ACUTE KIDNEY INJURY CHRONIC KIDNEY DISEASE IN CHILDREN





- Slides: 72

ACUTE KIDNEY INJURY & CHRONIC KIDNEY DISEASE IN CHILDREN Salma Ajarmeh, MD Pediatric Nephrologist ﺭﺍﺋﺪ ﻋﻠﻲ : ﺗﺒﻴﻴﺾ ﺍﻟﻄﺎﻟﺐ
• The term AKI has largely replaced acute renal failure (ARF). • Pediatric AKI presents with a wide range of clinical manifestations from a minimal elevation in serum creatinine to anuric renal failure • Arises from multiple causes and occurs in a variety of clinical settings
AKI • Definition • Overview of the causes of AKI • Clinical presentation of AKI • Diagnosis of AKI in children • Complications of AKI • The management of AKI in children
Acute kidney injury (AKI) Acute = Base line is normal or not known to have chronic kidney problems -Defined as the abrupt loss of kidney function that results in a decline in glomerular filtration rate (GFR). -Retention of urea and other nitrogenous waste products and manifested by an elevated serum creatinine -Dysregulation of extracellular volume and electrolytes. (edema , dysregulated bp , ph , electrolytes) Acute kidney injury : abrubt decline in GFR , result in elevated serum creatinine and retention of urea and other nitrogenous wast product , manifisted by (edema , dysregulated bp , ph , electrolytes elevated serum creatinine is indicate renal failure in all cases Not other indicators are not present in all pt , or may ass. With other condition s
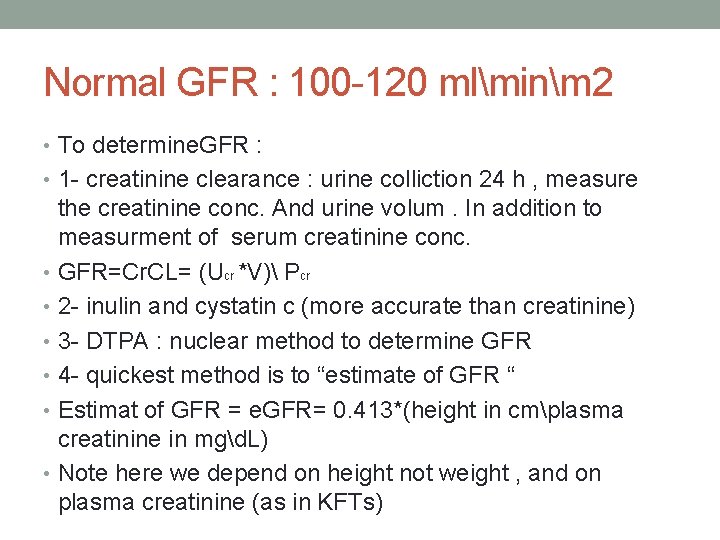
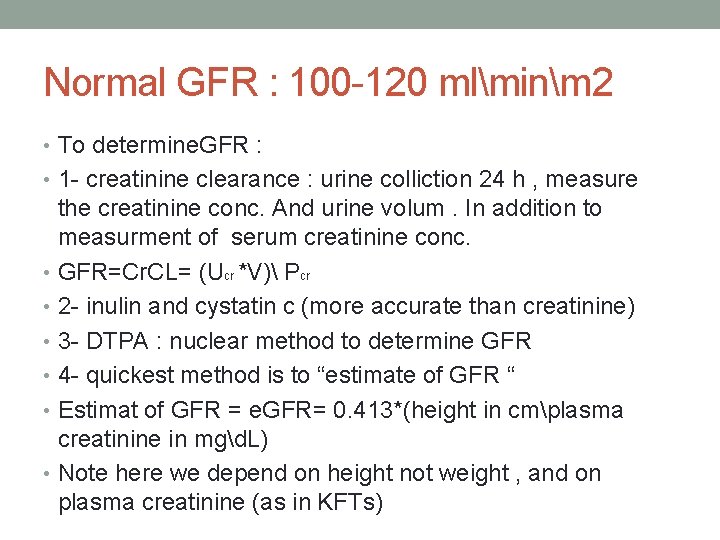
Normal GFR : 100 -120 mlminm 2 • To determine. GFR : • 1 - creatinine clearance : urine colliction 24 h , measure the creatinine conc. And urine volum. In addition to measurment of serum creatinine conc. • GFR=Cr. CL= (Ucr *V) Pcr • 2 - inulin and cystatin c (more accurate than creatinine) • 3 - DTPA : nuclear method to determine GFR • 4 - quickest method is to “estimate of GFR “ • Estimat of GFR = e. GFR= 0. 413*(height in cmplasma creatinine in mgd. L) • Note here we depend on height not weight , and on plasma creatinine (as in KFTs)
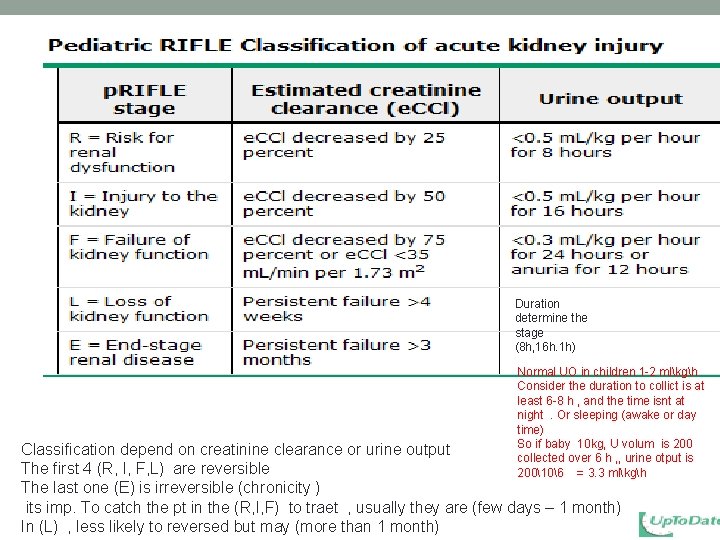
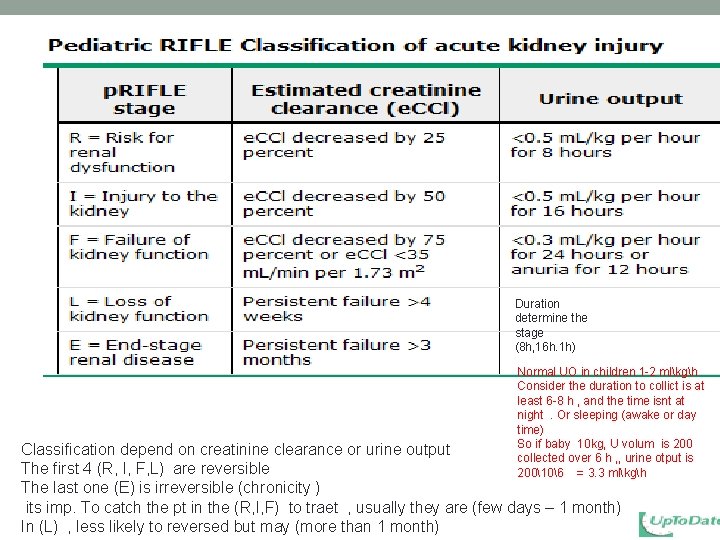
Duration determine the stage (8 h, 16 h. 1 h) Normal UO in children 1 -2 mlkgh Consider the duration to collict is at least 6 -8 h , and the time isnt at night. Or sleeping (awake or day time) So if baby 10 kg, U volum is 200 collected over 6 h , , urine otput is 200106 = 3. 3 mlkgh Classification depend on creatinine clearance or urine output The first 4 (R, I, F, L) are reversible The last one (E) is irreversible (chronicity ) its imp. To catch the pt in the (R, I, F) to traet , usually they are (few days – 1 month) In (L) , less likely to reversed but may (more than 1 month)
EPIDEMIOLOGY The underlying etiology of pediatric AKI varies globally! • In developed countries • In Developing countries The most common cause of acute kidney injury in pediatrics is HUS (it’s a renal cause : GN)
