Chronic Kidney Disease PARTNERS IN HEALTH C HRONIC

- Slides: 36
Chronic Kidney Disease PARTNERS IN HEALTH C HRONIC C ARE TRAINING FOR D ISTRICT H OSPITAL NUR SE S IN RWANDA 2013
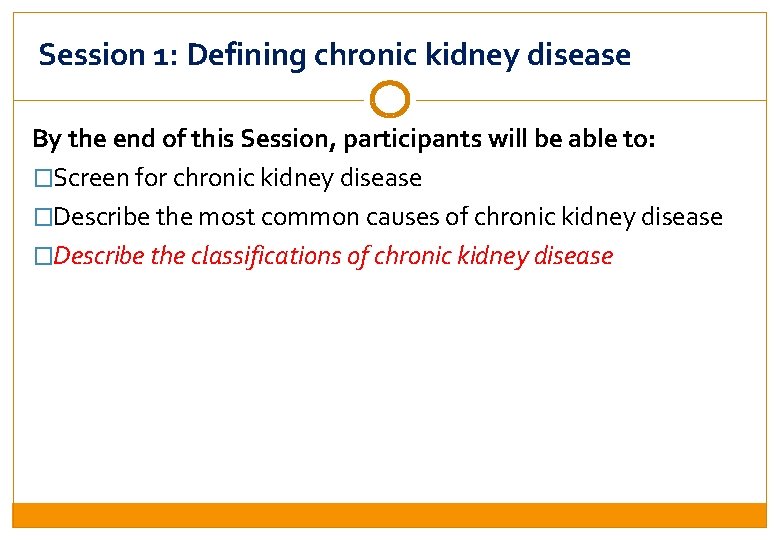
Session 1: Defining chronic kidney disease By the end of this Session, participants will be able to: �Screen for chronic kidney disease �Describe the most common causes of chronic kidney disease �Describe the classifications of chronic kidney disease

Session 1: Defining chronic kidney disease By the end of this Session, participants will be able to: �Screen for chronic kidney disease �Describe the most common causes of chronic kidney disease �Describe the classifications of chronic kidney disease
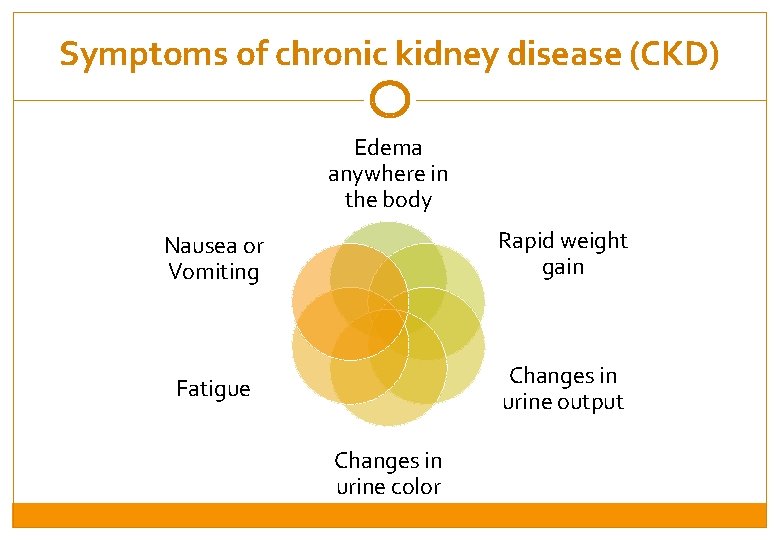
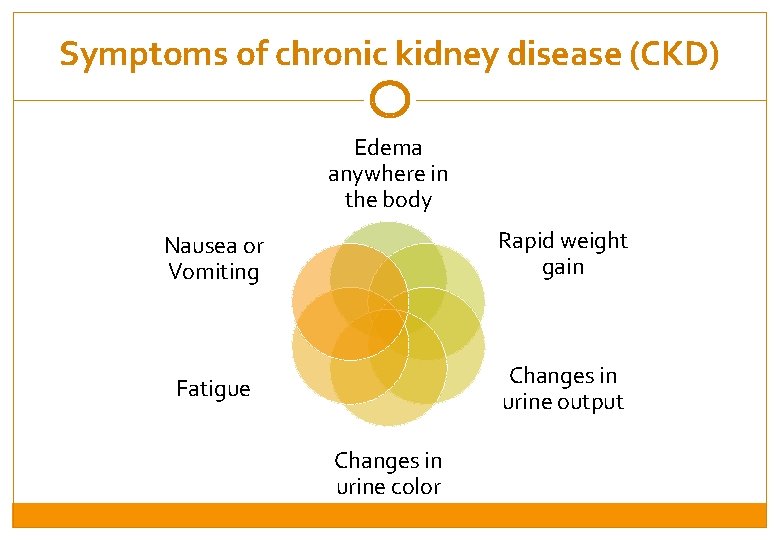
Symptoms of chronic kidney disease (CKD) Edema anywhere in the body Nausea or Vomiting Rapid weight gain Fatigue Changes in urine output Changes in urine color
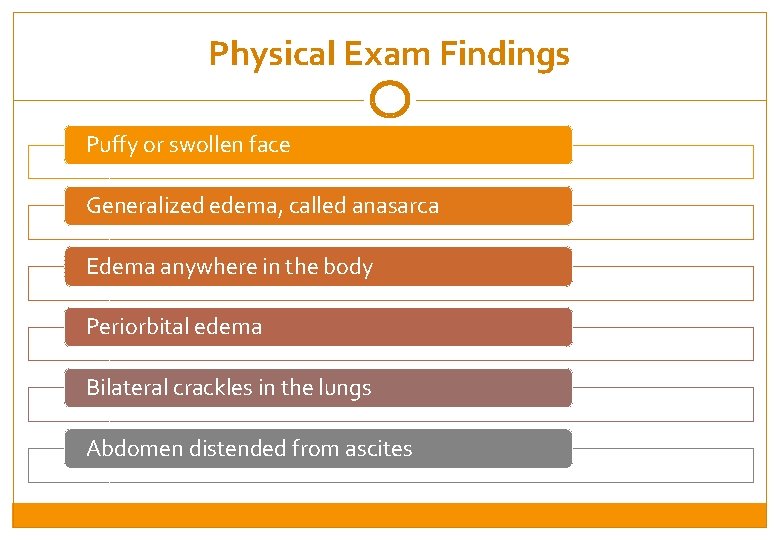
Physical Exam Findings Puffy or swollen face Generalized edema, called anasarca Edema anywhere in the body Periorbital edema Bilateral crackles in the lungs Abdomen distended from ascites
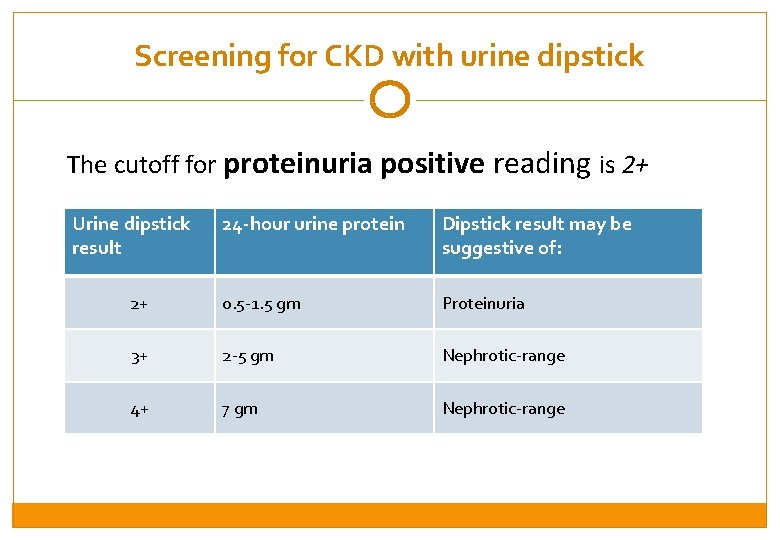
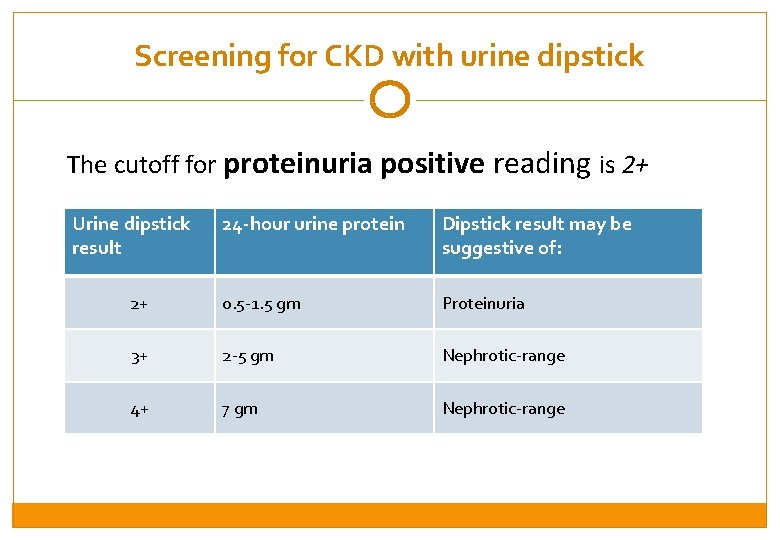
Screening for CKD with urine dipstick The cutoff for proteinuria positive reading is 2+ Urine dipstick result 24 -hour urine protein Dipstick result may be suggestive of: 2+ 0. 5 -1. 5 gm Proteinuria 3+ 2 -5 gm Nephrotic-range 4+ 7 gm Nephrotic-range
