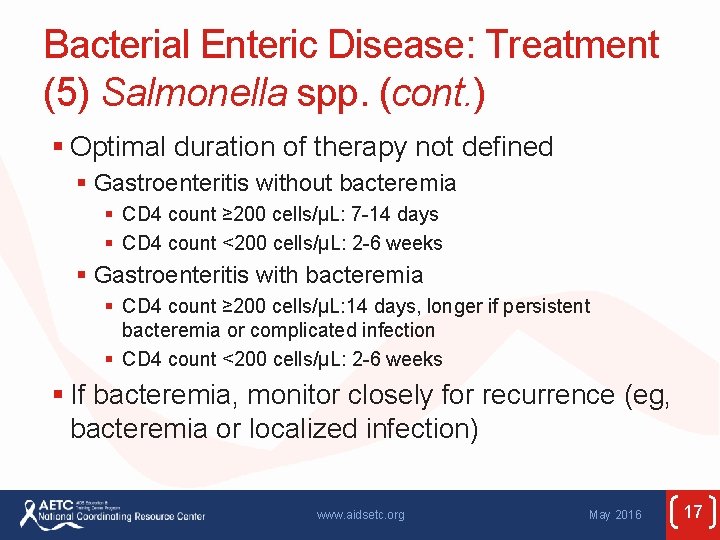
Bacterial Enteric Disease: Treatment (5) Salmonella spp. (cont. ) § Optimal duration of therapy not defined § Gastroenteritis without bacteremia § CD 4 count ≥ 200 cells/µL: 7 -14 days § CD 4 count <200 cells/µL: 2 -6 weeks § Gastroenteritis with bacteremia § CD 4 count ≥ 200 cells/µL: 14 days, longer if persistent bacteremia or complicated infection § CD 4 count <200 cells/µL: 2 -6 weeks § If bacteremia, monitor closely for recurrence (eg, bacteremia or localized infection) www. aidsetc. org May 2016 17
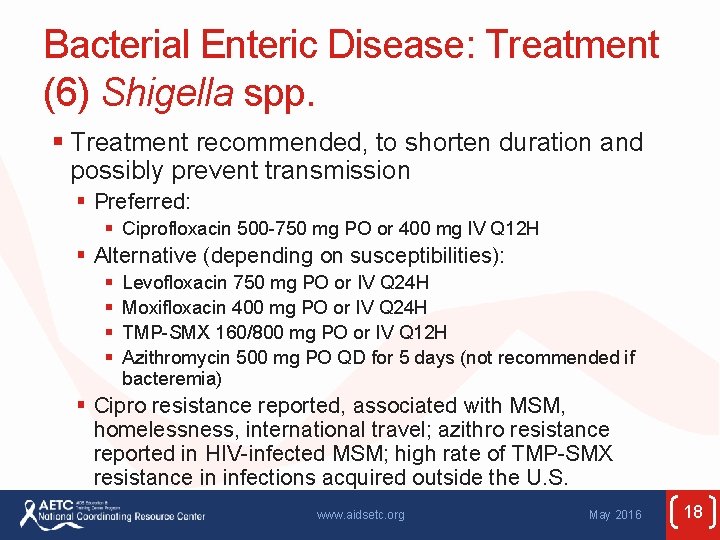
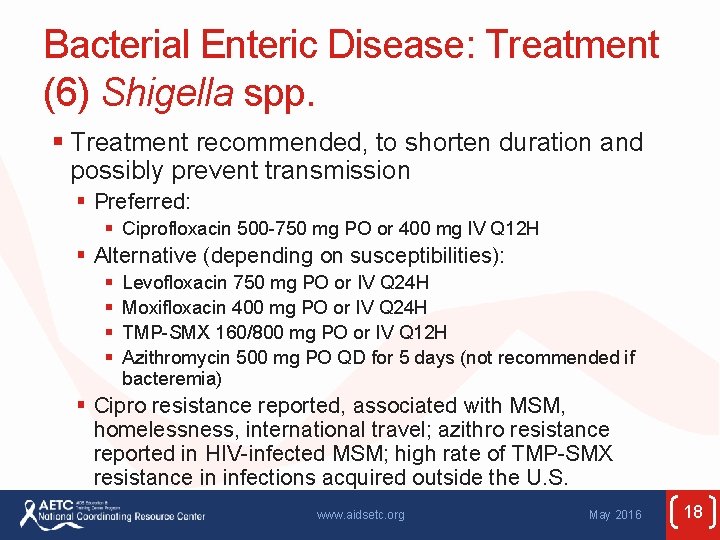
Bacterial Enteric Disease: Treatment (6) Shigella spp. § Treatment recommended, to shorten duration and possibly prevent transmission § Preferred: § Ciprofloxacin 500 -750 mg PO or 400 mg IV Q 12 H § Alternative (depending on susceptibilities): § § Levofloxacin 750 mg PO or IV Q 24 H Moxifloxacin 400 mg PO or IV Q 24 H TMP-SMX 160/800 mg PO or IV Q 12 H Azithromycin 500 mg PO QD for 5 days (not recommended if bacteremia) § Cipro resistance reported, associated with MSM, homelessness, international travel; azithro resistance reported in HIV-infected MSM; high rate of TMP-SMX resistance in infections acquired outside the U. S. www. aidsetc. org May 2016 18
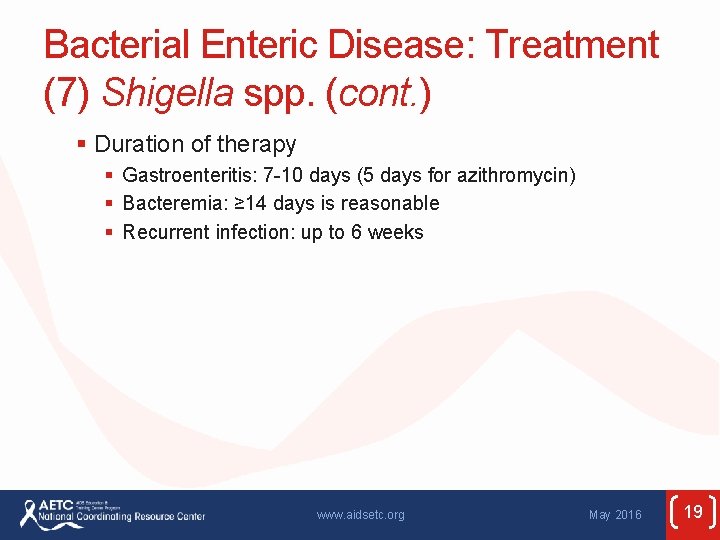
Bacterial Enteric Disease: Treatment (7) Shigella spp. (cont. ) § Duration of therapy § Gastroenteritis: 7 -10 days (5 days for azithromycin) § Bacteremia: ≥ 14 days is reasonable § Recurrent infection: up to 6 weeks www. aidsetc. org May 2016 19