EPIDEMIOLOGY • AKI present in more than 30 % of all preterm infants and 50 % of neonates with asphyxia • In children undergoing cardiac surgery for congenital heart diseases, incidence of AKI 30 to 40 % • In children with BMT, the incidence of AKI from 15 to 35 % • In children admitted to (PICU), the incidence of AKI is about 5 -10% • in some PICU study that only included children receiving mechanical ventilation and vasopressors, the incidence of AKI jumped to 82 %
CLASSIFICATIONS Prerenal disease – volume-responsive AKI: • caused by reduced renal perfusion. • It is the most common form of pediatric AKI due to: • True volume depletion bleeding (eg, surgery or trauma) intestinal loss (eg, gastroenteritis) excessive cutaneous loss (eg, burns) ﺍﺣﻔﻆ ﺍﻟﻬﺴﺘﻮﺭﻱ ﺍﻧﻪ ﻣﻤﻜﻦ ﻭﺍﺣﺪ ﻣﺮﺍﺟﻌﺔ ﻭﺍﺳﻬﺎﻝ ﺯ ﺍﻭ ﻣﺤﺮﻭﻕ ﺍﻭ ﺷﻮﻛﺪ
CLASSIFICATIONS Prerenal disease • reduction of effective circulatory volume: as result of decreased arterial pressure (due to decreased cardiac output as in heart failure) or decreased effective arterial blood volume (decreased intravascular volume despite normal or increased total body water [septic shock or cirrhosis]) Drugs : NSAID causes vasoconstriction so decrease renal perfusion In this AKI, although glomerular filtration rate (GFR) is reduced, renal tubular function remains intact with reabsorption of sodium and water in response to renal hypoperfusion, leading to oliguria. When normal renal perfusion is restored, urine flow and GFR usually return to normal.
CLASSIFICATIONS Intrinsic renal disease Intrinsic AKI is characterized by structural damage to the renal parenchyma. The most common causes are: • prolonged hypoperfusion(ATN/cortical necrosis) • Sepsis • Tubular (ATN) usualy due to pre renal cause so considered as pre and renal cause) • Vascular disease (Vasculitis) • Glomerular disease ( PSGN, HUS, HSP. . ) • Acute interstitial nephritis(TIN) (due to drugs , infection , (there are cause ) , eiosinophila in urine (high WBC), blood , diagnosed by biopsy • myoglobinuria due to rhabdomyolysis (trauma) • Tumer lyses syndrome (leuckemia after chemotherapy >> by uric acids in tubules • nephrotoxins
CLASSIFICATIONS Postrenal disease • obstructive AKI is typically the result of congenital or acquired anatomic obstructions to the lower urinary tract. Posterior urethral valve in new born male Then Neurogenic bladder. . .
Postrenal disease • Postrenal AKI Stones Strictures/stenosis Clots N Bladder Congenital anomalies(PUV)
renal compensatory mechanisms • There are several renal compensatory mechanisms that attempt to maintain GFR in patients with decreased renal perfusion
renal compensatory mechanisms • The most effective of these renal compensatory systems involves the increased intrarenal generation of vasodilatory prostaglandins. • Non-steroidal anti-inflammatory drugs, inhibit this response and precipitate AKI, especially when used in the setting of renal hypoperfusion. Ibuprofen and Indomethacin
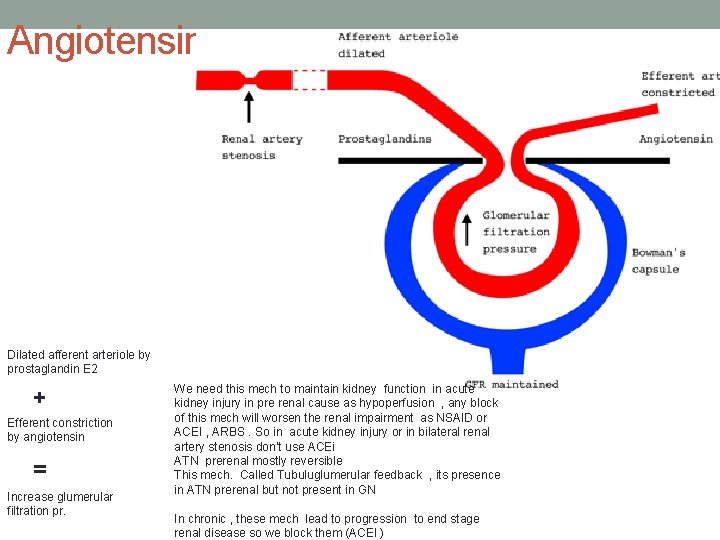
renal compensatory mechanisms • A second mechanism involves angiotensin II, which constricts the efferent arteriole leading to increased hydrostatic pressure across the glomerulus and maintenance of GFR. • The administration of angiotensin-converting enzyme (ACE) inhibitor therapy blocks this compensatory mechanism!