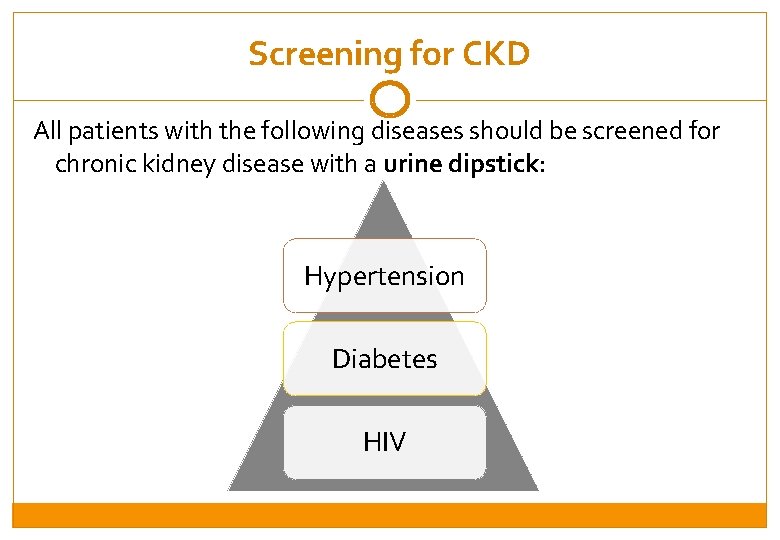
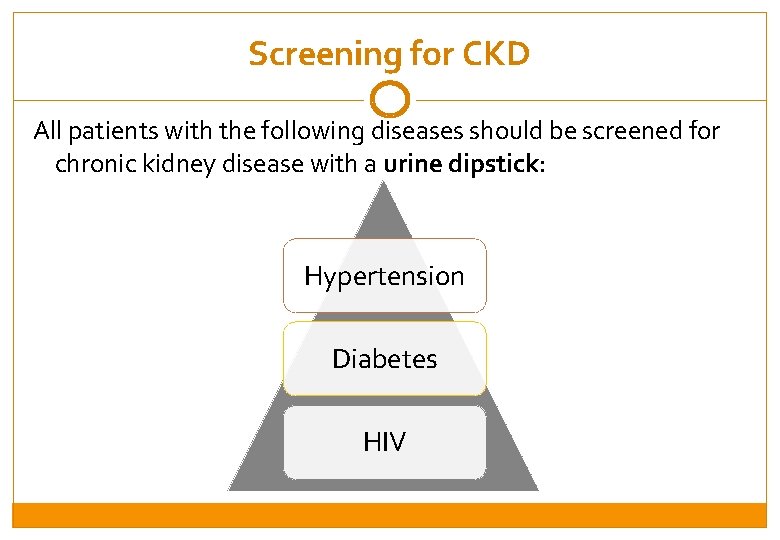
Screening for CKD All patients with the following diseases should be screened for chronic kidney disease with a urine dipstick: Hypertension Diabetes HIV
Session 1: Defining chronic kidney disease By the end of this Session, participants will be able to: �Screen for chronic kidney disease �Describe the most common causes of chronic kidney disease �Describe the classifications of chronic kidney disease
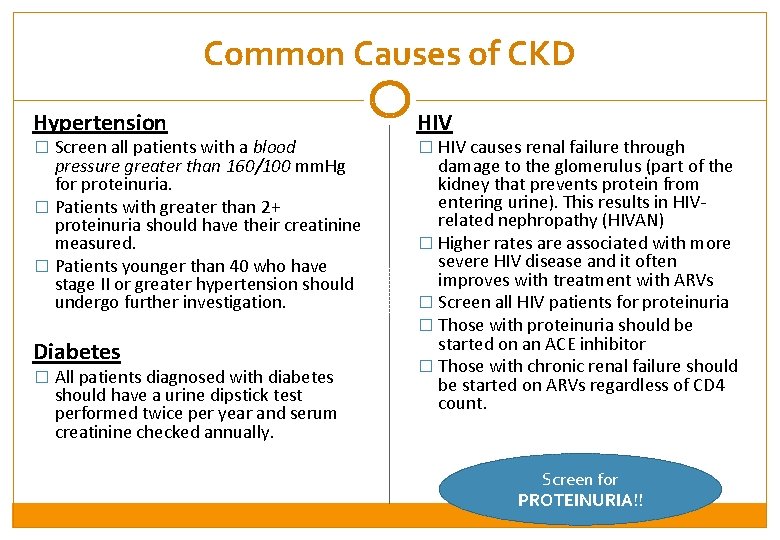
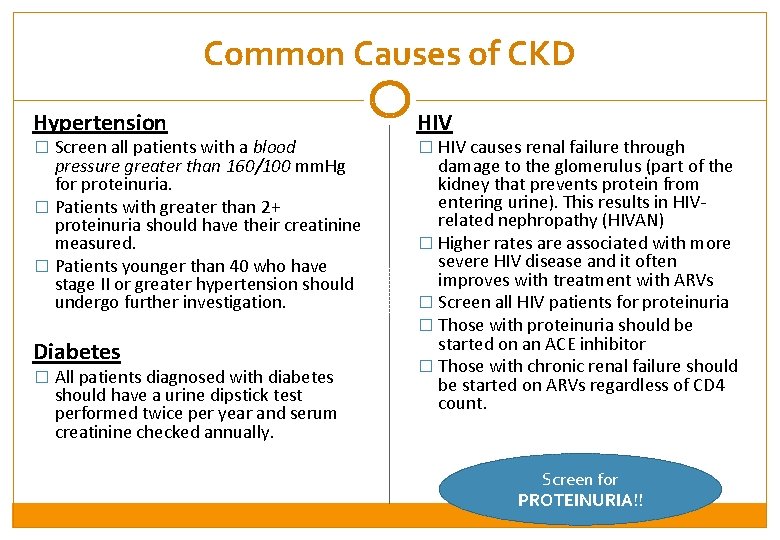
Common Causes of CKD Hypertension HIV pressure greater than 160/100 mm. Hg for proteinuria. � Patients with greater than 2+ proteinuria should have their creatinine measured. � Patients younger than 40 who have stage II or greater hypertension should undergo further investigation. damage to the glomerulus (part of the kidney that prevents protein from entering urine). This results in HIVrelated nephropathy (HIVAN) � Higher rates are associated with more severe HIV disease and it often improves with treatment with ARVs � Screen all HIV patients for proteinuria � Those with proteinuria should be started on an ACE inhibitor � Those with chronic renal failure should be started on ARVs regardless of CD 4 count. � Screen all patients with a blood Diabetes � All patients diagnosed with diabetes should have a urine dipstick test performed twice per year and serum creatinine checked annually. � HIV causes renal failure through Screen for PROTEINURIA!!