Bacterial Enteric Disease: Treatment (8) Campylobacter spp. § Optimal treatment in HIV poorly defined § Culture and susceptibility recommended § Rates of resistance to FQs and azithromycin differ by Campylobacter species www. aidsetc. org May 2016 20
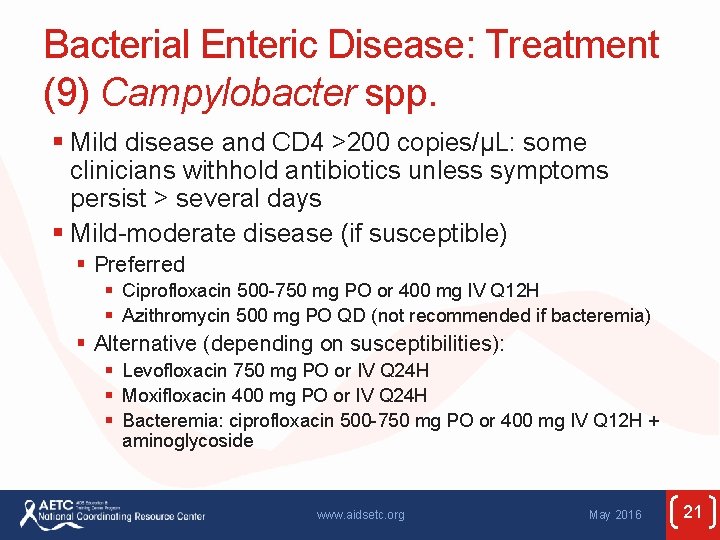
Bacterial Enteric Disease: Treatment (9) Campylobacter spp. § Mild disease and CD 4 >200 copies/µL: some clinicians withhold antibiotics unless symptoms persist > several days § Mild-moderate disease (if susceptible) § Preferred § Ciprofloxacin 500 -750 mg PO or 400 mg IV Q 12 H § Azithromycin 500 mg PO QD (not recommended if bacteremia) § Alternative (depending on susceptibilities): § Levofloxacin 750 mg PO or IV Q 24 H § Moxifloxacin 400 mg PO or IV Q 24 H § Bacteremia: ciprofloxacin 500 -750 mg PO or 400 mg IV Q 12 H + aminoglycoside www. aidsetc. org May 2016 21
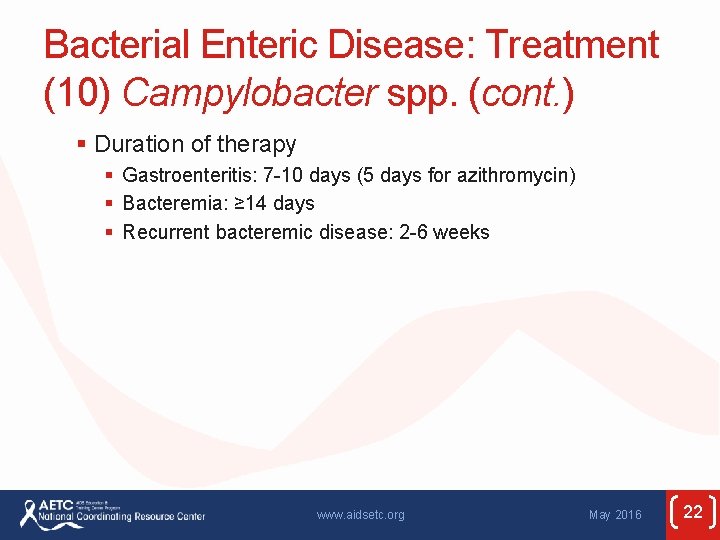
Bacterial Enteric Disease: Treatment (10) Campylobacter spp. (cont. ) § Duration of therapy § Gastroenteritis: 7 -10 days (5 days for azithromycin) § Bacteremia: ≥ 14 days § Recurrent bacteremic disease: 2 -6 weeks www. aidsetc. org May 2016 22
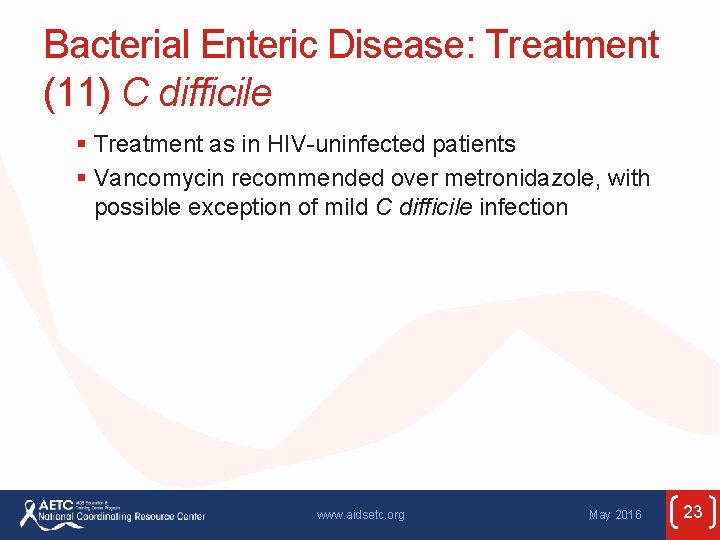
Bacterial Enteric Disease: Treatment (11) C difficile § Treatment as in HIV-uninfected patients § Vancomycin recommended over metronidazole, with possible exception of mild C difficile infection www. aidsetc. org May 2016 23
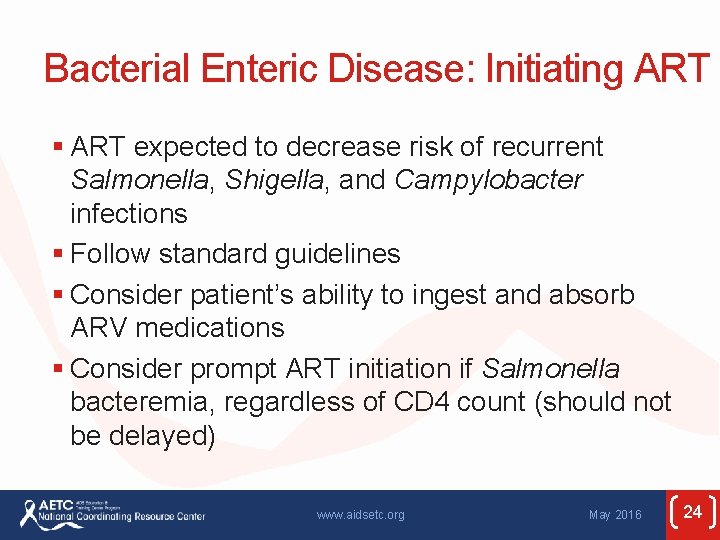