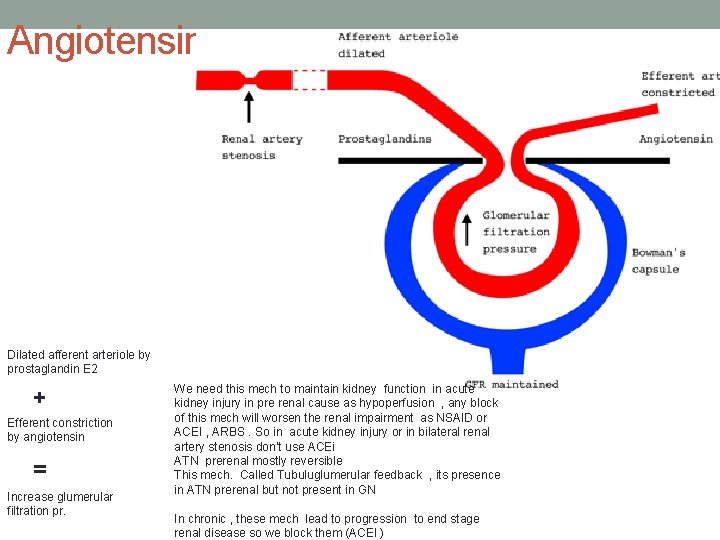
Angiotensin Dilated afferent arteriole by prostaglandin E 2 + Efferent constriction by angiotensin = Increase glumerular filtration pr. We need this mech to maintain kidney function in acute kidney injury in pre renal cause as hypoperfusion , any block of this mech will worsen the renal impairment as NSAID or ACEI , ARBS. So in acute kidney injury or in bilateral renal artery stenosis don’t use ACEi ATN prerenal mostly reversible This mech. Called Tubuluglumerular feedback , its presence in ATN prerenal but not present in GN In chronic , these mech lead to progression to end stage renal disease so we block them (ACEI )
Diagnosis The diagnosis is made clinically, based on the characteristic signs and symptoms, and laboratory findings indicative of an acute change in renal function. Pt 4 y creatinin 2. 5 , how to approach : 1 - etiology: #its acute if the pt not known to have choric renal disease #Most common cause is HUS and dehydration # : pre renal : vomiting , diarrhea , burn , , , #renal : GN : what type of GN , ask about heamaturia and HTN #post renal : known to have n. bladder , CNS problem , mass 2 - severtity or how sick is the pt (complication as fluid overload , HTN , electrolytes embalance ) so if edematous (severity , ask about SOB , sign of HF , ) sign of ecephalitis (due to HTN or ureamia)
CLINICAL PRESENTATION History • Edema(due to progressive fluid accumulation) • urine output : decreased or no urine output, • gross and microscopic hematuria, • hypertension. • a known etiologic factor that predisposes the child to AKI, such as shock or heart failure, • preceding streptococcal infection: post streptococcal glomerulonephritis. (history of pharyngitis or impetigo) • Known GN or CKD
History • vomiting, diarrhea, or decreased oral intake • history of bloody diarrhea • nephrotoxic medications • Prolonged hypotension/sepsis/shock ( in hospitalized patients) • systemic complaints (vasculitis) fever, joint complaints, arthritis and rash
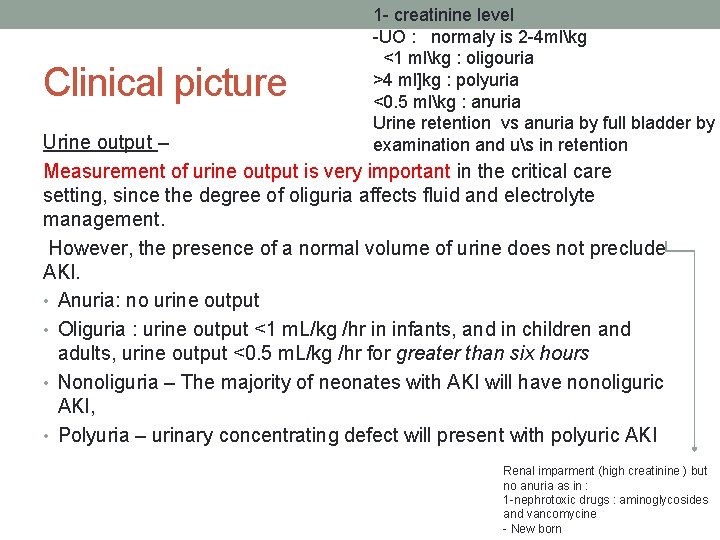
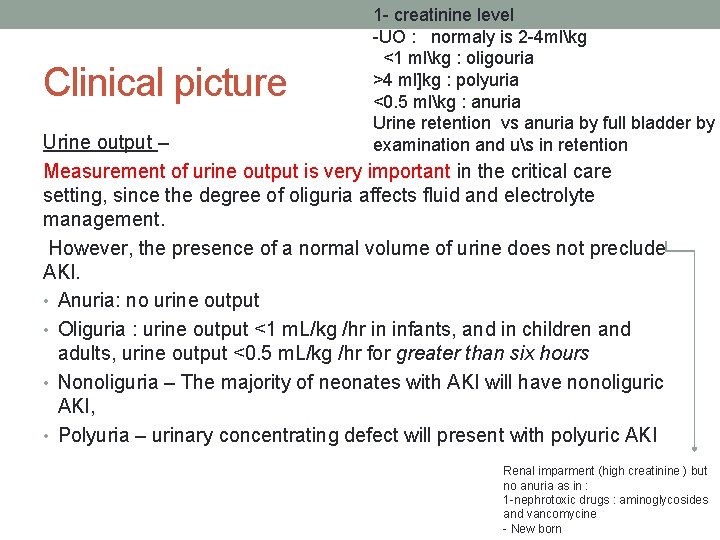
Clinical picture 1 - creatinine level -UO : normaly is 2 -4 mlkg <1 mlkg : oligouria >4 ml]kg : polyuria <0. 5 mlkg : anuria Urine retention vs anuria by full bladder by examination and us in retention Urine output – Measurement of urine output is very important in the critical care setting, since the degree of oliguria affects fluid and electrolyte management. However, the presence of a normal volume of urine does not preclude AKI. • Anuria: no urine output • Oliguria : urine output <1 m. L/kg /hr in infants, and in children and adults, urine output <0. 5 m. L/kg /hr for greater than six hours • Nonoliguria – The majority of neonates with AKI will have nonoliguric AKI, • Polyuria – urinary concentrating defect will present with polyuric AKI Renal imparment (high creatinine ) but no anuria as in : 1 -nephrotoxic drugs : aminoglycosides and vancomycine - New born