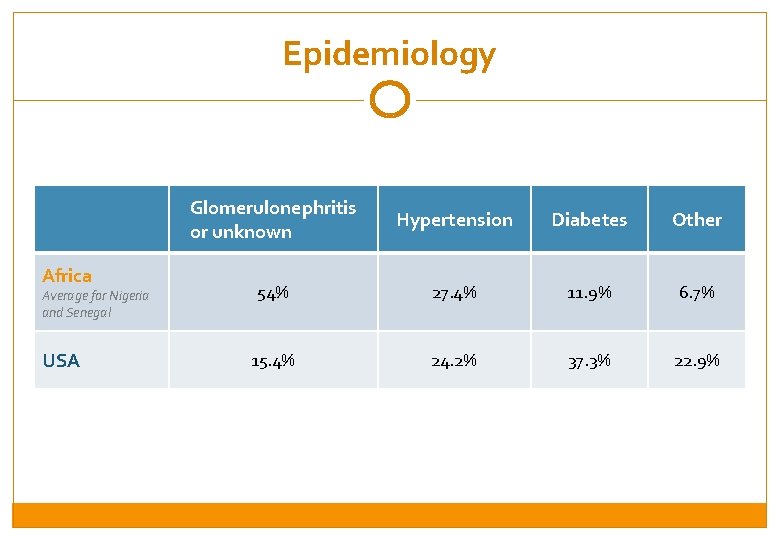
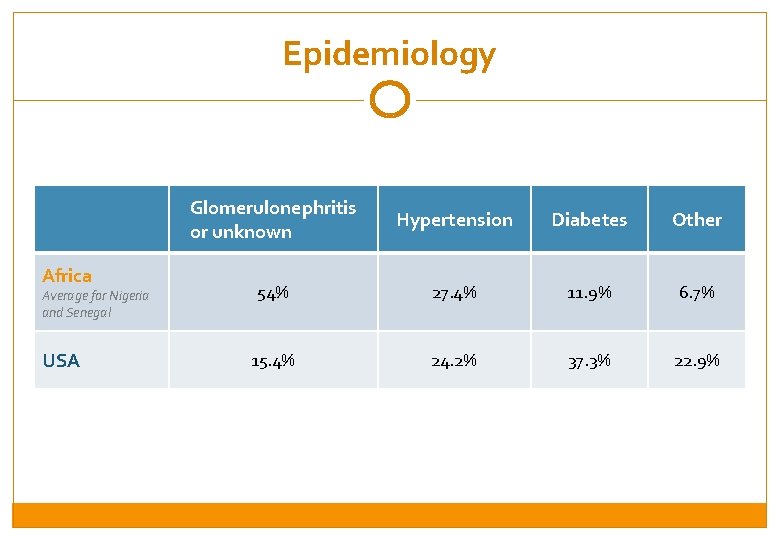
Epidemiology Africa Average for Nigeria and Senegal USA Glomerulonephritis or unknown Hypertension Diabetes Other 54% 27. 4% 11. 9% 6. 7% 15. 4% 24. 2% 37. 3% 22. 9%
Session 1: Defining chronic kidney disease By the end of this Session, participants will be able to: �Screen for chronic kidney disease �Describe the most common causes of chronic kidney disease �Describe the classifications of chronic kidney disease
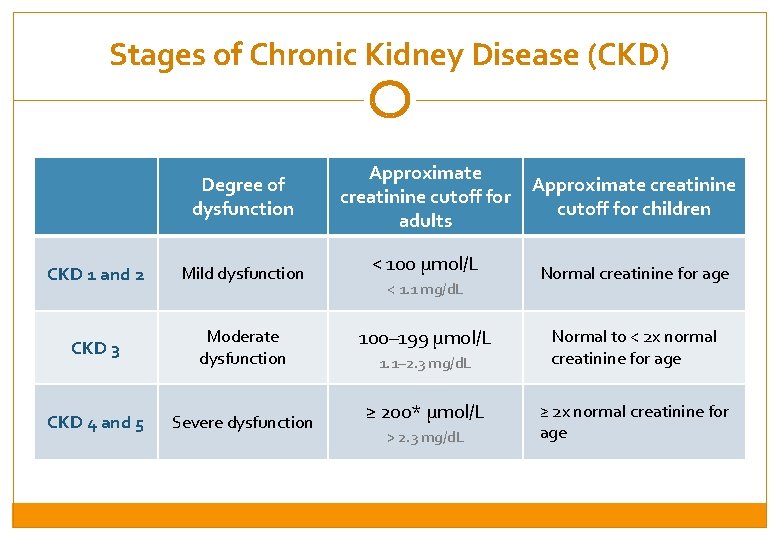
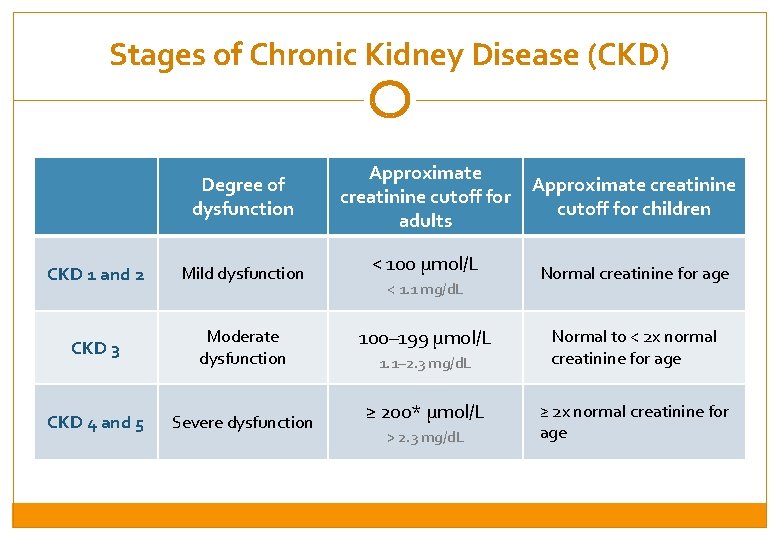
Stages of Chronic Kidney Disease (CKD) Degree of dysfunction CKD 1 and 2 Mild dysfunction CKD 3 Moderate dysfunction CKD 4 and 5 Severe dysfunction Approximate creatinine cutoff for adults < 100 µmol/L < 1. 1 mg/d. L 100– 199 µmol/L 1. 1– 2. 3 mg/d. L ≥ 200* µmol/L > 2. 3 mg/d. L Approximate creatinine cutoff for children Normal creatinine for age Normal to < 2 x normal creatinine for age ≥ 2 x normal creatinine for age
Session 2: Management of CKD in adults By the end of this Session, participants will be able to: �Describe the initial management of CKD 1 and 2 �Describe the initial and ongoing management of CKD 3, 4, and 5
Session 2: Management of CKD in adults By the end of this Session, participants will be able to: �Describe the initial management of CKD 1 and 2 �Describe the initial and ongoing management of CKD 3, 4, and 5
Overview of CKD Management �IF creatinine < 200 mmol/L: start an ACE inhibitor at a low dose with a goal blood pressure of less than 120/80 mm. Hg. �AVOID Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, and other kidney toxins �CAUTION with medications that can cause kidney toxicity ( Tenofovir, Gentamicin) �CHECK CREATININE every year through blood test
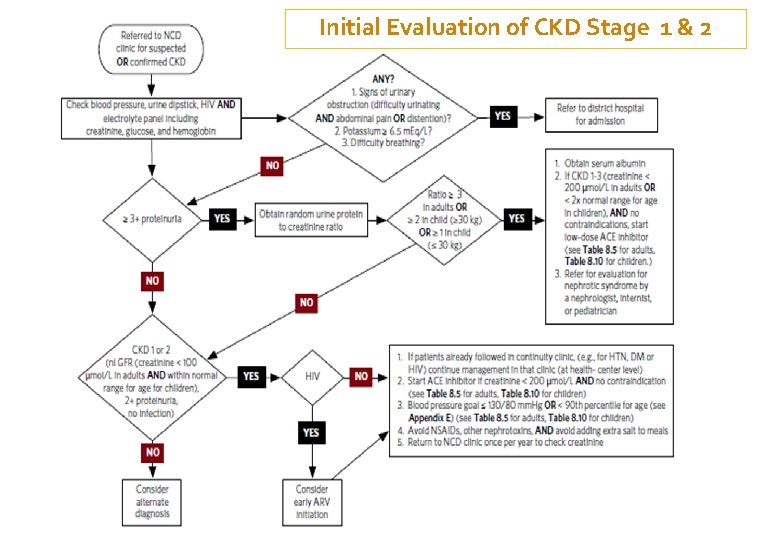
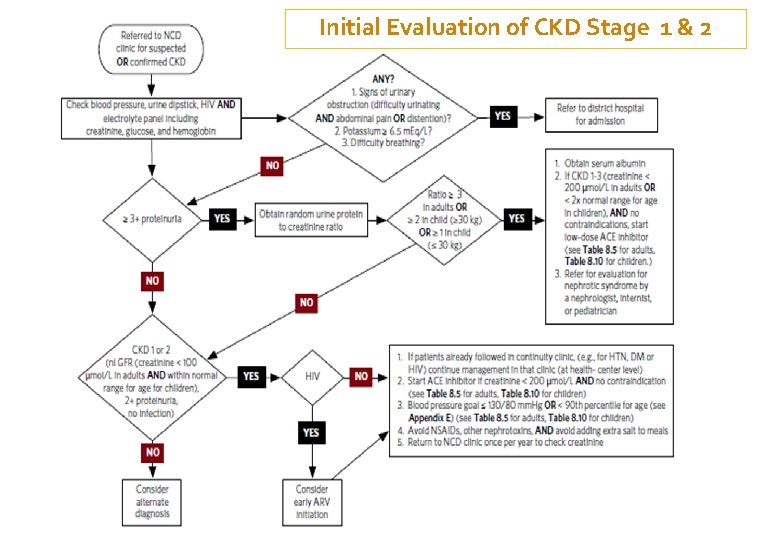
Initial Evaluation of CKD Stage 1 & 2
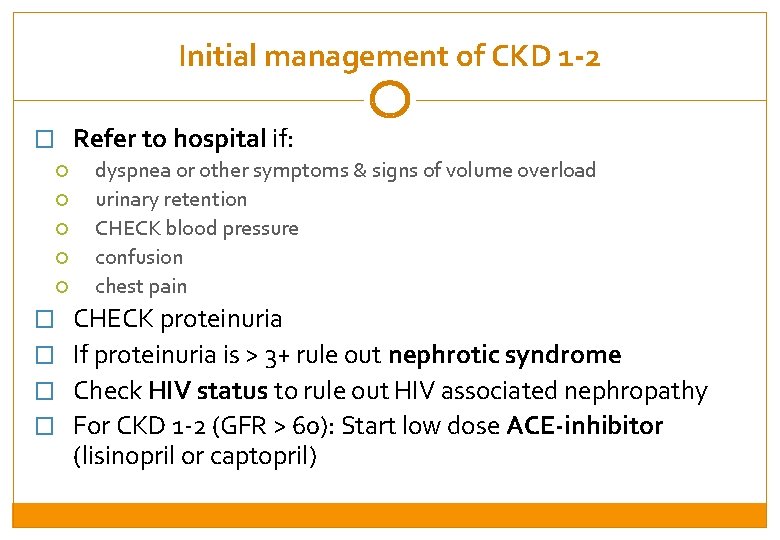