Bacterial Enteric Disease: Initiating ART § ART expected to decrease risk of recurrent Salmonella, Shigella, and Campylobacter infections § Follow standard guidelines § Consider patient’s ability to ingest and absorb ARV medications § Consider prompt ART initiation if Salmonella bacteremia, regardless of CD 4 count (should not be delayed) www. aidsetc. org May 2016 24
Bacterial Enteric Disease: Monitoring and Adverse Effects § Monitor closely for treatment response § Follow-up stool culture not required if clinical symptoms and diarrhea resolve § May be required if public health considerations and state law dictate § IRIS has not been described www. aidsetc. org May 2016 25
Bacterial Enteric Disease: Treatment Failure § Consider follow-up stool culture if lack of response to appropriate antibiotic therapy § Look for other enteric pathogens including C difficile; antibiotic resistance § Consider malabsorption of antibiotics: § Avoid coadministration of FQs with Mg- or Al-containing antacids, or with calcium, zinc, or iron (they interfere with FQ absorption § Use IV antibiotics if patient is clinically unstable www. aidsetc. org May 2016 26
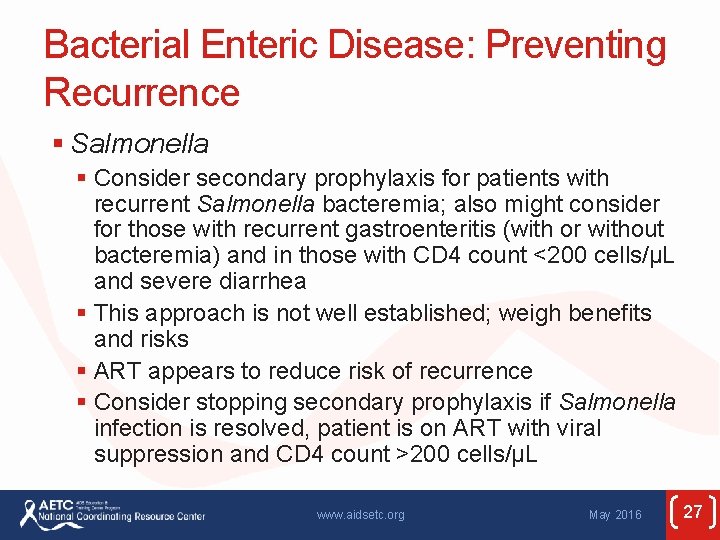
Bacterial Enteric Disease: Preventing Recurrence § Salmonella § Consider secondary prophylaxis for patients with recurrent Salmonella bacteremia; also might consider for those with recurrent gastroenteritis (with or without bacteremia) and in those with CD 4 count <200 cells/µL and severe diarrhea § This approach is not well established; weigh benefits and risks § ART appears to reduce risk of recurrence § Consider stopping secondary prophylaxis if Salmonella infection is resolved, patient is on ART with viral suppression and CD 4 count >200 cells/µL www. aidsetc. org May 2016 27