Physical examination • Volume status : depleted and dry vs Overloaded (edema) • BP (hypertension) • Cardiac exam • Chest exam • Abdominal mass ( palpable kidney) • Skin rash Physical exam doesn’t help you in specific etiology , the same manifestation (edema, HTN , ph , electrolytes)
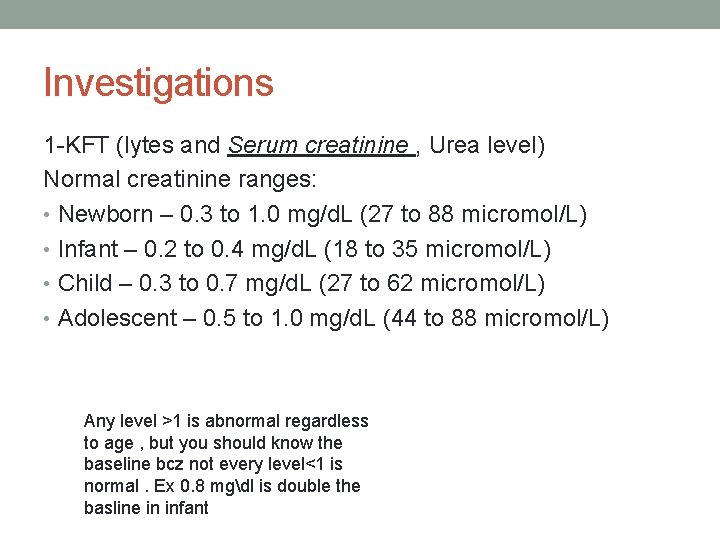
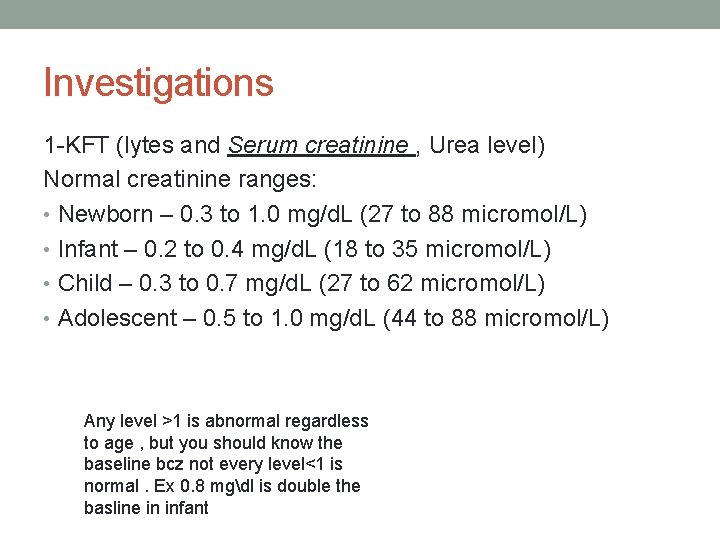
Investigations 1 -KFT (lytes and Serum creatinine , Urea level) Normal creatinine ranges: • Newborn – 0. 3 to 1. 0 mg/d. L (27 to 88 micromol/L) • Infant – 0. 2 to 0. 4 mg/d. L (18 to 35 micromol/L) • Child – 0. 3 to 0. 7 mg/d. L (27 to 62 micromol/L) • Adolescent – 0. 5 to 1. 0 mg/d. L (44 to 88 micromol/L) Any level >1 is abnormal regardless to age , but you should know the baseline bcz not every level<1 is normal. Ex 0. 8 mgdl is double the basline in infant
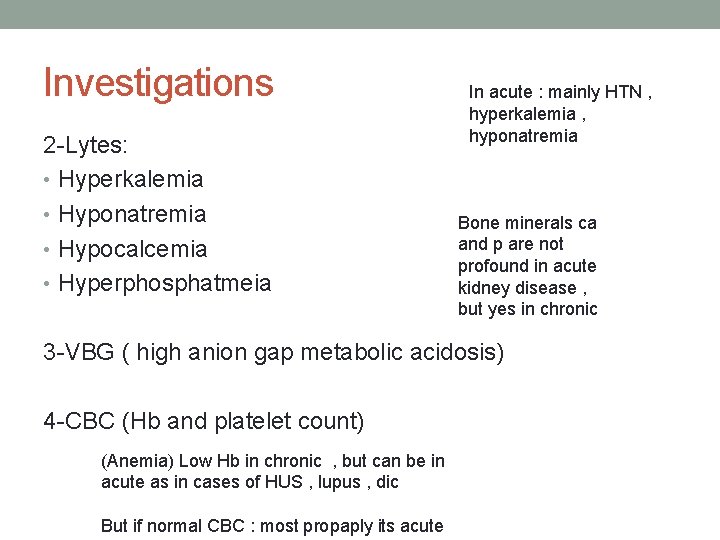
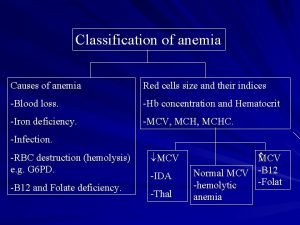
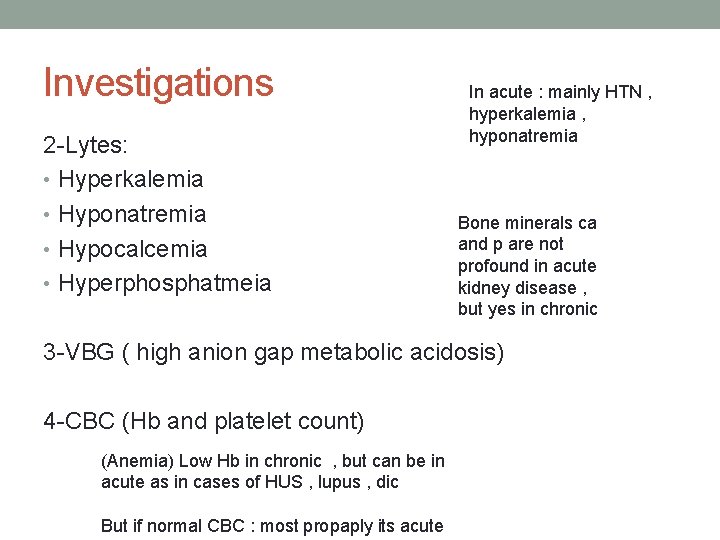
Investigations 2 -Lytes: • Hyperkalemia • Hyponatremia • Hypocalcemia • Hyperphosphatmeia In acute : mainly HTN , hyperkalemia , hyponatremia Bone minerals ca and p are not profound in acute kidney disease , but yes in chronic 3 -VBG ( high anion gap metabolic acidosis) 4 -CBC (Hb and platelet count) (Anemia) Low Hb in chronic , but can be in acute as in cases of HUS , lupus , dic But if normal CBC : most propaply its acute
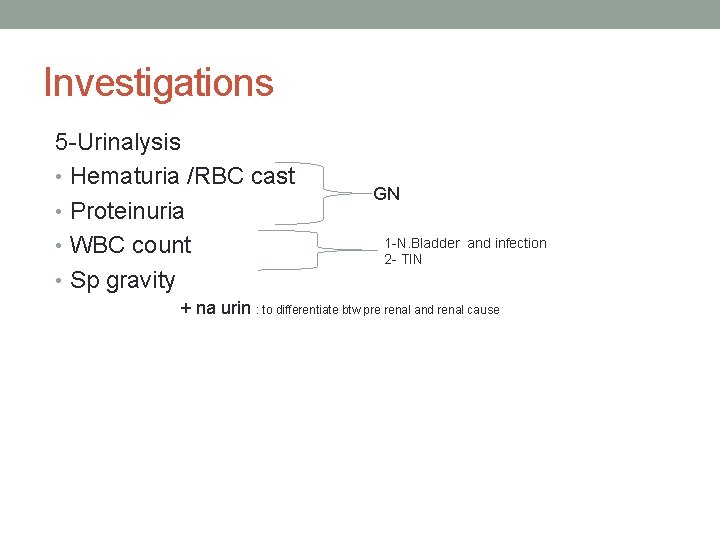
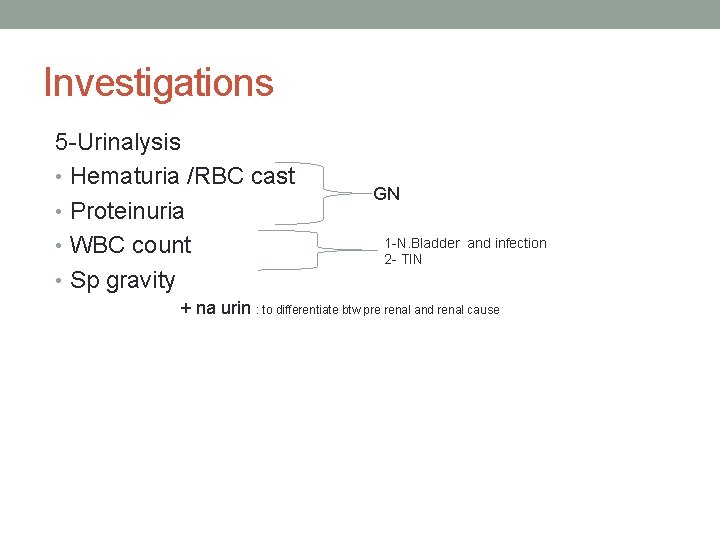
Investigations 5 -Urinalysis • Hematuria /RBC cast • Proteinuria • WBC count • Sp gravity GN 1 -N. Bladder and infection 2 - TIN + na urin : to differentiate btw pre renal and renal cause

Urine cast

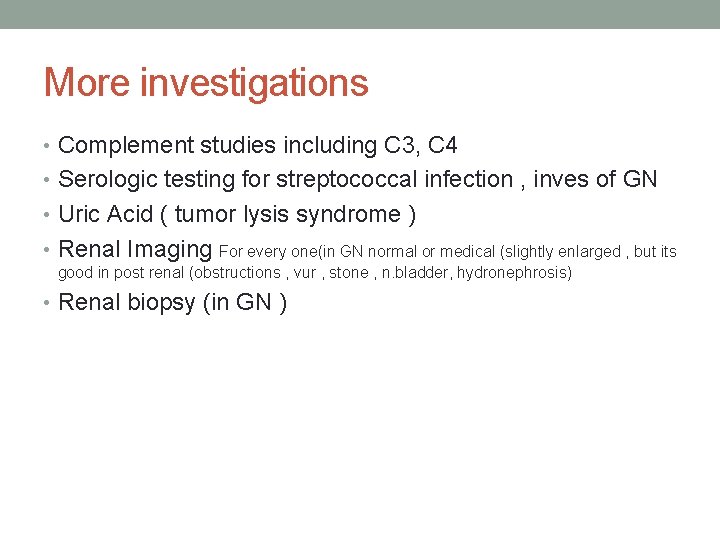
More investigations • Complement studies including C 3, C 4 • Serologic testing for streptococcal infection , inves of GN • Uric Acid ( tumor lysis syndrome ) • Renal Imaging For every one(in GN normal or medical (slightly enlarged , but its good in post renal (obstructions , vur , stone , n. bladder, hydronephrosis) • Renal biopsy (in GN )
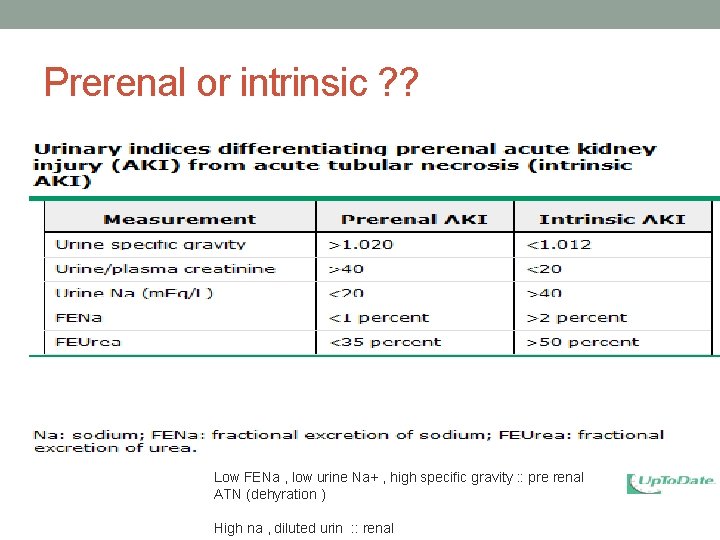
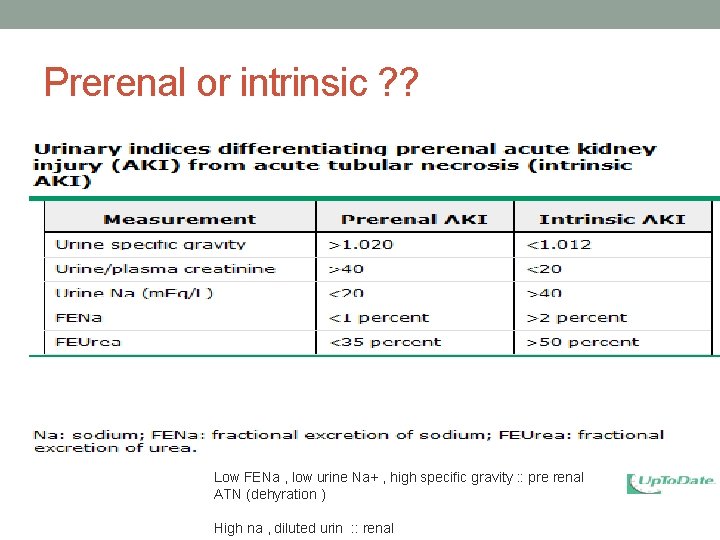
Prerenal or intrinsic ? ? Low FENa , low urine Na+ , high specific gravity : : pre renal ATN (dehyration ) High na , diluted urin : : renal
Novel biomarkers New AKI markers such as • neutrophil gelatinase-associated lipocalin (NGAL), • kidney injury molecule-1 (KIM-1), • interleukin-18 (IL-18) show promise in both their diagnostic and prognostic utility. May allow for early intervention
Management of AKI in Children The basic principles of the general management of the child with AKI include: • Specific treatment of the underlying cause • Fluid management • Electrolyte management • Treat acidosis (bicarb. ) • Nutritional support firsly the management is the same • Adjustment of drug dosing regardless to etiology : Aim : • Renal replacement therapy 1 - stabilize the pt Dialysis and transplantation 2 - figure out the etiology 3 - deal with lifethreatinig complication (fluid overload , HTN , electrolytes and acidosis)
Fluid Management
• 1 - estimate fluid status : • A- If every thing sugest the case is pre-renal (dehydration , sepsis , . . ) as sunken eyes , hypotensive , cold extremity, rapid puls , delayed perfusion or CV line indicative ) and presence Hx of fever , vomiting , diarrhea so : • Tx is fluid • 1 - start fluid therapy by emergency bollus (up to 3 time , assess after each bollus to detect any response by : • 1 -blood pr. Monitoring : increrase • 2 - pulse : down • 3 - urine output: increase • If improved , so the case is pre renal , then calculate as in fluid therapy seminar (maintainance , defect , …)
• B- if as previous scenario but not respond to fluid therapy (still no UO) or euvolemic and little pit edematous as(in GN case or in pre renal didn’t respond ) (pt isnt dehydrated) • Bp 1490 , tachypnic , tachycardia , no UO • 1 - challenge with loob diuritic , if improve ; there is hope in the kidney • 2 - calcuate insensible fluid (300 -400 m. L/m 2/day) ( no rule of mantainance here , maintanance as in fluid seminar is if there are normal kidney and urine output , if in case of renal failure , insensible fluid depending of surface area (bcz no loss by urine , the weight is not reflect the real (due to some fluid retention ) • (so the fluid therpy in those is insensible fluid not mantainance ) • Insensible fluid (400 mlm 2day ) + urine out put replacement • This mean if the pt pass urine you replace him the volume in addition to insensible fluid , if no urinoutput , just insensible
• C- indication of dialysis : • 1 -massive fluid overload pulmonary edema , HF, v. HTN • 2 - complete renal shut down • 3 - electrolyte disturbance • 4 - metabolic acidosis • 5 - ureamia
Fluid management • Accurate initial assessment is required to determine if the child is hypovolemic, euvolemic, or hypervolemic, and guides initial fluid management.
Hypovolemia: • If the physical exam and clinical history is consistent with dehydration and fluid loss : • give N/S 0. 9% bolus (10 to 20 m. L/kg over 30 minutes, can repeat x 3) • If still no UOP…. Bladder catheterization • At this point, other forms of invasive monitoring, such as measuring central venous pressure, may be required to adequately assess the fluid status and help guide furtherapy.
• In euvolemic • If presentation euvolemic , Or if after first resuscitation for hypovolemia the patient responds well with good UOP : • Can challenge with diuretic (Furesemide ) • Use insensible fluid (300 -400 m. L/m 2/day) plus urine and gastrointestinal losses replacement • Replace with ½ N/S every 6 hr over 6 h
Hypervolemia: signs of fluid overload (edema, heart failure and pulmonary edema) requires fluid removal and/or fluid restriction. • Furosemide trial and • Restrict fluids to insensible with replacement If no response or unstable. . . . Renal replacement therapy (RRT) should be considered for critically-ill children who are not expected to recover kidney function
Hyperkalemia LIFE threatining Hyperkalemia – Several factors may contribute to hyperkalemia in patients with AKI. • reduced GFR • decreased tubular secretion of potassium • tissue breakdown with release of intracellular potassium, • metabolic acidosis resulting in transcellular movement of potassium (each 0. 1 unit reduction in arterial p. H raises serum potassium by 0. 3 m. Eq/L). • Hyperkalemia is most pronounced in patients with significant tissue breakdown (rhabdomyolysis, hemolysis, and tumor lysis syndrome)
Hyperkalemia • Symptoms are non-specific and may include malaise, nausea, and muscle weakness. • Electrocardiogram (ECG) changes occur in patients with hyperkalemia > 7. 0 meq/L • These include (in sequence according to the severity of hyperkalemia) tall peaked T waves, prolonged PR interval, flattened P waves, widened QRS complex, ventricular tachycardia and fibrillation


Metabolic acidosis • Wide anion gap acidosis • Give Na bicarbonate Acidosis from renal failure require bicarbonate
Hyperphosphatmia and hypocalcemia • oral phosphate binders and dietary restriction of phosphorus are commonly used to decrease intestinal absorption of phosphorus. • Intravenous administration Calcium Gluconate should be considered only if hypocalcemia is severe!
Hypertension Several contributing factors may cause elevated blood pressure: • fluid overload • renin-mediated hypertension , especially in children with glomerulonephritis. - Initial management is typically administration of a diuretic. -Consider CCB , ACE and other agents
Drug management • Remove nephrotoxic agents • Adjust to the renal doses
Renal replacement therapy • Fluid overload that is unresponsive to diuretics a • Cannot provide adequate nutrition • Hyperkalemia unresponsive to medical therapy • BUN between 80 to 100 mg/d. L • life-threatening complications due to fluid overload such (pulmonary edema, heart failure, and hypertension ) • Severe metabolic acidosis not responding to therapy
Renal Replacement Therapy • HD • PD • CRRT
• HD: central vascular access, and the ability to tolerate a large extracorporeal blood volume is a problem for very small children. • PD: easy to perform and no requirement for specialized equipment, personnel, or systemic anti-coagulation. Peritoneal dialysis is frequently therapy of choice in neonates and small infants. • CRRT is especially useful in patients with hemodynamic instability and multi-organ dysfunction, since it allows continuous management of fluid overload without significant fluid shifts that may occur with HD.
Chronic Kidney Disease
Chronic Kidney Disease • Definition : the Kidney Disease Outcomes Quality Initiative (KDOQI) working group of the National Kidney Foundation (NKF) defined chronic kidney disease as "evidence of structural or functional kidney abnormalities (abnormal urinalysis, imaging studies, or histology) that persist for at least 3 months, with or without a decreased GFR. ” Not for children < 2 yr Every pt : High grade reflux , scarring , protien urea , GN , . . They are CKD
The major health consequences of chronic kidney disease include • progression to kidney failure & ESRD • increased risk of cardiovascular disease. • Growth and development retardation. Evidence-based clinical practice guidelines support early recognition and treatment of chronic kidney disease and its complications will improve growth and development and, ultimately, the quality of life in children.
Main causes of CKD in children include : • Obstructive uropathy • Renal hypoplasia and dysplasia • Reflux nephropathy • Childhood nephritis syndromes ( mainly FSGS) • AR and AD PKD
Pathophysiology of CKD once chronic kidney disease develops, (regardless of the etiology) the response of the failing kidney is similar. • The kidney initially adapts to damage by increasing the filtration rate in the remaining normal nephrons (adaptive hyperfiltration). So ; • patients with mild CKD often have near-normal serum creatinine. • this also keeps the serum sodium, potassium, calcium, and phosphorous and total body water to remain within the reference range, particularly among those with mild to moderate stages of CKD.
Pathophysiology of CKD Adaptive hyperfiltration is initially beneficial, but at the long run it will damage the remaining glomeruli: • Proteinuria • progressive kidney insufficiency. This irreversibility appears to be responsible for the development of end-stage kidney.
Progression to ESRD progression in CKD may be due to factors that are unrelated to the activity of the initial disease: • anemia, • systemic and intraglomerular hypertension, • proteinuria, • metabolic acidosis, • hyperlipidemia, • Tubulointerstetial disease,
Progression When (CKD) occurs, progression to (ESRD) appears certain. • The rate of progression depends on the primary diagnosis, and on successful early follow up and preventive measures. • About 70% of children with chronic kidney disease develop ESRD by age 20 years. • Children with ESRD have a 10 -year survival rate of about 80% • age-specific mortality rate of about 30 times that seen in children without ESRD. • The most common cause of death in these children is cardiovascular disease, followed by infection.