Initial management of CKD 1 -2 � Refer to hospital if: dyspnea or other symptoms & signs of volume overload urinary retention CHECK blood pressure confusion chest pain � CHECK proteinuria � If proteinuria is > 3+ rule out nephrotic syndrome � Check HIV status to rule out HIV associated nephropathy � For CKD 1 -2 (GFR > 60): Start low dose ACE-inhibitor (lisinopril or captopril)
Session 2: Management of CKD in adults By the end of this Session, participants will be able to: �Describe the initial management of CKD 1 and 2 �Describe the initial and ongoing management of CKD 3, 4, and 5
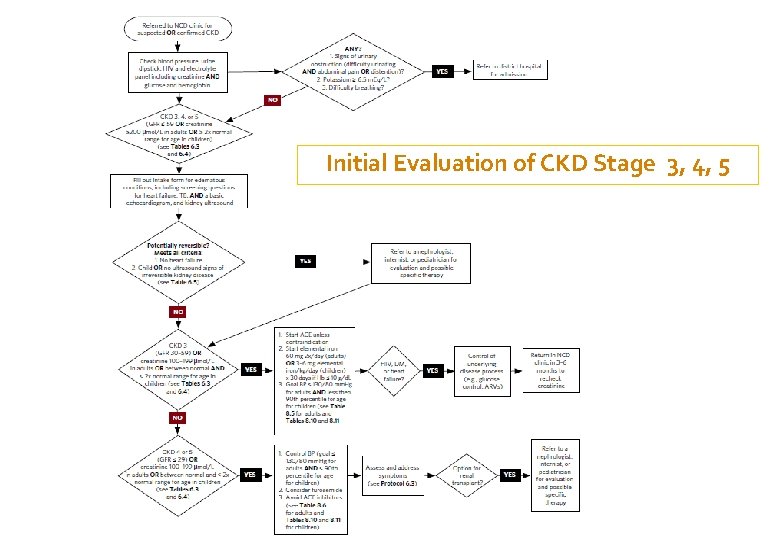
CKD Stage 3, 4, or 5 �Patients with moderate to severe CKD (CKD 3, 4, or 5) should be closely evaluated for reversible causes of their disease �Patients with CKD 3 (as well as with Stages 1 and 2) are usually asymptomatic and so are identified through screening because they have another disease (such as heart failure). �Patients with CKD 4 or 5 will often be symptomatic and initial evaluation will take place in the hospital.
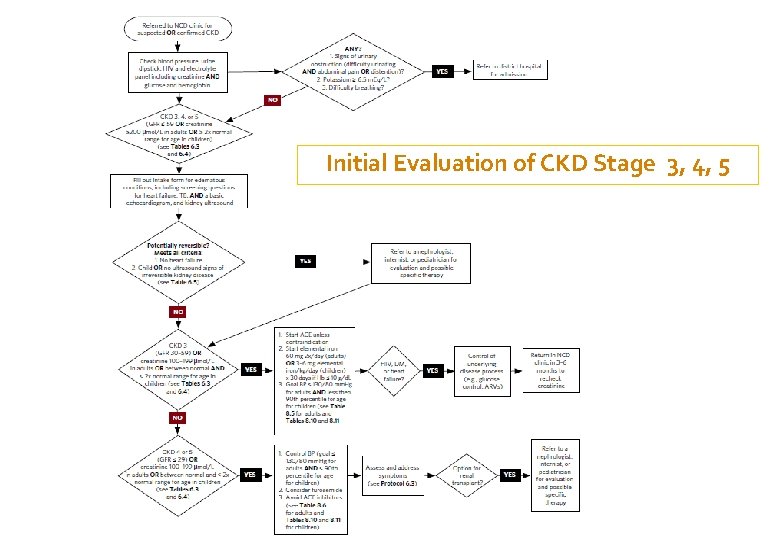
Initial Evaluation of CKD Stage 3, 4, 5
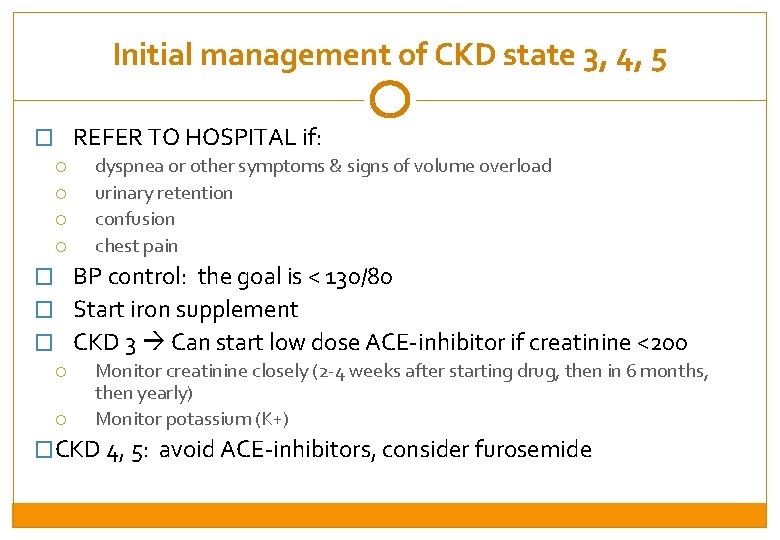
Initial management of CKD state 3, 4, 5 � REFER TO HOSPITAL if: dyspnea or other symptoms & signs of volume overload urinary retention confusion chest pain � BP control: the goal is < 130/80 � Start iron supplement � CKD 3 Can start low dose ACE-inhibitor if creatinine <200 Monitor creatinine closely (2 -4 weeks after starting drug, then in 6 months, then yearly) Monitor potassium (K+) �CKD 4, 5: avoid ACE-inhibitors, consider furosemide
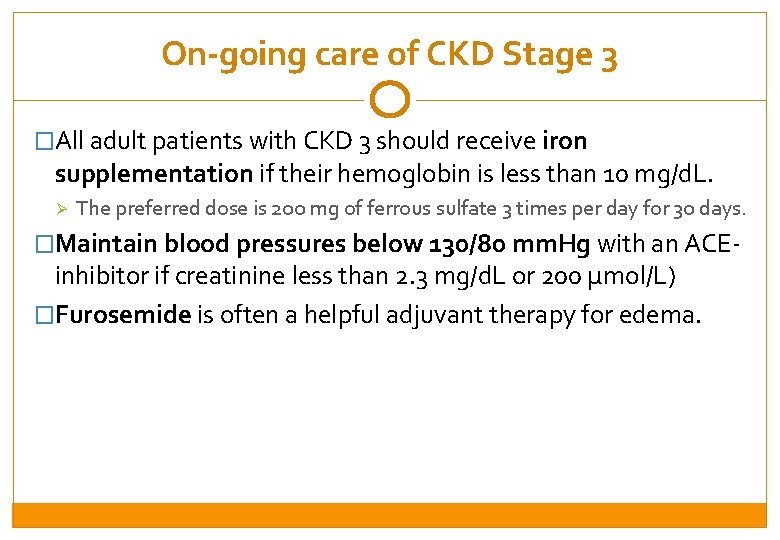
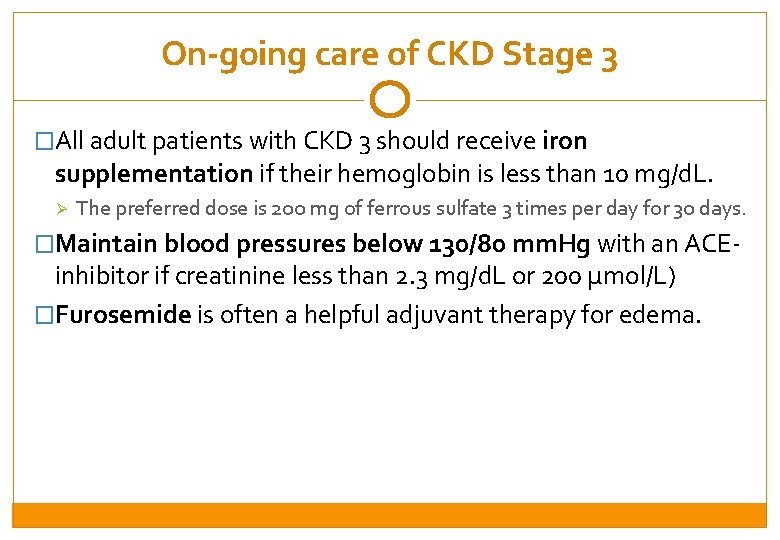
On-going care of CKD Stage 3 �All adult patients with CKD 3 should receive iron supplementation if their hemoglobin is less than 10 mg/d. L. Ø The preferred dose is 200 mg of ferrous sulfate 3 times per day for 30 days. �Maintain blood pressures below 130/80 mm. Hg with an ACE- inhibitor if creatinine less than 2. 3 mg/d. L or 200 µmol/L) �Furosemide is often a helpful adjuvant therapy for edema.