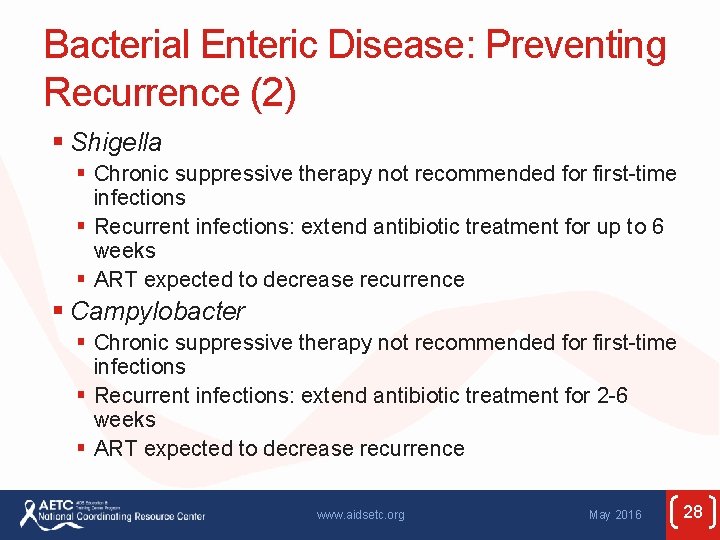
Bacterial Enteric Disease: Preventing Recurrence (2) § Shigella § Chronic suppressive therapy not recommended for first-time infections § Recurrent infections: extend antibiotic treatment for up to 6 weeks § ART expected to decrease recurrence § Campylobacter § Chronic suppressive therapy not recommended for first-time infections § Recurrent infections: extend antibiotic treatment for 2 -6 weeks § ART expected to decrease recurrence www. aidsetc. org May 2016 28
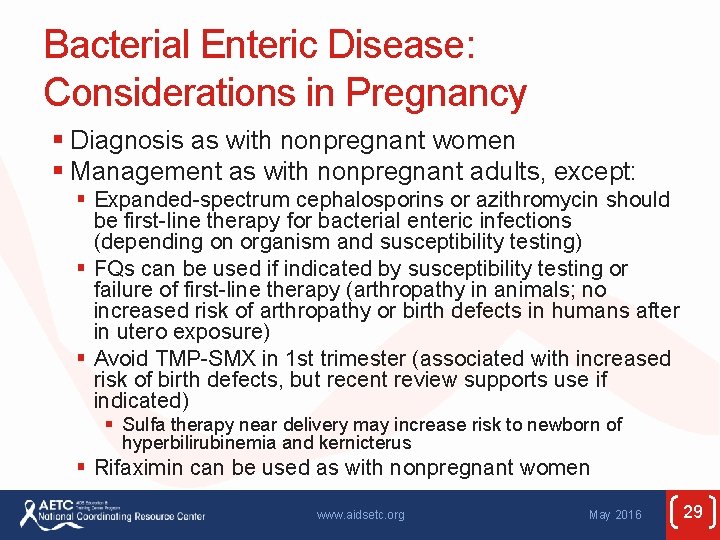
Bacterial Enteric Disease: Considerations in Pregnancy § Diagnosis as with nonpregnant women § Management as with nonpregnant adults, except: § Expanded-spectrum cephalosporins or azithromycin should be first-line therapy for bacterial enteric infections (depending on organism and susceptibility testing) § FQs can be used if indicated by susceptibility testing or failure of first-line therapy (arthropathy in animals; no increased risk of arthropathy or birth defects in humans after in utero exposure) § Avoid TMP-SMX in 1 st trimester (associated with increased risk of birth defects, but recent review supports use if indicated) § Sulfa therapy near delivery may increase risk to newborn of hyperbilirubinemia and kernicterus § Rifaximin can be used as with nonpregnant women www. aidsetc. org May 2016 29
Websites to Access the Guidelines § http: //www. aidsetc. org § http: //aidsinfo. nih. gov www. aidsetc. org May 2016 30
About This Slide Set § This presentation was prepared by Susa Coffey, MD, for the AETC National Resource Center in June 2013 and updated in May 2016 § See the AETC NRC website for the most current version of this presentation: http: //www. aidsetc. org May 2016 31
 Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Opportunistic approach adalah model proses untuk
Opportunistic approach adalah model proses untuk Focused opportunistic approach
Focused opportunistic approach Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Bone and joint infections
Bone and joint infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Transtubular potassium gradient
Transtubular potassium gradient Official disability guidelines texas
Official disability guidelines texas Sbp prophylaxis guidelines
Sbp prophylaxis guidelines Aria classification of allergic rhinitis
Aria classification of allergic rhinitis Allergy shiners
Allergy shiners Pressure management
Pressure management Diet hepatic encephalopathy
Diet hepatic encephalopathy Storch infections
Storch infections Storch infections
Storch infections Neurosiphyllis
Neurosiphyllis Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Amber blumling
Amber blumling Phagocytr
Phagocytr Classification of acute gingival infections
Classification of acute gingival infections Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering