Guidelines for Prevention and Treatment of Opportunistic Infections




- Slides: 26

Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents Herpes Simplex Virus Slide Set Prepared by the AETC National Coordinating Resource Center based on recommendations from the CDC, National Institutes of Health, and HIV Medicine Association/Infectious Diseases Society of America
About This Presentation These slides were developed using recommendations published in July 2013. The intended audience is clinicians involved in the care of patients with HIV. Certain sections have been updated to reflect changes in the published guidelines. Users are cautioned that, because of the rapidly changing field of HIV care, this information could become out of date quickly. Finally, it is intended that these slides be used as prepared, without changes in either content or attribution. Users are asked to honor this intent. – AETC National Coordinating Resource Center http: //www. aidsetc. org July 2013 2
Herpes Simplex Virus Disease § § § § Epidemiology Clinical Manifestations Diagnosis Preventing Disease Treatment Preventing Recurrence Considerations in Pregnancy www. aidsetc. org July 2013 3

Herpes Simplex Virus (HSV) Disease: Epidemiology § HSV-1: seroprevalence 60% among adults in the United States § HSV-2: seroprevalence 17% among persons aged ≥ 12 years in United States § 95% of HIV-infected persons are seropositive for either HSV-1 or HSV-2 § Most infections are not clinically evident § Reactivation occurs intermittently and can result in transmission www. aidsetc. org July 2013 4
HSV Disease: Epidemiology (2) § HSV-2 increases risk of HIV acquisition 2 - to 3 -fold § HSV-2 reactivation increases HIV RNA levels in blood and genital secretions of HIV-infected patients www. aidsetc. org July 2013 5
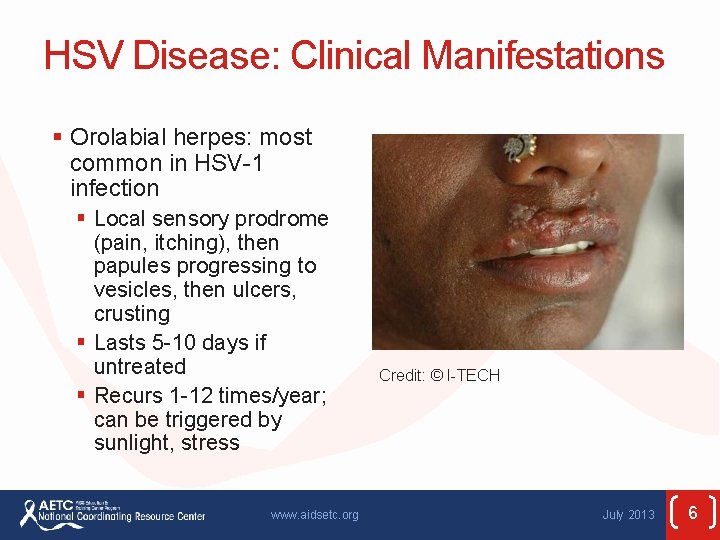
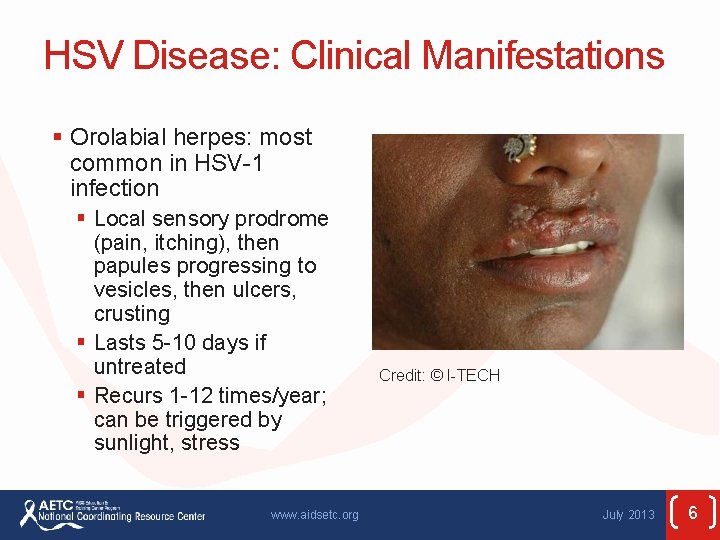
HSV Disease: Clinical Manifestations § Orolabial herpes: most common in HSV-1 infection § Local sensory prodrome (pain, itching), then papules progressing to vesicles, then ulcers, crusting § Lasts 5 -10 days if untreated § Recurs 1 -12 times/year; can be triggered by sunlight, stress www. aidsetc. org Credit: © I-TECH July 2013 6
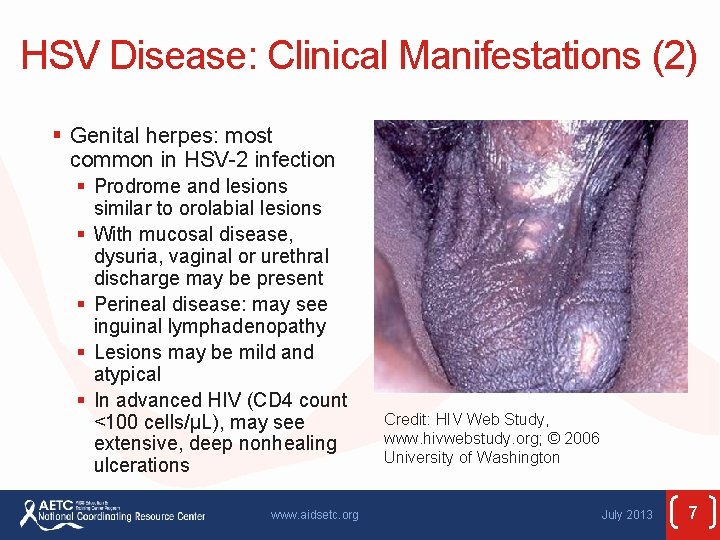
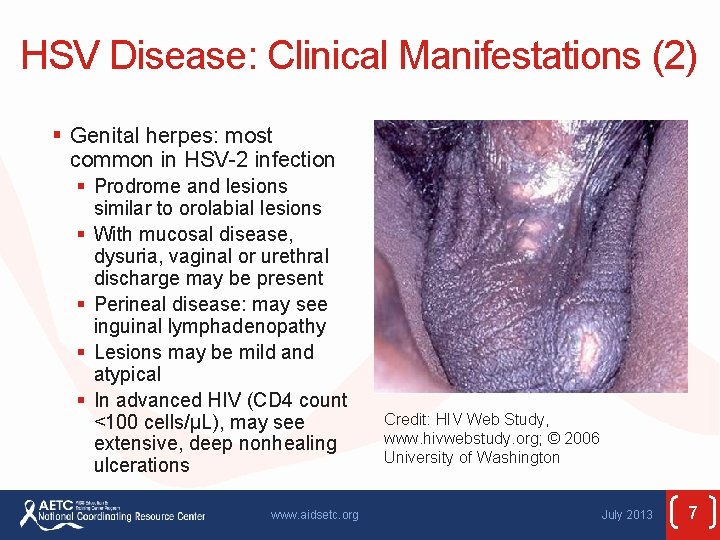
HSV Disease: Clinical Manifestations (2) § Genital herpes: most common in HSV-2 infection § Prodrome and lesions similar to orolabial lesions § With mucosal disease, dysuria, vaginal or urethral discharge may be present § Perineal disease: may see inguinal lymphadenopathy § Lesions may be mild and atypical § In advanced HIV (CD 4 count <100 cells/µL), may see extensive, deep nonhealing ulcerations www. aidsetc. org Credit: HIV Web Study, www. hivwebstudy. org; © 2006 University of Washington July 2013 7
HSV Disease: Clinical Manifestations (3) § Genital HSV-1 episodes indistinguishable from those of genital HSV-2 infection, but HSV-1 recurs less frequently www. aidsetc. org July 2013 8
HSV Disease: Clinical Manifestations (4) § Other manifestations: HSV keratitis, HSV encephalitis, HSV hepatitis, herpetic whitlow are similar in HIV infected and HIV uninfected § HSV retinitis: acute retinal necrosis; can rapidly cause vision loss § Disseminated HSV is rare www. aidsetc. org July 2013 9
HSV Disease: Diagnosis § Mucosal HSV cannot be diagnosed accurately by clinical exam, especially in HIV infection: laboratory diagnosis should be pursued § Swab base of fresh vesicle: § Viral culture § HSV DNA PCR (most sensitive; not widely available) § HSV antigen detection § If HSV detected, obtain type (genital HSV-1 recurs less frequently) www. aidsetc. org July 2013 10
HSV Disease: Diagnosis (2) § Type-specific serologic assays: can use in asymptomatic persons, or with atypical lesions § Consider routine serologic testing for HSV-2 in all HIVinfected patients § If infected with HSV-2: counsel about risk of transmission to sex partners, means of preventing transmission www. aidsetc. org July 2013 11
HSV Disease: Preventing Exposure § Most HIV-infected persons have HSV-1 and HSV-2 § If HSV-2 seronegative § Test partners for HSV-2 before initiating sexual activity § Latex barriers reduce HSV-2 acquisition (at least in heterosexual couples) § Avoid sexual contact with partners who have evident herpetic lesions § Sexual transmission of HSV-2 usually occurs during asymptomatic shedding § Antiviral therapy (valacyclovir) can reduce HSV-2 transmission (not studied in HIV infection) www. aidsetc. org July 2013 12
HSV Disease: Preventing Disease § Antiviral prophylaxis to prevent primary HSV is not recommended § Antiviral prophylaxis after exposure has not been studied www. aidsetc. org July 2013 13