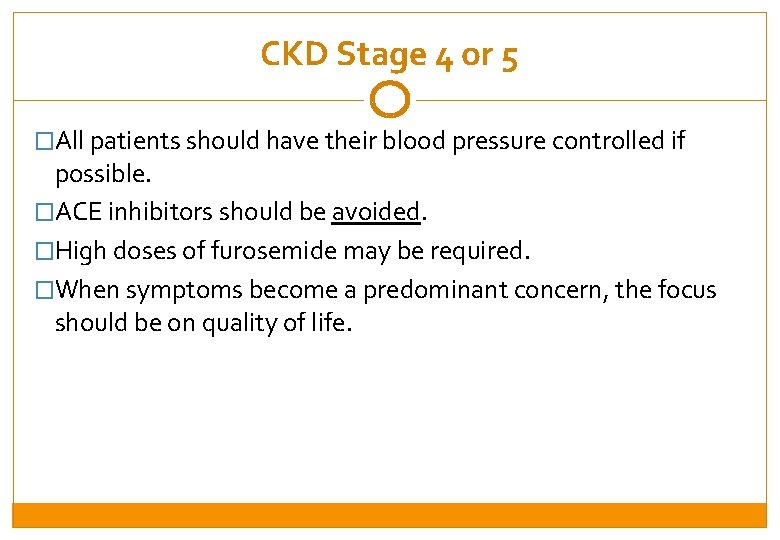
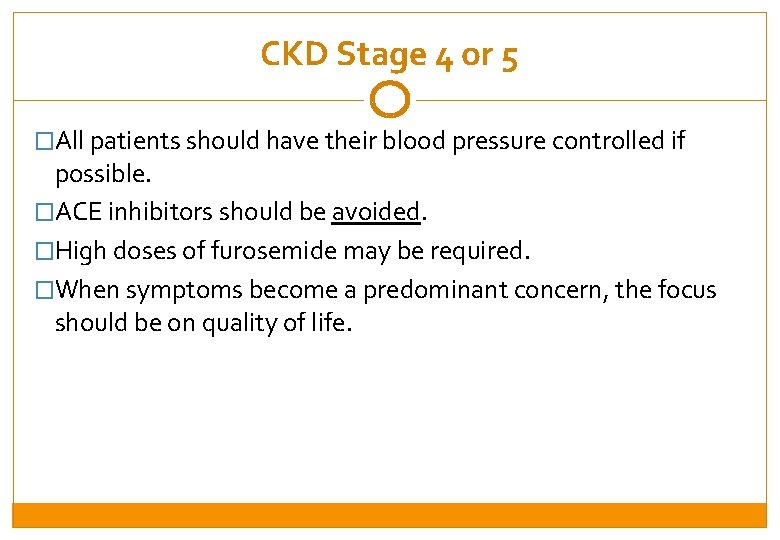
CKD Stage 4 or 5 �All patients should have their blood pressure controlled if possible. �ACE inhibitors should be avoided. �High doses of furosemide may be required. �When symptoms become a predominant concern, the focus should be on quality of life.
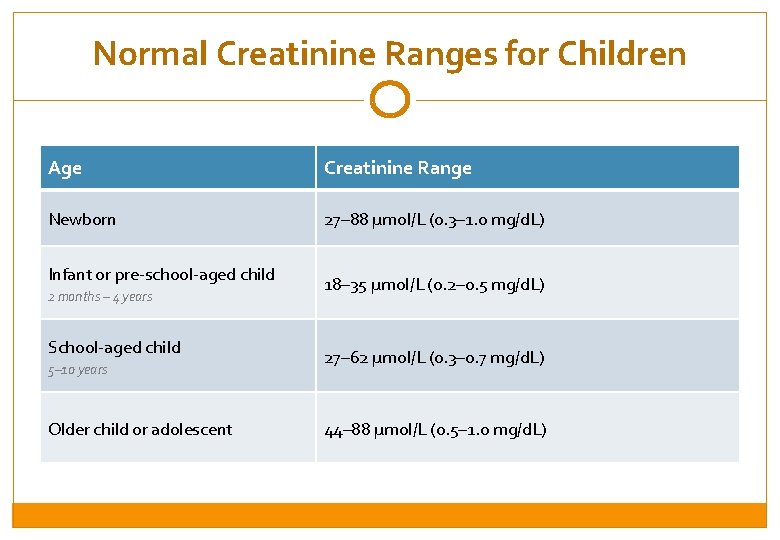
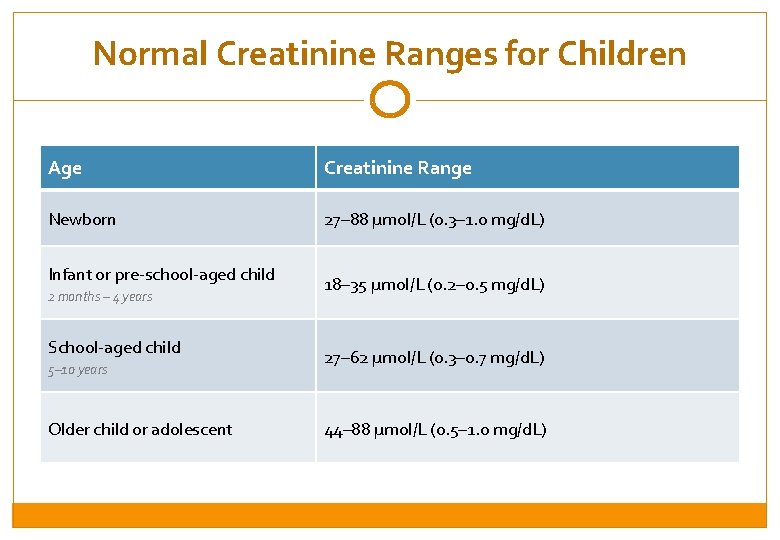
Normal Creatinine Ranges for Children Age Creatinine Range Newborn 27– 88 µmol/L (0. 3– 1. 0 mg/d. L) Infant or pre-school-aged child 2 months – 4 years School-aged child 5– 10 years Older child or adolescent 18– 35 µmol/L (0. 2– 0. 5 mg/d. L) 27– 62 µmol/L (0. 3– 0. 7 mg/d. L) 44– 88 µmol/L (0. 5– 1. 0 mg/d. L)
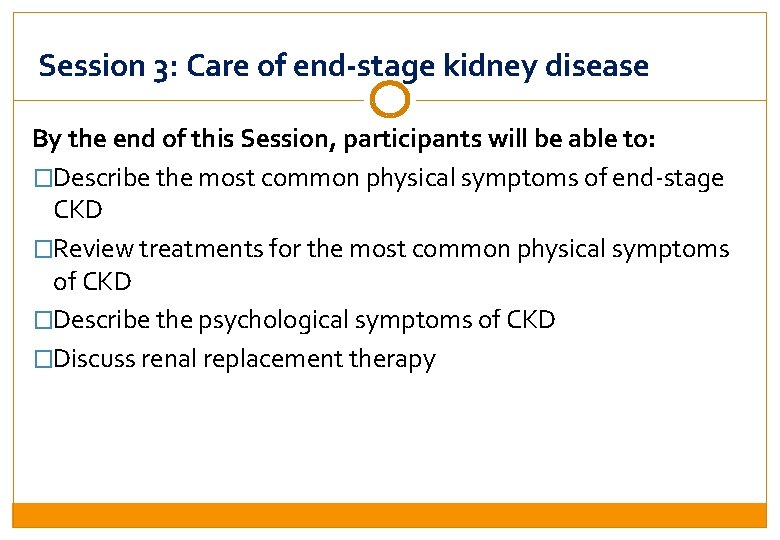
Session 3: Care of end-stage kidney disease By the end of this Session, participants will be able to: �Describe the most common physical symptoms of end-stage CKD �Review treatments for the most common physical symptoms of CKD �Describe the psychological symptoms of CKD �Discuss renal replacement therapy
Palliative Care �At any stage of CKD, pain, dyspnea, and other distressing symptoms may occur. Palliative and should be Role treated. Care Play: �Initiate conversations about goals of palliative care early and continue theparticipant discussion should include • The first willthroughout. play the role of. Conversations the nurse. The nurse discusses the information symptom as progresses, well as responses tothe symptomsabout that may develop ascontrol the disease and outlines Role Play Feedback palliative care responsesdistress. that are available. potential psychosocial �Explain to patients and families that in the later stages of CKD, • What did the nurse do will well? What could improve next 4 time? The second participant play the role ofthe thenurse patient with Stage CKD. many patients will have an increasing need for palliative care, • What are the next steps for the patient? are the next steps The patient is having pain and anxiety and is What concerned about what willfor including relief from physical symptoms