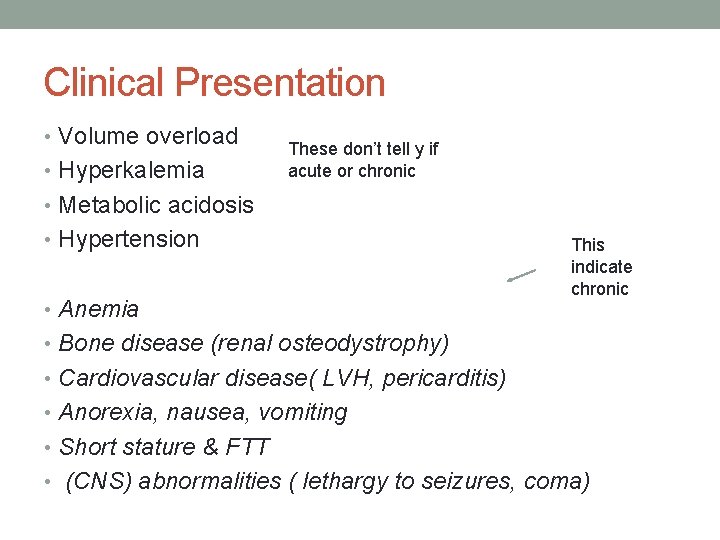
Clinical Presentation • Volume overload • Hyperkalemia These don’t tell y if acute or chronic • Metabolic acidosis • Hypertension • Anemia This indicate chronic • Bone disease (renal osteodystrophy) • Cardiovascular disease( LVH, pericarditis) • Anorexia, nausea, vomiting • Short stature & FTT • (CNS) abnormalities ( lethargy to seizures, coma)
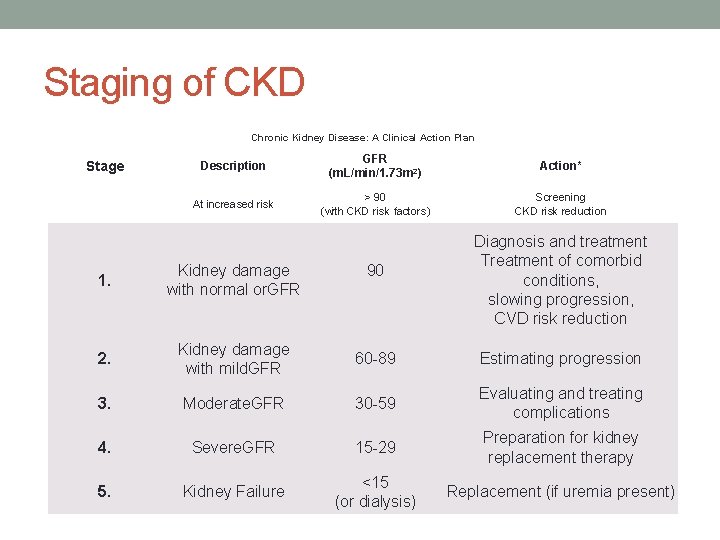
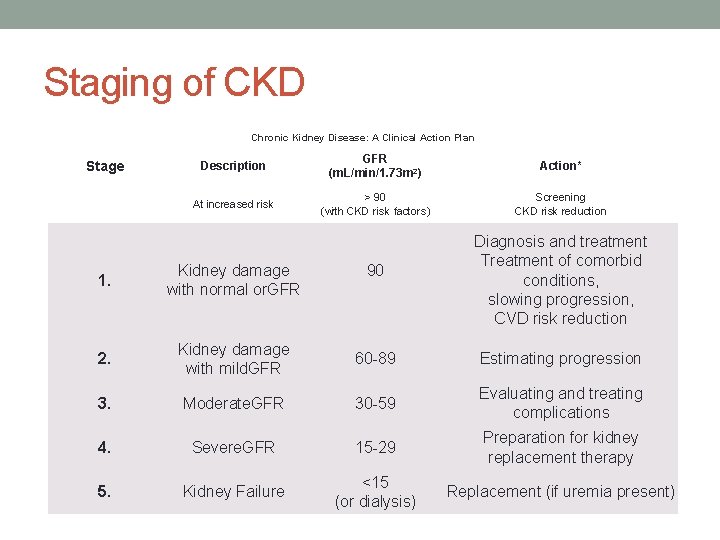
Staging of CKD Chronic Kidney Disease: A Clinical Action Plan Stage Description GFR (m. L/min/1. 73 m 2) Action* At increased risk > 90 (with CKD risk factors) Screening CKD risk reduction 90 Diagnosis and treatment Treatment of comorbid conditions, slowing progression, CVD risk reduction 1. Kidney damage with normal or. GFR 2. Kidney damage with mild. GFR 60 -89 Estimating progression 3. Moderate. GFR 30 -59 Evaluating and treating complications 4. Severe. GFR 15 -29 Preparation for kidney replacement therapy 5. Kidney Failure <15 (or dialysis) Replacement (if uremia present)
Complications of CKD
Anemia of CKD Anemia develops early in the course of CKD and is nearly universal in patients with CKD stage 4&5. • primary deficiency of erythropoietin production by the interstitial fibroblasts (type I interstitial cells) leading to anemia and it is directly related to the amount of residual renal function. The kidneys are responsible for approximately 90% of erythropoietin production in an individual. • Also other factors include ongoing blood loss, iron deficiency, and deficiencies of vitamin B 12 and/or folic acid.
Anemia Treatment : • Erythropoietin (EPO) replacement • Iron supplement • Maintain Hb level 11 -12 g dl
Renal Bone Mineral Metabolism IS a broad spectrum of disorders of mineral metabolism in CKD , terms such as “renal osteodystrophy” , “renal bone metabloic disease” and “CKD-mineral and bone disorder” be Replaced by Bone mineral metabolism TO define the mineral, bone, hormonal, and calcific cardiovascular abnormalities that are seen in CKD Manifested by : • (1) Abnormalities of calcium, phosphorus, parathyroid hormone (PTH), and vitamin D metabolism; • (2) abnormalities of bone turnover, mineralization, volume, linear growth, and strength; • (3) vascular or soft tissue calcification
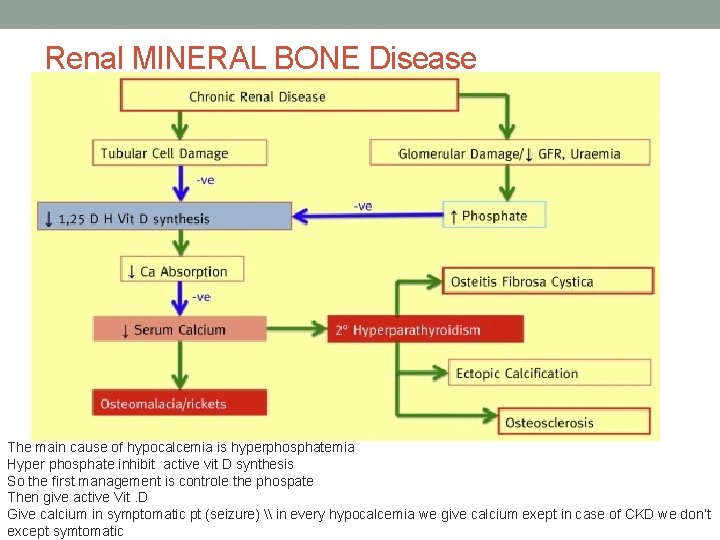
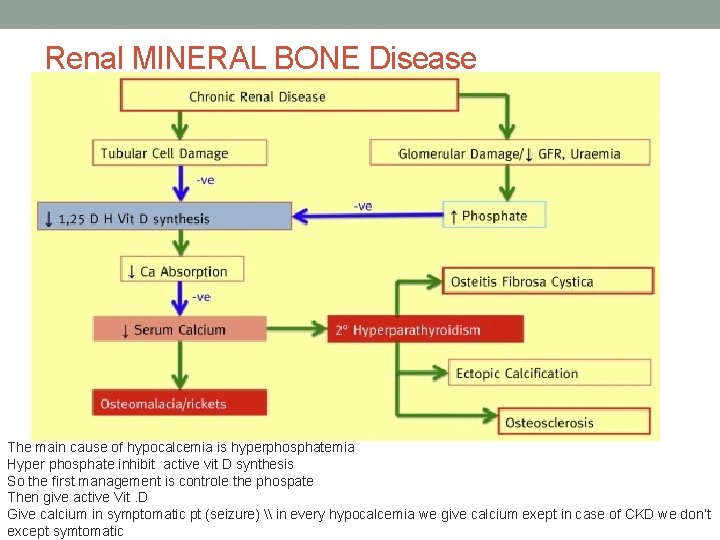
Renal MINERAL BONE Disease The main cause of hypocalcemia is hyperphosphatemia Hyper phosphate inhibit active vit D synthesis So the first management is controle the phospate Then give active Vit. D Give calcium in symptomatic pt (seizure) \ in every hypocalcemia we give calcium exept in case of CKD we don’t except symtomatic
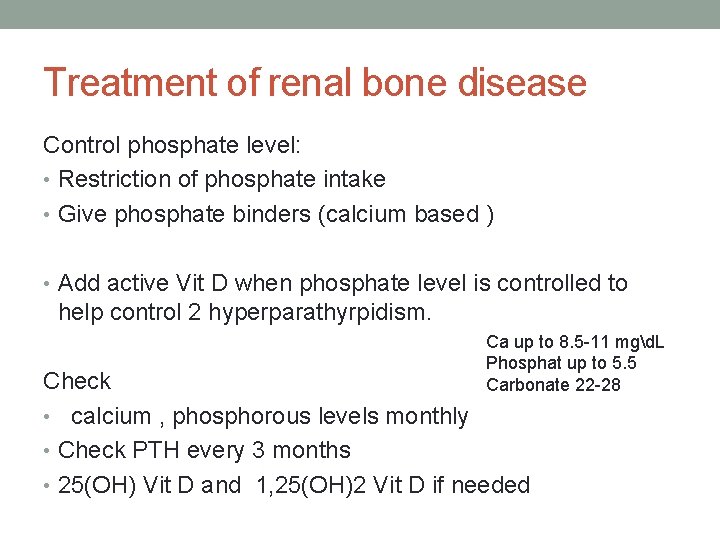
Treatment of renal bone disease Control phosphate level: • Restriction of phosphate intake • Give phosphate binders (calcium based ) • Add active Vit D when phosphate level is controlled to help control 2 hyperparathyrpidism. Ca up to 8. 5 -11 mgd. L Phosphat up to 5. 5 Carbonate 22 -28 Check • calcium , phosphorous levels monthly • Check PTH every 3 months • 25(OH) Vit D and 1, 25(OH)2 Vit D if needed
Hypertension • Hypertension is a highly significant and independent predictor for progression of chronic kidney disease (CKD) in children. • The optimal target blood pressure is recommended to be below the 90 th percentile for age. • Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) have benefit in patients slowing the rate of progressive renal injury, and controlling proteinuria
Metabolic Acidosis • In children, overt acidosis is characteristically present when the (e. GFR) is less than 30 m. L/min per 1. 73 m 2 (stage IV). • The acidosis in chronic kidney disease in children can be associated with an increased anion gap. • Treat by supplementing sodium bicarbonate to maintain HCO 3 range around 22 mmol L