HSV Disease: Treatment § Can treat episodically when lesions occur or with daily therapy to prevent recurrences; consider: § Frequency and severity of recurrences § Risk of HSV-2 transmission § Potential for adverse HSV-2 effect on HIV viral loads in plasma and genital secretions § Treatment of individual episodes does not reduce risk of HSV-2 transmission to sex partners www. aidsetc. org July 2013 14
HSV Disease: Treatment (2) § Orolabial HSV and genital HSV (initial or recurrent) § Valacyclovir 1 g PO BID, famciclovir 500 mg PO BID, or acyclovir 400 mg PO TID § Duration: 5 -10 days (orolabial); 5 -14 days (genital) § Severe mucocutaneous HSV § Acyclovir 5 mg/kg IV Q 8 H until lesions begin to regress, then PO therapy as above, until lesions have completely healed www. aidsetc. org July 2013 15
HSV Disease: Starting ART § Orolabial HSV usually should not influence decision about when to start ART § Prompt initiation of ART: chronic cutaneous or mucosal HSV refractory to treatment, visceral or disseminated HSV § ART with immune reconstitution may improve frequency and severity of genital HSV episodes § ART does not reduce frequency of genital HSV shedding www. aidsetc. org July 2013 16
HSV Disease: Monitoring and Adverse Events § No laboratory monitoring needed unless advanced renal impairment § Monitor renal function for patients on high-dose or prolonged therapy with IV acyclovir § High-dose (8 grams/day) valacyclovir may cause thrombotic thrombocytopenic purpura/hemolytic uremic syndrome; not reported at dosages used for HSV treatment § Atypical lesions reported in persons initiating ART www. aidsetc. org July 2013 17

HSV Disease: Treatment Failure § Lesions should begin to resolve within 7 -10 days of therapy initiation § Suspect drug resistance if no improvement § Culture lesion, perform susceptibility testing www. aidsetc. org July 2013 18
HSV Disease: Treatment Failure (2) § Acyclovir-resistant HSV § Preferred: § Foscarnet 80 -120 mg/kg/day IV in 2 -3 divided doses until clinical response § Alternatives (21 -28 days or longer): § Topical trifluridine, topical cidofovir, or topical imiquimod for external lesions § IV cidofovir www. aidsetc. org July 2013 19
HSV Disease: Preventing Recurrence § Suppressive therapy recommended for patients with frequent or severe recurrences; consider for all with HSV-2 § Valacyclovir 500 mg PO BID § Famciclovir 500 mg PO BID § Acyclovir 400 mg PO BID § Daily HSV suppressive therapy causes decrease in HIV RNA in plasma and anal and genital secretions, and lower risk of HIV progression § Suppressive HSV therapy does not decrease risk of HIV transmission § Suppressive therapy is continued indefinitely, regardless of CD 4 cell count improvement www. aidsetc. org July 2013 20
HSV Disease: Considerations in Pregnancy § Diagnosis of mucocutaneous HSV as in nonpregnant adults § Visceral disease more likely during pregnancy § May be transmitted to fetus or neonate § Risk of neonatal HSV greatest if mother has primary HSV infection during late pregnancy § In utero transmission rare, but severe cutaneous, ocular, and CNS damage § Most neonatal infection occurs via exposure to maternal genital fluids during birth www. aidsetc. org July 2013 21
HSV Disease: Considerations in Pregnancy (2) § Cesarean delivery lowers risk of transmission; recommended for women with prodrome or visible HSV genital lesions at onset of labor § Acyclovir or valacyclovir during late pregnancy suppresses genital HSV outbreaks and shedding in HIVuninfected women; reduces need for cesarean delivery; likely to have similar efficacy in HIV-infected women § Efficacy in reducing incidence of neonatal herpes is unknown www. aidsetc. org July 2013 22
HSV Disease: Considerations in Pregnancy (3) § Treatment § Acyclovir: most experience in pregnancy § Valacyclovir, famciclovir: appear to be safe and well tolerated during pregnancy § Suppressive therapy: § Valacyclovir or acyclovir recommended starting at 36 weeks, for pregnant women with recurrences of genital HSV during pregnancy www. aidsetc. org July 2013 23
HSV Disease: Considerations in Pregnancy (4) § Maternal genital HSV increases risk of perinatal HIV transmission in women not on ART; unknown effect for women on ART § Whether HSV suppression reduces risk of HIV transmission during pregnancy, birth, or breast-feeding is unknown www. aidsetc. org July 2013 24
Websites to Access the Guidelines § http: //www. aidsetc. org § http: //aidsinfo. nih. gov www. aidsetc. org July 2013 25
About This Slide Set § This presentation was prepared by Susa Coffey, MD, for the AETC National Resource Center in July 2013. § See the AETC NRC website for the most current version of this presentation: http: //www. aidsetc. org July 2013 26
 Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Opportunistic approach adalah model proses untuk
Opportunistic approach adalah model proses untuk Designing language curriculum
Designing language curriculum A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Methotrexate yeast infection
Methotrexate yeast infection Leuckocytosis
Leuckocytosis Odg-twc guidelines
Odg-twc guidelines Sbp paracentesis
Sbp paracentesis Allergy shiners
Allergy shiners Allergy shiners
Allergy shiners Ich treatment guidelines
Ich treatment guidelines Rifaximin in liver failure
Rifaximin in liver failure Storch infections
Storch infections Storch infections
Storch infections Cryptosporidiose
Cryptosporidiose Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Genital infections
Genital infections Nosocomial infections
Nosocomial infections Acute gingival infections
Acute gingival infections Formuö
Formuö