and psychosocial distress. happen as the disease gets worse. the family member? �In the moments before death, patients will also suffer intractable • The and thirdvomiting, participant will play the role of a family member. The family nausea mental status changes, and seizures as a member all his/her time comforting the patient, but does not know result of thespends buildup of urea and other toxins. what else to do to help.
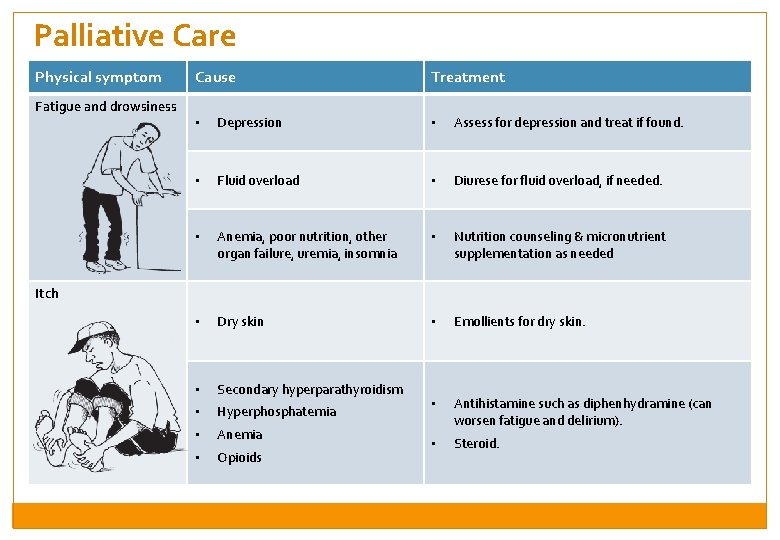
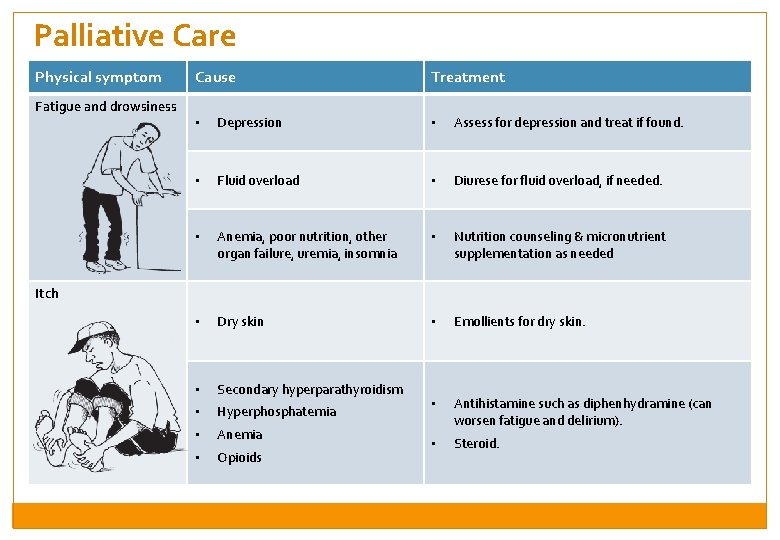
Palliative Care Physical symptom Fatigue and drowsiness Cause Treatment • Depression • Assess for depression and treat if found. • Fluid overload • Diurese for fluid overload, if needed. • Anemia, poor nutrition, other organ failure, uremia, insomnia • Nutrition counseling & micronutrient supplementation as needed • Dry skin • Emollients for dry skin. • Secondary hyperparathyroidism • Hyperphosphatemia • • Anemia Antihistamine such as diphenhydramine (can worsen fatigue and delirium). • Opioids • Steroid. Itch
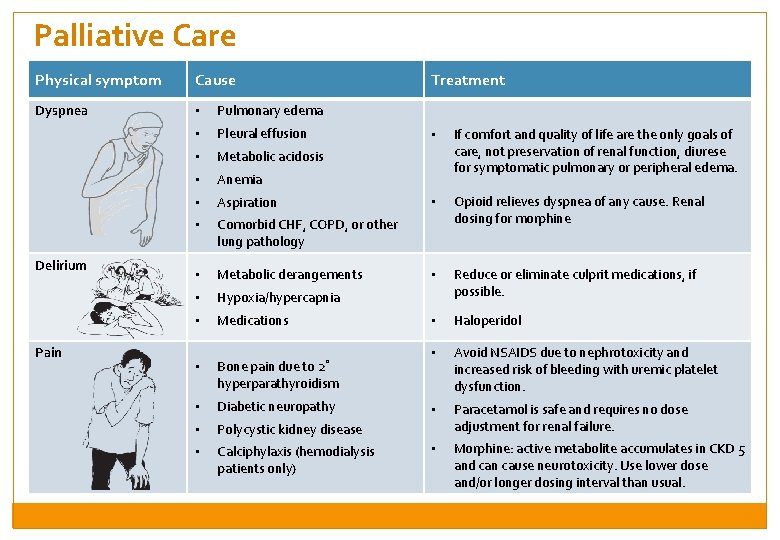
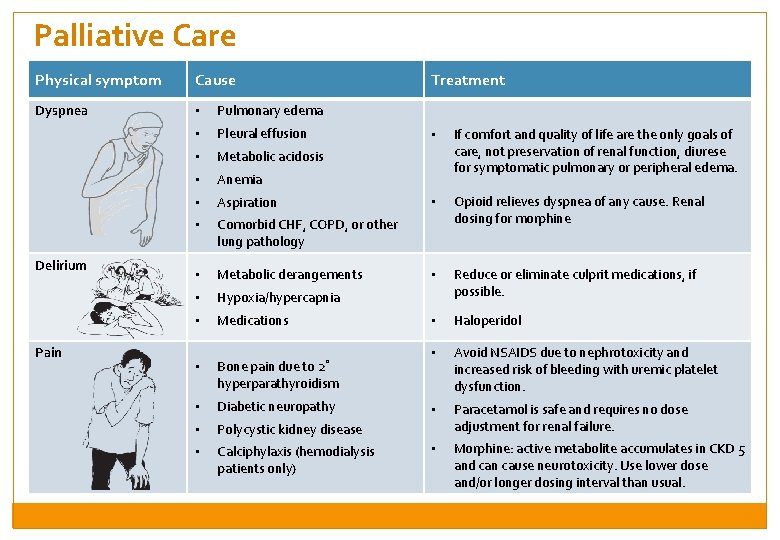
Palliative Care Physical symptom Cause Dyspnea • Pulmonary edema • Pleural effusion • Metabolic acidosis • Anemia • Aspiration • Comorbid CHF, COPD, or other lung pathology • Metabolic derangements • Hypoxia/hypercapnia • Medications • Bone pain due to 2˚ hyperparathyroidism • Diabetic neuropathy • Polycystic kidney disease • Calciphylaxis (hemodialysis patients only) Delirium Pain Treatment • If comfort and quality of life are the only goals of care, not preservation of renal function, diurese for symptomatic pulmonary or peripheral edema. • Opioid relieves dyspnea of any cause. Renal dosing for morphine • Reduce or eliminate culprit medications, if possible. • Haloperidol • Avoid NSAIDS due to nephrotoxicity and increased risk of bleeding with uremic platelet dysfunction. • Paracetamol is safe and requires no dose adjustment for renal failure. • Morphine: active metabolite accumulates in CKD 5 and can cause neurotoxicity. Use lower dose and/or longer dosing interval than usual.