Cardiovascular disease Left Ventricular Hypertrophy : • Both hypertension and anemia are associated with LVH in chronic renal disease. • Treatment of each condition causes regression of LVH in chronic renal disease.
Other issues with CKD in children • Growth retardation in CKD children - feeding issues -growth hormone supplement -dialysis for growth factors The only indication to give growth hormon in non endocrin disease is in CKD
Thank You
 Skt aki
Skt aki Nephrology near atwater
Nephrology near atwater Nih stroke scale
Nih stroke scale Chapter 18 common chronic and acute conditions
Chapter 18 common chronic and acute conditions Cyst granuloma abscess
Cyst granuloma abscess Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Morphological patterns of acute inflammation slideshare
Morphological patterns of acute inflammation slideshare Acute subacute chronic
Acute subacute chronic Acute vs chronic heart failure
Acute vs chronic heart failure Pigment gallstones causes
Pigment gallstones causes Leukemia death rate
Leukemia death rate Differences between acute and chronic inflammation
Differences between acute and chronic inflammation Battering intentional or unintentional
Battering intentional or unintentional Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Chronic disease
Chronic disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Developedbyed
Developedbyed Restrictive lung disease
Restrictive lung disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Chronic disease
Chronic disease Chronic granulomatous disease
Chronic granulomatous disease Chronic rheumatic heart disease
Chronic rheumatic heart disease Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Is cirrhosis treatable
Is cirrhosis treatable Jewish chronic disease hospital study
Jewish chronic disease hospital study An acute highly contagious viral disease
An acute highly contagious viral disease Nemo ckd
Nemo ckd Albumin kidney disease
Albumin kidney disease Sighns of kidney problems
Sighns of kidney problems Albumin kidney disease
Albumin kidney disease Natremia
Natremia Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Bharathi viswanathan
Bharathi viswanathan Chronic rejection
Chronic rejection Flinders model
Flinders model Endolaser dcr
Endolaser dcr Morphological patterns of acute inflammation
Morphological patterns of acute inflammation Chronic rejection
Chronic rejection Chronic inducible urticaria
Chronic inducible urticaria Indications of abg analysis
Indications of abg analysis Renal bruit auscultation
Renal bruit auscultation Perls stain
Perls stain Analglesia
Analglesia Chronic duodenitis with foveolar metaplasia
Chronic duodenitis with foveolar metaplasia Circulatory disturbances pathology
Circulatory disturbances pathology Wagner chronic care model 1998
Wagner chronic care model 1998 Chronic
Chronic Allergic conjunctivitis icd 9
Allergic conjunctivitis icd 9 Types of anemia
Types of anemia Hep b mode of transmission
Hep b mode of transmission Chronic pancreatitis
Chronic pancreatitis Treatment of cml
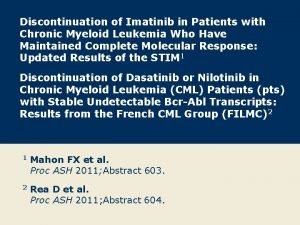
Treatment of cml Chronic rejection
Chronic rejection Chronic care
Chronic care Chronic frustration
Chronic frustration Diarea causes
Diarea causes Pulp stones
Pulp stones Iceberg phenomenon of disease
Iceberg phenomenon of disease Chronic care solutions
Chronic care solutions Chronic calculous cholecystitis
Chronic calculous cholecystitis Barrel chested man
Barrel chested man Chronic rejection
Chronic rejection Earthy look in chronic renal failure
Earthy look in chronic renal failure Patho
Patho Classification of antianginal drugs
Classification of antianginal drugs Lacrimal sac
Lacrimal sac Paul l marino
Paul l marino Chronic inducible urticaria
Chronic inducible urticaria Chronic sinusitis
Chronic sinusitis Chronic blood loss
Chronic blood loss Mild hepatic steatosis
Mild hepatic steatosis Chronic myeloid leukemia
Chronic myeloid leukemia