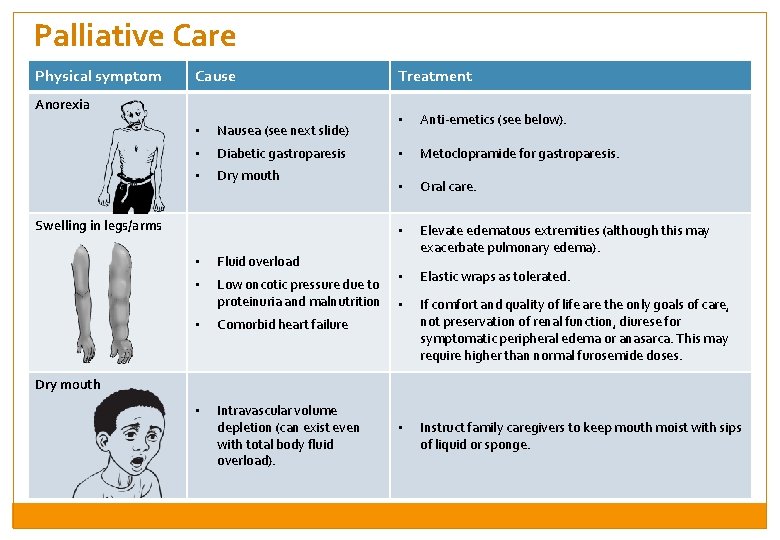
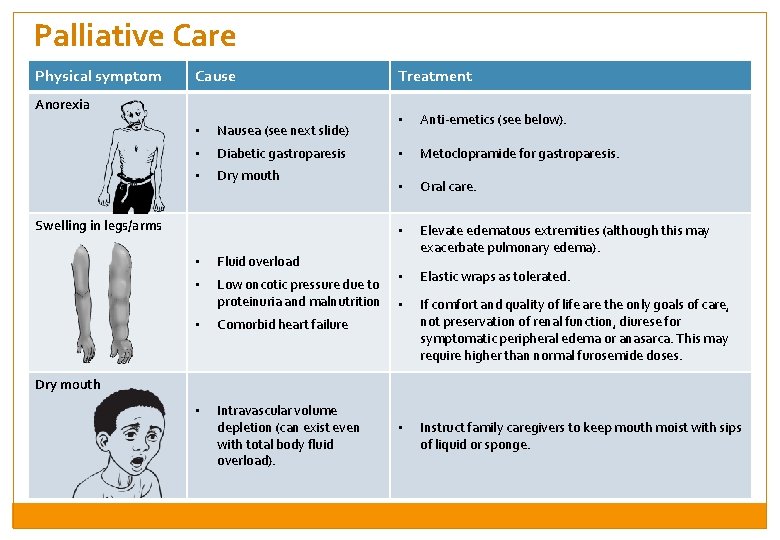
Palliative Care Physical symptom Cause Anorexia • Nausea (see next slide) • Diabetic gastroparesis • Dry mouth Swelling in legs/arms • Fluid overload • Low oncotic pressure due to proteinuria and malnutrition • Comorbid heart failure • Intravascular volume depletion (can exist even with total body fluid overload). Treatment • Anti-emetics (see below). • Metoclopramide for gastroparesis. • Oral care. • Elevate edematous extremities (although this may exacerbate pulmonary edema). • Elastic wraps as tolerated. • If comfort and quality of life are the only goals of care, not preservation of renal function, diurese for symptomatic peripheral edema or anasarca. This may require higher than normal furosemide doses. • Instruct family caregivers to keep mouth moist with sips of liquid or sponge. Dry mouth
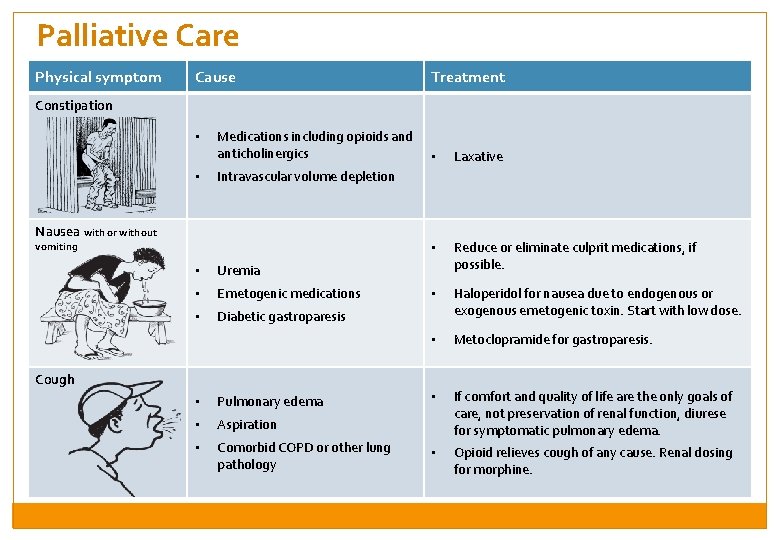
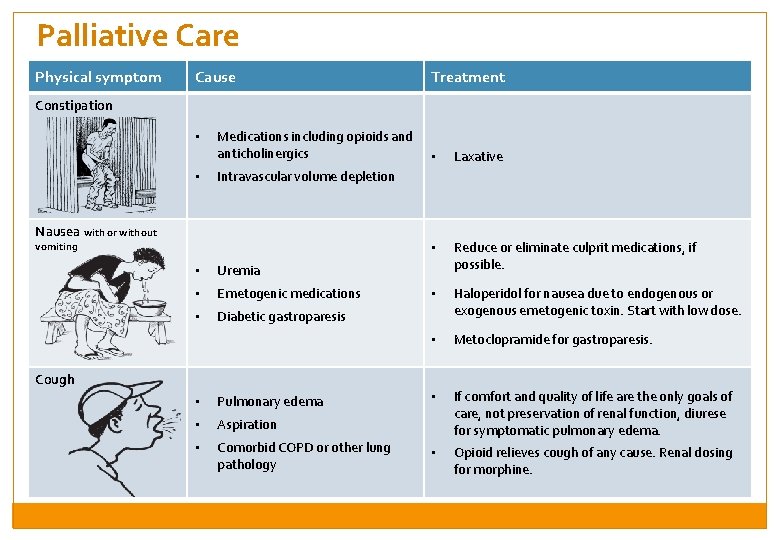
Palliative Care Physical symptom Cause Treatment Constipation • • Medications including opioids and anticholinergics • Laxative • Reduce or eliminate culprit medications, if possible. • Haloperidol for nausea due to endogenous or exogenous emetogenic toxin. Start with low dose. • Metoclopramide for gastroparesis. • If comfort and quality of life are the only goals of care, not preservation of renal function, diurese for symptomatic pulmonary edema. • Opioid relieves cough of any cause. Renal dosing for morphine. Intravascular volume depletion Nausea with or without vomiting • Uremia • Emetogenic medications • Diabetic gastroparesis Cough • Pulmonary edema • Aspiration • Comorbid COPD or other lung pathology
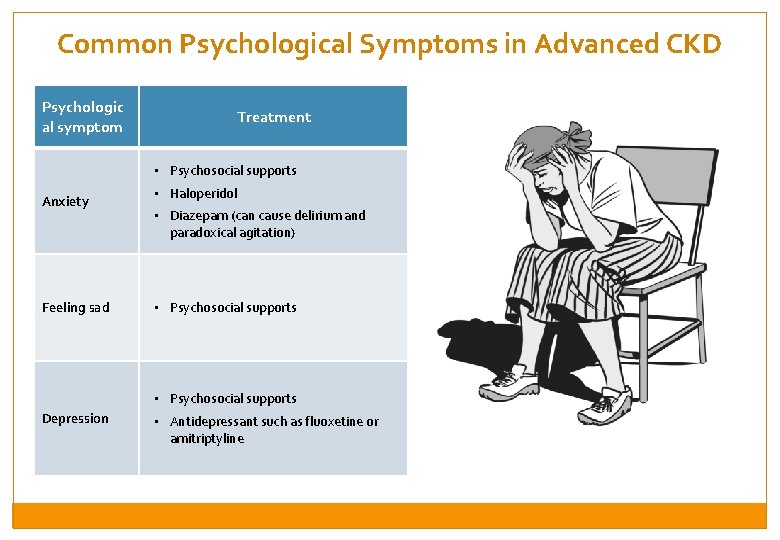
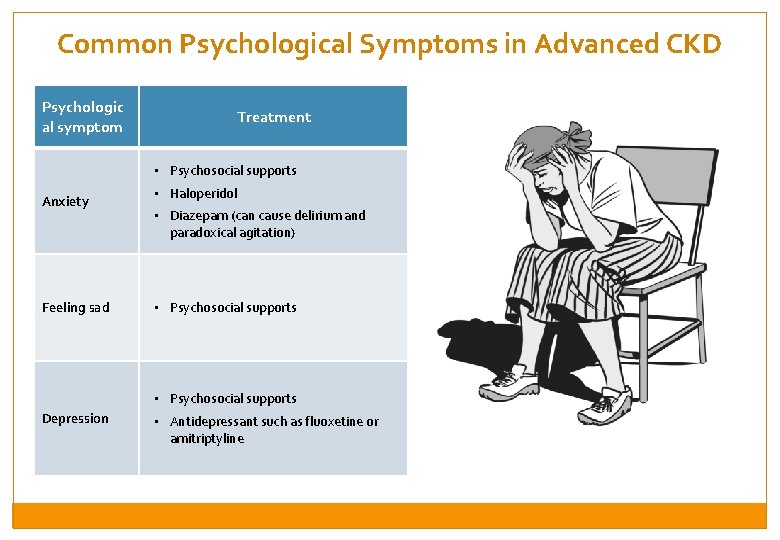
Common Psychological Symptoms in Advanced CKD Psychologic al symptom Treatment • Psychosocial supports Anxiety Feeling sad • Haloperidol • Diazepam (can cause delirium and paradoxical agitation) • Psychosocial supports Depression • Antidepressant such as fluoxetine or amitriptyline
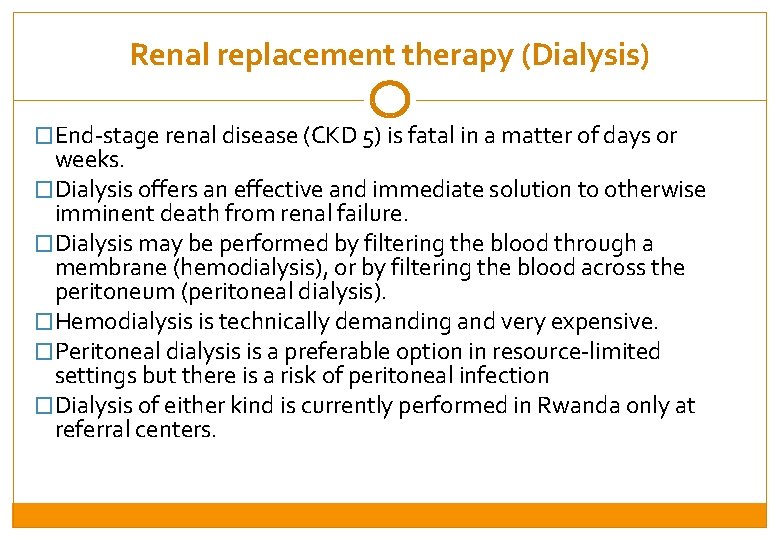
Renal replacement therapy (Dialysis) �End-stage renal disease (CKD 5) is fatal in a matter of days or weeks. �Dialysis offers an effective and immediate solution to otherwise imminent death from renal failure. �Dialysis may be performed by filtering the blood through a membrane (hemodialysis), or by filtering the blood across the peritoneum (peritoneal dialysis). �Hemodialysis is technically demanding and very expensive. �Peritoneal dialysis is a preferable option in resource-limited settings but there is a risk of peritoneal infection �Dialysis of either kind is currently performed in Rwanda only at referral centers.
Case Study 1 � 25 year old man complains of rapid weight gain and edema in his legs. What are the next steps in making the diagnosis? Urine dipstick for protein and creatinine (it is important to do both in order to stage the disease). If proteinuria is 2+ and the creatinine is elevated, refer for renal ultrasound. Also, check blood glucose, HIV status, and blood pressure. �What medications should he be started on? ACE inhibitor if creatinine <200, lasix for edema. May start other blood pressure medications if the BP is elevated. Consider starting ferrous sulfate if anemic.
Case Study 2 28 year old woman with CKD stage 4 presents to NCD clinic for a follow up visit. Her blood pressure is 15/9 and creatinine is 600 µmol/L. � What medications should she be started on? Lasix, perhaps doses as high as 200 mg BD Nifedipine, hydralazine, isosorbide, atenolol, or other medications to control BP to < 13/8. � What medications should be avoided? ACE inhibitors because of the elevated creatinine NSAIDS, and any nephrotoxic medications like gentamicin � What symptoms may she have at CKD stage 4 or 5 and what are some treatments? Nausea, vomiting: treat with metoclopramide Drowsiness, fatigue: assess for depression and treat with anafranil Dyspnea: increase lasix dose for comfort if necessary Itching: diphenhydramine, promethazine, or chlorpheniramine
Key Points Common causes of renal failure include HTN, HIV, DM, and infection. All patients with HTN, HIV, DM should be screened for renal failure by checking proteinuria. Patients with 3+ or 4+ proteinuria should be evaluated at the district hospital for nephrotic syndrome. Renal failure may be asymptomatic in early stages. In later stages, symptoms may include dyspnea, nausea/vomiting, edema/body swelling, abdominal distention/ascites. In patients with CKD, nephrotoxic medications should be avoided (NSAIDS, gentamicin and tenofovir). In all patients with CKD, BP, proteinuria and HIV status should be checked. Management of CKD includes BP control, iron supplement, diuretics if volume overloaded. In end-stage kidney disease, treatment should focus on palliation and psychosocial support.
Thank you for your hard work and dedication to health and human rights! Matilda Nikolasi talks with PIH clinician Joe Lusaka and was the first of many to be served during the new Dambe Health Center’s first day on April 25, 2016 in Malawi. She was screened for Hypertension, HIV and Diabetes during this visit through the SHARF (Screening for health and referrals at the facilities) initiative. (Photo by Nandi Bwanali / Partners In Health)
 Ersd
Ersd Nih score
Nih score Low potassium diet nemo
Low potassium diet nemo Sighns of kidney disease
Sighns of kidney disease Resonium por
Resonium por Albumin kidney disease
Albumin kidney disease Albumin kidney disease
Albumin kidney disease Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Chronic granulomatous disease
Chronic granulomatous disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Jewish chronic disease hospital
Jewish chronic disease hospital Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Developed by ed
Developed by ed Chronic disease
Chronic disease Stages of cirrosis
Stages of cirrosis Chronic disease
Chronic disease Copd means
Copd means Chronic rheumatic heart disease
Chronic rheumatic heart disease Communicable disease and non communicable disease
Communicable disease and non communicable disease Flinders model of chronic care self-management
Flinders model of chronic care self-management Bristol health partners
Bristol health partners Health partners
Health partners Po box 1220 philadelphia pa 19105 provider phone number
Po box 1220 philadelphia pa 19105 provider phone number Fmh rosehill radiology
Fmh rosehill radiology Classicism is health romanticism is disease
Classicism is health romanticism is disease Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Health promotion and levels of disease prevention
Health promotion and levels of disease prevention The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key Concepts of health and disease
Concepts of health and disease Introduction to community medicine
Introduction to community medicine The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key Adenomalacia is the abnormal hardening of a gland.
Adenomalacia is the abnormal hardening of a gland. Conclusion of national mental health programme
Conclusion of national mental health programme Conclusion of national mental health programme
Conclusion of national mental health programme